
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use
CRESTOR safely and effectively. See full prescribing information for
CRESTOR.
CRESTOR (rosuvastatin) tablets, for oral use
Initial U.S. Approval: 2003
------------------------ RECENT MAJOR CHANGES ---------------------------
Dosage and Administration Modifications Due to Drug Interactions (2.6)
07/2023
Contraindications, Pregnancy and Lactation (4) Removed 01/2023
Warnings and Precautions (5.2) 01/2023
Warnings and Precautions, Concomitant Coumarin Anticoagulants (5.4)
Removed 01/2023
------------------------ INDICATIONS AND USAGE ----------------------------
CRESTOR is an HMG Co-A reductase inhibitor (statin) indicated: (1)
• To reduce the risk of stroke, myocardial infarction, and arterial
revascularization procedures in adults without established coronary heart
disease who are at increased risk of cardiovascular (CV) disease based on
age, hsCRP ≥2 mg/L, and at least one additional CV risk factor.
• As an adjunct to diet to reduce LDL-C in adults with primary
hyperlipidemia.
• As an adjunct to diet to reduce low-density lipoprotein cholesterol (LDL-C)
and slow the progression of atherosclerosis in adults.
• As an adjunct to diet to reduce LDL-C in adults and pediatric patients aged
8 years and older with heterozygous familial hypercholesterolemia (HeFH).
• As an adjunct to other LDL-C-lowering therapies, or alone if such
treatments are unavailable, to reduce LDL-C in adults and pediatric patients
aged 7 years and older with homozygous familial hypercholesterolemia
(HoFH).
• As an adjunct to diet for the treatment of adults with:
o Primary dysbetalipoproteinemia.
o Hypertriglyceridemia.
----------------------- DOSAGE AND ADMINISTRATION --------------------
Take orally with or without food, at any time of day. (2.1
)
Assess LDL-C when clinically appropriate, as early as 4 weeks after
initiating CRESTOR, and adjust dosage if necessary. (2.1)
Adults: Recommended dosage range is 5 to 40 mg once daily. (2.1)
Pediatric Patients with HeFH: Recommended dosage range is 5 to 10 mg
once daily for patients aged 8 to less than 10 years of age, and 5 to 20 mg
once daily for patients aged 10 years and older. (2.2)
Pediatric Patients with HoFH: Recommended dosage is 20 mg once daily
for patients aged 7 years and older. (2.2)
Asian Patients: Initiate at 5 mg once daily. Consider risks and benefits of
treatment if not adequately controlled at doses up to 20 mg once daily. (2.4)
Patients with Severe Renal Impairment (not on hemodialysis): Initiate at 5
mg once daily; do not exceed 10 mg once daily. (2.5, 5.1, 8.6)
See full prescribing information for CRESTOR dosage and administration
modifications due to drug interactions. (2.6)
---------------------- DOSAGE FORMS AND STRENGTHS ------------------
Tablets: 5 mg, 10 mg, 20 mg, and 40 mg of rosuvastatin. (3)
------------------------------- CONTRAINDICATIONS ---------------------------
Acute liver failure or decompensated cirrhosis. (4)
Hypersensitivity to rosuvastatin or any excipients in CRESTOR. (4)
------------------------ WARNINGS AND PRECAUTIONS --------------------
• Myopathy and Rhabdomyolysis: Risk factors include age 65 years or
greater, uncontrolled hypothyroidism, renal impairment, concomitant use
with certain other drugs, and higher CRESTOR dosage. Asian patients may
be at higher risk for myopathy. Discontinue CRESTOR if markedly
elevated CK levels occur or myopathy is diagnosed or suspected.
Temporarily discontinue CRESTOR in patients experiencing an acute or
serious condition at high risk of developing renal failure secondary to
rhabdomyolysis. Inform patients of the risk of myopathy and
rhabdomyolysis when starting or increasing CRESTOR dosage. Instruct
patients to promptly report unexplained muscle pain, tenderness, or
weakness, particularly if accompanied by malaise or fever. (5.1, 7.1, 8.5,
8.6, 8.8)
• Immune-Mediated Necrotizing Myopathy (IMNM): Rare reports of IMNM,
an autoimmune myopathy, have been reported with statin use. Discontinue
CRESTOR if IMNM is suspected. (5.2)
• Hepatic Dysfunction: Increases in serum transaminases have occurred,
some persistent. Rare reports of fatal and non-fatal hepatic failure have
occurred. Consider testing liver enzymes before initiating therapy and as
clinically indicated thereafter. If serious hepatic injury with clinical
symptoms and/or hyperbilirubinemia or jaundice occurs, promptly
discontinue CRESTOR. (4, 5.3, 8.7)
------------------------------- ADVERSE REACTIONS ---------------------------
Most frequent adverse reactions (rate ≥2%) are headache, nausea, myalgia,
asthenia, and constipation. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact AstraZeneca
at 1-800-236-9933 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
------------------------------- DRUG INTERACTIONS ---------------------------
See full prescribing information for details regarding concomitant use of
CRESTOR with other drugs that increase the risk of myopathy and
rhabdomyolysis. (2.6, 7.1)
Aluminum and Magnesium Hydroxide Combination Antacids: Administer
CRESTOR at least 2 hours after the antacid. (2.6, 7.2)
Wafarin: Obtain INR prior to starting CRESTOR. Monitor INR frequently
until stable upon initiation, dose titration or discontinuation. (7.3)
----------------------- USE IN SPECIFIC POPULATIONS ---------------------
• Pregnancy: May cause fetal harm. (8.1)
• Lactation: Breastfeeding not recommended during treatment with
CRESTOR. (8.2)
See 17 for PATIENT COUNSELING INFORMATION and FDA-
approved patient labeling.
Revised: 07/2023
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 General Dosage and Administration Information
2.2 Recommended Dosage in Adult Patients
2.3 Recommended Dosage in Pediatric Patients
2.4 Dosing in Asian Patients
2.5 Recommended Dosage in Patients with Renal Impairment
2.6 Dosage and Administration Modifications Due to Drug Interactions
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Myopathy and Rhabdomyolysis
5.2 Immune-Mediated Necrotizing Myopathy
5.3 Hepatic Dysfunction
5.4 Proteinuria and Hematuria
5.5 Increases in HbA1c and Fasting Serum Glucose Levels
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Drug Interactions that Increase the Risk of Myopathy and
Rhabdomyolysis with CRESTOR
7.2 Drug Interactions that Decrease the Efficacy of CRESTOR
7.3 CRESTOR Effects on Other Drugs
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
8.8 Asian Patients
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
12.5 Pharmacogenomics
1
Reference ID: 5216297
This label may not be the latest approved by FDA.
For current labeling information, please visit https://www.fda.gov/drugsatfda

