
The
Direct Care
Workforce
YEAR IN REVIEW

Contents
1 Introduction
2 Statistical Snapshot of the Direct Care Workforce
4 How to Recruit and Retain Workers
6 A Home Care Approach for Rural America
8 Home Care Workers Speak Out
10 Federal Policy Spotlight
12 State Policy Spotlight
14 Technology and the Direct Care Workforce
17 Top 20 News Stories on Direct Care Workers
21 9 Publications for the Direct Care Sector
23 #60CaregiverIssues Campaign Recap
PHI works to transform eldercare and disability
services. We foster dignity, respect, and
independence for all who receive care, and
all who provide it. As the nation’s leading
authority on the direct care workforce,
PHI promotes quality direct care jobs as the
foundation for quality care.
© 2018 PHI

In 2018, we saw many great ideas take hold
for direct care workers—a workforce that has
long served as the paid frontline of long-term
care and as a lifeline for millions of people.
Unfortunately, the poor quali of direct care jobs
continues to drive away workers, threatening
the availabili of supports for older people and
people with disabilities.
Here are some of the great ideas that
emerged in 2018:
8
Home care providers in Minnesota
and Wisconsin co-launched initiatives to
improve home care jobs across their states,
particularly in rural areas.
8
Throughout the country, advocates
successfully moved policy measures to
improve recruitment and retention, strengthen
data collection, invest in geriatrics training,
and bolster the supports oered by family
caregivers and volunteer caregivers—among
other successes.
8
Organizations published a range of
reports related to direct care, while journalists
deepened their investigation of this workforce,
writing about sexual harassment, transportation
barriers, and the eects of anti-immigrant
sentiment on workforce supply, to name a few.
8
Our award-winning #60CaregiverIssues
campaign came to an end, after generating
headline after headline on the workforce
shortage in home care, and rightfully
positioning these workers at the center of the
national discourse.
But we need more great ideas. Direct care
workers deserve jobs that properly reflect
the central role they play in
our country’s care system.
Older people, people with
disabilities, and their
families need quali
supports. And long-term
care merits a larger
investment with greater
equi and access.
We’re a long way from
achieving this reali–but
the next great idea will
move us one step closer.
INTRODUCTION
What are the characteristics of a great idea? Does it solve a widespread
problem that seemed intractable? Does it help decision-makers see the larger
picture and connect all the dots? Does it inspire a community or a sector
to act decisively—drawing people out of the well of defeatism?
Great Idea
The Year of the
1
PHI
|
YEAR IN REVIEW 2018

8
The direct care workforce totaled 4.3 million in 2017.
8
The home care job is among the fastest-growing occupations
and will add 1 million jobs beeen 2016 and 2026–
more than any other single occupation.
8
Adjusted for inflation, wages for home care workers have remained stagnant
in the last decade:
$
10.66 in 2007 and
$
11.30 in 2017.
8
Nursing assistants are more than three times
likelier to experience injuries on the job than the pical U.S. worker.
8
One in four direct care workers is an immigrant—
totaling 1 million nationwide.
Neglected
A Growing Yet
Workforce
The direct care workforce expands every year–a trend spurred largely by
the persistent growth in the number of older adults and increased longevi
in the general population. Unfortunately, the quali of direct care jobs hasn’t
improved commensurate to this expansion, which forces many workers
to leave the sector and leaves clients stranded without support. Here’s the
latest data on this critical workforce.
A STATISTICAL SNAPSHOT OF THE DIRECT CARE WORKFORCE
KEY FACTS
2
PHI
|
YEAR IN REVIEW 2018
SOURCE: PHI. Immigrants and the Direct Care Workforce:
2018 Update. Bronx, NY: PHI, 2018; PHI. U.S. Home Care Workers:
Key Facts. Bronx, NY: PHI, 2018; PHI. U.S. Nursing Assistants
Employed in Nursing Homes: Key Facts. Bronx, NY: PHI, 2018.
IMMIGRANTS IN DIRECT CARE
Immigrants are a valuable part of the direct
care workforce–both now and in the future–yet they
have faced intensifying scrutiny in recent years as the
climate has become more hostile on immigration.
Here are three ways for long-term care leaders to
support this segment of the workforce:
1. Generate new studies on this sector
2. Promote culturally and linguistically
competent workforce supports
3. Form community partnerships with
immigrant-focused organizations
2.1 M
|
600,000
47
|
37
87%
|
91%
60%
|
55%
$
11.03
|
$
12.84
40%
|
24%
$
15,100
|
$
21,200
19%
|
15%
A STATISTICAL SNAPSHOT OF THE DIRECT CARE WORKFORCE
KEY DEMOGRAPHICS
TOTAL
MEDIAN AGE
% WOMAN
% PEOPLE OF COLOR
% IN POVERTY
MEDIAN INCOME
% PART TIME / YEAR
MEDIAN WAGE
HOME
CARE
WORKERS,
2016
NURSING
ASSISTANTS IN
NURSING
HOMES, 2016
|
What is a Direct
Care Worker?
Direct care workers assist older adults and
people with disabilities with daily tasks, such as
dressing, bathing, and eating. Direct care workers
include personal care aides, home health aides,
and nursing assistants. Personal care aides also
help their clients with housekeeping and might
assist them with errands, appointments, and
social engagements outside of the home.
Home health aides and nursing assistants also
perform clinical tasks, such as blood
pressure readings and
assistance with range-of-motion
exercises.
3
PHI
|
YEAR IN REVIEW 2018
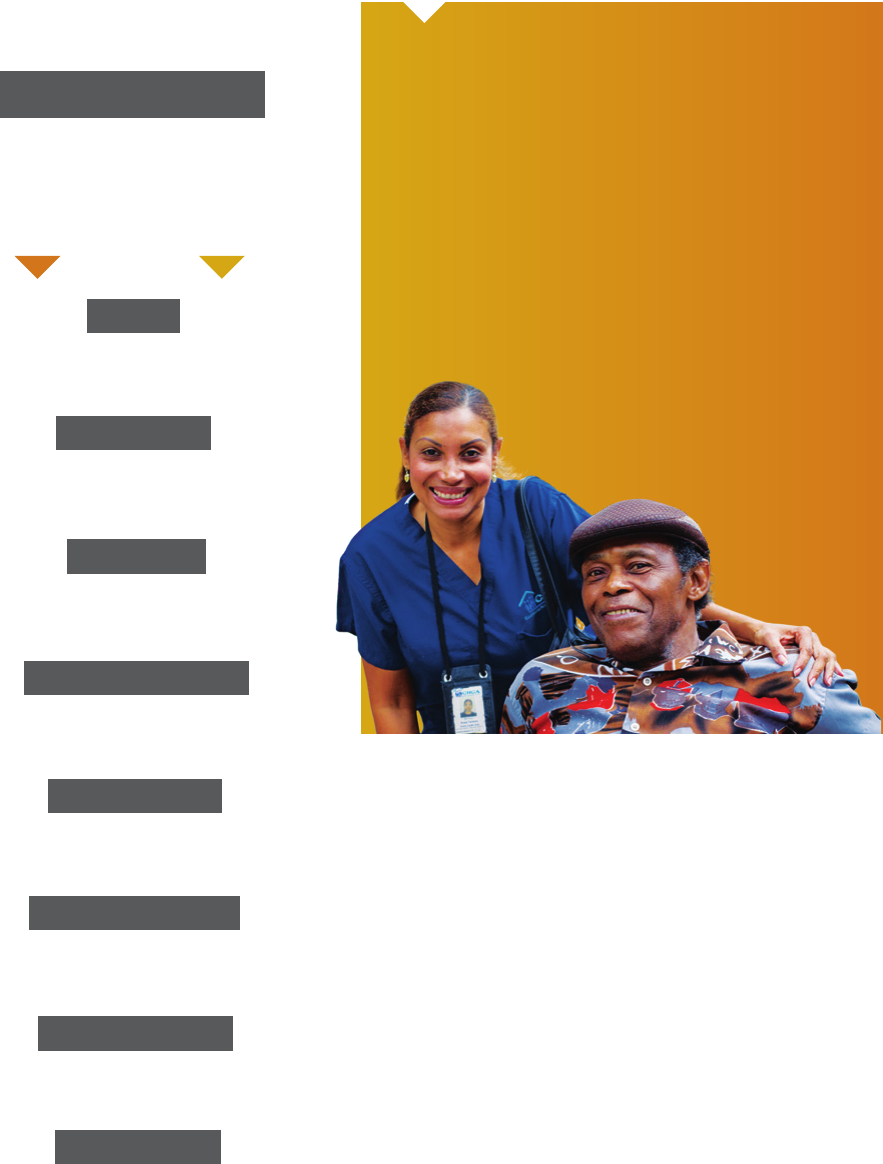
HOW TO RECRUIT AND RETAIN WORKERS
Guidance
Practical
for Employers
Across the country, home care providers are struggling to hire the right
candidates, find enough workers to fill cases, and keep strong employees in
these roles. Recognizing that the home care job needs a sector-wide
transformation to remain aractive, how can long-term care employers beer
recruit and retain home care workers? We have some ideas.
4
PHI
|
YEAR IN REVIEW 2018

