
August 2014
Implementation of modified
admission MRSA screening
guidance for NHS (2014)
Department of Health expert advisory committee on
Antimicrobial Resistance and Healthcare Associated
Infection (ARHAI)

2
You may re-use the text of this document (not including logos) free of charge in any format
or medium, under the terms of the Open Government Licence. To view this licence, visit
www.nationalarchives.gov.uk/doc/open-government-licence/
© Crown copyright
Published to gov.uk, in PDF format only.
www.gov.uk/dh
3
Implementation of modified
admission MRSA screening
guidance for NHS (2014)
Department of Health expert advisory committee
on Antimicrobial Resistance and Healthcare
Associated Infection (ARHAI)
Prepared by ARHAI MRSA Screening Implementation Group
Disclaimer
The MRSA Screening Implementation Group, comprising members from key
professional groups, was established to determine how to give implementation guidance
on MRSA screening to NHS England, in the context of recommendations from the NOW
study.
The Working Group members were: Mark Wilcox (Chair, ARHAI), Peter Cowling (BIA),
Brian Duerden, Carole Fry (DH), Susan Hopkins (PHE), Peter Jenks (HIS), Sally
Kingsland (NHS England), and Sally Palmer (IPS).
4
Contents
Contents ..................................................................................................................................... 4
Executive summary .................................................................................................................... 5
Introduction ................................................................................................................................ 6
Objective .................................................................................................................................... 8
High risk specialties/units ................................................................................................ 8
Interventions .............................................................................................................................. 9
Compliance and audit .............................................................................................................. 10
References ............................................................................................................................... 11
Appendix .................................................................................................................................. 12
Annex: Consultation ................................................................................................................. 16
5
Executive summary
The following guidance outlines a more focused, cost-effective approach to MRSA
screening. The recommendation for Trusts to move to focussed screening programmes
has been designed to promote a more efficient and effective method for identifying and
managing high risk MRSA positive patients. Importantly, focussed screening should be
adopted in line with local risk assessments to ensure that Trusts concentrate on reducing
negative patient outcomes for their own populations. Changes to current practice need to
be undertaken with a commitment to improved compliance with focussed screening, which
should be monitored and reported to Trust Boards and commissioners. Trusts will need to
regularly review (and where necessary improve) their compliance with national screening
guidance for each specialty, recent MRSA infection data, patient demographics and types
of services provided within individual organisations. Continued surveillance through both
local and national surveillance systems will be needed to monitor the levels of MRSA
infection. The outputs of the NOW study could be used to inform policy making decisions
should the prevalence of MRSA increase.
6
Introduction
In the last decade there have been very marked declines in morbidity and mortality related to
MRSA infection in England. Annual MRSA bacteraemia rates fell from 17.7 (April 2005-March
2006) to 3.2 cases per 100, 000 bed days (April 2011-March 2012).
1
Significant declines have
also been observed in surgical site infections (SSI) where MRSA was reported as the causative
micro-organism (from 27% in 2004-6 to only 4% in 2011/12).
2,3
The number of death
certificates in England and Wales mentioning MRSA infection has decreased each year since
2006, when the figure peaked at 1,652; in 2012, MRSA accounted for 292 mentions of MRSA
on death certificates (a 20% decrease on the previous year).
4
Until April 2009, national guidance in England recommended targeted screening of patients in
high risk specialties.
5
There were no randomised controlled trials, however, to provide
evidence on the most effective and cost-effective screening strategies. The Department of
Health (DH) in England introduced mandatory screening of all elective and emergency
admissions from April 2009 and December 2010, respectively. This decision was based on a
DH impact assessment that modelled the cost-effectiveness of different screening and
decolonisation strategies in preventing MRSA bacteraemias, wound infections and deaths. We
note that in other settings (e.g. Wales), where mandatory screening has not been implemented,
MRSA infection rates have fallen markedly.
6
The DH impact assessment committed to a review
of this policy with additional data; thus, the NOW study was commissioned in 2011. The study
report underwent peer review and its findings were endorsed by ARHAI.
A full report of the NOW study and a summary of its findings are available.
7,8,9
The study
showed that compliance with the current mandatory screening policy was poor (e.g. only 61%
were screened; about half of new positives were isolated when their result became known; and
about a quarter did not receive decolonisation therapy) (Appendix, Table 1). The prevalence of
MRSA in new admissions was low (1.5% overall), although this varied according to type of
admission (2.1% in emergency admissions, 0.9% elective admissions and 0.7% in day cases
admissions) (Appendix, Tables 2 &3). These observations mean that the numbers of patients
needed to be screened in order to identify one new positive were high in all admission types
(emergency n=102; elective n=180; and day case n=186).
8
The NOW study went on to model the effectiveness and cost-effectiveness of six different
screening strategies at a whole hospital level for the three categories of NHS Trust (acute,
teaching and specialty) at four different levels of MRSA prevalence (the current prevalence; and
twice, three and four times the current prevalence) and two levels of transmission (current and
twice the estimated transmission rate). Six screening and intervention strategies were
evaluated: 1) no screening (interventions applied to clinical cases only), 2) screening all
admissions (emergency and elective), 3) screening all admissions to high risk specialties, 4)
checklist activated screening of all admissions, 5) screening all admissions to high risk
specialties plus checklist activated screening of other admissions, and 6) screening all
admissions plus pre-emptive isolation of those known to be previously MRSA positive.
At current prevalence none of the screening strategies was likely to be cost-effective at
conventional NHS levels of ‘willingness to pay’ (less than £30,000 per QALY). Costs per QALY
for routine admission screening ranged from £86,000 - £170,000, and were consistently more
costly and less effective than alternatives for all hospital types. However, of the strategies
involving active screening, targeting high risk specialty patients was the optimal option; i.e.
mean incremental cost-effectiveness ratios (ICERs) of approximately £45,000 and £48,000 in
Acute, and Teaching Trusts, respectively (Appendix, Table 4) (see below for Specialist trust
results). As prevalence rose, the cost effectiveness of this strategy increased, and fell within
Implementation of modified admission MRSA screening guidance for NHS (2014)
7
the conventional NHS levels of ‘willingness to pay’ (Appendix, Table 4). The model results were
strongly influenced by the assessment of the risk of infection, which is greater in high risk
specialty patients, and has the largest impact on length of stay and mortality, the major
determinants of cost and health benefits. Importantly, lack of screening of MRSA in patients
admitted to low-risk specialties results in more transmission, but less proportionate risk of
serious infection and death than in high risk specialties. Approximately 60% of MRSA colonised
individuals will be detected by screening those known to be previously MRSA positive and high
risk specialty admissions. For acute and teaching trusts, the most cost effective of the
screening strategies is screening high risk specialties only, at both the current prevalence and
up to 4 times current prevalence (~5%). For specialist trusts, at current and twice current
prevalence, again the ‘no screening’ strategy has the greatest probability of being the most
cost-effective option. However, of the active screening strategies, screening high risk
specialities and performing check list activated screening of others is optimal. At higher
prevalence (>3%), high risk specialty screening alone becomes the most cost effective strategy
overall. However, the probability of cost-effectiveness for high risk specialty screening and high
risk specialty plus checklist activated screening cluster together closely. Thus, the most
pragmatic decision is that high risk screening for all trust types is the simplest and most cost
effective of the screening strategies (Appendix, Table 5).
A recent study examined MRSA control in an ICU setting in the US, (where all patients were
nursed in side-rooms), comparing screening and isolation with targeted or universal
decolonisation.
10
Universal decolonisation was found to be effective at reducing rates of MRSA
clinical isolates and any pathogen bloodstream infections in ICUs. However, universal
decolonisation has not been validated in this way outside the US or outside of the ICU setting,
and so no recommendation regarding this approach can be made at this time.
In summary, the results of the NOW study suggest that the current mandatory MRSA screening
policy is followed in less than two-thirds of admissions, but that even if compliance was 100%, it
would still not be cost-effective in any trust type or scenario. While no active screening strategy
was optimal at current MRSA levels, the most cost effective policy is one based on screening
admissions to high risk specialties; cost-effectiveness increases as MRSA prevalence rises.
Trusts would need however, to take measures to ensure high compliance with this strategy.

Objective
8
Objective
To focus and maximise the clinical impact for patients (adults and children) who are most likely
to benefit (i.e. those patients for whom MRSA colonisation carries the greatest risk of
infection/poor outcome), it is recommended that the current practice of mandatory MRSA
screening of acute and elective admissions to NHS hospitals in England is streamlined to the
following:
• All patients admitted to high risk units (defined below).
• All patients previously identified as colonised with or infected by MRSA.
High risk specialties/units
High risk specialties are defined as vascular, renal/dialysis, neurosurgery, cardiothoracic
surgery, haematology/oncology/bone marrow transplant, orthopaedics/trauma, and all
intensive care units (adult/paediatric ICUs, Neonatal Intensive Care Units, High dependency
units, Coronary Care Units).
• In addition, local risk assessment should be used to define other potential high MRSA
risk units/specialties; for example, according to provision of specialised services (e.g.
transplant, neonatal), and units with a history of high endemicity of MRSA. Local risk
assessment may increase the proportion of detected MRSA colonised individuals,
notably those patients at risk of poor outcome from MRSA.

