E
mployee
B
enefits
S
ecurity
A
dministration
U
.
S
.
D
epartment of
L
abor
November 2014
The Affordable Care Act
H
ealth
I
nsurance
P
ortability
and
A
ccountability
A
ct
Genetic Information Nondiscrimination
A
ct
Mental Health Parity Provisions
N
ewborns' and
M
others'
H
ealth
P
rotection
A
ct
W
omen's
H
ealth
and Cancer Rights Act
C
ompliance
A
ssistance
G
uide
H
ealth
B
enefits
C
overage
U
nder
F
ederal
L
aw...
H
ealth
B
enefits
C
overage
U
nder
F
ederal
L
aw...
C
M
Y
CM
MY
CY
CMY
K
covers Labor Compliance 2014mx.pdf 1 11/19/2014 2:05:01 PM

C
ompliance
A
ssistance
G
uide
H
ealth
B
enefits
C
overage
U
nder
F
ederal
L
aw...
H
ealth
B
enefits
C
overage
U
nder
F
ederal
L
aw...
This publication has been developed by the
U.S. Department of Labor, Employee Benefits
Security Administration (EBSA). To view this and
other EBSA publications, visit the agency’s Website at
dol.gov/ebsa.
To order publications or to request assistance from a
benefits advisor, contact us electronically at
askebsa.dol.gov.
Or call toll free 1-866-444-3272.
This material is available in alternative format to
persons with disabilities upon request:
Voice phone: (202) 693-8664
TDD: (202) 501-3911
This publication constitutes a small entity
compliance guide for purposes of the
Small Business Regulatory Enforcement
Fairness Act of 1996.
E
mployee
B
enefits
S
ecurity
A
dministration
U
.
S
.
D
epartment of
L
abor
The Affordable Care Act
H
ealth
I
nsurance
P
ortability
and
A
ccountability
A
ct of
1996
Genetic Information Nondiscrimination
A
ct
Mental Health Parity Provisions
N
ewborns' and
M
others'
H
ealth
P
rotection
A
ct of
1996
W
omen's
H
ealth
and Cancer Rights Act of
1998

C
ompliance
A
ssistance
G
uide
H
ealth
B
enefits
C
overage
U
nder
F
ederal
L
aw...
H
ealth
B
enefits
C
overage
U
nder
F
ederal
L
aw...
This publication has been developed by the
U.S. Department of Labor, Employee Benefits
Security Administration (EBSA). To view this and
other EBSA publications, visit the agency’s Website at
dol.gov/ebsa.
To order publications or to request assistance from a
benefits advisor, contact us electronically at
askebsa.dol.gov.
Or call toll free 1-866-444-3272.
This material is available in alternative format to
persons with disabilities upon request:
Voice phone: (202) 693-8664
TDD: (202) 501-3911
This publication constitutes a small entity
compliance guide for purposes of the
Small Business Regulatory Enforcement
Fairness Act of 1996.
E
mployee
B
enefits
S
ecurity
A
dministration
U
.
S
.
D
epartment of
L
abor
The Affordable Care Act
H
ealth
I
nsurance
P
ortability
and
A
ccountability
A
ct
Genetic Information Nondiscrimination
A
ct
Mental Health Parity Provisions
N
ewborns' and
M
others'
H
ealth
P
rotection
A
ct
W
omen's
H
ealth
and Cancer Rights Act
C
M
Y
CM
MY
CY
CMY
K
covers Labor Compliance 2014mx.pdf 2 11/19/2014 2:05:11 PM
Introduction...............................................................................................
The Aordable Care Act..........................................................................
HIPAA Portability Provisions................................................................
Special Enrollment........................................................................
Nondiscrimination Requirements..............................................
HIPAA and the Aordable Care Act Wellness
Program Requirements............................................................................
The Genetic Information Nondiscrimination Act..............................
Mental Health Parity Provisions............................................................
The Newborns’ and Mothers’ Health Protection Act.........................
The Women’s Health and Cancer Rights Act......................................
Applying and Enforcing Laws in Part 7 of ERISA.............................
Appendices
Appendix A: Self-Compliance Tools..............................................
Appendix B: Chart of Required Notices........................................
Appendix C: Model Notices..........................................................
5
9
17
19
23
27
33
41
49
53
57
61
131
137
Table of Contents

Health Benets Coverage Under Federal Law addresses the following laws that
can affect the health benets coverage provided by group health plans:
The Patient Protection and Affordable Care Act (Affordable Care Act)
The Health Insurance Portability and Accountability Act of 1996 (HIPAA)
(portability and nondiscrimination provisions only)
The Mental Health Parity and Addiction Equity Act (MHPAEA) and the
Mental Health Parity Act (MHPA) (Mental Health Parity Provisions)
The Newborns’ and Mothers’ Health Protection Act of 1996 (the
Newborns’ Act)
The Women’s Health and Cancer Rights Act of 1998 (WHCRA)
The Genetic Information Nondiscrimination Act of 2008 (GINA)
These health care laws are included in Part 7 of Title I of the Employee
Retirement Income Security Act of 1974 (Part 7 of ERISA). Also discussed
in this booklet are provisions of the Children’s Health Insurance Program
Reauthorization Act (CHIPRA) related to special enrollment rights, which are
included as part of the HIPAA Special Enrollment section on page 19.
The rules described in the following pages generally apply to group health
plans and group health insurance issuers (i.e., insurance companies). References
in this booklet are generally limited to “group health plans” or “plans” for
convenience. In addition, the booklet will help employers, plan sponsors, plan
administrators, third-party administrators, and other service providers to comply
with Part 7 of ERISA.
The requirements under Part 7 of ERISA generally apply to group health
plans with two or more participants who are current employees.
1
However, if
the coverage is insured, parallel provisions in the Public Health Service Act apply
to health insurance coverage offered in connection with group health plans with
as few as one employee who is a current participant under the plan. In addition,
1
The Mental Health Parity and Addiction Equity Act as included in Part 7 of ERISA exempts
group health plans of a small employer with 50 or fewer employees from its requirements.
However, insured group health plans in the small group market are required to comply with the
requirements of the Act in order to satisfy the essential health benets requirements under the
Affordable Care Act.
Introduction
5

the requirements of Part 7 of ERISA do not apply to excepted benets, such as
certain dental and vision coverage*.
The laws contained in Part 7 of ERISA (which is administered by the U.S.
Department of Labor) generally also appear in the Internal Revenue Code
(the Code), and the Public Health Service Act (PHSA). The Department of the
Treasury and the Internal Revenue Service administer the requirements under
the Code, and the U.S. Department of Health and Human Services (HHS)
administers the requirements under the PHSA.
For ease of use, Health Benets Coverage Under Federal Law is divided into
four sections:
The rst section includes general descriptions of the health care laws
mentioned above and frequently asked questions.
Following are self-compliance tools that can help to determine a plan’s
compliance with these laws. They include compliance tips that relate to
some common mistakes. (Note: please check the Website at dol.gov/ebsa/
healthlawschecksheets.html for updates to the self-compliance tools.)
Next, a chart summarizes the notices a plan must provide.
Finally, the last section includes model notices providing language that
may be used to comply with the various notice requirements.
While the booklet does not cover all the specics of these laws, it does assist
those involved in operating a group health plan to understand the laws and
related responsibilities. It provides an informal explanation of the statutes and
the most recent regulations and interpretations. The information is presented
as general guidance, however, and should not be considered legal advice. In
addition, some of the provisions discussed involve issues for which the rules
have not yet been nalized as of the date of publication of this booklet. The
proposed rules are noted. Periodically check the Department of Labor’s Website
(dol.gov/ebsa) under “Laws & Regulations” for publication of nal rules.
6
*See the Applying and Enforcing Laws in Part 7 of ERISA Section at page 57 of the Guide for a further discussion.

Some general notes:
As discussed later, States can change some of these Federal rules if
the State law is more protective of individuals (i.e., imposes stricter
obligations on health insurance issuers).
If the plan provides benets through an insurance policy or health
maintenance organization (HMO), you also may contact your State’s
insurance department. Visit the National Association of Insurance
Commissioners’ Website at naic.org for contact information.
If you have questions not specically addressed in this booklet, please
contact the Employee Benets Security Administration (EBSA) regional
office nearest you. A list of these offices is on the agency’s Website at dol.
gov/ebsa (view “About EBSA”). Or you may contact EBSA electronically
at askebsa.dol.gov or call toll free 1-866-444-3272.
7
The Aordable Care Act
The Patient Protection and Affordable Care Act (Affordable Care Act) was
signed into law on March 23, 2010. The Affordable Care Act added certain market
reform provisions to ERISA, making those provisions applicable to employment-based
group health plans. These provisions provide additional protections for benets under
employment-based group health plans. They include extending dependent coverage to age
26; prohibiting preexisting condition exclusions for all individuals and prohibiting the
imposition of lifetime and annual limits on essential health benets. As of 2014, most of
the Affordable Care Act protections are now in effect. The Departments of Labor, Health
and Human Services, and the Treasury (Departments) were tasked with issuing guidance
for the market reform provisions. The Departments continue to work with employers,
issuers, States, providers and other stakeholders to help them come into compliance with
the law and are working with families and individuals to help them understand the law
and benet from it, as intended.
Under the Affordable Care Act, plans can make some routine changes and generally
keep the coverage under their plan the same as it was on March 23, 2010. These
grandfathered health plans are required to comply with some but not all of the market
reform provisions under ERISA.
What is grandfathered status and how does a grandfathered plan
lose its status?
Generally, grandfathered plans are plans that were in existence, and in which
at least one individual was enrolled, on March 23, 2010. Grandfathered health
plans are exempt from many but not all Affordable Care Act market reforms.
Grandfathered plans lose their status if the plan makes one of the following six
changes:
1) Elimination of all or substantially all benets to diagnose or treat a
particular condition.
2) Increase in a percentage cost-sharing requirement (e.g., raising an
individual’s coinsurance requirement from 20% to 25%).
3) Increase in a deductible or out-of-pocket maximum by an amount that
exceeds medical ination plus 15 percentage points.
4) Increase in a copayment by an amount that exceeds medical ination
plus 15 percentage points (or, if greater, $5 plus medical ination).
5) Decrease in an employer’s contribution rate towards the cost of coverage
by more than 5 percentage points.
9
6) Imposition of annual limits on the dollar value of all benets below
specied amounts.
Additionally, plans must include a statement in any plan materials provided
to a participant or beneciary describing the benets provided under the plan,
that the plan or coverage believes it is a grandfathered health plan and it must
provide contact information for questions and complaints.
Which provisions of the Affordable Care Act apply to a grandfathered
health plan?
Grandfathered health plans are exempt from many, but not all Affordable Care
Act market reforms. Some of the new provisions applicable to grandfathered
plans include:
prohibition on preexisting condition exclusions
prohibition on excessive waiting periods
prohibition on lifetime/restricted annual limits
prohibition on rescissions
extension of dependent coverage
summary of benets and coverage and uniform glossary
Some of the new provisions not applicable to grandfathered plans include:
coverage of preventive services
internal claims and appeals and external review
patient protections
When do the provisions in the Affordable Care Act become
applicable?
The following provisions became effective for plan years beginning on or after
September 23, 2010.
prohibition on preexisting condition exclusions - only for individuals
under age 19
10
prohibition on lifetime limits (and restrictions on annual limits)
prohibition on rescissions
coverage of preventive services
extension of dependent coverage
internal claims and appeals and external review
patient protections
The Summary of Benets and Coverage and Uniform Glossary requirement
became effective as of September 23, 2012.
Other provisions became effective for plan years beginning on or after January 1,
2014.
prohibition on preexisting condition exclusions - for all individuals
wellness programs
prohibition on excessive waiting periods
prohibition on annual limits
Can plans require dependent children to be full-time students in
order to receive coverage to the age of 26?
No. Plans that offer dependent coverage for children are required to make the
coverage available until a child reaches the age of 26. Plans and issuers that offer
dependent coverage of children must offer coverage to enrollees’ adult children
until age 26, even if the young adult no longer lives with his or her parents, is not
a dependent on a parent’s tax return, or is no longer a student. This provision
applies to all group health plans regardless of grandfather status and became
effective for plan years beginning on or after September 23, 2010.
Can plans impose preexisting condition exclusions on new
enrollees?
No. Group health plans are prohibited from imposing any preexisting condition
exclusion. This prohibition generally is effective for plan years beginning on
or after January 1, 2014, but for enrollees who are under 19 years of age, this
prohibition became effective for plan years beginning on or after September 23,
2010. This provision applies to all group health plans regardless of grandfathered
status.
11

Can plans place lifetime or annual limits on the dollar value of
essential health benets?
Generally group health plans are prohibited from offering coverage that
establishes any lifetime or annual limits on the dollar value of essential health
benets. This prohibition became effective for plan years beginning on or after
September 23, 2010 for lifetime limits and January 1, 2014 for annual limits.
For more information regarding what benets are considered essential health
benets, visit HealthCare.gov. This provision applies to all group health plans
regardless of grandfathered status.
Are plans prohibited from rescinding group health plan coverage?
In general, a rescission is a retroactive cancellation of coverage. A group health
plan or a health insurance issuer can only rescind coverage in the case of fraud
or an intentional misrepresentation of a material fact, regardless of whether the
coverage is insured or self-insured, or whether the rescission applies to an entire
group or only to an individual within the group. Plans and issuers must provide
at least 30 days advance wrien notice to each participant who would be affected
by the rescission. The prohibition against rescissions became applicable for plan
years beginning on or after September 23, 2010 and applies to all group health
plans regardless of grandfathered status.
Are plans required to provide preventive services?
Group health plans must provide benets for certain recommended preventive
services and generally may not impose any cost-sharing for such services. The
recommended services, including immunizations and colonoscopies, are set
forth by the United States Preventive Services Task Force (USPSTF), the Health
Resources and Services Administration (HRSA) and the Advisory Commiee
on Immunization Practices (ACIP) of the Centers for Disease Control and
Prevention. A complete list of recommendations and guidelines that specify
the services that are required to be covered can be found at HealthCare.gov/
center/regulations/prevention.html. The preventive services provision became
applicable for plan years beginning on or after September 23, 2010, and does not
apply to grandfathered plans.
My plan requires participants to designate, among others, a
primary care provider. Is my plan required to comply with certain
requirements related to this designation?
If a group health plan requires the participant to choose a participating primary
care provider, the plan or issuer must allow the participant to choose any
participating primary care provider who is available to accept the participant.
With respect to a child, the plan or issuer must allow the designation of a
12
pediatrician as a child’s primary care provider if the provider participates in the
network of the plan or issuer. Furthermore, plans or issuers may not require
authorization or referral for a female participant who seeks coverage for OB/
GYN care provided by an OB/GYN specialist. The plan must provide a notice
informing the participants of the terms of the plan or health insurance coverage
regarding designation of a primary care provider. This provision became
applicable for plan years beginning on or after September 23, 2010, and does not
apply to grandfathered health plans.
Can plans continue to limit payments for out-of-network emergency
room services?
A group health plan that provides emergency services benets must cover
emergency services without preauthorization, even if the hospital or provider
is out-of-network. If the emergency services are provided out-of-network,
special rules related to cost-sharing requirements apply. Copayment amount
or coinsurance rates cannot exceed the cost-sharing requirements that would be
imposed if the services were provided in-network. Additionally, any other cost-
sharing requirement, such as a deductible or out-of-pocket maximum, can only
be imposed with respect to out-of-network emergency services if the cost-sharing
requirement generally applies to out-of-network benets. This provision became
applicable for plan years beginning on or after September 23, 2010, and does not
apply to grandfathered health plans.
Are all employment-based wellness programs subject to Affordable
Care Act requirements?
No. Many employers offer a wide range of programs to promote health and
prevent disease. For example, some employers may choose to provide or
subsidize healthier food choices in the employee cafeteria, provide pedometers
to encourage employee walking and exercise, pay for gym memberships, or ban
smoking on employer facilities and campuses. A wellness program is subject to
the Affordable Care Act and HIPAA nondiscrimination rules only if it is, or is
part of, a group health plan. If an employer operates a wellness program separate
from its group health plan(s), the program may be subject to other Federal
or State nondiscrimination laws, but it is generally not subject to the HIPAA
nondiscrimination regulations.
For a detailed discussion of the Affordable Care Act and HIPAA
nondiscrimination requirements that may apply to wellness programs offered
in connection with employment-based group health plan coverage, see page 27.
These provisions apply to both grandfathered and non-grandfathered plans and
became applicable for plan years beginning on or after January 1, 2014.
13
What requirements apply under the Affordable Care Act regarding
the claims and appeals processes that must be made available under
a group health plan?
All group health plans must maintain internal claims and appeals processes set
forth in the Department of Labor Claims Procedure rules. Additional protections
were added to ensure that participants have access to an effective appeals
process. The scope of adverse benet determinations eligible for internal claims
and appeals now includes a rescission of coverage. If an initial adverse benet
determination is an urgent care claim, the claimant must be notied of the benet
determination no later than 72 hours after the receipt of the claim.
If the plan denies the claim after the internal appeal, the Affordable Care
Act requires participants be given the opportunity to seek external review.
Plans must implement an effective review process that meets the minimum
requirements set forth in the regulations. The internal claims and appeals
and external review provisions do not apply to grandfathered plans and are
applicable for plan years beginning on or after September 23, 2010.
What is the Summary of Benets and Coverage and when must it be
provided?
Plans must provide a Summary of Benets and Coverage (SBC) that accurately
describes the benets and coverage under the applicable plan. The SBC is a
uniform template that uses clear, plain language to summarize key features
of the plan, such as covered benets, cost-sharing provisions and coverage
limitations. Plans and issuers must provide the SBC to participants and
beneciaries at certain times (including with wrien application materials, at
renewal, upon special enrollment and upon request). This provision became
applicable, generally, for plan years beginning on or after September 23, 2012,
and applies to all group health plans regardless of grandfathered status.
Can employers or plans require participants and beneciaries to be
in a waiting period before allowing them to enroll in a group health
plan?
Any waiting period that exceeds 90 days is prohibited. A waiting period is
dened as the period of time that must pass before coverage for an employee or
dependent who is otherwise eligible to enroll under the terms of the plan can
become effective. Eligibility conditions that are based solely on the lapse of a
time period are permissible for no more than 90 days. This provision became
applicable for plan years beginning on or after January 1, 2014, and applies to all
group health plans regardless of grandfather status.
14

What is the Marketplace and where can I learn more about it?
The Marketplace offers “one-stop shopping” for employees to nd and compare
private health insurance options that meet certain Federal requirements. It
simplies the search for individual health insurance by gathering all of the health
plan options into one Website and presenting the price and benet information
in simple terms. By purchasing insurance in the Marketplace, some employees
may be eligible for a tax credit that lowers monthly premiums or out-of-pocket
expenses. Persons eligible for COBRA due to a loss of employer-sponsored
coverage may choose to purchase less expensive coverage from the Marketplace
and may also qualify for the tax credits. Employees can also apply for Federal
health coverage programs such as Medicaid and the Children’s Health Insurance
Program through the Marketplace. For more information on the Marketplace,
visit HealthCare.gov.
Where can I get more information about the Affordable Care Act?
For more detailed information regarding the requirements under the Affordable
Care Act, visit the Employee Benets Security Administration’s Affordable Care
Act Web page at dol.gov/ebsa/healthreform or contact 1-866-444-3272.
15

The Health Insurance Portability and Accountability Act of 1996 (HIPAA)
includes provisions of Federal law governing health coverage portability, health
information privacy, administrative simplication, medical savings accounts, and long-
term care insurance. The responsibility of the Department of Labor and the subject of this
segment of the booklet are the law’s portability and nondiscrimination requirements.
HIPAA’s provisions affect group health plan coverage in the following ways:
Provide certain individuals special enrollment rights in group health coverage
when specic events occur, e.g., birth of a child (regardless of any open season);
Prohibit discrimination in group health plan eligibility, benets, and premiums
based on specic health factors; and
While HIPAA previously provided for limits with respect to preexisting
condition exclusions, new protections under the Affordable Care Act now prohibit
preexisting condition exclusions for plan years beginning on or after January 1,
2014.
2 1
2
For plan years beginning on or after January 1, 2014, plans are no longer required to issue the
general notice of preexisting condition exclusion and individual notice of period of preexisting con-
dition exclusion. Plans are also no longer required to issue certicates of creditable coverage after
December 31, 2014. These amendments were made because plans are prohibited from imposing
preexisting condition exclusions for plan years beginning on or after January 1, 2014.
HIPAA
17

Group health plans are required to provide special enrollment periods during
which individuals who previously declined health coverage for themselves and their
dependents may be allowed to enroll (regardless of any open enrollment period). In
addition to HIPAA special enrollment rights, the Children’s Health Insurance Program
Reauthorization Act (CHIPRA) added additional special enrollment rights under ERISA.
Rights related to CHIPRA special enrollment are discussed in this section.
Special enrollment rights can occur when:
An individual loses eligibility for coverage under a group health plan or other
health insurance coverage (such as an employee and his/her dependents’ loss of
coverage under the spouse’s plan) or when an employer terminates contributions
toward health coverage;
An individual becomes a new dependent through marriage, birth, adoption, or
being placed for adoption; and
An individual loses coverage under a State Children’s Health Insurance Program
(CHIP) or Medicaid, or becomes eligible to receive premium assistance under
those programs for group health plan coverage.
Employees must receive a description of special enrollment rights on or before the
date they are rst offered the opportunity to enroll in the group health plan (see model
notice on page 138).
In addition, employers that maintain a group health plan in a state with a CHIP or
Medicaid program that provides for premium assistance for group health plan coverage
must provide a notice (referred to as the Employer CHIP Notice) to all employees to
inform them of possible opportunities in the state in which they reside (for information on
a model Employer CHIP notice, see page 20).
Some individuals losing coverage under an employment-based group health plan
may want to consider enrolling for coverage in the Marketplace. For more information on
the Marketplace, visit HealthCare.gov.
Special Enrollment
19

