
FEDERAL
EMPLOYEES
HEALTH BENEFITS
PROGRAM
Additional Monitoring
Mechanisms and
Fraud Risk
Assessment Needed
to Better Ensure
Member Eligibility
Report to Congressional Requesters
December 2022
GAO-23-105222
United States Government Accountability Office

United States Government Accountability Office
Highlights of GAO-23-105222, a report to
congressional requesters
December 2022
FEDERAL EMPLOYEES HEALTH BENEFITS
PROGRAM
Additional Monitoring Mechanisms and Fraud Risk
A
ssessment Needed to Better Ensure Member
Eligibility
What GAO Found
The Office of Personnel Management (OPM) is responsible for administering the
Federal Employees Health Benefits (FEHB) program. OPM has taken steps to
enable a process for employing offices and FEHB carriers to identify and remove
ineligible FEHB members. For example, OPM amended its regulations in
January 2018 so that employing offices and FEHB carriers may—but are not
required to—request proof of family member eligibility at any time for existing
participants. OPM also issued new requirements in 2021 for employing offices
and FEHB carriers to verify family member eligibility for certain types of new
enrollments.
However, OPM does not plan to establish a monitoring mechanism to identify
and remove ineligible family members who already have FEHB coverage.
Without such a monitoring mechanism, ineligible family members may remain
covered and related improper payments may continue to accrue over time. OPM
has estimated these related improper payments could cost the program up to
approximately $1 billion per year.
OPM performs an annual fraud risk assessment of the FEHB program but has
not included ineligible members as a fraud risk to the program. In fiscal year
2020, OPM conducted a fraud risk assessment and documented a fraud risk
profile for the FEHB program. OPM determined the program was at a low risk of
fraud overall. However, OPM’s fraud risk assessment and profile did not include
fraud risks associated with ineligible members in the program.
OPM acknowledged in discussions with GAO that not verifying eligibility for
current members carries a risk of fraud and improper payments. OPM’s Office of
the Inspector General has also documented instances of fraud and improper
payments associated with ineligible members in the FEHB program. For
example, a federal employee fraudulently covered two individuals purported to be
his wife and stepchild in the FEHB program. The individuals were ineligible and
remained on FEHB health insurance for about 12 years. The FEHB program paid
claims totaling more than $100,000 on behalf of these ineligible individuals.
Until OPM assesses the likelihood and impact from the fraud risk of ineligible
FEHB members and documents that assessment, it cannot support its
determination that the program is at a low risk of fraud. As a result, the program
may remain vulnerable to the fraud risk associated with ineligible members.
View
GAO-23-105222. For more information,
contact
Seto J. Bagdoyan at (202) 512-6722
or
Why GAO Did This Study
FEHB is
the largest employer-
sponso
red health care program in the
country
. It provides health insurance
benefits to more than 8
million federal
employees
, family members, and
other
s at a cost of about $59 billion in
fiscal year
2021. Until 2021,
employing
offices were
not required to review
eligibility documentation to verify family
member eligibility
. This left the
program vulnerable to fraud and
improper payments associated with
ineligible family members
.
This report identifies
, among other
things,
the extent to which (1) OPM
has implemented control activities to
identify and remove ineligible
family
members
with FEHB coverage and (2)
OPM’s fraud risk assessment
for the
FEHB program
includes fraud risks
related to ineligible
FEHB members.
GAO analyzed
OPM documentation
and
interviewed OPM officials as well
as
officials from a nonprobability
sample of
five federal employing
offices
, selected to obtain views from
offices of
different workforce sizes.
GAO also interviewed
officials from
five
FEHB insurance car
riers representing
approximately 8
7 percent of FEHB
enrollment at the time of GAO’s
review
.
T
he interview information is illustrative
but
not generalizable.
What GAO Recommends
GAO
is making four recommendations
to OPM
, including that it implement a
monitoring mechanism
to identify and
remove ineligible family members from
the FEHB program
and assess and
document
the likelihood and impact of
fraud risks associated with ineligible
FEHB
members. OPM generally
agreed with our recommendations.

Page i GAO-23-105222 Federal Employees Health Benefits Program
Letter 1
Background 4
OPM has Implemented Preventative Controls But Cannot
Reasonably Ensure Ineligible Family Members are Not Covered
in FEHB Enrollments 10
OPM Relies on Limited Efforts to Identify and Remove Ineligible
Family Members with FEHB Coverage 14
OPM’s Fraud Risk Assessment does not Include Fraud Risks
Related to Ineligible Members in FEHB 20
Conclusions 21
Recommendations for Executive Action 22
Agency Comments and Evaluation 23
Appendix I Objectives, Scope, and Methodology 25
Appendix II Comments from the Office of Personnel Management 28
Appendix III GAO Contact and Staff Acknowledgments 31
Figures
Figure 1: The Four Components of the Fraud Risk Framework and
Selected Leading Practices 9
Figure 2: Examples of States that have performed or announced a
Dependent Eligibility Verification Audit (DEVA) for a State
Health Insurance Program (1992 - 2022) 17
Contents

Page ii GAO-23-105222 Federal Employees Health Benefits Program
Abbreviations
DEVA Dependent Eligibility Verification Audit
FEHB Federal Employees Health Benefits
GEMS Government-wide Enrollment and Member Support
OIG Office of Inspector General
OMB Office of Management and Budget
OPM Office of Personnel Management
QLE Qualifying Life Event
This is a work of the U.S. government and is not subject to copyright protection in the
United States. The published product may be reproduced and distributed in its entirety
without further permission from GAO. However, because this work may contain
copyrighted images or other material, permission from the copyright holder may be
necessary if you wish to reproduce this material separately.

Page 1 GAO-23-105222 Federal Employees Health Benefits Program
441 G St. N.W.
Washington, DC 20548
December 9, 2022
The Honorable Ron Johnson
Ranking Member
Permanent Subcommittee on Investigations
Committee on Homeland Security and Governmental Affairs
United States Senate
The Honorable Rick Scott
United States Senate
The Federal Employees Health Benefits (FEHB) program is the largest
employer-sponsored health care program in the country and provides
health insurance benefits to federal employees, retired federal
employees, other eligible individuals, and their eligible family members. In
fiscal year 2021, FEHB provided health insurance benefits to more than
8.2 million individuals at a cost of approximately $59 billion. FEHB-eligible
federal employees and retirees are entitled to enroll themselves and
cover eligible family members in a health insurance plan offered under
the program. The Office of Personnel Management (OPM) administers
the FEHB program by publishing regulations and guidance and
contracting with qualified health insurance carriers, among other
responsibilities. Health insurance carriers that provide FEHB coverage
contract with OPM to offer certain health benefits to all individuals who
enrolled in their participating health plans. Employing offices and FEHB
health insurance carriers bear responsibility for enrolling federal
employees and adding coverage for eligible family members.
1
Since the program’s inception in 1960, OPM has delegated responsibility
to employing offices to make eligibility determinations for enrollees and
covered family members. OPM did not require employing offices to review
supporting documentation to verify family member eligibility during new-
1
Under 5 C.F.R. § 890.101, an employing office is the office of a federal agency to which
jurisdiction and responsibility for employee health benefits actions have been delegated by
OPM. For retirees, the employing office will tentatively determine if an individual is eligible
to continue enrollment at the time of retirement. OPM’s Office of Retirement Programs is
responsible for reviewing the retirement and health benefits documents and making a final
determination of eligibility to continue the FEHB enrollment into retirement.
Letter

