
Benefits
Guide
Building Resilience. WellBeing. Mindfulness.
2023

2
hisdbenefits.org
EVERYTHING YOU NEED
TO KNOW ABOUT YOUR
2023 BENEFITS
DISCLAIMER: is guide provides an overview of your benet options. e
complete provisions of the plans, including legislated benets, exclusions, and
limitations, are set forth in the plan documents or insurance contracts. e in-
surance contracts are available for your review in the Benets Department. If the
information in this guide is not consistent with the plan documents or insurance
contracts or state and federal regulations, the plan documents, insurance con-
tracts, and state and federal regulations will prevail. is guide is not intended
as a contract of employment or a guarantee of current or future employment or
benets. is enrollment guide constitutes a Summary of Material Modications
(SMM) to the HISD Summary Plan Descriptions (SPD). It is meant to
supplement and/or replace certain information in the SPDS, so retain it for future
reference along with your SPDS. Please share these materials with your covered
family members.
ADA DISCLAIMER: If you cannot read this guide due to a disability,
please email benetsoce@houstonisd.org and let us know how we can
accommodate you. All the information in this guide is also available on our
website: www.hisdbenets.org.
RESPONSABILIDADES: esta guía proporciona una descripción general
de sus opciones de benecios. Las disposiciones completas de los planes, sus
benecios, exclusiones y limitaciones legislados, se establecen en los docu-
mentos del plan o en los contratos de seguro. Los contratos de seguro están
disponibles para su revisión en el Departamento de Benecios. Si la infor-
mación en esta guía no es consistente con los documentos del plan o contratos
de seguro o regulaciones estatales y federales, prevalecerán los documentos del
plan, los contratos de seguro y las regulaciones estatales y federales. Esta guía
no pretende ser un contrato de empleo o una garantía de empleo o Benecios
actual o futuro. Esta guía de inscripción constituye un Resumen de Modica-
ciones Materiales (SMM) a la Descripción resumida del plan (SPD) de HISD.
El propósito de esta guía es complementar y / o reemplazar cierta información
en el SPD, así que guárdelo para referencia futura junto con su SPD. Sientase
con la libertad de compartir estos materiales con los miembros de su familia
que están cubiertos bajo un plan.

3
877-780-HISD (4473).
TABLE OF CONTENTS
What’s new and notable in 2023
Dependent verication services
Preventive health care
Choose your plan
Medical plan options
Prescription benets
Compare coverage options
Voluntary options
FSA
Dental
EyeMed
Life and AD&D
Legal
Aac
Enroll For Coverage
Wellness Resources
Aetna Programs
Employee Assistance Program (EAP)
Retirement
Coverage Costs
Provider Contacts
04
09
12
15
20
28
32
36
36
38
47
49
52
59
68
70
74
84
86
89
94

4
hisdbenefits.org
Welcome to annual enrollment!
It’s time to take a look at your benets and the changes and elections you may
want to make for 2023. Whether you are new to HISD or returning to the district,
we have resources, information, and useful tools to guide you through your bene-
ts information. Even if you are not enrolling in some of the benet options, as an
employee of the district you have access to benets such as the Employee
Assistance Program and resources that may be useful.
New and better access to care is our goal for 2023. ere are now additional ways to access your
healthcare needs and make it even easier to get you and your family members the health care you need
to stay healthy or to get healthier. Our goal for 2023 is to help our employees connect to care whether
they need help locating a physician or help understanding the treatment plan they have been given.
We have resources for you to use. Please use this Benets Guide as the source of information about the
benets oered at HISD. e Benets Service Center is available and ready to assist with questions you
may have, as well as your enrollment opportunities.
LET’S START BY LOOKING AT WHAT’S
NEW AND NOTABLE FOR 2023.
What’s new and notable
in Benefits for 2023

5
877-780-HISD (4473).
New and improved Benets Service Center and enrollment site through Empyrean Benets
Solutions. We will maintain the same Benets Service Center telephone number of
877-780-4473, and the hours of operation will remain the same: Monday – Friday, 7:00 a.m.
to 7:00 p.m. Central Time, except holidays. You may use the Benets Service Center for questions
about your benets, dependent verication audits, enrollment, and benet changes such as life events
and beneciary changes. e Benets Service Center will send electronic communications to your
HISD email and paper mail to your address on record with HISD, so please check your address in
OneSource and make any necessary updates. Also, check your beneciaries and make any needed
changes through the Benets Service Center. A mobile app will be available so you can conveniently
enroll or change benets directly from your phone.
Access your medical plans when needed to search for Providers or review your benets summary.
e HISD medical plans will continue through Aetna for 2023. Most employees have the employee-
only medical option, and those rates will remain the same in 2023. Some of the increased medical costs
are impacting dependent tier levels, although HISD continues to work hard to maintain healthcare
contributions for all participants. In 2023, employee and child(ren) options will have a 4% increase,
employee and family rates a 7% increase, and employee and spouse an 8% increase. e 2023 employee
contributions per paycheck are:
*Employee-only rates will remain the same. e above deduction amounts are per pay period. HISD has
increased employer contributions to the health plan by 9% starting in July 2022.
Tier Kelsey Basic
ACO
Memorial
Hermann
Basic ACO
TX Medical
Neighbor-
hood Basic
Kelsey Plus
ACO
Memorial
Hermann
Plus ACO
TX Medical
Neighborhood
Plus
Ee only $19.25 $21.18 $33.59 $38.79 $42.67 $67.63
Ee + Spouse $108.21 $119.03 $188.65 $146.07 $160.68 $243.35
Ee +
Child(ren)
$100.22 $110.25 $174.77 $135.30 $148.83 $226.17
Ee + Family $185.39 $203.94 $323.27 $250.27 $275.31 $391.01
new and notable in Benefits for 2023

6
hisdbenefits.org
Kelsey Select Medical Plan – HISD has increased the annual salary threshold for the Kelsey Select
Plan eligibility from $29,120 to $31,000 to reect the salary increase for the 2022-2023 school year.
Benets packets will be mailed to the address of record for all employees who qualify for the Kelsey
Select Plan.
Medical Plan CVS Health Hub Access – HISD employees and dependents covered in all HISD
medical plans can now access the CVS Health Hubs located in most CVS pharmacies in their
neighborhood. For Memorial Hermann and Texas Medical Neighborhood plan participants, the
full cost of the visit may be required if deductibles have not been met. Please take advantage of this
additional benet, especially if you need acute care, chronic condition management, or behavioral
health services. Please note that some locations do not oer preventive care or other services. Visits
to the Health Hubs will generally cost less than going to an urgent care center or emergency room.
* For Kelsey ACO members, a primary care copay will apply for most visits, except a specialist
copay applies for behavioral health visits.
Employee Assistance Program (EAP)
Please continue to use your EAP features such as Better
Help (online counseling sessions for your convenience) and GuidanceConnect, the digital method
for making your appointments and selecting a counselor. ese features provide improved access to
the Employee Assistance Program. To register, visit www.guidanceresources.com.
new and notable in Benefits for 2023
MORE ACCESS TO HEALTH CARE AND HEALTH PLANS

7
877-780-HISD (4473).
• Legal, nancial, and grief resources
• Travel assistance
• Legacy planning resources
• Beneciary nancial counseling
• Advisor Connection: on-demand
nancial seminars
Securian increase 1X without any previous enrollment without Evidence of Insurability (EOI).
Employees may increase their life insurance election even if they have not made any election
to 1X annual salary without answering any health questions known as Evidence of Insurability.
Employees who are already enrolled can also take advantage of the one level increase during annual
enrollment up to 5X or $600,000 without evidence of insurability.
Dental Plan – Dental plans will remain through Cigna Dental, but contributions for the PPO and
HMO plans are increasing by 5% in 2023. See the chart below for the 2023 per paycheck deduction
amounts:
*
Tier Dental HMO Dental
PPO
Dental PPO
Buy-up
Dental
Discount Plan
Ee only $7.25 $19.62 $21.74 $2.50
Ee + Spouse $13.78 $38.86 $43.08 $5.00
Ee + Child(ren) $13.78 $38.77 $42.97 $5.00
Family $17.71 $60.63 $67.22 $5.00
*Discount Dental rates remain the same.
Increased lifestyle benets for members who have Securian life insurance – ese new benets
apply to participants who have basic life (all benets-eligible employees) and employees who have
elected supplemental, spouse, and child life benets. Additional benets include:

8
hisdbenefits.org
New Pharmacy ID cards will be issued to employees with coverage under the Express
Scripts pharmacy benet. e cards will feature new ESI member ID numbers to enhance
member security. You should receive your new cards before the new year. Your current card
will work until you receive your new card. Members may also access their digital ID cards
through express-scripts.com or the Express Scripts Mobile App.
e HISD Health & Wellness Center hours have changed. e clinics are open during
the lunch hour. e HMW clinic is open Monday-Friday from 9:00 a.m. to 4:30 p.m.
and Saturday from 8:00 a.m. to 1:00 p.m. e Attucks clinic is open Monday-Friday from
9:00 a.m. to 4:30 p.m. e clinics also screen for depression and can help you with your
chronic conditions, provide interim primary care, as well as meet your urgent care needs.
Give them a call!
TeleHealth and Chat for HISD medical plans – Memorial Hermann ACO and Texas
Medical Neighborhood medical plan members securely text with a doctor any day, any
time. e CareAccess Live app allows you to connect to easy, quality care from your
phone or computer. e next time you have a non-emergency medical question, try using
the CareAccess Live app to securely text with a doctor. ere is a $0 member cost share,
doctors are available 24/7, and you can talk for as long as you need to. Just download the
app from the App Store or Google Play or visit www.careaccesslive.com to sign up and
begin texting with a doctor in seconds.
Members in the Kelsey-Seybold medical plan may schedule a Telehealth visit by using the
MyKelsey app or going online to www.kelsey-seybold.com. Appointments may be made
for either a phone call or a video visit.
IMPORTANT REMINDERS
DOWNLOAD APPS FOR EACH OF THESE BENEFITS
new and notable in Benefits for 2023

9
877-780-HISD (4473).
dependent verification services
Frequently Asked Questions
ese questions and answers should provide employees with the information they need to complete
the process of adding any eligible dependents.
Q: Why is dependent verication being done?
A: At HISD, we are committed to providing aordable healthcare benets for all employees and their
eligible dependents. One way to ensure we eectively spend our benets dollars and provide an equal
level of benet to all employees is to verify we are only paying the expenses of eligible dependents as
specied in our healthcare plans.
Q: Who will be conducting the verication?
A: HISD has partnered with our Benets Service Center to conduct Dependent Eligibility Verication.
Q: Who will be included in the verication?
A: All active employees who wish to enroll in a medical, dental and/or vision plan will be required to
provide supporting documents to substantiate dependent eligibility.
Q: How do I know if my dependents are eligible?
A: e denition of eligible dependents is:
• Your legal spouse
• Your dependent children; Eligible dependent children under 26 years of age include:
• Your biological children
• Your stepchildren
• Your legally adopted children
• Your foster children, including any children placed with you for adoption
• Any children for whom you are responsible under a court order
• Your child who qualies as your dependent under the terms of a qualied medical child
support order (QMSCO )

10
hisdbenefits.org
dependent verification services
You must verify your dependents. Dependent verication is a way of showing proof that any dependent
you would like to enroll for benets coverage meets our plan guidelines for eligibility. It’s a very simple,
very important process. You only need to do it once. You will be required to show documentation that
your dependents meet the HISD plan guidelines. Employees and their dependents may lose or have their
benets eligibility suspended if they are found to have dependents on the plan who are not eligible.
For a child, one of these documents veries eligibility:
• Adoption certicate
• Birth certicate with parent’s name listed
• Documentation of legal guardianship
• Qualied medical child support order
• Adoption placement agreement
• Documentation of legal custody
• Hospital birth record (within 90 days of birth)
For a spouse, one of these documents veries eligibility:
• Declaration of informal marriage
• Marriage license or certicate. If your dependent is a stepchild, you must also provide a copy of a
marriage certicate to substantiate the child’s relationship to the employee or spouse.
If you have any questions, please call the HISD Benets Service Center at 877-780-HISD (4 473)
Q: What types of documentation do I need to provide to satisfy the verication requirements?
A: ere are multiple forms of documentation that will be accepted for your dependents.
Q: What will happen if I don’t respond to the verication letter?
A: Any dependent not veried by document submission by the verication deadline date will not have
coverage from HISD medical, dental and vision benets.
Q: Who should I contact for more information?
A: e HISD Benets Service Center will be available to you during the verication process to answer any
questions that you have. You can contact the Benets Service Center by calling 877-780-HISD (4473).
Representatives are available 7:00 a.m. to 7:00 p.m. CT, Monday-Friday (except holidays) to assist you.

11
877-780-HISD (4473).
Q: What should be provided to validate a Life Event?
A: You would need to provide any documentation that would support the life event you are declaring.
(ex. Marriage, you would prov ide a Marriage certicate that shows the date of Marriage. Dependent
Age out at 26, you would provide the notice received from the insurance company where you were
previously insured that shows you are losing coverage and shows the date coverage will be lost.
Q: What happens if I don’t receive that documentation?
A: You have 30 days to provide the documentation to support your life event . If you are experiencing
delays in receiving that information, please call the Benets Service Center immediately and let them
know you need more time, they are able to give you a small amount of additional time to receive and
submit your documents.
Q: What are some examples of life events?
A: Marriage, Birth of a Child, Adoption, adding a grandchild, divorce and death. If you have any
questions about your specic life event, you can contact the Benets Service Center at 877-780-4473
to ensure that you know how to declare your life event, as well as when to declare the life event so you
can make the changes that are consistent with that life event.
Q: What is a combo audit?
A: It is an audit that includes adding a dependent and a life event. In this case you would need to
provide documentation on your dependent such as a birth certicate or birth facts within 90 days of
birth from the hospital. For a grandchild, you would need to provide proof of guardianship or a custody
agreement from the courts that shows that you have legal custody of your grandchild.
Q: Who should I contact for more information?
A: Contact the Benets Service Center at 877-780-4473

12
hisdbenefits.org
You’re covered
Preventive care services* are covered at no extra cost through your health benefits and insurance plan when
you see a physician or provider in your plan’s network.
We’ve got you covered with no cost share**
Coverage includes routine screenings and checkups, as well as some counseling to prevent
illness, disease and other health problems.
Many of these services are covered as part of physical exams. You won’t have to pay out of pocket for these
preventive visits when they are provided in network.
They include:
Regular checkups
for adults
Routine gynecological
exams for women
Wellness exams
for children
These services are generally not preventive if you get them as part of your visit to diagnose, monitor or treat an
illness or injury. In these cases, copays, coinsurance and deductibles may apply.
Aetna follows preventive recommendations as determined by the U.S. Preventive Services Task Force, Centers
for Disease Control and Prevention and other advisory committees. Screenings, services
and other covered
preventive services can vary by age, gender and other factors. Be sure to talk with your doctor about which
services are right for you.
*Employers with grandfathered plans may choose not to cover some of these preventive services or to include cost
share (deductible, copay or coinsurance) for preventive care services. Certain religious employers and organizations
may choose not to cover contraceptive services as part of the group health coverage.
** Preventive care at no cost share covered in accordance with the Affordable Care Act.
You’re covered
Preventive care services* are covered at no extra cost through your health benefits and insurance plan when
you see a physician or provider in your plan’s network.
We’ve got you covered with no cost share**
Coverage includes routine screenings and checkups, as well as some counseling to prevent
illness, disease and other health problems.
Many of these services are covered as part of physical exams. You won’t have to pay out of pocket for these
preventive visits when they are provided in network.
They include:
Regular checkups
for adults
Routine gynecological
exams for women
Wellness exams
for children
These services are generally not preventive if you get them as part of your visit to diagnose, monitor or treat an
illness or injury. In these cases, copays, coinsurance and deductibles may apply.
Aetna follows preventive recommendations as determined by the U.S. Preventive Services Task Force, Centers
for Disease Control and Prevention and other advisory committees. Screenings, services
and other covered
preventive services can vary by age, gender and other factors. Be sure to talk with your doctor about which
services are right for you.
*Employers with grandfathered plans may choose not to cover some of these preventive services or to include cost
share (deductible, copay or coinsurance) for preventive care services. Certain religious employers and organizations
may choose not to cover contraceptive services as part of the group health coverage.
** Preventive care at no cost share covered in accordance with the Affordable Care Act.
Covered preventive services for adults
commonly include:
Screenings for:
• Abdominal aortic aneurysm (one-time screening for
men of specified ages who have ever smoked)
• Alcohol misuse
• Cholesterol (for adults of certain ages or at higher risk)
• Colorectal cancer*
• Depression
• Diabetes
• Hepatitis B surface antigen
• High blood pressure
• Human immunodeficiency virus (HIV)
• Lung cancer* (for adults with a history of smoking)
• Obesity
• Prostate cancer*
• Syphilis (for all adults at higher risk)
• Tobacco use
• Tuberculosis (TB) testing
Medicine and supplements
Doses, recommended ages and recommended populations vary.
• Aspirin for women at risk of preeclampsia and adults ages 50 – 69 with certain heart risk factors*
• Bowel preparation medication (for preventive colorectal cancer screening)
• Low-dosage statins: dependent on cardiovascular disease (CVD) and risk factors
• Tobacco-cessation medicine approved by the U.S. Food and Drug Administration (FDA), including over-the- counter
medicine when prescribed by a health care provider and
filled at a participating pharmacy
Counseling for:
• Alcohol misuse
• Domestic violence
• Nutrition (for adults with cardiovascular and
diet-related chronic disease)
• Obesity
• Sexually transmitted infection (STI) prevention (for
adults at higher risk)
• Tobacco use (including programs to help you stop
using tobacco)
Immunizations
Doses, recommended ages and recommended populations vary.
• Hepatitis A and B
• Herpes zoster
• Human papillomavirus (HPV)
• Influenza (flu)
• Measles,
mumps, rubella (MMR)
• Meningococcal (meningitis)
• Pneumococcal (pneumonia)
• Tetanus, diphtheria, pertussis (Tdap)
• Varicella (chickenpox)
*Subject to age restrictions.
Covered preventive services for adults
commonly include:
Screenings for:
• Abdominal aortic aneurysm (one-time screening for
men of specified ages who have ever smoked)
• Alcohol misuse
• Cholesterol (for adults of certain ages or at higher risk)
• Colorectal cancer*
• Depression
• Diabetes
• Hepatitis B surface antigen
• High blood pressure
• Human immunodeficiency virus (HIV)
• Lung cancer* (for adults with a history of smoking)
• Obesity
• Prostate cancer*
• Syphilis (for all adults at higher risk)
• Tobacco use
• Tuberculosis (TB) testing
Medicine and supplements
Doses, recommended ages and recommended populations vary.
• Aspirin for women at risk of preeclampsia and adults ages 50 – 69 with certain heart risk factors*
• Bowel preparation medication (for preventive colorectal cancer screening)
• Low-dosage statins: dependent on cardiovascular disease (CVD) and risk factors
• Tobacco-cessation medicine approved by the U.S. Food and Drug Administration (FDA), including over-the- counter
medicine when prescribed by a health
care provider and filled at a participating pharmacy
Counseling for:
• Alcohol misuse
• Domestic violence
• Nutrition (for adults with cardiovascular and
diet-related chronic disease)
• Obesity
• Sexually transmitted infection (STI) prevention (for
adults at higher risk)
• Tobacco use (including programs to help you stop
using tobacco)
Immunizations
Doses, recommended ages and recommended populations vary.
• Hepatitis A and B
• Herpes zoster
• Human papillomavirus (HPV)
• Influenza
(flu)
• Measles, mumps, rubella (MMR)
• Meningococcal (meningitis)
• Pneumococcal (pneumonia)
• Tetanus, diphtheria, pertussis (Tdap)
• Varicella (chickenpox)
*Subject to age restrictions.

13
877-780-HISD (4473).
Covered preventive services for adults
commonly include:
Screenings for:
• Abdominal aortic aneurysm (one-time screening for
men of specified ages who have ever smoked)
• Alcohol misuse
• Cholesterol (for adults of certain ages or at higher risk)
• Colorectal cancer*
• Depression
• Diabetes
• Hepatitis B surface antigen
• High blood pressure
• Human immunodeficiency virus (HIV)
• Lung cancer* (for adults with a history of smoking)
• Obesity
• Prostate cancer*
• Syphilis (for all adults at higher risk)
• Tobacco use
• Tuberculosis (TB) testing
Medicine and supplements
Doses, recommended ages and recommended populations vary.
• Aspirin for women at risk of preeclampsia and adults ages 50 – 69 with certain heart risk factors*
• Bowel preparation medication (for preventive colorectal cancer screening)
• Low-dosage statins: dependent on cardiovascular disease (CVD) and risk factors
• Tobacco-cessation medicine approved by the U.S. Food and Drug Administration (FDA), including over-the- counter
medicine when prescribed by a health
care provider and filled at a participating pharmacy
Counseling for:
• Alcohol misuse
• Domestic violence
• Nutrition (for adults with cardiovascular and
diet-related chronic disease)
• Obesity
• Sexually transmitted infection (STI) prevention (for
adults at higher risk)
• Tobacco use (including programs to help you stop
using tobacco)
Immunizations
Doses, recommended ages and recommended populations vary.
• Hepatitis A and B
• Herpes zoster
• Human papillomavirus (HPV)
• Influenza
(flu)
• Measles, mumps, rubella (MMR)
• Meningococcal (meningitis)
• Pneumococcal (pneumonia)
• Tetanus, diphtheria, pertussis (Tdap)
• Varicella (chickenpox)
*Subject to age restrictions.
Covered preventive services for women
commonly include:
Screenings and counseling for:
• Breast cancer chemoprevention if you’re at a higher risk
• Breast cancer (BRCA) gene counseling and genetic
testing if you’re at high risk with no personal history of
breast and/or ovarian cancer
• Breast cancer mammography*
• Cervical cancer*
• Chlamydia infection*
• Gonorrhea
• Interpersonal or domestic violence
• Osteoporosis* (depending on risk factors)
Medicine and supplements:
• Folic acid supplements (for women of childbearing ages)
• Risk-reducing medicine,
such as tamoxifen and raloxifene, for women with an increased risk for
breast cancer*
Counseling and services**:
• Prescribed FDA-approved over-the-counter or generic
female contraceptives*** when filled at a
network pharmacy
• Two visits a year for patient education and counseling
on contraceptives
• Voluntary sterilization services
Covered preventive services for pregnant women:
• Anemia screenings
• Bacteriuria, urinary tract or other infection screenings
• Breastfeeding interventions
to support and promote
breastfeeding after delivery, including up to six visits
with a lactation consultant
†
• Diabetes screenings
• Expanded counseling on tobacco use
• Hepatitis B counseling (at the first prenatal visit)
• Maternal depression screening
• Rh incompatibility screening, with follow-up testing for
women at higher risk
• Routine prenatal visits (you pay your normal cost
share for delivery, postpartum care, ultrasounds, or
other maternity procedures, specialist visits and
certain l
ab tests)
Covered preventive supplies for pregnant women:
• Breast pump supplies if you get pregnant again before you are eligible for a new pump
• Certain standard electric breastfeeding pumps (nonhospital grade) anytime during pregnancy or while you are
breastfeeding, once every three years
• Manual breast pump anytime during pregnancy or after delivery for the duration of breastfeeding
*Subject to age restrictions.
** Certain eligible religious employers and organizations may choose not to cover
contraceptive services as part of the
group health coverage.
*** Brand-name contraceptive drugs, methods or devices are only covered with no member cost sharing under certain
limited circumstances, including when required by your doctor due to medical necessity.
†
Limits may vary depending upon state requirements and applicability.
Covered preventive services for women
commonly include:
Screenings and counseling for:
• Breast cancer chemoprevention if you’re at a higher risk
• Breast cancer (BRCA) gene counseling and genetic
testing if you’re at high risk with no personal history of
breast and/or ovarian cancer
• Breast cancer mammography*
• Cervical cancer*
• Chlamydia infection*
• Gonorrhea
• Interpersonal or domestic violence
• Osteoporosis* (depending on risk factors)
Medicine and supplements:
• Folic acid supplements (for women of childbearing ages)
• Risk-reducing medicine,
such as tamoxifen and raloxifene, for women with an increased risk for
breast cancer*
Counseling and services**:
• Prescribed FDA-approved over-the-counter or generic
female contraceptives*** when filled at a
network pharmacy
• Two visits a year for patient education and counseling
on contraceptives
• Voluntary sterilization services
Covered preventive services for pregnant women:
• Anemia screenings
• Bacteriuria, urinary tract or other infection screenings
• Breastfeeding interventions
to support and promote
breastfeeding after delivery, including up to six visits
with a lactation consultant
†
• Diabetes screenings
• Expanded counseling on tobacco use
• Hepatitis B counseling (at the first prenatal visit)
• Maternal depression screening
• Rh incompatibility screening, with follow-up testing for
women at higher risk
• Routine prenatal visits (you pay your normal cost
share for delivery, postpartum care, ultrasounds, or
other maternity procedures, specialist visits and
certain l
ab tests)
Covered preventive supplies for pregnant women:
• Breast pump supplies if you get pregnant again before you are eligible for a new pump
• Certain standard electric breastfeeding pumps (nonhospital grade) anytime during pregnancy or while you are
breastfeeding, once every three years
• Manual breast pump anytime during pregnancy or after delivery for the duration of breastfeeding
*Subject to age restrictions.
** Certain eligible religious employers and organizations may choose not to cover contraceptive
services as part of the
group health coverage.
*** Brand-name contraceptive drugs, methods or devices are only covered with no member cost sharing under certain
limited circumstances, including when required by your doctor due to medical necessity.
†
Limits may vary depending upon state requirements and applicability.

