
MEDICAL GLOBAL
STANDARDS 2020

2©2020 Operation Smile, Inc. operationsmile.org
These Global Standards represent the eorts of our dedicated
volunteers and sta. We would appreciate requests to use
these materials. For permission to use the materials please
contact Operation Smile’s Medical Oversight Department.
3641 Faculty Boulevard, Virginia Beach, VA 23453 USA
1-888-OPSMILE
1-888-677-6453
+1-757-321-7645

3©2020 Operation Smile, Inc. operationsmile.org
CONTENTS
Introduction .............................................................................5
Organization Hierarchy of Documents......................................................6
Governance of Medical Documents ........................................................6
Medical Global Standard 1 – Facility..................................................7
1.1 Patient Lodging ................................................................7
1.2 Fact Find: Facility Assessment ...................................................7
1.3 Patient Screening ..............................................................8
1.4 Surgical Environment ...........................................................8
1.5 Non-Surgical Facility............................................................9
Medical Global Standard 2 – Team .................................................. 11
2.1 Fact Find: Team Assessment.................................................... 11
2.2 Team Members................................................................12
2.3 Team Leaders .................................................................13
2.4 Stang ......................................................................13
2.5 Team Qualifications............................................................15
Medical Global Standard 3 – Equipment, Supplies, and Pharmaceuticals..........17
3.1 Fact Find: Equipment, Supplies, and Pharmaceuticals Assessment ..................17
3.2 Integrity of Equipment, Supplies and Pharmaceuticals ............................18
3.3 Screening – Equipment, Supplies, and Pharmaceuticals ............................18
3.4 Surgical – Equipment, Supplies, and Pharmaceuticals..............................18
3.5 Anesthesia – Equipment, Supplies, and Pharmaceuticals ...........................19
3.6 Dental – Equipment, Supplies, and Pharmaceuticals (Dental and Surgical Mission) ...20
3.7 Speech – Equipment, Supplies, and Pharmaceuticals ............................. 20
3.8 Audiology / Ear, Nose & Throat – Equipment, Supplies, and Pharmaceuticals .........21
3.9 Psychosocial – Equipment, Supplies, and Pharmaceuticals .........................21
3.10 Post Anesthesia Care Unit (PACU) – Equipment, Supplies, and Pharmaceuticals ......21
3.11 Intensive Care – Equipment, Supplies, and Pharmaceuticals ....................... 22
3.12 Pre/Post-Operative Wards – Equipment, Supplies, and Pharmaceuticals ............ 22
3.13 Biomedical – Equipment and Supplies .......................................... 23

4©2020 Operation Smile, Inc. operationsmile.org
Medical Global Standard 4 – Patient Selection .................................... 26
4.1 Pre-Screening................................................................ 26
4.2 Screening ....................................................................27
4.3 Surgical Classification System ..................................................27
4.4 Patient Selection and Scheduling............................................... 29
4.5 Informed Consent ............................................................ 29
4.6 Surgical Deviations ...........................................................30
Medical Global Standard 5 – Medical Patient Management ....................... 32
5.1 Pre-admission ............................................................... 32
5.2 Patient and Caregiver Education . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 33
5.3 Surgical Admission ........................................................... 33
5.4 Surgical Process.............................................................. 34
5.5 Post-Surgical ................................................................ 36
5.6 Intensive Care................................................................ 38
5.7 Discharge and Ongoing Care .................................................. 39
Medical Global Standard 6 – Safety ................................................ 42
6.1 Emergency Preparedness ..................................................... 42
6.2 Blood Transfusion ............................................................ 43
6.3 Medications..................................................................44
6.4 Communication .............................................................. 45
6.5 Medical Record Documentation ................................................ 46
Medical Global Standard 7 – Quality ...............................................49
7.1 Reporting ...................................................................50
7.2 Medical Event Review ........................................................50
7.3 Quality Site Assist Visit.........................................................51
7.4 Infection Control Program ......................................................51
7.5 Surgical Site Infection Prevention ...............................................51
CONTENTS (continued)

5©2020 Operation Smile, Inc. operationsmile.org
INTRODUCTION
Today, Operation Smile believes the volume of patients who require cleft and essential surgical
care is very large and growing. Current health systems are not setup to provide all the care
required and the unmet need is so large that traditional services will never be enough to reach
all patients. Addressing the entirety of the problem will require an increase in programs and
operations, plus a disruptive level of innovation.
Operation Smile’s Medical Global Standards are a critical pillar in our response to the needs of
patients, and to the requirements of innovation and health systems strengthening. The 2020
standards reflect the diversity of care delivery and capacity building programs our community of
professionals have developed and implemented in the communities where we work. We continue
to place emphasis on the expansion of safe, eective, and timely care. Our primary focus is
always on patients, whose integration into family and societies is enabled through the inclusion
of multiple disciplines working together in their care.
The 2020 standards are supported by medical policies and procedures developed, reviewed,
refined, and approved by the Operation Smile Medical Oversight team. Operation Smile’s Medical
Global Standards embody the commitment of our global family to levels of performance in care
that can be consistently and uniformly expected by all patients, volunteers, sta, and supporters
in all Operation Smile Programs.
Our sincere recognition and thanks to the creators and pioneers of the first Global Standards
of Care developed in 2006/2007, revised in 2010 and 2014. The Medical Global Standards 2020
continue to build on the early eorts to ensure safe, high quality, ecient care to every
Operation Smile patient worldwide.
We extend our eternal gratitude to all who participated in the creation and updating of
Operation Smile’s Medical Global Standards 2020. We know that this is much more than a medical
exercise; it represents your pledge to our patients’ safety and wellbeing. Adhering to the 2020
standards is how we honor all who support us and believe children should receive excellent care,
no matter how much money they have or where they are born.
For almost 40 years, Operation Smile has provided care to
hundreds of thousands of patients born with cleft lip, cleft palate,
or other facial dierences. Operation Smile’s global network of
patients, families, sta, donors, and volunteers has extended to
more than 80 countries where it provides services, raises funds,
and recruits volunteers. This global network is the source
of strength and fuel which enables Operation Smile’s work.
Bill Magee Jr., D.D.S., M.D.
Operation Smile
Co-Founder and CEO
Kathy Magee, B.S.N., M.S.W., M.Ed.
Operation Smile
Co-Founder and President
6©2020 Operation Smile, Inc. operationsmile.org
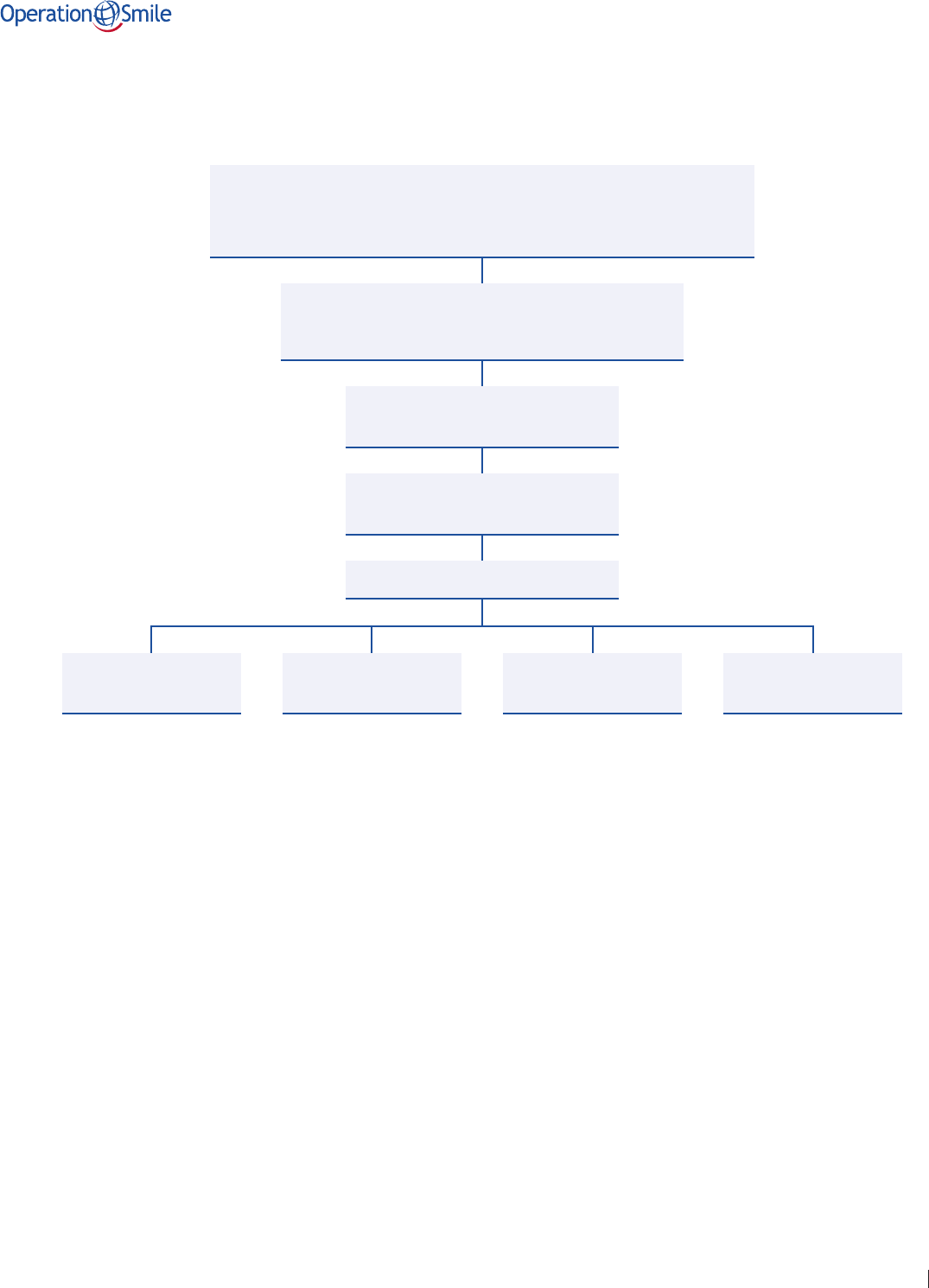
ORGANIZATION HIERARCHY OF DOCUMENTS
GOVERNANCE OF MEDICAL DOCUMENTS
The Operation Smile Medical Oversight Team is tasked with maintaining the integrity over
medical standards, policies, procedures, guidelines, and position statements. These documents
are created with input from medical leaders representing Operation Smile partner and
program countries.
Medical Oversight documents adhere to Operation Smile Inc.’s operational guidelines.
Operation Smile’s medical standards, policies, procedures, guidelines, and position statements
provide the framework for all care delivery.
We understand as programs grow, local regulations change, and healthcare systems are
strengthened there may be legitimate reasons to localize or vary from the current organizational
medical documents. Should a deviation be needed, a foundation should submit their proposed
variation for joint review with the Medical Oversight Team.
Global Medical Standard
Policy & Procedure
Guideline
Position Statement
Supporting Documents
Roles &
Responsibilities
Reports Forms Medical Record