Page 2 GAO-23-105222 Federal Employees Health Benefits Program
hire enrollment or certain qualifying life events (QLE) until 2021.
2
Not
doing so left the FEHB program vulnerable to improper payments caused
by inadvertent errors or fraud and abuse associated with ineligible family
members who should not be covered under FEHB. In October 2020,
OPM’s Office of the Inspector General (OIG) reported that OPM lacked
sufficient controls to prevent ineligible family members from being
covered in the FEHB program and recommended that OPM implement an
eligibility verification process for family members to participate in the
program.
3
You asked us to review OPM’s efforts to prevent, detect, and remove
ineligible family members from the FEHB program. This report identifies
the extent to which (1) OPM has implemented control activities to prevent
ineligible family members from being covered in FEHB enrollments; (2)
OPM has implemented control activities to identify and remove ineligible
family members with FEHB coverage; and (3) OPM’s fraud risk
assessment for the FEHB program includes risks related to ineligible
FEHB members.
4
To identify the extent to which OPM has implemented control activities to
(1) prevent ineligible family members from being covered in FEHB
enrollments and (2) identify and remove ineligible family members with
FEHB coverage, we interviewed officials from OPM, five employing
offices, and five FEHB health insurance carriers. To obtain views from
offices of differing employee size, for our interviews with five employing
offices we randomly selected one employing office each from two cabinet-
level departments, one employing office of a large independent federal
agency, one employing office of a medium independent federal agency,
2
As described in greater detail below, QLEs include a change in family status that results
in an increase or decrease in the number of eligible family members, such as marriage,
divorce, and the birth or adoption of a child.
3
OPM partially concurred with this recommendation. We describe actions OPM has taken
since the OIG’s October 2020 report—including issuing new guidance in April 2021—in
greater detail later in this report. Office of Personnel Management, Office of the Inspector
General, Audit of the U.S. Office of Personnel Management’s Administration of Federal
Employee Insurance Programs, (Washington, D.C.: October 2020).
4
In this report, we use the term “members” to refer to federal employees, retired federal
employees, other eligible individuals, and their eligible family members with health
insurance coverage in the FEHB program.
Page 3 GAO-23-105222 Federal Employees Health Benefits Program
and one employing office of a small independent federal agency, as
defined by OPM’s list of federal agencies.
5
For our interviews with FEHB health insurance carriers, we selected a
nonprobability sample of five FEHB carriers that had at least 1 percent of
total FEHB employee and retiree enrollment as of October 2021.
Combined, the five carriers we interviewed represented approximately 87
percent of FEHB employee and annuitant enrollment at the time of our
selection.
6
While the statements from the selected employing offices and
health insurance carriers we spoke with are not generalizable to their
entire populations, they provide specific information about their FEHB
responsibilities and operations. We also reviewed relevant
documentation, such as OPM regulations, FEHB guidance and
instructions for employing offices and health insurance carriers, and
OPM’s FEHB handbook.
For our second objective, we also reviewed relevant documentation,
including final audit reports on dependent eligibility verification audits
(DEVA) performed on behalf of states to prevent, identify, and remove
ineligible family members covered under state health benefit programs.
7
As part of this work, we interviewed three of the six vendors that
contracted with these state health benefit programs to conduct the
DEVAs we reviewed.
For our first and second objectives, we assessed the extent to which
OPM’s responses and documents aligned with principles in Standards for
Internal Control in the Federal Government, specifically the principles
5
OPM maintains a publicly available list of federal agencies and employment numbers on
its website that we used to select employing offices. OPM defines large independent
agencies as those having more than 1,000 employees, medium independent agencies as
those having between 100 and 999 employees, and small independent agencies as those
having less than 100 employees.
6
This percentage does not include family member coverage.
7
A dependent eligibility verification audit (DEVA) is an audit designed to verify the
eligibility of enrollees’ dependents, such as spouses and children. Typically, the entity
conducting the DEVA requests that enrollees provide marriage certificates, birth
certificates, or other documents to demonstrate eligibility.
Page 4 GAO-23-105222 Federal Employees Health Benefits Program
related to designing and developing monitoring mechanisms and
remediating internal control deficiencies.
8
To identify the extent to which OPM’s fraud risk assessment includes
fraud risks related to ineligible FEHB members, we analyzed additional
OPM documentation, such as the agency’s fraud risk assessment, and
interviewed OPM officials. We assessed the extent to which this
information aligned with relevant leading practices in GAO’s Framework
for Managing Fraud Risks in Federal Programs (Fraud Risk Framework),
specifically the leading practices related to identifying and assessing risks
to determine the program’s fraud risk profile.
9
For more information about
our objectives, scope, and methodology, see appendix I.
We conducted this performance audit from May 2021 to December 2022
in accordance with generally accepted government auditing standards.
Those standards require that we plan and perform the audit to obtain
sufficient, appropriate evidence to provide a reasonable basis for our
findings and conclusions based on our audit objectives. We believe that
the evidence obtained provides a reasonable basis for our findings and
conclusions based on our audit objectives.
Although there has been some minor fluctuation in the number of FEHB
members over time, total program coverage has remained around 8
million members since 2000. In the 2021 plan year, the FEHB program
covered approximately 8.2 million individuals, including 2.2 million federal
employees, 1.9 million retirees, and an estimated 4.1 million family
members.
10
For that plan year, OPM had 87 contracts with health
insurance carriers to provide health care coverage for FEHB members.
8
GAO, Standards for Internal Control in the Federal Government, GAO-14-704G
(Washington, D.C.: September 2014).
9
We selected leading practices from the Fraud Risk Framework’s second component that
are most relevant to this objective based on our review of OPM documents and
discussions with OPM staff. GAO, A Framework for Managing Fraud Risks in Federal
Programs, GAO-15-593SP (Washington, D.C.: July 28, 2015). More information on the
Fraud Risk Framework and its leading practices, which are organized into four
components, appears below.
10
A plan year is the 12-month period of benefits coverage under a group health plan. The
FEHB plan year begins on the first day of the first pay period that begins on or after
January 1.
Background
FEHB Program
Page 5 GAO-23-105222 Federal Employees Health Benefits Program
These health insurance carriers offer plans in which eligible individuals
may enroll to receive health care coverage for themselves and eligible
family members. According to OPM data for the 2021 plan year, federal
employees and retirees had the option to enroll in 276 different FEHB
plans. Approximately 66 percent of FEHB enrollees were enrolled in plans
offered by one health insurance carrier.
The FEHB program operates under a diffuse administrative structure.
OPM is responsible for administering the FEHB program. In doing so,
OPM relies on over 160 government employing offices—and 87 contracts
with health insurance carriers—to enroll and verify the eligibility of FEHB
members. There may be one employing office per agency, multiple
employing offices per agency, or multiple agencies could have one
employing office.
Eligible individuals have three opportunities to enroll in FEHB coverage:
• New-hire enrollment: New federal employees who are eligible for
FEHB coverage may enroll themselves and add coverage for eligible
family members in any available plan, option, and type of enrollment
within 60 days after becoming eligible.
• Open season: Eligible individuals can enroll in FEHB coverage,
change plans, and add family members to their plan during the annual
open season, which runs from the Monday of the second full
workweek in November through the Monday of the second full
workweek in December unless modified by OPM for a specific year.
• QLEs: Eligible individuals may enroll in FEHB coverage, change
plans, or add family members to their current plan within a specific
timeframe of experiencing a QLE.
11
QLEs include, but are not limited
to, a change in family status that results in an increase or decrease in
the number of eligible family members, such as a marriage, divorce,
and the birth or adoption of a child. Outside of new-hire and open
season enrollment, new enrollment or changes to FEHB coverage can
be made only in connection with QLEs.
Three types of FEHB enrollments are available:
• A “Self Only” enrollment only provides FEHB benefits for the enrollee.
11
A QLE is a term defined by OPM to describe events deemed acceptable by the Internal
Revenue Service that may allow premium conversion participants to change their
participation election for premium conversion outside of an Open Season.
FEHB Enrollment