Implementation of modified admission MRSA screening guidance for NHS (2014)
9
Interventions
1. Clear guidance on the local policy for MRSA screening should be made available to all
staff; this should be used as a standard against which audit is carried out.
2. Trusts should identify and screen patients in high MRSA risk specialties (as above).
3. Trusts should identify and re-screen any patient previously known to be MRSA positive
and isolate these pre-emptively, pending the results of laboratory tests.
4. NICE accredited Standards for Microbiology Investigations (SMIs) are available for
MRSA screening.
11
The most commonly practised methods of MRSA screening that
were recorded in the NOW study were based on culture on chromogenic agar (5% of
trusts routinely used PCR for emergency screens; 15% used PCR for some emergency
screening). Average MRSA screen turnaround times were 2.87 days for MRSA+ve and
1.75 days for MRSA-ve samples.
5. The most frequently sampled body sites included in current MRSA screening, as
identified in the NOW Study (i.e. as practised by at least 75% of trusts), are the nose,
groin/perineum and ‘other’ sites where appropriate (e.g. wounds, indwelling devices,
throat, etc).
6. The frequency of (repeat) screening should be determined locally and made explicit in
local guidance.
7. If MRSA transmission is detected/suspected in hitherto ‘low risk’ specialties then local
risk assessment should be used to determine the need for and extent of MRSA
screening, i.e. as befits normal infection prevention & control practice when investigating
clustering of cases or transmission.
8. All patients identified as MRSA positive must receive decolonisation/suppression
therapy; MRSA positive patients should normally be isolated until such time that MRSA
colonisation has been shown to be no longer present or local risk assessment
determines that isolation can be safely discontinued.
9. Local risk assessment in terms of isolation and decolonisation/suppression therapy will
be required for some persistently positive MRSA patients.
10. Trusts should continue to monitor MRSA rates.
Compliance and audit
10
Compliance and audit
1. Trusts should make every effort to ensure very high levels of screening in the patient
groups identified above.
2. Regular measurement/audit should be carried out to demonstrate compliance with local
MRSA screening guidance.
3. Audit should specifically include measurement of the appropriateness of decolonisation
(correct agents/dosages for correct time) and follow up.
4. Trusts should make performance/compliance data on MRSA screening and
decolonisation widely available within their organisations.
5. The Director of Infection Prevention and Control should provide assurance to the Trust
Board on the level of compliance with the local policy on MRSA screening
/decolonisation.
6. A qualitative study on the patient experience of MRSA screening and the impact of a
positive result found that the following are essential to securing and sustaining patients’
satisfaction and confidence in the care they receive in relation to preventing MRSA
infection:
1,2
i. patients need to be informed of the result of their screen, even if negative;
ii. information needs to be provided in an individualised way (both written and
verbal);
iii. staff need to be sufficiently knowledgeable and confident to invite patients’ and
carers’ questions and communicate information in a sensitive way;
iv. specific and comprehensive guidelines for home-based decolonisation are
required;
v. patients expect to see that standards of cleanliness and infection prevention, such
as hand hygiene, are practised; and
vi. measuring and acting on feedback from the patient experience is necessary.

Implementation of modified admission MRSA screening guidance for NHS (2014)
11
References
1. Available at: http://www.hpa.org.uk/
2. Health Protection Agency. Surveillance of surgical site infections in NHS hospitals in
England, 2011/2012. London: Health Protection Agency, December 2012. Available
from: www.hpa.org.uk
3. Health Protection Agency. Sixth report of the mandatory surveillance of surgical site
infection in orthopaedic surgery, April 2004 to March 2010. London: Health Protection
Agency, December 2010.
4. ONS. Deaths Involving MRSA: England and Wales, 2008 to 2012.
5. Coia JE, Duckworth GJ, Edwards DI, Farrington M, Fry C, Humphreys H, Mallaghan C,
Tucker DR; Joint Working Party of the British Society of Antimicrobial Chemotherapy;
Hospital Infection Society; Infection Control Nurses Association. Guidelines for the
control and prevention of meticillin-resistant Staphylococcus aureus (MRSA) in
healthcare facilities. J Hosp Infect 2006; 63 Suppl 1: S1–44.
6. Public Health Wales. Clostridium difficile and Staphylococcus aureus Bacteraemia
Monthly Update. Available at:
http://www.wales.nhs.uk/sites3/page.cfm?orgid=379&pid=67899 Last accessed 30 June
2014.
7. Fuller C, Robotham J, Savage J, Deeny S, Hopkins S, Cookson B, Stone S. Final report
of national one week prevalence audit of MRSA screening. Available at:
www.idrn.org/audit Last accessed 30 June 2014.
8. Fuller C, Robotham J, Savage J, Hopkins S, Deeny SR, et al. (2013) The National One
Week Prevalence Audit of Universal Meticillin-Resistant Staphylococcus aureus (MRSA)
Admission Screening 2012. PLoS ONE 8(9): e74219. doi:10.1371/journal.pone.0074219
9. Advisory Committee on Antimicrobial Resistance and Healthcare Associated Infection
(ARHAI). National one week (NOW) prevalence audit of MRSA screening report (ARHAI
22-13(02)). Available at: https://www.gov.uk/government/policy-advisory-
groups/advisory-committee-on-antimicrobial-resistance-and-healthcare-associated-
infection#minutes Last accessed 22 November 2013.
10. Huang SS, Septimus E, Kleinman K, et al. Targeted versus universal decolonization to
prevent ICU infection. N Engl J Med 2013;368:2255-65.
11. Public Health England. B 29 - Investigation of Specimens for Screening for MRSA.
Available at:
http://www.hpa.org.uk/ProductsServices/MicrobiologyPathology/UKStandardsForMicrobi
ologyInvestigations/TermsOfUseForSMIs/AccessToUKSMIs/SMIBacteriology/smiB29Inv
estigationofSpecimensforScreeningforMRSA/ Last accessed 22 November 2013.
12. Loveday H et al. The patient experience of the MRSA screening process and the impact
of a MRSA-positive result: a qualitative study. Antimicrobial Resistance and Infection
Control 2013;2 (Suppl 1):P56 http://www.aricjournal.com/content/2/S1/P56
MRSA Screening Implementation Group
April 2014
Updated post-consultation, June 2014
Appendix
12
Appendix
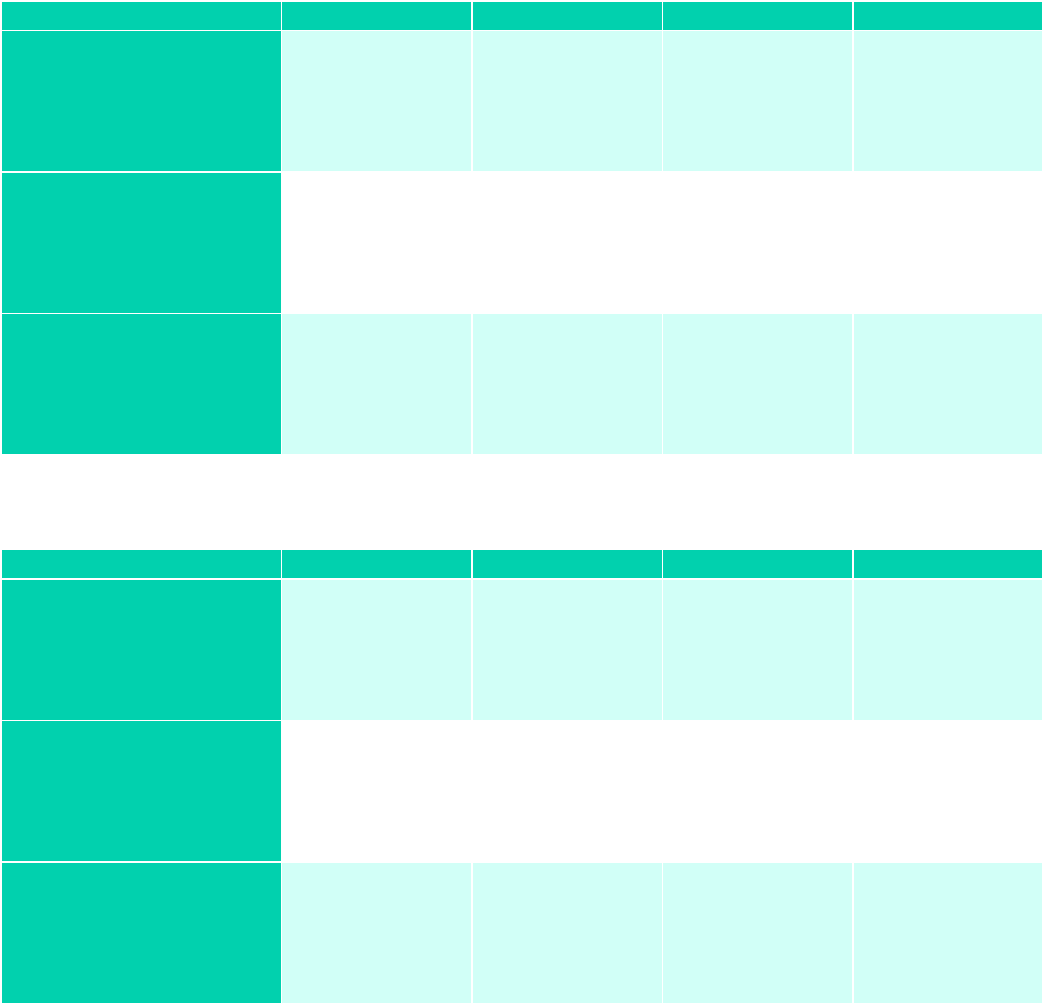
Table 1. NOW Study: Proportion of admissions screened for MRSA
Admission Category
All
Acute
Specialist
Teaching
Emergency
52788/87165
(61%)
Median 67.3%
IQR (47.5-85.8%)
n=132 trusts
38127/63577
(60%)
Median 67.1%
IQR (47.4-85.8%)
n=91
657/1166
(56%)
Median 85.9%
IQR (68.3-100%)
n=16
13736/21988
(62.5%)
Median 59.4%
IQR (48.9-89.2%)
n=22
Elective (not including
day-cases)
22773/27838
(81.8%)
Median 90%
IQR (58-118%)
n=115 trusts
14477/16497
(87.7%)
Median 92%
IQR (59-136%)
n=77
1652/2191
(75.4%)
Median 86%
IQR (62-100%)
n=16
6569/9044
(72.6%)
Median 73%
IQR (30-102%)
n=20
Day-cases (not
including dermatology,
endoscopy, ophthalmic
and paediatrics)
22416/46777
(47.9%)
Median 90%
IQR (23.2-78.9%)
n=110 trusts
14255/32927
(43.3%)
Median 36.5%
IQR (17.4-73.9%)
n=77
1153/1568
(73.5%)
Median 67.3%
IQR (42.6-100%)
n=13
6894/11927
(57.8%)
Median 48.3%
IQR (36.1-77.7%)
n=19
Table 2. NOW Study: Proportion of Admission Screens MRSA positive
Admission Category
All
Acute
Specialist
Teaching
Emergency
1075/52064
(2.1%)
Median 1.6%
IQR (1.1-2.7%)
n=129 trusts
836/37408
(2.2%)
Median 2%
IQR (1.2-2.7%)
n=90
5/652
(1%)
Median 0%
IQR (0-0.2%)
n=16
230/13736
(1.7%)
Median 1.7%
IQR (1.1-2.4%)
n=22
Elective (not including
day-cases)
188/20798
(0.9%)
Median 0.7%
IQR (0-1.9%)
n=101 trusts
110/13532
(0.8%)
Median 0.7%
IQR (0-1.8%)
n=68
25/1488
(1.7%)
Median 0.7%
IQR (0-2.5%)
n=15
53/5703
(0.9%)
Median 0.5%
IQR (0.3-1.5%)
n=14
Day-cases (not
including dermatology,
endoscopy, ophthalmic
and paediatrics)
150/21501
(0.7%)
Median 0%
IQR (0-1%)
n=112 trusts
58/13509
(0.4%)
Median 0%
IQR (0-0.6%)
n=76
6/1062
(0.6%)
Median 0%
IQR (0-1.1%)
n=16
85/6816
(1.2%)
Median 0.7%
IQR (0.3-1.2%)
n=19

