
U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES
Substance Abuse and Mental Health Services Administration
Report to Congress on the Nation’s
Substance Abuse and Mental Health Workforce Issues
January 24, 2013
__________________________
Pamela S. Hyde, J.D.
Administrator
Table of Contents
Executive Summary ........................................................................................................................ 1
Introduction to Report ..................................................................................................................... 2
Background ..................................................................................................................................... 4
Changing Landscape: Impact on the Workforce ........................................................................... 5
Demographic Information ............................................................................................................... 7
Workforce Conditions ..................................................................................................................... 9
High Turnover ............................................................................................................................. 9
Worker Shortages ...................................................................................................................... 10
Aging Workforce....................................................................................................................... 11
Perceptions about Behavioral Health Conditions and Those with Lived Experience............... 11
Inadequate Compensation ......................................................................................................... 12
Compensation for Specialty Behavioral Health Providers ........................................................ 15
Data on Recruitment, Retention and Distribution ..................................................................... 15
Special Issues of the Prevention Workforce ............................................................................. 17
Impact of Affordable Care Act and MHPAEA on the Behavioral Health Workforce ............. 18
Enumeration of Needs................................................................................................................... 19
SAMHSA and HRSA Workforce Initiatives ................................................................................ 21
SAMHSA Workforce Programs................................................................................................ 21
HRSA Behavioral Health Workforce Programs ....................................................................... 39
SAMHSA - HRSA Workforce Collaborative Initiatives .......................................................... 40
SAMHSA/HRSA Joint Listening Session ................................................................................ 45
Conclusion .................................................................................................................................... 47
APPENDIX A: Examples of SAMHSA-HRSA Activities Related to Behavioral Health
Workforce – Listening Session Summary .................................................................................... 49
APPENDIX B: Bibliography ....................................................................................................... 56

1
SUBSTANCE ABUSE AND MENTAL HEALTH SERVICES ADMINISTRATION
REPORT TO CONGRESS ON THE NATION’S
SUBSTANCE ABUSE AND MENTAL HEALTH WORKFORCE ISSUES
January 24, 2013
Executive Summary
In its report on the fiscal year (FY) 2012 budget for the Department of Health and Human
Services (HHS), the Senate Appropriations Committee Subcommittee on Labor, Health, and
Human Services, Education, and Related Agencies (LHHS-ED) requested the Substance Abuse
and Mental Health Services Administration (SAMHSA) provide the Committee with a
workforce report, specifically addressing the addictions workforce and SAMHSA’s collaboration
with the Health Resources and Services Administration (HRSA). The Subcommittee language is
as follows:
Addiction Services Workforce. – The Committee notes the growing workforce crisis in
the addictions field due to high turnover rates, worker shortages, an aging workforce,
stigma and inadequate compensation. The Mental Health Parity and Addiction Equity
Act and the Patient Protection and Affordable Care Act are anticipated to increase the
number of individuals who will seek substance use disorder services and may exacerbate
current workforce challenges. As the provision of quality substance use disorder services
is dependent on an adequate qualified workforce and SAMHSA is the lead federal agency
charged with improving these services, the Committee expects SAMHSA to focus on
developing the addiction workforce and identify ways to address the current and future
workforce needs of the addiction field. The Committee directs SAMHSA to submit a
report by March 31, 2012, on current workforce issues in the addiction field, as well as
the status and funding of its substance use disorder services workforce initiatives. This
report should also detail how SAMHSA is working with HRSA to address addiction
service workforce needs and should identify the two agencies’ specific roles,
responsibilities, funding streams and action steps aimed at strengthening the addiction
services workforce (Senate Report 112-84, page 122).
SAMHSA has prepared this report to Congress to provide an overview of the facts and issues
affecting the substance abuse and mental health workforce in America. While the workforce
report was requested specifically for the addiction treatment workforce, SAMHSA’s report will
cover the behavioral health workforce in its entirety because many data sources (including those
funded by HRSA’s Bureau of Health Professions and the Department of Labor) and programs
report by profession or discipline rather than population served (e.g., social workers,
psychologists, and counselors), whether providing prevention services or treatment and whether
serving persons with substance use disorders, mental health conditions, or both. Data specific to
the substance use disorder treatment workforce will be provided wherever available. This report
also will include demographic data as well as a discussion of key issues and challenges such as
staff turnover, aging of the workforce, inadequate compensation, worker shortages, licensing and
credentialing issues, and recruitment, retention and distribution of the workforce. The
misunderstandings and often inaccurate perceptions of society about mental illness and addiction

2
as these relate to workforce challenges are also discussed. The information on the behavioral
health
1
workforce is drawn from multiple resources as there is no single federal data source at
this point in time.
The impact of the Affordable Care Act and the Mental Health Parity and Addiction Equity Act
(MHPAEA), which will increase access and alter service settings, is also discussed. The
enactment of both of these laws may reshape the workforce and the delivery of services. For
example, the Affordable Care Act is moving the field toward the integration of services with
primary care, which has significant workforce implications in regard to team approaches and the
new roles and responsibilities for staff. Bureau of Labor Statistics (BLS) projections made prior
to the passage of MHPAEA and Affordable Care Act already indicated higher than normal
growth for a number of behavioral health professions.
This report also describes SAMHSA’s efforts to address many of these issues through its current
programs and its eight Strategic Initiatives. In addition, the report presents a summary of
collaborations between SAMHSA and HRSA, including a jointly sponsored listening session on
the behavioral health workforce. HRSA and SAMHSA have worked collaboratively to address
behavioral health workforce issues by sharing information about efforts within each agency and
by developing, funding, and managing joint projects such as the Center for Integrated Health
Solutions (CIHS), the minimum data set (MDS) project, and the training of practitioners about
military culture to enhance service provision for veterans and their families. Many of these
projects and efforts are described in this report.
SAMHSA is keenly aware that to achieve its mission to reduce the impact of substance abuse
and mental illness on America’s communities, a well-trained, educated and fully functioning
workforce is needed. Likewise, HRSA is aware that to achieve its mission to improve health and
achieve health equity through access to quality services, a skilled health workforce and
innovative programs, it must address behavioral health as an essential part of the health care
landscape in America. SAMHSA and HRSA are working
together toward these aims.
Intr
oduction to Report
An adequate supply of a well-trained workforce is the foundation for an effective service
delivery system. Workforce issues, which have been of concern for decades, have taken on a
greater sense of urgency with the passage of recent parity and health reform legislation.
SAMHSA is fully cognizant of the impact that workforce issues have on the infrastructure of the
1
In this report, the term “behavioral health” is used to encompass mental health conditions, mental illness,
substance abuse, substance use disorders, and addictions. In various contexts, the term is used to include emotional
health development, substance abuse and mental illness prevention services and activities, treatment services, and/or
recovery support activities and services for those in recovery from mental illness, mental health problems, and/or
addictions.

3
behavioral health delivery system and services, and seeks to address these issues through a
variety of initiatives and programs. SAMHSA also recognizes that increasing the size of the
workforce, recruiting a more diverse, younger workforce, and retaining trained and qualified
staff are necessary to provide for the behavioral health needs of the nation’s population.
In the past decade, SAMHSA commissioned workforce reports to identify major workforce
issues and develop recommendations to address these challenges. These reports, An Action Plan
for Behavioral Health Workforce Development (SAMHSA, 2007), Report to Congress:
Addiction Treatment Workforce Development (SAMHSA, 2006), and Strengthening Professional
Identity: Challenges of the Addition Treatment Workforce (SAMHSA, 2006a), led to the
continuing support of some existing programs and the development of some new workforce
efforts. Behavioral health workforce initiatives focus on technology transfer and training on
evidence-based practices, providing resources, supporting knowledge transfer, recruiting a
diverse workforce, and integrating primary and behavioral health care.
Since the publication of SAMHSA’s workforce reports, there have been a number of changes
that increase the need and demand for behavioral health services. The Affordable Care Act will
increase the number of people who are eligible for health care coverage through Medicaid and
Exchanges and includes parity for services within its covered services. In addition, as screening
for mental illness and substance abuse become more commonplace in primary care, more people
will be identified as needing services. Furthermore, workforce shortages will be impacted by
additional demands that result from: (1) a large number of returning veterans in need of services;
and (2) new state re-entry initiatives to reduce prison populations, a large majority of whom have
mental or substance use disorders.
Preparing a workforce that can meet the challenges of the 21
st
century is an essential component
of SAMHSA’s strategic plan and programs. SAMHSA has embedded workforce elements in
each of the eight Strategic Initiatives, as described in its strategic plan document, “Leading
Change: A Plan for SAMHSA's Roles and Actions 2011-2014,” (SAMHSA, 2011a). Examples
of workforce objectives in each of the Strategic Initiatives include:
1. Prevention of Substance Abuse and Mental Illness: Educate the behavioral health field
about successful interventions, such as screening, brief intervention, and referral to
treatment (SBIRT); and develop and implement training around suicide prevention and
prescription drug abuse.
2. Trauma and Justice: Provide technical assistance and training strategies to develop
practitioners skilled in trauma and trauma-related work and systems that have capacity to
prevent, identify, intervene and effectively treat people in a trauma-informed approach.
3. Military Families: Develop a public health-informed model of psychological health
service systems, staffed by a full range of behavioral health practitioners who are well
trained in the culture of the military and the military family and the special risks and
needs that impact this population, such as Post-Traumatic Stress Disorder (PTSD) and
Traumatic Brain Injury (TBI). The role of peer counselors within this model will also be
important to its success.
4. Recovery Support: Build an understanding of recovery-oriented practices, including
incorporating peers into the current workforce to support peer-run services. Emphasize

4
collaborative relationships with children, youth, and families that involve shared
decision-making service options.
5. Health Reform: Work with partners and stakeholders to develop a new generation of
providers, promote innovation of service delivery through primary care and behavioral
health care integration, and increase quality and reduce health care costs through health
insurance exchanges and the essential and benchmark benefit plans.
6. Health Information Technology: Promote the adoption of electronic health records
(EHRs) and the use of health information technology (HIT) through SAMHSA’s
discretionary program and Block Grant technical assistance efforts.
7. Data, Outcomes and Quality: Target quality improvement through workshops, intensive
training and resources that promote the adoption of evidence-based practices, and
activities to advance the delivery of clinical supervision to foster competency
development and staff retention.
8. Public Awareness and Support: Ensure that the behavioral health workforce has access
to information needed to provide successful prevention, treatment, and recovery services.
Background
The Institute of Medicine (IOM; 2006) chronicles efforts beginning as early as the 1970s that
attempt to deal with some of the workforce issues regarding mental and substance use disorders,
but notes that most have not been sustained long enough or been comprehensive enough to
remedy the problems. Shortages of qualified workers, recruitment and retention of staff and an
aging workforce have long been cited as problems. Lack of workers in rural/frontier areas and
the need for a workforce more reflective of the racial and ethnic composition of the U.S.
population create additional barriers to accessing care for many. Recruitment and retention
efforts are hampered by inadequate compensation, which discourages many from entering or
remaining in the field. In addition, the misperceptions and prejudice surrounding mental and
substance use disorders and those who experience them are imputed to those who work in the
field.
Of additional concern, a new IOM report (2012) notes that the current workforce is unprepared
to meet the mental and substance use disorder treatment needs of the rapidly growing population
of older adults. The IOM report’s data indicate that 5.6 to 8 million older adults, about one in
five, have one or more mental health and substance use conditions which compound the care
they need. However, there is a dearth of mental health or substance abuse practitioners who are
trained to deal with this population.
Pre-service education and continuing education and training of the workforce have been found
wanting, as evidenced by the long delays in adoption of evidence-based practices, under-
utilization of technology, and lack of skills in critical thinking (SAMHSA, 2007). These
education and training deficiencies are even more problematic with the increasing integration of
primary care and mental or substance use disorder treatment, and the focus on improving quality
of care and outcomes. As noted by the IOM (2003), all health care personnel, including
behavioral health clinicians, should be trained “to deliver patient centered care as members of an
5
interdisciplinary team, emphasizing evidence-based practice, quality improvement approaches
and informatics.”
Data reported in the 2010 and 2011 National Survey on Drug Use and Health (NSDUH)
demonstrates the current unmet need for behavioral health services:
• Approximately 21.6 million persons aged 12 or older (8.4 percent of this population)
needed treatment for an illicit drug or alcohol use problem.
• Only 2.3 million (10.8 percent) of those who needed treatment received treatment at a
specialty facility (SAMHSA, 2012b).
• Approximately 45.9 million adults aged 18 or older (20 percent of adults) in the United
States had any mental illness in the past year.
• Approximately 11.1 million adults aged 18 or older (4.9 percent of adults) reported an
unmet need for mental health care in the past year including 5.2 million adults aged 18 or
older who reported an unmet need for mental health care and did not receive mental
health services in the past year.
• Inability to afford care was cited as the most significant barrier to receiving care for
mental health services (43.7 percent of those surveyed who needed services); the lack of
coverage and cost of services was cited as a significant barrier in seeking substance use
disorders services (32.9 percent of those surveyed who needed services for a substance
use disorder (SAMHSA, 2011).
As indicated in the NSDUH data above, many individuals who may need behavioral health
services do not access them due to lack of health care coverage. However, health reform will
significantly reduce this barrier to behavioral health services. It is estimated that approximately
11 million of the individuals who will have access to coverage beginning in 2014 will have
mental and/or substance use disorders and will have access to care with the continued
implementation of health reform (SAMHSA, 2011). This increase is expected to strain an
already thinly stretched workforce.
In the absence of any available standardized survey instrument or national study that provides the
needed information, data for this report are taken from a number of sources. There are two
SAMHSA sponsored initiatives that will address the paucity of standardized workforce data.
SAMHSA and HRSA are working collaboratively on the development of a MDS, starting with
the major behavioral health professional disciplines, which may ameliorate the data scarcity
problem in the future. In addition, SAMHSA’s Addiction Technology Transfer Centers
(ATTCs) conducted a national workforce survey on the addiction treatment workforce which
was completed at the end of FY 2012.
Changing Landscape: Impact on the Workforce
In addition to the enactment of parity and health reform legislation, advancements in research,
demand for outcomes and quality improvements, and the empowerment of people in recovery are
contributing to changes in practice and the workforce. Major changes to the field include the
integration of behavioral health and primary care, a push to accelerate the adoption of evidence-
6
based practices, and a model of care that is recovery-oriented, person-centered, integrated, and
utilizes multi-disciplinary teams. Behavioral health has moved to a chronic care, public health
model to define needed services. This model recognizes the importance of prevention, the
primacy of long-term recovery as its key construct, and is shaped by those with lived experience
of recovery. This new care model will require a diverse, skilled, and trained workforce that
employs a range of workers, including people in recovery, recovery specialists, case workers and
highly trained specialists.
Integrated care will reduce medical costs and result in better outcomes. One study showed that
individuals with the most serious mental illnesses and co-occurring disorders living in publicly
funded inpatient facilities die at age 53, on average (Parks et al., 2006). A more recent study,
using a population based representative sample, found that people with mental health disorders
died on the average eight years younger than those without mental health disorders and these
deaths were largely due to medical causes rather than accidents or suicides (Druss et al., 2011).
People with mental and substance use disorders die from treatable medical conditions such as
smoking, obesity, high blood pressure and a variety of other medical disorders (Mertens et al.,
2003). Untreated mental and substance use disorders not only negatively impact a person’s
behavioral health but also lead to worse outcomes for co-occurring physical health problems.
Though the co-occurrence of behavioral and other medical conditions is common, individuals
with serious behavioral health conditions who lack financial resources are often unable to access
quality care, either for their behavioral health conditions or for other health problems. Good
behavioral health is associated with better physical health outcomes, improved educational
attainment, increased economic participation, and meaningful social relationships. Further, good
health is not possible without good behavioral health (Friedli & Parsonage, 2007). Receipt of
behavioral health treatment has been shown to decrease medical care costs significantly (Gerson
et al., 2001). Thomas (2006) reported savings of $140 per enrollee per month when coordinated
care was provided for high-cost, high-risk Medicaid patients with depression. This coordinated
care resulted in a 12.9 percent reduction in cost for this population. Unützer et al. (2008) found
that providing coordinated depression and primary care for older adults resulted in reduced
symptoms of depression in 45 percent of patients and reduced the per patient care cost an
average of $3,000 over four years.
Another significant change in health care is the use of SBIRT. As health reform takes effect,
SBIRT will become a part of the ongoing prevention activities resulting in the identification of
many more people with, or at risk for, depression and substance use disorders. Many individuals
who are identified will receive brief interventions or brief treatment, often conducted by health
educators, recovery specialists or other types of staff in the primary care system. Those needing
more intensive treatment/recovery services would be referred to specialty treatment
providers/practitioners.
The behavioral health care workforce is a complex system, comprising many different
professionals ranging from psychiatrists to non-degreed workers and para-professionals. The
integration of primary and behavioral health care will impact both the behavioral health and the
primary care workforce as primary care staff will be expected to have competencies in
behavioral health and behavioral health staff will need competencies associated with working in
7
primary care settings. A study done by the National Association of Community Health Centers
(NACHC; 2011) found that 43 percent of physicians working in Federally Qualified Health
Centers (FQHCs) were interested in training on medication assisted treatments for persons with
addictive disorders. Many FQHC staff also indicated interest in training on Motivational
Interviewing, Short-term Interventions, Problem-Focused Treatment, SBIRT, PTSD and trauma
interventions.
Trauma plays a central role in behavioral health disorders. Exposure to physically or
psychologically harmful or life-threatening events is a common risk factor for both mental and
substance use disorders (SAMHSA, 2004). Studies have also linked the experience of trauma to
other chronic physical diseases, such as obesity, diabetes and pulmonary diseases (Felitti et al.,
1998). Individuals with significant trauma histories are present not only in the behavioral health
specialty sector, but in child welfare, criminal and juvenile justice, domestic violence, education
and primary and specialty health care. Emerging studies have begun to document positive
outcomes in these sectors when trauma is addressed and appropriately treated. SAMHSA has
recognized the public health urgency to more systematically address trauma. Investments have
been made in the development of education and public awareness materials, screening and
assessments, treatment and recovery interventions, and organizational approaches to trauma.
Critical to this effort is the development of a workforce trained in trauma-specific or trauma-
informed approaches.
In addition, the shift to a recovery-oriented paradigm has resulted in an increased use of peers,
recovery support workers, care managers, patient navigators, and health educators. The role of
peer specialists is to provide ongoing recovery support for people with mental or substance use
disorders. As of September 2011, 23 states have developed certification programs for peer
specialists. Certified Peer Specialists/Recovery Coaches may work in many settings including
independent recovery community organizations, partial hospitalization or day programs,
inpatient or crisis centers, vocational rehabilitation or drop-in centers, residential programs, and
medication assisted programs. Peer support activities include self-determination and personal
responsibility, providing hope, recovery coaching, life skills, training, communication with
providers, health and wellness, illness management, addressing discrimination and promoting
full inclusion in the community, assistance with housing, education/employment, and positive
social activities (Center for Substance Abuse Treatment [CSAT], 2009; Daniels et al., 2011).
Demographic Information
This section will provide data on gender, race and educational level of the mental health and
addictions workforce.