20
Can the special enrollment notice be provided in the Summary Plan
Description (SPD)?
Yes, if the SPD is provided to the employee at or before the time the employee is
initially offered the opportunity to enroll in the plan. If the SPD is provided at a later
time, the special enrollment notice should be provided separately (for example, as
part of the application for coverage).
How can the employer notice regarding premium assistance under
Medicaid or CHIP (the Employer CHIP Notice) be provided?
Employers that maintain a group health plan are required to provide the Employer
CHIP Notice if they provide medical care in a State that operates a Medicaid or
CHIP premium assistance program. This notice may be provided with the SPD,
enrollment packets or open season materials as long as these materials are provided
no later than the date explained below, are provided to all employees, and are
provided in accordance with the Department of Labor’s disclosure rules. The notice
must be provided annually.
A model Employer CHIP Notice is available at dol.gov/ebsa/chipmodelnotice.doc.
The model notice includes State contact information for States that provide Medicaid
or CHIP premium assistance programs. This contact information will be updated
periodically, therefore, be sure to check the EBSA Website for the most recent
version.
Upon loss of eligibility for health coverage or termination of employer
contributions for health coverage, what are a plan’s obligations to offer
special enrollment?
When an employee or dependent loses eligibility for coverage under any group
health plan or health insurance coverage, or if employer contributions toward group
health plan coverage cease, a special enrollment opportunity may be triggered.
The employee or dependent must have had health coverage when the group health
plan benet package was previously declined. If the other coverage was COBRA
continuation coverage, special enrollment need not be made available until the
COBRA coverage is exhausted.
For example, if an employee’s spouse declined coverage when previously offered
due to coverage under her own employer’s plan, she and the employee must be
offered a special enrollment opportunity when her coverage ceases under that plan
or her employer terminates contributions to that plan.
Another example is if an employer offering two benet package options, an
HMO and an indemnity option, eliminates coverage under the indemnity option.
Employees, spouses, and other dependents must be offered a special enrollment
opportunity in the HMO option (and may also be eligible to special enroll in any
other plan for which they are otherwise eligible, such as any plan offered by the
spouse’s employer).
What are examples of a loss of eligibility for coverage?
Some examples of events that cause an individual to lose eligibility for health
coverage (there are other reasons as well):
Divorce or legal separation;
A dependent is no longer considered a dependent under the plan;
Death of the employee covered by the plan;
Termination of employment;
Reduction in the number of hours of employment;
The plan decides to no longer offer any benets to a class of similarly
situated individuals; or
An individual in an HMO or other arrangement no longer resides, lives,
or works in the service area.
If an employer terminates all contributions to a group health plan,
but individuals have the option to continue coverage and pay 100
percent of the cost themselves, would these individuals still have
a special enrollment right because the employer has terminated
contributions?
Yes. If all employer contributions have ended, individuals covered under the
plan would have a special enrollment right, regardless of their option to continue
coverage under the plan by paying the full cost of coverage.
If a plan has to offer a special enrollment period upon loss of
eligibility or termination of employer contributions, how long must
the special enrollment period run?
The plan has to provide at least 30 days for the employee or dependent to
request coverage after the loss of other coverage or termination of employer
contributions.
If an individual does request coverage within the 30-day period, the plan must
make the coverage effective no later than the rst day of the rst calendar month
beginning after the date the plan receives the enrollment request.
21
22
Upon marriage, birth, adoption, or placement for adoption, what are a
plan’s obligations to offer special enrollment?
Employees, as well as their spouses and dependents, may have special
enrollment rights after a marriage, birth, adoption, or placement for adoption.
In addition, new spouses and new dependents of retirees in a group health plan
also may have special enrollment rights after these events.
The plan has to provide at least 30 days for the employee or dependents to
request coverage after the occurrence of one of these events.
If the event was a marriage, the coverage is required to be effective no later than
the rst day of the rst calendar month beginning after the date the completed
request for enrollment is received by the plan.
In the case of birth, adoption, or placement for adoption, coverage is required to
be effective no later than the date of the event.
If an employee or dependent loses coverage under CHIP or Medicaid,
or becomes eligible for State premium assistance under those
programs, what are a plan’s obligations to offer special enrollment?
A special enrollment opportunity is triggered if the employee or dependent who
is otherwise eligible, but not enrolled in, a group health plan:
loses eligibility for coverage under a State Medicaid or CHIP program, or
becomes eligible for State premium assistance under a Medicaid or CHIP
program.
The plan must provide at least 60 days for the employee or dependent to request
coverage after the employee or dependent loses eligibility for coverage or
becomes eligible for premium assistance.
Can States modify HIPAA’s special enrollment requirement?
Yes, in certain circumstances. States may require additional special enrollment
periods with respect to insured group health plans.
State laws related to health insurance issuers generally continue to apply except
to the extent that such State law “prevents the application of” a requirement
of Part 7 of ERISA. Therefore, if health coverage is offered through an HMO
or an insurance policy, check with your State insurance department for more
information on that State’s insurance laws.
Under HIPAA, individuals may not be denied eligibility or continued eligibility to
enroll in a group health plan based on any health factors they may have. In addition, an
individual may not be charged more for coverage than any similarly situated individual
is being charged based on any health factor.
Note: Compliance with HIPAA’s nondiscrimination provisions does not in any
way reect compliance with any other provision of ERISA (including COBRA and
ERISA’s duciary provisions). Nor does it reect compliance with other State or Federal
laws (such as the Americans with Disabilities Act).
What are the “health factors”?
They are:
health status;
medical condition, including both physical and mental illnesses;
claims experience;
receipt of health care;
medical history;
genetic information;
evidence of insurability; and
disability.
The term “evidence of insurability” includes conditions arising from acts of
domestic violence, as well as participation in activities such as motorcycling,
snowmobiling, all-terrain vehicle riding, horseback riding, skiing, and other
similar activities.
Can a group health plan require an individual to pass a physical
examination in order to be eligible to enroll in the plan?
No. A group health plan may not require an individual to pass a physical exam
for enrollment, even if the individual is a late enrollee.
Can a plan require an individual to complete a health care
questionnaire in order to enroll?
Yes, provided that the questionnaire does not ask for genetic information
(including family medical history) and the health information is not used
to deny, restrict, or delay eligibility or benets, or to determine individual
premiums.
Nondiscrimination Requirements
23
24
Can plans exclude or limit benets for certain conditions or
treatments?
Group health plans may exclude coverage for a specic disease, limit or exclude
benets for certain types of treatments or drugs, or limit or exclude benets
based on a determination that the benets are experimental or medically
unnecessary – but only if the benet restriction applies uniformly to all similarly
situated individuals and is not directed at individual participants or beneciaries
based on a health factor they may have. (Plan amendments that apply to all
individuals in a group of similarly situated individuals and that are effective no
earlier than the rst day of the next plan year after the amendment is adopted
are not considered to be directed at individual participants and beneciaries.)
Whether any plan provision or practice with respect to benets complies with
this rule under HIPAA does not affect whether the provision or practice is
permied under other laws including the Affordable Care Act. For example,
the Affordable Care Act includes requirements related to coverage of certain
preventive services.
Can a plan deny benets otherwise provided for the treatment of an
injury based on the source of that injury?
If the injury results from a medical condition or an act of domestic violence,
a plan may not deny benets for the injury – if it is an injury the plan would
otherwise cover.
For example, a plan may not exclude coverage for self-inicted injuries (or
injuries resulted from aempted suicide) if the individual’s injuries are otherwise
covered by the plan and if the injuries are the result of a medical condition (such
as depression).
However, a plan may exclude coverage for injuries that do not result from a
medical condition or domestic violence, such as injuries sustained in high-risk
activities (for example, bungee jumping). But the plan could not exclude an
individual from enrollment for coverage because the individual participated in
bungee jumping.
Can a plan charge individuals with histories of high claims more than
similarly situated individuals based on their claims experience?
No. Group health plans cannot charge an individual more for coverage than
other similarly situated individuals based on any health factor.
How are groups of similarly situated individuals determined?
Distinctions among groups of similarly situated participants in a health plan
must be based on bona-de employment-based classications consistent with the
25
employer’s usual business practice. Distinctions cannot be based on any of the
health factors noted earlier.
For example, part-time and full-time employees, employees working in different
geographic locations, and employees with different dates of hire or lengths
of service can be treated as distinct groups of similarly situated individuals,
with different eligibility provisions, different benet restrictions, or different
costs, provided the distinction is consistent with the employer’s usual business
practice.
In addition, a plan generally may treat participants and beneciaries as two
separate groups of similarly situated individuals. The plan also may distinguish
between beneciaries based on, for example, their relationship to the plan
participant (such as spouse or dependent child) or based on the age or student
status of dependent children.
In any case, a plan cannot create or modify a classication directed at individual
participants or beneciaries based on one or more of the health factors.
Is it permissible for a health insurance issuer to charge a higher
premium to one group health plan (or employer) that covers
individuals, some of whom have adverse health factors, than it
charges another group health plan comprised of fewer individuals
with adverse health factors?
Yes. In fact, HIPAA does not restrict a health insurance issuer from charging a
higher rate to one group health plan (or employer) over another. An issuer
may take health factors of individuals into account when establishing blended,
aggregate rates for group health plans (or employers). This may result in one
health plan (or employer) being charged a higher premium than another for the
same coverage through the same issuer. Whether any plan provision or practice
with respect to benets complies with this rule under HIPAA does not affect
whether the provision or practice is permied under the Affordable Care Act
(including the requirements related to community rating administered by HHS).
Can a health insurance issuer charge an employer different
premiums for each individual within a group of similarly situated
individuals based on each individual’s health status?
No. Issuers may not charge or quote an employer or group health plan separate
rates that vary for individuals (commonly referred to as “list billing”) based on
any of the health factors.
HIPAA does not prevent issuers from taking the current health status of
each individual into account when establishing a blended, aggregate rate for
26
providing coverage to the employment-based group overall. (However, the
Affordable Care Act generally prohibits this practice with respect to small
group insurance plans.) (Note: group health plans cannot adjust premium or
contribution rates based on genetic information of one or more individuals in
the group. For more information, refer to the section on GINA on page 33). Also,
under the Affordable Care Act, the issuer may then charge the employer (or plan)
a higher overall rate, or a higher blended per-participant rate.
While HIPAA prohibits list billing based on health factors, it does not restrict
communications between issuers and employers (or plans) regarding the factors
considered in the rate calculations.
Can a group health plan impose a nonconnement clause (e.g., a
clause stating that if an individual is conned to a hospital at the
time coverage would otherwise take effect, coverage would not begin
until that individual is no longer conned)?
No. A group health plan may not deny or delay an individual’s eligibility,
benets, or the effective date of coverage because that individual is conned to
a hospital or other health care facility. In addition, a health plan may not set an
individual’s premium rate based on that individual’s connement.
Can a group health plan impose an “actively-at-work” provision (e.g.,
a requirement that an employee be actively at work after a waiting
period for enrollment in order to have health coverage become
effective on that day)?
No. Generally a group health plan may not refuse to provide benets because
an individual is not actively at work on the day that individual would otherwise
become eligible for benets. However, plans may have actively-at-work clauses
if the plan treats individuals who are absent from work due to a health factor
(for example, individuals taking sick leave) as if they are actively at work for
purposes of health coverage.
Plans may require individuals to report for the rst day of work before coverage
may become effective. In addition, plans may distinguish among groups of
similarly situated individuals in their eligibility provisions. For example, a plan
may require an individual to work full time, such as 250 hours per quarter or 30
hours per week, to be eligible for health plan coverage.
Is it permissible for a group health plan that generally provides
coverage for dependents only until age 26 to continue health
coverage past that age for disabled dependents?
Yes, a plan can treat an individual with an adverse health factor more favorably
by offering extended coverage.
27
HIPAA and the Aordable
Care Act Wellness Program
Requirements
The U.S. Departments of Labor, Health and Human Services and the Treasury is-
sued nal regulations on incentives for nondiscriminatory wellness programs in group
health plans under the Affordable Care Act and the HIPAA nondiscrimination provi-
sions. These rules apply to both grandfathered and nongrandfathered group health plans.
Are wellness programs provided in connection with a group health
plan allowed under the Affordable Care Act and HIPAA?
The Affordable Care Act and HIPAA generally prohibit group health plans from
charging similarly situated individuals different premiums or contributions or
imposing different deductibles, copayment or other cost sharing requirements
based on a health factor. However, there is an exception that allows plans to offer
wellness programs.
There are two types of wellness programs provided in connection with a
group health plan. Participatory wellness programs are generally available
without regard to an individual’s health status. Either no reward is offered,
or none of the conditions for obtaining a reward are based on an individual
satisfying a standard related to a health factor. These programs comply with the
nondiscrimination requirements so long as the program is made available to all
similarly situated individuals. For example:
A program that reimburses employees for all or part of the cost for
memberships in a tness center.
A diagnostic testing program that provides a reward for participation and
does not base any part of the reward on outcomes.
A program that reimburses employees for the costs of participating, or
that otherwise provides a reward for participating, in a smoking cessation
program without regard to whether the employee quits smoking.
A program that provides a reward to employees for aending a monthly,
no-cost health education seminar.
28
Health-contingent wellness programs require participants to satisfy a standard
related to a health factor in order to obtain a reward. There are two types of
health-contingent wellness programs: activity-only and outcome-based. Activity-
only programs require an individual to perform or complete an activity related
to a health factor in order to obtain a reward. Examples include a walking, diet
or exercise program. Outcome-based programs require an individual to aain
or maintain a specic health outcome (such as not smoking or aaining certain
results on biometric screenings) in order to obtain a reward. To comply with the
nondiscrimination rules, health-contingent wellness programs must meet ve
requirements described in the nal rules.
What are the ve requirements for health-contingent wellness
programs under the nal regulations?
1) The program must give individuals eligible to participate the opportunity
to qualify for the reward at least once per year.
2) The total reward for all the plan’s wellness programs that require
satisfaction of a standard related to a health factor is limited – generally,
it must not exceed 30 percent (or 50 percent for programs designed to
prevent or reduce tobacco use) of the cost of employee-only coverage
under the plan. If dependents (such as spouses and/or dependent
children) may participate in the wellness program, the reward must not
exceed 30 percent (or 50 percent) of the cost of the coverage in which an
employee and any dependents are enrolled.
3) The program must be reasonably designed to promote health and prevent
disease. (Note: different requirements apply for activity-only and
outcome-based programs, as described later in this section.)
4) The full reward must be available to all similarly situated individuals.
This means the program must allow a reasonable alternative standard
(or waiver of the otherwise applicable standard). (Note: different
requirements apply for activity-only and outcome-based programs, as
described later in this section.)
5) The plan must disclose in all materials describing the terms of the
program the availability of a reasonable alternative standard (or the
possibility of a waiver of the otherwise applicable standard). (Note:
different requirements apply for activity-only and outcome-based
programs, as described later in this section.) Model language is available
(see page 139).
29
What factors may be considered in determining whether a program is
reasonably designed to promote health and prevent disease?
An activity-only or outcome-based program is considered reasonably designed
to promote health or prevent disease, if the program has a reasonable chance
of improving the health of, or preventing disease in, participating individuals;
is not overly burdensome; is not a subterfuge for discrimination based on a
health factor; and is not highly suspect in the method chosen to promote health
or prevent disease. The determination is based on all the relevant facts and
circumstances.
To ensure that an outcome-based wellness program is reasonably designed to
improve health and does not act as a subterfuge for underwriting or reducing
benets based on a health factor, a reasonable alternative standard to qualify for
the reward must be provided to any individual who does not meet the initial
standard based on a test or screening that is related to a health factor.
Under what circumstances must a reasonable alternative standard
be offered?
For activity-only programs, a reasonable alternative standard (or waiver of the
otherwise applicable standard) must be offered to any individual for whom
it is unreasonably difficult due to a medical condition to satisfy the otherwise
applicable standard, or for whom it is medically inadvisable to aempt to
satisfy the otherwise applicable standard. Plans can seek physician verication
with respect to a request for a reasonable alternative standard, if the request is
reasonable under the circumstances.
For outcome-based programs, the reasonable alternative standard (or waiver of
the otherwise applicable standard) must be offered to any individual who does
not meet the initial standard based on the measurement, test or screening. If
the reasonable alternative standard is, itself, another outcome-based wellness
standard, the reasonable alternative cannot be a requirement to meet a different
level of the same standard without additional time to comply that takes into
account the individual’s circumstances and an individual must be given the
opportunity to comply with the recommendations of their personal physician as
a second reasonable alternative standard (if the physician joins in the request).
It is not reasonable for plans to seek physician verication that a health factor
makes it unreasonably difficult for the individual to satisfy, or medically
inadvisable for the individual to aempt to satisfy a standard under an outcome-
based wellness program.
30
For all health-contingent wellness programs (whether activity-only or
outcome-based), all of the facts and circumstances are taken into account when
determining whether a plan has provided a reasonable alternative standard,
including but not limited to the following:
If the reasonable alternative standard is completion of an educational
program, the plan or issuer must make the educational program available
or assist the employee in nding such a program (instead of requiring an
individual to nd such a program unassisted), and may not require an
individual to pay for the cost of the program.
The time commitment required must be reasonable (for example,
requiring aendance nightly at a one hour class would be unreasonable).
If the reasonable alternative standard is a diet program, the plan or issuer
is not required to pay for the cost of food but must pay any membership
or participation fee.
If an individual’s personal physician states that a program standard
(including, if applicable, the recommendations of the plan’s medical
professional) is not medically appropriate for that individual, the plan or
issuer must provide a reasonable alternative standard that accommodates
the recommendations of the individual’s personal physician with regard
to medical appropriateness. Plans and issuers may impose standard
cost sharing under the plan or coverage for medical items and services
furnished pursuant to the physician’s recommendations.
What disclosure is required for the availability of a reasonable
alternative standard?
Plans and issuers must disclose the availability of a reasonable alternative
standard to qualify for the reward (and, if applicable, the possibility of waiver
of the otherwise applicable standard) in all plan materials describing the terms
of a health-contingent wellness program (both activity-only and outcome-
based wellness programs). This disclosure must include contact information
for obtaining the alternative and a statement that recommendations of an
individual’s personal physician will be accommodated. If plan materials merely
mention that such a program is available, without describing its terms, this
disclosure is not required.
In addition, for outcome based-wellness programs, this notice must also be
included in any disclosure that an individual did not satisfy an initial outcome-
based standard, for example a notice that an individual did not meet the BMI
target range to qualify for the reward.
31
How do the wellness program rules apply to a group health plan that
offers a reward to individuals who participate in voluntary testing for
early detection of health problems? The plan does not use the test
results to determine whether an individual receives a reward or the
amount of an individual’s reward.
Such a program is considered a participatory wellness program since it does
not base any reward on the outcome of the testing. Thus, it is allowed under the
HIPAA nondiscrimination provisions as long as the program is made available to
all similarly situated individuals, without being subject to the ve requirements
that apply to health-contingent wellness programs.
Can a plan provide a premium differential between smokers and
nonsmokers?
The plan is offering a reward based on an individual’s ability to stop smoking.
This is considered an outcome-based wellness program. For the plan to
implement this type of program, the plan’s nonsmoking program would need to
meet the ve requirements for wellness programs that require satisfaction of a
standard related to a health factor.
Accordingly, this wellness program is permied if:
The premium differential is not more than 50 percent of the total cost
of employee-only coverage (or 50 percent of the cost of coverage if
dependents can participate in the program);
The program is reasonably designed to promote health and prevent
disease;
Individuals eligible for the program are given an opportunity to qualify
for the discount at least once per year;
The program provides a reasonable alternative standard, without
physician verication that the individual met the standard, to all
individuals who do not meet the otherwise applicable standard (those
who use tobacco products). For example, the reasonable alternative
standard could include discounts in return for aending educational
classes or for trying a nicotine patch; and
Plan materials describing the terms of the premium differential (and
any disclosure that an individual did not satisfy the wellness program
standard) describe the availability of a reasonable alternative standard to
qualify for the lower premium.
Title I of the Genetic Information Nondiscrimination Act of 2008 (GINA) includes
provisions that generally prohibit group health plans and health insurance issuers from
discriminating based on genetic information. These provisions amend the Employee
Retirement Income Security Act (ERISA), administered by the Department of Labor
(DOL); the Public Health Service Act (PHSA Act), administered by the Department
of Health and Human Services (HHS); and the Internal Revenue Code (the Code),
administered by the Department of the Treasury (the Treasury) and the Internal Revenue
Service (IRS). DOL has jurisdiction with respect to employment-based group health
plans. HHS, in conjunction with the States, administers these provisions with respect to
health insurance issuers. The Treasury and IRS administer these provisions with respect
to employers. Title I of GINA also includes individual insurance market provisions under
the PHSA and privacy and condentiality provisions under the Social Security Act,
which are both within the jurisdiction of HHS. Title II of GINA, under the jurisdiction
of the Equal Employment Opportunity Commission, addresses discrimination in
employment based on genetic information.
The subject of these Frequently Asked Questions is the requirements of Title I of
GINA under ERISA, prohibiting discrimination in group health plan coverage based on
genetic information.
GINA expands the genetic information nondiscrimination protections included
in Title I of the Health Insurance Portability and Accountability Act of 1996 (HIPAA).
Under GINA, group health plans cannot base premiums for a plan or a group of similarly
situated individuals on genetic information. GINA generally prohibits plans from
requesting or requiring an individual to undergo genetic tests, and prohibits a plan from
collecting genetic information (including family medical history) prior to or in connection
with enrollment, or for underwriting purposes.
GINA applies generally to group health plans. Unlike the provisions under Title I of
HIPAA, there is no exception for very small health plans with less than two participants
who are current employees.
The Genetic Information
Nondiscrimination Act
33
How does GINA expand the genetic information nondiscrimination
protections in HIPAA?
Before the Affordable Care Act, HIPAA prevented a plan or issuer from imposing
a preexisting condition exclusion based solely on genetic information. Under the
Affordable Care Act, plans are prohibited from excluding coverage or benets
due to any preexisting condition. HIPAA continues to prohibit discrimination in
individual eligibility, benets, or premiums based on any health factor (including
genetic information). GINA provides additional underwriting protections,
prohibits requesting or requiring genetic testing, and restricts the collection of
genetic information. Specically:
GINA provides that group health plans cannot adjust premiums or
contribution amounts for a plan, or any group of similarly situated
individuals under the plan, based on genetic information of one or more
individuals in the group. (However, premiums may be increased for
the group based upon the manifestation of a disease or disorder of an
individual enrolled in the plan.)
GINA generally prohibits plans from requesting or requiring an
individual to undergo a genetic test. However, a health care professional
providing health care services to an individual is permied to request a
genetic test. A plan or issuer may request the results of a genetic test to
determine payment of a claim for benets, but only the minimum amount
of information necessary in order to determine payment. There is also a
research exception that permits a plan or issuer under certain conditions
to request (but not require) that a participant or beneciary undergo a
genetic test.
GINA prohibits plans from collecting genetic information (including
family medical history) from an individual prior to or in connection with
their enrollment in the plan, or at any time for underwriting purposes.
Under GINA, underwriting purposes includes rules for determination of
eligibility for benets and the computation of premium and contribution
amounts. Thus, under GINA, plans are generally prohibited from
offering rewards in return for the provision of genetic information,
including family medical history information collected as part of a Health
Risk Assessment (HRA). GINA includes an exception for incidental
collection of genetic information, provided the information is not used
for underwriting purposes. However, the regulations make clear that the
incidental collection exception is not available if it is reasonable for the
plan or issuer to anticipate that health information will be received in
response to a collection, unless the collection explicitly states that genetic
information should not be provided.
34
What is genetic information?
Genetic information means information about an individual’s genetic tests, the
genetic tests of family members of the individual, the manifestation of a disease
or disorder in family members of the individual or any request for or receipt
of genetic services, or participation in clinical research that includes genetic
services by the individual or a family member of the individual. The term genetic
information includes, with respect to a pregnant woman (or a family member of
a pregnant woman) genetic information about the fetus and with respect to an
individual using assisted reproductive technology, genetic information about the
embryo.
Genetic information does not include information about the sex or age of any
individual.
Genetic information includes information about an individual’s
genetic services and tests. What do these include?
Genetic services mean genetic tests, genetic counseling, or genetic education.
Genetic test means an analysis of human DNA, RNA, chromosomes, proteins,
or metabolites, if the analysis detects genotypes, mutations, or chromosomal
changes. A genetic test does not include an analysis of proteins or metabolites
directly related to a manifested disease, disorder, or pathological condition.
Therefore, some examples of genetic tests are tests to determine whether an
individual has a BRCA1, BRCA2, or colorectal cancer genetic variant. In contrast,
an HIV test, complete blood count, cholesterol test, liver function test, or test for
the presence of alcohol or drugs is not a genetic test.
Genetic information includes an individual’s genetic tests and
information about the manifestation of a disease or disorder in
an individual’s family member. A genetic test does not include
an analysis of proteins or metabolites that is directly related to a
manifested disease, disorder, or pathological condition. What is a
manifested disease?
A manifested disease is a disease, disorder, or pathological condition for which
an individual has been or could reasonably be diagnosed by a health care
professional (with appropriate training and expertise in the eld of medicine
involved).
A disease is not manifested if a diagnosis is based principally on genetic
information. For example, an individual whose genetic tests indicate a genetic
variant associated with colorectal cancer and another that indicates an increased
35
risk of developing cancer, but who has no signs or symptoms of disease and
has not and could not reasonably be diagnosed with a disease does not have a
manifested disease.
While plans are prohibited from adjusting group premiums or contributions
based on genetic information, plans can increase the premium or contribution
based on the manifested disease or disorder of an individual enrolled in the plan.
This is because information about an individual’s manifested disease or disorder
is not genetic information with respect to that individual. This is discussed
further below.
GINA prohibits a plan from collecting genetic information (including
family medical history) prior to or in connection with enrollment, or
at any time for underwriting purposes. What does “collect” include?
Collect means to request, require, or purchase genetic information.
Can a group health plan adjust the premium that an employer or
group of similarly situated individuals must pay under the plan based
on genetic information of an individual or individuals covered under
the group?
No. GINA prohibits a group health plan from adjusting group premium or
contribution amounts for a group of similarly situated individuals based on the
genetic information of members of the group. This is a change from HIPAA’s
prior nondiscrimination requirements, which allowed plans to adjust premiums
or contributions for the group health plan or group of similarly situated
individuals (but not for specic individuals within the group) based on genetic
information, as well as other health factors. Therefore, even if a plan obtained
individual genetic information about group members before GINA’s effective
date, it cannot be used to adjust the group premium.
Under GINA and HIPAA, a plan can charge a higher overall, blended per-
participant amount based on the manifestation of a disease or a disorder of an
individual enrolled in the plan. However, a plan cannot use the manifestation of
a disease or disorder in one individual as genetic information about other group
members to further increase the group premium.
A plan can take into account the costs associated with providing benets for
covered genetic tests or genetic services in determining overall premium or
contribution amounts. Note, under HIPAA, a plan cannot charge an individual
more for coverage than other similarly situated individuals in the group based
on any health factor, including a manifested disease or disorder.
For further discussion of what “manifested disease” means, see above.
36
Can an individual’s doctor or other health care provider request that
the individual undergo a genetic test?
Generally, yes. GINA prohibits a group health plan from requesting or requiring
an individual or a family member of an individual to undergo genetic tests.
Nonetheless, under GINA, a health care professional who is providing health
care services to an individual can request that an individual undergo a genetic
test. A health care professional includes but is not limited to a physician, nurse,
physician’s assistant, or technicians that provide health care services to patients.
For example, if during the course of a routine physical exam, a physician
learns that an individual has family medical history indicating a potential risk
for Huntington’s disease, the physician can recommend that the individual
undergo a related genetic test. This would not violate GINA. This would be
true even if the doctor were employed by an HMO, so long as the physician was
providing health care services to the individual for whom the genetic test was
recommended.
Can a health plan obtain the results of a genetic test to make a
determination regarding payment of a claim for benets under the
plan?
Generally, yes. If a plan conditions payment for an item or service based on
medical appropriateness and the medical appropriateness depends on the
genetic makeup of the patient, then the plan is permied to condition payment
for the item or service on the outcome of a genetic test. The plan may also refuse
payment in that situation if the patient does not undergo the genetic test. The
plan may request only the minimum amount of information necessary to make a
determination regarding payment.
If a plan normally covers mammograms for participants and
beneciaries starting at age 40, but covers them at age 30 for
individuals with a high risk of breast cancer, may the plan require
that an individual under 40 submit genetic test results or family
medical history as evidence of high risk of breast cancer, in order to
have a claim for a mammogram paid?
Generally, yes. Under GINA, a plan may request and use the results of a genetic
test to make a determination regarding payment, as long as the plan requests
only the minimum amount of information necessary.
Plans may also request genetic information for the purpose of determining the
medical appropriateness of a treatment or service. Because the medical
appropriateness of the mammogram depends on the patient’s genetic makeup,
the minimum amount of information necessary for determining payment of the
claim may include the results of a genetic test or the individual’s family medical
history.
37

Can a plan request that a participant or beneciary undergo a genetic
test for research purposes?
Under GINA, a plan is permied to request, but not to require, that a participant
or beneciary undergo a genetic test for research purposes if the following four
requirements are met:
The plan makes the request pursuant to research. (Research is dened
in 45 CFR 46.102(d).) The research must comply with 45 CFR Part 46 or
equivalent Federal regulations and any applicable State or local law or
regulation for the protection of human subjects in research.
The plan must make the request for the genetic test in writing and clearly
indicate to each participant and beneciary that the request is voluntary
and will have no eect on eligibility.
No genetic information collected pursuant to this research exception can
be used for underwriting purposes.
The plan must complete a copy of the “Notice of Research Exception
under the Genetic Information Nondiscrimination Act” and provide the
notice to the address specied in the instructions. You can access this
notice at dol.gov/ebsa/GINAexceptioninstructions.html.
GINA prohibits a group health plan from collecting genetic
information for underwriting purposes. What does underwriting
purposes mean?
Under GINA, the denition of underwriting purposes is broader than
merely activities relating to rating and pricing a group policy. Under GINA,
underwriting purposes means, with respect to a group health plan:
Rules for or determination of eligibility (including enrollment and
continued eligibility) for benets under the plan or coverage (including
changes in deductibles or other cost-sharing mechanisms in return
for activities such as completing a health risk assessment (HRA) or
participating in a wellness program);
Computation of premium or contribution amounts under the plan
(including discounts, rebates, payments in kind, or other premium
differential mechanisms in return for activities such as completing an
HRA or participating in a wellness program);
The application of any preexisting condition exclusion under the plan;
and
38
Other activities related to the creation, renewal, or replacement of a
contract of health insurance or health benets.
Can a plan require an individual to complete a health risk assessment
(HRA) prior to or as part of the enrollment process for the plan?
GINA prohibits a plan from collecting genetic information (including family
medical history) prior to or in connection with enrollment. Thus, under GINA,
plans must ensure that any HRA conducted prior to or in connection with
enrollment does not collect genetic information, including family medical history.
Under GINA, there is an exception for genetic information that is obtained
incidental to the collection of other information, if 1) the genetic information that
is obtained is not used for underwriting purposes and 2) if it is reasonable to
anticipate that the collection will result in the plan receiving health information,
the plan explicitly noties the person providing the information that genetic
information should not be provided.
Therefore, a plan conducting an HRA prior to or in connection with enrollment,
should ensure that the HRA explicitly states that genetic information should not
be provided.
Can a plan require that an individual complete a health risk
assessment (HRA) that requests family medical history in order to
receive a wellness program reward, such as a nancial incentive, in
return for the completion of the HRA?
GINA prohibits a plan from collecting genetic information (including family
medical history):
prior to or in connection with enrollment; or
at any time for underwriting purposes.
Because completing the HRA results in a reward, the request is for underwriting
purposes and is prohibited.
A plan may use an HRA that requests family medical history, if it is requested
to be completed after and unrelated to enrollment and if there is no premium
reduction or any other reward for completing the HRA.
A plan may offer a premium discount or other reward for completion of an HRA
that does not request family medical history or other genetic information, such as
information about any genetic tests the individual has undergone.
39
The plan should ensure that the HRA explicitly states that genetic information
should not be provided. This is because GINA provides an exception for genetic
information that is obtained incidental to the collection of other information, if
1) the genetic information that is obtained is not used for underwriting purposes
and 2) if in connection with any collection it is reasonable to anticipate that
health information will be received, the collection explicitly states that genetic
information should not be provided.
Plans may use two separate HRAs; one that collects genetic information, such
as family medical history, which is conducted after and unrelated to enrollment
and is not tied to a reward, and another HRA that does not request genetic
information, which can be tied to a reward. In addition, under GINA group
health plans may also reward:
Participation in an annual physical examination with a physician (or
other health care professional) who is providing health care services to
the individual, even if the physician may ask for family medical history as
part of the examination;
More favorable cost-sharing for preventive services, including genetic
screening; and
Participation in certain disease management or prevention programs.
The incentives to participate in such programs must also be available to
individuals who qualify for the program but have not volunteered family
medical history information through an HRA.
40

Mental Health Parity
Provisions
The Mental Health Parity and Addiction Equity Act of 2008 (MHPAEA) was
signed into law on October 3, 2008 and became effective for plan years beginning after
October 3, 2009. MHPAEA greatly expands on an earlier law, the Mental Health
Parity Act of 1996 (MHPA). On November 8, 2013, the Departments of Health and
Human Services, Labor and the Treasury jointly issued nal regulations implementing
MHPAEA, which became applicable for plan years beginning on or after July 1, 2014.
MHPAEA generally applies to group health plans and health insurance issuers that
provide coverage for either mental health or substance use disorder benets and medical/
surgical benets. These FAQs provide basic information about the important protections
MHPAEA provides with respect to parity in coverage of mental health and substance
use disorder benets and medical/surgical benets provided by employment-based group
health plans.
Reviewing your group health plan for compliance with the mental health parity
requirements may be complicated depending on your plan’s design. If you have questions
about MHPAEA or the mental health or substance use disorder benets under your plan,
contact the Department of Labor at askebsa.dol.gov or 1-866-444-3272.
What additional protections does MHPAEA provide for participants
and beneciaries?
MHPA required parity with respect to aggregate lifetime and annual dollar
limits for mental health benets and medical/surgical benets. MHPAEA
expands those provisions to include substance use disorder benets. Thus, under
MHPAEA group health plans generally may not impose a lifetime or annual
dollar limit on mental health or substance use disorder benets that is lower than
the lifetime or annual dollar limit imposed on medical/surgical benets.
3
MHPAEA also requires group health plans to ensure that nancial requirements
(such as copays and deductibles), and quantitative treatment limitations (such
as visit limits), applicable to mental health or substance use disorder benets
are generally no more restrictive than the requirements or limitations applied to
3
However, note that the Affordable Care Act prohibits lifetime and annual limits on the dollar
amount of essential health benets. The denition of essential health benets includes ``mental
health and substance use disorder services, including behavioral health treatment.’’
41
medical/surgical benets. The MHPAEA regulations also require plans to ensure
parity with respect to nonquantitative treatment limitations (such as medical
management standards).
Can group health plans still apply nancial requirements and
treatment limitations, such as copays or visit limits on mental health
and substance use disorder benets?
Generally, yes. Group health plans may still apply nancial requirements and
treatment limitations with respect to mental health and substance use disorder
benets; however, they must do so in accordance with the requirements under
MHPAEA.
There is a test for determining whether a nancial requirement or treatment
limitation for mental health or substance use disorder benets is permissible.
The general rule is that a plan may not impose a nancial requirement or
quantitative treatment limitation applicable to mental health or substance
use disorder benets in any classication that is more restrictive than the
predominant nancial requirement or quantitative limitation of that type applied
to substantially all medical/surgical benets in the same classication. How to
apply this test is discussed in more detail in the following FAQs.
What is a nancial requirement or quantitative treatment limitation?
The most common types of nancial requirements include deductibles, copays,
coinsurance, and out-of-pocket maximums. Types of quantitative treatment
limitations include annual, episode, and lifetime day and visit limits, for
example, number of treatments, visits, or days of coverage. These are just
examples; therefore, you could nd a type of nancial requirement and
quantitative treatment limitations that is not specically listed here.
The test for determining parity refers to levels of types of nancial
requirements or treatment limitations. What is a level of a type of
nancial requirement or treatment limitation?
The level of a type of nancial requirement or treatment limitation refers to
the magnitude of the type of nancial requirement or treatment limitation.
For example, different levels of coinsurance include 20 percent and 30 percent,
different levels of copays include $15 and $20, or different levels of an episode
limit include 21 inpatient days per episode and 30 inpatient days per episode.
42

How can I determine if a nancial requirement or quantitative
treatment limitation applicable to mental health and substance use
disorder benets is permissible?
To determine if a quantitative nancial requirement (such as a copay) or
quantitative treatment limitation (such as a visit limit) is permissible, the parity
analysis must be applied for that type of nancial requirement or treatment
limitation within a coverage unit for each of the six classications of benets
separately. A coverage unit refers to the way in which a plan groups individuals
for purposes of determining benets, premiums or contributions (for example,
self-only, family, employee plus spouse). Under MHPAEA, the six classications
of benets
4
are:
1) Inpatient in-network;
2) Inpatient out-of-network;
3) Outpatient in-network;
4) Outpatient out-of-network;
5) Emergency care;
6) Prescription drugs.
If a type of nancial requirement or quantitative treatment limitation applies
to substantially all medical/surgical benets in a classication (for example, if
a copay applies to substantially all medical/surgical benets), then it may be
permissible for that requirement or limitation (the copay) to apply to mental
health or substance use disorder benets in the same classication. In some
circumstances plans can subdivide certain classications to account for multiple
network tiers, among other things. This is discussed later in this section.
Generally, a nancial requirement or treatment limitation is considered to apply
to substantially all medical/surgical benets if it applies to two-thirds or more of
the medical/surgical benets for the same classication and coverage unit. This
two-thirds calculation is based on the dollar amount of all plan payments for
medical/surgical benets expected to be paid for the year (or portion of the plan
year after a change in plan benets that affects the applicability of the nancial
requirement or quantitative treatment limitation).
The predominant level of a type of requirement or limitation applicable to
medical/surgical benets within a classication is the most restrictive level of
the requirement or limitation that can be imposed on mental health or substance
use disorder benets within that classication. There is a detailed test for
determining the predominant level which is discussed in the next FAQ. If, for
4
For more information regarding the outpatient in-network and outpatient out-of-network
classications, see the FAQ at: dol.gov/ebsa/faqs/faq-mhpaea.html.
43

example, for self-only coverage a $10 copay is the predominant level of copay
that applies to substantially all inpatient in-network medical/surgical benets,
that is the most restrictive copay level that can apply to inpatient in-network
mental health or substance use disorder benets. With respect to the prescription
drug classication, there is a special rule for multi-tiered prescription drug
benets.
5
If as determined under MHPAEA, it is permissible for my plan
to impose a copay on my inpatient, in-network mental health or
substance use disorder benets, is there any restriction on the
amount of copay that can apply?
Yes. The predominant level of a type of requirement or limitation applicable to
medical/surgical benets within a classication is the most restrictive level of the
requirement or limitation that can be imposed on mental health or substance use
disorder benets within that classication.
Generally, the predominant level will apply to more than one-half of the medical/
surgical benets in that classication subject to the requirement or limitation.
If there is no single level that applies to more than one-half of medical/surgical
benets in the classication, the plan can combine levels until the combination
of levels applies to more than one-half of medical/surgical benets subject to
the requirement or limitation in the classication.
6
The least restrictive level
within the combination is considered the predominant level. The determination
of the portion of medical/surgical benets in a classication subject to a nancial
requirement or treatment limitation is based on the dollar amount of all plan
payments for medical/surgical benets in the classication expected to be paid
under the plan for the plan year.
Can I use sub-classications within the six classications?
The nal regulations allow for a plan to create two sub-classications for
purposes of applying the nancial requirement and treatment limitation rule
under MHPAEA:
Plans can sub-divide the outpatient classication into office visits and all
other outpatient services.
Plans can sub-divide in-network classications for plans with multiple
network tiers if the tiering is based on reasonable factors and without
regard to whether a provider is a mental health or substance use disorder
provider or a medical/surgical provider.
5
See 29 CFR 2590.712(c)(3)(iii).
6
For this purpose the plan may combine the most restrictive levels rst, with each less restrictive
level added to the combination until the combination applies to more than one-half of the benets
subject to the nancial requirement or treatment limitation.
44
After the sub-classications are established, the plan or issuer may not impose
any nancial requirement or treatment limitation on mental health or substance
use disorder benets in any sub-classication (i.e., office visits or non-office
visits) that is more restrictive than the predominant nancial requirement or
treatment limitation that applies to substantially all medical/surgical benets in
the sub-classication.
Plans cannot use any other type of sub-classications, such as those based on the
classication of generalists or specialists.
Can my plan impose different levels of copays on different tiers of
prescription drug benets?
In addition to the permied sub-classications discussed above, the regulations
provide a special rule for multi-tiered prescription drug benets. A plan can
apply different levels of nancial requirements to different tiers of prescription
drug benets if two conditions are met. First, the tiering must be based
on reasonable factors determined in accordance with the rules relating to
requirements for nonquantitative treatment limitations. Reasonable factors
include cost, efficacy, generic versus brand name, and mail order versus
pharmacy pick-up. Second, the tiering and nancial requirements must be made
without regard to whether a drug is prescribed for a medical/surgical condition
or a mental health or substance use disorder condition.
Can my plan impose a higher “specialist” nancial requirement with
respect to mental health and substance use disorder benets?
As stated above, a plan may not create sub-classications for generalists and
specialists to determine separate predominant nancial requirements and
treatment limitations that apply to substantially all medical/surgical benets.
However, if the predominant level of a type of nancial requirement that
applies to substantially all medical/surgical benets in a classication is the one
charged for a medical/surgical specialist, then that level of that type of nancial
requirement can be applied for mental health or substance use disorder benets
within that classication. On the other hand, if the predominant level of a type of
nancial requirement that applies to substantially all medical/surgical benets in
a classication is the one charged for a medical/surgical generalist, then the level
of that nancial requirement charged for mental health or substance use disorder
benets within that classication cannot be higher than the level of that nancial
requirement for “generalist” medical/surgical benets.
45
If a plan previously had separate deductibles for medical/surgical
benets and mental health or substance use disorder benets, how
should those deductibles be combined now?
While plans can no longer have separate deductibles for mental health
or substance use disorder benets and for medical/surgical benets in a
classication, they do have exibility in how they choose to combine these
deductibles. For example, if a plan previously had a $500 deductible on medical/
surgical benets, and a $500 deductible on mental health or substance use
disorder benets, the plan could now choose to have a combined $750 deductible
for all benets. As long as there is no separate deductible that applies only to
mental health or substance use disorder benets, generally the plan can set the
combined deductible at whatever amount it chooses.
What are nonquantitative treatment limitations?
Nonquantitative treatment limitations include:
Medical management standards limiting or excluding benets based on
medical necessity or medical appropriateness, or based on whether the
treatment is experimental or investigative;
Formulary design for prescription drugs;
For plans with multiple network tiers (such as preferred providers and
participating providers), network tier design;
Standards for provider admission to participate in a network, including
reimbursement rates;
Plan methods for determining usual, customary, and reasonable charges;
Refusal to pay for higher-cost therapies until it can be shown that a
lower-cost therapy is not effective (also known as fail-rst policies or step
therapy protocols);
Exclusions based on failure to complete a course of treatment; and
Restrictions based on geographic location, facility type, provider
specialty, and other criteria that limit the scope or duration of benets for
services provided under the plan or coverage.
This is an illustrative, non-exhaustive list.
46