Page 6 GAO-23-105222 Federal Employees Health Benefits Program
• A “Self Plus One” enrollment provides benefits for the enrollee and
one eligible family member.
• A “Self and Family” enrollment provides benefits for the enrollee and
all eligible family members.
Family members eligible for coverage under an employee’s “Self Plus
One” or “Self and Family” enrollment include spouses, children under the
age of 26 (including biological children, stepchildren, adopted children,
and foster children), and a child of any age who is incapable of self-
support.
12
Both the federal government and enrollees, through their contributions
toward health insurance premiums, contribute to the FEHB program.
Generally, as set by statute, the government pays 72 percent of the
average premium across all FEHB plans—but no more than 75 percent of
any particular plan’s premium—while enrollees pay the balance.
13
In fiscal
year 2021, the FEHB program had a combined annual premium value
paid by the government and enrollees of approximately $59 billion.
Premiums vary by plan option and depend on whether the enrollment is
for “Self Only,” “Self Plus One,” or “Self and Family” coverage. Premiums
are intended to cover members’ health care costs (including claims),
plans’ administrative expenses, reserve accounts specified by law, plan
profits, and OPM’s administrative costs.
Improper payments are payments that should not have been made or
were made in the incorrect amount—i.e., an overpayment or
underpayment—under a statutory, contractual, administrative, or other
legally applicable requirement.
14
Improper payments can be a result of
mismanagement, errors, or fraud and abuse. Within the FEHB program,
improper payments include payments for premiums or claims for ineligible
12
A stepchild includes the child of an enrollee’s spouse even after the enrollee’s divorce
from the spouse or death of the spouse, so long as the child continues to live with the
enrollee in a regular parent-child relationship. A child incapable of self-support due to a
mental or physical disability is eligible to be covered under a federal employee’s FEHB
plan if the disabling condition began before the age of 26.
13
5 U.S.C. § 8906(b).
14
Also included are any payment to an ineligible recipient, any payment for an ineligible
good or service, any duplicate payment, any payment for a good or service not received
(except for such payments where authorized by law), and any payment that does not
account for credit for applicable discounts. 31 U.S.C. § 3351(4).
FEHB Premiums and
Funding
Improper Payments

Page 7 GAO-23-105222 Federal Employees Health Benefits Program
members, including family members, according to OPM officials. OPM is
currently unable to identify or estimate how many ineligible family
members receive benefits from the FEHB program or the total cost to the
program of those improper payments and did not report an improper
payment estimate for fiscal year 2021. According to OPM’s OIG, the high
costs of improper payments without accurate accounting of improper
payment rates in the FEHB program is a persistent top management
challenge.
15
In July 2022, OPM officials told us they were updating their method for
estimating the agency’s improper payments and exploring how to define
improper payments in the FEHB program for the purposes of reporting
improper payments to the Office of Management and Budget’s (OMB)
www.paymentaccuracy.gov website. OPM officials told us this work was
in response to a 2020 OPM OIG report that determined OPM’s current
improper payment methodology could result in a substantial
underreporting of estimated improper payments in a given fiscal year. For
example, OPM did not include an estimate of improper payments
associated with ineligible members in the estimate of improper payments
it had previously reported to OMB. Instead, OPM’s calculation reported an
improper payment rate that was based in part on judgmentally selected
samples of claims the OIG audited each year at a small percentage of
FEHB carriers, leaving a large amount of claims not considered for
OPM’s improper payment rate.
16
Fraud and fraud risk are distinct concepts. Fraud—obtaining something of
value through willful misrepresentation—is challenging to detect because
of its deceptive nature. Fraud risk—a function of likelihood and impact—
exists when people have an opportunity to engage in fraudulent activity,
have an incentive or are under pressure to commit fraud, or are able to
rationalize committing fraud. When fraud risks can be identified and
mitigated, fraud may be less likely to occur. Although the occurrence of
15
Office of Personnel Management, Office of the Inspector General, Office of Audits, Final
Report: The U.S. Office of Personnel Management’s Top Management Challenges for
Fiscal Year 2022 (Washington, D.C.: October 13, 2021).
16
For more information, see Office of Personnel Management, Office of the Inspector
General, Audit of the U.S. Office of Personnel Management’s Federal Employees Health
Benefits Program and Retirement Services Improper Payments Rate Methodologies
(Washington, D.C.: April 2020).
Fraud Risk Management

Page 8 GAO-23-105222 Federal Employees Health Benefits Program
fraud indicates there is a fraud risk, a fraud risk can exist even if actual
fraud has not yet occurred or been identified.
Managers of federal programs maintain the primary responsibility for
fraud risk management. The objective of fraud risk management is to
ensure program integrity by continuously and strategically mitigating both
the likelihood and effects of fraud. Effectively managing fraud risk helps to
ensure that federal programs’ services fulfill their intended purpose—that
funds are spent effectively and assets are safeguarded.
In July 2015, we issued the Fraud Risk Framework, which provides a
comprehensive set of key components and leading practices that serves
as a guide for agency managers to use when developing efforts to
combat fraud in a strategic, risk-based way.
17
Additionally, the Fraud
Reduction and Data Analytics Act of 2015 required that OMB establish
guidelines for federal agencies to create controls to identify and assess
fraud risks and to design and implement anti-fraud control activities.
18
The
act also required that OMB incorporate the leading practices from the
Fraud Risk Framework in its guidelines. The Payment Integrity
Information Act of 2019, which repealed the Fraud Reduction and Data
Analytics Act of 2015, requires these guidelines to remain in effect,
subject to modification by OMB as necessary and in consultation with
GAO.
19
As figure 1 shows, the Fraud Risk Framework describes leading
practices within four components: commit, assess, design and implement,
and evaluate and adapt.
17
GAO-15-593SP.
18
Pub. L. No. 114-186, 130 Stat. 546 (2016).
19
Pub. L. No. 116-117, § 2(a), 134 Stat. 113, 131 - 132 (2020), codified at 31 U.S.C. §
3357.

Page 9 GAO-23-105222 Federal Employees Health Benefits Program
Figure 1: The Four Components of the Fraud Risk Framework and Selected Leading Practices
If implemented appropriately, these leading practices can help ensure
that federal program managers and their stakeholders are able to meet
their responsibilities for managing fraud risks. Specifically, the second
component—assess—calls for program managers to plan regular fraud
risk assessments and assess risks to determine a fraud risk profile.
Specific leading practices associated with these concepts include
• identifying the range of inherent fraud risks affecting the program,
20
20
Inherent fraud risk is the risk to an entity prior to considering management’s response to
the risk.