Growing a Strong Direct
Care Workforce
1
In 2018, we published a guide to support
long-term care employers in their recruitment
and retention eorts. Here are 10 strategies
described in this guide:
1. Recruit the Right Staff
2. Improve the Hiring Process
3. Strengthen Entry-Level Training
4. Provide Employment Supports
5. Promote Peer Support
6. Ensure Effective Supervision
7. Develop Advancement
Opportunities
8. Invite Participation
9. Recognize and Reward Staff
10. Measure Progress
Expanding the Labor Pool
The pical direct care worker is a woman in her
late 30s or early 40s. To ensure enough direct
care workers in the years ahead, this sector must
aract a more diverse labor pool. Here are three
workforce segments that hold potential:
•
Younger workers. The U.S. labor force
includes 31 million younger workers aged
18 to 24. This demographic makes up 16
percent of the direct care workforce.
2
• Older workers. Roughly one in four direct
care workers is aged 55 and older, many
of whom bring significant work and life
experience to these roles.
3
• Men. Men make up roughly half of the U.S.
labor force yet only 14 percent of the labor
force. Many men connect their experiences
as family caregivers to direct care.
4
HOW TO RECRUIT AND RETAIN WORKERS
Did you know?
• One in four Americans will be aged
65 and older in 2060.
• More than half of this population will
need long-term care at some point.
• Home care will add more than one
million jobs between 2016 and 2026.
• Turnover in this sector generally
ranges from 45 to 60 percent.
• The estimated cost for replacing a
direct care worker is $2,200.
5
PHI | YEAR IN REVIEW 2018
5
PHI
|
YEAR IN REVIEW 2018
1. PHI. 2018. Growing a Strong Direct Care Workforce: A Recruitment
and Retention Guide for Employers. Bronx, NY: PHI.
2. PHI. 2018. Younger Workers and the Direct Care Workforce. Bronx, NY: PHI.
3. PHI. 2018. Older Workers and the Direct Care Workforce. Bronx, NY: PHI.
4. PHI. 2018. Men and the Direct Care Workforce. Bronx, NY: PHI.

A HOME CARE APPROACH FOR RURAL AMERICA
6
PHI | YEAR IN REVIEW 2018
PHI’s Anna Ortigara and Cean
Eppelheimer (back, left to right) facilitated
a training for the providers participating
in PHI’s multi-year initiative to improve
home care jobs in Minnesota. Graduates of
the training left the week of education with
the ability to teach coaching supervision
and coaching communication to their
staff, improving workplace culture and the
quality of their jobs.

A HOME CARE APPROACH FOR RURAL AMERICA
Home Care
The Rural
Dilemma
As in many other parts of the country, Minnesota and Wisconsin are
facing a severe shortage in home care workers that threatens to worsen.
Complicating this problem are the unique challenges of delivering home
care to rural parts of these states, where health-related resources are
thinner, and the “care gap” beeen older people and available workers
grows larger every year. Nevertheless, a solution is on the horizon.
Elevating the Role of the
Home Care Worker
To meet the growing demand for care
statewide, and to support workers in making
ends meet, the quali of home care jobs must
be transformed. “Elevating the role of the
aide” in the home care system—training and
supporting them to have more expansive roles
in this sector—is a critical strategy for improving
this sector. Advanced roles and proper training
can lead to improved job satisfaction and
retention among home care workers, and to
higher quali care for consumers.
A Multi-Year Intervention,
a National Solution
PHI has brought together various leading home
care providers in Minnesota and Wisconsin to
implement a large-scale solution to the growing
workforce shortage in home care. Over the
next year, PHI is working with these providers
to implement various interventions: advanced
roles, coaching supervision, e-learning and
entry-level training, and a range of recruitment
and retention strategies. What is our aim? To
transform this sector and create a model that
informs rural home care strategies around the
country. Rural residents deserve beer.
INITIATIVE PARTNERS
7
PHI
|
YEAR IN REVIEW 2018

HOME CARE WORKERS SPEAK OUT
Own Voices
In Their
Our home care initiatives in Wisconsin and Minnesota speak to the
importance of home care workers to older people and people with disabilities
across the state, the long-term care system, and the broader economy. But
nothing demonstrates more the value of these jobs than the voices of workers
themselves. Here’s what they had to say about their roles.
“ Being a home health
nurse means you have to
think outside the box.
You care for a whole family,
not just a patient.”
— Barb Bull, Minnesota Registered
Nurse Case Manager
“ Caring for others means so much
more than what I do. It gives
others independence and choice.
They are able to make an impact
on our community because
of what I do….That’s what
caregivers do; they understand
others and help them to be the
person that they are.”
— Sam, Home Care Specialist, Wisconsin
PHI
|
YEAR IN REVIEW 2018
8

HOME CARE WORKERS SPEAK OUT
“ Making them smile, laugh, carrying
on conversations, encouraging
them to be independent, and
helping them stay at home as long
as possible–these are all things
I love about my job.”
— Janet Wilkins, Home Health Aide,
Minnesota
“ I learned from my clients
that every day is beautiful
and they live their lives to the
fullest with a little help from
their caregivers. They need to
know that they can trust you
with their well-being.”
— Becky Boldt, Program Manager
and Care Giver, Wisconsin
“ The impact of being a caregiver
was not immediate for me.
After about a month, I got it….
If you are new to caregiving…
give yourself a chance to
understand and feel the difference
you can make in another person’s
life, and the difference they can
make in yours.”
— Lynn Jenkins, Care Giver, Wisconsin
“ …becoming a Home Care
Specialist has changed my life.
Meeting new people almost
every day has given me a
new perspective…I teach my
kids about awareness and
that everyone has a story they
could learn from.”
— Priscilla, Home Care Specialist,
Wisconsin
“ I have dedicated
my adult life to the
health care eld and
it’s a very rewarding
and helpful job in
more ways than one.”
— Prema Friedlein,
Program Manager/Caregiver,
Wisconsin
9
PHI
|
YEAR IN REVIEW 2018

FEDERAL POLICY SPOTLIGHT
Offense
From Defense to Strategic
The federal landscape is essential to the direct care workforce. It shapes how these
workers are compensated, trained, and supported, as well as the extent to which the
long-term services and supports system is properly structured and funded. This year,
a varie of developments related to direct care workers went virtually unnoticed in
the public eye, obscured by more dramatic stories. Here’s what you missed.
JANUARY
Family Caregivers. Direct care
workers play a key role in sup-
porting family caregivers, many of
whom are saddled with the
nancial and psychological costs
of providing unpaid care. In
January, Congress passed the
RAISE Family Caregivers Act, which
will devise a national strategy to
support family caregivers.
MAY
Eldercare Training. Direct care
workers are a key segment of the
eldercare workforce, which could
benet from improved geriatrics
training. In May, the Geriatrics
Workforce Improvement Act was
introduced in the Senate, paving
the way for strengthening the
health care sector’s ability to
support older Americans.
JULY
Geriatrics Funding. Geriatrics
workforce enhancement programs
train health care professionals on
how to support older people. In
July, the U.S. House of Repre-
sentatives passed the Educating
Medical Professionals and Opti-
mizing Workforce Efciency and
Readiness (EMPOWER) Act, which
would continue funding for these
programs, including ones based
in home and community-based
settings and nursing homes.
JULY
Weakening Health Care. In the
four years after the Affordable
Care Act became law, half a million
direct care workers obtained health
coverage. This year, the Trump ad-
ministration continued to tear at this
legislation by de-funding and legally
challenging key elements, such as
ACA navigators and the “individual
mandate,” among others.
SEPTEMBER
Punishing Immigrants. One in
four direct care workers is an immi-
grant, and because of low-paying
jobs, 52 percent access public
benets to survive. In September,
the U.S. Department of Homeland
Security announced they could
begin denying lawful permanent
residence to immigrants who
access certain public benets.
Supporting Volunteers. Older
people and people with disabil-
ities rely on various people for
support–from direct care workers
to family caregivers, and more.
In September, the U.S. House
of Representatives provided $5
million in funding to support Care
Corps grants, which would create
a caregiving volunteer program
that provides non-medical services
to people in need.
6 Key Moments in 2018
PHI
|
YEAR IN REVIEW 2018
10
1
3
4
6
5
2

