
How Affordable Care Act Repeal and Replace Plans Might
Shift Health Insurance Tax Credits
Cynthia Cox, Gary Claxton, Larry Levitt
An important part of the repeal and replacement discussions around the Affordable Care Act (ACA) will involve
the type and amount of subsidies that people get to help them afford health insurance. This is particularly
important for lower and moderate income individuals who do not have access to coverage at work and must
purchase coverage directly.
The ACA provides three types of financial assistance to help people afford health coverage: Medicaid expansion
for those with incomes below 138% of poverty (the Supreme Court later ruled this to be at state option);
refundable premium tax credits for people with incomes from 100% to 400% of the poverty level who purchase
coverage through federal or state marketplaces; cost-sharing subsidies for people with incomes from 100% to
250% of poverty to provide lower deductibles and copays when purchasing silver plans in a marketplace.
This analysis focuses on alternative ways to provide premium assistance for people purchasing individual
market coverage, explaining how they work, providing examples of how they’re calculated, and presenting
estimates of how assistance overall would change for current ACA marketplace enrollees. Issues relating to
changing Medicaid or methods of subsidizing cost-sharing will be addressed in other analyses.
The ACA and leading replacement proposals rely on refundable tax credits to help individual market enrollees
pay for premiums, although the credit amounts are set quite differently. The House Leadership proposal
released on March 6, the American Health Care Act, proposes refundable tax credits which vary with age (with
a phase-out for high-income enrollees) and grow annually with inflation. The tax credits under the ACA vary
with family income and the cost of insurance where people live, as well as age, and grow annually if premiums
increase.
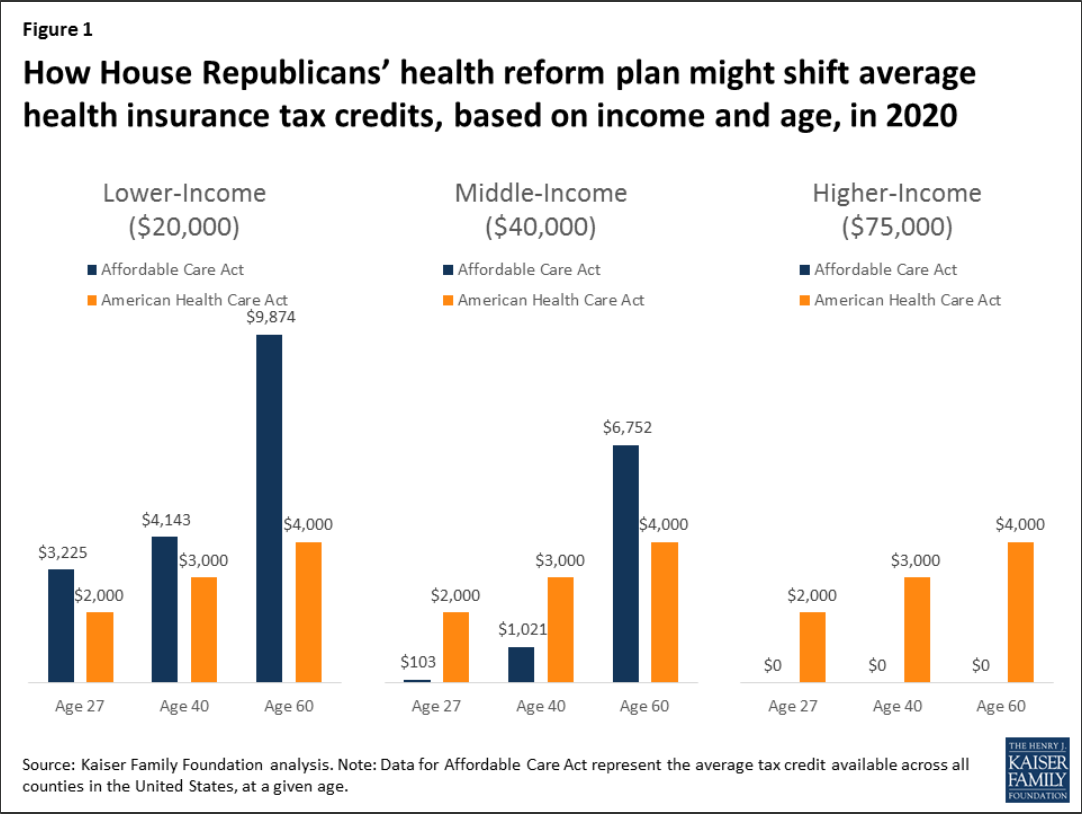
These various tax credit approaches can have quite different implications for different groups of individual
market purchasers. For example, the tax credits under the ACA are higher for people with lower incomes than
for people with higher incomes, and no credit is provided for individuals with incomes over 400% of poverty.
The current replacement proposal, in contrast, is flat for incomes up to $75,000 for an individual and
$150,000 for a married couple, and so would provide relatively more assistance to people with upper-middle
incomes. Similarly, the ACA tax credits are relatively higher in areas with higher premiums (like many rural
areas), while the replacement proposal credits do not vary by location. If premiums grow more rapidly than