13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14
16
17
CLINICAL STUDIES
HOW SUPPLIED/STORAGE AND HANDLING
PATIENT COUNSELING INFORMATION
*Sections or subsections omitted from the full prescribing information are not listed.
2
Reference ID: 5216297
This label may not be the latest approved by FDA.
For current labeling information, please visit https://www.fda.gov/drugsatfda
FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
CRESTOR is indicated:
• To reduce the risk of stroke, myocardial infarction, and arterial revascularization
procedures in adults without established coronary heart disease who are at increased risk
of cardiovascular (CV) disease based on age, hsCRP ≥2 mg/L, and at least one additional
CV risk factor.
• As an adjunct to diet to:
o Reduce LDL-C in adults with primary hyperlipidemia.
o Reduce low-density lipoprotein cholesterol (LDL-C) and slow the progression of
atherosclerosis in adults.
o Reduce LDL-C in adults and pediatric patients aged 8 years and older with
heterozygous familial hypercholesterolemia (HeFH).
• As an adjunct to other LDL-C-lowering therapies, or alone if such treatments are
unavailable, to reduce LDL-C in adults and pediatric patients aged 7 years and older with
homozygous familial hypercholesterolemia (HoFH).
• As an adjunct to diet for the treatment of adults with:
o Primary dysbetalipoproteinemia.
o Hypertriglyceridemia.
2 DOSAGE AND ADMINISTRATION
2.1 General Dosage and Administration Information
• Administer CRESTOR orally as a single dose at any time of day, with or without food.
The tablet should be swallowed whole.
• Assess LDL-C when clinically appropriate, as early as 4 weeks after initiating
CRESTOR, and adjust the dosage if necessary.
• If a dose is missed, advise patients not take an extra dose. Resume treatment with the next
dose.
2.2 Recommended Dosage in Adult Patients
• The dosage range for CRESTOR is 5 to 40 mg orally once daily.
• The recommended dose of CRESTOR depends on a patient’s indication for usage, LDL-
C, and individual risk for cardiovascular events.
3
Reference ID: 5216297
This label may not be the latest approved by FDA.
For current labeling information, please visit https://www.fda.gov/drugsatfda
2.3 Recommended Dosage in Pediatric Patients
Dosage in Pediatric Patients 8 Years of Age and Older with HeFH
The recommended dosage range is 5 mg to 10 mg orally once daily in patients aged 8 years to
less than 10 years and 5 mg to 20 mg orally once daily in patients aged 10 years and older.
Dosage in Pediatric Patients 7 Years of Age and Older with HoFH
The recommended dosage is 20 mg orally once daily.
2.4 Dosing in Asian Patients
Initiate CRESTOR at 5 mg once daily due to increased rosuvastatin plasma
concentrations. Consider the risks and benefits of CRESTOR when treating Asian
patients not adequately controlled at doses up to 20 mg once daily [see Warnings and
Precautions (5.1), Use in Specific Populations (8.8), and Clinical Pharmacology
(12.3)].
2.5 Recommended Dosage in Patients with Renal Impairment
In patients with severe renal impairment (CL
cr
less than 30 mL/min/1.73 m
2
) not on
hemodialysis, the recommended starting dosage is 5 mg once daily and should not exceed 10 mg
once daily [see Warnings and Precautions (5.1) and Use in Specific Populations (8.6)].
There are no dosage adjustment recommendations for patients with mild and moderate renal
impairment.
2.6 Dosage and Administration Modifications Due to Drug Interactions
CRESTOR Dosage Modifications Due to Drug Interactions
Table 1 displays dosage modifications for CRESTOR due to drug interactions [see Warnings
and Precautions (5.1) and Drug Interactions (7.1)].
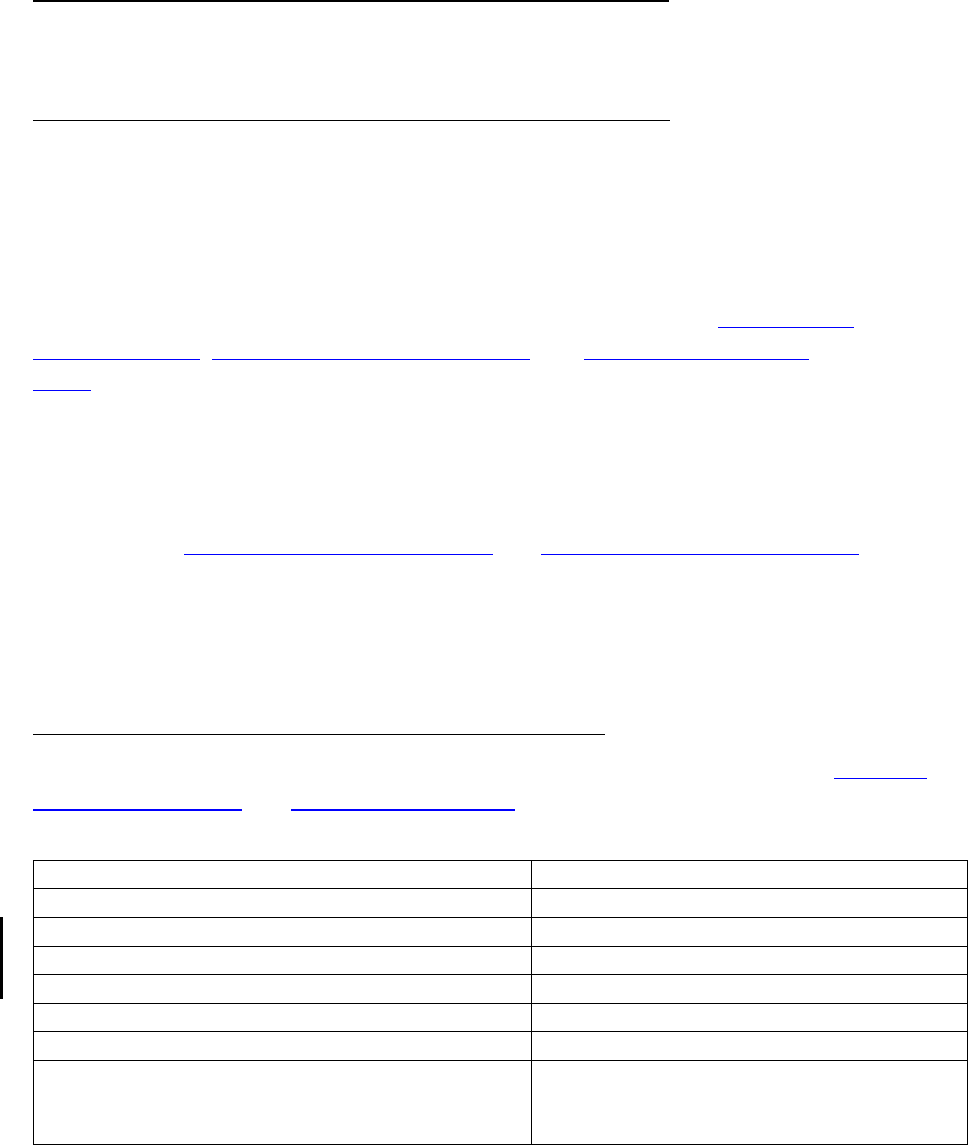
Table 1: CRESTOR Dosage Modifications Due to Drug Interactions
Concomitantly Used Drug
CRESTOR Dosage Modifications
Cyclosporine
Do not exceed 5 mg once daily.
Teriflunomide
Do not exceed 10 mg once daily.
Enasidenib
Do not exceed 10 mg once daily.
Capmatinib
Do not exceed 10 mg once daily.
Fostamatinib
Do not exceed 20 mg once daily.
Febuxostat
Do not exceed 20 mg once daily.
Gemfibrozil
Avoid concomitant use. If used
concomitantly, initiate at 5 mg once daily
and do not exceed 10 mg once daily.
4
Reference ID: 5216297
This label may not be the latest approved by FDA.
For current labeling information, please visit https://www.fda.gov/drugsatfda