How has President Trump changed the federal
policy landscape for the eldercare workforce?
York: With any new president there is always an
adjustment period. We are fortunate that many
of the issues around the workforce that cares for
older adults are universal. However, we have seen a
significant shift in priorities on a number of issues
that impact the eldercare workforce. Immigration
is the most drastic of changes, but we have also
seen some proposed elimination of the only federal
training program in geriatrics. We are definitely
playing defense on a number of issues.
However, I think the biggest change in this
Administration is that the daily news cycle and
Tweets drive the Congressional agenda now more
than ever. It makes it even more dicult to predict
the Congressional process. In my 25-plus years of
living in DC, I have never seen an environment like
we have today.
Is there a policy win for these workers
that stood out for you in 2018?
McReynolds: The Recognize, Assist, Include,
Support, and Engage (RAISE) Family Caregivers
Act (S. 1028/H.R. 3759) was the biggest
straightforward win for the eldercare workforce.
Appropriators funded RAISE at $300,000 earlier
this year and took nominations for the advisory
commiee. For the roughly 35 million Americans
that provide unpaid care to an older adult in the
U.S., this law would instruct the Secretary of Health
and Human Services to develop, update, and
maintain a strategy to recognize and support family
caregivers—a huge step forward in addressing a
pressing issue for us all as we age.
What’s the mood on the Hill these days
regarding eldercare workers?
McReynolds: Overall, I would say the mood is
positive. There are many lawmakers and sta
members that have a genuine passion and see
the pressing need to both address the eldercare
workforce shortage and invest in continued
training of this workforce. We were pleased to
see a $2 million increase in geriatrics workforce
programs last fiscal year—in a year when the
budget was a largely divisive issue. We continue
to work hard to get that number increased so we
can adequately address the workforce shortage.
Who are some of the leading champions
in Congress on this issue?
McReynolds: Rep. Jan Schakowsky (D-IL) was
the lead sponsor on the geriatrics workforce
reauthorization bill (HR 3713) in the House. She
has been an outspoken leader on these issues for
years. Rep. Doris Matsui (D-CA) and Rep. David
McKinley (R-WV) were also co-sponsors, showing
that this issue is truly bipartisan.
Most recently, Sen. Susan Collins (R-ME) and
Sen. Bob Casey (D-PA) introduced the Geriatrics
Workforce Improvement Act (S. 2888), a companion
to the House bill, to reauthorize geriatrics
workforce programs. At a time when so many
issues have become partisan, the fact that these
issues have bipartisan, bicameral support highlights
the importance of issues relating to the eldercare
workforce.
What is one federal goal you have for
this workforce beyond 2018?
York: Moving forward into 2019, we will have
a divided government again. I don’t expect any
drastic changes in the 116th Congress. However,
I am optimistic that the family caregiver panel
will jump in and begin to develop a plan to
support family caregivers.
Much of that support comes from the workforce.
We have an important mission to ensure that the
workforce and family caregivers are adequately
prepared to care for all of us as we age. This plan is
an opportuni to address these important issues.
FEDERAL POLICY SPOTLIGHT
Amy York and Brett McReynolds, EWA
The Eldercare Workforce Alliance (EWA) is a group of 31 national organizations representing consumers, family caregivers,
the direct care workforce, and health care professionals. EWA’s Amy York and Brett McReynolds shared their personal
reections on the federal landscape and what it means for direct care workers and the full eldercare workforce.
11
PHI
|
YEAR IN REVIEW 2018

STATE POLICY SPOTLIGHT
Pave the Way
States
When it comes to policy reforms on the direct care workforce, states are increasingly
assuming the mantle–creating stronger compensation and training standards,
promoting recruitment and retention, and imagining workforce solutions that meet the
unique characteristics of their states, among other measures. What are some highlights
from this year, and what’s in store for the years ahead? Here are our thoughts.
It seems that states are gradually enacting
policy reforms that strengthen the direct care
workforce. What’s driving this trend?
Stephen Campbell: Policymakers are acting now
because advocates have successfully explained
how the workforce shortage aects socie and the
economy. The new demand for care has led many
states to help people pay for services. Yet they still
don’t have enough workers, and people can’t get
the services they need.
Allison, we often tout New York as a state
that has taken impressive strides toward
strengthening the direct care workforce.
What are some of those achievements?
Allison Cook: New York has a long history of
strengthening this workforce. It has set wage
and benefit minimums for certain segments of
the home care workforce, passed the nation’s
first “Domestic Worker’s Bill of Rights,” and
implemented paid family medical leave—among
other achievements.
Stephen, is there a state-level policy
development from this year that holds
promise for the future of the eld?
Campbell: Texas will soon collect more data on
the home care workforce, which they will use
to create workforce solutions. According to the
state’s report on this topic, these interventions
could support wages, training, supervision, child
care support, and peer mentorship for workers.
That’s the kind of innovative thinking we need
right now.
Allison, what are New York policymakers
considering right now for this workforce?
Cook: They are largely trying to figure out what
to do about the workforce shortage. How do we
ensure that we have enough quali home care
workers? We oered some ideas this fall, but it’s
going to take a strong, concerted eort from
state advocates.
Stephen Campbell
and Allison Cook, PHI
Stephen Campbell and Allison Cook drive PHI’s state advocacy
around the country, monitoring and advising on key developments
for this workforce. Here they reect on the enormous potential
of state leadership in a rapidly evolving policy landscape.
PHI
|
YEAR IN REVIEW 2018
12

Are there specic New York policy approaches
for this workforce that you want other states
to replicate?
Cook: Two come to mind. The first is New
York’s “Workforce Innovation Program,” which
dedicates Medicaid funding to support training
for long-term care workers. The second is
the state’s new advanced home health aide
occupation, which New York is beginning to
implement. By allowing advanced aides to
administer certain medications, consumers
will have beer supports and workers will have
access to a career ladder.
Stephen, you recently spoke in Maine about
the importance of state-based strategies that
make long-term care more affordable to the
state’s residents. Why are these strategies
also important for the direct care workforce?
Campbell: Maine considered a ballot initiative
that could have gone a long way toward fixing
our broken system. Most people spend down
their money on care until they’re poor enough to
qualify for Medicaid. That disturbing trend also
strains state budgets, which in turn limits funding
to this sector, exacerbating the workforce
shortage in direct care. Programs like the one
proposed in Maine could save people from
pover and bolster the workforce.
Stephen, you’ve written several case studies
where state policy leaders succeeded largely
by bringing together a range of stakeholders.
What is the value of this approach?
Campbell: We can only create programs and
policies that work for everyone when everyone
has a seat at the table. At a minimum, workers,
employers, state ocials, and people who need
care should all have a say. There’s no limit to
what we can accomplish when we come together
and work toward a common goal.
As you look ahead, where would you want
you want state lawmakers to focus their
attention regarding this workforce?
Campbell: We need beer data on the workforce.
We don’t know the precise scope of the
workforce shortage, and we rarely ask workers
what they need to stay on the job. We can
only solve our problems after we have clearly
identified and understood them.
Allison, what is your biggest hope for
New York’s home care sector in 2019?
Cook: My biggest hope is for the state to establish
a Home Care Jobs Innovation Fund. It would
support pilot projects to address recruitment and
retention in this sector. Policymakers could also
use the results from these pilot studies to help
address the workforce shortage.
MINNESOTA
Minnesota launched
Direct Support Connect,
a statewide job board
that helps consumers
nd workers and helps
workers nd the right
employment t.
TEXAS
The Texas Health and
Human Services Commission
issued a report to improve
recruitment and retention
among the state’s Medicaid-
funded personal care aides.
WISCONSIN
Wisconsin launched
WisCaregiver, a
training program for
new nursing assistants
that also matches
them with employers.
MASSACHUSETTS
Massachusetts enacted a
law that will require LGBT
cultural competency training
for state-funded or licensed
providers of services to
older adults.
MAINE
Maine passed a bill
to increase Medicaid
reimbursement rates for
direct care workers, helping
to improve wages for
workers who support older
people and people with
disabilities.
ARIZONA
Arizona required Medicaid
health plans to collect data
and develop workforce
interventions that will improve
recruitment and retention
among direct care workers.
STATE POLICY SPOTLIGHT
6 KEY STATE POLICY
DEVELOPMENTS
IN 2018
13
PHI
|
YEAR IN REVIEW 2018