How Affordable Care Act Repeal and Replace Plans Might Shift Health Insurance Tax Credits 2
inflation over time (which they generally have), the replacement proposal tax credits will grow more slowly
than those provided under the ACA.
What is a Tax Credit, and How is it Different from a Deduction?
A tax credit is an amount by which a taxpayer can reduce the amount they owe in federal income tax; for
example, if a person had a federal tax bill of $2,500 and a tax credit of $1,000, their tax liability would be
reduced to $1,500. A refundable tax credit means that if the amount of the tax credit is greater than the
amount of taxes owed, the taxpayer receives a refund of the difference; for example, if a person had a
federal tax bill of $1000 and a tax credit of $1,500, they would receive a refund of $500. Making the
credit refundable is important if a goal is to assist lower-income families, many of whom may not owe
federal income tax. An advanceable tax credit is made available at the time a premium payment is owed
(which similarly benefits lower-income families so that they can receive the financial assistance upfront).
The ACA and a number of replacement proposals allow for advance payment of credits.
A tax credit is different from a tax deduction. A deduction reduces the amount of income that is taxed,
while a credit reduces the amount of tax itself. For example, if a person has taxable income of $30,000, a
$500 deduction reduces the amount of taxable income to $29,500. If the person’s marginal tax rate is
15%, the deduction reduces the person’s taxes by 15% of $500, or $75. Because people with lower incomes
have lower marginal tax rates than people with higher incomes – and, typically don’t itemize their
deductions – tax credits are generally more beneficial to lower income people than deductions.
The next section describes the differing tax credit approaches in more detail and draws out some of the
implications for different types of purchasers.
The ACA provides tax credits for individuals with family incomes from 100% to 400% of poverty ($11,880 to
$47,520 for a single individual in 2017) if they are not eligible for employer-provided or public coverage and if
they purchase individual market coverage in the federal or a state marketplace. The tax credit amounts are
calculated based on the family income of eligible individuals and the cost of coverage in the area where the live.
More specifically, the ACA tax credit for an eligible individual is the difference between a specified percentage
of his or her income (Table 1) and the premium of the second-lowest-cost silver plan (referred to as the
benchmark premium) available in the area in which they live. There is no tax credit available if the benchmark
premium is less than the specified percentage of income (which can occur for younger purchasers with
relatively higher incomes) or if family income falls outside of the 100% to 400% of poverty range. For families,
the premiums for family members are added together (including up to 3 children) and compared to specified
income percentages. ACA tax credits are made available in advance, based on income information provided to
the marketplace, and reconciled based on actual income when a person files income taxes the following.