8
Gender
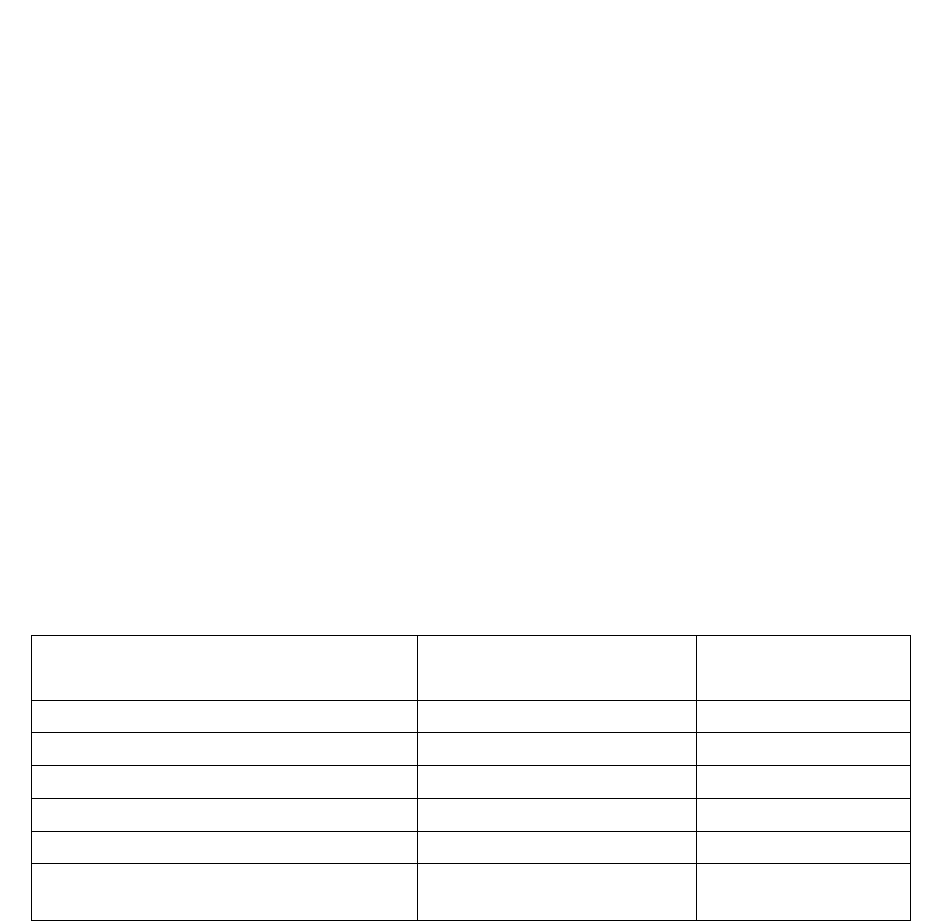
The gender breakdown for some of the major professions working in the field is listed in Table 1.
Table 1
Occupation
Male
Female
Psychologists
33.5%
66.5%
Psychiatrists
70%
30%
Social Workers
19.2%
80.8%
Counselors
28.8%
71.2%
Bureau of Labor Statistics, Department of Labor, Occupational Outlook Handbook 2010-11 http://bls.gov/oco/
A sample of 260 Certified Peer Specialists from 28 states found that 33 percent were male and
66 percent were female, and one percent reported they were transgender (Salzer et al., 2010).
Similar data were found in several studies that looked at turnover and other staffing issues in the
addictions field. These studies reported the percentage of women in the addiction treatment field
at 60 percent or higher (Knight et al., 2012; Knudsen et al., 2006; Curtis & Eby, 2010).
Information obtained by the International Certification and Reciprocity Consortium (IC&RC)
from 15 certification boards
2
reporting on 30,742 counselors found that 61.9 percent were
women and 38.1 percent were men (2011).
Racial Composition
Racial and ethnic minorities as a whole comprise approximately 30 percent of the U.S.
population (U.S. Census, 2010), and a similar percentage of those receiving services (SAMHSA,
2012; 2008). However, African Americans are represented at a higher rate among service
recipients for both mental health and addictions services. As indicated in Mental Health, United
States, 2010 (SAMHSA, 2012a) report, racial minorities account for only:
• 19.2 percent of all psychiatrists;
• 5.1 percent of psychologists;
• 17.5 percent of social workers;
• 10.3 percent of counselors; and
• 7.8 percent of marriage and family therapists.
Information reported from eight certification boards which are members of IC&RC, representing
21,681 counselors as of March 1, 2012, found the racial makeup as described in Table 2 below.
2
There are credentialing boards for addiction counselors in all 50 States; however, not all of them collect data on a
consistent basis nor do they all collect data on the same variables. Therefore in several places in this Demographic
Information section the numbers of certification boards responding may vary.

9
Table 2
Racial Composition
Race
Percent
White
55.8%
Black/African-American
27.9%
Hispanic/Latino
11.1%
American Indian/Alaska Native
0.7%
Asian/Pacific Islander
2.8%
N = 21,681 from 8 boards.
A sample of certified peer specialists found that 21 percent of those respondents were from
minority populations (Salzer et al., 2010). The ongoing disparity in the demographics of the
workforce and patient population suggest that training in cultural competence will be important.
Education Levels
Dilonardo (2011) reported that almost all states (98 percent) required a master’s degree to qualify
as a mental health counselor but 45 percent of states did not require any college degree to qualify
as a substance abuse counselor. For behavioral health care disciplines, independent practice
requires a master’s degree in most states; however, for addiction counselors, data available a
decade ago indicated that about 50-55 percent of those certified or practicing in the field had at
least a master’s degree, 75 percent hold a bachelor’s degree, and the reminder had either some
college, a high school diploma or equivalent (Kaplan, 2003).
Workforce Conditions
This section briefly summarizes some of the major factors that impact the workforce, including
high turnover, worker shortages, an aging workforce, inadequate compensation, and recruitment,
retention and distribution of the workforce, as well as misperception and prejudice about mental
illness and addiction.
High Turnover
Staff turnover is costly in monetary terms with regard to replacement expenses and also
disruptive to the therapeutic relationship. SAMHSA’s workforce studies (2007, 2006, 2006a) all
found high turnover rates reported in the literature at those times. Recent studies corroborate
those earlier findings. The 2012 ATTCs workforce survey reported an average annual turnover
of addiction services professionals at 18.5 percent across the country (Ryan et.al., 2012). Eby et
al. (2010) conducted a study of 739 clinicians over a two-year time period in 27 geographically
dispersed public and private treatment organizations and found annual turnover rates of 33.2
percent for counselors and 23.4 percent for clinical supervisors. A study of adolescent treatment
programs (Garner et al., 2012) found turnover rates of 31 percent for clinicians and 19 percent
for clinical supervisors. These rates are substantially higher when compared to primary care

10
physicians in managed care organizations who had a median turnover rate of approximately
seven (7.1) percent (Plomondon et al., 2007). As reported by Anderson (2012), nurse
practitioners and physicians assistants had 12 percent turnover rates.
A meta-analysis found that burn-out, stress and lack of social support are antecedents to worker
turnover in the social service sector (MorBarak et al., 2001). Other studies found that better
opportunities were key reasons for leaving (Eby et al., 2010; Gulf Coast ATTC, 2005). Reported
turnover appeared to be worse in rural agencies (Knudsen et al., 2005). Another study by Knight
et al. (2012) demonstrated that high turnover produced increased stress and workforce demand
for the remaining staff. One study found that clinical supervision reduced emotional exhaustion
and turnover intention in counselors working in treatment agencies (Knudsen et al., 2008).
In a Gulf Coast ATTC survey, directors reported annual staff turnover rate was 42 percent. The
leading reason for leaving was a better opportunity in the field, followed by personal reasons
(illness, family issues, child care, etc.), and inadequate salary. In 2004, program directors in
Tennessee reported turnover rates from 15-22 percent. Reported turnover appeared to be higher
in rural agencies (Knudsen et al., 2005).
High turnover most often had a negative impact on implementation of evidence-based practices,
although some teams were able to use strategies to improve implementation through turnover.
Implementation models must consider turbulent behavioral health workforce conditions
(Woltmann et al., 2009). Carise et al., (2005) worked with nine community-based treatment
centers in Philadelphia to implement a new assessment tool and had trouble recruiting staff for
the study due to staff turnover rates of 32 percent among the agencies involved.
Worker Shortages
Concerns about worker shortages have been indicated for a number of years. As reported in An
Action Plan for Behavioral Health Workforce Development (SAMHSA, 2007), it is projected
that by 2020, 12,624 child and adolescent psychologists will be needed but a supply of only
8,312 is anticipated. Mental Health, United States, 2008 (SAMHSA, 2010), found more than
two-thirds of primary care physicians who tried to obtain outpatient mental health services for
their patients reported they were unsuccessful because of shortages in mental health care
providers, health plan barriers, and lack of coverage or inadequate coverage.
As of March 30, 2012, HRSA reported that there were 3,669 Mental Health, Health Professional
Shortage Areas (HPSAs)
3
containing almost 91 million people. It would take 1,846 psychiatrists
and 5,931 other practitioners to fill the needed slots. This shortage of workers is not evenly
distributed as 55 percent of U.S. counties, all rural, have no practicing psychiatrists,
psychologists, or social workers (SAMHSA, 2007). Another study (Thomas et al., 2009) found
that 77 percent of counties had a severe shortage of mental health workers, both prescribers and
non-prescribers and 96 percent of counties had some unmet need for mental health prescribers.
3
The Mental Health HPSAs do not include consideration of shortages of specialty addiction services professionals.

11
The two characteristics most associated with unmet need in counties were low per capita income
and rural areas.
Ascertaining the supply of addiction treatment workers has been difficult due to a lack of
ongoing data collection. In surveys conducted by various regional ATTCs, program directors
have indicated problems recruiting adequately prepared staff, often citing at least one or more
unfilled full time equivalent (FTE) positions (RMC, 2003; Knudsen et al., 2005). Reasons for
recruiting difficulties include insufficient numbers of applicants who meet minimum
qualifications (due to lack of experience, certification, or education), a small applicant pool in
specific geographic areas, and a lack of interest in the positions due to salary and limited funding
(Ryan et al., 2012; Gulf Coast ATTC, 2007). In addition, the Gulf Coast study found that even if
all of the 105 positions were filled, 34 percent of agencies would still be understaffed. Agencies
reported a need for 56 additional budgeted positions statewide. A survey of agencies in
Tennessee conducted by the Central East ATTC (Knudsen et al., 2005) found that program
directors reported an average staff shortage of 1.27 FTEs across programs.
Aging Workforce
According to the BLS the median age of various professionals who work in the mental health
and addiction field are shown in Table 3 below.
Table 3
Occupation
Median Age
Psychologists
50.3
Psychiatrists
55.7 (46% are 65+)
Social Workers
42.5
Counselors
42
Bureau of Labor Statistics, Department of Labor, Occupational Outlook Handbook 2010-11 http://bls.gov/oco/
In 2006, more than 50 percent of male U.S. psychiatrists and 25 percent of female psychiatrists
were aged 60 or older (SAMHSA, 2010). Recent studies, using samples of hundreds of
counselors across programs in many states, reported consistent findings for counselors working
in addiction treatment, with an average age in the mid-40s (Knight et al., 2012; Knudsen et al.,
2006). The current addiction treatment workforce is middle-aged and even new workers entering
the field do so relatively late in their careers (RMC, 2003; RMC, 2003a; National Association for
Alcoholism and Drug Abuse Counselors [NAADAC], 2003). Many counselors come into the
field as second careers, entering the profession in their mid-forties (SAMHSA, 2006a).
Recruiting students into the field, particularly from under represented populations, can serve as a
counterbalance to an aging workforce.
Perceptions about Behavioral Health Conditions and Those with Lived Experience
People with mental and substance use disorders often face misunderstanding and discrimination
for having these conditions. Those working in the behavioral health field often face the same
misperceptions and judgments about their value as clinicians which results in recruitment
12
difficulties and lower pay than comparable fields (National Council of Community Health
Centers [NCCBHC], 2011; SAMHSA, 2007; SAMHSA, 2006).
A 2011 compensation study found that the negative beliefs and misunderstandings associated
with people suffering mental illnesses and substance use disorders also impacts those working in
the field, even as compared to other segments of health care. At a mental health center, a
master’s level social worker earns $45,344 and an entry level social worker earns $30,000 while
in a general health care agency, a social worker earns $50,470. A registered nurse working in a
behavioral health organization makes $52,987 while the national average for nurses is $66,530
(NCCBH, 2011).
Most staff in a Northwest Frontier ATTC survey reported that they had lower professional status
than other health professionals (RMC, 2003). A series of focus groups throughout New York
State indicated that the prejudice and misunderstanding of alcoholism and drug addiction
prevents other professions from recognizing and accepting addictions professionals as peers
(New York State Office of Alcoholism and Substance Abuse Services [NYS OASAS], 2002).
As discussed in the workforce survey conducted in Texas (Gulf Coast ATTC, 2007), the
perception that addictions counselors have low status may also contribute to professionals
leaving the field and difficulty in recruiting replacements. Seventy-five percent of directors
thought that addictions counselors have lower status than other helping professionals and only
four percent thought that addictions counselors have higher status. Among those who thought
status was lower, the primary reason was that addictions counselors have less formal education
or training.
A number of workforce studies conducted in the past decade found that addiction counselors had
lower status than other professionals (NYS OASAS, 2002; RMC, 2003; Gulf Coast ATTC,
2007). Knudsen et al. (2005) also reported that some clinicians may also have lower status due
to their own history of substance use disorders. In a series of focus groups conducted primarily
with African-American and Hispanic early and mid-career populations, participants stated that
addictions treatment was not valued in the larger society and that, therefore, workers were not
well compensated or offered supports to avoid burn-out. The lack of information about the field
and the perception that the field is not viewed as a valued profession appear to be recruitment
barriers for some individuals (Gaumond et al., 2007).
Inadequate Compensation
Compensation for those working in behavioral health is significantly lower than for other health
related or other comparable professions. The National Council for Community Behavioral
Healthcare (NCCBH) has a membership of over 1,950 community-based, largely non-profit
providers delivering both mental health and substance abuse services for persons with mental
illness, addictive disorders or both. A 2011 survey conducted by the NCCBH found a strong
positive relationship between salary and organizational size/revenue. In addition, geographic
differences in salaries were noted, especially with those in the Northeast when compared to the
rest of the county. Also, psychiatrists working in rural settings had higher salaries compared to
psychiatrists working in other locations. The NCCBH study also found differences in executive
13
salaries, with the vast majority of executive salaries at mental health centers below $150,000.
The average salary of a Chief Executive Officer (CEO) at a community mental health center was
$114,247, compared to $136,168 for a CEO at a FQHC. Both of these were significantly less
than the top management official at a non‐profit hospital, which was $408,927.
This survey also found that salaries for positions in behavioral health care were much lower than
reference professions both in other service areas within the health care industry and outside
health care. For example, a licensed professional social worker, requiring a Master’s degree and
typically 2,000 hours of post-graduate experience, earned less than the manager of a fast food
restaurant. The median salary for a direct care worker in a 24-hour residential treatment center
was $23,000 compared to $25,589, the median salary for an assistant manager at Burger King
(NCCBH, 2011).
Compensation for those working in the addictions field is notoriously low. In fact, earlier studies
(Kaplan, 2003) suggested that inadequate compensation contributes to high turnover with
counselors engaging in significant churning or movement from one job to another to increase
their salaries, often by only $1,000 a year. NAADAC (2006) noted that “[m]any of our
Addiction Professionals across the USA can currently qualify for food stamps - this is not
acceptable - especially if we want quality, competent and long-term professionals.” The
disparity in the salary for substance abuse counselors and other professional groups is due in part
to the difference in credentialing/ licensure standards. The lack of national standards for
addiction counselors and the absence of any specific degree requirements across many states
impact the overall compensation for this group of workers.
Average wages for behavioral health professionals are shown in Table 4.
Table 4
Average Wages from the Bureau of Labor Statistics
Profession
Bureau of Labor
Statistics*
National Council
Salary Survey
Psychiatrists
$163,660
$168,163
Psychologists
$84,220
$79,900
Marriage & Family Therapists
$49,020
$42,605
Social Worker (MSW)
$50,470
$45,344
Mental Health Counselors (MA)
$41, 710
$41,313
Substance Abuse & Behavioral
Disorders Counselors (Certified/BA)
$37,030
$34,331
* Bureau of Labor Statistics, - Occupational Outlook Handbook 2009
Fo
r comparative purposes, the NCCBH in its 2011 salary survey looked at average salaries for
selected professions that required comparable education and training to the professions listed in
Table 4 for those disciplines that required a master’s degree or less. The selection provides a
comparison of average salaries between standard behavioral health professions and allied
health/public service workers. These are shown in Table 5.
Table 5

14
Average Wages of Reference Professions
Reference Profession
Average Wage
Physician Assistant
$84,830
Physical Therapist
$76,220
Dental Hygienist
$67,860
Secondary School Teacher
$55,150
Subway /Metro Operator
$52,800
Firefighters
$47,270
BLS found similar low wages in Table 6 below.
Table 6
Profession
Median Wage
Psychiatrists
$164,220
Psychologists
$63,140
Marriage & Family Therapists
$44,590
Mental Health and Substance Abuse
Social Workers
$37,210
Substance Abuse & Behavioral
Disorders Counselors
$37,030
Mental Health Counselors
$36,810
Bureau of Labor Statistics, Department of Labor, Occupational Outlook Handbook 2010-11 http://bls.gov/oco/
The middle 50 percent of substance abuse and behavioral disorders counselors earned between
$29,410 and $47,290. The lowest 10 percent earned less than $24,240, and the highest 10
percent earned more than $59,460. Median annual wages in the industries employing the largest
numbers of substance abuse and behavioral disorder counselors were as follows:
Table 7
Wages by Setting
Setting
Median Wage
General medical and surgical hospitals
$44,130
Local government
$41,660
Outpatient care centers
$36,650
Individual and family services
$35,210
Residential mental retardation, mental
health and substance facilities
$31,300
Bureau of Labor Statistics, Department of Labor, Occupational Outlook Handbook 2010-11 http://bls.gov/oco/

15
A column in an online employment service cited chemical dependency counseling as one of the
five most high stress and low paying jobs in the country.
4
The median annual salary it reported
was $38,900 with annual salaries ranging from $25,079-$48,517. As reported in this column,
many counselors deal with addicted individuals who are often mandated to treatment, and who
do not want any interventions.
“While the work can be compelling, substance-abuse counseling ranks as one of the most
difficult social work jobs due to its emotional challenges. Watching clients relapse and
sometimes become ill or die can take its toll. The combination of being stressed out and broke
trumps all other career-related gripes.” Unfortunately, as with chemical-dependency counselors
or parole officers, many of the workers dealing with high stress and low pay provide essential
social services. “We can't have a society with no probation officers, no social workers,” says Al
Lee, director of quantitative analysis at PayScale.com. We should maybe talk about where we
want to spend our money as a society” (Leonardi, 2012).
Compensation for Specialty Behavioral Health Providers
Congress determined long ago that community health providers funded by HRSA to serve those
without access to other health care and often without insurance should be compensated at cost.
These providers receive grants through HRSA and special and higher rates through Medicaid if
they are determined to be FQHCs meeting HRSA-determined criteria for service provision and
quality. On the other hand, community mental health and substance abuse providers do not have
to meet federally determined criteria for service provision and quality. They must meet state
certification or credentialing requirements which vary from no special requirements to extensive
requirements. These state credentialed providers serve a disproportionate number of low-income
and uninsured individuals and are often reimbursed through Medicaid or through state block
grants (administered through SAMHSA) at whatever rate or for whatever budget the particular
state offers, regardless of the cost of delivering that care.
Likewise, community behavioral health is generally not structured as physician-based practices
the way private sector practitioners are structured. Hence, the incentives for development and
use of health information technology have not been funded for community behavioral health
providers as they have for hospitals or practitioner-based providers. The inconsistency in
funding for FQHCs and community-based behavioral health care providers makes recruiting and
retaining practitioners particularly difficult for these specialty providers serving some of the
nation’s most-in-need persons with addictions and/or mental illness.
Data on Recruitment, Retention and Distribution
As cited in the major SAMHSA workforce report of 2007, An Action Plan for Behavioral Health
Workforce Development, “[e]xamining workforce need nationally is complicated by a host of
factors. There is no national census on behavioral health workforce that adequately captures the
number of trained or employed individuals.” As mentioned previously, this lack of data on the
4
All salary data are provided by online salary database PayScale.com. Salaries listed are median, annual salaries
for full-time workers with five to eight years of experience and include all bonuses, commissions or profit-sharing.