MAXIMIZING
COMMUNICATION
In home care, handheld devices
such as smartphones and tablets
can improve communication
among the worker, client, and
full care team. A worker can use
technology to report and manage
changes in a client’s health
condition, among other uses.
FROM THE FIELD: PHI’s
approach to “upskilling” home
care workers draws on handheld
devices to report and manage
client issues, such as health
conditions, risk factors, stressors
in the home, social connections,
and more.
BOOSTING
RECRUITMENT
Long-term care advocates have
used social media to engage
the public, and now employers
are turning to these platforms to
improve recruitment. Social
media can easily reach larger,
more targeted audiences, and
it can simplify the candidate
outreach process.
FROM THE FIELD: A Minnesota-
based digital media rm worked
with a local provider to boost
its recruitment gures–using
paid ads to target key markets
and driving them to apply online
through their mobile devices.
ENGAGING ONLINE
AUDIENCES
Through a range of technology
tools and digital media platforms,
long-term care employers are
improving communication
with their clients and workers.
Advocates are also relying on
new technologies to build public
support for pressing issues.
FROM THE FIELD: PHI worked
with providers in Minnesota and
Wisconsin to launch month-long
social media campaigns in each
state that built public awareness
of the challenges facing both
home care workers and clients.
IS OUR SECTOR PREPARED FOR NEW TECHNOLOGIES?
Technology
As technology innovations gain traction in the long-term care industry, PHI
remains clear about one stance in particular: automation and robots cannot
replace the value of personal connection and hands-on support in direct care,
and it should not displace direct care workers from their jobs. Nevertheless,
technology continues to show promise in the direct care sector–from handheld
devices to social media, and much more. Here are seven examples of
technology strengthening the direct care workforce.
and the Direct Care Workforce
PHI
|
YEAR IN REVIEW 2018
14

SUPPORTING
INDEPENDENCE
Many people with disabilities rely
on technology supports to live
independently in their homes.
These technologies include
sensors that monitor the health
and safety of individuals, remote
monitoring technology, smart
homes, voice assistants, and more.
FROM THE FIELD: In 2017, the
President’s Committee for People
with Intellectual Disabilities
issued a policy report on direct
support professionals, citing
technology supports as one of
10 core recommendations.
IMPROVING
WORK HOURS
Many home care workers work
part time because of health
conditions, because they’re caring
for relatives, or because they
can’t nd full-time work. An online
jobs platform can address these
concerns, allowing workers to
create the schedules they want.
(Matching service registries, which
are described below, also make
use of online job platforms but
are more focused on “matching”
consumers and workers.)
FROM THE FIELD: A Washington,
DC-based company created
an online jobs platform where
employers can post jobs and
search for workers based on
location, skills, and experience–
and workers can nd jobs that
meet their needs.
CONNECTING
WORKERS AND
CLIENTS
Matching service registries gather
information about the needs and
preferences of consumers, and the
availability, skills, and preferences
of workers–creating a centralized,
region-specic online resource
where both sides can “match”
with one another.
FROM THE FIELD: PHI’s
Matching Services Project houses
a state-by-state online listing of
matching service registries in the
U.S., including information on
their location, funding sources,
geographic focus, and more.
TRAINING
WIDESPREAD
AUDIENCES
E-learning methodologies have
the potential to improve learning
outcomes for large numbers
of direct care workers. These
methods can also reach workers
who aren’t able to attend training
sessions in person, and they might
be cost-effective in the long-term.
FROM THE FIELD: PHI will soon
unveil its e-learning and training
“specialty” curricula for direct
care workers, which blends our
25-year expertise on training this
workforce with best practices in
e-learning.
IS OUR SECTOR PREPARED FOR NEW TECHNOLOGIES?
Philip: The term “e-learning”
is believed to have been first
used in the late 1990’s as part
of a computer-based training
systems seminar in Los Angeles,
California. E-learning emerged
out of the technology waves
of “personal” computing
in the 1980’s and 1990’s,
broadband availabili in the
2000’s, smartphones in the
late 2000’s, and the
widespread adoption
of social media over
the last decade.
Jerry Philip
Director of Workforce Training Solutions, PHI
E-learning has increasingly captivated long-term care leaders who want to tap
the power of technology to effectively train direct care workers, while improving
learning outcomes and achieving cost efciencies. But what exactly is its
potential for this workforce? PHI’s Jerry Philip weighs in.
Can you give us a sense of history–how did e-learning emerge?
Q&A
(continued on pg. 16)
15
PHI
|
YEAR IN REVIEW 2018

We saw schools oering online
courses in the 1990’s, businesses
beginning to use e-learning to
train workers in the 2000’s, and
e-learning formats inspired by
social media this decade. In short,
computers became smaller, cheaper, and more
widely available; the internet became a reliable
pipeline for content and transactions; and
we’ve adapted ourselves to consume content,
socialize, work, and learn online. Organizations
have been trying to make the most of these
changes through e-learning.
Can you paint a picture of how an
e-learning course works in the direct care
context? What are some of the most
popular elements?
Philip: From our point of view, eective
e-learning for direct care workers is scenario-
based, which means that we’re interested in
combining case study principles with those
scenarios. We want to introduce the learner
[the worker] to a client using a narrative
with pictures and audio to help them see the
individual and to understand their needs.
We then want to simulate scenarios that give
learners a chance to “practice” key caregiving
skills. The scenarios and the accompanying story
are designed to “unfold” in unexpected ways.
We want learners to reflect on their “practice”
experiences. Lastly, we want to give our learners
a chance to finish the story of their client. We’re
using the basic elements of e-learning—video,
audio, textual elements, and branching—for
storytelling, and other interactive elements to
make the experience as engaging as possible.
It seems that long-term care providers are
increasingly using an e-learning model to
train their workers, ensuring they have the
skills and knowledge to succeed in their
roles. What’s the appeal of eLearning?
Philip: It can be seen as a cost-saving strategy.
It oers a way to train workers without the
same expense of trainers, curriculum writing,
and, for some, training space. The flexibili
to train workers when they need it and
wherever they have Wi-Fi is powerful when
you are dealing with scheduling and stang
challenges.
What are the benets of e-learning
for direct care workers?
Philip: The primary benefit of e-learning for
direct care workers is that workers can access
training when it works best for them. This is
particularly meaningful for those workers who
face considerable transit challenges, or child
and family care responsibilities. E-learning
also oers the potential benefit of training in
multiple languages for workers with limited
English proficiency. And it can serve as a
real-time job aid or refresher, particularly for
workers in home or communi-based seings
who have limited access to live support.
What is the appeal for businesses to
adopt e-learning technologies?
Philip: Businesses—even in sectors that are
pically late adopters of technology—have
recognized the cost and time savings of
e-learning. Workers with greater technological
literacy are well equipped to benefit from
e-learning, and their success with this format
has helped justify organizational investments.
Are there any technology innovations
in recent years that have the potential to
improve training among the direct care
workforce?
Philip: Augmented and virtual reali
technologies oer the chance to narrow the gap
beeen training and real-world caregiving by
making the experience truer-to-life while building
empathy. This really maers when we are trying
to help learners combine and apply all their
new knowledge and skills to real-life scenarios,
particularly for clients with complex needs. AR-
or VR-assisted simulations give workers a chance
to feel the emotion of the case and to “see” the
impact of their actions on care. This helps the
workers retain more of what they’ve learned and
makes it easier and more likely for them to put
their new skills into practice.
IS OUR SECTOR PREPARED FOR NEW TECHNOLOGIES?
Q&A
PHI
|
YEAR IN REVIEW 2018
16
(continued from pg. 15)

“HEALTH CARE JUST
BECAME THE U.S.’S
LARGEST EMPLOYER”
In the rst quarter of
2018—and for the rst
time in history–the
number of U.S. jobs in
health care surpassed
those in manufacturing
and retail, a trend driven
largely by the growth in
older people and rising
health care costs. The
Atlantic explored this
historic development,
noting that personal care
aides and home health
aides will represent one
in 10 new jobs over the
next decade.
(January 9, 2018)
“HOW A HEATED
IMMIGRATION
DEBATE MIGHT AFFECT
GRANDMA’S CARE”
One of many articles
over the last year that
covered the role of
immigrants in eldercare,
this article from The Wall
Street Journal drew an
illustrative link between
the care received by
older people—or
“grandparents,” which
personalized the issue
for readers—and the
growing hostility toward
immigrants, many of
whom are on the front
lines of that care.
(January 22, 2018)
“FOR HEALTH CARE
WORKERS, THE
WORST COMMUTES
IN THE CITY”
Delrisa Sewell-Henry,
the New York City home
health aide at the center
of this article from The
New York Times, spends
hours every day on
public transportation to
reach her client. Long
commutes are especially
tough for home care
workers, who can lose
earnings for being
late, as well as for their
clients, who experience
disruptions in their care.
(January 22, 2018)
“HELPING EMPLOYERS
FIND SUCCESS”
While other articles
explored the negative
consequences of
anti-immigrant policies
on the direct care sector,
Provider Magazine took
a different approach. It
proled an assortment
of long-term care
providers around
the country that are
intentionally recruiting
foreign-born workers and
instituting immigrant-
friendly supports in their
workplaces.
(January 22, 2018)
TOP 20 NEWS STORIES ON DIRECT CARE WORKERS
Newspapers
How
Told the Workforce Story
Media outlets do more than relate the latest news and opinions–they shape
the public’s beliefs about major issues. Their stories frame the national
conversation and influence what policymakers consider important, bringing
pressing issues to life. This year, the news coverage on direct care workers
seemed stronger than ever, covering an array of topics–immigration,
transportation, nursing homes, and much more. Here are 20 highlights.
17
PHI
|
YEAR IN REVIEW 2018
1 2 3 4
1
2
3
4