How does MHPAEA provide for parity with respect to nonquantitative
treatment limitations?
Under MHPAEA, a plan may not impose a nonquantitative treatment limitation
with respect to mental health or substance use disorder benets in any
classication (such as inpatient, out-of-network) unless under the terms of the
plan as wrien and in operation, any processes, strategies, evidentiary standards,
or other factors used in applying the limitation to mental health or substance
use disorder benets in the classication are comparable to and applied no more
stringently than the processes, strategies, evidentiary standards or other factors
used in applying the limitation with respect to medical/surgical benets in the
classication.
What information must be provided to participants and beneciaries
when a request for mental health benets is denied?
Under MHPAEA, the criteria for medical necessity determinations made under
a group health plan (or health insurance coverage offered in connection with
the plan) with respect to mental health or substance use disorder benets must
be made available by the plan administrator or the health insurance issuer
to any current or potential participant, beneciary, or contracting provider
upon request. In addition, under the internal appeals and external review
requirements added by the Affordable Care Act, non-grandfathered group
health plans must provide to an individual (or a provider or other individual
acting as a patient’s authorized representative), upon request and free of charge,
reasonable access to and copies of all documents, records, and other information
relevant to the individual’s claim for benets consistent with the Department
of Labor claims procedure regulation.
7
Documents with information on the
medical necessity criteria for both medical/surgical benets and mental health
or substance use disorder benets are plan documents, and copies must be
furnished within 30 days of your request under ERISA.
8
Are there plans that are exempt from MHPAEA?
Yes. MHPAEA applies to most employment-based group health coverage, but
there are a few exceptions. MHPAEA contains an exemption for a group health
plan of a small employer. However, under HHS nal rules, non-grandfathered
7
See dol.gov/ebsa/healthreform for consumer information on internal claims and appeals, external
review of health plan decisions, and grandfathered health plans under the Patient Protection and
Affordable Care Act.
8
See 29 CFR 2520.104b-1
47

health insurance coverage in the individual and small group markets generally
must provide all categories of essential health benets, including mental health
and substance use disorder benets, and such benets must be provided in
compliance with the requirements of the MHPAEA rules.
9
MHPAEA also contains an increased cost exemption available to plans that meet
the requirements for the exemption. The nal rules establish standards and
procedures for claiming the exemption under MHPAEA.
10
Additionally, plans
for State and local government employees that are self-insured may opt-out
of MHPAEA’s requirements if certain administrative steps are taken (such as
sending notice to enrollees).
11
Finally, MHPAEA does not apply to retiree-only
plans.
12
Where can I nd more information about the protections available
under MHPAEA?
Additional information and FAQs regarding MHPAEA are available on the
Department of Labor’s Mental Health Parity Web page at dol.gov/ebsa/
mentalhealthparity.
9
78 FR 12834
10
For more information on MHPAEA’s increased cost exemption, see Q7 of the FAQs available at
dol.gov/ebsa/faqs/faq-aca17.html.
11
If you are an employee of a State or local government that sponsors a self-insured plan and
would like to know if your employment-based plan has opted out, see the list of HIPAA opt-out
elections for self-funded, non-federal governmental plans, available at cms.gov/cciio/Resources/
Forms-Reports-and-Other-Resources/index.html#Self-Funded Non-Federal Governmental Plans.
12
See preamble to the nal rules implementing MHPAEA published on November 13, 2013.
48
The Newborns’ and Mothers’ Health Protection Act (the Newborns’ Act) provides
protections for mothers and their newborn children relating to the length of their hospital
stays following childbirth.
Group health plans that are subject to the Newborns’ Act may not restrict benets
for a hospital stay in connection with childbirth to less than 48 hours following a vaginal
delivery or 96 hours following a delivery by cesarean section. However, the aending
provider may decide, after consulting with the mother, to discharge the mother and/or her
newborn child earlier.
Many states have enacted their own version of the Newborns’ Act for insured
coverage. In these states, State law can govern in lieu of the Federal requirements.
What group health plans must comply with the Newborns’ Act?
If a plan offers benets for hospital stays in connection with childbirth, the
Newborns’ Act applies if the coverage is “self-insured” by an employment-based
plan.
If the coverage is provided by an insurance company or HMO (an “insured”
plan), and your State has a law regulating coverage for newborns and mothers
that meets specic criteria, then State law, rather than the Newborns’ Act,
applies. If this is the case, the State law may differ slightly from the Newborns’
Act requirements, so it is important to know which law applies to the coverage
offered by your plan.
For those plans with coverage that is insured by an insurance company or HMO,
contact your State insurance department for the most current information on the
State laws that pertain to hospital length of stay in connection with childbirth.
For those plans covered by the Federal law, the following questions apply:
When does the 48-hour (or 96-hour) period start?
If a woman delivers her baby in the hospital, the 48-hour period (or 96-hour
period) starts at the time of delivery. As an example: if a woman goes into labor
and is admied to the hospital at 10 p.m. on June 11, but gives birth by vaginal
delivery at 6 a.m. on June 12, the 48-hour period begins at 6 a.m. on June 12.
However, if the woman delivers outside the hospital and is later admied to
the hospital in connection with childbirth (as determined by the aending
The Newborns’ and Mothers’
Health Protection Act
49
50
provider), the period begins at the time of the hospital admission. For example, if a
woman gives birth at home by vaginal delivery, but begins bleeding excessively in
connection with childbirth and is admied to the hospital, the 48-hour period starts
at the time of admission.
Who is the attending provider?
An aending provider is an individual licensed under State law who is directly
responsible for providing maternity or pediatric care to a mother or newborn child.
A nurse midwife or a physician assistant may be an aending provider if licensed
in the State to provide maternity or pediatric care in connection with childbirth.
A health plan, hospital, insurance company, or HMO, however, would not be an
aending provider.
The aending provider cannot receive incentives or disincentives to discharge the
mother or her child earlier than 48 hours (or 96 hours).
May a group health plan require an individual to get permission
(sometimes called prior authorization or precertication based upon
medical necessity) for a 48-hour or 96-hour hospital stay?
A plan cannot deny a mother or her newborn child coverage for a 48-hour stay (or
96-hour stay) because the plan claims that the mother or her aending provider has
failed to show that the 48-hour stay (or 96-hour stay) is medically necessary.
However, plans generally can require an individual to notify the plan of the
pregnancy in advance of an admission in order to use certain providers or facilities
or to reduce the individual’s out-of-pocket costs.
Under the Newborns’ Act, may group health plans impose deductibles
or other cost-sharing provisions for hospital stays in connection with
childbirth?
Yes, but only if the deductible, coinsurance, or other cost-sharing for the laer part of
a 48-hour (or 96-hour) stay is not greater than that imposed for the earlier part of the
stay. For example, with respect to a 48-hour stay, a group health plan is permied
to cover only 80 percent of the cost of the hospital stay. However, a plan covering 80
percent of the cost of the rst 24 hours could not reduce coverage to 50 percent for
the second 24 hours.

51
Does the Newborns’ Act require a plan to offer maternity benets?
No. The Newborns’ Act does not require plans to provide coverage for hospital
stays in connection with childbirth. However, other legal requirements, including
Title VII of the Civil Rights Act of 1964, may require this type of coverage.
Questions regarding Title VII should be directed to the Equal Employment
Opportunity Commission. See the agency’s Website at eeoc.gov.
Are group health plans required to tell participants and beneciaries
about the Newborns’ Act and any applicable State law protections?
A group health plan that provides maternity or newborn infant coverage must
include in its SPD a statement describing the Federal or State law requirements
applicable to the plan (or any health insurance coverage offered under the plan)
relating to hospital length of stay in connection with childbirth for the mother or
newborn child. If the Federal Newborns’ Act law applies in some areas in which
the plan operates and State laws apply in others, the SPD must describe the
Federal and State law requirements that apply in each area covered by the plan.
Model language to describe the Federal law requirements is included on page
140.
The Women’s Health and Cancer Rights Act (WHCRA) provides protections for
individuals who elect breast reconstruction after a mastectomy. Under WHCRA, group
health plans offering mastectomy coverage must also provide coverage for certain services
relating to the mastectomy, in a manner determined in consultation with the aending
physician and the patient. Required coverage includes all stages of reconstruction of
the breast on which the mastectomy was performed, surgery and reconstruction of the
other breast to produce a symmetrical appearance, prostheses, and treatment of physical
complications of the mastectomy, including lymphedema.
Wrien notice about the availability of these mastectomy-related benets must
be delivered to participants in a group health plan upon enrollment and then each year
afterwards.
Does WHCRA apply to individuals who have not been diagnosed with
cancer but who must undergo a mastectomy due to other medical
reasons?
Despite the title, nothing in the law limits entitlement to WHCRA benets
to cancer patients. If an individual is receiving benets in connection with a
mastectomy and the group health plan covers mastectomies, then the individual is
entitled to WHCRA benets.
Also, despite the title, nothing in the law limits WHCRA entitlements to women.
Does WHCRA mandate minimum hospital lengths of stay in
connection with mastectomy or breast reconstruction?
No, but many State laws applicable to insured coverage provide more protections
than WHCRA. Thus, if a plan provides coverage through an insurance company,
covered individuals may be entitled to minimum hospital stays under State law.
If your plan is insured, check with your State insurance department for more
information.
The Women’s Health
and Cancer Rights Act
53

54
May group health plans impose deductibles or coinsurance
requirements on the coverage specied in WHCRA?
Yes, but only if the deductibles and coinsurance are consistent with those
established for other medical/surgical benets under the plan or coverage.
Can my plan refuse to cover reconstructive surgery benets because
the mastectomy was performed when the participant was covered
under a different insurance company?
If the plan provides coverage for mastectomies and the participant is receiving
benets under the plan that is related to a mastectomy, then the plan generally
is required to cover reconstructive surgery upon request. In addition, the plan
generally is required to cover the other benets specied in WHCRA. It does not
maer that the participant was not enrolled in the current plan and/or was not
covered by the same insurance company at the time of the mastectomy.
There are additional related protections under the Affordable Care Act. For plan
years beginning on or after January 1, 2014, a group health plan generally cannot
limit or deny benets relating to a health condition that was present before
enrollment in the plan (a preexisting condition). For more information see the
Affordable Care Act section of this publication at page 9 or visit the Affordable
Care Act Web page of the Department of Labor’s Employee Benets Security
Administration (EBSA) at dol.gov/ebsa/healthreform/ or the Department of
Health and Human Services’ Website at HealthCare.gov.
Is my plan required to provide preventive services related to the
detection of breast cancer?
Under the Affordable Care Act, plans must provide certain preventive services,
such as breast cancer mammography screenings for women 40 years of age and
older, with no copayment, coinsurance or deductible (or other cost-sharing). For
more information, visit HealthCare.gov/what-are-my-preventive-care-benets/.
WHCRA does not require coverage for preventive services related to the
detection of breast cancer.
What information should be included in the notice provided when
participants enroll in the plan?
The enrollment notice must state that, for an individual who is receiving
mastectomy-related benets, coverage will be provided in a manner determined
in consultation with the aending physician and the patient for:
55
All stages of reconstruction of the breast on which the mastectomy was
performed;
Surgery and reconstruction of the other breast to produce a symmetrical
appearance;
Prostheses; and
Treatment of physical complications of the mastectomy, including
lymphedema.
The enrollment notice must also describe any deductibles and coinsurance
limitations applicable to such coverage. Under WHCRA, coverage of breast
reconstruction and other benets specied in WHCRA may be subject only to
deductibles and coinsurance limits consistent with those established for other
medical/surgical benets under the plan or coverage.
A copy of a model enrollment notice is included on page 141.
What information should be included in the annual notice to
participants in the plan?
The annual notice should describe the four categories of coverage required
and should contain information on how to obtain a detailed description of
the mastectomy-related benets available under the plan. To satisfy this
annual notice requirement, the plan may provide the same notice it provided
to individuals upon enrollment in the plan if it contains the appropriate
information as described above.
A model annual notice is included on page 142.
How must the plan provide these notices to participants?
These notices must be delivered in accordance with the Department of Labor’s
disclosure rules applicable to furnishing Summary Plan Descriptions. For
example, the notices may be provided by rst class mail or any other means of
delivery prescribed in the regulation. A separate notice must be furnished to a
group health plan beneciary where the last known address of the beneciary is
different than the last known address of the covered participant.
To avoid duplication of notices, a group health plan can satisfy the WHCRA
notice requirements by contracting with another party that provides the required
notice. For example, in the case of an insured group health plan, the plan will
satisfy the notice requirements with respect to a particular participant if the
issuer timely provides the notice including the information required by WHCRA.

Where can I nd more information about the requirements under
WHCRA?
WHCRA is administered by the U.S. Departments of Labor and Health and
Human Services.
For more information regarding an employer-sponsored group health
plan’s responsibilities under WHCRA, visit the Website of the Department
of Labor’s Employee Benets Security Administration at dol.gov/ebsa/
healthlawschecksheets.html.
For more information on WHCRA, visit the Website of the Department of Health
and Human Services’ Centers for Medicare & Medicaid Services at
cms.gov/CCIIO/Programs-and-Initiatives/Other-Insurance-Protections/whcra_
factsheet.html.
56
Applying and Enforcing
Laws in Part 7 of ERISA
Are certain benets exempt from the requirements in Part 7 of
ERISA, including HIPAA and the Affordable Care Act?
Part 7 of ERISA (Part 7) does not apply to plans with respect to their provision of
“excepted benets.”
Some benets, such as accidental death and dismemberment benets, are always
excepted benets and are not subject to the laws in Part 7, including HIPAA and
the Aordable Care Act. Other benets, including 1) limited-scope dental and
limited-scope vision benets, 2) benets under certain health exible spending
arrangements, 3) noncoordinated benets, and 4) supplemental benets may be
excepted if certain criteria are met.
More specic information on dental-only and vision-only coverage and
supplemental excepted benets is provided in this section. For more information
on other types of excepted benets, see 29 CFR 2590.732(c) or contact the EBSA
office nearest you.
Are dental-only and vision-only coverage subject to Part 7?
It depends. These benets may constitute limited-scope excepted benets (and,
therefore, are not subject to Part 7) if:
The benets are oered under a separate insurance policy, certicate, or
contract of insurance. (This is an option for insured plans only.)
OR
The benets are “not an integral part of the plan.” (This is an option
for both insured and self-insured plans.) Under the nal rules issued in
September 2014, benets are not an integral part of the plan if participants
have the right to elect not to receive coverage for the benets.
57

Is supplemental health insurance coverage subject to Part 7?
It depends. Three types of coverage may qualify as supplemental excepted
benets (and, therefore, are not subject to Part 7): Medicare supplemental
health insurance, TRICARE supplemental programs, and similar supplemental
coverage provided to coverage under a group health plan.
Coverage will be treated as “similar supplemental coverage” if it is provided
under a separate policy, certicate, or contract of insurance, and it satises these
requirements:
The supplemental coverage must be issued by an entity that does not
provide the plan’s primary coverage;
It must be specically designed to ll gaps in primary coverage, such as
coinsurance or deductibles (but does not include coverage that becomes
secondary or supplemental only under a coordination-of-benets
provision);
The cost of supplemental coverage must not exceed 15 percent of the cost
of primary coverage; and
The supplemental coverage must not differentiate among individuals
and dependents in eligibility, benets, or premiums based on any health
factor.
See Field Assistance Bulletin 2007-04 at dol.gov/ebsa for more information.
Who enforces the requirements of Part 7 of ERISA and parallel
requirements under the Internal Revenue Code and the Public Health
Service Act?
The Secretary of Labor enforces the requirements under ERISA for private-sector
group health plans. In addition, participants and beneciaries can sue both plans
and issuers to enforce their rights under ERISA.
The Secretary of the Treasury enforces requirements for private-sector group
health plans under the Code. A taxpayer that fails to comply may be subject to
certain excise taxes or penalties.
States also have enforcement responsibility, including sanctions available under
State law, for requirements imposed on health insurance issuers. If a State does
58
not act in the areas of its responsibility or does not have authority to enforce, the
Secretary of Health and Human Services may assert Federal authority to enforce,
and impose sanctions on insurers as specied in the statute, including civil
monetary penalties.
Can States laws apply to employment-based group health plan
coverage?
State laws related to health insurance issuers generally continue to apply except
to the extent that such State law “prevents the application of” a requirement
of Part 7 of ERISA. Therefore, if health coverage is offered through an HMO
or an insurance policy, check with your State insurance department for more
information on that State’s insurance laws.
59
Appendix A:
Self-Compliance Tools
61

INTRODUCTION
Self-Compliance Tool for Part 7 of ERISA:
Health Care-Related Provisions
This self-compliance tool is intended to help group
health plans, plan sponsors, plan administrators,
health insurance issuers, and other parties determine
whether a group health plan is in compliance with
some of the provisions of Part 7 of ERISA.
The requirements described in this Part 7 tool
generally apply to group health plans and group
health insurance issuers. However, references in
this tool generally are limited to “group health
plans” or “plans” for convenience. In addition, these
provisions generally do not apply to retiree-only or
excepted benets plans (See 29 CFR 2590.732).
This self-compliance tool is not meant to be
considered legal advice. Rather, it is intended to give
the user a basic understanding of Part 7 of ERISA
to beer carry out plan-related responsibilities. It
provides a summary of the statute, recent regulations
and other guidance issued by the Department.
In addition, some of the provisions discussed involve
issues for which rules have not yet been nalized.
Proposed rules, interim nal rules, and transition
periods generally are noted. Periodically check the
Department of Labor’s Website (dol.gov/ebsa) under
Laws & Regulations for publication of nal rules.
Cumulative List of Self-Compliance Tool Questions for Health Care-Related
Statutes Added to Part 7 of ERISA
I. Determining Compliance with the HIPAA Provisions in Part 7 of ERISA
If you answer “No” to any of the questions below, the group health plan
is in violation of the HIPAA provisions in Part 7 of ERISA.
The Health Insurance Portability and Accountability Act (HIPAA) includes
provisions of Federal law governing health coverage portability, health information
privacy, administrative simplication, medical savings accounts, and long-term
care insurance. The Department of Labor is responsible for the law’s portability and
nondiscrimination requirements.
HIPAA’s portability provisions affect group health plan coverage in the following
ways:
Provide certain individuals special enrollment rights in group health coverage
when specic events occur, e.g., birth of a child (regardless of any open season)
(see Section A), and
Prohibit discrimination in group health plan eligibility, benets, and premiums
based on specic health factors (see Sections B-C).
YES
NO N/A
u
u
62
YES
NO N/A
While HIPAA previously provided for limits with respect to preexisting condition
exclusions, new protections under the Affordable Care Act now prohibit the
imposition of preexisting condition exclusions for plan years beginning on or
after January 1, 2014. For plan years beginning on or after January 1, 2014,
plans are no longer required to issue the general notice of preexisting condition
exclusion or individual notice of period of preexisting condition exclusion.
HIPAA certicates of creditable coverage must be provided through the end
of 2014 (December 31, 2014) so that individuals who may need to offset a
preexisting condition exclusion under a non-calendar year plan would still have
access to a certicate of creditable coverage through the end of 2014. See 29 CFR
2590.701-3, 5; 29 CFR 2590.715-2704 (a).
SECTION A – Compliance with the Special Enrollment Provisions
Group health plans must allow individuals (who are otherwise eligible) to enroll
upon certain specied events, regardless of any late enrollment provisions, if
enrollment is requested within 30 days (or 60 days in the case of the special
enrollment rights added by the Children’s Health Insurance Program
Reauthorization Act of 2009 (CHIPRA), discussed in Question 3) of the event.
The plan must provide for special enrollment, as follows:
Question 1 – Special enrollment upon loss of other coverage
Does the plan provide full special enrollment rights upon loss of other
coverage? ................................................................................................................
A plan must permit loss-of-coverage special enrollment upon: (1) loss of
eligibility for group health plan coverage or health insurance coverage; and
(2) termination of employer contributions toward group health plan coverage.
See ERISA section 701(f)(1); 29 CFR 2590.701-6(a).
When a current employee loses eligibility for coverage, the plan must permit
the employee and any dependents to special enroll. See 29 CFR 2590.701-
6(a)(2)(i).
When a dependent of a current employee loses eligibility for coverage, the
plan must permit the dependent and the employee to special enroll. See 29
CFR 2590.701-6(a)(2)(ii).
Examples: Examples of reasons for loss of eligibility include: legal separation,
divorce, death of an employee, termination or reduction in the number of hours
of employment - voluntary or involuntary (with or without electing COBRA),
exhaustion of COBRA, reduction in hours, “aging out” under other parent’s
coverage, or moving out of an HMO’s service area. Loss of eligibility for
coverage does not include loss due to the individual’s failure to pay premiums or
termination of coverage for cause - such as for fraud. See 29 CFR 2590.701-6(a)
(3)(i).
When employer contributions toward an employee’s or dependent’s coverage
terminates, the plan must permit special enrollment, even if the employee or
u
u
u
u
63

YES
NO N/A
dependent did not lose eligibility for coverage. See 29 CFR 2590.701-6(a)
(3)(ii).
Plans must allow an employee a period of at least 30 days to request
enrollment. See 29 CFR 2590.701-6(a)(4)(i).
Coverage must become effective no later than the rst day of the rst
month following a completed request for enrollment. See 29 CFR
2590.701-6(a)(4)(ii).
Tip: Ensure that the plan permits special enrollment upon all of the loss of
coverage events described above.
Question 2 – Dependent special enrollment
Does the plan provide full special enrollment rights to individuals upon
marriage, birth, adoption, and placement for adoption? ...............................
Plans must generally permit current employees to enroll upon marriage and
upon birth, adoption, or placement for adoption of a dependent child. See
ERISA section 701(f)(2); 29 CFR 2590.701-6(b)(2).
Plans must generally permit a participant’s spouse and new dependents
to enroll upon marriage, birth, adoption, and placement for adoption. See
ERISA section 701(f)(2); 29 CFR 2590.701-6(b)(2).
Plans must allow an individual a period of at least 30 days to request
enrollment. See 29 CFR 2590.701-6(b)(3)(i).
In the case of marriage, coverage must become effective no later than the
rst day of the month following a completed request for enrollment. See 29
CFR 2590.701-6(b)(3)(iii)(A).
In the case of birth, adoption, or placement for adoption, coverage must
become effective as of the date of the birth, adoption, or placement for
adoption. See 29 CFR 2590.701-6(b)(3)(iii)(B).
Tips: Remember to allow all eligible employees, spouses, and new dependents
to enroll upon these events. Also, ensure that the effective date of coverage
complies with HIPAA, keeping in mind that some effective dates of coverage
are retroactive.
Question 3 – Special enrollment rights provided through CHIPRA
Does the plan provide full special enrollment rights as required under
CHIPRA? ...........................................................................................................
Under the following conditions a group health plan must allow an employee
or dependent (who is otherwise eligible) to enroll, regardless of any late
enrollment provisions, if enrollment is requested within 60 days:
u
u
u
u
u
u
u
64

YES
NO N/A
When an employee or dependent’s Medicaid or CHIP coverage is terminated.
When an employee or dependent is covered under a Medicaid plan under title
XIX of the Social Security Act or under a State Children’s Health Insurance
Plan (CHIP) under title XXI of the Social Security Act and coverage of the
employee or dependent is terminated as a result of loss of eligibility, a group
health plan must allow special enrollment. The employee or dependent must
request special enrollment within 60 days after the date of termination of
Medicaid or CHIP coverage. See ERISA section 701(f)(3).
Upon Eligibility for Employment Assistance under Medicaid or CHIP. When
an employee or dependent becomes eligible for premium assistance, with
respect to coverage under the group health plan or health insurance coverage
under a Medicaid plan or State CHIP plan, the group health plan must
allow special enrollment. The employee or dependent must request special
enrollment within 60 days after the employee or dependent is determined to
be eligible for assistance. See ERISA section 701(f)(3).
Note: In addition, employers that maintain a group health plan in a state with a
CHIP or Medicaid program that provides for premium assistance for group health
plan coverage must provide a written notice (referred to as the Employer CHIP
Notice) to each employee to inform them of possible opportunities available
in the state in which they reside for premium assistance for health coverage of
employees or dependents. A model notice is available at dol.gov/ebsa/newsroom/
fschip.html.
Question 4 – Treatment of special enrollees
Does the plan treat special enrollees the same as individuals who enroll when
rst eligible, for purposes of eligibility for benet packages and premiums?
If an individual requests enrollment while the individual is entitled to special
enrollment, the individual is a special enrollee, even if the request for
enrollment coincides with a late enrollment opportunity under the plan. See
29 CFR 2590.701-6(d)(1).
Special enrollees must be offered the same benet packages available to
similarly situated individuals who enroll when rst eligible. (Any difference
in benets or cost-sharing requirements for different individuals constitutes a
different benet package.) In addition, a special enrollee cannot be required
to pay more for coverage than a similarly situated individual who enrolls in
the same coverage when rst eligible. See 29 CFR 2590.701-6(d)(2).
Question 5 – Notice of special enrollment rights
Does the plan provide timely and adequate notices of special enrollment
rights? ......................................................................................................................
On or before the time an employee is offered the opportunity to enroll in
the plan, the plan must provide the employee with a description of special
enrollment rights.
u
u
u
u
u
65

YES
NO N/A
Tip: Ensure that the special enrollment notice is provided at or before the time
an employee is initially offered the opportunity to enroll in the plan. This may
mean breaking it off from the SPD. The plan can include its special enrollment
notice in the SPD if the SPD is provided at or before the initial enrollment
opportunity (for example, as part of the application materials). If not, the special
enrollment notice must be provided separately to be timely. A model notice is
provided in the Model Disclosures on page 138.
SECTION B – Compliance with the HIPAA Nondiscrimination Provisions
Overview. HIPAA prohibits group health plans and health insurance issuers
from discriminating against individuals in eligibility and continued eligibility for
benets and in individual premium or contribution rates based on health factors.
These health factors include: health status, medical condition (including both
physical and mental illnesses), claims experience, receipt of health care, medical
history, genetic information, evidence of insurability (including conditions
arising out of acts of domestic violence and participation in activities such as
motorcycling, snowmobiling, all-terrain vehicle riding, horseback riding, skiing,
and other similar activities), and disability. See ERISA section 702; 29 CFR
2590.702.
Similarly Situated Individuals. It is important to recognize that the
nondiscrimination rules prohibit discrimination within a group of similarly
situated individuals. Under 29 CFR 2590.702(d), plans may treat distinct
groups of similarly situated individuals differently, if the distinctions between
or among the groups are not based on a health factor. If distinguishing among
groups of participants, plans and issuers must base distinctions on bona de
employment-based classications consistent with the employer’s usual business
practice. Whether an employment-based classication is bona de is based
on relevant facts and circumstances, such as whether the employer uses the
classication for purposes independent of qualication for health coverage. Bona
de employment-based classications might include: full-time versus part-time
employee status; different geographic location; membership in a collective
bargaining unit; date of hire or length of service; or differing occupations. In
addition, plans may treat participants and beneciaries as two separate groups
of similarly situated individuals. Plans may also distinguish among beneciaries.
Distinctions among groups of beneciaries may be based on bona de
employment-based classications of the participant through whom the
beneciary is receiving coverage, relationship to the participant (such as spouse
or dependent), marital status, age of dependent children, or any other factor that
is not a health factor. However, see section 2714 of the PHS Act, as amended by
the Affordable Care Act and incorporated into section 715 of ERISA, for rules on
dening dependents under the plan. (For information regarding the Affordable
Care Act, please visit our Website at dol.gov/ebsa/healthreform).
Exception for benign discrimination: The nondiscrimination rules do not
prohibit a plan from establishing more favorable rules for eligibility or premium
rates for individuals with an adverse health factor, such as a disability. See 29
CFR 2590.702(g).
66

YES
NO N/A
Check to see that the plan complies with HIPAA’s nondiscrimination provisions
as follows:
Question 6 – Nondiscrimination in eligibility
Does the plan allow individuals eligibility and continued eligibility under the
plan regardless of any adverse health factor? .....................................................
Examples of plan provisions that violate ERISA section 702(a) because they
discriminate in eligibility based on a health factor include:
Plan provisions that require “evidence of insurability,” such as passing a
physical exam, providing a certication of good health, or demonstrating
good health through answers to a health care questionnaire in order to
enroll. See 29 CFR 2590.702(b)(1).
Also, note that it may be permissible for plans to require individuals to
complete physical exams or health care questionnaires for purposes other
than for determining eligibility to enroll in the plan, such as for determining
an appropriate blended, aggregate group rate for providing coverage to the
plan as a whole. See 29 CFR 2590.702(b)(1)(iii) Example 1.
Tip: Eliminate plan provisions that deny individuals eligibility or continued
eligibility under the plan based on a health factor, even if such provisions apply
only to late enrollees.
Question 7 – Nondiscrimination in benets
Does the plan uniformly provide benets to participants and beneciaries,
without directing any benet restrictions at individual participants and
beneciaries based on a health factor? ................................................................
Benets provided must be uniformly available and any benet restrictions
must be applied uniformly to all similarly situated individuals and cannot
be directed at any individual participants or beneciaries based on a health
factor. If benet exclusions or limitations are applied only to certain
individuals based on a health factor, this would violate ERISA section 702(a)
and 29 CFR 2590.702(b)(2).
Examples of plan provisions that may be permissible under ERISA section
702(a) include:
Limits or exclusions for certain types of treatments or drugs,
Limitations based on medical necessity or experimental treatment, and
Cost-sharing,
if the limit applies uniformly to all similarly situated individuals and is not
directed at individual participants or beneciaries based on a health factor.
However, other provisions of law, such as the Affordable Care Act, may prohibit
some of these limitations (such as PHS Act section 2713, requiring plans and
issuers to provide coverage for, and not impose cost-sharing requirements with
u
u
v
u
u
v
v
v
67

YES
NO N/A
respect to, certain recommended preventive services. (For information regarding
the Affordable Care Act, please visit our Website at dol.gov/ebsa/healthreform).
Question 8 – Source-of-injury restrictions
If the plan imposes a source-of-injury restriction, does it comply with the
HIPAA nondiscrimination provisions? ................................................................
Plans may exclude benets for the treatment of certain injuries based on the
source of that injury, except that plans may not exclude benets otherwise
provided for treatment of an injury if the injury results from an act of
domestic violence or a medical condition. See 29 CFR 2590.702(b)(2)(iii).
An example of a permissible source-of-injury exclusion would include:
A plan provision that provides benets for head injuries generally, but
excludes benets for head injuries sustained while participating in
bungee jumping.
An impermissible source-of-injury exclusion would include:
A plan provision that generally provides coverage for medical/surgical
benets, including hospital stays that are medically necessary, but
excludes benets for self-inicted injuries or attempted suicide. This is
impermissible because the plan provision excludes benets for treatment
of injuries that may result from a medical condition (depression).
If the plan does not impose a source-of-injury restriction, check “N/A” and
skip to Question 9.
Question 9 – Nondiscrimination in premiums or contributions
Does the plan comply with HIPAA’s nondiscrimination rules regarding
individual premium or contribution rates? .........................................................
Under ERISA section 702(b) and 29 CFR 2590.702(c), plans may not require
an individual to pay a premium or contribution that is greater than a premium
or contribution for a similarly situated individual enrolled in the plan on the
basis of any health factor. For example, it would be impermissible for a plan
to require certain full-time employees to pay a higher premium than other
full-time employees based on their prior claims experience.
Nonetheless, the nondiscrimination rules do not prohibit a plan from
providing a reward based on adherence to a wellness program. See ERISA
section 702(b)(2)(B); PHS Act section 2705. Final rules for wellness
programs were published on June 6, 2013 at 29 CFR 2590.702 and 29
CFR 2590.715-2705. (These rules were issued through authority under
the Affordable Care Act (PHS section 2705) and under the HIPAA
nondiscrimination provisions. These rules apply to both grandfathered and
nongrandfathered group health plans.)
u
v
v
u
u
u
u
68

