
Nursing past,
present and future
A publication in celebration of the
Royal College of Nursing’s centenary year

Introduction ...........................................1
Nursing in the Past .....................................2
A district nurse’s tale in the 1960’s ............................................... 2
Jackie Burns’ trip down memory lane ............................................. 4
Biographies of nurses from the past…Minnie Wood and Agnes Jones .................... 6
From hospital nursing to military nursing to the world of academia… ..................... 8
Nursing in the Present .................................10
From nursing to education… .................................................. 10
Nurse managed DVT service adopts ‘one-stop shop’ approach ....................... 11
Nursing behind closed doors .................................................. 12
RCN raises awareness of caring for people with dementia in an acute setting. . . . . . . . . . . . . . 14
How to nurse patients living in the past in the present ................................ 15
A Prole of Florence Bawak, matron for dementia care at
Stockport NHS Foundation Trust, Stepping Hill Hospital .............................. 18
A day in the life of a matron for dementia care ..................................... 19
Pioneering nurse Fiona is awarded MBE .......................................... 20
Nursing in the Future .................................22
How research has changed the face of nursing .................................... 22
Nursing in the 21
st
Century from a student perspective ............................... 23
A snapshot of our future… .................................................... 24
Contents

A publication in celebration of the Royal College of Nursing’s centenary year page 1
Welcome to the RCN North West commemorative centenary publication. The RCN has been enjoying a year
of celebrations, showcasing the wonderful nursing profession and the inspiring people who have made the
RCN what it is today.
2016 marks an important milestone in history of the
RCN. Here in the North West, we wanted to ensure
that we make our own mark in history by creating this
publication. When the RCN celebrates its 200
th
year,
we want our future members and staff to look back on
this publication with interest and see how nursing has
evolved and how we have overcome the considerable
challenges our profession faces.
In our publication, we are proud to showcase the work
of the nursing workforce, spanning a century, covering
specialisms such as dementia, acute, military and
education. We delve into how nurses carried out their
role in the past, we explore their position in the present
and we look at how not only our future nurses hope to
make an impact, but also
how research will play a
major part in patient care.
I hope you enjoy reading
about the fantastic work
our nursing workforce has
carried out over the past
100 years.
Best wishes
Estephanie Dunn
Regional Director,
RCN North West
The RCN has come a very long way in the past 100 years. In 1916, the RCN began with just 34 members and
a vision to create a register of qualied nurses. A century later, we have 435,000 members and nursing staff
with nearly 50,000 of those coming from the North West region.
Today we work in challenging times and we are facing
unprecedented pressures in both the NHS and the
independent sector. At the same time you consistently
show amazing dedication to the patients and clients
you treat and to their families and carers. You provide
continual high standards of care and at the same
timepush the boundaries of traditional practice.
RCN activists and staff in the North West work tirelessly
to safeguard the interests of our members and lead
in the development of excellent nursing practice. Your
board, your branches and your forums are dedicated
to supporting you to help you provide thebest possible
care and to help develop the nursing profession for the
next 100 years to come.
This publication offers
a fascinating insight
into nursing throughout
the ages and it is a
timely reminder on what
has been achieved by
generation after generation
of RCN activists.
Best wishes
Dave Dawes
Chair
RCN North West Regional Board
Introduction
Foreword from Estephanie Dunn, Regional Director
Welcome from Dave Dawes, Chair of the Regional Board

page 2 Celebrating 100 years of excellence • Nursing past, present and future
A history
“District Nursing began in Liverpool and the founder member
was William Rathbone. The Queens Institute was responsible
for the training of district nurses from 1889 to 1968 and the
criteria for acceptance was to have completed three years
training as a State Registered Nurse. The qualication was a
Queens Certicate in District Nursing.
“The district nurses were employed by the Liverpool
Corporation and would attend the same depot as the bus
drivers and conductors for their uniforms. This consisted of
a gabardine cap and coats, a starched apron and collar. The
apron had to be folded in the regimented manner we have
been taught underneath the coat which also had to be folded
in a set way when in a patient’s house. This would then be
laid on a clean piece of newspaper in case of tiny ‘unwanted
visitors’ which might invade it! The nurses’ salaries were
funded on the rates.”
My career
“I qualied as a State Registered Nurse in 1966 and
commenced training as a Queens Nurse in 1967, based in
Walton. This was not just a district nursing case but also a
training school serving nurses from Wales and the Isle of
Man. We were responsible to a Senior Nurse known as the
Superintendent whose word was ‘the law’. Most district nurses
of the time would walk or ride a bicycle. The walkers, like
myself, were issued with bus tickets. My pockets were usually
full of them because most bus conductors would not take a
fare from a nurse in uniform.”
The equipment
“We carried two bags which had to be maintained by a ritual
one afternoon a week followed by an inspection from the
Superintendent. The General Nursing Bag had a removable
boilable lining, the contents being a variety of instruments.
Rubber catheters and full enema equipment, rubber gloves
and lotions, all carried in individual cotton bags.
Nursing in the Past
A District Nurse’s Tale in the 1960s
General nursing care
“We collected our
uniforms for the
same depot as the
bus drivers.”
By Sylvia Thomas, Liaison and District Planning Nurse
Late night visit
Surgical dressings

A publication in celebration of the Royal College of Nursing’s centenary year page 3
“The instruments would
have to be boiled in a
pan before and after use
on the patient’s stove.
The contents of the
accessory bag consisted
of a nailbrush, soap box,
hand towel (the nurse
always carried her own)
thermometer, spatulas
and nail scissors.
"Each nurse had to
pack a biscuit tin with
dressings and bake
them in the patient’s
oven. This often gave
rise to problems,
considering the fact that the tins varied in thickness and
also the variety of gas, electric and sometimes coal re
ovens. It was difcult to gauge for how long to bake
them!”
The routine
"The nurse’s day would start with visits to the diabetic
patients who had to endure the discomfort of re-usable
needles and syringes. This equipment had to be boiled
regularly and stored in a glass jar of spirit. The needles
became blunt and often caused complications for their
patients.
"The district nurse was taught to carry out meticulously
the doctor’s orders. Now, the Superintendent has
long gone and the district nurse is aware of her own
professional responsibilities. She is responsible for
planning and delivering all forms of care to the patient
and it is not uncommon for the nurse and doctor to
make a joint decision on medical care. In some cases
Sylvia Thomas receiving her SRN qualication in 1966 from the Mayoress of Bootle
the training remains post-registered but now most
district nurses are trained to degree level. Pre-sterilised
disposable equipment may have changed but the
principles of district nursing remain the same today.
These are:
● Adapting hospital skills to nursing in the home.
● Being fully aware of the nursing and social needs of
the patient and family.
● Establishing and maintaining good human
relationships.
● Teaching relatives to care for the patient between
nursing visits.
● Communicating and cooperating with workers in
other services concerned with the health and welfare
of the community.
● Using every opportunity to educate the patient and
his/her family in health matters."
Principles quoted from the ‘General Principles of
District Nursing Standard Practice’, Queens Institute
of District Nursing – 1996 edition.

