
This guide will lead you through the steps to connue your
insurance aer leaving acve employment and explain which
included forms you must complete.
Your member status
Years of service you need to continue
insurance at retirement
•
When you leave acve employment, you are
given a member status based on your vesng
right with a state funded rerement system or
your years of employment service. There are
four member status categories:
• Vested – You have worked long enough to
keep insurance benets and you contributed
to a rerement system, but you are not ready
to draw your rerement benets.
• Non-vested – You have worked long enough
to keep insurance benets, but you did
not contribute to a rerement system that
parcipates with the Employees Group
Insurance Division, or you withdrew your
contribuons from your rerement system.
• Reree – You have worked long enough to
leave acve employment, keep insurance
benets and draw your rerement benets.
• Defer – You have worked long enough to
qualify as a vested, non-vested or reree
member, but you elect to transfer your
health, dental or vision insurance to your
spouse’s current insurance through EGID.
If you leave acve employment, lose coverage
because of reduced hours or your employment
is terminated for reasons other than gross
misconduct, you can connue health, dental and
vision coverage for up to 18 months under the
Consolidated Omnibus Budget Reconciliaon Act.
Coverage connued under COBRA is temporary.
You are encouraged to retain your insurance
benets in a vested, non-vested, reree or defer
status if you meet the qualicaons.
• Teachers' Retirement System (TRS) – Ten
years minimum of creditable service.
• Oklahoma Public Employees Retirement
System (OPERS) – Eight years minimum of
creditable service.
• Oklahoma Law Enforcement Retirement
System (OLERS) – Eight years minimum of
creditable service.
• Oklahoma Pathfinders Plan – Five years
minimum of creditable service.
• Other or no retirement system – Employment
years may qualify as creditable service to
continue insurance. Contact EGID Member
Services for specific information.
Plan premiums
Refer to the premium rate charts in this guide.
Premium payment opons
• Rerement check deducon – Your monthly
premium for the previous month's coverage is
automacally withheld from your rerement
check. When selecng this opon, the
premium withheld is for the previous month's
coverage.
• Direct bill – You are directly billed for your
monthly premium due by the 20th of each
month.
• Automac dra – Your monthly premium
is automacally draed from your checking
account on or around the 20th of each month.
To elect this opon, select the direct bill
opon on the Applicaon for Reree/Vested/
Non-Vested/Defer Insurance Coverage (Page
A2) and provide EGID an Electronic Fund
Transfer Authorizaon and a voided check.
This form (Page D1-D2) is available on the
EGID website or by contacng member
services.
2

Retirement system contribution to your
monthly insurance premium
Your rerement system may contribute toward
your health insurance premium.
• TRS contributes between $100 to $105
monthly.
• OPERS contributes $105 monthly.
• OLERS contributes $105 monthly.
• Pathnders does not contribute.
The premiums listed in this guide do not reect
any rerement system contribuon.
When you leave
active employment
Keep all the coverage you think you will need
in rerement. You can drop or reduce benets
later, but you cannot add health, dental or life
insurance aer you leave acve employment.
Rerement is not a qualifying event that allows
you to make plan changes unless you or your
covered dependent is Medicare eligible. All
covered dependents must enroll in the same
plan. For example, if you are enrolled in an MAPD
plan, your pre-Medicare dependents must enroll
in the HMO opon of that plan. If you move
out of your health plan’s service area, you are
allowed to change health plans within 30 days of
your move.
EGID Administrave Rule 260:50-3-13 (h)
states that you must return to work for an EGID
parcipang employer for three years to qualify
to retain benets not elected upon ceasing
current employment.
If your employer oers these benets through
EGID, the following rules apply:
Health and dental insurance – You can add,
keep, drop or defer coverage within 30 days of
leaving acve employment.
Vision insurance – You can add, keep, drop or
defer coverage within 30 days of leaving acve
employment or during the annual Opon Period.
Once you leave acve employment, vision
insurance is the only benet that can be added
during the annual Opon Period.
Life insurance – You can keep, reduce or drop
life coverage you have in place at the me
you leave acve employment. You must make
the elecon within 30 days of leaving acve
employment. You cannot add or increase life
insurance at rerement. Life insurance cannot
be deferred and must be kept in your rerement
account.
Life insurance must be kept in $5,000 units.
Refer to the premium charts included in this
guide.
Life insurance connued at rerement does not
include Accidental Death and Dismemberment
benets.
If you connue life insurance coverage when you
leave acve employment, it is very important
to keep your beneciary informaon current. If
you are unsure of your beneciary designaons,
please complete the Beneciary Designaon
Form (Page E1). Instrucons are on the back of
the form.
HealthChoice must pay life benets to the
beneciaries listed on the most recent beneciary
designaon. If there is no signed beneciary
designaon, benets are paid to the estate.
Coverage for your dependents
You can add, keep or drop health, dental and
vision coverage for your spouse and other
eligible dependents at rerement; however,
dependent life insurance must be in eect
before you leave acve employment. Dependent
coverage must be with the same carrier as the
member.
3

You can exclude your spouse from health, dental
and vision coverage and cover your other eligible
dependents. Your spouse must sign the Spouse
Exclusion Cercaon secon of the Applicaon
for Reree/Vested/Non-Vested/Defer Insurance
Coverage (Page A2).
If you add or keep coverage for your dependent
children, including disabled dependents, you
must cover all your eligible dependents up to
age 26.
You can exclude dependents from coverage
if they have other group coverage or are
eligible for Indian Health Services or military
health benets. You can also exclude eligible
dependents who do not reside with you, are
married or are not nancially dependent on you.
Aer rerement, you cannot add dependents
to any coverage except vision, unless one of the
following qualifying events occurs:
• Birth of a child.
• Your spouse or eligible dependents lose other
group coverage.
• You marry.
• You adopt or gain legal guardianship of a child
under age 26.
You must add your spouse and any eligible
dependents within 30 days of the qualifying
event.
Dependent life insurance
You can keep dependent life insurance in eect
at rerement but cannot add or increase it later.
It must be kept in $500 units and each covered
dependent pays a separate, individual premium.
• For your spouse – The amount you keep for
your spouse can be dierent from the amount
you keep for your covered dependents.
• For your dependents – The amount you
keep must be the same for each covered
dependent.
Surviving Dependents
In the event of your death, your surviving
dependents may connue their insurance
coverage. A surviving spouse can connue their
insurance benets, including Dependent Life,
as long as the premiums are paid. The spouse
will be moved to their own account and pay the
primary member rate.
Surviving dependent children can also connue
coverage, including Dependent Life, unl age 26.
A leer will be sent by EGID to your surviving
dependents advising them of their opons.
Dependents have 60 days to nofy EGID that
they wish to connue insurance coverage.
If you decide to work past age 65
If you decide to work past age 65, you may
contact Social Security to delay your enrollment
in Medicare Part B. Your employer insurance
will be primary payer while working. Since all
insurance oered through EGID is creditable
coverage, you will not be assessed a penalty
once employer insurance ends.
When you turn age 65 after you leave
active employment
If you are close to age 65 and are not receiving
Social Security benets, you need to enroll in
Medicare Part A and Part B.
To enroll, contact Social Security at least three
months before you turn age 65. By enrolling
early, you avoid any delay in the start of your
Medicare coverage.
COBRA
To comply with federal guidelines, a COBRA
packet will be mailed to you when you leave
employment. Do NOT complete this packet if
you are elecng to connue your insurance
coverage as a Former Employee
4

The Enrollment Process
If you are not yet
eligible for Medicare
To connue your insurance
You must complete the Applicaon for Reree/
Vested/Non-Vested/Defer Insurance Coverage
(Page A1) and return it to EGID.
To defer (transfer) your coverage to your
spouse’s plan
If your spouse works and is currently enrolled
in coverage through EGID, you can transfer
your health, dental and vision coverage to your
spouse’s coverage as a dependent.
Life insurance cannot be deferred and must be
kept in your rerement account.
To transfer your coverage to your spouse’s plan:
• Mark Defer on the Applicaon for Reree/
Vested/Non-Vested/Defer Insurance Coverage
(Page A1-A2) and return it to EGID.
• Your spouse must contact their employer to
add you to their coverage as a dependent.
• Any rerement system contribuon paid
toward your health insurance premium will
not be paid during the deferral period.
As long as your former employer group connues
to parcipate with EGID, you can transfer your
coverage back to your own EGID account at any
me by compleng the Applicaon for Reree/
Vested/Non-Vested/Defer Insurance Coverage.
If you are eligible for Medicare
About Medicare
Medicare is the federal health insurance
program for people age 65 or older, people
under age 65 with certain disabilies and those
with end-stage renal disease or amyotrophic
lateral sclerosis.
• Medicare Part A pays for hospitalizaon
services.
• Medicare Part B pays for doctor and
outpaent medical services. Call Social
Security for informaon on your Part B
premiums. Refer to Contact Informaon at
the back of this guide.
• Medicare Part D pays for prescripon drug
coverage. All the plans oered through EGID
provide Part D coverage. This means the
plans all meet the benet guidelines set by
Medicare for creditable prescripon drug
coverage.
Your enrollment in Medicare is handled in one
of two ways:
• Automac enrollment (depending on your
individual circumstances).
• Applicaon for enrollment. You should apply
three months prior to turning 65 to avoid a
possible delay in the start of your coverage.
Contact Social Security for more informaon.
5