14
hisdbenefits.org
Covered preventive services for women
commonly include:
Screenings and counseling for:
• Breast cancer chemoprevention if you’re at a higher risk
• Breast cancer (BRCA) gene counseling and genetic
testing if you’re at high risk with no personal history of
breast and/or ovarian cancer
• Breast cancer mammography*
• Cervical cancer*
• Chlamydia infection*
• Gonorrhea
• Interpersonal or domestic violence
• Osteoporosis* (depending on risk factors)
Medicine and supplements:
• Folic acid supplements (for women of childbearing ages)
• Risk-reducing medicine,
such as tamoxifen and raloxifene, for women with an increased risk for
breast cancer*
Counseling and services**:
• Prescribed FDA-approved over-the-counter or generic
female contraceptives*** when filled at a
network pharmacy
• Two visits a year for patient education and counseling
on contraceptives
• Voluntary sterilization services
Covered preventive services for pregnant women:
• Anemia screenings
• Bacteriuria, urinary tract or other infection screenings
• Breastfeeding interventions
to support and promote
breastfeeding after delivery, including up to six visits
with a lactation consultant
†
• Diabetes screenings
• Expanded counseling on tobacco use
• Hepatitis B counseling (at the first prenatal visit)
• Maternal depression screening
• Rh incompatibility screening, with follow-up testing for
women at higher risk
• Routine prenatal visits (you pay your normal cost
share for delivery, postpartum care, ultrasounds, or
other maternity procedures, specialist visits and
certain l
ab tests)
Covered preventive supplies for pregnant women:
• Breast pump supplies if you get pregnant again before you are eligible for a new pump
• Certain standard electric breastfeeding pumps (nonhospital grade) anytime during pregnancy or while you are
breastfeeding, once every three years
• Manual breast pump anytime during pregnancy or after delivery for the duration of breastfeeding
*Subject to age restrictions.
** Certain eligible religious employers and organizations may choose not to cover contraceptive
services as part of the
group health coverage.
*** Brand-name contraceptive drugs, methods or devices are only covered with no member cost sharing under certain
limited circumstances, including when required by your doctor due to medical necessity.
†
Limits may vary depending upon state requirements and applicability.
Covered preventive services for children
commonly include:
Screening and assessments* for:
• Adolescent depression screening
• Alcohol and drug use
• Anemia
• Attention deficit disorder (ADD)
• Autism
• Behavioral and psychological issues
• Congenital hypothyroidism
• Development
• Hearing
• Height, weight and body mass index
• Hematocrit or hemoglobin
• Hemoglobinopathies or sickle cell
• Hepatitis B
• HIV
• Lead (for children at risk for exposure)
• Lipid disorders (dyslipidemia screening for
children at higher risk)
• Medical history
• Newborn blood screen
ings
• Obesity
• Oral health (risk assessment)
• STIs
• TB testing
• Vision
Medicine and supplements:
• Gonorrhea preventive medicine for the eyes of all newborns
• Oral fluoride for children* (prescription supplements for children without fluoride in their water source)
• Topical application of fluoride varnish by primary care providers
Counseling for:
• Obesity
• STI prevention (for adolescents at higher risk)
Immunizations
From birth to age 18 — doses, recommended ages and recommended populations vary.
• Haemophilus influenzae type B
• Hepatitis A and B
• HPV
• Inactivated poliovirus
• Influenza
• Meningococcal (meningitis)
• MMR
• Pneumococcal (pneumonia)
• Rotavirus
• Tdap/diphtheria, tetanus, pertussis (DTaP)
• Varicella (chickenpox)
*Subject to age restrictions.
Covered preventive services for children
commonly include:
Screening and assessments* for:
• Adolescent depression screening
• Alcohol and drug use
• Anemia
• Attention deficit disorder (ADD)
• Autism
• Behavioral and psychological issues
• Congenital hypothyroidism
• Development
• Hearing
• Height, weight and body mass index
• Hematocrit or hemoglobin
• Hemoglobinopathies or sickle cell
• Hepatitis B
• HIV
• Lead (for children at risk for exposure)
• Lipid disorders (dyslipidemia screening for
children at higher risk)
• Medical history
• Newborn blood screen
ings
• Obesity
• Oral health (risk assessment)
• STIs
• TB testing
• Vision
Medicine and supplements:
• Gonorrhea preventive medicine for the eyes of all newborns
• Oral fluoride for children* (prescription supplements for children without fluoride in their water source)
• Topical application of fluoride varnish by primary care providers
Counseling for:
• Obesity
• STI prevention (for adolescents at higher risk)
Immunizations
From birth to age 18 — doses, recommended ages and recommended populations vary.
• Haemophilus influenzae type B
• Hepatitis A and B
• HPV
• Inactivated poliovirus
• Influenza
• Meningococcal (meningitis)
• MMR
• Pneumococcal (pneumonia)
• Rotavirus
• Tdap/diphtheria, tetanus, pertussis (DTaP)
• Varicella (chickenpox)
*Subject to age restrictions.

15
877-780-HISD (4473).
Know your options
HISD provides a wide array of valuable benets, from medical coverage to life insurance, and from
dental plans to wellness programs. HISD also provides an excellent selection of voluntary benets
such as Accident, Cancer and Specied Diseases, Critical Illness, and Hospital Indemnity, as well as
Disability and additional life insurance and legal plans. Many of these plans provide additional benets,
including cash payouts that are paid in addition to other benets such as your medical plan benets.
Take your time. Study your options.
Everyone has dierent needs, health challenges, budgets, and goals. By choosing your options carefully,
you and your family can get the coverage that ts your needs—and the support to use your benets to
your advantage.
Complete your Health Risk Assessment on aetna.com
Just think of it as a condential mini survey of your health history and habits with instant
results and advice that you can take with you forever.
You can:
• Learn about your health risks and how to lower them
• Gain real-life tips for better well-being
• Share results with your doctor
CHOOSE YOUR PLAN
Are you ready to get healthy or maintain your health?
Here are the steps you can take toward a healthy you (dependents covered under the medical plan
can also take these steps).
Register on aetna.com
is will allow you to access all your benets for medical, HRA, FSA, and claims. Most
importantly, you can access your ID cards immediately.
Select a Primary Care Physician (PCP)
If you don’t have a regular doctor with whom you have established a relationship, now is the time
to nd one using aetna.com. Selecting a Primary Care Physician will help you build a relationship
with your own selected medical professional who will gather and keep up with your medical
history, as well as help coordinate your care. A PCP can be a doctor who practices general
medicine, family medicine, internal medicine or a pediatrician for your children.
Know your benefits
Read your Explanation of Benets (EOB) each time you visit a healthcare professional and they
le a claim. Be sure you understand the terms and how claims are paid. is will help to ensure
your benets are administered correctly.
1
2
3

16
hisdbenefits.org
Important reminders
Take advantage of the tools on HISDbenets.org
to get started.
Other items to note
Working couples
If you and your spouse both work for HISD, each of you may have coverage, but only one of you
can cover your eligible dependents. In addition, only one employee can enroll in life insurance for
their spouse.
Eligible dependents coverage
Every year it is important to review your eligible dependents, as they are the only dependents
who can be covered under your plans. It is your responsibility to change coverage levels if you
have over-age dependents (life, accident, hospital indemnity, critical illness, cancer, etc.).
If you have a dependent who no longer qualies as an eligible dependent, you must notify
the Benets Service Center at 877-780-4473 immediately. If you fail to do so, we will make an
adjustment to remove the dependent when we discover the ineligible dependent while auditing
our plans, and there will be no refund of premiums paid.
Employer-provided Life and AD&D Insurance
HISD provides $10,000 each of Life and Accidental Death and Dismemberment (AD&D)
insurance coverage at no cost to all employees who are eligible for health benets. You also
may purchase supplemental life with a matching AD&D benet for you, your spouse, and your
dependent children.
Annual Enrollment Is
November 1-18, 2022

17
877-780-HISD (4473).
Choosing benefits plan
Choose the plan that’s the right fit
HISD oers several options for your medical plan. Be clear on what’s important to you.
Verify which network your doctors are in with Aetna. And this year, pay particular
attention to your plan options to ensure you nd the right t for the things that are
most important to you. Once your plan starts you will not be able to make changes
without a qualied life event.
Compare your coverage options
You can expect to pay more in premiums when you choose a medical plan with greater
exibility in the doctors you use - or one that requires you to pay less when you use your
health care. It’s a trade o that may not always be worth it. ink about how you use care,
and gauge your comfort level to nd the right balance.
Consider your voluntary options
Add on the extras that make sense for you and your family.
Now you’re ready to enroll
Log onto myHISD to get started.
A step-by-step guide to
choosing the benefits
that work for you
Check plan networks for the doctors you use.

18
hisdbenefits.org
Everyone has dierent needs, health challenges, budgets, and goals. By carefully considering
your medical plan options, you can choose the plan that works best for you and your family.
With options being oered for 2023, it’s especially important to:
• Know how the plans work. is section has descriptions of your 2023 medical plan options.
Be sure to read about each plan before you enroll for benets during Annual Enrollment.
Check Medical Plan 101 below for denitions of common terms.
• ink about how you and your family use health care. Do you use mostly preventive services
during the year? Are you anticipating a hospital stay? Do you live with a chronic medical
condition? e more health care you use, the more coverage you may need.
• Consider your budget. Check the plan charts in this section to see what you will pay in contributions
for each option. Compare contributions to see how much you pay for care versus how much the plan
pays. e more you pay of your own healthcare costs, the less you will pay in contributions and
vice versa.
While your 2023 plan options oer dierent coverage levels and contribution rates, they have
features in common.
HISD no longer contributes to the Healthcare Reimbursement Account (HRA). e HRA is an
HISD-funded account for those who were previously enrolled in one of the legacy Consumer or
Select plan options that may be used to pay for covered services under the medical and pharmacy plan,
up to plan limits. Members may continue to use any funds left over from previous years to pay for eli-
gible expenses, as long as they are currently enrolled in an HISD medical plan. Unused HRA balances
are forfeited when an employee is no longer enrolled in an HISD medical plan or is no longer
employed with HISD.
For members who have existing HRAs, your amounts will rollover until exhausted, and these funds
have been added to your debit card. e HRA account will pay rst when you have eligible expenses,
and then your exible spending account healthcare funds will be used.
Should you have questions, please contact PayFlex at 888-678-8242.
medical plan 101
Choosing benefits plan

19
877-780-HISD (4473).
All medical plan options pay benets ONLY when you receive care from network providers.
If you seek care outside the network, you will pay the full cost of care out of your own pocket
unless you seek emergency medical services.
If you choose a plan with a low deductible, the plan will start to pay sooner, but you will pay
more in contributions. A plan with a higher deductible will cost less in contributions, but you will
pay more of your own expenses before the plan starts to pay.
• Once you meet the deductible, the plan pays a percentage of covered services. You pay a
percentage as well. is is called your coinsurance. For example, if the plan covers a service
at 80%, your coinsurance is 20% once you’ve met the deductible. Plans that pay a higher
percentage of your covered expenses cost more in contributions than those that pay a
lower percentage.
• If there is money in your HRA, you may swipe your Payex debit card to pay for eligible
expenses. If not, and you elect a Health Care Flexible Spending Account (FSA) during
Annual Enrollment, you can use your FSA to pay toward your out-of-pocket expenses.
In addition to assisting with medical conditions, CareAccess Live doctors provide help with
psychiatric diagnosis and treatment of mental health conditions that can be safely managed through
telemedicine. CareAccess Live can treat and provide longitudinal care including starting or adjusting
medications – for behavioral health conditions such as depression, anxiety, insomnia, and
adjustment disorders.
Services available to you and your dependants
• Message a doctor 24/7
• Connect with a doctor in seconds
• Access to care from anywhere
• No appointments or wait times
For conditions consistent with complex mood disorders or psychotic illness, CareAccess Live works
with the patient to get them connected to the right resources for care. For substance abuse disorders,
CareAccess Live providers advise the patient on ways to stay safe and understand their willingness to
engage in the treatment and direct the member to the ER if clinically appropriate.”
CareAccess Live-Memorial Hermann ACO and Texas Medical Neighborhood plan members

20
hisdbenefits.org
your 2023 medical PLAN OPTIONS
If you enroll in an Accountable Care Organization (ACO) plan, you will have a care team of
doctors, nurses, and other providers who belong to the ACO network. ey are dedicated to your
good health and work to:
• Help you get and stay healthy
• Achieve better outcomes when you need care
• Share information and coordinate services
• Spot potential problems
• Encourage you to play an active role in your health and health care
• For some types of medical or prescription drug expenses, you may pay a at fee or copay.
If you elect a Health Care Flexible Spending Account during Annual Enrollment, you can
use your healthcare FSA to pay copays.
• Once the total amount you pay in deductible and coinsurance reaches the annual out-of-pocket
maximum, the plan pays covered expenses at 100% for the rest of the plan year.
You’ll be able to view Explanation of Benets (EOB) statements on your member website at Aetna.com.
e charts in this guide show each plan’s deductible, coinsurance, copay,
and out-of-pocket maximum amounts.
Each time your network doctor or other care provider les a claim with Aetna, an Explanation
of Benets (EOB) statement is generated. It shows the service provided, how the claim was
processed, any amounts paid, and how much you may owe. It also shows your progress toward
meeting the plan’s deductible and out-of-pocket maximum.
21
877-780-HISD (4473).
a Go to Aetna.com
a Select Find a doctor
a Under guests, select “Plan from an employer”
a Under continue as guest, enter your zip code or city (you can also select number
of miles to look within)
a Click Search (this takes you to the networks)
a Go to the category State-Based Plans
a Select TX Medical Neighborhood – Houston Aetna Select
a Select (under State-Based Plans) TX KelseyCare – HMO
a Go to Aetna Whole Health Plans (this is the very rst group)
a Select TX Aetna Whole Health – Memorial Hermann Accountable Care Network
Elect Choice/Aetna Select
Are your doctors in the network?
You can nd out by...
Texas Medical Neighborhood
KelseyCare ACO
Memorial Hermann ACO
There are three Networks
* If you have registered an out of area dependant refer to instructions you were provided
at the time of enrollment.

22
hisdbenefits.org
There are two Memorial Hermann plan options.
memorial hermann aco plans
• More than 900 primary care doctors
• More than 5,000 specialists
• 12 acute care hospitals
• 62 walk-in clinics
• 86 urgent care centers
• Help keep you healthy or improve your health, not just treat you when you’re sick or injured
• Better coordinate your care and keep tabs on your prescriptions, lab results, health history, and more
• Spot problems and build personalized care plans to treat you
• Encourage you to play an active and informed role in your health and healthcare decisions
e Memorial Hermann ACO network plans are designed to improve the quality of your care, provide
a better experience for you and your family, and save you money. You will have access to an integrated
network of primary care doctors, specialists, and hospitals focused on you. Led by a primary care doc-
tor you choose (recommended but not required), your care team will work with you to:
Important: e Memorial Hermann ACO plan pays benets ONLY when you receive
care from the Memorial Hermann ACO network providers. If you seek care outside the
network, you will pay the full cost of care out of your own pocket.
Both plan options include prescription drug benets administered by Express Scripts. You
meet a separate prescription drug deductible each year and then pay the appropriate copay
for your prescriptions.
The Basic plan
oers lower contributions than Plus
options but has higher deductible and
coinsurance amounts. is means you
will pay more when you need health care.
If you don’t visit the doctor oen and use
the plan mostly for preventive care, the
Basic option may be right for you.
The Plus plan
has higher contributions than the Basic
plan, but the deductible and coinsurance
amounts are lower. is means more of
your expenses will be covered when you
need care. If you think you will visit the
doctor oen and need more care, the
Plus option may be right for you.
e Memorial Hermann ACO network is a healthcare system with:
23
877-780-HISD (4473).
Memorial Hermann
Basic ACO
Memorial Hermann
Plus ACO
RATES
Based on 24 pay periods Employee only $21.18 $42.67
Employee + spouse $119.03 $160.68
Employee + child(ren) $110.25 $148.83
Employee + family $203.94 $275.31
PLAN LIMITS
Annual deductible Individual $2,500 $1,750
Family $5,000 $3,500
Annual out-of-pocket max
(includes all medical and pharmacy deductibles,
copays, and coinsurance)
Individual $6,900 $5,150
Family $13,800 $10,300
COST FOR COVERED SERVICES AFTER YOUR DEDUCTIBLE HAS BEEN MET
Preventive care exams
6
Free Free
Primary care (PCP) 25% 20%
Specialists 25% 20%
HISD clinics
2
Free Free
Inpatient—hospital
3
25% 20%
Outpatient—hospital
3
25% 20%
Outpatient—freestanding and surgical center
3
25% 20%
Emergency care
25% + $300 copay
(Copay waived if admitted)
20% + $300 copay
(Copay waived if admitted)
Virtual Health/Telemedicine
CareAceess Live
Free Free
N/A N/A
Urgent care facility 25% 20%
Lab, X-ray, diagnostic mammogram 25% 20%
Diagnostic scans (MRI, MRA, CAT, PET) 25% 20%
Maternity—delivery 25% 20%
Mental
health and substance abuse—inpatient 25% 20%
Mental health and substance abuse—outpatient 25% 20%
1. Kelsey ACO PCP and specialist copays do not count toward the annual deductible but do apply toward the annual out-of-pocket maximum
2. Free if you are enrolled in an HISD medical plan
3. Pre-certication may be required
4. OBGYN Specialists are tiered.
5. Copay applies aer pharmacy deductible has been met
6. Preventive services are not subject to the deductible
7. e copays in the Kelsey plans are not subject to the deductible
If footnote is not shown on this chart it does not apply to this plan option.

24
hisdbenefits.org
There are three Kelsey-Seybold plan options.
Important: the Kelsey-Seybold ACO plan pays benets ONLY when you receive care from
Kelsey Seybold ACO network providers. If you seek care outside the network, you will pay the
full cost of care out of your own pocket.
All plan options include prescription drug benets administered by Express Scripts. With
the exception of the Kelsey Select plan, you must meet a separate prescription drug deductible
each year and then pay the appropriate copay for your prescriptions.
The Kelsey-Seybold ACO network
e Kelsey-Seybold ACO network is a provider group that includes:
• More than 500 doctors representing 55 medical specialties at 31 Houston-area Kelsey-Seybold
Clinic locations with two more locations opening by the end of 2022
• More than 300 primary care doctors and 400 specialists
• 2 accredited ambulatory surgery centers
• 2 cancer center locations
• 1 sleep center
If you need hospital care, your Kelsey-Seybold doctor will determine the most appropriate
hospital for your care.
Kelsey-Seybold has onsite pharmacies located at most of their clinics. Kelsey-Seybold is also
approved by Express Scripts as a Smart 90 pharmacy, so you can even get your 90-day
maintenance medications lled at a Kelsey-Seybold pharmacy.
The Basic plan
oers lower contributions than Plus
options but has higher deductible and
coinsurance amounts. is means you
will pay more when you need health care.
If you don’t visit the doctor oen and use
the plan mostly for preventive care, the
Basic option may be right for you.
The Plus plan
has higher contributions than the Basic
plan, and the deductible and coinsurance
amounts are lower. is means more of
your expenses will be covered when you
need care. If you think you will visit the
doctor oen and need more care, the
Plus option may be right for you.
The Kelsey select plan
has the lowest deductible and out-of-pocket maximum, but this option is only available to
employees who make $31,000 or less in annual base salary.
Kelsey-Seybold aco plans

25
877-780-HISD (4473).
Kelsey
Basic ACO
Kelsey
Plus ACO
RATES
Based on 24 pay periods Employee only
Employee + spouse
Employee + child(ren)
Employee + family
PLAN LIMITS
Annual deductible Individual
Family
Annual out-of-pocket max
(includes all medical and pharmacy deductibles,
copays, and coinsurance)
Individual
Family
COST FOR COVERED SERVICES AFTER YOUR DEDUCTIBLE HAS BEEN MET
Preventive care exams
6
Free Free
Primary care (PCP) $30 copay
1
$30 copay
1
Specialists $65 copay
1
$65 copay
1
HISD clinics
2
Free Free
Inpatient—hospital
3
25% 20%
Outpatient—hospital
3
25% 20%
Outpatient—freestanding and surgical center
3
25% 20%
Emergency care
25% + $300 copay
(Copay waived if admitted)
20% + $300 copay
(Copay waived if admitted)
Virtual Health/Telemedicine N/A N/A
Kelsey Telemedicine
$20 PCP/$55 Specialist
1
$20 PCP/$55 Specialist
1
Urgent care facility 25% 20%
Lab, X-ray, diagnostic mammogram 25% 20%
Diagnos
tic scans (MRI, MRA, CAT, PET) 25% 20%
Maternity—delivery 25% 20%
Mental health and substance abuse—inpatient 25% 20%
Mental health and substance abuse—outpatient $65 Copay
1
$65 Copay
1
$38.79
$146.07
$135.30
$250.27
$1,750
$3,500
$5,150
$10,300
$19.25
$108.21
$100.22
$185.39
$2,500
$5,000
$6,900
$13,800
1. Kelsey ACO PCP and specialist copays do not count toward the annual deductible but do apply toward the annual out-of-pocket maximum
2. Free if you are enrolled in an HISD medical plan
3. Pre-certication may be required
4. OBGYN Specialists are tiered.
5. Copay applies aer pharmacy deductible has been met
6. Preventive services are not subject to the deductible
7. e copays in the Kelsey plans are not subject to the deductible
If footnote is not shown on this chart it does not apply to this plan option.

26
hisdbenefits.org
texas medical neighborhood plans
There are two Texas Medical Neighborhood plan options.
The Basic plan
oers lower contributions each month but
has higher deductible and co–insurance
amounts. is means you will pay more
when you need health care. If you don’t
visit the doctor oen and use the plan
mostly for preventive care, the Basic
option may be right for you.
The Plus plan
has higher contributions than the Basic
plan, but the deductible and coinsurance
amounts are lower. is means more of
your expenses will be covered when you
need care. If you think you will visit the
doctor oen and need more care, the
Plus option may be right for you.
When you enroll in the plan, you are required to select a Primary Care Physician from the Texas
Medical Neighborhood Network. If you do not select a Primary Care Physician, one will be assigned
to you based on your zip code. Your primary care doctor will provide routine and preventive care, and
help you nd the right network specialists when you need one. However, specialist referrals are not
necessary if you want to see a specialist.
Important: e Texas Medical Neighborhood Network plan pays benets ONLY when you re-
ceive care from network providers. If you seek care outside the network, you will pay the full cost
of care out of your own pocket. Both plans include prescription drug benets administered
by Express Scripts. You must meet a separate prescription drug deductible each year and then
pay the appropriate copay for your prescriptions.
The Texas Medical Neighborhood Network
For the Texas Medical Neighborhood plan participants, there are 20 specialties that are tiered. Tier
1 is Maximum Savings and Tier 2 is Standard Savings. When you see a physician in one of these
specialties, you will save more if you select one where Maximum Savings are indicated. is is
just a guide to help you save on your health care. As long as your physicians are in your network,
benets will pay in accordance with your plan. Maximum Savings will save you from paying more
out of pocket than needed. e 20 specialties are:
• Allergy/Immunology
• Cardiology
• Cardiothoracic Surgery
• Dermatology
• Endocrinology
• Gastroenterology
• Infectious Disease
• Nephrology
• Neurology
• Neurosurgery
• Obstetrics/Gynecology
• Ophthalmology
• Orthopedics
• Otolaryngology
• Plastic Surgery
• Pulmonary/Critical Care
• Rheumatology
• Surgery
• Urology
• Vascular Surgery

27
877-780-HISD (4473).
TX Medical
Neighborhood Basic
TX Medical
Neighborhood Plus
RATES
Based on 24 pay periods Employee only
Employee + spouse
Employee + child(ren)
Employee + family
PLAN LIMITS
Annual deductible Individual
Family
Annual out-of-pocket max
(includes all medical and pharmacy deductibles,
copays, and coinsurance)
Individual
Family
COST FOR COVERED SERVICES AFTER YOUR DEDUCTIBLE HAS BEEN MET
Preventive care exams
6
Free Free
Primary care (PCP) 25% 20%
Specialists 25%/45% 20%/40%
HISD clinics
2
Free Free
Inpatient—hospital
3
25% 20%
Outpatient—hospital
3
25% 20%
Outpatient—freestanding and surgical center
3
25% 20%
Emergency care
25% + $300 copay
(Copay waived if admitted)
20% + $300 copay
(Copay waived if admitted)
Virtual Health/Telemedicine
CareAceess Live
Free Free
N/A N/A
Urgent care facility 25% 20%
Lab, X-ray, diagnostic mammogram 25% 20%
Diagnostic scans (MRI, MRA, CAT, PET) 25% 20%
Maternity—delivery 25%/45%
4
20%/40%
4
Mental health and substance abuse—inpatient 25% 20%
Mental health and substance abuse—outpatient 25% 20%
$33.59
$188.65
$174.77
$323.27
$2,500
$5,000
$6,900
$13,800
$67.63
$243.35
$226.17
$391.01
$1,750
$3,500
$5,150
$10,300
1. Kelsey ACO PCP and specialist copays do not count toward the annual deductible but do apply toward the annual out-of-pocket maximum
2. Free if you are enrolled in an HISD medical plan
3. Pre-certication may be required
4. OBGYN Specialists are tiered.
5. Copay applies aer pharmacy deductible has been met
6. Preventive services are not subject to the deductible
7. e copays in the Kelsey plans are not subject to the deductible
If footnote is not shown on this chart it does not apply to this plan option.

28
hisdbenefits.org
All medical plan options include prescription drug benets through Express Scripts available
at any participating pharmacy and through mail order.
Here’s how the plan works:
• You pay a separate prescription drug deductible each year before the plan starts to pay its share of your
prescription drug costs.
• Once you have met your deductible, you pay a copay for your prescriptions.
• e money you pay out of pocket for drugs, either in copays or in meeting your deductible, is applied
toward meeting your medical plan’s annual out-of-pocket maximum, except for the specialty drug
copays through the SaveonSP Manufacturer Copay Assistance Program.
• When your medical annual out-of-pocket maximum is met, your prescription drugs will be
covered at no cost to you for the remainder of the plan year.
No-cost prescriptions for high blood pressure, high cholesterol,
and diabetes
Generic drugs for high blood pressure, high cholesterol, and diabetes (including injectable insulin)
remain available at no cost to you, as long as you are enrolled in an HISD medical plan and purchase
90-day supplies through Express Scripts or at an Express Scripts retail Smart90 pharmacy partner.
HISD plans also cover women’s generic contraceptives (as well as those that have no generic available)
at 100%.
Filling prescriptions at retail pharmacies
With Express Scripts, HISD’s pharmacy benets management company, you have a choice of
participating pharmacies. If you need a short-term prescription like an antibiotic or pain medication,
take the prescription and your Express Scripts member ID card to any of the participating pharmacies.
For long-term and maintenance medications, the Smart90 Program allows you to receive a 90-day
supply of your medication in two ways—either through the Express Scripts' Mail Service Pharmacy
(online, by phone or through mail) or at a Smart90 retail pharmacy near you. No matter which option
you choose, your copay remains the same. You must obtain a 90-day prescription from your physician,
and you can pick up your 90-day maintenance prescription locally at Costco, HEB, Kelsey-Seybold,
Kroger, Randall's, and Walmart or through mail order. Refer to www.Express-Scripts.com or
call Express Scripts at 855-712-0331 for the most current network information.
YOUR PRESCRIPTION BENEFITS

29
877-780-HISD (4473).
For new long-term drug prescriptions, you can get two 30-day supplies of your medication at any
network retail pharmacy for the retail copay, but aer that you will need to use the Smart 90 Program
described above or you will have to pay the mail copay to receive a 30-day supply at any network retail
pharmacy. Ordering a 90-day supply through Express Scripts Mail Service Pharmacy or a Smart90 retail
pharmacy (retail location or mail order) will result in substantial savings to you for long-term and mainte-
nance medications.
Filling prescriptions with the mail order service
e Express Scripts mail order service is a cost-eective and convenient choice for lling long-term
prescriptions, including those for maintenance medications provided at no charge. To use the mail
order service:
• Go to HISDBenets.org and click on Resources then forms.
• Complete the mail order form and mail to the address indicated.
• Once you’ve placed your order, you can sign up for the Express Scripts automatic rell
program. Express Scripts will even request a new prescription from your doctor when your rells
are up or your prescription has expired.
If you need specialty drugs
When you have chronic or complex medical conditions such as multiple sclerosis or rheumatoid arthritis,
your doctor may prescribe specialty drugs. ese drugs typically require special handling, administration
or monitoring. You can order specialty drugs through Accredo, the Express Scripts specialty mail order
pharmacy.
You also may be able to take advantage of the Express Scripts SaveonSP (Specialty Pharmacy)
Manufacturer Copay Assistance Program. is program is designed to help you save money on
certain specialty medications. If you participate, certain specialty medications will be free of charge ($0).
Your prescriptions will still be lled through Accredo, your existing specialty mail pharmacy.
Express Scripts will contact you if you are eligible to participate in the SaveonSP program. Enrollment
in the program is voluntary. If you choose not to participate, you will be responsible for the applicable
prescription copay. Keep in mind that the copay will not count toward your deductible or out-of-pocket
maximums.
For more information about the SaveonSP Manufacturer Copay Assistance Program, please contact
SaveonSP at 800-683-1074 Monday-ursday 8:00 a.m.-8:00 p.m., and Friday 8:00 a.m.-6:00 p.m.
Eastern Time.