page 4 Celebrating 100 years of excellence • Nursing past, present and future
At the young age of 17, Jackie Burns, started
as a cadet nurse in Hudderseld in 1959. After
qualifying, she worked in hospitals for a few years
before specialising as a practice nurse for 27 years
in Didsbury. During her time as a nurse and after
retirement she was on council for the Royal College
of Nursing – the rst practice nurse to be on council.
The mum of two – and grandmother to nine, has had
an amazing career that has seen her help thousands of
people. It has also left the 74-year-old with many tales
to tell, which includes escaping the watchful eye of
the matron by using the re escape to go out dancing
and writing to a family for losing a patient’s teeth, to
writing publications and lecturing on immunisation and
vaccinations.
Starting out…
“I started as a cadet nurse in Hudderseld in 1959, at
the age of 17, living in shared accommodation, we had
our own room but a shared bathroom.
“Living in was great fun, it was basic but comfortable
and great friendships were formed. I remember it was
an old building with big deep baths and loads of hot
water. The downside was cockroaches, which came out
from the steam pipes at night.
“Being a cadet nurse involved study of anatomy and
physiology, arranging owers on the wards, and ufng
cotton wool and folding gauze to be autoclaved for use
in dressings. For this we were paid £2.19 shillings per
month, plus board and lodging.
“Our curfew was 10pm, and you could occasionally get
late passes for 11pm, but we used to sneak out at night
to go dancing and one person would take turns to stay
in and keep watch. The re escape came in very useful!
“I rst worked on Nightingale wards – and my very rst
was the male orthopaedic. My rst job in the morning at
7.30am was to help make beds. Bed wheels all had to
be aligned and coverlets turned down to the same level.
Screens were on wheels and moved from bed to bed.
“Talking to patients, apart from necessary treatments,
was discouraged, but you were expected to know
name, diagnosis and treatment of everyone on the
ward.
“Patients’ diets were treated very seriously, everything
was weighed carefully to get the proper balance and
they were quite small portions too.”
Big differences
“Some things have changed dramatically in treatment.
We tested urines with Bunsen burners. Syringes and
needles were boiled in a hot water steriliser, and they
were always very blunt.
“Iodine was a favourite antiseptic, penicillin powder was
put on to wounds and burns with a rubber bulb, raising
the foot of a bed was achieved with wooden blocks,
Trip down memory lane
By Jackie Burns
“Guinness and
champagne were
occasionally
prescribed.”
Nursing in the Past
Jackie Burns

A publication in celebration of the Royal College of Nursing’s centenary year page 5
and fractured femur patients were in bed with awful
metal splints for weeks and had an overhead hoist to lift
themselves.
“Guinness and champagne were very occasionally
prescribed by consultants for patients who didn’t
thrive. Thermometers were kept in antiseptic, with just
one or two per ward – it was a big day when a tray of
thermometers arrived, one for each bed.
“Also, it would have been the end of the world if one
of your patients got a bed sore – you would have been
sent to the Matron’s ofce. It was part of our rounds to
rub bottoms!”
Visits to the Matron’s ofce
“The matrons were formidable ladies, usually with
tailored dresses and frilly hats. We had to stand to
attention if we passed Matron in the hospital corridor.
“I once dropped a tray of thermometers and I was
giving a big telling off by the Matron and sent to the
stores to apologise. Another time, a patient vomited into
a kidney dish pot – so I emptied it down the sluice – but
unfortunately, the patient’s teeth also went with it! I had
to write to the family to apologise.
“I qualied in 1963 and was obliged to stay in the
hospital where I trained for 12 months before moving
on. I later became a pupil midwife at St Mary’s,
Manchester.
“After qualifying I then moved on to be a staff nurse
at The Christie in surgical theatre, and later became a
junior sister at Withington Hospital, and then a senior
sister on the gynaecology ward. I was presented with
frilly cuffs and a hat and allowed to wear a silver belt
buckle when I became a senior sister. After having my
two children, I returned as a night sister.
Practice Nursing
“Iin 1974 I became a practice nurse. Barlow Medical
Centre was a very forward thinking practice and already
employed a practice nurse, but I was appointed on
August 1 the same year, earning £88.42, and I stayed
for 27 years.
“The role was originally appointed as nurse/receptionist!
I enjoyed the autonomy of the role, with freedom of
choice and action. The role included dressings, routine
injections, travel injections, baby clinic and I gradually
developed to specialist status – one of only 12 nurses in
Manchester were granted this by the UKCC.
“During my time as a nurse, I helped develop practice
training at Manchester Metropolitan University and
lectured on the course as a visiting lecturer. I wrote and
lectured widely on immunisation and vaccination and
helped write a handbook on pneumococcal vaccination,
for which I was put forward for practice nurse of the
year and was proud to be a nalist. I was also a rst
nurse member of an investigative team on a failed GP.
“I was the rst practice nurse elected to RCN Council
where I served for seven years. I wanted to raise the
prole of practice nursing. I loved every moment of it.
They were the most stimulating years of my career.
Nursing future
“There have been a lot of changes over the years. I think
it is more relaxed these days, there is not the same
hierarchy, it gave us a framework and these days you
can walk into a hospital and not know who is who.
“But there have been huge developments in training for
nurses. With the amount of technology and variety now,
training is very different.”

page 6 Celebrating 100 years of excellence • Nursing past, present and future
Minnie Wood was
born in Birstall, Batley,
West Yorkshire on
14 October 1880.
Her brothers all died
in infancy and she
had one younger
sister, Elsie. She was
privately educated at a
school run by the Miss
Sandbaches in Hull.
She trained as a
nurse at Salford Royal
Hospital from 1905-8.
She stayed there as a
staff nurse before progressing to sister until she joined
the Queen Alexandra’s Imperial Military Nursing Service
in 1912.
She spent the whole of WW1 nursing in Flanders - in
casualty clearing stations, in a eld ambulance andin
stationery hospitals.
A total of 146 nurses received a military medal during
WW1 including Minnie in 1917 for her work during the
Battle of Passchendaele:
“For most courageous devotion to duty. On the 21st
August 1917, this lady was Sister-in-Charge at No.44
Casualty Clearing Station, Brandhoek, when it was
shelled at short intervals from 11am. till night, one Sister
being killed. This lady never lost her nerve for a moment
and during the whole of a most trying day, carried out
her duties with the greatest steadiness and coolness.
By her work and example she greatly assisted in the
speedy evacuation of the patients and the transfer of
the Sisters” (London Gazette,17 October 1917).
At the end of the war she was sent to work in Germany,
but was found to be suffering from ‘debility’ at a
medical board in July 1919 and sent to a hydropathic
establishment in Ilkley for a month. She then resumed
her duties in the military hospitals in Devonport and then
Licheld. She went sent to Malta in 1922 before being
sent to Belfast in 1923.
She resigned from the army citing ‘private’ reasons
concerning ‘only family affairs’ in January 1924. Her
mother died the same year and her father three years
later so one theory why Minnie left was to go home to
nurse them. However, the trail goes cold at this point
and Dr Chatterton is still trying to nd out when and
how she died.
Minnie’s medals are on display at the University of
Salford. One of their new simulation laboratories was
recently named after her, together with Edith Cavell
(who also has links to Salford) at a special event on
Nurses’ Day:
http://www.salford.ac.uk/news/events/2016/
courage-in-healthcare-edith-cavell-and-sister-
minnie-wood
Should you have any more information about
the remainder of Minnie’s life, email:
Nursing in the Past
Biographies of nurses from the past…
“The most courageous
devotion to duty.”
One of our North West Regional Board members, Dr Claire Chatterton, Staff Tutor, School of
Wellbeing, Health and Social Care, has been researching nurses from the past and explored the life of
Military Nurse Minnie Wood, and Agnes Jones…
Minnie Wood