“IF IMMIGRANTS ARE
PUSHED OUT, WHO
WILL CARE FOR THE
ELDERLY?”
The New York Times
captured the immediate
consequences of the
Trump administration’s
anti-immigrant actions
on the caregiving system:
the growing fear among
people who rely on
home care workers to
get through the day, as
well as the challenges
faced by long-term
care employers that rely
on immigrant workers
and can’t nd enough
job applicants to ll
positions.
(February 2, 2018)
“MAINE BALLOT
EFFORT WOULD
MANDATE HOME
CARE FOR ELDERLY,
DISABLED”
Long-term care is
profoundly expensive,
and people who don’t
qualify for Medicaid
have limited options.
In response, states are
increasingly considering
policy options that
would make long-term
care more affordable to
their residents.
This Associated Press
article covered a ballot
initiative in Maine that
was part of the growing
momentum for these
reforms.
(February 4, 2018)
“WHERE WILL OUR
HOME CARE AIDES
COME FROM?”
Tax and retirement
expert–and Forbes
columnist–Howard
Gleckman nicely
summarized the
pressures facing the
home care workforce:
low wages, benets, and
the challenge of lling
these marginal positions,
among others. Worse,
many people can’t afford
these services. Gleckman
wrote: “Demand for
those aides will increase
by 50% over just the
next decade, to 3 million.
But where will they
come from?”
(February 28, 2018)
“AS TRUMP TARGETS
IMMIGRANTS,
ELDERLY AND OTHERS
BRACE TO LOSE
CAREGIVERS”
When the Trump
administration
announced it would end
Temporary Protected
Status for various
countries, including
Haiti, Kaiser Health
News investigated the
impact of this change
on workers, clients, and
the broader caregiving
system, where immigrants
are substantial. Two
Boston residents form the
heart of this story: Nirva,
a Haitian immigrant,
and her client, Isolina,
a 96-year-old Italian
immigrant.
(March 26, 2018)
NY DOCTORS DON’T
PAY ATTENTION TO
HOME HEALTH CARE
PLANS”
How much time do
physicians spend
reviewing home health
care plans for their
patients? Forty-seven
percent spend less
than one minute,
and only 21 percent
spend more
than two minutes. Reuters
explored these startling
ndings, emphasizing
the importance
of strengthening
relationships between
doctors and the home
care system, among
other solutions.
(April 2, 2018)
“THE U.S. CAN’T KEEP
UP WITH DEMAND
FOR HEALTH AIDES,
NURSES AND
DOCTORS”
This article from CNN
had three alarming
statistics to substantiate
its dire claim: by
2025, the health care
system will need 2.3
million new health
care workers, including
nurses, physicians, lab
technicians, and other
workers. The largest need
will be for home health
aides, at about 423,000
jobs. And what’s the
estimated shortage for
home health aides in that
period? 446,300.
(May 4, 2018)
5
8
6
7
TOP 20 NEWS STORIES ON DIRECT CARE WORKERS
18
5
6
8
10
10
7
9
9
PHI
|
YEAR IN REVIEW 2018

“HOW TRUMP’S
IMMIGRATION
POLICIES COULD HURT
SENIOR CARE”
TIME magazine built
on previous news stories
about immigrants in
the direct care sector
by analyzing how these
workers are being
affected by the federal
administration’s recent
actions. It reported that
about 34,600 workers
originated from countries
that will lose Temporary
Protected Status in the
next two years because of
a new Trump-era policy.
The article asks: without
enough immigrants,
who will take these
poor-quality jobs?
(May 10, 2018)
“WHEN YOUR SEXUAL
ABUSER IS ALSO
YOUR PATIENT”
The #MeToo movement
reached the home care
industry this summer
when The Hufngton
Post released an exposé
on sexual harassment in
home care, centered
on a New York City
home care worker
experiencing sexual
harassment from
her client. The article
also opined on the larger
context: “All of which is
to say this is a vulnerable
group of workers, often
shouldering the triple
burden of racism, sexism
and near-poverty wages.”
(June 2, 2018)
“IT’S ALMOST LIKE A
GHOST TOWN.’ MOST
NURSING HOMES
OVERSTATED STAFFING
FOR YEARS”
Nursing home advocates
have long raised
concerns about stafng
levels at nursing homes
and the measures used
to assess those levels.
This New York Times
article blew the lid off this
topic, exploring new data
from Kaiser Health News
that showed signicant
stafng challenges
among more than 14,000
nursing homes–all
based on new payroll
records from Medicare,
as required by the
Affordable Care Act.
(July 7, 2018)
“MINNESOTA ROLLS
OUT FIRST STATEWIDE
JOB BOARD FOR HOME
CARE SUPPORT”
Online job portals–and
“matching service
registries”–are gaining
traction in states as a way
for consumers to nd
workers who meet their
needs and preferences–
and for workers to nd
jobs or employers that
match their interests.
Minnesota’s Star Tribune
reported on a new
statewide portal in
Minnesota that will do
exactly that, making life
easier for consumers
and workers.
(July 12, 2018)
“WHY DOES ONE OF
THE MOST NEEDED
JOBS PAY SO
POORLY? PT. 1”
“THE U.S. NEEDS
MORE HOME CARE
WORKERS. IS THIS
THE SOLUTION? PT. 2”
PBS traveled to
Minnesota to examine
the growing challenges
in recruiting and
retaining home care
workers. The rst part
in this two-part series
looked at the primary
reasons for high turnover
in this sector, including
a $10 wage that has
remained stagnant for
years, making it difcult
to compete with other
low-wage industries. Part
two explored solutions,
including the potential of
advanced roles in raising
compensation levels for
home care workers.
(Jul 26, 2018)
(August 9, 2018))
“MEDICARE SLASHES
STAR RATINGS FOR
STAFFING AT 1 IN 11
NURSING HOMES”
Shortly after Medicare
published new payroll
data on nursing homes,
Kaiser Health News (and
The New York Times)
uncovered severe stafng
challenges in these
homes, placing residents
at enormous risk. In July,
the Times published
a follow-up piece on
Medicare’s decision to
lower its star rating on
stafng levels, which
affected one out of
11 nursing homes–
1,400 in total.
(July 27, 2018)
16
11
12
14
TOP 20 NEWS STORIES ON DIRECT CARE WORKERS
19
PHI
|
YEAR IN REVIEW 2018
11
13
13
12
14
16
15
15

“LITTLE WAGE
GROWTH FOR HOME
CARE WORKERS IN
LAST DECADE”
PHI’s annual data on
home care workers and
nursing assistants have
provided an essential
benchmark to assess how
workers fare over time.
Home Health Care News
reported on an unnerving
statistic in this year’s
research: over the last
decade, personal care
aide wages increased
by only 95 cents, while
home health aide and
nursing assistant wages
dropped by 11 cents.
Wages in this sector are
at a standstill.
(September 4, 2018)
“AMERICANS WANT TO
BELIEVE JOBS ARE THE
SOLUTION TO POVERTY.
THEY’RE NOT.”
The New York Times
issued this searing and
illuminating essay on
poverty, challenging the
notion that employment
necessarily keeps people
out of poverty. At the
center of this article is
Vanessa Solivan, a home
health aide in New
Jersey, whose life vividly
embodies how poverty
becomes entrenched,
perhaps inescapable, for
many low-wage workers.
(September 11, 2018)
“MISSED
OPPORTUNITIES:
COULD HOME
HEALTH AIDES PLAY
A GREATER ROLE?”
Can the home care
job be re-imagined,
creating more satisfying
and expansive roles for
workers, and improving
the quality of supports
for clients? Would these
roles save the system
money? And what’s
preventing the eld
from adopting these
roles? These are a few
questions that WTVF (an
NPR afliate) examined
in its in-depth article on
home care aides and
advanced roles.
(September 25, 2018)
“A RADICAL SOLUTION
TO THE IMPOSSIBLE
COST OF CARING FOR
THE ELDERLY”
The heart-wrenching
protagonists of this story
from Mother Jones are
a working-class family
struggling to obtain paid
support as they care
for each other through
dementia, cancer, and
the frailty of old age. It
argued that “universal
home care”–an idea
emerging at the state
level–could make life
much easier for this
family, and in turn, the
rest of us. But will it
become reality?
(October 2018)
TOP 20 NEWS STORIES ON DIRECT CARE WORKERS
PHI
|
YEAR IN REVIEW 2018
20
17
20
19
18
17 18 19
20
PHInational.org
Learn about our consulting services,
policy research, advocacy, and public
education campaigns
Scroll through our multi-media library of
research, analysis, and other resources
Download state-by-state data on the
direct care workforce
Bookmark our newsroom for the latest
news and opinion: PHInational.org/news/
Subscribe to our monthly newsletter:
PHInational.org/sign-up/
Join our online community on Facebook,
Twitter, and LinkedIn (@PHInational)