Tafamidis
Avoid concomitant use. If used
concomitantly, initiate at 5 mg once daily
and do not exceed 20 mg once daily.
Antiviral Medications
o Sofbuvir/velpatasvir/voxilaprevir
o Ledipasvir/sofosbuvir
Concomitant use not recommended.
o Simeprevir
o Dasabuvir/ombitasvir/paritaprevir/ritonavir
o Elbasvir/Grazoprevir
o Sofosbuvir/Velpatasvir
o Glecaprevir/Pibrentasvir
o Atazanavir/Ritonavir
o
Lopinavir/Ritonavir
Initiate at 5 mg once daily. Do not exceed
10 mg once daily.
Darolutamide
Do not exceed 5 mg once daily.
Regorafenib
Do not exceed 10 mg once daily.
CRESTOR Administration Modifications Due to Drug Interactions
When taking CRESTOR with an aluminum and magnesium hydroxide combination antacid,
administer CRESTOR at least 2 hours before the antacid [see Drug Interactions (7.2)].
3 DOSAGE FORMS AND STRENGTHS
CRESTOR tablets:
• 5 mg of rosuvastatin: yellow, round, biconvex, coated tablets. Debossed “ZD4522” and
“5” on one side of the tablet.
• 10 mg of rosuvastatin: pink, round, biconvex, coated tablets. Debossed “ZD4522” and
“10” on one side of the tablet.
• 20 mg of rosuvastatin: pink, round, biconvex, coated tablets. Debossed “ZD4522” and
“20” on one side of the tablet.
• 40 mg of rosuvastatin: pink, oval, biconvex, coated tablets. Debossed “ZD4522” on one
side and “40” on the other side of the tablet.
4 CONTRAINDICATIONS
CRESTOR is contraindicated in the following conditions:
• Acute liver failure or decompensated cirrhosis [see Warnings and Precautions (5.3)].
• Hypersensitivity to rosuvastatin or any excipients in CRESTOR. Hypersensitivity reactions
including rash, pruritus, urticaria, and angioedema have been reported with CRESTOR [see
Adverse Reactions (6.1)].
5
Reference ID: 5216297
This label may not be the latest approved by FDA.
For current labeling information, please visit https://www.fda.gov/drugsatfda
5 WARNINGS AND PRECAUTIONS
5.1 Myopathy and Rhabdomyolysis
CRESTOR may cause myopathy [muscle pain, tenderness, or weakness associated with elevated
creatine kinase (CK)] and rhabdomyolysis. Acute kidney injury secondary to myoglobinuria and
rare fatalities have occurred as a result of rhabdomyolysis with statins, including CRESTOR.
Risk Factors for Myopathy
Risk factors for myopathy include age 65 years or greater, uncontrolled hypothyroidism, renal
impairment, concomitant use with certain other drugs (including other lipid-lowering therapies),
and higher CRESTOR dosage. Asian patients on CRESTOR may be at higher risk for myopathy
[see Drug Interactions (7.1) and Use in Specific Populations (8.8)]. The myopathy risk is greater
in patients taking CRESTOR 40 mg daily compared with lower CRESTOR dosages.
Steps to Prevent or Reduce the Risk of Myopathy and Rhabdomyolysis
The concomitant use of CRESTOR with cyclosporine or gemfibrozil is not recommended.
CRESTOR dosage modifications are recommended for patients taking certain antiviral
medications, darolutamide, and regorafenib [see Dosage and Administration (2.6)]. Niacin,
fibrates, and colchicine may also increase the risk of myopathy and rhabdomyolysis [see Drug
Interactions (7.1)].
Discontinue CRESTOR if markedly elevated CK levels occur or if myopathy is either diagnosed
or suspected. Muscle symptoms and CK elevations may resolve if CRESTOR is discontinued.
Temporarily discontinue CRESTOR in patients experiencing an acute or serious condition at
high risk of developing renal failure secondary to rhabdomyolysis (e.g., sepsis; shock; severe
hypovolemia; major surgery; trauma; severe metabolic, endocrine, or electrolyte disorders; or
uncontrolled epilepsy).
Inform patients of the risk of myopathy and rhabdomyolysis when starting or increasing the
CRESTOR dosage. Instruct patients to promptly report any unexplained muscle pain, tenderness
or weakness, particularly if accompanied by malaise or fever.
5.2 Immune-Mediated Necrotizing Myopathy
There have been rare reports of immune-mediated necrotizing myopathy (IMNM), an
autoimmune myopathy, associated with statin use, including reports of recurrence when the same
or a different statin was administered. IMNM is characterized by proximal muscle weakness and
elevated serum creatine kinase that persist despite discontinuation of statin treatment; positive
anti-HMG CoA reductase antibody; muscle biopsy showing necrotizing myopathy; and
improvement with immunosuppressive agents. Additional neuromuscular and serologic testing
may be necessary. Treatment with immunosuppressive agents may be required. Discontinue
CRESTOR if IMNM is suspected.
6
Reference ID: 5216297
This label may not be the latest approved by FDA.
For current labeling information, please visit https://www.fda.gov/drugsatfda

5.3 Hepatic Dysfunction
Increases in serum transaminases have been reported with use of CRESTOR [see Adverse
Reactions (6.1)]. In most cases, these changes appeared soon after initiation, were transient, were
not accompanied by symptoms, and resolved or improved on continued therapy or after a brief
interruption in therapy. In a pooled analysis of placebo-controlled trials, increases in serum
transaminases to more than three times the ULN occurred in 1.1% of patients taking CRESTOR
versus 0.5% of patients treated with placebo. Marked persistent increases of hepatic
transaminases have also occurred with CRESTOR. There have been rare postmarketing reports
of fatal and non-fatal hepatic failure in patients taking statins, including CRESTOR.
Patients who consume substantial quantities of alcohol and/or have a history of liver disease may
be at increased risk for hepatic injury [see Use in Specific Populations (8.7)].
Consider liver enzyme testing before CRESTOR initiation and when clinically indicated
thereafter. CRESTOR is contraindicated in patients with acute liver failure or decompensated
cirrhosis [see Contraindications (4)]. If serious hepatic injury with clinical symptoms and/or
hyperbilirubinemia or jaundice occurs, promptly discontinue CRESTOR.
5.4 Proteinuria and Hematuria
In the CRESTOR clinical trial program, dipstick-positive proteinuria and microscopic hematuria
were observed among CRESTOR treated patients. These findings were more frequent in patients
taking CRESTOR 40 mg, when compared to lower doses of CRESTOR or comparator statins,
though it was generally transient and was not associated with worsening renal function. Although
the clinical significance of this finding is unknown, consider a dose reduction for patients on
CRESTOR therapy with unexplained persistent proteinuria and/or hematuria during routine
urinalysis testing.
5.5 Increases in HbA1c and Fasting Serum Glucose Levels
Increases in HbA1c and fasting serum glucose levels have been reported with statins, including
CRESTOR. Based on clinical trial data with CRESTOR, in some instances these increases may
exceed the threshold for the diagnosis of diabetes mellitus [see Adverse Reactions (6.1)].
Optimize lifestyle measures, including regular exercise, maintaining a healthy body weight, and
making healthy food choices.
6 ADVERSE REACTIONS
The following important adverse reactions are described below and elsewhere in the labeling:
Myopathy and Rhabdomyolysis [see Warnings and Precautions (5.1)]
Immune-Mediated Necrotizing Myopathy [see Warnings and Precautions (5.2)]
Hepatic Dysfunction [see Warnings and Precautions (5.3)]
Proteinuria and Hematuria [see Warnings and Precautions (5.4)]
7
Reference ID: 5216297
This label may not be the latest approved by FDA.
For current labeling information, please visit https://www.fda.gov/drugsatfda