7©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 1 – FACILITY
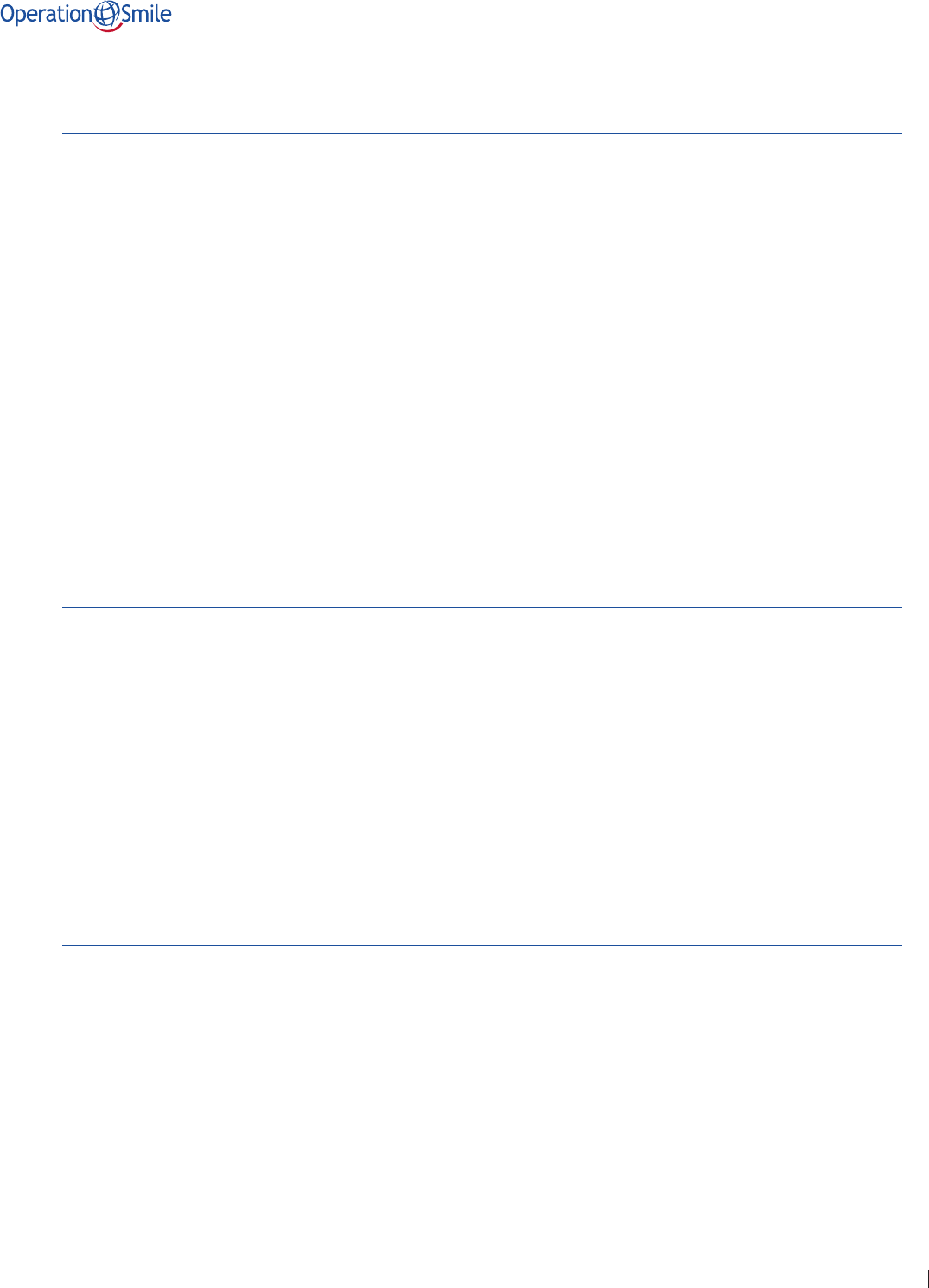
Medical Global Standard 1 – Facility
Approval Date: June 26, 2020 Replaces: 2015 GS 4-6,16
Eective Date: July 1, 2020 Category: Medical Oversight
Current Revision Date: March 2, 2020 Responsible Party: Chief Medical Ocer
Last Review Date: 2015 Review Schedule: 4 years
All facilities used for an Operation Smile program should be verified safe and
appropriate for the intended use.
1.1 Patient Lodging
A facility may be made available by the local foundation to temporarily house patients. Safety and
medical considerations should be adhered to when choosing and augmenting a facility for these
purposes. Communication between shelter sta and the medical team leadership is essential to
successful care delivery.
1.2 Fact Find: Facility Assessment
A proper site assessment should be performed and approved by the Operation Smile Quality
Team prior to patient care or as part of periodic reviews of centers which should occur no
less frequently than every 2 years. Facility assessments should be completed by a program
coordinator accompanied the following credentialed volunteers:
• Anesthesiologist
• Biomedical Technician
• Clinical Coordinator (recommended)
8©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 1 – FACILITY
1.3 Patient Screening
A safe and appropriate facility for patient screening should include:
• Adequate physical space and setup that allows controlled patient flow.
• Adequate lighting, electrical outlets, and furniture.
• Quiet screening areas for those who must perform pulmonary and cardiac auscultation,
speech assessment and those who need to communicate sensitive information.
1.4 Surgical Environment
A safe and appropriate facility for delivery of surgical care should include:
• A clean environment with washrooms and toilets in all patient care areas.
• A consistently adequate supply of water and electricity, including a backup electrical
generator or other power source that allows a safe plan for completing any surgery that is
ongoing at the time of a power outage.
• A supply of oxygen that is reliable and enough for the planned surgeries.
• Adequate lighting, electrical outlets, furniture (including beds), and physical space in all
patient care areas.
• A post-anesthesia care unit (PACU) that has adequate space and proximity to operating
rooms (ORs) and ward, so that safe transportation can occur from the ORs to the PACU,
and from the PACU to the post-operative ward.
• Adequate space to set up instrument cleaning and sterilization adjacent to the ORs.
• A designated emergency bed space on the post-operative ward, only to be used for
patients who need monitoring and/or emergency care.
• Adequate physical space for Speech, Psychosocial, Dental, Biomedical, Patient Imaging,
and other ancillary services.
• Dedicated space for biomedical waste as stated in the policy.
• Secure, environmentally controlled space for storage of equipment, pharmaceuticals,
and consumables.
• Support services:
– Laboratory available 24/7 (or point-of-care device available
and capable of supplying the same)
– Blood access 24/7
– Radiology service able to perform a chest-x-ray 24/7
– Intensive care unit (ICU) in the hospital or, if nearby, plans in place
for stabilization and transportation to that ICU.
– Cardiology services including ECG and ultrasound (recommended)

9©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 1 – FACILITY
1.5 Non-Surgical Facility
A safe and appropriate center that provides consultations and/or procedures without general
anesthesia or monitored anesthesia should include:
• Physical area with adequate space and controlled patient flow to achieve objective.
• A stable supply of water and electricity.
• Adequate lighting, electrical outlets, and furniture.
• Quiet screening space for those who must perform pulmonary and cardiac auscultation,
speech assessment and those who need to communicate sensitive information.
• Dedicated space for biomedical waste as stated in the policy.
• Secure environmentally controlled space for storage of equipment, pharmaceuticals,
and consumables.
Supporting Operation Smile Standard 1 – Policies & Procedures:
1. Fact Find Policy

10©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 1 – FACILITY
Supporting Operation Smile Standard 1 – Forms
1. Fact-Find Form
2. Rapid Fact-Find Form
3. Dental Fact-Find Form
4. Center Fact-Find Form
Supporting Operation Smile Standard 1 – References
Anaesthesia facility assessment tool. wfsahq.org. https://www.wfsahq.org/resources/anaesthesia-facility-assessment-tool.
Accessed September 30, 2019.
Carlson LC, Lin JA, Ameh EA, et al. Moving from data collection to application: A systematic literature review of surgical
capacity assessments and their applications. World J Surg. 2015;39:813–821.
Emergency and essential surgical care: Equipment lists and needs assessment. who.int. https://www.who.int/surgery/
publications/immesc_equipt_needsmaneg/en/.
Accessed October 1, 2019.
Emergency and essential surgical care: Surgical capacity. who.int. https://www.who.int/surgery/publications/esc_
surgcapacity/en/. Accessed October 1, 2019.
Goodman LF, St-Louis E, Yousef Y, et al. The Global Initiative for Children’s Surgery: Optimal resources for improving care.
Eur J Pediatr Surg. 2018;28(1):51–59.
Groen RS, Kamara TB, Dixon-Cole R, et al. A tool and index to assess surgical capacity in low income countries: An initial
implementation in Sierra Leone. World J Surg. 2012;36:1970–1977. doi:10.1007/s00268-012-1591-3
Operation Smile, Inc. Code of Conduct. Virginia Beach, VA: OSI; 2019.
Osen H, Chang D, Choo S, et al. Validation of the World Health Organization tool for situational analysis to assess
emergency and essential surgical care at district hospitals in Ghana. World J Surg. 2011;35(3):500–504. doi:10.1007/
s00268-010-0918-1
WHO-PGSSC Surgical Assessment Tool (SAT). globalchildrenssurgery.org. https://www.globalchildrenssurgery.org/wp-
content/uploads/2019/03/Surgical-assessment-tool.pdf. Accessed October 1, 2019.

11©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 2 – TEAM
Medical Global Standard 2 – Team
Approval Date: June 26, 2020 Replaces: 2015 GS-11, 12
Eective Date: July 1, 2020 Category: Medical Oversight
Current Revision Date: March 2, 2020 Responsible Party: Chief Medical Ocer
Last Review Date: 2015 Review Schedule: 4 years
Operation Smile oers a multidisciplinary team approach to the care of all
patients. In order to deliver safe, optimal care, dierent variables including
patient population characteristics, care-provider qualifications, location,
equipment, and local healthcare infrastructure should be considered when
stang teams.
2.1 Fact Find: Team Assessment
During a Fact Find Assessment, it is important to verify the human resources available to assist in
the care of Operation Smile patients. The assessment of hospital resources should be performed
prior to care delivery and/or as part of periodic reviews of centers. These support resources
should also be discussed with hospital and department leadership in advance of any short-term
program taking place, or on an as-needed basis for an on-going program format such as a center
or clinic. Specific areas/human resources to confirm include:
• Intensive Care Unit stang
• General patient care stang
• Operating Room stang

12©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 2 – TEAM
2.2 Team Members
Each team should consist of medical professionals and others practicing in the
following disciplines:
CleftSurgical Care
• Surgery
• Anesthesia
• Nursing
• PostAnesthesia Care
• Pediatrics
• Dentistry
• Medical Records
• Patient Imaging
• Biomedical
• Speech
• Psychosocial
The care team can be further enhanced by the inclusion of the followingspecialty providers:
• Ear, Nose & Throat specialist
• Audiologist
• Orthodontist
• Nutrition Specialist
• Geneticist
Non-Cleft Surgical Care
Operation Smile’s safe surgical delivery platform has oered opportunities for addressing surgical
needs other than cleft lip and cleft palates.Operation Smile may partner with other organizations
to enhance surgical care opportunities.
Operation Smile requires its partners who are administering surgical care in conjunction with
Operation Smile to adhere to the current Operation Smile’s Medical Global Standards while
acknowledging and adhering to partner standards and practices as agreed upon in organizational
agreements or memorandums of understanding.All volunteers from other organizations
functioning on Operation Smile programs must meet the same Operation Smile competency and
review requirements.
Additional partnership stang andpositionsmay be considered and approved on a case by
casebasisby Medical Oversight and Volunteer Management.
Operation Smile educational programs such as visiting professorships and/or educational rotations
typically take place within a host’s home hospital environment and may involve non-cleft surgical,
anesthetic, critical, and general care. Those educational programs may adhere to hospital practice
standards rather than Operation Smile standards in order to optimize teaching.
Non-Surgical Care
Additional services, such as consultations, therapy, orthodontic, and other procedures should be
staed according to the patient services provided.

13©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 2 – TEAM
2.3 Team Leaders
Medical Programs
Medical Specialty Team Leaders should be assigned for all short-term surgical
programs, including:
• Surgery Team Leader
• Anesthesia Team Leader
• Clinical Coordinator (nursing leader)
• Post Anesthesia Care Unit (PACU) Physician
• Pediatrician
Medical Specialty Team leaders should be assigned in consultation with Medical Oversight
and Regional Medical Ocers based on Operation Smile experience, previous training, or
experience as a team leader and overall practice experience. Anesthesia team leaders will be
physician anesthetists.
Centers and Non-Cleft Programs
Specialty Team Leaders should be assigned based on center services and program needs.
2.4 Stang
Operation Smile programs, which could include short-term cleft, dental, and/or orthognathic
surgery programs, and center activity should be staed according tominimum
requirements below:
All positions listed below will be filled by Operation Smile credentialed volunteers.
• Cleft Surgeons:1 cleft surgeon for each general anesthesia table and 1 for each local
anesthesia table, plus at least 1 additional float surgeon (no more than 5 surgical tables to
be covered by 1 float surgeon). Surgery team leader is included in the ratio above.
• Physician Anesthesiologists and Non-Physician Anesthesia Providers: 1 physician or
non-physician anesthesia providers for each general anesthesia table and 1 for each local
anesthesia table whenever sedation is planned, plus at least 1 additional float physician
anesthesiologist (no more than 5 surgical tables to be covered by 1 floater). The anesthesia
team leader is included in the ratio above and should be the float physician anesthesiologist.
– Minimum of 1 physician pediatric anesthesiologist for each team; additional pediatric
anesthesiologists or physician anesthesiologists who regularly care for infants may
be needed whenever there are plans to operate on large numbers of infants.
– No more than 2 total non-physician anesthesia providers plus first-time Operation
Smile physician anesthesiologists per team providing anesthesia at any point in time.
• Supervision ratio is 1 physician anesthesiologist to 2 non-physician
anesthesia providers/first-time Operation Smile physician anesthesiologist.
The supervising physician anesthesiologist may be the float physician
anesthesiologist or another physician anesthesiologist who is available to
circulate and is not concurrently providing anesthesia.