To connue your insurance and enroll in a
Medicare supplement or MAPD plan
There are two forms you must complete to
connue your health coverage:
• The Applicaon for Reree/Vested/Non-
Vested/Defer Insurance Coverage (Page A1).
• You must also complete the form associated
with the plan you are enrolling in – the
Applicaon for Medicare Supplement With
Prescripon Drug Plan or the Applicaon
for Medicare Advantage Prescripon Drug
(MAPD) Plan.
Refer to Page 9 for the available Medicare plans.
To enroll in a Medicare supplement plan
A Medicare supplement plan helps pay for
some of the remaining out-of-pocket costs
that original Medicare doesn’t pay, such as
copayments, coinsurance and deducbles. A
Medicare supplement plan is in addion to
original Medicare. To parcipate in a Medicare
supplement plan, you must be entled to
benets under Medicare Part A. EGID has three
Medicare supplement plans. BCBSOK-BlueSecure
requires Part B enrollment to parcipate in
their plan. HealthChoice SilverScript High and
Low Opon Medicare Supplement plans do not
require you to be enrolled in Part B, but pay
benets as if you are.
To enroll in a Medicare supplement plan,
complete and return the Applicaon for Medicare
Supplement With Prescripon Drug Plan (Page
B1). You must provide your Medicare ID number
to coordinate your benets with Medicare.
To enroll in a Medicare Advantage
Prescripon Drug plan
MAPD plans contract with Medicare to provide
benets for Medicare Part A and Part B covered
services, as well as Part D prescripon drug
benets.
You must be enrolled in Medicare Part A and Part
B to be eligible for enrollment. When you enroll
in an MAPD plan, the plan replaces Medicare as
your primary insurer.
To be eligible to enroll in an MAPD HMO, you
must also live in the plan’s approved ZIP code
service area. You can receive services only within
the plan’s network.
To be eligible to enroll in an MAPD PPO, you
may live anywhere in the United States. You can
receive services anywhere in the U.S. as long as
the provider is a Medicare eligible provider and
accepts the plan’s payment terms and condions.
To enroll in an MAPD plan, you must complete
and return the Applicaon for Medicare
Advantage Prescripon Drug (MAPD) Plan
(Page C1). Be sure to provide your Medicare ID
number on your applicaon.
Enrollment deadline
If you are not eligible for Medicare
EGID Administrave Rules allows 30 days from
the day your acve insurance ends to elect to
begin or connue your insurance.
Failure to add, keep or defer coverage within
30 days of your acve coverage ending cancels
eligibility in the plans oered through EGID.
If you are eligible for Medicare
It is important that your applicaon is received
at least 30 days prior to the day you leave acve
employment. This gives EGID enough me to
process applicaons and resolve problems before
coverage is eecve. It also prevents delays in
enrolling in a Part D prescripon drug plan.
If your applicaon is not received prior to your
employment terminaon, you may be enrolled in
a HealthChoice Medicare supplement plan that
includes creditable prescripon drug benets, but
not Part D prescripon drug benets, unl the
rst of the following month. This is to prevent you
from having a break in coverage. Be aware the
premium for this temporary plan is higher.
6

Plan ID cards
Confirmation statement
If you enroll in a Medicare plan through EGID, a
new ID card will be issued. Do not destroy your
current cards unl you receive your new ones.
If you move outside
your plan’s service area
If you are not eligible for Medicare
If you are enrolled in an HMO plan and move
outside your plan’s ZIP code service area, you
must nofy EGID in wring of your new address.
To connue your health coverage, you will need
to select a new plan that is in your service area.
If you are eligible for Medicare
If you are enrolled in an MAPD HMO plan and
move outside your plan’s ZIP code service
area, you must contact EGID to disenroll. To
change your coverage to a plan including Part D
prescripon drug benets, you must complete
an Applicaon for Medicare Supplement With
Prescripon Drug Plan or an Applicaon for
Medicare Advantage Prescripon Drug (MAPD)
Plan.
Address information
It is important to keep your mailing and email
addresses current, or you risk delaying claims
processing or missing important communicaons.
Medicare requires that you report any change in
your home address to your insurance plan.
Contact EGID Member Services for a Change of
Address form, or submit a wrien request to:
EGID
P.O. Box 11137
Oklahoma City, OK 73136-9998
You can email your signed form to
[email protected]. Verbal requests for
address changes are not accepted.
When you enroll as a former employee or make
changes to your coverage, EGID mails you a
conrmaon statement which lists the coverage
you are enrolled in, the eecve date of your
coverage and the premium amounts.
Check it carefully. If incorrect, immediately
contact EGID Member Services. Correcons
must be submied to EGID within 60 days of
the elecon. Correcons reported aer 60 days
are eecve the rst of the month following
nocaon. Refer to Contact Informaon at the
back of this guide.
Option Period
Aer you leave acve employment, EGID mails
your Opon Period materials directly to you.
To make plan changes, complete your Opon
Period form and return it directly to EGID. Keep a
copy of your form for your records. EGID will mail
you a conrmaon statement.
If you have no plan changes, do not return
your form. You will not receive a conrmaon
statement.
7

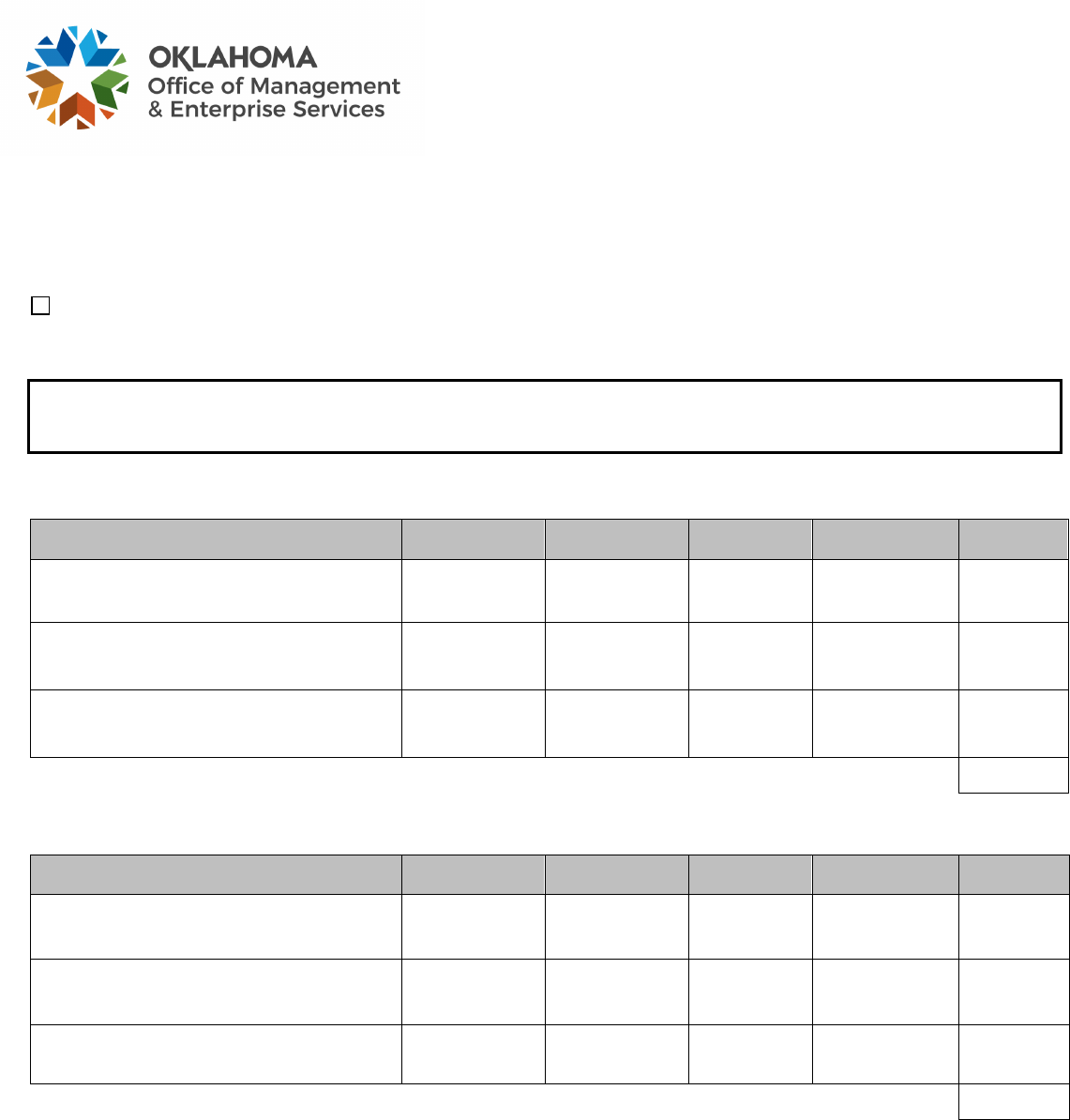
Monthly Premiums for Former Employees
and Surviving Dependents
Plan Year Jan. 1-Dec. 31, 2024
O°ce of Management
& Enterprise Services
HEALTH PLANS MEMBER SPOUSE CHILD CHILDREN
Blue Cross Blue Shield of Oklahoma – BlueLincs HMO
$ 600.78 $ 825.98 $ 556.90 $ 1299.08
CommunityCare HMO
$ 650.06 $ 762.16 $ 326.98 $ 554.88
GlobalHealth HMO
$ 979.42 $ 1445.72 $ 559.30 $ 913.38
HealthChoice High and High Alternative
$ 679.62 $ 796.80 $ 341.86 $ 580.10
HealthChoice Basic and Basic Alternative
$ 543.08 $ 637.32 $ 280.06 $ 473.72
HealthChoice High Deductible Health Plan (HDHP) $ 473.68 $ 556.24 $ 244.66 $ 413.06
BCBSOK – BlueCare Dental High Plan
$ 35.08 $ 35.08 $ 28.44 $ 72.52
DENTAL PLANS MEMBER SPOUSE CHILD CHILDREN
BCBSOK – BlueCare Dental Low Plan
$ 23.84 $ 23.84 $ 20.60 $ 50.40
Cigna Prepaid High (K1I09)
$ 13.56 $ 10.98 $ 8.40 $ 14.44
Cigna Prepaid Low (OKIV9)
$ 10.48 $ 6.80 $ 4.62 $ 10.42
Delta Dental PPO
$ 39.70 $ 39.70 $ 34.54 $ 87.30
Delta Dental PPO – Choice
$ 17.88 $ 40.50 $ 40.80 $ 99.02
HealthChoice Dental
$ 48.58 $ 48.58 $ 39.28 $ 100.74
MetLife High Classic MAC
$ 50.90 $ 50.90 $ 43.62 $ 107.98
MetLife Low Classic MAC
$ 28.90 $ 28.90 $ 24.78 $ 60.94
Sun Life Preferred Active PPO
$ 34.98 $ 34.80 $ 26.12 $ 70.14
Primary Vision Care Services (PVCS)
$ 10.40 $ 9.28 $ 9.20 $ 11.50
VISION PLANS MEMBER SPOUSE CHILD CHILDREN
Superior Vision
$ 7.40 $ 7.34 $ 6.96 $ 14.30
Vision Care Direct
$ 15.48 $ 10.96 $ 10.96 $ 24.48
VSP (Vision Service Plan)
$ 8.62 $ 5.66 $ 5.58 $ 12.22
LIFE PLAN FOR PRE-MEDICARE RETIREES/VESTED MEMBERS
From $5,000 to $40,000 $3.12 Per $1,000 unit
AGE-RATED SUPPLEMENTAL LIFE – Cost per $1,000 unit for $41,000 and up
<30
–
$0.06
45-49
–
$0.14
65-69
–
$0.74
30-34
–
$0.06
50-54
–
$0.26
70-74
–
$1.28
35-39
–
$0.06
55-59
–
$0.40
75+
–
$1.96
40-44
–
$0.08
60-64
–
$0.46
Spouse
Child (live birth to age 26)
$ 6,000 of coverage
$ 3,000 of coverage
$ 10,000 of coverage
$ 5,000 of coverage
$ 20,000 of coverage
$ 10,000 of coverage
DEPENDENT LIFE
$1.56 per $500 unit, per dependent
MONTHLY LIFE INSURANCE PREMIUMS FOR SURVIVING DEPENDENTS
Surviving Dependents of Current Employees Low Option $2.60 Standard Option $4.32 Premier Option $11.26
Surviving Dependents of Former Employees $1.56 per $500 unit, per dependent
These rates do not reect any retirement system contribution.
4951
8

