
Implementing Care for
Alcohol & Other Drug Use
in Medical Settings
An Extension of SBIRT
SBIRT Change Guide 1.0
February 2018

Introduction ....................................................................................................................................................................................................................... 1
Overview of Clinical and Organizational Changes Recommended ...................................................................................................3
Clinical Changes .............................................................................................................................................................................................................. 5
Change #1: Screen All Adults At Least Annually ..........................................................................................................................................5
Change #2: Eliciting Symptoms of Alcohol and/or Other Drug Use Disorders ............................................................................. 9
Change #3: Brief Counseling ............................................................................................................................................................................... 13
Change #4: Management of Alcohol or Other Drug Use Disorders ................................................................................................. 16
Change #5: Follow-up with Monitoring ........................................................................................................................................................20
Organizational Changes........................................................................................................................................................................................... 23
Change #6: Leaders Actively Support Improvements ............................................................................................................................ 23
Change #7: Use Quality Improvement Processes .................................................................................................................................... 26
Change #8: Train Primary Care Teams .......................................................................................................................................................... 28
Change #9: Billing and Identifying Revenues for Alcohol and/or Other Drug Care ................................................................ 30
Appendix ........................................................................................................................................................................................................................... 32
Change #1 Resources: Screen All Adults At Least Annually ............................................................................................................... 32
Change #2 Resources: Eliciting Symptoms ................................................................................................................................................ 34
Change #3 Resources: Brief Counseling ..................................................................................................................................................... 35
Change #4 Resources: Management .............................................................................................................................................................37
Change #5 Resources: Monitoring .................................................................................................................................................................40
Change #8 Resources: Train Primary Care Teams .................................................................................................................................. 42
Change #9 Resources: Billing and Finances .............................................................................................................................................. 43
The Current State of SBIRT in Practice and Research ..........................................................................................................................47
References ........................................................................................................................................................................................................................ 49
This SBIRT Change Guide was developed by the National Council for Behavioral Health with funding from the Substance
Abuse and Mental Health Services Administration (SAMHSA) contract no. HHSP233201600258A (February 2018).
SBIRT CHANGE GUIDE 1.0

Katharine Bradley, MD, MPH
Practice Transformation Team Chair
Senior Investigator, Kaiser Permanente Washington
Health Research Institute
Henry Chung, MD
Practice Transformation Team Advisor
Senior Medical Director, Behavioral Health Integration;
Strategy Montefiore Care Management Organization
Professor of Psychiatry, Albert Einstein College of
Medicine
Richard L. Brown, MD, MPH
Professor, University of Wisconsin Department of Family
Medicine and Community Health
Tillman Farley, MD
Chief Medical Ocer, Salud Family Health Centers
Leigh Fischer, MPH
Associate, Abt Associates
Eric Goplerud, PhD
Vice President, National Opinion Research Center;
(NORC) at the University of Chicago Senior Fellow,
NORC at the University of Chicago
Sandeep Kapoor, MD
Director, SBIRT, Division of General Internal Medicine,
Department of Emergency Medicine, Department of
Psychiatry/Behavioral Health, Northwell Health
Hillary Kunins, MD, MPH, MS
Assistant Commissioner, Bureau of Alcohol and Drug
Use, New York City Department of Health and Mental
Hygiene; Clinical Professor, Departments of Medicine,
Psychiatry and Behavioral Sciences, Family and Social
Medicine, Albert Einstein College of Medicine
Richard Saitz, MD, MPH
Chair and Professor of Community Health Sciences
(CHS), Boston University School of Public Health;
Professor of Medicine, Boston University School of
Medicine
Mary Velasquez, PhD
Professor and Director, Health Behavior Research and
Training Institute, The University of Texas at Austin
School of Social Work
Acknowledgements
SBIRT Change Guide Expert Panel

Jake Bowling, MSW
Senior Advisor, Policy and Practice Improvement,
National Council for Behavioral Health
Reed Forman, MSW
Lead Public Health Advisor, SAMHSA
Tom Hill, MSW
Vice President, Addictions and Recovery, National
Council for Behavioral Health
Chuck Ingoglia, MSW
Senior Vice President, Public Policy and Practice
Improvement, National Council for Behavioral Health
Brie Reimann, MPA
Director, SAMHSA-HRSA Center for Integrated Health
Solutions, National Council for Behavioral Health
Pam Pietruszewski, MA
Integrated Health Consultant, National Council for
Behavioral Health
Nick Szubiak, MSW, LCSW
Director, Clinical Excellence in Addictions, National
Council for Behavioral Health; Integrated Health
Consultant, National Council for Behavioral Health
Mohini Venkatesh, MPH
Vice President, Policy and Practice Improvement,
National Council for Behavioral Health
Aaron Williams, MA
Senior Director, Training and Technical Assistance for
Substance Use, National Council for Behavioral Health
Consultant, Substance Abuse and Mental Health
Services Administration (SAMHSA)/Health Resources
and Service Administration (HRSA) Center for Integrated
Health Solutions
Teresa Halliday, MA
Director, Practice Improvement, National Council for
Behavioral Health
Julia Schreiber, MPH
Project Manager, National Council for Behavioral Health
Sharday Lewis, MPH
Project Manager, National Council for Behavioral Health
Alexandra Meade
Project Coordinator, National Council for Behavioral
Health
Stephanie Swanson
Project Assistant, National Council for Behavioral Health
Megan O’Grady, PhD
Technical Writer; Research Scientist & Associate
Director of Health Services Research, the National
Center on Addiction and Substance Abuse
Acknowledgements, CONT.
Other Contributing Experts Project Management Team

1
T
his change guide is designed to assist primary care clinicians and leaders to integrate care for patients with
unhealthy alcohol and/or other drug use into routine medical care. As behavioral health care is increasingly
integrated into medical settings, especially primary care, the focus is often on depression and anxiety. Care for
alcohol and/or other drugs is often omitted or minimized, likely reflecting: stigma, lack of workforce training/education,
and the traditional separation of care for alcohol and other drugs from traditional health care (e.g., primary care,
emergency care, and behavioral health, etc.). This guide expands on and updates the widely recognized model of
Screening, Brief Intervention, and Referral to Treatment (SBIRT).
1-3
The SBIRT change guide is organized around nine significant changes that most practices need to make to improve
alcohol and/or other drug-related care based a consensus of the authors. Five changes relate to components of clinical
care and four changes address organizational requirements for implementation of the five clinical changes (Figure 1).
Changes #1-3 overlap with the traditional SBIRT model. However, in this guide, “referral to treatment” — the RT in SBIRT
— becomes part of a broader program of management in primary care. This reflects the availability of both evidence-
based medications and ongoing follow-up and counseling that can be provided in primary care (clinical Changes
#4 and #5), independently or in conjunction with specialty addiction treatment.
Each section outlines the rationale for the change, the specific practices recommended, workflow considerations or
components of implementation, and how to measure progress on the recommended change(s) with a recommended
target or “benchmark”. This model, which “extends” the SBIRT model, is intended to support practice improvement and
integration of care for alcohol and/or other drug use into medical settings, as it builds on previous SBIRT guides. Primary
care practices that are already oering SBI for alcohol may also benefit from adding management and monitoring of
alcohol and/or other drug use in primary care. It is not expected that all the changes be implemented at the same time.
Instead, practices can prioritize which changes to implement based on organizational need, resources, and readiness.
Introduction
Figure 1. Overview of the Changes Needed to Address Alcohol and/or Other Drug Use in Primary Care
Clinical Changes Needed Organizational Changes Needed
#6: Leaders actively support
improvements
#7: Use quality improvement
processes
#8: Primary care workforce is trained
in alcohol- and/or other drug-related care
#9: Bill and identify other financial resources
for alcohol- and/or other drug-related care
#1: Screen all adults at least annually
#2: Elicit symptoms
#3: Brief counseling
#4: Manage use
disorders
#5: Follow-up w/
monitoring

2
The Clinical Changes Outlined in Figure 1 are:
(1) Screen all adults at least annually for unhealthy alcohol use
4, 5
and other drug use as part of population-based
prevention and treatment.
(2) Elicit symptoms related to alcohol and/or other drug use from patients with high-positive screens.
(3) Oer brief counseling for unhealthy alcohol
4, 5
and/or other drug use at least annually to all patients with positive
screens.
(4) Manage alcohol and other drug use disorders using shared decision-making
6
to oer medications, counseling,
peer support, referral to specialty addiction treatment programs, and/or home-based services.
(5) Follow-up with monitoring for patients with high-positive screens or symptoms of alcohol and/or other drug
use disorders.
The Organizational Changes Outlined in Figure 1 are:
(6) Leaders actively support improvements in care for patients with unhealthy alcohol and/or other drug use.
(7) Use quality improvement processes to implement each of the five clinical changes.
(8) Train primary care workforce to manage alcohol and other drug use, and/or use disorders, as appropriate.
(9) Bill and identify other financial resources for alcohol and/or other drug related care.
Measuring Successful Change(s). This guide includes recommended metrics for each clinical and organizational change.
They can be used to monitor implementation, inform quality improvement eorts, and quantify progress. Quality
improvement and data system infrastructures are an essential foundation for implementation of improved alcohol- and/
or other drug-related care.
6-8
In most cases, these metrics and benchmarks are based on consensus recommendations
by authors.
Introduction, CONT.

3
Overview: Recommended Clinical & Organizational Changes
Screen all adult patients (≥ 18 years old) for alcohol and other drug use, at least annually, using a structured screening
tool and document the screen scores in the patient’s medical record.
CLINICAL CHANGES
Change #1: Screen All Adults at Least Annually
Use the AUDIT-C for alcohol screening and single-item screening questions for cannabis and other drug use
(AUDIT-C Plus 2).
•
Use a structured questionnaire to assess and document alcohol- and/or other drug-related symptoms if:
Change #2: Eliciting Symptoms
Patients have “high-positive” screening results; and/or
Patients have a clinical evaluation that suggests possible alcohol and/or other drug use disorder.
Use recommended Symptoms Checklists or other validated approaches to elicit alcohol- and drug-related symptoms.
Record questionnaire scores and results in the electronic health record (EHR).
Use patients’ symptoms as a way to engage them in discussions of alcohol- and/or other drug use.
•
•
•
•
•
Oer brief counseling at least once a year for unhealthy alcohol and/or other drug use to all patients with positive screens.
Change #3: Brief Counseling
•
•
•
Patients with unhealthy alcohol use should be oered patient-centered advice about recommended limits and
feedback linking alcohol use to relevant health conditions, based on U.S. Prevention Services Task Force recommendation.
Similar counseling can be oered for cannabis use monthly or more often.
For the subset of patients with high-positive alcohol or other drug screens, experts recommend that patients be
offered ongoing, patient-centered brief counseling, repeated at every visit, in addition to care in Changes #4 and #5.
Manage patients with alcohol- and/or other drug-related symptoms: oer repeated visits for brief counseling and shared
decision-making regarding treatment options and referral, as appropriate.
Change #4: Management
Oer patients shared decision-making about five types of options — medications, one-on-one counseling, peer
support, group-based addiction treatment and patient resources for self-management — including providing referral
for services not provided in primary care, as needed.
•
•
•
Continue ongoing brief counseling as above (i.e. repeated visits with primary care provider, integrated mental health
clinician or specialty addiction treatment, per patient preference).
Adapt care based on results of monitoring, changes in symptoms and patient preferences over time.
Arrange follow-up to monitor alcohol and/or other drug use and symptoms with a structured tool in all patients with high-
positive alcohol and/or other drug screens, or reporting symptoms on the Symptom Checklist.
Change #5: Follow-up with Monitoring
Select a tool for monitoring patients with symptoms.
At a minimum, monitor alcohol and/or other drug use and related symptoms, with repeated brief counseling.
Track alcohol and/or other drug use and symptoms (ideally with a population-based EHR registry).
•
•
•

4
Overview: Recommended Clinical & Organizational Changes
Leaders actively support improvements in alcohol and other drug-related care.
ORGANIZATIONAL CHANGES
Change #6: Leaders Actively Support Improvements
All leaders actively articulate the rationale for improving alcohol- and other drug-related care.
•
•
Use population-based quality improvement processes for each of the five clinical changes.
Change #7: Use Quality Improvement Processes
Assess current gaps in alcohol- and other drug-related care.
Prioritize critical changes to implement (Changes #1 to #5).
Local implementation team (champions) meets regularly; pilot, then implement.
Monitor metrics and set up a quality improvement system, e.g. Plan-Do-Check-Act (PDCA).
Demonstrate progress on selected change concepts at six months.
•
•
•
•
•
Train primary care teams to address alcohol and other drug use and use disorders in primary care, as appropriate.
Change #8: Train Primary Care Teams
Assess training needs of key sta required for each change.
•
•
Plan training for the entire primary care team (e.g. front desk, sta who conduct patient intakes, primary care clinicians,
behavioral health clinicians), including ongoing assessment of needs and new sta onboarding.
Bill for screening, brief counseling, management, and monitoring, and explore other revenue sources to support the cost
of provision of alcohol- and/or other drug-related services in primary care.
Change #9: Billing and Identifying Other Revenue
If appropriate, use screening and brief intervention, collaborative care or care coordination billing codes.
•
•
Develop a financial model where revenue covers the cost of delivery of alcohol- and other drug-related services.
Leaders select change(s) to implement, identify sta to lead the improvement eort, provide time and resources to
support implementation, set expectations for targets/timing and monitor and provide feedback on performance.

5
Screening identifies patients who are at risk of health or other problems related to their use of alcohol and/or other
drugs, as well as those who have already developed problems.
Unhealthy alcohol and other drug use are common. One in eight adults consumes alcohol at unhealthy levels
and one in 10 people in the U.S. use other drugs.
9
Many patients with alcohol and drug use problems are seen in
primary care
10
; screening and treating these conditions are consistent with patient-centered care.
For unhealthy alcohol use
11
, screening and brief counseling—ongoing on repeated occasions—is one
of the highest prevention priorities recommended by the U.S. Preventive Services Task Force (USPSTF)
4, 5
based
on cost-effectiveness and burden of preventable disease.
12
For other drug use, screening allows clinicians to open a dialogue with patients about symptoms and other
eects on their health and lives.
Knowing about patients’ alcohol and/or other drug
use is critical to high-quality medical care. Just as
for tobacco use, this information helps clinicians to
properly diagnose, prescribe medications,
13, 14
and
support self-management for chronic diseases (e.g.,
hypertension,
15
diabetes,
15, 16
hepatitis C virus
17, 18
).
Most patients are willing to discuss their alcohol
and drug use and its connection to health
19
and
screening has been associated with improved
patient satisfaction in several studies.
20
Clinical Changes
Change #1: Screen All Adults At Least Annually
For individuals at risk for or diagnosed
with chronic health conditions
(cardiovascular disease, diabetes,
stroke, cancer, among others), alcohol
and other drug use impacts treatment
outcomes via treatment adherence,
medication interactions, and
physiological eects of alcohol and/or
other drug use.
Rationale for Screening
•
•
•
•
•
POPULATIONBASED SCREENING FOR UNHEALTHY ALCOHOL AND OTHER DRUG USE
Screen all adult patients (≥ 18 years old) for alcohol and other drug use, at least annually, using a structured
screening tool and document the screen scores in the patient’s medical record.
Recommendation
Metric
Benchmark
Use the AUDIT-C Plus 2 which combines screens for alcohol (three items), cannabis (one item) and
other drugs (one item), each scored independently.
Proportion of patients with screening results documented.
80%

6
Recommended Screening Tool: The AUDIT-C PLUS 2
Screening tools are available that vary in length, time
needed to administer, and type of drug screened.
3, 21-25
There are a number of factors to consider when
selecting a screening tool for a particular clinical setting
— time needed to administer, validity and reliability, ease
of use, and workforce training are just a few. Screens that
allow patient self-administration are most ecient and
speed workflow. Screening tools that take more than
a few minutes to administer may limit the feasibility of
screening all primary care patients at least annually. This
screen combines validated brief screens for alcohol and
other drugs that are easy for patients to answer, yet useful
for monitoring changes over time. It can be combined
with screening for depression and/or tobacco use.
AUDIT-C Plus 2 Screening Questions
1
* if patient needs further explanation, “for example, for the feeling or experience it caused.”
1
The AUDIT-C has been validated with a past-year timeframe and without any timeframe. The authors recommend a past 3-month timeframe so the
AUDIT-C can be used for monitoring (“Change #5”).
Change #1: Screen All Adults At Least Annually, CONT.
Varying cultural perceptions of alcohol
and other drug use requires clinicians
to implement cultural adaptations to
eectively support diverse populations.
Special attention must be given to
validated screeners, appropriate use
of language/literacy, trust building,
and incorporation of patient and
community healthcare preferences.
To start, consider selecting tools that
are validated in multiple languages,
such as the AUDIT-C.
Click to Access a PDF of the AUDIT-C Plus 2
In the past 3 months...
1. How often did you have
a drink containing alcohol?
2. How many drinks
containing alcohol did you
have on a typical day when
you were drinking?
3. How often did you have
5 or more drinks on one
occasion?
4. How often have you
used marijuana?
5. How often have you
used an illegal drug or a
prescription medication for
non-medical reasons*?
Never
0
Monthly or less
1
2-4 times a month
2-3 times a week 4+ times a week
2 3 4
Never
1 or 2
drinks
0 0 1 2 4
3 or 4
drinks
5 or 6
drinks
7, 8 or 9
drinks
10 or more
drinks
3
Never
0
Less than
monthly
1
Monthly
Weekly
Daily or
almost daily
2 3 4
Never
0
Not monthly
1
Monthly
Weekly Daily or almost
2 3 4
Never
0
Less than
monthly
1
Monthly Weekly
Daily or
almost daily
2 3 4