A publication in celebration of the Royal College of Nursing’s centenary year page 7
Agnes Elizabeth
Jones was born
on 10 November
1832 into a wealthy
military family in
Cambridge. Because
of her father’s army
career she and her
family spent time
in Mauritius. They
then settled in Fahan
inCounty Donegal in
Ireland.
Agnes grew up with
a deep religious faith
and a strong social
conscience. She was encouraged by her family to take
part in a variety of philanthropic activities including
teaching local children and visiting the sick in the local
area. These factors together with seeing the nursing
workof the deaconesses from Kaiserworth, where
Florence Nightingale had gained valuable experience, all
inspired her to train as a nurse.
By 1856 she was nursing at Dublin Hospital and in
1859 she went to London, where she met with Florence
Nightingale and Mrs Wardroper, senior nurse at St
Thomas Hospital. Three years later she began her
training in the Nightingale School at St Thomas Hospital.
She was later described byNightingale as ‘one of our
best pupils’.
After completing her training she continued to work
in London,but in 1865 she moved to the North
West. William Rathbone, a Liverpool merchant and
philanthropist, effectively ‘head hunted’ her as result of a
new project that he had initiated.
He was appalled by the terrible conditions in the
Brownlow Hill Workhouse in Liverpool, which was
one of the biggest in England. In common with other
workhouse inrmaries of this period, the perfunctory
nursing care provided was by other female inmates.
Rathbone decided to recruit trained nurses in an
attempt to ameliorate the situation. He enlisted Florence
Nightingale’s help and she recommended Agnes Jones
for the post of Lady Superintendent. Her role was to
lead a team of 12 trained nurses and 65 assistant
nurses to reform the inrmary – a huge task as it could
contain up to 2,000 beds. She was the rst trained
nurse to take on such a role.
Due to the poor conditions and overcrowding, cholera
and typhus were both rife and one of the rst tasks for
Agnes and her team was to scrub and clean all the
wards and bed linen. As conditions improved and the
death rate declined they continued to work but, sadly,
on 19 February 1868 at the age of only 35, she died of
typhus fever herself. Florence Nightingale said of her
‘she overworked as others underwork. I looked upon
hers as one of the most valuable lives in England’. She
‘died at her post’ she said, ‘amongst the poor and sick,
while yet in the ower of her age.’
Her contributions to nursing were remembered in
avariety of ways. Her body was returned to her
family in Ireland and she is buried in the graveyard in
Fahan, where there is also a memorial to her in her
family’s church. In Liverpool she can be found in the
‘Notable Women’stained glass windows in the Lady
Chapel in the Anglican Cathedral. William Rathbone
commissioned a monument which is now housed in
the Oratory by the Anglican Cathedral (now part of
the Walker Art Gallery). A student hall of residence is
also named after her (housed in the former Liverpool’s
Women’s Hospital building).
For further information see http://nurseagnesjones.com/
“Agnes was one of our
best pupils”
Florence Nightingale
Agnes Elizabeth Jones
page 8 Celebrating 100 years of excellence • Nursing past, present and future
Alan Finnegan
has enjoyed a long
and varied career.
After qualifying as a
Registered General
Nurse in 1984 at
North Manchester
General Hospital,
he then obtained
a mental health
nursing qualication
in Birmingham before
joining the Army in
1987.
Alan, who sits on the
RCN North West Regional Board, went into nursing as
he was interested in working with people and the variety
and diversity of the job. Changing from one healthcare
setting to another was particularly appealing.
He believes that a nurse needs to be caring,
compassionate and trustworthy adding: “Obviously they
need to have the correct skills sets to safely practice
within their own scope of practice. Nurses should also
be an advisor, teacher, researcher, role model, team
player and patient’s advocate.
Alan said: “While nurses have a key role within the multi-
professional team, they nonetheless have a distinct
and unique role. Many patients look to nurses to be
their advocate, the person who they build a relationship
with, and who respects them irrespective of the faith,
afliations, views or culture”
Alan thinks that the fundamental aspects of nursing
have remained remarkably consistent over the last 100
years and that nurses are an integral part of the multi
professional team and the focus for patient care.
He said: “Some of the nursing leaders of 100 years
ago showed remarkable fortitude, resilience, exibility,
leadership skills and courage. Current nurses have
similar characteristics, notably demonstrated by our
colleagues who cared for the sick during the Ebola Virus
Disease outbreak in Sierra Leone.”
For the best part of 30 years, Alan followed a fairly
typical Nursing Ofcer career trajectory, mixing clinical
practice and wider military employment with academic
progression and operational tours. In his nal years he
had the honour to be the senior military nurse based
within the University of Birmingham NHS Foundation
Trust which was the receiving hospital for military
casualties injured in Iraq and Afghanistan.
He said: “Having a role to play in their care and
supporting their families was challenging but
exceptionally rewarding. My nal appointment as the
Ministry of Defence Professor of Nursing provided an
opportunity to try and raise the prole of Nursing in the
Armed Forces.”
Alan added: “My career has now transitioned into full
time academia at the University of Chester; which is
very rewarding. I’m fortunate to enjoy my job and enjoy
going to work and still hope to produce outputs that
can make a difference.”
Nursing in the Past
From hospital nursing to military nursing to the
world of academia…
“Nurses should also
be an advisor, teacher,
researcher, role model,
team player and
patient’s advocate.”
Alan Finnegan
at the University of Chester

A publication in celebration of the Royal College of Nursing’s centenary year page 9

page 10 Celebrating 100 years of excellence • Nursing past, present and future
Nursing in the Present
Helen Walker, an Associate Assistant Principal at
Manchester Health Academy, an 11 – 18 Academy
in Wythenshawe, Manchester, trained at Manchester
Royal Inrmary in 1983 as a Registered General Nurse.
Following qualication she worked on both Medical and
Gynaecology Units before completing her midwifery
training in 1988 at Saint Mary’s Hospital, Manchester.
While she was working at Saint Mary’s as a midwife
Helen completed a part time Further and Adult
Education Teacher’s Certicate. She was then employed
as a Lecturer in Health at Salford College of Further
Education. During this time Helen completed a BSc
in Health Care and Welfare and a Post Graduate
Certicate in Education.
She worked in Further and Sixth Form Education for
the next 15 years before moving to Manchester Health
Academy in 2010 where she was employed to support
the setting up of the new 6th Form and to integrate
health across the Curriculum working specically with
the sponsor, Central Manchester University Hospitals
NHS Foundation Trust. She is currently a member of
the Senior Leadership Team and has responsibility for
promoting the Health Specialism. Helen has also just
graduated having completed an MA in Education at
MMU.
Helen decided to go into Nursing following a careers trip
to Manchester Royal Inrmary. She added: “I felt that
working with patients in a hospital environment would
enhance my skills, qualities and personality. My parents
were teachers and my brother was a doctor so they
inspired me through their own commitment to helping
others.”
Helen said: “I have looked back on my own experiences
both in nursing and teaching and really understand
the need for compassion and care. Patients hang on
to every word that health professionals say to them
so I think tact and sensitivity is really important too. In
today’s busy world where we don’t have a lot of time it’s
important to make sure those people around us know
we are interested and care about them.”
“I still enjoy visiting my students during placements.
I often go back to the hospitals where I trained and
remember my own early career experiences. I enjoy the
pastoral work that I am involved in as so many of my
nursing skills are transferable. Our Academy is situated
in an area of real need. There are lots of challenges for
our students to overcome.”
Although Helen no longer practices as a nurse, she is
aware of recent strategies such as the 6 C’s. She said:
“My training was very structured and disciplined and this
has stood me in good stead in my current career as I try
to maintain high standards for my own practice. I was
working on the wards when I was 18 which was very
challenging at times.
“My second ward was Haematology where I remember
my rst experience of a patient death; a young man
who had leukaemia. I grew up very quickly during this
time. I learnt how to work in a different team every six to
eight weeks, how to work cooperatively with managers
and developed skills and values I have carried with me
during my own life and career.”
From Nursing to Education…
“Our Academy is
situated in an area
of real need. There
are lots of challenges
for our students to
overcome. ”
at Manchester Health Academy
Helen with some of her students