Monthly Premiums for
Medicare Eligible Members
Plan Year Jan. 1-Dec. 31, 2024
O°ce of Management
& Enterprise Services
MEDICARE SUPPLEMENT PLANS
BCBSOK – BlueSecure
SM
$ 466.02 per covered person
HealthChoice SilverScript High Option Medicare Supplement
$ 437.00 per covered person
HealthChoice SilverScript Low Option Medicare Supplement
$ 356.06 per covered person
MEDICARE ADVANTAGE PRESCRIPTION DRUG (MAPD) PLANS
BCBSOK – MAPD
$ 238.40 per covered person
CommunityCare Senior Health Plan
$ 215.64 per covered person
Generations by GlobalHealth
$ 199.00 per covered person
Humana MAPD PPO
$ 192.92 per covered person
DENTAL PLANS MEMBER SPOUSE CHILD CHILDREN
BCBSOK – BlueCare Dental High Plan
$ 35.08 $ 35.08 $ 28.44 $ 72.52
BCBSOK – BlueCare Dental Low Plan
$ 23.84 $ 23.84 $ 20.60 $ 50.40
Cigna Prepaid High (K1I09)
$ 13.56 $ 10.98 $ 8.40 $ 14.44
Cigna Prepaid Low (OKIV9)
$ 10.48 $ 6.80 $ 4.62 $ 10.42
Delta Dental PPO
$ 39.70 $ 39.70 $ 34.54 $ 87.30
Delta Dental PPO – Choice
$ 17.88 $ 40.50 $ 40.80 $ 99.02
HealthChoice Dental
$ 48.58 $ 48.58 $ 39.28 $ 100.74
MetLife High Classic MAC
$ 50.90 $ 50.90 $ 43.62 $ 107.98
MetLife Low Classic MAC
$ 28.90 $ 28.90 $ 24.78 $ 60.94
Sun Life Preferred Active PPO
$ 34.98 $ 34.80 $ 26.12 $ 70.14
Primary Vision Care Services (PVCS)
$ 10.40 $ 9.28 $ 9.20 $ 11.50
VISION PLANS MEMBER SPOUSE CHILD CHILDREN
Superior Vision
$ 7.40 $ 7.34 $ 6.96 $ 14.30
Vision Care Direct
$ 15.48 $ 10.96 $ 10.96 $ 24.48
VSP (Vision Service Plan)
$ 8.62 $ 5.66 $ 5.58 $ 12.22
LIFE PLAN
From $5,000 to $40,000 $3.12 Per $1,000 unit
AGE-RATED SUPPLEMENTAL LIFE – Cost per $1,000 unit for $41,000 and up
<30
–
$0.06 30-34
–
$0.06 35-39
–
$0.06 40-44
–
$0.08
45-49
–
$0.14 50-54
–
$0.26 55-59
–
$0.40 60-64
–
$0.46
65-69
–
$0.74 70-74
–
$1.28 75+
–
$1.96
DEPENDENT LIFE
$1.56 per $500 unit, per dependent
These rates do not reect any contribution from your retirement system.
4952
9