7
INTERPRETING SCREENING RESULTS
This table shows the recommended screening thresholds and clinical implications for the AUDIT-C Plus 2.
3, 26
See the
Appendix for more information on why these screens are recommended.
Change #1: Screen All Adults At Least Annually, CONT.
Click to Access a PDF of the Interpreting
AUDIT-C Plus 2 Screening Results Table
Table 1.1 Interpreting AUDIT-C Plus 2 Screening Results
Screening Measure
Consider oering positive feedback and
educating patients who drink and use
cannabis about:
•
Recommended drinking limits
27
Screening Results Interpretation Clinical Guidance
AUDIT-C
(0-12 points)
Women: < 3 points
Men: < 4 points
Cannabis question
(0-4 points)
0-1 points
(0 or < monthly)
Other drugs question
(0-4 points)
0 points
(no use)
AUDIT-C
(0-12 points)
Women:
3-6 points
Men:
4-6 points
Cannabis question
(0-4 points)
2-3 points
(monthly or
weekly)
AUDIT-C
(0-12 points)
≥ 7 points
30, 31
Cannabis question
(0-4 points)
4 points
(daily or almost)
Other drugs question
(0-4 points)
1-4 points
(any use)
Negative Screen —
lowest risk (if no
contraindications
for drinking or
cannabis use)
Positive Screen —
drinks or uses
cannabis regularly,
at levels that can
impact health
High Positive Screen —
drinks, uses cannabis
and/or other drugs at
a level that is more
likely to impact health
and therefore needs
further assessment
Low-risk cannabis use.
28
Health risks of alcohol (e.g. cancers,
driving after drinking, pregnancy or
planning)
29
and cannabis use (e.g.
impaired driving, use disorder).
28
•
•
•
Brief counseling per Key Elements in
a patient-centered manner consistent
with motivational interviewing:
Begin conversation, build rapport
Provide feedback on screening
Provide advice or recommendation
Support patient in setting a goal
and/or making a plan
•
•
•
•
•
Elicit symptoms (Change #2)
Ongoing brief counseling (Change #3)
Manage alcohol and/or other drug use
disorders (Change #4)
Follow-up monitoring of use and
symptoms and progress towards goal
(Change #5)
•
•
•
•

8
The recommended target rate (benchmark) for alcohol and/or other drug screening is 80 percent (rather than 100%)
because patients who are in hospice, cognitively impaired, in acute pain, or acutely medically or psychiatrically unstable
may not be appropriate for screening. The screening questions can also be used to monitor patient alcohol or other
drug use over time
34
(see Change #5), so that they are appropriate even for patients who have previously screened
positive or been diagnosed with alcohol or other drug use disorders (who do not need to be “screened,” per se).
Change #1: Screen All Adults At Least Annually, CONT.
Using Metrics to Measure Changes in Screening Rates Over Time
What will you screen for—alcohol only or cannabis and/or other drug use, too? This guide recommends
screening for alcohol, cannabis, and other drugs with five questions; however, you should consider what is most
feasible for your practice.
Will it be combined with a screen for other behavioral health issues? This guide recommends to add the PHQ-2
for depression, if depression screening is not already in place.
32
How often will you screen: annually, at each visit, other? This guide recommends that patients are screened at
least annually.
How will screening questions be administered: computer, paper, sta interview? The most accurate responses
are obtained if patients complete self-report paper or tablets, since reliability of interviews can be low (insensitive
33
).
Results should then be recorded in an EHR.
Will screening questions be built into your EHR? This is recommended, if possible. Alcohol screening should be
entered where other behavioral health screens are entered (e.g., PHQ-2 for depression) so that clinicians can see
responses to individual questions, as well as look at trends for scores over time (for monitoring)—(Change #5). If
so, work with a programmer or EHR vendor early in your implementation process.
How will clinicians be sure to see results of screening at the point of care? Most practices learn that entering
results into the EHR before the clinician sees a patient—if possible—is optimal. This allows for a prompt to the team
for follow-up care (Change #2-4). If clinical sta who do vitals or “room” patients are available, they can ask the
patient to complete a Symptom Checklist to assess for alcohol or drug use disorders, if appropriate (Change #2);
clip a patient handout to the chart or enter a template into the EHR to prompt brief counseling (Change #3); or
alert the clinicians to high-positive screens that needs follow-up.
WORKFLOW CONSIDERATIONS FOR SCREENING

9
Change #2: Eliciting Symptoms of Alcohol and/or Other Drug Use Disorders
A positive alcohol or other drug use screen identifies the spectrum of unhealthy alcohol and drug use from “risky” use
that has not yet caused the patient any problems, to alcohol or other drug use disorders with severe impairment.
30, 31
Eliciting symptoms of alcohol and/or other drug use disorders can help determine where patients are on that spectrum.
Patients’ alcohol and other drug-related symptoms may be powerful motivators of change.
The recommended Symptom Checklists include:
Common problems people have due to alcohol or other drug use,
35
and
The 11 criteria for alcohol and/or other drug use disorders, according to the Diagnostic and Statistical
Manual 5
th
edition (DSM-5).
36, 37
The number of symptoms reflects the severity of alcohol or other drug use disorders.
38, 39
As the number of symptoms increases, readiness to change generally increases.
40
Once a patient identifies a symptom, the clinician can elicit more details (e.g., “You indicated you sometimes drink
more than you want, can you tell me more about that?”).
RATIONALE FOR ELICITING SYMPTOMS
•
•
•
•
•
•
•
Use a structured questionnaire to assess and document alcohol- and/or other drug-related symptoms if:
Recommendation
Metric
Benchmark
Use the recommended Symptom Checklist with a three-month timeframe or a validated
approach to elicit common symptoms.
Among those with high-positive screen scores, proportion of patients who have documented
assessment of alcohol- and/or other drug-related symptoms in their medical record.
80%
Patients have “high-positive” screening results (e.g., AUDIT-C scores of 7-12 points, daily cannabis
use, any other drug use); and/or
Patients have a clinical evaluation that suggests possible alcohol and/or other drug use disorder.
•
•
Record results of questions and scores in the EHR.
Use patients’ symptoms to engage them in discussions about alcohol and/or other drug use.
•
•
•

10
When Should Symptoms of Alcohol or other Drug Use Disorders Be Elicited?
Symptoms due to alcohol and/or other drug use disorders should be elicited with a standardized tool if patients:
Score “high-positive” on an alcohol or other drug screen (Table 1).
14, 33, 41-53
Are trying to change their alcohol and/or other drug use, but have been unable.
Might benefit from a medication for alcohol or opioid use disorder.
Symptom assessment can also be triggered by other clinical factors such as: vital signs that suggest withdrawal (e.g.,
blood pressure, pulse), lab work suggesting alcohol and/or other drug use disorders
54
(e.g., abnormal liver enzymes),
medications that could be addictive (e.g., opioids, benzodiazepines), psychiatric/medical co-morbidities, and/or severe
social or other life problems due to alcohol and/or other drug use.
Symptom Checklists for Problems Due to Alcohol and Other Drugs
This guide recommends simple Symptom Checklists with 11 items that can be completed quickly and eciently. The
checklists are based on the DSM-5 diagnostic criteria for alcohol or other drug use disorders
36, 37
with a past three-
month timeframe so symptoms can be monitored over time. Elicitation of these symptoms can be used to engage
patients in discussions of alcohol- and/or other drug-related problems.
55
The Symptom Checklist can assist with making
a diagnosis.
36, 37
The 11 criteria are used to determine the presence of an alcohol or other drug use disorder.
2-3 symptoms indicate mild alcohol and/or other drug use disorder.
4-5 symptoms indicate moderate alcohol and/or other drug use disorder.
6+ symptoms indicate severe alcohol and/or other drug use disorder.
Medication treatment is an option for moderate to severe for alcohol or opioid use disorders (four or more symptoms).
Change #2: Eliciting Symptoms of Alcohol, Other Drug Use Disorders, CONT.
•
•
•
•
•
•

11
Access a PDF of the Symptom Checklists
Change #2: Eliciting Symptoms of Alcohol, Other Drug Use Disorders, CONT.
Alcohol Symptom Checklist Other Drugs Symptom Checklist
In the past three months, have you: In the past three months, have you:
Had times when you ended up drinking more, or
for longer than you intended?
More than once, wanted to cut down or stop
drinking, or tried to, but couldn’t?
Spent a lot of time drinking, being sick after
drinking, or getting over the after-eects?
Experienced craving — a strong need, or urge, to
drink?
Found that drinking — or being sick from
drinking — often interfered with taking care of
your home or family, caused job troubles or
school problems?
Continued to drink even though it was causing
trouble with your family or friends?
Given up or cut back on activities that were
important or interesting to you, or gave you
pleasure, in order to drink?
More than once, gotten into situations while or
after drinking that increased your chances of
getting hurt (such as driving, swimming, using
machinery, walking in a dangerous area or
having unsafe sex)?
Continued to drink even though it was making
you feel depressed or anxious or adding to
another health problem, or after having had a
memory blackout?
Had to drink much more than you once did to
get the eect you want, or found that your usual
number of drinks had much less eect than
before?
Found that when the eects of alcohol were
wearing o, you had withdrawal symptoms, such
as trouble sleeping, shakiness, irritability, anxiety,
depression, restlessness, nausea or sweating, or
sensed things that were not there?
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
Y N
Y N
Y N
Y N
Y N
Y N
Y N
Y N
Y N
Y N
Y N
Had times when you ended up using drugs
more, or for longer than you intended?
More than once, wanted to cut down or stop
using drugs, or tried to, but couldn’t?
Spent a lot of time using drugs, being sick after
use, or getting over the after-eects?
Experienced craving — a strong need, or urge, to
use drugs?
Found that using drugs — or being sick from
using drugs — often interfered with taking care
of your home or family, caused job troubles or
school problems?
Continued to use drugs even though it was
causing trouble with your family or friends?
Given up or cut back on activities that were
important or interesting to you, or gave you
pleasure, in order to use drugs?
More than once, gotten into situations while or
after using drugs that increased your chances
of getting hurt (such as driving, swimming,
using machinery, walking in a dangerous area or
having unsafe sex)?
Continued to use drugs even though it was
making you feel depressed or anxious or adding
to another health problem, or after having had a
memory blackout?
Had to use drugs much more than you once did
to get the eect you want, or found that your
usual number of drinks had much less eect
than before?
Found that when the eects of drugs were
wearing o, you had withdrawal symptoms, such
as trouble sleeping, shakiness, irritability, anxiety,
depression, restlessness, nausea or sweating, or
sensed things that were not there?
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
Y N
Y N
Y N
Y N
Y N
Y N
Y N
Y N
Y N
Y N
Y N

12
The recommended target rate (benchmark) for completion of alcohol and/or other drug Symptom Checklists is 80
percent among those with high-positive screen scores. This is not 100 percent because these assessments may not be
appropriate for patients who are in hospice, cognitively impaired, in acute pain, or acutely medically or psychiatrically
unstable, or when other more urgent clinical matters need to be prioritized.
Change #2: Eliciting Symptoms of Alcohol, Other Drug Use Disorders, CONT.
Measuring the Proportion of Eligible Patients Who Complete Symptom Checklists
How soon after a high positive screen should symptoms be elicited? Ideally, symptoms can be assessed the
same day as a high positive screen, but if there are competing priorities that make that impossible, this guide
recommends eliciting symptoms within 3 visits.
Which healthcare clinician or sta will administer the Symptoms Checklist? One approach is to have the person
who rooms patients collect screens and give the Symptom Checklist to patients to fill out before the appointment.
How often will the checklist be administered once a patient has screened as high-positive? At the time of a
high-positive screen and annually thereafter, unless it is being used for monitoring.
Will Symptom Checklists be built into the EHR? If yes, it is recommended that you start working with a programmer
or your EHR vendor very early in your implementation process.
Who will enter results into the EHR so that they can be monitored over time? The person who gives patients
the questionnaires can typically enter results into the EHR at the same time so they are available for all clinicians.
WORKFLOW CONSIDERATIONS FOR ELICITING SYMPTOMS

13
Change #3: Brief Counseling
Brief counseling for unhealthy alcohol use results in decreased drinking among adults with unhealthy alcohol use.
4, 5
Given
the burden of preventable alcohol-related health conditions, and the possible cost-eectiveness of brief counseling,
57
the U.S. Commission on Prevention Priorities ranked brief alcohol counseling one of highest priority preventive services
for U.S. adults.
12
While brief counseling on one or two occasions has not been shown to decrease use of other drugs, one study with
repeated brief counseling suggested it may be eective.
58
Patient-centered discussions about drug use can also help
identify drug use disorders, so that patients can be oered treatment.
The specific elements of brief counseling for patients with unhealthy alcohol and/or other drug use are outlined below
in Table 2, broken into three groups based on the results of screening. However, the frequency and intensity of brief
counseling will depend on the severity of alcohol and/or other drug use, as reflected by the screening score(s) and
drug(s) used, symptoms of alcohol and/or other drug use disorders(s), and clinical knowledge of the patient.
Why Oer Brief Counseling for Unhealthy Alcohol and/or Other Drug Use?
Oer brief counseling at least once a year for unhealthy alcohol and/or other drug use to all patients with
positive screens.
Recommendation
Metric
Benchmark
Patients with unhealthy alcohol use should be oered patient-centered advice about
recommended limits
27
and feedback linking alcohol use to health conditions relevant to the
patient,
56
based on USPSTF recommendation.
4, 5
Among patients with positive screens for alcohol and/or other drug use, the proportion who have
brief counseling documented in their medical records in the last year.
80%
Similar counseling can be oered to patients with at least weekly-to-monthly cannabis use.
28
For the subset of patients with high-positive alcohol or other drug screens, experts recommend
that patients be oered ongoing, patient-centered brief counseling, repeated at every visit, in
addition to care outlined in Changes #4-5.
•
•
•

14
Change #3: Brief Counseling, CONT.
TABLE 2. KEY ELEMENTS OF BRIEF COUNSELING
In this section, expert opinion is outlined on elements of brief counseling that can be oered by primary care
clinicians, or expanded on by behavioral health clinicians who practice in primary care. All elements are
offered using the style and skills from Motivational Interviewing (MI). Components of MI are: open-ended
questions, reflective listening, asking permission before offering advice, eliciting the patient’s perspective after
information is provided, and eliciting statements from the patient for why they want to change. It’s recommended
the clinician elicit the patient’s thoughts. Any goal setting should be arrived at using shared decision-making.
1. Begin the conversation—build rapport
The first task is to build rapport and communicate caring, concern, and non-judgment. Elements included are:
Ask patients if it is okay with them to discuss alcohol and/or other drug use. This can be repeated with each
step below (“Is it okay if I provide some information on results of your screening?”).
Ask open-ended questions about how alcohol and drugs fit into the patient’s life. Explore what types of
alcohol they drink and/or which other drugs they use, with whom, when, where (“Tell me about…”).
2. Provide feedback on results of screening and assessment
The next task is to share with the patient the relevance of alcohol and/or other drug use to his/her health, while
making it clear the clinician respects the patient to make the choices that are right for him/her.
Explore the patient’s experience (“When you completed our form you noted sometimes you are drinking
more than you want. Can you tell me about that?”).
Connect alcohol and/or other drug use to health: specifically link alcohol and/or other drug use to any
symptoms or conditions the patient has or is concerned about, if possible. (“While I hear that drinking is a
critical part of your social life, I’m concerned it may be raising your blood glucose.”)
Elicit patients’ thoughts (“What do you make of this information?”).
3. Provide advice or a clinical recommendation
Recommendations depend on the patient, drug(s) used, severity of use and symptoms, and resources. Management
of patients with high-positive screens, symptoms, or alcohol and/or other drug use disorders are addressed in Change
#4, but brief counseling based on MI and decision-making provides the foundation of ongoing management.
For alcohol, all patients should be advised about recommended drinking limits that decrease the risk of
developing or re-developing adverse consequences due to drinking (National Institute on Alcohol Abuse
and Alcoholism [NIAAA] provides guidelines on recommended limits).
For less than daily cannabis use, explore reasons for use (medical, recreational) and ways to minimize health risks.
For patients with alcohol and/or other drug use disorders, stopping use improves outcomes.
Give patients the opportunity to express desires, reasons, commitment, and ability to change.
4. Support the patient in setting a goal and making a plan
Explore options that the patient feels are realistic and obtainable.
Arrange follow-up to monitor and adapt management.
•
•
•
•
•
•
•
•
•
•
•
15
Using Metrics to Measure Changes in Counseling Rates Over Time
If screening is recorded with an EHR registry, measurement of documented brief counseling can also use the EHR
registry, either through a field that notes this was done, via billing codes, or non-billable z-codes. If paper charts are
used, then some number of chart reviews for patients who had positive screens can be performed to assess “crude” brief
counseling percentages.
WORKFLOW CONSIDERATIONS FOR BRIEF COUNSELING
Which healthcare clinicians or sta will oer ongoing brief counseling? Often this will be provided by the primary
care clinician but sometimes, when a patient has a high-positive screen, alcohol or other drug use disorder, or other
mental health conditions, a warm hand-o to an integrated behavioral health clinician (if available) is optimal.
How often will brief counseling be provided? This will depend on the severity of symptoms (if any) and the resources
of the medical setting. At a minimum, patients with alcohol and/or other drug use disorders should be scheduled for
follow-up and monitoring quarterly, even if they are not interested in treatment.
When does brief counseling fit in during the visit? Oering brief counseling can often be linked to the chief complaint
(e.g., hypertension, insomnia, fracture) or can be added at the end of the appointment after asking permission to discuss
the patient’s screening. If the counseling is oered by an integrated behavioral health clinician, it can be after the
appointment with the primary care clinician.
How will the brief counseling session be documented? If counseling is part of an appointment billed with an E&M
code, the counseling can be documented with a non-billable z-code. When a warm hand-o to an integrated behavioral
health clinician occurs, brief counseling can be documented with an SBI code if >15 minutes and not part of another
appointment.
Change #3: Brief Counseling, CONT.