Increases in HbA1c and Fasting Serum Glucose Levels [see Warnings and Precautions (5.5)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates
observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials
of another drug and may not reflect the rates observed in clinical practice.
Adverse reactions reported in ≥2% of patients in placebo-controlled clinical studies and at a rate
greater than placebo are shown in Table 2. These studies had a treatment duration of up to
12 weeks.
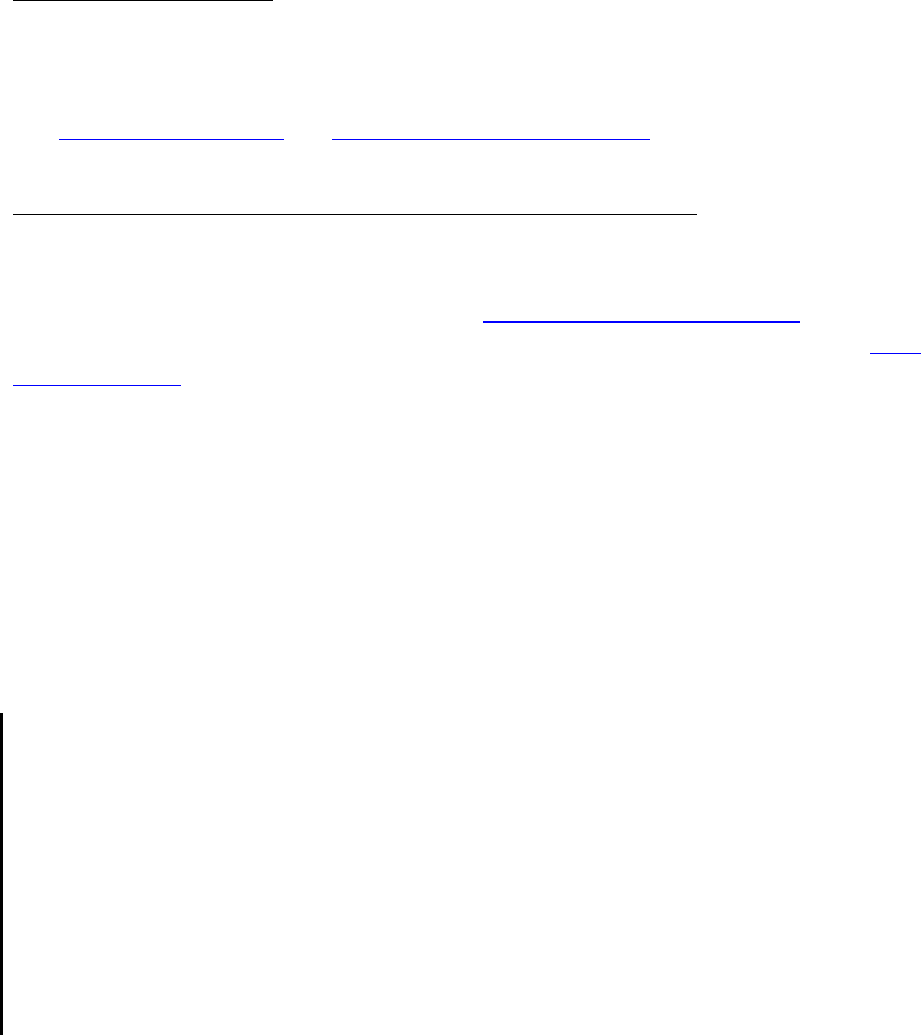
Table 2: Adverse Reactions Reported in ≥2% of Patients Treated with CRESTOR and
> Placebo in Placebo-Controlled Trials
Adverse
Reactions
Placebo
N=382
%
CRESTOR
5 mg
N=291
%
CRESTOR
10 mg
N=283
%
CRESTOR
20 mg
N=64
%
CRESTOR
40 mg
N=106
%
Total
CRESTOR
5 mg-40 mg
N=744
%
Headache
5.0
5.5
4.9
3.1
8.5
5.5
Nausea
3.1
3.8
3.5
6.3
0
3.4
Myalgia
1.3
3.1
2.1
6.3
1.9
2.8
Asthenia
2.6
2.4
3.2
4.7
0.9
2.7
Constipation
2.4
2.1
2.1
4.7
2.8
2.4
Other adverse reactions reported in clinical studies were abdominal pain, dizziness,
hypersensitivity (including rash, pruritus, urticaria, and angioedema) and pancreatitis. The
following laboratory abnormalities have also been reported: dipstick-positive proteinuria and
microscopic hematuria; elevated creatine phosphokinase, transaminases, glucose, glutamyl
transpeptidase, alkaline phosphatase, and bilirubin; and thyroid function abnormalities.
In the METEOR study, patients were treated with CRESTOR 40 mg (n=700) or placebo (n=281)
with a mean treatment duration of 1.7 years. Adverse reactions reported in ≥2% of patients and at
a rate greater than placebo are shown in Table 3.
Table 3: Adverse Reactions Reported in ≥2% of Patients Treated with
CRESTOR and > Placebo in the METEOR Trial
Adverse Reactions
Placebo
N=281
%
CRESTOR 40 mg
N=700
%
Myalgia
12.1
12.7
Arthralgia
7.1
10.1
Headache
5.3
6.4
Dizziness
2.8
4.0
Increased CPK
0.7
2.6
Abdominal pain
1.8
2.4
ALT greater than 3x ULN
1
0.7
2.2
1
Frequency recorded as abnormal laboratory value.
8
Reference ID: 5216297
This label may not be the latest approved by FDA.
For current labeling information, please visit https://www.fda.gov/drugsatfda

In the JUPITER study, patients were treated with CRESTOR 20 mg (n=8901) or placebo
(n=8901) for a mean duration of 2 years. In JUPITER, there was a significantly higher frequency
of diabetes mellitus reported in patients taking CRESTOR (2.8%) versus patients taking placebo
(2.3%). Mean HbA1c was significantly increased by 0.1% in CRESTOR-treated patients
compared to placebo-treated patients. The number of patients with a HbA1c >6.5% at the end of
the trial was significantly higher in CRESTOR-treated versus placebo-treated patients [see
Clinical Studies (14)].
Adverse reactions reported in ≥2% of patients and at a rate greater than placebo are shown in
Table 4.
Table 4: Adverse Reactions Reported in ≥2% of Patients Treated with
CRESTOR and > Placebo in the JUPITER Trial
Adverse Reactions
Placebo
N=8901
%
CRESTOR 20 mg
N=8901
%
Myalgia
6.6
7.6
Arthralgia
3.2
3.8
Constipation
3.0
3.3
Diabetes mellitus
2.3
2.8
Nausea
2.3
2.4
Pediatric Patients with HeFH
In a 12-week controlled study in pediatric patients 10 to 17 years of age with HeFH with
CRESTOR 5 to 20 mg daily [see Use in Specific Populations (8.4) and Clinical Studies (14)],
elevations in serum CK greater than 10 x ULN were observed more frequently in CRESTOR-
treated patients compared with patients receiving placebo. Four of 130 (3%) patients treated with
CRESTOR (2 treated with 10 mg and 2 treated with 20 mg) had increased CK greater than
10 x ULN, compared to 0 of 46 patients on placebo.
6.2 Postmarketing Experience
The following adverse reactions have been identified during postapproval use of CRESTOR.
Because these reactions are reported voluntarily from a population of uncertain size, it is not
always possible to reliably estimate their frequency or establish a causal relationship to drug
exposure.
Blood Disorders: thrombocytopenia
Hepatobiliary Disorders: hepatitis, jaundice, fatal and non-fatal hepatic failure
Musculoskeletal Disorders: arthralgia, rare reports of immune-mediated necrotizing myopathy
associated with statin use
Nervous System Disorders: peripheral neuropathy, rare postmarketing reports of cognitive
impairment (e.g., memory loss, forgetfulness, amnesia, memory impairment, and confusion)
9
Reference ID: 5216297
This label may not be the latest approved by FDA.
For current labeling information, please visit https://www.fda.gov/drugsatfda

associated with the use of all statins. The reports are generally nonserious, and reversible upon
statin discontinuation, with variable times to symptom onset (1 day to years) and symptom
resolution (median of 3 weeks). There have been rare reports of new-onset or exacerbation of
myasthenia gravis, including ocular myasthenia, and reports of recurrence when the same or a
different statin was administered.
Psychiatric Disorders: depression, sleep disorders (including insomnia and nightmares)
Reproductive System and Breast Disorders: gynecomastia
Respiratory Disorders: interstitial lung disease
Skin and Subcutaneous Tissue Disorders: drug reaction with eosinophilia and systemic
symptoms (DRESS), lichenoid drug eruption
7 DRUG INTERACTIONS
7.1 Drug Interactions that Increase the Risk of Myopathy and
Rhabdomyolysis with CRESTOR
Rosuvastatin is a substrate of CYP2C9 and transporters (such as OATP1B1, BCRP).
Rosuvastatin plasma levels can be significantly increased with concomitant administration of
inhibitors of CYP2C9 and transporters. Table 5 includes a list of drugs that increase the risk of
myopathy and rhabdomyolysis when used concomitantly with CRESTOR and instructions for
preventing or managing them [see Warnings and Precautions (5.1) and Clinical Pharmacology
(12.3)].
Table 5: Drug Interactions that Increase the Risk of Myopathy and Rhabdomyolysis with
CRESTOR
Cyclosporine
Clinical Impact:
Cyclosporine increased rosuvastatin exposure 7-fold. The risk of
myopathy and rhabdomyolysis is increased with concomitant use of
cyclosporine or gemfibrozil with CRESTOR.
Intervention:
If used concomitantly, do not exceed a dose of CRESTOR 5 mg
once daily.
Teriflunomide
Clinical Impact:
Teriflunomide increased rosuvastatin exposure more than 2.5-fold.
The risk of myopathy and rhabdomyolysis is increased with
concomitant use.
Intervention:
In patients taking teriflunomide, do not exceed a dose of CRESTOR
10 mg once daily.
Enasidenib
Clinical Impact:
Enasidenib increased rosuvastatin exposure more than 2.4-fold. The
risk of myopathy and rhabdomyolysis is increased with concomitant
use.
Intervention:
In patients taking enasidenib, do not exceed a dose of CRESTOR 10
mg once daily.
Capmatinib
10
Reference ID: 5216297
This label may not be the latest approved by FDA.
For current labeling information, please visit https://www.fda.gov/drugsatfda