30
hisdbenefits.org
The Express Scripts Discount Rx Program
If you waive HISD-sponsored medical coverage, you may enroll in the Express Scripts Discount
Rx program. Eligible employees can enroll by:
• Signing up via the HISD portal
• Calling the HISD Benets Service Center from 7:00 a.m.- 7 p.m., Monday-Friday,
at 877-780-HISD (4473).
You can enroll at initial eligibility, annual enrollment or during a qualifying life event change.
e program entitles you to a cash discount through Express Scripts participating pharmacies and
mail service. e Discount Rx card is not insurance, and you do not have a copay amount. You are
responsible for paying 100% of the discounted Express Scripts price and any dispensing fee. Express
Scripts will provide you an ID card when you enroll.
THINGS TO CONSIDER ABOUT YOUR PHARMACY PLAN
Express Scripts prior authorization drives plan savings by monitoring the dispensing of high-cost
medications and those with the potential for misuse.
e Step erapy program applies edits to drugs in specic therapeutic classes at the point of sale.
Coverage for back-up therapies (second/third step) is determined at the patient level based on the
presence or absence of front-line drugs or other automated factors in the patient’s claims history.
e Drug Quantity Management program manages prescription costs by ensuring that the quantity
of units supplied for each copayment is consistent with clinical dosing guidelines. e program is
designed to support safe, eective, and economic use of drugs while giving patients access to
quality care.
YOUR PRESCRIPTION BENEFITS

31
877-780-HISD (4473).

32
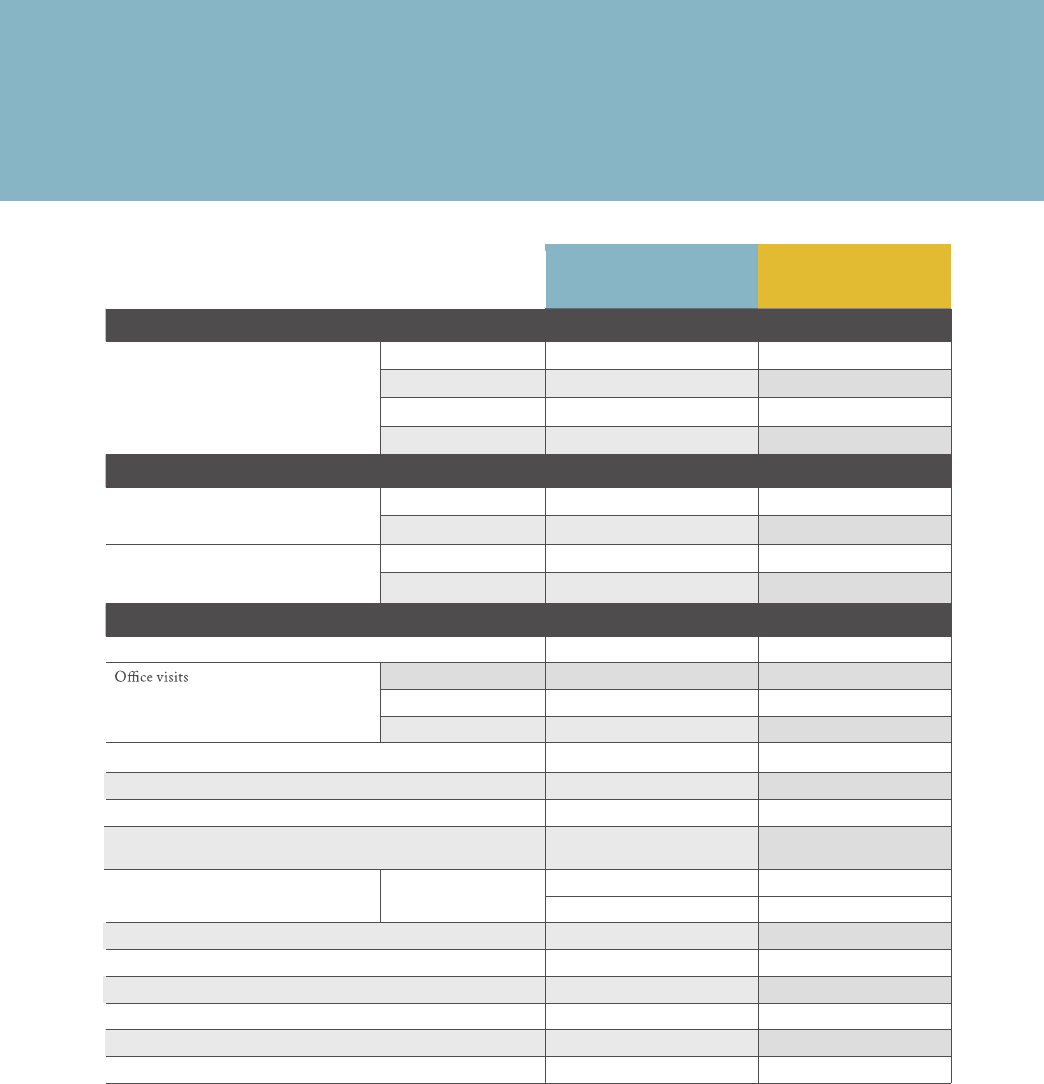
hisdbenefits.org
Kelsey
Basic ACO
Memorial Hermann
Basic ACO
TX Medical
Neighborhood Basic
Kelsey
Plus ACO
Memorial Hermann
Plus ACO
TX Medical
Neighborhood Plus
RATES
Based on 24 pay periods Employee only $19.25 $21.18
$33.59
$38.79 $42.67 $67.63
Employee + spouse $108.21 $119.03
$188.65
$146.07 $160.68 $243.35
Employee + child(ren) $100.22 $110.25
$174.77
$135.30 $148.83 $226.17
Employee + family $185.39 $203.94
$323.27
$250.27 $275.31 $391.01
PLAN LIMITS
Annual deductible Individual $2,500 $2,500
$2,500
$1,750 $1,750 $1,750
Family $5,000 $5,000
$5,000
$3,500 $3,500 $3,500
Annual out-of-pocket max
(includes all medical and pharmacy deductibles,
copays, and coinsurance)
Individual $6,900 $6,900
$6,900
$5,150 $5,150 $5,150
Family $13,800 $13,800
$13,800
$10,300 $10,300 $10,300
COST FOR COVERED SERVICES AFTER YOUR DEDUCTIBLE HAS BEEN MET
Preventive care exams
6
Free Free Free Free Free Free
Primary care (PCP) $30 copay
1,7
25% 25% $30 copay
1,7
20% 20%
Specialists $65 copay
1,7
25% 25%/45% $65 copay
1,7
20% 20%/40%
HISD clinics
2
Free Free Free Free Free Free
Inpatient—hospital
3
25% 25% 25% 20% 20% 20%
Outpatient—hospital
3
25% 25% 25% 20% 20% 20%
Outpatient—freestanding and surgical center
3
25% 25% 25% 20% 20% 20%
Emergency care
25% + $300 copay
(Copay waived if admitted)
25% + $300 copay
(Copay waived if admitted)
25% + $300 copay
(Copay waived if admitted)
20% + $300 copay
(Copay waived if admitted)
20% + $300 copay
(Copay waived if admitted)
20% + $300 copay
(Copay waived if admitted)
Virtual Health/Telemedicine
Kelsey Telemedicine
CareAceess Live
$20 PCP/$55 Specialist
1
CareAcess Live CareAcess Live $20 PCP/$55 Specialist
1
CareAcess Live CareAcess Live
Urgent care facility 25% 25% 25% 20% 20% 20%
Lab, X-ray, diagnostic mammogram 25% 25% 25% 20% 20% 20%
Diagnostic scans (MRI, MRA, CAT, PET) 25% 25% 25% 20% 20% 20%
Maternity—delivery 25% 25% 25%/45%
4
20% 20% 20%/40%
4
Mental health and substance abuse—inpatient 25% 25% 25% 20% 20% 20%
Mental health and substance abuse—outpatient $65 Copay
1
25% 25% $65 Copay
1
20% 20%
2023
Medical plan comparison
1. Kelsey ACO PCP and specialist copays do not count toward the annual deductible but do apply toward the annual out-of-pocket maximum
2. Free if you are enrolled in an HISD medical plan
3. Pre-certification may be required
4. OBGYN Specialists are tiered.
5. Copay applies after pharmacy deductible has been met
6. Preventive
services are not subject to the deductible
7.
COMPARE YOUR COVERAGE OPTIONS

33
877-780-HISD (4473).
Kelsey
Basic ACO
Memorial Hermann
Basic ACO
TX Medical
Neighborhood Basic
Kelsey
Plus ACO
Memorial Hermann
Plus ACO
TX Medical
Neighborhood Plus
RATES
Based on 24 pay periods Employee only $19.25 $21.18
$33.59
$38.79 $42.67 $67.63
Employee + spouse $108.21 $119.03
$188.65
$146.07 $160.68 $243.35
Employee + child(ren) $100.22 $110.25
$174.77
$135.30 $148.83 $226.17
Employee + family $185.39 $203.94
$323.27
$250.27 $275.31 $391.01
PLAN LIMITS
Annual deductible Individual $2,500 $2,500
$2,500
$1,750 $1,750 $1,750
Family $5,000 $5,000
$5,000
$3,500 $3,500 $3,500
Annual out-of-pocket max
(includes all medical and pharmacy deductibles,
copays, and coinsurance)
Individual $6,900 $6,900
$6,900
$5,150 $5,150 $5,150
Family $13,800 $13,800
$13,800
$10,300 $10,300 $10,300
COST FOR COVERED SERVICES AFTER YOUR DEDUCTIBLE HAS BEEN MET
Preventive care exams
6
Free Free Free Free Free Free
Primary care (PCP) $30 copay
1,7
25% 25% $30 copay
1,7
20% 20%
Specialists $65 copay
1,7
25% 25%/45% $65 copay
1,7
20% 20%/40%
HISD clinics
2
Free Free Free Free Free Free
Inpatient—hospital
3
25% 25% 25% 20% 20% 20%
Outpatient—hospital
3
25% 25% 25% 20% 20% 20%
Outpatient—freestanding and surgical center
3
25% 25% 25% 20% 20% 20%
Emergency care
25% + $300 copay
(Copay waived if admitted)
25% + $300 copay
(Copay waived if admitted)
25% + $300 copay
(Copay waived if admitted)
20% + $300 copay
(Copay waived if admitted)
20% + $300 copay
(Copay waived if admitted)
20% + $300 copay
(Copay waived if admitted)
Virtual Health/Telemedicine
Kelsey Telemedicine
CareAceess Live
$20 PCP/$55 Specialist
1
CareAcess Live CareAcess Live $20 PCP/$55 Specialist
1
CareAcess Live CareAcess Live
Urgent care facility 25% 25% 25% 20% 20% 20%
Lab, X-ray, diagnostic mammogram 25% 25% 25% 20% 20% 20%
Diagnostic scans (MRI, MRA, CAT, PET) 25% 25% 25% 20% 20% 20%
Maternity—delivery 25% 25% 25%/45%
4
20% 20% 20%/40%
4
Mental health and substance abuse—inpatient 25% 25% 25% 20% 20% 20%
Mental health and substance abuse—outpatient $65 Copay
1
25% 25% $65 Copay
1
20% 20%
2023
Medical plan comparison
1. Kelsey ACO PCP and specialist copays do not count toward the annual deductible but do apply toward the annual out-of-pocket maximum
2. Free if you are enrolled in an HISD medical plan
3. Pre-certification may be required
4. OBGYN Specialists are tiered.
5. Copay applies after pharmacy deductible has been met
6. Preventive
services are not subject to the deductible
7.

34
hisdbenefits.org
Annual pharmacy deductible $50 per person $50 per person
$50 per person $50 per person $50 per person $50 per person
Prescription drugs
(30-day retail)
5
Generic $20 $20
$20 $15 $15 $15
Preferred brand $50 $50
$50 $40 $40 $40
Non-preferred brand generic $70 $70
$70 $60 $60 $60
Prescription drugs
(90-day mail or retail)
5
Generic $50 $50
$50 $37.50 $37.50 $37.50
Preferred brand $125 $125
$125 $100 $100 $100
Non-preferred brand generic $175 $175
$175 $150 $150 $150
Specialty (30-day supply)
5
$150 $150
$150 $100 $100 $100
5. Copay applies after pharmacy deductible has been met
Kelsey
Basic ACO
Memorial Herman
n
Basic ACO
TX Medical
Neighborhood Basic
Kelsey
Plus ACO
Memorial Hermann
Plus ACO
TX Medical
Neighborhood Plus
PRESCRIPTION
2023
prescription drug comparison
BE CAREFUL
If you or your physician request a brand-name drug when a generic drug is
available, you pay the brand copay PLUS the dierence in cost between the two
drugs, along with any remaining prescription deductible.
COMPARE YOUR COVERAGE OPTIONS

35
877-780-HISD (4473).
Annual pharmacy deductible $50 per person $50 per person
$50 per person $50 per person $50 per person $50 per person
Prescription drugs
(30-day retail)
5
Generic $20 $20
$20 $15 $15 $15
Preferred brand $50 $50
$50 $40 $40 $40
Non-preferred brand generic $70 $70
$70 $60 $60 $60
Prescription drugs
(90-day mail or retail)
5
Generic $50 $50
$50 $37.50 $37.50 $37.50
Preferred brand $125 $125
$125 $100 $100 $100
Non-preferred brand generic $175 $175
$175 $150 $150 $150
Specialty (30-day supply)
5
$150 $150
$150 $100 $100 $100
5. Copay applies after pharmacy deductible has been met
Kelsey
Basic ACO
Memorial Herm
ann
Basic ACO
TX Medical
Neighborhood Basic
Kelsey
Plus ACO
Memorial Hermann
Plus ACO
TX Medical
Neighborhood Plus
PRESCRIPTION
2023
prescription drug comparison
36
hisdbenefits.org
Flexible spending accounts allow you to set aside money to pay for eligible health and dependent
care expenses.
Your contributions are taken out of your paycheck before taxes, which means your money goes further
because it’s tax-free. at’s why an FSA can be a smart choice for anyone who has regular predictable
health or dependent care costs.
You decide the amount ahead of time based on your expected out-of-pocket expenses for the entire
plan year. For more information, visit the IRS website at IRS.Gov/Publications for a full list of eligible
expenses.
If you already have your PayFlex debit card and decide to enroll in the Healthcare Flexible Spending
Account (FSA) for 2023, you will be able to use the same card, which is already active and ready to go.
Please retain this debit card for use as you continue to enroll each year in the healthcare exible
spending account. Take note of the expiration date – you will be issued a new debit card based on
this date.
Flexible Spending Accounts (FSA)
payflex debit card
Please note
You have to enroll in your FSA each year.
ere’s no automatic enrollment.
If you join HISD after January 1, 2023,
your deductions are allocated over
the remaining pay periods for
the plan year to reach your
annual goal amount.
Be careful
Estimate the amount you
expect to spend carefully.
You lose any funds you don’t use.
consider your voluntary options

37
877-780-HISD (4473).
Please note
You will receive a healthcare debit card
from Payex (an Aetna partner) with your
available funds.
important
If you have money in a previous year’s
Health Reimbursement Account, you
must use this money rst to pay for
eligible medical expenses before using
your Healthcare FSA.
Health care FSA
• You can set aside up to $2,850.00 pre-tax to pay for eligible healthcare expenses that are not
reimbursable from any other source.
• You can use your FSA for all eligible healthcare costs for you and your dependents, including vision
and dental, even if your dependents are not covered under an HISD medical plan.
• 2023 FSA contribution limits will be posted aer the IRS releases the information in
late November 2022.
• e full amount you set aside is available to you on January 1, 2023, even though it is deducted
from your paycheck over 24 pay periods.
• You have a 2½-month grace period (March 15) to incur additional claims and until May 15, to le
for reimbursement generally.
Dependent care FSA
• You and your spouse can set up a combined total of up to $5,000 pre-tax to pay for childcare and
eldercare expenses for a qualied person so you can work or look for work.
• Unlike the health care FSA, you can only be reimbursed funds that have already been withheld
from your paycheck.
• Eligible expenses include daycare, nursery school, aer-school care, summer day camp and
elder day care.
You can not use your dependent care FSA to pay for your dependent medical expenses.

38
hisdbenefits.org
Cigna Dental HMO - CIGNA'S ACCESS PLUS NETWORK
• Coverage includes dental implants and teeth whitening.
• You must choose a Network General Dentist (NGD) and use only providers in this
Cigna DHMO network. e cuto for choosing or changing your NGD is the 15th
of each month in order to be eective the rst of the following month.
• You must be referred for specialty services through your NGD before specialty
services can be rendered. For more information visit HISDBenets.org.
• You pay the set copays when you receive covered services, but you don’t pay deductibles or have
to le claim forms. Visit hisdbenets.org to review the copayment schedule.
• Services outside the network are covered only in emergencies and require prior approval
from Cigna Dental.
• Orthodontia is included.
• No annual limits.
• Cigna’s Oral Health Integration Program provides extra cleanings and services for
chronic medical conditions.
Cigna Dental PPO
• Coverage includes dental implants and adult orthodontia.
• You pay a deductible before the plan begins to pay its share of covered expenses.
• You may use any provider you choose, but keep in mind you generally save money by using an
in-network provider. If you use an out-of-network provider, you are responsible for costs that may
exceed the usual, customary, and reasonable guidelines; in this case, you must le a claim form.
• ere is an annual maximum benet of $1,350 to $1,650 per person in the PPO or $2,000
for the buyup option.
• is plan includes a Wellness Plus feature. You and your covered dependents can increase
your annual maximum by $100 in the following year (up to a total maximum of $1,650) by taking
advantage of the plan’s preventive care.
• e PPO buyup plan does not have a deductible for preventive.
You must use the DHMO fee schedule to
determine covered expenses and copays.
consider your voluntary options

39
877-780-HISD (4473).
Cigna Dental HMO - CIGNA'S ACCESS PLUS NETWORK
• Coverage includes dental implants and teeth whitening.
• You must choose a Network General Dentist (NGD) and use only providers in this
Cigna DHMO network. e cuto for choosing or changing your NGD is the 15th
of each month in order to be eective the rst of the following month.
• You must be referred for specialty services through your NGD before specialty
services can be rendered. For more information visit HISDBenets.org.
• You pay the set copays when you receive covered services, but you don’t pay deductibles or have
to le claim forms. Visit hisdbenets.org to review the copayment schedule.
• Services outside the network are covered only in emergencies and require prior approval
from Cigna Dental.
• Orthodontia is included.
• No annual limits.
• Cigna’s Oral Health Integration Program provides extra cleanings and services for
chronic medical conditions.
Cigna Dental PPO
• Coverage includes dental implants and adult orthodontia.
• You pay a deductible before the plan begins to pay its share of covered expenses.
• You may use any provider you choose, but keep in mind you generally save money by using an
in-network provider. If you use an out-of-network provider, you are responsible for costs that may
exceed the usual, customary, and reasonable guidelines; in this case, you must le a claim form.
• ere is an annual maximum benet of $1,350 to $1,650 per person in the PPO or $2,000
for the buyup option.
• is plan includes a Wellness Plus feature. You and your covered dependents can increase
your annual maximum by $100 in the following year (up to a total maximum of $1,650) by taking
advantage of the plan’s preventive care.
• e PPO buyup plan does not have a deductible for preventive.
Cigna Dental Benefit Summary
Houston ISD
Plan Renewal Date: 01/01/2023
Insured by: Cigna Health and Life Insurance Company
This material is for informational purposes only and is designed to highlight some of the benefits available under this plan. Consult the plan documents
to determine specific terms of coverage relating to your plan. Terms include covered procedures, applicable waiting periods, exclusions and limitations.
You r plan al l ows you to se e any l icens ed de ntist, bu t u sing an i n-network de ntist may minimize your out-of -pocket expenses.
Cigna Dental Choice Plan
Network Options
In-Network:
Total Cigna DPPO Network
Out-of-Network:
See Non-Network Reimbursement
Reimbursement Levels
Based on Contracted Fees
Max imum Reimbursable Charge
Calendar Year Benefits Maximum
Applies to: Class I, II, III & IX expenses
$2,000
$2,000
Calendar Year Deductible
In dividual
Family
$50
$150
$50
$150
Benefit Highlights
Plan Pays
You Pay
Plan Pays
You Pay
Class I: Diagnostic & Preventive
Oral Evaluations
Prophylaxis: routine cleanings
X-rays: routine
X-rays: non-routine
Fluo ride Application
Sealants: per tooth
Space Maintainers: non-orthodontic
Emergency Care to Relieve Pain
100%
No Deduct ible
No Charge
100%
No Deduct ible
No Charge
Class II: Basic Restorative
Restorative: fillings
Endodontics: minor and major
Periodontics: minor and major
Oral Surgery: minor and major
Anesthesia: general and IV sedation
Repairs: bridges, crowns and inlays
Repairs: dentures
Denture Relines, Rebases and Adjustments
80%
After Deduct ible
20%
After Deduct ible
80%
After Deduct ible
20%
After Deduct ible
Class III: Major Restorative
Inlays and Onlays
Prosthesis Over Implant
Crowns: prefabricated stainless steel / resin
Crowns: permanent cast and porcelain
Bridges and Dent ures
50%
After Deduct ible
50%
After Deduct ible
50%
After Deduct ible
50%
After Deduct ible
Class IV: Orthodontia
Coverage for Employee and All Dependents
Lifet ime Benefit s Maximum: $2,000
50%
No Deduct ible
50%
No Deduct ible
50%
No Deduct ible
50%
No Deduct ible
Class IX: Implants
50%
After Deduct ible
50%
After Deduct ible
50%
After Deduct ible
50%
After Deduct ible
Benefit Plan Provisions:
In-Network Reimbursement
For services provided by a Cigna Dental PPO network dentist, Cigna Dental will reimburse the
dentist according to a Fee Schedule or Discount Schedule.
Non-Network Reimbursement
For services provided by a non-network dentist, Cigna Dental will reimburse according to the
Maximum Reimbursable Charge. The MRC is calculated at the 80th percentile of all provider
submit ted am ount s in the geographic area. T he dentist may balance bill up to their usual fees.
Cross Accumulation
All deductibles, plan maximums, and service specific maximums cross accumulate between in
and out of network. Benefit frequency limitations are based on the date of service and cross
accumulate between in and out of network.
Calendar Year Benefits Maximum
The plan will only pay for covered charges up to the yearly Benefits Maximum, when
applicable. Benefit-specific Maximums may also apply.
Calendar Year Deductible
This is the amount you must pay before the plan begins to pay for covered charges, when
applicable. Benefit-specific deductibles may also apply.