A publication in celebration of the Royal College of Nursing’s centenary year page 11
A nurse’s dedication to improving patient
satisfaction within the DVT service has led to Bolton
NHS Foundation Trust gaining exemplar status for
its work in this eld.
The previous Deep Vein Thrombosis (DVT) service did
not always receive good patient feedback, due to delays
in medical review and in radiology department imaging.
Medical Nurse Consultant Beatrice Fox, who has
worked at Royal Bolton Hospital for 12 years, identied
that major improvements could be made to this service.
She led a major piece of work to move to a nursing
managed service.
The team introduced Independent Vascular Service
imaging (IVS), which provides them with a much greater
degree of exibility. They are now able to scan every
patient within 24 hours. When a patient is referred from
A&E or in the community they can also be scanned and
diagnosed generally on that day – waits were previously
around ten days.
More than 98% of all referrals into the service are
now managed as outpatients, and they are more than
meeting their increased patient levels.
Beatrice has championed the nurse managed DVT
service and facilitated work towards the Trust achieving
national venous thromboembolism (VTE) exemplar
status. She has played a great role in staff professional
development, and has ensured that all her team have
been trained in non-medical prescribing.
Bolton is now a beacon site for VTE across the region,
and frequently facilitates visits from Trusts across the
region looking to implement the system that they have
in place.
Nurse managed DVT service adopts ‘one-stop
shop’ approach
“Thank you so much for
all your help and kindness
in dealing with my mum
and myself. Mum had a
suspected DVT following
hip surgery.
“Wearrived at the DVT
clinic and you dealt with
everything and everyone
so efficiently, ensuring we
were dealt with quickly
and also arranging
teaand toast while we
waited for the ambulance
to take us home - that
was alifesaver!”
at Bolton NHS Foundation Trust
Beatrice Fox

page 12 Celebrating 100 years of excellence • Nursing past, present and future
Bob Downs joined
the Prison Service,
as a prison ofcer,
in 1985 and was
posted to HMP
Manchester in 1987.
The majority of his
working days in
Manchester were
spent working within
the Healthcare Unit
and he found the
variation in work
both rewarding and
challenging.
As a prison ofcer
he had received no
formal healthcare
training so, in
1989, he applied to
undertake the Healthcare Ofcer training. This consisted
of six months’ training, both practical and theoretical, in
physical and mental health. He undertook placements
at Rampton High Secure Hospital, Whiston General
Hospital, Rainhill Psychiatric Hospital and Walton
General Hospital.
In 2002 he gained a secondment, at Manchester
University, to undertake the Enhanced Diploma in
Mental Health. On completion of training he returned to
HMP Manchester.
He said: “The skills I learnt during my training allowed
me to contribute to the delivery of care with more
condence, and a greater insight, than previously.”
Bob believes that whatever branch of nursing you are in,
the qualities needed are fairly similar adding: “The ability
to be caring and compassionate is central to nursing
as are good communication and listening skills. A nurse
also needs to constantly reect on their own practice
and take the lead in their own personal development.”
He said: “Prison nursing can be an extremely
challenging environment to work in. Many in our client
group are high prole, and I have often been asked
how we can provide healthcare for people who many
of the public don’t feel deserve it. The ability to be
non-judgemental in such an environment is essential in
ensuring our clients receive the same level of healthcare
they would expect to receive in the community.
“The prison can be an extremely challenging and difcult
place to work. A nurse needs to be resilient, exible,
reliable, and also have self-awareness
“Education and health promotion is a fundamental,
and extremely important, part of the role undertaken
in prisons. Addressing clients health needs, and giving
them appropriate health promotion and education, is
known to have a positive impact on re-offending rates
and can also impact on the health and wellbeing of
communities.”
Bob spoke about how he thinks the role of the nurse
as changed over the last 100 years saying that the
role of the universities in training nurses, as opposed
to pure ward-based training, is one that continues to
cause debate. He found the theoretical knowledge
gained during his training invaluable in underpinning his
practical skills on placement.
He thinks one of the biggest changes is the emphasis
on patients being involved in their own care, as
opposed to decisions being made for them. Patient
involvement in the care planning and decision-making
Nursing in the Present
Nursing behind bars
“Prison nursing can be
an extremely challenging
environment.”
Bob (left) receiving the Lifetime
Achievement Award at the 2012 High
Security Directorate Prison Service
Ofcer of the Year awards from Phil
Copple, Director of High Secure
Prisons.
at Manchester Mental Health and Social Care NHS Trust

A publication in celebration of the Royal College of Nursing’s centenary year page 13
process can only be a positive move and leads to better
outcomes.
Bob has been working in and around healthcare for
the last 31 years, all in prison establishments. When
he rst started, the budget for healthcare sat within
the main prison budget and, where the overriding risk
for a prison establishment is security, it was inevitable
that healthcare funding would not meet the need of its
service users.
When the responsibility for healthcare delivery in
prisons switched to the Department of Health, around
2004, they saw a big increase in human and nancial
resources. This has allowed them to deliver major
improvements across all areas of healthcare including
services, training, equipment and facilities.
Bob said: “I think it is fair to say that healthcare delivery
within prisons is certainly on a par with what a prisoner
would expect to receive in the community, and this is a
major improvement.”
One of the biggest challenges for prison nursing is
to ensure that, on reception, they accurately assess
each patient’s health needs and risks. There cannot be
many GP practices which have over 350 new patients
registered each month.
Bob explained: “Between 70% and 80% of all those
in prison have a mental health or substance misuse
problem, and you can see how reception screening
paves the way for individual care provision. This is one
area where we cannot afford to get it wrong.
“As the Head of Healthcare it is a daily challenge to
combine healthcare delivery with working in a high
secure environment.
“The favourite part of my job is to know that we provide
a great service to our client group. Receiving feedback
from our clients, or inspectors, saying that we provide a
quality service is the icing on the cake.”
The day in the life of a
prison nurse…
by Bob Downs
A prison nurse will start at 7.00am. Like at an
airport, all items are X-rayed and you walk
through a metal detector. Unfortunately there
is no aeroplane on the other side and that is
where the similarity ends. There is also no
access to social media as phones, tablets etc.
cannot be brought in.
Following handovers, medication administration
rounds will start at 8.00am until about 9.00am
when the nursing staff will return to their dedicated
areas. Nurses will run independent clinics, work in
reception, on the 19-bed inpatient unit, or within
the mental health and substance misuse teams.
We have 24-hour nursing cover so we have an
RGN and RMN working nights. All staff are trained
in Immediate Life Support and a dedicated nurse
will attend to alarm bells or medical emergencies.
All our healthcare staff, including HCAs, have
transferable skills and are able to work in all areas
of the prison. This ensures there is variety for them
and the ability to progress.
We have staff trained in chronic disease
management, palliative care, non-medical
prescribing, venepuncture and communicable
diseases, amongst other things. The prison regime
can change at a moment’s notice, for operational
reasons, and nursing staff have to be able to
adapt quickly and at short notice.