16
Rationale for Managing Alcohol and/or Other Drug Use in Primary Care
Alcohol and/or other drug use disorders are common conditions appropriate for long-term primary care.
64
Management in primary care oers patients more immediate care within a familiar system.
65
Specialty addiction treatment is often not available.
Many patients don’t feel like their problems require
“treatment,” so they don’t accept a referral,
66, 67
but
they can succeed in patient-centered primary care.
Even when patients do accept referral to specialty
treatment, drop-out rates may be high, and unless
patients are treated with medications, treatment is
usually short-term (12 weeks), and many patients still
need chronic management in primary care.
A number of studies have demonstrated how
alcohol and/or opioid use disorders can be
managed in primary care.
1, 68-75
Change #4: Management of Alcohol or Other Drug Use Disorders
•
•
•
•
•
•
Options for Managing Patients in
Primary Care
Medication
Counseling
Referral to
group-based
addiction
treatments
Peer support
Primary
care support
for self-
management
Manage patients with alcohol- and/or other drug-related symptoms: oer repeated visits for brief counseling
and shared decision-making regarding treatment options and referral, as appropriate.
Recommendation
Metric
Benchmark
Oer patients shared decision-making about five types of options and refer as needed if services are
not available in primary care.
o Medications such as naltrexone and acamprosate for alcohol disorders and buprenorphine
naltrexone, or methadone for opioid use disorders in primary or specialty care.
59
o One-on-one behavioral treatments for alcohol and/or other drug use disorders by a
behavioral health clinician (e.g., cognitive behavioral therapy, motivational enhancement
therapy),
1, 60, 61
which can be integrated into primary care.
64
o Peer support groups (e.g., Alcoholics, Narcotics Anonymous (AA, NA,
62
, SMART Recovery
63
).
o Group-based treatment as provided by most specialty addiction treatment programs.
o No treatment at this time, but possible self-management, with continued primary care
support with monitoring and motivational interviewing.
Among patients with alcohol and/or other drug use symptoms on a structured tool, the proportion
who have a follow-up visit that addresses alcohol and/or other drug use within 90 days.
80%
• Continue ongoing brief counseling. Provide ongoing alcohol- and/or other drug-related care
(i.e., repeated visits)—within primary care, mental health, or specialty addiction treatment
settings, per patient preference—to support self-management and change.
• Adapt care based on results of monitoring and changes in symptoms and patient preferences.
•
•
•
•
•
•
•

17
ELEMENTS OF PRIMARY CARE MANAGEMENT
Treatment of alcohol and/or other drug use disorders can include medications and counseling, encouraging
peer support, referral to specialty addiction treatment (in the medical setting or in the community) and support
for patient self-management. Utilizing the collaborative care consulting methodology, either virtually or on-site,
primary care physicians may benefit from the expertise of addictions specialists. Sites may choose to embed this
practice with regular supervision or through contracting with a colleague for ad hoc consultation on complex cases.
Medications for Alcohol and Drug Use Disorders
Medications for alcohol use disorders (AUDs) improve response to behavioral treatment,
59, 76
and naltrexone can
decrease heavy drinking as well.
70
The FDA has approved three medications for alcohol use disorders: naltrexone, acamprosate, and disulfiram.
These medications can be prescribed in primary care with medication management focused on assessing
use and symptoms, recommending abstinence in a patient-centered manner, medication adherence, and
encouraging participation in peer support.
70
Follow-up can be every 1-2 weeks for 2 months and then monthly
when patients are stable.
Care management by a nurse, recommending abstinence and naltrexone, is associated with improved
engagement in alcohol-related care and decreased drinking compared to “referral to treatment” in primary care
patients not seeking addiction treatment.
70
Two medications for opioid use disorders (OUDs)
71, 77
—methadone or buprenorphine—improve patient outcomes for
OUDs, and are far superior compared to counseling and other behavioral treatments alone.
78, 79
Opioid use disorders
due to heroin and prescription opioids are responsive to these treatments.
80
Methadone and buprenorphine both lead
to decreased mortality and morbidity for patients on these medications long-term (i.e. maintenance therapy). Evidence
for the eectiveness of injectable, extended release naltrexone is emerging.
81
Buprenorphine can be prescribed in primary care by primary care providers who have a buprenorphine waiver
from the DEA (requiring an 8-hour course that can be taken online).
71, 81, 82
Free virtual mentorship for treating
OUDs with buprenorphine is also available.
82
Extended release naltrexone can also be prescribed in primary care with monthly injections.
OUDs can only be treated with methadone in special Outpatient Treatment Programs approved for methadone
maintenance.
Care management for OUDs is associated with high rates of retention, and a central part of primary care
management.
Medication to prevent opioid overdose if patients are still using opioids or at risk of relapse.
Naloxone (Narcan—not to be confused with naltrexone) can decrease death due to overdose.
Change #4: Management of Alcohol or Other Drug Use Disorders, CONT.
•
•
•
•
•
•
•

18
ONEONONE COUNSELING
Motivational Interviewing, cognitive behavioral therapy (CBT), and other one-on-one counseling approaches are
eective for alcohol and/or other drug use disorders.
60, 61
A primary care trial suggests a six session CBT/MI brief therapy
is eective when provided to patients not seeking treatment by an integrated behavioral health clinician in primary
care.
1
The FDA recently approved a proven digital counseling program for alcohol and/or other drug use disorders.
83
Encourage Participation in Peer Support
84, 85
Peer support groups can help patients who want to make changes. AA is associated with improved outcomes, in part due
to new social networks. Alternatives to AA and other twelve-step programs, like Self-Management and Recovery Training
(SMART) recovery
63
provide an alternative for those who are uncomfortable with the spiritual component of AA.
Referral to Specialty Addiction Treatment
Referral to specialty treatment options. A small percentage of patients may need and be open to referral to
specialty alcohol and/or other drug treatment. It is important to improve engagement in treatment by having
protocols and procedures for linking patients to internal (within the same organization) or external treatment
resources. In order to optimize the chances of a successful specialty treatment referral, it is crucial to develop a
standard and consistent workflow.
Specialty addiction treatment in the medical setting. When internal specialty addition treatment is available, the ease
of linking to treatment may have significant advantages, such as: capability for warm hand-os; documentation
within the same medical record and collaboration with primary care. Even with these seeming advantages, a detailed
workflow is highly recommended with defined roles in order to achieve high engagement rates.
External addiction treatment programs. When internal resources are not available, forging strong partnerships
with external addiction specialists is essential to improving access to care and improving patient satisfaction.
Successful referrals to external services require addiction specialists and primary care clinicians to communicate,
collaborate, and evaluate the eectiveness of the relationship. Identification of available, accessible treatment
resources is key and developing functional partnerships with external specialty addiction treatment clinicians in
the community will improve patient care.
Confidentiality of Care in Specialty Addiction Treatment Programs. Confidentiality must be considered when
making referrals for specialty addiction treatment. Sharing of treatment information is strongly recommended and
documented patient consent to share addiction treatment program information is legally required under 42CFR
Part II. For more information, see SAMHSA’s A Guide to Substance Abuse Services for Primary Care Clinicians..
Monitoring in primary care after treatment. If a patient is referred to specialty addition treatment, the primary
care team should follow-up to determine if the patient engaged in treatment, and to monitor response to, and
for relapse after, treatment.
Resources regarding specialty addiction treatment.
Selecting from a spectrum of treatment intensities. See Appendix or an overview of levels of care for
alcohol and other drug use disorders.
Successful referral practices for alcohol and/or other drug use disorders. See Appendix for more information.
See Management Resources in the Appendix for more information on treatment options.
Change #4: Management of Alcohol or Other Drug Use Disorders, CONT.
•
•
•
•
•
•
•
•
•

19
SHARED DECISIONMAKING
In shared decision-making, clinicians work collaboratively with patients when there are multiple options for care—
for example, considering treatment options for alcohol or opioid use disorder (e.g., medications, counseling, group-
based specialty addiction treatment, peer support, or self-management). Shared decision-making is particularly
important when the patient has to execute the treatment—as in behavior change—as well as when choices patients
might make would dier from those clinicians might recommend.
86
When oering shared decision-making,
clinicians help patients understand they have choices (including no treatment), provide information comparing
options, elicit patient values and preferences, and support them in making a decision that fits them best.
70, 87
In
shared decision-making, the patient is the expert.
88
Shared decision-making is essential to patient-centered care
for alcohol and/or other drug use disorders.
35
There is a progression of steps when using shared decision-making
that help patients make informed decisions.
89
Clinicians inform patients on choices: medications, one-on-one counseling, group-based treatments, peer
support, and no treatment (but continued primary care support), depending on the patients’ alcohol and/or
other drug use disorder and the availability of treatments in the community.
Patients’ preferences, values, and priorities are considered. These include, but are not limited to: privacy,
logistics, cost, and preferred treatment approaches.
Patients should be supported in making a decision and accessing treatment.
Provision of decision aids (print, video, and/or online resources) can assist in helping the patient and clinician
better understand and weigh options together. A decision aid tool for opioid use disorder treatment is
available through SAMHSA.
Change #4: Management of Alcohol or Other Drug Use Disorders, CONT.
•
•
•
•
Patient Self-Management with Repeated Brief Counseling and Monitoring in Primary Care
Patients with alcohol and/or other drug use disorders who are not interested in medications for AUD or OUD, counseling,
specialty treatment, or peer support, should nonetheless be oered repeated brief counseling with MI and shared
decision-making in primary care. Several studies support repeated brief counseling for high-risk drinking and/or alcohol
and/or other drug use disorders.
58, 68-70
Treatment of comorbid mental health and/or medical conditions may also be used to build rapport and engagement in
treatment, or can lead to changes in alcohol and/or other drug use.
Patient or
provider
conveys that
treatment
choices exist
Patient is
informed
about
treatment
options
Support
patient in
exploring own
values and
preferences
Support
patient in
making a
decision on
their own

20
Rationale
Follow-up with systematic symptom monitoring is critical for knowing:
Whether patients’ symptoms are increasing or decreasing.
Whether or not patients treated with medications or counseling in primary care are benefiting and if they are
achieving their goals.
When treatment needs to be changed or augmented if there is not adequate improvement.
Change #5: Follow-Up With Monitoring
•
•
•
Arrange follow-up to monitor alcohol and/or other drug use and symptoms with a structured tool in all patients
with high-positive alcohol and/or other drug screens, or reporting symptoms on the Symptom Checklist.
Recommendation
Metric
Benchmark
Select a tool for monitoring patients with symptoms.
At a minimum, monitor frequency of use with the AUDIT-C Plus 2 every three months.
90
Ideally, also monitor symptoms of use (questions #2-5 of the Short Alcohol Monitor and/or
Short Drug Use Monitor).
Ideally, monitor whether patient is achieving their own goals regarding alcohol and/or other
drug use (Questions #1 of the Short Alcohol Monitor and/or Short Drug Use Monitor). If
patients are not responding to treatment, reassess with MI and shared decision-making and
adapt or change treatment(s).
Among patients with high-positive screening scores or alcohol- or other drug-related symptoms,
proportion who have a follow-up contact within three months of high-positive screening score or
report of alcohol- or other drug-related symptoms.
80%
•
•
Repeated visits for monitoring should include: repeated brief counseling with MI and shared decision-
making, tracking alcohol and/or other drug use and symptoms, and patient self-assessment of alcohol
and/or other drug use.
Develop tracking protocols (e.g., EHR registry) for ensuring population-based follow-up based on
clinical severity, at least every three months.

21
WHAT ARE THE IMPORTANT COMPONENTS OF FOLLOWUP WITH MONITORING?
1. Monitoring: systematic measurement over time to guide care
Quality improvement research over the past 20 years has shown that whether one is treating hypertension, diabetes,
or depression, measurement-based care improves outcomes. Unfortunately, unlike depression (for which there is
widespread use of the PHQ-9 to monitor symptoms and response to treatment), there is no standard practical approach
to systematic monitoring of alcohol and/or other drug-use and symptoms in primary care. However, several systems
have successfully used alcohol and/or other drug use screening questions for monitoring,
91
and validated discriminating
questions for alcohol and/or other drug use disorders have been identified by the National Institute of Health (NIH)
Patient-Reported Outcomes Measurement Information System (PROMIS).
92, 93
Important dimensions of alcohol and/or other drug use to monitor likely include:
The extent to which alcohol or other drug use is interfering with patients’ goals (family, relationships, health).
Severity of consequences due to alcohol and/or other drug use.
Severity of symptoms of loss of control over alcohol and/or other drug use or craving.
Level of current alcohol and/or other drug use.
Experience with depression management in primary care indicates that brief instruments should be used for monitoring.
Thus, this guide recommends use of the AUDIT-C Plus 2 screening questions, at a minimum (with a past three-month
timeframe). Additionally, this guide recommends five-item tools to monitor symptoms and functioning — one for
alcohol and one for other drugs, as outlined in the following table. These ten items can be administered along with the
AUDIT-C Plus 2. Questions #2-5 are adapted from the PROMIS.
94,92, 93
*Response choices for all: Never, Rarely, Sometimes, Often, Almost Always
Alternative options for monitoring are the full AUDIT (alcohol),
22
CUDIT
95
(cannabis), and DUDIT
96
(other drugs). For
these tools, the monitoring timeframe should be adjusted from one year to three months. The ASSIST
97, 9 8
can also be
used. Another alternative is to monitor with the Alcohol or Drug Use Symptom Checklists. These tools may have merit,
but they are longer and more specific to individual drugs. Nevertheless, these may be reasonable options in settings
where these tools are already being used systematically.
•
•
•
•
Change #5: Follow-Up With Monitoring, CONT.
Short Alcohol Monitor Short Drug Monitor
How often in the past 2 weeks... How often in the past 2 weeks...
1.
2.
3.
4.
5.
1.
2.
3.
4.
5.
Were you bothered by how your drinking impacted your
health, relationships, goals or life?
Did you have trouble controlling your drinking, drink too
much or spend too much time drinking?
Was it dicult to get the thought of drinking out of your mind?
Did you disappoint yourself or others due to drinking?
Have you had trouble getting things done due to drinking?
Were you bothered by how your drug use impacted your
health, relationships, goals or life?
Did you spend a lot of time using drugs?
Were drugs the only thing you could think about?
Did you disappoint yourself or others due to drug use?
Did you feel your drug use was out of control?