16
workforce has been a major challenge in documenting workforce demand and supply. There is a
paucity of information on recruitment. The extensive SAMHSA 2007 Action Plan report found
that the existing literature focused on engaging minorities in graduate-level training.
Recruitment efforts are not well documented and little data exists on results of recruitment
initiatives. Some workforce studies that were conducted specifically on the addiction workforce
reported that staff recruitment was hampered by low salaries as cited by a majority of program
directors surveyed (RMC, 2003; RMC, 2003a; NYS OASAS, 2002). Management staff also
reported that candidates often did not meet the minimum job requirements due to lack of training
and education or experience in substance abuse treatment. In a workforce report conducted in
Texas in 2007, program directors cited the primary reasons for recruiting difficulties are
insufficient numbers of applicants who meet minimum qualifications due to lack of experience,
certification, or education (Gulf Coast ATTC, 2007).
More literature exists on retention of staff; however, most of the literature focuses only on the
addiction services workforce. In these studies, the turnover rates range from 18.5 percent
(Knudsen et al., 2003) to over 50 percent (McLellan et al., 2003). Kaplan (2003) found that
inadequate compensation contributed to high turnover of addiction counselors which resulted in
movement from one job/agency to another in search of salary increases.
Growth across the behavioral health professions is not consistent. As cited in Mental Health,
United States, 2002 (Sullivan et al., 2004), an increase in the number of both psychologists and
social workers has been noted for years, and, as noted on page 12, the number of psychiatrists
has been stable and therefore not keeping up with the growth in population. As Table 8
demonstrates, the projected growth identified by the BLS for behavioral health occupations is in
many cases greater than the average for most occupations. Given that there are many reports that
cite workforce shortages for addiction counselors, it is clear that strategies need to be developed
to address the field’s recruitment issues.
Table 8
Projected Growth of Specific Occupations
Profession
2008 Workforce
2018 Projection
Increase
Substance Abuse & Behavioral
Disorders Counselors*
86,100
104,200
18,100 (21%)
Mental Health Counselors*
113,000
140,400
27,200 (24%)
Mental Health & Substance
Abuse Social Workers
137,300
164,100
26,800 (20%)
Psychologists
152,000
168,800
16,800 (11%)
Marriage and Family Therapists
27,300
31,300
3,900 (14%)
*Projected growth rate much higher than average for other professions. Bureau of Labor Statistics, Department of Labor, Occupational Outlook
Handbook 2010-11 http://bls.gov/oco/
The CEO of NAADAC addressed the issue of recruitment, retention and reimbursement in a
2006 commentary entitled Blueprint for the States: Policies to Improve the Way States Organize
and Deliver Alcohol and Drug Prevention Treatment (Tuohy, 2006). In this Blueprint, Tuohy
calls for increased understanding of addiction as a disease and increased attention to incentive
such as loan repayments and forgiveness, specifically for addictions counselors, as key
17
ingredients for success in recruitment. Tuohy also calls for adequate rewards as careers progress,
with promotions and recognition, as well as assistance for addictions counselors to remain up-to-
date on the latest advances in the addiction treatment and recovery field in order to retain a
highly qualified workforce. Finally, Tuohy recognizes the need for adequate compensation and
therefore higher rates of reimbursement for addictions professionals. Tuohy discusses the lack of
common national standards or competing standards for key professional areas, especially for
addictions professionals, while calling on multiple credentialing bodies to work together toward
core competencies that could be widely accepted.
As noted in the aforementioned demographic information, the majority of behavioral health
workers are white females in their mid-40s. In its publication, In the Nation’s Compelling
Interest: Ensuring Diversity in the Health-Care Workforce, the IOM (2004) reported that racial
and ethnic minority health care professionals are significantly more likely than their white peers
to serve minority and medically underserved communities, which would improve problems of
limited minority access to care. This report also cites studies that found that minority patients
who have a choice are more likely to select health care professionals of their own racial or ethnic
background, and that they are generally more satisfied with the care that they receive from
minority professionals.
There is also a significant mal-distribution of workers. As found by Greiner and Knebel (2003),
behavioral health professionals are in short supply in rural and low income communities. In fact,
55 percent of U.S. counties – all rural – do not have any practicing behavioral health workers.
And, as reported earlier, more than three-quarters of counties in the United States have a serious
shortage of mental health professionals (Thomas,et al.,2009). Data on the distribution of peers
working in either rural or urban areas are not available at this time. Though there is some
information about peer specialists, the information is limited in scope.
Data are available on a number of variables for the major disciplines comprising the workforce
providing services for persons with mental or substance use disorders. However, these data can
only be obtained from a variety of sources. No single source of workforce data, either discipline
specific or on a national level, exists that details the demographics, supply, demand or practice
information.
Special Issues of the Prevention Workforce
Particularly difficult issues confront the prevention workforce in behavioral health.
Underpinning some of these issues are different models of what constitutes prevention. In the
1950s, public health classified preventive measures in three basic categories, primary, secondary,
and tertiary. But in the 1980s, Dr. Robert Gordon proposed a new Operational Classification of
Disease Prevention (1983), which restricted “the use of the term ‘preventive’ to measures,
actions, or interventions that are practiced by or on persons who are not, at the time, suffering
from any discomfort or disability due to the disease or condition being prevented.” As
articulated by Gordon and reiterated by the Institute of Medicine in 2004 in the context of
behavioral health, these approaches may be for the whole population (universal prevention), for
selected sub-populations (selective prevention) or at-risk individuals (indicated) prevention. The
18
implementation of this model in behavioral health depends on a data-driven continuum of
evidence-based services.
The lack of a wide-spread understanding of the primary prevention model and the role of
prevention in behavioral health leads to a concomitant lack of priority given to funding
prevention activities which are evidence-based, well-documented, and known to be both
efficacious and cost-effective. The effect of this disparity is cumulative: low salaries force many
qualified individuals to leave the field; high staff turnover creates the need for additional
training; the cost of training can be prohibitive for programs and individuals.
An additional challenge for prevention professionals is the lack of a national standard for
credentialing. Despite the existence of the International Certification Reciprocity
Consortium/Alcohol and Other Drug Abuse which provides certification of competency for
prevention specialists, state and local programs may use their own certification standards or
impose no standards at all. This lack of standardization is compounded by the fact that states
vary significantly in their prevention approaches – some are bringing behavioral health and
primary care under one roof while others have substance abuse prevention programs within
public health or mental illness prevention integrated into specialty mental health services –
which further complicates the question of creating one national certification standard to apply
across the board.
Impact of Affordable Care Act and MHPAEA on the Behavioral Health Workforce
In 2014, up to 38 million more Americans will have an opportunity to be covered by health
insurance due to changes under the Affordable Care Act (Congressional Budget Office [CBO],
2010; SAMHSA, 2011). Between 20 to 30 percent of these people (as many as 11 million) may
have a serious mental illness or serious psychological distress, and/or a substance use disorder
(SAMHSA, 2011). Among the currently uninsured aged 22 to 64 with family income of less
than 150 percent of the federal poverty level, 36.8 percent had illicit drug or alcohol
dependence/abuse or mental illness (SAMHSA, 2011). However, the Supreme Court decision
on June 28, 2012 gave the states the option to expand Medicaid as stipulated in the Affordable
Care Act. The CBO therefore reduced by 6 million the number of people who may be covered
by Medicaid and the Children’s Health Insurance Program (CBO, 2012).
This growth in the number of people who will be identified with a mental or substance use
disorder requires an expanded workforce. However, the composition of the workforce will be
reshaped by the Affordable Care Act with the move toward more integrated primary and
behavioral health care. New integrated care structures such as accountable care organizations
and health homes funded or promoted by the Affordable Care Act offer new opportunities for
persons with behavioral health conditions, and will necessitate additional training for primary
care workers as well as new specialty practitioners as part of the multi-disciplinary teams. Brief
interventions and brief treatment will likely be delivered by staff in primary care settings as
screening for depression, alcohol and substance abuse becomes a standard part of care. Staff will
include health educators, nurse practitioners, care managers, physicians as well as counselors,
social workers, psychologists, and addiction specialists.
19
Primary care settings differ from the specialty sector. As integration of primary and behavioral
health services becomes the standard, there will be a greater emphasis on evidence-based
practices and outcomes, especially in light of the HHS National Quality Strategy and
SAMHSA’s National Behavioral Health Quality Framework which are focused on improving
quality of care as well as improving both administrative and clinical processes.
People with more severe and persistent mental and substance use disorders will receive longer
term and more intensive treatment, either within a primary care setting or specialty setting. The
use of peers to promote long-term recovery is also expanding across the country. These peer
specialists, who in some states are now being certified, play a key role in the recovery process
serving as role models, navigators, recovery coaches, as well as providing hope, a critical part of
the recovery process. These peer specialists are also an important addition to the workforce to
help meet the need for services and supports that can be provided by trained persons who are
certified but not licensed as traditional health or behavioral health care practitioners.
Creative retooling and repurposing of the existing behavioral health workforce will be required
to support integration, with some workers in significantly expanded and changed roles with
broader competencies. Great strides will need to be made in the adoption of evidence-based
practices, team work skills and collaboration. In primary care setting a team–based approach is
used which requires more flexibility in scheduling. New or expanded roles and types of workers
are also likely to be needed to facilitate integration, including health educators, behavioral health
specialists, and care managers (SAMHSA, 2011).
Enumeration of Needs
A number of challenges await the workforce over the next several years. As discussed above,
both the demand for services and where services are delivered will change in the coming years.
The rise in the use of medications for mental and substance use disorders as well as the
integration of care are reshaping who and how services are provided. The use of psychotropic
medications has grown exponentially over the past decade. Mojtabai and Olfson (2011) found
that antidepressants are the third most prescribed class of medications in the country. However,
often these patients are not clearly diagnosed or referred for further assessment as primary care
physicians are concerned about a diagnosis that could result in prejudice for the patient and lack
of easy access to mental health and addiction professionals. The use of medication assisted
addiction treatment is also increasing (SAMHSA, 2011).
Integrated care is predicated on a holistic, public health care model requiring a team approach to
primary and behavioral health services. Integrated care will bring additional challenges to the
field. Requirements for licensure/certification are not standardized across states and include
little, if any, preparation related to physical health conditions or working in primary care settings.
National core competencies for behavioral health care are lacking. Practice will be based on
science; employing evidence-based approaches will become the norm. However, the adoption of
evidenced-based practices still often has a lag time of about 15-20 years. The majority of
members of the core primary disciplines (physicians, nurses, social workers, psychologists,
physicians’ assistants and others) are also likely to have insufficient training in behavioral health.
20
In addition, the need for and adoption of interoperable electronic health records and other health
information technology is changing practice and increasing the accountability for quality. All of
these issues indicate successful integration of care will be predicated on comprehensive training
for all staff involved in providing services, whether in primary or specialty care settings and
whether in traditional or multi-disciplinary practices.
The prevalence of co-occurring mental and substance use disorders has been documented in the
2010 NSDUH. The findings indicate that 45.1 percent (9.2 million) of the 20.3 million adults
with substance use disorders also had a mental illness as compared to 17.6 percent without a
substance use disorder. Of the 45.9 million adults who had any mental illness, 20 percent or 9.2
million had a co-occurring substance use disorder. Comparatively, 11.2 million or 6.1 percent of
adults with a substance use disorder did not have a mental illness in the past year (SAMHSA,
2011). This underscores the need for the development and promotion of behavioral health
competencies among both the addictions and the mental health workforce.
As the use of medication assisted treatment increases and treatment for co-occurring disorders
becomes more frequent, employment of physicians in behavioral health settings may increase.
Physicians in primary care are also more likely to be prescribing such medications and treating
individuals with addictions. The use of physicians also increases the likelihood that primary care
will be delivered onsite in community mental health and substance abuse facilities. In a recent
study, almost 75 percent of the participating substance abuse treatment organizations indicated
that finding a physician in the local community who had experience treating substance use
disorders was somewhat or very difficult. More importantly, inadequate funding for physicians’
services was negatively associated with the employment of physicians (Knudsen et al., 2012).
Physicians report barriers to the use of medication assisted treatment and screening and brief
intervention, including not feeling comfortable in managing all components of either type of
intervention (Dilonardo, 2011).
Meeting the country’s behavioral health needs requires a sufficient supply of well trained,
competent workforce. Given the issues discussed in this paper there are some strategies that will
help us achieve the promise of better outcomes for people with and at risk for mental and
substance use disorders. These may include:
• Promoting cross training for the behavioral health workforce to enhance capabilities to
serve individuals with co-occurring disorders and how to work in complex multi-
disciplinary teams;
• Fostering the expansion of the workforce by recruiting a more diverse workforce and
concentrating on underserved populations. Specific populations that need additional
services include children and adolescents, geriatric patients, and those living in rural
areas. Increasing the use of consumers/persons in recovery, parent/family, and other
peers, as well as paraprofessionals and practitioner extenders;
• Disseminating and promoting the adoption of evidence-based practices to reduce the
delay in adoption of science-based interventions including ongoing supervision to ensure
treatment fidelity;
• Encouraging the development and dissemination of behavioral health core competencies
for the primary and other health care workforce;

21
• Providing training and education on recovery-oriented care and recovery principles for
the behavioral health field; and
• Developing standardized workforce data collection elements that can be collected and
analyzed on a regular basis to assist in gathering demographic, setting and practice
information.
SAMHSA and HRSA Workforce Initiatives
SAMHSA and HRSA each fund workforce initiatives that address many of the challenges facing
the behavioral health field. These initiatives provide a broad range of activities that address the
needs of the current workforce and provide support for future growth.
On June 5, 2012, SAMHSA and HRSA Administrators held a joint listening session with key
behavioral health field leaders. From that session, a consensus emerged about many issues that
need to be tackled if the behavioral health workforce is to keep pace with the growing need and
rapidly changing health care environment.
This portion of the report is divided into two sections. The first highlights SAMHSA’s and
HRSA’s current workforce programs and other activities to advance the behavioral health
workforce, and the second describes workforce collaborations between SAMHSA and HRSA,
including results from the joint listening session. Note that for programs spending only a portion
of their funds on workforce development activities. The FY 2012 funding levels provided are
approximate. Expenditures of FY 2012 funds may vary during project execution in order to be
responsive to emerging program needs (e.g., in a given year, a cohort of grantees may or may not
demonstrate a need for technical assistance on workforce development).
SAMHSA Workforce Programs
Addiction Technology Transfer Centers
The ATTC network, which was first funded in 1993, consisted of 14 regional centers and one
national coordinating center in the cohort that ended in FY 2011. They provide services in all 50
states, the District of Columbia, Puerto Rico and the Caribbean Basin, and the Pacific Islands.
The purpose of this program is to develop and strengthen the workforce that provides addiction
treatment services. The ATTCs partner with substance abuse Single State Authorities, treatment
provider associations, addiction counselors, multidisciplinary professionals, faith and recovery
community leaders, family members of those in recovery, and other stakeholders to: (1) raise
awareness of evidence-based and promising treatment and recovery practices; (2) build skills to
prepare the workforce to deliver state-of-the-art addiction treatment and recovery services; (3)
and change practice by incorporating these new skills into everyday use for the purpose of
improving addiction treatment and recovery outcomes. For the first time in its history, the
ATTC network has conducted a national workforce survey to obtain information on the state of
the current workforce.
This survey, Vital Signs: Taking the Pulse of the Addiction Treatment Profession (Ryan,
Murphy, & Krom, 2012), provides an overview of the characteristics and workforce
development needs of the substance use disorders treatment field.
22
The data collection process included a survey of clinical directors; telephone interviews with a
selected group of clinical directors; telephone interviews with thought leaders; and a review of
existing literature and data sets. The 57-item instrument survey was distributed by ATTC
Regional Centers to a sample of 631 programs drawn from the Inventory of Substance Abuse
Treatment Services using a dual sampling method to ensure that data would be both nationally
and regionally representative. The response rate was 88 percent.
A summary of the national findings about the substance abuse workforce as identified by the
ATTC survey is described below.
Basic demographics of the Substance Abuse workforce.
• Sixty-five percent of clinical directors had at least a master’s degree and they have, on
average, 17 years of experience in the field. Seventy-seven percent are state licensed or
certified. About one third are identified as being in recovery from a substance use
disorder.
• Thirty-six percent of direct care staff had a Master’s degree, and 24 percent had a
bachelor’s degree as their highest level of education. The majority of direct care staff is
currently licensed/certified or seeking licensure/certification. Slightly less than one-third
of direct care staff are in recovery from substance use disorders as estimated by their
clinical directors.
• Almost one-third of clinical directors are only somewhat proficient in web-based
technologies, and almost half of substance use disorder facilities do not have an
electronic health record system in place.
Common strategies and methodologies to prepare, retain, and maintain the Substance Abuse
workforce.
• Substance use disorder treatment facilities most commonly offer professional
development for staff through new employee orientation, ongoing training, and direct
supervision. When facilities do not provide for staff training and continuing education,
the most commonly reported reason was a lack of funds.
• The majority of survey respondents reported that staff at their facility had been trained in
both culturally responsive and gender responsive substance use disorder treatment.
• Clinical directors interviewed emphasized the positive effects that developing
relationships with colleges and universities can have on recruiting qualified professionals.
In order to achieve the major goals, the ATTCs utilize technology transfer as a systematic
process through which skills, techniques, models and approaches emanating from research are
translated, disseminated and adopted by practitioners. They also develop curricula standards for
pre-service and academic programs which are compatible with and support SAMHSA’s
Addiction Counseling Competencies (CSAT, 2006; 2007) and provide a coordinated approach to
the training and technology transfer needs of clinical supervisors. ATTCs develop and
disseminate educational materials and resources on substance use treatment. They also
collaborate on developing and supporting emerging leaders in the field.