YES
NO N/A
To help evaluate whether this exception is available, refer to Section C on page
70. Once you have completed Section C, return to this page to continue with
Question 10, below.
Question 10 – List billing
Is there compliance with the list billing provisions? ...........................................
Under 29 CFR 2590.702(c)(2)(ii), plans and issuers may not charge or quote
an employer a different premium for an individual in a group of similarly
situated individuals based on a health factor. This practice is commonly
referred to as list billing. If an issuer is list billing an employer and the plan is
passing the separate and different rates on to the individual participants and
beneciaries, both the plan and the issuer are violating the prohibition against
discrimination in premium rates. This does not prevent plans and issuers
from taking the health factors of each individual into account in establishing
a blended/aggregate rate for providing coverage to the plan.
Note: Plans and issuers are not permitted to adjust premium or contribution
rates based on genetic information of one or more individuals in the group.
For more information on discrimination based on genetic information, refer to
Section V. Note also that, under the Affordable Care Act, certain premium rating
requirements apply to health insurance coverage in the small group market. Visit
HealthCare.gov for more information.
Question 11 – Nonconnement clauses
Is the plan free of any nonconnement clauses? .................................................
Typically, a nonconnement clause will deny or delay eligibility for some
or all benets if an individual is conned to a hospital or other health
care institution. Sometimes nonconnement clauses also deny or delay
eligibility if an individual cannot perform ordinary life activities. Often a
nonconnement clause is imposed only with respect to dependents, but they
sometimes are also imposed with respect to employees. 29 CFR 2590.702(e)
(1) explains that these nonconnement clauses violate ERISA sections 702(a)
(if the clause delays or denies eligibility) and 702(b) (if the clause raises
individual premiums).
Tip: Delete all nonconnement clauses.
Question 12 – Actively-at-work clauses
Is the plan free of any impermissible actively-at-work clauses?.........................
Typically, actively-at-work provisions delay eligibility for benets based on
an individual being absent from work. 29 CFR 2590.702(e)(2) explains that
actively-at-work provisions generally violate ERISA sections 702(a) (if the
clause delays or denies eligibility) and 702(b) (if the clause raises individual
premiums or contributions), unless absence from work due to a health factor
is treated, for purposes of the plan, as if the individual is at work.
u
u
u
69

YES
NO N/A
Nonetheless, an exception provides that a plan may establish a rule for
eligibility that requires an individual to begin work for the employer
sponsoring the plan before eligibility commences. Further, plans may
establish rules for eligibility or set any individual’s premium or contribution
rate in accordance with the rules relating to similarly situated individuals
in 29 CFR 2590.702(d). For example, a plan that treats full-time and part-
time employees differently for other employment-based purposes, such as
eligibility for other employee benets, may distinguish in rules for eligibility
under the plan between full-time and part-time employees.
Tip: Carefully examine any actively-at-work provision to ensure consistency
with HIPAA.
SECTION C – Compliance with the Wellness Program Provisions
Use the following questions to help determine whether the plan offers a program
of health promotion or disease prevention that is required to comply with
the Department’s nal wellness program regulations and, if so, whether the
program is in compliance with the regulations. See nal regulations issued by
the Departments on June 6, 2013 at 29 CFR 2590.702 and 29 CFR 2590.715-
2705. These regulations use joint authority under HIPAA and the ACA and
apply for plan years beginning on or after January 1, 2014, however regulations
under HIPAA’s nondiscrimination provisions relating to wellness programs
were applicable for plan years prior to the applicability of these nal wellness
program rules. The requirements relating to wellness programs apply to both
grandfathered and non-grandfathered group health plans (See further discussion
of grandfather status under the ACA section VII, A of this tool).
Question 13 – Does the plan have a wellness program? .....................................
A wide range of wellness programs exist to promote health and prevent
disease. However, these programs are not always labeled “wellness
programs.” Examples include: a program that reduces individuals’ cost-
sharing for complying with a preventive care plan; a diagnostic testing
program for health problems; and rewards for attending educational classes,
following healthy lifestyle recommendations, or meeting certain biometric
targets (such as weight, cholesterol, nicotine use, or blood pressure targets).
Tip: Ignore the labels – wellness programs can be called many things. Other
common names include: disease management programs, smoking cessation
programs, and case management programs.
Question 14 – Is the wellness program part of a group health plan? ................
The wellness program is only subject to Part 7 of ERISA if it is part of a
group health plan. If the employer operates the wellness program separate
from the group health plan, the program may be regulated by other laws, but
it is not subject to the group health plan rules discussed here.
u
u
70

YES
NO N/A
Example: An employer institutes a policy that any employee who smokes will
be red. Here, the anti-smoking policy is not part of the group health plan, so the
wellness program rules do not apply. (But see 29 CFR 2590.702, which claries
that compliance with the HIPAA nondiscrimination rules, including the wellness
program rules, is not determinative of compliance with any other provision of
ERISA or any other State or Federal law, such as the Americans with Disabilities
Act.)
Question 15 – Does the program discriminate based on a health factor (i.e., is
it a health-contingent program)?...........................................................................
A program discriminates based on a health factor if it requires an individual
to meet a standard related to a health factor in order to obtain a reward (or
requires an individual to undertake more than a similarly situated individual
based on a health factor in order to obtain the same reward). A reward can be
in the form of a discount or rebate of a premium or contribution, a waiver of
all or part of a cost-sharing mechanism (such as deductibles, copayments, or
coinsurance), an additional benet, or any other nancial or other incentive.
A reward can also be the avoidance of a penalty (such as the absence of a
surcharge, or other nancial or nonnancial disincentive).
If none of the conditions for obtaining a reward is based on an individual
satisfying a standard that is related to a health factor (or if a wellness
program does not provide a reward), the wellness program is a participatory
wellness program. See 29 CFR 2590.702 (f)(1)(ii).
Example 1: Plan participants who have a cholesterol level under 200 will
receive a premium reduction of 30 percent. In this Example 1, the plan requires
individuals to meet a standard related to a health factor in order to obtain a
reward.
Example 2: A plan requires all eligible employees to complete a health risk
assessment to enroll in the plan. Employee answers are fed into a computer
that identies risk factors and sends educational information to the employee’s
home address. In this Example 2, the requirement to complete the assessment
does not, itself, discriminate based on a health factor. However, if the plan used
individuals’ specic health information to discriminate in individual eligibility,
benets, or premiums, there would be discrimination based on a health factor.
Tip: Participatory wellness programs are permissible, provided the program is
made available to all similarly situated individuals, regardless of health status.
u
u
71
If you answered “No” to ANY of the above questions 13-15, STOP. The plan is not subject to the HIPAA
wellness rules. If you are completing this section as part of a review of your plan, please continue to Section D.

YES
NO N/A
v
u
u
u
Question 16 – If the program discriminates based on a health factor, is the
program saved by the benign discrimination provisions? .................................
The Department’s regulations at 29 CFR 2590.702(g) permit discrimination
in favor of an individual based on a health factor.
Example: A plan grants participants who have diabetes a waiver of the plan’s
annual deductible if they enroll in a disease management program that consists
of attending educational classes and following their doctor’s recommendations
regarding exercise and medication. This is benign discrimination because the
program is offering a reward to individuals based on an adverse health factor.
Tip: The benign discrimination exception is NOT available if the plan asks
diabetics to meet a standard related to a health factor (such as maintaining
a certain body mass index (BMI)) in order to get a reward. In this case, an
intervening discrimination is introduced and the plan cannot rely solely on the
benign discrimination exception.
72
If you answered “Yes” to this question, STOP. There does not appear to be a violation of the wellness program
rules. If you are completing this section as part of a review of your plan, please continue to Section D.
If you answered “No” to this question, proceed to Questions 17 and 18. The health-contingent wellness
program must meet the 5 criteria.
Question 17— Within the health-contingent wellness program category, is
the program an activity-only program?................................................................
An activity-only wellness program is a type of health-contingent wellness
program that requires an individual to perform or complete an activity
related to a health factor in order to obtain a reward but does not require
the individual to attain or maintain a specic health outcome. See 29 CFR
2590.702 (f)(1)(iv).
Examples include walking, diet or exercise programs.
If you answered “Yes” to this question, proceed to Question 19.
If you answered “No” to this question, proceed to Question 18.
Question 18— Within the health-contingent wellness program category, is
the program an outcome-based program?............................................................
An outcome-based wellness program is a type of health-contingent wellness
program that requires an individual to attain or maintain a specic health
outcome (such as not smoking or attaining certain results on biometric
screenings) in order to obtain a reward. See 29 CFR 2590.702 (f)(1)(iv).

YES
NO N/A
73
Question 19—Is the health-contingent program in compliance with the ve
requirements?..............................................................................................................
A. Is the amount of the reward offered under the plan limited to 30 percent
(or 50 percent for programs designed to prevent or reduce tobacco use)
of the applicable cost of coverage? (29 CFR 2590.702 (f)(3)(ii) and 29
CFR 2590.702(f)(4)(ii)).....................................................................................
If only employees are eligible to participate, the amount of the reward must
not exceed 30 percent (or 50 percent) of the cost of employee-only coverage
under the plan. If employees and any class of dependents are eligible to
participate, the reward must not exceed 30 percent of the cost of coverage in
which an employee and any dependents are enrolled.
The 30 percent (or 50 percent) limitation on the amount of the reward
applies to all of a plan’s wellness programs that require individuals to meet a
standard related to a health factor.
Example: If the plan has two wellness programs with standards related to a
health factor, a 20 percent reward for meeting a BMI target and a 10 percent
reward for meeting a cholesterol target, it would meet the maximum limit on
the total reward available, which is 30 percent. If instead, the program offered
a 20 percent reward for meeting a body mass index target, a 10 percent reward
for meeting a cholesterol target, and a 10 percent reward for completing a health
risk assessment (regardless of any individual’s specic health information),
the rewards would not need to be adjusted because the 10 percent reward for
completing the health risk assessment does not require individuals to meet a
standard related to a health factor.
B. Is the plan reasonably designed to promote health or prevent disease?
(29 CFR 2590.702(f)(2)(iii) and 29 CFR 2590.702(f)(4)(iii)).........................
The program must be reasonably designed to promote health or prevent
disease. The program should have a reasonable chance of improving the
health of or preventing disease in participating individuals, not be overly
burdensome, not be a subterfuge for discriminating based on a health
factor, and not be highly suspect in the method chosen to promote health
or prevent disease. This determination is based on all the relevant facts and
circumstances.
C. Are individuals who are eligible to participate given a chance to qualify
at least once per year? (29 CFR 2590.702(f)(3)(i) and 29 CFR 2590.702(f)
(4)(i))..................................................................................................................

YES
NO N/A
u
u
u
u
74
D. Is the reward available to all similarly situated individuals? Does the
program offer a reasonable alternative standard? (29 CFR 2590.702(f)
(3)(iv) and 29 CFR 2590.702(f)(4)(iv))............................................................
The wellness program rules require that the reward be available to all
similarly situated individuals. A component of meeting this criterion is
that the program must have a reasonable alternative standard (or waiver
of the otherwise applicable standard) that is furnished by the plan upon a
participant’s request.
Activity-only programs
A reasonable alternative standard must be available for obtaining the reward
for any individual for whom, for that period, it is unreasonably difcult
due to a medical condition to satisfy the otherwise applicable standard or
medically inadvisable to attempt to satisfy the otherwise applicable standard.
See 29 CFR 2590.702(f)(3)(iv)(A)(1)
If reasonable under the circumstances, a plan or issuer may seek verication,
such as a statement from an individual’s personal physician, that a health
factor makes it unreasonably difcult for the individual to satisfy, or
medically inadvisable for the individual to attempt to satisfy, the otherwise
applicable standard. See 29 CFR 2590.702(f)(3)(iv)(A)(2)
Outcome-based wellness programs
The reasonable alternative standard must be available to any individual
who does not meet the initial standard based on the measurement, test, or
screening. See 29 CFR 2590.702(f)(4)(iv)(A)
Plans may not seek verication, such as a statement from an individual’s
personal physician, that a health factor makes it unreasonably difcult for the
individual to satisfy, or medically inadvisable for the individual to attempt to
satisfy the standard. See 29 CFR 2590.702(f)(4)(iv)(E)
E. Does the plan disclose the availability of a reasonable alternative
standard in all plan materials describing the program? (29 CFR
2590.702(f)(3)(v)) .............................................................................................
The plan or issuer must disclose the availability of a reasonable alternative
standard in all plan materials describing the program and in any disclosure
that an individual did not satisfy an initial outcome-based standard. If plan
materials merely mention that the program is available, without describing its
terms, this disclosure is not required.
Tip: The disclosure does not have to say what the reasonable alternative standard
is in advance. The plan can individually tailor the standard for each individual, on
a case-by-case basis.

YES
NO N/A
75
The following sample language can be used to satisfy this requirement: “If it is
unreasonably difcult due to a medical condition for you to achieve the standards
for the reward under this program, or if it is medically inadvisable for you to
attempt to achieve the standards for the reward under this program, call us at
[insert telephone number] and we will work with you to develop another way to
qualify for the reward.”
Note: This section highlights the ve requirements for a health-contingent
program and briey describes the separate requirements for an activity-only
program and an outcome-based program. For more information on the ve
requirements and differences between the activity-only and outcome-based
programs, please visit our Website at dol.gov/ebsa/healthreform.
Taking into consideration whether the health-contingent wellness program is activity-only or outcome-based:
If you answered “Yes” to all of the 5 questions on wellness program criteria, there does not appear to be a
violation of the HIPAA wellness program rules.
If you answered “No” to any of the 5 questions on wellness program criteria, the plan has a wellness program
compliance issue. Specically,
Violation of the general benet discrimination rule (29 CFR 2590.702(b)(2)(i), 29 CFR 2590.715-
2705(a)) – If the wellness program varies benets, including cost-sharing mechanisms (such as deductible,
copayment, or coinsurance) based on whether an individual meets a standard related to a health factor and the
program does not satisfy the requirements of 29 CFR 2590.702(f), the plan is impermissibly discriminating in
benets based on a health factor. The wellness program exception at 29 CFR 2590.702(b)(2)(ii) is not satised
and the plan is in violation of 29 CFR 2590.702(b)(2)(i) and 29 CFR 2590.715-2705(a).
Violation of general premium discrimination rule (29 CFR 2590.702(c)(1), 29 CFR 2590.715-2705(a)) –
If the wellness program varies the amount of premium or contribution it requires similarly situated individuals
to pay based on whether an individual meets a standard related to a health factor and the program does not
satisfy the requirements of 29 CFR 2590.702(f), the plan is impermissibly discriminating in premiums based
on a health factor. The wellness program exception at 29 CFR 2590.702(c)(3) is not satised and the plan is in
violation of 29 CFR 2590.702(c)(1) and 29 CFR 2590.715.2705(a).

YES
NO N/A
SECTION D – Compliance with the MEWA or Multiemployer Plan
Guaranteed Renewability Provisions
If the plan is a multiple employer welfare arrangement (MEWA) or a
multiemployer plan, it is required to provide guaranteed renewability of coverage
in accordance with ERISA section 703. If the plan is a MEWA or multiemployer
plan, it must meet the criteria described in Question 20. If the plan is not a
MEWA or multiemployer plan, check “N/A” and go to Part II of this
self-compliance tool. ................................................................................................
Question 20 – Multiemployer plan and MEWA guaranteed renewability
If the plan is a multiemployer plan, or a MEWA, does the plan provide
guaranteed renewability? ......................................................................................
Group health plans that are multiemployer plans or MEWAs may not deny an
employer continued access to the same or different coverage, other than:
For nonpayment of contributions;
For fraud or other intentional misrepresentation by the employer;
For noncompliance with material plan provisions;
Because the plan is ceasing to offer coverage in a geographic area;
In the case of a plan that offers benets through a network plan, there
is no longer any individual enrolled through the employer who lives,
resides, or works in the service area of the network plan and the plan
applies this paragraph uniformly without regard to the claims experience
of employers or any health-related factor in relation to such individuals
or dependents; or
For failure to meet the terms of an applicable collective bargaining
agreement, to renew a collective bargaining or other agreement requiring
or authorizing contributions to the plan, or to employ employees covered
by such agreement.
See ERISA section 703.
**Note: The Public Health Service (PHS) Act contains guaranteed renewability
requirements for issuers.
u
v
v
v
v
v
v
76

II. Determining Compliance with the Mental Health Parity Act (MHPA) and
Mental Health Parity and Addiction Equity Act (MHPAEA) Provisions in Part 7 of ERISA
(together, the mental health parity provisions)
If you answer “No” to any of the questions below, the group health plan is in violation of the mental health
parity provisions in Part 7 of ERISA.
Introduction
If the plan provides either mental health or substance use disorder benets, in
addition to medical/surgical benets, the plan may be subject to the mental health
parity provisions in Part 7 of ERISA. Retiree-only plans, and those offering
excepted benets, are generally not subject to the mental health parity provisions
under part 7 of ERISA. See 29 CFR 2590.732 for further discussion. (Note: if
under an arrangement(s) to provide medical care by an employer or employee
organization, any participant or beneciary can simultaneously receive coverage for
medical/surgical benets and mental health or substance use disorder benets, the
mental health parity requirements apply separately with respect to each combination
of medical/surgical benets and mental health/substance use disorder benets and
all such combinations are considered to be a single group health plan. See 29 CFR
2590.712(e).) If this is the case, answer Questions 21-28.
If the plan does not provide mental health or substance use disorder benets, check
“N/A” here and skip to Part III of this checklist. Also, the plan may be exempt from
the mental health parity provisions under the small employer (50 employees or
fewer) exception or the increased cost exception. (To be eligible for the increased
cost exception, the plan must have led a notice with EBSA and notied participants
and beneciaries.) Unless a plan is exempt as previously described, the requirements
of MHPAEA generally apply to both grandfathered and non-grandfathered group
health plans
13
, as dened under the Affordable Care Act. Note that the Department
of Health and Human Services’ nal rule regarding essential health benets (EHB)
requires health insurance issuers offering non-grandfathered health insurance
coverage in the small group market through an Affordable Health Insurance
Exchange (Marketplace) or outside of a Marketplace to comply with MHPAEA in
order to satisfy the requirement to provide EHB.
In addition, under MHPAEA, if a plan or issuer provides mental health or substance
use disorder benets in any classication described in the MHPAEA nal regulation,
mental health or substance use disorder benets must be provided in every
classication in which medical/surgical benets are provided. Under the Affordable
Care Act, PHSA section 2713, non-grandfathered group health plans are required
to provide certain preventive services with no cost-sharing, which includes, among
YES
NO N/A
77
13
Mental health and substance use disorder benets are dened under the terms of the plan, in accordance
with applicable Federal and State law. Any condition or disorder dened by the plan as being or as not being
a mental health condition or substance use disorder must be dened in a manner consistent with generally
recognized independent standards of current medical practice (e.g., the most current version of the DSM or
ICD or State guidelines).

YES
NO N/A
other things, alcohol misuse screening and counseling, depression screening,
and tobacco use screening. However, the Departments claried that nothing in
MHPAEA requires a group health plan that provides mental health or substance
use disorder benets only to the extent required under PHSA section 2713,
to provide additional mental health or substance use disorder benets in any
classication.
14
If the plan is exempt, check “N/A” here and skip to Part III of this checklist. .......
SECTION A. Lifetime and Annual Limits
Question 21 – Does the plan comply with the mental health parity
requirements regarding lifetime dollar limits on mental health/substance use
disorder benets? ...................................................................................................
A plan generally may not impose a lifetime dollar limit on mental health/
substance use disorder benets that is lower than the lifetime dollar limit
imposed on medical/ surgical benets. See 29 CFR 2590.712(b). (Only
limits on what the plan would pay are taken into account, as contrasted with
limits on what an individual may be charged.)
Note: These provisions are affected by section 2711 of the Public Health Service
Act, as amended by the Patient Protection and Affordable Care Act. Specically,
PHS Act section 2711 generally prohibits lifetime and annual dollar limits on
essential health benets (EHB), which includes mental health and substance
use disorder services. Accordingly, for mental health and substance use disorder
benets that are EHB, plans cannot impose lifetime limits. For mental health and
substance use disorder benets that are not EHB, parity requirements regarding
aggregate lifetime dollar limits apply. (For information regarding the Affordable
Care Act, please visit our Website at dol.gov/ebsa/healthreform).
Question 22 – Does the plan comply with the mental health parity
requirements regarding annual dollar limits on mental health/substance use
disorder benets? ...................................................................................................
A plan generally may not impose an annual dollar limit on mental health/
substance use disorder benets that is lower than the annual dollar limit
imposed on medical/surgical benets. See 29 CFR 2590.712(b). (Again, only
limits on what the plan would pay are taken into account, as contrasted with
limits on what an individual may be charged.)
Tip: There is a different rule for cumulative limits other than aggregate lifetime
or annual dollar limits discussed later in this checklist at Question 26. A plan
may impose annual out-of-pocket dollar limits on participants and beneciaries if
done in accordance with the rule regarding cumulative limits.
u
u
78
14
See 29 CFR 2590.712(e)(3)(i)

YES
NO N/A
Note: These provisions are affected by section 2711 of the Public Health Service
Act, as amended by the Patient Protection and Affordable Care Act. Specically,
PHS Act section 2711 generally prohibits annual dollar limits on essential health
benets, which includes mental health and substance use disorder services.
Accordingly, the parity requirements regarding annual dollar limits only apply to the
provision of mental health and substance use disorder benets that are not Essential
Health Benets. Note also that for plan years beginning in 2015, the annual
limitation on an individual’s maximum out-of-pocket (MOOP) costs in effect under
ACA is $6,600 for self-only coverage and $13,200 for coverage other than self-only
coverage. See ACA Implementation FAQ Part XXI at dol.gov/ebsa/faqs/faq-aca21.
html.
(For information regarding the Affordable Care Act, please visit our Website at
dol.gov/ebsa/healthreform).
SECTION B. Financial Requirements and Quantitative Treatment Limitations
Question 23 – Does the plan comply with the mental health parity
requirements for parity in nancial requirements and quantitative treatment
limitations? ..................................................................................................................
A plan may not impose a nancial requirement or quantitative treatment
limitation applicable to mental health/substance use disorder benets in any
classication that is more restrictive than the predominant nancial requirement
or quantitative treatment limitation of that type that is applied to substantially all
medical/surgical benets in the same classication. See 29 CFR 2590.712(c)(2).
Types of nancial requirements include deductibles, copayments,
coinsurance, and out-of-pocket maximums. See 29 CFR 2590.712(c)(1)(ii).
Types of quantitative treatment limitations include annual, episode, and
lifetime day and visit limits, for example, number of treatments, visits, or
days of coverage. See 29 CFR 2590.712(c)(1)(ii).
The six classications* of benets are:
1) inpatient, in-network;
2) inpatient, out-of-network;
3) outpatient, in-network;
4) outpatient, out-of-network;
5) emergency care; and
6) prescription drugs.
See 29 CFR 2590.712(c)(2)(ii).
Under the plan, any nancial requirement or quantitative treatment limitation
that applies to mental health/substance use disorder benets within a particular
classication cannot be more restrictive than the predominant requirement or
limitation that applies to substantially all medical/surgical benets within the
same classication. See 29 CFR 2590.712(c)(2).
v
u
79
v
u
u
*See page 81 for special rules related to classications.

YES
NO N/A
Detailed steps for applying these rules are set forth below:
To determine compliance, each type of nancial requirement or quantitative
treatment limitation within a coverage unit
15
must be analyzed separately
within each classication. See 29 CFR 2590.712(c)(2)(i). If a plan applies
different levels of a nancial requirement or quantitative treatment limitation
to different coverage units in a classication of medical/surgical benets (for
example, a $15 copayment for self-only and a $20 copayment for family
coverage), the predominant level is determined separately for each coverage
unit. See 29 CFR 2590.712(c)(3)(ii).
Step One: First determine if a particular type of nancial requirement or
quantitative treatment limitation applies to substantially all medical/surgical
benets in the relevant classication of benets.
Generally, a nancial requirement or quantitative treatment limitation
is considered to apply to substantially all medical/surgical benets
if it applies to at least two-thirds of the medical/surgical benets in
the classication. See 29 CFR 2590.712(c)(3)(i)(A). This two-thirds
calculation is generally based on the dollar amount of plan payments
expected to be paid for the plan year. See 29 CFR 2590.712(c)(3)(i)(C).
(Any reasonable method can be used for this calculation. See 29 CFR
2590.712(c)(3)(i)(E).)
Step Two: If the type of nancial requirement or quantitative treatment
limitation applies to at least two-thirds of medical/surgical benets in that
classication, then determine the predominant level of that type of nancial
requirement or quantitative treatment limitation that applies to medical/
surgical benets subject to that type of nancial requirement or quantitative
treatment limitation in that classication of benets. (Note: If the type of
nancial requirement or quantitative treatment limitation does not apply to
at least two-thirds of medical/surgical benets in that classication, it cannot
apply to mental health/substance use disorder benets in that classication.)
Generally, the predominant level will apply to more than one-half
of the medical/surgical benets in that classication subject to the
nancial requirement or quantitative treatment limitation. See 29 CFR
2590.712(c)(3)(i)(B)(1). If there is no single level that applies to more
than one-half of medical/surgical benets in the classication, the plan
can combine levels until the combination of levels applies to more than
one-half of medical/surgical benets subject to the nancial requirement
or quantitative treatment limitation in the classication. The least
restrictive level within the combination is considered the predominant
level.
16
See 29 CFR 2590.712(c)(3)(i)(B)(2).
u
u
v
80
u
v
15
Coverage unit refers to the way in which a plan groups individuals for purposes of determining benets, or premiums or
contributions, for example, self-only, family, and employee plus spouse. See 29 CFR 2590.712(c)(1)(iv).
16
For a simpler method of compliance, a plan may treat the least restrictive level of nancial requirement or treatment limitation
applied to medical/surgical benets as predominant.

YES
NO N/A
*Note: Special rules related to classications
1. Special rule for outpatient sub-classications:
For purposes of determining parity for outpatient benets (in-network and
out-of network), a plan or issuer may divide its benets furnished on an
outpatient basis into two sub-classications: (1) ofce visits and (2) all
other outpatient items and services, for purposes of applying the nancial
requirement and treatment limitation rules.
After the sub-classications are established, the plan or issuer may not
impose any nancial requirement or quantitative treatment limitation on
mental health/substance use disorder benets in any sub-classication (i.e.,
ofce visits or non-ofce visits) that is more restrictive than the predominant
nancial requirement or treatment limitation that applies to substantially all
medical/surgical benets in the sub-classication using the methodology set
forth in the nal rules.
Other than as explicitly permitted under the nal rules, sub-classications
are not permitted when applying the nancial requirement and treatment
limitation rules under MHPAEA. Accordingly, separate sub-classications
for generalists and specialists are not permitted. (See Question 24 for more
information regarding specialists and generalists.)
2. Special rule for prescription drug benets:
There is a special rule for multi-tiered prescription drug benets. A plan
complies with the mental health parity provisions if the plan applies different
levels of nancial requirements to different tiers of prescription drug benets
based on reasonable factors and without regard to whether a drug is generally
prescribed for medical/surgical or mental health/substance use disorder
benets. Reasonable factors include cost, efcacy, generic versus brand
name, and mail order versus pharmacy pick-up. See 29 CFR 2590.712(c)(3)
(iii).
3. Special rule for multiple network tiers:
There is a special rule for multiple network tiers. If a plan provides
benets through multiple tiers of in-network providers (such as in-network
preferred and in-network participating providers), the plan may divide
its benets furnished on an in-network basis into sub-classications that
reect network tiers, if the tiering is based on reasonable factors (such as
quality, performance, and market standards) and without regard to whether a
provider provides services with respect to medical/surgical benets or mental
health or substance use disorder benets. After the sub-classications are
established, the plan or issuer may not impose any nancial requirement or
treatment limitation on mental health or substance use disorder benets in
any sub-classication that is more restrictive than the predominant nancial
requirement or treatment limitation that applies to substantially all medical/
surgical benets in the sub-classication.
u
u
u
81
u
u

YES
NO N/A
Tips: Ensure that the plan does not impose cost-sharing requirements or
quantitative treatment limitations that are applicable only to mental health/
substance use disorder benets.
Ensure that with respect to conducting the predominant/substantially all test,
the analysis must be done with respect to the dollar amount of all plan payments
expected to be paid for the relevant plan year. Basing the analysis on an insurer’s
entire overall book of business for the year or book of business in a specic
region or State is not a permissible analysis for demonstrating compliance with
MHPAEA.
Question 24 – If the plan imposes a higher, specialist nancial requirement,
such as a copay, on mental health/substance use disorder benets, can the
plan demonstrate that the specialist level of the nancial requirement is the
predominant level that applies to substantially all medical/surgical benets
within the classication? ........................................................................................
The six classications outlined in Question 23 are the only classications
that may be used when determining the predominant nancial requirements
or quantitative treatment limitations that apply to substantially all medical/
surgical benets. See 29 CFR 2590.712(c)(2)(ii). A plan may not use a
separate sub-classication under these classications for generalists and
specialists. See preamble language at 75 FR 5413.
Tip: A plan may still be able to impose the specialist level of a nancial
requirement or quantitative treatment limitation if it is the predominant level that
applies to substantially all medical/surgical benets within a classication. For
example, if the specialist level of copay is the predominant level of copay that
applies to substantially all medical/surgical benets in the outpatient, in-network
classication, the plan may apply the specialist level copay to mental health/
substance use disorder benets in the outpatient, in-network classication. See 29
CFR 2590.712(c)(3).
SECTION C. Coverage in all Classications
Question 25 – Does the plan comply with the mental health parity
requirements for coverage in all classications? .................................................
If a plan provides mental health/substance use disorder benets in any
classication of benets (the classications are listed in Question 23),
mental health/substance use disorder benets must be provided in every
classication in which medical/surgical benets are provided. See 29 CFR
2590.712(c)(2)(ii)(A).
In determining the classication in which a particular benet belongs, a
plan must apply the same standards to medical/surgical benets and to
mental health/substance use disorder benets. See 29 CFR 2590.712(c)
(2)(ii)(A). This rule also applies to intermediate services provided under
the plan or coverage. Plans must assign covered intermediate mental
health and substance use disorder benets (such as residential treatment,
partial hospitalization and intensive outpatient treatment) to the
u
v
u
82

YES
NO N/A
existing six classications in the same way that they assign comparable
intermediate medical/surgical benets to these classications. For
example, if a plan classies skilled nursing and rehabilitation hospitals
for medical/surgical benets as inpatient benets, it must classify
residential treatment facilities for mental health and substance use
disorder benets as inpatient benets. If a plan treats home health care
as an outpatient benet, then any covered intensive outpatient mental
health/substance use disorder services and partial hospitalization must
be considered outpatient benets as well. A plan must also comply with
MHPAEA’s NQTL rules, discussed in the following section, in assigning
any benets to a particular classication. See 29 CFR 2590.712(c)(4).
Tips:
If the plan does not contract with a network of providers, all benets are out-
of-network. If a plan that has no network imposes a nancial requirement or
treatment limitation on inpatient or outpatient benets, the plan is imposing
the requirement or limitation within classications (inpatient, out-of-network
or outpatient, out-of-network), and the rules for parity will be applied
separately for the different classications. See 29 CFR 2590.712(c)(2)(ii)(C),
Example 1.
If a plan covers the full range of medical/surgical benets (in all
classications, both in-network and out-of-network), beware of exclusions on
out-of-network mental health and substance use disorder benets.
The plan must ensure that all combinations of benets comport with parity.
Note: As explained in the Introduction to this section, nothing in MHPAEA
requires a non-grandfathered group health plan that provides mental health or
substance use disorder benets only to the extent required under PHSA section
2713, to provide additional mental health or substance use disorder benets in
any classication.
SECTION D. Cumulative Financial Requirements and Treatment
Limitations
Question 26 – Does the plan comply with the mental health parity provisions
on cumulative nancial requirements or cumulative quantitative treatment
limitations? .............................................................................................................
A plan may not apply any cumulative nancial requirement or cumulative
quantitative treatment limitation for mental health/substance use disorder
benets in a classication that accumulates separately from any established
for medical/surgical benets in the same classication. See 29 CFR
2590.712(c)(3)(v).
Cumulative nancial requirements are nancial requirements that
determine whether or to what extent benets are provided based on
accumulated amounts and include deductibles and out-of-pocket
maximums (but do not include aggregate lifetime or annual dollar limits
because these two terms are excluded from the meaning of nancial
u
83
u
u
v