Page 10 GAO-23-105222 Federal Employees Health Benefits Program
• assessing the likelihood and impact of inherent fraud risks, and
• documenting these risks in a fraud risk profile.
As discussed in the Fraud Risk Framework, managers who effectively
assess fraud risks attempt to fully consider the fraud risks facing their
program, analyze the potential likelihood and impact of fraud schemes,
and then ultimately document prioritized fraud risks. The fraud risk profile
documents the key findings and conclusions from the fraud risk
assessment. The profile is an essential piece of an overall antifraud
strategy and can inform the specific antifraud control activities that
managers design and implement.
OPM recently implemented control activities designed to prevent ineligible
family members from being covered in the FEHB program. As mentioned,
from the FEHB program’s inception in 1960, OPM has delegated
responsibility to employing offices to make family member eligibility
determinations, but did not require employing offices to review
documentation to verify family member eligibility during new hire, QLE, or
open season enrollments.
21
However, beginning in 2018, OPM put in
place a new regulation and guidance that establish requirements and
21
During our review, each of the five selected employing offices we spoke with told us they
did not verify family member eligibility during new-hire enrollments prior to OPM’s April
2021 guidance, which required them to begin doing so, as described in greater detail
below.
OPM Has
Implemented
Preventative Controls
but Cannot
Reasonably Ensure
Ineligible Family
Members Are Not
Covered in FEHB
Enrollments
OPM Recently
Implemented Preventative
Controls

Page 11 GAO-23-105222 Federal Employees Health Benefits Program
control activities designed to prevent ineligible family members from being
covered in the FEHB program. Specifically:
• Amended regulations. In 2018, OPM published amended
regulations stating that proof of family member eligibility must be
provided to the FEHB health insurance carrier, employing office, or
OPM upon request. These regulations also establish a process for the
removal of individuals who are not found to be eligible.
22
Pursuant to
these regulations, employing offices and FEHB carriers may—but are
not required to— request proof of family member eligibility at any time
for existing participants.
• Guidance to employing offices. In April 2021, OPM issued guidance
to federal employing offices that required them to begin verifying
family member eligibility for new-hire and QLE enrollments by July
2021.
23
However, this guidance does not require employing offices to
verify family member eligibility during the annual open season, as
described in greater detail below.
24
Employing offices remained
responsible for processing all changes in enrollment that affect
premium withholdings, such as changes from “Self Plus One” to “Self
and Family.”
• Guidance to FEHB carriers. Also in April 2021, OPM issued
guidance to the FEHB carriers that requires them to obtain proof of
family member eligibility when adding family members to an existing
“Self and Family” plan.
25
For example, if an employee wants to add a
child to an existing “Self and Family” plan, the FEHB carrier must
obtain proof of the child’s eligibility—such as a birth certificate—before
adding the child to the “Self and Family” plan.
OPM’s 2021 guidance to employing offices and carriers also outlines
what documents may be used as proof of eligibility. For example, a
government-issued marriage certificate may be used as proof of
22
83 Fed. Reg. 3059 (Jan. 23, 2018).
23
Office of Personnel Management, Family Member Eligibility Verification for Federal
Employees Health Benefits Program Coverage, Benefits Administration Letter 21-202
(April 15, 2021).
24
Open season is an annual opportunity for FEHB members to make enrollment changes
to their FEHB coverage.
25
Office of Personnel Management, Family Member Eligibility Verification for Federal
Employees Health Benefits Program Coverage, Federal Employees Health Benefits
Program Carrier Letter 2021-06 (April 15, 2021).

Page 12 GAO-23-105222 Federal Employees Health Benefits Program
marriage, and a government-issued birth certificate may be used to add
coverage to a biological child under the age of 26. Proof of eligibility is
also required for other FEHB family members such as common-law
spouses, adopted children, foster children, and children over the age of
26 who are incapable of self-support because of a mental or physical
disability.
OPM’s 2021 guidance to employing offices also discusses the process for
an employing office to request proof of family member eligibility and the
actions the employing office must take based on an employee’s
response. Specifically, if an employing office determines that eligibility
documents are insufficient, it must provide the employee with a written
notice of its initial decision, with an explanation of the decision, and
provide notice of the right to a reconsideration of the employing office’s
initial decision.
According to OPM’s 2021 guidance and OPM officials, employing offices
may—but are not required to—verify family member eligibility during the
FEHB open season. Similarly, FEHB health insurance carriers are not
required to verify family member eligibility during open season. Officials
from OPM told us that verifying eligibility during the approximately 4 to 5
week open season was currently not feasible because of the high number
of enrollment transactions that occur during the period.
We recognize the challenge of verifying eligibility during open season.
However, we also note that beyond not verifying family members’
eligibility during open season, OPM has not required employing offices or
carriers to verify eligibility since the program’s inception in 1960,
emphasizing the need for a monitoring mechanism to identify and remove
ineligible members from the FEHB program, as we discuss later in this
report.
Since OPM’s April 2021 guidance was put into effect, OPM has not
designed or implemented monitoring mechanisms to ensure employing
offices and insurance carriers are complying with the guidance’s
requirements to verify the eligibility of family members for new-hire and
QLE enrollments. OPM officials told us they do not have the funding
necessary to perform monitoring of employing offices or carriers and have
no plans to conduct this monitoring in the future.
Standards for Internal Control in the Federal Government states that
management should establish and operate monitoring activities to monitor
OPM Cannot Reasonably
Ensure Employing Offices
and Carriers are
Preventing Ineligible
Family Members from
Being Covered in FEHB

Page 13 GAO-23-105222 Federal Employees Health Benefits Program
the internal control system and evaluate the results.
26
Without monitoring
employing offices and insurance carriers’ implementation of its new
guidance, OPM cannot have reasonable assurance that employing offices
and carriers are implementing control activities to prevent FEHB coverage
of ineligible family members.
We found that not all employing offices are implementing such control
activities. Specifically, our interviews with five employing offices found
that one employing office within a cabinet-level department was not
reviewing family member eligibility for all new-hire or QLE enrollments as
OPM’s guidance requires. Officials from this employing office cited the
large number of transactions and technology issues as challenges to
complying with OPM’s guidance. Officials from this employing office told
us that OPM was aware of their noncompliance and that they were
working toward complying with the OPM requirements in the future.
Officials from the other four employing offices we interviewed stated that
they were following the eligibility verification requirements for new-hire
and QLE coverage outlined in OPM guidance. Officials from each of the
carriers we met with told us that they verified family member eligibility
when an individual was added to existing “Self and Family” enrollments,
as required by the 2021 carrier letter.
However, as with employing offices, OPM does not conduct monitoring to
verify that the health insurance carriers are properly and consistently
verifying individuals’ eligibility. While the example of employing office
noncompliance we identified is not generalizable to all employing offices,
it nonetheless highlights how OPM monitoring could help ensure all
offices and carriers implement required control activities for preventing
ineligible family members from being covered in the FEHB program.
Without monitoring the population of FEHB employing offices and carriers
responsible for verifying family members’ FEHB eligibility during a new
hire or QLE, OPM cannot be certain of how many employing offices and
carriers are not meeting OPM’s eligibility verification requirements
because of information technology or staffing limitations, high transaction
volume, or other reasons. Unless OPM establishes a mechanism to
monitor employing offices and carriers to ensure they are implementing
requirements to verify family members’ eligibility, the FEHB program may
26
GAO-14-704G

Page 14 GAO-23-105222 Federal Employees Health Benefits Program
continue to be vulnerable to improper payments resulting from ineligible
family member participation in FEHB.
OPM’s amended regulations and guidance establish a process for
removing ineligible family members from the FEHB program, and OPM
relies on limited efforts by employing offices and FEHB health insurance
carriers to identify and remove ineligible family members. However, OPM
officials told us the agency itself does not monitor—and does not plan to
begin regularly monitoring—family members who already have FEHB
coverage to identify and remove those who are ineligible from the
program. As described previously in this report, in January 2018, OPM
published amended regulations that require enrollees to submit proof of
family member eligibility to employing offices or carriers upon request.
These regulations also provide a process for removing ineligible family
members from the FEHB program. OPM has also issued guidance to
employing offices that details the process for removing ineligible family
members from the FEHB program.
27
Pursuant to these regulations and
the OPM guidance, employing offices and FEHB carriers may—but are
not required to—request proof of family member eligibility at any time for
existing participants.
Officials from the five selected employing offices we spoke with told us
that they perform limited activities to identify and remove ineligible family
members from the FEHB program. Specifically, officials from each of
these five selected employing offices told us they do not regularly perform
any ongoing monitoring or eligibility verification for currently participating
family members. Instead, these officials noted that they might discover
ineligible family members when employees make coverage changes that
reveal ineligible family members who are currently covered or when
notified by an employee. For example, if an employee tries to enroll a new
spouse, the employing office might discover that the employee never
removed their ex-spouse from their plan; in this way, the employing office
would discover the ineligible family member at the time of the coverage
change. During this review, officials from OPM and some of the
employing offices we spoke with acknowledged that relying on tips or
enrollment changes to discover ineligible family members creates a risk
that family members will continue to be covered even after they are
27
Office of Personnel Management, Removal of Ineligible Family Members from
Enrollments, Benefits Administration Letter 20-203 (Nov. 5 2020).
OPM Relies on
Limited Efforts to
Identify and Remove
Ineligible Family
Members with FEHB
Coverage