page 14 Celebrating 100 years of excellence • Nursing past, present and future
As the Royal College of Nursing celebrates its
Centenary, the Isle of Man branch organised two
workshops to coincide with Alzheimer’s awareness
week in May.
The theme was ‘Caring for people with dementia in an
acute setting’, with an emphasis on communication.
Expert speakers Claire Chatterton from the Open
University, Jane Kemp from the RCN and Susan Walker,
an island based dementia support worker all made
valuable contributions to sessions, which were held at
the Isle of Man Government’s Learning, Education and
Development (LEaD) Division’s HQ.
Chair of the RCN Isle of Man branch, Verna Phillips
said: “The speakers were knowledgeable, relaxed and
made a difcult subject interesting. They had excellent
presentation skills.
“Both workshops were oversubscribed and involved
plenty of participation. We were given comprehensive
handouts and feedback proved learning had taken
place.
“I am sure the day enhanced the knowledge
and perceptions of our nurses and carers when
communicating and treating one of the most vulnerable
and growing sections of our community.”
Chief Nurse for the Isle of Man, Linda Radcliffe added:
“As the Royal College of Nursing celebrates its 100th
anniversary and we look back over the past century –
one of the biggest changes is the signicant increase
in life expectancy. With the eradication of many lethal
communicable diseases, people are living longer.
“As we look to the future and the challenges of the next
100 years, it is clear the rise of long term conditions,
such as dementia, will test our skills, resilience and
ability to adapt as a profession.
“ Workshops, such as these, are vital to ensuring nurses
can grow their skill set to continue to offer exceptional
and compassionate care.”
Nursing in the Present
Meeting the Dementia challenge
Jane Kemp, Dr Claire Chatterton and Verna Philips.
Linda Radcliffe
in the Isle of Man

A publication in celebration of the Royal College of Nursing’s centenary year page 15
● There are 850,000 people living with dementia in the UK, with numbers set to
rise to over 1 million by 2025. This will soar to 2 million by 2051.
● 225,000 will be diagnosed with dementia this year, that’s one every three
minutes.
● 1 in 6 people over the age of 80 have a diagnosis of dementia.
● 70 per cent of people in care homes have a diagnosis of dementia or severe
memory problems.
● There are over 40,000 people under 65 living with dementia in the UK.
● More than 25,000 people from black, Asian and minority ethnic groups in the
UK are affected.
How to nurse patients living in the past in the present
at Stockport NHS Foundation Trust
Florence and one of her patients
Stockport NHS Foundation Trust has a variety of
projects aimed at supporting patients living with
a diagnosis of dementia along with their carers.
There is also an emphasis on person-centred care
which aims to see the person with dementia as an
individual.
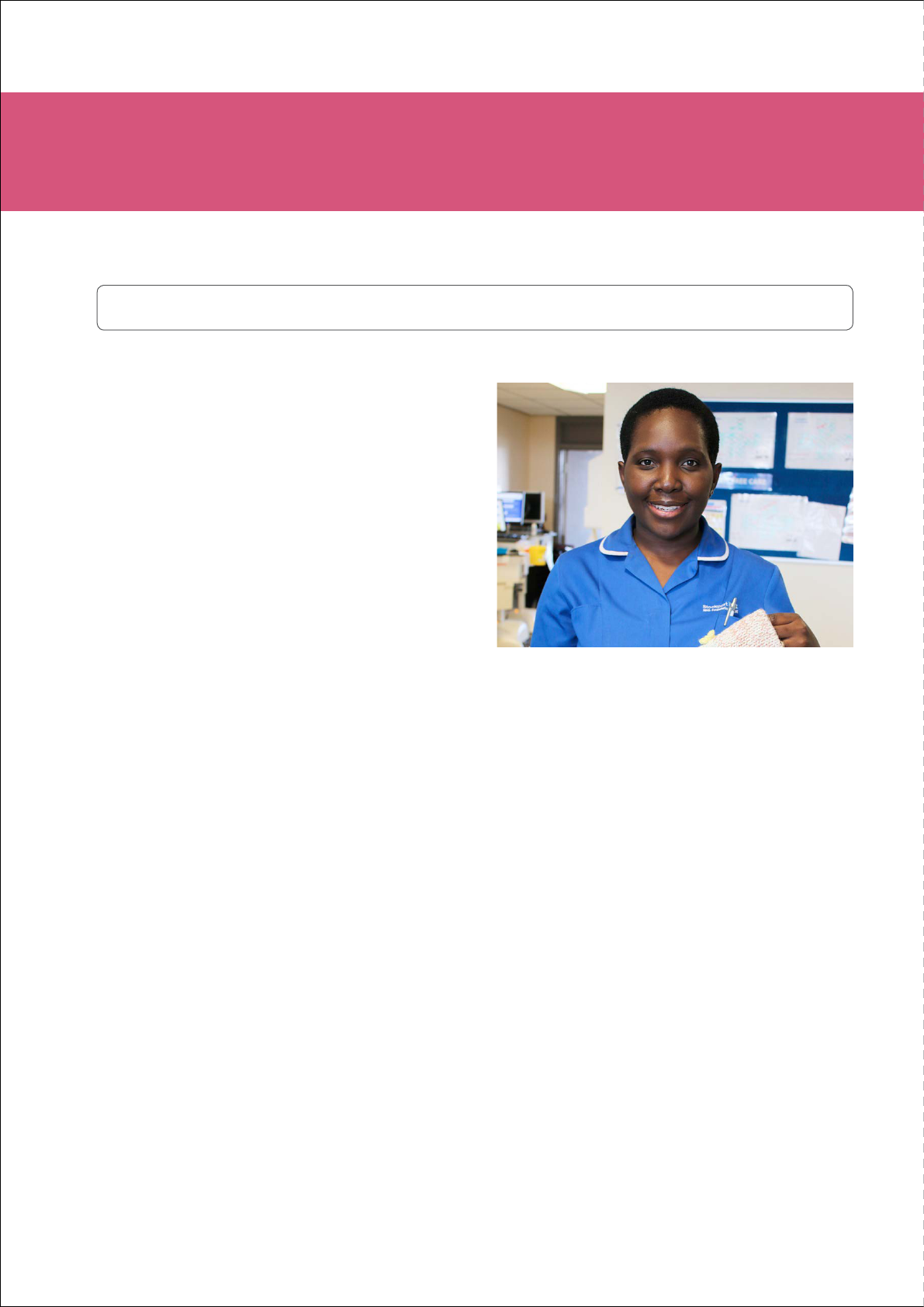
Matron for Dementia Care, Florence Bawak, began
working at the organisation in July 2015 and since then,
has continued the Trust’s good work with patients with
a diagnosis of dementia and their carers.
Dr Peter Ngoma runs theMemory Clinicevery other
Wednesday with a registrar and specialist nurse. Part
of the rst attendance at clinic is for an assessment
and establishing if the patients need an MRI or CT scan
or further tests to rule out any other physical health
problems that present similar to dementia. Florence is
notied of all patients who are newly diagnosed and
contacts the patients and their families/carers and refers
them to Signpost for carers or the Alzheimer’s Society
where they can receive additional support.