10
*FORMER*
Employees Group Insurance Division
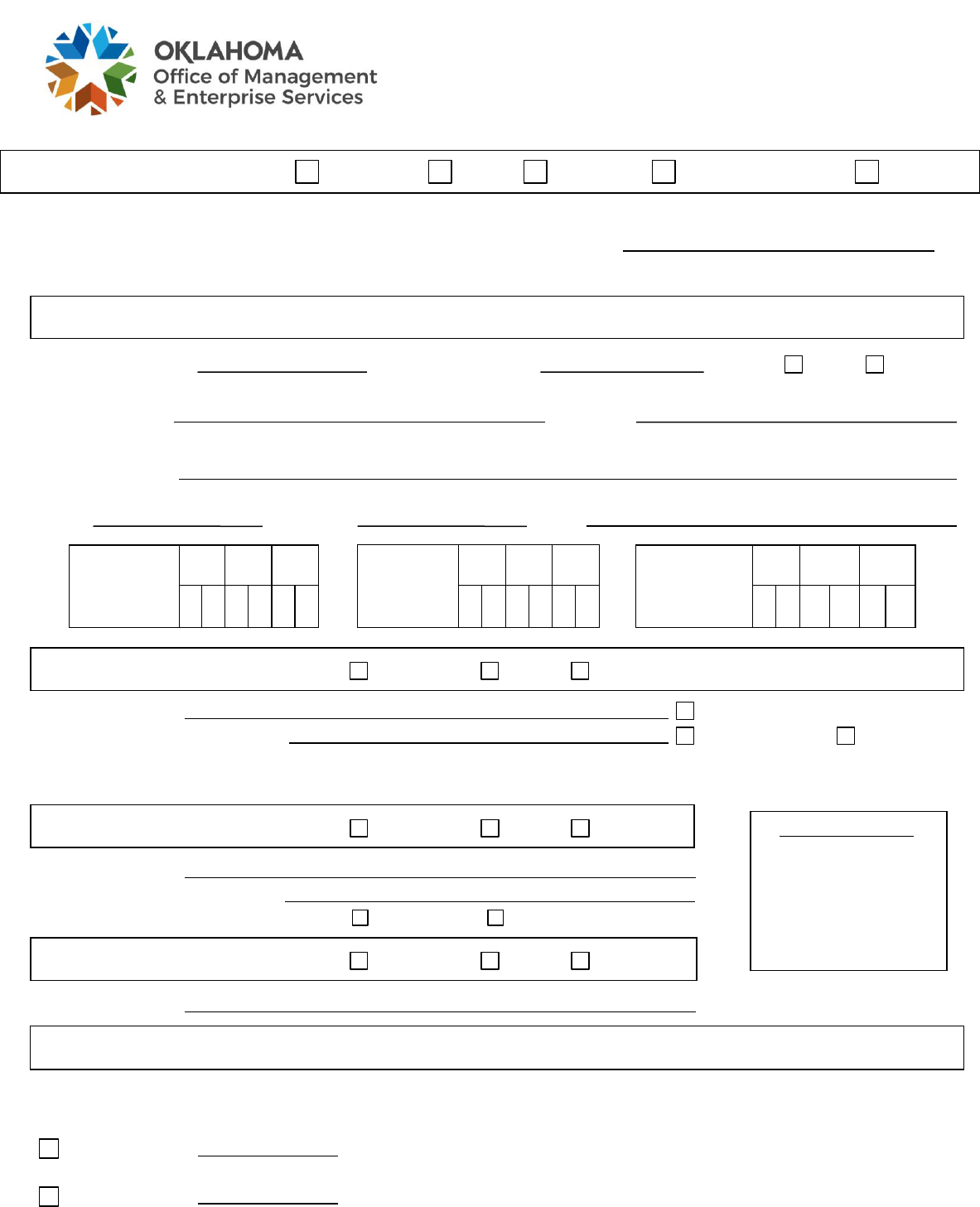
APPLICATION FOR RETIREE/VESTED
NON-VESTED/DEFER INSURANCE COVERAGE
RETIREMENT SYSTEM OPERS TRS OLERS PATHFINDER OTHER
My member status will be Retiree Vested Non-vested Defer (See instructions on page 3.)
For defer only: Spouse’s Social Security number or member ID number
Cancel my deferment and reinstate my retiree/vested/non-vested insurance coverage.
MEMBER INFORMATION
SSN or member ID Member’s birth date Gender Male Female
Member’s name Employer
First M.I. Last
Mailing address
Street City State ZIP code
Phone Alt. phone Email
Last date of
employee
insurance
coverage
Mo.
Day
Yr.
Vested/
non-vested
Mo.
Day
Yr.
Retirement
Insurance
Mo.
Day
Yr.
insurance
effective date
0
1
effective
date
0
1
MEMBER HEALTH PLAN Add/keep Drop Defer
Health plan name Check if Medicare-eligible*
Primary physician (HMO only) Current patient New patient
* If you and/or your dependents are eligible for Medicare, an additional application must be completed. Please
contact EGID Member Services to request an application.
For EGID Use Only
MEMBER DENTAL PLAN Add/keep Drop Defer
Dental plan name
Primary dentist (Prepaid only)
Current patient New patient
MEMBER VISION PLAN Add/keep Drop Defer
Vision plan name
MEMBER LIFE INSURANCE
You can keep a minimum of $5,000 up to the total amount of your current life insurance. You cannot enroll in more life insurance than you
currently have. You must keep life insurance on yourself to be able to keep life insurance on your dependents. You cannot increase life
insurance after this election. Life insurance cannot be deferred and must be carried as a primary retiree/vested member.
I elect to keep $ ($5,000 to $40,000 in $5,000 units) of member life insurance at a
flat rate per $1,000 of coverage.
I elect to keep $ (amount above $40,000 in $5,000 units) of additional life insurance.
Revised 12/29/2021
A1

DEPENDENT INFORMATION
NOTE: If you and/or your dependents are eligible for Medicare, an additional application must be completed.
Please contact EGID Member Services to request an application. You cannot add dependent life if you do not
already have it. The dependent life amount must be the same for each child, though the amount for your spouse
can be different.
SPOUSE
Name Check if Medicare-eligible.
Add/keep Drop SSN Date of birth Male Female
Health Primary physician (HMO only) New patient Current patient
Dental Primary dentist (Prepaid only) New patient Current patient
Vision
Dep. life I elect to keep $ (in $500 units) of dependent life insurance.
Does your spouse currently have coverage through OMES EGID? Yes No
(If yes, list name and Social Security number above.)
CHILD
Name Check if Medicare-eligible.
Add/keep Drop SSN Date of birth Male Female
Health Primary physician (HMO only) New patient Current patient
Dental Primary dentist (Prepaid only) New patient Current patient
Vision
Dep. life I elect to keep $ (in $500 units) of dependent life insurance.
CERTIFICATION SIGNATURES
I authorize EGID to deduct the amount of my premiums from my retirement check according to Administrative
Rule 260:50-3-5. (You must verify with your retirement system that your retirement check will cover your
premiums.)
I request EGID direct bill me for my monthly premiums at the mailing address on this form.
Spouse must sign if being excluded from health, dental and/or vision or if they are a common-law spouse.
Spouse exclusion certification: I certify that I am aware I am being excluded from health, dental and/or vision
coverage as indicated on this form. I am also aware that I cannot be added to coverage at a later date except
within 30 days of the loss of other coverage. (Required only if children are covered and spouse is not.)
Common-law spouse certification: I certify the person listed as my spouse and I have an actual and mutual
agreement between ourselves to be married; that this is a permanent relationship; that our relationship is
exclusive, as proven by our cohabitation as spouses; and that we do hereby hold ourselves out publicly as
married. I am aware this relationship can be dissolved only by legal divorce.
Spouse signature
Date
I understand that no coverage, except vision, can be added at a later date.
Member signature Date
A2
Revised 12/29/2021

Retirement information can be found at oklahoma.gov/omes.
You can carry health, dental, vision and life insurance on yourself and your dependents.
The health, dental and life coverage you take into retiree/vested/non-vested status is the only coverage you can have
with EGID through your retirement years. If you do not keep coverage now, you cannot add it later. Plan changes can
be made during the annual Option Period.
If you are insuring one dependent, you must insure all eligible dependents (for any given coverage) unless they are
covered by other insurance or Indian or military benefits. Children who have Indian or military benefits or other
insurance may be required to show proof of coverage.
Following your retirement, dependents can be added only within 30 days of one of the following events: birth,
adoption or guardianship, marriage or loss of other group insurance.
DEFER INSTRUCTIONS: If your spouse has separate coverage through EGID at the time you terminate
employment, you can transfer your individual health, dental and/or vision coverage to dependent coverage under
your spouse’s coverage. Your spouse must contact their employer to add you as a dependent. You must elect to
transfer coverage within 30 days of your termination of employment. Any 30-day break in coverage voids your
eligibility to keep coverage in the future. Life insurance cannot be deferred and must be carried as a primary
retiree/vested/non-vested member. When you are ready to return to retiree/vested/non-vested status, you must again
complete this form and mark the box on Page 1 of your form to cancel your deferment.
THINGS TO CONSIDER AS A RETIREE WHEN YOU BECOME MEDICARE-ELIGIBLE
IMPORTANT: If you are under age 65 and eligible for Medicare, you must notify EGID and provide your
Medicare number as it appears on your Medicare card. Medicare supplement coverage is effective the date you
become eligible for Medicare or the first day of the month following notification of your Medicare eligibility,
whichever is later.
When you turn age 65, you have the option to enroll in either a Medicare supplement with prescription drug plan or a
Medicare Advantage prescription drug plan.
BCBSOK-BlueSecure and all MAPD plans offered through EGID require you to have both Medicare Part A
and Medicare Part B.
If you are eligible and do not enroll in Medicare Part B, there are two Medicare supplement plans available to you:
HealthChoice SilverScript High Option Medicare Supplement Plan and HealthChoice SilverScript Low Option
Medicare Supplement Plan. All medical benefits under these plans are paid as if you are enrolled in both Medicare
Part A and Part B. If you are not enrolled in Medicare Part B, your plan will estimate Medicare’s benefits and
provide supplemental coverage as if Medicare is the primary carrier. This means HealthChoice pays secondary and
you are responsible for the primary share of the claim.
For information concerning HMO, MAPD, Medicare supplement, dental or vision plans, contact their customer
service numbers.
For information regarding enrollment, or to obtain an application for a Medicare supplement plan or
MAPD plan, call 405-717-8780 or toll-free 800-752-9475 or TTY 711 or contact:
OMES Employees Group Insurance Division
P.O. Box 11137
Oklahoma City, OK 73136-9998
Revised 12/29/2021
A3
14