Page 15 GAO-23-105222 Federal Employees Health Benefits Program
ineligible, resulting in improper payment vulnerabilities in the FEHB
program.
28
Similarly, officials from each of the five FEHB insurance carriers we spoke
with told us they perform limited activities to identify and remove ineligible
family members from the FEHB program. For example, officials from each
of the five carriers told us they perform regular monitoring to identify
family members who become ineligible when they turn 26 years old. At
the same time, officials from each of the five carriers told us they do not
monitor members for ineligibility due to divorce, stating they rely on
enrollees to inform them about their divorces. These responses from the
employing offices and carriers are not generalizable to their respective
universes. However, they highlight control weaknesses that could
heighten the risk that ineligible members remain in the FEHB program
undetected. As described below, the potential costs associated with this
risk are considerable.
OPM does not have a precise estimate of how many ineligible members
exist and at what cost to the program. OPM officials told us they
recognize ineligible individuals may be covered in FEHB, and information
from OPM indicates the cost savings from performing a DEVA for all
existing family members to be in the estimated range of $360 million to
about $1 billion.
29
According to OPM officials, these estimated cost
savings would generally be an avoidance of future claims costs as
opposed to current return of actual dollars. As mentioned, FEHB
28
Officials from OPM and some employment offices we spoke with noted that employees
may retain ex-spouses on their plans out of confusion, rather than as an act of fraud. For
example, employees may receive a court order to continue health insurance coverage for
their ex-spouse as part of their divorce. Employees might incorrectly interpret the court
order to indicate that they are allowed to keep their ex-spouse covered in the FEHB
program as a dependent. However, OPM officials stated this is not permitted, even with a
court order.
29
As previously mentioned, a DEVA is an audit designed to verify the eligibility of currently
covered dependents, such as spouses and children. Typically the entity conducting the
DEVA requests that enrollees provide marriage certificates, birth certificates, or other
documents to demonstrate eligibility. GAO did not independently verify the accuracy of
OPM’s estimate. OPM notes this estimate has limitations, including that it did not take into
account the cost of the audit and that the cost data averages derived from this estimate
are from one health care provider and may not represent cost data averages for the entire
FEHB program. These limitations may result in an underestimate or overestimate of cost
savings. OPM’s OIG estimates the cost of ineligibles at between $250 million and $3
billion annually. OPM has stated it believes the OPM OIG’s estimate is too high, in part
because of the cost of certain family members. GAO did not independently verify the
accuracy of the OIG estimate.

Page 16 GAO-23-105222 Federal Employees Health Benefits Program
premiums paid by the government and enrollees are intended to cover
members’ health care costs (including claims), plans’ administrative
expenses, and other costs. Thus, these estimates would represent
savings to the federal government and enrollees who pay FEHB
premiums.
OPM officials told us that in 2014 they explored performing a DEVA for
the FEHB program as a monitoring control activity. However, OPM
subsequently decided not to pursue a DEVA, citing the need to establish
regulations providing it the authority to remove any ineligible family
members identified by such an audit, among other issues. After
publishing amended regulations in 2018 (as described above), OPM
explored auditing a sample of members for continued eligibility. However,
OPM ultimately did not pursue a request for funding to complete this
work, which was never initiated due to competing priorities, according to
OPM officials.
During our review, OPM officials told us they believed performing a one-
time audit of all FEHB members was not feasible given the size and
scope of the FEHB program population. We recognize the challenge of
performing a one-time audit of all FEHB members given the size and
scope of the FEHB program population. However, we also note that
DEVAs may be structured with different scopes and methodologies, such
as auditing samples of the population over several years, rather than
attempting to audit the entire population all at once. For example, during
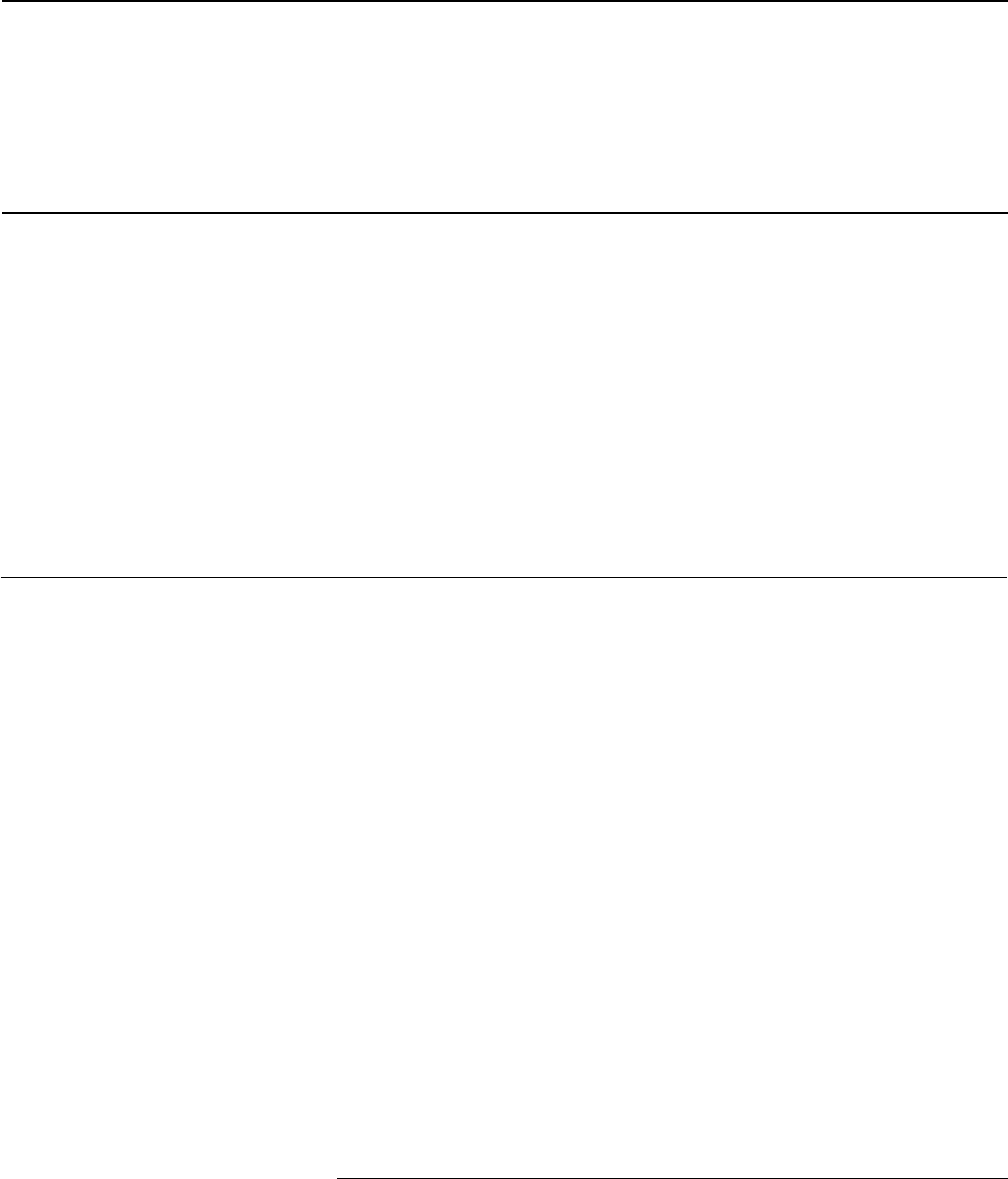
our review we identified 25 states that have conducted or announced
plans to conduct a DEVA for their respective state healthcare insurance
programs (see fig. 2 below).
30
30
Additional states may have monitored or announced plans to monitor dependent
eligibility in their state health program that are not included in this review. Additional
information on our methodology for reviewing these DEVAs appears in appendix I.