Implementation of modified admission MRSA screening guidance for NHS (2014)
13
Table 3. NOW Study: Proportion of admission screens newly positive for MRSA
Admission Category
All
Acute
Specialist
Teaching
Emergency
498/50739
(1.0%)
Median 0.9%
IQR (0.4-1.3%)
n=127 trusts
374/36083
(1.0%)
Median 1.0%
IQR (0.5-1.5%)
n=88
4/652
(0.6%)
Median 0%
IQR (0-0%)
n=16
119/13736
(0.9%)
Median 0.8%
IQR (0.5-1.3%)
n=22
Elective (not including
day-cases)
107/19283
(0.6%)
Median 0.4%
IQR (0-1.2%)
n=98 trusts
68/12953
(0.5%)
Median 0.4%
IQR (0-1.7%)
n=68
16/1346
(1.2%)
Median 0.4%
IQR (0-1.5%)
n=14
23/4909
(0.5%)
Median 0.5%
IQR (0-1.4%)
n=15
Day-cases (not
including dermatology,
endoscopy, ophthalmic
and paediatrics)
79/20461
(0.4%)
Median 0%
IQR (0-0.1%)
n=110 trusts
27/12469
(0.2%)
Median 0%
IQR (0-0.2%)
n=74
5/1062
(0.5%)
Median 0%
IQR (0-0%)
n=16
47/6816
(0.7%)
Median 0.1%
IQR (0-0.7%)
n=19
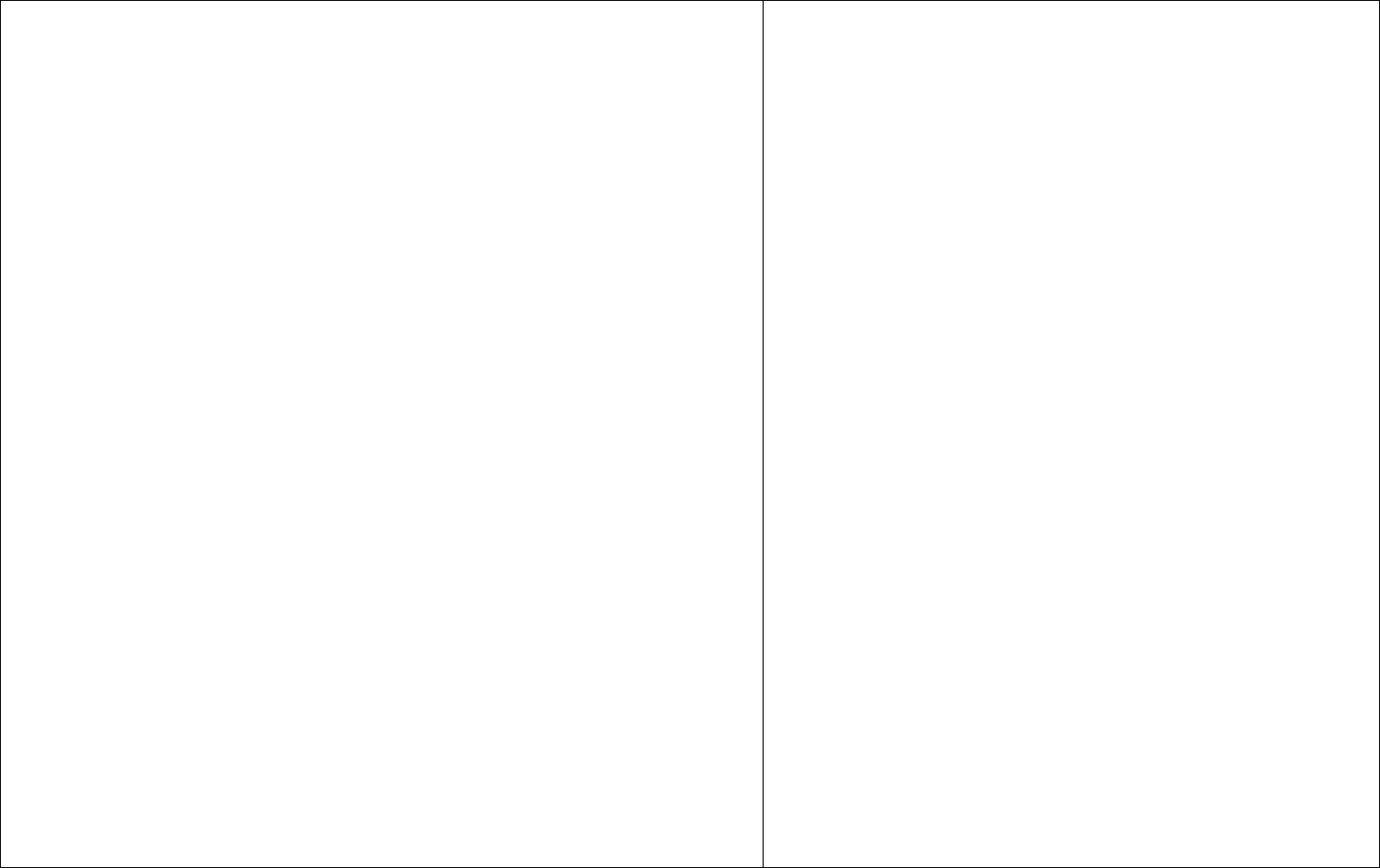
Table 4. NOW Study: Cost-effectiveness of screening strategies by trust type and MRSA
admission prevalence. Incremental cost per QALY gained is shown for strategies considered
both cost-effective
†
and non-cost-effective. Any remaining strategies for each prevalence
scenario were dominated
††
.
Trust
type
MRSA prevalence
on admission
Cost-effective strategies : Mean
(range
†††
)*
Non cost-effective strategies : Mean
(range
†††
)*
ACUTE
Baseline -
Strategy 3: £45,198/QALY
(£35,314-£61,390)
Strategy 5: £216,449/QALY
(£112,948-£1,770,724)
Moderate (x2) -
Strategy 3: £48,655/QALY
(£38,417-£64,899)
Strategy 6: £70,930/QALY
(£43,581-£161,673)
Strategy 5: £72,545/QALY
(£42,552-£206,075)
High (x3)
Strategy 3 :£29,565/QALY
(£25,660-£34,389)
Strategy 5: £159,566/QALY
(£95,476-£412,113)
Very high (x4)
Strategy 3: £28,708/QALY
(£25,479-£32,609)
-