14©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 2 – TEAM
• Post Anesthesia Care Unit Physician: 1 Post Anesthesia Care Unit physician for 5 surgical
tables or less. Additional stang may be required for6 or more surgical tables.
• Pediatrician: 1 pediatrician for 5 surgical tables or less. Additional stang may be required
for 6 or more surgical tables.
• Clinical Coordinator (CC): At least 1 clinical coordinator per team; increased number may be
required for special programs.
• Surgical Circulating Nurse: 1 nurse per operating room. If more than 2 surgical tables in a
room, 1 nurse per two surgical tables.
• Surgical Scrub Personnel: 1 per surgical table.
• Post Anesthesia Care Unit Nurse: 1 nurse per 1.5 surgical tables.
• Pre/Post-Operative Day-Shift Nurses: Minimum of 2 nurses for 1-2 surgical tables, 3 nurses
for 3 surgical tables, 4 nurses for 4-5 surgical tables, 5 nurses for 6-7 surgical tables.
• Pre/Post-Operative Night-Shift Nurses: Minimum of 2 nurses for up to 3 surgical tables,
3 nurses for 4-6 surgical tables; 4 nurses for 7 surgical tables.
• Psychosocial Provider: Minimum of 1 per team; 2 recommendedwhen when 4 surgical
tables or more.
• Speech Language Pathology Provider:
– 2 speech providers on surgical programs with 4 surgical tables or more and/or
programs with projection of high volume of secondary palate repairs.
• One of the speech providers should be a credentialed speech
language pathologist.
– 1 speech provider for centers and programs with 3 surgical tables or less.
• If there is only 1 speech provider on a surgical program, it should be a
credentialed speech language pathologist.
– 1 credentialed speech language pathologist for education programs/rotations
when applicable.
• Dental Provider: Minimum of 1 dental provider with maxillofacial prosthesis and pre-surgical
molding experience; addition of 1 dental provider recommendedfor 7 surgical tables
or more.
• Biomedical Technician:Minimum of 1 biomedical technician per program, with no more than
6 surgical tables per biomedical technician.
• Medical Records: Minimum of 1 trained medical records volunteer to manage the medical
records for 1 – 2 surgical tables, 2 trained medical records volunteers (1 may be an
assistant) for 3 – 4 surgical tables, and 3 trained medical records volunteers (1 or 2 may be
assistants) for 5 or more surgical tables.
– If an electronic system is being used, at least 1 medical records volunteer trained to
use the electronic system should be on the team or the use of the electronic system
may need to be omitted.
• Patient Imaging Technician: Minimum of 1 trained patient imaging technician for 1-2 surgical
tables, 2 trained patient imaging technicians for 3- 5 surgical tables, 3 trained patient
imaging technicians for 6 or more surgical tables.
Operation Smile carries out a variety of care delivery and education/training programs. Stang
standards may be adjusted to match programmatic needs with the prior approval of the Regional
Medical Ocer and/or Medical Oversight.

15©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 2 – TEAM
2.5 Team Qualifications
Medical volunteers with Operation Smile will provide evidenceas defined by Medical Oversight
Policyof the following:
• Graduation from an academic or training program.
• Certificationand/or licensureas required by specialtypractice in home country.
• Current professional experience as defined by specialty.
• Demonstrated expertisein specialty.
• Life support certificationif applicable.
All medical and non-medical volunteers must remain current and in good standing according to
specialty qualifications and volunteer management.
Supporting Operation Smile Standard 2 – Policies & Procedures:
1. Volunteer Qualifications Policy
2. Stang Policy

16©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 2 – TEAM
Supporting Operation Smile Standard 2 – Forms
1. Skills Evaluation Form
2. Team Leader Evaluation of Team Leaders Form
3. Team Leader Evaluation of Team Members Form
4. Team Leader Evaluation of Program Form
Supporting Operation Smile Standard 2 – References
Aiken LH. Nurses hold the key to providing safer, more eective care and achieving better outcomes for patients. nursing.
upenn.edu. https://www.nursing.upenn.edu/live/profiles/93-linda-h-aiken. Accessed December 9, 2019.
Assaye A, Wiechula R, Schultz T, Feo R. Impact of nurse stang on patient and nurse workforce outcomes in acute care
settings in low- and middle-income countries: A systematic review protocol. JBI Database System Rev Implement Rep.
2018;16(12):2260-2267. doi:10.11124/JBISRIR-2017-003707
Gelb A, Morriss W, Johnson W, et al; International Standards for a Safe Practice of Anesthesia Workgroup. World Health
Organization-World Federation of Societies of Anaesthesiologists (WHO-WFSA). International Standards for a Safe
Practice of Anaesthesia. Anesth Analg. 2018;126(6):2047-2055. doi:10.1213/ANE.0000000000002927
Koller D. Evidence-based practice statements. Preparing children and adolescents for medical procedures. childlife.org.
https://www.childlife.org/docs/default-source/research-ebp/ebp-statements.pdf. Accessed December 9, 2019.
Kouatly I, Nassar N, Nizam M, Badr L. Evidence on nurse stang ratios and patient outcomes in a low-income country:
Implications for future research and practice. World Evid Based Nurs. 2018;15(5):353-360. doi:10.1111/wvn.12316
Politis G, Schneider W, Van Beek A, et al. Guidelines for pediatric perioperative care during short-term plastic
reconstructive surgical projects in less developed nations. Anesth Analg. 2011;112(1):183-190. doi:10.1213/
ANE.0b013e3181fdfab7
Speech-language pathology assistants. asha.org. https://www.asha.org/PracticePortal/Professional-Issues/Speech-
Language-Pathology-Assistants/. Accessed December 9, 2019.
Standards of approval for team care. acpa-cpf.org. https://acpa-cpf.org/team-care/standardscat/standards-of-approval-
for-team-care/. Accessed December 9, 2019.
Standards for improving the quality of care for children and young adolescents in health facilities. who.int. https://www.
who.int/maternal_child_adolescent/documents/quality-standards-child-adolescent/en/. Published 2018. Accessed
December 9, 2019.

17©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 3 – EQUIPMENT, SUPPLIES, AND PHARMACEUTICALS
Medical Global Standard 3 – Equipment, Supplies, and Pharmaceuticals
Approval Date: June 26, 2020 Replaces: 2015 GS-1,2,3,4,5,6
Eective Date: July 1, 2020 Category: Medical Oversight
Current Revision Date: March 2, 2020 Responsible Party: Chief Medical Ocer
Last Review Date: 2015 Review Schedule: 4 years
All Operation Smile surgical and non-surgical services should have an equipment
and supply management program to promote the availability and integrity
of equipment, supplies, and pharmaceuticals. The organization endeavors to
strengthen medical supply management.
3.1 Fact Find: Equipment, Supplies, and Pharmaceuticals Assessment
As part of the Fact Find, an equipment, supply, and pharmaceutical assessment should be
performed and approved by the Operation Smile Quality Team prior to patient care or as part of
periodic reviews of centers which should occur no less frequently than every 2 years.
Pharmaceuticals and supplies will be available in enough quantity and age appropriate sizes for
patient objectives.
18©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 3 – EQUIPMENT, SUPPLIES, AND PHARMACEUTICALS
3.2 Integrity of Equipment, Supplies and Pharmaceuticals
Operation Smile strives to promote the integrity of equipment, supplies, and pharmaceuticals for
the benefit of enhancing safety and quality patient care by:
• Enhanced awareness of the threats posed by substandard, falsified, and counterfeit
medical products.
• Sourcing pharmaceutical supplies and medical equipment from reputable manufacturers
and distributors.
• Enhanced deterrence of substandard, falsified, and counterfeit medical products by
maintaining awareness of the supply chain, and by requesting distributors to provide
information on immediate sources of these products.
• Partaking in pharmacovigilance eorts to detect, assess, understand, and prevent
adverse eects.
• Promptly responding to recalls and notifying Operation Smile’s Quality Department of
proper disposal of substances and/or supplies and disposition of devices in question.
• Storing and managing equipment, supplies, and pharmaceuticals in accordance with the
product labels/packaging.
3.3 Screening – Equipment, Supplies, and Pharmaceuticals
Preparation for screening of patients should include the following:
• Equipment for the psychological preparation of the patient and family.
• Equipment and consumables for medical screening and patient assessment.
• Equipment for measuring vital signs, oxygen saturation, weight, and height.
• Equipment for recording medical histories and physical examinations.
• Photographic equipment for patient imaging and identification.
• Equipment to obtain and process needed laboratory analyses.
• Equipment and supplies for patient tracking and scheduling.
3.4 Surgical – Equipment, Supplies, and Pharmaceuticals
Delivery of surgical care requires the following:
• Appropriate type and quantity of surgical instruments for the planned procedures.
• Surgical instruments inventoried, checked, and maintained at routine intervals.
• Sterile sutures and consumables in type and quantity appropriate for the
planned procedures.
• Equipment, medications, and treatment environment for providing nerve blocks or local
anesthetic infiltration.
• Functioning suction machine with associated supplies.
• Functioning electrocautery machine and associated supplies.

19©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 3 – EQUIPMENT, SUPPLIES, AND PHARMACEUTICALS
• Adequate lighting for illumination of the surgical field.
• Supplies and equipment for proper cleaning high level disinfection and sterilization.
• Placement of a suture or tag (that extrudes from the mouth) attached to any packing
material placed in the oropharynx, according to the Operation Smile Throat Pack/Retained
Surgical Items Policy.
• Palatal evaluation of patients seeking optimal secondary surgical procedures, preferably by
nasal endoscopy for location of velopharyngeal gap.
3.5 Anesthesia – Equipment, Supplies, and Pharmaceuticals
Delivery of anesthetic care requires the following (in age appropriate sizes where applicable):
• An anesthesia machine with the following capabilities/qualifications:
– Delivery of medical oxygen.
– Oxygen analyzer.
– Oxygen supply failure alarm at the anesthesia machine.
– Available mount for agent specific vaporizer for sevoflurane or other locally
available volatile agent if approved by Medical Oversight. Agent specific vaporizers
must only be used with the volatile agent for which they are designed.
– Ability to deliver fresh gas and volatile anesthesia without electrical power.
– Fresh gas outlet that allows connection to a Mapleson breathing system, or a
machine that can be used with a circle-system.
– Available mechanism for waste gas scavenging.
• Backup oxygen cylinder(s).
• Face masks.
• Endotracheal tubes with stylets.
• Oral and nasopharyngeal airways.
• Laryngoscope blades with handles.
• Equipment to manage unanticipated dicult airway (Dicult Airway box).
• Anesthesia breathing systems, such as Mapleson D circuits (preferred Mapleson circuit for
Operation Smile practice) or circle circuit if circle-system used.
• Adult and pediatric self-inflating bag-valve-mask systems for emergency administration of
positive pressure breathing.
• Functioning suction machine with all associated supplies.
• Isotonic Intravenous (IV) solutions including Ringers lactate (Hartmann’s solution) and
normal saline.
• Equipment for administration of IV fluids to include pediatric volumetric
administration devices.
• Medication in type and quantity appropriate for the planned procedures. Sevoflurane is
the preferred volatile anesthetic agent and use of other volatile agents requires Medical
Oversight approval.