40
hisdbenefits.org
Pretreatment Review
Pretreatment review is available on a voluntary basis when dental work in excess of $200 is
proposed.
Alternate Benefit Provision
When more than one covered Dental Service could provide suitable treatment based on common
dental standards, Cigna will determine the covered Dental Service on which payment will be
based and the expenses that will be included as Covered Expenses.
Oral Health Integration Program
®
The Cigna Dental Oral Health Integration Program offers enhanced dental coverage for
customers we have identified as having certain medical conditions. There is no additional charge
to participate in the program. Those who qualify can receive reimbursement of their coinsurance
for eligible dental services. Eligible customers can also receive guidance on behavioral issues
related to oral health. Reimbursements under this program are not subject to the annual
deduct ible, but will be applied to the plan annual maximum.
For more information on how to enroll in this program and a complete list of terms and eligible
conditions, go to www.m ycign a . co m or call customer service 24/7 at 1-800-Cigna24.
Timely Filing
Out of network claims submitted to Cigna after 365 days from date of service will be denied.
Benefit Limitations:
Missing Toot h Limit ation
For teeth missing prior to coverage with Cigna, the amount payable is 50% of the amount
otherwise payable until covered for 12 months; thereafter, considered a Class III expense.
Oral Evaluations/Exams
2 per calendar year.
X-rays (routine)
Bitewings: 2 per calendar year.
X-rays (non-routine)
Complete series of radiographic images and panoramic radiographic images: Limited to a
combined total of 1 per 36 months.
Diagnostic Casts
Payable only in conjunction wit h orthodontic workup.
Cleanings
2 per calendar year, including periodontal maintenance procedures following active therapy.
Fluoride Application
2 per calendar year for children under age 19.
Sealants (per tooth)
Limit ed to posterior tooth. 1 treatment per tooth every 36 months for children under age 16.
Space Maintainers
Limited to non-orthodontic treatment for children under age 19.
Inlays, Crowns, Bridges, Dentures and Partials
Replacement every 60 months if unserviceable and cannot be repaired. Benefits are based on the
amount payable for non-precious metals. No porcelain or white/tooth-colored material on molar
crown s or bridges.
Denture and Bridge Repairs
Reviewed if more than once.
Denture Adjustments, Rebases and Relines
Covered if more than 6 months after installation.
Prosthesis Over Implant
1 every 60 months if unserviceable and cannot be repaired. Benefits are based on the amount
payable for non-precious metals. No porcelain or white/tooth colored material on molar crowns
or bridges.
Benefit Exclusions:
Covered Expenses will not include, and no payment will be made for the following:
Procedures and services not included in the list of covered dental expenses;
Diagnostic: cone beam imaging;
Preventive Services: instruction for plaque control, oral hygiene and diet;
Restorative: veneers of porcelain, ceramic, resin, or acrylic materials on crowns or pontics on or replacing the upper and or lower first, second and/or
third molars;
Periodontics: bite registrat ions; splinting;
Prosthodontics: precision or semi-precision attachments;
Procedures, appliances or restorations, except full dentures, whose main purpose is to change vertical dimension, diagnose or treat conditions of
dysfunction of the temporomandibular joint (TMJ), stabilize periodontally involved teeth or restore occlusion;
At hlet ic mout h guards;
Services performed primarily for cosmetic reasons;
Personalization or decoration of any dental device or dental work;
Replacement of an appliance per benefit guidelines;
Services that are deemed to be medical in nature;
Services and supplies received from a hospital;
Drugs: p rescrip t ion drugs;
Charges in excess of the Maximum Reimbursable Charge.
This document provides a summary only. It is not a contract. If there are any differences between this summary and the official plan documents, the terms
of the official plan document s will prevail.
Product availability may vary by location and plan type and is subject to change. All group dental insurance policies and dental benefit plans contain
exclusions and limitations. For costs and details of coverage, review your plan documents or contact a Cigna representative.
All Cigna products and services are provided exclusively by or through operating subsidiaries of Cigna Corporation, including Cigna Health and Life
Insurance Company (CHLIC), Connecticut General Life Insurance Company, and Cigna Dental Health, Inc.
© 2021 Cigna / version 09152021

41
877-780-HISD (4473).
Cigna Dental Benefit Summary
Houston ISD
Plan Renewal Date: 01/01/2023
Insure d by: Cigna Health and Life Insurance Company
This material is for informational purposes only and is designed to highlight some of the benefits available under this plan. Consult the plan documents
to determine specific terms of coverage relating to your plan. T erms include covered procedures, applicable waiting periods, exclusions and limitations.
Receiving regular dental care can not only catch minor problems before they become major and expensive to treat - it may even help improve your
overall health. Gum disease is increasingly being linked to complications for pre-term birth, heart disease, stroke, diabetes, osteoporosis and other
health issues. That’s why this dental plan includes Cigna De ntal WellnessPl us
SM
features. When you or your family members receive any preventive
care service in one plan year, the annual dollar maximum will increase in the following plan year. When you or your family members remain enrolled
in the plan and continue to receive preventive care, the annual dollar maximum will increase in the following plan year, until it reaches the level
specified below. Please refer to your plan materials for additional information on this plan feature. You r plan allows you to see any licensed dentist,
but using an in-network dentist may minimize your out-of-pocket expenses.
Cigna Dental Choice Plan
Network Options
In-Network:
Total Cigna DPPO Network
Out-of-Network:
See Non-Network Reimbursement
Reimbursement Levels
Based on Contracted Fees
Maximum Reimbursable Ch arge
WellnessPlus
SM
Progressive Maximum Benefit:
When you or your family members receive any preventive care service during one plan year, the annual dollar maximum will incr ease in the
following plan year; until it reaches the highest level specified below. Please refer to your plan materials for additional information on t his plan
feature.
Calendar Year Benefits Maximum
Applies to: Class I, II, III & IX expenses
Year 1: $1,350
Year 2: $1,450
Year 3: $1,550
Year 4 & Beyond: $1,650
Year 1: $1,350
Year 2: $1,450
Year 3: $1,550
Year 4 & Beyond: $1,650
Calendar Year Deductible
In div idual
Family
$50
$150
$50
$150
Benefit Highlights
Plan Pays
You Pay
Plan Pays
You Pay
Class I: Diagnostic & Preventive
Oral Evaluations
Prophylaxis: routine cleanings
X-rays: routine
X-rays: non-routine
Fluoride Application
Sealants: per tooth
Space Maintainers: non-orthodontic
100%
Aft er Deduct ible
0%
Aft er Deduct ible
100%
Aft er Deduct ible
0%
Aft er Deduct ible
Class II: Basic Restorative
Restorative: fillings
Endodontics: minor and major
Periodontics: minor and major
Oral Surgery: minor and major
Anesthesia: general and IV sedation
Emergency Care to Relieve Pain
80%
Aft er Deduct ible
20%
Aft er Deduct ible
80%
Aft er Deduct ible
20%
After Deduct ible
Class III: Major Restorative
Inlays and Onlays
Prosthesis Over Implant
Crowns: prefabricated stainless steel / resin
Crowns: permanent cast and porcelain
Bridges and Dent ures
Repairs: Bridges, Crowns and Inlays
Repairs: Dentures
Denture Relines, Rebases and Adjustments
50%
Aft er Deduct ible
50%
Aft er Deduct ible
50%
Aft er Deduct ible
50%
Aft er Deduct ible
Class IV: Orthodontia
Coverage for Employee and All Dependents
Lifetime Benefits Maximum: $2,000
50%
After Deductible
50%
After Deductible
50%
After Deductible
50%
After Deductible
Class IX: Implants
50%
After Deductible
50%
Aft er Deduct ible
50%
Aft er Deduct ible
50%
Aft er Deduct ible

42
hisdbenefits.org
Benefit Plan Provisions:
In-Network Reimbursement
For services provided by a Cigna Dental PPO network dentist, Cigna Dental will reimburse
the dentist according to a Fee Schedule or Discount Schedule.
Non-Network Reimbursement
For services provided by a non-network dentist, Cigna Dental will reimburse according to the
Maximum Reimbursable Charge. The MRC is calculated at the 80th percentile of all provider
submit t ed amounts in the geographic area. The dentist may balance bill up to their usual fees.
Cross Accumulation
All deductibles, plan maximums, and service specific maximums cross accumulate between
in-network and out-of-network. Benefit frequency limitations are based on the date of service
and cross accumulate between in and out of network.
Calendar Year Benefits Maximum
The plan will only pay for covered charges up to the yearly Benefits Maximum, when
applicable. Benefit-specific Maximums may also apply.
Calendar Year Deductible
This is the amount you must pay before the plan begins to pay for covered charges, when
applicable. Benefit-specific deductibles may also apply.
Pretreatment Review
Pretreatment review is available on a voluntary basis when dental work in excess of $200 is
proposed.
Alternate Benefit Provision
When more than one covered Dental Service could provide suitable treatment based on
common dental standards, Cigna will determine the covered Dental Service on which
payment will be based and the expenses that will be included as Covered Expenses.
Oral Health Integration Program
®
The Cigna Dental Oral Health Integration Program offers enhanced dental coverage for
customers we have identified as having certain medical conditions. There is no additional
charge to participate in the program. Those who qualify can receive reimbursement of their
coinsurance for eligible dental services. Eligible customers can also receive guidance on
behavioral issues related to oral health. Reimbursements under this program are not subject to
t he annual deduct ible, but will be applied to the plan annual maximum.
For more information on how to enroll in this program and a complete list of terms and
eligible conditions, go to www.m y c ign a. c o m or call customer service 24/7 at 1-800-Cigna24.
Timely Filing
Out of network claims submitted to Cigna after 365 days from date of service will be denied.
Benefit Limitations:
Missing Tooth Limit ation
For teeth missing prior to coverage with Cigna, the amount payable is 50% of the amount
otherwise payable unt il covered for 12 months; thereafter, considered a Class III expense.
Oral Evaluations/Exams
2 per calendar year.
X-rays (routine)
Bitewings: 2 per calendar year.
X-rays (non-routine)
Complete series of radiographic images and panoramic radiographic images: Limited to a
combined total of 1 per 36 months.
Diagnostic Casts
Payable only in conjunction wit h orthodontic workup.
Cleanings
2 per calendar year, including periodontal maintenance procedures following active therapy.
Fluoride Application
2 per calendar year for children under age 19.
Sealants (per tooth)
Limit ed to posterior tooth. 1 treatment per tooth every 36 months for children under age 16.
Space Maintainers
Limited to non-orthodontic treatment for children under age 19.
Inlays, Crowns, Bridges, Dentures and Partials
Replacement every 60 months if unserviceable and cannot be repaired. Benefits are based on
the amount payable for non-precious metals. No porcelain or white/tooth-colored material on
molar crowns or bridges.
Denture and Bridge Repairs
Reviewed if more than once.
Denture Relines, Rebases and Adjustments
Covered if more than 6 months after installation.
Prost hesis Over Implant
1 every 60 months if unserviceable and cannot be repaired. Benefits are based on the amount
payable for non-precious metals. No porcelain or white/tooth colored material on molar
crowns or bridges.
Benefit Exclusions:
Covered Expenses will not include, and no payment will be made for the following:
Procedures and services not included in the list of covered dental expenses;
Diagnostic: cone beam imaging;
Preventive Services: instruction for plaque control, oral hygiene and diet;
Restorative: veneers of porcelain, ceramic, resin, or acrylic materials on crowns or pontics on or replacing the upper and or lower first, second
and/or third molars;
Periodontics: bite regist rations; splinting;
Prosthodontic: precision or semi-precision attachments;

43
877-780-HISD (4473).
Procedures, appliances or restorations, except full dentures, whose main purpose is to change vertical dimension, diagnose or treat conditions of
dysfunction of the temporomandibular joint (TMJ), stabilize periodontally involved teeth or restore occlusion;
At hlet ic mout h guards;
Services performed primarily for cosmetic reasons;
Personalization or decoration of any dental device or dental work;
Replacement of an appliance per benefit guidelines;
Services that are deemed to be medical in nature;
Services and supplies received from a hospital;
Drugs: prescript io n drugs;
Charges in excess of the Maximum Reimbursable Charge.
This document provides a summary only. It is not a contract. If there are any differences between this summary and the official plan documents, the
terms of t he official plan documents will prevail.
Product availability may vary by location and plan type and is subject to change. All group dental insurance policies and den tal benefit plans contain
exclusions and limitations. For costs and details of coverage, review your plan documents or contact a Cigna representative.
All Cigna products and services are provided exclusively by or through operating subsidiaries of Cigna Corporation, including Cigna Health and Life
Insurance Company (CHLIC), Connecticut General Life Insurance Company, and Cigna Dental Health, Inc.
© 2021 Cigna / version 10122021

44
hisdbenefits.org
830527n 06/21
Oered by: Cigna Health and Life Insurance Company,
Connecticut General Life Insurance Company, or their aliates.
Cigna Dental
Oral Health
Integration
Program
®
Improved health
starts with the
mouth
Are you making
the most of your
dental benefits?
A Cigna Dental Health Connect
®
solution

45
877-780-HISD (4473).
What dental services are covered under the Cigna Dental Oral Health Integration
Program?:
1
How to enroll?
To get reimbursed, you first have to enroll in the
Cigna Dental Oral Health Integration Program by either:
›
Going to myCigna.com, selecting Coverage > Dental
and filling out the registration form online
›
Calling the number on the back of your Cigna ID card
and asking for a mailed registration form
What is the reimbursement process?
1. Go to your dentist and pay the copay or coinsurance for
the covered treatment.
2. If your dentist is in the Cigna network, they’ll send us a
claim for reimbursement. If your dentist isn’t in the Cigna
network, you might need to submit the claim.**
3. We’ll review the claim and mail reimbursements for eligible
dental services in about 30 days.
What is the Cigna Dental Oral Health
Integration Program?
It’s a program that reimburses out-of-pocket costs for
preventive dental treatments to combat dental issues such
as gum disease and tooth decay. The program is for people
with certain medical conditions with a higher risk of oral
health issues. There’s no additional cost for the Oral Health
Integration Program – if you qualify, you get reimbursed.*
Friendly customer support
Get guidance on everything from overcoming dental-related
anxiety to understanding the impact of tobacco.
Who qualifies?
If you have a Cigna dental plan, you’re eligible for the
program. You do NOT have to be enrolled in a Cigna
medical plan to be eligible for this program. You must be
treated by a doctor for any of the following conditions:
›
Heart disease
›
Stroke
›
Diabetes
›
Maternity
›
Chronic kidney
disease
›
Organ
transplants
›
Radiation for
head or neck
cancers
›
Rheumatoid
arthritis
›
Sjogren's
syndrome
›
Lupus
›
Parkinson’s
disease
›
Amyotrophic
lateral sclerosis
(ALS)
›
Huntington’s
disease
›
Opioid misuse
and addiction
Condition
Heart
disease
Stroke Diabetes Maternity
Chronic
kidney
disease
Organ
transplants
Radiation
for head or
neck cancers
Rheumatoid
arthritis
Sjogren's
syndrome
Lupus
Parkinson's
disease
ALS
Huntington's
disease
Opioid misuse
and addiction
Gum treatment
1,2
D4341 D4342 D4910
✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓
Gum evaluation
1,3
D0180
✓
Oral evaluation
1,3
D0120 D0140 D0150
✓ ✓
Cleaning
1,4
D1110
✓
Deep cleaning and plaque
removal
1,4
D4346
✓
Emergency pain relief
treatment
1,5
D9110
✓
Fluoride and
fluoride varnish
1,6
D1206
✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓
Fluoride
(no varnish)
1,6
D1208
✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓
Sealants
6
D1351
✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓
Sealant repair
6
D1353
✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓
Interim caries
arresting medicament
application D1354
✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓
Caries preventive
medicament
application D1355
✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓
1. Eligibility, reimbursement and coverage for eligible services are subject to plan year maximums. 2. Two additional treatments per year than the plan covers. 3. One additional
evaluation. 4. One additional cleaning. 5. Unlimited visits. 6. Open to all ages, but plan limits apply.
The Cigna Dental Oral Health Integration Program may not be available under your specific plan. Reimbursement under OHIP is subject to plan terms and conditions, including applicable annual
benefit maximums and other exclusions and limitations. For costs and details of coverage, contact your Cigna representative or see your plan documents.
All Cigna products and services are provided exclusively by or through operating subsidiaries of Cigna Corporation, including Cigna Health and Life Insurance Company (CHLIC), Connecticut
General Life Insurance Company (CGLIC), Cigna HealthCare of Connecticut, Inc., Tel-Drug, Inc., Tel-Drug of Pennsylvania, L.L.C., and Cigna Dental Health, Inc. and its subsidiaries, including Cigna
Dental Health Plan of Arizona, Inc., Cigna Dental Health of California, Inc., Cigna Dental Health of Colorado, Inc., Cigna Dental Health of Delaware, Inc., Cigna Dental Health of Florida, Inc., a
Prepaid Limited Health Services Organization licensed under Chapter 636, Florida Statutes, Cigna Dental Health of Kansas, Inc., Cigna Dental Health of Kentucky, Inc., Cigna Dental Health of
Maryland, Inc., Cigna Dental Health of Missouri, Inc., Cigna Dental Health of New Jersey, Inc., Cigna Dental Health of North Carolina, Inc., Cigna Dental Health of Ohio, Inc., Cigna Dental Health of
Pennsylvania, Inc., Cigna Dental Health of Texas, Inc., and Cigna Dental Health of Virginia, Inc. In Texas, the insured dental plan is known as Cigna Dental Choice, and this plan uses the national
Cigna DPPO network. "Cigna Home Delivery Pharmacy" refers to Tel-Drug, Inc. and Tel-Drug of Pennsylvania, L.L.C. Policy forms: OK – Indemnity/DPPO: HP-POL99 (CHLIC) and GM6000 ELI288 et
al (CGLIC), DHMO: POL115 (CHLIC) and GM6000 DEN201V1 (CGLIC); TN – Indemnity/DPPO: HP-POL69/HC-CER2V1 et al, DHMO: HP-POL134/HC-CER17V1 et al (CHLIC). The Cigna name, logo, and other
Cigna marks are owned by Cigna Intellectual Property, Inc.
830527n 06/21 © 2021 Cigna. Some content provided under license.
* You do not have to meet your DPPO or indemnity deductible to receive reimbursement for these services. However, reimbursement will
apply to and is subject to your annual benefits maximum for traditional indemnity and DPPO plans as well as plan rules for visits to network
dentists and out-of-network dentists.
**The reimbursement for out-of-network services will also be subject to plan limitations for out-of-network care costs.
Questions?
Reach out to us 24/7 at
800.Cigna24 (800.244.6224).

46
hisdbenefits.org
cIGNA Discount dental
• Website: www.CignaPlusSavings.com
• Customer service: 1-877-521-0244
• You pay set fees for selected services and receive a discount for other services.
• You agree to use Cigna network providers for your care.
• You don’t pay deductibles, le claim forms or have restrictions for pre-existing conditions
or number of visits.
• is is not insurance.
Vision
• You may choose between Basic and Plus options.
• Both options have a retail frame allowance of $150.
• With both, you receive a 40 percent discount o a second pair of glasses at most participating
in-network providers.
• Both give you access to online ordering tools, including Glasses.com and ContactsDirect.com.
• Both options oer in- and out-of-network benets.
• ere’s a copay, but both options oer added coverage for progressive lenses and lens options,
including UV coating, tint, basic polycarbonate, and standard anti-reective lenses.
• Both cover an annual in-network eye exam for a $10 copay.
• Both cover eyeglass lenses or contacts every 12 months aer a set materials copay of $20 for
Basic and $10 for Plus.
• Vision Basic covers new frames every 24 months; Vision Plus covers new frames every 12 months.

47
877-780-HISD (4473).
eye med basic option
Version 7
Vision Care Services
Out-of-Network Reimbursement*
Exam with Dilation as Necessary $40
Retinal Imaging Benefit N/A
Exam Options:
Standard Contact Lens Fit and Follow-Up: N/A
Premium Contact Lens Fit and Follow-Up: N/A
Frames:
Any available frame at provider location
Standard Plastic Lenses
Single Vision $40
Bifocal $60
Trifocal $80
Lenticular $80
Standard Progressive Lens $60
Premium Progressive Lens $60
Lens Options:
UV Treatment
N/A
Tint (Solid and Gradient)
N/A
Standard Plastic Scratch Coating
$8
Standard Polycarbonate - Adults
N/A
Standard Polycarbonate - Kids under 19
N/A
Standard Anti-Reflective Coating
N/A
Polarized
N/A
Photocromatic / Transitions Plastic
N/A
Premium Anti-Reflective
N/A
Other Add-Ons
N/A
Contact Lenses
(Contact lens allowance includes materials only)
Conventional $125
Disposable $125
Medically Necessary $210
Laser Vision Correction
Lasik or PRK from U.S. Laser Network N/A
Frequency:
Examination
Lenses or Contact Lenses
Frame
Monthly Rate
Subscriber
Subscriber + Spouse
Subscriber + Child(ren)
Subscriber + Family
All plans are based on a 48-month contract term and 48-month rate guarantee.
Additional Discounts:
Member receives a 20% discount on items not covered by the plan at network Providers. Discount does not apply to EyeMed Provider's professional services, or contact lenses. Plan discounts cannot be
Members also receive 15% off retail price or 5% off promotional price for Lasik or PRK from the US Laser Network, owned and operated by LCA Vision.
After initial purchase, replacement contact lenses may be obtained via the Internet at substantial savings and mailed directly to the member. Details are available at www.eyemedvisioncare.com.
The contact lens benefit allowance is not applicable to this service.
Benefit Allowances provide no remaining balance for future use within the same Benefit Frequency.
Certain brand name Vision Materials in which the manufacturer imposes a no-discount practice.
Rates are valid only when the quoted plan is the sole stand-alone vision plan offered by the group
Rates are valid for groups domiciled in the State of TX.
Fees quoted will be valid until the 1/1/2021 plan implementation date. Date quoted: 2/21/2020.
Rates assume Employer contribution of 20% or less for employees and dependents
Insured Plans are underwritten by Fidelity Security Life Insurance Company of Kansas City, Missouri, except in New York
Policy number VC-19/VC-20, form number M-9083
Plan Exclusions:
1) Orthoptic or vision training, subnormal vision aids and any associated supplemental testing; Aniseikonic lenses; 2) Medical and/or surgical treatment of the eye, eyes or supporting structures;
3) Any eye or Vision Examination, or any corrective eyewear required by a Policyholder as a condition of employment; Safety eyewear
4) Services provided as a result of any Workers’ Compensation law, or similar legislation, or required by any governmental agency or program whether federal, state or subdivisions thereof;
5) Plano (non-prescription) lenses and/or contact lenses; 6) Non-prescription sunglasses; 7) Two pair of glasses in lieu of bifocals;
8) Services rendered after the date an Insured Person ceases to be covered under the Policy, except when Vision Materials ordered before coverage ended are delivered,
and the services rendered to the Insured Person are within 31 days from the date of such order; 9) Services or materials provided by any other group benefit plan providing vision care;
10) Lost or broken lenses, frames, glasses, or contact lenses will not be replaced except in the next Benefit Frequency when Vision Materials would next become available.
If Houston ISD has chosen this benefit design with the attached supplement, sign here:
Signature Date TC0
$10 Copay
$20 Copay
$20 Copay
Up to $39
$75
Members also receive a 40% discount off complete pair eyeglass purchases and a 15% discount
off conventional contact lenses once the funded benefit has been used.
Up to $40
$0 Copay
$45
combined with any other discounts or promotional offers. Services or materials provided by any other group benefit plan providing vision care may not be covered.
Once every 12 months
Once every 12 months
$3.66
$45
$0 Copay, Paid-in-Full
20% off Retail Price
$40
$7.23
$6.91
Houston ISD
EyeMed Insight Plan H, Fixed Fee
Voluntary
Option Base as is
Member Cost In-Network
Premium is subject to adjustment even during a rate guarantee period in the event of any of the following events: changes in benefits, employee contributions, the number of eligible employees, or the
imposition of any new taxes, fees or assessments by Federal or State regulatory agencies
$15
EyeMed Vision Care in conjunction with Fidelity Security Life Insurance Company
10% off Retail Price
15% off Retail Price or 5% off promotional price
$85 Copay
$20 Copay
Once every 24 months
20% off Retail Price
$15
$20 Copay
$0 Copay; $125 allowance, plus balance over $125
$0 Copay; $150 Allowance, 20% off balance over $150
See attached Fixed Premium Progressive price list
See attached Fixed Premium Anti-Reflective Coating list
$40
$0 Copay; $125 allowance, 15% off balance over $125
Amplifon Hearing Health Care
Hearing Health Care from Amplifon Hearing Health Care Network
Members receive a 40% discount off hearing exams and a low price guarantee on discounted
hearing aids.
N/A
* Member Reimbursement Out-of-Network will be the lesser of the listed amount or the member’s actual cost from the out-of-network provider. In certain states members may be required to pay the full retail rate and not
the negotiated discount rate with certain participating providers. Please see EyeMed’s online provider locator to determine which participating providers have agreed to the discounted rate
$13.51
Additional Pairs Benefit:
N/A
Member Cost In-Network
(Includes Lens Copay)
Standard Progressive
$85 Copay
Premium Progressives as Follows:
Tier 1
$105 Copay
Tier 2
$115 Copay
Tier 3
$130 Copay
Tier 4
$85 Copay, 80% of charge less $120 allowance
Member Cost In-Network
Standard Anti-Reflective Coating
$45
Premium Anti-Reflective Coatings as Follows:
Tier 1
$57
Tier 2
$68
Tier 3
80% of charge
Member Cost In-Network
Photochromic (Plastic)
$75
Polarized
80% of charge
For a current listing of brands by tier, go to:
http://www.eyemedvisioncare.com/theme/pdf/microsite-template/eyemedlenslist.pdf
*Fixed pricing is reflective of brands at the listed product level. All providers are not required to carry all brands at all levels.
Houston ISD
Option Base as is
Progressive Price List*
Anti-Reflective Coating Price List*
Other Add-ons Price List
EyeMed Vision Care reserves the right to make changes to the products on each tier and the member out-of-pocket costs.
Supplement
cIGNA Discount dental
• Website: www.CignaPlusSavings.com
• Customer service: 1-877-521-0244
• You pay set fees for selected services and receive a discount for other services.
• You agree to use Cigna network providers for your care.
• You don’t pay deductibles, le claim forms or have restrictions for pre-existing conditions
or number of visits.
• is is not insurance.
• You may choose between Basic and Plus options.
• Both options have a retail frame allowance of $150.
• With both, you receive a 40 percent discount o a second pair of glasses at most participating
in-network providers.
• Both give you access to online ordering tools, including Glasses.com and ContactsDirect.com.
• Both options oer in- and out-of-network benets.
• ere’s a copay, but both options oer added coverage for progressive lenses and lens options,
including UV coating, tint, basic polycarbonate, and standard anti-reective lenses.
• Both cover an annual in-network eye exam for a $10 copay.
• Both cover eyeglass lenses or contacts every 12 months aer a set materials copay of $20 for
Basic and $10 for Plus.
• Vision Basic covers new frames every 24 months; Vision Plus covers new frames every 12 months.