23
Another critical component of technology transfer is to reduce the time it takes for evidence-
based practices to be adopted by practitioners. Toward that end, SAMHSA and the National
Institute on Drug Abuse (NIDA) have an inter-agency agreement (IAA) to facilitate cooperative
effort that foster the timely transfer and implementation of research-based findings from NIDA-
conducted research, including NIDA's Clinical Trials Network. Through this IAA, NIDA
transfers $1.5 million each year to SAMHSA for the ATTCs to support the NIDA/SAMHSA
Blending Initiative. Begun in 2001, this project is designed to meld science and practice together
to improve substance use disorder treatment and accelerate the dissemination of research-based
drug abuse treatment findings into community-based practice.
There are three components to the Blending Initiative:
• Blending Conferences – Each is designed to enhance bidirectional communication
between researchers, clinical practitioners, and policy-makers regarding innovative
scientific findings about drug abuse and addiction.
• State Agency Partnerships – NIDA works closely with federal and state policy-makers to
help identify strategies to accelerate the adoption of science-based practices.
• Development of Products and Tools – Blending Teams composed of members from the
ATTC Network, NIDA researchers, and community treatment providers participating in
NIDA's Clinical Trials Network, are convened to design user-friendly tools or “products”
that are based on recently tested NIDA research.
These products are introduced to treatment providers to facilitate the adoption of science-based
interventions in their communities at nearly the same time that research results are published in
peer-reviewed journals.
The ATTC Network touches many people working in the addiction services field, which is
attested to by the following data taken from 2010:
• ATTC Network listserv has over 57,000 subscribers.
• There were 987 events with 26,655 participants.
• One hundred eighty-five products accessible on the ATTC Network Websites received
19,940 downloads.
• The ATTC Web site had almost a million (979,680) unique visits and many people
visited more than once as there were 2,612,592 total views.
The ATTC program was re-competed in 2012 with 10 geographic ATTCs reflecting the 10 HHS
geographic regions, four specialty ATTCS for (1) SBIRT; (2) HIT in Rural Areas; (3) American
Indians and Alaska Natives; and (4) Hispanic and Latino Issues and a National Coordinating
Center. Funding for the ATTC program was $9,081,000 in FY 2011 and $9,064,000 in FY 2012.
Partners for Recovery
Partners for Recovery (PFR) is an initiative sponsored by SAMHSA to address issues of national
significance with respect to recovery, cross-systems collaboration, workforce development,
leadership development, and promotion of accurate perceptions of addiction and mental illness
and those who experience these conditions. The PFR Initiative supports and provides technical

24
resources to those who deliver services related to the prevention and treatment of substance use
disorders and co-occurring mental health disorders and seeks to build capacity and improve
services and systems of care. One of PFR’s core activities is developing and implementing a
comprehensive strategy to address workforce issues for the addiction treatment and recovery
field. Below are the workforce activities that PFR supported in FY 2011.
• Advanced Leadership Institute – The Advanced Leadership Institute (ALI) was designed
to enhance the leadership development skills of emerging leaders in the addiction field.
An objective of the program is to further the development of leaders to impact policy and
systems change. This 11-month program trained 28 leaders from across the nation.
Leaders’ skills are enhanced through an extensive set of development experiences,
including individual assessments, an intensive four-day Leader Development Immersion
Session, ongoing coaching, a mid-year two-day Booster (i.e., follow-up) Session, and a
sophisticated knowledge- and skill-application project. This programming is all
supported by a suite of online and print resources available via a site tailored to meet the
particular needs of ALI leaders and their coaches. FY 2011 Budget $510,000.
• School for Prevention Leadership – The School for Prevention Leadership was
specifically designed to bolster the substance abuse prevention workforce and to
contribute to the professionalization of the field. The School includes a class of 24
scholars, who were competitively selected from across the country. This 10-month
program consists of individual and team assessments, a week-long immersion training, a
two-and-a-half day re-immersion training, mentoring, and a graduation. FY 2011 Budget
$336,000.
• Environmental Scan on Certification for Peer Specialists and Recovery Coaches – PFR
conducted a study to create a more complete picture of the number of, and process for
developing, recovery coaches and certified peer specialists, and to facilitate states’
readiness for the Affordable Care Act implementation. The report provides information
about states that currently have a certification and training process for peer support
service provision, the states’ expectations concerning competencies, use of a defined
curriculum, and the funding streams for these services. The report also provides
information concerning Medicaid billing for peer service delivery and the barriers that
impede Medicaid reimbursement. Because the Affordable Care Act will result in an
increased demand for services for substance use disorders, the use of peer
specialists/recovery coaches can help meet the demand for increased services and
promote recovery management. FY 2011 Budget $56,900.
• Lonnie E. Mitchell Historically Black Colleges and Universities Behavioral Health
Policy Academy – The 4
th
Annual Dr. Lonnie E. Mitchell Historically Black Colleges and
Universities (HBCU) Behavioral Health Policy Academy provided a unique forum to
promote behavioral health on HBCU campuses and build workforce capacity to address
the behavioral health needs of the American public. This policy academy offered a
framework for facilitated team discussions to support proposed mini-grant
implementation plans. Teams left the Policy Academy with action plans for
implementing their mini-grant projects and creating sustainable systems of change on
their campuses. The Academy continues the legacy and work of the late Dr. Lonnie E.
Mitchell, an accomplished educator, administrator, policy advisor and psychotherapist.
The 21 mini-grant recipients who attended this conference were charged with the

25
following activities during the conference: (1) review campus-specific projects related to
identified behavioral health priorities; (2) refine proposed activities to ensure sustainable
outcomes; and (3) identify opportunities for collaboration and confirm implementation
strategies. FY 2011 Budget $390,000.
The total budget for the workforce initiatives under PFR was $1,292,900 in FY 2011. SAMHSA
estimates based on planned activities that the total budget for the workforce initiatives under PFR
is $300,000 for FY 2012. The funding is from two budget lines: (1) CSAT Program of Regional
and National Significance (PRNS) Program Coordination and Evaluation; and, (2) CSAT PRNS
Special Initiatives/Outreach.
Historically Black Colleges and Universities – Center for Excellence in Behavioral Health at
Morehouse School of Medicine
The HBCU- Center for Excellence (HBCU-CFE) has three major goals which encompass
promoting behavioral health to positively impact student retention, expanding campus service
capacity, including the provision of culturally appropriate behavioral health resources, and
facilitating best practices dissemination and behavioral health workforce development. Though
the latter goal most directly relates to workforce development, the workforce development tasks
assigned to the HBCU-CFE are:
• Promoting evidence-based and emerging best practices in behavioral health and
disseminating information about effective practices to member institutions;
• Facilitating on-site and distance learning opportunities for HBCU students and faculty in
behavioral health and workforce development, leadership, and other related activities;
• Facilitating the mentoring of students by schools and highlighting model programs in
behavioral health;
• Partnering with programs for regional and local training initiatives with tracks
specifically addressing HBCUs; and
• Promoting awareness and access to behavioral health resources, SAMHSA’s publications
and web-based material and other related resources.
In addition, a number of specific activities performed by the HBCU-CFE that are directed toward
enhancing the capability and capacity of the workforce include the following:
• Enhance workforce development opportunities through partnerships with community-
based providers and organizations.
• Increase the number of HBCU students interning in the behavioral health field.
• Increase HBCU student exposure to career options in the behavioral health workforce.
• Establish and/or increase HBCU partnerships with local, regional and state entities
committed to increasing diversity in the behavioral health workforce.
Funding for the HBCU-CFE in FY 2011 was $1.5 million. Funding for the HBCU-CFE in FY
2012 was $500,000.

26
Minority Fellowship Program
The objective of the Minority Fellowship Programs (MFP) is to increase the knowledge of issues
related to mental health conditions and addictions among minorities, and to improve the quality
of mental health services and substance abuse prevention and treatment delivered to ethnic
minority populations. SAMHSA provides grants to encourage and facilitate the doctoral and
post-doctoral development of nurses, psychiatrists, social workers, psychologists, marriage and
family therapists, and professional counselors by providing funding to organizations which
oversee the fellowship opportunities.
Program goals are to support doctoral training in mental health and substance abuse services by:
• Promoting culturally competent mental health and substance abuse services provided to
ethnic minority populations;
• Increasing the number of professionals delivering mental health and substance abuse
services to ethnic minority populations; and
• Increasing the general knowledge and research of issues related to ethnic minority and
substance abuse treatment.
The MFP increases the pool of professionals qualified to provide leadership, consultation,
training, and administration to government and public and private organizations concerned with
the development and implementation of programs and services for under-served ethnic minority
persons with mental and/or substance use disorders. In FY 2011, there were 120 fellows in the
MFP and, of those, six reported they are planning to specialize in the substance use disorders
field.
In 2011, SAMHSA funded a three-year program which awarded five grants for a total amount of
$4,073,000, from the Center for Mental Health Services (CMHS; $3,455,000), Center for
Substance Abuse Prevention (CSAP; $71,000), and CSAT ($547,000). In 2012, SAMHSA
awarded five continuation grants and one new grant to include professional counselors in the
program for a total amount of $4,975,941, from CMHS ($4,388,665), CSAP ($67,471), and
CSAT ($519,807).
Knowledge Application Program
SAMHSA’s Knowledge Application Program (KAP) addresses the knowledge application needs
of behavioral health treatment providers by synthesizing, publishing, and disseminating
substance abuse treatment and related mental health best practices.
KAP serves as a primary source of information dissemination on strategies, best practices, and
protocols for service delivery by the workforce. KAP is responsible for identifying target
audiences for the SAMHSA products, tailoring products to the specific needs of those audiences,
and developing specialized marketing plans for the products to ensure the appropriate
information is transmitted to the right audience in the most effective format in a timely manner.
It is supported by follow-on activities which help the intended audience use the information.
Among the products developed by KAP are the Treatment Improvement Protocols (TIPs) and the
TIP collateral products; Technical Assistance Publications (TAPs), independent publications on

27
topics such as Anger Management, Substance Abuse Relapse Prevention for Older Adults, and
Brief Counseling for Marijuana Dependence; and many consumer publications/brochures.
In 2011, the KAP program:
• Cleared and printed two TIPS;
• Produced 41 TIP collateral and other materials including Quick Guides, KAP Keys, and
Consumer booklets;
• Produced and disseminated five Advisories and a SAMHSA In Brief;
• Produced a DVD with three family education videos;
• Continued the development of eight TIPS and two TAPs; and
• Started the development of one new TIP.
In addition, KAP is moving ahead with strategies in knowledge dissemination using modern
technology.
SAMHSA funding for the KAP program was $3,893,339 in FY 2011. SAMHSA funding for the
KAP program was $2,500,000 in FY 2012. The funding for the KAP for FY 2012 is from:
CSAT PRNS Screening for Brief Intervention and Referral Treatment, Targeted Capacity
Expansion-General, Post Partum Women, Access to Recovery, Children & Families, Treatment
Systems for Homelessness, Minority AIDs Initiative, Opioid Treatment Programs/Regulatory
Activities, Substance Abuse Prevention and Treatment and Block Grant-Set Aside.
Screening, Brief Intervention and Referral to Treatment Medical Residency Program
General medicine physicians are positioned to play a critical role in the recognition and treatment
of patients with, or at risk for, substance use disorders. Since its inception in 2008, the SBIRT
Medical Residency Program’s primary purpose has been to develop and implement training
programs to teach medical residents skills to provide evidence-based screening, brief
intervention, brief treatment and referral to specialty treatment for patients who have, or are at
risk for, a substance use disorder. Another purpose of the program is to promote adoption of
SBIRT through delivery of training to local and statewide medical communities for wider
dissemination of SBIRT practices. This program promotes systemic change in residency
programs by integrating SBIRT into the curriculum on a long-term basis so that SBIRT will be a
component of the education provided to each successive class of medical residents. SBIRT
Medical Residency Program grant funds are used to develop SBIRT curricula and clinical
training as part of residency programs for physicians in primary care to include family medicine,
internal medicine, obstetrics and gynecology, pediatrics, emergency medicine, trauma,
psychiatry and others. In 2011, there were 17 medical residency programs participating in the
program.
In 2011, 1,335 residents were trained through the Medical Residency grant program, with a total
of 3,998 trained to date. In addition, grantees have trained 1,944 non-residents (e.g., physician
assistants, psychologists, social workers, other health care professionals) during the 2011
reporting period, and 8,572 since 2008.

28
In 2011, the SBIRT Medical Residency program was funded at $5,865,000. In 2012, the SBIRT
Medical Residency program was funded at $6,221,000.
Prescribing Opioids for Chronic Pain
SAMHSA'S courses on "Prescribing Opioids for Chronic Pain: Balancing Safety & Efficacy" are
designed for primary care physicians, as well as dentists and oral surgeons, advance practice
nurses, and physician assistants. They were developed in consultation with the American
Academy of Pain Medicine and an independent panel of experts in medical education,
pharmacology, pain management, regulation, and addiction. The courses are approved for 6.5
hours of Category one credit under the Physician Recognition Award
TM
program of the American
Medical Association, as well the accreditation programs of the American Academy of Family
Physicians and the American Osteopathic Association. Topics addressed in this training include
evidence-based strategies for patient selection, risk assessment, and patient education, factors in
selecting an appropriate opioid, techniques for effective patient monitoring, and knowledge of
why and how to stop prescribing opioids and management of the patient with a different
approach.
Courses are delivered in face-to-face training sessions and are also available online. Through
September 2011, courses have been delivered at 40 sites in the continental U.S. and Alaska and
have reached more than 6,000 health professionals. Special versions of the course have been
developed for military medical personnel and staff of the Indian Health Service. Actual
attendance at the 12 courses delivered between October 1, 2010, and September 29, 2011, was
1,478. In addition, an estimated 1,800 physicians have viewed recordings of the live courses that
are posted on the sponsors' websites or distributed on DVDs. During this same time period,
more than 2,500 registrants had completed at least one online course, and over 3,000 separate
course certificates had been issued.
For FY 2011, the cost to conduct seven live and three online courses was $350,000. For FY
2012, the cost is $350,000.
Physician Clinical Support System for the Treatment of Substance Use Disorders
The Physician Clinical Support System (PCSS) is a national project to support physicians who
are treating opioid dependent persons with methadone or buprenorphine. In July 2011,
SAMHSA awarded the PCSS for Opioid Therapies, to the American Academy of Addiction
Psychiatry. The purpose of this grant is to develop a free national mentoring network that will
provide clinical support (e.g., clinical updates, consultations, evidence-based outcomes, and
training) to physicians, dentists and other medical professionals in the appropriate use of opioids
for the treatment of chronic pain and opioid-related addiction. This initiative contributes to
SAMHSA’s efforts to address the nationwide issue of morbidity and mortality caused by
misuse/abuse and fatal drug interactions involving opioids used in the treatment of addiction and
chronic pain. The target population for the clinical support system includes primary care
physicians, pain specialists, psychiatrists, and other non-addiction medical practitioners who
treat opioid dependent patients and are less familiar with opioid dependence treatment than
addiction specialists. In addition, addiction specialists will also be encouraged to participate in
the PCSS or serve as mentors for physicians desiring to treat opioid dependent patients with
buprenorphine products.