WORKPLACE INJURIES
AND THE DIRECT CARE
WORKFORCE
Direct care work can
often lead to injuries,
including sprains, tears,
soreness, and pain.
This study showed
that injury rates are
alarmingly high for
direct care workers,
especially among
nursing assistants
who often overexert
themselves while
repositioning multiple
clients a day. In 2016,
the injury rate (per
10,000 workers) for
nursing assistants was
337, compared to 100
among all occupations.
BENCHMARKING
THE ELDERCARE
WORKFORCE: A
COMMUNITY FOCUS
How should we measure
the need for eldercare
workers in a geographic
community, taking into
account the population’s
needs, worker availability
and caseloads, and hours
of support (among other
variables)? This report
tackled this question by
devising a method that
estimated workforce
need in the Washington,
DC area, and provided
a thoughtful benchmark
that could yield more
data and better
measures in the
years ahead.
USING TELEHEALTH TO
IMPROVE HOME-BASED
CARE FOR OLDER
ADULTS AND FAMILY
CAREGIVERS
Telehealth has the
potential to lower costs
and to improve access
and care outcomes
among older consumers
in home care. This
publication examined
various telehealth
strategies in home care,
including transitional care
for heart failure, palliative
care, and more. It also
encouraged policymakers
to better reimburse
the costs of telehealth
in home care and to
limit harmful restrictions
regarding its use.
THE PART-TIME
DILEMMA FOR DIRECT
CARE WORKERS
The combination of
low wages and part-
time hours forces many
workers into poverty.
This study revealed
that one in three direct
care workers works part
time, many of whom
are supporting family
members, retired,
enrolled in school, or
dealing with health
conditions that prevent
full-time hours. One in
four part-time workers
works part time due to
conditions at their place
of work or in their local
economy.
9 PUBLICATIONS FOR THE DIRECT CARE SECTOR
Organizations
How
Examined the Workforce
Nonprofit and government leaders are increasingly shining a spotlight on direct
care workers, analyzing their experiences and needs, as well as their relationship
to the long-term care system. This year, a varie of reports explored the direct
care workforce across an array of topics, from workplace safe to transportation,
and much more. Here are nine reports that caught our eye.
21
PHI
|
YEAR IN REVIEW 2018
PHI
1
ALTARUM
2
AARP
PUBLIC POLICY
INSTITUTE
3
PHI
4

FILLING THE CARE GAP:
INTEGRATING FOREIGN-
BORN NURSES AND
PERSONAL CARE
ASSISTANTS INTO
THE FIELD OF
LONG-TERM SERVICES
AND SUPPORTS
The sharp growth in
older people–both
domestically and
abroad–has compelled
signicant demand for
long-term care workers
around the world. This
report examined the
potential of foreign-
born workers to ll
this gap, reporting
on workforce data
across occupations,
identifying strategies
to hire and retain
immigrant workers,
and offering a slate
of recommendations
to strengthen this
critical segment of the
workforce.
AN UNHEALTHY
COMMUTE: THE
TRANSIT CHALLENGES
FACING NEW YORK
CITY’S HEALTHCARE
SECTOR
In a given week, the
typical home care
worker in New York City
travels hours through
public transit to multiple
homes. Unfortunately,
many of these trips are
extremely long, highly
stressful, and costly—all
of which contribute to
high turnover. These
challenges also threaten
the quality of care
for consumers. This
report examined the
transportation concerns
facing healthcare
workers in the largest
city in the country.
COMPETENCY GUIDE
FOR DEMENTIA
CARE: DIRECT
CARE WORKFORCE
DEVELOPMENT
Approximately 5.7
million people in the
United States live with
dementia, a population
that requires urgent
and tailored support,
particularly from
direct care workers.
Unfortunately, these
workers are rarely
trained in dementia
care, leaving many
people without proper
care. This competency
guide outlines the
main topics and
competencies related
to dementia care, as
well as key training
elements.
ACROSS THE STATES
2018: PROFILES OF
LONG-TERM SERVICES
AND SUPPORTS
For 24 years, this
valuable reference
book has provided
annual state data,
rankings, and national
averages across a range
of topics related to
long-term services and
supports, including
age demographics and
projections, costs of
care, disability rates,
and more. One notable
nding from this year:
state Medicaid
systems are dedicating
a higher percentage
of spending for home
and community-based
services.
DIRECT CARE WORKER
RACIAL DISPARITIES SERIES:
ASIAN AND PACIFIC
ISLANDER DIRECT CARE
WORKERS
BLACK/AFRICAN
AMERICAN WORKERS
IN DIRECT CARE
HISPANIC/LATINO
DIRECT CARE WORKERS
This research series
took a closer look at
the unique challenges
facing people color
who work in direct care.
Two notable ndings:
the series found that
nearly half of Hispanic/
Latino direct care
workers are immigrants,
and U.S.-born Black/
African American
workers are more likely
to live in poverty than
white workers and
Black immigrants. This
research makes the
case for race-explicit
workforce strategies
that address these racial
inequities.
PHI
|
YEAR IN REVIEW 2018
22
9 PUBLICATIONS FOR THE DIRECT CARE SECTOR
GLOBAL AGEING
NETWORK &
THE LEADINGAGE
LTSS CENTER
@UMASS BOSTON
5
CENTER FOR AN
URBAN FUTURE
6
GEORGIA
ALZHEIMER’S
AND RELATED
DEMENTIAS
COLLABORATIVE
7
AARP
PUBLIC POLICY
INSTITUTE
8
PHI
9

Solutions
When we imagined #60CaregiverIssues, we sought to address one clear
problem: the worsening workforce shortage in home care. Within o years,
we unveiled 60 solutions, one idea at a time. And it worked—we
substantially grew our base of online supporters, generated significant
media coverage, and inspired policymakers to focus on the range of
challenges facing this job sector. As this campaign comes to an end, our
country seems to understand this problem in a whole new way—as one
that affects all of us, and one that can be xed.
From a Workforce Shortage to Concrete
#60CAREGIVERISSUES CAMPAIGN RECAP
23
PHI
|
YEAR IN REVIEW 2018

Learn About the Shortage
of Paid Caregivers
Issue Brief
As the number of older people
rises, the demand for home
care workers gets larger every
year. However, the poor quali
of home care jobs keeps away
good candidates. We examined
eight aspects of this shortage,
laying the foundation for this
campaign. (Feb 7, 2017)
Use a ‘Quality Jobs’
Framework to Measure
Policy Progress In Your State
Issue Brief
In the last decade, New York
State has implemented various
policy changes to strengthen
the home care workforce.
We used our “nine essential
elements of a quali job”
framework to examine how
New York fares when it comes
to direct care workers.
(Feb 22, 2017)
Expand Health
Coverage for the Direct
Care Workforce
Research Brief
Beeen 2010 and 2014, half
a million direct care workers
gained health coverage, and
the uninsured rate across
this workforce decreased
by 26 percent. Our research
brief oered another lens on
the renewed debate on the
Aordable Care Act.
(Mar 7, 2017)
Take Federal Action
to Strengthen the
Direct Care Workforce
Report
A federal investment in the
home care workforce would
promote beer wages and
benefits, enhance training,
and create advanced roles—
and it would create a vibrant
system of care. We outlined
five urgent areas where federal
policymakers could act.
(Mar 21, 2017)
Create a Funding
Pool to Incentivize
Quality Jobs
Issue Brief
In 2014, New York State
created a funding pool that
supported licensed home care
agencies that met specific
training and employment
standards, incentivizing the
field to strengthen its home
care workforce. We analyzed
the impact of this approach.
(Apr 4, 2017)
Map the Direct Care
Workforce in Your State
Research Brief
A state-level snapshot of
the home care workforce
provides a quick, initial view
of the challenges facing this
workforce. In that spirit,
we produced a detailed fact
sheet on Illinois’ home care
workforce, including key
demographics and employment
data. (Apr 18, 2017)
Map the Home Care
Industry in Your State
Report
Our landscape studies widen
the pical lens on home care
workers–capturing critical
insights about the broader
industry. Our report on home
care in Minnesota used this
analytical approach to inform a
multi-year, state-level initiative
led by PHI. (May 2, 2017)
PHI
|
YEAR IN REVIEW 2018
24
1
4
6
7
5
2
3
#60CAREGIVERISSUES CAMPAIGN RECAP