Who can use this form? People with Medicare who want to join a Medicare prescription drug plan.
To join a plan, you must:
• Be a United States citizen or be lawfully present in the U.S.
• Live in the plan’s service area.
Important:
To join a HealthChoice SilverScript Medicare supplement with prescription drug plan, you must have either, or
both:
• Medicare Part A (hospital insurance).
• Medicare Part B (medical insurance).
To join the BCBSOK Medicare supplement with prescription drug plan, you must have both:
• Medicare Part A (hospital insurance) and Medicare Part B (medical insurance).
When do I use this form?
You can join a plan:
• Between Oct. 15-Dec. 7 each year (for coverage starting Jan. 1).
• Within three months of first getting Medicare.
• In certain situations where you’re allowed to join or switch plans. Visit Medicare.gov to learn more about
when you can sign up for a plan.
What do I need to complete this form?
• Your Medicare Number (the number on your red, white and blue Medicare card).
• Your permanent address and phone number.
Reminder:
• If you want to join a plan during fall open enrollment (Oct. 15-Dec. 7), the plan must have your
completed form by Dec. 7.
What happens next?
Send your completed and signed form to:
OMES EGID
P.O. Box 11137
Oklahoma City, OK 73136-9998
Once they process your request to join, they’ll contact you.
How do I get help with this form?
Call EGID Member Services at 405-717-8780 or toll-free 800-752-9475 Monday-Friday, 8 a.m. to 4:30 p.m.
Central time to see if you are eligible to enroll. TTY users call 711. Or, call Medicare at 800-MEDICARE (800-
633-4227). TTY users call 877-486-2048. En español: Llame a EGID al 800-752-9475/TTY 711 o a Medicare
gratis al 800-633-4227 y oprima el 2 para asistencia en español y un representante estara disponible para
asistirle.
Individuals experiencing homelessness
If you want to join a plan but have no permanent residence, a post office box, an address of a shelter or clinic,
or the address where you receive mail (e.g., Social Security checks) may be considered your permanent
residence address.
Rev. August 2023 MSP
B1

*MCENRL*
Employees Group Insurance Division
APPLICATION FOR MEDICARE SUPPLEMENT
WITH PRESCRIPTION DRUG PLAN
Member information
Member name (First MI Last) Member ID
Date of birth
Male Female
Member SSN
Permanent address (P.O. Box not allowed) City State ZIP code
Mailing address (if different from above) City State ZIP code
Phone Alternate phone Email
Dependent information (only if enrolling in Medicare)
Dependent name (First MI Last)
Date of birth
Male Female
Dependent SSN
Your Medicare information (required to process your application)
Name on Medicare card:
Medicare number: - -
Part A effective date:
Part B effective date:
To participate in the BCBSOK Medicare supplement plan, you must be enrolled in both Medicare Part A (hospital) and Part B
(medical) and continue to pay your monthly Part B premium. To participate in the HealthChoice Medicare supplement plans,
you must be entitled to benefits under Medicare Part A. You are not required to be in enrolled in Part B, but the plan pays
Answer these important questions
benefits as if you are. To maximize your benefits, you need to be enrolled in Medicare Part B.
1. In which Medicare supplement with Medicare Part D prescription drug plan do you want to enroll?
HealthChoice SilverScript Medicare Supplement Plan
High Low
BCBSOK – BlueSecure
2. Some individuals may have other drug coverage through private insurance, TRICARE, federal employee
health benefits, VA benefits or state pharmaceutical assistance programs. Will you have other
prescription drug coverage in addition to your coverage through OMES Employees Group Insurance
Division?
Name of other coverage ID# Group#
No
Yes
3.
Typically, you can enroll in a Medicare prescription drug plan only during the annual enrollment period
from Oct. 15 through Dec. 7. Additionally, there are exceptions that may allow you to enroll in a Medicare
prescription drug plan outside of the Annual Enrollment Period. (Refer to statements on Page 2.)
I am enrolling during an Annual Enrollment Period (Option Period).
B2

Read the following statements and check the box if the statement applies to you. By checking any of the
following boxes, you are certifying that, to the best of your knowledge, you are eligible for an enrollment
period. If we later determine that this information is incorrect, you may be disenrolled.
I am new to Medicare.
I recently moved outside of the service area of my current plan. I moved on (insert date):
I recently was released from incarceration. I was released on (insert date):
I recently returned to the U.S. after living permanently outside of the U.S.
I returned to the U.S. on (insert date):
I recently obtained lawful presence status in the U.S. I got this status on (insert date):
I recently had a change in my Medicaid (newly got Medicaid, had a change in level of Medicaid assistance or lost
Medicaid) on (insert date):
I recently had a change in my Extra Help paying for Medicare prescription drug coverage (newly got Extra Help, had a
change in level of Extra Help or lost Extra Help) on (insert date):
I have both Medicare and Medicaid or I get Extra Help paying for my Medicare prescription drug coverage, but I haven’t
had a change.
I live in or recently moved out of a long-term care facility (for example, a nursing home or other long-term care facility).
I moved/will move into/out of the facility on (insert date):
I recently left a PACE program on (insert date):
I recently involuntarily lost my creditable prescription drug coverage (as good as Medicare’s). I lost my drug coverage on
(insert date):
I am leaving employer or union coverage on (insert date):
I belong to a pharmacy assistance program provided by my state.
I was enrolled in a plan by Medicare (or my state), and I want to choose a different plan. My enrollment in that plan
started on (insert date):
I was affected by an emergency or major disaster (as declared by the Federal Emergency Management Agency (FEMA) or
by a federal, state or local government entity. One of the other statements here applied to me, but I was unable to make
my enrollment request because of the disaster.
My plan is ending its contract with Medicare, or Medicare is ending its contract with my plan.
None of these statements apply to me. Call EGID at 405-717-8780 or toll-free 800-752-9475 Monday-Friday, 8 a.m. to
4:30 p.m. Central time to see if you are eligible to enroll. TTY users call 711.
Answering these questions is your choice. You cannot be denied coverage if you don’t
answer.
4. Are you Hispanic, Latino/a, or Spanish origin? Select all that apply.
No, not of Hispanic, Latino/a, or Spanish origin Yes, Mexican, Mexican American, Chicano/a
Yes, Puerto Rican Yes, Cuban
Yes, another Hispanic, Latino/a, or Spanish origin
I choose not to answer.
5. What’s your race?
American Indian or Alaska Native Asian Indian Black or African American
Chinese Filipino Guamanian or Chamorro
Japanese Korean Native Hawaiian
Other Asian Other Pacific Islander Samoan
Vietnamese White
I choose not to answer.
B3

–
–
Signatures Important: Read and sign below
• I must keep Part A or Part B to stay in the plans offered by EGID.
• By joining this Medicare supplement with prescription drug plan, I acknowledge that the Medicare supplement with
prescription drug plans offered by EGID will release my information to Medicare, who may use it to track beneficiary
enrollment, for payment and other purposes applicable to federal statutes that authorize the collection of this information
(see Privacy Act Statement below).
• Your response to this form is voluntary. However, failure to respond may affect enrollment.
• The information on this enrollment form is correct to the best of my knowledge. I understand that if I intentionally provide
false information on this form, I will be disenrolled from the plan.
• I understand that people with Medicare are generally not covered under Medicare while out of the country, except for
limited coverage near the U.S. border.
• I understand that my signature (or the signature of the person legally authorized to act on my behalf) on this application
means I have read and understand the contents of this application. If signed by an authorized representative (as described
above), this signature certifies that:
1) This person is authorized under state law to complete this enrollment.
2) Documentation of this authority is available upon request by Medicare.
Member signature Date
Dependent signature (only if dependent is enrolling in Medicare) Date
If you are the authorized representative, you must sign above and provide this information:
Name Phone
Address
Relationship to enrollee
Mail or fax the form to Attn: Member Accounts
Mail: OMES EGID
Fax: 405-717-8939
P.O. Box 11137
Oklahoma City, OK 73136-9998
2024 monthly premium information does not reflect any retirement system contribution
MEDICARE SUPPLEMENT WITH PRESCRIPTION DRUG PLANS
BCBSOK – BlueSecure $466.02 per covered person
HealthChoice SilverScript High Option Medicare Supplement $437.00 per covered person
HealthChoice SilverScript Low Option Medicare Supplement
Privacy Act Statement
$356.06 per covered person
The Centers for Medicare & Medicaid Services (CMS) collects information from Medicare plans to track beneficiary enrollment in Medicare
Advantage (MA) Plans, improve care, and for the payment of Medicare benefits. Sections 1860D-1 of the Social Security Act and 42 CFR §§
423.30 and 423.32 authorize the collection of this information. CMS may use, disclose and exchange enrollment data from Medicare beneficiaries
as specified in the System of Records Notice (SORN) “Medicare Advantage Prescription Drug (MARx)”, System No. 09-70-0588. Your response
to this form is voluntary. However, failure to respond may affect enrollment in the plan.
If you have questions, call EGID Member Services at
405-717-8780 or toll-free 800-752-9475. TTY users call 711.
B4

Who can use this form? People with Medicare who want to join a Medicare Advantage prescription drug plan.
To join a plan, you must:
• Be a United States citizen or be lawfully present in the U.S.
• Live in the plan’s service area.
Important:
To join a Medicare prescription drug plan, you must also have both:
• Medicare Part A (hospital insurance).
• Medicare Part B (medical insurance).
When do I use this form?
You can join a plan:
• Between Oct. 15-Dec. 7 each year (for coverage starting Jan. 1).
• Within three months of first getting Medicare.
• In certain situations where you’re allowed to join or switch plans. Visit Medicare.gov to learn more about
when you can sign up for a plan.
What do I need to complete this form?
• Your Medicare Number (the number on your red, white and blue Medicare card).
• Your permanent address and phone number.
Reminder:
• If you want to join a plan during fall open enrollment (Oct. 15-Dec. 7), the plan must have your
completed form by Dec. 7.
What happens next?
Send your completed and signed form to:
OMES EGID
P.O. Box 11137
Oklahoma City, OK 73136-9998
Once they process your request to join, they’ll contact you.
How do I get help with this form?
Call EGID Member Services at 405-717-8780 or toll-free 800-752-9475 Monday-Friday, 8 a.m. to 4:30 p.m.
Central time to see if you are eligible to enroll. TTY users call 711. Or, call Medicare at 800-MEDICARE (800-
633-4227). TTY users can call 877-486-2048. En español: Llame a EGID al 800-752-9475/TTY 711 o a
Medicare gratis al 800-633-4227 y oprima el 2 para asistencia en español y un representante estara disponible
para asistirle.
Individuals experiencing homelessness
If you want to join a plan but have no permanent residence, a post office box, an address of a shelter or clinic,
or the address where you receive mail (e.g., Social Security checks) may be considered your permanent
residence address.
Rev. August 2023 MAPD
C1