48
hisdbenefits.org
Version 7
Vision Care Services
Out-of-Network Reimbursement*
Exam with Dilation as Necessary $40
Retinal Imaging Benefit N/A
Exam Options:
Standard Contact Lens Fit and Follow-Up: N/A
Premium Contact Lens Fit and Follow-Up: N/A
Frames:
Any available frame at provider location
Standard Plastic Lenses
Single Vision $40
Bifocal $60
Trifocal $80
Lenticular $80
Standard Progressive Lens $60
Premium Progressive Lens $60
Lens Options:
UV Treatment
N/A
Tint (Solid and Gradient)
N/A
Standard Plastic Scratch Coating
$8
Standard Polycarbonate - Adults
N/A
Standard Polycarbonate - Kids under 19
N/A
Standard Anti-Reflective Coating
N/A
Polarized
N/A
Photocromatic / Transitions Plastic
N/A
Premium Anti-Reflective
N/A
Other Add-Ons
N/A
Contact Lenses
(Contact lens allowance includes materials only)
Conventional $125
Disposable $125
Medically Necessary $210
Laser Vision Correction
Lasik or PRK from U.S. Laser Network N/A
Frequency:
Examination
Lenses or Contact Lenses
Frame
Monthly Rate
Subscriber
Subscriber + Spouse
Subscriber + Child(ren)
Subscriber + Family
All plans are based on a 48-month contract term and 48-month rate guarantee.
Additional Discounts:
Member receives a 20% discount on items not covered by the plan at network Providers. Discount does not apply to EyeMed Provider's professional services, or contact lenses. Plan discounts cannot be
Members also receive 15% off retail price or 5% off promotional price for Lasik or PRK from the US Laser Network, owned and operated by LCA Vision.
After initial purchase, replacement contact lenses may be obtained via the Internet at substantial savings and mailed directly to the member. Details are available at www.eyemedvisioncare.com.
The contact lens benefit allowance is not applicable to this service.
Benefit Allowances provide no remaining balance for future use within the same Benefit Frequency.
Certain brand name Vision Materials in which the manufacturer imposes a no-discount practice.
Rates are valid only when the quoted plan is the sole stand-alone vision plan offered by the group
Rates are valid for groups domiciled in the State of TX.
Fees quoted will be valid until the 1/1/2021 plan implementation date. Date quoted: 2/21/2020.
Rates assume Employer contribution of 20% or less for employees and dependents
Insured Plans are underwritten by Fidelity Security Life Insurance Company of Kansas City, Missouri, except in New York
Policy number VC-19/VC-20, form number M-9083
Plan Exclusions:
1) Orthoptic or vision training, subnormal vision aids and any associated supplemental testing; Aniseikonic lenses; 2) Medical and/or surgical treatment of the eye, eyes or supporting structures;
3) Any eye or Vision Examination, or any corrective eyewear required by a Policyholder as a condition of employment; Safety eyewear
4) Services provided as a result of any Workers’ Compensation law, or similar legislation, or required by any governmental agency or program whether federal, state or subdivisions thereof;
5) Plano (non-prescription) lenses and/or contact lenses; 6) Non-prescription sunglasses; 7) Two pair of glasses in lieu of bifocals;
8) Services rendered after the date an Insured Person ceases to be covered under the Policy, except when Vision Materials ordered before coverage ended are delivered,
and the services rendered to the Insured Person are within 31 days from the date of such order; 9) Services or materials provided by any other group benefit plan providing vision care;
10) Lost or broken lenses, frames, glasses, or contact lenses will not be replaced except in the next Benefit Frequency when Vision Materials would next become available.
If Houston ISD has chosen this benefit design with the attached supplement, sign here:
Signature Date TC0
$10 Copay
$10 Copay
$10 Copay
Up to $39
$75
Members also receive a 40% discount off complete pair eyeglass purchases and a 15% discount
off conventional contact lenses once the funded benefit has been used.
Up to $40
$0 Copay
$45
combined with any other discounts or promotional offers. Services or materials provided by any other group benefit plan providing vision care may not be covered.
Once every 12 months
Once every 12 months
$5.71
$45
$0 Copay, Paid-in-Full
20% off Retail Price
$40
$11.89
$11.33
Houston ISD
EyeMed Insight Plan H, Fixed Fee
Voluntary
Option Buyup as is
Member Cost In-Network
Premium is subject to adjustment even during a rate guarantee period in the event of any of the following events: changes in benefits, employee contributions, the number of eligible employees, or the
imposition of any new taxes, fees or assessments by Federal or State regulatory agencies
$15
EyeMed Vision Care in conjunction with Fidelity Security Life Insurance Company
10% off Retail Price
15% off Retail Price or 5% off promotional price
$75 Copay
$10 Copay
Once every 12 months
20% off Retail Price
$15
$10 Copay
$0 Copay; $125 allowance, plus balance over $125
$0 Copay; $150 Allowance, 20% off balance over $150
See attached Fixed Premium Progressive price list
See attached Fixed Premium Anti-Reflective Coating list
$40
$0 Copay; $125 allowance, 15% off balance over $125
Amplifon Hearing Health Care
Hearing Health Care from Amplifon Hearing Health Care Network
Members receive a 40% discount off hearing exams and a low price guarantee on discounted
hearing aids.
N/A
* Member Reimbursement Out-of-Network will be the lesser of the listed amount or the member’s actual cost from the out-of-network provider. In certain states members may be required to pay the full retail rate and not
the negotiated discount rate with certain participating providers. Please see EyeMed’s online provider locator to determine which participating providers have agreed to the discounted rate
$18.24
Additional Pairs Benefit:
N/A
Member Cost In-Network
(Includes Lens Copay)
Standard Progressive
$75 Copay
Premium Progressives as Follows:
Tier 1
$95 Copay
Tier 2
$105 Copay
Tier 3
$120 Copay
Tier 4
$75 Copay, 80% of charge less $120 allowance
Member Cost In-Network
Standard Anti-Reflective Coating
$45
Premium Anti-Reflective Coatings as Follows:
Tier 1
$57
Tier 2
$68
Tier 3
80% of charge
Member Cost In-Network
Photochromic (Plastic)
$75
Polarized
80% of charge
For a current listing of brands by tier, go to:
http://www.eyemedvisioncare.com/theme/pdf/microsite-template/eyemedlenslist.pdf
*Fixed pricing is reflective of brands at the listed product level. All providers are not required to carry all brands at all levels.
Houston ISD
Option Buyup as is
Progressive Price List*
Anti-Reflective Coating Price List*
Other Add-ons Price List
EyeMed Vision Care reserves the right to make changes to the products on each tier and the member out-of-pocket costs.
Supplement
eye med plus option

49
877-780-HISD (4473).
Life and Accidental Death and Dismemberment (AD&D)
HISD provides $10,000 each of life and AD&D coverage at no cost to all employees who are
eligible for benets. You may purchase supplemental life and a matching AD&D benet for
yourself. If you do, you may also add supplemental coverage for your spouse and/or
dependent child(ren).
During annual enrollment, employees are eligible for an enhancement to their life insurance
program. They are able to enroll or increase their life insurance benefit one times their annual salary
with no evidence of insurability up to five times their annual salary or $600,000, whichever comes
first. A micro-site will be available to answer questions and guide you through the process.
Supplemental life and matching AD&D for yourself
Coverage is available for up to eight times your annual base salary, up to a maximum of $1,000,000.
Guaranteed issue (no EOI required) up to ve times your annual salary or $600,000, whichever is less.*
*Try Benets Scout, which oers suggestions on how much life insurance you may need.
Visit HISDbenets.org to access.
Supplemental life and matching AD&D for your spouse
• Coverage is available at one to three times your salary, equal to your total supplemental
life coverage amount or $250,000, whichever is less. Guaranteed issue (no EOI required) or
$100,000, or your total supplemental life coverage amount, whichever is less.
• If your spouse also works for HISD, only one of you can be covered by supplemental or spouse
life and AD&D. If both parents work for HISD and are both eligible for HISD benets,
only one employee should cover their dependent child(ren)
consider your voluntary options

50
hisdbenefits.org
Child life and matching AD&D with options available at $5,000, $10,000, $15,000
or $20,000
A child may not be covered by more than one employee. You must designate or update your
beneciary online, and the actively at-work provision applies to all.
For elections under the guaranteed issue*, no EOI is required:
• If you or your spouse or your child enroll as a new employee or within 31 days of becoming eligible.
• When you increase existing coverage by one multiple of your salary
(i.e., 1x to 2x or 2x to 3x) during annual enrollment, if already enrolled
• When you elect or increase coverage by one multiple of your salary within 31 days
of a qualied status change (i.e., 1x to 2x or 2x to 3x).
Employee
1x, 2x, 3x, 4x, 5x, 6x, 7x, 8x annual base salary up to
$1 million
Spouse
1x, 2x, 3x your annual base salary up to amount of
employee supplemental life or $250,000, whichever
is less
Child(ren)
$5,000, $10,000, $15,000 or $20,000
According to the policy, all children are eligible from
live birth to the attainment of age 26. Grandchildren
are eligible up to age 25.*
Plan maximums
* Must meet eligibility requirements
consider your voluntary options

51
877-780-HISD (4473).
Disability
is plan pays up to a maximum monthly benet up to $8,000 after a set elimination
period if you are disabled and unable to work due to an injury, illness or pregnancy.
• You have a choice of elimination periods (30, 60, 90 or 180 days) before
benets begin, and you select the percentage of annual base salary
(40%, 50% or 66.67%) that you want to replace each month.
• No evidence of insurability is required to enroll or increase coverage.
• 3/12 pre-existing condition and actively at-work provisions apply.
• is benet is oset by any other sources of income.
3/12 pre-existing condition
Disability coverage only
New or increased disability coverage is subject to a 3/12 pre-existing condition exclusion. is means that if
you have a condition that was treated or medically advised in the three months before your coverage eective
date, you are not covered for that condition for the rst 12 months.
12-month pre-existing condition
Cancer and specied diseases coverage only
e plan doesn’t cover pre-existing conditions. A pre-existing condition is any sickness or loss for which medical
advice or treatment was received or recommended within 12 months prior to the eective date of coverage.
Actively at work
(Life and AD&D, disability, cancer and specied diseases, critical illness, hospital indemnity, and accident
coverage)
If you are not actively at work when coverage is scheduled to become eective, your coverage does not take
eect until you complete your rst day at work.
Accident, Cancer and Specied Diseases, Critical Illness, and Hospital Indemnity Insurance are underwritten
by Continental American Insurance Company (CAIC), a proud member of the Aac family. CAIC is not
licensed to solicit business in New York, Guam, Puerto Rico, or the Virgin Islands.
Important voluntary plan exclusions

52
hisdbenefits.org
2
1.
provide personal guidance to employees and former employees of companies providing PlanSmart’s Retirewise through MetLife.
2.
Legal Plans.
3. Does not cover DUI.
4.
Plan Features and Rates*
Our Legal Plan Plus Parents plan helps your employees and their parents navigate life’s twists and turns.
Services in bold
Money Matters
Financial Education Workshops
1
Identity Management Services
2
Identity Theft Defense
Personal Bankruptcy
Promissory Notes
Tax Audit Representation
Home & Real
Estate
Deeds
Eviction Defense
Foreclosure
Mortgages
Security Deposit Assistance
Tenant Negotiations
Zoning Applications
Estate Planning
Codicils
Complex Wills
Healthcare Proxies
Living Wills
Powers of Attorney
(Healthcare, Financial,
Childcare, Immigration)
Simple Wills
Family &
Personal
Adoption
Affidavits
Demand Letters
Garnishment Defense
Guardianship
Immigration Assistance
Personal Property Issues
Prenuptial Agreement
Protection from Domestic
Violence
Review of ANY Personal Legal
Document
School Hearings
Civil Lawsuits
Administrative Hearings
Incompetency Defense
Elder-Care
Issues
Consultation & Document Review
for Issues Related to Your
Parents:
Deeds
Leases
Medicaid
Medicare
Notes
Nursing Home Agreements
Powers of Attorney
Prescription Plans
Wills
Criminal Matters
Defense of Traffic Tickets
3
Driving Privileges Restoration
Defense
Felony Defense
License Suspension Due to DUI
Misdemeanor Defense
Repossession
Rate:
4
Price per month for employee
Legal Plan:
Covers spouse and
dependents
Proposed Plus Parents Buy Up Rate:
The option to add Plus Parents for an additional $6 per month
Covers spouse, dependents, employee’s and spouse’s parents
Single Rate $9.54 per month $9.54 per month + $6.00 per month = $15.54 per month
Famiy Rate $13.44 per month $13.44 per month + $6.00 per month = $19.44 per month
Additional Features:
Access to a digital estate planning solution for wills, living wills, power of attorney and living trusts.
Reduced Fees:
E-services:
®
Rate guarantees: Five years.
Usage reports: Usage reports, and analysis and evaluation of the reports.
Portability:
Personal legal plan
is plan provides personal legal guidance on a variety of issues and services such as will
preparation, trac ticket defense, and consumer matters. Issues related to your employment
are excluded.
2
1.
provide personal guidance to employees and former employees of companies providing PlanSmart’s Retirewise through MetLife.
2.
Legal Plans.
3. Does not cover DUI.
4.
Plan Features and Rates*
Our Legal Plan Plus Parents plan helps your employees and their parents navigate life’s twists and turns.
Services in bold
Money Matters
Financial Education Workshops
1
Identity Management Services
2
Identity Theft Defense
Personal Bankruptcy
Promissory Notes
Tax Audit Representation
Home & Real
Estate
Deeds
Eviction Defense
Foreclosure
Mortgages
Security Deposit Assistance
Tenant Negotiations
Zoning Applications
Estate Planning
Codicils
Complex Wills
Healthcare Proxies
Living Wills
Powers of Attorney
(Healthcare, Financial,
Childcare, Immigration)
Simple Wills
Family &
Personal
Adoption
Affidavits
Demand Letters
Garnishment Defense
Guardianship
Immigration Assistance
Personal Property Issues
Prenuptial Agreement
Protection from Domestic
Violence
Review of ANY Personal Legal
Document
School Hearings
Civil Lawsuits
Administrative Hearings
Incompetency Defense
Elder-Care
Issues
Consultation & Document Review
for Issues Related to Your
Parents:
Deeds
Leases
Medicaid
Medicare
Notes
Nursing Home Agreements
Powers of Attorney
Prescription Plans
Wills
Criminal Matters
Defense of Traffic Tickets
3
Driving Privileges Restoration
Defense
Felony Defense
License Suspension Due to DUI
Misdemeanor Defense
Repossession
Rate:
4
Price per month for employee
Legal Plan:
Covers spouse and
dependents
Proposed Plus Parents Buy Up Rate:
The option to add Plus Parents for an additional $6 per month
Covers spouse, dependents, employee’s and spouse’s parents
Single Rate $9.54 per month $9.54 per month + $6.00 per month = $15.54 per month
Famiy Rate $13.44 per month $13.44 per month + $6.00 per month = $19.44 per month
Additional Features:
Access to a digital estate planning solution for wills, living wills, power of attorney and living trusts.
Reduced Fees:
E-services:
®
Rate guarantees: Five years.
Usage reports: Usage reports, and analysis and evaluation of the reports.
Portability:

53
877-780-HISD (4473).

54
hisdbenefits.org

55
877-780-HISD (4473).

56
hisdbenefits.org

57
877-780-HISD (4473).

58
hisdbenefits.org

59
877-780-HISD (4473).
Q: I was diagnosed with COVID-19. Will Aac pay benets for the period of time I am
unable to work? Will I have to pay premiums during that time?
A:
You will need to look to your Disability coverage for help during this time
period. Aac’s plans oered at HISD do not specically address time o from work.
Q: I am in the hospital with COVID-19. Will Aac cover that?
A: Aac will pay benets under those circumstances if you have Aac’s Hospital
indemnity insurance .
Q: I have tested positive for COVID-19. My local hospital is at full capacity. ey have
created an alternative care site, and that is where I’m receiving my treatment. Will
Aac cover that?
A: Alternative care sites are occurring in many states, and we treat them like standard
hospitals if they provide hospital-level care and care in a hospital was not available.
Q: I need to be tested for COVID-19. Will Aac cover that?
A: Your test would be covered under the wellness /screening benet provided by the
Accident, Hospital, Cancer, and Critical Illness plans.
Q: What if I am unable to see a doctor in person, so I use telemedicine? Will Aac still
cover me?
A: Aac considers a telemedicine visit the same as an in-person visit to the doctor.
Q:
I haven’t tested positive for COVID-19. However, I possibly have been exposed to the
virus. My doctor thinks it is best that I remain in self-isolation or the government has
put me under quarantine. Will Aac pay benets while I’m staying home?
A: Not under these specic plans.
Please review the FAQs below for answers to your questions
concerning your Aflac benefits and COVID-19.
Covid-19 and your aflac benefits
Accident, Cancer and Specied Diseases, Critical Illness, and Hospital Indemnity Insurance are underwritten
by Continental American Insurance Company (CAIC), a proud member of the Aac family. CAIC is not
licensed to solicit business in New York, Guam, Puerto Rico, or the Virgin Islands.
is is a brief description of coverage and is not a contract. Read your certicate carefully for exact terms and
conditions. In Texas, Policy Forms HCP3000TX, HCP8500TX 09, CAI7700TX THCP, and C21100TX.

60
hisdbenefits.org
CANCER AND SPECIFIED DISEASES • HOSPITAL INDEMNITY • CRITICAL ILLNESS • ACCIDENT
Even a small trip to the hospital can have a major impact on your nances.
Here’s a way to help make your visit a little more aordable.
Aflac Group Insurance Plans
AFLAC GROUP CANCER PLAN
OPTION 1 OPTION 2
HOSPITAL CONFINEMENT (first continuous 30 days)
We will pay the amount shown for Hospital Confinement for the first continuous 30 days of hospital confinement due to
Internal Cancer. Benefit: Per Day / No Lifetime Limit
$200 $300
HOSPITAL CONFINEMENT (31st day and thereafter)
We will pay the amount shown after the 31st day for hospital confinement due to Internal Cancer. Benefit: Per Day / No
Lifetime Limit
$400 $600
SURGICAL BENEFIT
We will pay the amount shown in the Surgical Schedule section of the plan for surgery performed on an insured for a
diagnosed cancer. Benefits are payable for in or out of hospital surgery in accordance with the Surgical Schedule.
Benefit: Per Procedure / No Lifetime Limit on Number of Operations
$95 –
$3,000
$100 –
$5,000
SECOND SURGICAL OPINION
We will pay up to the amount shown for a second surgical opinion by a licensed physician, not a relative, concerning cancer
surgery for each positively diagnosed cancer. This benefit is payable once for each malignant condition. Not payable for
reconstructive surgery or skin cancer.
Benefit: Per Malignant Condition / No Lifetime Limit
$200 $250
FIRST OCCURRENCE BENEFIT
We will pay this benefit the first time the insured is diagnosed as having internal (not skin) cancer. This benefit is payable
only once for each insured and will be paid in addition to any other benefit in the plan. Internal cancer includes melanomas
classified as Clark’s Level III and higher. In addition to the pathological or clinical diagnosis required by the plan, we may
require additional information from the attending physician and hospital.
$1,500 $5,000
CANCER SCREENING/WELLNESS BENEFIT
For each insured, we will pay the actual incurred charges up to the amount shown for: · Bone Marrow Testing · Biopsy ·
Breast Ultrasound · CA 125 (blood test for ovarian cancer) · CA 15-3 (blood test for breast cancer) · CEA (blood test for
colon cancer) · Chest X-Ray · Colonoscopy · Flexible Sigmoidoscopy · Hemocult Stool Analysis · Mammography · Pap Smear
· PSA (blood test for prostate cancer) · Serum Protein Electrophoresis (blood test for myeloma) · Thermography
No Lifetime Limit
$50 $100
RADIATION AND CHEMOTHERAPY
We will pay up to the amount shown for each day the insured receives radioactive or chemical treatments prescribed by
a doctor for the destruction of abnormal tissue during the treatment of Cancer. For oral chemotherapy not requiring the
administration by medical personnel, we will pay the amount shown for each prescription not to exceed $800 a month for
Option I and $1,200 a month for Options II and III.
Benefit: Per Day / No Lifetime Limit
$200 $300
EXPERIMENTAL TREATMENT
We will pay the charges incurred, up to the amount shown, per day for an insured who receives experimental cancer
treatment for the purpose of modification or destruction of abnormal tissue. The treatments must be consistent with one or
more National Cancer Institute sponsored protocols.
This benefit does not pay for laboratory tests, diagnostic X-rays, immunoglobulins, immunotherapy, colony-stimulating
factors, and therapeutic devices or other procedures related to these therapy treatments.
Benefit: Per Day / No Lifetime Limit
$200 $300
SKIN CANCER SURGERY
We will pay the amount shown in the Surgical Schedule section of the Plan for surgery performed on an insured for a
diagnosed cancer. Benefits are payable for in or out of hospital surgery in accordance with the Surgical Schedule.
Benefit: Per Malignant Condition / No Lifetime Limit
$100 $600
IN-HOSPITAL BLOOD AND PLASMA
We will pay the amount shown for each day an insured receives blood or plasma during a covered hospital confinement.
Benefit: Per Day / No Lifetime Limit
$50 $100
Benefits Overview
AFLAC GROUP CANCER PLAN
Policy Form Number HCP3000TX

61
877-780-HISD (4473).
BOTH PLANS
NATIONAL CANCER CONSULTATION
We will pay up to the amount shown when consultation at an NCI-sponsored cancer center as a result of receiving a prior diagnosis of
internal cancer. The purpose of the evaluation/consultation must be to determine the appropriate course of cancer treatment. We will pay
$250 for the transportation and lodging of the covered person receiving the evaluation/consultation. The NCI-sponsored cancer center
must be more than 100 miles from the covered person's residence for the transportation and lodging portion of this benefit to be payable.
This benefit is payable once per insured.
No Lifetime Limit
$500
ANESTHESIA
We will pay 25% of the amount shown in the Surgical Schedule opposite the appropriate surgical procedure if the insured receives
anesthesia administered by an anesthesiologist or anesthetist during a surgical procedure which is performed for the treatment of cancer.
This benefit is not payable for reconstructive surgery.
Benefit: Per Procedure / No Lifetime Limit
25% of surgery
ANTI-NAUSEA MEDICATION
We will pay up to the amount shown for anti-nausea medication as a result of radiation/chemotherapy treatments and as prescribed by a
Physician. We will pay this benefit for no more than the number of days the insured receives treatment for radiation/chemotherapy.
Benefit: Per Month / No Lifetime Limit
$100
NURSING SERVICES
We will pay the amount shown per day for full-time nursing services (not performed by a relative) while hospitalized. Benefit: Per Day / No
Lifetime Limit
$100
HOME HEALTH CARE
We will pay charges incurred up to $50.00 per day for visits by a home health care agency. This benefit is limited to 30 visits per calendar
year.
Incurred
charges up
to $50 per
day
OPTION 1 OPTION 2
OUTPATIENT BLOOD AND PLASMA
We will pay up to the amount shown for each day an insured receives blood or plasma as an outpatient in a doctor’s
office, clinic, hospital, or ambulatory surgical center due to cancer.
Benefit: Per Day / No Lifetime Limit
$200 $250
PROSTHESIS/ARTIFICIAL LIMB
We will pay the amount shown for each prosthetic device or artificial limb surgically implanted which is prescribed as a
result of surgery for cancer treatment. Lifetime limit is benefit shown for each option per insured.
We will pay up to $200 for the charges incurred for prosthetic devices prescribed as a direct result of cancer treatment
that does not require surgical implantation. Lifetime limit $200 per insured.
Benefit: Per Device
Incurred
charges up
to:
$2,500
Incurred
charges up
to:
$3,000
TRANSPORTATION BENEFIT
We will pay the amount shown for the insured’s transportation to and from a hospital located outside a 100 mile radius of
their legal residence.
The insured must require special treatment for internal cancer which has been prescribed by the local attending physician
and which cannot be obtained locally.
This benefit will be paid only for the insured person for whom this special treatment is prescribed, unless the treatment is
for a dependent child, then the child’s parent or legal guardian who travels with the dependent child will also receive this
benefit (only one person will be paid to travel with such dependent child).
No Lifetime Limit
Automobile:
$0.40
per mile
up to $1,200
Airfare or other
commercial
travel:
up to
$1,200
round trip
Automobile:
$0.50
per mile
up to $1,500
Airfare or other
commercial
travel:
up to
$1,500
round trip
FAMILY MEMBER LODGING BENEFIT
We will pay the amount shown per day for each night’s lodging in a motel/hotel room for the insured or any one family
member when an insured person is confined to a hospital for internal cancer treatment. The hospital and motel/hotel
room must be more than 100 miles from the insured’s residence. The special cancer treatment must be prescribed by a
local physician.
Benefit: Per Day / Lifetime limit 60 days per covered person
$50 $60
BOTH PLANS
HOSPICE CARE
We will pay the amount shown for care provided by a hospice. The insured must be diagnosed with cancer and therapeutic intervention
directed toward the cure of the disease is medically determined to be no longer appropriate, and if medical prognosis indicates a life
expectancy of six months or less as a direct result of cancer.
Benefit: Per Day / Lifetime limit of $12,000 per insured
$100
per day/first
60 days
$50
per day
thereafter
EXTENDED CARE FACILITY
We will pay $100 per day when the insured person is confined to a section of the hospital used as an Extended Care Facility, a Skilled
Nurses Facility, or any bed designated as a swing bed. Confinement must follow hospitalization and the insured must be receiving benefit
under the Hospital Confinement Benefit. Limited to the same number of days the insured received Hospital Confinement Benefits.
Benefit: Per Day / Lifetime limit of 365 days per insured
$100
AMBULANCE
We will pay the amount shown if an insured requires transportation to a hospital, within 100 miles of the insured person’s residence,
for overnight confinement for cancer treatment. This benefit is limited to two (2) trips per confinement. This ambulance service must be
performed by a licensed professional ambulance company.
Benefit: Per Trip / No Lifetime Limit
Incurred
Charges
BONE MARROW TRANSPLANT
We will pay the charges incurred up to $10,000 for the harvesting and reinfusion of bone marrow if the insured requires a bone marrow
transplantation during a covered hospital confinement.
We will pay the charges incurred up to $5,000 for the harvesting and reinfusion of bone marrow performed on an outpatient basis.
We will pay an indemnity of $1,000 to the bone marrow donor for his or her expenses incurred as a result of the transplantation procedure.
Benefit: Per Procedure / No Lifetime Limit
Incurred
charges
up to:
$10,000
in-hospital
$5,000
outpatient
$1,000
donor
indemnity
STEM CELL TRANSPLANTATION
We will pay the charges incurred up to $2,500 if an insured receives a peripheral stem cell transplantation for the treatment of cancer.
This benefit is payable once per insured. This benefit is not payable in conjunction with the payment of the Bone Marrow Transplantation
Benefit.
Lifetime Maximum of $2,500 per insured
Incurred
charges up
to: $2,500
WAIVER OF PREMIUM
If the insured, due to having internal cancer, is completely unable to do all of the usual and customary duties of your occupation for a period of 90 continuous
days, we will waive, from month to month, any premiums falling due during your continued inability. For premiums to be waived, we will require an employer's
statement (if applicable) and a physician's statement of the insured’s inability to perform said duties or activities, and may each month thereafter require a
physician's statement that total inability continues.
SPECIFIED DISEASE BENEFIT
We will pay $200 per day for the first 30 days and $500 per day thereafter for hospital confinement when such confinement is due to the treatment of a
specified disease if: 1. the insured receives treatment for a specified disease beginning while the Certificate is in force; and 2. it is not excluded by name or
specific description.
Benefits will be paid from the first day of hospital confinement due to a specified disease. We will pay the daily amount regardless of whether the insured is
charged by the hospital for such confinement. If more than one specified disease is diagnosed at the same time then we will only pay the amount shown for
one disease but not both.
Covered Diseases Include: Addison’s disease, Amyotrophic Lateral Sclerosis (ALS), Cerebral palsy, Cerebrospinal Meningitis, Cystic fibrosis, Diphtheria,
Encephalitis, Huntington’s chorea, Legionnaires’ disease, Malaria, Meningitis (bacterial), Multiple sclerosis, Muscular dystrophy, Myasthenia gravis,
Necrotizing fasciitis, Osteomyelitis, Polio, Rabies, Scleroderma, Sickle cell anemia, Systemic lupus, Tetanus, Tuberculosis.
The lifetime maximum benefit payable under this benefit is $100,000 per insured.
OPTIONAL INTENSIVE CARE BENEFIT / $600 A DAY IN HOSPITAL Benefits will be paid if the insured is confined in a Hospital Intensive Care Unit (ICU).
This benefit is limited to 30 days per period of confinement.
Aflac Group Insurance Plans