Appendix
14
Trust
type
MRSA prevalence
on admission
Cost-effective strategies : Mean
(range
†††
)*
Non cost-effective strategies : Mean
(range
†††
)*
TEACHING
Baseline -
Strategy 3: £47,936/QALY
(£34,585-£74,757)
Moderate (x2) -
Strategy 3: £33,751/QALY
(£26,828-£43,702)
Strategy 2: 1,425,323/QALY
(£213,225-cost/health-loss)
High (x3) -
Strategy 3: £43,686/QALY
(£33,921-£59,612)
Strategy 5: £175,973/QALY
(£78,509-cost/health-loss)
Very high (x4) -
Strategy 3: £37,369/QALY
(£31,218-£37,369)
Strategy 6: £239,808/QALY
(£129,780-£11,238,684)
SPECIALIST
Baseline -
Strategy 5: £62,566/QALY
(£47,979-£89,425)
Moderate (x2) -
Strategy 5: £31,248/QALY
(£27,276-£36,499)
High (x3)
Strategy 3: £24,009/QALY
(£20,764 - £28,362)
Strategy 5: £26,411/QALY
(£17,071-£54,549)
-
Very high (x4)
Strategy 3: £19,331/QALY
(£17,295-£21,860)
Strategy 5: £24,503/QALY
(£16,421 - £45,503)
-
† An ICER of less than £30,000 per QALY is considered cost-effective. An ICER of more than £30,000 is not
considered cost-effective. £30,000 is the upper limit of the usual NHS willingness to pay range.
†† Dominated strategies are those that are more costly and provide less benefit than one other strategy or a
combination of two other strategies. Since it can never be cost-effective to pay more for less benefit, ICERs were
not calculated for these strategies.
††† ICER ranges were calculated using mean costs and QALYs ±1standard error, where the minimum = smallest
possible difference in cost / greatest possible difference in health benefits, and maximum = greatest possible
difference in cost/ smallest possible difference in health benefits.
*Further bootstrapped confidence intervals will be added.

Implementation of modified admission MRSA screening guidance for NHS (2014)
15
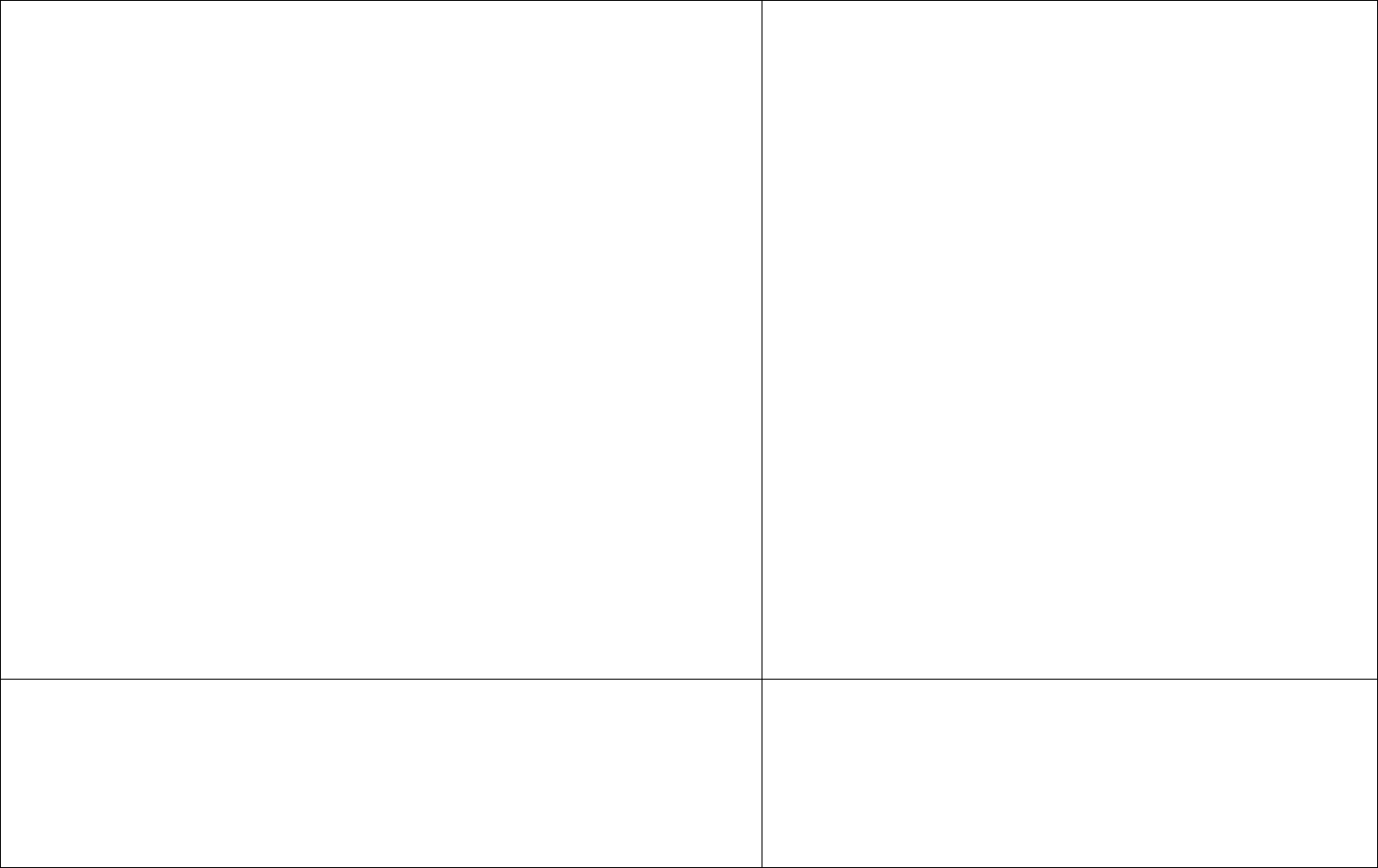
Table 5. Cost-effectiveness acceptability frontiers. Lines depict the optimal strategies (i.e. those
with the highest expected net monetary benefit) dependent on the willingness to pay for health
benefits, while dotted vertical lines show the willingness to pay values at which the decision
changes.
Acute
Teaching
Specialist
Baseline
prevalence
Acute: 1.4%
Teaching : 1.3%
Specialist: 1.04%
2x prevalence
Acute: 2.8%
Teaching: 2.6%
Specialist: 2.08%
3x prevalence
Acute: 4.2%
Teaching: 3.9%
Specialist: 3.12%
4x prevalence
Acute: 5.6%
Teaching: 5.2%
Specialist: 4.13%
Twice
transmission

16
Annex: Consultation
Consultation on ‘Implementation of modified admission MRSA screening guidance for NHS (2014)’
Comments
(the names of individuals providing comments are withheld here)
Response
A sensible and well written document. However it is rather "England -centric"
for the BIA. There is no mention of the Welsh experience where universal
screening was always eschewed and where rates of MRSA have also fallen.
Thank you.
Advice for Wales is not our remit. However, the observation
about declining MRSA rates in Wales in the absence of a
mandatory screening programme is pertinent – we have
added a note to our discussion.
Thank you for these draft guidelines, I do support the strategies proposed.
My only comment is that I would like to see similar guidelines provided in due
course for community hospital and mental health settings as specific
guidance has been previously issued, for example:
http://webarchive.nationalarchives.gov.uk/20101125133833/http://www.clean-
safe-care.nhs.uk/Documents/MRSA_Emergency_Screening_-_FAQs_-
_Apr_2010.pdf
Our own experience in mental health is that if all patients listed within the
possible risk groups are screened, very few are detected that were not known
MRSA positives. As such we have stepped down to screening only known
previous MRSA positives on admission to our mental health wards. It would
be useful to see a more cost effective strategy also advocated for non acute
trusts.
Thank you. This is however beyond our remit.

Implementation of modified admission MRSA screening guidance for NHS (2014)
17
We wish to respond as follows to 'Implementation of modified admission
MRSA screening guidance for NHS (2014)', the consultation document
prepared by the Department of Health’s 'MRSA Screening Implementation
Group', whose membership we note is not provided.
A) One of the arguments cited in favour of targeted rather than universal
screening is that compliance with universal screening is poor. However this is
not in itself a reason to prefer a different strategy, unless there are reasons to
believe that compliance with a different strategy would change in such a way
that outcomes would improve. We can't think of any plausible reason why this
should be so.
B) A second argument cited is the low prevalence of MRSA. Unlike the poor
compliance argument, this is relevant to choice of screening strategy, but
only insofar as it affects the cost-benefit analysis - it is not an argument in its
own right. It could also be turned on its head: it is possible that the current
low prevalence is a consequence of universal screening and that, without
universal screening, MRSA’s ‘R-nought’ value would exceed one and the
prevalence would begin to rise again. In other words we are at risk of
abandoning a strategy simply because it has been successful. Under the
‘targeted screening’ proposal, is there a prevalence at which we would go
back to universal screening?
C) The low prevalence of MRSA is also pertinent to the comparative
performance of different screening methodologies (because
prevalence affects the predictive value of the test) so it is a shame that the
proposal says nothing about this. This is a missed opportunity to define best
practice on questions that would benefit from a standardised NHS approach,
such as pooled processing vs separate processing, nose only vs nose and
throat vs nose/throat/perineum, selective media vs selective differential
media, solid media vs broth enrichment, place of PCR etc. What were the
The omission of names was an oversight that has now been
corrected.
A) Universal screening has not been optimally implemented.
Poor implementation is however not the most pressing reason
to consider alternatives. We have altered the wording in the
guidance document to make this point clearer and reflect the
finding in the report that, even if compliance were 100%,
routine screening would still be the least cost-effective policy
in all trust types and scenarios. The NOW study concluded
that a move to targeted screening of high risk plus checklist
activated screening of low risk, which in certain circumstances
in specialty hospitals is marginally more cost effective than
high risk screening, would be even harder to implement.
B) The guidance clearly states the need to review screening
policy based on prospective surveillance. A threshold has not
been set. Even if MRSA prevalence quadruples universal
screening remains cost ineffective.
C) This is outside of the remit of the NOW study; its aim was
to evaluate universal vs targeted approaches. i.e. who should
be screened rather than how. However, the effect of
prevalence on test predictive value was accounted for in the
assumptions in the NOW study.
The NOW study modelled what actually happens in the NHS,
which is that PCR based screening is rarely used routinely.
The use of standard methods is cited in the implementation