*MAPDEN*
Employees Group Insurance Division
APPLICATION FOR MEDICARE ADVANTAGE
PRESCRIPTION DRUG (MAPD) PLAN
Member information
Member name (First MI Last) Member ID
Date of birth
Male Female
Member SSN
Permanent address (P.O. Box not allowed) City State ZIP code
Mailing address (if different from above) City State ZIP code
Phone Alternate phone Email
Dependent information (only if enrolling in Medicare)
Dependent name (First MI Last)
Date of birth
Male Female
Dependent SSN
Your Medicare information (required to process your application)
Name on Medicare card:
Medicare number: - -
Part A effective date:
Part B effective date:
You must have Medicare Part A and Part B to join an MAPD plan.
Answer these important questions
1. In which MAPD plan do you want to enroll?
BCBSOK – MAPD Generations by GlobalHealth
CommunityCare Senior Health Plan Humana MAPD PPO
2.
Some individuals may have other drug coverage through private insurance, TRICARE, federal employee
health benefits, VA benefits or state pharmaceutical assistance programs. Will you have other
prescription drug coverage in addition to your coverage through OMES Employees Group Insurance
Division?
Name of other coverage ID# Group#
No
Yes
3.
Typically, you can enroll in a Medicare prescription drug plan only during the annual enrollment period
from Oct. 15 through Dec. 7 each year. Additionally, there are exceptions that may allow you to enroll in a
Medicare prescription drug plan outside of the Annual Enrollment Period. (Refer to statements on Page 2.)
I am enrolling during an Annual Enrollment Period (Option Period).
C2

Read the following statements and check the box if the statement applies to you. By checking any of the
following boxes, you are certifying that, to the best of your knowledge, you are eligible for an enrollment
period. If we later determine that this information is incorrect, you may be disenrolled.
I am new to Medicare.
I recently moved outside of the service area of my current plan. I moved on (insert date):
I recently was released from incarceration. I was released on (insert date):
I recently returned to the U.S. after living permanently outside of the U.S.
I returned to the U.S. on (insert date):
I recently obtained lawful presence status in the U.S. I got this status on (insert date):
I recently had a change in my Medicaid (newly got Medicaid, had a change in level of Medicaid assistance or lost
Medicaid) on (insert date):
I recently had a change in my Extra Help paying for Medicare prescription drug coverage (newly got Extra Help, had a
change in level of Extra Help or lost Extra Help) on (insert date):
I have both Medicare and Medicaid or I get Extra Help paying for my Medicare prescription drug coverage, but I haven’t
had a change.
I live in or recently moved out of a long-term care facility (for example, a nursing home or other long-term care facility).
I moved/will move into/out of the facility on (insert date):
I recently left a PACE program on (insert date):
I recently involuntarily lost my creditable prescription drug coverage (as good as Medicare’s). I lost my drug coverage on
(insert date):
I am leaving employer or union coverage on (insert date):
I belong to a pharmacy assistance program provided by my state.
I was enrolled in a plan by Medicare (or my state), and I want to choose a different plan. My enrollment in that plan
started on (insert date):
I was affected by an emergency or major disaster (as declared by the Federal Emergency Management Agency (FEMA) or
by a federal, state or local government entity. One of the other statements here applied to me, but I was unable to make
my enrollment request because of the disaster.
My plan is ending its contract with Medicare, or Medicare is ending its contract with my plan.
None of these statements apply to me. Call EGID at 405-717-8780 or toll-free 800-752-9475 Monday-Friday, 8 a.m. to
4:30 p.m. Central time to see if you are eligible to enroll. TTY users call 711.
Answering these questions is your choice. You cannot be denied coverage if you don’t
answer.
4. Are you Hispanic, Latino/a, or Spanish origin? Select all that apply.
No, not of Hispanic, Latino/a, or Spanish origin Yes, Mexican, Mexican American, Chicano/a
Yes, Puerto Rican Yes, Cuban
Yes, another Hispanic, Latino/a, or Spanish origin
I choose not to answer.
5. What’s your race?
American Indian or Alaska Native Asian Indian Black or African American
Chinese Filipino Guamanian or Chamorro
Japanese Korean Native Hawaiian
Other Asian Other Pacific Islander Samoan
Vietnamese White
I choose not to answer.
6. Would you prefer that the MAPD plan send you information in a language other than English or in
another format?
Yes No
C3

–
–
Primary care physician selection
As an MAPD plan member with CommunityCare Senior Health Plan or Generations by GlobalHealth, you must choose a PCP
who will coordinate your health care. You can obtain a list of the plan’s network physicians by contacting the plan or visiting
their website.
Physician name (First Last) Are you a current patient of this physician?
Yes
No
Signatures Important: Read and sign below
• I must keep both Part A and Part B to stay in the plans offered by EGID.
• By joining this Medicare Advantage plan, I acknowledge the Medicare Advantage prescription drug plans offered by EGID
will release my information to Medicare, who may use it to track beneficiary enrollment, for payment and other purposes
applicable to federal statutes that authorize the collection of this information (see Privacy Act Statement below).
• Your response to this form is voluntary. However, failure to respond may affect enrollment.
• The information on this enrollment form is correct to the best of my knowledge. I understand that if I intentionally provide
false information on this form, I will be disenrolled from the plan.
• I understand that people with Medicare are generally not covered under Medicare while out of the country, except for
limited coverage near the U.S. border.
• I understand that when my MAPD coverage through EGID begins, I must get all of my medical and prescription drug
benefits from that plan. Benefits and services provided by my plan and contained in my evidence of coverage document
(also known as a member contract or subscriber agreement) will be covered. Neither Medicare nor my plan will pay for
benefit or services that are not covered.
• I understand that my signature (or the signature of the person legally authorized to act on my behalf) on this application
means I have read and understand the contents of this application. If signed by an authorized representative (as described
above), this signature certifies that:
1) This person is authorized under state law to complete this enrollment.
2) Documentation of this authority is available upon request by Medicare.
Member signature
Date
Dependent signature (only if dependent is enrolling in Medicare) Date
If you are the authorized representative, you must sign above and provide this information
Name Phone
Address
Relationship to enrollee
Mail or fax the form to Attn: Member Accounts
Mail: OMES EGID Fax: 405-717-8939
P.O. Box 11137
Oklahoma City, OK 73136-9998
2024 monthly premium information does not reflect any retirement system contribution
MEDICARE ADVANTAGE PRESCRIPTION DRUG (MAPD) PLANS
BCBSOK – MAPD $238.40 per covered person
CommunityCare Senior Health Plan $215.64 per covered person
Generations by GlobalHealth $199.00 per covered person
Humana MAPD PPO $192.92 per covered person
Privacy Act Statement
The Centers for Medicare & Medicaid Services (CMS) collects information from Medicare plans to track beneficiary enrollment in Medicare
Advantage (MA) Plans, improve care, and for the payment of Medicare benefits. Sections 1860D-1 of the Social Security Act and 42 CFR §§
423.30 and 423.32 authorize the collection of this information. CMS may use, disclose and exchange enrollment data from Medicare beneficiaries
as specified in the System of Records Notice (SORN) “Medicare Advantage Prescription Drug (MARx)”, System No. 09-70-0588. Your response
to this form is voluntary. However, failure to respond may affect enrollment in the plan.
If you have questions, call EGID Member Services at
405-717-8780 or toll-free 800-752-9475. TTY users call 711.
C4

Re: Automatic Bank Withdrawal for Insurance Premium
The Office of Management and Enterprise Services Employees Group Insurance
Division is pleased to offer you a convenient way to pay your monthly insurance
premiums. Through a program established by the Office of the State Treasurer, upon
your authorization, EGID will automatically draft your bank account for your monthly
insurance premiums.
If you wish to participate, your bank account will be debited on the 20th of each month,
and you will not need to mail a check for your insurance premium. There is no charge
for this service.
Once you are enrolled in this process, you will no longer receive a monthly bill from us.
EGID will notify you of any change in the monthly debit amount. This process will
continue as long as you have insurance through EGID, until you notify us in writing that
you no longer wish to participate, or until a debit does not clear your bank.
We encourage you to take advantage of direct debiting by completing the enclosed
authorization form. A confirmation will be sent to you showing the amount that will be
debited every month along with the month in which this process will begin.
The authorization form must be received in our office by the 10th of the month to
be effective for the current month’s premium. Forms received after the 10th will
be effective the following month. Premiums are required to be paid in full prior to
enrolling in direct debiting.
If you have any questions, call EGID Member Services at 405-717-8780 or 800-752-
9475. TTY users call 711.
D1
Revised 01/14/2022