How Affordable Care Act Repeal and Replace Plans Might Shift Health Insurance Tax Credits 3
Take, for example, a person age 40 with income
of $30,000, which is 253% of poverty. At this
income, the person’s specified percentage of
income is 8.28% in 2017, which means that the
person receives a tax credit if he or she has to pay
more than 8.28% of income (or $2,485 annually)
for the second-lowest-cost silver premium where
he or she lives. If we assume a premium of
$4,328 (the national average benchmark
premium for a person age 40 in 2017), the
person’s tax credit would be the difference
between the benchmark premium and the
specified percentage of income, or $4,328 -
$2,485 = $1,843 (or $154 per month).
The American Health Care Act takes a simpler approach and specifies the actual dollar amounts for a new
refundable tax credit that could be used to purchase individual market coverage. The amounts vary only with
age up until an income of $75,000 for a single individual, at which point they begin to phase out. Tax credits
range from $2,000 for people under age 30, to $2,500 for people ages 30 to 39, $3,000 for people age 40 to
49, $3,500 for people age 50 to 59, and $4,000 for people age 60 and over starting in 2020. Eligibility for the
tax credit phases out starting at income above $75,000 for single individuals (the credit is reduced, but not
below zero, by 10 cents for every dollar of income above this threshold, reaching zero at an income of $95,000
for single individuals up to age 29 or $115,000 for individuals age 60 and older). For joint filers, credits begin
to phase out at an income of $150,000 (the tax credit is reduced to zero at an income of $190,000 for couples
up to age 29; it is reduced to zero at income $230,000 for couples age 60 or older; and it is reduced to zero at
income of $290,000 for couples claiming the maximum family credit amount). People who sign up for public
programs such as Medicare, Medicaid, public employee health benefit programs, would not be eligible for a tax
credit. The proposal further limits eligibility for tax credits to people who do not have an offer available for
employer-provided health benefits.
Table 2 shows how projected ACA tax credits in 2020 compare to what would be provided under the American
Health Care Act for people at various incomes, ages, and geographic areas. To show the ACA amounts in 2020,
we inflated all 2017 premiums based on projections for direct purchase spending per enrollee from the
National Health Expenditure Accounts. This method applies the same premium growth across all ages and
geographic locations. Note that the table does not include cost-sharing assistance under the ACA that lowers
deductibles and copayments for low-income marketplace enrollees. For example, in 2016, people making
between 100 – 150% of poverty enrolled in a silver plan on healthcare.gov received cost-sharing assistance
worth $1,440; those with incomes between 150 – 200% of poverty received $1,068 on average; and those with
incomes between 200 – 250% of poverty received $144 on average.
Income
% Poverty
Premium Cap
(maximum % of income one must pay for
second-lowest silver plan available to in
their area)
Under 100%
No Cap
100% – 133%
2.04%
133% – 150%
3.06% – 4.08%
150% – 200%
4.08% – 6.43%
200% – 250%
6.43% – 8.21%
250% – 300%
8.21% – 9.69%
300% – 400%
9.69%
Over 400%
No Cap
Source: Kaiser Family Foundation