Annex: Consultation
18
terms of reference of the MRSA Screening Implementation Group if not to
debate such questions?
D) The cost effectiveness modelling on which the group’s proposals are
based is very difficult to assess. The members have drawn heavily from the
NOW study, but the NOW study has not been published in a peer-reviewed
journal and seems to exist only as a 320-page document on the UCL and
IDRN websites. It describes limited aspects of its modelling but directs the
reader for further information to a reference (Robotham JV, Graves N,
Barnett AG, et al (2011). Model-based evaluation and cost-effectiveness
analysis of MRSA intervention policies) that again is not peer-reviewed and in
fact doesn’t seem to be available any longer. This is a serious criticism of a
study that seeks to inform public policy, and of the current consultation
process.
E) It is important that the membership of the MRSA Screening
Implementation Group is disclosed. Have they been asked to appraise
critically the NOW study or are they the same people who wrote it?
F) Acknowledging that we are not given full details about the NOW study’s
modelling, the information that is provided leads us to regard the cost-
effectiveness calculations with scepticism. In particular it is proposed that,
compared to universal screening, high-risk area screening would save the
NHS as a whole £250m per year and the average NHS trust £1.6m per year,
at the cost of a small number of cases of infection. These figures seem
designed to catch the chief executive's eye (or to justify withdrawal of funding
from NHS trusts) but are implausible when set against the model's
parameters of swabbing costs of £3.20, laboratory costs of £4.24 (negative
test) or £7.24 (positive test), and an estimated universal screening load for
the average 553-bed NHS trust of 790 screens per week. The answer is
almost certainly in figure A3 (see below), which confirms that it is the costs of
isolation, not the costs of screening, that make by far the largest impact on
guidance.
D) The reference that is mentioned is a DH report (from the 3
year DoH funded modelling study MECAMIP), which was peer
reviewed; although it is no longer available online, it is
available on request. This resulted in a BMJ publication
(Robotham JV, et al. BMJ 2011;343:d5694. doi:
10.1136/bmj.d5694) and an accompanying editorial. There
have been three associated publications further detailing the
methodologies (Worby CJ, et al. Am J Epidemiol
2013;177:1306-13. Barnett AG et al. Am J Epidemiol
2009;170:1186-94. Deeny SR, et al. J Hosp Infect
2013;85:33-44). The NOW study report itself was peer
reviewed by four referees including a health economist. The
audit data from the NOW study have been published (Fuller
C, et al. PLoS One 2013;8:e74219). The main study
publication is in final stages or preparation before submission.
The current version of the NOW study report is available at
www.idrn.org/audit. This reference has been updated in the
implementation guidance.
We believe that it would not be ideal to wait for publication
and then consider how to implement the findings of the study,
not least considering the costing conclusions.
E) The names of the Implementation Group have been added
to the report, along with its remit.
F/G) We agree that much of the anticipated savings come
from reductions in isolation, and accept that this is a

Implementation of modified admission MRSA screening guidance for NHS (2014)
19
the modelled costs of each strategy. These isolation costs themselves are
plausible (£333 per day for a standard bed and an additional £88.43 per day
for isolation nursing) but it is wholly disingenuous to use these to inform
decisions about screening. The argument becomes essentially that we
should screen fewer patients in order to isolate fewer patients. Setting aside
the point acknowledged by the NOW study itself that many carriers identified
are not isolated anyway (so these savings are not there to be had), as an
attempt to inform national screening policy this is either cynical or muddle-
headed.
G) Using the modelling parameters in the NOW study, for the average acute
trust we calculate that the saving in screening costs of high-risk area
screening compared to universal screening would be about £260k pa. If we
accept that only 61% of universal screens are actually taken then the saving
would be at most £158k (if only 61% of targeted screens were taken) and
possibly as little as £63k (if all targeted screens were taken). These
calculations assume that the costs of laboratory processing are independent
of screening volume – in reality the fixed nature of laboratory costs will mean
that the savings are less – but as a ball-park figure we might say that
targeted rather than universal screening has the potential to save the
average trust about £100k per annum. This, not £1.6 million, and is the figure
to weigh carefully against the costs and risks.
contentious issue. However, there is insufficient capacity to
isolate patients for infection reasons. MDR GNB threat needs
to be managed. The current recommendations help rather
than hinder the MDR GNB challenge.
The costs calculated from the model are not simply cost
savings resulting from screens ‘prevented’. They encapsulate
all bed day costs, infection-related costs, and intervention
related costs associated with onward transmission within the
whole hospital population (and therefore differences in lengths
of patient stay, movement around the hospital and risk of
death).
It is correct that the differences in cost of isolation outweigh
differences in cost of screens. However, given that the
effectiveness of any screening strategy is entirely dependent
on the control measures that accompany the screening,
screening and control were necessarily modelled, and
evaluated, together. Screening in itself does not create any
effect ( i.e. health benefits), and so to evaluate the cost-
effectiveness of screening in and of itself makes little sense in
this case. The only difference in effect brought about by
different screening options will be the difference in level of
control imposed. It is therefore the effect that these differing
levels of control result in, that are estimated. Both costs and
effects therefore need to be evaluated in terms of both
screening and accompanying control. This is also the
practice used elsewhere - see for example the Scottish
Pathfinder MRSA evaluation of MRSA screening.
The more important point though, is that it is the difference in
bed day costs, far exceed any intervention related costs (e.g.
either screening or isolation costs), and it is differences in
mortality and length of stay between infected and uninfected
patients, that dominate the cost results.

Annex: Consultation
20
H) As well as over-estimating the benefits of the proposed change, the
proposal underestimates the costs and risks. In particular, knowledge that a
patient's recent MRSA screen was negative is useful information when
choosing empiric antimicrobials: absence of a negative screening result might
lower the threshold for expensive (and potentially toxic) treatments such as
linezolid and daptomycin in patients with suspected staphylococcal infections,
while absence of a positive screening result might delay the initiation of
appropriate anti-MRSA treatment and cause treatment failure. Another
advantage of universal screening is that it facilitates detection of in-hospital
MRSA acquisitions, events that can be a bell-wether for lapses in infection
control practice generally. As far as we can tell, none of these was included
in the modelling.
I) Finally, the proposed small increase in transmission events is impossible to
affirm without seeing the calculation, but even if we take the figures at face
value these will translate into real infections and real deaths in NHS patients.
If that harm is really felt to be outweighed by the benefits then the Dept of
Health must disavow its previous zero tolerance of MRSA infections.
H) The perspective of the study is that of a regional or
national level healthcare decision maker, i.e. with the whole
health economy to consider. We agree that there may be
other benefits of universal screening, not included in the
model; for example, antibiotic choice. However, without data
on these additional benefits, for example the impact of
‘knowledge of MRSA status’ on antibiotic decision making,
and the subsequent effects that that decision making has
(primarily on patient’s length of stay and mortality) – any effect
of screening on antibiotic choice could only be included as a
scenario analysis. Given the given the current low prevalence
of MRSA, the number of scenarios in which infections that
would otherwise have been ‘detected’ (by ‘universal’
screening) is likely to be very small. The model does
acknowledge that a very small number of MRSA infections will
be missed.
With reference to the reviewer’s point regarding ‘missing’ any
in hospital transmission – this is true. We acknowledge that
the cost/QALY approach used here will not identify the ‘best’
policy if the desired outcome is monitoring (and subsequent
reduction) of colonisation within the hospital. The evaluation
was conducting to identify the ‘best’ policy option in terms of
cost per quality adjusted life year gained (which, in this case,
largely related to those policies best able to reduce infections
as opposed to colonisations).
I) There is no contradiction between the Government’s stated
policy of zero tolerance and an effective, targeted, evidence-
based screening policy for MRSA bloodstream infections.
The transmission dynamic modelling based approach was
used specifically to capture the infections and deaths