22
WORKFLOW CONSIDERATIONS FOR FOLLOWUP WITH MONITORING
Who will schedule follow-up? Will it be in person or by phone? This will depend on patients’ other medical
conditions and treatments, how soon they are willing to return or have a phone appointment, and co-pays.
How often? This guide recommends monitoring at least quarterly.
Who will do the monitoring? Generally, monitoring fits into the workflow just as screening does.
How will the system know if a patient does not make a follow-up appointment or cancels? EHR registries
can assist a behavioral health clinician in primary care or a nurse managing a population of patients with alcohol
and/or other drug use disorders.
What communication strategies will be used between internal and/or external behavioral health clinicians?
An EHR registry as above can also assist in monitoring patients who are receiving outside treatment.
2. Repeated brief counseling as part of monitoring
Given the considerable impact of alcohol and/or other drug use disorders on patients’ health and well-being, it is
appropriate and essential to incorporate routine follow-up for all patients with symptoms of alcohol and/or other
drug use disorders into standard care. Research shows that brief multi-contact counseling, as described previously,
along with shared decision-making, is eective. Comorbid medical conditions (e.g., anxiety, depression, HCV) can be
managed concurrently.
3. Medication management, integrated with monitoring, as appropriate
For patients on medications, close follow-up is important to assess for side-eects and monitor adherence. Care
management for medications for alcohol use disorders often includes encouraging peer support, while monitoring for
medications for opioid use disorders often includes urine drug screens.
4. Monitoring after referral—both internal to the health care organization and external
Some patients with alcohol and/or other drug use disorders will benefit from specialty addiction treatment or
other mental health services for comorbid conditions. When patients choose specialty treatment, clinicians must
be prepared to support patients connecting to treatment resources and to follow-up after the patient engages in
specialty treatment.
Change #5: Follow-Up With Monitoring, CONT.

23
Rationale
Clinical Changes #1-5 are complex changes to the way patient care is provided for all primary care team members.
Leaders, at all levels of a health system, need to actively support clinical changes to ensure successful and sustained
implementation.
What is active leadership support?
Active support for improvements in alcohol and/or other drug use in primary care includes:
Leaders select which change to implement. Leaders can start by assessing gaps in alcohol- and/or other drug-
related care or can select the first change(s) to implement based on knowledge of their clinic(s). Often, clinics
start with screening (Change #1), eliciting alcohol and/or other drug related symptoms with a standard tool
(Change #2), and brief counseling (Change # 3) – “SBI” of “SBIRT”. While 15-25 percent of patients will have
unhealthy use of alcohol or other drugs, only 1-2 percent of patients typically screen high-positive or have
alcohol and/or other drug use disorders. However, addressing management of alcohol and/or other drug use
disorders (Change #4)—and sta training needs regarding management—can improve clinician comfort when
those patients are identified.
Organizational Changes
Change #6: Leaders Actively Support Improvements
Leaders actively support improvements in alcohol and other drug-related care.
Recommendation
Metric
Benchmark
Leaders at all levels of the organization actively articulate the rationale for integrating improved
alcohol- and/or other drug-related prevention and management as part of primary care.
Leaders need to:
Select the clinical change(s) to implement (#1-5).
Identify champions to lead the alcohol and/or other drug use quality improvement eort in
each clinic (implementation team).
Provide time and resources to support implementation.
Set expectations for targets and timing and provide monitoring and feedback on performance.
Leadership selects an implementation team and prioritizes one or more clinical Changes (#1-5) to
be implemented.
Implementation meets benchmark(s) for the clinical change selected (#1-5) within six months.
•
•
•
•

24
Other Considerations
Identifying sta to lead quality improvement in the clinics: Identify an interdisciplinary team in each clinic to be responsible
for implementation of a selected change. This should include at a minimum: a primary care physician/clinician, support
sta (e.g., nurse, medical assistant, or health tech), and an integrated behavioral health clinician, if one practices in the clinic.
Other suggested champions include: front desk sta, administrative leadership or sta, float sta, pharmacists, a quality
improvement expert, billing representative, peer navigators, other key clinic personnel, and a clinical EHR programmer for
assistance with EHR development and adjustments.
Committing resources: Provide an initial financial investment of time for local implementation team meetings and piloting,
time for clinicians to partner with IT/programmers to develop EHR decision support, time for work force development,
commitment to stang with behavioral health clinicians in primary care (e.g., social work, nurses), support for data analytics
for timely reports on metrics, and time to identify and partner with community resources.
Monitoring and feedback: Attend/lead regular quality improvement meetings to review metrics and problem-solve using
PDCA, and to hold direct reports accountable for measurement and meeting selected targets.
Leadership provides ongoing support for the value and the importance of the changes: Leaders tell stories about the
central value of the work and frontline experience of success.
Augmenting the primary care team: Consider hiring a dedicated care manager or care coordinator, preferably with a
behavioral health background to help manage patients with alcohol and/or other drug use disorders in addition to other
behavioral health needs. Care coordinators, typically nurses or social workers, provide services like case management,
medication management, monitoring of patient health status, and counseling and support for patient self-management
of their alcohol and/or other drug use. Peer navigators can also help connect patients to needed resources.
Change #6: Leaders Actively Support Improvements, CONT.
ROADMAP FOR CLINIC LEADERSHIP SUPPORT
Set implementation in motion. If large health system, leader(s) select pilot clinics and key gap(s) in quality via assessment
of the current state. Leaders select initial change (#1-5) to implement, tools, and targets.
Select and empower interdisciplinary local implementation team. Explain the gap and expectation for change to the
local implementation team. Leaders arrange for workforce development for local implementation team.
Leaders kick-o initial pilot with primary care clinician champion(s) and medical assistant or dyad partner(s). Pilot
includes iterative huddles or meetings to problem-solve challenges (Plan-Do-Check-Act [PDCA]).
Oversee iterative improvement. Local implementation team meetings occur weekly/biweekly (1 hour). Leaders review
progress monthly at quality improvement (PDCA) meetings.
Support the importance of the work. Communicate expectations to leaders at all levels of the organization regarding
importance of the quality improvement eort. Leaders at all levels continually spread positive stories.
Consider hiring a dedicated care manager/coordinator or expanding the role of health coaches or care managers to
include alcohol and/or other drug use.

25
Establishing and maintaining partnerships with specialty addiction treatment services: For internal partnerships, leaders
create the platform for internal planning discussions and sponsor the infrastructure needed to support the collaboration. If
the partnership is external, leaders broker the arrangement and maintain a relationship with the partner leadership team,
to develop seamless communication pathways and follow-up. This is especially critical given that 42 CFR Part II requires
specific written documentation of consent for sharing information from a specialty addiction treatment program.
Troubleshooting challenges and celebrating small successes: Leaders problem-solve barriers and highlight the
incremental successes that lead to achieving organizational change.
Change #6: Leaders Actively Support Improvements, CONT.

26
Rationale
Implementing improved alcohol and/or other drug care is a major quality improvement (QI) initiative, not dissimilar
from other primary care QI projects focused on the triple aim. In June 2017, the National Committee for Quality
Assurance added the Unhealthy Alcohol Use Screening and Follow-Up measure to the Healthcare Eectiveness Data and
Information Set (HEDIS) 2018 for health plan reporting. This measure assesses the percentage of health plan members
eighteen years and older who were screened for unhealthy alcohol use and, if screened positive, received appropriate
follow-up care within two months. As health systems move toward EHRs, building structured fields and approaches
for standardized screening tools and follow-up care will encourage screening and allow easier monitoring of quality of
care. Clinician education on evidence-based models, as well as aligned incentives to oer screening and follow-up, will
help encourage their administration.
To achieve the goal of sustainable alcohol- and/or other drug-related care, attention must be given to: 1) planning
for implementation, 2) piloting to make rapid cycle changes to refine workflow before changes are disseminated to
others in a clinical practice, 3) assessing the pilot impact and outcomes, and 4) creating organizational buy-in to spread
changes in workflow to the entire clinical practice.
Change #7: Use Quality Improvement Processes
Use population-based quality improvement processes for each of the five clinical changes.
Recommendation
Metric
Benchmark
Assess current gaps in alcohol and/or other drug-related care.
Prioritize clinical Changes(s) #1-5 to implement.
Local implementation team members (i.e., champions) meet regularly: pilot, then implement.
Monitoring metrics by establishing a quality improvement system (e.g., PDCA).
Demonstrate progress on selected change concepts at six months.
Prioritized changes are in rapid cycle pilot testing within 2 months and implemented at six months
and sustained at 12 months
100%
•
•
•
•
•

27
Change #7: Use Quality Improvement Processes, CONT.
•
•
•
•
•
•
•
•
•
•
•
•
ROADMAP FOR QUALITY IMPROVEMENT
1. Planning for implementation
Prioritize change(s) to implement. Identification of key gap(s) via assessment of the current state and
selection of CHANGE (#1-5), tools and targets. (If not selected by leadership, leadership support must be
obtained.)
Develop and execute a plan to measure processes of care. A process is needed for systematically
tracking clearly defined care processes.
Interdisciplinary local implementation team. Start by describing the current organizational state and
plan an approach to change. Identify gaps in workforce knowledge and skills and plan for workforce
development, first for the local implementation team, and then for all sta.
2. Piloting
Engage primary care clinician champion(s), including primary care clinician(s) and dyad partner(s) (e.g.
medical assistant) in planning.
Conduct a pilot. One or two dyads test the workflow, until an ecient process is developed.
3. Pilot Team assesses outcomes and refines workflow
Review performance. The local implementation team evaluates data on processes of clinical care during
piloting, ideally using metrics for the targeted clinical change (#1-5) and data from the EHR.
Problem-solve barriers and identify facilitators of eciently providing the desired care in a patient-
centered manner.
Adjust workflow as needed, and repeat with iterative PDCA cycles: piloting for 1-5 days, evaluating,
refining and piloting again until targets are met for the pilot team.
4. Launch clinical change to the remainder of the clinical practicePrepare and train all sta. Workforce
development is critical, and includes all individuals who work in the clinical practice. See Change #8
below.
Launch. After all sta have been trained and prepared for launch, start the new process (the clinical
change) on a specified day.
Continue iterative PDCA meetings. The local implementation team now meets to review the entire
clinical practice’s data weekly-monthly.
Problem-solve challenges and share positive stories with the clinic in huddles or meetings.
Regular meetings with leaders to monitor metrics and plan next steps. Leaders review progress
monthly at quality improvement (PDCA) meetings. After one change has been successfully implemented,
select the next.

28
Change #8: Train Primary Care Teams
Rationale
It is critical to have a primary care workforce that is prepared to provide non-judgmental, patient-centered care for
alcohol- and/or other drug-related care. Therefore, training all clinic sta is recommended. It can be helpful to address
the stigma surrounding alcohol and/or other drug use disorders in trainings. Videos and handouts have been developed
to facilitate patient-centered care (e.g., ”A ReThink of the Way We Drink”).
Common Training Needs
Addressing stigma—and the crucial need for non-judgmental approaches—should be woven through all training. Below
is an outline of possible training needs. See Appendix for training resources.
Train primary care teams to address alcohol and other drug use and use disorders in primary care, as
appropriate.
Recommendation
Metric
Benchmark 100%
Assess training needs of key sta for each change.
Plan training for the entire primary care team (e.g., front desk, sta who conduct patient intakes,
primary care clinicians, behavioral health clinicians).
Ongoing assessment of training and work force development needs.
Plan training for new sta onboarding.
•
•
•
•
Training needs are identified during pilot testing (within 2 months)
Training implemented before launch
Additional training needs evaluated at 3, 6, and 12 months
•
•
•

29
Change #8: Train Primary Care Teams, CONT.
Table 8.1 Outline of Possible Training Needs
How to support primary care teams
doing warm hand-os
Primary Care
Clinician
(MD, NP, DO, PA)
Medical Assistant,
Health Technician,
Nurse
Behavioral Health Clinician
Practicing in Primary Care
(Social Work, etc.)
Change #1 —
Screen
Interpretation
of screens
Change #2 —
Elicit symptoms
Diagnosing alcohol
and/or other drug
use disorders
Change #3 —
Brief counseling
Brief counseling for
patients with positive
screens using MI skills
Change #4 —
Management
Shared decision-
making re:
Medications:
Change #5 —
Follow-up
with monitoring
Scripts for handing
out screens, data
entry in EHR
Scripts for handing
out questions about
symptoms, data entry
in EHR
Conducting formal diagnostic assessments
for alcohol and/or other drug use disorders
and engaging in shared decision-making
re: alcohol- and drug-related care
Alerting clinicians
to patients for brief
counseling (template
in EHR, handout
clipped to chart, etc.)
Counseling for patients with high positive
screens or alcohol or other drug disorders,
treating comorbid mental health conditions
AUD: Naltrexone vs
acamprosate vs
disulfiram
OUD: Buprenorphine
vs injectable
naltrexone vs refer
for methadone
Opioid use:
Naloxone
Alerting primary care
and/or behavioral
health clinicians re:
high-positive screens
or possible alcohol or
other drug use
disorders
Shared decision-making and treatment
options in the community, MI and CBT,
supporting engagement in peer support
Follow-up
monitoring and
adapting treatment
Outreach and sending
monitoring tools, or
inviting patients to
schedule follow-up
Monitoring all patients on medications
and after short-term (12 week) treatment,
managing a registry

30
Change #9: Billing and Identifying Revenues for Alcohol and/or Other Drug Care
Rationale
Billing for alcohol- and/or other drug-related care may help ensure their sustainability.
SBI codes can be used for screening and brief counseling. These codes can be used by integrated behavioral health
clinicians after screening, assessment of symptoms, and a warm hand-o for unhealthy alcohol and/or other drug use,
or alcohol and/or other drug use disorders, if counseling lasts 15-30 minutes. Under the Aordable Care Act (ACA), they
should not result in patient copays.
In addition, recently approved Medicare codes for collaborative care and care coordination
99
can improve revenues.
Alcohol- and/or other drug-related care may show a return on investment in primary care settings and may help
primary care settings perform better under alternative reimbursement and payment systems.
Alcohol-and/or other drug-related care may improve performance on CMS quality metrics for accountable-care
organizations (ACOs) and Merit-based Incentive Payment System (MIPS). The augmented model of care for alcohol
and/or other drug use described in this guide qualifies as an innovative practice under MIPS and may generate shared
savings for ACOs and improve cost performance.
Alcohol and/or other drug-related care is often a billable service — Medicaid, Medicare, and commercial billing codes
are available in many states and can support sustainable programs.
100
Bill for screening, brief counseling, management, and monitoring, and explore other revenue sources to
support the cost of provision of alcohol- and/or other drug-related services in primary care.
Recommendation
Metric
Benchmark
100% (completion) for both process measures
Work towards a financial model where the ratio of revenue/cost is greater than one.
If appropriate, use SBI, collaborative care, or care coordination codes to support the spectrum of
alcohol- or other drug-related care.
Develop a financial model where revenue fully covers the cost of delivery of alcohol and other
drug-related care.
•
•
Process measure: Estimate costs and revenue per month of alcohol and/or other drug use
care (screening, assessments to elicit symptoms, brief counseling, and care management) and
calculate revenue/cost ratio.
Process measure: Meet at least twice a year to review costs and revenue for providing alcohol-
and other drug-related care.
•
•
•
•

31
Making the Business Case for Implementing Care for Alcohol AND Other Drug Use in Medical Settings
There is a growing evidence base suggesting that improvements in alcohol and/or other drug care are a good
business decision. It could make an impact in the healthcare settings’ bottom line by addressing alcohol and/or other
drug use in a way that could decrease costly services like hospitalizations and readmissions. Systematically screening,
counseling, and managing patients with alcohol and/or other drug use problems could help meet challenges in the
emerging clinician-based risk models, such as ACOs and value-based payment contracts.
101
Screening and brief counseling for alcohol use among adults has been consistently ranked among the top
preventive services in terms of cost-eectiveness and health impact—ranking higher than screening for
hypertension and cholesterol.
12, 102, 103
Research on cost-benefit of SBIRT programs and savings when SBI is implemented suggest that the practice
can make financial sense.
104
Change #9: Billing, Identifying Revenues for Alcohol, Other Drug Care, CONT.
•
•

32
THE AUDITC SCREEN FOR UNHEALTHY ALCOHOL USE
The first three questions of the World Health Organization’s (WHO) 10-item AUDIT, called the AUDIT-C, is used
because it yields a helpful score (range 0-12) for assessing alcohol use severity and for monitoring alcohol use
over time.
Recommended thresholds: ≥3 and ≥4 points for a positive screen for women and men, respectively, and ≥7 for
high-positive for women and men, are based on numerous validation studies.
3, 26, 105
Patients who screen positive with scores below 7 are appropriate for brief preventive counseling (Change #3).
Patients with high-positive scores (7-12 points) should have symptoms of alcohol use disorders elicited (Change
#2). They are also appropriate for ongoing (repeated) brief counseling in primary care (Change #4).
Specific advantages of the AUDIT-C:
Validated and reliable and has been widely implemented in primary care.
106
It is in the public domain and has been translated to and validated in many languages.
Can easily be added to other brief screens or protocols (e.g., cannabis, other drugs, depression and smoking
screening, vital signs), and can be administered by sta interview or patient administration (the latter is
recommended).
Yields a score (0-12) that is strongly associated with level of consumption, severity of risk and probability of
DSM-5 alcohol use disorders (AUDs).
Can be used to monitor changes over time in drinking and changes in annual screening scores are associated
with changes in objective health outcomes.
Two Screening Questions for Cannabis and Other Drug Use
The two optional drug screening items (one for cannabis and one for other drugs scored separately) have many of
the qualities described above. The cannabis screen is adapted from a validated tool (i.e., the Cannabis Use Disorders
Identification Test [CUDIT]
107
) and the screen for other drug use has been adapted from a single item screen.
108
Research
indicates that single-question screening tools can identify unhealthy drug use, including cannabis, cocaine, heroin, and
hallucinogens, as well as recreational or non-medical use of prescription medications (i.e., without a prescription, more
than prescribed or to get high).
25
Appendix
Change #1 Resources: Screen All Adults at Least Annually
•
•
•
•
•
•
•
•
•