Page 17 GAO-23-105222 Federal Employees Health Benefits Program
Figure 2: Examples of States That Have Performed or Announced a Dependent Eligibility Verification Audit (DEVA) for a State
Health Insurance Program (1992–2022)
Note: Additional states may have monitored or announced plans to monitor dependent eligibility in
their state health program that are not included in this review. Additional information on our
methodology for reviewing these DEVAs appears in appendix I.
These state DEVAs used varying scopes and methodologies to verify
family member eligibility. Some states performed one-time audits of the
entire member population, while other states audited samples of the
population over several years. For example:
• In 2018, Florida’s State Group Health Insurance Program contracted
with a third party audit vendor that conducted a DEVA requesting
Page 18 GAO-23-105222 Federal Employees Health Benefits Program
verification for all participating dependents. The audit identified 3
percent of the dependent population as ineligible for coverage. Based
on a detailed claims analysis, the annual cost avoidance to the State
Group Health Insurance Program was estimated at $20.4 million.
• In 2015, the California Public Employees’ Retirement System
conducted an audit. The system requires all employees to reverify
dependents every 3 years based on the dependent’s birth month.
After its audit, the California retirement system removed 2.6 percent of
dependents because of ineligibility and estimated it saved nearly $122
million.
• In 2020, the Kansas State Employee Health Plan contracted with a
third party audit vendor that conducted a DEVA using two sample
groups. According to the final report, the DEVA included (1) a
statistically valid sample of 200 employees with dependents, and (2) a
targeted sample of 200 employees with dependents who had medical
or prescription drug claims during the audit period. The Kansas State
Employee Health Plan found that of the 400 employees sampled, 348
(87 percent), provided documentation of their dependents’ eligibility.
31
We asked OPM officials whether they were pursuing funding for a DEVA
with a different scope, such as auditing samples of the population over
several years—similar to some state DEVAs we reviewed—rather than
attempting to audit the entire population all at once. In response, the
officials told us they did not plan to pursue funding for a DEVA—whether
on a one-time basis or a smaller, sample basis—due to alternative
funding priorities. Specifically, OPM officials told us they were focusing
instead on developing and pursuing funding for the Government-wide
Enrollment and Member Support (GEMS) program to centralize the
enrollment process, rather than establishing mechanisms to monitor
current member eligibility. OPM officials told us they believe focusing on
acquiring GEMS is a better use of funds, which would allow for a
centralized enrollment process and OPM oversight of eligibility
verification.
However, we reviewed documentation related to OPM’s plans for GEMS
and found no evidence that this project would establish a monitoring
31
Employees who did not verify their dependents’ eligibility either did not respond or failed
to submit sufficient paperwork. The names of the employees with dependents not verified
were provided to State Employee Health Plan Membership Services for review. The
findings report we reviewed did not include information on cost savings stemming from
this DEVA.
Page 19 GAO-23-105222 Federal Employees Health Benefits Program
mechanism as called for by the Standards for Internal Control in the
Federal Government. We also found no indication it would identify
ineligible family members for removal from the FEHB program. Further,
as of March 2022 OPM had not established a date for completing the
development of GEMS and was in the process of determining how to fund
the project. This raises questions as to when OPM will begin and finish its
work on GEMS.
As previously mentioned, Standards for Internal Control in the Federal
Government states that management should establish and operate
activities to monitor the internal control system and evaluate the results.
32
In doing so, management should monitor the internal control system
through ongoing monitoring and separate evaluations, such as audits.
These standards note that audits and other evaluations may be
performed by internal auditors, external auditors, or other external
reviewers. Many of the states we identified as having conducted or
announced plans to conduct a DEVA for their state health insurance
program performed this work through external auditors or other external
reviewers, indicating this approach might also be an option for OPM.
Standards for Internal Control in the Federal Government also states that
management should remediate identified internal control deficiencies on a
timely basis. As mentioned, OPM recognizes that ineligible family
members may be covered in the FEHB program. Further, the risk posed
by ineligible family members—and the corresponding need to put in place
a monitoring mechanism to identify and remove ineligible family
members—is heightened by the fact that OPM does not require
employing offices and carriers to verify family member’s eligibility during
open season. Previously, OPM did not require employing offices or
carriers to verify family member eligibility since the program’s inception.
For example, as discussed above, each of the five selected employing
offices we spoke with told us they did not verify eligibility for family
members of new hires prior to the OPM requirement to do so in 2021.
The longer OPM delays its efforts to establish a monitoring mechanism to
identify and remove ineligible members from FEHB, the more ineligible
members and related improper payments in the program may continue to
accrue, costing the program millions, or up to approximately one billion
dollars per year according to OPM’s own estimate. Further, these
ineligible members could file insurance claims, leading to potentially
32
GAO-14-704G