Implementation of modified admission MRSA screening guidance for NHS (2014)
21
In summary, we accept the suggestion that compared to universal screening,
some kind of targeted screening strategy might detect 80% of colonised
patients while incurring only half as many screens. However we do not
accept that a robust cost-benefit assessment has yet been made –
specifically we do not accept that the costs of isolation nursing are germane
to a decision on screening strategy. Removing those costs, we calculate that
this change would save the average NHS trust something like £100,000 per
annum at the expense of increases in MRSA infections, empiric antibiotic
costs, the consequences of delayed treatment of MRSA infections and other
non-trivial adverse outcomes: this is the cost-effectiveness calculation that
needs to be undertaken before an evidence-based policy change can be
made.
Finally, we wish to express surprise at the way in which the results of an
unpublished and methodologically opaque study are being misrepresented to
influence this important debate.
Fig A3 (NOW study p72) showing that the cost-effectiveness modelling is
overwhelmingly about the costs of isolation, not the costs of screening.
associated with each of the strategy options (and especially to
the knock on infections and deaths brought about due to
transmission). Total quality adjusted life years gained under
each strategy are compared. The cost/QALY approach is
therefore used in order for these infections and deaths to be
included within the decision making process. The purpose of
presenting health benefits as QALYs is to allow decisions
across the health sector to be compared (using the same
units) and so to enable rational decision making.
The differences in the numbers of infections and colonisations
are the output of the transmission dynamic model, simulating
transmission throughout the hospital for each scenario over a
5 year period. i.e. 13,000 lines of computer code – run 1000’s
of times. It is therefore difficult to provide a ‘calculation’. This
is the case with any such model-based cost-effectiveness
evaluation. It is the model structure and the inputs that are
driving the simulation.
The computer code itself is available on request. However,
reassurance should come from the fact that the code has
been developed by a team of mathematical modellers, subject
to a multitude of checks, and resulted in numerous peer
reviewed publications.
Methodology (A)
We note that the recommendations are based on the findings of the NOW
study. It would appear that the NOW report has not been published in any
peer-reviewed format, although it is available on certain websites. Page
numbers below refer to the copy of the publication on the idrn.org web site.
Furthermore, the consultation paper refers to a “report on file” in the DH
(reference 8).
A) Please see above answers (4) regarding NOW study
availability, publication and peer review.

Annex: Consultation
22
Assumptions
(B) The rationale for some of the assumptions are puzzling. For example,
“Direct infection from a susceptible state cannot occur in low risk specialty
settings and patients must first become colonised” (pg 193)
We have reviewed the assumed parameters (pg 210). Unfortunately, due to
the time scales available, detailed review of the sources of the information,
and the extent that the data could be extrapolated from one setting to another
was not possible.
(C) The principal driver of changes in costs in the economic model appeared
to be the bed day costs for the admission of individual patients, set at an
average of £333 (pgs 210, 234) and incremental costs of placing a patient in
an isolation room, set at £88.43/day. We note that 100% bed occupancy is
assumed in the model (pg 193). Therefore, there would not be any
incremental costs directly resulting from patient admission or placement in a
single room. Indeed, if the report’s conclusion that there will be an increase,
however “minimal” (pg. 12), in infections consequent to the proposed
changes in screening practice is accepted, a increase in total bed days would
be expected, bed capacity permitting. It is therefore unclear why bed days
costs would be lower in strategy 1 (pg 234).
(D) We also note that contact precaution costs per se were set at £19.53/day.
In our experience, wards do not normally increase their staffing complement
in reaction to small changes in the number of patients being nursed in single
rooms. Furthermore, we presume that this cost cannot relate exclusively to
consumables; if this includes costs such as enhanced cleaning, in a context
where highest possible standards of cleaning are expected on an ongoing
basis (and indeed demanded by regulatory authorities), it is difficult to see
how such additional costs would be incurred. Indeed, if the consequence of a
reduction in screening were to be considered to its natural conclusion, this
B) The value of this parameter for a high risk setting was
extremely low, and therefore it can reasonably be assumed to
be lower for low risk specialities. As this is such a rare event,
it was computationally sensible to assume this to be zero.
This assumption enabled transmission estimates for this
setting to be estimated using hospital data. It is worth noting
that patients could acquire colonisation on day x, and
subsequently become infected on day x+1, and the probability
of each of these transitions was estimated using individual
level hospital data. Furthermore, given that susceptible and
colonised patients were assumed equally infectious, there
would be no difference in their transmission potential.
C) Increases in numbers of infections resulted in (on average)
longer patient stays. While we absolutely agree with the
reviewer that under the assumption of 100% bed occupancy,
this does not, in itself, result in increased bed day costs.
However, it is the opportunity cost of bed days lost to treat
other patients that we describe. Results presented are
divided by the number of admissions. Therefore, longer stays
will prevent admissions, decreasing this denominator, and
increase bed day costs per admission.
D) Contact precaution costs were taken from the Scottish
MRSA Screening pathfinder study, in which they updated the
estimates from the previous HTA Report (Ritchie K, et al.
Consultation report on health technology: Clinical and cost
effectiveness of screening for MRSA. NHS Quality
Improvement Scotland, 2006. Available at:
http://www.nhshealthquality.org/nhsqis/3780.html
In brief, this included: 12 patient contacts per day by

Implementation of modified admission MRSA screening guidance for NHS (2014)
23
will lead to a modest increase in infections, and logically a greater inevitable
increase in unrecognised colonised individuals - cleaning standards would
therefore need to be increased across the board, in order to compensate
from the inevitably increased risk of transmission of MRSA.
(E) The report states that the average charge made by laboratories for MRSA
screening was £5.68, (sd = £4.44), pg. 19. In the model, different costs were
used, £7.24 for a positive, £4.24 for a negative test (pg.210). It is widely
known that the cost of reagents and associated laboratory staff costs, ranging
from specimen reception, through processing and result issue would scarcely
lead to cash releasing savings of more than around £1 per screen set, as all
fixed costs (ranging from estate and major equipment to managerial and
medical costs) would still have to be met, but in the NHS economic model,
these fixed costs would be included in quoted costs (only 2% of hospitals use
private providers, where a reduction in total specimen volume might lead to a
cash-releasing savings in excess of reagent and direct staff costs).
Incidentally, the author recently attended a UEMS Microbiology section
meeting where it was reported that private laboratories in Germany charge
between Euro 1.50 to 3.50 per patient screen (these quoted costs would
include a contribution to fixed costs), thereby providing some validation of the
suggested true marginal costs above, assuming that UK laboratories are
organised in an optimal efficient manner.
Similarly, swabbing cost of £4.20 was used (pg. 210). Other than the true
marginal costs of the swabs themselves, a reduction in nursing time spent
swabbing a patient would not lead to any reduction in the staffing
complement on the ward and would therefore not release any savings.
(F) Modelling
No sensitivity analysis to changes in the cost parameters was presented. It
would be instructive to see the effect of re-running the model with marginal
costs to take into account reasonably expected cash releasing.
healthcare staff (3 minutes per contact needed to ensure
compliance). Plus consumables for each contact of one pair
of gloves and one plastic apron. Providing a total daily cost
including overheads. (see pg 64 of HTA report for more
information).
E) Again, screen costs were taken form the best available
evidence, which was again from the Scottish Pathfinder study.
It is worth reemphasising that all of these costs will be
dwarfed by differences in cost brought about by differences in
length of stay and mortality (due to differences in numbers of
infections between strategies). Note the differences in scale
between each of the cost components on any of the cost
plots.
Having said this, large reductions in testing could release
estate/space/staffing, or make these available for other
purposes e.g. CPE screening, nurse directed care, etc.
F) Indeed, it would be ideal to include uncertainty in these
cost estimates, in the full probabilistic sensitivity analysis.
However, it is unlikely that the decision between strategies
would change under different cost assumptions (other than
the cost of bed days which dominate the evaluation).

Annex: Consultation
24
The model also appears to be static in time and does not take into account
the reasonable expectation of an inevitable increase in colonisation rates that
would occur over time in those strategies that entail lower screening and
therefore detection rates. Over a period of several years, it can be expected
intuitively that as colonisation rates increase, so will transmission, with an
inevitable acceleration in infections.
(G) We could find no evidence that the model took into account changes in
compliance with screening in the different models. One of the implicit
criticisms of universal screening in the consultation paper is the observed
compliance rate of 61%. Intuitively, compliance with various forms of check-
list activated compliance is unlikely to exceed this figure. Experience of
practitioners practising in the field of IPC would argue that compliance is very
much aided when embedded in routine practice. Therefore a change away
from universal screening can be reasonably expected to lead to a greater
proportion of unisolated MRSA patients, with a consequently greater risk of
transmission to others.
(H) Screening practice
The consultation paper states that screening compliance at the time of the
NOW study data collection period was 61%.
However, the data collection period was in May 2011 (pg. 8), only a few
months after the introduction of universal mandatory emergency admission
screening. It is reasonable to assume that in the early months, Trusts were
still developing their systems and that compliance has improved considerably
since. It would therefore be inappropriate to use data that applied in 2011 to
inform current practice, particularly as there is considerable anecdotal
evidence from IPC practitioners in London who are members of this Forum,
that compliance with established screening policies is very high in most
organisations.
Admission colonization rates fell in the years before
implementation of the current screening guidance.
Also, guidance states that local decisions about who/where to
screen may be required according to local epidemiology.
G) This is true. However, we took the decision early on in the
NOW study to compare each of the strategies against one
another ‘on a level playing field’ and to see how each fared
under the assumption of 100% compliance.
Actually, recently published evidence from Scotland
(http://www.bmj.com/content/348/bmj.g1697/rapid-responses
)
provides further evidence that risk-based approaches to
MRSA screening can be successful in clinical practice and
maximise cost-effectiveness.
H) The modelling assumed 100% compliance with each
policy.