Consider How Benets
Affect Earnings
Slideshow
The interplay beeen wages
and benefit eligibili can mean
that many low-income workers
don’t earn higher incomes
simply by working more hours.
We studied this phenomenon
and showed how workers
might be wrongly incentivized
to limit their work hours.
(May 16, 2017)
Create an Advanced
Role to Improve Care
Video
With proper training, home
care workers can take on more
expansive roles that improve
care for clients and promote
job satisfaction. We partnered
with WorkingNation to
produce a video on a
successful advanced role
model from PHI.
(May 30, 2017)
Support Immigrants
in the Direct Care
Workforce
Research Brief
One in four home care workers
is an immigrant, and nearly
1 million immigrants work in
the direct care sector. Yet they
face unique challenges that
are made worse by increased
public hostili. We produced
new data on this critical
workforce segment.
(June 20, 2017)
Convene a Home
Care Dialogue
Issue Brief
As various trends and new
laws reshape the home care
industry, home care providers
must find ways to engage each
other and forge solutions.
In May 2017, PHI gathered
seven New York agencies for a
roundtable discussion on the
future of home care.
(July 11, 2017)
Provide Adult Learner-
Centered Training
Issue Brief
Adult learner-centered
training enhances learning
by incorporating a range of
methods, such as games,
role-playing, and more. In
2015, PHI worked with home
care providers in Chicago
to develop a training rooted
in adult learner-centered
philosophy. (July 25, 2017)
Map the Direct Care
Workforce in Your City
Research Brief
In many cities, home care
jobs boost the economy, yet
wages in this sector remain
catastrophically low. As a
result, home care workers can’t
support themselves and they
eventually leave the sector.
We studied the home care
workforce in Detroit.
(Aug 9, 2017)
25
PHI
|
YEAR IN REVIEW 2018
8
9
11
10 12
13
THE FUTURE OF
LONG-TERM CARE
EVERYTHING SHIFTS. THE FUTURE
BELONGS TO THOSE WHO ENVISION IT.

Implement a Tested
Workforce Approach
Research Brief
Long-term care providers
are seeking strategies that
successfully recruit and
retain home care workers,
recognizing how dicult it has
become to sta their agencies.
We compiled six approaches
that PHI has used to strengthen
this workforce. (Aug 22, 2017)
Improve Wages and
Hours for Workers
Research Brief
Low wages and insucient
hours make home care jobs
unaordable and unappealing
for workers. In turn, the
workforce shortage worsens.
Our annual data on home care
workers and nursing assistants
describes, in statistical terms,
the state of these jobs.
(Sept 6, 2017)
Adopt Training
Standards for Personal
Care Aides
Case Study
Personal care aides nationwide
have marginal training
standards, which leaves many
of them ill-prepared to provide
quali care and succeed on
the job. We studied the process
through which Arizona enacted
uniform training standards for
these workers. (Sept 12, 2017)
Enhance Access
to Rural Home Care
Report
Home care delivery is
complicated in rural America,
where health resources are
thin, and workers are in short
supply, often traveling long
distances to reach clients.
We studied the home care
landscape in Wisconsin,
exploring these dynamics.
(Sept 21, 2017)
Train and Certify
Workers Across Settings
Case Study
Too often, the training
requirements for home health
aides far surpasses what exists
for personal care aides. We
explored how Iowa is trying
to create a competency-based
training and certification
system that spans all direct
care workers. (Sept 26, 2017)
Reform the Training
System for Personal
Care Aides
Case Study
Training requirements aren’t
the only way to improve
training for home care workers.
Our case study on Washington
State showed how a state
ballot initiative increased
training hours and introduced
certification requirements for
personal care aides.
(Oct 3, 2017)
PHI
|
YEAR IN REVIEW 2018
26
TRAINING AND
ADVANCED ROLES
BECAUSE A GOOD JOB SHOULD
LEAD TO A GREAT CAREER.
14
15
17
16 18
19

Invest Federal Dollars
in Advanced Roles
Fact Sheet
Advanced roles that allow
direct care workers to handle
new responsibilities can
improve care and reduce
costs. This fact sheet profiled a
federal bill that would establish
demonstration projects that
test advanced roles in home
care. (Oct 10, 2017)
Fund a National
Strategy for
Recruitment and Retention
Fact Sheet
Strategies that eectively
recruit and retain home care
workers can transform the
quali of care. This fact sheet
described a federal bill that
would promote recruitment,
retention, and advancement
opportunities among direct
care workers. (Oct 17, 2017)
Formulate a National
Policy Vision
Journal Article
As the policy landscape shifts
for direct care workers, the
home care field needs a
national roadmap that spans a
multitude of issues. This article
from Public Policy & Aging
Report described the various
considerations for developing
this vision. (Oct 24, 2017)
Examine Racial and
Gender Disparities
Research Brief
In an already marginalized
workforce, some workers fare
worse than others. Our study
on racial and gender disparities
in the direct care workforce
found that women of color
have higher pover rates and
access public benefits more
than their peers. (Nov 8, 2017)
Train Workers
in Alzheimer’s and
Dementia
Issue Brief
Despite the growing number
of people with Alzheimer’s
disease and other forms of
dementia, home care workers
are rarely trained on this topic.
We outlined five state-level
policy recommendations to
improve home care training on
dementia. (Nov 21, 2017)
Bolster the
Economy through
Direct Care Jobs
Research Brief
A startling fact from 2017:
from 2016 to 2026, the
long-term care sector
will create 1.8 million jobs,
including 1.2 million jobs in
direct care. We examined what
it means that job creation is
increasingly driven by jobs
that are poor in quali.
(Nov 28, 2017)
Develop a Statewide
Matching Service Registry
Online Map
A statewide matching service
registry helps home care
workers and consumers find
each other. It can also improve
employment in this sector.
We created an online state
data map depicting the status
of matching service registries
nationwide. (Dec 5, 2017)
Track Data on the
Direct Care Workforce
Workforce Data Center
Regular data on the direct care
workforce help long-term
care leaders understand
how these workers fare
over time and by state,
as well as where we
need more data.
We rebooted
our online workforce
data center to
provide this crucial
information.
(Dec 7, 2017)
27
PHI
|
YEAR IN REVIEW 2018
20
21
22
23
26
27
24
25
#60CAREGIVERISSUES CAMPAIGN RECAP

Articulate a State
Policy Agenda
Policy Brief
From raising wages to
improving training, and much
more, states are shifting how
they support the direct care
workforce. We partnered with
the Working Poor Families
Project to produce a review of
state policy strategies related
to this workforce.
(Dec 14, 2017)
Adopt a Culturally
Competent Approach
Q&A
Home care leaders are
gradually responding to
the growing diversi in
our country by developing
culturally competent workforce
approaches. We spoke
with a New Mexico-based
organization about its home
care training program for
immigrants. (Dec 19, 2017)
Launch a Public
Education Campaign
Campaign Recap
To change minds and compel
action, public education
raises the visibili of
home care workers and the
growing workforce
shortage in this sector.
We summarized the first
30 issues in our award-
winning #60CaregiverIssues
campaign. (Dec 27, 2017)
Support Black
Direct Care Workers
Research Brief
Do racial and gender
inequalities make it more
dicult for certain segments
of the home care workforce to
succeed? To understand this
question, we launched a three-
part research series on racial
and ethnic disparities within the
direct care workforce.
(Feb 6, 2018)
Support Latino
Direct Care Workers
Research Brief
Latino home care workers
might be facing unique
obstacles on the job, which
aects turnover. The second
part in our disparities series
showed that although one in
six direct care workers is
Latino, many of these workers
struggle with pover.
(Feb 13, 2018)
Support Asian and
Pacic Islander Workers
Research Brief
Tailored training and on-the-
job supports can stabilize
employment for many people
of color working in direct care.
The third part in our disparities
series revealed significant
disparities within Asian and
Pacific Islanders workers in
direct care. (Feb 20, 2018)
Create a Division
of Paid Care
Q&A
Cities and towns can also find
ways to strengthen jobs for
home care workers. We spoke
with New York Ci’s division
of paid care, which was
established in 2016 to support
home care workers, childcare
workers, and housecleaners
throughout the ci.
(Mar 13, 2018)
PHI
|
YEAR IN REVIEW 2018
28
28
29
31
33
34
30
32
#60CAREGIVERISSUES CAMPAIGN RECAP