Page 20 GAO-23-105222 Federal Employees Health Benefits Program
higher premium costs for the federal government and FEHB enrollees in
future years.
As part of managing fraud risks, the Fraud Risk Framework calls on
federal managers to plan regular fraud risk assessments that are tailored
to the program and assess risks to determine the program’s fraud risk
profile.
33
Specific leading practices associated with these concepts
include
• identifying the range of inherent fraud risks affecting the program;
• assessing the likelihood and impact of inherent fraud risks; and
• documenting these risks in the fraud risk profile.
Consistent with these leading practices, OPM performs an annual fraud
risk assessment and has documented a fraud risk profile for the FEHB
program that includes inherent fraud risks affecting the program, as well
as the likelihood and impact of those inherent fraud risks. For example, in
fiscal year 2020, OPM conducted a fraud risk assessment and
subsequently documented a fraud risk profile for the FEHB program.
OPM’s fiscal year 2020 fraud risk profile identified three inherent fraud
risks facing the FEHB program, all of which relate to fraud by providers.
The specific risks identified are: (1) providers billing for tests or services
not covered or not performed; (2) providers overbilling for services
performed; and (3) providers falsifying a patient’s diagnosis. Based on
this fraud risk assessment and profile, OPM determined that the FEHB
program’s overall fraud risk was low.
However, OPM’s fiscal year 2020 fraud risk assessment and profile did
not include ineligible members as an inherent fraud risk. OPM’s OIG has
noted that identifying ineligible family members is often difficult and that
fraud, waste, and abuse can occur over years before being discovered.
Moreover, OPM’s OIG has documented cases of fraud associated with
ineligible members in the FEHB program, further underscoring the need
for OPM to assess the risk of fraud in the program such members pose
and ensure it has antifraud controls to mitigate this risk. Some examples
of fraud involving ineligible FEHB members from OIG reports are noted
below:
33
GAO-15-593SP
OPM’s Fraud Risk
Assessment Does
Not Include Fraud
Risks Related to
Ineligible Members in
FEHB
Page 21 GAO-23-105222 Federal Employees Health Benefits Program
• An FEHB program enrollee submitted altered official court documents
when removing an ex-spouse and adding a new spouse to the
enrollee’s FEHB insurance plan. The altered document indicated that
the enrollee divorced their ex-spouse in January 2017 when in fact
they had divorced in April 1993. The FEHB program paid more than
$150,000 in claims on behalf of the ex-spouse over the 14 years of
ineligible coverage. In June 2019, the enrollee pleaded guilty to
making false statements.
• A federal employee fraudulently covered two individuals purported to
be the employee’s wife and stepchild in the FEHB program. The
individuals were ineligible and remained on FEHB health insurance
from January 2005 to January 2017. The FEHB program paid claims
totaling more than $100,000 on behalf of the ineligible individuals. The
employee pleaded guilty and was sentenced to 24 months of
supervised release.
• A federal employee added multiple ineligible individuals as family
members to an FEHB program health insurance plan. The FEHB
program paid more than $12,000 for services provided to these
ineligible individuals. In February 2018, the employee and a
codefendant were indicted for making false statements relating to
health care matters, as well as aiding and abetting the same. In July
2018, the employee pleaded guilty, and in April 2019 was sentenced
to 3 years of probation and ordered to pay more than $12,000 in
restitution.
The OPM OIG’s work demonstrating fraud in the FEHB program, and
OPM’s acknowledgement that not verifying eligibility for current members
carries fraud risk, indicates that OPM has identified ineligible members as
an inherent fraud risk. However, when asked, OPM officials could not
explain to us why OPM’s fraud risk profile did not include an assessment
of the likelihood and impact of ineligible FEHB members. Until OPM
assesses the likelihood and impact of the fraud risk of ineligible FEHB
members and documents its assessment in a fraud risk profile, it cannot
support its determination that the FEHB program is at a low risk of fraud,
and the FEHB program may remain vulnerable to the fraud risk
associated with ineligible members.
The FEHB program is the largest employer-sponsored group health
insurance program in the country, providing coverage for over 8.2 million
members at a cost of approximately $59 billion in fiscal year 2021. OPM
has the overall responsibility for administering the FEHB program and for
ensuring only eligible family members receive coverage. However, the
Conclusions

Page 22 GAO-23-105222 Federal Employees Health Benefits Program
size of the program and diffuse administrative structure make that task
challenging, and pose risks for potential fraud, as OPM relies on over 160
employing offices and multiple insurance carriers to ensure eligibility
requirements are enforced for millions of federal employees, retirees, and
their family members.
In 2021, OPM began requiring that employing offices and insurance
carriers verify family members’ eligibility for new-hire and QLE
transactions—an important step in mitigating improper payments,
including those resulting from fraud, in the FEHB program. However,
OPM cannot reasonably ensure that employing offices and insurance
carriers are verifying family members’ eligibility as required. Unless OPM
establishes a mechanism to monitor employing offices and carriers to
ensure that such verification occurs, the FEHB program may continue to
be vulnerable to improper payments resulting from ineligible family
members’ participation in FEHB.
Further, OPM recognizes ineligible individuals are likely participating in
FEHB. However, it does not have a monitoring mechanism in place to
identify and remove ineligible members from the program. Without such a
mechanism in place, the more ineligible participants and related improper
payments in the program may continue to accrue, costing the program
millions.
OPM performs an annual fraud risk assessment of the FEHB program.
However, it has not assessed fraud risks associated with ineligible
members in a manner consistent with leading practices. OPM recognizes
that the size and scope of the program, and the lack of monitoring for
dependent eligibility for current members, carries a risk for improper
payments and fraud. However, OPM has not assessed the likelihood and
impact associated with coverage of ineligible family members in the
FEHB fraud risk assessment and profile. Until OPM assesses the
likelihood and impact of ineligible FEHB members and documents its
assessment in a fraud risk profile, it cannot support its determination that
the FEHB program is at low risk of fraud. As a result, the FEHB program
may remain vulnerable to the fraud risk associated with ineligible
members.
We are making the following four recommendations to OPM:
The Director of OPM should implement a monitoring mechanism to
ensure employing offices and carriers are verifying family member
eligibility as required by OPM’s 2021 guidance. (Recommendation 1)
Recommendations for
Executive Action
Page 23 GAO-23-105222 Federal Employees Health Benefits Program
The Director of OPM should implement a monitoring mechanism to
identify and remove ineligible family members from the FEHB program.
(Recommendation 2)
The Director of OPM should assess the likelihood and impact of the fraud
risk related to ineligible FEHB members. (Recommendation 3)
The Director of OPM should document its assessment of the fraud risk
related to ineligible members in its fraud risk profile for the FEHB
program. (Recommendation 4)
We provided a draft of this report to OPM for review and comment. In its
written comments, reproduced in appendix II, OPM concurred with three
of the four recommendations and partially concurred with one
recommendation. OPM also provided technical comments, which we
incorporated as appropriate.
OPM partially concurred with our first recommendation to implement a
monitoring mechanism to ensure employing offices and FEHB carriers
are verifying family member eligibility as required by OPM’s 2021
guidance. In its comments, OPM identified steps it has taken to ensure
that its 2021 guidance is consistently followed. This included surveying
agencies and carriers related to verification practices and providing
training. At the same time, OPM agreed that further monitoring through
comprehensive audit may be appropriate. The steps described in OPM’s
comments are positive actions to help ensure compliance. However, as
OPM acknowledged, it may need to take additional action to implement a
monitoring mechanism to ensure employing offices and FEHB carriers
are verifying family member eligibility going forward. As such, we believe
this recommendation is still warranted.
If you or your staff have any questions about this report, please contact
Offices of Congressional Relations and Public Affairs may be found on
the last page of this report. GAO staff who made key contributions to this
report are listed in appendix III.
Agency Comments
and Evaluation

Page 24 GAO-23-105222 Federal Employees Health Benefits Program
As agreed with your offices, unless you publicly announce the contents of
this report earlier, we plan no further distribution until 30 days from the
report date. At that time, we will send copies to the appropriate
congressional committee and the Director of OPM. In addition, the report
will be available at no charge on the GAO website at
https://www.gao.gov.
Seto J. Bagdoyan
Director, Audit Services
Forensic Audits and Investigative Service

Appendix I: Objectives, Scope, and
Methodology
Page 25 GAO-23-105222 Federal Employees Health Benefits Program
This report discusses the extent to which (1) the Office of Personnel
Management (OPM) has implemented control activities to prevent
ineligible family members from being covered in Federal Employees
Health Benefits (FEHB) program enrollments; (2) OPM has implemented
control activities to identify and remove ineligible family members with
FEHB coverage; and (3) OPM’s fraud risk assessment for the FEHB
program includes fraud risks related to ineligible FEHB members.
1
As part of this work, we determined that internal controls were significant
to our first and second objectives. Specifically, the monitoring component
of internal control—along with the related principles that (1) management
should establish and operate monitoring activities to monitor the internal
control system and evaluate the results, and (2) management should
remediate identified internal control deficiencies—as outlined in
Standards for Internal Control in the Federal Government, were
significant to our first and second objectives.
2
To assess relevant control
activities in both objectives, we reviewed federal regulations and OPM
guidance. We also interviewed officials and reviewed relevant
documentation from OPM, OPM’s Office of the Inspector General (OIG),
federal employing offices, FEHB health insurance carriers, and others, as
described in greater detail below.
For our first two objectives, we conducted interviews with officials from
OPM, five employing offices, and five FEHB health insurance carriers. To
obtain views from offices of differing employee size, for our interviews
with five employing offices we randomly selected one employing office
each within two cabinet level departments, one employing office of a large
independent federal agency, one employing office of a medium
independent federal agency, and one employing office of a small
independent federal agency, as defined by OPM’s list of federal
1
In this report, we use the term “members” to refer to federal employees, retired federal
employees, other eligible individuals, and their eligible family members with health
coverage in the FEHB program.
2
GAO, Standards for Internal Control in the Federal Government, GAO-14-704G
(Washington, D.C.: September 2014).
Appendix I: Objectives, Scope, and
Methodology