62
hisdbenefits.org
BOTH PLANS
HOSPICE CARE
We will pay the amount shown for care provided by a hospice. The insured must be diagnosed with cancer and therapeutic intervention
directed toward the cure of the disease is medically determined to be no longer appropriate, and if medical prognosis indicates a life
expectancy of six months or less as a direct result of cancer.
Benefit: Per Day / Lifetime limit of $12,000 per insured
$100
per day/first
60 days
$50
per day
thereafter
EXTENDED CARE FACILITY
We will pay $100 per day when the insured person is confined to a section of the hospital used as an Extended Care Facility, a Skilled
Nurses Facility, or any bed designated as a swing bed. Confinement must follow hospitalization and the insured must be receiving benefit
under the Hospital Confinement Benefit. Limited to the same number of days the insured received Hospital Confinement Benefits.
Benefit: Per Day / Lifetime limit of 365 days per insured
$100
AMBULANCE
We will pay the amount shown if an insured requires transportation to a hospital, within 100 miles of the insured person’s residence,
for overnight confinement for cancer treatment. This benefit is limited to two (2) trips per confinement. This ambulance service must be
performed by a licensed professional ambulance company.
Benefit: Per Trip / No Lifetime Limit
Incurred
Charges
BONE MARROW TRANSPLANT
We will pay the charges incurred up to $10,000 for the harvesting and reinfusion of bone marrow if the insured requires a bone marrow
transplantation during a covered hospital confinement.
We will pay the charges incurred up to $5,000 for the harvesting and reinfusion of bone marrow performed on an outpatient basis.
We will pay an indemnity of $1,000 to the bone marrow donor for his or her expenses incurred as a result of the transplantation procedure.
Benefit: Per Procedure / No Lifetime Limit
Incurred
charges
up to:
$10,000
in-hospital
$5,000
outpatient
$1,000
donor
indemnity
STEM CELL TRANSPLANTATION
We will pay the charges incurred up to $2,500 if an insured receives a peripheral stem cell transplantation for the treatment of cancer.
This benefit is payable once per insured. This benefit is not payable in conjunction with the payment of the Bone Marrow Transplantation
Benefit.
Lifetime Maximum of $2,500 per insured
Incurred
charges up
to: $2,500
WAIVER OF PREMIUM
If the insured, due to having internal cancer, is completely unable to do all of the usual and customary duties of your occupation for a period of 90 continuous
days, we will waive, from month to month, any premiums falling due during your continued inability. For premiums to be waived, we will require an employer's
statement (if applicable) and a physician's statement of the insured’s inability to perform said duties or activities, and may each month thereafter require a
physician's statement that total inability continues.
SPECIFIED DISEASE BENEFIT
We will pay $200 per day for the first 30 days and $500 per day thereafter for hospital confinement when such confinement is due to the treatment of a
specified disease if: 1. the insured receives treatment for a specified disease beginning while the Certificate is in force; and 2. it is not excluded by name or
specific description.
Benefits will be paid from the first day of hospital confinement due to a specified disease. We will pay the daily amount regardless of whether the insured is
charged by the hospital for such confinement. If more than one specified disease is diagnosed at the same time then we will only pay the amount shown for
one disease but not both.
Covered Diseases Include: Addison’s disease, Amyotrophic Lateral Sclerosis (ALS), Cerebral palsy, Cerebrospinal Meningitis, Cystic fibrosis, Diphtheria,
Encephalitis, Huntington’s chorea, Legionnaires’ disease, Malaria, Meningitis (bacterial), Multiple sclerosis, Muscular dystrophy, Myasthenia gravis,
Necrotizing fasciitis, Osteomyelitis, Polio, Rabies, Scleroderma, Sickle cell anemia, Systemic lupus, Tetanus, Tuberculosis.
The lifetime maximum benefit payable under this benefit is $100,000 per insured.
OPTIONAL INTENSIVE CARE BENEFIT / $600 A DAY IN HOSPITAL Benefits will be paid if the insured is confined in a Hospital Intensive Care Unit (ICU).
This benefit is limited to 30 days per period of confinement.
AFLAC GROUP HOSPITAL INDEMNITY PLAN Policy Form Number HCP8500TX 09
HIGH LOW
HOSPITAL ADMISSION BENEFIT (once per confinement)
This benefit is paid when you are admitted to a hospital and confined as a resident bed patient because of injuries
received in a covered accident or because of a covered sickness. We will pay this benefit once for each covered
accident or covered sickness. Confinement must be within 6 months of a covered accident.
$500
per
confinement
$300
per
confinement
HOSPITAL CONFINEMENT BENEFIT (up to 365 days per confinement)
The amount indicated is paid for overnight hospital confinement. This benefit begins with the first day of confinement
and lasts up to 365 days. Confinement must be within 6 months of a covered accident.
$150
per day
$75
per day
HOSPITAL INTENSIVE CARE BENEFIT (365-day maximum for any one period of confinement)
The amount indicated is paid for overnight hospital intensive care unit confinement. The benefit begins the first day of
confinement and lasts up to 365 days. *Total daily benefit if confined to an Intensive Care Unit.
$300
per day
$150
per day
Benefits Overview
The plan has limitations and exclusions that may affect benefits payable. This brochure is for illustrative purposes only. Refer to the plan for complete details,
definitions, limitations, and exclusions.
WAIVER OF PREMIUM
If the insured, due to having internal cancer, is completely unable to do all of the usual and customary duties of your occupation for a period of 90 continuous
days, we will waive, from month to month, any premiums falling due during your continued inability. For premiums to be waived, we will require an employer's
statement (if applicable) and a physician's statement of the insured’s inability to perform said duties or activities, and may each month thereafter require a
physician's statement that total inability continues.
SPECIFIED DISEASE BENEFIT
We will pay $200 per day for the first 30 days and $500 per day thereafter for hospital confinement when such confinement is due to the treatment of a
specified disease if: 1. the insured receives treatment for a specified disease beginning while the Certificate is in force; and 2. it is not excluded by name or
specific description.
Benefits will be paid from the first day of hospital confinement due to a specified disease. We will pay the daily amount regardless of whether the insured is
charged by the hospital for such confinement. If more than one specified disease is diagnosed at the same time then we will only pay the amount shown for
one disease but not both.
Covered Diseases Include: Addison’s disease, Amyotrophic Lateral Sclerosis (ALS), Cerebral palsy, Cerebrospinal Meningitis, Cystic fibrosis, Diphtheria,
Encephalitis, Huntington’s chorea, Legionnaires’ disease, Malaria, Meningitis (bacterial), Multiple sclerosis, Muscular dystrophy, Myasthenia gravis,
Necrotizing fasciitis, Osteomyelitis, Polio, Rabies, Scleroderma, Sickle cell anemia, Systemic lupus, Tetanus, Tuberculosis.
The lifetime maximum benefit payable under this benefit is $100,000 per insured.
OPTIONAL INTENSIVE CARE BENEFIT / $600 A DAY IN HOSPITAL Benefits will be paid if the insured is confined in a Hospital Intensive Care Unit (ICU).
This benefit is limited to 30 days per period of confinement.
WELLNESS BENEFIT
We will pay the amount shown when a covered person visits a doctor and the covered person is neither injured nor
sick. This benefit is payable once per calendar year per covered person.
$100
per calendar
year
$50
per calendar
year
GROUP PREMIUM
Once enrolled in the program premiums will not increase because of age.
WAIVER OF PREMIUM
We will waive an insured’s premium after he or she is continuously confined to a hospital for 14 days. We will waive premium until he or she is discharged from
the hospital or for 12 months, whichever comes first. This benefit applies only to the insured employee, not spouse or children.
AFLAC GROUP HOSPITAL INDEMNITY
INSURANCE

63
877-780-HISD (4473).
AFLAC GROUP CRITICAL ILLNESS PLAN Policy Series C21100TX
COVERED CRITICAL ILLNESSES:
CANCER (Internal or Invasive) 100%
HEART ATTACK (Myocardial Infarction) 100%
STROKE (Ischemic or Hemorrhagic) 100%
KIDNEY FAILURE (End-Stage Renal Failure) 100%
BONE MARROW TRANSPLANT (Stem Cell Transplant) 100%
SUDDEN CARDIAC ARREST 100%
MAJOR ORGAN TRANSPLANT (25% of this benefit is payable for insureds placed on a transplant list for a major organ transplant) 100%
NON-INVASIVE CANCER 25%
CORONARY ARTERY BYPASS SURGERY 25%
INITIAL DIAGNOSIS
We will pay a lump sum benefit upon initial diagnosis of a covered critical illness when such diagnoses is caused by or solely
attributed to an underlying disease. Cancer diagnoses are subject to the cancer diagnosis limitation. Benefits will be based on
the face amount in effect on the critical illness date of diagnosis.
ADDITIONAL DIAGNOSIS
We will pay benefits for each different critical illness after the first when the two dates of diagnoses are separated by at least 6
consecutive months. Cancer diagnoses are subject to the cancer diagnosis limitation.
REOCCURRENCE
We will pay benefits for the same critical illness after the first when the two dates of diagnoses are separated by at least 6
consecutive months. Cancer diagnoses are subject to the cancer diagnosis limitation.
CHILD COVERAGE AT NO ADDITIONAL COST
Each dependent child is covered at 50 percent of the primary insured’s benefit amount at no additional charge. Children-only
coverage is not available.
SKIN CANCER BENEFIT
We will pay $250 for the diagnosis of skin cancer. We will pay this benefit once per calendar year.
WAIVER OF PREMIUM
If you become totally disabled due to a covered critical illness prior to age 65, after 90 continuous days of total disability, we
will waive premiums for you and any of your covered dependents. As long as you remain totally disabled, premiums will be
waived up to 24 months, subject to the terms of the plan.
SUCCESSOR INSURED BENEFIT
If spouse coverage is in force at the time of the primary insured’s death, the surviving spouse may elect to continue coverage.
Coverage would continue at the existing spouse face amount and would also include any dependent child coverage in force at
the time.
HEALTH SCREENING BENEFIT
You may receive a maximum of $100 High Option or $50 Low Option for health screening tests performed while an insured’s
coverage is in force. We will pay this benefit once per calendar year.
This benefit is only payable for health screening tests performed as the result of preventive care, including tests and diagnostic
procedures ordered in connection with routine examinations. This benefit is payable for the covered employee, spouse and
dependent children.
AFLAC GROUP CRITICAL ILLNESS
INSURANCE
AFLAC GROUP HOSPITAL INDEMNITY PLAN Policy Form Number HCP8500TX 09
HIGH LOW
HOSPITAL ADMISSION BENEFIT (once per confinement)
This benefit is paid when you are admitted to a hospital and confined as a resident bed patient because of injuries
received in a covered accident or because of a covered sickness. We will pay this benefit once for each covered
accident or covered sickness. Confinement must be within 6 months of a covered accident.
$500
per
confinement
$300
per
confinement
HOSPITAL CONFINEMENT BENEFIT (up to 365 days per confinement)
The amount indicated is paid for overnight hospital confinement. This benefit begins with the first day of confinement
and lasts up to 365 days. Confinement must be within 6 months of a covered accident.
$150
per day
$75
per day
HOSPITAL INTENSIVE CARE BENEFIT (365-day maximum for any one period of confinement)
The amount indicated is paid for overnight hospital intensive care unit confinement. The benefit begins the first day of
confinement and lasts up to 365 days. *Total daily benefit if confined to an Intensive Care Unit.
$300
per day
$150
per day
Benefits Overview
The plan has limitations and exclusions that may affect benefits payable. This brochure is for illustrative purposes only. Refer to the plan for complete details,
definitions, limitations, and exclusions.
WAIVER OF PREMIUM
If the insured, due to having internal cancer, is completely unable to do all of the usual and customary duties of your occupation for a period of 90 continuous
days, we will waive, from month to month, any premiums falling due during your continued inability. For premiums to be waived, we will require an employer's
statement (if applicable) and a physician's statement of the insured’s inability to perform said duties or activities, and may each month thereafter require a
physician's statement that total inability continues.
SPECIFIED DISEASE BENEFIT
We will pay $200 per day for the first 30 days and $500 per day thereafter for hospital confinement when such confinement is due to the treatment of a
specified disease if: 1. the insured receives treatment for a specified disease beginning while the Certificate is in force; and 2. it is not excluded by name or
specific description.
Benefits will be paid from the first day of hospital confinement due to a specified disease. We will pay the daily amount regardless of whether the insured is
charged by the hospital for such confinement. If more than one specified disease is diagnosed at the same time then we will only pay the amount shown for
one disease but not both.
Covered Diseases Include: Addison’s disease, Amyotrophic Lateral Sclerosis (ALS), Cerebral palsy, Cerebrospinal Meningitis, Cystic fibrosis, Diphtheria,
Encephalitis, Huntington’s chorea, Legionnaires’ disease, Malaria, Meningitis (bacterial), Multiple sclerosis, Muscular dystrophy, Myasthenia gravis,
Necrotizing fasciitis, Osteomyelitis, Polio, Rabies, Scleroderma, Sickle cell anemia, Systemic lupus, Tetanus, Tuberculosis.
The lifetime maximum benefit payable under this benefit is $100,000 per insured.
OPTIONAL INTENSIVE CARE BENEFIT / $600 A DAY IN HOSPITAL Benefits will be paid if the insured is confined in a Hospital Intensive Care Unit (ICU).
This benefit is limited to 30 days per period of confinement.
WELLNESS BENEFIT
We will pay the amount shown when a covered person visits a doctor and the covered person is neither injured nor
sick. This benefit is payable once per calendar year per covered person.
$100
per calendar
year
$50
per calendar
year
GROUP PREMIUM
Once enrolled in the program premiums will not increase because of age.
WAIVER OF PREMIUM
We will waive an insured’s premium after he or she is continuously confined to a hospital for 14 days. We will waive premium until he or she is discharged from
the hospital or for 12 months, whichever comes first. This benefit applies only to the insured employee, not spouse or children.

64
hisdbenefits.org
• 24-Hour Coverage.
• No limit on the number of claims.
• Supplements and pays regardless of any other insurance programs.
• Benefits available for spouse and/or dependent children.
• Benefits for both inpatient and outpatient treatment of covered accidents.
• Guaranteed Issue - No underwriting required to qualify for coverage.
• Waiver of Premium
AC CIDENTA L DE AT H AND DISM EMBERMENT
HIGH LOW
Accidental Common Carrier Death (Plane, Train, Boat or Ship)
$100,000 $50,000
Accidental Death
$50,000 $25,000
Catastrophic Accident
$100,000 $50,000
Loss of hand, foot, or sight-single loss
$6,250 $3,125
Loss of hand, foot, or sight-double loss
$25,000 $12,500
Loss of one or more ngers or toes
$1,250 $625
Partial Amputation of nger(s) or toe(s) including at least one joint
$100 $100
HOS PITA L BENEFITS
HIGH LOW
Paralysis
$5,000-$10,000 $2,500-$5,000
Hospital Admission
$1,500 $750
Hospital Intensive Care (per day)
$600 $300
Hospital Connement (per day)
$300 $150
Medical Fees
$250 $125
SPECIFIC INJ URIES
HIGH LOW
Burns
$180-$18,000 $180-$18,000
Lacerations
$25-$200 $25-$100
Ruptured Disc
$100-$400 $100-$400
Tendons/Ligaments
$400-$600 $400-$600
Torn Knee Cartilage
$100-$400 $100-$400
Eye Injuries
$250 $125
Coma
$10,000 $5,000
Concussion
$200 $100
Emergency Dental Work
$50-$150 $25-$100
AFLAC GROUP ACCIDENT ADVANTAGE PLUS INSURANCE
GROUP ACCIDENTAL INJURY INSURANCE – 24-HOUR PLAN
OPTIONAL BENEFITS RIDER
Percentage of
Face Amount
BENIGN BRAIN TUMOR 100%
ADVANCED ALZHEIMER’S DISEASE 25%
ADVANCED PARKINSON’S DISEASE 25%
These benefits will be paid based on the face amount in effect on the critical illness date of diagnosis. We will pay the optional
benefit if the insured is diagnosed with one of the conditions listed in the rider schedule if the date of diagnosis is while the
rider is in force.
PROGRESSIVE DISEASES RIDER
AMYOTROPHIC LATERAL SCLEROSIS (ALS or Lou Gehrig’s Disease) 25%
SUSTAINED MULTIPLE SCLEROSIS 25%
This benefit is paid based on your selected Progressive Disease Benefit amount. We will pay the benefit shown upon
diagnosis of one of the covered diseases if the date of diagnosis is while the rider is in force.
SPECIFIED DISEASES RIDER
HUMAN CORONAVIRUS SPECIFIED DISEASE BENEFIT
We will pay the benefit if an insured is diagnosed with Human Coronavirus and if the date of diagnosis is
while the rider is in force.
In order to receive a benefit for Human Coronavirus, the insured must be confined to a Hospital or
confined to a Hospital Intensive Care Unit for the minimum number of days shown. Only the highest
eligible benefit amount shown will be payable under these benefits. In the event a lower benefit amount
was previously paid under these benefits for any period of Hospital Confinement and that confinement
is extended or the insured is moved to an Intensive Care Unit triggering a higher payment, the difference
between the previous paid benefit amount and the new benefit amount will be provided.
Payment of all benefits contained in the rider is subject to the Critical Illness Benefit provisions. The
benefits contained in the rider are considered to be Critical Illnesses.
Hospitalization:
4 or more days
10%
Hospitalization:
10 or more days
25%
Hospitalization:
ICU 40%
ADDITIONAL SPECIFIED DISEASES BENEFITS
We will pay the benefit an insured is diagnosed with one of the diseases listed if the date of diagnosis is
while the rider is in force.
Payment of benefits contained in the rider is subject to the Critical Illness benefit provisions. The
benefits contained in the rider are considered to be Critical Illnesses.
Addison’s Disease, Cerebrospinal Meningitis, Cerebral Palsy, Cystic Fibrosis, Encephalitis, Diphtheria,
Huntington’s Chorea, Legionnaire’s Disease, Malaria, Muscular Dystrophy, Myasthenia Gravis,
Necrotizing Fasciitis, Osteomyelitis, Poliomyelitis (Polio), Rabies, Sickle Cell Anemia, Systemic Lupus,
Systemic Sclerosis (Scleroderma), Tetanus, Tuberculosis
25%
HIGH LOW
HOSPITAL ADMISSION
We will pay this benefit when you are admitted to a hospital and confined as a resident bed patient because of
injuries received in a covered accident within six months of the date of the accident. We will pay this benefit once
per calendar year. We will not pay this benefit for confinement to an observation unit, or for emergency room
treatment or outpatient treatment.
$1,500 $750
HOSPITAL CONFINEMENT (per day)
We will provide this benefit on the first day of hospital confinement for up to 365 days when you are confined to a
hospital due to a covered accident. Hospital confinement must begin within 90 days from the date of the accident.
$300 $150
HOSPITAL INTENSIVE CARE (per day)
We will pay this benefit for up to 30 days if you are injured in a covered accident and the injury causes you to be
confined to a hospital intensive care unit. This benefit is payable in addition to the Hospital Confinement Benefit.
$600 $300
MEDICAL FEES (for each accident)
If you are injured in a covered accident and receive treatment within one year after the accident, we will pay up
to the maximum benefit amount for physician charges, emergency room services, supplies, and X-rays. Initial
treatment must be received within 60 days after the accident.
$250 for
employee/
spouse
$125
children
$125 for
employee/
spouse
$62.50
children
PARALYSIS (lasting 90 days or more and diagnosed by a physician within 90 days)
Quadriplegia
Paraplegia
$10,000
$5,000
$5,000
$2,500
Paralysis means the permanent loss of movement of two or more limbs. If you are injured in a covered accident
and the injury causes paralysis which lasts more than 90 days and is diagnosed by a physician within 90 days after
the accident, we will pay the appropriate amount shown. The amount paid will be based on the number of limbs
paralyzed.
If this benefit is paid and you later die as a result of the same covered accident, we will pay the appropriate Death
Benefit, less any amounts paid under the Paralysis Benefit.
AFLAC GROUP ACCIDENT ADVANTAGE PLUS INSURANCE
GROUP ACCIDENTAL INJURY INSURANCE – 24-HOUR PLAN
Policy Series CAI7700TX THCP
FEATURES:
• 24-Hour Coverage.
• No limit on the number of claims.
• Supplements and pays regardless of any other insurance programs.
• Benefits available for spouse and/or dependent children.
• Benefits for both inpatient and outpatient treatment of covered accidents.
• Guaranteed Issue - No underwriting required to qualify for coverage.
• Waiver of Premium
Benefits Overview
65
877-780-HISD (4473).
ACCIDENTAL DEATH AND DISMEMBERMENT
HIGH LOW
Accidental Common Carrier Death (Plane, Train, Boat or Ship)
$100,000
employee
$100,000
spouse
$50,000
child
$50,000
employee
$50,000
spouse
$10,000
child
Accidental Death
$50,000
employee
$50,000
spouse
$10,000
child
$25,000
employee
$25,000
spouse
$5,000
child
Loss of hand, foot, or sight-single loss
$6,250
employee
$6,250
spouse
$1,250
child
$3,125
employee
$3,125
spouse
$625
child
Loss of hand, foot, or sight-double loss
$25,000
employee
$25,000
spouse
$5,000
child
$12,500
employee
$12,500
spouse
$2,500
child
Loss of one or more fingers or toes
$1,250
employee
$1,250
spouse
$250
child
$625
employee
$625
spouse
$125
child
Partial Amputation of finger(s) or toe(s) including at least one joint $100 $100
Dismemberment - If you are injured in a covered accident and the injury causes loss of a hand, foot or sight within 90 days after the accident, we will pay
the amount shown.
If a covered accident causes you to lose one hand, foot or the sight of one eye, we will pay the single loss dismemberment benefit shown. If you lose both
hands, feet, the sight of both eyes, or a combination of any two, we will pay the Double Dismemberment Benefit shown.
If you lose one or more fingers or toes in a covered accident, we will pay the finger/toe benefit shown.
Dismemberment means loss of a hand: the hand is cut off at or above the wrist joint; or loss of a foot: the foot is cut off at or above the ankle; or loss of
sight: at least 80% of the vision in one eye is lost. Such loss of sight must be permanent and irrecoverable or loss of a finger/toe: the finger or toe is cut off at or
above the joint where it is attached to the hand or foot.
If you do not qualify for the Dismemberment Benefit but lose at least one joint of a finger or toe, we will pay the Partial Dismemberment Benefit.
If this benefit is paid and you later die as a result of the same covered accident, we will pay the appropriate Accidental-Death Benefit less any amounts paid
under this benefit.
* If you are injured in a covered accident and the injury causes death within 90 days after the accident, we will pay the Accidental-Death Benefit shown. If the
Accidental-Death Benefit is paid, we will not pay the Accidental Common Carrier Death Benefit.
If you are injured in a covered accident as a result of traveling as a fare-paying passenger on a common carrier and the injury causes death days after the ac-
cident, we will pay the Accidental Common Carrier Death Benefit in the amount shown.
Common carrier means an airline carrier which is licensed by the United States Federal Aviation Administration and operated by a licensed pilot on a
regular schedule between established airports; or a railroad train which is licensed and operated for passenger service only; or a boat or ship which is licensed
for passenger service and operated on a regular schedule between established ports.
If the Accidental Common Carrier Death Benefit is paid, we will not pay the Accidental-Death Benefit.
Accidental injury means bodily injury caused solely by or as the result of a covered accident.
Covered accident means an accident that occurs on or after the effective date, while the certificate is in force, and that is not specifically excluded.
CATASTROPHIC ACCIDENT RIDER HIGH LOW
We will pay the applicable amount shown at the end of the Catastrophic Accident Elimination Period if any insured: (1)
sustains a Catastrophic Loss as the result of a covered accident; (2) is under the appropriate care of a physician during the
Catastrophic Accident Elimination Period; and (3) Remains alive at the end of the Catastrophic Accident Elimination Period.
Benefit payable after 365-day elimination period. Benefit reduces by 50% at age 65.
$100,000
employee
$100,000
spouse
$50,000
child
$50,000
employee
$50,000
spouse
$25,000
child
HIGH LOW
HOSPITAL ADMISSION
We will pay this benefit when you are admitted to a hospital and confined as a resident bed patient because of
injuries received in a covered accident within six months of the date of the accident. We will pay this benefit once
per calendar year. We will not pay this benefit for confinement to an observation unit, or for emergency room
treatment or outpatient treatment.
$1,500 $750
HOSPITAL CONFINEMENT (per day)
We will provide this benefit on the first day of hospital confinement for up to 365 days when you are confined to a
hospital due to a covered accident. Hospital confinement must begin within 90 days from the date of the accident.
$300 $150
HOSPITAL INTENSIVE CARE (per day)
We will pay this benefit for up to 30 days if you are injured in a covered accident and the injury causes you to be
confined to a hospital intensive care unit. This benefit is payable in addition to the Hospital Confinement Benefit.
$600 $300
MEDICAL FEES (for each accident)
If you are injured in a covered accident and receive treatment within one year after the accident, we will pay up
to the maximum benefit amount for physician charges, emergency room services, supplies, and X-rays. Initial
treatment must be received within 60 days after the accident.
$250 for
employee/
spouse
$125
children
$125 for
employee/
spouse
$62.50
children
PARALYSIS (lasting 90 days or more and diagnosed by a physician within 90 days)
Quadriplegia
Paraplegia
$10,000
$5,000
$5,000
$2,500
Paralysis means the permanent loss of movement of two or more limbs. If you are injured in a covered accident
and the injury causes paralysis which lasts more than 90 days and is diagnosed by a physician within 90 days after
the accident, we will pay the appropriate amount shown. The amount paid will be based on the number of limbs
paralyzed.
If this benefit is paid and you later die as a result of the same covered accident, we will pay the appropriate Death
Benefit, less any amounts paid under the Paralysis Benefit.
AFLAC GROUP ACCIDENT ADVANTAGE PLUS INSURANCE
GROUP ACCIDENTAL INJURY INSURANCE – 24-HOUR PLAN
Policy Series CAI7700TX THCP
FEATURES:
• 24-Hour Coverage.
• No limit on the number of claims.
• Supplements and pays regardless of any other insurance programs.
• Benefits available for spouse and/or dependent children.
• Benefits for both inpatient and outpatient treatment of covered accidents.
• Guaranteed Issue - No underwriting required to qualify for coverage.
• Waiver of Premium
Benefits Overview