This authorization form must be received in our office by the 10th of the month to be
effective for the current month’s premium. Forms received after the 10th will be effective
the following month. Premiums are required to be paid in full prior to enrolling in direct
debiting.
Employees Group Insurance Division
ELECTRONIC FUND TRANSFER
AUTHORIZATION
Member name
SSN or member ID
Member’s financial institution
I hereby authorize the Office of the State Treasurer to initiate debit entries for the
checking account at the financial institution indicated above for amounts due to the
Office of Management and Enterprise Services Employees Group Insurance Division.
This authority is to remain in full force and effect until one of the following occurs:
• EGID has received notification from the insured of his or her desire to stop
participating in automatic bank withdrawals. The notice must be made at least
one week before the debit date.
• The Office of the State Treasurer is unable to debit the account for any month
because of a closed account, insufficient funds or any other reason.
Signature Date
Attach a voided check here. Deposit slips will not be accepted.
ATTACH CHECK HERE
Please mail this completed form to:
EGID MEMBER ACCOUNTS
P.O. BOX 11137
OKLAHOMA CITY, OK 73136 9998
-
D2
__________________________________________ ______________________
*BENEFI*
Employees Group Insurance Division
Beneficiary Designation Form
Please read the instructions carefully and complete this form in ink.
SSN or Member ID: __________________ Member Name: _____________________________________
First MI Last
Address: ___________________________________________________________________________
New Address Street City State ZIP
Phone: (____) ___________________________ Alt Phone: (____) ________________________
Important*: Please ensure the “Share Percentage” section in both Primary Beneficiary(ies) and Contingent Beneficiary(ies)
add up to 100 percent. Payment will be made in equal shares to all surviving beneficiaries unless otherwise indicated.
P
RIMARY BENEFICIARY(IES)
Primary Beneficiary’s Name and Address
SSN
Phone #
Relationship
Date of Birth
Share
Percentage
100%
CONTINGENT BENEFICIARY(IES)
Proceeds are paid to the contingent beneficiary(ies) identified below only if there is no surviving primary beneficiary(ies).
Contingent Beneficiary’s Name and Address
SSN
Phone #
Relationship
Date of Birth
Share
Percentage
100%
I have named the above beneficiary(ies) to receive my life insurance benefits from HealthChoice. I
understand this form replaces and cancels all prior beneficiary designations and will become effective
only when it is received by EGID.
Member Signature - original signature required Date
Mail this form to OMES EGID at P.O. Box 11137, Oklahoma City, OK 73136-9998
E1
Instructions for Completing the Beneficiary Designation Form
This beneficiary form applies to the HealthChoice Life Insurance Plan offered through the Office of Management
and Enterprise Services Employees Group Insurance Division. If you are retired, it does not affect the beneficiaries
for any death benefit you may have through your retirement system.
The beneficiary designations you make on this form replace and cancel all prior life insurance beneficiary
designations with EGID. Your designations do not become effective until this form is signed and received by
EGID. Do not alter this form or attach additional pages.
It is very important that you provide the full legal name, address, relationship, date of birth and Social
Security number of each beneficiary you designate. This information is essential in ensuring that your named
beneficiaries can be located and receive your intended benefit amount. The Beneficiary Designation Form has
three parts: Member Information, Primary and Contingent Beneficiary Designation and Signature. Please print
clearly in ink.
Employer Name – Provide the name of your employer. This information is not required of a former
employee/retiree.
Member Information – Provide your name, SSN or Member ID and address.
Primary Beneficiary Designation – You can designate one or more primary beneficiaries. All primary
beneficiaries share equally, unless you note otherwise. In the event that multiple primary beneficiaries are
named and a primary beneficiary dies before or simultaneously with you, the remaining primary
beneficiary(ies) will be entitled to equal share of the deceased beneficiary’s designated benefit amount.
Contingent Beneficiary Designation – You can designate one or more contingent beneficiaries.
Contingent beneficiaries receive benefits only in the event all primary beneficiaries die before or
simultaneously with you. All contingent beneficiaries share equally, unless you note otherwise on your form.
In the event that multiple contingent beneficiaries are named and a contingent beneficiary dies before or
simultaneously with you, the remaining contingent beneficiary(ies) will be entitled to equal share of the
deceased beneficiary’s designated benefit amount.
Signature – You must sign and date your form.
Special Beneficiary Designations
Sometimes members wish to make a special designation for trusts, minors or institutions. If you wish to make a
special designation, please read the following information carefully.
Designating a trust as beneficiary – To designate a trust as beneficiary, provide the actual name of the
trust and the date the trust was created in the space provided.
Designating a minor as beneficiary – A minor can be named your beneficiary; however, it is often difficult
and costly for a minor to receive payment, especially if the amount exceeds $10,000. Before you designate a
minor as your beneficiary, you should consult an attorney or professional financial advisor.
Designating an institution as beneficiary – To designate an institution (church, charity, funeral home, etc.)
as your beneficiary, provide the full name of the institution and list the address in the space provided.
After you complete and sign the Beneficiary Designation Form, mail it to:
Office of Management and Enterprise Services
Employees Group Insurance Division
P.O. Box 11137, Oklahoma City, OK 73136-9998
Remember to keep a copy of your completed form for your records.
E2

State of Oklahoma
Office of Management and Enterprise Services
Privacy Notice
Revised October 2023
This notice describes how medical information about you may be used and disclosed and
how you can get access to this information. Please review this notice carefully.
For questions or complaints regarding privacy concerns with OMES, please contact:
OMES HIPAA Privacy Officer
P.O. Box 11137, Oklahoma City, OK 73136
405-717-8780 or toll-free 800-752-9475
TTY 711
oklahoma.gov/omes
Why is the notice of privacy practices important?
This notice provides important information about the practices of OMES pertaining to the way it
gathers, uses, discloses and manages your Protected Health Information and also describes how
you can access this information. PHI is health information that can be linked to a particular person by
certain identifiers including, but not limited to, names, Social Security numbers, addresses and birth
dates.
Oklahoma privacy laws and the federal Health Insurance Portability and Accountability Act of 1996
(HIPAA) protect the privacy of an individual’s health information. Please note, in general the laws
and regulations of HIPAA do not apply to the Health Choice Disability Plan and HealthChoice Life
Insurance Plan. For HIPAA purposes, OMES has designated itself as a hybrid entity. This means
that HIPAA only applies to areas of OMES operations involving health care and not to all lines of
service offered by OMES. This notice applies to the privacy practices of the following OMES
divisions and positions that may share or access your PHI as needed for treatment, payment and
health care operations:
• Employees Group Insurance Division (EGID).
• General Counsel Legal.
• Information Services as it applies to maintenance and storage of PHI.
• The Director of Public Affairs and Grants Management and the Legislative Liaison.
OMES is committed to protecting the privacy and security of your PHI as used within the
components listed above.
27
4997
Your information. Your rights. Our responsibilities.
Your rights
When it comes to your health information, you have certain rights. This section explains your
rights and some of our responsibilities to help you.
Get an electronic or paper copy of your health and claims records.
• You can ask to see or get an electronic copy of your medical record and other health
information we have about you. Ask us how to do this using the contact information at the
beginning of this notice.
• We will provide a copy or a summary of your health and claims records, usually within 30 days
of your request. We may charge a reasonable, cost-based fee.
Ask us to correct health and claims records.
• You can ask us to correct your health and claims records if you think they are incorrect or
incomplete. Ask us how to do this using the contact information at the beginning of this
notice.
• We may decline your request but will explain the reasons in writing within 60 days.
Request confidential communications.
• You can ask us to contact you in a specific manner; e.g., home or office phone, or to send
mail to an alternate address.
• We will consider all reasonable requests.
o If declining would put you in danger, tell us and we will automatically approve your
request.
Ask us to limit what we use or share.
• You can ask us not to use or share certain health information for treatment, payment or our
operations.
o We are not required to approve your request and may decline if it would affect your
care.
Get a list of those with whom we’ve shared information.
• You can ask for an accounting of the times we’ve shared your health information for six
years prior to the date you ask, who we shared it with and why.
• We will include all the disclosures except for those about treatment, payment andhealth care
operations, and certain other disclosures (such as any you asked us to make).
• We will provide one free accounting per year but will charge a reasonable fee if you request
an additional accounting within 12 months.
Get a copy of this privacy notice.
You can ask for a paper copy of this notice at any time, even if you have agreed to receive the
notice electronically. We will promptly provide you with a paper copy.
28