20©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 3 – EQUIPMENT, SUPPLIES, AND PHARMACEUTICALS
• Monitoring equipment capable of continuous monitoring of electrocardiography (EKG),
pulse oximetry, capnography, temperature, and intermittent noninvasive blood pressure
(NIBP) measurement.
• Point of care (POC) device capable of measuring glucose (recommended).
• Point of care (POC) device capable of measuring hemoglobin (recommended).
• Immediate access to defibrillator/cardioverter with pediatric and adult paddles.
• Medications required for administration of advanced life support.
• Emergency code sheet in medical record of each patient, indicating calculated doses per
weight for each medication and intervention.
• Equipment to establish vascular access.
• Dantrolene in adequate quantity to treat an adult malignant hyperthermia case.
• Equipment and soaking solutions for the high-level disinfection and/or sterilization of
non-disposable anesthesia equipment.
• Type-Rh specific blood if available; if not available, two (2) units of O negative or O positive
blood screened for Hepatitis B, C and HIV.
3.6 Dental – Equipment, Supplies, and Pharmaceuticals (Dental and
Surgical Mission)
Delivery of dental services should include the following:
• Appropriate type and quantity of dental instruments for the planned procedures.
• Dental instruments inventoried, checked, and maintained at routine intervals.
• Equipment, medications, and treatment environment for providing safe local anesthesia.
• Basic monitoring equipment including intermittent blood pressure measurement and
pulse oximetry.
• Consumables appropriate to patient procedures.
• Functioning suction device with associated supplies.
• Functioning suction machine with air compressor recommended.
• Mobile table recommended.
• Access to X-ray machine and lead apron when indicated.
• Equipment for proper cleaning, high level disinfection, and sterilization.
• Medications and equipment for administration of basic life support and emergency
response i.e., allergic reactions (Dental Emergency Box).
– Glucometer (recommended).
3.7 Speech – Equipment, Supplies, and Pharmaceuticals
Delivery of speech services should include the following:
• Consumables appropriate to patient therapy services.
• Nasal endoscope and topical anesthetic (recommended).
• Voice recording device (recommended).

21©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 3 – EQUIPMENT, SUPPLIES, AND PHARMACEUTICALS
3.8 Audiology / Ear, Nose & Throat – Equipment, Supplies,
and Pharmaceuticals
Delivery of audiology and ENT services should include the following:
• Consumables appropriate to patient therapy services.
• Otoscope (recommended).
• Tympanometer / Audiometer (recommended).
3.9 Psychosocial – Equipment, Supplies, and Pharmaceuticals
Delivery of psychosocial support services should include the following:
• Supplies and consumables relevant to psychological preparation of the patient and family
during the entire spectrum of treatment and to integration into home and social settings.
3.10 Post Anesthesia Care Unit (PACU) – Equipment, Supplies,
and Pharmaceuticals
Delivery of post anesthesia care requires the following (in age appropriate sizes where applicable):
• One (1) post anesthesia care unit bed for each general anesthesia table.
• Isotonic intravenous (IV) solutions.
• Equipment for administration of IV fluids to include pediatric volumetric
administration devices.
• Monitoring equipment with size appropriate accessories capable of continuous monitoring
of electrocardiography, pulse oximetry, temperature, and intermittent noninvasive blood
pressure measurement should be available in the following ratio:
– 1 machine for 1-2 post anesthesia care unit beds.
– 2 machines for 3-4 post anesthesia care unit beds.
– 3 machines for 5-6 post anesthesia care unit beds.
• Immediate access to defibrillator/cardioverter with pediatric and adult paddles.
• Medications and equipment for administration of advanced life support (Code Box and
Malignant Hyperthermia Box).
• Bag-valve-mask for infant, child, and adult.
• Small volume nebulizer and Metered Dose Inhaler (MDI).
• Emergency code sheet in medical record with calculated doses per weight for each
medication and or intervention.
• Point of care device capable of measuring glucose (recommended).
• Point of care device capable of measuring hemoglobin (recommended).

22©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 3 – EQUIPMENT, SUPPLIES, AND PHARMACEUTICALS
• Oxygen source with associated supplies available for each post anesthesia care unit bed
and for transport if needed.
• Functioning suction machine with associated supplies available for each post anesthesia
care unit bed.
• Medication and consumables in type and quantity appropriate for the planned procedures.
• Access to laboratory and radiology services.
• Ability to transport patients from post anesthesia care unit to an intensive care facility in a
timely manner.
3.11 Intensive Care – Equipment, Supplies, and Pharmaceuticals
Delivery of intensive care requires the following:
• Ability to provide directly or through a partnership with a hospital facility to have Intensive
Care Unit services available for all Operation Smile patients.
• The Intensive Care setting should provide:
– Adult and pediatric ventilatory management.
– Immediate access to defibrillator/cardioverter with pediatric and adult paddles.
– Monitoring equipment to include cardiac monitoring, respiratory rate, capnography,
oxygen saturation, temperature, and blood pressure measurements.
– Oxygen and oxygen administration supplies.
– Functioning suction machine with associated supplies.
– Medications for administration of advanced cardiac life support.
– Emergency code sheet in medical record with calculated doses per weight for each
medication and or intervention.
• Consumables in type and quantity appropriate for planned procedures.
• Whenever the above required services are not rapidly obtainable in an actual hospital
intensive care setting, then plans should be in place to provide those services in the post
anesthesia care unit.
3.12 Pre/Post-Operative Wards – Equipment, Supplies,
and Pharmaceuticals
Delivery of pre- and post-operative care should include the following:
Pre-operative Ward:
• Equipment with size appropriate accessories capable of measuring pulse oximetry, blood
pressure, and temperature.
• Consumables for pre-surgical bathing.
• Clean gown for each surgical patient.
• Operation Smile Patient Care Booklet.

23©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 3 – EQUIPMENT, SUPPLIES, AND PHARMACEUTICALS
Post-operative Ward
• One (1) bed for each surgical patient.
• One (1) designated emergency bed for emergency monitoring only (required).
• Equipment with size appropriate accessories capable of measuring pulse oximetry, blood
pressure, and temperature.
• Intravenous (IV) solutions such as D5% ¼ NS, normal saline, and Ringers lactate.
• Equipment for administration of IV fluids to include pediatric volumetric
administration devices.
• Access to defibrillator/cardioverter with pediatric and adult paddles.
• Medications and equipment for administration of advanced cardiac life support (Code Box).
– Oxygen and suction with associated supplies at emergency bed.
– Bag-valve-mask device for infant, child, and adult.
– Emergency code sheet in medical record with calculated doses per weight for each
medication and or intervention.
• Medications and consumables in type and quantity appropriate for the planned procedures.
• Small volume nebulizer/aerosolizer.
• Point of care device capable of measuring glucose (recommended).
• Point of care device capable of measuring hemoglobin (recommended).
In a non-surgical setting, equipment, supplies, and medications will be available for basic
life support.
3.13 Biomedical – Equipment and Supplies
Provision and support of equipment and supplies should include the following:
• Operation Smile should provide or have signed vendor agreements to set up, calibrate, and
maintain required and recommended equipment.
• An active inventory, maintenance, and repair program.
• A climate-controlled area for consumables and pharmaceuticals.
• Availability of backup oxygen.
• Availability of a backup generator.
• Oxygen tanks which have a safety collar or chain to prevent accidental tipping of the tank.

24©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 3 – EQUIPMENT, SUPPLIES, AND PHARMACEUTICALS
Supporting Operation Smile Standard 3 – Policies & Procedures
1. Storage Space Requirements Policy
2. Medical Equipment Maintenance Policy
3. Surgical Instrument Maintenance Policy
4. Oxygen Reserve Policy
5. Use and Maintenance of Point of Care Equipment Policy
6. Pharmaceutical Integrity, Substitutions and Storage Policy
7. Medical Waste Management Policy
8. Throat Pack and Retained Surgical Items Policy
Supporting Operation Smile Standard 3 – Forms
1. Dicult Airway Box Inventory
2. Code Box Inventory
3. Malignant Hyperthermia Box Inventory
4. Post-Program Instrument Report
5. Instrument Set Check List
6. Dental Emergency Box Inventory

25©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 3 – EQUIPMENT, SUPPLIES, AND PHARMACEUTICALS
Supporting Operation Smile Standard 3 – References
Blackstone EA, Fuhr JP Jr, Pociask S. The health and economic eects of counterfeit drugs. Am Health Drug Benefits.
2014;7(4):216–224.
Caudron J, Ford N, Henkens M, et al. Substandard medicines in resource-poor settings: A problem that can no longer be
ignored. Trop Med Int Health. 2008;13:1062-1072. doi:10.1111/j.1365-3156.2008.02106.x
Essential Medicines and Health Products. Guidelines. who.int. https://www.who.int/medicines/areas/quality_safety/quality_
assurance/guidelines/en/. Accessed September 20, 2019.
Ferrario A, Orubu ESF, Adeyeye MC, et al. The need for comprehensive and multidisciplinary training in substandard and
falsified medicines for pharmacists. BMJ Glob Health. 2019;4(4):e001681. doi:10.1136/bmjgh-2019-001681
Guidelines on Validation – Appendix 6 Validation on Qualification of Systems, Utilities, and Equipment. who.int. https://
www.who.int/medicines/areas/quality_safety/quality_assurance/Guidelines_validation_qualification_systems-utilities-
equipment_QAS16-673.pdf. Published June 2016. Accessed December 10, 2019.
Larach MG, Klumpner TT, Brandom BW, et al. Succinylcholine use and Dantrolene availability for malignant
hyperthermia treatment: Database analyses and systematic review. Anesthesiology. 2019;130(1):41-54. doi: 10.1097/
ALN.0000000000002490.
Medical Devices. who.int. https://www.who.int/medical_devices/en/. Accessed August 27, 2019.
Operation Smile Inc. Operation Smile Pharmacopeia. Virginia Beach, VA: OSI; 2017.
Promoting the Safety of Medication in Children. who.int. http://apps.who.int/medicinedocs/index/assoc/s14235e/s14235e.
pdf. Published 2007. Accessed December 10, 2019.
Ravinetto R, Vandenbergh D, Macé C, et al. Fighting poor-quality medicines in low- and middle-income countries: The
importance of advocacy and pedagogy. J Pharm Policy Pract. 2016;9:36. doi:10.1186/s40545-016-0088-0
The International Pharmacopeia. who.int. http://apps.who.int/phint/2018/index.html#p/home. Published 2018. Accessed
December 10, 2019.
United States Pharmacopoeia and USAID Joint Project to Promote Quality of Medicines in Developing Countries
(PQM). usp.org. http://www.usp.org/global-health-programs/promoting-quality-medicines-pqmusaid. Accessed
September 25, 2019.

26©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 4 – PATIENT SELECTION
Medical Global Standard 4 – Patient Selection
Approval Date: June 26, 2020 Replaces: 2015 GS-1,8,7
Eective Date: July 1, 2020 Category: Medical Oversight
Current Revision Date: March 2, 2020 Responsible Party: Chief Medical Ocer
Last Review Date: 2015 Review Schedule: 4 years
Operation Smile utilizes population and patient data to recruit, screen, and select
patients to optimize well-timed surgery and related care. All Operation Smile
surgical procedures are elective and therefore general health status must be
considered to determine eligibility for anesthesia and surgery.
4.1 Pre-Screening
Pre-screening of patients is recommended to assess and prepare patients for potential surgical
treatment or additional therapies. This may be done 2 to 12 weeks before surgery. Pre-screening
should include:
• Screening for nutritional deficiencies.
• Screening for medical conditions.
• Anthropometric measures must include:
– Length/height for age Z-score (standard deviation) taking possible prematurity
into account.
– Weight for length/height Z-score (standard deviation).
– Middle upper arm circumference (MUAC) (recommended).
– Body mass index (BMI) (recommended).
• Screening for immunization status; recommending vaccination when applicable.
• Physical examination.
• Appropriate laboratory tests, when available.