33
The Cannabis Use Screen (0-4 points) is included to allow clinicians to assess the frequency of cannabis use separately
from other drug use. Such screening allows clinicians to assess and address reasons for use (medical, recreational, or both).
Screening may be desirable in states that permit legal medical and/or recreational use. As cannabis legalization
expands, and the number of cannabis users increases—and daily cannabis users at greatest risk for a cannabis use
disorder
109
– increase,
110
clinicians will likely want to know whether their patients are using cannabis regularly.
Patients who report monthly or weekly cannabis use can be oered brief counseling (Change #3).
The authors recommend eliciting symptoms of a cannabis use disorder for patients who report daily use
because 25-50 percent of patients who use cannabis daily develop cannabis use disorders (Change #2).
111, 112
For patients who have a cannabis use disorder, ongoing brief counseling (Change #3), management as
appropriate based on shared decision-making (Change #4) and monitoring (Change #5) are recommended.
Other Drug Use Screen (0-4 points) is included to identify patients who might benefit from ongoing brief counseling
alone or assessment for a drug use disorder. Although most trials of screening and brief preventive counseling for non-
alcohol drug use in primary care have found no benefit, awareness of patients’ drug use is critical to high quality medical
care because it allows assessment of symptoms of other drug use disorders to permit diagnosis and treatment of drug
use disorders, as well as awareness of when drug use complicates management of other conditions (e.g., HIV or HCV,
depression).
Selecting a Screening Tool
There are many considerations when choosing a screening tool. The following factors were considered when
recommending the AUDIT-C Plus 2 tool. If a practice opts to select a dierent tool, the authors recommend considering
the following.
Considerations for Selecting a
Screening Tool
Valid and reliable?
Brief?
Free to use?
Recommended by authorities?
Available in multiple languages?
Widely used in the U.S. and Canada?
Used to identify unhealthy use?
Used to guide clinical next steps?
Useful for monitoring change in use patterns?
A good fit with other screeners?
Easy to administer?
•
•
•
•
•
•
•
•
•
•
•
Change #1 Resources: Screen All Adults at Least Annually, CONT.
•
•
•
•

34
Using symptoms of alcohol and/or other drug use to engage patients.
Understanding patients’ symptoms due to alcohol and/or other drugs opens an opportunity to engage the patient in a
conversation about how their alcohol and/or other drug use is impacting their lives and health. This allows the clinician
to understand the patient’s experience and engage them in care. In short, the information gained from systematically
eliciting symptoms will help engage patients in shared decision-making to identify the appropriate next steps.
Eliciting symptoms also facilitates diagnosis of alcohol and/or other drug use disorders.
Extensive research has documented that clinicians often do not recognize alcohol and/or other drug use disorders
without systematic screening and assessments. Alcohol and/or other drug use disorders are currently defined based on
DSM-5. Two or more symptoms out of 11 total symptoms define an alcohol and/or other drug use disorder. The more
symptoms a patient has, the more severe the alcohol and/or other drug use disorder.
The risk of alcohol and/or other drug use disorders is increased by genetics and age of first use, as well as other risk
factors, but the repeated exposure of the brain to high levels of alcohol and/or other drugs is a critical risk factor. The
probability of developing an alcohol and/or other drug use disorder increases, therefore, as the frequency and intensity
of a person’s alcohol and/or other drug use increases. As a result, screens that assess the frequency and intensity of
alcohol and/or other drug use (like the AUDIT-C Plus 2) are also excellent for identifying patients who deserve systematic
assessment for alcohol and/or other drug use disorders.
Change #2 Resources: Eliciting Symptoms

35
MOTIVATIONAL INTERVIEWING MI RESOURCES
Motivational Interviewing and Shared Decision Making are the foundation of brief counseling (Change #3) and
management of alcohol and other drug use in primary care (Change #4). Motivational Interviewing (MI) and shared
decision-making are complementary approaches that can be used together
89
by sta and clinicians who interact with
patients. When using these approaches—MI can help motivate change in alcohol and other drug use. Then, shared
decision-making can drive decisions on the preferred approach to that change and treatment plans. MI can continue to
be helpful as many patients who initiate change continue to have ambivalence.
MOTIVATIONAL INTERVIEWING
MI is a collaborative, conversational approach to counseling aimed at strengthening a patient’s own motivation
and commitment to change, and can be useful for a range of health issues. MI helps patients to identify and resolve
ambivalence about changing their alcohol and/or other drug use and involves building a collaborative partnership
with patients, eliciting the patient’s own motivations for change, and builds on patients’ strengths.
113
A recent
systematic review showed that clinicians can successfully use MI as part of patient consultations to reduce alcohol
and/or other drug use as well as increase exercise and weight loss and lower important health indicators (e.g., HIV
viral loads, blood pressure, cholesterol).
114
MI skills include open-ended questions, reflective listening, eliciting reasons for change (i.e., “change talk”), and
developing discrepancy between the patient’s values and current situation. There are four components that
capture the spirit of MI (partnership and collaboration, eliciting the patient’s reasons for change, acceptance, and
compassion/empathy).
115
Change #3 Resources: Brief Counseling
For additional information on MI:
SAMHSA-HRSA’s MI Resources Page
SAMHSA’s Guide on Enhancing Motivation to Change Substance Use
Motivational Interviewing Network of Trainers website
Book: Motivational Interviewing: Preparing People for Change, 3
rd
Addition
113
•
•
•
•

36
LOWRISK DRINKING GUIDELINES
Advising patients about these recommended limits is a key element of brief counseling for unhealthy alcohol use. The
National Institute on Alcohol Abuse and Alcoholism (NIAAA) recommends:
Change #3 Resources: Brief Counseling, CONT.
It is important to note that “low risk” is not “no risk.” Even within these limits, alcohol can cause problems if people
drive after drinking, have health problems, or are older (recommended limits for both men and women over 65 are no
more than three drinks on any day and 7 per week). Based on patients’ health and how alcohol aects them, they may
need to drink less or not at all. The NIAAA recommends avoiding alcohol in the following situations:
Taking medications that interact with alcohol.
Managing a medical condition that can be made worse by drinking.
Underage drinking increases the risk of alcohol use disorders
Planning to drive a vehicle or operate machinery.
Pregnant or trying to become pregnant.
Resources to Help Patients Make Changes in Alcohol or Other Drug Use:
The following resources may be useful for patients interested in making changes to their alcohol and/other drug
use. Sometimes, it helps patients to use worksheets and have access to tips for cutting down when they are making
changes.
For patients considering changes to drinking: https://www.rethinkingdrinking.niaaa.nih.gov/Thinking-about-
a-change/Its-up-to-you/Planning-For-Change.aspx (online or free booklet)
For patients considering changes to other drug use:
https://www.drugabuse.gov/publications/resource-guide/change-plan-worksheet
•
•
•
•
•
•
•

37
Change #4 Resources: Management
Table A.1 below briefly describes a number of evidence-based practices for alcohol and/or other drug use disorder.
Other helpful online overviews include:
NIAAA’s Clinicians Guide – Helping Patients Who Drink Too Much
NIDA Principles of Drug Addiction Treatment
SAMHSA’s Guide to Medication and Treatment
•
•
•
In cognitive behavioral therapy (CBT), individuals learn to identify and correct problematic
behaviors by applying a range of dierent skills that can be used to help them change alcohol
and/or other drug use and address a range of other problems that often co-occur with it.
Brief Description
Cognitive Behavioral
Therapy
Treatment
Motivational enhancement therapy (MET) is an approach that uses MI to help individuals resolve
their ambivalence about changing their alcohol and/or other drug use. MET aims to evoke internal
motivations to change.
Motivational
Enhancement Therapy
Twelve-step facilitation therapy is an active engagement strategy designed to increase the
likelihood of an individual with alcohol and/or other drug use disorders becoming aliated with
and actively involved in 12-step self-help groups, thereby promoting abstinence.
12-Step Facilitation
Family behavior therapy (FBT) is aimed at addressing alcohol and/or other drug use problems, as
well as other co-occurring problems, such as conduct disorders, child mistreatment, depression,
family conflict, and unemployment. FBT combines behavioral contracting with contingency
management.
Family Behavior
Therapy
Contingency management involves giving patients tangible rewards to reinforce positive
behaviors, such as abstinence.
Contingency
Management
Community reinforcement approach (CRA) is an intensive 24-week outpatient therapy that uses
a range of recreational, familial, social, and vocational reinforcers, along with material incentives,
to make a non-drug-using lifestyle more rewarding than alcohol and/or other drug use.
Community
Reinforcement
Approach
Medication can be used with counseling to assist patients in changing their alcohol or other
drug use. Medications for opioid use disorders have been shown to: 1) improve patient survival
for opioid use disorder, 2) increase retention in treatment, 3) decrease illicit opiate use and other
criminal activity, 4) increase patients’ ability to gain and maintain employment, and 5) improve
birth outcomes among women who have alcohol and/or other drug use disorders and are
pregnant. Commonly used medications are:
Opiate Use Disorder (OUD): methadone, buprenorphine, injectable naltrexone
Alcohol Use Disorder (AUD): naltrexone (oral or injectable), acamprosate, disulfiram
Medication Treatment
Table A.1 Evidence-Based Practices for Alcohol and/or Other Drug Use Disorders

38
SELECTING FROM A SPECTRUM OF TREATMENT INTENSITIES
There are dierent levels of care in which a patient’s alcohol and/or other drug use disorder can be managed, representing
dierent settings and intensities of treatment. As discussed throughout this guide, medications for alcohol and opioid
use disorder, as well as short behavioral therapy, can be oered in primary care. Specialty addiction treatment programs
are also an option. Treatment should be oered depending on the patient’s needs, psychiatric/medical co-morbidities,
risk level, and preference. Primary care clinicians should consider several factors in helping patients select the optimal
intensity of treatment: What level of care will meet the patient’s needs? What level of care is the patient willing to go
to? What quality programs are available in primary care and/or the community? What will insurance cover? Medications
for alcohol or opioid use disorders should be oered to patients as appropriate at any level of care; however, specialty
opioid treatment programs are the only ones that can currently legally oer methadone for treating opioid use disorder.
The American Society of Addiction Medicine has tools and criteria for determining appropriate treatment placement.
Change #4 Resources: Management, CONT.
Primary Care-Based Treatment
Outpatient Treatment
Intensive Outpatient Treatment
Opioid Treatment Programs
Residential/Inpatient Treatment
Residential/Inpatient Treatment
Therapy and medication (except methadone) can be oered within primary care, depending on resources, unless the patient
prefers to receive care in a specialty treatment program or the needs are too complex to be managed well within primary care.
Table A.2 Levels of Care for Treatment of Alcohol or Other Drug Use Disorders
Patients typically meet with a therapist or counselor weekly for a period dependent on progress and the treatment plan. This
level of treatment is most appropriate for people who are not using alcohol and/or other drugs in ways that put them at
imminent risk (e.g., drinking and driving), who have relatively stable living situations, and who do not have serious psychiatric
or medical co-morbidities that warrant 24-hour medical oversight. Individual, group, and family therapy are typically oered.
Intensive outpatient treatment is for patients in need of more support than outpatient treatment, and typically includes at least
nine hours of individual, group or family therapy per week. Patients can often attend in the evening or weekends, but live at
home. Similar to outpatient treatment, this is most appropriate for people who are not using alcohol and/or other drugs in ways
that put them at imminent risk, who have relatively stable living situations, and who do not have serious psychiatric or medical
co-morbidities that warrant 24-hour medical oversight.
Opioid treatment programs are the only available level of care where methadone for opioid use disorders (OUDs) is available.
These programs are certified by SAMHSA to provide supervised assessment and medication treatment and supportive counseling
to people with OUD. Many programs are now expanding beyond methadone to other appropriate medications for OUD.
This is an intensive level of care for patients who have not only severe addiction, but also have complex psychiatric, family, social,
or medical problems that would interfere with treatment and the ability to recover. Residential/inpatient treatment includes
programs that provide treatment in a residential setting and typically includes medical oversight for co-occurring conditions.
This is the highest level of treatment and is most appropriate for patients whose alcohol and/or other drug use, medical, and
psychiatric problems are so severe that they require 24-hour medical care.

39
SUCCESSFUL REFERRAL TO TREATMENT FOR ALCOHOL OR OTHER DRUG USE DISORDERS
Both literature and real world experience have demonstrated that referral from primary care settings to behavioral
health services is often not successful. Barriers arise even when the patient agrees to engage in a higher level of care
(e.g., insurance, admission procedures, etc.). To optimize the success of referral for those in need of specialty treatment,
primary care clinics should have a standardized protocol and materials ready for referrals to care, internal or external.
Internal Specialty Treatment
With an increase in integration of behavioral health services into primary healthcare settings, many primary care clinics
have embedded behavioral health clinicians trained in specialty addiction treatment. In such instances, a “warm hand-
o” or internal referral for diagnostic assessment and acute treatment can be made directly from the primary care
clinician to the embedded behavioral health clinician. Internal referrals may benefit from the familiar, trusted, non-
stigmatized setting and potentially fewer logistical barriers compared to external treatment programs.
External Specialty Treatment
Primary care clinics without internal behavioral health clinicians will need to identify and partner with external
treatment programs. Clinic personnel who will be making referrals, should at minimum, understand or have access
to information about the services oered by each treatment program, the basic criteria for attendance (age, gender,
severity, insurance), and the program’s process for referrals and intakes. Ideally, a designated contact/intake person for
the treatment program will have been identified. Considerations regarding confidentiality, the exchange of information,
and establishing follow-up protocols should be explored, with the aim of developing eective policies and procedures.
Specialty Treatment Referral Workflow Development
Internal and external referral processes benefit from a written workflow including the development of a policy and
procedure. The workflow should specify the following:
1. How referrals can be made and scheduled (warm hand-o, phone call, scheduler, fax, email, EHR communication,
required prior tests such as urine drug screens, etc.).
2. Expected timeliness of appointments (emergency, urgent, routine).
3. Expected engagement responsibilities and accountability (if patient no-shows, who does follow up; if patient
shows once but does not return, who gets notified, etc.?).
4. How information is shared (verbal and/or written consent, minimum treatment information to be shared by all
parties, frequency of routine communication).
5. Expected frequency of workflow/policies and procedures review (quarterly with new workflows, annually or
biannually with established workflows).
Shared Decision-Making Resources
There are many good shared decision-making resources available, including the tool for opioid treatment.
For additional information:
SAMHSA Shared Decision-Making Resources
SAMHSA BRSS TACS Opioid Treatment Shared Decision-Making Tools
Change #4 Resources: Management, CONT.