Implementation of modified admission MRSA screening guidance for NHS (2014)
25
(I) The report states that at the time of the survey, the turnaround time for a
positive result was nearly 3 days, and nearly 2 days for a negative result (pg.
19). In our opinion, there is considerable scope for improvement, which may
well have been achieved, at least in some laboratories, particularly those that
have embraced continuous quality improvement initiatives. For example, in
the author’s laboratory (until 2013) negative results and presumptive positive
results were routinely issued within 24 hours, 7 days per week.
For patients whose results become available after discharge, in our
experience, systems have been put into place in many hospitals to notify
primary care of the result, enabling GPs to prescribe suppressive /
decolonisation therapy should this be considered beneficial. In any case
given the high frequency of re-admission, this provides additional useful
information to inform patient placement immediately on presentation should
re-admission be required.
(J) Patient placement and decolonisation / suppression management
The report states that the one-day audit demonstrated that only 55% of new
MRSA patients were isolated and that decolonsation / suppression therapy
had been started in only 73% (pg. 19). The audit did not appear to collect
data on time from MRSA detection to implementation of isolation and
commencement of decolonisation / suppression treatment. It is therefore
unclear whether these deficiencies were merely temporal and the proportion
of unisolated / untreated patients at, say 6 and 24 hours does not appear to
be know in this study cohort.
Sensitivity analysis of costs at various colonisation rates
The authors of the NOW report have run the model at various prevalence of
colonisation. There are limited data on prevalence of MRSA among
emergency admissions. However, a “very high” rate of 5% may well be less
than the rate that may be encountered should national guidelines
I) This evaluation was an extension to previous work, and at
the time of being conducted, the turnaround times
represented synthesised estimates from a review of the
available evidence in the literature; these accurately reflected
the turnaround times for MRSA positive patients reported in
the NOW audit. We acknowledge that these may indeed be
reducing all the time. This is an inherent problem in the
evaluation of screening, with ever faster (and cheaper) tests
being developed.
(J) National audit data from individual patients were used
here. The study recorded if all positive patients that week, or
randomly chosen negative patients, were isolated before or
after screening result became available. Isolation usually
occurred as soon as a positive result was known, but many
patients were home before results were available.
The model reviewed multiple scenarios, including varying
MRSA rates. Guidance clearly cites the need for prospective
surveillance and review of policy.
Note that previous modelling work (DH MECAMIP study)
found that while screening and control is likely to be cost
effective at a prevalence of 10% (including universal
screening) in ICU settings, this was not the case in general
medical wards. The NOW study included data on all
emergency admissions in England during one week. We are

Annex: Consultation
26
recommend selective screening once again. For example, G Rao et al (JHI.
2007; 66: 15) had observed MRSA colonisation rates of 8.6% among
admissions (6.7% of individual patients). The author had also observed
colonisation rates of 6-8% among emergency admissions in 2008 prior to
introduction of universal MRSA screening at his hospital (unpublished data).
(K) Additional, practical, considerations
Most experienced practitioners do not consider that it is practical or feasible
to identify high risk patients in an A&E environment. There is published
evidence to support this (for example G Rao et al. JHI. 2007; 66: 15).
(L) At high levels of bed occupancy, patients are frequently transferred
between wards, including those that are classified as high and low risk.
Allowance for this effect does not appear to have been made in the model.
Practical considerations around this would be considerable.
Experienced practitioners recognise that IPC operates in a human
environment. Consequently, application of precautions intended to minimize
transmission (e.g. effective hand hygiene) are more likely to be applied
consistently when risks are known, such as in known MRSA colonised
patients, who are being nursed with contact precautions.
Knowledge of an individual patient’s MRSA status is valuable in empirical
antimicrobial choices, thereby potentially leading to increases in antimicrobial
costs if this information is not available. This element was not included in the
costing model.
unaware of any more extensive data, including in the Scottish
pathfinder study.
(K) This is not true. Patients at high risk of infections are/can
reasonably be screened in A&E e.g. influenza, viral
gastroenteritis, SARS, etc. Infection control teams should
turn their attention from screening everyone to ensuring that
high risk patients are screened. For a fraction of the costs of
routine screening, one could invest in audit and feedback
systems to ensure that compliance with high risk screening is
high.
(L) High risk and low risk ward transfers were estimated using
individual-level hospital data, and therefore aimed to reflect
real hospital movements. These transfers were included in
the model.
All of which comes at a cost. National audit data were used in
order to make the modelling representative of clinical practice.
This is not in accordance with the application and practice of
standard precautions.
Please see above response regarding empirical prescribing.
The aim was to estimate the optimal policy; ‘optimal’ was
defined in terms of cost/QALY. We agree that if the definition
of optimal differed, e.g. instead the policy that best enabled
monitoring (or reduction) of colonisations, then the decision
would have differed.

Implementation of modified admission MRSA screening guidance for NHS (2014)
27
(M) Centres that implemented universal MRSA screening at a time when
‘avoidable’ cases of MRSA bacteraemia had already been all but eliminated
observed a rapid and marked reduction in true hospital acquired infections or
colonisations. For example G Rao et al. JHI. 2007; 66: 15, Sarma et al. ARIC
2013; 2: 2, A. Mifsud unpublished observations.
(N) Once systems have been established for screening, these can be
relatively easily adapted to take into account changing needs, such as
screening for CROs and other emerging infections. Dismantling of universal
programmes will make subsequent re-instatement difficult.
(O) It has been suggested that universal use of antisepsis may reduce the
impact of reduced screening. However, the recent recognition of MRSA
strains carrying the antiseptic resistance genes, such that they are clinically
resistant to chlorhexidine, should strike a note of caution against its
unfettered use (Edgeworth JAC. 2011: 66 s2: ii41)
(P) DIPC Forum recommendation
We have concerns around the assumptions used in the economic model,
such that we suspect that the financial case may not be as stark as
presented. We are certain that genuine cash releasing savings may well ot
ensue, and indeed, if the history of management of MRSA in the UK in the
1980s and 1990s is repeated, a large increase in infections and therefore
costs can be anticipated with a high degree of probability.
M) The Rao et al study was observational over a one year
period and noted ‘The study was not designed to establish
whether this reduction was causally associated with the
screening programme.’ In the Sarma et al single centre
observational study, multiple interventions occurred
(‘Following the introduction of Root Cause Analysis in May
2006 a number of interventions were made in quick
succession as part of the MRSA improvement programme’).
Whilst there was a significant association with the introduction
of screening, it is not possible to conclude that other
measures drove or part drove the observed decline in MRSA
infection.
N) We are not advocating dismantling systems for screening.
Targeted MRSA screening reasonably can release resources
to implement other screening e.g. for CROs.
O) We have not advocated ‘universal use of antisepsis.’
P) There is no contradiction between the Government’s stated
policy of zero tolerance and an effective, targeted, evidence-
based screening policy for MRSA bloodstream infections.
Furthermore, nothing in this revised guidance negates the
need for effective surveillance, screening and reporting
generally. In fact, the guidance makes it clear that ‘Trusts will
need to regularly review (and where necessary improve) their
compliance with national screening guidance for each

Annex: Consultation
28
In principle we are not supportive of mandatory measures. However, in this
particular case, we are convinced that withdrawal of universal MRSA
screening will inevitably lead to an increase in MRSA colonisation rates
which, over time, will lead to an increase in colonisation rates in the
community and will impact on the spread of MRSA in other hospitals in the
vicinity. Relaxed control of MRSA in one hospital can be expected to give rise
to a geometric build up of cases within the community and will impact on
cases in adjacent hospitals.
Furthermore, the removal of mandated MRSA screening is incongruous in
the context of the DH’s stated objective of zero tolerance of avoidable
infections. The current performance management regime around MRSA
bacteraemia management includes stringent criticism and sanctions. A
system that allows sub-ideal performance in some respects but not in others
appears perverse.
We would suggest that efforts are focussed on fine-tuning the current MRSA
management pathways, for example by reviewing screening in situations
where transmission is unlikely, e.g. in most day case surgeries,
improvements in compliance with universal emergency admission screening
(if poor performance still occurs), improving laboratory testing and reporting
processes, such that cash releasing savings could be accrued by withdrawal
of molecular testing , and improving the primary / secondary care interface to
ensure good flow of information and action across the sectors.
specialty, recent MRSA infection data, patient demographics
and types of services provided within individual organisations.’
The guidance also clearly states need for continued
local/national surveillance. If MRSA rates increase then can
revisit case for screening. The guidance also states that local
risk assessment can be used to make decisions about
who/where to screen.
Cost effectiveness is not perverse. It is one of the
requirements of good management of public resources. The
key reason to conduct evaluations such as the NOW study is
to provide a rational basis for decision making and allocation
of scarce resources. We do not have any other evidence
from RCTs etc for whole hospitals based on representative
national data. The model and report are from the perspective
of the regional health policy maker who is considering the
picture for the health economy.
The suggested alternatives remain conjecture.
Introduction section
* Not sure if this part will be included in final guidance??
Introduction section, 3rd paragraph
* Re: The NOW study showing that 'compliance with current mandatory
Yes it will but modified as above.