Support Part-Time
and Full-Time Workers
Research Brief
One in three direct care workers
works part time, sometimes
because they can’t obtain full-
time hours, and in other cases
because they’re raising children,
supporting family members, or
aending school. We studied the
reasons for part-time schedules.
(Mar 27, 2018)
Recruit Younger
Workers
Fact Sheet
Younger people aged 18 to
24 comprise nearly 13 percent
of the U.S. labor force and
could help broaden the labor
pool of direct care workers.
We provided a snapshot of this
workforce segment as part of a
series on “new populations”
for direct care. (Apr 3, 2018)
Recruit Older Workers
Fact Sheet
Workers aged 55 and over
currently make up 23 percent
of the direct care workforce
and might comprise a larger
portion in future years, as the
number of older adults grows.
We took a closer look at this
growing segment of the U.S.
labor force. (Apr 10, 2018)
Recruit Men
to Direct Care
Fact Sheet
The U.S. labor force includes
99 million men, many of whom
could fill the demand for direct
care workers as the country
rapidly ages. We studied this
small but growing segment
of the direct care workforce,
arguing for gender-specific
employment supports.
(Apr 17, 2018)
Promote
Workplace Safety
Fact Sheet
Home care workers and
nursing assistants experience
exceptionally high rates of
occupational injury, many
of which can be prevented.
We studied the main causes
of injury among direct care
workers and identified
strategies for mitigating those
risks. (Apr 24, 2018)
Craft a Recruitment
and Retention Strategy
Guide
Long-term care employers
struggle to recruit and retain
direct care workers, largely
because the quali of these
jobs remains poor. In response,
we outlined 10 strategies
that employers can use to
successfully hire and hold onto
these workers. (May 15, 2018)
29
PHI
|
YEAR IN REVIEW 2018
STORIES FROM THE FIELD
MEET THE PEOPLE AND PROVIDERS
WHO CARE FOR OUR FAMILIES.
35
36
37
38
39
40

Enact Paid Family and
Medical Leave
Slideshow
Direct care workers should be
able to take paid time o to
support themselves or their
loves ones, yet these laws exist
in few parts of the country.
We identified various ways for
states to provide paid family
and medical leave for this
workforce. (May 30, 2018)
Recruit Through
Social Media
Slideshow
Social media has the potential
to improve recruitment
for home care providers.
We profiled a Minnesota-
based digital media firm
that partnered with a nearby
provider to overhaul its
recruitment strategies–within
a year, recruitment figures
skyrocketed. (June 19, 2018)
Create a Person-
Centered Workplace
Videos
A person-centered approach in
direct care honors both clients
and workers, ensuring that
clients receive the support they
want, and workers access the
workplace supports they need.
We featured o experts who
explained how to create this
approach. (Jul 17, 2018)
Develop Effective
Supervisors
Videos
When supervisors build trust
and impart a sense of belief,
their employees stay on the
job. In contrast, when that
trust is breached, workers lose
interest, and many leave their
direct care roles. Our videos
oered tips for improving
supervision. (Jul 31, 2018)
Form a Statewide
Coalition
Webinar
A unified voice in support of
direct care workers can change
this sector for the beer, and
in many states, coalitions
are creating that voice. PHI
interviewed a group of leading
experts to understand how
coalitions are improving rural
home care. (Aug 29, 2018)
Establish a National
Benchmark
Research Brief
Annual data on U.S. home care
workers helps reveal how these
workers are doing over time
and where they need support.
Our annual research brief on
home care workers oered a
detailed snapshot, reinforcing
an important benchmark for
our field. (Sep 4, 2018)
INNOVATIONS
BECAUSE EVERY STEP TOWARDS
PROGRESS BEGINS WITH A SMART IDEA.
PHI
|
YEAR IN REVIEW 2018
30
41
42
44
46
4543

Strengthen the Entire
Workforce
Research Brief
When we strengthen jobs for
nursing assistants, we elevate
the value of direct care workers
across the sector. Our annual
data on nursing assistants
employed in nursing homes
illustrates the various ways in
which this workforce continues
to struggle. (Sep 6, 2018)
Create Immigrant-
Specic Supports
Fact Sheet
How can we ensure that
immigrants continue to be a
strong part of the direct care
workforce? Our data update
on immigrants in this
workforce oered three
concrete ways for long-term
care leaders to bolster supports
for this segment of workers.
(Sep 11, 2018)
Examine County-Level
Workforce Data
Research Brief
A coun-level data analysis can
bring to light dierences within
a state–an important lens when
developing a statewide strategy
for the direct care workforce.
We used a coun-level analysis
to study this workforce in
Maryland and DC.
(Sep 27, 2018)
Propose Concrete
Policy Fixes
Fact Sheet
States can enact various policy
reforms to strengthen this
workforce–but this begins with
a concise platform. We outlined
seven policy recommendations
for New York State, including
funding to improve recruitment
and retention in our sector, and
six more. (Oct 9, 2018)
Elevate Direct Support
Professionals
Slideshow & Lecture
Direct support professionals are
vital to people with intellectual
and developmental disabilities,
yet their jobs are in jeopardy.
We delivered a lecture on this
topic for The Boggs Center on
Developmental Disabilities at
Rutgers New Jersey Medical
School. (Oct 16, 2018)
Support Worker-
Centered Technology
Article
Technological innovations are
gaining traction in long-term
care, spurring conversations
about their potential to
improve both jobs and care.
We identified seven ways that
long-term care leaders are using
technology to support direct
care workers. (Oct 23, 2018)
Promote E-Learning
Approaches
Q&A
E-learning approaches
are becoming increasingly
popular in the long-term care
sector, allowing employers to
eciently train larger numbers
of workers, while potentially
saving costs. PHI’s Jerry Philip
oers an analysis on e-learning
in direct care. (Nov 6, 2018)
Change the Media
Narrative
Article
When journalists write in-depth,
balanced articles on the direct
care workforce, they help their
readers understand the breadth
and complexi of issues facing
these workers. We selected the
top 20 news stories of 2018 on
the direct care workforce.
(Nov 13, 2018)
Examine County-Level
Workforce Data
Research Brief
A coun-level data analysis
can illuminate similarities and
dierences–an important lens
when developing a statewide
strategy to strengthen the
direct care workforce. We used
a coun-level analysis to study
this workforce in Maryland and
DC. (Sep 11, 2018)
31
PHI | YEAR IN REVIEW 2018
47
50
53
48
51
52
54
49
31
PHI
|
YEAR IN REVIEW 2018
#60CAREGIVERISSUES CAMPAIGN RECAP

Produce An
Original Report
Article
Organizations are increasingly
publishing important reports
on direct care, bringing their
unique lens and organizational
expertise to one of the most
critical workforces in the
country. We profiled nine
policy reports from 2018 that
caught our eye. (Nov 20, 2018)
Establish State-
Sponsored Curricula
Research Brief
To raise the bar on personal
care aide (PCA) training, six
states have developed model
curricula. We examined these
state-sponsored curricula
to identify best practices in
training methods and content
for PCAs and other direct care
workers. (Nov 27, 2018)
Listen to
Worker Stories
Infographic
We compiled an array of
compelling stories from home
care workers in Wisconsin
that illustrate their skills and
dedication. These stories
also exemplify why it’s essential
to tap into the wisdom of
workers to strengthen
workforce interventions.
(Dec 4, 2018)
Educate Through
Social Media
Article
With its vast reach and
widespread use, social media
has the potential to improve
how home care workers are
valued in today’s world—and
long-term care leaders are
increasingly tapping its power.
We oered six lessons from
o successful campaigns in
2018. (Dec 11, 2018)
Stay Current on
News and Trends
Year in Review
Staying on top of current
developments ensures that
leaders have the latest insights
into how direct care is
changing—and where it’s going.
Our first-ever “Year in Review”
summarized the year’s most
important developments for
the direct care workforce.
(Dec 18, 2018)
Dream Big Ideas
Article
In our final issue, we celebrate
the imagination and the end
of #60CaregiverIssues by
reflecting on 60 great ideas.
The workforce shortage in
home care at one point seemed
unsolvable—but a creative
education campaign helped
illuminate the way forward.
(Dec 26, 2018)
PHI
|
YEAR IN REVIEW 2018
32
2018 Communicator Award
In 2018, #60CaregiverIssues received an Award of Distinction in integrated campaigns from
the Academy for Interactive Visual Arts. The Communicator Awards is the largest and most
competitive awards program honoring creative excellence for communications professionals.
55
57
59
58
60
56
#60CAREGIVERISSUES CAMPAIGN RECAP

AUTHOR: Robert Espinoza
DESIGN: RD Design
PHOTOGRAPHY: (pg. 4) Valdek Dmytrowski
(pg. 8) Laurie Falk McVean
ILLUSTRATION: (pg. 23-31): Mark Conlan

400 East Fordham Road, 11th Floor
Bronx, NY 10458
Phone: 718.402.7766
Fax: 718.585.6852
Email: [email protected]g
PHInational.org
60CaregiverIssues.org
f
t
i