Clinical Impact:
Capmatinib increased rosuvastatin exposure more than 2.1-fold. The
risk of myopathy and rhabdomyolysis is increased with concomitant
use.
Intervention:
In patients taking capmatinib, do not exceed a dose of CRESTOR 10
mg once daily.
Fostamatinib
Clinical Impact:
Fostamatinib increased rosuvastatin exposure more than 2.0-fold.
The risk of myopathy and rhabdomyolysis is increased with
concomitant use.
Intervention:
In patients taking fostamatinib, do not exceed a dose of CRESTOR
20 mg once daily.
Febuxostat
Clinical Impact:
Febuxostat increased rosuvastatin exposure more than 1.9-fold. The
risk of myopathy and rhabdomyolysis is increased with concomitant
use.
Intervention:
In patients taking febuxostat, do not exceed a dose of CRESTOR 20
mg once daily.
Gemfibrozil
Clinical Impact:
Gemfibrozil significantly increased rosuvastatin exposure and
gemfibrozil may cause myopathy when given alone. The risk of
myopathy and rhabdomyolysis is increased with concomitant use of
gemfibrozil with CRESTOR.
Intervention:
Avoid concomitant use of gemfibrozil with CRESTOR. If used
concomitantly, initiate CRESTOR at 5 mg once daily and do not
exceed a dose of CRESTOR 10 mg once daily.
Tafamidis
Clinical Impact:
Tafamidis significantly increased rosuvastatin exposure and
tafamidis may cause myopathy when given alone. The risk of
myopathy and rhabdomyolysis is increased with concomitant use
of tafamidis with CRESTOR.
Intervention:
Avoid concomitant use of tafamidis with CRESTOR. If used
concomitantly, initiate CRESTOR at 5 mg once daily and do not
exceed a dose of CRESTOR 20 mg once daily. Monitor for signs of
myopathy and rhabdomyolysis if used concomitantly with
CRESTOR.
Anti-Viral Medications
Clinical Impact:
Rosuvastatin plasma levels were significantly increased with
concomitant administration of many anti-viral drugs, which
increases the risk of myopathy and rhabdomyolysis.
Intervention:
• Sofosbuvir/velpatasvir/voxilaprevir
• Ledipasvir/sofosbuvir
Avoid
concomitant use
with CRESTOR.
• Simeprevir
• Dasabuvir/ombitasvir/paritaprevir/ritonavir
• Elbasvir/grazoprevir
Initiate with
CRESTOR 5 mg
once daily, and
11
Reference ID: 5216297
This label may not be the latest approved by FDA.
For current labeling information, please visit https://www.fda.gov/drugsatfda

• Sofosbuvir/velpatasvir
• Glecaprevir/pibrentasvir
• Atazanavir/ritonavir
• Lopinavir/ritonavir
do not exceed a
dose of
CRESTOR 10
mg once daily.
Darolutamide
Clinical Impact:
Darolutamide increased rosuvastatin exposure more than 5-fold. The
risk of myopathy and rhabdomyolysis is increased with concomitant
use.
Intervention:
In patients taking darolutamide, do not exceed a dose of CRESTOR
5 mg once daily.
Regorafenib
Clinical Impact:
Regorafenib increased rosuvastatin exposure and may increase the
risk of myopathy.
Intervention:
In patients taking regorafenib, do not exceed a dose of CRESTOR
10 mg once daily.
Fenofibrates (e.g., fenofibrate and fenofibric acid)
Clinical Impact:
Fibrates may cause myopathy when given alone. The risk of
myopathy and rhabdomyolysis is increased with concomitant use of
fibrates with CRESTOR.
Intervention:
Consider if the benefit of using fibrates concomitantly with
CRESTOR outweighs the increased risk of myopathy and
rhabdomyolysis. If concomitant use is decided, monitor patients for
signs and symptoms of myopathy, particularly during initiation of
therapy and during upward dose titration of either drug.
Niacin
Clinical Impact:
Cases of myopathy and rhabdomyolysis have occurred with
concomitant use of lipid-modifying doses (≥1 g/day) of niacin with
CRESTOR.
Intervention:
Consider if the benefit of using lipid-modifying doses (≥1 g/day) of
niacin concomitantly with CRESTOR outweighs the increased risk
of myopathy and rhabdomyolysis. If concomitant use is decided,
monitor patients for signs and symptoms of myopathy, particularly
during initiation of therapy and during upward dose titration of
either drug.
Colchicine
Clinical Impact:
Cases of myopathy and rhabdomyolysis have been reported with
concomitant use of colchicine with CRESTOR.
Intervention:
Consider if the benefit of using colchicine concomitantly with
CRESTOR outweighs the increased risk of myopathy and
rhabdomyolysis. If concomitant use is decided, monitor patients for
signs and symptoms of myopathy, particularly during initiation of
therapy and during upward dose titration of either drug.
12
Reference ID: 5216297
This label may not be the latest approved by FDA.
For current labeling information, please visit https://www.fda.gov/drugsatfda

7.2 Drug Interactions that Decrease the Efficacy of CRESTOR
Table 6 presents drug interactions that may decrease the efficacy of CRESTOR and instructions
for preventing or managing them.
Table 6: Drug Interactions that Decrease the Efficacy of CRESTOR
Antacids
Clinical Impact:
Concomitant aluminum and magnesium hydroxide combination antacid
administration decreased the mean exposure of rosuvastatin 50% [see Clinical
Pharmacology (12.3)].
Intervention:
In patients taking antacid, administer CRESTOR at least 2 hours after the
antacid .
7.3 CRESTOR Effects on Other Drugs
Table 7 presents CRESTOR’s effect on other drugs and instructions for preventing or managing
them.
Table 7: CRESTOR Effects on Other Drugs
Warfarin
Clinical Impact:
Rosuvastatin significantly increased the INR in patients receiving warfarin [see
Clinical Pharmacology (12.3)].
Intervention:
In patients taking warfarin, obtain an INR before starting CRESTOR and
frequently enough after initiation, dose titration or discontinuation to ensure that
no significant alteration in INR occurs. Once the INR is stable, monitor INR at
regularly recommended intervals.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Discontinue CRESTOR when pregnancy is recognized. Alternatively, consider the ongoing
therapeutic needs of the individual patient.
CRESTOR decreases synthesis of cholesterol and possibly other biologically active substances
derived from cholesterol; therefore, CRESTOR may cause fetal harm when administered to
pregnant patients based on the mechanism of action [see Clinical Pharmacology (12.1)]. In
addition, treatment of hyperlipidemia is not generally necessary during pregnancy.
Atherosclerosis is a chronic process and the discontinuation of lipid-lowering drugs during
pregnancy should have little impact on the outcome of long-term therapy of primary
hyperlipidemia for most patients.
Available data from case series and prospective and retrospective observational cohort studies
over decades of use with statins in pregnant women have not identified a drug-associated risk of
major congenital malformations. Published data from prospective and retrospective observational
13
Reference ID: 5216297
This label may not be the latest approved by FDA.
For current labeling information, please visit https://www.fda.gov/drugsatfda