Appendix I: Objectives, Scope, and
Methodology
Page 26 GAO-23-105222 Federal Employees Health Benefits Program
agencies.
3
For our interviews with FEHB health insurance carriers, we
selected a non-probability sample of five FEHB carriers that had at least 1
percent of total FEHB employee and retiree enrollment as of October
2021. The five carriers we interviewed represented a combined total of
approximately 87 percent of FEHB employee and annuitant enrollment at
the time of our selection.
4
While the statements from the selected
employing offices and carriers we spoke with are not generalizable to
their entire populations, they provided specific information about their
FEHB responsibilities and operations. We also reviewed relevant
documentation, such as OPM regulations, FEHB guidance and
instructions for employing offices and health insurance carriers, and
OPM’s FEHB handbook.
For our second objective, we reviewed additional documentation,
including final audit reports on dependent eligibility verification audits
(DEVAs) performed by states as a control activity to identify and remove
ineligible family members covered under state health benefit programs.
5
To identify examples of states that have performed or announced DEVAs,
we sent out an inquiry to the National Association of State Auditors
requesting information on this topic. We also performed web searches
and reviewed state auditor websites for all 50 states. However, additional
states may have monitored or announced plans to monitor dependent
eligibility in their state health programs that are not included in this review
because, for example, these states did not provide us information on
those efforts or it was not published on the internet or State Auditor
websites.
As part of this work, we also interviewed three of the six vendors we
identified that contracted with these state health benefit programs to
conduct the DEVAs we reviewed. We attempted to meet with all six
3
OPM maintains a publicly available list of federal agencies and employment numbers on
its website that we used to select employing offices. OPM defines large independent
agencies as those having more than 1,000 employees, medium independent agencies as
those having between 100 and 999 employees, and small independent agencies as those
having less than 100 employees.
4
This percentage does not include family member enrollment.
5
A dependent eligibility verification audit (DEVA) is an audit designed to verify the
eligibility of enrollees’ dependents, such as spouses and children. Typically, the entity
conducting the DEVA requests that enrollees provide marriage certificates, birth
certificates, or other documents to demonstrate eligibility.

Appendix I: Objectives, Scope, and
Methodology
Page 27 GAO-23-105222 Federal Employees Health Benefits Program
vendors we identified as having conducted DEVAs, but three either
declined or did not respond to our request for a meeting. For our first and
second objectives, we also assessed the extent to which OPM’s
responses and documents aligned with principles in Standards for
Internal Control in the Federal Government –specifically those principles
related to designing and developing monitoring mechanisms and
remediating internal control deficiencies.
6
For our third objective, we analyzed OPM’s fraud risk assessment and
interviewed agency officials. We assessed the extent to which OPM’s
fraud risk assessment for the FEHB program aligned with relevant leading
practices in GAO’s A Framework for Managing Fraud Risks in Federal
Programs - specifically those leading practices related to identifying and
assessing risks to determine the program’s fraud risk profile.
7
We conducted this performance audit from May 2021 to December 2022
in accordance with generally accepted government auditing standards.
Those standards require that we plan and perform the audit to obtain
sufficient, appropriate evidence to provide a reasonable basis for our
findings and conclusions based on our audit objectives. We believe that
the evidence obtained provides a reasonable basis for our findings and
conclusions based on our audit objectives.
6
GAO, Standards for Internal Control in the Federal Government, GAO-14-704G
(Washington, D.C.: September 2014).
7
We selected leading practices from the Fraud Risk Framework’s second component that
are most relevant to this objective based on our review of OPM documents and
discussions with OPM staff. GAO, A Framework for Managing Fraud Risks in Federal
Programs, GAO-15-593SP
(Washington, D.C.: July 2015).

Appendix II: Comments from the Office of
Personnel Management
Page 28 GAO-23-105222 Federal Employees Health Benefits Program
Appendix II: Comments from the Office of
Personnel Management
Appendix II: Comments from the Office of
Personnel Management
Page 29 GAO-23-105222 Federal Employees Health Benefits Program

Appendix II: Comments from the Office of
Personnel Management
Page 30 GAO-23-105222 Federal Employees Health Benefits Program
Appendix III: GAO Contact and Staff
Acknowledgments
Page 31 GAO-23-105222 Federal Employees Health Benefits Program
In addition to the contact named above, Jonathon Oldmixon (Assistant
Director), Scott Clayton (Analyst in Charge), Daniel Silva, and Kaitlyn
Brown made key contributions to this report. Other contributors include
James Murphy and Andrew Stavisky.
Appendix III: GAO Contact and Staff
Acknowledgments
GAO Contact
Staff
Acknowledgments
(105222)

The Government Accountability Office, the audit, evaluation, and investigative
arm of Congress, exists to support Congress in meeting its constitutional
responsibilities and to help improve the performance and accountability of the
federal government for the American people. GAO examines the use of public
funds; evaluates federal programs and policies; and provides analyses,
recommendations, and other assistance to help Congress make informed
oversight, policy, and funding decisions. GAO’s commitment to good government
is reflected in its core values of accountability, integrity, and reliability.
The fastest and easiest way to obtain copies of GAO documents at no cost is
through our website. Each weekday afternoon, GAO posts on its website newly
released reports, testimony, and correspondence. You can also subscribe to
GAO’s email updates to receive notification of newly posted products.
The price of each GAO publication reflects GAO’s actual cost of production and
distribution and depends on the number of pages in the publication and whether
the publication is printed in color or black and white. Pricing and ordering
information is posted on GAO’s website, https://www.gao.gov/ordering.htm.
Place orders by calling (202) 512-6000, toll free (866) 801-7077, or
TDD (202) 512-2537.
Orders may be paid for using American Express, Discover Card, MasterCard,
Visa, check, or money order. Call for additional information.
Connect with GAO on Facebook, Flickr, Twitter, and YouTube.
Subscribe to our RSS Feeds or Email Updates. Listen to our Podcasts.
Visit GAO on the web at https://www.gao.gov.
Contact FraudNet:
Website:
https://www.gao.gov/about/what-gao-does/fraudnet
Automated answering system: (800) 424-5454 or (202) 512-7700
A. Nicole Clowers, Managing Director, ClowersA@gao.gov, (202) 512-4400, U.S.
Government Accountability Office, 441 G Street NW, Room 7125, Washington,
DC 20548
Chuck Young, Managing Director, young[email protected], (202) 512-4800
U.S. Government Accountability Office, 441 G Street NW, Room 7149
Washington, DC 20548
Stephen J. Sanford, Managing Director, [email protected], (202) 512-4707
U.S. Government Accountability Office, 441 G Street NW, Room 7814,
Washington, DC 20548
GAO’s Mission
Obtaining Copies of
GAO Reports and
Testimony
Order by Phone
Connect with GAO
To Report Fraud,
Waste, and Abuse in
Federal Programs
Congressional
Relations
Public Affairs
Strategic Planning and
External Liaison
Please Print on Recycled Paper.