66
hisdbenefits.org
• A fracture is a break in the bone which
can be seen by X-ray. If you fracture
a bone in a covered accident, and it is
diagnosed and treated by a doctor, we
will pay the appropriate amount shown.
• Dislocation means a completely
separated joint. If you dislocate a joint in
a covered accident, and it is diagnosed
and treated by a doctor within 90 days
after the accident, we will pay the
amount shown.
• We will pay no more than 150% of the
benefit amount for the bone fracture or
dislocated joint which has the higher
dollar value. If you fracture a bone and
dislocate a joint, we will pay for both,
but no more than 150% of the benefit
amount for the bone fractured or joint
dislocated that has the higher dollar
value.
• Open reduction is paid at 150%
of closed reduction. Fracture and
Dislocation benefits amounts are for
open reduction. See certificate schedule
for closed reduction amounts.
• A chip facture is a piece of bone which is
completely broken off near a joint. Chip
fractures are paid at 10% of the benefit
shown.
• Partial dislocations are paid at 25% of
the dislocation benefit.
MAJOR INJURIES / FRACTURES / OPEN REDUCTION
HIGH LOW
Hip/Thigh
$6,750 $3,750
Vertebrae (except processes)
$6,075 $3,375
Pelvis
$5,400 $3,000
Skull (depressed)
$5,063 $2,813
Leg
$4,050 $2,250
Forearm / Hand / Wrist / Foot / Ankle / Knee cap
$3,375 $1,875
Shoulder blade / Collar bone / Lower Jaw (Mandible)
$2,700 $1,500
Skull (Simple) / Upper Arm / Upper Jaw
$2,363 $1,313
Facial bones (except teeth)
$2,050 $1,125
Vertebral Processes
$1,350 $750
Coccyx/Rib/Finger/Toe
$540 $300
ACCIDENTAL DEATH AND DISMEMBERMENT
HIGH LOW
Accidental Common Carrier Death (Plane, Train, Boat or Ship)
$100,000
employee
$100,000
spouse
$50,000
child
$50,000
employee
$50,000
spouse
$10,000
child
Accidental Death
$50,000
employee
$50,000
spouse
$10,000
child
$25,000
employee
$25,000
spouse
$5,000
child
Loss of hand, foot, or sight-single loss
$6,250
employee
$6,250
spouse
$1,250
child
$3,125
employee
$3,125
spouse
$625
child
Loss of hand, foot, or sight-double loss
$25,000
employee
$25,000
spouse
$5,000
child
$12,500
employee
$12,500
spouse
$2,500
child
Loss of one or more fingers or toes
$1,250
employee
$1,250
spouse
$250
child
$625
employee
$625
spouse
$125
child
Partial Amputation of finger(s) or toe(s) including at least one joint $100 $100
MAJOR INJURIES / DISLOCATIONS / OPEN REDUCTION
HIGH LOW
Hip
$4,050 $2,025
Knee (not knee cap)
$2,925 $1,462.50
Shoulder
$2,250 $1,125
Foot/Ankle
$1,800 $900
Hand
$1,575 $787.50
Lower Jaw
$1,350 $675
Wrist
$1,125 $562.50
Elbow
$900 $450
Finger/Toe
$360 $180
RUPTURED DISC (treatment within 60 days; surgical repair within one year)
Injury occurring during first certificate year $100 $100
Injury occurring after first certificate year $400 $400
TENDONS/LIGAMENTS (within 60 days; surgical repair within 90 days)
If you tear, sever, or rupture a tendon or ligament in a covered accident, receive treatment from a doctor within 60 days, and
have surgical repair within 90 days after the accident, we will pay the appropriate amount shown. The amount paid will be
based on the number (single or multiple) of tendons or ligaments repaired.
If you fracture a bone or dislocate a joint in addition to tearing, severing, or rupturing a tendon or ligament,
we will only pay one benefit. We will pay the largest of the fracture, dislocation, tendon, or ligament benefits.
$600
(Multiple)
$400
(Single)
$600
(Multiple)
$400
(Single)
TORN KNEE CARTILAGE (treatment within 60 days; surgical repair within one year)
Injury occurring during first certificate year
$100 $250
Injury occurring after first certificate year
$400 $400
EYE INJURIES
Treatment and surgical repair within 90 days
$250 $125
Removal of foreign body, with or without anesthesia
$50 $25
CONCUSSION (a head injury resulting in electroencephalogram abnormality)
$400 $200
COMA (a state of profound unconsciousness lasting more than 30 days)
$10,000 $5,000
EMERGENCY DENTAL (injury to sound natural teeth)
Repaired with crown
$150 $100
Resulting in extraction
$50 $25
CATASTROPHIC ACCIDENT RIDER HIGH LOW
We will pay the applicable amount shown at the end of the Catastrophic Accident Elimination Period if any insured: (1)
sustains a Catastrophic Loss as the result of a covered accident; (2) is under the appropriate care of a physician during the
Catastrophic Accident Elimination Period; and (3) Remains alive at the end of the Catastrophic Accident Elimination Period.
Benefit payable after 365-day elimination period. Benefit reduces by 50% at age 65.
$100,000
employee
$100,000
spouse
$50,000
child
$50,000
employee
$50,000
spouse
$25,000
child
ACCIDENTAL DEATH AND DISMEMBERMENT
HIGH LOW
Accidental Common Carrier Death (Plane, Train, Boat or Ship)
$100,000
employee
$100,000
spouse
$50,000
child
$50,000
employee
$50,000
spouse
$10,000
child
Accidental Death
$50,000
employee
$50,000
spouse
$10,000
child
$25,000
employee
$25,000
spouse
$5,000
child
Loss of hand, foot, or sight-single loss
$6,250
employee
$6,250
spouse
$1,250
child
$3,125
employee
$3,125
spouse
$625
child
Loss of hand, foot, or sight-double loss
$25,000
employee
$25,000
spouse
$5,000
child
$12,500
employee
$12,500
spouse
$2,500
child
Loss of one or more fingers or toes
$1,250
employee
$1,250
spouse
$250
child
$625
employee
$625
spouse
$125
child
Partial Amputation of finger(s) or toe(s) including at least one joint $100 $100
Dismemberment - If you are injured in a covered accident and the injury causes loss of a hand, foot or sight within 90 days after the accident, we will pay
the amount shown.
If a covered accident causes you to lose one hand, foot or the sight of one eye, we will pay the single loss dismemberment benefit shown. If you lose both
hands, feet, the sight of both eyes, or a combination of any two, we will pay the Double Dismemberment Benefit shown.
If you lose one or more fingers or toes in a covered accident, we will pay the finger/toe benefit shown.
Dismemberment means loss of a hand: the hand is cut off at or above the wrist joint; or loss of a foot: the foot is cut off at or above the ankle; or loss of
sight: at least 80% of the vision in one eye is lost. Such loss of sight must be permanent and irrecoverable or loss of a finger/toe: the finger or toe is cut off at or
above the joint where it is attached to the hand or foot.
If you do not qualify for the Dismemberment Benefit but lose at least one joint of a finger or toe, we will pay the Partial Dismemberment Benefit.
If this benefit is paid and you later die as a result of the same covered accident, we will pay the appropriate Accidental-Death Benefit less any amounts paid
under this benefit.
* If you are injured in a covered accident and the injury causes death within 90 days after the accident, we will pay the Accidental-Death Benefit shown. If the
Accidental-Death Benefit is paid, we will not pay the Accidental Common Carrier Death Benefit.
If you are injured in a covered accident as a result of traveling as a fare-paying passenger on a common carrier and the injury causes death days after the ac-
cident, we will pay the Accidental Common Carrier Death Benefit in the amount shown.
Common carrier means an airline carrier which is licensed by the United States Federal Aviation Administration and operated by a licensed pilot on a
regular schedule between established airports; or a railroad train which is licensed and operated for passenger service only; or a boat or ship which is licensed
for passenger service and operated on a regular schedule between established ports.
If the Accidental Common Carrier Death Benefit is paid, we will not pay the Accidental-Death Benefit.
Accidental injury means bodily injury caused solely by or as the result of a covered accident.
Covered accident means an accident that occurs on or after the effective date, while the certificate is in force, and that is not specifically excluded.
CATASTROPHIC ACCIDENT RIDER HIGH LOW
We will pay the applicable amount shown at the end of the Catastrophic Accident Elimination Period if any insured: (1)
sustains a Catastrophic Loss as the result of a covered accident; (2) is under the appropriate care of a physician during the
Catastrophic Accident Elimination Period; and (3) Remains alive at the end of the Catastrophic Accident Elimination Period.
Benefit payable after 365-day elimination period. Benefit reduces by 50% at age 65.
$100,000
employee
$100,000
spouse
$50,000
child
$50,000
employee
$50,000
spouse
$25,000
child
BURNS (treatment within 72 hours and based on percent of body surface burned / First-degree burns are not covered.)
Second-Degree Burns
Less than 10% $180 $180
At least 10%, but less than 25% $360 $360
At least 25%, but less than 35% $900 $900
35% or more $1,800 $1,800
Third-Degree Burns
Less than 10% $900 $900
At least 10%, but less than 25% $5,400 $5,400
At least 25%, but less than 35% $12,600 $12,600
35% or more $18,000 $18,000
LACERATIONS (treatment and repair within 72 hours)
2" to 5" long
$200 $100
Lacerations not requiring stitches
$25 $25
Multiple Lacerations: We will pay for the largest single laceration requiring stitches.
WELLNESS BENEFIT (per 12-month period)
While coverage is in force, we will pay this benefit for preventive testing once each 12-month period. Benefits include and are
payable for annual physical exams, mammograms, Pap smears, eye examinations, immunizations, flexible sigmoidoscopies,
PSA tests, ultrasounds, and blood screenings.
$100
$50
AMBULANCE
AIR AMBULANCE
If you require transportation to a hospital by a professional ambulance or air ambulance service within 90 days after a
covered accident, we will pay the amount shown.
$500
$1,500
$250
$750
BLOOD/PLASMA
If you receive blood or plasma within 90 days following a covered accident, we will pay the amount shown.
$400
$200
APPLIANCES
We will pay this benefit when you are advised by a physician to use a medical appliance due to injuries received in a covered
accident. Benefits are payable for crutches, wheelchairs, leg braces, back braces, and walkers.
$100
$50
INTERNAL INJURIES
We will pay this benefit if you have internal injuries as the result of a covered accident which results in open abdominal or
thoracic surgery.
$1,200
$750
ACCIDENT FOLLOW-UP TREATMENT (maximum 6 visits)
We will pay this benefit for up to six treatments per covered accident, per insured for follow-up treatment. The insured must
have received initial treatment within 72 hours of the accident, and the follow-up treatment must begin within 30 days of
the covered accident or discharge from the hospital. This benefit is not payable for the same visit that the Physical Therapy
Benefit is paid.
$50
$35
EXPLORATORY SURGERY (e.g., arthroscopy)
We will pay the amount shown in if a covered accident causes you to have exploratory surgery (without repair). The
exploratory surgery must be required as the result of an injury.
$400
$200
PROSTHESIS
If you require the use of a prosthetic device due to injuries received in a covered accident, we will pay this benefit. Hearing
aids, wigs, or dental aids, including but not limited to false teeth, are not covered.
$1,000
$500

67
877-780-HISD (4473).
BURNS (treatment within 72 hours and based on percent of body surface burned / First-degree burns are not covered.)
Second-Degree Burns
Less than 10% $180 $180
At least 10%, but less than 25% $360 $360
At least 25%, but less than 35% $900 $900
35% or more $1,800 $1,800
Third-Degree Burns
Less than 10% $900 $900
At least 10%, but less than 25% $5,400 $5,400
At least 25%, but less than 35% $12,600 $12,600
35% or more $18,000 $18,000
LACERATIONS (treatment and repair within 72 hours)
2" to 5" long
$200 $100
Lacerations not requiring stitches
$25 $25
Multiple Lacerations: We will pay for the largest single laceration requiring stitches.
WELLNESS BENEFIT (per 12-month period)
While coverage is in force, we will pay this benefit for preventive testing once each 12-month period. Benefits include and are
payable for annual physical exams, mammograms, Pap smears, eye examinations, immunizations, flexible sigmoidoscopies,
PSA tests, ultrasounds, and blood screenings.
$100
$50
AMBULANCE
AIR AMBULANCE
If you require transportation to a hospital by a professional ambulance or air ambulance service within 90 days after a
covered accident, we will pay the amount shown.
$500
$1,500
$250
$750
BLOOD/PLASMA
If you receive blood or plasma within 90 days following a covered accident, we will pay the amount shown.
$400
$200
APPLIANCES
We will pay this benefit when you are advised by a physician to use a medical appliance due to injuries received in a covered
accident. Benefits are payable for crutches, wheelchairs, leg braces, back braces, and walkers.
$100
$50
INTERNAL INJURIES
We will pay this benefit if you have internal injuries as the result of a covered accident which results in open abdominal or
thoracic surgery.
$1,200
$750
ACCIDENT FOLLOW-UP TREATMENT (maximum 6 visits)
We will pay this benefit for up to six treatments per covered accident, per insured for follow-up treatment. The insured must
have received initial treatment within 72 hours of the accident, and the follow-up treatment must begin within 30 days of
the covered accident or discharge from the hospital. This benefit is not payable for the same visit that the Physical Therapy
Benefit is paid.
$50
$35
EXPLORATORY SURGERY (e.g., arthroscopy)
We will pay the amount shown in if a covered accident causes you to have exploratory surgery (without repair). The
exploratory surgery must be required as the result of an injury.
$400
$200
PROSTHESIS
If you require the use of a prosthetic device due to injuries received in a covered accident, we will pay this benefit. Hearing
aids, wigs, or dental aids, including but not limited to false teeth, are not covered.
$1,000
$500
BURNS (treatment within 72 hours and based on percent of body surface burned / First-degree burns are not covered.)
Second-Degree Burns
Less than 10% $180 $180
At least 10%, but less than 25% $360 $360
At least 25%, but less than 35% $900 $900
35% or more $1,800 $1,800
Third-Degree Burns
Less than 10% $900 $900
At least 10%, but less than 25% $5,400 $5,400
At least 25%, but less than 35% $12,600 $12,600
35% or more $18,000 $18,000
LACERATIONS (treatment and repair within 72 hours)
2" to 5" long
$200 $100
Lacerations not requiring stitches
$25 $25
Multiple Lacerations: We will pay for the largest single laceration requiring stitches.
PHYSICAL THERAPY (maximum 6 visits)
We will pay this benefit for up to six treatments per covered accident, per insured for treatment from a physical therapist. The
insured must have received initial treatment within 72 hours of the accident, and physical therapy must begin within 30 days
of the covered accident or discharge from the hospital. Treatment must take place within six months after the accident. This
benefit is not payable for the same visit that the Accident Follow-Up Treatment Benefit is paid.
$75
$50
TRANSPORTATION
If hospital treatment or diagnostic study is recommended by your physician and is not available in your city of residence, we
will pay the amount shown. Transportation must begin within 90 days from the date of the covered accident.
The distance to the hospital must be greater than 50 miles from your residence.
$300
(train/plane)
$300
(bus)
$150
(train/plane)
$150
(bus)
FAMILY LODGING BENEFIT (per night)
If you are required to travel more than 100 miles from your home for inpatient treatment of injuries received in a covered
accident, we will pay this benefit for an immediate adult family member’s lodging. Benefits are payable up to 30 days per
accident and only while you are confined to the hospital. The treatment must be prescribed by your local physician.
$100 $50
MAJOR DIAGNOSTIC TESTING
If a covered person requires one of the following exams for Injuries sustained in a covered accident and a charge is incurred,
we will pay the amount shown for the following exams: CT (computerized tomography) scan; MRI (magnetic resonance
imaging); or EEG (electroencephalogram).
These exams must be performed in a Hospital, a Physician's office, or an Ambulatory Surgical Center. The Insured must
incur a charge for the exam. This benefit is limited to one payment per calendar year, per covered person. No lifetime
maximum.
$400 $200
REHABILITATION UNIT
We will pay this benefit when a covered person is confined in a Hospital and is transferred to a bed in a Rehabilitation Unit
of a Hospital for a covered Injury for each day you are charged for a room. This benefit is limited to 30 days for each Insured
per Period of Confinement and is limited to a calendar year maximum of 60 days. No lifetime maximum. Limitation - The
Hospital Confinement benefit and the Rehabilitation Unit benefit will not be paid on the same day; only the highest eligible
benefit will be paid.
$150
per day
$75
per day

68
hisdbenefits.org
GO ONLINE AND MAKE IT OFFICIAL
Online enrollment made easy
Once you’ve studied your options and made your selections, it’s time to let us know about them.
Here’s how you get there.
1. Log into myHISD.
2. Click the Benets heart icon. is takes you to HISDBenets.org.
3. Click Enrollment at the top of the page.
4. Click Enroll Now on the le-hand side and then follow the instructions.
REMINDER
Don’t miss the deadline. Online enrollment ends at 12:00 p.m. CT
and phone enrollment ends at 7:00 p.m. CT on November 18, 2022.
ANNUAL ENROLLMENT DATES
November 1-18, 2022
enroll for coverage

69
877-780-HISD (4473).
For New Employees
If you’re a new employee, look for your benets enrollment email from the HISD Benets Oce
following the date that you are entered in the HISD HR system. You must enroll within 30 days of your
hire date or you will need to wait until the next Annual Enrollment period or until you experience a
qualifying life event. Aer you successfully enroll, you will receive a conrmation notice.
If you are a new hire in August, you will need to enroll for Benets as new hire and then also
participate in annual enrollment and enroll again to ensure that you have the benets you want for
the new year whether you want to change anything or not. is is required since you will have two
concurrent events happening at the same time.
Dependent Verification
It’s important you understand who can and can’t be considered a dependent on your plan.
Documentation is required to support the eligibility status of each of your dependents. If you don’t
provide it, your dependents will not be covered, regardless of their eligibility, and you won’t be able to
add them until the next enrollment period or in the case of a life event. For more information about
dependent eligibility, see HISDBenets.org.
When do benefits begin?
If you are a new employee, a rehire outside of 31 days or newly eligible, your benets coverage begins
on your benets eective date, which is the rst of the month following 30 days after your new
employee date of hire or transfer date for the newly eligible, as long as you select benets before your
benets eective date or the date you become eligible for benets. For example, if you start work or
become benets eligible on February 12, your benets begin April 1, as long as you select your benets
before April 1. For benets selected during the annual enrollment period, coverage begins January 1 of
the following year. For benets requiring evidence of insurability, coverage begins the beginning of the
month following carrier approval of your application. If you are in an Aordable CareAct stability
period, your benets eective date could start sooner.

70
hisdbenefits.org
Your HISD medical plan includes benets, programs, and services that can help you and your
family live healthier lives and save money. Get to know what’s available and take advantage of
them to reach your wellness goals.
Preventive care covered at 100%
Routine preventive care is one of the keys to good health. Even if you are in the best shape
of your life, a serious condition with no symptoms could put your health at risk. By getting
preventive care, you and your doctor can catch problems early and prevent certain conditions altogether.
HISD follows the American Medical Association’s guidelines for preventive care. ey dene
preventive care as services provided when you do not have any symptoms and have not been
diagnosed with a health issue connected with a preventive service. Examples are screening
mammograms, prostate exams, and colonoscopies. Preventive care that meets the AMA’s guidelines
is covered at 100%.
If your doctor determines that you have a health issue, any additional screenings and tests after your
diagnosis are not considered preventive. ese services are covered at the appropriate coinsurance
once you have met the deductible.
wellness resources
71
877-780-HISD (4473).
See how HISD HELPS KEEP CARE
ACCESSIBLE & AFFORDABLE
1
2
Free medical care at HISD Employee Health & Wellness Centers
If you are enrolled in a HISD medical plan, you and your covered dependents ages 5 and up pay
nothing for your medical care at the HISD Employee Health & Wellness Centers. If you are eligible
for benets but not enrolled in an HISD medical plan, you can still use the centers for
$65 per visit plus any applicable lab fees.
With two onsite locations, the centers provide a great alternative to high-cost
emergency centers or urgent care facilities for low-cost, non-emergency services, including:
a Preventive care and limited chronic conditions
a Limited immunizations (for example; Flu, Tetanus)
a Acute and urgent care for infections, minor burns, and more
Please note: e centers do not have x-ray services. X-rays are available at the
16 Next Level centers.
In addition to these onsite clinics, medical plan members and their covered dependents can visit one
of the 16 Next Level centers under contract with HISD for a at fee of $20. Kelsey Select ACO Plan
members and covered dependents can access these centers at no cost.
Savings on lab work with Quest and LabCorp
You can save big on lab services with Quest Diagnostics and LabCorp, Aetna’s
preferred national labs. Here’s how:
a If your doctor is collecting your sample in the oce, ask that it be sent to a Quest or
LabCorp lab.
a If your doctor is sending you to a lab for the testing, ask for a lab requisition for Quest
or LabCorp lab.
a Please remember, if you are in the Kelsey- Seybold plans, you cannot use Quest Labs; you must
use the lab facility in the Kelsey clinics (LabCorp)
It’s easy to nd a lab near you. Just log in to Aetna.com and click “Find Care & Pricing” on the home
page. Register rst if you have not already. Or you can call Aetna Member Services at
877-224-6857. You can save on wait time and schedule an appointment ahead of time by
visiting QuestDiagnostics.com or LabCorp.com.

72
hisdbenefits.org
HISD Employee
HEALTH & WELLNESS CENTERs
by
HISD Health and Wellness Centers operated by Next Level Urgent Care.
care close to where they work. Walk-in patients are welcome, but we recommend booking an appointment on the
Next Level app or by calling 281-869-3630.
• Urgent Care
• Sports Physicals
• Headaches
• Rashes
• Sprains & Strains
• Lacerations
• Urinary Tract Infections
• Labs
• Flu Shots
• Wellness Physicals
• INTERIM CARE
Convenient medical care
for employees and
covered dependents
PERSONAL, HIGH-QUALITY MEDICAL CARE
HISD Employee Health & Wellness Centers are here for most of your
day-to-day healthcare and wellness
exams. Even better, if you are enrolled in an
includes care for your covered dependents, age 5 and older.
HISD medical plan, you can still use the centers for just $65-$125 per visit,
plus any additional lab fees.
Both centers ARE OPEN DURING THE MIDDAY LUNCH hour
4400 West 18th Street, Houston, Texas 77092
281-869-3630
Monday-Friday
: 9:00 a.m. to 4:30 p.m.
Saturday: 8:00 a.m. to 1:00 p.m.
Hattie Mae White
Educational Support Center
4330 Bellfort Street, Houston, Texas 77051
281-869-3630
Monday-Friday
: 9:00 a.m. to 4:30 p.m.
Attucks
Middle School
www.nextlevelurgentcare.com/onsite-clinic
TO MAKE AN APPOINTMENT ONLINE:
Get the Next Level App
Click the menu in upper left corner
Click “Schedule Appointment”
Select HISD clinic and follow instructions
www.nextlevelurgentcare.com/onsite-clinic
Click the link where it says "Onsite Member? Click Here."
This will bring you to the Next Level Client Login page.
Log in using the following:
Username: HISD
Password: Nextlevel
NOTE: The centers do not treat workers’ compensation injuries.
hisdbenefitshisdbenefits
houstonisdbenefits

73
877-780-HISD (4473).
HISD
URGENT CARE SERVICES
16 locations to serve you
Open until 9 P.M. | 7 DAYS A WEEK!
Common Conditions We Treat
Ear infections • Cold/flu
Cough/Sore throat • Minor burns
Lacerations • Rash/skin infections
Sprains • broken bones
Dehydration • STDs
No cost to Select
Plan members
$20 for members
enrolled in an
HISD medical plan
Dehydration • STDs
3 ways to get in line
Call 281-783-8162
for a list of locations or to Get in line online: nextlevelurgentcare.com
Text “NLUCAPP” to 313131 to download the app
We also take walk-ins!

74
hisdbenefits.org
Health and Wellness Programs and Services
Your 2023 medical plan also includes these no-cost programs and services:
Try the Aetna Maternity Program for a healthier pregnancy and healthy baby. is program
provides personal support from a trained OB/GYN nurse to help you make choices for a healthy
pregnancy, lower your risk for early labor, cope with postpartum depression, and even stop smoking.
Your secure member website at Aetna.com
Your secure member website is your one stop for benets and health information, tools, and
wellness resources. Log in to check on a claim payment, nd network providers, get
started with your member discounts, and much more. You can also take a Health
Assessment to learn more about your current state of health, any risk factors, and steps
you can take to avoid health problems and live well.
If you are already registered with Aetna.com, you can use your current login. If you are not
registered with the site or you are new to Aetna, you can register and create your login once you’re
an enrolled member. Just visit Aetna.com and click Individuals>Login>
Don’t Have an Account?>Register.
You can also get the Aetna Health app to use the best features of the site wherever you go. Look for
network providers, nd an urgent care center, make a doctor’s appointment, get cost estimates, and
more. You can download the app at the App Store or Google Play.
wellness resources

75
877-780-HISD (4473).

76
hisdbenefits.org

77
877-780-HISD (4473).
e Informed Health® Line is a 24/7 service that puts you in touch with a nurse who can answer
questions and provide information on a wide variety of health-related topics. Learn more about a
medical diagnosis. Ask about the latest tests and treatments. Get help with a non-emergency
problem until you can see a doctor.

78
hisdbenefits.org
Able To is a condential program that lets you talk by phone with a therapist twice a week. e program
is designed to provide help with issues such as grief and loss, depression and anxiety, caregiver stress,
dealing with a new or continuing health condition, cancer recovery, and more.
79
877-780-HISD (4473).