27©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 4 – PATIENT SELECTION
The optimal pre-screening team from the local community may include:
• Nurse experienced in pediatric growth and development.
• Nutritionist.
• Pediatrician.
• Surgeon and/or Anesthesiologist.
4.2 Screening
Operation Smile aims to provide a full medical screening of all presenting patients. A
multidisciplinary approach is utilized to determine general health status, anthropometric
measures, and readiness for surgery and to provide psychosocial preparation. To determine
the specific cleft surgical or non-surgical procedure(s), collaboration between Surgery, Speech
Language, and Dental/Orthodontic providers is recommended. More complex procedures (e.g.,
orthognathic and facial clefts) require advanced planning and preparation.
Medical screening of patients will include:
• Screening for malnutrition should use the World Health Organization (WHO) and/or
national anthropometric growth charts and middle upper arm circumference (MUAC).
• Screening for medical conditions by obtaining a thorough patient history.
• Screening for physical conditions by performing a thorough physical examination.
• Screening for hematologic conditions, including anemia, by performing laboratory tests:
– Serum hemoglobin.
– Blood type and Rh factor for patients having surgeries with risk for substantial
blood loss, including palatoplasty.
– Evaluation of coagulation may be considered for patients having surgeries with risk
for substantial blood loss, including palatoplasty.
The following specialties should evaluate patients:
• Surgery
• Anesthesiology
• Pediatrics
• Nursing
• Speech
• Dental/orthodontic
• Psychosocial
• Other(s) as applicable
4.3 Surgical Classification System
The selection of patients for surgical intervention is guided by Operation Smile’s Screening,
Classification, and Selection Policy. Operation Smile’s Surgical Classification System is designed to
guide the selection of eligible patients for surgery.
Operation Smile’s Screening, Classification, and Selection Policy emphasizes the following:
• Patients must be selected after confirming that there is nothing in the medical history and
current general health status to contra-indicate anesthesia and surgery.

28©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 4 – PATIENT SELECTION
• Cleft surgical interventions should be appropriately timed and sequenced to enhance the
benefits for patients.
• Palate repairs are time sensitive for cleft palate patients as it relates to normal
speech development.
• Alveolar bone graft and revision palate surgery (including surgery for velopharyngeal
insuciency and fistula) should be considered specialized surgery, performed only when
appropriate expertise is present and, ideally, in patients selected and prepared in advance.
• Patients needing palate surgery for speech improvement should be given high consideration
for scheduling when the right expertise and environment for care are available.
• Patients who have had presurgical orthodontics should receive high consideration for
scheduling given the specific time frame surgery must be completed.
• Options for care, rehabilitation, and other therapies should be considered during the
surgical patient selection/scheduling process.
• Eligible surgical patients previously not selected for surgical intervention can be given a
higher level of consideration for scheduling within their classification group.
• Operation Smile may oer non-cleft surgical interventions in places where there is need
and teams are properly qualified, prepared, and resourced to successfully carry out such
interventions and post-operative care.
Surgical Classification System
Category 1: Primary lip repair, age three months through seven (7) years (up to 8th birthday).
Priority to patients who have both cleft lip and palate. This category also includes repeat surgery
for complete lip dehiscence when timing is appropriate. See age deviation for infants between 3
and 6 months of age.
Category 2: Primary palate repair, age nine (9) months through seven (7) years (up to 8th
birthday). Revision palate surgery in this age group. Speech surgery including palate lengthening,
pharyngeal surgery, and repair of fistulas when speech is aected. Pharyngeal surgery for speech
shall only be considered under appropriate conditions in cleft centers or tertiary care settings*.
See age deviation policy for infants between 9 and 12 months of age.
Category 3: Primary lip repair from age (8) years and older.
Category 4: Primary palate repair from eight (8) years and older (as prioritized by speech
language pathologist).
Category 5: Secondary cleft lip. Can include minor nasal revisions (one element significantly o
or two elements with minor asymmetries. May include tip plasty.
Category 6: Additional cleft procedures (**alveolar bone graft, rhinoplasty, ***orthognathic
surgery, etc.)
Category 7: Other (syndactyly, ****frenulectomy, nevi removal, burns etc.).
Note: Patients in categories 1-4 who have been denied care previously are prioritized within
each category.
Not a candidate: A patient’s condition does not fall within any of the above categories treated by
Operation Smile and is not a candidate for the current program, any future program, nor
world care.
Potential World Care Candidate: Candidates for surgery whose condition is too complex to
be treated during an Operation Smile program or are unable to receive surgery due to time or
resource constraints.

29©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 4 – PATIENT SELECTION
* These include a qualified team of surgeons, speech language pathologists and dentist/orthodontists to evaluate and
plan care. See Surgical Classification Policy for further detail on requirements. With respect to closure of fistulas, priority is
given to fistulas that aect speech.
**Alveolar bone grafts should be considered specialized surgery that is performed only when appropriate expertise is
present. Ideally, these patients should have been selected and prepared in advance. Patients that have had presurgical
orthodontics should also receive high priority on the surgical schedule because we have committed to complete these
operations within a specified time frame.
***Orthognathic surgery is only to be performed on designated orthognathic programs.
****Frenulectomy for feeding diculties may be scheduled.
4.4 Patient Selection and Scheduling
Patient selection should be based on cleft surgical classification, overall anthropometric and
general health status, laboratory values, and consent to treat. Patients with medical conditions
and syndromes should be carefully screened and a decision to proceed with surgery on those
patients should be agreed upon by team leaders.
For education purposes or non-cleft patients, selection may dier according to overall goals and
objectives of the program.
All patients who will receive surgery should have a hemoglobin level of 9 or greater.
States of malnutrition where weight for length/height is below -2 SD should not be scheduled.
Length/height for age and other anthropometric measures may be considered by all team leaders
to rearm readiness for surgery or suggest other therapeutic measures.
For cleft programs, team leaders from anesthesia, surgery, and nursing, as well as the PACU
physician, pediatrician, dentist, and speech provider collaboratively consider the following points
during patient selection and scheduling:
• Length of surgical day should be limited to 10 hours from the first patient on the surgical
table to the last patient o the surgical table.
• Anesthetic care for children under 1 year of age (infants) should be provided by a
pediatric anesthesiologist or another anesthesiologist who also regularly provides
anesthesia for infants.
• Infants should be scheduled as early in the day as possible.
• Palate surgeries should be scheduled as early in the day as possible.
All patients have the right to receive feedback on the results of their screening evaluations.
Whether a patient is selected for surgical treatment and multidisciplinary care by Operation Smile
or whether a candidate for referral and care by another team, facility or entity, information should
be delivered by a medical provider in a respectful and considerate manner.
4.5 Informed Consent
Patients and caregivers (if the patient is a minor) should be well informed and involved in decisions
regarding their own care or the care of their minor children. Treatment will only be provided after
the proper informed consent has been obtained from the patient (if of legal age) or from the
patient’s caregivers (if the patient is a minor). Consent should be “knowing” which involves clear
explanations of care, including multifaceted staged treatment such as orthognathic care.

30©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 4 – PATIENT SELECTION
Consent for Examination and Treatment
• This consent gives permission for photo imaging, physical examination, psychosocial
evaluation, blood sampling, and other testing needed to assess whether the patient is a
candidate for surgery and should be obtained when the medical record is initiated.
Consent for Surgical Treatment
• This consent gives permission for administration of anesthesia, administration of blood
products, and performance of a designated surgical procedure and should be obtained
prior to surgery.
Consent for Dental Treatment
• This consent gives permission for performing dental procedures and treatment and should
be obtained prior to treatment.
4.6 Surgical Deviations
All cases requiring deviations related to age, surgical tables, surgical time, or surgical procedure
must be reviewed and approved by all team leaders and by the applicable Regional Medical
Ocer prior to scheduling those cases.
Age Deviation
A cleft lip patient less than 3 months is NOT safe for an Operation Smile surgical program and will
not receive surgery. A cleft lip patient between the ages of 3 months and 6 months is considered
an Age Deviation and may be scheduled for a cleft lip repair only if the child has no medical
conditions, is currently healthy and well nourished, and has normal serum hemoglobin as outlined
in Operation Smile policy.
A cleft palate patient less than 9 months is NOT safe for an Operation Smile surgical program
and will not receive surgery. A cleft palate patient between the ages of 9 months and 1 year is
considered an Age Deviation and may be scheduled for a cleft palate repair only if the child has
no medical conditions, is currently healthy and well nourished, and has normal serum hemoglobin
as outlined in Operation Smile policy.
A non-cleft patient under 1 year of age will be considered an age-deviation for general anesthesia.
Surgical Procedure Deviation
Any unplanned advanced or complex procedures, including but not limited to flaps, bone grafts,
complex maxillofacial defects such as facial clefts, are considered a Surgical Procedure Deviation
and must be approved as noted above.
Any unplanned advanced or unusually complex procedure beyond Operation Smile’s typical
scope of practice is considered a Surgical Procedure Deviation and must be approved as
noted above.
Any patient with an expected dicult mask airway or an expected dicult intubation to the
degree that a video laryngoscope or fiberoptic scope is likely to be required for intubation is a
Surgical Procedure Deviation and must be approved as noted above.

31©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 4 – PATIENT SELECTION
Surgical Time Deviation
Any surgical procedure with a duration of more than 3 hours is considered a Surgical Time
Deviation and must be approved as noted above.
Surgical Table Deviation
Any addition or adjustment in the number of planned local anesthesia or general anesthesia
surgical tables during a surgical program is considered a Surgical Table Deviation and must be
approved as noted above. Adequate equipment, supplies, pharmaceuticals, beds, and sta must
be confirmed prior to approving a Surgical Table Deviation.
Surgical Table Deviations include:
• Adding a general anesthesia surgical table.
• Adding a local anesthesia surgical table.
• Converting a local anesthesia surgical table to a general anesthesia surgical table.
Supporting Operation Smile Standard 4 – Policies & Procedures
1. Patient Screening, Classification, and Selection Policy
2. Age, Table, Procedure, and Time Deviation Policy
Supporting Operation Smile Standard 4 – Forms
1. Pre-Screening Form
2. Age Deviation Form
3. Surgical Procedure and Surgical Time Deviation Form
4. Surgical Table Deviation Form
5. WHO weight to length growth chart for gender/age
Supporting Operation Smile Standard 4 – References
Child Growth Standards – WHO Anthro Survey Analyser and Other Tools. who.int. https://www.who.int/childgrowth/
software/en/. Accessed August, 2019.
Hughes CD, Babagian A, McCormack S, et al. The clinical and economic impact of a sustained program in global
plastic surgery: Valuing cleft care in resource-poor settings. Plast Reconstr Surg. 2012;30(1):87e-94e. doi:10.1097/
PRS.0b013e318254b2a2
Lewis CW, Jacob LS, Lehmann CU; AAP Section on Oral Health. The primary care pediatrician and the care of children
with cleft lip and/or cleft palate. Pediatrics. 2017;139(5):e20170628.
Operation Smile, Inc. Code of Conduct. Virginia Beach, VA: OSI; 2019.
Patel PB, Hoyler M, Maine R, et al. An opportunity for diagonal development in global surgery: Cleft lip and palate care in
resource-limited settings. Plast Surg Int. 2012;2012:892437. doi:10.1155/2012/892437
Politis G, Schneider W, Van Beek A, et al. Guidelines for pediatric perioperative care during short-term plastic
reconstructive surgical projects in less developed nations. Anesth Analg. 2011;112(1):183-190. doi:10.1213/
ANE.0b013e3181fdfab7

32©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 5 – MEDICAL PATIENT MANAGEMENT
Medical Global Standard 5 – Medical Patient Management
Approval Date: June 26, 2020 Replaces: 2015 GS-1,9,10,13,14,15
Eective Date: July 1, 2020 Category: Medical Oversight
Current Revision Date: March 2, 2020 Responsible Party: Chief Medical Ocer
Last Review Date: 2015 Review Schedule: 4 years
Operation Smile is committed to safe and comprehensive treatment for
patients and families. A multidisciplinary team approach allows for a thorough
assessment, diagnoses, and treatment plan. We aim for full integration of the
patient into family and society.
5.1 Pre-admission
Patients may be admitted from home or a patient shelter/village before screening.
Operation Smile may organize patient lodging and arrange for additional support as part of its
strategies to expand access and aordability of care. Such accommodations should be designed
to minimize the risk of spread of infection by observing infection prevention measures.
Patient lodging should be maximized to provide supporting services and patient education
by nursing (highly recommended), pediatrics, psychosocial care, dental, speech, nutrition, and
others. Support may include surgical and non-surgicalservices to patients who may or may not
be receiving surgeryprior to and following discharge from the hospital/clinic.