29
In FY 2011, funding for this program was $500,000. In FY 2012, funding for this program was
$500,000.
Physician Clinical Support System-Opioids
The purpose of the PCSS-Opioids grant is to develop a free national mentoring network that will
provide clinical support (e.g., clinical updates, consultations, evidence-based outcomes and
training) to physicians, dentists, and other medical professionals in the appropriate use of opioids
for the treatment of chronic pain and opioid-related addiction. This initiative is targeted to
prescribers (physicians, dentists) and other health professionals working in SAMHSA-certified
opioid treatment programs as well as those prescribers using opiate-based therapy for chronic
pain. The training and clinical support provided under this initiative address the specific
complexities that are inherent in opioid-based therapy and the ways in which those complexities
affect the appropriate care of individuals being treated for chronic pain and opioid-related
addiction.
The PCSS-Opioids grant funds are used primarily to support infrastructure development,
including the following types of activities:
• Establish and maintain a cadre of expert clinicians and educators to provide support for
qualified health care providers preparing for, or engaging in, opioid use in treatment of
chronic pain and opioid-related addiction;
• Disseminate authoritative and standardized clinical materials and clinical tools;
• Promote PCSS-Opioids services to identified target populations;
• Provide mentoring support, observation of practice, and consultative services by phone
and e-mail that promote and support qualified health care providers in the use of opioids
in the treatment of opioid-related addiction and chronic pain; and
• Educate prospective practitioners through web site (educational webinars) and published
resources, such as TIPS containing science-based best practice guidelines for the
treatment and maintenance of patients with opioid dependency and chronic pain.
Funding was provided to the following groups: American Academy of Addiction Psychiatry;
American Osteopathic Academy of Addiction Medicine; American Psychiatric Association,
American Dental Association, American Society for Pain Management Nursing, and
International Nurses Society on Addictions.
In FY 2011, funding for this program was $500,000. In FY 2012, funding for this program was
$500,000. In FY 2011, this program was funded from the Opioid Treatment
Programs/Regulatory Activities budget. In FY 2012, this program was funded from the Opioid
Treatment Programs/Regulatory Activities budget.
Prevention Fellowship Program
The Prevention Fellowship Program, funded by the SAMHSA’s CSAP, was launched in 2006 as
an effort to build a workforce of substance abuse prevention professionals. The Prevention
Fellowship Program addresses workforce development issues in the substance abuse prevention
field by:

30
• Addressing the challenges facing the substance abuse field, including barriers to effective
staff recruitment and retention, low wages, high turnover, inconsistent training and
credentialing, and aging worker retirements;
• Providing opportunities for individuals to strengthen and apply knowledge gained
through their academic programs and work experience in prevention service programs,
sharpen their skills, and develop strong networks among a range of other public health
professionals; and
• Covering all of the cross-cutting principles in the SAMHSA Strategic Plan through
formal educational experiences, training, work experience, coaching, mentoring, and
research/literature review.
The 103 fellows, who have participated in the Prevention Fellowship Program since its inception
in 2006, represent 43 states, six U.S. territories, and two national organizations that support
substance abuse prevention systems. Of the four completed cohorts from 2006 through 2009, 74
participants have enrolled in the program and over 70 percent have graduated. Of the program
graduates, 85 percent have become certified by the IC&RC. Post fellowship employment data
indicate that over 45 percent of fellows have pursued positions and/or post graduate education in
the prevention field. There were 15 fellows in the FY 2011 cohort.
FY 2011 funding was $1,691,284 for the Prevention Fellows Program. FY 2012 funding was
$1,058,771 for the Prevention Fellows Program. This program is funded from the CSAP PRNS
Strategic Prevention Framework.
Recovery to Practice Initiative
This initiative seeks to advance a recovery-oriented approach to mental health care by
developing, promoting, and disseminating training curricula on how to translate the concept of
mental health recovery into practice; and by providing a Recovery to Practice (RTP) Recovery
Resource Center for mental health professionals engaged in this work. The RTP initiative
includes two complementary components: (1) creating a Recovery Resource Center for mental
health professionals complete with web-based and print materials, training, and technical
assistance for professionals engaged in the transformation process; and (2) creating and
disseminating recovery-oriented training materials for each of the major mental health
professions. Through these two major components, the RTP initiative aims to foster a better
understanding of recovery, recovery-oriented practices, and the roles of the various professions
in promoting recovery.
The national mental health professional organizations that are receiving funding to develop
recovery-oriented educational materials and train thousands of psychiatrists, psychologists,
psychiatric nurses, social workers, and mental health peer specialists are: American Psychiatric
Association, American Psychological Association, American Psychiatric Nurses Association,
Council on Social Work Education, and National Association of Peer Specialists. In addition to
these organizations, beginning in 2011, NAADAC has also been included as a key partner in the
Recovery to Practice initiative.

31
With recovery-oriented training materials, mental health professionals will be able to embrace
and practice recovery-oriented approaches while enhancing their core personal and professional
values. In addition, they will learn new ways of working collaboratively across professions to
more effectively support individuals with mental illnesses in entering into and pursuing recovery.
In FY 2011, the funding was $836,000. In FY 2012, the funding was $1,030,000.
Mental Health Care Provider Education in HIV/AIDS Program
The Mental Health Care Provider Education (MHCPE) in HIV/AIDS Program trains mental
health professionals who are currently providing services for individuals living with
HIV/AIDS. The MHCPE curriculum focuses on building a knowledge base and skills in the
medical, neurobehavioral, psychosocial, counseling and testing issues that may arise for mental
health care providers as they care for individuals affected by HIV/AIDS. Three organizations
currently provide the bulk of the training to their respective affiliates. The American Psychiatric
Association provides training to psychiatrists, residents, and psychiatry medical students on the
psychiatric and neuropsychiatric aspects of HIV/AIDS. The American Psychological
Association primarily provides training to psychologists through their HIV Office for
Psychology Education Program. This includes training in the ethics curriculum, with 10
additional HIV specific curricula. The National Association of Social Workers provides training
primarily to social workers and social work trainers, focusing on triple diagnosis and adherence.
In FY 2011, 3,000 persons were trained.
In FY 2011, the funding for this training program was $973,544. In FY 2012, the funding for
this training program was $785,717.
Supplemental Security Income and Social Security Disability Insurance Outreach, Access and
Recovery Training
The primary goal of the Supplemental Security Income (SSI) and Social Security Disability
Insurance (SSDI) Outreach, Access, and Recovery (SOAR) Initiative is to train providers to
develop successful SSI and SSDI applications for individuals who are homeless by increasing
the quality of the disability applications and thereby reducing the decision time cycle for
approvals.
In 2011, the SOAR Technical Assistance Center conducted five four-day train-the-trainer
workshops in 41 states and the District of Columbia resulting in 131 new trainees. Five two-day
trainings were conducted by SOAR technical assistance Center staff in four states with 140
participants. An additional 160 trainings were conducted by SOAR trainers in 40 states and the
District of Columbia for a total of 4,138 participants.
In FY 2011, the funding for the SOAR training program was $2,141,668. In FY 2012, the
funding for the SOAR training program was $2,355,824.
Parent Support Provider Initiative
The purpose of the National Parent Support Provider and Youth Support Specialist Initiative is to
expand the children’s behavioral health workforce in America. This initiative addresses the
critical shortage of trained workers in the field of children’s services delivery by developing core

32
competencies and conducting workforce trainings. Certification is provided through the
Certification Commission of the National Federation of Families for Children’s Mental Health
which requires a national exam and on-going training and supervision. In the first month of the
national certification (March 2012), 70 persons applied for testing.
In FY 2011, the funding for this initiative was $150,000. No SAMHSA funds were available for
FY 2012.
Child and Adolescent Psychiatry Resident Fellowship
The purpose of SAMHSA’s Child and Adolescent Psychiatry Fellowship Program is to train
child and adolescent psychiatry second year residents in public sector service and community-
based child and adolescent psychiatry policy and practice. The fellows receive an introduction
into the operation of the federal government and the American Academy of Child and
Adolescent Psychiatry, including issues related to federal and state programs for children who
have mental health challenges. The selected fellows have the opportunity to become involved
with research, as well as to improve their writing, evaluation, and presentation abilities.
This program does not have a budget, but is supported by SAMHSA staff’s time with the
fellows.
National Suicide Prevention Lifeline
An objective of the National Suicide Prevention Lifeline is to increase and improve public access
to crisis intervention services while promoting a consistent and evidence-informed approach to
crisis hotline, chat, and text services throughout the network. Since its launch in January 2005,
the Lifeline has sponsored nine Applied Suicide Intervention Skills Training (ASIST) workshops
for Trainers during which 88 Lifeline centers received training. ASIST is a training program
which offers a complete model of suicide first-aid intervention that provides a consistent
approach to helping those contemplating suicide from initial contact through follow-up. As a
result, 390 ASIST workshops have trained a total of 4,650 individuals, both professionals and
volunteers alike.
In FY 2011, funding for the Lifeline training was $100,000.
Prevention Practices in School Program – Implementing the Good Behavior Game in the
Nation’s Disadvantaged Communities
The Prevention Practices in School initiative trains teachers and school staff to implement the
Good Behavior Game (GBG) which prevents aggressive and disruptive behavior among young
children in the short term and prevents antisocial behavior and the use of illicit drugs in the
longer term.
Workforce development is continuous throughout the project cycle and an integral part of this
program. Teachers must meet specific criteria to be considered fully trained, and the coaching
models implemented in schools ensure that this is being accomplished. Training also takes place
repeatedly every school year, and teachers, coaches, and project directors are able to take booster
training sessions. Furthermore, specific aspects or parts of the GBG are also offered to non-
teaching school staff.

33
At the close of the first year of the project, more than 400 coaches and teachers have been trained
in GBG, and over 250 teachers are implementing GBG successfully in 21 school districts. In FY
2011, this program was funded at $735,000.
Suicide Prevention Resource Center
The Suicide Prevention Resource Center (SPRC) has been funded by SAMHSA since 2003 to
provide technical assistance, training, and materials to increase the knowledge and expertise of
suicide prevention practitioners and other professionals serving people at risk for suicide. SPRC
also promotes collaboration among a variety of organizations that play a role in developing the
field of suicide prevention. SPRC created a Provider Initiatives staff team to develop initiatives
to increase the capacity of health and behavioral health care providers who can play a role in
identifying and helping individuals at risk of suicide. Specifically, SPRC’s Provider Initiatives
aim to serve five provider groups with the potential to intervene effectively with suicidal
patients: primary care, emergency departments, inpatient psychiatry, substance abuse, and mental
health. SPRC’s current Provider Initiatives include the following:
• Assessing and Managing Suicide Risk: Core Competencies for Mental Health
Professionals – A one-day workshop to increase the knowledge and confidence of
behavioral health professionals to work with suicidal clients and patients. Between
October 2010 and the present, 4,267 social workers, psychologists, mental health
counselors, psychiatrists, psychiatric nurses, and other professionals completed Assessing
and Managing Suicide Risk through workshops sponsored across the country. This total
includes 1,087 professionals of the U.S. Navy.
• Counseling on Access to Lethal Means – An online workshop designed for providers who
counsel people at risk for suicide, primarily mental health and medical providers, but also
clergy and social service providers. Since the course was launched in October 2011, 364
professionals have completed the course.
• The Suicide Prevention Toolkit for Rural Primary Care Practices – Offered online, as a
downloadable PDF, and in hard-copy. The Toolkit, developed by SPRC in collaboration
with the Western Interstate Commission for Higher Education (WICHE), offers
information and tools necessary to equip primary care settings to reduce suicide risk
among their patients. The online Toolkit received 9,860 unique hits since October 1,
2011. SPRC staff co-led several of WICHE’s in-person workshops based on the toolkit
and have provided technical assistance to approximately 75 primary care practices in 20
states, including Alaska, Hawaii, Idaho, and Washington, during that time period.
In FY 2011, funding for the SPRC training program was $470,000. In FY 2012, funding for the
SPRC training program was $470,000.
National Action Alliance for Suicide Prevention
The Action Alliance is a private-public collaborative advanced by SAMHSA to support
implementation of the Surgeon General’s National Strategy for Suicide Prevention and to
increase and support both public and private efforts to reduce deaths by suicide and provide
services for persons with serious thoughts of suicide. The Clinical Care and Intervention Task
Force of the Action Alliance produced a report, Suicide Care in Systems Framework, which
34
recommended a “whole systems” model for implementing innovative, effective suicide care in
health and behavioral health populations. The Clinical Care and Intervention Task Force is
working with SPRC to develop web content, materials, and technical assistance for health and
behavioral health organizations wishing to adopt the leadership, systems, and workforce
development required for success. Another task force, the Clinical Workforce Preparedness
Task Force, is working to define the gaps, problems, or opportunities in training relevant to
suicide prevention across all health and behavioral health professions. Research has indicated
that many behavioral health professionals do not receive training in suicide risk assessment,
management or treatment. The task force is in the process of assessing the current standards in
the field, including assessing the presence of training standards with regard to suicide in all state
licensing organizations, among health and mental health professional organizations, and in post-
graduate degree programs.
Total funding for the Action Alliance was $1,000,000 in FY 2011 and $500,000 in FY 2012.
This funding covered convening, educating, report production, and other costs, including staffing
of the Action Alliance. Of this total, the amount spent on preparing workforce standards cannot
be separated from the other expenses associated with that task force or of the overall Action
Alliance.
Garrett Lee Smith Campus and State/Tribal Grantee Workforce Development Efforts
The goals of the Garrett Lee Smith (GLS) Suicide Prevention Program are: assisting
communities, colleges, and universities in their efforts to prevent suicide attempts and
completions, and to enhance services for youth aged 10-24, including college students with
mental health and substance abuse problems that may lead to suicidal thoughts or actions. The
GLS grantees use a portion of their funding to train behavioral health providers both on
campuses and in the surrounding communities. Grantees provide trainers to conduct evidence-
based clinical intervention programs for mental health providers; the overwhelming majority of
who have not yet received professional training in assessing patients for suicidal risk or
managing suicidal patients. An estimated 91,811 behavioral health care workforce persons have
been trained in the GLS state and tribal program and 30,120 from the Campus program for a total
of 121,931 trained. Some of the evidence-based trainings they conduct include Assessing and
Managing Suicide Risk, Recognizing and Responding to Suicide Risk: Essential Skills for
Clinicians, Dialectical Behavioral Therapy and Motivational Interviewing.
In 2011, funding for these cooperative agreements was $34,500,000. In 2012, funding for these
cooperative agreements was $34,300,000. As described above, some of these funds are being
used for workforce activities. However, separating out the funds used exclusively for workforce
activities has not been possible to date.
Project Linking Actions for Unmet Needs in Children's Health
Project Linking Actions for Unmet Needs in Children's Health (LAUNCH) is an early
childhood-focused, prevention and wellness promotion grant program, the goal of which is to
ensure that all young children (birth to age 8) reach their developmental potential so that they can
be successful in school and beyond. Project LAUNCH grantees work at the state, tribal and local
community levels to increase coordination across child serving systems, and improve access to
high quality care and evidence-based programs for young children and their families. Key to the

35
Project LAUNCH model is workforce development activities that increase knowledge about
healthy child development (particularly healthy social and emotional development) and
behavioral health issues. Project LAUNCH grantees conduct a wide variety of workforce
development activities with providers from multiple disciplines, including primary care
providers, teachers (early education and elementary schools), home visitors, child care providers,
child welfare professionals, and policymakers. Workforce development activities seek to: (1)
increase knowledge of early child development, particularly social and emotional development,
and children’s behavioral health; (2) train providers on the appropriate use of developmental
screening and assessments (including administration and interpretation); (3) train providers in
evidence-based prevention practices, including individual, group, child- and family-focused
interventions; and (4) help child care providers and educators to create center and classroom
environments that foster healthy child development and appropriately address behavioral
challenges.
In the first two and half years of the Project LAUNCH Initiative, grantees trained over 11,000
providers in 24 states and communities.
Grantees generally spend about 10-12 percent of their budgets on workforce development.
Depending on the cohort (as each cohort is funded at a different level) this comes out to about
$70,000–$100,000 per year/grantee. In addition, at the initiative level, the Technical Assistance
Center (with an annual budget of $1.72 million) spends roughly 45 percent of its budget on
training and workforce development for grantees.
In FY 2011, the approximate annual expenditure on workforce development through Project
LAUNCH was about $2,700,000. In FY 2012, the approximate annual expenditure on
workforce development through Project Launch was about $3,749,000.
National Child Traumatic Stress Network
Through cross-network collaborations, the National Child Traumatic Stress Network (NCTSN)
groups have developed intervention approaches and associated training and dissemination
products that are now being used and evaluated to improve treatment and services for children
and adolescents who experience domestic and community violence, medical trauma, refugee
trauma, out-of-home placement, and traumatic grief.
The NCTSN has provided over 20,000 trainings to over one million people and has developed
resources for child/adolescent trauma on the NCTSN website, which receives more than 2,000
visits a day and houses over 150 Network-developed resources downloaded more than 50,000
times a year. They have developed online training in evidence-based trauma interventions, one
of which has had more than 20,000 participants complete the program. A Learning Center
website has also been developed that provides access to 10 expert webinars on trauma topics that
have been viewed by over 7,000 individuals. In addition, the Network has developed an
intensive learning collaborative model for service providers and conducted 17 of these learning
collaboratives for more than 800 service providers.
In FY 2011 and FY 2012, the funding for NCTSN grantees to conduct provider training and
other workforce development activities was approximately $10,000,000 per year.

36
Center for Promoting Alternatives to Seclusion and Restraint Through Trauma-Informed
Approaches and the National Center for Trauma Informed Care
The purpose of this Center is to provide national leadership in reducing the pervasive, harmful,
and costly health impact of violence and trauma by integrating trauma-informed approaches
throughout health and behavioral health systems, and to divert people with substance abuse and
mental health disorders from criminal and juvenile justice systems into trauma-informed
treatment, supports, and recovery. The goals for the Center are to expand the use of trauma-
informed practices to end the use of seclusion, restraint, and other coercive practices. The
contract tasks provide for the development of a structured learning process to be used in
implementation of trauma informed care in a collaborative and integrated manner that integrates
consumer/ survivor voice and leadership, including training, virtual training, remote and on-site
technical assistance, meeting logistics, product development, process evaluation, and knowledge
dissemination.
In 2012, the Center completed 157 training/technical assistance events. Forty-one events
focused principally on trauma-informed practices and 116 focused on the reduction of seclusion
and restraint through trauma-informed practices. Many requests involved multiple systems, and
project staff work with applicants to encourage collaboration and cross-systems training
whenever possible. Approximately 10,000 people received training/technical assistance through
this contract since 2010. In addition to the trainings, four webinars were conducted. The Center
also produced a number of products including reports, issue briefs and guides, and have
convened conferences focused on the use of peers to prevent the use of seclusion and restraints
and implementing trauma informed care in services systems.
The budget for the Center for FY 2011 was $2,477,198. The FY 2012 budget was $2,612,681.
SAMHSA GAINS Center for Behavioral Health and Justice Transformation
The SAMHSA GAINS Center's primary focus is on expanding access to community-based
services for adults diagnosed with co-occurring mental illness and substance use disorders at all
points of contact with the justice system. The SAMHSA GAINS Center developed curricula to
train criminal justice professionals to understand the impact of trauma on men and women with
serious mental illness and to improve safety by learning new ways to interact with people who
are traumatized. The training is targeted to police, community corrections (probation, parole,
and pre-trial service officers), and court personnel (judges, attorneys, case managers and
treatment providers). Over the past 12 months, 350 people have been trained in 10 cities.
The program also includes a train-the-trainer curriculum that focuses on justice specific
community service providers, court administrators, court deputies, district and assistant district
attorneys, judges, probation officers, re-entry staff, treatment court coordinators, forensic or
clinical caseworkers, community service boards, and state mental health and substance abuse
agencies. In February 2012, a day and a half train-the-trainer event was held for 36 individuals
including community service providers, court administrators, court deputies, district and assistant
district attorneys, judges, probation officers, re-entry staff, treatment court coordinators, forensic
or clinical caseworkers, community service boards, and state behavioral health agencies.