Implementation of modified admission MRSA screening guidance for NHS (2014)
29
screening policy was poor (e.g. only 61% were screened;...'
o More informative to give the breakdown by admission type as given by
NOW study: the NOW study showed this related to 61% of patients in the
emergency admissions category and 41% in the eligible day case admissions
category but it was highest in the elective admissions category (81% of
patients).
* The next point: ..'about half of new positives were isolated when their
result became known'
o Better to make clear that overall, 55% of new positives were isolated
once results were confirmed
* The next point: 'and about a quarter did not receive decolonisation
therapy..'
o First this information is not included in the Appendix of the consultation
o Second, the result quoted is confusing. The NOW report showed that
34% of Trusts did not use pre-emptive suppression/decolonisation on any
admitted patient (see Table 9 in NOW report). Or was consultation referring
to 27% of patients that did not receive decolonisation once their MRSA result
was known.
Introduction section, 5th paragraph
The reader can refer to the NOW study for more detail if
required - this is an overview.
OK.
Do not understand the point.
The latter.

Annex: Consultation
30
* Re: 'Approximately 60% of MRSA colonised individuals will be
detected by screening those known to be previously MRSA positive and high
risk specialty admissions'.
o I did not see this result anywhere in the NOW report. This statement
implies that three pieces of information needed, a denominator for all risk
factors, the numerator for prior MRSA and numerator for high risk specialty.
In fact if 60% refers to these two groups they must be mutually exclusive and
another numerator should be included which comprises patients with both
these risk factors present (even if 0). Is his based on Table 29a? Whatever
the 60% refers to, this needs to be clarified.
Summary
* Re: 'Importantly, focussed screening should be adopted in line with
local risk assessments..'
o If focussed screening to be main national policy then better to say:
'Importantly, focussed screening should be adopted, where necessary, as
indicated by local risk assessments..'
* Re: 'Trusts will need to consider current compliance with mandatory
screening guidance for each specialty...'
o This sentence refers to the 'current' situation regarding compliance to
existing guideline. Once the existing guideline (screening all admissions)
becomes obsolete everything else will by association be irrelevant. Better to
say: 'Trusts need to regularly review and where necessary, improve their
compliance with national screening guidance for each specialty...'
This is calculated from data in the report. Simplistically, 50%
are previous MRSA +ves plus high risk screening identifies a
further 10%.
Suggested rewording is not what we mean.
OK.

Implementation of modified admission MRSA screening guidance for NHS (2014)
31
After Objective, add a short Background section - this will include definition of
MRSA/ habitat/transmission dynamics/impact on length of stay,
morbidity/mortality
The screening groups are confusingly written. Due to layout there is a
possibility of misinterpretation. Solution advised as follows.
After Background section, important to add a section called: Screening
categories.
* For clarity re-organise information under Screening categories:
o Keep: 'Elective or acute admissions to high risk specialties (defined
below)'.
o Remove the sub-bullet point: 'all patients admitted to critical care units' -
these are already included in the high risk specialties list.
o Remove the sub-bullet point: 'all patients previously identified as
colonised with or infected by MRSA' - these would be included in the local
risk assessment component. (The NOW study in fact identified high risk
specialty screening (reverting to previous strategy) as the most cost-effective
strategy. The NOW report did not specifically have findings for 'prior MRSA'
alone (in any case it was embedded in the strategy that included all
admissions i.e. strategy #6).
o Add: 'Additional specified patient groups identified through local risk
No, too much detail. This information is widely accessible.
Formatting will be checked in published guidance.
We are not just charged with implementing the NOW findings
but are to use our judgment in using that evidence to revise
guidance.
Annex: Consultation
32
assessment'
So the 'Screening categories' plus sub bullets would finally look like as
follows:
Screening categories
* Elective or acute admissions to high risk specialties (defined below):
o Sub-bullet point: High risk specialties are defined as vascular,
renal/dialysis, neurosurgery, cardiothoracic surgery,.........Coronary Care
Units
* Additional specified patient groups identified through local risk
assessment
o Sub-bullet point: Local risk assessment should be used to define other
potential high MRSA risk units/specialties; for example, according to
provision of localised specialised services.....endemicity of MRSA.
o Add after this: 'Include all patients previously known to be MRSA
positive'.
o The continue with: 'Local risk assessment may increase the proportion of
detected colonised individuals, notably.....poor outcome from MRSA. (bold as
Implementation of modified admission MRSA screening guidance for NHS (2014)
33
found in consultation)
Interventions, No.8, add word 'effective'
* All patients identified as MRSA positive must receive effective
decolonisation/suppression therapy
Compliance and audit
* Suggested edits as follows:
o Remove i. and keep the statement: 'Trusts should make every
effort....groups identified above' as opening descriptive statement.
o The next point ii should now be i
• vi (which is now v) should begin with: Patient feedback of results is
important. A qualitative study on the patient experience.......experience
is necessary'
•
Unnecessary – we would not advocate ineffective therapy.
Thank you for the suggestions, but we have elected to keep
the original version as others have not commented on a need
for change here.
(A) Concerns that the modelling used in the NOW study is flawed
because of the underlying assumptions.
Other modelling studies have suggested that a combined approach of
isolation and screening confers efficacy (e.g. Bootsma‐M et al. 2006 PNAS;
103: 5620–5625). Coia
‐
J (BMJ 2014;348:g1697) wrote: “A prospective case
‐
control study of more than 12000 patients showed that screening strategies
(A) Indeed, the transmission dynamic model was informed
assuming that isolating patients is an effective control
measure. Precisely, the model input was a 64% (S.D. 14%)
reduction in transmissibility due to isolation. This is reflected
in the model results – where reductions in transmissions,
infections and deaths are seen for all strategies involving
screening and isolation. Furthermore, the strategies were

Annex: Consultation
34
of sufficient sensitivity require screening of 65% of admissions (Harbarth S at
al. Evaluating the probability of previously unknown carriage of MRSA at
hospital admission. Am J Med 2006;119:275.e15‐23)
(B) Importance of Medical Devices in patients
Members experience suggests that serious MRSA infections and
bacteraemias have been seen in subgroups of patients with long term
medical devices in situ especially those devices that patients take with them
into community settings e.g. nephrostomies, central intravascular devices,
long term urinary catheters.
This is seen especially in patients with underlying malignancy. This needs to
be factored in when writing screening guidance for practical use, maybe at
the specific trust level.
(C) Practical problems in implementation
In hospitals with >95% adult bed occupancy rate, many patients are
transferred several times during an admission, including transfers between
“low risk” wards and “high risk” wards. Thus, even if identifying populations at
high risk for MRSA carriage may be feasible, universal screening may be
easier to implement, as risk categorisation may have to change throughout
admissions due to the mix of patients in different wards and clinical areas.
(D) Realisation of projected cost savings
Cost savings make some assumptions that may not be practically realisable.
In addition there are additional costs to not having MRSA status from recent
screening. Savings are based on not screening (cost of implementing
screening) and not therefore isolating patients. However many patients are
not isolated in single rooms in low risk areas. Knowledge of MRSA status is
compared in terms of these effects combined with costs.
(B) There is no clinical and cost-effectiveness evidence to
support the screening of patients with medical devices and
this was not considered by the NOW Study. However, the
guidance allows local risk assessment to define other high
MRSA risk groups, which may include these groups of
patients.
(C) Although it is recognised that the process may not always
be straightforward, appropriate risk assessment should be
able to categorise the majority of patient groups correctly.
Issues with implementation are not a justifiable argument to
sustain universal screening in the absence of cost-
effectiveness data.
(D) Please see answers above.
Briefly, savings are not due to not isolating patients, but
instead due (primarily) to reductions in infections (and
therefore length of stay). The cost figures demonstrate that
any differences in isolation costs are dwarfed by the
differences in bed day costs (brought about by reduction in
length of stay – in turn brought about by reduction in
infections).
The potential costs of not knowing MRSA status are difficult to
quantify, but are not likely to be significant in low risk patient
groups. Issues with implementation are not a justifiable
argument to sustain universal screening in the absence of
cost-effectiveness data.

Implementation of modified admission MRSA screening guidance for NHS (2014)
35
believed to prompt enhanced precautions in staff – encourages compliance
i.e. modifying behaviour to reduce transmission risk. There is a cost in
implementing selective screening in the training, auditing, time necessary to
achieve a more complex system. It is likely to be hard to successfully
implement and maintain compliance. Knowledge of MRSA screening results
gives confidence in not using agents such as linezolid or daptomycin in the
initial treatment of serious infections with a likely staphylococcal cause.
(E) Long term implications
Risk‐based screening for MRSA carriage is likely to miss too many carriers of
MRSA to achieve meaningful control of MRSA infections including prevention
of MRSA bloodstream infections in the long term (5‐10 years).
(F) Stratified Implementing of revised screening policies
NHS hospitals that suffer from >95% adult bed occupancy rates and continue
to have seen hospital‐acquired MRSA bloodstream infection in the last 24
months, should continue with universal admission screening. NHS hospitals
that have not seen any hospital‐acquired MRSA bloodstream infection in the
last 24 months could trial alternative practical strategies of screening for
MRSA that are less costly.
(E) There is no evidence to support that appropriate risk-
based screening will fail to achieve meaningful control of
MRSA. The guidance does advocate prospective surveillance
to determine if revised risk assessment and policy change is
required.
(F) There is no evidence to support this statement. The
guidance allows local risk assessment to identify appropriate
high risk groups of patients who should be screened The
guidance does advocate prospective surveillance to
determine if revised risk assessment and policy change is
required.
Compiled by Prof Mark Wilcox on behalf of MRSA Screening Implementation Group, June 2014