YES
NO N/A
requirements). See 29 CFR 2590.712(a).
Cumulative quantitative treatment limitations are treatment limitations
that determine whether or to what extent benets are provided based on
accumulated amounts, such as annual or lifetime day or visit limits. See
29 CFR 2590.712(a).
For example, a plan may not impose an annual $250 deductible on all
medical/surgical benets and a separate $250 deductible on all mental health/
substance use disorder benets.
SECTION E. Nonquantitative Treatment Limitations
Question 27 – Does the plan comply with the mental health parity provisions
for parity within nonquantitative treatment limitations?...................................
Nonquantitative treatment limitations (NQTLs) include:
Medical management standards limiting or excluding benets based on
medical necessity or medical appropriateness, or based on whether the
treatment is experimental or investigative;
Formulary design for prescription drugs;
For plans with multiple network tiers (such as preferred providers and
participating providers), network tier design;
Standards for provider admission to participate in a network, including
reimbursement rates;
Plan methods for determining usual, customary, and reasonable charges;
Refusal to pay for higher-cost therapies until it can be shown that a
lower-cost therapy is not effective (also known as fail-rst policies or
step therapy protocols);
Exclusions based on failure to complete a course of treatment; and
Restrictions based on geographic location, facility type, provider
specialty, and other criteria that limit the scope or duration of benets for
services provided under the plan or coverage.
This is an illustrative, nonexhaustive list. See 29 CFR 2590.712(c)(4)(ii).
General rules:
A plan may not impose an NQTL with respect to mental health/substance
use disorder benets in any classication (such as inpatient, out-of-
network) unless, under the terms of the plan (as written and in operation),
any processes, strategies, evidentiary standards, or other factors used in
applying the NQTL to mental health/substance use disorder benets in the
classication are comparable to and applied no more stringently than the
processes, strategies, evidentiary standards or other factors used in applying
the NQTL with respect to medical/surgical benets in the classication. See
29 CFR 2590.712(c)(4)(i).
A group health plan may consider a wide array of factors in designing
medical management techniques for both mental health/substance use
disorder benets and medical/surgical benets, such as cost of treatment;
u
v
u
u
u
84
v
v
v
v
v
v
v
v

YES
NO N/A
high cost growth; variability in cost and quality; elasticity of demand;
provider discretion in determining diagnosis, or type or length of treatment;
clinical efcacy of any proposed treatment or service; licensing and
accreditation of providers; and claim types with a high percentage of fraud.
Based on application of these or other factors in a comparable fashion, an
NQTL, such as prior authorization, may be required for some (but not all)
mental health/substance use disorder benets, as well as for some medical/
surgical benets, but not for others. See 29 CFR 2590.712(c)(4), Example 8.
Examples: The Departments have published several examples that help illustrate
how the MHPAEA regulations apply to some common plan NQTLs, including:
1) The penalty for failure to obtain preauthorization is more punitive with
respect to mental health/substance use disorder benets than with respect
to medical/surgical benets. See 2590.712(c)(4)(iii), Example 3.
2) The plan uses an employee assistance program as a gatekeeper to
obtaining mental health or substance use disorder benets. See
2590.712(c)(4)(iii), Example 6.
3) Utilization management practices that differ among different plan
benets. See 29 CFR 2590.712(c)(4)(iii), Example 8.
Tips: Do not focus on results. Look at the underlying processes and
strategies used in applying NQTLs (such as utilization review (UR) and
standards for network admission). Are there arbitrary or discriminatory
differences in how the plan is applying those processes and strategies to medical/
surgical benets versus mental health/substance use disorder benets?
A plan or issuer that limits eligibility for mental health and substance use disorder
benets until after benets under an EAP are exhausted has established an
NQTL subject to the parity requirements. If no comparable requirement applies
to medical/surgical benets such a requirement could not be applied to mental
health or substance use disorder benets.
Questions You Might Ask:
1) What classication of benets is being analyzed? Does the plan clearly
dene which benets are treated as medical/surgical and which benets
are treated as mental health/substance use disorder under the plan. Are
benets (such as non-hospital inpatient and partial hospitalization)
assigned to classications using a comparable methodology across
medical/surgical benets and mental health/substance use disorder
benets?
2) What is the type and description of any NQTL being applied and is it
applied in parity?
3) Overall explanation of how each NQTL is applied with respect to
medical/surgical benets and mental health and substance use disorder
benets. (Note: this includes requirements that both the participant
and provider may be subject to pursuant to the NQTL). If only certain
benets are subject to an NQTL, such as meeting a fail rst protocol or
requiring preauthorization, how were the specic medical/surgical and
85

86
YES
NO N/A
mental health or substance use disorder benets subject to the NQTL
determined? To the extent medical guidelines are relied upon, is there
a process for determining variation/application of the guidelines that is
comparable with respect to both medical/surgical and mental health or
substance use disorder benets?
4) Even if benets are subject to the same NQTL, does the plan impose
stricter penalties for noncompliance with respect to mental health and
substance use disorder benets (for example, reducing benets to 50%
of eligible expenses for failure to obtain prior authorization for mental
health and substance use disorder benets, vs. 20% for medical/surgical
benets)?
5) If utilization review is conducted by different entities/individuals
for medical/surgical and mental health or substance use disorder
benets provided under the plan, what processes are in place to ensure
comparability in the standards used for UR and comparability in the
independence and qualications of the individuals performing UR?
6) Has the plan documented its analysis that its NQTL processes and
strategies (such as UR) are comparable across medical/surgical and
mental health/substance use disorder benets?
Tip: Plans should keep records documenting NQTL processes and how they are
being applied to both medical/surgical as well as mental health and substance use
disorder benets to ensure they can demonstrate compliance with the law. Such
records may also be helpful to plans in responding to inquiries from participants
and beneciaries regarding benets under the plan. See a more detailed
discussion of disclosure requirements in the following section.
Illustrations. Set forth below are additional illustrations of how a plan may have
differences in nonquantitative treatment limitations:
NQTLs but may still comply with the Departments’ regulations, based on the
facts and circumstances involved:
Plan X covers neuropsychological testing but only for certain conditions.
In such situations, look to see whether the exclusion is based on evidence
addressing for example, clinical efcacy of such testing for different
conditions and the degree to which such testing is used for educational
purposes with regard to different conditions. Does the plan rely on
criteria and evidence from comparable sources with respect to medical/
surgical and mental health conditions? Does the plan have documentation
indicating the criteria used and evidence supporting the plan’s determination
of the diagnoses for which they will cover this service and the rationale
for excluding certain diagnoses? The result may be that the plan covers
neuropsychological testing for some medical/surgical or mental health
conditions, but not for all. This outcome may be permissible to the extent the
plan has based the exclusion on clinical efcacy and/or other factors if done
in a comparable manner and applies the NQTL in a comparable manner.
u

YES
NO N/A
Plan Y uses diagnosis related group (DRG) codes in their standard utilization
review process to actively manage hospitalization utilization. For all
non-DRG hospitalizations (whether due to an underlying medical/surgical
condition or a mental health or substance use disorder condition), the plan
requires precertication for hospital admission and incremental concurrent
review. The precertication and concurrent review processes review unique
clinical presentation, condition severity, expected course of recovery,
quality and efciency. The evidentiary standards and other factors used in
the development of the concurrent review process are comparable across
medical/surgical benets and mental health/substance use disorder benets,
and are well documented. These evidentiary standards and other factors are
available to participants and beneciaries free of charge upon request. In this
example, it appears that, under the terms of the plan as written and in practice,
the processes, strategies, evidentiary standards, and other factors considered
by the plan in implementing its precertication and concurrent review of
hospitalizations is comparable and applied no more stringently with respect
to mental health and substance use disorder benets than those applied with
respect to medical/surgical benets.
Plan Z classies care in skilled nursing facilities or rehabilitation hospitals as
inpatient benets and likewise treats any covered care in residential treatment
facilities for mental health or substance use disorders as an inpatient benet.
In addition, the plan treats home health care as an outpatient benet and,
likewise treats intensive outpatient and partial hospitalization for mental health
or substance use disorder services as outpatient benets. In this example, the
plan assigns covered intermediate mental health and substance use disorder
benets to the six classications in the same way that it assigns comparable
intermediate medical/surgical benets.
Master’s degree training and state licensing requirements often vary among
provider types. Plan Z consistently applies its standard that any provider must
meet whatever is the most stringent licensing requirement standard related
to supervised clinical experience requirements in order to participate in the
network. Therefore, Plan Z requires master’s-level therapists to have post-
degree, supervised clinical experience in order to join their provider network.
There is no parallel requirement for master’s-level general medical providers
because their licensing does require supervised clinical experience. In addition,
the plan does not require post-degree, supervised clinical experience for
psychiatrists or PhD level psychologists since their licensing already requires
supervised training. The requirement that master’s-level therapists must have
supervised clinical experience to join the network is permissible, as the plan
consistently applies the same standard to all providers even though it may have
a disparate impact on certain mental health providers.
u
u
u
87

YES
NO N/A
SECTION F. Disclosure Requirements
Question 28 – Does the plan comply with the mental health parity disclosure
requirements? .........................................................................................................
The plan administrator (or the health insurance issuer) must make available
the criteria for medical necessity determinations made under a group health
plan with respect to mental health/substance use disorder benets (or health
insurance coverage offered in connection with the plan with respect to such
benets) to any current or potential participant, beneciary, or contracting
provider upon request. See 29 CFR 2590.712(d)(1).
The plan administrator (or health insurance issuer) must make available
the reason for any denial under a group health plan (or health insurance
coverage) of reimbursement or payment for services with respect to mental
health/substance use disorder benets to any participant or beneciary in a
form and manner consistent with the rules in 29 CFR 2560.503-1 (the DOL
claims procedure rule) and 29 CFR 2590.715-2719. (internal claims and
appeals and external review processes).
Pursuant to the internal claims and appeals and external review rules under
the Affordable Care Act, applicable to all non-grandfathered group health
plans, claims related to medical judgment (including mental health/substance
use disorder) are eligible for external review. The internal claims and appeals
rules include the right of claimants (or their authorized representative) to be
provided upon request and free of charge, reasonable access to and copies of
all documents, records, and other information relevant to the claimant’s claim
for benets. This includes documents with information about the processes,
strategies, evidentiary standards, and other factors used to apply an NQTL
with respect to medical/surgical benets and mental health/substance use
disorder benets under the plan. See 29 CFR 2590.712(d)(3).
If coverage is denied based on medical necessity, medical necessity criteria
for the mental health/substance use disorder benets at issue and for medical/
surgical benets in the same classication must be provided within 30 days
of the request to the participant, beneciary, or provider or other individual if
acting as an authorized representative of the beneciary or participant. See
29 CFR 2520.104b-1; 29 CFR 2590.712(d)(1).
Make Showing Compliance Simple!
Documents or Plan Instruments Participants and Beneciaries or DOL may
request:
Participants and beneciaries may request documents and plan instruments
regarding whether the plan is providing benets in accordance with MHPAEA
and copies must be furnished within 30 days of request. This may include
documentation that illustrates how the health plan has determined that any
nancial requirement, quantitative treatment limitation, or nonquantitative
treatment limitation is in compliance with MHPAEA. For example, participants
and beneciaries may ask for:
u
u
u
88
u

u
YES
NO N/A
An analysis showing that the plan meets the predominant/substantially
all test. The plan may need to provide information regarding the amount
of medical/surgical claims subject to a certain type of QTL, such as a co-
payment, in the prior year in a classication or its basis for calculating claims
expected to be subject to a certain type of QTL in the current plan year in a
classication, for purposes of determining the plan’s compliance with the
predominant/substantially all test.
A description of an applicable requirement or limitation, such as
preauthorization or concurrent review, that the plan has authorized for mental
health/substance use disorder services and medical/surgical benets within
the relevant classication (in- or out-of-network, in- or outpatient). These
might include references to specic plan documents, for example provisions
as stated on specied pages of the SPD, or other underlying guidelines or
criteria not included in the SPD that the Plan has consulted or relied upon;
Information regarding factors, such as cost or recommended standards of
care, that are relied upon by a plan for determining which medical/surgical
or mental health or substance use disorder benets are subject to a specic
requirement or limitation. These might include references to specic related
factors or guidelines, such as applicable utilization review criteria;
A description of the applicable requirement or limitation that the plan
believes have been used in any given mental health/substance use
disorder service adverse benet determination (ABD) within the relevant
classication;
Medical necessity guidelines relied upon for in and out-of-network medical/
surgical and mental health and substance use disorder benets.
Tips:
Participants, beneciaries and contracting providers may request information to
determine whether benets under a plan are being provided in parity even in the
absence of any specic adverse benet determination.
Plans may need to work with insurance carriers providing coverage on behalf
of an insured group health plan or with third party administrators administering
the plan to ensure that such service providers either directly or in coordination
with the plan are providing participants and beneciaries any documents or
information to which they are entitled.
If a plan uses mental health and substance use disorder vendors and carve-
out service providers, the plan must ensure that all combinations of benets
comport with parity, therefore vendors and carve out providers should provide
documentation of the necessary information to the Plan to ensure that all
combination of benets comport with parity.
Note: Compliance with the disclosure requirements of MHPAEA is not
determinative of compliance with any other provision or other applicable Federal
or State law. Be sure that the Plan, in addition to these disclosure requirements, is
disclosing information relevant to medical/surgical, mental health, and substance
use disorder benets as required pursuant to other applicable provisions of law.
u
u
u
89
u

III. Determining Compliance with the Newborns’ Act Provisions in Part 7 of ERISA
If you answer “No” to any of the questions below, the group health plan is
in violation of the Newborns’ Act provisions in Part 7 of ERISA.
SECTION A – Newborns’ Act Substantive Provisions
The substantive provisions of the Newborns’ Act apply only to certain plans, as
follows:
If the plan does not provide benets for hospital stays in connection with
childbirth, check “N/A” and go to Part IV of this self-compliance tool. (Note:
Under the Pregnancy Discrimination Act, most plans are required to cover
maternity benets.)
Special applicability rule for insured coverage that provides benets for hospital
stays in connection with childbirth:
If the plan provides benets for hospital stays in connection with childbirth, the
plan is insured, and the coverage is in Wisconsin and several U.S. territories, it
appears that the Federal Newborns’ Act applies to the plan. If this is the case,
answer the questions in SECTION A and SECTION B. If the plan provides
benets for hospital stays in connection with childbirth and is insured, whether
the plan is subject to the Newborns’ Act depends on State law. Based on a
recent preliminary review of State laws, if the coverage is in any other state or
the District of Columbia, it appears that State law applies in lieu of the Federal
Newborns’ Act. If this is the case, check “N/A” and skip to SECTION B.
Self-insured coverage that provides benets for hospital stays in connection
with childbirth: If the plan provides benets for hospital stays in connection with
childbirth and is self-insured, the Federal Newborns’ Act applies. Answer the
questions in SECTION A and SECTION B.
Question 29 – General 48/96-hour stay rule
Does the plan comply with the general 48/96-hour rule? .........................................
Plans generally may not restrict benets for a hospital length of stay in
connection with childbirth to less than 48 hours in the case of a vaginal delivery
(See ERISA section 711(a)(1)(A)(i)), or less than 96 hours in the case of a
cesarean section (See ERISA section 711(a)(1)(A)(ii)).
Therefore, a plan cannot deny a mother or her newborn benets within a 48/96-
hour stay based on medical necessity. (A plan may require a mother to notify the
plan of a pregnancy to obtain more favorable cost-sharing for the hospital stay.
This second type of plan provision is permissible under the Newborns’ Act if the
cost-sharing is consistent throughout the 48/96-hour stay.)
YES
NO N/A
u
u
90
YES
NO N/A
An attending provider may, however, decide, in consultation with the mother,
to discharge the mother or newborn earlier.
Question 30 – Provider must not be required to obtain authorization
from plan
Plans may not require providers to obtain authorization from the plan to
prescribe a 48/96-hour stay. Does the plan comply with this rule?.....................
Plans may not require that a provider (such as a doctor) obtain authorization
from the plan to prescribe a 48/96-hour stay. See ERISA section 711(a)(1)(B);
29 CFR 2590.711(a)(4).
Tips: Watch for plan preauthorization requirements that are too broad. For
example, a plan may have a provision requiring preauthorization for all hospital
stays. Providers cannot be required to obtain preauthorization from the plan
in order for the plan to cover a 48-hour (or 96-hour) stay in connection with
childbirth. Therefore, in this example, the plan must add clarifying language to
indicate that the general preauthorization requirement does not apply to 48/96-
hour hospital stays in connection with childbirth. (Conversely, plans generally
may require participants or beneciaries to give notice of a pregnancy or hospital
admission in connection with childbirth in order to obtain, for example, more
favorable cost-sharing.) Nonetheless, the Newborns’ Act does not prevent plans
and issuers from requiring providers to obtain authorization for any portion of a
hospital stay that exceeds 48 (or 96) hours.
Question 31 – Incentives/penalties to mothers or providers
Does the plan comply with the Newborns’ Act by avoiding impermissible
incentives or penalties with respect to mothers or attending providers?.............
Penalties to attending providers to discourage 48/96-hour stays violate ERISA
section 711(b)(3) and 29 CFR 2590.711(b)(3)(i).
Incentives to attending providers to encourage early discharges violate ERISA
section 711(b)(4) and 29 CFR 2590.711(b)(3)(ii).
Penalties imposed on mothers to discourage 48/96-hour stays violate ERISA
section 711(b)(1) and 29 CFR 2590.711(b)(1)(i)(A).
Incentives to mothers to encourage early discharges violate ERISA section
711(b)(2) and 29 CFR 2590.711(b)(1)(i)(B).
An example of this would be if the plan waived the mother’s copayment
or deductible if the mother or newborn leaves within 24 hours.
Benets and cost-sharing may not be less favorable for the latter portion of
any 48/96-hour hospital stay. In this case less favorable benets would violate
ERISA section 711(b)(5) and 29 CFR 2590.711(b)(2) and less favorable cost-
sharing would violate ERISA section 711(c)(3) and 29 CFR 2590.711(c)(3).
u
u
u
u
u
v
u
u
91

YES
NO N/A
SECTION B – Disclosure Provisions
Group health plans that provide benets for hospital stays in connection with
childbirth are required to make certain disclosures, as follows:
Question 32 – Disclosure with respect to hospital lengths of stay in
connection with childbirth
Does the plan comply with the notice provisions relating to hospital stays in
connection with childbirth?....................................................................................
Group health plans that provide benets for hospital stays in connection with
childbirth are required to make certain disclosures. Specically, the group
health plan’s SPD must include a statement describing any requirements
under Federal or State law applicable to the plan, and any health insurance
coverage offered under the plan, relating to hospital length of stay in
connection with childbirth for the mother or newborn child. See the SPD
content regulations at 29 CFR 2520.102-3(u).
Tip: Whether the plan is insured or self-insured, and whether the Federal New-
borns’ Act provisions or State law provisions apply to the coverage, the plan
must provide a notice describing any requirements relating to hospital length
of stays in connection with childbirth. A model notice is provided in the Model
Disclosures on page 140.
u
92

IV. Determining Compliance with the WHCRA Provisions in Part 7 of ERISA
If you answer “No” to any of the questions below, the group health plan is
in violation of the WHCRA provisions in Part 7 of ERISA.
WHCRA applies only to plans that offer benets with respect to a mastectomy. If
the plan does not offer these benets, check “N/A” and go to Part V of this self-
compliance tool..............................................................................................................
If the plan does offer benets with respect to a mastectomy, answer
Questions 33-36.
Question 33 – Four required coverages under WHCRA
Does the plan provide the four coverages required by WHCRA? .........................
In the case of a participant or beneciary who is receiving benets in connection
with a mastectomy, the plan shall provide coverage for the following benets for
individuals who elect them:
All stages of reconstruction of the breast on which the mastectomy has been
performed;
Surgery and reconstruction of the other breast to produce a symmetrical
appearance;
Prostheses; and
Treatment of physical complications of mastectomy, including lymphedema,
in a manner determined in consultation with the attending provider and the
patient. See ERISA section 713(a).
These required coverages can be subject to annual deductibles and coinsurance
provisions if consistent with those established for other medical/surgical benets
under the plan or coverage.
Tip: Plans that cover benets for mastectomies cannot categorically exclude
benets for reconstructive surgery or certain post-mastectomy services. In addition,
time limits for seeking treatment may run afoul of the general requirement to provide
the four required coverages.
Question 34 – Incentive provisions
Does the plan comply with WHCRA by not providing impermissible incentives
or penalties with respect to patients or attending providers? .................................
A plan may not deny a patient eligibility to enroll or renew coverage solely to
avoid WHCRA’s requirements under ERISA section 713(c)(1).
In addition, under ERISA section 713(c)(2), a plan may not penalize or offer
incentives to an attending provider to induce the provider to furnish care in a
manner inconsistent with WHCRA.
YES
NO N/A
u
u
u
u
v
v
v
v
93

YES
NO N/A
Question 35 – Enrollment notice
Does the plan provide adequate and timely enrollment notices as required by
WHCRA? ...............................................................................................................
Upon enrollment, a plan must provide a notice describing the benets
required under WHCRA. See ERISA section 713(a).
The enrollment notice must describe the benets that WHCRA requires the
group health plan to cover, specically:
All stages of reconstruction of the breast on which the mastectomy was
performed,
Surgery and reconstruction of the other breast to produce a symmetrical
appearance,
Prostheses, and
Physical complications resulting from mastectomy (including lymphe-
dema).
The enrollment notice must describe any deductibles and coinsurance
limitations applicable to such coverage. (Note: Under WHCRA, coverage
of the required benets may be subject only to deductibles and coinsurance
limitations consistent with those established for other medical/surgical
benets under the plan or coverage.)
Tip: A model notice is provided in the Model Disclosures on page 141.
Question 36 – Annual notice
Does the plan provide adequate and timely annual notices as required by
WHCRA? ...............................................................................................................
Plans must provide notices describing the benets required under WHCRA
once each year. See ERISA section 713(a).
To satisfy this requirement, the plan may redistribute the WHCRA enrollment
notice or the plan may use a simplied disclosure that:
Provides notice of the availability of benets under the plan for
reconstructive surgery, surgery to achieve symmetry between the breasts,
prostheses, and physical complications resulting from mastectomy
(including lymphedema); and
Contact information (e.g., telephone number) for obtaining a detailed
description of WHCRA benets available under the plan.
Tip: The WHCRA annual notice can be provided in the SPD if the plan
distributes SPDs annually. If not, the plan should break off the annual notice into
a separate disclosure. A model notice is provided in the Model Disclosures on
page 142.
u
v
v
v
v
u
u
v
v
u
94
u

V. Determining Compliance with the GINA Provisions in Part 7 of ERISA
If you answer “No” to any of the questions below, the group health plan is
in violation of the GINA provisions in Part 7 of ERISA.
Unlike HIPAA, the GINA provisions generally do apply to very small health plans
(plans with less than two participants who are current employees), including retiree-
only health plans.
Denitions (for all dened terms under GINA, see 29 CFR 2590.702-1(a)):
Genetic information means, with respect to an individual, information about the
individual’s genetic tests, the genetic tests of family members of the individual, the
manifestation (see denition below) of a disease or disorder in family members of
the individual or any request for or receipt of genetic services or participation in
clinical research which includes genetic services by the individual or any family
member of the individual.
Genetic information includes, with respect to a pregnant woman or family
member of the pregnant woman, genetic information of any fetus carried by the
pregnant woman.
Genetic information includes, with respect to an individual who is utilizing an
assisted reproductive technology, genetic information of any embryo legally held
by the individual or family member.
Genetic information does NOT include information about the sex or age of any
individual.
Family member means, with respect to an individual, a dependent of the individual
or any person who is a rst-degree, second-degree, third-degree, or fourth-degree
relative of the individual or a dependent of the individual. Relatives of afnity
(such as by marriage or adoption) are treated the same as relatives by consanguinity
(that is, relatives who share a common biological ancestor). Relatives by less than
full consanguinity (such as half-siblings, who share only one parent) are treated
the same as relatives by full consanguinity (such as siblings who share both
parents). Therefore, family members include parents, spouses, siblings, children,
grandparents, grandchildren, aunts, uncles, nephews, nieces, great-grandparents,
great-grandchildren, great aunts, great uncles, rst cousins, great-great grandparents,
great-great grandchildren, and children of rst cousins.
Manifestation means, with respect to a disease, disorder, or pathological condition,
that an individual has been or could reasonably be diagnosed with the disease,
disorder, or pathological condition by a health care professional with appropriate
training and expertise in the eld of medicine involved. A disease, disorder, or
pathological condition is not manifested if a diagnosis is based principally on genetic
information.
YES
NO N/A
u
u
u
95

YES
NO N/A
Genetic services means a genetic test, genetic counseling (including obtaining,
interpreting, or assessing genetic information) or genetic education.
Genetic test means an analysis of human DNA, RNA, chromosomes, proteins,
or metabolites, if the analysis detects genotypes, mutations, or chromosomal
changes.
A genetic test does NOT include an analysis of proteins or metabolites that is
directly related to a manifested disease, disorder, or pathological condition. For
example, a test to determine whether an individual has a BRCA1 or BRCA2,
genetic variants associated with a signicantly increased risk for breast cancer, is
a genetic test. An HIV test, complete blood count, cholesterol test, liver function
test, or test for the presence of alcohol or drugs is not a genetic test.
Question 37 – Does the plan comply with GINA’s prohibition against group-
based discrimination based on genetic information? .........................................
A group health plan cannot adjust premium or contribution amounts for the
plan, or any similarly situated individuals under the plan, on the basis of
genetic information. See 29 CFR 2590.702-1(b)(1).
Nothing limits a plan from increasing the premium for the group health plan
or for a group of similarly situated individuals under the plan based on the
manifestation of a disease or disorder of an individual enrolled in the plan.
However, the manifestation of the disease in one individual cannot be used
as genetic information about other group members to further increase the
premium for a group health plan or a group of similarly situated individuals
under the plan. See 29 CFR 2590.702-1(b)(2).
Question 38 – Does the plan comply with GINA’s limitation on
requesting or requiring genetic testing? ..............................................................
A group health plan generally must not request or require an individual
or family member of the individual to undergo a genetic test. See 29 CFR
2590.702-1(c)(1).
Exceptions:
A health care professional who is providing health care services to an
individual can request that the individual undergo a genetic test. See 29
CFR 2590.702-1(c)(2).
A plan can obtain and use the results of a genetic test for making a
determination regarding payment. However, the plan is permitted to
request only the minimum amount of information necessary to make the
determination. See 29 CFR 2590.702-1(c)(4).
Exception for research: a plan or issuer may request, but not require,
that a participant or beneciary undergo a genetic test if the request
is pursuant to research and several conditions are met. See 29 CFR
2590.702-1(c)(5).
u
u
u
u
v
v
96
v

YES
NO N/A
Question 39 – Does the plan comply with GINA’s prohibition on collection of
genetic information, prior to or in connection with enrollment?........................
A plan cannot collect genetic information prior to an individual’s effective
date of coverage under that plan or coverage, nor in connection with the rules
for eligibility that apply to that individual. See 29 CFR 2590.702-1(d)(2)(i).
Whether or not an individual’s information is collected prior to that
individual’s effective date of coverage is determined at the time of collection.
Exception for incidental collection:
If a plan obtains genetic information incidental to the collection of other
information concerning any individual, the collection is not a violation,
as long as the collection is not for underwriting purposes. See 29 CFR
2590.702-1(d)(2)(ii)(A).
However, the incidental collection exception does not apply in
connection with any collection where it is reasonable to anticipate that
health information would be received, unless the collection explicitly
states that genetic information should not be provided. See 29 CFR
2590.702-1(d)(2)(ii)(B).
Question 40 – Does the plan comply with GINA’s prohibition on
collection of genetic information, for underwriting purposes? ............................
A plan cannot request, require, or purchase (“collect”) genetic information
for underwriting purposes. See 29 CFR 2590.702-1(d)(1)(i).
Underwriting purposes means, with respect to any group health plan:
Rules for determination of eligibility (including enrollment and
continued eligibility) for benets under the plan or coverage (including
changes in deductibles or other cost-sharing mechanisms in return for
activities such as completing a health risk assessment or participating in
a wellness program);
The computation of premium or contribution amounts under the
plan or coverage (including discounts, rebates, payments in kind, or
other premium differential mechanisms in return for activities such
as completing a health risk assessment or participating in a wellness
program);
The application of any preexisting condition exclusion under the plan or
coverage; and
Other activities related to the creation, renewal, or replacement of a
contract of health insurance or health benets. See 29 CFR 2590.702-
1(d)(1)(ii).
Exception for medical appropriateness (only if an individual seeks a benet
under the plan):
If an individual seeks a benet under a plan, the plan may limit or
exclude the benet based on whether the benet is medically appropriate
and the determination of whether the benet is medically appropriate is
not for underwriting purposes.
u
u
v
v
v
v
97
u
u
u
v
v
u
v

YES
NO N/A
If a plan conditions a benet on medical appropriateness, and medical
appropriateness depends on the genetic information of an individual, the
plan can condition the benet on genetic information. A plan or issuer
is permitted to request only the minimum amount of genetic information
necessary to determine medical appropriateness. See 29 CFR 2590.702-
1(d) (1)(iii) and (e).
v
98
If you answered “Yes” to ALL of the above questions, there does not appear to be a violation of the GINA
regulations.