33©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 5 – MEDICAL PATIENT MANAGEMENT
5.2 Patient and Caregiver Education
Patients and caregivers are an integral part of the medical team. Patient centered decision making
should be incorporated to facilitate understanding of screening through after-care, procedure
expectations, and physical/psychologic care.
Evidence based, standardized materials that consider patient/caregiver literacy and language
needs should be used for education.
Patient preparation and education concerning surgery or other procedures should be provided by
the multi-disciplinary team to include:
• Etiology, condition.
• Procedure description, expectations, and/or follow up therapy.
• Food and fluid restriction before surgery.
• Post-operative diet following surgery and after discharge.
• Warning signs and complications to report to medical sta.
• Medication use and administration.
• Pain management.
• Wound care and infection prevention.
• Discharge and follow-up care.
5.3 Surgical Admission
All Operation Smile patients will be assigned an Operation Smile medical record number. The
Operation Smile medical record should include the full name, address, contact information,
date of birth using day/month/year (dd/mm/yyyy) format, next of kin, and other demographic
information. An identification photo should be in the medical record.
On admission to the hospital or center for surgery an identification band will be placed on the
patient’s wrist or ankle. The identification band will contain at minimum:
• The patient’s name.
• The patient’s Operation Smile medical record number.
At least 2 unique identifiers will be used for all patients when receiving any care, medication, or
surgery. Other unique identifiers, in addition to the above, that may be used include:
• Identification photo in the medical record.
• Date of birth.
• Name and address or contact information of the parent/caregiver or guardian.

34©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 5 – MEDICAL PATIENT MANAGEMENT
Pre-operative
A safe holding space should be provided for patients before entering the surgical area.
Psychosocial providers may facilitate therapeutic play and patient education while
awaiting surgery.
Prior to a patient being taken to the operating room or dental treatment area, the medical record
should be reviewed to check patient identity, surgical procedure, and side/site of surgery.
The following team members will use the chart to confirm patient identification and validate
the following:
• Operative surgeon/dentist assuring there is a signed consent and operative plan.
• Anesthesia/pediatrician to assure health and required nil per os (NPO) status are
acceptable for surgery.
– 6 hours for non-clear liquids and solids.
– 4 hours for breastmilk.
– 1 hour for clear glucose fluids.
• Surgical circulating nurse and clinical coordinator will confirm a signed consent, laboratory
values, vital signs, and an appropriate emergency code sheet.
The surgeon and anesthesia provider or dental provider should:
• Introduce his/herself to the patient/caregiver.
• Examine patient and verify identification.
• Verify the planned procedure with the patient/caregiver.
• Ask the patient/caregiver if there are any questions.
5.4 Surgical Process
The Operative Area
Verification of the care team, equipment, and processes should occur before taking any patient to
the operating room.
Patient imaging photographs should be secured at designated points:
• Pre-surgical patient image: after induction and prior to application of skin
disinfection solution.
• Post-surgical patient image: before extubation with mouth gag still in place (palates)
and after surgical site is cleaned (lips).

35©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 5 – MEDICAL PATIENT MANAGEMENT
Surgical Safety Check
A three-step surgical safety “Time-Out” is required for ALL patients. This occurs at:
• Sign In: when the patient enters the operating room before induction of anesthesia.
• Time Out: before the skin incision or dental extractions.
• Sign Out: On completion of case before the patient is extubated (timing is in order to
confirm throat packs have been removed).
All items listed should be verified by the: surgeon, anesthesia provider, surgical scrub personnel,
and the surgical circulating nurse. This process is usually led by an anesthesia provider or surgical
circulating nurse.
Intra-Operative Management
Anesthetic induction must be attended by two credentialed anesthesia providers. An
Operation Smile credentialed anesthesia provider must always remain with an anesthetized
patient. Anesthetic emergence and extubation must be attended by the anesthesia provider
and one other team member (circulating anesthesiologist when available, otherwise surgical
circulating nurse).
For patients undergoing general anesthesia or monitored sedation, intraoperative monitoring
must include: continuous capnography (not possible for monitored sedation cases that prohibit
use of nasal cannula capnography), electrocardiogram (EKG), temperature, pulse oximetry, and
non-invasive intermittent blood pressure (NIBP) measurements cycling every 5 minutes or less.
Fluid management should follow Operation Smile policy.
Multi-modal analgesia should utilize nerve blocks when appropriate and
pre-operative and intra-operative analgesic medications of dierent classes.
Intravenous antibiotics will be administered within one hour prior to surgical incision. Current
evidence does not support the use of postoperative antibiotics.
A tongue stitch may be placed for palatoplasty patients, with placement and time of removal at
the discretion of surgical/anesthesia/pediatric teams.
Throat Pack
All palate and select lip procedures with an uncued endotracheal tube should have a throat
pack placed with approved suture tail and signage. Throat packs may be used with a cued
endotracheal tube at the discretion of the anesthesiologist and surgeon. Construction of gauze
packing that goes into the oral cavity and placement of a suture or tag (that extrudes from the
mouth) must be done according to Operation Smile policy. Insertion and removal of oral packing
must be verbally acknowledged and documented on the surgical safety checklist and anesthesia
record.
Local Anesthesia
Patients may receive local anesthesia, no sedation, and surgery without involvement of an
anesthesia provider. Whenever local anesthesia patients receive intravenous sedation, an
anesthesia provider must be present to administer sedatives and continuously monitor (according
to intraoperative standard above) and care for those patients.

36©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 5 – MEDICAL PATIENT MANAGEMENT
Care of surgical patients receiving local anesthesia and no sedation should include:
• An interpreter/translator (when necessary) for proper communication between the patient
and the surgical team.
• Measurement of heart rate, respiratory rate, oxygen saturation, and blood pressure prior to
and at the end of the procedure and, as needed, by the surgical circulating nurse.
• Documentation by surgical circulating nurse on the operating room notes should include:
– Intravenous fluid and antibiotic administration.
– Heart rate, respiratory rate, oxygen saturation, and blood pressure prior to and at
the end of the procedure and as needed.
• Monitored in the PACU until hemodynamically stable.
Attire
Operating Room sta will wear approved attire for clean procedures to minimally include:
• Head and hair covering.
• Face mask.
• Sterile gloves (surgeons, scrub nurses).
Local regulations may have additional requirements that should be adhered to.
Case Cancellation
In the event a surgical patient needs to be cancelled, a medical provider and a psychosocial
provider should explain to the patient/caregiver the cause of the cancellation and potential future
therapeutic options. The medical chart should have documentation of the cancellation, the cause,
and follow-up options.
5.5 Post-Surgical
Post Anesthesia Care Unit (PACU)
This critical high-observation unit is designed to provide close observation and monitoring as the
patient emerges from anesthesia.
Patients should be extubated prior to entry to the post anesthesia care unit.
Hand o should occur between the anesthesia provider and a member of the post anesthesia
care sta.
The following care must be provided to post anesthesia care patients:
• Continuous pulse oximetry and blood pressure measurements with availability of
continuous electrocardiography to be used as needed.
• Pain and emergence delirium management using approved intravenous analgesics
(judiciously), sedatives, and other non-pharmacologic modalities.

37©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 5 – MEDICAL PATIENT MANAGEMENT
• Vital signs and Post Anesthesia Recovery Score must be assessed and documented every
5 minutes until the patient is awake, then every 15 minutes until discharge to the
post-operative ward.
• Discharge readiness is when:
– The patient is conscious and hemodynamically stable, with pain and
bleeding controlled.
– The vital signs return to age appropriate baseline.
– Supplemental oxygen is no longer needed.
– The Post Anesthesia Recovery Score is 8 or better.
– A minimum of 30 minutes monitoring in the post anesthesia care unit with the
following exceptions:
• Stable local anesthesia patients after a brief evaluation and vital sign check.
• When anesthesia time is less than 30 minutes, such as in a frenulectomy.
Post-Operative Ward
Hand o should occur between the post anesthesia care sta and the receiving post-operative
ward sta.
Post-operative care is provided continuously by credentialed Operation Smile sta from
admission to the ward until discharge.
Elbow restraints may be used at the discretion of the post-operative sta.
Assessment, vital signs, and pain scores should be performed and documented every 4 hours
(or more frequently if needed).
Additional services may be provided on the pre/post-operative ward to include but not limited to
speech, psychosocial, or other services pertinent to the scheduled or performed procedure.
Pain Management on Ward
Multi-modal pain management will occur using approved oral pharmacologic and non-
pharmacologic modalities. Intravenous or intramuscular analgesics are discouraged but may
be necessary in cases of severe unrelenting pain, especially after bone grafts or maxillo-facial
surgery. The patient and caregivers are an integral part in assessment and pain management.
The medical team should work with the patient and caregivers through regular assessment and
ongoing education. Pain should be assessed using valid, age appropriate scoring systems.
Length of Stay
Patient length of stay should be decided individually for each patient by the team leaders.
The following variables should be considered in these decisions: patient age and health status,
distance from home, local protocols and regulations, follow-up treatment, and education needs.
Average length of stay may be:
• 1 night for uncomplicated surgeries.
• 2 nights for patients requiring additional observation.
• 2 hours (minimum for local anesthesia patients).

38©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 5 – MEDICAL PATIENT MANAGEMENT
5.6 Intensive Care
Operation Smile teams will be prepared for intraoperative critical events that indicate need for
ongoing intensive care and for postoperative escalation of care using advanced monitoring. Any
need for intensive care must be documented as a medical event.
Return to Post Anesthesia Care Unit
Any ward patient in need of escalation of care with advanced monitoring and/or critical care
interventions (including airway management) will be admitted back to the post anesthesia
care unit.
Return to the Operating Room
An “on call” operating team must be available for any complication requiring a return to the
operating room.
Intensive Care
Operation Smile should ensure on-site availability of a satisfactory intensive care setting,
including medical sta, monitors, equipment, and supplies for patients in need of intensive care.
When unavailable, a plan should be in place for transport to an o-site intensive care facility.
Intensive Care in the Post Anesthesia Care Unit
For short term monitoring or in the absence of adequate intensive care facilities at or near the
mission site, a patient in need of intensive care should be moved to the post anesthesia care unit.
Downsizing of the program’s surgical tables and overall plans may be necessary to safely care for
other patients while allowing adequate stang for an intensive care patient managed in the post
anesthesia care unit.
Hospital Based Intensive Care Unit (ICU)
Prior to conducting surgery, a plan should be in place to provide intensive care services for
patients should they be needed. Intensive care services are generally located within the
hospital where the program takes place or a hospital a short distance away. The plan (to
include transportation if the ICU facility is osite) should be documented in a memorandum of
understanding. A non-Operation Smile intensive care unit must have the following:
• A bed with monitoring capabilities for continuous electrocardiography, heart rate,
respiratory rate, oxygen saturation, capnography, and temperature.
• Ventilator(s) capable of pediatric and adult use.
• A 24-hr. laboratory available for hematology, blood gasses, and chemistry parameters.
• Radiology and cardiology services available.
• Qualified physicians and nurses available for 24-hour care for the patient.

39©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 5 – MEDICAL PATIENT MANAGEMENT
5.7 Discharge and Ongoing Care
Local resources should be identified for ongoing patient care after discharge.
Patient Discharge
Patient discharge is a collaborative decision between the surgeon and pediatrician with input
from nursing and other disciplines as indicated. Patients should be hemodynamically stable and
pain adequately managed prior to discharge.
When a patient is cleared for discharge, the discharging nurse or pediatrician should assure the
patient/caregiver can verbalize the following:
• Wound care instructions.
• Nutrition/diet/hydration guidelines.
• Pain management strategies.
• Purpose and administration of medications.
• Identification and management of complications.
Patient Follow-Up
Operation Smile supports capacity building eorts to expand access to ongoing post-operative
services via centers, partnerships, or integration with local health services.
Patients should return to a designated site 4-7 days following surgery to be examined by a
surgeon experienced in assessing wound healing and other potential complications related to
cleft surgery. The following team members should perform this assessment:
• Surgeon.
• Patient imaging technician.
• Pediatrician or nurse.
• Speech and/or psychosocial provider (recommended).
Patients should return to a designated site 6 months to 1 year after surgery to be examined for
further assessment of results and needs for further services. The following team members should
perform this assessment:
• Surgeon.
• Patient imaging technician.
• Pediatrician or nurse.
• Speech and/or psychosocial provider (recommended).
Patients undergoing surgical procedures other than cleft lip or cleft palate should have a defined
multi-disciplinary follow-up plan of care to include timeline and procedures/treatments.