37
In FY 2011, funding for the GAINS Center training program was $70,000. In FY 2012, funding
for the GAINS Center training program was $70,000.
Bringing Recovery Support Services to Scale – Technical Assistance Center Services
The Bringing Recovery Supports to Scale Technical Assistance Center Strategy (BRSS TACS)
contract meets a major need to identify effective approaches to develop and sustain behavioral
health care recovery support initiatives in states and systems across the nation. Specifically, it
will provide policy and practice guidelines and information and technical assistance to states,
systems, providers, and others to assist in transforming behavioral health services.
This project intends to support the expansion and integration of recovery supports via the
development and operation of a Resource Center on Recovery Supports. This will be
accomplished through three main tasks – policy and practice analyses, training and education,
and technical assistance. The Resource Center is a partnership among people in recovery from
addictions who have experience working in the addictions recovery field and people in recovery
from mental health problems and conditions and/or serious emotional disabilities who have
experience working in the mental health consumer field, as well as people with co-occurring
disorders, trauma, and a variety of allies, supporters, and other stakeholders in recovery-oriented
services and systems.
As part of SAMHSA's BRSS TACS initiative, SAMHSA hosted an Expert Panel on the
provision of peer recovery support services which included components specifically focused on
the development of Recovery Coaches/Peer Specialists. One outcome of this effort is to develop
guidelines for States working with Recovery Coaches and Peer Specialists working with both the
mental health and addictions recovery populations.
In FY 2011, this effort totaled approximately $50,000. In FY 2012, this effort totaled
approximately $50,000.
The National Network to Eliminate Disparities in Behavioral Health
In 2008, SAMHSA established the National Network to Eliminate Disparities in Behavioral
Health (NNED) to promote workforce development for community-based behavioral health
organizations that serve diverse racial, ethnic and sexual minority communities.
These organizations often have limited resources for and access to training for their staff. The
NNED, a virtual network of these community-based provider organizations, provides the
following opportunities to advance the capacity and strengthen the quality of this workforce:
• Best practices in implementation science – NNEDLearn provides six training tracks on
selected evidence-based and culturally adapted practices. These are practices that have
been selected by the NNED membership. Participants in these tracks convene with a
master trainer for a two-day training, and continue with six months of regular follow-up
coaching to support implementation of the newly acquired practice. Examples of training
tracks include Motivational Interviewing, Culturally Adapted Cognitive Behavioral
Therapy for Latinos, Empowering Our Spirit Suicide Prevention for Tribes, and
Strengthening Families, Seeking Safety. In the past two years of the NNEDLearn

38
training, 250 participants representing over 45 community-based organizations have
participated in this intensive, skill-building training.
• Virtual Communities of Practice – Training on a specific practice through webinars,
teleconferences and a virtual online “office space” and discussion forum. Each
Communities of Practice (CoP) is led by an expert trainer or developer of the practice.
Examples of interventions addressed in these CoPs include Project Venture (an
evidenced-based substance abuse prevention practice for tribal youth), Multi-Family
Group Treatment for Latino Families, and Bienvenido – A Mental Health Promotion for
Latino Immigrants. Nine CoPs have been offered, serving over 150 practitioners from
community-based behavioral health organizations.
• NNEDShare – A repository of emerging and innovative interventions geared to
improving outreach, engagement, practice and outcomes for diverse cultural populations.
This is a searchable database on the NNED website that promotes cross-agency sharing
and peer-to-peer training and technical assistance. The NNED has been effective in
bringing workforce training opportunities and in–language training to diverse
community-based organizations.
Evidence-based and community-culturally based practices have been shared and collaborations
built among the participants in the NNED, toward the goal of advancing quality care for these
communities. Since 2008, the NNED has grown from 35 to 534 community-based organizations
in 2012.
In both FY 2011 and 2012, the NNED initiative was funded at $625,000. This activity is funded
out of the agency overhead funds, consistent with our 501(d)(3) authority. The 501(d)(3)
authority allows SAMHSA to tap programs to “carry out administrative and financial
management, policy development & planning….functions.”
Provider Business Operations Contract
In light of coming changes brought by the opportunities of the Affordable Care Act, SAMHSA is
undertaking a special effort to train and develop learning collaboratives for providers serving
persons with behavioral health needs in a specialty setting. This effort will assist providers with
business planning, compliance requirements, use of HIT, billing requirements, and the process of
being part of a provider network for an insurance company. Without this help, many specialty
providers will not be ready to move into the world of provider networks that are part of Qualified
Health Plans and increasing managed care in Medicaid and employer-based insurance
mechanisms. Furthermore, the number of available specialty providers serving persons with
more extensive addiction and mental health needs will decline below already unacceptable
levels.
FY 2012 funding for this effort includes $1,627,972. This activity is funded out of the agency
overhead funds, consistent with our 501(d)(3) authority. The 501(d)(3) authority allows
SAMHSA to tap programs to “carry out administrative and financial management, policy
development & planning….functions.”

39
HRSA Behavioral Health Workforce Programs
HRSA recognizes the importance of behavioral health and the links among mental, physical and
emotional wellbeing. This is reflected across HRSA’s broad portfolio of programs and services.
HRSA promotes integrated behavioral health service delivery in primary care settings and
effective referral arrangements, when indicated, to specialty behavioral health provider
organizations.
Delivering mental health and addiction services in primary care settings helps to reduce the
prejudice and discrimination often experienced by persons with mental health or substance abuse
problems. Serving people with behavioral health concerns in collaborative primary care settings
supports a “no wrong door” approach to care.
The framework HRSA uses is built on efforts to position primary care within the broader context
of community health, to align primary care and behavioral health seamlessly, and to consistently
build relationships with stakeholders to improve the delivery and access of health and behavioral
health services to vulnerable populations. Examples of HRSA programs focusing on behavioral
health include the following.
Health Centers
The Affordable Care Act makes a major investment in Health Centers expanding and
strengthening these providers. Today these centers operate 8,500 clinics across the country,
serving over 20 million patients regardless of their ability to pay. Two-thirds of health centers
provide mental health treatment or counseling services, and one-third provides substance abuse
counseling and treatment. According to health center data, depression is among the top ten
primary reasons that patients visit a health center.
These services are provided in large part through over 5,000 FTE behavioral health providers in
health centers. This includes more than 400 psychologists, 400 psychiatrists, nearly 1,400
licensed clinical social workers, 1,000 licensed mental health counselors, and 875 substance use
disorder treatment providers. HRSA provides training and resources for these professionals and
for the primary care professionals to increase their knowledge and skills about the prevention and
treatment of mental and substance use disorders.
HRSA encourages its health center grantees to include the SBIRT approach; and SBIRT is now a
service indicated on the yearly health center data reporting system that HRSA administers.
HRSA Workforce Specific Programs
Strengthening the behavioral health workforce is a critically important component of HRSA’s
overall efforts to expand the nation’s health care workforce. HRSA’s National Health Service
Corps, which also received strong support through the Affordable Care Act, are health
professionals who provide primary health care services in underserved communities in exchange
for either loan repayment assistance or scholarships to help pay the costs of their medical
education. With investments from the Affordable Care Act, the Corps had over 9,908 health
professionals serving in underserved communities in 2012.

40
In 1995, when psychologists, social workers, psychiatrists and other behavioral health providers
were first admitted to the Corps, there were exactly five awardees. As of September 2012,
roughly three out of 10 NHSC clinicians in the field are primary care mental health or substance
abuse practitioners for a total of 2,809 practitioners in the following disciplines: psychiatrists,
clinical psychologists, clinical social workers, licensed professional counselors, marriage and
family therapists, and psychiatric nurse specialists. NHSC mental and behavioral health
practitioners may provide substance abuse treatment.
HRSA also supports the Graduate Psychology Education Program which provides grants to train
psychologists working with underserved populations. For academic year 2010-2011, there were
710 trainees, of which 416 (58 percent) served in medically underserved communities.
HRSA has a new Mental and Behavioral Health Education and Training Grants Program that
aims to increase the number of social workers and psychologists who pursue clinical work with
high-need and high-demand populations. As a result of this funding, accredited graduate social
work schools and accredited psychology schools will be able to increase their overall number of
enrolled students, create more field placement and internship slots for students, and ultimately
increase the number of clinical providers working with underserved populations. These
professionals may work with individuals with mental illness, with substance use disorders, or
with both.
HRSA’s Veterans’ Mental Health Project was created to address the post-deployment mental
health and substance abuse issues of veterans and their families through the training of primary
care providers across the nation.
SAMHSA - HRSA Workforce Collaborative Initiatives
Implementation of the Affordable Care Act will require an expanded and appropriately trained
workforce. Many of the authorized workforce activities were delegated to HRSA for
implementation either through the expansion of existing programs or new authorizations. To
better integrate the delivery of behavioral health and primary care in this new environment,
SAMHSA and HRSA began a number of collaborative efforts to enhance the workforce. Some
of these activities are supported through a formal IAA, while others reflect a more informal
emphasis on data analysis, model development for integrated primary and behavioral health care,
technical assistance for integrated programs or those wishing to develop integrated approaches,
information sharing, joint training, and other collaborative efforts.
Center for Integrated Health Solutions
SAMHSA and HRSA are jointly funding a national resource center that provides training and
technical assistance to community behavioral health programs, community health centers, and
other primary care organizations. The resource center helps develop models of integrated care
across behavioral health and primary care. This effort recognizes the increasing role primary
care plays in screening, preventing and treating mental health and substance abuse problems, and
the need for persons with serious mental illness to have their primary health care needs addressed
in the same setting where they receive care for the mental health condition(s).
41
The CIHS provides training and technical assistance on the bi-directional integration of primary
and behavioral health care and related workforce development. The CIHS provides training and
technical assistance to the currently funded 64 community behavioral health organizations that
have SAMHSA Primary and Behavioral Health Care Integration (PBHCI) grants as well as to
community health centers and other primary care and behavioral health organizations.
The CIHS has engaged in a wide array of activities that impact the full continuum of workforce
communities under PBHCI. Some of the highlights are below.
Curriculum Development
• Psychiatrist Training Curriculum – Developed a 6 Module Psychiatrist Curriculum
designed to increase psychiatrists’ capacity to practice and/or consult in integrated health
settings.
o Module 1: Introduction to Primary Care Consultation Psychiatry
o Module 2: Building a Collaborative Care Team
o Module 3: Psychiatrist Consulting in Primary Care
o Module 4: Behavioral Health in Primary Care
o Module 5: Medical Patients with Psychiatric Illness
o Module 6: The role of the Psychiatrist in the Public Mental Health System.
• Whole Health Action Management – Developed a national curriculum and pilot tested the
curriculum with consumers and staff representatives from 50 out of 56 SAMHSA PBHCI
grantees. The program creates workforce capacity by preparing consumers to serve as
health educators and coaches. The two-day Whole Health Action Management Peer
Support Training guides participants through a person-centered planning process to set a
whole health and resiliency goal. Once the goal is set, the participant guide shifts to
creating and self-managing new health behavior by implementing an eight-week whole
health peer support group that engages in a weekly action plan for success. The training
is designed to support the emerging peer workforce to move into new health integration
service models like health homes.
• Primary Care Physician Training Curriculum – Developed a Primary Care Physician
Training Curriculum designed to create capacity for primary care physicians to treat and
support individuals with a serious mental illness. Prevalence, Serious Mental iIllness
Characteristics, Pharmacological and Behavioral Interventions are highlighted.
o Module 1: Working with Patients with a Severe and Persistent Mental Illness; What
Should Primary Care Physicians Know?
o Module 2: Update on Psychopharmacology for Primary Care Physicians; Depression
and Anxiety Part I & II.
• Masters Level Social Work Competency-Based Curriculum – The Integrated Healthcare
Curriculum for Schools of Social Works is a competency-based curriculum to prepare
Masters of Social Work students for behavioral health practice focused on integrative and
collaborative primary-behavioral health care. The curriculum will prepare future Masters
level social workers to enter the workforce with the needed competencies to provide and
lead integrated health care.
42
Trainings
• Health Navigator/Care Management Training – The Health Navigator/Care Management
training program is designed to transform traditional mental health case management
programs into assuming responsibility for the whole health of the individuals they serve.
The day-long training covers a variety of topics related to a new and broader knowledge
base for case managers. The program conducted seven, two-day Health Navigator
Trainings for SAMHSA PBHCI grantee organizations.
• Mental Health First Aid Training – Mental Health First Aid (MHFA) is a public
education program that creates capacity within communities to identify, understand, and
respond to signs of mental illnesses and substance use disorders. MHFA introduces
individual participants to risk factors and warning signs of mental health problems and
substance use disorders, builds understanding of their impact, and overviews common
treatments. Those who take the 12-hour course to certify as Mental Health First Aiders
learn a five-step action plan encompassing the skills, resources and knowledge to help an
individual in crisis connect with appropriate professional, peer, social, and self-help care.
o Trained five rural health centers in MHFA.
o MHFA training for federal staff.
o Provided statewide Primary Care Association training to Northwest Region for 25
FQHCs.
o Provided MHFA Training for three federal agencies.
o Completed a Spanish translation of MHFA.
• Suicide Prevention Training for Primary Care Practices – This training is targeted to
increasing the capacity of primary care practitioners and behavioral health professionals
who work in or frequently collaborate with primary care, rural providers, FQHC’s, and
residency programs in family medicine to identify and intervene with those at risk of
suicide. Seventy-six percent of individuals who die by suicide had contact with their
primary care practitioners in the month prior to their suicide. The training supports the
implementation of state-of-the-art suicide prevention practices while minimizing the
disruption of normal operations. The training is tailored to meet the needs of the primary
care site or educational center. CIHS conducted four trainings in rural communities.
• Integrated Care Conference Track – The NACHC developed an integrated care track for
FQHC on the importance of Integrated Healthcare and factors they could consider when
training their workforce.
Integrated Health & Wellness Training Scholarships
• Cherokee Integrated Health Model – CIHS provided two scholarships for SAMHSA
PBHCI Grantee teams to visit Cherokee Health Systems to learn from integrated
treatment team approaches.
• University of Massachusetts Certificate Program in Primary Care Behavioral Health –
CIHS provided scholarships for up to 80 individuals from PBHCI grantee organizations
the opportunity to participate in the Certificate Program in Primary Care Behavioral
Health provided by the University of Massachusetts Medical School.
• University of Colorado Denver Tobacco Cessation and Wellness Program – CIHS
contracted with the University of Colorado Tobacco Cessation and Wellness Program to
develop an assessment tool to provide direct technical assistance. The assessment tool is
being piloted with SAMHSA PBHCI grantees.
43
Stakeholder Meeting
• Workforce Issues: Integrating Substance Abuse Services into Primary Care Summit –
CIHS provided technical and logistical support to the White House Office of National
Drug Control Policy, SAMHSA, and HRSA hosted event about Workforce Issues:
Integrating Substance Abuse Services into Primary Care Summit on August 10-11, 2011.
Deliverables included Meeting Planning, Workforce Report, Presentation, and Summit
Summary Report.
Workforce Webinars
CIHS conducts various webinars targeted towards different workforce areas, for example:
• Sharing of information in an electronic environment.
• Specific confidentiality and consent law and regulations for certain substance abuse
treatment records (42 CFR Part 2).
• Motivational Interviewing.
• The role and practice of peer supports.
• National Health Service Corp (NHSC).
• InSHAPE approach to wellness for individuals with a serious mental illness.
• Short-term behavioral health interventions in primary care.
• Smoking cessation, for practitioners working in FQHCs.
Products
• Accessing the National Health Service Corp: A Guide for Community Behavioral Health
Providers and Primary Care Partners – This guide assists behavioral health sites in
becoming NHSC-approved sites and expanding the behavioral health workforce in those
communities. The guide includes opportunities to recruit practitioners and clinicians
interested in NHSC employment and an overview of the NHSC loan repayment benefits.
• CIHS Workforce Guiding Principles – This document is a compilation of areas and
characteristics that organizations implementing integrated health strategies can use to
guide the development of workforce strategic plans.
• Workforce Resource Inventory – This inventory is a compilation of workforce resources
(trainings, articles, literature, tools) related to integrated primary and behavioral health
care.
• Gap Analysis of Integrated Health Workforce – This analysis is a review and synthesis of
existing literature and resources related to integrated primary and behavioral health
workforce to identify gaps and develop recommendations for future initiatives.
• Peer Roadmap – This product outlines the states that have incorporated a definition for
the use of peers for the delivery of services within their Medicaid State Plan.
In FY 2011, funding for this cooperative agreement was $350,000 from HRSA and $5 million
from SAMHSA’s PBHCI program funding As described above, funds are being used for
workforce activities; however, separating out the funds specific to workforce development
activities has not been possible, as many activities support grantees, develop workforce, provide
training, and produce and disseminate materials at once.

44
In FY 2012, the funding from SAMHSA for this Center was limited by Congressional
Appropriations to $2,000,000, and now supports only SAMHSA grantees. HRSA continued to
contribute $365,000 for this joint effort allowing CIHS to maintain a broader impact within the
limits of available funding.
SAMHSA and HRSA Behavioral Health Minimum Data Set Project
As has been referenced in this report, the lack of any national database or information on the
addiction services and mental health workforce is a major hindrance in identifying and
remedying issues. In 2011, SAMHSA entered into an IAA with HRSA to ensure the inclusion of
the behavioral health workforce in HRSA’s development of a Minimum Data Set (MDS) for the
health care workforce. The purpose of this IAA is to:
• Develop guidelines for minimum data sets;
• Support and assist stakeholders with the collection of behavioral health professions data;
• Provide technical assistance and resources to enhance stakeholder data collection efforts;
• Build a national behavioral health workforce dataset; and
• Identify possible methods for providing federal agencies access to such data.
In order to accomplish the objectives of this project, HRSA and SAMHSA are identifying which
occupations to include in the behavioral health workforce database, data sources, and what data
are being collected; developing the questionnaire to be used; identifying the organizations in
each chosen behavioral health care profession that are best able to implement the MDS; and
recruiting these organizations to participate in the MDS.
This is a one-year project that is underway, with HRSA’s National Center for Healthcare
Workforce Analysis taking the lead. SAMHSA and HRSA are working closely together, with
SAMHSA staff providing subject matter expertise to HRSA staff that provides oversight and
management of the project.
In FY 2011, the budget for this project was $500,000. No SAMHSA funds were available for
FY 2012.
Military Culture Training
The purpose of the IAA is to facilitate cooperative efforts between SAMHSA and HRSA,
Bureau of Health Professions in order to provide technical assistance, competency and
curriculum development, continuing education, and related evaluation to the primary care and
education field related to the mental and behavioral health and substance abuse issues of veterans
and their families.
SAMHSA provides technical consultation on the mental and behavioral health and substance
abuse needs of veterans and their families to the project team, as requested, and provides
necessary feedback, review, and comment to HRSA in order to provide technical direction to the
contractor. HRSA through the National AHEC Organization (NAO) provides technical
assistance to the primary care and education workforce focused on the mental and substance
abuse issues of veterans and their families to include curriculum development and inter-
professional continuing education for health care providers on the mental and substance abuse

45
issues of veterans and their families. In addition, the NAO will evaluate the effect of the
continuing education curriculum/courses on the practice of participating health care providers.
SAMHSA provided $500,000 in FY 2011 to support this effort. No SAMHSA funds were
available for FY 2012.
Other SAMHSA/HRSA Collaborations
Given the importance of workforce issues, SAMHSA and HRSA are working to optimize the
potential to collaborate, maximizing the efficiency of authorized and appropriated funds.
Examples of such collaborations include HRSA’s request for SAMHSA’s assistance on the
selection of behavioral health training and speakers for the NHSC Awardee conferences, which
are conducted several times a year for those in the loan repayment program. The topics are
reviewed annually and are selected based on the needs expressed by the conference attendees and
the evidence-based practices that are available.
Another example is the coordination of education and training opportunities in HBCUs through
the respective contracts that SAMHSA and HRSA have with the Morehouse School of Medicine.
Though only just begun, the goal of this collaboration is to foster more cross-training that would
enhance integration and provide expanded audiences for the offerings from each of these centers.
SAMHSA and HRSA are also identifying information and materials available from SAMHSA
needed by HRSA funded community health centers to make those resources available to
practitioners in those settings.
SAMHSA and HRSA are also working with other HHS agencies and offices to develop training
for community health workers on the use of SBIRT. This training will be conducted in
collaboration with the Department of Labor and through a HRSA-funded AHEC provider, with
funding from HRSA, SAMHSA and the Office of Assistant Secretary for Health.
SAMHSA/HRSA Joint Listening Session
Recognizing the importance of the behavioral health workforce, SAMHSA and HRSA jointly
hosted a listening session for behavioral health stakeholders on June 5, 2012, specifically to
discuss and identify behavioral health workforce issues and approaches to addressing them.
5
The joint listening session focused on four behavioral health workforce areas: (1) capacity; (2)
data; (3) training and education; and (4) the non-traditional workforce. This summary
incorporates the major themes that SAMHSA and HRSA heard during this listening session, as
well as written comments received after the meeting. SAMHSA and HRSA thank those in
attendance, both in person and by teleconference, for their involvement and efforts on workforce
issues, and also those who took the time to provide additional written comments.
Behavioral Health Workforce Capacity
5
A summary of current HRSA and SAMHSA workforce activities related to topics raised or addressed at the joint
listening session are captured in Appendix A, some of which are also captured in the body of this report.