VI. Compliance with Michelle’s Law
If you answer “No” to any of the questions below, the group health plan is
in violation of the Michelle’s Law provisions in Part 7 of ERISA.
**Note: Under the Affordable Care Act group health plans and issuers are
generally required to provide dependent coverage to age 26 regardless of
student status of the dependent. Nonetheless, under some circumstances, such
as a plan that provides dependent coverage beyond age 26, Michelle’s Law
provisions may apply.
Question 41 – Does the plan comply with the Michelle’s Law requirement not
to terminate coverage of dependent students on medically necessary leave of
absence? ........................................................................................................................
Medically necessary leave of absence means with respect to a dependent child
in connection with a group health plan or health insurance coverage offered in
connection with a group health plan, a leave of absence from or other change in
enrollment status in a postsecondary educational institution that begins while the
child is suffering from a serious illness or injury; is medically necessary; and causes
the child to lose student status for purposes of coverage under the terms of the plan
or coverage.
A dependent child is a beneciary who is a dependent child under the terms of
the plan or coverage, of a participant or beneciary under the plan or coverage
and who was enrolled in the plan or coverage on the basis of being a student at
a postsecondary educational institution immediately before the rst day of the
medically necessary leave of absence involved.
A group health plan or issuer shall not terminate coverage of a dependent child
due to a medically necessary leave of absence that causes the child to lose
student status before the date that is the earlier of:
the date that is one year after the rst day of the medically necessary leave
of absence; or
the date on which such coverage would otherwise terminate under the terms
of the plan or health insurance coverage. See ERISA section 714(b).
Tip: The group health plan or issuer can require receipt of written certication by a
treating physician of the dependent child which states that the dependent child
is suffering from a serious illness or injury and that the leave of absence (or other
change of enrollment) is medically necessary.
YES
NO N/A
u
v
v
99
YES
NO N/A
Question 42 – Does the plan comply with Michelle’s Law’s notice
requirement? ..........................................................................................................
A group health plan or issuer must include with any notice regarding a
requirement for certication of student status for coverage, a description
of the Michelle’s law provision for continued coverage during medically
necessary leaves of absence. See ERISA section 714(c).
u
100

VII. Determining Compliance with the Affordable Care Act Provisions in Part 7 of ERISA
The Affordable Care Act was signed into law by the President on March 23, 2010. Amendments to the
Affordable Care Act made through the Health Care Education and Reconciliation Act (Reconciliation
Act) were signed into law on March 30, 2010. Generally, the Affordable Care Act’s market reform
provisions amend title XXVII of the Public Health Service Act (PHS Act), which is administered
by the Department of Health and Human Services. The Affordable Care Act also creates section
715 of the Employee Retirement Income Security Act (ERISA), administered by the Department of
Labor, Employee Benets Security Administration, and section 9815 of the Internal Revenue Code,
administered by the Department of Treasury (the Treasury) and the Internal Revenue Service (IRS),
to incorporate the market reform provisions of the PHS Act into ERISA and the Code, and make them
applicable to group health plans and health insurance issuers providing group health insurance
coverage. Under section 1251 of the Affordable Care Act, grandfathered health plans are required to
comply with some, but not all, of the market reform provisions. In addition, these provisions do not
apply to retiree-only or excepted benets plans (See ERISA Section 732). The Departments of Labor,
HHS, and the Treasury have been issuing guidance on an ongoing basis since May 2010.
Note, that the Affordable Care Act, PHSA Section 2705 included requirements relating to wellness
programs. The Departments issued nal regulations June 6, 2013 at 29 CFR 2590.702 and 29 CFR
2590.715-2705 using joint authority under HIPAA and the ACA. These requirements relating to
wellness programs are discussed in the HIPAA section of this tool at I (C).
See EBSA’s Website: dol.gov/ebsa/healthreform/ for the most up-to-date guidance.
This compliance aid will be updated in the future to further address additional requirements as they
become applicable, as enforcement grace periods expire, or as the Departments issue additional
guidance.
101
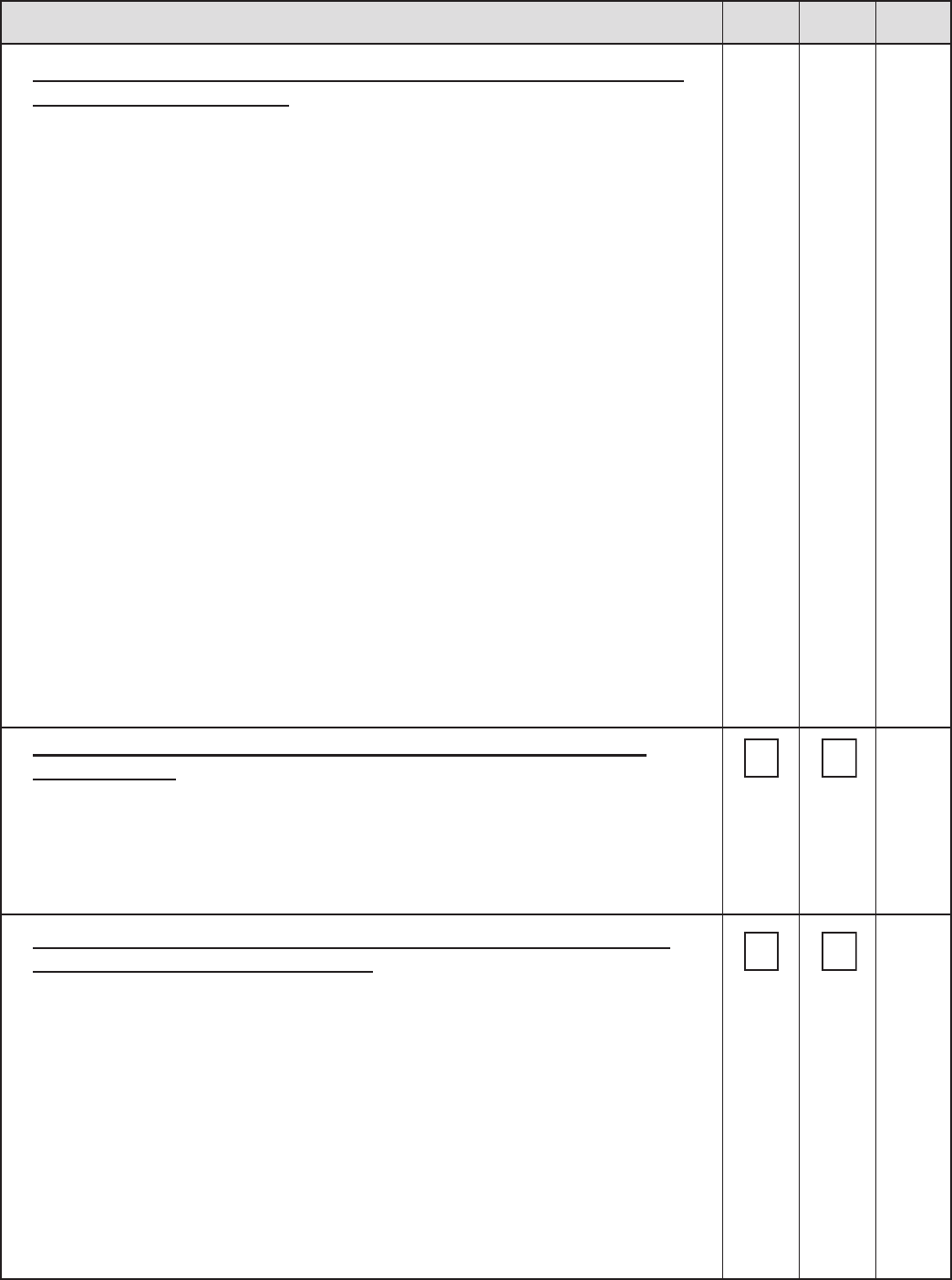
YES
NO N/A
Section A. Determining Grandfather Status Under the Affordable Care Act
Provisions in Part 7 of ERISA
Note: The grandfathered status of a plan will affect whether a plan must comply
with certain provisions of the Affordable Care Act (ACA). There are also special
rules for collectively bargained plans. See also the rules at 29 CFR 2590.715-
1251(f).
Grandfathered status is intended to allow people to keep their coverage as it
existed on March 23, 2010, while giving plans some exibility to make “normal”
changes while retaining grandfathered status. Restrictions and requirements
on grandfathered health plan coverage provides individuals’ protection from
signicant reductions in coverage, provides for coverage to include numerous
protections implemented through the Affordable Care Act, and allows employers
the exibility to manage costs.
The analysis for determining grandfathered status applies separately to each
benet package or option. Accordingly, grandfathered status might be retained
for some benet packages or options and relinquished for others. By contrast, if
an employer relinquished grandfathered status for self-only, family, or any other
tier within a benets package, it would relinquish grandfathered status for the
entire package. See 29 CFR 2590.715-1251(a)(1)(i).
If the plan is not claiming grandfathered status, proceed to Section B.
If the answer is “yes” to questions 43 and 44 below the group health plan
may be a grandfathered health plan.
Question 43 – Did the plan exist with at least one individual enrolled on
March 23, 2010?......................................................................................................
A grandfathered group health plan must have been in existence with an
enrolled individual on March 23, 2010. Any plan that does not meet this
requirement is not in grandfathered status. See 29 CFR 2590.715-1251(a)(1)
(i).
Question 44 – Has the plan continuously covered someone (not necessarily
the same person) since March 23, 2010? ..............................................................
A group health plan will not relinquish its grandfathered status merely
because one or more (or all) individuals enrolled on March 23, 2010, cease to
be covered. However, a grandfathered health plan must continuously cover
someone (not necessarily the same person) since March 23, 2010, to maintain
its status. See 29 CFR 2590.715-1251(a)(1)(i).
If the answers to questions 43 and 44 were “yes”, complete questions 45-
53. If the answer is “no” to either question 43 or 44, the group health plan
cannot claim grandfathered status; proceed to Section B.
u
u
102

YES
NO N/A
Tip: Provided changes are made without exceeding the other standards that
cause a plan to relinquish grandfathered status, changes that generally will not
cause plans to relinquish grandfathered status include changes to: premiums;
to comply with Federal or State legal requirements; to voluntarily comply with
provisions of the Affordable Care Act; third party administrators; network plan’s
provider network; and to a prescription drug formulary.
Question 45 – Has the plan eliminated all or substantially all benets to
diagnose or treat a particular condition? .............................................................
For the purpose of determining grandfathered status, the elimination of
benets for any necessary element to diagnose or treat a condition is
considered the elimination of all or substantially all benets to diagnose or
treat a particular condition. See 29 CFR 2590.715-1251(g)(1)(i).
Question 46 – Has the plan increased a percentage cost-sharing requirement
(such as an individual’s coinsurance)? .................................................................
Any increase measured from March 23, 2010, in a percentage cost-sharing
requirement causes a plan to relinquish grandfathered status. See 29 CFR
2590.715-1251(g)(1)(ii).
Question 47 – Has the plan increased a xed-amount cost-sharing
requirement other than a copayment (such as a deductible or out-of-pocket
limit) such that the total percentage increase measured from March 23, 2010
exceeds the maximum percentage increase? .......................................................
The maximum percentage increase is medical ination, expressed as a
percentage, plus 15 percentage points. See 29 CFR 2590.715-1251(g)(3)(ii).
Medical ination is the increase since March 2010, in the overall medical
care component of the Consumer Price Index for All Urban Consumers
(CPI-U) (unadjusted) published by the Department of Labor using the 1982-
1984 base of 100. See 29 CFR 2590.715-1251(g)(3)(i).
Question 48 – Has the plan increased a xed-amount copayment such
that the increase measured from March 23, 2010 exceeds the greater of:
the maximum percentage increase, or an amount equal to $5 plus medical
ination? .................................................................................................................
The maximum percentage increase is medical ination, expressed as a
percentage, plus 15 percentage points. See 29 CFR 2590.715-1251(g)(3)(ii).
Medical ination is the increase since March 2010 in the overall medical care
component of the Consumer Price Index for All Urban Consumers (CPI-U)
(unadjusted) published by the Department of Labor using the 1982-1984 base
of 100. See 29 CFR 2590.715-1251(g)(3)(i).
u
u
u
u
103

YES
NO N/A
Question 49 – Has there been a decrease in the contribution rate by the
employer (or employee organization) towards the cost of any tier of coverage
for any class of similarly situated individuals by more than 5 percentage
points below the contribution rate for the coverage period that includes
March 23, 2010? .....................................................................................................
If the contribution rate is based on a formula, was there a decrease in the
contribution rate by more than 5 percentage points below the contribution
rate for the coverage period that includes March 23, 2010? See 29 CFR
2590.715-1251(g)(1)(v)(B).
Tip: If a group health plan modies the tiers of coverage it had on March 23,
2010 (for example, from self-only and family to a multi-tiered structure of self-
only, self-plus-one, self-plus-two, and self-plus-three-or-more), the employer
contribution for any new tier would be tested by comparison to the contribution
rate for the corresponding tier on March 23, 2010. If the plan adds one or more
new coverage tiers without eliminating or modifying any previous tiers and those
new coverage tiers cover classes of individuals that were not covered previously
under the plan, the new tiers would not be analyzed under the standards of
paragraph (g)(1). See DOL FAQs About the Affordable Care Act Implementation
Part II, question 3 at dol.gov/ebsa/faqs/faq-aca2.html.
In cases of a multiemployer plan that has either a xed-dollar employee
contribution or no employee contribution towards the cost of coverage, if the
employer’s contribution rate changes, provided any changes in the coverage
terms would not otherwise cause the plan to cease to be grandfathered and
there continues to be no employee contribution or no increase in the xed-
dollar employee contribution towards the cost of coverage, the change of
the employer’s contribution rate will not, in and of itself, cause a plan that is
otherwise a grandfathered health plan to relinquish grandfathered status. See
DOL FAQs About the Affordable Care Act Implementation Part I, question 4 at
dol.gov/ebsa/faqs/faq-aca.html.
Question 50 – Has the plan added or decreased an overall annual limit on
benets? ..................................................................................................................
A plan will relinquish its grandfathered status if it:
Adds an overall annual limit on the dollar value of all benets when it
did not previously impose an overall annual limit (See 29 CFR 2590.715-
1251(g)(1)(vi)(A));
Previously imposed an overall lifetime limit on the dollar value of
benets (but no overall annual limit) and adopts an overall annual limit
at a dollar value that is lower than the dollar value of the lifetime limit on
March 23, 2010 (See 29 CFR 2590.715-1251(g)(1)(vi)(B)); or
Decreases the dollar value of the overall annual limit that was in place on
March 23, 2010 (See 29 CFR 2590.715-1251(g)(1)(vi)(C)).
u
v
v
v
u
104

YES
NO N/A
Note: For plan years beginning on or after January 1, 2014, a plan may not
establish, for any individual, an annual limit on the dollar amount of benets that
are essential health benets. See 29 CFR 2590.715-2711(b)(1).
If the answer to any of questions 45-50 was “yes”, the plan is NOT a
grandfathered plan, proceed to Section B.
Question 51 – Did the plan change issuers after March 23, 2010? ....................
If the answer to question 51 is “yes”, if the group health plan changed issuers
after March 23, 2010, and the change in issuer was effective on or after
November 15, 2010, the plan will continue to be a grandfathered plan provided
no other changes that would relinquish grandfathered status are made. See 29
CFR 2590.715-1251(a)(1)(ii), as amended. Proceed to question 53.
If a group health plan changed issuers after March 23, 2010, and the change
was effective prior to November 15, 2010, the plan will have relinquished
grandfather status. The plan is not a grandfathered plan; proceed to Section
B.
Tip: The operative date is the effective date of the new contract, not the date
the new contract was entered into. Special rules apply for collectively bargained
plans. See 29 CFR 2590.715-1251(f) for collectively bargained plans.
Question 52 – Did the plan change from self-insured to fully-insured after
March 23, 2010? .....................................................................................................
If the group health plan was self-insured and changed to fully insured after March
23, 2010, and the change was effective on or after November 15, 2010, the plan
will continue to be a grandfathered plan provided no other changes are made that
would relinquish grandfathered status. See 29 CFR 2590.715-1251(a)(1)(ii), as
amended. Proceed to question 53.
If a group health plan was self-insured and changed to fully-insured after
March 23, 2010, and the change was effective prior to November 15, 2010,
the plan will have relinquished grandfathered status. The plan is not a
grandfathered plan; proceed to Section B.
If Questions 51 and 52 are not applicable to the group health plan, continue
to Question 54 to continue the grandfather status analysis.
105

YES
NO N/A
Question 53 – If the group health plan changed issuers (including a plan
that was self-insured and changed to fully insured) and has maintained
grandfathered status, did the plan provide documentation to the new issuer
of the plan terms under the prior health coverage sufcient to determine
whether any other change was made that would relinquish grandfathered
status? ......................................................................................................................
To maintain status as a grandfathered health plan, the plan must provide to
the new issuer (and the new issuer must require) documentation of plan terms
(including benets, cost sharing, employer contributions, and annual limits)
under the prior health coverage sufcient to determine whether any other
change is being made that would relinquish grandfathered status. See 29
CFR 2590.715-1251(a)(3)(ii), as amended.
Question 54 – Does the plan include a statement that it believes it is a
grandfathered health plan in any plan materials provided to participants
and beneciaries that describe the benets provided under the plan? .............
To maintain status as a grandfathered group health plan, the plan must
include a statement, in any plan materials provided to a participant or
beneciary describing the benets under the plan, that the plan believes it
is a grandfathered health plan within the meaning of section 1251 of the
Affordable Care Act and must provide contact information for questions and
complaints. Model language is available. See 29 CFR 2590.715-1251(a)(2).
For all plans that, based on questions 43 through 54, have not relinquished
grandfathered status, complete question 55.
Question 55 – Is the plan maintaining records documenting the terms of the
plan in connection with the coverage in effect on March 23, 2010, and are
these records made available upon request?........................................................
To maintain status as a grandfathered group health plan the plan must
maintain records documenting the terms of the plan in connection with the
coverage that was in effect on March 23, 2010, and any other documents
necessary to verify, explain, or clarify its status as a grandfathered health
plan. These records must be maintained for as long as the plan takes the
position that it is grandfathered, and must be available for examination upon
request. See 29 CFR 2590.715-1251(a)(3)(i)(A) & (i)(B), as amended.
u
u
u
106

YES
NO N/A
Section B. Determining Compliance with the Affordable Care Act Extension
of Dependent Coverage of Children to Age 26 Provisions in Part 7 of ERISA
Note: This provision is applicable for plan years beginning on or after Sept. 23,
2010. This provision applies to both grandfathered and non-grandfathered group
health plans.
Question 56 – Does the plan provide coverage for dependent
children?......................................................................................................................
If the answer to this question is no, proceed to Section C. These provisions
are only applicable to group health plans that provide coverage to dependent
children. If the answer is “yes”, proceed to question 57.
If the answer to the question below is “yes”, the plan is in compliance with
the rules regarding Dependent Coverage to Age 26.
Question 57 – Does the plan make dependent coverage available for children
to age 26? ................................................................................................................
Plans and issuers cannot deny or restrict dependent coverage for a child who
is under age 26 other than in terms of a relationship between a child and the
participant. Thus, plans and issuers cannot deny or restrict dependent coverage
for a child who is under age 26 based on the presence or absence of nancial
dependency upon or residency with the participant or any other person, student
status, employment or any combination of these factors. In addition, plans and
issuers cannot limit dependent coverage based on whether the child under age 26
is married. The Affordable Care Act and implementing regulations do not require
plans to cover children of children. See 29 CFR 2590.715-2714(b) & (c).
The terms of the plan or coverage cannot vary based on age, except for children
who are age 26 or older. See 29 CFR 2590.715-2714(d).
Tip: A plan or issuer does not fail to satisfy the requirements regarding
Dependent Coverage to Age 26 because the plan limits health coverage for
children until the child turns 26 to only those children who are described in
section 152(f)(1) of the Code (That section of the Code denes children to
include only sons, daughters, stepchildren, adopted children (including children
placed for adoption), and foster children.). For an individual not described
in Code section 152(f)(1), such as a grandchild or niece, a plan may impose
additional conditions on eligibility for health coverage, such as a condition that
the individual be a dependent for income tax purposes. See DOL FAQs About the
Affordable Care Act Implementation Part I, question 14 at dol.gov/ebsa/faqs/faq-
aca.html.
107

Section C. Determining Compliance with the Affordable Care Act
Rescission Provisions in Part 7 of ERISA
Note: This provision is applicable for plan years beginning on or after Sept. 23,
2010. This provision applies to both grandfathered and non-grandfathered group
health plans.
A rescission is a cancellation or discontinuance of coverage that has retroactive
effect; this includes a cancellation that treats a policy as void from the time of
the group’s enrollment or a cancellation that voids benets paid up to one year
before the cancellation. A rescission is not the cancellation or discontinuance of
coverage that has only a prospective effect; or the cancellation or discontinuance
of coverage if effective retroactively to the extent it is based on a failure to timely
pay required premiums or contributions towards the cost of coverage. See
29 CFR 2590.715-2712(a)(2).
If the answer to the question below is “yes” the plan is in compliance with
the rules regarding rescission of coverage.
Question 58 – Does the plan only rescind coverage for instances where
an act, practice, or omission that constitutes fraud, or an intentional
misrepresentation of material fact has occurred? ...............................................
A group health plan, or health insurance issuer offering group health
insurance coverage, must not rescind coverage with respect to an individual
(including a group to which the individual belongs, or family coverage
in which the individual is included) once the individual is covered under
the plan or coverage, unless the individual (or a person seeking coverage
on behalf of the individual) performs an act, practice, or omission that
constitutes fraud, or makes an intentional misrepresentation of material fact,
as prohibited by the terms of the plan or coverage. See 29 CFR 2590.715-
2712(a)(1).
Tip: Some employers’ human resource departments may reconcile lists of
eligible individuals with their plan or issuer via data feed only once per month.
If a plan covers only active employees (subject to the COBRA continuation
coverage provisions) and an employee pays no premiums for coverage after
termination of employment, the Departments do not consider the retroactive
elimination of coverage back to the date of termination of employment, due
to delay in administrative record-keeping, to be a rescission. Similarly, if a
plan does not cover ex-spouses (subject to the COBRA continuation coverage
provisions) and the plan is not notied of a divorce and the full COBRA premium
is not paid by the employee or ex-spouse for coverage, the Departments do
not consider a plan’s termination of coverage retroactive to the divorce to be
a rescission of coverage. (Of course, in such situations COBRA may require
coverage to be offered for up to 36 months if the COBRA applicable premium is
paid by the qualied beneciary.) See DOL FAQs About the Affordable Care Act
Implementation Part II, question 7 at dol.gov/ebsa/faqs/faq-aca2.html.
YES
NO N/A
u
108

YES
NO N/A
Section D. Determining Compliance with the Affordable Care Act
Prohibitions on Lifetime Limits and Restrictions on Annual Limits in Part 7
of ERISA
Note: This provision is applicable for plan years beginning on or after Sept. 23,
2010. This provision applies to both grandfathered and non-grandfathered group
health plans.
The restrictions on annual limits do not apply to health exible spending
arrangements (FSAs), medical savings accounts (MSAs), or health savings
accounts (HSAs). In the case of health reimbursement accounts (HRAs) that
are integrated with other group health plan coverage which complies with the
prohibitions on lifetime and annual limits, the fact that benets under the HRA
by itself are limited does not violate these rules. Stand-alone HRAs limited to
retirees only are not subject to these rules. (For more information about the
application of the market reforms and other provisions of the Affordable Care Act
to HRAs, health FSAs, and certain other employer healthcare arrangements, see
Technical Release 2013-03, available at dol.gov/ebsa/newsroom/tr13-03.html.
1. Lifetime Limits
If the answer to the question below is “yes” the plan is in compliance with
the rules regarding prohibitions on lifetime limits.
Question 59 – Does the plan comply with the Affordable Care Act’s
prohibition on lifetime limits?................................................................................
A group health plan or issuer may not establish any lifetime limit on the
dollar amount of benets for any individual. This prohibition applies for
plan years beginning on or after September 23, 2010. See 29 CFR 2590.715-
2711(a)(1).
Tip: These rules do not prevent a plan or issuer from placing lifetime dollar
limits with respect to any individual on specic covered benets that are not
essential health benets (to the extent this is permissible under applicable Federal
and State law). See 29 CFR 2590.715-2711(b)(1).
Note: “Essential health benets” refers to essential benets under Section
1302(b) of the Affordable Care Act and applicable regulations (issued by HHS)
including the Frequently Asked Question on Essential Health Benets Bulletin.
For plan years beginning before the issuance of regulations dening “essential
health benets,” for purposes of enforcement, the Departments will take into
account good faith efforts to comply with a reasonable interpretation of the term
“essential health benets.” For this purpose, a plan or issuer must apply the
denition of essential health benets consistently. See Preamble to Interim
Final Regulations, at 75 FR 37188, 37191.
u
109

YES
NO N/A
2. Annual Limits
If the answer to the question below is “yes” the plan is in compliance with
the rules regarding prohibitions/restrictions on annual limits.
Question 60 – Does the plan comply with the Affordable Care Act’s
prohibition on annual limits?.................................................................................
For plan years beginning on or after January 1, 2014, a plan may not establish,
for any individual, an annual limit on the dollar amount of benets that are
essential health benets.
Tip: These rules do not prevent a plan or issuer from placing annual dollar limits
with respect to any individual on specic covered benets that are not essential
health benets (to the extent this is permissible under applicable Federal and
State law). See 29 CFR 2590.715-2711(b)(1).
Section E. Determining Compliance with the Affordable Care Act
Prohibition on Preexisting Condition Exclusions
This provision applies to both grandfathered and non-grandfathered group health
plans.
The denition of preexisting condition exclusion includes any limitation
or exclusion of benets (including a denial of coverage) applicable to an
individual as a result of information relating to an individual’s health status
before the individual’s effective date of coverage (or if coverage is denied, the
date of denial), such as a condition identied as a result of a pre-enrollment
questionnaire or a physical examination given to the individual, or a review of
medical records relating to the pre-enrollment period. See 29 CFR 2590.701-2.
If the answer to the following question is “yes” the plan is in compliance
with the prohibition on preexisting condition exclusions.
Question 61 – Does the plan comply with the Affordable Care Act by not
imposing a preexisting condition exclusion? .......................................................
For plan years beginning on or after January 1, 2014, group health plans may
not impose any preexisting condition exclusions. See 29 CFR 2590.715-
2704(a)(1).
Tip: Some preexisting condition exclusions are clearly designated as such in
the plan documents. Others are not. Check for hidden preexisting condition
exclusion provisions. A hidden preexisting condition exclusion is not designated
as a preexisting condition exclusion, but restricts benets based on when a
condition arose in relation to the effective date of coverage.
u
110

YES
NO N/A
Example: A plan excludes coverage for cosmetic surgery unless the surgery
is required by reason of an accidental injury occurring after the effective date
of coverage. This plan provision operates as a preexisting condition exclusion
because only people who were injured while covered under the plan receive
benets for treatment. People who were injured while they had no coverage (or
while they had prior coverage) do not receive benets for treatment. Accordingly,
this plan provision limits benets relating to a condition because the condition
was present before the effective date of coverage, and is considered a preexisting
condition exclusion.
SECTION F- Compliance with the 90-day Waiting Period Limitation
Provision
Use the following questions to help determine whether the group health plan
complies with the Departments’ 90-day waiting period limitation regulations.
See nal regulations issued by the Departments on February 24, 2014 at 29 CFR
2590.715-2708.
Note: PHS Act section 2708, as added by the Affordable Care Act and
incorporated into section 715 of ERISA, prohibits the application of any waiting
period that exceeds 90 days. Plans are not required to have a waiting period, and
the provision does not require plan sponsors to offer coverage to any particular
employee or class of employees. This provision applies to grandfathered health
plans and non-grandfathered plans.
Question 62- Does the plan apply a waiting period that exceeds 90-days? .......
A waiting period is dened as the period that must pass before coverage for
an individual who is otherwise eligible to enroll under the terms of a group
health plan can become effective. See ERISA section 701(b)(4); 29 CFR
2590.715-2708(b)
Being eligible for coverage under the terms of the plan generally means
having met the plan’s substantive eligibility conditions (such as, for example,
being in an eligible job classication, achieving job-related licensure
requirements specied in the plan’s terms, or satisfying a reasonable
and bona de employment-based orientation period). See 29 CFR 2590-
715.2708(c)(1).
Variable Hour Employees:
If a plan conditions eligibility on an employee regularly having a specied
number of hours of service per period (or working full-time), and it cannot be
determined that a newly hired employee is reasonably expected to regularly
work that number of hours per period (or work full-time), the plan may
take a reasonable period of time, not to exceed 12 months and beginning
on any date between the employee’s start date and the rst day of the rst
calendar month following the employee’s start date, to determine whether
the employee meets the plan’s eligibility condition. See 29 CFR 2590.715-
2708(c)(3)(i).
111
u
u
u

YES
NO N/A
Tip: Except in cases in which a waiting period that exceeds 90 days is imposed
in addition to a measurement period, the time period for determining whether
an employee meets the plan’s eligibility condition will not be considered to be
designed to avoid compliance with the 90-day waiting period limitation if the
coverage is made effective no later than 13 months from the employee’s start
date, plus any time remaining until the rst day of the next calendar month.
Cumulative Hours of Service Requirements:
If a plan conditions eligibility on an employee having completed a number of
cumulative hours of service, the eligibility condition is not considered to be
designed to avoid compliance with the 90-day waiting period limitation if the
cumulative hours-of-service requirement does not exceed 1,200 hours. The
plan’s waiting period must begin once the new employee satises the plan’s
cumulative hours-of-service requirement. See 29 CFR 2590.715-2708(c)(3)
(ii).
Limitation on Orientation Periods
To the extent that an orientation period is not used as a subterfuge for the
passage of time, or designed to avoid compliance with the 90-day waiting period
limitation, an orientation period is permitted only if it does not exceed one
month. One month is determined by adding one calendar month and subtracting
one calendar day, measured from an employee’s start date in a position that is
otherwise eligible for coverage. See 29 CFR 2590.715-2708 (c)(3)(iii).
Tip: It is not permissible under the 90-day rule to delay coverage until the rst
day of the month following completion of a 90-day waiting period. See 29 CFR
2590.715-2708 (e).
If you answered “Yes” to the above question under Section F, the plan
violates PHS Act Section 2708.
Section G. Determining Compliance with the Affordable Care Act
Provisions Regarding the provision of the Summary of Benets and
Coverage (SBC) and Uniform Glossary
Note: These provisions do apply to grandfathered health plans.
The Affordable Care Act provides for new disclosure tools, the Summary of
Benets and Coverage (SBC) and Uniform Glossary, to help consumers better
compare coverage options available to them in both the individual and group
health insurance coverage markets. Generally, group health plans and health
insurance issuers are required to provide the SBC and Uniform Glossary free of
charge. The Departments published a nal rule setting forth the requirements for
who must provide and who is entitled to receive an SBC and Uniform
Glossary, when these documents must be provided, the content required in the
documents, and the form and manner of how the documents can be provided. In
addition, the Departments published a notice that sets forth the required template
for the SBC and Uniform Glossary documents along with instructions and sample
112
u

YES
NO N/A
language for completing the template. These documents are available on the EBSA
Website at: dol.gov/ebsa/healthreform/. The SBC and Uniform Glossary must
be provided in a culturally and linguistically appropriate manner. The rules for
determining whether a language other than English must be made available are the
same as the rules for Internal Claims and Appeals and External Review, discussed
in Section J of this compliance aid. HHS has made available translated versions of
the template and glossary in the potentially required languages at: cciio.cms.gov/
resources/other/index.html.
Transitional Relief Providing Flexibility and Emphasizing Good Faith
Progress Towards Compliance
The Department is working together with employers and issuers to assist them in
coming into compliance with these requirements. Specically, in the instructions
for completing the SBC, the Department stated that to the extent a plan’s terms
do not reasonably correspond to the template and instructions, the template
should be completed in a manner that is as consistent with the instructions as
reasonably as possible, while still accurately reecting the plan’s terms. See
Instructions Guide for Group Coverage, page 1 General Instructions. In addition,
compliance assistance is a high priority for the Departments. Implementation
will be marked by an emphasis on assisting (rather than imposing penalties on)
plans and issuers that are working diligently and in good faith to understand and
come into compliance with the new law. During the rst year of applicability,
17
the Departments did not impose penalties on plans and issuers that were working
diligently and in good faith to comply. The Departments are extending the
previously-issued enforcement and transition relief until further guidance is issued.
The Departments will continue to work with stakeholders over time to achieve
maximum uniformity for consumers and certainty for the regulated community.
See ACA Implementation FAQ Part XIX, Q8.
The questions below focus on provision of the SBC by group health plans
to participants and beneciaries. The nal regulations also require health
insurance issuers to provide the SBC to group health plan sponsors and
participants and beneciaries. More information on these requirements can
be found at dol.gov/ebsa/healthreform.
The following questions have been developed to assist in determining
compliance with the rules regarding the Summary of Benets and Coverage
and Uniform Glossary.
17
The term “rst year of applicability” refers to SBCs and uniform glossaries provided with
respect to coverage beginning before January 1, 2014.
113
17
The term “rst year of applicability” refers to SBCs and uniform glossaries provided with
respect to coverage beginning before January 1, 2014.