40
Using a registry can be helpful for monitoring patients: AIMS Center at the University of Washington provides resources
on creating a registry, as well as a registry example.
Recommended monitoring tools: AUDIT-C Plus 2 and additional questions about patient goals and symptoms due to
alcohol and/or other drug use.
Once a year, we ask all our patients to complete this form on conditions that
aect their health. Please help us provide you with the best medical care by
answering the questions below.
Please circle the best response to each question.
Alcohol and Substance Use Screening Questionnaire
Change #5 Resources: Monitoring
* if patient needs further explanation, “for example, for the feeling or experience it caused.”
Click to Access a PDF of the AUDIT-C Plus 2
In the past 3 months...
Patient Label
1. How often did you have
a drink containing alcohol?
2. How many drinks
containing alcohol did you
have on a typical day when
you were drinking?
3. How often did you have
5 or more drinks on one
occasion?
4. How often have you
used marijuana?
5. How often have you
used an illegal drug or a
prescription medication for
non-medical reasons*?
Never
0
Monthly or less
1
2-4 times a month 2-3 times a week 4+ times a week
2 3 4
Never
1 or 2
drinks
0 0 1 2 4
3 or 4
drinks
5 or 6
drinks
7, 8 or 9
drinks
10 or more
drinks
3
Never
0
Less than
monthly
1
Monthly Weekly
Daily or
almost daily
2 3 4
Never
0
Not monthly
1
Monthly Weekly Daily or almost
2 3 4
Never
0
Less than
monthly
1
Monthly Weekly
Daily or
almost daily
2 3 4
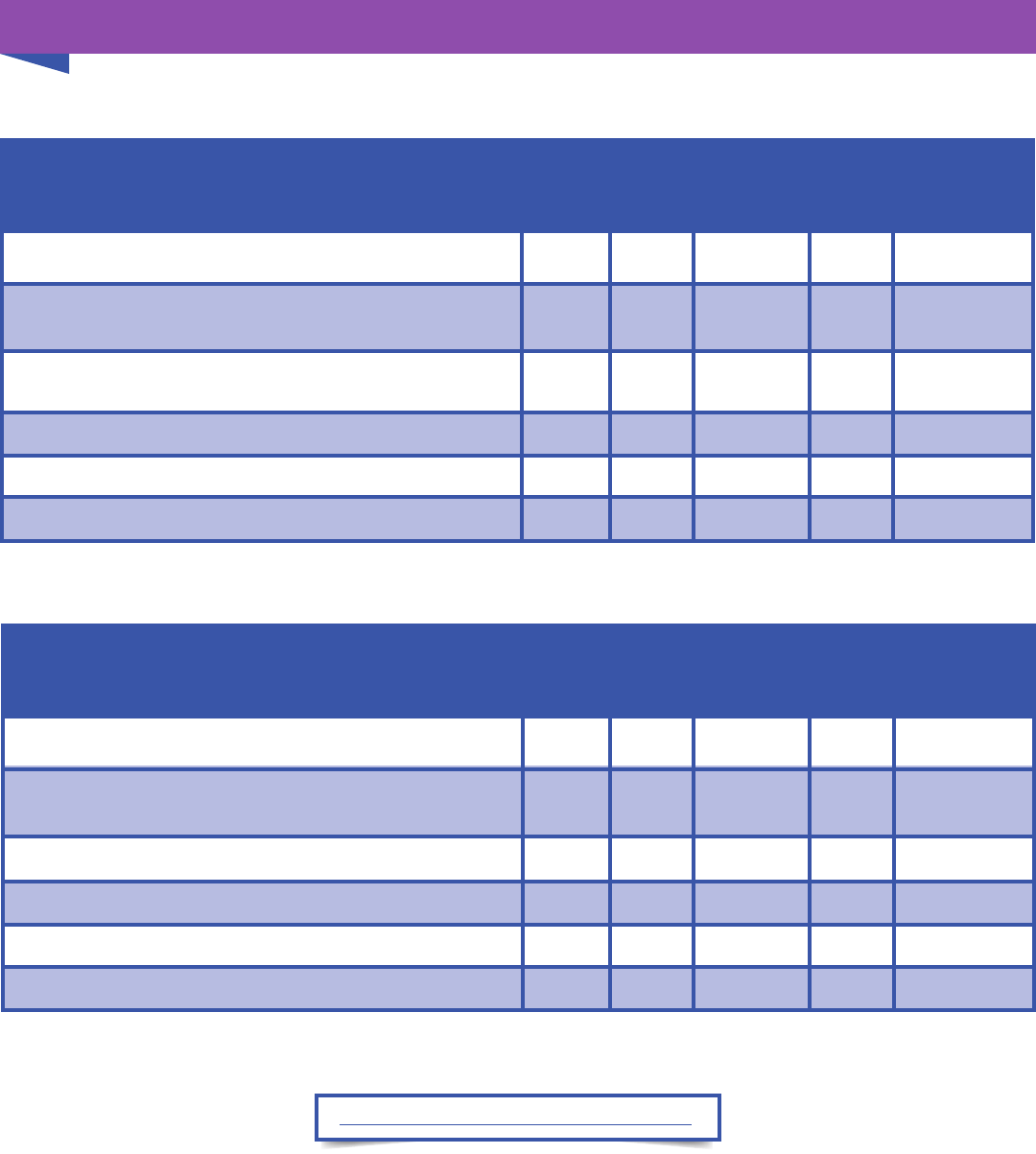
41
Click to Access a PDF of the SAM and SDUM
Change #5 Resources: Monitoring, CONT.
How often in the past 2 weeks...
1.
2.
3.
4.
5.
Were you bothered by how your drinking impacted your
health, relationships, goals or life?
Did you have trouble controlling your drinking, drink too
much or spend too much time drinking?
Was it dicult to get the thought of drinking out of your mind?
Did you disappoint yourself or others due to drinking?
Have you had trouble getting things done due to drinking?
Never Rarely Sometimes Often Almost always
Never Rarely Sometimes Often Almost always
Never Rarely Sometimes Often Almost always
Never Rarely Sometimes Often Almost always
Never Rarely Sometimes Often Almost always
0 1 2 3 4
Short Drug Use Monitor (SDUM)
How often in the past 2 weeks...
1.
2.
3.
4.
5.
Were you bothered by how your drug use impacted your
health, relationships, goals or life?
Did you spend a lot of time using drugs?
Were drugs the only thing you could think about?
Did you disappoint yourself or others due to drug use?
Did you feel your drug use was out of control?
These questions are to help you and your medical team monitor how your drug use may be aecting you.
Circle one best answer for each question.
Never Rarely Sometimes Often Almost always
Never Rarely Sometimes Often Almost always
Never Rarely Sometimes Often Almost always
Never Rarely Sometimes Often Almost always
Never Rarely Sometimes Often Almost always
0 1 2 3 4
Short Alcohol Monitor (SAM)
These questions are to help you and your medical team monitor how your drinking may be aecting you.
Circle one best answer for each question.

42
TRAINING OPPORTUNITIES
IRETA Training and Technical Assistance
Relias - SBIRT: Intervention and Treatment Services for Individuals with Substance Use Issues
ATTC National Registry of SBIRT Trainers
National Council Consulting Service
Find more training opportunities at the SAMHSA HRSA Center for Integrated Health Solutions
Change #8 Resources: Train Primary Care Teams

43
ALTERNATIVE PAYMENT PROGRAMS: THE CMS MIPS PROGRAM
CMS Quality Payment Program
The Centers for Medicare and Medicaid Services (CMS) launched the new Quality Payment Program on January 1,
2017. This program only applies to certain clinicians who bill Medicare Part B using the physician fee schedule. The
vast majority of eligible clinicians in 2017 will participate through the Merit-based Incentive Payment System (MIPS).
Individual clinicians and clinician groups are scored in several MIPS performance categories, including Quality (60
percent of the total score) and Improvement Activities (15 percent of the total score). The higher the score, the more
likely the clinician or clinician group is to receive a positive payment adjustment.
MIPS Quality measures include:
Preventive care and screening: Unhealthy alcohol use—Percentage of patients aged 18 years and older who were
screened for unhealthy alcohol use using a systematic screening method at least once within the last 24 months AND
who received brief counseling if identified as an unhealthy alcohol user.
MIPS Improvement Activities include:
Unhealthy alcohol use: Regular engagement of MIPS eligible clinicians or groups in integrated prevention and treatment
interventions, including screening and brief counseling (refer to NQF #2152) for patients with co-occurring behavioral
or mental health conditions.
See the Quality Payment Program website for more information.
Change #9 Resources: Billing and Finances

44
Change #9 Resources: Billing and Finances, CONT.
SBIRT BILLING CODES
The American Medical Association (AMA) has approved several billing codes that will allow practices to be reimbursed
for providing screening and brief intervention services. Medical procedures are coded using Common Procedure and
Terminology (CPT) and Healthcare Common Procedure Coding System (HCPCS) codes. Screening and brief intervention
may be provided in an oce, emergency department, or inpatient visit for both new and established patients. Payers
often use AMA’s Evaluation and Management (E&M) CPT codes to pay physicians’ services. Many payers reimburse for
independent licensed health practitioners, such as advance practice nurses, psychologists, and Masters-level social
workers. A few will pay for service provided by health professionals under the supervision of a physician.
*Several CPT codes can be used. The information in the table above shows the most commonly used codes.
**See Reimbursement for SBIRT for more information.
Payer Code Description
Commercial
Insurance, Medicaid
99408
Alcohol and/or drug use structured screening and brief intervention
services; 15 to 30 minutes
Commercial
Insurance, Medicaid
99409
Alcohol and/or drug use structured screening and brief intervention
services; greater than 30 minutes
Medicare G0396
Alcohol and/or drug use structured screening and brief intervention
services; 15 to 30 minutes
Medicare G0397
Alcohol and/or drug use structured screening and brief intervention
services; greater than 30 minutes
Medicare G0442
Prevention: Screening for alcohol misuse in adults including pregnant
women once per year. No coinsurance; no deductible for patient
www.cms.gov/medicare-coverage-database/details/nca-
decision-memo.aspx
Medicare G0443
Prevention: Up to four, 15-minute, brief face-to-face behavioral
counseling interventions per year for individuals, including
pregnant women, who screen positive for unhealthy alcohol use;
No coinsurance; no deductible for patient http://www.cms.hhs.
gov/medicare-coverage-database/details/nca-decision-memo.
aspx?NCAId=249
Medicaid H0049 Alcohol and/or other drug screening (code not widely used)
Medicaid H0049
Alcohol and/or other drug service, brief intervention, per 15 minutes
(code not widely used)
Table A.2 SBI Billing Codes

45
Change #9 Resources: Billing and Finances, CONT.
SBIRT ICD10 CODES
When a diagnosis code is needed, ICD-10 codes in the F10 to F19 section for mental and behavioral disorders due to
alcohol and/or other drug use are used, for example:
For more information, see WHO’s ICD-10 Classification of Mental and Behavioral Disorders: Clinical descriptions
and diagnostic guidelines.
Table A.3 ICD Codes for Alcohol and/or Other Drug Use
F10. Mental and behavioral disorders due to use of alcohol
F11. Mental and behavioral disorders due to use of opioids
F12. Mental and behavioral disorders due to use of cannabinoids
F13. Mental and behavioral disorders due to use of sedative hypnotics
F14. Mental and behavioral disorders due to use of cocaine
F15. Mental and behavioral disorders due to use of other stimulants, including caeine
F16. Mental and behavioral disorders due to use of hallucinogens
F17. Mental and behavioral disorders due to use of tobacco
F18. Mental and behavioral disorders due to use of volatile solvents
F19. Mental and behavioral disorders due to multiple drug use and use of other psychoactive substances

46
Change #9 Resources: Billing and Finances, CONT.
RETURN ON INVESTMENT
SBIRT might generate shared savings (e.g., Accountable Care Organizations) and improve cost performance under MIPS.
The following table describes three SBIRT studies and the modeling of the savings that might have resulted from each
program.
* Paraprofessionals elicited greater reductions in alcohol consumption than master’s-level sta
Alcohol and drugs
Fleming et al.,
2000
116, 117
Estee et al.,
2000
118
Paltzer et al.,
2016
119
Alcohol and/or
Other Drugs:
Alcohol Alcohol and drugs
Primary careSetting: Primary care
Emergency
departments
All adultsPatients: All adults
Disabled adults
with Medicaid
Two-thirds paraprofessionals*,
one-third Masters-level counselors
and social workers
Intervention sta:
Physicians and
nurses
Chemical dependency
counselors
$48 (1 year), $96 (2 years)
Investment:
$205
$15
$439 (1 year), $878 (2 years)
Savings & timeframe:
$523 (1 year)
$4,392 (1 year)
$391 (1 year), $782 (2 years)
Net savings & timeframe:
$318 (1 year)
$4,377 (1 year)
8.1
Return on investment
1.6
292
Table A.4 SBIRT Cost Savings

47
Over the past 15 to 20 years, SAMHSA as well as other organizations have encouraged healthcare settings, such as
emergency departments and primary care practices, to implement Screening, Brief interventions, and Referral to Treatment
(SBIRT) to better address alcohol and/or other drug use in mainstream medical care. There have also been many practice-
based studies and research on the eectiveness of SBIRT for alcohol and other drugs, as well as on barriers and facilitators
to implementation of SBIRT.
Practice
Since 2003, SAMHSA has funded states, academic medical programs, and college campuses to implement SBIRT services
and training programs which has led to states and organizations across the country to implement improved alcohol and/
or other drug-related care in medical settings. There are now vast resources and examples for training, implementation,
evaluation, fidelity monitoring, EHR programming, screening tools, brief intervention models, and computerized SBIRT
programs and applications. While there are documented benefits to implementing SBIRT
103, 117
, there are also a variety of
barriers that have kept the practice from becoming part of regular care in medical settings in the United States, including
factors at the national, system, organization, and individual (patient, clinician, and sta) levels.
120, 121
A major challenge
has been sustaining ongoing improvements in care when funding from SAMHSA ended.
Research
The most robust evidence for screening and brief intervention (SBI) is in primary care practices for alcohol; there is good
evidence that patients report reducing their drinking after receiving brief intervention in primary care.
2
However, there
are three main areas in the SBIRT research literature that highlight the limitations of the model:
Emergency departments have shown mixed evidence for ecacy of SBIRT.
122
There is a lack of ecacy for SBI for non-alcohol drug use in primary care practices.
123
Inconsistent success of referrals to treatment, and ineective engagement in specialty treatment for alcohol
and/or other drug use disorders as a result of referral as part of SBIRT.
124, 125
USPSTF currently recommends alcohol screening and counseling for adult primary care patients (Category B). The
USPSTF does not currently recommend screening and brief intervention for other drugs, given the lack of evidence
(their recommendations will be updated again in 2017). This mixed evidence for SBIRT has led experts to question
whether screening and brief intervention should be implemented for other drugs in emergency departments; it has also
posed a challenge to the field regarding how to move forward in implementing care for alcohol and/or other drugs in
healthcare settings.
122, 126
The Current State of SBIRT in Practice and Research
•
•
•

48
Why an Extension and Update of the SBIRT Model?
SBIRT has been an important step in highlighting and potentially improving the care of patients with alcohol and/or
other drug use problems in medical settings. As the primary care environment continues to evolve to better achieve
primary and behavioral healthcare integration and in light the current state of research, the SBIRT model must be
updated. There are exceptional opportunities in primary care given healthcare reforms that are making integrated care
in primary care settings more common and achievable. These opportunities to extend the model include integration
of evidence-based medications for alcohol and opioid use disorders, payment and reimbursement models (e.g., care
coordination billing codes, and value based payment), newer practice models (e.g., patient-centered medical homes,
collaborative care), and ability to align with the best evidence-based practices for alcohol and/or other drug use care in
primary care settings. Despite the lack of evidence for the full SBIRT model as we know it today for other drug use, there
is still a need to address drug use in healthcare settings because of the benefit of treating drug use disorders.
The major expansions and updates to the SBIRT model that are proposed in this guide include monitoring and
management of patients with alcohol and/or other drug use problems within the primary care practice, rather than
solely relying on referrals to specialty treatment providers, as has been historically done. This expanded model builds
on the successful management of depression and anxiety in primary care, using collaborative care principles and
measurement-based care, and moves the field toward more comprehensive care of people with harmful use of alcohol
and/or other drugs within primary care. Most importantly, it prepares primary care clinicians to integrate care for alcohol
and/or other drug into routine care in a manner consistent with the patient-centered medical home (PCMH) and value-
based incentives to improve clinical outcomes.
The Current State of SBIRT in Practice and Research, CONT.