46
Increasing the behavioral health workforce capacity was a major area of concern and the themes
from the discussants included:
• Continue to build behavioral health workforce capacity through the NHSC.
• Develop, recruit and support for behavioral health professions at all educational levels.
• Improve professional training through development of more internship placements in
safety net provider locations, such as health centers, and provide direct student support
for education through scholarships and loan repayment.
• Encourage the use of technology to expand the reach to clinicians, such as use of Internet
capabilities for therapies, while ensuring clear standards and monitoring of professionals
to assure public protection.
• Modeled on the SAMHSA-HRSA CIHS, expand efforts to provide professional cross
training of staff in both primary and behavioral health care to promote integrated care for
persons with mental health or addiction problems.
• Recruit potential workers earlier in the educational pipeline to encourage interest in
behavioral health careers.
• Promote development of career development pathways, especially for substance abuse
counselors.
• Identify and address the state credentialing and licensure issues that make it increasingly
difficult for those with lower level licenses to bill independently in insurance-based
payment systems.
• Address inadequate payment issues for services performed by community mental health
and substance abuse centers.
Data Needs and Collection Processes
Several of the attendees expressed enthusiasm for the current SAMHSA-HRSA MDS initiative
and recommended:
• Continue support to develop the MDS for behavioral health professionals as it will
provide core, consistent, and continuous data on demographics, practices, and settings.
• Review current public and professional association data collection efforts to see what
workforce elements they contain that could be incorporated into the MDS.
Training and Education Needs
A number of key themes arose during this part of the listening session including:
• Increase efforts to train the workforce in cultural diversity (including lesbian, gay,
bisexual, and transgender [LGBT] issues) and promote internship training in culturally
diverse settings.
• Expand pre-professional efforts such as cross-training of behavioral staff and primary
care staff regarding integrated care and disseminate information on how to develop
effective multidisciplinary primary and behavioral health teams.
• Encourage the incorporation of technology to more effectively deliver training and
education.
• Promote training on motivational interviewing and other evidence-based practices for
behavioral health services.
47
• Foster effective methods of teaching evidence-based practices to increase adoption in the
field, such as greater use of clinical supervision and applied continuing education
programs.
• Encourage the inclusion of peers, persons in recovery, mental health consumers, and
family members in professional education and training programs and in research
programs that identify evidence-based practices.
• Assist providers and persons in recovery to develop and capture practice-based evidence
to identify effective and emerging practices.
• Prepare primary and behavioral health safety net professionals to successfully join
provider networks of managed behavioral health organizations.
Non-Traditional Workforce
Comments on the growth and greater use of the non-traditional workforce related to such issues
as the need for appropriate training and education, as well as increased treatment capacity. The
non-traditional workforce needs to be included in data collection efforts, including those in
recovery from mental and substance use conditions, as well as community health workers,
patient navigators, and health educators. Additional recommendations included:
• Continue to support the clarification of needed competencies for peers and family
members; encourage creation of a peer professional career ladder, including training and
supervision of peers by peers.
• Collect and disseminate information on state-specific descriptions of peer services for
Medicaid programs and other insurers, including: identification of peer services that are
reimbursed; descriptions of coverage limitations or specific supervision or training
requirements; payment mechanisms and rates; and how to encourage the greater inclusion
of peers in integrated health care teams.
• Encourage funding of innovations and services that include peers in accountable care and
other alternative payment programs, as well as in block grant and competitive grant
programs where possible.
• Build bridges between peer counselors, health educators, and community health workers
in primary care settings; encourage their participation in prevention and wellness issues
as well as programs or activities that help people maintain their recovery.
• Include peers as navigators and enrollment/eligibility assistants in state and federally
facilitated health insurance marketplaces and in Medicaid expansion programs.
• Work with community colleges to develop curriculum and supports for peer and other
alternative practitioners to assist licensed behavioral health practitioners.
Conclusion
The behavioral health workforce in the United States is dedicated, passionate and capable.
Whether conducting prevention activities or services; serving persons with addictions, persons
with mental illness, persons with both, or their families; or supporting people in recovery, they
are without question a small but mighty force working to protect, maintain and improve the
health of America. Yet, as a whole, the workforce is too few, aging into retirement, inadequately
reimbursed; inadequately supported and trained, and facing significant changes affecting
practice, credentialing, funding, and ability to keep up with changes in practice models driven by
48
changing science, technologies and systems. Additionally, the aging of the population, the many
new veterans with behavioral health needs and individuals with new access to coverage making
it possible for them to get treatment for their addiction and/or mental illness will strain the
already overtaxed workforce. Prevention, treatment and recovery supports will not be available,
if there are not sufficient numbers of adequately trained preventionists, mental health and
addictions professionals, and licensed or certified peer and alternative providers.
While SAMHSA and HRSA, as federal agencies, collaborate extensively and have significant
programs and activities to train and support new and existing providers, each is limited by its
authorities and its funding in what they can do to address the critical issues.
The issue of workforce development in the behavioral health field has long been a critical one.
Recent moves in the behavioral health care field toward services integration along with the
passage of health reform legislation have further heightened the need for the development of a
well-trained, highly skilled, diverse and productive workforce. Now, more than ever, the
scarcity of strong, standardized data on the workforce poses itself as an issue to be addressed.
SAMHSA and HRSA will continue to include this significant issue in their strategic planning
and programming to the extent their authorities and funding allow. They will also continue their
collaborative efforts with each other and with other federal partners to ensure that the needs of
the addiction and mental health workforce are identified and at the forefront as other health care
workforce issues are discussed and addressed.

49
APPENDIX A:
Examples of SAMHSA-HRSA Activities Related to Behavioral Health Workforce –
Listening Session Summary
On June 5, 2012, the Substance Abuse and Mental Health Services Administration (SAMHSA)
and the Health Resources and Services Administration (HRSA) hosted a listening session with
stakeholders that focused on four behavioral health workforce areas: capacity, data, training and
education, and the non-traditional workforce. The thoughtful input, both at the meeting and in
correspondence, is being considered as both agencies move forward with program plans. To
assist in understanding SAMHSA and HRSA workforce activities already underway, the
following summary of current SAMHSA and HRSA activities was developed.
Behavioral Health Workforce Capacity
OVERALL CAPACITY
The Mental and Behavioral Health Education and Training Grants (MBHETG) Program:
HRSA has awarded 24 accredited social work and psychology programs with 3-year funding.
The MBHETG program encourages education and training addressing the behavioral health
needs of high-need and high-demand populations by: (1) increasing the number of enrolled
graduate social work and psychology students; and (2) creating more internship and field
placement slots to increase the number of knowledgeable clinical providers working with high-
need and high-demand populations.
National Health Services Corps (NHSC):
HRSA’s NHSC builds healthy communities by strengthening the health care workforce and
continues to support individuals in behavioral and mental disciplines and practices/sites. The
SAMHSA-HRSA Center for Integrated Health Solutions (CIHS) has developed a guide to assist
behavioral health sites in understanding the NHSC and the process for becoming an approved
NHSC site (see http://www.integration.samhsa.gov/sliders/NHSC_doc.pdf
).
Advanced nursing educational efforts include behavioral health:
HRSA’s Advanced Education Nursing Traineeship (AENT) supports traineeships for primary
care Nurse Practitioners (NP), some of which are psychiatric/mental health NPs. The Advanced
Nursing Education (ANE) program and the Nurse Education, Practice, Quality, and Retention
(NEPQR) program promote inter-professional education with behavioral health social workers.
INTEGRATED PRIMARY CARE AND BEHAVIORAL CARE WORKFORCE
Integrated Summit: In August 2011, ONDCP, HRSA, and SAMHSA sponsored the “Workforce
Issues: Integrating Substance Abuse Services into Primary Care Summit.” Identified workforce
needs included: increasing addictions training in primary care professional’s curricula, the
necessity for career ladders and greater role definitions between primary care and behavioral

50
health specialists.
Graduate Psychology Education (GPE) Program:
HRSA grants in the GPE program support interdisciplinary training for health service
psychologists to provide mental and behavioral health care services to underserved populations,
such as those in rural areas, older adults, children, chronically ill or disabled persons, and victims
of abuse or trauma, including returning military personnel.
Geriatric Training for Physicians, Dentists, and Behavioral and Mental Health Professionals
Program: The Geriatric Training for Physicians, Dentists, and Behavioral and Mental Health
Professionals Program supports 1-year faculty retraining and 2-year fellowship programs to
assist physicians, dentists, and behavioral and mental health professionals who teach or plan to
teach geriatric medicine, geriatric dentistry, or geriatric behavioral and mental health. The
program supports learning on caring for elderly people at different levels of wellness and
functioning. It provides training with elderly from diverse socioeconomic, racial, and ethnic
backgrounds in a range of services, such as geriatric consultation, acute care, dental care,
psychiatry, day and home care, rehabilitation, extended care, ambulatory care, and community
care for older people with mental retardation.
INTEGRATED PRIMARY CARE AND BEHAVIORAL CARE IN THE WORKFORCE
Integrated Summit: In August 2011, the White House Office of National Drug Control Policy,
HRSA, and SAMHSA sponsored the “Workforce Issues: Integrating Substance Abuse Services
into Primary Care Summit.” The summit identified many workforce needs, including:
increasing addictions training in primary care professional’s curricula, the necessity for career
ladders, and a greater role for definitions between primary care and behavioral health specialists.
Multidisciplinary training includes behavioral health under Area Health Education Centers
(AHECs):
HRSA’s AHEC grantees (i.e., medical schools, nursing schools, and health sciences centers)
organize interdisciplinary and inter-professional training involving psychologists and other
behavioral health professionals as practicable. Specific behavioral health topics include
motivational interviewing, other evidence-based practices, and inclusion of peers/consumers in
education and training.
Regional workforce training:
SAMHSA’s Addiction Technology Transfer Centers (ATTCs) accelerate lasting change in
behavioral health care systems by translating, disseminating and promoting the adoption and
implementation of effective and culturally-sensitive clinical practices. They offer distance
education productions and workforce development. In addition to providing region-specific
training and systems change efforts, the ATTC Network has areas of national focus that include
leadership institutes and collaboration with the National Institute on Drug Abuse (NIDA) to
develop products and promote the adoption of evidence-based practices.
Behavioral health workforce in health centers:
HRSA’s Bureau of Primary Health Care (BPHC) is working through the SAMHSA-HRSA CIHS

51
to build workforce capacity across health centers with limited behavioral health capacity through
the provision of training and technical assistance on integrated care.
CROSS TRAINING BETWEEN PRIMARY CARE AND BEHAVIORAL CARE
Training in pain management for prescribing physicians, nurses and dentists:
SAMHSA supports face-to-face and online continuing medical education (CME) courses,
entitled Prescribing Opioids for Chronic Pain: Balancing Safety & Efficacy, on safe opioid
prescribing for chronic pain for primary care physicians, oral surgeons, advanced practice nurses,
and physician assistants.
Training physicians for prescribing buprenorphine:
Through the Prescribers Clinical Support System for Buprenorphine (PCSS-B), SAMHSA offers
the eight hour training required to apply for a buprenorphine waiver required to prescribing
privileges. The training is a combination of CD-based training and face-to-face training.
Screening, Brief Intervention and Referral to Treatment (SBIRT) Medical Residency Training:
SAMHSA supports the SBIRT Medical Residency Training grants, designed to train the next
generation of physicians in SBIRT practice. This program includes curriculum development and
training for current residents and the primary care community in SBIRT practices.
Psychologists in Health Centers:
In July 2011, HRSA’s BPHC hosted a grantee training specific to the hiring of psychologists at
health centers: “The Value of Psychologists in Health Centers.” Topics covered included
current statistics on psychologists in health centers and how integrated service increases financial
outcomes and quality of care; improves clinical staff recruitment and retention; and provides
other benefits for the health centers.
PIPELINE ACTIVITIES FOR BEHAVIORAL HEALTH PROFESSIONS
The Health Careers Opportunity Program (HCOP):
HRSA’s HCOP exposes students throughout the educational pipeline to a wide array of health
careers, including careers in behavioral health. The grantees provide academic enhancement,
structured summer programming in health centers, academic health careers clubs and grade-
specific curriculum.
NHSC pipeline activity:
HRSA’s NHSC attended the National Association of Student Financial Aid Administrators
National Conference in Chicago in July 2012 and will generate awareness amongst financial aid
administrators, including those in the mental and behavioral health field.
AHEC pipeline activities:
HRSA’s AHEC grantees provided health career training and/or academic enhancement
experiences to 9-12th graders that included behavioral health careers. Emphasis is placed on

52
outreach to underrepresented minority populations, educationally or economically disadvantaged
individuals, and/or rural populations.
WORKFORCE DIVERSITY AND CAREER LADDERS
National Network for the Elimination of Disparities in Behavioral Health (NNED):
SAMHSA’s NNED works to increase capacities to address the behavioral health care needs of
racially and ethnically diverse populations.
Center for Excellence in Historically Black Colleges:
SAMHSA’s cooperative agreement with Historically Black Colleges and Universities supports a
Center for Excellence in Substance Abuse and Mental Health which provides student internships
at minority serving institutions.
The Minority Fellowship Program (MFP):
SAMHSA’s MFP provides funding to oversee the fellowship opportunities to behavioral health
professionals that encourage doctoral and post-doctoral development of nurses, psychiatrists,
social workers, psychologists, marriage and family therapists, and professional counselors.
Addictions counselor pathways:
SAMHSA supported the development of pathways for the addictions counseling profession,
which can serve as a model to assist providers in staff retention.
Data Needs and Collection Processes
Minimum Data Set (MDS) on behavioral health professionals:
The HRSA National Center for Health Workforce Analysis, in collaboration with SAMHSA, is
actively developing a Minimum Data Set (MDS) to collect more information on the core
behavioral health professions. Current efforts are focused on engaging multiple behavioral
health professional organizations in convening meetings to review the necessary data elements
for a survey instrument in their field. The professions currently involved include psychiatrists,
psychologists, social workers, licensed professional counselors, and substance abuse counselors.
Training and Education Needs
CULTURALLY COMPETENT AND SPECIAL POPULATIONS TRAINING
Cultural, including LGBT, training:
HRSA’s HIV/AIDS Bureau (HAB), through AIDS Education and Training Centers (AETCs),
provides training to the workforce on cultural diversity. From July 2010 through June 2011,
over 4,000 behavioral health professionals attended one or more training events sponsored by
AETCs.