YES
NO N/A
Question 63 – Does the plan provide an SBC, as required? ................................
In Connection with Enrollment
When providing the SBC to participants and beneciaries, group health
plans and issuers must provide the SBC with respect to each benet package
offered for which they are eligible (See 29 CFR 2590.715-2715(a)(1)(ii)
(A)) as part of any written application materials distributed by the plan or
issuer for enrollment. If no written application materials are distributed for
enrollment, the SBC must be provided no later than the rst date a participant
is eligible to enroll in coverage for themselves or any beneciaries. See
29 CFR 2590.715-2715(a)(1)(ii)(B). For this purpose, written application
materials include any forms or requests for information, in paper form or
through a Website or email, that must be completed for enrollment. See ACA
Implementation FAQ Part VIII, Q9.
Tips: The requirement to provide an SBC by both a health insurance issuer and a
group health plan to participants and beneciaries can be satised for both entities
as long as one entity provides the required SBC within the required timeframes.
See 29 CFR 2590.715-2715(a)(1)(iii)(A).
If a participant and any beneciaries are known to reside at the same address, a
single SBC provided to that address will satisfy the obligation to provide for all
individuals at the address. Under this circumstance, the obligation will also be
satised if the SBC is furnished to the participant in electronic form. However
if a beneciary’s last known address is different than the participant’s address, a
separate SBC must be mailed to the beneciary’s address. See 29 CFR 2590.715-
2715(a)(1)(iii)(B) and ACA Implementation FAQ Part VIII, Q10.
Group health plans are permitted to integrate the SBC with other summary
materials, such as the SPD, as long as the SBC is intact and prominently displayed
at the beginning of the materials (for example, immediately after the table of
contents in an SPD) and all of the timing requirements are met. See 77 FR 8707.
The Departments generally allow electronic delivery of the SBC and Uniform
Glossary where appropriate. For participants and beneciaries who are already
enrolled in coverage under a group health plan, an SBC may be provided
electronically if the requirements of the Department of Labor’s electronic
safe harbor are met. See ACA Implementation FAQ Part VIII, Q10 citing the
Department of Labor’s disclosure regulation at 29 CFR 2520.104b-1. For
participants and beneciaries who are eligible but not enrolled for coverage, the
SBC may be provided electronically if the format is readily accessible; the SBC
is provided in paper form upon request; and if the electronic form is an Internet
posting, the plan or issuer timely noties the individual that the documents are
available in paper form upon request. See 29 CFR 2590.715-2715(a)(3). An SBC
may be provided electronically to participants and beneciaries in connection
with their online enrollment or online renewal of coverage under the plan. SBCs
114

u
u
YES
NO N/A
may also be provided electronically to participants and beneciaries who request
an SBC online. In either instance, a paper copy must be provided upon request.
See ACA Implementation FAQ Part IX, Q1.
Question 64 – Does the plan make available the Uniform Glossary, as
required? .................................................................................................................
The Uniform Glossary includes statutorily required terms, as well as multiple
additional terms recommended by the NAIC. The Uniform Glossary is
available on the DOL Website at dol.gov/ebsa/healthreform/. The Uniform
Glossary may not be modied by plans or issuers. See 29 CFR 2590.715-
2715(c)(3); 77 FR 8708.
The nal rule requires group health plans and issuers to make the Uniform
Glossary available upon request, in either paper or electronic form (as
requested), within seven business days. See 29 CFR 2590.715-2715(c)(4).
This requirement may be satised by providing an internet address where an
individual may review and obtain the Uniform Glossary as well as a contact
phone number to obtain a paper copy of the Uniform Glossary. See 29 CFR
2590.715-2715(a)(2)(i)(L).
Section H. Determining Compliance with the Patient Protection Provisions
of the Affordable Care Act in Part 7 of ERISA
Note: This provision is applicable for plan years beginning on or after Sept. 23,
2010. This provision does not apply to grandfathered health plans.
1. Choice of Healthcare Professional
A plan or issuer that requires or provides for a participant or beneciary to
designate a participating primary care provider must permit each participant or
beneciary to designate any participating primary care provider who is available
to accept the participant or beneciary. With respect to a child, the plan or
issuer must permit the designation of a physician who specializes in pediatrics
as a child’s primary care provider, if the provider participates in the network of
the plan or issuer and is available to accept the child. See 29 CFR 2590.715-
2719A(a)(1) & (a)(2).
A group health plan or issuer that provides obstetrical or gynecological (OB/
GYN) care and requires the designation of an in-network primary care provider,
may not require authorization or referral by the plan, issuer, or any person
(including a primary care provider) for a female participant or beneciary
who seeks coverage for OB/GYN care provided by a participating health care
professional who specializes in obstetrics and gynecology. (This includes any
individual authorized under State law to provide OB/GYN care, including a
person other than a physician). See 29 CFR 2590.715-2719A(a)(3).
115
If you are completing this section as part of a review of a grandfathered health plan, STOP here. The
following sections address provisions that do not apply to grandfathered health plans.
YES
NO N/A
Question 65 – Does the plan require or provide for designation
of a participating primary care provider by any participant or
beneciary?.................................................................................................................
If the answer is ‘no’, enter ‘N/A’ for the following questions and proceed to
Question 72.
If the answer to ALL of the questions below is “yes” the plan is in
compliance with the choice of healthcare professional provisions of the rules
regarding patient protections.
Question 66 – Does the plan permit each participant or beneciary to
designate any participating primary care provider who is available to accept
the participant or beneciary? .............................................................................
If a group health plan, or a health insurance issuer offering group health
insurance coverage, requires or provides for designation by a participant or
beneciary of a participating primary care provider, then the plan or issuer
must permit each participant or beneciary to designate any participating
primary care provider who is available to accept the participant or
beneciary. See 29 CFR 2590.715-2719A(a)(1)(i).
Question 67 – Does the plan provide a notice informing each participant of
the terms of the plan or health insurance coverage regarding designation of
a primary care provider? .....................................................................................
If a group health plan or health insurance issuer requires the designation by a
participant or beneciary of a primary care provider, the plan or issuer must
provide a notice informing each participant of the terms of the plan or health
insurance coverage regarding designation of a primary care provider that any
participating primary care provider who is available to accept the participant
or beneciary can be designated. See 29 CFR 2590.715-2719A(a)(4)(i)(A).
Tip: This notice must be provided any time the plan provides a participant with
an SPD or other similar description of benets under the plan. See 29 CFR
2590.715-2719A(a)(4)(ii).
Question 68 – With respect to a child, does the plan permit the participant
or beneciary to designate a physician who specializes in pediatrics as the
child’s primary care provider if the provider participates in the network of
the plan or issuer and is available to accept the child? .....................................
If a group health plan, or a health insurance issuer offering group health
insurance coverage, requires or provides for the designation of a participating
primary care provider for a child by a participant or beneciary, the plan or
issuer must permit the participant or beneciary to designate a physician
(allopathic or osteopathic) who specializes in pediatrics as the child’s primary
care provider if the provider participates in the network of the plan or issuer
and is available to accept the child. See 29 CFR 2590.715-2719A(a)(2)(i).
u
u
u
116

YES
NO N/A
Question 69 – With respect to a child, does the plan provide a notice
informing each participant of the terms of the plan or health insurance
coverage regarding designation of a primary care provider and the right to
designate any participating physician who specializes in pediatrics as the
primary care provider? .........................................................................................
If a group health plan or health insurance issuer requires the designation
by a participant or beneciary of a primary care provider, the plan or issuer
must provide a notice informing each participant of the terms of the plan or
health insurance coverage regarding designation of a primary care provider
with respect to a child, that any participating physician who specializes
in pediatrics can be designated as the primary care provider. See 29 CFR
2590.715-2719A(a)(4)(i)(B).
Tip: This notice must be provided any time the plan provides a participant with
an SPD or other similar description of benets under the plan. See 29 CFR
2590.715-2719A(a)(4)(ii).
Question 70 – Does the plan provide coverage for OB/GYN care provided
by a participating health care professional who specializes in obstetrics
or gynecology for a female participant or beneciary without requiring
authorization or referral by the plan, issuer, or any person (including a
primary care provider)? ........................................................................................
For purposes of this provision, a health care professional who specializes in
obstetrics or gynecology is any individual (including a person other than a
physician) who is authorized under applicable State law to provide obstetrical
or gynecological care. The plan or issuer may require such a professional to
agree to otherwise adhere to the plan’s or issuer’s policies and procedures,
including procedures regarding referrals and obtaining prior authorization
and providing services pursuant to a treatment plan (if any) approved by the
plan or issuer. See 29 CFR 2590.715-2719A(a)(3)(i)(A).
A plan or issuer must treat the provision of OB/GYN care, and the ordering
of related OB/ GYN items and services, by a participating health care
professional who specializes in obstetrics or gynecology as the authorization
of the primary care provider. See 29 CFR 2590.715-2719A(a)(3)(i)(B).
Question 71 – Does the plan provide a notice informing each participant of
the terms of the plan or coverage regarding designation of a primary care
provider and that the plan may not require authorization or referral for
obstetrical or gynecological care by a participating health care professional
who specializes in obstetrics or gynecology? .......................................................
If a group health plan or health insurance issuer requires the designation by a
participant or beneciary of a primary care provider, the plan or issuer must
provide a notice informing each participant of the terms of the plan or health
insurance coverage regarding designation of a primary care provider that the
plan may not require authorization or referral for obstetrical or gynecological
u
u
u
117
u

YES
NO N/A
care by a participating health care professional who specializes in obstetrics
or gynecology. See 29 CFR 2590.715-2719A(a)(4)(i)(C).
Tip: This notice must be provided anytime the plan provides a participant with
an SPD or other similar description of benets under the plan. See 29 CFR
2590.715-2719A(a)(4)(ii).
2. Coverage of Emergency Services
Question 72 – Does the plan provide any benets with respect to services in
an emergency department of a hospital? .............................................................
If the answer is ‘no,’ enter ‘N/A’ for the following questions and proceed to
Section I.
Note: Small group insured plans are required to cover essential health benets,
which include emergency services.
If the answer to ALL of the questions below is “yes” the plan is in
compliance with the coverage of emergency services provisions of the rules
regarding patient protections.
Question 73 – Does the plan provide coverage of emergency services without
the need for any prior authorization determination, even if the emergency
services are provided on an out-of-network basis?.............................................
A plan or issuer subject to the requirements of this section must provide
coverage for emergency services without the need for any prior authorization
determination, even if the emergency services are provided on an out-of-
network basis. See 29 CFR 2590.715-2719A(b)(2)(i).
Question 74 – Does the plan provide coverage of emergency services
without regard to whether the health care provider furnishing the
emergency services is a participating network provider with respect to the
services?.......................................................................................................................
A plan or issuer subject to the requirements of this section must provide
coverage for emergency services without regard to whether the health
care provider furnishing the emergency services is a participating network
provider with respect to the services. See 29 CFR 2590.715-2719A(b)(2)(ii).
Question 75 – Does the plan provide coverage of emergency services
provided out-of-network without imposing any administrative requirement
or limitation on coverage that is more restrictive than the requirements that
apply to emergency services provided in-network? ............................................
If the emergency services are provided out-of-network, the plan must provide
the emergency services without imposing any administrative requirement
or limitation on coverage that is more restrictive than the requirements
u
u
u
118

YES
NO N/A
or limitations that apply to emergency services received from in-network
providers. See 29 CFR 2590.715-2719A(b)(2)(iii).
Question 76 – When providing emergency services out-of-network, does the
plan impose cost-sharing requirements that comply with the requirements of
the interim nal regulations? ................................................................................
Any cost-sharing requirement expressed as a copayment amount or
coinsurance rate imposed with respect to a participant or beneciary for out-
of-network emergency services cannot exceed the cost-sharing requirement
imposed with respect to a participant or beneciary if the services were
provided in-network. However, a participant or beneciary may be required
to pay, in addition to the in-network cost sharing, the excess of the amount
the out-of-network provider charges over the amount the plan or issuer is
required to pay under this section. See 29 CFR 2590.715-2719A(b)(3)(i).
A plan or issuer complies with the requirements if it provides benets with
respect to an emergency service in an amount equal to the greatest of the
following three amounts (which are adjusted for in-network cost-sharing
requirements):
(A) The amount negotiated with in-network providers for the emergency
service furnished, excluding any in-network copayment or coinsurance
imposed. (See 29 CFR 2590.715-2719A(b)(3)(i)(A) for more detailed
information, including how to determine this amount if there is more
than one amount negotiated with in-network providers for the emergency
service.)
(B) The amount for the emergency service calculated using the same
method the plan generally uses to determine payments for out-of-
network services (such as the usual, customary, and reasonable amount),
excluding any in-network copayment or coinsurance imposed. See 29
CFR 2590.715-2719A(b)(3)(i)(B).
(C) The amount that would be paid under Medicare for the emergency
service, excluding any in-network copayment or coinsurance imposed.
See 29 CFR 2590.715-2719A(b)(3)(i)(C).
Tip: Any other cost-sharing requirement, such as a deductible or out-of-pocket
maximum, may be imposed with respect to out-of-network emergency services
only if the cost-sharing requirement generally applies to out-of-network benets.
See 29 CFR 2590.715-2719A(b)(3)(ii).
u
119
u

YES
NO N/A
Question 77 – Does the plan provide coverage of emergency services without
regard to any other term or condition of the coverage, other than the
exclusion or coordination of benets, a permissible afliation or waiting
period, or applicable cost-sharing requirements? ..............................................
A plan or issuer subject to the requirements of this section must provide
coverage for emergency services without regard to any other term or
condition of the coverage, other than the exclusion or coordination of
benets, an afliation or waiting period permitted under part 7 of ERISA,
part A of title XXVII of the PHS Act, or chapter 100 of the Internal Revenue
Code, or applicable cost sharing. See 29 CFR 2590.715-2719A(b)(2)(v).
Section I. Determining Compliance with the Affordable Care Act Coverage
of Preventive Services Provisions in Part 7 of ERISA
Note: This provision is applicable for plan years beginning on or after Sept. 23,
2010. This provision does not apply to grandfathered health plans.
Group health plans and health insurance issuers must provide coverage for, and
must not impose cost-sharing requirements with respect to, certain recommended
preventive services. Nothing prevents plans or issuers from providing coverage
for preventive items and services in addition to the recommended preventive
services required under these regulations. See 29 CFR 2590.715-2713(a)(1) & (a)
(5).
A complete list of recommendations and guidelines that include services that
are required to be covered under these interim nal regulations can be found
at HealthCare.gov/center/regulations/prevention.html. Any changes to or new
recommendations and guidelines will be noted at this site. Plans must cover any
new recommended service within one year after the date the recommendation or
guidance is issued. Therefore, by visiting the site once per year, plans and issuers
will have straightforward access to all the information necessary to determine any
additional items and services that must be covered without cost-sharing and any
items or services that are no longer required to be covered.
If the answer to ALL of the questions below is “yes” the plan is in
compliance with the rules regarding preventive services.
Question 78 – Does the plan provide coverage without imposing any cost-
sharing requirements for evidence-based items or services that have in effect
a rating of A or B in the current recommendations of the United States
Preventive Services Task Force? ...........................................................................
Plans and issuers must provide coverage for evidence-based items or services
that have in effect a rating of A or B in the current recommendations of the
United States Preventive Services Task Force. See 29 CFR 2590.715-2713(a)
(1)(i).
u
u
120

u
YES
NO N/A
Note: Recommendations of the United States Preventive Services Task Force
regarding breast cancer screening, mammography, and prevention issued in or
around November 2009 are not considered to be current.
Question 79 – Does the plan provide coverage without imposing any
cost-sharing requirements for immunizations for routine use in children,
adolescents, and adults that have in effect a recommendation from the
Advisory Committee on Immunization Practices of the Centers for Disease
Control and Prevention?.........................................................................................
For the purpose of this section, a recommendation from the Advisory
Committee on Immunization Practices of the Centers for Disease Control and
Prevention is considered in effect after it has been adopted by the Director
of the Centers for Disease Control and Prevention, and a recommendation is
considered to be for routine use if it is listed on the Immunization Schedules
of the Centers for Disease Control and Prevention. See 29 CFR 2590.715-
2713(a)(1)(ii).
Question 80 – With respect to infants, children, and adolescents, does the
plan provide coverage without imposing any cost-sharing requirements
for evidence-informed preventive care and screenings provided for in
comprehensive guidelines supported by the Health Resources and Services
Administration?..........................................................................................................
With respect to infants, children, and adolescents, a plan or issuer must
provide coverage for evidence-informed preventive care and screenings
provided for in comprehensive guidelines supported by the Health Resources
and Services Administration. See 29 CFR 2590.715-2713(a)(1)(iii).
Question 81 – With respect to women, does the plan provide coverage
without imposing any cost-sharing requirements for evidence-informed
preventive care and screenings provided for in comprehensive guidelines
supported by the Health Resources and Services Administration? ..................
A complete list of guidelines that are required to be covered can be found at:
hrsa.gov/womensguidelines/. (Note: there is a limited exception for certain
employers regarding coverage for certain women’s preventive services; see
dol.gov/ebsa/healthreform for updated guidance).
With respect to women, a plan or issuer must provide coverage for evidence-
informed preventive care and screenings provided for in comprehensive
guidelines supported by the Health Resources and Services Administration.
See 29 CFR 2590.715-2713(a)(1)(iv).
u
u
121
u

YES
NO N/A
Question 82 – Does the plan provide coverage for ofce visits without
imposing cost sharing requirements when recommended preventive services
are not billed separately from an ofce visit and is the primary purpose of
the ofce visit? ........................................................................................................
If a recommended preventive service or item is not billed separately (or is not
tracked as individual encounter data separately) from an ofce visit and the
primary purpose of the ofce visit is the delivery of such a service or item,
then a plan or issuer may not impose cost-sharing requirements with respect
to the ofce visit. See 29 CFR 2590.715-2713(a)(2)(ii).
Tip: If a recommended preventive service is billed separately from an ofce
visit, or if the recommended preventive service is not billed separately and the
primary purpose of the ofce visit is not delivery of the recommended preventive
service, then a plan or issuer may impose cost-sharing with respect to the ofce
visit. See 29 CFR 2590.715-2713(a)(2)(i) & (iii).
Additional tips:
Plans and issuers that have a network of providers are not required to provide
coverage for and may impose cost-sharing requirements for recommended
preventive services delivered by an out-of-network provider. See 29 CFR
2590.715-2713(a)(3).
Plans and issuers may use reasonable medical management techniques
to determine the frequency, method, treatment, or setting for the
recommended preventive services to the extent these are not specied in the
recommendations or guidelines. See 29 CFR 2590.715-2713(a)(4).
Plans and issuers can impose cost-sharing for a treatment that is not a
recommended preventive service under these regulations, even if the
treatment resulted from a recommended preventive service. See 29 CFR
2590.715-2713(a)(5) and ACA Implementation FAQs Part XII Q5.
Section J. Determining Compliance with the Affordable Care Act Provisions
Regarding Internal Claims and Appeals and External Review in Part 7 of
ERISA
The internal claims and appeals and external review provisions of Part 7 of
ERISA do not apply to grandfathered health plans.
Note: There have been several phases of guidance issued regarding the internal
claims and appeals and external review provisions under the Affordable Care
Act. More information about the requirements regarding internal claims and
appeals and external review processes under ERISA is available at dol.gov/ebsa.
u
122
u
u
u

u
YES
NO N/A
1. Internal Claims and Appeals
Under the Affordable Care Act group health plans and health insurance issuers
offering group health insurance coverage were required to implement an
effective internal claims and appeals process for plan years beginning on or after
September 23, 2010. In general, the interim nal regulations require plans and
issuers to comply with the DOL claims procedure rule under 29 CFR 2560.503-
1 and impose specic additional requirements and include some clarications
(referred to as the “additional standards” for internal claims and appeals). In
addition to meeting the following requirements, the plan is required to comply
with all of the requirements of the DOL claims procedure rule under 29 CFR
2560.503-1.
The following questions have been developed to assist in determining
compliance with the additional standards for internal claims and appeals
processes and is not intended to determine compliance with the DOL claims
procedure rule.
Question 83 – Does the plan provide internal claims and appeals processes
with respect to rescissions of coverage? ...............................................................
Under the DOL claims procedure rule, adverse benet determinations
eligible for internal claims and appeals processes generally include denial,
reduction, or termination of, or a failure to provide or make a payment (in
whole or in part) for a benet (including a denial, reduction, termination, or
failure to make a payment based on the imposition of a preexisting condition
exclusion, a source of injury exclusion, or other limitation on covered
benets). See 29 CFR 2560.503-1(m)(4).
The Department’s regulations broaden the DOL claims procedure rule’s
denition of “adverse benet determination” to include rescissions of
coverage. Therefore, rescissions of coverage are also eligible for internal
claims and appeals processes, whether or not the rescission has an adverse
effect on any particular benet at the time of an appeal. See 29 CFR
2590.715-2719(a)(2)(i); 29 CFR 2560.503-1.
This provision is applicable for plan years beginning on or after September
23, 2010. See 29 CFR 2590.715-2719(g).
Question 84 – Does the plan provide claimants with any new or additional
evidence or rationale considered in connection with a claim? ...........................
The Department’s regulations clarify that plans or issuers must provide
to claimants, free of charge, any new or additional evidence considered,
relied upon, or generated by (or at the direction of) the plan or issuer in
connection with a claim. This evidence must be provided as soon as possible
and sufciently in advance of the date on which the notice of nal internal
u
u
u
123

YES
NO N/A
adverse benet determination is required to be provided in order to give the
claimant a reasonable opportunity to respond prior to that date. Similarly,
before a plan or issuer can issue a nal internal adverse benet determination
based on a new or additional rationale, the claimant must be provided, free
of charge, with the rationale. This rationale must be provided as soon as
possible and sufciently in advance of the date on which the notice of nal
internal adverse benet determination is required to be provided in order to
give the claimant a reasonable opportunity to respond prior to that date. See
29 CFR 2590.715-2719(b)(2)(ii)(C).
This provision is applicable for plan years beginning on or after September
23, 2010. See 29 CFR 2590.715-2719(g).
Question 85 – Does the plan ensure that claims and appeals are adjudicated
in a manner that maintains independence and impartiality of decision
making? ...................................................................................................................
The Department’s regulations clarify that plans or issuers must ensure
that all claims and appeals are adjudicated in a manner designed to ensure
the independence and impartiality of the persons involved in making the
decision. Accordingly, decisions regarding hiring, compensation, termination,
promotion, or other similar matters with respect to any individual (such as
a claims adjudicator or medical expert) must not be made based upon the
likelihood or perceived likelihood that the individual will support or tend to
support a denial of benets. See 29 CFR 2590.715-2719(b)(2)(ii)(D).
This provision is applicable for plan years beginning on or after September
23, 2010. See 29 CFR 2590.715-2719(g).
Question 86 – Complete the following questions to ensure that the plan
complies with the additional content requirements for any notice of adverse
benet determination or nal internal adverse benet determination:
86a. Does the plan or issuer ensure that any notice of adverse benet
determination or nal internal adverse benet determination includes
information sufcient to identify the claim involved? .......................................
The Department’s regulations provide that plans and issuers must ensure that
any notice of adverse benet determination or nal internal adverse benet
determination includes information sufcient to identify the claim involved
including the date of service, the health care provider, and the claim amount
(if applicable), and a statement describing the availability, upon request, of
the diagnosis code and its corresponding meaning, and the treatment code,
and its corresponding meaning. See 29 CFR 2590.715-2719(b)(2)(ii)(E)(1).
This provision is applicable for plan years beginning on or after July 1, 2011.
See T.R. 2011-01 at dol.gov/ebsa/newsroom/tr11-01.html.
u
u
u
u
124

YES
NO N/A
Plans or issuers must also provide to participants and beneciaries, as soon
as practicable, upon request, the diagnosis and treatment codes (and their
meanings), associated with any adverse benet determination or nal internal
adverse benet determination. The plan or issuer must not consider a request
for such diagnosis and treatment information, in itself, to be a request for an
internal appeal or external review. See 29 CFR 2590.715-2719(b)(2)(ii)(E)
(1), as amended. This provision is applicable for plan years beginning on or
after January 1, 2012. See T.R. 2011-01 at dol.gov/ebsa/newsroom/tr11-01.
html.
86b. Does the plan or issuer ensure that any notice of adverse benet
determination or nal internal adverse benet determination includes an
adequate description of the reasons for the adverse benet determination or
nal internal adverse benet determination? ......................................................
The Department’s regulations provide that plans and issuers must ensure
that the reasons for the adverse benet determination or nal internal
adverse benet determination includes the denial code and its corresponding
meaning, as well as a description of the standard that was used in denying the
claim. In the case of a notice of nal internal adverse benet determination,
this description must include a discussion of the decision. See 29 CFR
2590.715-2719(b)(2)(ii)(E)(3).
This provision is applicable for plan years beginning on or after July 1, 2011.
See T.R. 2011-01 at dol.gov/ebsa/newsroom/tr11-01.html.
86c. Does the plan or issuer ensure that any notice of adverse benet
determination or nal internal adverse benet determination includes
a description of available internal appeals and external review
processes?....................................................................................................................
The Department’s regulations provide that plans and issuers must provide
a description of available internal appeals and external review processes,
including information regarding how to initiate an appeal. See 29 CFR
2590.715-2719(b)(2)(ii)(E)(4).
This provision is applicable for plan years beginning on or after July 1, 2011.
See T.R. 2011-01 at dol.gov/ebsa/newsroom/tr11-01.html.
86d. Does the plan or issuer ensure that any notice of adverse benet
determination or nal internal adverse benet determination disclose the
availability of, and contact information for, any applicable ofce of health
insurance consumer assistance or ombudsman established under PHS Act
section 2793?............................................................................................................
The Department’s regulations provide that plans and issuers must disclose
the availability of, and contact information for, any applicable ofce of
health insurance consumer assistance or ombudsman established under PHS
Act section 2793 to assist enrollees with the internal claims and appeals and
external review processes. See 29 CFR 2590.715-2719(b)(2)(ii)(E)(5).
u
u
u
u
u
u
125

YES
NO N/A
An updated list of the State Consumer Assistance Programs is available on the
Department of Labor Website at dol.gov/ebsa/capupdatelist.doc.
These provisions are applicable for plan years beginning on or after July 1,
2011. See T.R. 2011-01 at dol.gov/ebsa/newsroom/tr11-01.html.
Question 87 – Does the plan defer to the attending provider as to whether
a claim involves urgent care and provide notice regarding such urgent care
claim as required?....................................................................................................
As under 29 CFR 2560.503-1(f)(2)(i), plans or issuers must notify a claimant
of a benet determination (whether adverse or not) with respect to a claim
involving urgent care as soon as possible, taking into account the medical
exigencies, but not later than 72 hours after the receipt of the claim by the plan
or issuer. 29 CFR 2590.715-2719(b)(2)(ii)(B), as amended.
The determination as to whether a claim involves urgent care is determined by
the attending provider and the plan or issuer must defer to such determination.
See 29 CFR 2590.715-2719(b)(2)(ii)(B), as amended.
This provision is applicable for plan years beginning on or after January 1,
2012. See T.R. 2011-01 at dol.gov/ebsa/newsroom/tr11-01.html.
Question 88 – Does the plan comply with the requirements regarding deemed
exhaustion of internal claims and appeals processes? ..........................................
In the case of a plan or issuer that fails to adhere to all the requirements of
the Interim Final Rules relating to the Internal Claims and Appeals process
with respect to a claim, the claimant is deemed to have exhausted the internal
claims and appeals process. The internal claims and appeals process will
not be deemed exhausted as long as the violation was: de minimus, does not
cause, and is not likely to cause, prejudice or harm to the claimant, attributable
to good cause or due to matters beyond the control of the plan or issuer, in
the context of an ongoing, good faith exchange of information between the
plan and the claimant, and is not reective of a pattern or practice of non-
compliance. See 29 CFR 2590.715-2719(b)(2)(ii)(F), as amended.
In the event that the claimant requests a written explanation of the violation,
the plan or issuer must provide such explanation within 10 days, including a
specic description of its bases, if any, for asserting that the violation should
not cause the internal claims and appeals process to be deemed exhausted. See
29 CFR 2590.715-2719(b)(2)(ii)(F), as amended.
In the case that the external review rejects the claimant’s immediate review,
the plan must provide the claimant notice of the opportunity to resubmit and
pursue the internal appeal of the claim. This notice must be sent within a
reasonable time after the external reviewer rejects the claim for immediate
review, not later than 10 days. See 29 CFR 2590.715-2719(b)(2)(ii)(F), as
amended.
u
u
u
u
126
u
u
u
u

v
v
v
YES
NO N/A
These provisions are applicable for plan years beginning on or after January
1, 2012. See T.R. 2011-01 at dol.gov/ebsa/newsroom/tr11-01.html.
Question 89 – Does the plan provide culturally and linguistically appropriate
notices in a county that meets the applicable threshold?....................................
The Department’s regulations provide that plans and issuers must provide
relevant notices in a culturally and linguistically appropriate manner.
The Department’s regulations establish a single threshold with respect to the
percentage of people who are literate only in the same non-English language
for both the group and individual markets. With respect to plans and issuers,
the threshold percentage is set at 10 percent or more of the population
residing in the claimant’s county, as determined based on American
Community Survey (ACS) data published by the United States Census
Bureau. The list of counties determined to meet the threshold is available at
cms.gov/CCIIO/Resources/Fact-Sheets-and-FAQs/Downloads/2013-clas-
data.pdf. This list will be updated annually. See 29 CFR 2590.715-2719(e)
(3), as amended.
If the answer to this question is “Yes,” proceed to question 90. If the answer
is “No,” proceed to the next section.
Question 90 – Does the plan provide notices in a culturally and linguistically
appropriate manner with respect to internal claims and appeals processes?
To meet this requirement the plan or issuer must:
include a one-sentence statement in the relevant non-English language
about the availability of language services on each notice sent to an
address in a county that meets the threshold;
provide, upon request, a notice in any applicable non-English language;
and
provide a customer assistance process (such as a telephone hotline)
with oral language services in the non-English language and provide
written notices in the non-English language upon request. See 29 CFR
2590.715-2719(e), as amended.
The translated statements are available at dol.gov/ebsa/IABDModelNotice2.
doc.
These provisions are applicable for plan years beginning on or after January 1,
2012. See T.R. 2011-01 at dol.gov/ebsa/newsroom/tr11-01.html.
127
u
u
u
u
u

YES
NO N/A
2. External Review
Plans and issuers must comply with either a State external review process or
the Federal external review process. The external review provisions of Part 7 of
ERISA do not apply to grandfathered health plans.
The following questions have been developed to assist in determining
compliance with the rules regarding the external review processes.
Question 91 – Is the plan subject to the requirements of a State external
review process or the HHS-Administered Federal External Review
Process? ...................................................................................................................
Non-grandfathered, self-insured group health plans subject to ERISA and the
Code:
Generally follow requirements of the private accredited IRO process
(established by TR 2010-01, modied by TR 2011-02).
Non-grandfathered, insured coverage:
Generally, issuers must follow the State process if the external review
process meets either the NAIC-Similar or NAIC-Parallel process as
determined by HHS.
However, issuers in States without a conforming State process and self-
insured non-federal governmental plans may either:
Utilize the private accredited IRO process (established by TR 2010-
01, and modied by TR 2011-02); or
Utilize the HHS-Administered Federal External Review Process.
Background information regarding external review processes for insured
plans:
For insured coverage, HHS has determined which State external review
processes meet the minimum requirements to apply to issuers in those States.
See cms.gov/CCIIO/Resources/Files/external_appeals.html.
If you answered “Yes” to Question 91 above, STOP. The plan is not subject
to the DOL Private Accredited IRO process. If you answered “No” to
Question 91 above, continue to Question 92.
u
u
v
v
−
128
v
−
u

u
YES
NO N/A
Question 92 – DOL Private Accredited IRO process: Does the plan provide
external review for the required scope of adverse benet determinations? .....
Under the Department’s regulations the scope of the Federal external review
process applies to:
An adverse benet determination, including a nal internal adverse benet
determination, by a plan or issuer that involves medical judgment, including
but not limited to those based on the plan’s or issuer’s requirements for
medical necessity, appropriateness, health care setting, level of care, or
effectiveness of a covered benet; or its determination that a treatment is
experimental or investigational; and
A rescission of coverage (regardless of whether or not the rescission has any
effect on any particular benet at that time). See 29 CFR 2590.715-2719(d)
(1)(ii), as amended.
An adverse benet determination that relates to a participant’s or
beneciary’s failure to meet the requirements for eligibility under the
terms of a group health plan (i.e., worker classication or similar issue) is
not within the scope of the Federal external review process. See 29 CFR
2590.715-2719(d)(1)(i), as amended.
Question 93 – DOL Private Accredited IRO process: Does the plan provide
an effective external review process? ...................................................................
Self-insured coverage subject to ERISA and the Code may either comply
with the standards of the private accredited IRO process or voluntarily
comply with a State external review process if the State allows access.
If the plan is complying with the private accredited IRO process, ensure the
plan complies with all of the standards articulated in TR 2011-02 including:
Providing effective written notice of external review
Providing limits related to ling fees
Providing claimant at least 4 months to le for external review
Requiring that IROs must be accredited
Requiring that IROs may not have conicts of interest that inuence
independence
Providing that IRO decisions are binding on the insurer and the claimant
Requiring IROs to maintain written records for at least three years
Department of Labor claried in TR 2011-02 that to be eligible for a safe
harbor from enforcement from the Department of Labor and the IRS (as
previously set forth in sub-regulatory guidance issued in ACA FAQs Part 1
on September 20, 2010), self-insured plans will be required to contract with
at least three IROs by July 1, 2012.
See TR 2010-01 at dol.gov/ebsa/pdf/ACATechnicalRelease2010-01.pdf, and TR-
2011-02 at dol.gov/ebsa/newsroom/tr11-02.html.
u
u
v
v
v
v
v
v
u
v
u
u
129
Appendix B:
Chart of Required Notices
131

For group health plans subject to Part 7 of ERISA, required disclosures include:
Type of Disclosure Applicability Content Summary Timing
The notice must disclose the availability of a
reasonable alternative standard (or possibility
of waiver of the otherwise applicable
standard).
Disclosure must include contact information
for obtaining the alternative standard and a
statement that recommendations of an
individual’s personal physician will be
accommodated.
For group health plans
offering a health
contingent wellness
program in order to
obtain a reward.
In all plan materials that describe the
terms of a health contingent wellness
program (both activity-only and
outcome-based wellness programs). If
the plan materials merely mention that
a program is available, without
describing its terms, this disclosure is
not required.
For outcome-based wellness programs,
this notice must also be included in any
disclosure that an individual did not
satisfy an initial outcome-based
standard.
At or before the time an employee is
initially offered the opportunity to enroll
in a group health plan.
A description of individuals’ special enrollment
rights.
All group health plans.
Description of rights
with respect to hospital
stays in connection with
childbirth
(§711(d); 29 CFR
2520.102-3(u))
Group health plans that
provide maternity or
newborn infant coverage.
The plan’s SPD must include a statement
describing any requirements under Federal or
State law applicable to the plan, and any health
insurance coverage offered under the plan,
relating to any hospital length of stay in
connection with childbirth for a mother or
newborn child. If the Federal law applies in
some areas in which the plan operates and State
law applies in other areas, the SPD should
describe the different areas and the Federal or
State requirements applicable in each.
In the SPD (or SMM).
Notice of special
enrollment rights
(29 CFR 2590.701-6(c))
Wellness program
disclosure
(§702; 29 CFR
2590.702(f)(2)(v))
132