cohort studies with CRESTOR use in pregnant women are insufficient to determine if there is a
drug-associated risk of miscarriage (see Data).
In animal reproduction studies, no adverse developmental effects were observed in pregnant rats
or rabbits orally administered rosuvastatin during the period of organogenesis at doses that
resulted in systemic exposures equivalent to human exposures at the maximum recommended
human dose (MRHD) of 40 mg/day, based on AUC and body surface area (mg/m
2
), respectively
(see Data).
The estimated background risk of major birth defects and miscarriage for the indicated
population is unknown. In the U.S. general population, the estimated background risk of major
birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%,
respectively.
Data
Human Data
A Medicaid cohort linkage study of 1152 statin-exposed pregnant women compared to 886,996
controls did not find a significant teratogenic effect from maternal use of statins in the first
trimester of pregnancy, after adjusting for potential confounders – including maternal age,
diabetes mellitus, hypertension, obesity, and alcohol and tobacco use – using propensity score-
based methods. The relative risk of congenital malformations between the group with statin use
and the group with no statin use in the first trimester was 1.07 (95% confidence interval 0.85 to
1.37) after controlling for confounders, particularly pre-existing diabetes mellitus. There were
also no statistically significant increases in any of the organ-specific malformations assessed
after accounting for confounders. In the majority of pregnancies, statin treatment was initiated
prior to pregnancy and was discontinued at some point in the first trimester when pregnancy was
identified. Study limitations include reliance on physician coding to define the presence of a
malformation, lack of control for certain confounders such as body mass index, use of
prescription dispensing as verification for the use of a statin, and lack of information on non-live
births.
Animal Data
In female rats given 5, 15 and 50 mg/kg/day before mating and continuing through to gestation
day 7 resulted in decreased fetal body weight (female pups) and delayed ossification at
50 mg/kg/day (10 times the human exposure at the MRHD dose of 40 mg/day based on AUC).
In pregnant rats given 2, 10 and 50 mg/kg/day of rosuvastatin from gestation day 7 through
lactation day 21 (weaning), decreased pup survival occurred at 50 mg/kg/day (dose equivalent to
12 times the MRHD of 40 mg/day based body surface area).
In pregnant rabbits given 0.3, 1, and 3 mg/kg/day of rosuvastatin from gestation day 6 to day 18,
decreased fetal viability and maternal mortality was observed at 3 mg/kg/day (dose equivalent to
the MRHD of 40 mg/day based on body surface area).
14
Reference ID: 5216297
This label may not be the latest approved by FDA.
For current labeling information, please visit https://www.fda.gov/drugsatfda

Rosuvastatin crosses the placenta in rats and rabbits and is found in fetal tissue and amniotic
fluid at 3% and 20%, respectively, of the maternal plasma concentration following a single
25 mg/kg oral gavage dose on gestation day 16 in rats. In rabbits, fetal tissue distribution was
25% of maternal plasma concentration after a single oral gavage dose of 1 mg/kg on gestation
day 18.
8.2 Lactation
Risk Summary
Limited data from case reports in published literature indicate that CRESTOR is present in
human milk. There is no available information on the effects of the drug on the breastfed infant
or the effects of the drug on milk production. Statins, including CRESTOR, decrease cholesterol
synthesis and possibly the synthesis of other biologically active substances derived from
cholesterol and may cause harm to the breastfed infant.
Because of the potential for serious adverse reactions in a breastfed infant, based on the
mechanism of action, advise patients that breastfeeding is not recommended during treatment
with CRESTOR [see Use in Specific Populations (8.1) and Clinical Pharmacology (12.1)].
8.4 Pediatric Use
The safety and effectiveness of CRESTOR as an adjunct to diet to reduce LDL-C have been
established in pediatric patients 8 years of age and older with HeFH. Use of CRESTOR for this
indication is based on one 12-week controlled trial with a 40-week open-label extension period
in 176 pediatric patients 10 years of age and older with HeFH and one 2-year open-label,
uncontrolled trial in 175 pediatric patients 8 years of age and older with HeFH [see Clinical
Studies (14)]. In the 1-year trial with a 12-week controlled phase, there was no detectable effect
of CRESTOR on growth, weight, BMI (body mass index), or sexual maturation in patients aged
10 to 17 years.
The safety and effectiveness of CRESTOR as an adjunct to other LDL-C-lowering therapies to
reduce LDL-C have been established pediatric patients 7 years of age and older with HoFH. Use
of CRESTOR for this indication is based on a randomized, placebo-controlled, cross-over study
in 14 pediatric patients 7 years of age and older with HoFH [see Clinical Studies (14)].
The safety and effectiveness of CRESTOR have not been established in pediatric patients
younger than 8 years of age with HeFH, younger than 7 years of age with HoFH, or in pediatric
patients with other types of hyperlipidemia (other than HeFH or HoFH).
8.5 Geriatric Use
Of the total number of CRESTOR-treated patients in clinical studies, 3159 (31%) were 65 years
and older, and 698 (6.8%) were 75 years and older. No overall differences in safety or
effectiveness were observed between these subjects and younger subjects.
15
Reference ID: 5216297
This label may not be the latest approved by FDA.
For current labeling information, please visit https://www.fda.gov/drugsatfda
Advanced age (≥65 years) is a risk factor for CRESTOR-associated myopathy and
rhabdomyolysis. Dose selection for an elderly patient should be cautious, recognizing the greater
frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other
drug therapy and the higher risk of myopathy. Monitor geriatric patients receiving CRESTOR for
the increased risk of myopathy [see Warnings and Precautions (5.1)].
8.6 Renal Impairment
Rosuvastatin exposure is not influenced by mild to moderate renal impairment
(CL
cr
≥30 mL/min/1.73 m
2
). Exposure to rosuvastatin is increased to a clinically significant
extent in patients with severe renal impairment (CL
cr
<30 mL/min/1.73 m
2
) who are not
receiving hemodialysis [see Clinical Pharmacology (12.3)].
Renal impairment is a risk factor for myopathy and rhabdomyolysis. Monitor all patients with
renal impairment for development of myopathy. In patients with severe renal impairment not on
hemodialysis, the recommended starting dosage is 5 mg daily and should not exceed 10 mg daily
[see Dosage and Administration (2.5) and Warnings and Precautions (5.1)].
8.7 Hepatic Impairment
CRESTOR is contraindicated in patients with acute liver failure or decompensated cirrhosis.
Chronic alcohol liver disease is known to increase rosuvastatin exposure. Patients who consume
substantial quantities of alcohol and/or have a history of liver disease may be at increased risk for
hepatic injury [see Contraindications (4), Warning and Precautions (5.3) and Clinical
Pharmacology (12.3)].
8.8 Asian Patients
Pharmacokinetic studies have demonstrated an approximate 2-fold increase in median exposure
to rosuvastatin in Asian subjects when compared with White controls. Adjust the CRESTOR
dosage in Asian patients [see Dosage and Administration (2.4) and Clinical Pharmacology
(12.3)].
10 OVERDOSAGE
No specific antidotes for CRESTOR are known. Hemodialysis does not significantly enhance
clearance of rosuvastatin. Contact Poison Control (1-800-222-1222) for latest recommendations.
11 DESCRIPTION
CRESTOR (rosuvastatin) is a 3-hydroxy-3-methylglutaryl coenzyme A (HMG CoA)-reductase
inhibitor.
16
Reference ID: 5216297
This label may not be the latest approved by FDA.
For current labeling information, please visit https://www.fda.gov/drugsatfda