page 16 Celebrating 100 years of excellence • Nursing past, present and future
Nursing in the Present
How to nurse patients living in the past in the present
at Stockport NHS Foundation Trust
Music in Hospitalshave visited the hospital to perform
for the patients. Patients form a connection with music
and staff see a very different side to them. Music can
help with reminiscence and relaxation. It also helps
patients make positive connections with others as it
triggers memories. All wards now have CD players
and CDs to help relieve anxiety in patients living with a
diagnosis of dementia.
A ‘forget me knot ower’ schemeenabling staff in
their A&E and other departments, to easily recognise
patients living with dementia has also been established.
This sign serves as a visual reminder for staff to
remember the person.
Clearer signagefor patients with dementia
and‘memory boards’reminding patients instantly what
date and time it is have also been introduced as well
as70 dementia championsacross the organisation
There is a full timepsychiatric liaison servicefor
older adults and the organisation has also run atraining
course for drivers of a local taxi rm so they are better
trained to support patients living with dementia. Metro
Taxis pick up and drop off thousands of passengers
at the hospital every year, and a large number of these
have dementia or memory loss. Our nurses have taught
drivers the best way to make sure these passengers
have comfortable and secure journeys. The rm
sponsored the ‘This is Me’ booklets that are used in
the hospital to provide additional support for patients
living with dementia who nd themselves in a new and
unfamiliar environment.
Fundraising is currently taking place to introducea
‘dementia café’in the hospital. This will be a relaxing
environment where carers and patients living with
dementia can go for a chat, or just some quiet time.
The café will also have tea and coffee making facilities.
These rooms reect bygone times, complete with décor
and music from the era. They are proven to create a
therapeutic and relaxing environment for patients living
with dementia and their carers.
Last year, student volunteers all in their second or
third year of health and social care studies at Stockport
college, worked one day a week on a voluntary basis
to support patients living with a diagnosis of dementia.
They spent time on the wards and helping with meals.
The students also spent time talking with them on a
1:1 basis or engaging with them in activities. A movie
afternoon on one of the wards was a great success.
Activity Mitts,also known as ‘Twiddle muffs’, are
knitted or crocheted band with items attached, such
as ribbons, buttons, zips and beads which provide
sensory stimulation.They are also conversation starters
as patients living with a diagnosis of dementia nd it
difcult to nd the words. Activity mitts are also proven
to help relax and distract patients.
Florence Bawak and a pile of Activity Mitts
Music in Hospitals

A publication in celebration of the Royal College of Nursing’s centenary year page 17
There is also a reminiscence roomin one of the
older people’s wards. This room is decorated in period
décor and helps keep the patients calmer and happier.
It is often used as a quiet room or for patients to enjoy
movies and music of their choice. This room is kept
open throughout the day.
We have also implemented memory boxes. These are
activity boxes containing reminiscence cards, sensory
balls, aqua paint cards and paint brushes. The purpose
of these boxes is to stimulate activities and reduce
boredom in patients living with a diagnosis of dementia.
Carers’ passports have been introduced in support of
John’s campaign. These passports allow carers to visit
and support their relatives at any time. The passports
have led to improved relationships and partnership
working between carers and staff.
Within the Accident and Emergency Department,
there is a dementia trolley containing the ‘This is Me’
booklets, carers passports, activity mitts, dolls, sensory
balls, aqua paint cards and reminiscence cards. When
it was implemented, Stockport’s communications team
tweeted about this with posts going viral. They have
since had interest from as far as Australia enquiring
about the contents of the trolley and how they are
using it. This has sparked an interest in research on
the importance of activity in people with dementia.
The dementia champion in A&E has been key to the
success of this implementation and also has had a
music app installed on out of use iPads for patients to
enjoy whilst in the emergency department.
Doll Therapy has also been successfully introduced on
older people’s wards for patients who are agitated and
anxious about their children.
Miguel Serrano and the Dementia Trolley
Dementia Orientation Board
page 18 Celebrating 100 years of excellence • Nursing past, present and future
Florence Bawak, Matron for Dementia Care at
Stepping Hill Hospital in Stockport, was inspired
to go into nursing by her mother who was a
registered general nurse (RGN) and worked in
several specialities in Cameroon. She particularly
remembers going to see her at work at the
children’s unit and in theatre and loved the way she
interacted with the patients and communicated with
her colleagues.
Florence’s mother has always been her inspiration;
but she worked long hours and was rarely at home
so although she wanted to be a nurse she decided
she didn’t want to be an RGN. She was interested in
sociology and how people interact so, when the time
came to decide, she picked mental health nursing
instead and has enjoyed it ever since.
Florence said: “I believe a nurse needs to be patient
and calm, listen actively and with compassion, be ready
to give time to all their patients and above all make the
patient feel they are not a burden. A nurse also needs
to be ready to offer reassurance to all her patients
and treat them with dignity and respect and act as an
advocate for them, ensuring that their concerns are fed
back to the medical team.
“Often patients are given a diagnosis, with a lot of
explanations at the same time. Very often all they hear
is the diagnosis, and, as they process this information,
they will have lots of questions often when the doctor is
not available. It very often falls on the nurse to provide
them with reassurance and sometimes answers to their
questions.”
Florence added: “In my opinion, most of the changes
in the role of the nurse have been around additional
responsibilities. I do believe this is a positive change as
it has led to nurses progressing further in their careers.
I believe nurses are being recognised now more and
more as the skilled professionals that they are.”
She added: “I love when staff engage in training and
understand that, behaviours that dementia patients
exhibit is a form of communication. And that people
with a diagnosis of dementia will display complex
behaviours because emotions are the only manner of
communication sometimes left for them to use.”
She particularly loves the effect that music has on a
person. Florence states “it’s just magical to watch a
person’s personality come through when they listen
to music and how this helps them make positive
connections with their families again.”
Florence believes mental health nurses must be
equipped with communication skills, de-escalation skills
and undertake regular updates on prevention of violence
and aggression throughout their training. These skills
prepare them for when they qualify and start practising.
Florence said: “All of these valuable skills are put to
the test when RGNs are faced with a patient with a
diagnosis of dementia, who is unable to comprehend
what is being asked of them and declines interventions
that are necessary to improve their health. The nurse
is then faced with the question, how I am supposed
to carry out my job? As newly qualied nurses on the
ward, it really is the beginning of learning a whole new
set of skills. However, what I have noticed is that they
remain dedicated to doing their best for the patient
and to develop and learn a whole new set of skills to
enable them to support the patients better. This is what
I admire about all the nurses in Stepping Hill Hospital.”
Matron for Dementia Care, Florence Bawak
Nursing in the Present
A Prole of Florence Bawak, Matron for Dementia Care
at Stockport NHS Foundation Trust, Stepping Hill Hospital