49
References
1. Watkins, K. E., Ober, A. J., Lamp, K., Lind, M., Setodji, C., Osilla, K. C., . . . Pincus, H. A. (2017). Collaborative Care for Opioid and Alcohol
Use Disorders in Primary Care: The SUMMIT Randomized Clinical Trial. JAMA Intern Med. doi:10.1001/jamainternmed.2017.3947
2. Babor, T. F., Del Boca, F., & Bray, J. W. (2017). Screening, Brief Intervention and Referral to Treatment: implications of SAMHSA’s SBIRT
initiative for substance abuse policy and practice. Addiction, 112 Suppl 2, 110-117. doi:10.1111/add.13675
3. Johnson, J. A., Lee, A., Vinson, D., & Seale, J. P. (2013). Use of AUDIT-based measures to identify unhealthy alcohol use and alcohol
dependence in primary care: a validation study. Alcohol Clin Exp Res, 37 Suppl 1, E253-259. doi:10.1111/j.1530-0277.2012.01898.x
4. Jonas, D. E., Garbutt, J. C., Amick, H. R., Brown, J. M., Brownley, K. A., Council, C. L., . . . Richmond, E. M. (2012). Behavioral counseling
after screening for alcohol misuse in primary care: a systematic review and meta-analysis for the U.S. Preventive Services Task Force.
Ann Intern Med, 157. doi:10.7326/0003-4819-157-9-201211060-00544
5. Moyer, V. A., & Preventive Services Task Force. (2013). Screening and behavioral counseling interventions in primary care
to reduce alcohol misuse: U.S. preventive services task force recommendation statement. Ann Intern Med, 159(3), 210-218.
doi:10.7326/0003-4819-159-3-201308060-00652
6. Bradley, K. A., & Kivlahan, D. R. (2014). Bringing patient-centered care to patients with alcohol use disorders. JAMA, 311(18), 1861-
1862. doi:10.1001/jama.2014.3629
7. Rose, H. L. (2008). Alcohol screening and brief counseling in a primary care hypertensive population: a quality improvement
intervention. Addiction (Abingdon, England), 103(8), 1271-1280. doi:10.1111/j.1360-0443.2008.02199.x
8. Williams, E. C., Rubinsky, A. D., Chavez, L. J., Lapham, G. T., Rittmueller, S. E., Achtmeyer, C. E., & Bradley, K. A. (2014). An early
evaluation of implementation of brief intervention for unhealthy alcohol use in the US Veterans Health Administration. Addiction,
109(9), 1472-1481. doi:10.1111/add.12600
9. SAMHSA. (2016). Key substance use and mental health indicators in the United States: Results from the 2015 National Survey on
Drug Use and Health. Retrieved from http://www.samhsa.gov/data/
10. Wu, L. T., McNeely, J., Subramaniam, G. A., Brady, K. T., Sharma, G., VanVeldhuisen, P., . . . Schwartz, R. P. (2017). DSM-5 substance
use disorders among adult primary care patients: Results from a multisite study. Drug Alcohol Depend, 179, 42-46. doi:10.1016/j.
drugalcdep.2017.05.048
11. Saitz, R. (2005). Clinical practice. Unhealthy alcohol use. N Engl J Med, 352(6), 596-607. doi:10.1056/NEJMcp042262
12. Solberg, L. I., Maciosek, M. V., & Edwards, N. M. (2008). Primary care intervention to reduce alcohol misuse ranking its health impact
and cost eectiveness. Am J Prev Med, 34(2), 143-152.
13. Saitz, R., Horton, N. J., & Samet, J. H. (2003). Alcohol and medication interactions in primary care patients: common and
unrecognized. Am J Med, 114(5), 407-410.
14. Bryson, C. L., Au, D. H., Sun, H., Williams, E. C., Kivlahan, D. R., & Bradley, K. A. (2008). Alcohol screening scores and medication
nonadherence. Ann Intern Med, 149(11), 795-804.
15. Chi, F. W., Weisner, C. M., Mertens, J. R., Ross, T. B., & Sterling, S. A. (2017). Alcohol brief intervention in primary care: Blood pressure
outcomes in hypertensive patients. J Subst Abuse Treat, 77, 45-51. doi:10.1016/j.jsat.2017.03.009
16. Ahmed, A. T., Karter, A. J., & Liu, J. (2006). Alcohol consumption is inversely associated with adherence to diabetes self-care
behaviours. Diabet Med, 23(7), 795-802.
17. Hellard, M., Sacks-Davis, R., & Gold, J. (2009). Hepatitis C Treatment for Injection Drug Users: A Review of the Available Evidence.
Clinical Infectious Diseases, 49(4), 561-573. doi:10.1086/600304
18. Pessione, F., Degos, F., Marcellin, P., Duchatelle, V., Njapoum, C., Martinot-Peignoux, M., . . . Rue, B. (1998). Eect of alcohol
consumption on serum hepatitis C virus RNA and histological lesions in chronic hepatitis C. Hepatology, 27(6), 1717-1722. doi:10.1002/
hep.510270635
19. Miller, P. M., Thomas, S. E., & Mallin, R. (2006). Patient attitudes towards self-report and biomarker alcohol screening by primary care
physicians. Alcohol Alcohol, 41(3), 306-310. doi:10.1093/alcalc/agl022
20. Simonetti, J. A., Lapham, G. T., & Williams, E. C. (2015). Association Between Receipt of Brief Alcohol Intervention and Quality of
Care among Veteran Outpatients with Unhealthy Alcohol Use. J Gen Intern Med, 30(8), 1097-1104. doi:10.1007/s11606-015-3218-5

50
21. Smith, P. C., Schmidt, S. M., Allensworth-Davies, D., & Saitz, R. (2010). A single-question screening test for drug use in primary care.
Arch Intern Med, 170(13), 1155-1160. doi:10.1001/archinternmed.2010.140
22. Babor, T. F., Higgins-Biddle, J. C., Saunders, J. B., & Monteiro, M. G. (2001). AUDIT: The Alcohol Use Disorders Identification Test:
Guidelines for Use in Primary Care, 2nd Edition. Retrieved from http://www.dass.stir.ac.uk/DRUGS/pdf/audit.pdf
23. Tiet, Q. Q., Leyva, Y. E., Moos, R. H., Frayne, S. M., Osterberg, L., & Smith, B. (2015). Screen of Drug Use: Diagnostic Accuracy of a
New Brief Tool for Primary Care. JAMA Intern Med, 175(8), 1371-1377. doi:10.1001/jamainternmed.2015.2438
24. McNeely, J., Wu, L. T., Subramaniam, G., Sharma, G., Cathers, L. A., Svikis, D., . . . Schwartz, R. P. (2016). Performance of the Tobacco,
Alcohol, Prescription Medication, and Other Substance Use (TAPS) Tool for Substance Use Screening in Primary Care Patients. Ann
Intern Med, 165(10), 690-699. doi:10.7326/M16-0317
25. McNeely, J., Cleland, C. M., Strauss, S. M., Palamar, J. J., Rotrosen, J., & Saitz, R. (2015). Validation of Self-Administered Single-Item
Screening Questions (SISQs) for Unhealthy Alcohol and Drug Use in Primary Care Patients. J Gen Intern Med, 30(12), 1757-1764.
doi:10.1007/s11606-015-3391-6
26. Bush, K., Kivlahan, D. R., McDonell, M. B., Fihn, S. D., & Bradley, K. A. (1998). The AUDIT alcohol consumption questions (AUDIT-C):
an eective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders
Identification Test. Arch Intern Med, 158(16), 1789-1795.
27. National Institute on Alcohol Abuse and Alcoholism. (2005). Helping Patients Who Drink Too Much: A Clinician’s Guide (Updated
2005 Edition) (NIH Publication 07–3769). Retrieved from Washington, D.C.: http://pubs.niaaa.nih.gov/publications/Practitioner/
CliniciansGuide2005/guide.pdf
28. Fischer, B., Russell, C., Sabioni, P., van den Brink, W., Le Foll, B., Hall, W., . . . Room, R. (2017). Lower-Risk Cannabis Use Guidelines: A
Comprehensive Update of Evidence and Recommendations. Am J Public Health, 107(8), 1277. doi:10.2105/AJPH.2017.303818a
29. Rehm, J., Dawson, D., Frick, U., Gmel, G., Roerecke, M., Shield, K. D., & Grant, B. (2014). Burden of disease associated with alcohol
use disorders in the United States. Alcohol Clin Exp Res, 38(4), 1068-1077. doi:10.1111/acer.12331
30. Rubinsky, A. D., Dawson, D. A., Williams, E. C., Kivlahan, D. R., & Bradley, K. A. (2013). AUDIT-C scores as a scaled marker of mean
daily drinking, alcohol use disorder severity, and probability of alcohol dependence in a U.S. general population sample of drinkers.
Alcohol Clin Exp Res, 37(8), 1380-1390. doi:10.1111/acer.12092
31. Rubinsky, A. D., Kivlahan, D. R., Volk, R. J., Maynard, C., & Bradley, K. A. (2010). Estimating risk of alcohol dependence using alcohol
screening scores. Drug Alcohol Depend, 108(1-2), 29-36. doi:10.1016/j.drugalcdep.2009.11.009
32. Reynolds, C. F., 3rd, & Frank, E. (2016). US Preventive Services Task Force Recommendation Statement on Screening for Depression
in Adults: Not Good Enough. JAMA Psychiatry, 73(3), 189-190. doi:10.1001/jamapsychiatry.2015.3281
33. Bradley, K. A., Rubinsky, A. D., Sun, H., Bryson, C. L., Bishop, M. J., Blough, D. K., . . . Kivlahan, D. R. (2011). Alcohol screening and
risk of postoperative complications in male VA patients undergoing major non-cardiac surgery. J Gen Intern Med, 26(2), 162-169.
doi:10.1007/s11606-010-1475-x
34. Bradley, K., Rubinsky, A., Lapham, G., & al, e. (2016). Predictive validity of clinical AUDIT-C alcohol screening scores and changes in
scores for three objective alcohol-related outcomes in a Veterans Aairs population. Addiction, 111(11), 1975-1984.
35. Saha, T. D., Chou, S. P., & Grant, B. F. (2006). Toward an alcohol use disorder continuum using item response theory: results from
the National Epidemiologic Survey on Alcohol and Related Conditions. Psychol Med, 36(7), 931-941. doi:
36. Hasin, D. S., O’Brien, C. P., Auriacombe, M., Borges, G., Bucholz, K., Budney, A., . . . Grant, B. F. (2013). DSM-5 criteria for substance use
disorders: recommendations and rationale. Am J Psychiatry, 170(8), 834-851. doi:10.1176/appi.ajp.2013.12060782
37. American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders, 5th Edition. Washington D.C.:
American Psychiatric Association.
38. Dawson, D. A., & Grant, B. F. (2010). Should symptom frequency be factored into scalar measures of alcohol use disorder severity?
Addiction, 105(9), 1568-1579. doi:10.1111/j.1360-0443.2010.02994.x
39. Dawson, D. A., Saha, T. D., & Grant, B. F. (2010). A multidimensional assessment of the validity and utility of alcohol use disorder
severity as determined by item response theory models. Drug and Alcohol Dependence, 107(1), 31-38. doi:S0376-8716(09)00353-6
[pii] 10.1016/j.drugalcdep.2009.08.019
References, CONT.

51
References, CONT.
40. Williams, E. C., Kivlahan, D. R., Saitz, R., Merrill, J. O., Achtmeyer, C. E., McCormick, K. A., & Bradley, K. A. (2006). Readiness to change
in primary care patients who screened positive for alcohol misuse. Ann Fam Med, 4(3), 213-220. doi:10.1370/afm.542
41. Au, D. H., Kivlahan, D. R., Bryson, C. L., Blough, D., & Bradley, K. A. (2007). Alcohol screening scores and risk of hospitalizations for
GI conditions in men. Alcohol Clin Exp Res, 31(3), 443-451. doi:10.1111/j.1530-0277.2006.00325.x
42. Berger, D., Williams, E. C., Bryson, C. L., Rubinsky, A. D., & Bradley, K. A. (2013). Alcohol questionnaires and HDL: screening scores
as scaled markers of alcohol consumption. Alcohol, 47(6), 439-445. doi:10.1016/j.alcohol.2013.07.001
43. Chavez LJ, Liu CF, Tet N, Hebert P, Clark B, Rubinsky AD, . . . Bradley KA. (2015). Unhealthy alcohol use in older adults: Association
with 30-day readmissions and emergency department use in the 30 days after hospital discharge. Drug and Alcohol Dependence(in
press).
44. Chew, L. D., Nelson, K. M., Young, B. A., & Bradley, K. A. (2005). Association between alcohol consumption and diabetes preventive
practices. Fam Med, 37(8), 589-594.
45. Harris, A. H., Bradley, K. A., Bowe, T., Henderson, P., & Moos, R. (2010). Associations between AUDIT-C and mortality vary by age
and sex. Popul Health Manag, 13(5), 263-268. doi:10.1089/pop.2009.0060
46. Harris, A. H., Bryson, C. L., Sun, H., Blough, D., & Bradley, K. A. (2009). Alcohol screening scores predict risk of subsequent fractures.
Subst Use Misuse, 44(8), 1055-1069. doi:10.1080/10826080802485972
47. Harris, A. H., Lembke, A., Henderson, P., Gupta, S., Moos, R., & Bradley, K. A. (2012). Risk of future trauma based on alcohol screening
scores: a two-year prospective cohort study among US veterans. Addict Sci Clin Pract, 7, 6. doi:10.1186/1940-0640-7-6
48. Kinder, L. S., Bryson, C. L., Sun, H., Williams, E. C., & Bradley, K. A. (2009). Alcohol screening scores and all-cause mortality in male
Veterans Aairs patients. J Stud Alcohol Drugs, 70(2), 253-260.
49. Lembke, A., Bradley, K. A., Henderson, P., Moos, R., & Harris, A. H. (2011). Alcohol screening scores and the risk of new-onset
gastrointestinal illness or related hospitalization. J Gen Intern Med, 26(7), 777-782. doi:10.1007/s11606-011-1688-7
50. Peytremann-Bridevaux, I., Bryson, C. L., Au, D. H., McDonell, M. B., Fihn, S. D., & Bradley, K. A. (2004). The association between
AUDIT-C and health status. Paper presented at the Society for General Internal Medicine, Chicago, IL.
51. Rubinsky, A. D., Bishop, M. J., Maynard, C., Henderson, W. G., Hawn, M. T., Harris, A. H. S., . . . Bradley, K. A. (To be submitted).
Postoperative risks associated with alcohol screening depend on documented drinking at the time of surgery.
52. Williams EC, Bryson CL, Sun H, Chew RB, Chew LD, Blough DK, . . . Bradley KA. (2012). Association between alcohol screening
results and hospitalizations for trauma in Veterans Aairs outpatients. Am J Drug Alcohol Abuse, 38(1), 73-80.
53. Roth, J. A., Bradley, K., Thummel, K. E., Veenstra, D. L., & Boudreau, D. (2015). Alcohol misuse, genetics, and major bleeding among
warfarin therapy patients in a community setting. Pharmacoepidemiol Drug Saf, 24(6), 619-627. doi:10.1002/pds.3769
54. Peterson, K. (2004/2005). Biomarkers for Alcohol Use and Abuse. Alcohol Research and Health, 28.
55. Bradley, K. A., Ludman, E. J., Chavez, L. J., Bobb, J. F., Ruedebusch, S. J., Achtmeyer, C. E., . . . Kivlahan, D. R. (2017). Patient-centered
primary care for adults at high risk for AUDs: the Choosing Healthier Drinking Options In primary CarE (CHOICE) trial. Addiction
Science & Clinical Practice, 12(1), 15. doi:10.1186/s13722-017-0080-2
56. Whitlock, E. P., Polen, M. R., Green, C. A., Orleans, T., & Klein, J. (2004). Behavioral counseling interventions in primary care to
reduce risky/harmful alcohol use by adults: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med,
140(7), 557-568.
57. Latimer, N., Guillaume, L., Goyder, E., Chilcott, J., & Payne, N. (2009). Alcohol Use Disorders - Preventing Harmful Drinking. Screening
and Brief Interventions: Cost Eectiveness Review. Retrieved from http://www.shef.ac.uk/polopoly_fs/1.43294!/file/Alcohol-2_3.pdf
58. Gelberg, L., Andersen, R. M., Afifi, A. A., Leake, B. D., Arangua, L., Vahidi, M., . . . Baumeister, S. E. (2015). Project QUIT (Quit Using
Drugs Intervention Trial): a randomized controlled trial of a primary care-based multi-component brief intervention to reduce risky
drug use. Addiction, 110(11), 1777-1790. doi:10.1111/add.12993
59. Jonas, D. E., Amick, H. R., Feltner, C., Bobashev, G., Thomas, K., Wines, R., . . . Garbutt, J. C. (2014). Pharmacotherapy for adults
with alcohol use disorders in outpatient settings: a systematic review and meta-analysis. JAMA, 311(18), 1889-1900. doi:10.1001/
jama.2014.3628