Type of Disclosure Applicability Content Summary Timing
Upon enrollment in the plan.
A statement that for participants and
beneficiaries who are receiving mastectomy-
related benefits, coverage will be provided in
a manner determined in consultation with the
attending physician and the patient, for:
All stages of reconstruction of the breast
on which the mastectomy was performed;
Surgery and reconstruction of the other
breast to produce a symmetrical
appearance;
Prostheses; and
Treatment of physical complications of
the mastectomy, including lymphedema.
A description of any annual deductibles and
coinsurance limitations applicable to such
coverage.
Group health plans that
provide coverage for
mastectomy benefits.
WHCRA enrollment
notice
(§713(a))
A copy of the WHCRA enrollment notice, or
A simplified disclosure providing notice of
the availability of benefits for the four
required coverages and information on how
to obtain a detailed description.
Group health plans that
provide coverage for
mastectomy benefits.
WHCRA annual
notice
(§713(a))
Once each year after enrollment in the
plan.
Potential opportunities currently available in
the State in which the employee resides for
premium assistance under CHIP or Medicaid
for health coverage for the employee or the
employee’s dependents.
Information on how to contact the State in
which the employee resides for additional
information on premium assistance under
these programs.
Description of special enrollment opportunity
if eligible for premium assistance under these
programs.
Employers that maintain
a group health plan in a
state with a CHIP or
Medicaid program that
provides for premium
assistance for group
health plan coverage
must provide this notice
to all employees.
Employer Notice
regarding Premium
Assistance under
Medicaid or CHIP
(29 CFR
2590.701(f)(3)(B)(i))
* Note, the employer
(rather than the group
health plan or issuer) is
required to provide this
notice.
May be provided with enrollment
packets, open season materials, or the
Summary Plan Description.
133

Type of Disclosure Applicability Content Summary Timing
Must include a description of the Michelle’s
law provision for continued coverage during
medically necessary leaves of absence.
All group health plans
Michelle’s Law
Enrollment Notice
Notice must provide the criteria for medically
necessary determinations with respect to
mental health/substance use disorder benefits.
All group health plans
subject to MHPAEA
Mental Health Parity
and Addiction Equity
Act (MHPAEA)
Criteria for Medically
Necessary
Determination Notice
Notice must be provided to any
current or potential participant,
beneficiary, or contracting provider
upon request.
Notice must provide the reason for any denial
of reimbursement or payment for services
with respect to mental health/substance use
disorder benefits.
All group health plans
subject to MHPAEA
MHPAEA Claims
Denial Notice
Notice must be provided to
participants and beneficiaries upon
request or as otherwise required by
other laws.
Notice must be included with any
notice regarding a requirement for
certification of student status for
coverage under the plan.
Note: Under the Affordable Care Act,
plans cannot deny or restrict coverage
for a child under the age of 26 based
on student status.
A group health plan claiming MHPAEA’s
increased cost exemption must notify plan
participants and beneficiaries, the
Department of Labor, and the appropriate
State agencies of the plan’s exemption from
the parity requirements.
Group health plans
claiming a MHPAEA
cost exemption
MHPAEA Increased
Cost Exemption
Notice must be provided if using the
cost exemption.
Notice must disclose that the plan is
grandfathered and must include contact
information.
Group health plans
claiming grandfathered
status
1
Grandfathered Plan
Disclosure/Notice
Notice must be included in any plan
materials describing the benefits or
health coverage.
1
Under the Affordable Care Act, generally, grandfathered plans are plans that were in existence, and in which at least one individual was enrolled, on
March 23, 2010. Grandfathered health plans are exempt from many but not all Affordable Care Act market reforms. For further discussion, see the
Affordable Care Act section of this publication or visit dol.gov/ebsa.
134

Type of Disclosure Applicability Content Summary Timing
A template that describes the benefits and
coverage under the plan, and a uniform
glossary defining statutorily and NAIC
recommended terms.
The SBC must include an internet address
where an individual can review the Uniform
Glossary as well as contact information for
obtaining a paper copy.
The required SBC template is available at
dol.gov/ebsa/pdf/correctedsbctemplate2.pdf
The Uniform Glossary is available at
dol.gov/ebsa/pdf/SBCUniformGlossary.pdf.
All group health plans
Summary of Benefits
and Coverage (SBC)
and Uniform Glossary
If a plan makes a material modification in
any of the plan terms that would affect the
content of the SBC that is not reflected in the
most recently provided SBC, the plan must
provide notice of such change. This does not
apply to changes that occur in connection
with a renewal or reissuance.
All group health plans
Summary of Benefits
and Coverage: Notice
of Modification
Notice must be provided no later than
60 days prior to the date on which the
modification will become effective.
If a plan requires a participant or beneficiary
to designate a primary care provider, the plan
must provide notice of the terms of the plan
or coverage regarding designation of a
primary care provider and participants’ rights
to designate any participating primary care
provider who is available to accept the
participant; with respect to a child, to
designate any participating physician who
specializes in pediatrics; and that the plan
may not require authorization or referral for
OB/GYN care by a participating OB/GYN
professional.
All non-grandfathered
group health plans
2
Notice Regarding
Designation of a
Primary Care
Provider
Notice must be provided with the
Summary Plan Description or any
other similar description of benefits.
SBC must be provided to participants
and beneficiaries with enrollment
materials and upon renewal or reissu-
ance of coverage. SBC must also be
provided to special enrollees no later
than the date by which an SPD is
required to be provided (90 days from
enrollment).
The SBC and a copy of the Uniform
Glossary must also be provided upon
request within 7 days.
2
Under the Affordable Care Act, generally, grandfathered plans are plans that were in existence, and in which at least one individual was enrolled, on
March 23, 2010. Grandfathered health plans are exempt from many but not all Affordable Care Act market reforms. For further discussion, see the
Affordable Care Act section of this publication or visit dol.gov/ebsa.
135

Type of Disclosure Applicability Content Summary Timing
Internal Claims and Appeals: Plans must
provide notice of adverse benefit determina-
tion and notice of final internal adverse
benefit determination.
External Review:
For plans following the independent
review organization (IRO) process, the
IRO must issue a notice of final external
review decision.
For plans following a State process, the
state office administering external
appeals process for health insurance
companies must issue a notice of final
external review decision.
All non-grandfathered
group health plans
Internal Claims and
Appeals and External
Review Notices
Plans must provide a description of the
external review process in or attached to the
Summary Plan Description, policy, certifi-
cate, or other evidence of coverage provided
to participants, beneficiaries, or enrollees.
All non-grandfathered
group health plans
External Review
Process Disclosure
The description of external review
processes must be provided in the
Summary Plan Description or other
evidence of coverage provided to
enrollees.
Employers subject to the Fair Labor
Standards Act must provide a written notice
informing the employee of the existence of
the Marketplace, the potential availability of
a tax credit and that an employee may lose
the employer contribution if the employee
purchases a qualified health plan.
Model notices are available at
dol.gov/ebsa/healthreform/regulations/
coverageoptionsnotice.html
All employers subject to
the Fair Labor Standards
Act
Employer Notice to
Employees of
Coverage Options
Notice must be provided to all new
employees.
For internal claims and appeals,
timing of the notices vary based on the
type of claim.
For external review the timing of the
notice may vary based on the type of
claims and whether the state or the
federal process applies.
Preexisting Condition Exclusion Notices and Certificates of Creditable Coverage
For plan years beginning on or after January 1, 2014, plans are no longer required to issue the general notice of preexisting condition exclusion and
individual notice of period of preexisting condition exclusion. Plans are also no longer required to issue certificates of creditable coverage after December
31, 2014. These amendments were made because plans are prohibited from imposing preexisting condition exclusions for plan years beginning on or after
January 1, 2014. For more information see 79 Fed. Reg. 10296-317 (Feb. 24, 2014)
136
Appendix C:
Model Notices
137

Model Special Enrollment Notice
The following is language that group health plans may use as a guide when
crafting the special enrollment notice:
If you are declining enrollment for yourself or your dependents
(including your spouse) because of other health insurance or group health
plan coverage, you may be able to enroll yourself and your dependents in
this plan if you or your dependents lose eligibility for that other coverage
(or if the employer stops contributing toward your or your dependents’
other coverage). However, you must request enrollment within [insert
“30 days” or any longer period that applies under the plan] after your
or your dependents’ other coverage ends (or after the employer stops
contributing toward the other coverage).
In addition, if you have a new dependent as a result of marriage, birth,
adoption, or placement for adoption, you may be able to enroll yourself
and your dependents. However, you must request enrollment within
[insert “30 days” or any longer period that applies under the plan] after
the marriage, birth, adoption, or placement for adoption.
To request special enrollment or obtain more information, contact [insert
the name, title, telephone number, and any additional contact information
of the appropriate plan representative].
138

Your health plan is commied to helping you achieve your best health.
Rewards for participating in a wellness program are available to
all employees. If you think you might be unable to meet a standard
for a reward under this wellness program, you might qualify for an
opportunity to earn the same reward by different means. Contact us at
[insert contact information] and we will work with you (and, if you wish,
with your doctor) to nd a wellness program with the same reward that
is right for you in light of your health status.
Model Wellness Program Disclosure
For group health plans offering a wellness program that requires an
individual to satisfy a standard related to a health factor, the following is model
language that may be used to satisfy the requirement that the availability of a
reasonable alternative standard be disclosed:
139

Model Newborns’ Act Disclosure
The following is language that group health plans subject to the Newborns’
Act may use in their SPDs to describe the Federal requirements relating to
hospital lengths of stay in connection with childbirth:
Group health plans and health insurance issuers generally may not,
under Federal law, restrict benets for any hospital length of stay in
connection with childbirth for the mother or newborn child to less than
48 hours following a vaginal delivery, or less than 96 hours following
a cesarean section. However, Federal law generally does not prohibit
the mother’s or newborn’s aending provider, after consulting with the
mother, from discharging the mother or her newborn earlier than 48
hours (or 96 hours as applicable). In any case, plans and issuers may not,
under Federal law, require that a provider obtain authorization from the
plan or the insurance issuer for prescribing a length of stay not in excess
of 48 hours (or 96 hours).
Plans subject to State law requirements will need to prepare SPD statements
describing any applicable State law.
140

Model WHCRA Enrollment Notice
The following is language that group health plans may use as a guide when
crafting the WHCRA enrollment notice:
If you have had or are going to have a mastectomy, you may be entitled
to certain benets under the Women’s Health and Cancer Rights Act of
1998 (WHCRA). For individuals receiving mastectomy-related benets,
coverage will be provided in a manner determined in consultation with
the aending physician and the patient, for:
All stages of reconstruction of the breast on which the mastectomy
was performed;
Surgery and reconstruction of the other breast to produce a
symmetrical appearance;
Prostheses; and
Treatment of physical complications of the mastectomy, including
lymphedema.
These benets will be provided subject to the same deductibles and
coinsurance applicable to other medical and surgical benets provided
under this plan. Therefore, the following deductibles and coinsurance
apply: [insert deductibles and coinsurance applicable to these benets].
If you would like more information on WHCRA benets, call your plan
administrator [insert phone number].
141

Model WHCRA Annual Notice
The following is language that group health plans may use as a guide when
crafting the WHCRA annual notice:
Do you know that your plan, as required by the Women’s Health and
Cancer Rights Act of 1998, provides benets for mastectomy-related ser-
vices including all stages of reconstruction and surgery to achieve sym-
metry between the breasts, prostheses, and complications resulting from
a mastectomy, including lymphedema? Call your plan administrator at
[insert phone number] for more information.
142

Model Notice of Adverse B
enefit Determination – Revised as of July 3, 2014
OMB Control Number 1210-0144 (expires 07/31/2015)
Date of Notice
Name of Plan Telephone/Fax
Address Website/Email Address
This document contains important information that you should retain for your records.
This document serves as notice of an adverse benefit determination. We have declined to
provide benefits, in whole or in part, for the requested treatment or service described below. If
you think this determination was made in error, you have the right to appeal (see the back of this
page for information about your appeal rights).
Case Details:
Patient Name: ID Number:
Address: (street, county, state, zip)
Claim #: Date of Service:
Provider:
Reason for Denial (in whole or in part):
Amt.
Charged
Allowed
Amt.
Other
Insurance
Deductible Co-pay Coinsurance Other Amts.
Not Covered
Amt. Paid
YTD Credit toward Deductible: YTD Credit toward Out-of-Pocket Maximum:
Description of service: Denial Codes:
[If denial is not related to a specific claim, only name and ID number need to be included in the
box. The reason for the denial would need to be clear in the narrative below.]
Explanation of Basis for Determination:
If the claim is denied (in whole or in part) and there is more explanation for the basis of the
denial, such as the definition of a plan or policy term, include that information here.
[Insert language assistance disclosure here, if applicable.
SPANISH (Español): Para obtener asistencia en Español, llame al [insert telephone number].
TAGALOG (Tagalog): Kung kailangan ninyo ang tulong sa Tagalog tumawag sa [insert
t
elephone number].
CHINESE (
୰ᩥ): ዴᯝ㟂せ୰ᩥⓗᖎຓ㸪実㊐ㇻ征᷒⎟䞩 [insert telephone number]ࠋ
NAVAJO (Dine): Dinek'ehgo shika at'ohwol ninisingo, kwiijigo holne' [insert telephone number]. ]
143
Model Notice of Adverse Benefit Determination – Revised as of July 3, 2014
Important Information about Your Appeal Rights
What if I need help understanding this denial?
Contact us at [insert contact information] if you need
assistance understanding this notice or our decision to
deny you a service or coverage.
What if I don’t agree with this decision? You have a
right to appeal any decision not to provide or pay for
an item or service (in whole or in part).
How do I file an appeal? [Complete the bottom of
this page, make a copy, and send this document to
{insert address}.] [or] [insert alternative instructions]
See also the “Other resources to help you” section of
this form for assistance filing a request for an appeal.
What if my situation is urgent? If your situation
meets the definition of urgent under the law, your
review will generally be conducted within 72 hours.
Generally, an urgent situation is one in which your
health may be in serious jeopardy or, in the opinion of
your physician, you may experience pain that cannot
be adequately controlled while you wait for a decision
on your appeal. If you believe your situation is urgent,
you may request an expedited appeal by following the
instructions above for filing an internal appeal and also
[insert instructions for filing request for simultaneous
external review)].
Who may file an appeal? You or someone you name
to act for you (your authorized representative) may file
an appeal. [Insert information on how to designate an
authorized representative.]
Can I provide additional information about my
claim? Yes, you may supply additional information.
[Insert any applicable procedures for submission of
additional information.]
Can I request copies of information relevant to my
claim? Yes, you may request copies (free of charge).
If you think a coding error may have caused this claim
to be denied, you have the right to have billing and
diagnosis codes sent to you, as well. You can request
copies of this information by contacting us at [insert
contact information].
What happens next? If you appeal, we will review
our decision and provide you with a written
determination. If we continue to deny the payment,
coverage, or service requested or you do not receive a
timely decision, you may be able to request an external
review of your claim by an independent third party,
who will review the denial and issue a final decision.
Other resources to help you: For questions about
your rights, this notice, or for assistance, you can
contact: [if coverage is group health plan coverage,
insert: the Employee Benefits Security Administration
at 1-866-444-EBSA (3272)] [and/or] [if coverage is
insured, insert State Department of Insurance contact
information]. [Insert, if applicable in your state:
Additionally, a consumer assistance program can help
you file your appeal. Contact [insert contact
information].]
Appeal Filing Form
NAME OF PERSON FILING APPEAL: ____________________________
Circle one: Covered person Patient Authorized Representative
Contact information of person filing appeal (if different from patient)
Address: _________________ Daytime phone:________________ Email:_______________
If person filing appeal is other than patient, patient must indicate authorization by signing here:
_______________________________________________
Are you requesting an urgent appeal? Yes No
Briefly describe why you disagree with this decision (you may attach additional information, such as a
physician’s letter, bills, medical records, or other documents to support your claim):
______________________________________________________________________________
______________________________________________________________________________
Send this form and your denial notice to: [Insert name and contact information]
Be certain to keep copies of this form, your denial notice, and all documents and correspondence related
to this claim.
144
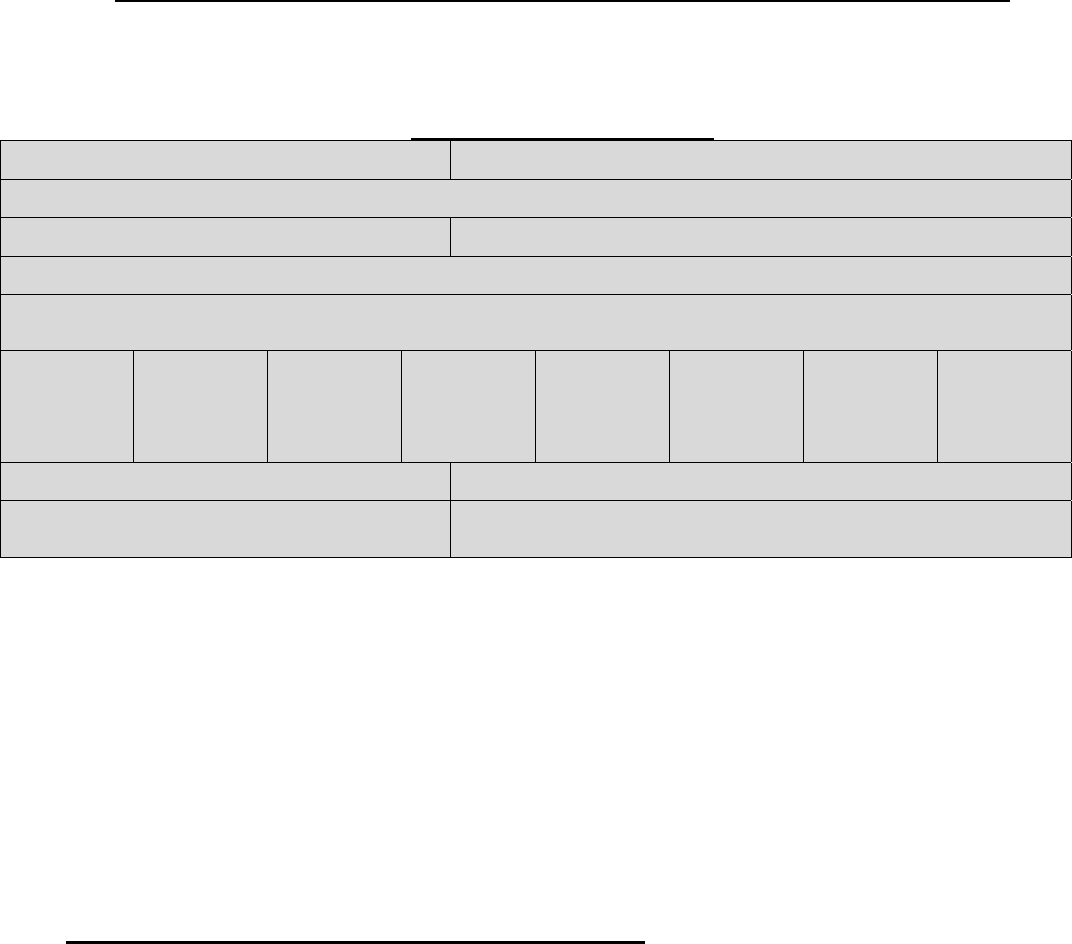
Model Notice of Fin
al Internal Adverse Benefit Determination – Revised as of July 3, 2014
OMB Control Number 1210-0144 (expires 07/31/2015)
Date of Notice
Name of Plan Telephone/Fax
Address Website/Email Address
This document contains important information that you should retain for your records.
This document serves as notice of a final internal adverse benefit determination. We have declined to
provide benefits, in whole or in part, for the requested treatment or service described below. If you
think this determination was made in error, you may have the right to appeal (see the back of this page
for information about your appeal rights).
Internal Appeal Case Details:
Patient Name: ID Number:
Address: (street, county, state, zip)
Claim #: Date of Service:
Provider:
Reason for Upholding Denial (in whole or in part):
Amt.
Charged
Allowed
Amt.
Other
Insurance
Deductible Co-pay Coinsurance Other Amts.
Not Covered
Amt. Paid
YTD Credit toward Deductible: YTD Credit toward Out-of-Pocket Maximum:
Description of Service: Denial Codes:
[If denial is not related to a specific claim, only name and ID number need to be included in the box.
The reason for the denial would need to be clear in the narrative below.]
Background Information: Describe facts of the case including type of appeal and date appeal filed.
Final Internal Adverse Benefit Determination: State that adverse benefit determination has been
upheld. List all documents and statements that were reviewed to make this final internal adverse
benefit determination.
Findings: Discuss the reason or reasons for the final internal adverse benefit determination.
[Insert language assistance disclosure here, if applicable.
SPANISH (Español): Para obtener asistencia en Español, llame al [insert telephone number].
TAGALOG (Tagalog): Kung kailangan ninyo ang tulong sa Tagalog tumawag sa [insert telephone
number].
CHINESE (
୰ᩥ): ዴᯝ㟂せ୰ᩥⓗᖎຓ㸪実㊐ㇻ征᷒⎟䞩 [insert telephone number]ࠋ
NAVAJO (Dine): Dinek'ehgo shika at'ohwol ninisingo, kwiijigo holne' [insert telephone number]. ]
145

Model Notice of Final
Internal Adverse Benefit Determination – Revised as of July 3, 2014
Important Information about Your Rights to External Review
What if I need help understanding this denial?
Contact us [insert contact information] if you need
assistance understanding this notice or our decision
to deny you a service or coverage.
What if I don’t agree with this decision? For
certain types of claims, you are entitled to request
an independent, external review of our decision.
Contact [insert external review contact information]
with any questions on your rights to external
review. [For insured coverage, insert: If your claim
is not eligible for independent external review but
you still disagree with the denial, your state
insurance regulator may be able to help to resolve
the dispute.] See the “Other resources section” of
this form for help filing a request for external
review.
How do I file a request for external review?
Complete the bottom of this page, make a copy, and
send this document to {insert address}.] [or] [insert
alternative instructions.] See also the “Other
resources to help you” section of this form for
assistance filing a request for external review.
What if my situation is urgent? If your situation
meets the definition of urgent under the law, the
external review of your claim will be conducted as
expeditiously as possible. Generally, an urgent
situation is one in which your health may be in
serious jeopardy or, in the opinion of your
physician, you may experience pain that cannot be
adequately controlled while you wait for a decision
on the external review of your claim. If you believe
your situation is urgent, you may request an
expedited external review by [insert instructions to
begin the process (such as by phone, fax, electronic
submission, etc.)].
Who may file a request for external review?
You or someone you name to act for you (your
authorized representative) may file a request for
external review. [Insert information on how to
designate an authorized representative.]
Can I provide additional information about my
claim? Yes, once your external review is initiated,
you will receive instructions on how to supply
additional information.
Can I request copies of information relevant to
my claim? Yes, you may request copies (free of
charge) by contacting us at [insert contact
information].
What happens next? If you request an external
review, an independent organization will review our
decision and provide you with a written
determination. If this organization decides to
overturn our decision, we will provide coverage or
payment for your health care item or service.
Other resources to help you: For questions about
your rights, this notice, or for assistance, you can
contact: [if coverage is group health plan coverage,
insert: the Employee Benefits Security
Administration at 1-866-444-EBSA (3272)]
[and/or] [if coverage is insured, insert State
Department of Insurance contact information].
[Insert, if applicable in your state: Additionally, a
consumer assistance program can help you file your
appeal. Contact:[insert contact information].]
NAME OF PERSON FILING REQUEST FOR EXTERNAL REVIEW: _________________________
Circle one: Covered person Patient Authorized Representative
Contact information of person filing request for external review (if different from patient)
Address: _________________ Daytime phone:________________ Email:_______________
If person filing request for external review is other than patient, patient must indicate authorization by
signing here: _______________________________________________
Are you requesting an urgent review? Yes No
Briefly describe why you disagree with this decision (you may attach additional information, such as a
physician’s letter, bills, medical records, or other documents to support your claim):
______________________________________________________________________________
______________________________________________________________________________
Send this form and your denial notice to: [Insert name and contact information]
Be certain to keep copies of this form, your denial notice, and all documents and correspondence related
to this claim.
146
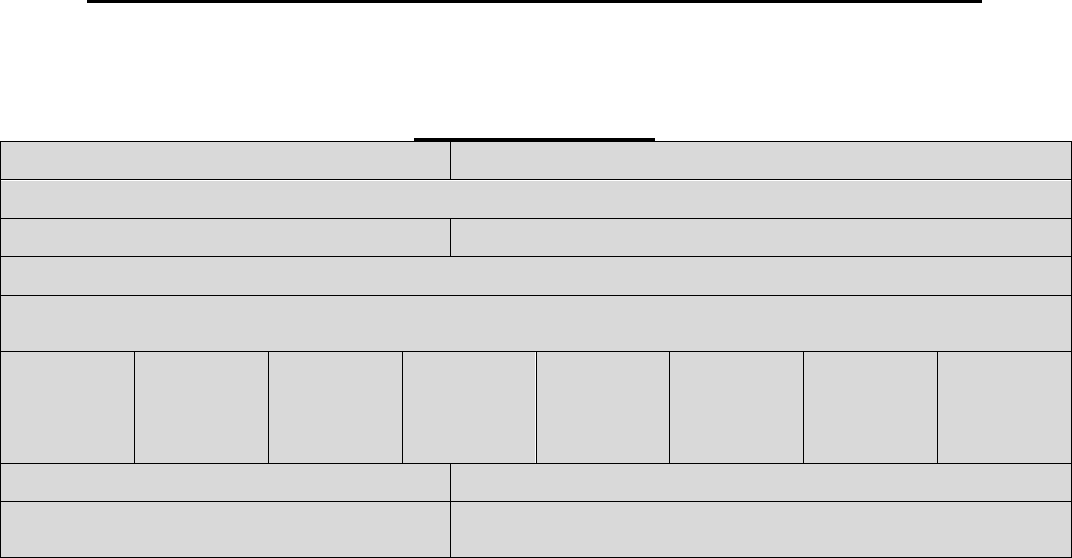
OMB Control Number 1210-0144 (expires 07/31/2015)
Model Notice of Final External Review Decision – Revised July 3, 2014
Date of Notice
Name of Plan Telephone/Fax
Address Website/Email Address
This document contains important information that you should retain for your records.
This document serves as notice of a final external review decision. We have
[upheld/overturned/modified] the denial of your request for the provision of, or payment for, a
health care service or course of treatment.
Historical Case Details:
Patient Name: ID Number:
Address: (street, county, state, zip)
Claim #: Date of Service:
Provider:
Reason for Denial (in whole or in part):
Amt.
Charged
Allowed
Amt.
Other
Insurance
Deductible Co-pay Coinsurance Other Amts.
Not Covered
Amt. Paid
YTD Credit toward Deductible: YTD Credit toward Out-of-Pocket Maximum:
Description of Service: Denial Codes:
[If denial is not related to a specific claim, only name and ID number need to be included in the
box. The reason for the denial would need to be clear in the narrative below.]
Background Information: Describe facts of the case including type of appeal, date appeal
filed, date appeal was received by IRO and date IRO decision was made.
Final External Review Decision: State decision. List all documents and statements that were
reviewed to make this final external review decision.
Findings: Discuss the principal reason or reasons for IRO decision, including the rationale and
any evidence-based standards or coverage provisions that were relied on in making this
decision.
147
Model Notice of Final Exter
nal Review Decision – Revised July 3, 2014
Important Information about Your Appeal Rights
What if I need help understanding this decision?
Contact us [insert IRO contact information] if you need assistance understanding this notice.
What happens now? If we have overturned the denial, your plan or health insurance issuer will
now provide service or payment.
If we have upheld the denial, there is no further review available under the appeals process.
However, you may have other remedies available under State or Federal law, such as filing a
lawsuit.
Other resources to help you: For questions about your appeal rights, this notice, or for
assistance, you can contact [if coverage is group health plan coverage, insert: the Employee Benefits
Security Administration at 1-866-444-EBSA (3272)] [and/or] [if coverage is insured, insert State
Department of Insurance contact information]. [Insert, if applicable in your state: Additionally, you can
contact your consumer assistance program at [insert contact information].]
148

Model Notice for Grandfathered
Health Plans
To maintain status as a grandfathered health plan, a plan or health
insurance coverage must include a statement, in any plan materials provided to
a participant or beneciary describing the benets provided under the plan or
health insurance coverage, that the plan or coverage believes it is a grandfathered
health plan within the meaning of section 1251 of the Patient Protection and
Affordable Care Act and must provide contact information for questions and
complaints.
The following model language can be used to satisfy this disclosure
requirement:
This [group health plan or health insurance issuer] believes this
[plan or coverage] is a “grandfathered health plan” under the Patient
Protection and Affordable Care Act (the Affordable Care Act). As
permied by the Affordable Care Act, a grandfathered health plan can
preserve certain basic health coverage that was already in effect when
that law was enacted. Being a grandfathered health plan means that
your [plan or policy] may not include certain consumer protections
of the Affordable Care Act that apply to other plans, for example, the
requirement for the provision of preventive health services without
any cost sharing. However, grandfathered health plans must comply
with certain other consumer protections in the Affordable Care Act,
for example, the elimination of lifetime limits on benets.
Questions regarding which protections apply and which protections
do not apply to a grandfathered health plan and what might cause a
plan to change from grandfathered health plan status can be directed
to the plan administrator at [insert contact information]. [For ERISA
plans, insert: You may also contact the Employee Benets Security
Administration, U.S. Department of Labor at 1-866-444-3272 or
dol.gov/ebsa/healthreform. This Website has a table summarizing
which protections do and do not apply to grandfathered health
plans.] [For individual market policies and nonfederal governmental
plans, insert: You may also contact the U.S. Department of Health and
Human Services at healthreform.gov.]
149

Patient Protection Model Disclosure
When applicable, it is important that individuals enrolled in a plan or
health insurance coverage know of their rights to (1) choose a primary care
provider or a pediatrician when a plan or issuer requires designation of a
primary care physician; or (2) obtain obstetrical or gynecological care without
prior authorization. Accordingly, the interim nal regulations regarding patient
protections under section 2719A of the Affordable Care Act require plans and
issuers to provide notice to participants of these rights when applicable. The
notice must be provided whenever the plan or issuer provides a participant with
a Summary Plan Description or other similar description of benets under the
plan or health insurance coverage. This notice must be provided no later than
the rst day of the rst plan year beginning on or after September 23, 2010.
The following model language can be used to satisfy the notice requirement:
For plans and issuers that require or allow for the designation of primary
care providers by participants or beneciaries, insert:
[Name of group health plan or health insurance issuer] generally
[requires/allows] the designation of a primary care provider.
You have the right to designate any primary care provider who
participates in our network and who is available to accept you or
your family members. [If the plan or health insurance coverage
designates a primary care provider automatically, insert: Until you
make this designation, [name of group health plan or health insurance
issuer] designates one for you.] For information on how to select a
primary care provider, and for a list of the participating primary care
providers, contact the [plan administrator or issuer] at [insert contact
information].
For plans and issuers that require or allow for the designation of a
primary care provider for a child, add:
For children, you may designate a pediatrician as the primary care
provider.
For plans and issuers that provide coverage for obstetric or gynecological
care and require the designation by a participant or beneciary of a
primary care provider, add:
You do not need prior authorization from [name of group health
plan or issuer] or from any other person (including a primary care
provider) in order to obtain access to obstetrical or gynecological care
from a health care professional in our network who specializes in
obstetrics or gynecology. The health care professional, however, may
be required to comply with certain procedures, including obtaining
prior authorization for certain services, following a pre-approved
treatment plan, or procedures for making referrals. For a list of
participating health care professionals who specialize in obstetrics
or gynecology, contact the [plan administrator or issuer] at [insert
contact information].
150

E
mployee
B
enefits
S
ecurity
A
dministration
U
.
S
.
D
epartment of
L
abor
September 2014
The Affordable Care Act
H
ealth
I
nsurance
P
ortability
and
A
ccountability
A
ct of
1996
Genetic Information Nondiscrimination
A
ct
Mental Health Parity Provisions
N
ewborns' and
M
others'
H
ealth
P
rotection
A
ct of
1996
W
omen's
H
ealth
and Cancer Rights Act of
1998
C
ompliance
A
ssistance
G
uide
H
ealth
B
enefits
C
overage
U
nder
F
ederal
L
aw...
H
ealth
B
enefits
C
overage
U
nder
F
ederal
L
aw...