A publication in celebration of the Royal College of Nursing’s centenary year page 19
by Florence Bawak
A Day in the Life of a Matron for Dementia Care
“A typical day for me starts at about 9am with
the completion of the FAIR (Find,Assessand
Investigate, Refer) assessments. This is an
assessment completed for all patients who are 75
and above who have had an emergency admission
to hospital. The purpose of this assessment is to
raise awareness about dementia by giving people
an opportunity to talk about any concerns they
have had about their memory. This is a valuable
assessment as, people in this age group, are
considered a high risk group for developing
dementia. The assessment also identies patients
with a diagnosis of dementia and those in an acute
state of confusion (delirium).
“I enjoy this part of my job very much because I get to
meet some very interesting and knowledgeable people.
It is also often very reassuring when patients talk about
some of their concerns around their memory and get
some relief following a memory assessment test that,
what they are going through is not the beginning of
dementia. Completing these assessments is the most
structured part of my day.
“Whilst walking round the wards completing these
FAIR assessments, I am often approached by staff with
concerns about a patient with a diagnosis of dementia.
Most of the time I discuss the patient with them straight
away and, where possible, see the patient at the same
time and set up a plan for the nurses.
“However, today this is not the case, I received a bleep
from a ward prior to commencing my FAIR assessments
and organised to get there for 12.30pm to meet with a
relative to discuss concerns and offer support. At 1pm
it is time to go and deliver dementia awareness training
to our preceptorship nurses. These are newly qualied
nurses. We start off as always with the icebreaker and
they are keen to contribute. Training lasts for one hour
allowing time for questions.
“It is now 2.04pm and I am late to deliver an update
on dementia care to the patient health and quality
committee. I rush there to discover I am 36 minutes
early. This gives me time to look through my talking
points to refocus. Time goes by quickly and it is now
time to talk to the committee. We go through the
dementia strategy and how we are achieving it with
examples of practice. The talk is a success and I am
promised the committee’s support if required at any time
to support our dementia initiatives.
“It is now 3pm and I still have one appointment on the
ward to speak with a member of staff who is nding
it difcult to support patients with dementia who
are acutely unwell alongside other complex patients
receiving end of life care on a busy 34 bedded ward.
“Arriving on the ward I am met by the ward manager.
They have had a total of four patients with a diagnosis
of dementia transferred to the ward today. One of them I
know very well and have been supporting on a previous
ward. This patient worked as a matron in older people’s
medicine and most of her communication now centres
on her job. She is frustrated she is no longer able to
walk; is in pain and is adjusting to having a catheter. As
a result she is convinced she is having a baby.
“The ward staff have offered her a doll which is helping
at the moment to keep her settled. I now talk to the
nurse I had originally come to see on the ward. I leave
the ward at 4.15pm and head back to the ofce. My
head is buzzing so I spend some time debrieng about
the events of the past 4 hours with my colleague.
“Debrief over, I realise I have a voicemail and I pick it up,
it was a member of a community team returning my call.
She needs some information about a patient in their care.
I ring her back, nd out what she needs, and set about
phone calls to acquire this information. It is 4.45pm when
I contact the community team, and give them a verbal
response to their query and then send them the required
information via fax.
“It is now 5pm and it is time for me to go home, I check
my diary for tomorrow and sign off my computer, ready
to pick up everything again tomorrow. I am happy with
the day I have had and it is now time to see my family.”

page 20 Celebrating 100 years of excellence • Nursing past, present and future
Nursing in the Present
A nurse who has led innovative bereavement and
donor work in Greater Manchester and shared it
across the country has been awarded the MBE
in the Queen’s Birthday Honours. Fiona Murphy,
Assistant Director of Nursing for Bereavement and
Donor Support at Bolton, Salford and Wigan, has
dedicated much of her 30 year nursing career to
caring for dying patients and their families.
Fiona - winner in 2011 of the Nursing Standard Nurse of
the Year award and Lancashire Life Woman of the Year–
began this work in 2002 at the Royal Bolton Hospital as
Donor Liaison Sister.
She is now the driving force behind the Royal
Alliance Bereavement and Donor Service, a nurse-led
innovation that has transformed practice across three
large foundation trusts, Salford Royal, Bolton, and
Wrightington, Wigan and Leigh.
The pioneering work has dramatically improved end of
life care and successfully promotes patient choice and
dignity. Fiona has spoken about bereavement work at
many national conferences and is currently shortlisted
in the national Patient Safety Awards in the category for
Clinical Leadership.
Fiona said: “I’m proud of each and every healthcare
professional who has played their part in breaking down
some of the barriers in caring well for the dying and
the dead. For me, this is testament that we are getting
somewhere in getting it right for every patient every
time.”
The three trusts’ bereavement teams provide support
to patients and their families during the last hours of life
and immediately after death.
They regularly pull out all the stops to make a dying
patient’s wishes come true including hosting birthday
parties at the bedside and they have even arranged
for some pets to make a special visit to hospital. They
offer relatives the opportunity to have locks of hair or
handprints of their loved ones.
Pioneering nurse Fiona is awarded MBE
at Bolton NHS Foundation Trust
“I am overwhelmed
and delighted to
receive this accolade
for our services
to nursing and
bereavement care. I
feel truly humbled.”
Fiona Murphy

A publication in celebration of the Royal College of Nursing’s centenary year page 21