40©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 5 – MEDICAL PATIENT MANAGEMENT
Supporting Operation Smile Standard 5 – Policies & Procedures
1. Medication Administration Policy
2. General Anesthesia: Delivery, Monitoring, and Care Policy
3. Local Anesthesia: Delivery, Monitoring, and Care Policy
4. Emergence Delirium and Post-Operative Pain Policy
5. Fluid Management Policy
6. Transfer of Patient Care Policy
7. Throat Pack and Retained Surgical Items Policy
8. Speech, Language, and Feeding Management Policy
9. Psychosocial Care Policy
10. Dental Management Policy
Supporting Operation Smile Standard 5 – Forms
1. Operation Smile Patient Chart
2. Surgical Safety Checklist
3. Operation Smile Patient Care Booklet
4. Nursing Guideline to Cleft Care Education
5. Transfer of Care Form
6. Call Team Communication Form

41©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 5 – MEDICAL PATIENT MANAGEMENT
Supporting Operation Smile Standard 5 – References
Echaniz G, De Miguel M, Merritt G, et al. Bilateral suprazygomatic maxillary nerve blocks vs. infraorbital and palatine nerve
blocks in cleft lip and palate repair: A double-blind, randomised study. Eur J Anaesthesiol. 2019;36(1):40-47.
Feriani G, Hatanaka E, Torloni MR, da Silva EM. Infraorbital nerve block for postoperative pain following cleft lip repair in
children. Cochrane Database Syst Rev. 2016(4):CD011131. doi:10.1002/14651858.CD011131.pub2
Hughes CD, Babagian A, McCormack S, et al. The clinical and economic impact of a sustained program in global
plastic surgery: Valuing cleft care in resource-poor settings. Plast Reconstr Surg. 2012;30(1):87e-94e. doi:10.1097/
PRS.0b013e318254b2a2
Lewis CW, Jacob LS, Lehmann CU; AAP Section on Oral Health. The primary care pediatrician and the care of children
with cleft lip and/or cleft palate. Pediatrics. 2017;139(5):e20170628.
Malherbe V, Bosenberg AT, Lizarraga Lomeli AK, et al. Regional anaesthesia for cleft lip surgery in a developing world
setting. S Afr J Surg. 2014;52(4):108-110. doi:10.7196/SAJS.1917
Mesnil M, Dadure C, Captier G, et al. A new approach for peri-operative analgesia of cleft palate repair in infants: The
bilateral suprazygomatic maxillary nerve block. Paediatr Anaesth. 2010;20(4):343-349.
Michelotti B, Long RE, Leber D, et al. Should surgeons use arm restraints after cleft surgery? Ann Plast Surg.
2012;69(4):387-388.
Patel PB, Hoyler M, Maine R, et al. An opportunity for diagonal development in global surgery: Cleft lip and palate care in
resource-limited settings. Plast Surg Int. 2012;2012:892437. doi:10.1155/2012/892437
Small L, Melnyk BM. Early predictors of post-hospital adjustment problems in critically ill
young children. Res Nurs Health. 2006;29(6):622-635. doi:10.1002/nur.20169
Statement on the Principles of Patient Education. facs.org.
https://www.facs.org/about-acs/statements/85-patient-education. Published May 2, 2016. Accessed Dec. 13, 2019.
Tokioka K, Park S, Sugawara Y, Nakatsuka T. Video recording study of infants undergoing primary cheiloplasty: Are arm
restraints really needed? Cleft Palate Craniofac J. 2009;47(4):494-497.
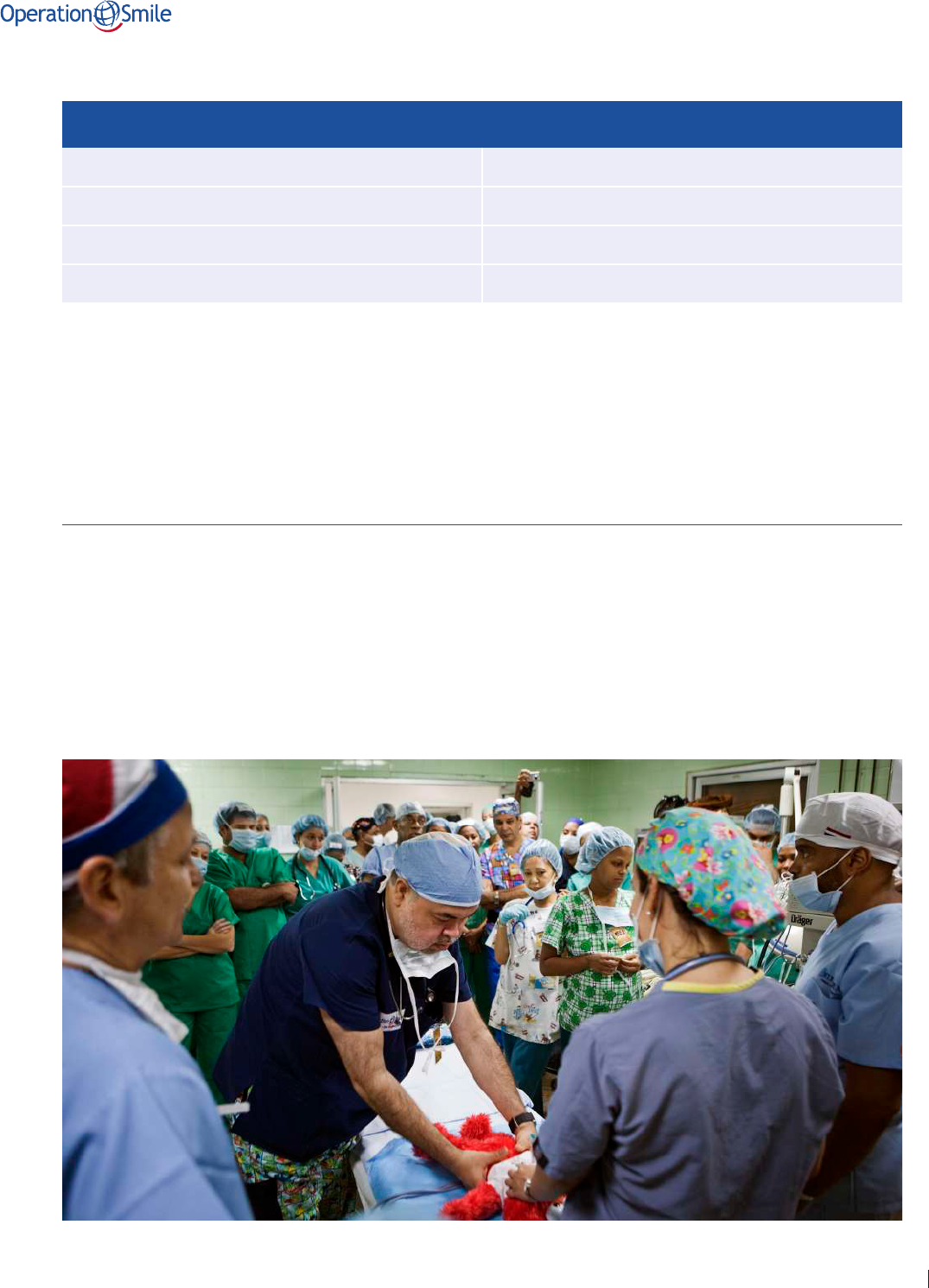
42©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 6 – SAFETY
Medical Global Standard 6 – Safety
Approval Date: June 26, 2020 Replaces: 2015 GS-9
Eective Date: July 1, 2020 Category: Medical Oversight
Current Revision Date: March 2, 2020 Responsible Party: Chief Medical Ocer
Last Review Date: 2015 Review Schedule: 4 years
Operation Smile prioritizes safety for patients, caregivers, and health workers.
Achieving safe, quality care is a multidisciplinary eort. Operation Smile
promotes a culture of safety through the establishment of a safe environment of
care, safe medical practice, availability of necessary equipment and medications,
readiness for unplanned emergencies and secure handling of patient information.
6.1 Emergency Preparedness
Operation Smile provides qualified teams and processes to allow rapid and timely response to
medical events or emergencies.
A Crisis Notification Plan will be in place for all Operation Smile programs and centers to ensure
management of critical events.
Team members should be familiar with equipment, medications, and policies allowing rapid
response to medical events or life-threatening emergencies.

43©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 6 – SAFETY
The following emergency boxes, kits, and equipment must be available, fully stocked, current, and
in working order as applicable:
• Code Box.
• Malignant Hyperthermia Box.
• Dicult Airway Box.
• Dental Emergency Box.
• Post Exposure Prophylaxis Kit.
• Team Kit.
• Defibrillator.
An emergency preparedness drill will be conducted to review and demonstrate equipment
operation and location, and to designate team roles and responsibilities during emergencies.
• Medical Program: drill occurs on the first day of surgery before any procedure begins.
– Night shift personnel: drill occurs at the start of the first post-op night shift.
• Dental Program: drill occurs on the first day of program before any procedures begins.
• Center-based surgical and/or dental services: drill occurs on a regular basis for existing
and new personnel.
For Centers with non-surgical services:
• A basic emergency plan for response capabilities is recommended.
In any surgical setting, the following designated leaders will direct the emergency response
and care:
• Surgical Area – Anesthesia Team Leader
• Post Anesthesia Care Unit – PACU Physician
• Ward – Pediatrician, with assistance from one of the above
In any dental or non-surgical setting, an identified lead medical professional will direct emergency
response and care.
6.2 Blood Transfusion
Operation Smile normally performs elective surgical procedures which mandates screening,
medical clearance, and selection of patients for surgery.
A blood transfusion may NOT be given to elevate an unacceptably low hemoglobin to reach the
accepted threshold value. Those anemic patients should be referred to local medical services for
evaluation and treatment.
A blood transfusion may be given in the course of managing an Operation Smile patient who has
an unanticipated significant surgical blood loss. The blood administered should be cross-matched,
type, and Rh specific whenever time allows. Whenever time is inadequate to crossmatch, type
and RH specific non-cross-matched blood may be transfused. In emergent situations, O negative
or O positive if O negative is unavailable may be used.

44©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 6 – SAFETY
Blood Administration
Safety checks for blood administration that adhere to Operation Smile policy and procedure must
be followed and include the following:
• A physician’s order.
• A check by two medical providers to include the blood label and patient information prior
to administering the blood.
• Close observation during the first 15 minutes of the infusion for potential reaction and
continued monitoring throughout the entire transfusion.
• Use of the Operation Smile Blood Transfusion documentation form.
• Initiation of blood within 30 min of leaving the controlled blood bank refrigerator and
discontinuation of blood within 4 hours.
Blood Transfusion Documentation and Reporting
The medical record of a patient receiving a blood transfusion must contain:
• Signed patient consent to receive blood (found on the surgical consent).
• Blood administration order.
• Blood bank tags identifying the unit(s) administered.
• Completed transfusion record.
A medical event report will be submitted whenever a transfusion is given so that
Operation Smile’s quality assurance program can evaluate the event and track all transfusions.
6.3 Medications
Only non-expired, clearly labeled medications will be used.
Medication substitutions not included in the Operation Smile Pharmacopeia should be approved
by the Regional Medical Ocer or Medical Director.
The chain of custody and integrity of medications should adhere to Operation Smile policy and
local regulation.
Eight Rights of Medication Administration should be observed:
• The right medicine – Clearly identified and labeled.
• The right patient – confirm 2 unique patient identifiers.
• The right dose – double check dose calculation.
• The right time – confirm time of last dose.
• The right route – confirm ordered route.
• The right reason – confirm correct indication.
• The right documentation – verify order before administration and document
AFTER administration.
• The right eect – assess and chart patient response.