Choose someone to act for you.
• If you have named a medical power of attorney, or if someone is your legal guardian,
that person can exercise your rights and make decisions about your health information.
• We will verify the person has this authority and can act for you before any action is
taken.
File a complaint if you feel your rights are violated.
• You can file a complaint if you feel we have violated your rights by contacting us using
the information at the beginning of this notice.
• You may also file a complaint with the U.S. Department of Health and Human Services
Office for Civil Rights by sending a letter to 200 Independence Ave., S.W., Washington,
D.C. 20201, calling 1-877-696-6775, or visiting
hhs.gov/ocr/privacy/hipaa/complaints/.
• We will not retaliate against you for filing a complaint.
Your choices
For certain health information, you can tell us your choices about what we share. If you
have a clear preference for how we share your information in the situations described below, talk
to us. Tell us what you want us to do, and we will follow your instructions.
In these cases, you have both the right and choice to tell us to:
• Share information with your family, close friends, or others involved in payment for your
care.
• Share information in a disaster relief situation.
• Contact you for fundraising efforts.
If you are not able to tell us your preference (e.g., if you are unconscious), we may share your
information if we believe it is in your best interest. We may also share your information when needed
to lessen a serious and imminent health or safety threat.
In these cases, we never share your information unless you give us written permission:
• Marketing purposes.
• Sale of your information.
• Most sharing of psychotherapy notes.
Our uses and disclosures
How do we typically use or share your health information?
Your PHI is used and disclosed by OMES employees and other entities under contract with OMES
according to HIPAA Privacy Rules and the “minimum necessary” standard, which releases only the
minimum necessary health information to achieve the intended purpose or to carry out a desired
function within OMES.
29

We typically use or share your health information in the following ways:
Help manage the health care treatment you receive.
• We can use your health information and share it with professionals who are treating you.
Example: A doctor sends us information about your diagnosis and treatment plan so we can
arrange additional services.
Run our organization.
• We can use and disclose your information to run our organization and contact you when
necessary.
• We are not allowed to use genetic information to decide whether we will give you coverage
and the price of that coverage. This does not apply to long term careplans.
Examples: We use health information about you to develop better services for you, provide customer
service, resolve member grievances, member advocacy, conduct activities to improve member
health and reduce costs, assist in the coordination and continuity of health care, and to set premium
rates.
Pay for your health services.
• We can use and disclose your health information as we pay for your eligible health services.
Example: We share information about you with your dental plan to coordinate payment for your
dental work.
Administer your plan.
• We may disclose summarized health information to your health plan sponsor for
plan administration.
Example: Your employer contracts with us to provide a health plan, and we provide the
employer with certain statistics to explain the premiums we charge.
How else can we use or share your health information?
We are allowed or required to share your information in other ways – usually in ways that contribute
to the public good, such as public health and research. We must comply with the law to share your
information for these purposes. For more information, refer to
hhs.gov/ocr/privacy/hipaa/understanding/consumers/index.html.
Help with public health and safety issues.
We can share your health information for certain situations such as:
• Preventing disease.
• Helping with product recalls.
• Reporting adverse reactions to medications.
• Reporting suspected abuse, neglect or domestic violence.
• Preventing or reducing a serious threat to anyone’s health or safety.
30

Do research.
We can use or share your information for health research, as permitted by law.
Comply with the law.
We will share information about you if state or federal laws require it, including with the Department
of Health and Human Services if it wants to ensure we are complying with federal privacy laws.
Respond to organ and tissue donation requests.
We can share health information about you with organ procurement organizations.
Work with a medical examiner or funeral director.
We can share health information with a coroner, medical examiner or funeral director when an
individual dies.
Address workers’ compensation, law enforcement and other government requests.
We can use or share health information about you:
• For workers’ compensation claims.
• For law enforcement purposes or with a law enforcement official.
• With health oversight agencies for activities authorized by law.
• For special government functions such as military, national security, and presidential
protective services.
Respond to lawsuits and legal actions.
We can share health information about you in response to a court or administrative order or in
response to a subpoena.
Our responsibilities
When it comes to your health information, we have specific obligations such as:
• We are required by law to maintain the privacy and security of your Protected Health
Information.
• We will let you know promptly if a breach occurs that may have compromised the privacy or
security of your PHI.
• Wemust follow the duties and privacy practices described in this notice and give you a copy
of it.
• We will not use or share your PHI other than as described here unless you notify us in writing
that wecan. You may change your mind at any time but must let us know in writing if you do.
For more information, refer to
hhs.gov/ocr/privacy/hipaa/understanding/consumers/noticepp.html.
Changes to the terms of this notice.
We can change the terms of this notice, and the changes will apply to all information we have about
you. The new notice will be available upon request, on our website, and we will deliver a copy to
you. You may also subscribe online to receive notice of changes to this page via email or text
message.
31

Contact Informaon
Health plans
BCBS – BlueLincs
855-609-5684
bcbsok.com/state
CommunityCare
918-594-5242 or 800-777-4890
TDD/TTY 800-722-0353
state.ccok.com
GlobalHealth Inc.
405-280-5600 or 877-280-5600
TTY 711
GlobalHealth.com/Oklahoma/mystateplan
HealthChoice
Medical
800-323-4314
TTY 711
HealthChoiceOK.com
Pharmacy
877-720-9375
TTY 711
Caremark.com
Health Plans – Medicare
Supplement Plans
BCBSOK Member Services
833-418-0443
TTY 711
bcbsok.com/reree-medicare-state
HealthChoice
Medical
800-323-4314
TTY 711
HealthChoiceOK.com
Pharmacy
866-275-5253
TTY 711
Caremark.com
Health Plans – MAPD Plans
BCBSOK Member Services
833-418-0443
TTY 711
bcbsok.com/retiree-medicare-state
CommunityCare Senior Health Plan
918-594-5323 or 800-642-8065
TDD/TTY 800-722-0353
stateshp.ccok.com
Generations by GlobalHealth
Prospective Members:
844-322-8322
Current Members:
405-280-5555 or 844-280-5555
TTY 711
GlobalHealth.com/Oklahoma/osr
Humana Group Medicare Customer Care
Identify yourself as a retiree with the State of
Oklahoma/EGID when calling as a prospective
member.
866-396-8810
TTY 711
7 a.m. to 8 p.m. CT
your.humana.com/ok-medicare
Dental Plans
BCBS – BlueCare
855-609-5684
Bcbsok.com/state/dental
Cigna Prepaid Dental
800-244-6224
Hearing-impaired relay 800-654-5988
view.ceros.com/cigna/ok-ins-benets
Delta Dental
405-607-2100 or 800-522-0188
DeltaDentalOK.org/client/OK
32

405-521-2387 or 877-738-6365
ok.gov/trs
Oklahoma Law Enforcement
Retirement System
405-522-4931 or 877-213-0856
olers.state.ok.us
Contact Informaon
HealthChoice
Customer Care 800-323-4314
TTY 711
HealthChoiceOK.com
MetLife
855-676-9443
metlife.com/Oklahoma
Sun Life
800-442-7742
onboard.sunlifeconnect.com
Life Plans
HealthChoice
Customer Care 800-323-4314
TTY 711
HealthChoiceOK.com
Vision plans
Primary Vision Care Services (PVCS)
888-357-6912
TDD 800-722-0353
pvcs-usa.com/okstate
Superior Vision
800-507-3800
TDD 916-852-2382
superiorvision.com/stateofoklahoma/benets
Vision Care Direct
855-918-2020
TTY 711
okstate.vision
VSP
800-877-7195
TDD 800-428-4833
stateofok.vspforme.com
Other important numbers
Employees Group Insurance Division
405-717-8780 or 800-752-9475
TTY 711
Oklahoma.gov/omes
Social Security Administraon
800-772-1213
TTY 800-325-0778
SSA.gov
Medicare
800-633-4227
TTY 877-486-2048
Medicare.gov
Oklahoma Public Employees
Rerement System
405-858-6737 or 800-733-9008
opers.ok.gov
Oklahoma Teachers’
Rerement System
405-521-2387 or 877-738-6365
ok.gov/trs
Oklahoma Law Enforcement
Rerement System
405-522-4931 or 877-213-0856
olers.state.ok.us
33

Forms you must complete to continue
benefits when you leave active employment
INSURANCE
FORMS
IF YOU ARE A
PRE-MEDICARE
MEMBER
IF YOU ARE A
MEMBER ENROLLING
IN A MEDICARE
SUPPLEMENT PLAN
IF YOU ARE
A MEMBER
ENROLLING IN A
MEDICARE ADVANTAGE
PRESCRIPTION DRUG
(MAPD) PLAN
Application for
Retiree/Vested/Non-
Vested/Defer Insurance
Coverage
(Page A1)
Yes Yes
Application for Medicare
Supplement With
Prescription Drug Plan
(Page B1)
No
Yes
Each enrollee must
complete an application
No
Application for Medicare
Advantage Prescription
Drug (MAPD) Plan
(Page C1)
No No
Yes
Each enrollee must
complete an application
Beneficiary Designation
Form
(If continuing life
insurance coverage)
(Page E1)
Yes Yes Yes
Yes
34
This publication was printed by the Office of Management and Enterprise Services as authorized by Title 62, Section 34. 1,500 copies have been
printed at a cost of $1,920. A copy has been submitted to Documents.OK.gov in accordance with the Oklahoma State Government Open Documents
Initiative (62 O.S. 2012, § 34.11.3). This work is licensed under a Creative Attribution- NonCommercial-NoDerivs 3.0 Unported License.