How Affordable Care Act Repeal and Replace Plans Might Shift Health Insurance Tax Credits 4
Income
(2020 FPL)
Age
Reno,
NV
Mobile,
AL
Reno,
NV
Mobile, AL
(160% FPL)
27
$2,899
$3,225
$4,522
$2,000
$2,000
$2,000
$3,745
$5,725
$3,000
$3,000
60
$9,030
$9,874
$13,235
$4,000
$4,000
$4,000
(320% FPL)
27
$0
$103
$1,400
$2,000
$2,000
$2,000
$623
$2,603
$3,000
$3,000
60
$5,908
$6,752
$10,113
$4,000
$4,000
$4,000
(600% FPL)
27
$0
$0
$0
$2,000
$2,000
$2,000
$0
$0
$3,000
$3,000
60
$0
$0
$0
$4,000
$4,000
$4,000
(800% FPL)
27
$0
$0
$0
$0
$0
$0
$0
$0
$500
$500
60
$0
$0
$0
$1,500
$1,500
$1,500
Source: Kaiser Family Foundation analysis.
Notes: In the 2017 ACA exchange markets, premiums in Reno, NV and Mobile, AL are
approximately representative of the 25th and 75th percentile, respectively. 2017 ACA
premiums were increased according to National Health Expenditure projections for direct
purchase. Under the ACA, people with incomes below 250% of the poverty level receive
additional financial assistance for cost-sharing (not shown above).
Under the ACA in 2020, we project that a typical 40-year-old making $20,000 per year would be eligible for
$4,143 in premium tax credits (not including the additional cost-sharing subsidies to lower his or her
deductibles and copayments), while under the American Health Care Act, this person would be eligible $3,000.
For context, we project that the average ACA premium for a 40-year-old in 2020 would be $5,101 annually
(meaning the tax credit in the ACA would cover 81% of the total premium) for a benchmark silver plan with
comprehensive benefits and reduced cost-sharing. A $3,000 tax credit for this same individual under the
American Health Care Act would represent 59% of the average 40-year-old benchmark silver premium under
the ACA.
Generally, the ACA has higher tax credit amounts than the replacement plan for lower-income people –
especially for those who are older and live in higher-cost areas – and lower credits for those with higher
incomes. Unlike the ACA, the replacement plan provides tax credits to people over 400% percent of the poverty
level (phasing out around 900% of poverty for a single person), as well as to people current buying individual
market coverage outside of the marketplaces (not included in this analysis).
While replacement plan tax credits vary by age – by a factor of 2 to 1 for older adults relative to younger ones –
the variation is substantially less than under the ACA. The big differences in ACA tax credits at different ages is
due to the fact that premiums for older adults can be three times the level of premiums for younger adults
under the ACA, but all people at a given income level are expected to pay the same percentage of their income
towards a benchmark plan. The tax credit fills in the difference, and this amount is much higher for older
adults. These differences by age would be even further magnified under the American Health Care Act (which
permits premiums to vary by a factor of 5 to 1 due to age). Before the ACA, premiums for older adults were
typically four or five times the premiums charged to younger adults.
How Affordable Care Act Repeal and Replace Plans Might Shift Health Insurance Tax Credits 5
The tax credits in the ACA vary significantly with premium costs in an area (see Table 2 and Figure 2). At a
given income level and age, people receive bigger tax credits in a higher premium area like Mobile, Alabama
and smaller tax credits in a lower premium area like Reno, Nevada. Under the ACA in 2017, premiums in
Mobile, Alabama and Reno, Nevada approximately represent the 75
th
and 25
th
percentile, respectively.

How Affordable Care Act Repeal and Replace Plans Might Shift Health Insurance Tax Credits 6
The disparities between the ACA tax credits and those in the American Health Care Act will therefore vary
noticeably across the country. For more on geographic differences between the ACA and the replacement plan,
see Tax Credits under the Affordable Care Act vs. the American Health Care Act: An Interactive Map.

How Affordable Care Act Repeal and Replace Plans Might Shift Health Insurance Tax Credits 7
The same general pattern can be seen for families as individuals, with lower-income families – and particularly
lower-income families in higher-cost areas – receiving larger tax credits under the ACA, while middle-income
families in lower-cost areas would receive larger tax credits under the American Health Care Act (Figure 3).
Figure 4 below shows how tax credits under the ACA differ from those in the American Health Care Act for a
couple in their 60’s with no children. In this scenario, because premiums for older adults are higher and the
ACA ties tax credits to the cost of premiums, a 60-year-old couple would receive larger tax credits under the
ACA than the American Health Care Act at lower and middle incomes, but would receive a larger tax credit
under the American Health Care Act at higher incomes.

How Affordable Care Act Repeal and Replace Plans Might Shift Health Insurance Tax Credits 8
We estimated the average tax credits that current ACA marketplace enrollees are receiving under the ACA and
what they would qualify for if the American Health Care Act were in place.
$4,615
$2,957
-36%
$5,342
$3,160
-41%
$6,648
$3,729
-44%
Source: Kaiser Family Foundation analysis of data from Healthcare.gov, state-based
exchanges, and Congressional Budget Office. Note: Amounts above represent the average tax
credit received based on the age distribution of current Marketplace enrollees.