page 22 Celebrating 100 years of excellence • Nursing past, present and future
Nursing in the Future
How research has changed the face of nursing
Lady Jacqueline A Pirmohamed, the Chief
Operating Ofcer of North West Coast NIHR Clinical
Research Network (CRN), went into nursing as she
wanted to do a job that she felt added some value
and support to people, at a time in their life when they
needed it most.
She said that no two days as a research nurse will
be the same. The NIHR CRN is the research arm of
the NHS and employs thousands of research nurses
across the NHS, covering all specialties and disease
areas. The role of the research nurse is typically
involved from the outset of a patient’s research journey.
Lady Jacqueline said: “Research nursing is a key focus
in the UK today; the Royal College of Nursing has a
Research Society Forum with 5,000 members. Most
importantly research nurses in the year 2015/16 alone,
working across the NIHR, have helped to recruit over
605,000 people into clinical research studies, with
more than 3 million patients recruited since 2008, as
reported in the Guardian in 2014.
“In addition 100% of NHS Trusts and 42% of GP
practices now regularly participate in clinical research.
Without research nurses this simply would not happen.
As a profession we should stand proud that we have
all helped this to happen to benet patients. There has
never been a more exciting time to embark on a career
in research as a nurse.”
"Florence Nightingale
was considered to
be an early pioneer
of research nursing
which is often
overlooked. In a
book which contains
many of her own
records from the
Crimean War it can
be seen how she
relentlessly pursued
new knowledge and
used evidence based
frameworks to try and
influence change"
L McDonald, 2010
at North West Coast NIHR Clinical Research Network (CRN)
Lady Jacqueline A Pirmohamed & Matron Sarah Dyas
A publication in celebration of the Royal College of Nursing’s centenary year page 23
How research has changed the face of nursing
Research Nurse Matron Sarah Dyas went into nursing
because she wanted to do something that would make a
difference to people’s lives. She believes that the qualities
a nurse needs are essentially - care and compassion,
but also stoicism, patience and ability to remain calm
in urgent situations. Prioritisation, efciency and good
organisational skills are needed, but can be learned
Sarah thinks that the role of a nurse is to be patients’
advocate at all times - ensuring that they are fully
informed of their condition, the treatment options
available and procedures involved; providing clinical care
to a high standard; anticipating their needs; providing
a calm, clean and efcient environment and supporting
them emotionally throughout their period of sickness
Over the last 100 years, Sarah thinks that the role of the
nurse has extended considerably as nurses have taken
on more responsibilities, initially to relieve junior doctors
– (venepuncture, cannulation, minor surgical roles –
suturing, prescribing). As a result, nurses have become
more autonomous, moving into Nurse Specialist,
Advance Nurse Practitioner and Nurse Consultant roles.
Sarah said: “In my current role as Research Nurse
Matron for the Network, my favourite part is working
alongside the research staff in the ‘Task Force’ team,
either in clinical supervision or in discussing research
studies to ensure their most effective delivery. The most
challenging is trying to keep clinicians happy whilst
juggling staff resources within the Network to meet the
needs of the research portfolio. It is like being a gloried
PA!”
No day is the same for a research nurse. They might be
visiting clinics to approach patients for their participation
in a study. Otherwise, they might be conducting study
visits for patients already recruited to studies; screening
patients to determine their eligibility for studies; entering
data for visits already completed; addressing queries
raised by the sponsor on data already entered; having
meetings with Principal Investigators for the studies;
liaising with the sponsors for studies; updating study
master les; looking at protocols for potential future
studies to determine their feasibility; attending /
presenting at MDT or Grand Rounds on studies being
undertaken.
Sarah spoke about how research nursing has changed
over the decades, mainly the use of technology. Most
sponsors use electronic data bases. These systems
can identify simple errors in transcription from source
data which can be resolved easily at site. Electronic
data bases allow sponsors to monitor studies more
effectively in terms of recruitment rates, adverse events
and to recognise early trends in a study.
Technology is also being introduced to studies with
patients entering their own data through the use of
smartphones and iPads. Patients then enter details of
changes in their condition in real time, for example, the
worsening of a respiratory condition - and according
to the data they have already input onto the device,
it will advise them how to treat it – without having to
consult their GP. This has huge implications for patients,
empowering them to be in control of their symptoms.
Treatments/ therapies are becoming more tailored to the
individual, through pharmacogenetics, which enables
dosages to be predetermined and helps reduce adverse
effects and patients are much more informed.
"The research that
we are doing is in
response to changes
in demography, social
trends and public
health concerns. It is
a dynamic and varied
environment in which
to work."

page 24 Celebrating 100 years of excellence • Nursing past, present and future
Nursing in the Future
Nursing in the 21st Century from a student perspective
"My training has
inspired me for the
future and shown
me what is possible,
though it can be very
daunting and difficult
to integrate yourself
into a new team on
each placement."
Gareth McLean is a third year student at Liverpool
John Moores University. The 30-year-old who hails
from Leeds, previously studied for a degree in English
Literature. He is also the RCN North West Region
Student Committee Representative. During this time, he
carried out some voluntary work with a church group
which took a group of older people and people with
disabilities on pilgrimage to Lourdes in France.
Gareth said: “I really enjoyed it and found it extremely
rewarding, and one of the nurses who worked in the
hospital that the pilgrims were staying in said that I had
a good manner with them and should consider a caring
profession. When I left university the rst time I applied
for a job as a support worker and I haven’t looked back
since. In my opinion, nursing is both the hardest and
most rewarding profession you can do.”
He thinks that overall, a nurse primarily needs good
communication skills and empathy adding: “We
often encounter people during a really traumatic and
distressing time in their lives. Often, what patients
remember most are the kind words of a nurse or
someone who seems to understand what they are
going through. Good communication between patients
and nurses which is built on honesty and openness can
be the rst step in building a trusting relationship.”
Gareth believes that primarily, the role of a nurse is to be
an advocate for their patients and service users and that
it is important for nurses to have the courage to stand
up when they see something that they don’t believe is
right or when they don’t think their patients are receiving
the care that they deserve.
He said: “I think that the role of the nurse is to be a
constant for the patient; the person that they can go to
with concerns or ask advice of; the person that doctors
and other professionals can ask questions of.”
Gareth told the RCN that he thinks nurses’ roles have
become more specialised and nurses nd themselves
carrying out tasks which might have been reserved for
doctors. This can make the role even more fullling but

A publication in celebration of the Royal College of Nursing’s centenary year page 25
with an increased role comes increased responsibility
and accountability. Although the specics of a nurse’s
role have changed, they remain that bridge between the
medical professionals and the patient.
However, like most nursing students, he thinks that the
most difcult part is juggling academic work, practice
work and then usually part-time agency work adding:
Often student nurses are working 30 hours a week on
placement, completing assignments in the evenings
and then working part-time at weekends to make ends
meet.”
An average day for Gareth involves attending the
morning handover meeting, before his mentor gives
him a rundown of the people they will be seeing that
day. As a third year student, Gareth has his own small
caseload of settled patients to work with. He is currently
helping one person access employment services and
he is encouraging another to engage with community
activities to aid their recovery.
Gareth said: “I still get the butteries of anxiety and
excitement as I near the hospital that I will be working in
that day! After work I get home and spend a couple of
hours working on assignments and then read for a bit
before getting an early night.”
He feels strongly about the changes to student
bursaries and believes that this will have an impact
on the future of the nursing profession. Gareth said:
“The problem is that the majority of student nurses are
‘mature’ students and many of these already have a
degree in another subject. This means that they will
likely already have student loan debt and might be more
likely to have dependents and nancial constraints such
as mortgages. This means they would likely be put off
by having to take on more debt by taking out another
student loan. What it also means of course, is that
student nurses are much more likely to have invaluable
life experiences.”
Gareth strongly believes that the services available for
those living with dementia and the support given to
families and carers could be improved. He feels that
families and carers are our greatest asset in providing
personalised care and services should be working more
collaboratively with these people; service users and
families/carers should be at the centre of the team.
A snapshot of our future…
Louise Bennett
1
, 30, University of Chester
(Leighton site), Future employment: Mid
Cheshire Hospital, Stroke Ward
Marta Quilliam
2
, 34, study at University
of Chester (Clatterbridge site), Future
employment: Hoping to work at Countess of
Hospital, Chester - Fertility Clinic, or Liverpool
Women’s Hospital – Embryology
Gillian Heath
3
, 41, University of Manchester, Future employment:
Tameside & Glossop Integrated Care NHS Foundation Trust -
Women’s Health Unit
Katie Sutton
4
, 29, University of Salford, Future employment:
Calverton Hill, Nottingham (thanks to an RCN Jobs Fair!)
Louise Ranger
5
, 20, University of Liverpool, Future
employment: Hoping to be working in an acute setting such as a
surgicalassessment unitin the Liverpool area
1 2
4
3
5

Royal College of Nursing North West Region
Chesham House
St George’s Square
Bolton
BL1 2HB
Telephone: 0345 7726100
Email: northwest.region@rcn.org.uk
Website: www.rcn.org.uk/northwest
Facebook: https://www.facebook.com/RCNNorthWest/
Twitter: @Estephanie_RCN