52
References, CONT.
60. Carroll, K. M. (2012). Dissemination of evidence-based practices: how far we’ve come, and how much further we’ve got to go.
Addiction, 107(6), 1031-1033. doi:10.1111/j.1360-0443.2011.03755.x
61. McCrady, B. S. (2013). Health-care reform provides an opportunity for evidence-based alcohol treatment in the USA: the National
Institute for Health and Clinical Excellence (NICE) guideline as a model. Addiction, 108(2), 231-232. doi:10.1111/j.1360-0443.2012.04052.x
62. Kelly, J. F., Stout, R. L., Magill, M., & Tonigan, J. S. (2011). The role of Alcoholics Anonymous in mobilizing adaptive social network
changes: a prospective lagged mediational analysis. Drug Alcohol Depend, 114(2-3), 119-126. doi:10.1016/j.drugalcdep.2010.09.009
63. Beck, A. K., Forbes, E., Baker, A. L., Kelly, P. J., Deane, F. P., Shakeshaft, A., . . . Kelly, J. F. (2017). Systematic review of SMART Recovery:
Outcomes, process variables, and implications for research. Psychol Addict Behav, 31(1), 1-20. doi:10.1037/adb0000237
64. Watkins, K., Pincus, H. A., Tanielian, T. L., & Lloyd, J. (2003). Using the chronic care model to improve treatment of alcohol use
disorders in primary care settings. J Stud Alcohol, 64(2), 209-218.
65. Institute of Medicine. (2006). Improving the Quality of Health Care for Mental and Substance-Use Conditions: Quality Chasm
Series. Washington, DC: National Academies Press.
66. Cohen, E., Feinn, R., Arias, A., & Kranzler, H. R. (2007). Alcohol treatment utilization: findings from the National Epidemiologic
Survey on Alcohol and Related Conditions. Drug Alcohol Depend, 86(2-3), 214-221. doi:S0376-8716(06)00229-8 [pii] 10.1016/j.
drugalcdep.2006.06.008
67. Glass, J. E., Hamilton, A. M., Powell, B. J., Perron, B. E., Brown, R. T., & Ilgen, M. A. (2015). Specialty substance use disorder services
following brief alcohol intervention: a meta-analysis of randomized controlled trials. Addiction, 110(9), 1404-1415. doi:10.1111/
add.12950
68. Willenbring, M. L., & Olson, D. H. (1999). A randomized trial of integrated outpatient treatment for medically ill alcoholic men. Arch
Intern Med, 159(16), 1946-1952.
69. Willenbring, M. L., Olson, D. H., & Bielinski, J. (1995). Integrated outpatients treatment for medically ill alcoholic men: results from
a quasi-experimental study. J Stud Alcohol, 56(3), 337-343.
70. Oslin, D. W., Lynch, K. G., Maisto, S. A., Lantinga, L. J., McKay, J. R., Possemato, K., . . . Wierzbicki, M. (2014). A randomized clinical trial
of alcohol care management delivered in Department of Veterans Aairs primary care clinics versus specialty addiction treatment. J
Gen Intern Med, 29(1), 162-168. doi:10.1007/s11606-013-2625-8
71. Alford, D. P., LaBelle, C. T., Kretsch, N., Bergeron, A., Winter, M., Botticelli, M., & Samet, J. H. (2011). Collaborative care of opioid-
addicted patients in primary care using buprenorphine: five-year experience. Arch Intern Med, 171(5), 425-431. doi:10.1001/
archinternmed.2010.541
72. LaBelle, C. T., Han, S. C., Bergeron, A., & Samet, J. H. (2016). Oce-Based Opioid Treatment with Buprenorphine (OBOT-B):
Statewide Implementation of the Massachusetts Collaborative Care Model in Community Health Centers. J Subst Abuse Treat, 60,
6-13. doi:10.1016/j.jsat.2015.06.010
73. Fiellin, D. A., & O’Connor, P. G. (2002). Clinical practice. Oce-based treatment of opioid-dependent patients. N Engl J Med, 347(11),
817-823. doi:10.1056/NEJMcp013579
74. Fiellin, D. A., Pantalon, M. V., Chawarski, M. C., Moore, B. A., Sullivan, L. E., O’Connor, P. G., & Schottenfeld, R. S. (2006). Counseling plus
buprenorphine-naloxone maintenance therapy for opioid dependence. N Engl J Med, 355(4), 365-374. doi:10.1056/NEJMoa055255
75. Fiellin, D. A., Pantalon, M. V., Pakes, J. P., O’Connor, P. G., Chawarski, M., & Schottenfeld, R. S. (2002). Treatment of heroin dependence
with buprenorphine in primary care. Am J Drug Alcohol Abuse, 28(2), 231-241.
76. Anton, R. F., O’Malley, S. S., Ciraulo, D. A., Cisler, R. A., Couper, D., Donovan, D. M., . . . Combine Study Research Group. (2006).
Combined pharmacotherapies and behavioral interventions for alcohol dependence: the COMBINE study: a randomized controlled
trial. JAMA, 295(17), 2003-2017. doi:10.1001/jama.295.17.2003
77. Dunlap, B., & Cifu, A. S. (2016). Clinical Management of Opioid Use Disorder. JAMA, 316(3), 338-339. doi:10.1001/jama.2016.9795
78. Ling, W., Hillhouse, M., Ang, A., Jenkins, J., & Fahey, J. (2013). Comparison of behavioral treatment conditions in buprenorphine
maintenance. Addiction, 108(10), 1788-1798. doi:10.1111/add.12266

53
References, CONT.
79. Amato, L., Minozzi, S., Davoli, M., & Vecchi, S. (2011). Psychosocial combined with agonist maintenance treatments versus agonist
maintenance treatments alone for treatment of opioid dependence. Cochrane Database Syst Rev(10), CD004147. doi:10.1002/14651858.
CD004147.pub4
80. Weiss, R. D., Potter, J. S., Fiellin, D. A., Byrne, M., Connery, H. S., Dickinson, W., . . . Ling, W. (2011). Adjunctive counseling during brief
and extended buprenorphine-naloxone treatment for prescription opioid dependence: a 2-phase randomized controlled trial. Arch
Gen Psychiatry, 68(12), 1238-1246. doi:10.1001/archgenpsychiatry.2011.121
81. Lee, J. D., Friedmann, P. D., Kinlock, T. W., Nunes, E. V., Boney, T. Y., Hoskinson, R. A., Jr., . . . O’Brien, C. P. (2016). Extended-Release
Naltrexone to Prevent Opioid Relapse in Criminal Justice Oenders. N Engl J Med, 374(13), 1232-1242. doi:10.1056/NEJMoa1505409
82. Providers’ Clinical Support System for Opioid Therapies. Retrieved from http://pcss-o.org/
83. Pear Therapeutics. (2017). Pear Therapeutics Obtains FDA Clearance of the First Prescription Digital Therapeutic to Treat Disease
[Press release]
84. Kelly, J. F., & McCrady, B. S. (2008). Twelve-step facilitation in non-specialty settings. Recent Dev Alcohol, 18, 321-346.
85. Ferri, M., Amato, L., & Davoli, M. (2006). Alcoholics Anonymous and other 12-step programmes for alcohol dependence. Cochrane
Database Syst Rev(3), CD005032. doi:10.1002/14651858.CD005032.pub2
86. Barry, M. J., & Edgman-Levitan, S. (2012). Shared decision making—pinnacle of patient-centered care. N Engl J Med, 366. doi:10.1056/
NEJMp1109283
87. Elwyn, G., Frosch, D., Thomson, R., Joseph-Williams, N., Lloyd, A., Kinnersley, P., . . . Barry, M. (2012). Shared decision making: a
model for clinical practice. J Gen Intern Med, 27(10), 1361-1367. doi:10.1007/s11606-012-2077-6
88. Miller, W. R. (2016). Sacred Cows and Greener Pastures: Reflections from 40 Years in Addiction Research. Alcoholism Treatment
Quarterly, 34(1), 92-115. doi:10.1080/07347324.2015.1077637
89. Elwyn, G., Dehlendorf, C., Epstein, R. M., Marrin, K., White, J., & Frosch, D. L. (2014). Shared decision making and motivational
interviewing: achieving patient-centered care across the spectrum of health care problems. Ann Fam Med, 12(3), 270-275. doi:10.1370/
afm.1615
90. Bradley, K. A., Rubinsky, A. D., Lapham, G. T., Berger, D., Bryson, C., Achtmeyer, C., . . . Kivlahan, D. R. (2016). Predictive validity of
clinical AUDIT-C alcohol screening scores and changes in scores for three objective alcohol-related outcomes in a Veterans Aairs
population. Addiction, 111(11), 1975-1984. doi:10.1111/add.13505
91. Bobb, J., Lee, A., Lapham, G., & al., e. (2017). Evaluation of a Pilot Implementation to Integrate Alcohol-Related Care within Primary
Care. Int J Environ Res Public Health, 14(9).
92. Pilkonis, P. A., Yu, L., Dodds, N. E., Johnston, K. L., Lawrence, S. M., & Daley, D. C. (2016). Validation of the alcohol use item banks
from the Patient-Reported Outcomes Measurement Information System (PROMIS). Drug Alcohol Depend, 161, 316-322. doi:10.1016/j.
drugalcdep.2016.02.014
93. Pilkonis, P. A., Yu, L., Dodds, N. E., Johnston, K. L., Lawrence, S. M., Hilton, T. F., . . . McCarty, D. (2015). Item banks for substance use
from the Patient-Reported Outcomes Measurement Information System (PROMIS[R]): Severity of use and positive appeal of use. Drug
Alcohol Depend, 156, 184-192. doi:10.1016/j.drugalcdep.2015.09.008
94. Pilkonis, P. A. (2013). Item banks for alcohol use from the Patient-Reported Outcomes Measurement Information System : Use,
consequences, and expectancies. Drug and alcohol dependence, 130(1-3), 167-177. doi:10.1016/j.drugalcdep.2012.11.002
95. Annaheim, B., Scotto, T. J., & Gmel, G. (2010). Revising the Cannabis Use Disorders Identification Test (CUDIT) by means of Item
Response Theory. Int J Methods Psychiatr Res, 19(3), 142-155. doi:10.1002/mpr.308
96. Voluse, A. C., Voluse, A. C., Gioia, C. J., Sobell, L. C., & Dum, M. (2012). Psychometric properties of the Drug Use Disorders
Identification Test (DUDIT) with substance abusers in outpatient and residential treatment. Addictive behaviors, 37(1), 36-41.
doi:10.1016/j.addbeh.2011.07.030
97. Babor TF. (2002). The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): development, reliability and feasibility.
Addiction, 91, 1183-1194.

54
References, CONT.
98. World Health Organization. (2010). The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): Manual for use in
primary care. Retrieved from http://apps.who.int/iris/bitstream/10665/44320/1/9789241599382_eng.pdf?ua=1
99. Press, M. J., Howe, R., Schoenbaum, M., Cavanaugh, S., Marshall, A., Baldwin, L., & Conway, P. H. (2017). Medicare Payment for
Behavioral Health Integration. N Engl J Med, 376(5), 405-407. doi:10.1056/NEJMp1614134
100. Cowell, A. J., Dowd, W. N., Mills, M. J., Hinde, J. M., & Bray, J. W. (2017). Sustaining SBIRT in the wild: simulating revenues and costs
for Screening, Brief Intervention and Referral to Treatment programs. Addiction, 112 Suppl 2, 101-109. doi:10.1111/add.13650
101. Brown, R. L. (2015). The business case for hospital-based Behavioral Screening and Intervention. Journal of Hospital Administration,
4, 95-103.
102. Maciosek, M. V., Coeld, A. B., Edwards, N. M., Flottemesch, T. J., Goodman, M. J., & Solberg, L. I. (2006). Priorities among eective
clinical preventive services results of a systematic review and analysis. Am J Prev Med, 31(1), 52-61 (see erratum page 458 Volume
432, Number 455).
103. Maciosek, M. V., LaFrance, A. B., Dehmer, S. P., McGree, D. A., Flottemesch, T. J., Xu, Z., & Solberg, L. I. (2017). Updated Priorities
Among Eective Clinical Preventive Services. Ann Fam Med, 15(1), 14-22. doi:10.1370/afm.2017
104. Quanbeck, A., Lang, K., Enami, K., & Brown, R. L. (2010). A cost-benefit analysis of Wisconsin’s screening, brief intervention, and
referral to treatment program: adding the employer’s perspective. WMJ, 109(1), 9-14.
105. Bradley, K., Bush, K., Epler, A., Dobie, D., Davis, T., Sporleder, J., . . . Kivlahan, D. (2003). Two brief alcohol-screening tests From the
Alcohol Use Disorders Identification Test (AUDIT): validation in a female Veterans Aairs patient population. Arch Intern Med, 163(7),
821-829.
106. Bush, K., Kivlahan, D. R., McDonell, M. B., Fihn, S. D., Bradley, K. A., & for the Ambulatory Care Quality Improvement, P. (1998). The
audit alcohol consumption questions (audit-c): An eective brief screening test for problem drinking. Archives of Internal Medicine,
158(16), 1789-1795. doi:10.1001/archinte.158.16.1789
107. Adamson, S. J., Kay-Lambkin, F. J., Baker, A. L., Lewin, T. J., Thornton, L., Kelly, B. J., & Sellman, J. D. (2010). An improved brief
measure of cannabis misuse: the Cannabis Use Disorders Identification Test-Revised (CUDIT-R). Drug Alcohol Depend, 110(1-2), 137-
143. doi:10.1016/j.drugalcdep.2010.02.017
108. McNeely, J., Wu, L., Subramaniam, G., & et al. (2016). PErformance of the tobacco, alcohol, prescription medication, and other
substance use (taps) tool for substance use screening in primary care patients. Annals of Internal Medicine, 165(10), 690-699.
doi:10.7326/M16-0317
109. Moss, H. B., Chen, C. M., & Yi, H. Y. (2012). Measures of substance consumption among substance users, DSM-IV abusers, and
those with DSM-IV dependence disorders in a nationally representative sample. J Stud Alcohol Drugs, 73(5), 820-828.
110. Hall, W., & Weier, M. (2015). Assessing the public health impacts of legalizing recreational cannabis use in the USA. Clin Pharmacol
Ther, 97(6), 607-615. doi:10.1002/cpt.110
111. Hall, W., & Degenhardt, L. (2009). Adverse health eects of non-medical cannabis use. Lancet, 374(9698), 1383-1391. doi:10.1016/
S0140-6736(09)61037-0
112. Hall, W. (2009). The adverse health eects of cannabis use: what are they, and what are their implications for policy? Int J Drug
Policy, 20(6), 458-466. doi:10.1016/j.drugpo.2009.02.013
113. Rollnick, S., Miller, W.R., Butler, C.C. . (2013). Motivational Interviewing in Health Care. New York, NY: Guilford.
114. Lundahl, B., Moleni, T., Burke, B. L., & Butters, R. (2013). Motivational interviewing in medical care settings: A systematic review
and meta-analysis of randomized controlled trials. Patient Education and Counseling, 93(2), 157-168. doi:10.1016/j.pec.2013.07.012
115. Babson, K. A., Boden, M. T., Harris, A. H., Stickle, T. R., & Bonn-Miller, M. O. (2013). Poor sleep quality as a risk factor for lapse
following a cannabis quit attempt. J Subst Abuse Treat, 44(4), 438-443. doi:10.1016/j.jsat.2012.08.224
116. Fleming M.F., Mundt M.P., French M.T., Manwell L.B., Stauacher E.A., & K.L., B. (2000). Benefit-cost analysis of brief physician advice
with problem drinkers in primary care settings. Medical Care 38:7-18.
117. Fleming, M. F., Barry, K. L., Manwell, L. B., Johnson, K., & London, R. (1997). Brief physician advice for problem alcohol drinkers. A
randomized controlled trial in community-based primary care practices. JAMA, 277(13), 1039-1045.

55
References, CONT.
118. Estee S., Wickizer T., He L., Shah M.F., & D., M. (2010). Evaluation of the Washington State screening, brief intervention and referral
to treatment project: cost outcomes for Medicaid patients screened in hospital emergency departments. Medical Care, 48, 18-24.
119. Paltzer J., Brown R.L., Burns M., Moberg D.P., Mullahy J., Sethi A., & D., W. (2017). Substance use screening, brief Intervention, and
referral to treatment among Medicaid patients in Wisconsin: impacts on healthcare utilization and costs. Journal of Behavioral Health
Services and Research, 44, 102-112.
120. Nilsen, P., Aalto, M., Bendtsen, P., & Seppa, K. (2006). Eectiveness of strategies to implement brief alcohol intervention in primary
healthcare. A systematic review. Scand J Prim Health Care, 24(1), 5-15. doi:10.1080/02813430500475282
121. Williams, E. C., Johnson, M. L., Lapham, G. T., Caldeiro, R. M., Chew, L., Fletcher, G. S., . . . Bradley, K. A. (2011). Strategies to
implement alcohol screening and brief intervention in primary care settings: a structured literature review. Psychol Addict Behav,
25(2), 206-214. doi:10.1037/a0022102
122. Field, C. A., Baird, J., Saitz, R., Caetano, R., & Monti, P. M. (2010). The mixed evidence for brief intervention in emergency
departments, trauma care centers, and inpatient hospital settings: what should we do? Alcohol Clin Exp Res, 34(12), 2004-2010.
doi:10.1111/j.1530-0277.2010.01297.x
123. Saitz, R. (2014). Screening and brief intervention for unhealthy drug use: little or no ecacy. Front Psychiatry, 5, 121. doi:10.3389/
fpsyt.2014.00121
124. Krupski, A., Sears, J. M., Joesch, J. M., Estee, S., He, L., Dunn, C., . . . Ries, R. (2010). Impact of brief interventions and brief treatment
on admissions to chemical dependency treatment. Drug Alcohol Depend, 110(1-2), 126-136. doi:10.1016/j.drugalcdep.2010.02.018
125. Kim, T. W., Bernstein, J., Cheng, D. M., Lloyd-Travaglini, C., Samet, J. H., Palfai, T. P., & Saitz, R. (2017). Receipt of addiction treatment
as a consequence of a brief intervention for drug use in primary care: a randomized trial. Addiction, 112(5), 818-827. doi:10.1111/
add.13701
126. Saitz, R. (2014). Lost in translation: The perils of implementing alcohol brief intervention when there are gaps in evidence and its
interpretation. Addiction, 109(7), 1060-1062. doi:10.1111/add.12500