The chemical name for rosuvastatin calcium is bis[(E)-7-[4-(4-fluorophenyl)-6-isopropyl-2-
[methyl(methylsulfonyl)amino] pyrimidin-5-yl](3R,5S)-3,5-dihydroxyhept-6-enoic acid]
calcium salt with the following structural formula:
The empirical formula for rosuvastatin calcium is (C
22
H
27
FN
3
O
6
S)
2
Ca and the molecular weight
is 1001.14. Rosuvastatin calcium is a white amorphous powder that is sparingly soluble in water
and methanol, and slightly soluble in ethanol. Rosuvastatin calcium is a hydrophilic compound
with a partition coefficient (octanol/water) of 0.13 at pH of 7.0.
CRESTOR tablets for oral use contain rosuvastatin 5 mg, 10 mg, 20 mg, or 40 mg (equivalent to
5.2 mg, 10.4 mg, 20.8 mg, and 41.6 mg rosuvastatin calcium) and the following inactive
ingredients: crospovidone NF, hypromellose NF, lactose monohydrate NF, magnesium stearate
NF, microcrystalline cellulose NF, red ferric oxide NF, titanium dioxide USP, triacetin NF,
tribasic calcium phosphate NF and yellow ferric oxide.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
CRESTOR is an inhibitor of HMG-CoA reductase, the rate-limiting enzyme that converts
3-hydroxy-3-methylglutaryl coenzyme A to mevalonate, a precursor of cholesterol.
12.2 Pharmacodynamics
Inhibition of HMG-CoA reductase by rosuvastatin accelerates the expression of LDL-receptors,
followed by the uptake of LDL-C from blood to the liver, leading to a decrease in plasma LDL-C
and total cholesterol. Sustained inhibition of cholesterol synthesis in the liver also decreases
levels of very-low-density lipoproteins. The maximum LDL-C reduction of CRESTOR is usually
achieved by 4 weeks and is maintained after that.
12.3 Pharmacokinetics
Absorption
In clinical pharmacology studies in man, peak plasma concentrations of rosuvastatin were
reached 3 to 5 hours following oral dosing. Both C
max
and AUC increased in approximate
proportion to CRESTOR dose. The absolute bioavailability of rosuvastatin is approximately
17
Reference ID: 5216297
This label may not be the latest approved by FDA.
For current labeling information, please visit https://www.fda.gov/drugsatfda

20%. The AUC of rosuvastatin does not differ following evening or morning drug
administration.
Effect of food
Administration of CRESTOR with food did not affect the AUC of rosuvastatin.
Distribution
Mean volume of distribution at steady-state of rosuvastatin is approximately 134 liters.
Rosuvastatin is 88% bound to plasma proteins, mostly albumin. This binding is reversible and
independent of plasma concentrations.
Elimination
Metabolism
Rosuvastatin is not extensively metabolized; approximately 10% of a radiolabeled dose is
recovered as metabolite. The major metabolite is N-desmethyl rosuvastatin, which is formed
principally by cytochrome P450 \ 2C9, and in vitro studies have demonstrated that N-desmethyl
rosuvastatin has approximately one-sixth to one-half the HMG-CoA reductase inhibitory activity
of the parent compound. Overall, greater than 90% of active plasma HMG-CoA reductase
inhibitory activity is accounted for by the parent compound.
Excretion
Following oral administration, rosuvastatin and its metabolites are primarily excreted in the feces
(90%). After an intravenous dose, approximately 28% of total body clearance was via the renal
route, and 72% by the hepatic route. The elimination half-life of rosuvastatin is approximately 19
hours.
Specific Populations
Geriatric Patients
There were no differences in plasma concentrations of rosuvastatin between the nonelderly and
elderly populations (age ≥65 years).
Pediatric Patients
In a population pharmacokinetic analysis of two pediatric trials involving patients with
heterozygous familial hypercholesterolemia 10 to 17 years of age and 8 to 17 years of age,
respectively, rosuvastatin exposure appeared comparable to or lower than rosuvastatin exposure
in adult patients.
Male and Female Patients
There were no differences in plasma concentrations of rosuvastatin between men and women.
18
Reference ID: 5216297
This label may not be the latest approved by FDA.
For current labeling information, please visit https://www.fda.gov/drugsatfda

Racial or Ethnic Groups
A population pharmacokinetic analysis revealed no clinically relevant differences in
pharmacokinetics among Caucasian, Hispanic, and Black or Afro-Caribbean groups. However,
pharmacokinetic studies, including one conducted in the US, have demonstrated an approximate
2-fold elevation in median exposure (AUC and C
max
) in Asian subjects when compared with a
Caucasian control group.
Patients with Renal Impairment
Mild to moderate renal impairment (CL
cr
≥30 mL/min/1.73 m
2
) had no influence on plasma
concentrations of rosuvastatin. However, plasma concentrations of rosuvastatin increased to a
clinically significant extent (about 3-fold) in patients with severe renal impairment (CL
cr
<30
mL/min/1.73 m
2
) not receiving hemodialysis compared with healthy subjects
(CL
cr
>80 mL/min/1.73 m
2
).
Steady-state plasma concentrations of rosuvastatin in patients on chronic hemodialysis were
approximately 50% greater compared with healthy volunteer subjects with normal renal function.
Patients with Hepatic Impairment
In patients with chronic alcohol liver disease, plasma concentrations of rosuvastatin were
modestly increased.
In patients with Child-Pugh A disease, C
max
and AUC were increased by 60% and 5%,
respectively, as compared with patients with normal liver function. In patients with Child-Pugh
B disease, C
max
and AUC were increased 100% and 21%, respectively, compared with patients
with normal liver function.
Drug Interactions Studies
Rosuvastatin clearance is not dependent on metabolism by cytochrome P450 3A4 to a clinically
significant extent.
Rosuvastatin is a substrate for certain transporter proteins including the hepatic uptake
transporter organic anion-transporting polyprotein 1B1 (OATP1B1) and efflux transporter breast
cancer resistance protein (BCRP). Concomitant administration of CRESTOR with medications
that are inhibitors of these transporter proteins (e.g. cyclosporine, certain HIV protease
inhibitors) may result in increased rosuvastatin plasma concentrations [see Dosage and
Administration (2.6) and Drug Interactions (7.1)].
19
Reference ID: 5216297
This label may not be the latest approved by FDA.
For current labeling information, please visit https://www.fda.gov/drugsatfda

Table 8: Effect of Coadministered Drugs on Rosuvastatin Systemic Exposure
Coadministered drug and dosing
regimen
Rosuvastatin
Mean Ratio
(ratio with/without
coadministered drug)
No Effect=1.0
Dose (mg)
1
Change in
AUC
Change in C
max
Sofosbuvir/velpatasvir/voxilaprevir
(400 mg-100 mg-100 mg) +
Voxilaprevir (100 mg) once daily for 15
days
10 mg, single
dose 7.39
2
(6.68-8.18)
3
18.88
2
(16.23-21.96)
3
Cyclosporine – stable dose required
(75 mg – 200 mg BID)
10 mg, QD for
10 days 7.1
2
11
2
Darolutamide 600 mg BID, 5 days
5 mg, single
dose
5.2
2
~5
2
Regorafenib 160 mg QD, 14 days
5 mg, single
dose
3.8
2
4.6
2
Atazanavir/ritonavir combination
300 mg/100 mg QD for 8 days 10 mg 3.1
2
7
2
Simeprevir 150 mg QD, 7 days
10 mg, single
dose
2.8
2
(2.3-3.4)
3
3.2
2
(2.6-3.9)
3
Velpatasvir 100 mg once daily
10 mg, single
dose
2.69
2
(2.46-2.94)
3
2.61
2
(2.32-2.92)
3
Ombitasvir 25 mg/paritaprevir 150 mg/
ritonavir 100 mg + dasabuvir 400 mg
BID
5 mg, single
dose
2.59
2
(2.09-3.21)
3
7.13
2
(5.11-9.96)
3
Teriflunomide
Not available
2.51
2
2.65
2
Enasidenib 100 mg QD, 28 days
10 mg, single
dose
2.44 3.66
Elbasvir 50 mg/grazoprevir 200 mg
once daily
10 mg, single
dose
2.26
2
(1.89-2.69)
3
5.49
2
(4.29-7.04)
3
Glecaprevir 400 mg/pibrentasvir
120 mg once daily
5 mg, once
daily
2.15
2
(1.88-2.46)
3
5.62
2
(4.80-6.59)
3
Lopinavir/ritonavir combination
400 mg/100 mg BID for 17 days
20 mg, QD for
7 days
2.1
2
(1.7-2.6)
3
5
2
(3.4-6.4)
3
Capmatinib 400 mg BID
10 mg, single
dose
2.08
2
(1.56-2.76)
3
3.04
2
(2.36-3.92)
3
Fostamatinib 100 mg BID
20 mg, single
dose
1.96
2
(1.77-2.15)
3
1.88
2
(1.69-2.09)
3
20
Reference ID: 5216297
This label may not be the latest approved by FDA.
For current labeling information, please visit https://www.fda.gov/drugsatfda