80
hisdbenefits.org
Member discounts save you and your family money on health-related products and services. As an
Aetna member, you will be able to take advantage of special rates on vision and hearing care, tness mem-
berships and equipment, health coaching, natural products and services, oral health products, and more.
Fitness discounts
A little help reaching your best health
No stopping you
Every time you take the stairs, eat a healthy snack or kick
a bad habit, your body gets stronger. Now here’s some
motivation to keep up the good work: good savings.
With your Aetna
®
plan, you get discounts on gym
memberships, health coaching and much more
through LifeMart
®
.
Built-in plan discounts with
no referrals, claims or limits.
Your family can use them, too.
aetna.com
45.03.915.1 (12/18)

81
877-780-HISD (4473).
Healthy lifestyle discounts
Save on gym memberships, health coaching, fitness gear
and nutrition products that support a healthy lifestyle.
You also save on:
• Wearables
• Yoga, meditation and wellness programs
• Group fitness on demand
Even more savings
If you’d like to work toward your fitness goals at home,
you’ll love these savings.
One-on-one health coaching
Get support to lose weight, ease stress and more.
Online group fitness sessions
Try a class on your schedule, in private, with online,
on-demand fitness sessions.
At-home weight-loss programs
Get weight-loss tips and menus and track progress
from the privacy of your home.
How to get started
Log in to aetna.com and look
for the “Stay Healthy” tab.
You’ll find discounts on fitness
and much more.
Through our partnership with LifeMart, you can also save on thousands of products and services including health and
wellness products, tickets, car rentals and coupons.
LifeMart is a registered trademark of LifeCare, Inc.
THIS IS NOT INSURANCE. THIS IS A DISCOUNT PROGRAM ONLY.
Aetna is the brand name used for products and services provided by one or more of the Aetna group of
subsidiary companies. Health benefits and health insurance plans are offered, administered and/or
underwritten by Aetna Health Inc., Aetna Health Insurance Company of New York, Aetna Health Insurance
Company, Aetna HealthAssurance Pennsylvania Inc. and/or Aetna Life Insurance Company (Aetna). In Florida,
by Aetna Health Inc. and/or Aetna Life Insurance Company. In Utah and Wyoming, by Aetna Health of Utah
Inc. and Aetna Life Insurance Company. In Maryland, by Aetna Health Inc., 151 Farmington Avenue, Hartford,
CT 06156. Each insurer has sole financial responsibility for its own products.
This material is for information only. Discount offers are available to people who have health benefits plans that are
issued, administered or serviced by Aetna or our affiliates. Discount offers provide access to discounted services and are
not part of an insured plan or policy. Discount offers are rate-access offers and may be in addition to any plan benefits.
Check any insurance benefits you have before using these discount offers, as those benefits may result in lower costs to
you than using these discounts. Discount offers are not guaranteed and may be discontinued at any time. Aetna makes
no payment to the discount vendor. You are responsible for the full cost of the discounted services. Aetna does not
endorse any vendor, product or service associated with these discount offers. Vendors are independent of Aetna, not
agents or employees. Programs, products and services may not be available at all times. Certain offers may not be
available in some states. Products may be subject to a warranty from the manufacturer. Aetna makes no representations
or warranties, and disclaims all product warranties. Aetna has no liability for providing or guaranteeing service and
assumes no liability for the quality of service rendered. Aetna may receive a percentage of the fee paid to a discount
vendor. Information is believed to be accurate as of the production date; however, it is subject to change.
aetna.com
©2018 Aetna Inc.
45.03.915.1 (12/18)

82
hisdbenefits.org
Your digital tools
The Aetna Health
SM
app and Aetna
®
member website
Personalized tools make your plan easier to use.
Connect to care
Find in-network providers, facilities and procedures
near you. And you’ll get personalized search results
based on your health benefits and insurance plan. You
can even get cost estimates for visits and procedures
before you go.
Manage claims
You can pay claims and view up to two years of claims
details for your whole family. Filter by member, provider,
facility, service or date.
Get proactive with your health
You’ll get simple, personalized health actions
recommended to you, based on your unique profile.
This could include a reminder to get a shot when
there’s a flu outbreak near you. Or a reminder that a
preventive doctor’s visit can help you stay on top of
your health and well-being.
$
$
Seamlessly connect with care
and manage benefits — at home
or on the go.
In Idaho, health benefits and health insurance plans are offered and/or underwritten by Aetna Health of Utah Inc.
and Aetna Life Insurance Company. For all other states, health benefits and health insurance plans are offered
and/or underwritten by Aetna Health Inc., Aetna Health of California Inc., Aetna Health Insurance Company of New
York, Aetna Health Insurance Company, Aetna HealthAssurance Pennsylvania Inc. and/or Aetna Life Insurance
Company (Aetna). In Florida, by Aetna Health Inc. and/or Aetna Life Insurance Company. In Utah and Wyoming, by
Aetna Health of Utah Inc. and Aetna Life Insurance Company. In Maryland, by Aetna Health Inc., 151 Farmington
Avenue, Hartford, CT 06156. Each insurer has sole financial responsibility for its own products.
Aetna.com
11.03.345.1 B (8/20)

83
877-780-HISD (4473).
Take charge of your benefits
With the Aetna Health app and the
Aetna member website, you can:
View your health plan summary and get detailed
information about what’s covered
View claim details and pay claims for your
whole family
Search for providers, procedures and medications
Get cost estimates before you get care
Track spending and progress toward meeting
the deductibles for you and your family
Access your ID card whenever you need it
Get recommended health actions based
on your profile
Once you’re a member, here’s
how you can connect:
Your Aetna
member website
Go to Aetna.co m to create an account
and log in to your member website.
The Aetna Health app
Get the Aetna Health app by texting “GETAPP”
to 90156 for a link to download the app and
create an account. Message and data rates
may apply.*
*Terms and conditions: Bit.ly/2nlJFYG. Privacy policy: Aetna.com/legal-notices/privacy.html. By texting 90156,
you consent to receive a one-time marketing automated text message from Aetna with a link to download the Aetna
Health app. Consent is not required to download the app. You can also download it from the App Store® or the Google
Play™ store.
Apple® and the Apple logo are trademarks of Apple Inc., registered in the U.S. and other countries. App Store is a service
mark of Apple Inc. Android™ and Google Play are trademarks of Google LLC.
Program features and availability may vary by location and are subject to change. This material is for information only.
Health information programs provide general health information and are not a substitute for diagnosis or treatment
by a physician or other health care professional. Health benefits and health insurance plans contain exclusions and
limitations. Estimated costs not available in all markets. The tool provides an estimate of what would be owed for a
particular service based on the plan at that very point in time. Actual costs may differ from an estimate if, for example,
claims for other services are processed after the estimate is provided but before the claim for this service is submitted.
Or if the doctor or facility performs a different service at the time of the visit. Health maintenance organization (HMO)
members can only look up estimated costs for doctor and outpatient facility services. Information is believed to be
accurate as of the production date; however, it is subject to change. Refer to Aetna.com for more information about
Aetna® plans.
Aetna.com
©2020 Aetna Inc.
11.03.345.1 B (8/20)

84
hisdbenefits.org
You and your household members have access to free benets available through our Employee Assistance
Program (EAP). Our EAP provider is ComPsych, and their GuidanceResources® program is a network
of services that can help you improve your emotional, mental, physical and nancial health, achieve
more at work and home, and handle many personal or professional challenges you face. e program is an
award-winning, comprehensive, interactive service that provides unique tools to assist you in every aspect
of your life.
ComPsych’s GuidanceResources® are provided free of charge and oer someone to talk to when you need them,
as well as resources to consult for a variety of expert content. ese services are strictly condential, and they are
available to you and your household members 24 hours a day, seven days a week, either by phone or online.
Take advantage of these valuable resources, which include:
• Condential emotional support with eight (8) free counseling sessions per member, per issue, per year
• Financial resources
• Legal guidance
• Unlimited work-life solutions
• Online support
e EAP’s GuidanceConnect feature allows you to schedule an appointment with a network therapist through
the online portal. Log on to guidanceresources.com. At the top of the page, click on the Find a erapist”
menu. After answering a few simple questions, you will be matched to a pool of therapists who meet your
clinical needs and preferences. Whether you’re looking for in-person, telephone, video or chat counseling, you
can select your preferred therapist right in the portal.
Chat Counseling is available through the ComPsych EAP’s collaboration with BetterHelp. Real-time,
scheduled chat counseling sessions are provided by licensed counselors and available through a secure portal.
Have a quick question or want to share your progress? Participants can always text their counselors directly on
a 24/7 basis once enrolled in the chat feature.
During the intake process, the GuidanceConsultant (GC) administers a comprehensive assessment and
determines the level of risk or presenting issue. If the GC determines that digital/chat counseling may be
appropriate based on the presenting issue, the GC will gauge the member’s comfort level with that technology
and provide a referral. e member will receive a chat counseling invite via email which will take them to the
chat platform to schedule their appointment at a time/date of their preference.
To learn more about how your EAP benets can help you and your household with many of life’s challenges,
call ComPsych Guidance Resources EAP at 1-833-812-5181 or log on to www.guidanceresources.com and sign
in. For members who have not yet registered for the online site, you will need to register using HISD as the
Organization Web ID and create an online account
EMPLOYEE ASSISTANCE PROGRAM

85
877-780-HISD (4473).
We have the solutions you need.
Call: 833.812.5181
TT Y: 800.697.0353
Online: guidanceresources.com
App: GuidanceNow
SM
Web ID: HISD
Available 24/7
Copyright © 2020 ComPsych Corporation. All rights reserved. is information is for educational purposes only.
ComPsych complies with applicable federal civil rights laws and does not discriminate on the basis of race, color, national origin, age, disability or sex
Get It
Together
It can be hard to figure
out how all the pieces of
your life fit together. Your
GuidanceResources program can
help. The program is provided
free of charge and offers someone
to talk to and resources to consult
whenever and wherever you need
them. Call us anytime, 24 hours
a day, seven days a week, for
confidential help.

86
hisdbenefits.org
Eligible HISD employees are automatically enrolled
Mandatory Contribution: 8.65% from each paycheck
Before Tax: 8.0% is applied to your membership account (tax deferred;
refundable upon resignation)
After Tax: 0.65% is applied to a general insurance fund (non-refundable)
Your Responsibilities as a TRS Member
1. Keep your mailing address current: Annual statement of account, newsletters, election ballots, information
brochures, and other important communications are mailed.
2. Notify TRS of name changes: Written noticat
ion is required.
3. Keep your Beneciary Designation current: Your beneciary designation instructs TRS on how to distribute your
benets upon your death. Review your beneciary designation when signicant life events occur such as
marriage, divorce, birth of a child, death of a spouse or designated beneciary, or if the beneciary
becomes eligibl
e for Medicaid or other "needs-based" assistance programs.
Teacher
Retirement
System of Texas
403(B)
457 PLAN
TRS is a governmental, tax-exempt benet retirement plan.
is pension trust fund provides service anddisability retirement, as well as death and survivor benets,
to eligible Texas public education employees and their beneciaries
It is never too late to start saving!
Some retirement savings is better than no retirement savings. Choose a provider and open an account today.
Have questions?
Attend the Retirement Storefront Choice Session to learn more.
Contact HISD Benets Support
Ph: 713-695-5561
Fax: 713-695-5723
Manage your
TRS account
online at
TRS.Texas.gov
Retirement Storefront
retirement
Eligible HISD employees are automatically enrolled
Mandatory Contribution: 8.65% from each paycheck
Before Tax: 8.0% is applied to your membership account (tax deferred;
refundable upon resignation)
After Tax: 0.65% is applied to a general insurance fund (non-refundable)
Your Responsibilities as a TRS Member
1. Keep your mailing address current: Annual statement of account, newsletters, election ballots, information
brochures, and other important communications are mailed.
2. Notify TRS of name changes: Written notication is required.
3. Keep your Beneciary Designation current: Your beneciary designation instructs TRS on how to distribute your
benets upon your death. Review your beneciary designation when signicant life events occur such as
marriage, divorce, birth of a child, death of a spouse or designated beneciary, or if the beneciary
becomes eligibl
e for
Medicaid or other "needs-based" assistance programs.
Teacher
Retirement
System of Texas
403(B)
457 PLAN
TRS is a governmental, tax-exempt benet retirement plan.
is pension trust fund provides service anddisability retirement, as well as death and survivor benets,
to eligible Texas public education employees and their beneciaries
It is never too late to start saving!
Some retirement savings is better than no retirement savings. Choose a provider and open an account today.
Have questions?
Attend the Retirement Storefront Choice Session to learn more.
Contact HISD Benets Support
Ph: 713-695-5561
Fax: 713-695-5723
Manage your
TRS account
online at
TRS.Texas.gov

87
877-780-HISD (4473).
Eligible HISD employees are automatically enrolled
Mandatory Contribution: 8.65% from each paycheck
Before Tax: 8.0% is applied to your membership account (tax deferred;
refundable upon resignation)
After Tax: 0.65% is applied to a general insurance fund (non-refundable)
Your Responsibilities as a TRS Member
1. Keep your mailing address current: Annual statement of account, newsletters, election ballots, information
brochures, and other important communications are mailed.
2. Notify TRS of name changes: Written noticat
ion is required.
3. Keep your Beneciary Designation current: Your beneciary designation instructs TRS on how to distribute your
benets upon your death. Review your beneciary designation when signicant life events occur such as
marriage, divorce, birth of a child, death of a spouse or designated beneciary, or if the beneciary
becomes eligibl
e for Medicaid or other "needs-based" assistance programs.
Teacher
Retirement
System of Texas
403(B)
457 PLAN
TRS is a governmental, tax-exempt benet retirement plan.
is pension trust fund provides service anddisability retirement, as well as death and survivor benets,
to eligible Texas public education employees and their beneciaries
It is never too late to start saving!
Some retirement savings is better than no retirement savings. Choose a provider and open an account today.
Have questions?
Attend the Retirement Storefront Choice Session to learn more.
Contact HISD Benets Support
Ph: 713-695-5561
Fax: 713-695-5723
Manage your
TRS account
online at
TRS.Texas.gov
Voluntary Retirement Savings Plans: 403(b) and 457
Visit the HISD Retirement Storefront website
For a list of providers, enrollment details, and voluntary retirementplan information.
How to visit the website
1. Log into myHISD
2. Scroll down to Employee Resources
3. Click on the “403(b)/457 Plan administration” link
What is a 403(b) or 457 retirement plan?
All active HISD employees are eligible to voluntarily participate in the 403(b) and 457 retirement plans sponsored
by the district, which are like a 401(k). Both type of plans allows for tax deferred growth, meaning more money can
accumulate without paying taxes on the interest or growth each year.
How does a 403(b) and 457 Plan work?
HISD employees voluntarily elect to set aside pre-tax money from their paychecks to save for retirement. HISD
sends the money directly to the employee’s chosen nancial institution. Each employee chooses the account type
that’s right for them, including interest bearing or equity (stock market) accounts. e money grows without paying
taxes (tax deferred) until withdrawal, preferably aer retirement.
Who may contribute to the 403(b) and 457 Plan?
You may choose to contribute to the 403(b) or 457 plan or both. Voluntary retirement plans are funded by
employee contributions only. No contributions are made by the district.
How do I choose a provider?
Each provider and each product is dierent so it’s important to understand how the 403(b)/457 contract works.
Know the costs to get ‘in and out’ of the contract. Ask questions to understand multiple options (not just the one
sold by the representative). You should receive clear answers to your questions and know what’s happening with
your money.
Which is better - a 403(b) or a 457 plan?
Speak with your provider(s) for details on which plan best suits your personal nancial goals and
circumstances. Plan features provided here may not be oered by all provider contracts.
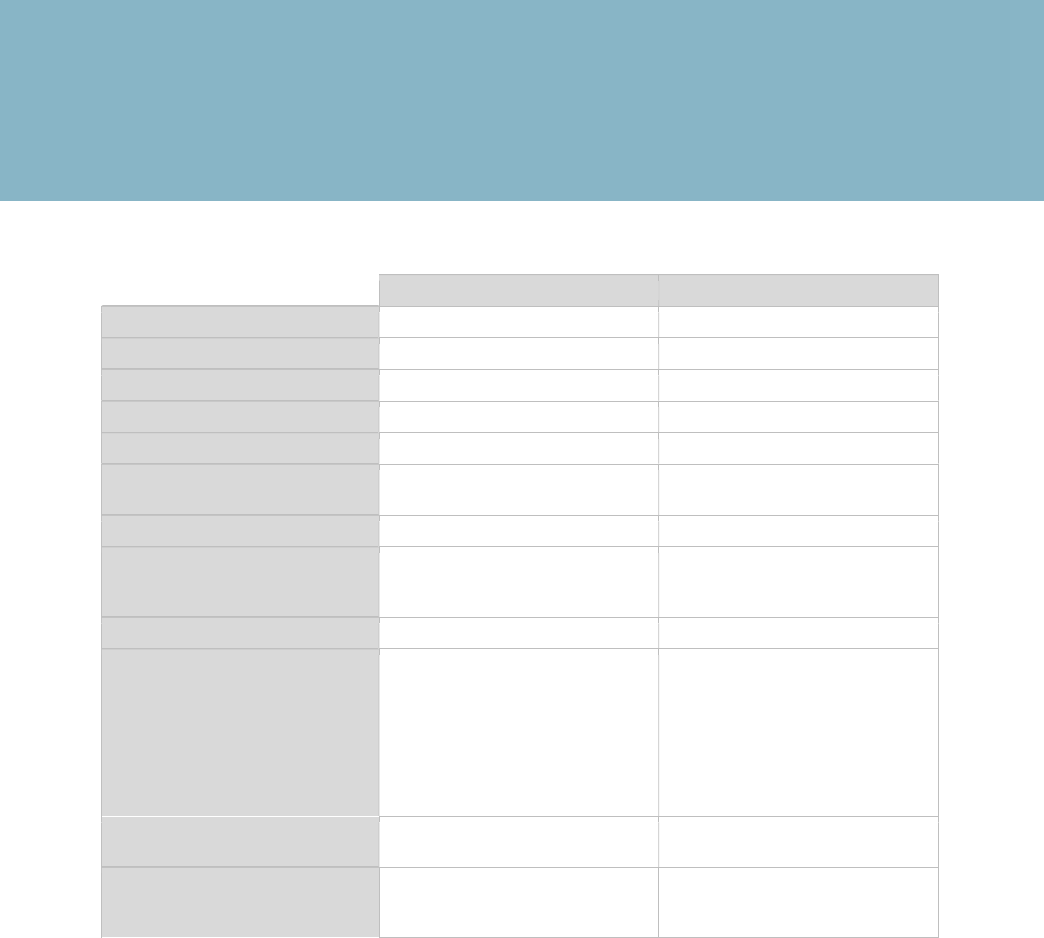
88
hisdbenefits.org
Speak with your provider(s) for details on which plan best suits your personal
nancial goals and circumstances. Plan features provided here may not be
oered by all provider contracts.
HISD Voluntary Retirement Plan Comparison Table 2022
All Employees All Employees
33 3
Yes Yes
Yes Yes
Yes No
No No
$22,500 $22,500
$29,500
Yes Yes
403(b) 457
Yes No
59 ½ 70 ½
Plan Eligibility
Number of Providers
Pre-Tax Contribution
Tax Deferred Interest and Earnings
After-Tax Roth Contributions*
Minimum Contribution
Requirement
Contribution Limit: Under Age 50
Contribution Limit: Age 50
and Over
Loan Availability
In-Service Hardship Distribution
Availability**
IRS 10% Excise Tax
(Early Withdrawal Penalty) ***
Unrestricted In-Service Distribution
Age (For withdrawal by active
employees)
*e after-tax Roth feature is oered in the HISD 403(b) but not in the 457. Contributions to a Roth 403(b) are
after-tax, and the interest & investment returns are tax free upon withdrawal when two conditions are met:
• Participant is at least age 59 ½
• Roth 403(b) has been open at least 5 years
**If employed at HISD and under age 59 ½, withdrawals are called “hardship distributions”.
***Withdrawals from the 403(b) by separated employees under age 59 ½ may be subject to an IRS 10% early
withdrawal penalty. Please contact a nancial advisor for more information or visit the HISD Benets portal.
How do I access my 403(b) or 457 retirement money?
Active employees under age 59 ½ have limited access to 403(b)/457 plan money. Taking a retirement plan
loan is usually the rst option to access the funds. Many providers oer loans, some do not.
Active employees may not withdraw funds from a 457 plan until age 70 ½. Instead, active employees may
access funds through loans and unforeseeable emergency withdrawals based on IRS rules.
Penalty-free distributions from a 403(b) may occur under certain circumstances. Please see a nancial advisor
or visit the HISD Benets portal.
Special provisions have been made for distributions related to COVID-19, according to section 2202 of the
CARES ACT.
1. Funeral/Burial Expenses
2. Post-Secondary Education
3. Prevent Eviction or Foreclosure
4. Purchase Principal Residence
5. Uninsured Home Repairs Due to Peril
6. Unreimbursed Medical
Unforeseeable emergency
causing severe nancial hardship
$29,500
retirement

89
877-780-HISD (4473).
*Rates shown are per paycheck based on 24 pay periods.
coverage costs
Medical Plans
Kelsey
Basic ACO
Memorial
Hermann
Basic ACO
TX Medical
Neighborhood
Basic
Kelsey
Plus ACO
Memorial
Hermann
Plus ACO
TX
Medical
Neighborhood
Plus
Employee only
$19.25 $21.18 $33.59 $38.79 $42.67 $67.63
Employee + spouse
$108.21 $119.03 $188.65 $146.07 $160.68 $243.35
Employee + child(ren)
$100.22 $110.25 $174.77 $135.30 $148.83 $226.17
Employee + family
$185.39 $203.94 $323.27 $250.27 $275.31 $391.01
vision plans
Basic Plus
Employee only $1.83 $2.86
Employee + spouse $3.46 $5.67
Employee + child(ren) $3.62 $5.95
Employee + family $6.76 $9.12
dental plans
HMO Plus PPO PPO BUYUP Discount Dental
Employee only $7.25 $19.62 $21.74 $2.50
Employee + spouse $13.78 $38.86 $43.08 $5.00
Employee + child(ren) $13.78 $38.77 $42.97 $5.00
Employee + family $17.71 $60.63 $67.22 $5.00

90
hisdbenefits.org
AD&D rate is included in employee rates.
If your spouse also works for the district,
you may each have employee supplemental
life and AD&D and the other have
spouse life and AD&D, but not both.
Your age
(January 1 of plan year)
Rate
< 30 $0.024
30 – 34 $0.024
35 – 39 $0.024
40 – 44 $0.038
45 – 49 $0.062
50 – 54 $0.091
55 – 59 $0.153
60 – 64 $0.181
65 – 69 $0.310
70+ $0.467
Your age
(January 1 of plan year)
Rate
< 30 $0.0395
30 – 34 $0.0495
35 – 39 $0.0545
40 – 44 $0.0745
45 – 49 $0.1295
50 – 54 $0.1995
55 – 59 $0.3295
60 – 64 $0.3845
65 – 69 $0.6695
70+ $1.0395
AD&D rate is included in spouse rates.
e benet is based on your benet level
and salary, up to the maximum benet—
the lesser of employee supplemental life
and AD&D coverage or $250,000.
Benet level $5,000 $10,000 $15,000 $20,000
Rate $0.28 $0.55 $0.82 $1.09
Dependent Life and AD&D
Supplemental Life and AD&D Spouse Life and AD&D
coverage costs
*Rates shown are per paycheck based on 24 pay periods.

91
877-780-HISD (4473).
Elimination period Option Cost
30 days
40% $0.186 x annual salary ÷ 1200
50% $0.239 x annual salary ÷ 1200
67.67% $0.642 x annual salary ÷ 1200
60 days
40% $0.138 x annual salary ÷ 1200
50% $0.206 x annual salary ÷ 1200
66.67% $0.404 x annual salary ÷ 1200
90 days
40% $0.125 x annual salary ÷ 1200
50% $0.170 x annual salary ÷ 1200
67.67% $0.327 x annual salary ÷ 1200
180 days
40% $0.065 x annual salary ÷ 1200
50% $0.081 x annual salary ÷ 1200
67.67% $0.190 x annual salary ÷ 1200
Disability
Personal legal
Basic
Plus
Incl. Parents
Employee only $4.77 $7.77
Employee + family $6.72 $9.72
*Rates shown are per paycheck based on 24 pay periods.

92
hisdbenefits.org
Critical illness : low
Your age
(January 1 of plan year)
Employee
only
Employee
+ spouse
Employee
+ child(ren)
Employee
+ family
18 – 24 $1.21 $2.10 $1.21 $2.10
25 – 29 $1.57 $2.64 $1.57 $2.64
30 – 34 $1.73 $2.88 $1.73 $2.88
35 – 39 $2.53 $4.08 $2.53 $4.08
40 – 44 $3.41 $5.40 $3.41 $5.40
45 – 49 $4.93 $7.68 $4.93 $7.68
50 – 54 $5.41 $8.40 $5.41 $8.40
55 – 59 $10.21 $15.60 $10.21 $15.60
60+ $20.01 $30.30 $20.01 $30.30
Your age
(January 1 of plan year)
Employee
only
Employee
+ spouse
Employee
+ child(ren)
Employee
+ family
18 – 24 $2.17 $3.54 $2.17 $3.54
25 – 29 $3.07 $4.89 $3.07 $4.89
30 – 34 $3.47 $5.49 $3.47 $5.49
35 – 39 $5.47 $8.49 $5.47 $8.49
40 – 44 $7.67 $11.79 $7.67 $11.79
45 – 49 $11.47 $17.49 $11.47 $17.49
50 – 54 $12.67 $19.29 $12.67 $19.29
55 – 59 $24.67 $37.29 $24.67 $37.29
60+ $49.17 $74.04 $49.17 $74.04
Critical illness : high
*Rates shown are per paycheck based on 24 pay periods.
coverage costs

93
877-780-HISD (4473).
Accident
Low High
Employee only $3.08 $5.33
Employee + spouse $4.95 $8.45
Employee + child(ren) $5.99 $10.10
Employee + family $7.86 $13.22
Hospital indemnity
Low High
Employee only
$2.36 $4.48
Employee + spouse
$4.42 $8.40
Employee + child(ren)
$4.17 $7.79
Employee + family
$6.23 $11.71
*Rates shown are per paycheck based on 24 pay periods.
Cancer and
specified diseases
Low Low + ICU High High + ICU
Employee only $5.18 $8.18 $9.42 $12.42
Employee + spouse $8.64 $14.81 $17.10 $23.28
Employee + child(ren) $6.63 $12.82 $12.48 $18.66
Employee + family $8.64 $14.81 $17.10 $23.28

94
hisdbenefits.org
24/7 Nurse Line
877-780-HISD (4473)
Aordable Care Act/
Health Reform Information
Healthcare.gov
Aetna Medical Plan
Aetna.com
877-224-6857
Care Acess Live
careacesslive.com
Cancer and Specied Diseases, Critical
Illness, Hospital Indemnity, Accident plans
Aac
Aacgroupinsurance.com
800-433-3036
Dental HMO/PPO
Cigna Dental
Cigna.com
800-244-6224
Discount Dental
Cigna Dental
CignaPlusSavings.com
877-521-0244
Disability
Unum
Unum.com
800-858-6843
Employee Assistance Program (EAP)
ComPsych
guidanceresources.com
To access website:
Click Register
Organization Web ID-HISD
833-812-5181
Flexible Spending Accounts
Healthcare FSA
Dependent day-care FSA
payex.com
888-678-8242
HISD Employee Health &
Wellness Centers
Hattie Mae White
Educational Support Center
4400 West 18th Street
Houston, Texas 77092
281-869-3630
Attucks Middle School
4330 Bellfort Street
Houston, Texas 77051
281-869-3630
IRS
IRS.Gov/publications/index.html
800-TAX-FORM (829-3676)
Kelsey-Seybold
Kelsey-seybold.com
713-442-0000
Life and Accidental Death
and Dismemberment
Securian Financial
Securian.com
Medical underwriting: 800-872-2214
Claims: 888-658-0193
Personal Legal
MetLifeLegal
legalplans.com
800-821-6400
Passwords for login:
3720010 (family coverage)
3730010 (single coverage)
Prescription Drug Benets
Express Scripts
Express-Scripts.com
855-712-0331
Accredo Specialty Pharmacy
Accredo.com
877-222-7336
Vision
EyeMed
EyeMed.com
844-409-3402
Benets Service Center: 877-780-4473

KNOW YOUR NUMBERS
Here is a way to keep track of the results of some annual physicals.
Blood Pressure: Date:
Glucose: Date:
Annual Physical:
Annual Well Woman:
Annual Well Male:
Cholesterol: Date:
A1C: Date:
Weight: Date:
Mammogram:
PSA:
Blood Pressure: Date:
Glucose: Date:
Annual Physical:
Annual Well Woman:
Annual Well Male:
Cholesterol: Date:
A1C: Date:
Weight: Date:
Mammogram:
PSA:
Blood Pressure: Date:
Glucose: Date:
Annual Physical:
Annual Well Woman:
Annual Well Male:
Cholesterol: Date:
A1C: Date:
Weight: Date:
Mammogram:
PSA:
Blood Pressure: Date:
Glucose: Date:
Annual Physical:
Annual Well Woman:
Annual Well Male:
Cholesterol: Date:
A1C: Date:
Weight: Date:
Mammogram:
PSA:
Blood Pressure: Date:
Glucose: Date:
Annual Physical:
Annual Well Woman:
Annual Well Male:
Cholesterol: Date:
A1C: Date:
Weight: Date:
Mammogram:
PSA:

www.hisdbenefits.org
hisdbenefits hisdbenefits houstonisdbenefits