How Affordable Care Act Repeal and Replace Plans Might Shift Health Insurance Tax Credits 9
The average estimated tax credit received by ACA marketplace enrollees in 2017 is $3,617 on an annual basis,
and that this amount will rise to $4,615 by 2020 based on projected growth rates from the Congressional
Budget Office. This includes the 81% who receive premium subsidies as well as the 19% who do not.
We estimate – based on the age distribution of marketplace enrollees – that current enrollees would receive an
average tax credit under the American Health Care Act of $2,957 in 2020, or 36% less than under the ACA (see
Table 3 and Figure 3). While many people would receive lower tax credits under the Affordable Health Care
Act, some would receive more assistance, notably the 19% of current marketplace enrollees who do not qualify
for ACA subsidies.
While ACA tax credits grow as premiums increase over time, the tax credits in the American Health Care Act
are indexed to inflation plus 1 percentage point. Based on CBO’s projections of ACA tax credit increases and
inflation, the disparity between the average credits under the ACA and the two replacement plans would widen
over time. The average tax credit current marketplace enrollees would receive under the American Health Care
Act would be 41% lower than under the ACA in 2022 and 44% lower in 2027.

How Affordable Care Act Repeal and Replace Plans Might Shift Health Insurance Tax Credits 10
Like the ACA itself, the American Health Care Act includes refundable tax credits to help make premiums more
affordable for people buying their own insurance. This might seem like an area where a replacement plan could
preserve a key element of the ACA. However, the tax credits are, in fact, structured quite differently, with
important implications for affordability and which groups may be winners or losers if the ACA is repealed and
replaced.
For current marketplace enrollees, the American Health Care Act would provide substantially lower tax credits
overall than the ACA on average. People who are lower income, older, or live in high premium areas would be
particularly disadvantaged under the American Health Care Act. People with incomes over 400% of the poverty
level – including those buying individual market insurance outside of the marketplaces – do not get any
financial assistance under the ACA but many would receive tax credits under the replacement proposal.
The underlying details of health reform proposals, such as the size and structure of health insurance tax
credits, matter crucially in determining who benefits and who is disadvantaged.

The Henry J. Kaiser Family Foundation Headquarters: 2400 Sand Hill Road, Menlo Park, CA 94025 | Phone 650-854-9400
Washington Offices and Barbara Jordan Conference Center: 1330 G Street, NW, Washington, DC 20005 | Phone 202-347-5270
www.kff.org | Email Alerts: kff.org/email | facebook.com/KaiserFamilyFoundation | twitter.com/KaiserFamFound
Filling the need for trusted information on national health issues, the Kaiser Family Foundation is a nonprofit organization based in Menlo Park, California.
We compare estimated tax credit amounts for the year 2020 because that is the first year credits are available
under the American Health Care Act. To inflate ACA tax credits, we started by inflating unsubsidized premiums
across all ages and geographies according to the National Health Expenditure (NHE) projections for growth in
direct purchase insurance spending per enrollee, then inflated poverty guidelines using CPI projections from
the Congressional Budget Office (CBO), and required premium contributions using the ratio of growth in
employer-sponsored insurance spending per enrollee and GDP per capita (from NHE).
To compare the average tax credit received by current marketplace enrollees (in Table 3 and Figure 3) under
the ACA, we estimated the average 2017 tax credit across all states (in state-based exchanges, we based this on
premium growth in those states, adjusted for differences in how fast tax credits grow relative to premiums)
then adjusted for the share of Marketplace enrollees receiving a tax credit and inflated it based on CBO
projections for average tax credits. For the American Health Care Act, average tax credits were weighted based
on the age distribution of current marketplace enrollees and then indexed based on CPI + 1%. Although tax
credits phase out for high-income enrollees in the AHCA, we assume that very few current marketplace
enrollees have incomes high enough for the tax credit to phase out, and thus do not take this into account in
calculating the average tax credit under the AHCA for current marketplace enrollees.