53
Health center training on LGBT issues:
HRSA’s BPHC has a national cooperative agreement for the National LGBT Health Education
Center to help community health centers improve the health of LGBT populations. The Center
has conducted national and local trainings, and provided consultations with health centers, many
of which include behavioral health professionals.
Substance abuse treatment providers on LGBT issues:
SAMHSA’s ATTC Network has developed a curriculum for substance abuse providers on
treating LGBT individuals with substance use disorders.
Training in behavioral health in geriatrics training:
HRSA has four programs that provide geriatric training and education that include mental health
and substance abuse issues. These programs provide education and training in the areas health
problems of the elderly and their caregivers including mental health and substance abuse
problems.
Emergency preparedness for elders:
In 2006, HRSA’s Geriatric Education Centers received the SAMHSA-supported curricula
developed by the Annapolis Coalition on the Behavioral Health Workforce on emergency
preparedness for behavioral health professionals working with the elderly. This curricula
continues to be revised and updated to reflect the latest research and information and is used both
nationally and internationally.
Hiring veterans at health centers:
HRSA has partnered with the National Association of Community Health Centers (NACHC) to
assist veterans in obtaining jobs with health centers around the country.
TRAINING FOR EVIDENCE-BASED PRACTICES
Training for physicians, dentists and others prescribing opioid therapies:
SAMHSA has two efforts providing training for prescribers: Opioid Therapies (PCSS-O) and
Buprenorphine (PCSS-B) grants. The PCSS-O assists physicians, dentists and other medical
professionals in the appropriate use of opioids for the treatment of chronic pain and opioid-
related addiction. The PCSS-B assists physicians in treating patients dependent on heroin or
prescription opioid drugs with buprenorphine. Both provide training through webinars, online
modules, peer support programs, listservs, virtual patients, and phone apps. HRSA plans to
promote the availability of the PCSS-O and PCSS-B training to NHSC scholars and loan re-
payers in field placement sites.
CIHS, ATTCs, and AHECs provide EBP training:
Promotion of behavioral health EBP is provided regularly by the SAMHSA-HRSA CIHS, the
SAMHSA ATTCs and the HRSA AHECs through webinars, conference training and
dissemination of materials.
TECHNOLOGY IN TRAINING AND PRACTICE

54
Telebehavioral health activities:
HRSA’s BPHC and HAB collaborated with SAMHSA on the Secretary’s Minority AIDS
Initiative to expand HIV/AIDS care, viral hepatitis care, and behavioral health care to health
centers through telehealth technology.
Medication Assisted Treatment (MAT) and telemedicine:
SAMHSA has initiated a cross-agency discussion on the use of telemedicine to provide
medication assisted treatment (MAT) to treat substance use disorders which will clarify current
regulations around the prescription of controlled substances and the use of telemedicine. The
goal is to establish clear standards and practice guidelines on the use of telemedicine in
delivering MAT.
Other telehealth activities:
HRSA’s Office of Rural Health Policy (ORHP) and Office of Special Health Affairs (OSHA) are
developing a telebehavioral services manual to encourage HRSA grantee providers to better
incorporate the use of telehealth platforms for behavioral health services. In addition, ORHP’s
Office for the Advancement of Telehealth has numerous grants, some of which provide
behavioral health services, promoting the use of telehealth technologies for health care delivery,
education, and health information services.
READINESS OF SAFETY NET PROVIDERS FOR MANAGED CARE
Provider readiness:
CIHS plans to host a webinar for behavioral health and primary care provider organizations on
how to participate in managed behavioral health care provider networks. This web-based
training will be held in collaboration with the Association for Behavioral Health and Wellness.
Non-Traditional Workforce
Paraprofessional training in SBIRT:
SAMHSA’s State SBIRT demonstration grants have focused on the training and utilization of
paraprofessional staff including health educators, health navigators and health promotion
advocates working under the supervision of licensed physicians or the health care system.
Report on bringing recovery services to scale:
SAMHSA is preparing a report from an expert panel meeting on Peer Specialists and Recovery
Coaches that was convened in March 2012 by Bringing Recovery Services to Scale – Technical
Assistance Center Strategy (BRSS-TACS). It will include recommendations on increasing the
utilization of peers in the behavioral health workforce.

55
Recovery to Practice:
This SAMHSA effort is advancing a recovery-oriented approach to behavioral health care by
developing, promoting, and disseminating training curricula on how to translate the concept of
mental health recovery into practice.
Community Health Worker (CHW) curriculum and training:
HRSA’s AHEC program has implemented CHW training programs in collaboration with state
and local partners, including the Department of Labor and Workforce Investment Boards.
AHECs have trained CHWs on topics such as: cancer, diabetes, tobacco cessation and chronic
disease self-management.
Promoting CHWs:
Texas AHEC East worked with the Department of Labor to have CHWs deemed as an
apprentice-able trade. Apprenticeship training is designed to prepare individuals for occupations
and combines supervised on-the-job learning with classroom instruction.

56
APPENDIX B:
Bibliography
Anderson, C. (2012, March 12). Managing doctor, nurse practitioner turnover rates key to
collaborative care | Healthcare Finance News. Healthcare Finance News. Retrieved from
http://www.healthcarefinancenews.com/news/managing-doctor-nurse-practitioner-
turnover-rates-key-delivery-collaborative-care-model
Carise, D., Gurel, O., McMellan, A. T., Dugosh, K., & Kending, C. (2005). Getting patients the
services they need using a computer-assisted system for patient assessment and referral
referral? CASPAR. Drug and Alcohol Dependence, (80), 177-189.
doi:10.1016/j.drugalcdep.2005.03.024
Center for Substance Abuse Treatment. (2006). Addiction Counseling Competencies: The
Knowledge, Skills, and Attitudes of Professional Practice. (Technical Assistance
Publication Series 21. DHHS Publication No. SMA 08-4171). Rockville, MD: Substance
Abuse and Mental Health Services Administration, (2006), reprinted 2007and 2008.
Center for Substance Abuse Treatment. (2007). Competencies for Substance Abuse Treatment
Clinical Supervisors. (Technical Assistance Publication Series 21-A. DHHS Publication
No. SMA 08-4243). Rockville, MD: Substance Abuse and Mental Health Services
Administration reprinted 2008.
Center for Substance Abuse Treatment. (2009). What Are Peer Recovery Support Services?
(HHS Publication No. SMA 09-4454.) Rockville, MD: Substance Abuse and Mental
Health Services Administration.
Congressional Budget Office. (2012). Estimates for the Insurance Coverage Provision of the
Affordable Care Act Updated for the Recent Supreme Court Decision. Retrieved January
4, 2013, from http://www.cbo.gov/publication/43472
Congressional Budget Office. (2010). Selected CBO publications related to health care
legislation, (2009–2010). Retrieved March 25, 2011, from
http://www.cbo.gov/ftpdocs/120xx/doc12033/12-23-SelectedHealthcarePublications.pdf
Curtis, S. L., & Eby, L. T. (2010). Recovery at work: The relationship between social identity
and commitment among substance abuse counselors. Journal of Substance Abuse
Treatment, 39, 248-254.
Daniels, A. S., Fricks, L., & Tunner, T. P., (Eds). (2011). Pillars of Peer Support - Support -2:
expanding the role of peer support services in mental health systems of care and
recovery. Retrieved February 2011, from
http://www.pillarsofpeersupport.org/POPS2010-2.pdf
Dilonardo, J. (2011). Workforce Issues in Integrated Behavioral Healthcare: A Background
Paper. Unpublished Paper, National Council for Community Behavioral Healthcare.
57
Druss, B. G., Zhao, L., Von Esenwein, S., Morrato, E. H., & Marcus, S. C. (2011).
Understanding excess mortality in persons with mental illness. Medical Care, 49(6),
599-604.
Delaney K.R. Duffy F.F., Dwyer K.P., West J.C., Wilk J., Narrow W.E., Hales D., et al.
(2002) Mental health practitioners and trainees. In Manderscheid, R.W., Henderson
M.J., (Eds). Mental Health, United State (pp. 327–368). Rockville, MD: Substance
Abuse and Mental Health Services Administration.
Eby, L. T., Burke, H., & Maher, C. P. (2010). How serious of a problem is staff turnover in
substance abuse treatment? A longitudinal study of actual turnover. Journal of Substance
Abuse Treatment, 39, 264-271. doi:10.1016/j.jsat.2010.06.009
Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., et al.
(1998). Relationship of child abuse and household dysfunction to many of the leading
causes of death in adults: The Adverse Childhood Experiences Study. American Journal
of Preventive Medicine, 14, 245-258.
Friedli, L., & Parsonage, M. (2007). Mental health promotion: Building an economic case.
Northern Ireland Association for Mental Health. Retrieved March 25, 2011, from
http://www.chex.org.uk/uploads/mhpeconomiccase.pdf?sess_scdc=ee4428ebde41914ab
ac0e0535f55861c
Garner, R., Hunter, B. D., Modisetter, K. C., Ihnes, P. C., & Godley, S. H. (2012). Treatment
staff turnover in organizations implementing evidence-based practices: Turnover rates
and their association with client outcomes. Journal of Substance Abuse Treatment, 42,
134-142.
Gaumond, P., Baytop. C., Whitter, M. (2007). Informing marketing strategies for recruitment
into the addictions treatment workforce. Abt Associates. Retrieved from
http://partnersforrecovery.samhsa.gov/docs/informing_marketing_strategies.pdf
Gerson, L. W., Boex, J., Hua, K., Luckett, R. A., Zumbar, W. R., Bush, D., & Givens, C. (2001).
Medical care used by treated and untreated substance abusing Medicaid patients. Journal
of Substance Abuse Treatment, 20, 115-120.
Greiner, A., & Knebel, E. (Eds.). (2003). Health professions education: A bridge to quality.
Washington, DC: National Academies Press.
Gulf Coast Addiction Technology Transfer Center. (2007). Status of the workforce: addiction
treatment in Texas - 2007 report. ATTC Network. Retrieved from
http://www.attcnetwork.org/userfiles/file/GulfCoast/Texas_Addictions_Workforce_Rep
ort_2007.pdf
Institute of Medicine. (2006). Improving the quality of health care for mental and substance-use
conditions. Washington, DC: National Academies Press.

58
Institute of Medicine. (2003) Greiner, A., & Knebel, E. (Eds.). Health professions education: A
bridge to quality. Washington, DC: National Academies Press.
Institute of Medicine. (2004). Smedley, B. D., Butler, A. S., Bristow, L. R. (Eds.). In the nation's
compelling interest: Ensuring diversity in the health-care workforce. Washington, DC:
National Academies Press.
Institute of Medicine, & Eden, J. (2012). The mental health and substance use workforce for
older adults: In whose hands? Washington, DC: National Academies Press.
International Certification and Reciprocity Consortium. (2012, March 1) Correspondence based
on data from some member certification boards.
Kaplan, L. (2003). Substance abuse treatment workforce environmental scan. (Contract No.
28298-006) Bethesda, MD: Abt Associates.
Knight, D. K., Becan, J. E., & Flynn, P. M. (2012). Organizational consequences of staff
turnover in outpatient substance abuse treatment programs. Journal of Substance Abuse
Treatment, 42, 143-150.
Knudsen, H. K., Ducharme, L. J., & Roman, P. (2008). Clinical supervision, emotional
exhaustion, and turnover intention: A study of substance abuse treatment counselors in
the Clinical Trials Network of the National Institute on Drug Abuse. Journal of
Substance Abuse Treatment, 35, 387-395.
Knudsen, H. L., Ducharme, L. J., & Roman, P. (2006). Counselor emotional exhaustion and
turnover intention in therapeutic communities. Journal of Substance Abuse Treatment,
31, 173-180.
Knudsen, H. K., Johnson, J.A., & Roman, P. M. (2003). Retaining counseling staff at substance
abuse treatment centers: effects of management practices. Journal of Substance Abuse
Treatment, 24, 129-135.
Knudsen, H. K., Oser, C. B., Abraham, A. J., & Roman, P. M. (2012). Physicians in the
substance abuse treatment workforce: Understanding their employment within publicly
funded treatment organizations. Journal of Substance Abuse Treatment, 43, 152-160.
Knudsen, J. R., Williams, A. M., & Perry, S. W. (2005). Tennessee Workforce Survey: Results
of a Statewide Needs Assessment of Behavioral Health Professionals. Central East
Addiction Technology Transfer Center. Retrieved from
http://www.attcnetwork.org/explore/priorityareas/wfd/overview/documents/Central%20
East/TN_WorkforceReport_2004.pdf
Leonardi, L. (2012). Five Low-Paying, High-Stress Jobs. Career advice, interview questions,
salary comparisons, and resume tips from Monster. Retrieved from http://career-
advice.monster.com/salary-benefits/salary-information/low-paying-high-stress-
jobs/article.aspx

59
McLellan, A. T., Carise, D., & Kleber, H. D. (2003). Can the national addiction treatment
infrastructure support the public’s demand for quality care? Journal of Substance Abuse
Treatment, 25, 117-121.
Mertens, J. R., Lu, Y. W., Parthasarathy, S., Moore, C., & Weisner, C. M. (2003). Medical and
psychiatric conditions of alcohol and drug treatment patients in an HMO. Archives of
Internal Medicine, 163, 2511-2517.
Mojtabai, R., & Olfson, M. (2011). Proportion of Antidepressants Prescribed Without A
Psychiatric Diagnosis Is Growing. Health Affairs, 30(8), 1434-1442.
doi:10.1377/hlthaff.2010.1024
Mor Barak, M., Nissly, J., & Levin, A. (2001). Antecedents to retention and turnover among
child welfare, social work, and other human service employees: What can we learn from
past research? A review and metanalysis. The Social Service Review, 75(4), 625-667.
National Association of Alcoholism and Drug Abuse Counselors. (2003). Practice Research
Network. Report. Author.
National Association of Community Health Centers. (2011). NACHC 2010 Assessment of
behavioral health services in federally qualified health centers. Author. Retrieved from
http://www.nachc.com/client/NACHC%202010%20Assessment%20of%20Behavioral%2
0Health%20Services%20in%20FQHCs_1_14_11_FINAL.pdf
National Council for Community Behavioral Healthcare. (2011). Behavioral health salary
survey. Retrieved from
http://www.thenationalcouncil.org/cs/2011_behavioral_health_salary_survey
New York State Office of Alcoholism and Substance Abuse Services. (2002). The addictions
profession: a workforce in crisis. A compilation of the results of the 2001 regional
workforce development focus groups. Author.
Parks, J., & National Association of State Mental Health Program Directors. (2006). Morbidity
and mortality in people with serious mental illness. Alexandria, VA: National
Association of State Mental Health Program Directors Medical Directors Council.
Plomondon, M. E., Magid, D. J., Steiner, J. F., MaWhinney, S., Gifford, B. D., Shih, S. C.,
Grunwald, G. K., et al. (2007). Primary care provider turnover and quality in managed
care organizations. American Journal of Managed Care, 13(8), 465-472.
RMC Research Corporation. (2003). Advancing the current state of addiction treatment. A
regional needs assessment of substance abuse treatment professionals in the pacific
northwest. Portland, OR. Author.
RMC Research Corporation. (2003a). Kentucky workforce survey 2002. Results of a statewide
needs assessment of substance abuse treatment professionals. Portland, OR: Author.

60
Ryan, O., Murphy, D., Krom, L. (2012). Vital Signs: Taking the Pulse of the Addiction
Treatment Workforce, A National Report - Executive Summary. Kansas City, MO:
Addiction Technology Transfer Center National Office in residence at the University of
Missouri-Kansas City.
Salzer, M. S., Schwenk, E. S., & Brsilovskiy, E. (2010). Certified Peer Specialist Roles and
Activities: Results from a National Survey. Psychiatric Services, 61(5), 520-523.
Substance Abuse and Mental Health Services Administration. (2006). Report to Congress
Addiction Treatment Workforce Development. Retrieved from
http://partnersforrecovery.samhsa.gov/docs/Report_to_Congress.pdf
Substance Abuse and Mental Health Services Administration. (2006a) Strengthening
Professional Identity: Challenges of the Addiction Treatment Workforce. Retrieved from
http://partnersforrecovery.samhsa.gov/docs/Strengthening_Professional_Identity.pdf
Substance Abuse and Mental Health Services Administration. (2007) An Action Plan for
Behavioral Health Workforce Development. (HHS Publication No. SMA 11-4629.)
Rockville, MD: Substance Abuse and Mental Health Services Administration. Retrieved
from: http://www.samhsa.gov/workforce/annapolis/workforceactionplan.pdf
Substance Abuse and Mental Health Services Administration. (2008). Unpublished. SAMHSA
data, 2008 National Survey of Mental Health Treatment Facilities.
Substance Abuse and Mental Health Services Administration. (2009). What are Peer Recovery
Support Services? Retrieved from http://store.samhsa.gov/shin/content//SMA09-
4454/SMA09-4454.pdf
Substance Abuse and Mental Health Services Administration. (2010). Mental Health, United
States, 2008. (HHS Publication No. SMA 10-4590.) Rockville, MD: Substance Abuse
and Mental Health Services Administration.
Substance Abuse and Mental Health Services Administration. (2010). National survey of
substance abuse treatment services: Data on substance abuse treatment facilities.
Rockville, MD: Substance Abuse and Mental Health Services Administration.
Substance Abuse and Mental Health Services Administration. (2011a). Leading Change: A Plan
for SAMHSA’s Roles and Actions 2011-2014. (HHS Publication No. SMA 11-4629).
Rockville, MD: Substance Abuse and Mental Health Services Administration.
Substance Abuse and Mental Health Services Administration. (2011b). Scopes of Practice and
Career Ladder for Substance Use Disorders Counseling.
http://store.samhsa.gov/product/Scopes-of-Practice-and-Career-Ladder-for-Substance-
Use-Disorders-Counseling/PEP11-SCOPES

61
Substance Abuse and Mental Health Services Administration. (2011). Results from the 2010
National Survey on Drug Use and Health: Summary of national findings. (NSDUH
Series H-41, HHS Publication No. (SMA) 11-4658). Rockville, MD: Substance Abuse
and Mental Health Services Administration.
Substance Abuse and Mental Health Services Administration (2012a). Mental Health, United
States, 2010. (HHS Publication No. (SMA) 12-4681). Rockville, MD: Substance Abuse
and Mental Health Services Administration, Center for Mental Health Services.
Substance Abuse and Mental Health Services Administration. (2012b). Results from the 2011
National Survey on Drug Use and Health: Summary of national findings. Rockville, MD:
Substance Abuse and Mental Health Services Administration, Center for Behavioral
Health Statistics and Quality.
Substance Abuse and Mental Health Services Administration. (2012). Treatment Episode Data
Set: 2001-2010. National Admissions to Substance Abuse Treatment Services. (DASIS
Series S-61, Publication No. SMA 12-4701.) Rockville, MD: Substance Abuse and
Mental Health Services Administration, Center for Behavioral Health Statistics and
Quality.
Substance Abuse and Mental Health Services Administration & National Association of State
Mental Health Program Directors. (2004). The damaging consequences of violence and
trauma. Retrieved from
http://www.nasmhpd.org/general_files/publications/ntac_pubs/reports/Trauma%20Servic
es%20doc%20FINAL-04.pdf
Thomas, M., (February, 2006). State Medicaid Strategies for Integrated Care: Health Plan
Experience, a Presentation to RWJ Depression in Primary Care Annual Meeting.
Thomas, K. C., Ellis, A. R., Konard, T. R., Holzer, C. E., & Morrissey, J. P. (2009). County-
level Estimates of Mental Health Professional Shortage in the United States. Psychiatric
Services, 60(10), 1323-1328.
Touhy, C. M. (2006). Blueprint for the States: Policies to Improve the Way States Organize and
Deliver Alcohol and Drug Prevention Treatment. National Association for Alcoholism
and Drug Abuse Counselors. Retrieved from
http://www.naadac.org/component/content/article/54-resources/349-pr175
U.S. Census Bureau (2010). 2010 Census. Census Bureau. Retrieved from
http://www.census.gov/2010census/
Unützer, J., Katon, W. J., Fan, M. Y., Schoenbaum, M. C., Lin, E. H., Della Penna, R. D., &
Powers, D. (2008). Long-term cost effects of collaborative care for late-life depression.
American Journal of Managed Care, 14(2), 95-100.
62
Woltmann, E. M., Whitley, R., McHugo, G. J., Brunette, M., Torrey, W. C., Coots, L., Lynde,
D., et al. (2008). The Role of Staff Turnover in the Implementation of Evidence-Based
Practices in Mental Health Care. Psychiatric Services, 59(7), 732-737.
doi:10.1176/appi.ps.59.7.732