45©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 6 – SAFETY
6.4 Communication
Eective communication is essential for safety. Acknowledging and addressing language and
knowledge barriers are essential for clear communication.
Translation/Interpretation
Medical interpreters can bridge language and cultural divides between healthcare providers and/
or patients. Whenever patients/caregivers cannot communicate clearly with an Operation Smile
health care provider because they do not speak the same language, translation/interpretation
should be provided.
Interpreters should be fluent in relevant languages and/or dialects for the setting.
Interpreters should be familiar with medical terminology and concepts appropriate for the setting.
Team Communication
A process for clear, concise, and continuous team communication should be established:
• Between team leaders and team members.
• Between the anesthesia team leader, post anesthesia care physician, clinical coordinator,
and pediatrician to assure safe, continuous care from admission to discharge.
An agreed upon mode of secure communication between team leaders should be established and
utilized for all medical programs.
A clear, consistent form of hand-o communication should be utilized when transferring patient
care from one area/medical team to another. The hand o should be between medical
professionals and include the following information:
• Situation.
• Background.
• Assessment.
• Recommendation.
Patient/Caregiver Communication
Operation Smile acknowledges the rights of patients and the caregivers to be informed and
involved in decision making regarding their care. This is accomplished through mutual respect
and communication as partners in care.
Any medical information shared with a patient and/or caregiver should be communicated by a
medical professional.
Assessment of and attention to language, knowledge, and learning barriers/needs are essential
for clear communication and is known to enhance patient satisfaction.
Each member of the medical care team should communicate to the patient and caregiver their
name, title, and role in care.
Patients and caregivers should be empowered to ask questions and clarify information.

46©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 6 – SAFETY
6.5 Medical Record Documentation
Operation Smile strives to keep an accurate and secure medical record in order to properly
document ongoing medical care and assess patient outcomes. Operation Smile patients should
have a paper and/or electronic record with a distinct identifier for each surgery.
The Operation Smile medical record should include:
• Patient demographic information.
• Photo identification.
• Medical assessment.
• Physical examination.
• Medical and surgical diagnoses.
• Treatment plan including all planned operations or treatments.
• Consent forms.
• Documentation of treatment and patient care.
• Discharge disposition.
Each credentialed team member is responsible for documentation.
Non-credentialed medical providers need a co-signature from a credentialed provider.
Operation Smile patients may have their medical care documented in host country medical charts
by host facility personnel, as required by local regulation. Such documentation DOES NOT replace
Operation Smile’s own required documentation.
Operation Smile programs that utilize an existing hospital system in order to teach and care for
patients, such as visiting professorships and center partnerships, will in some cases utilize host
charting within their own medical records rather than creating Operation Smile medical records.
Confidentiality
Patients are entitled to privacy and the protection of their personal health information (PHI).
Therefore, any patient’s PHI and other confidential information that is shared with
Operation Smile’s providers, or placed in any patient’s Operation Smile medical record is
accessible only to those providers involved in that patient’s medical care or in maintaining
that patient’s medical record, unless the patient/guardian consents to the sharing of that PHI
or the disclosure of that PHI is required by law.
Confidential patient data include:
• Verbal communication with a patient.
• Medical records in either paper or electronic formats.
• Written information about a patient maintained outside the medical record.
• Photos, videos, and voice recordings.
Access to identifiable patient data should be limited to personnel involved in patient care.

47©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 6 – SAFETY
Supporting Operation Smile Standard 6 – Policies and Procedures
1. Blood Transfusion Policy
2. Emergency Preparedness Policy
3. Dicult Airway Management Policy
4. Malignant Hyperthermia Policy
5. Communication Policy
6. Documentation Policy
7. Informed Consent Policy
Supporting Operation Smile Standard 6 – Forms
1. Code Box Inventory
2. Dicult Airway Box Inventory
3. Code Documentation Form
4. Malignant Hyperthermia Box Inventory
5. Malignant Hyperthermia Documentation Form
6. Malignant Hyperthermia Information Poster
7. Blood Component Transfusion Record
8. Blood Request Form
9. Surgical Safety Checklist
10. Dental Emergency Box Inventory

48©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 6 – SAFETY
Supporting Operation Smile Standard 6 – References
Impact of Communication in Healthcare. healthcarecomm.org. https://healthcarecomm.org/about-us/impact-of-
communication-in-healthcare/. Published July 2011. Accessed December 13, 2019.
Medical Records Manual. A Guide for Developing Countries. who.int. http://www.wpro.who.int/publications/docs/
MedicalRecordsManual.pdf. Published 2006. Accessed December 13, 2019.
Medication Safety (2016). Patientsafetyinstitute.ca. https://www.patientsafetyinstitute.ca/en/Topic/Pages/Medication-
Safety.aspx. Accessed December 13, 2019.
Merry AF, Cooper JB, Soyannwo O, et al. International standards for a safe practice of anesthesia 2010. Can J Anaesth.
2010;57(11):1027-1034. doi:10.1007/s12630-010-9381-6.
Meuter RFI, Gallois C, Segalowitz NS, et al. Overcoming language barriers in healthcare: A protocol for investigating
safe and eective communication when patients or clinicians use a second language. BMC Health Serv Res. 2015;15:371.
doi:10.1186/s12913-015-1024-8.
Patient safety. who.int. https://www.who.int/patientsafety/en/. Accessed December 13, 2019.
SBAR Tool: Situation-Background-Assessment-Recommendation. ihi.org. http://www.ihi.org/resources/Pages/Tools/
SBARToolkit.aspx. Accessed December 13, 2019.
Stupnyckyj C, Smolarek S, Reeves C, et al. Changing blood transfusion policy and practice. Am J Nurs. 2014;114(12):50-59.
doi:10.1097/01.NAJ.0000457412.68716.3b
The Clinical Use of Blood. who.int. https://www.who.int/bloodsafety/clinical_use/en/Handbook_EN.pdf. Accessed
December 13, 2019.

49©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 7 – QUALITY
Medical Global Standard 7 – Quality
Approval Date: June 26, 2020 Replaces: GS 17
Eective Date: July 1, 2020 Category: Medical Oversight
Current Revision Date: March 2, 2020 Responsible Party: Chief Medical Ocer
Last Review Date: 2015 Review Schedule: 4 years
Operation Smile’s culture of safety promotes and supports an environment
that encourages quality care, patient safety, risk management, and
transparent reporting.
Quality Assurance (QA) and Quality Improvement (QI) depend on mutual trust,
transparency, collaborative engagement, data collection/analysis and sharing,
thorough evaluation of medical events, and the dissection of organizational
systems that may need to be altered to eect positive change.
Operation Smile’s quality management strategies include:
• Commitment to a culture of safety including patient and volunteer safety.
• Reduction of morbidity and mortality (M&M).
• Improving outcomes other than morbidity and mortality, including
reduction of the inequality in availability of safe and timely surgical care.
• Empowering team members to identify unsafe care and encourage reporting.
• Tracking of medical events and other data to eect system changes.
Operation Smile respects applicable international, national, and local
regulatory requirements.

50©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 7 – QUALITY
7.1 Reporting
Operation Smile endeavors to collect and share accurate data in a timely manner.
Data include:
• Medical Events.
• Center Reports.
• Program Data Reports.
– Medical Oversight Committee Reports.
– Post-operative Patient Evaluations.
– Age, Surgical Procedure and Time Deviations.
– Surgical Table Deviations.
– Biomedical and Instrument Reports.
• Surgical/Patient outcomes.
Data are used to ensure safe clinical practice, to determine quality of interventions, and to
identify trends and analyze factors that facilitate planning and implementation of Quality
Improvement solutions.
7.2 Medical Event Review
Operation Smile’s culture of safety promotes the reporting of medical events. A medical event is
anything that happens or could happen with potential or actual psychologic or physical harm to a
patient, caregiver, or volunteer.
A medical event should abide by the following:
• Transparent and timely event reporting.
• Timely response of medical leaders.
• Joint engagement and quality review after the medical event.
Medical events that cause serious patient harm or death will be analyzed in a peer review
process involving Operation Smile’s Medical Oversight Committee and medical and surgical
specialty advisors.

51©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 7 – QUALITY
7.3 Quality Site Assist Visit
A quality site assist visit is a collaborative process of information gathering, observation, and
analysis in order to enable discussion of findings with those involved in Operation Smile’s
delivery of care.
• The Operation Smile Quality Team should engage with Operation Smile Foundations in site
assist visits and share findings, highlights, and recommendations.
• An after-action report provides mutually identified goals and measurements of success.
• Operation Smile’s Quality and Medical Oversight Teams should collaborate with
Operation Smile Foundations and use the analyses of results and trends to develop
quality improvement initiatives.
7.4 Infection Control Program
Operation Smile’s safety culture involves adherence to infection control practices.
Operation Smile programs and centers will have defined guidelines and programs that include:
• Description and function of the surgical program/dental program/center.
• Basic infection prevention measures, including hand hygiene, disinfection and sterilization,
environmental control, and isolation.
• Specific infection control measures directed at program location or program specific
risk areas.
• Preventive measures to counter spread of infection to and between patients and personnel.
• Appropriate use of antibiotics.
• Infection surveillance measures.
7.5 Surgical Site Infection Prevention
Operation Smile supports the following evidence based global guidelines for the prevention of
surgical site infections:
• Pre-operative hygiene measures.
• Hand hygiene.
• Protective attire – gloves, facemasks, gowns, aprons, footwear.
• Inspection, cleaning, decontamination, and sterilization of surgical instruments prior to use.
• High Level Disinfection (HLD) on any semi-critical instrument/equipment.
• Surface and environmental disinfection practices.
• Administration of prophylactic antibiotics within 1 hour of surgical incision when indicated
and discontinued within 24 hours after surgery.

52©2020 Operation Smile, Inc. operationsmile.org
MEDICAL GLOBAL STANDARD 7 – QUALITY
Supporting Operation Smile Standard 7 – Policies and Procedures
1. Quality Management Policy
2. Infection Control Policy
3. Medical Event Policy
Supporting Operation Smile Standard 7 – Forms
1. Medical Event Report
2. Quality Site Assist Assessment
Supporting Operation Smile Standard 7 – References
Anderson DJ, Podgorny K, Berríos-Torres SI, et al. Strategies to prevent surgical site infections in acute care hospitals: 2014
update. Infect Control Hosp Epidemiol. 2014;35(6):605-627. doi:10.1086/676022
Aznar ML, Schönmeyr B, Echaniz G, et al. Role of postoperative antimicrobials in cleft palate surgery. Plast Reconstr Surg.
2015;136(1):59e-66e. doi: 10.1097/prs.0000000000001324
Clean Care is Safer Care. Global Guidelines on the Prevention of Surgical Site Infection. who.int. https://www.who.int/gpsc/
ssi-guidelines/en/. Published November 3, 2016. Accessed December 13, 2019.
Disinfection and Sterilization. Guideline for Disinfection and Sterilization in Healthcare Facilities. cdc.gov. https://www.cdc.
gov/infectioncontrol/guidelines/disinfection/. Published 2008. Accessed December 13, 2019.
Fast O, Fast C, Fast D, et al. Limited sterile processing capabilities for safe surgery in low-income and middle-income
countries: Experience in the Republic of Congo, Madagascar and Benin. BMJ Global Health. 2017;2:e000428. doi:10.1136/
bmjgh-2017-000428
Hollier L. Discussion: Antibiotic use in primary palatoplasty: A survey of practice patterns, assessment of ecacy, and
proposed guidelines for use. Plast Reconstr Surg. 2016;137(2):583–584. doi:10.1097/01.prs.0000475803.99973.db
Infection Prevention and Control. who.int. https://www.who.int/infection-prevention/en/. Accessed May 4, 2019.
Quality of Care. A Process for Making Strategic Choices in Health Systems. who.int. https://www.who.int/management/
quality/assurance/QualityCare_B.Def.pdf. Published 2006. Accessed December 13, 2019.
Reddy RR, Reddy SG, Banala B, et al. Placement of an antibiotic oral pack on the hard palate after primary cleft
palatoplasty: A randomized controlled trial into the eect on fistula rates. Clin Oral Invest. 2017;22(5):1953–1958.
doi:10.1007/s00784-017-2286-9
Rottgers SA, Camison L, Mai R, et al. Antibiotic use in primary palatoplasty: A survey of practice patterns, assessment
of ecacy, and proposed guidelines for use. Plast Reconstr Surg. 2016;137(2):574–582. doi:10.1097/01.
prs.0000475784.29575.d6
Stanley C, Igala S. Eect of dierent storage conditions on the stability and ecacy of some reconstituted oral antibiotic
suspensions sold in Port Harcourt, Nigeria. JPRI. 2017;20(3):1–10.