Table 8: Effect of Coadministered Drugs on Rosuvastatin Systemic Exposure
Coadministered drug and dosing
regimen
Rosuvastatin
Mean Ratio
(ratio with/without
coadministered drug)
No Effect=1.0
Dose (mg)
1
Change in
AUC
Change in C
max
Febuxostat 120 mg QD for 4 days
10 mg, single
dose
1.9
2
(1.5-2.5)
3
2.1
2
(1.8-2.6)
3
Gemfibrozil 600 mg BID for 7 days
80 mg
1.9
2
(1.6-2.2)
3
2.2
2
(1.8-2.7)
3
Tafamidis 61 mg BID on Days 1 & 2,
followed by QD on Days 3 to 9
10 mg
1.97
2
(1.68-2.31)
3
1.86
2
(1.59-2.16)
3
Eltrombopag 75 mg QD, 5 days
10 mg
1.6
(1.4-1.7)
3
2
(1.8-2.3)
3
Darunavir 600 mg/ritonavir 100 mg
BID, 7 days
10 mg, QD for
7 days
1.5
(1.0-2.1)
3
2.4
(1.6-3.6)
3
Tipranavir/ritonavir combination
500 mg/200 mg BID for 11 days
10 mg
1.4
(1.2-1.6)
3
2.2
(1.8-2.7)
3
Dronedarone 400 mg BID
10 mg 1.4
Itraconazole 200 mg QD, 5 days
10 mg or 80 mg
1.4
(1.2-1.6)
3
1.3
(1.1-1.4)
3
1.4
(1.2-1.5)
3
1.2
(0.9-1.4)
3
Ezetimibe 10 mg QD, 14 days
10 mg, QD for
14 days
1.2
(0.9-1.6)
3
1.2
(0.8-1.6)
3
Fosamprenavir/ritonavir
700 mg/100 mg BID for 7 days 10 mg 1.1 1.5
Fenofibrate 67 mg TID for 7 days
10 mg ↔
1.2
(1.1-1.3)
3
Rifampicin 450 mg QD, 7 days
20 mg
↔
Aluminum & magnesium hydroxide
combination antacid
Administered simultaneously
Administered 2 hours apart
40 mg
40 mg
0.5
2
(0.4-0.5)
3
0.8
(0.7-0.9)
3
0.5
2
(0.4-0.6)
3
0.8
(0.7-1.0)
3
Ketoconazole 200 mg BID for 7 days
80 mg
1.0
(0.8-1.2)
3
1.0
(0.7-1.3)
3
Fluconazole 200 mg QD for 11 days
80 mg
1.1
(1.0-1.3)
3
1.1
(0.9-1.4)
3
Erythromycin 500 mg QID for 7 days
80 mg
0.8
0.7
21
Reference ID: 5216297
This label may not be the latest approved by FDA.
For current labeling information, please visit https://www.fda.gov/drugsatfda

Table 8: Effect of Coadministered Drugs on Rosuvastatin Systemic Exposure
Coadministered drug and dosing
regimen
Rosuvastatin
Mean Ratio
(ratio with/without
coadministered drug)
No Effect=1.0
Dose (mg)
1
Change in
AUC
Change in C
max
(0.7-0.9)
3
(0.5-0.9)
3
QD= Once daily, BID= Twice daily, TID= Three times daily, QID= Four times daily
1
Single dose unless otherwise noted.
2
Clinically significant [see Dosage and Administration (2) and Warnings and Precautions (5)]
3
Mean ratio with 90% CI (with/without coadministered drug, e.g., 1= no change, 0.7 = 30% decrease,
11=11-fold increase in exposure)
Table 9: Effect of Rosuvastatin Coadministration on Systemic Exposure to Other Drugs
Rosuvastatin
Dosage Regimen
Coadministered Drug
Mean Ratio
(ratio with/without
coadministered drug)
No Effect=1.0
Name and Dose
Change in
AUC
Change in
C
max
40 mg QD for
10 days
Warfarin
1
25 mg single dose
R- Warfarin
1.0
(1.0-1.1)
2
S-Warfarin
1.1
(1.0-1.1)
2
R-Warfarin
1.0
(0.9-1.0)
2
S-Warfarin
1.0
(0.9-1.1)
2
40 mg QD for
12 days
Digoxin
0.5 mg single dose
1.0
(0.9-1.2)
2
1.0
(0.9-1.2)
2
40 mg QD for
28 days
Oral Contraceptive
(ethinyl estradiol 0.035 mg & norgestrel
0.180, 0.215 and 0.250 mg) QD for 21 Days
EE 1.3
(1.2-1.3)
2
NG 1.3
(1.3-1.4)
2
EE 1.3
(1.2-1.3)
2
NG 1.2
(1.1-1.3)
2
EE = ethinyl estradiol, NG = norgestrel, QD= Once daily
1
Clinically significant pharmacodynamic effects [see Drug Interactions (7.3)]
2
Mean ratio with 90% CI (with/without coadministered drug, e.g., 1= no change, 0.7=30% decrease,
11=11-fold increase in exposure)
22
Reference ID: 5216297
This label may not be the latest approved by FDA.
For current labeling information, please visit https://www.fda.gov/drugsatfda

12.5 Pharmacogenomics
Disposition of rosuvastatin, involves OATP1B1 and other transporter proteins. Higher plasma
concentrations of rosuvastatin have been reported in very small groups of patients (n=3 to 5) who
have two reduced function alleles of the gene that encodes OATP1B1 (SLCO1B1 521T > C). The
frequency of this genotype (i.e., SLCO1B1 521 C/C) is generally lower than 5% in most
racial/ethnic groups. The impact of this polymorphism on efficacy and/or safety of CRESTOR
has not been clearly established.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
In a 104-week carcinogenicity study in rats at dose levels of 2, 20, 60, or 80 mg/kg/day by oral
gavage, the incidence of uterine stromal polyps was significantly increased in females at
80 mg/kg/day at systemic exposure 20 times the human exposure at 40 mg/day based on AUC.
Increased incidence of polyps was not seen at lower doses.
In a 107-week carcinogenicity study in mice given 10, 60, or 200 mg/kg/day by oral gavage, an
increased incidence of hepatocellular adenoma/carcinoma was observed at 200 mg/kg/day at
systemic exposures 20 times the human exposure at 40 mg/day based on AUC. An increased
incidence of hepatocellular tumors was not seen at lower doses.
Rosuvastatin was not mutagenic or clastogenic with or without metabolic activation in the Ames
test with Salmonella typhimurium and Escherichia coli, the mouse lymphoma assay, and the
chromosomal aberration assay in Chinese hamster lung cells. Rosuvastatin was negative in the in
vivo mouse micronucleus test.
In rat fertility studies with oral gavage doses of 5, 15, 50 mg/kg/day, males were treated for
9 weeks prior to and throughout mating and females were treated 2 weeks prior to mating and
throughout mating until gestation day 7. No adverse effect on fertility was observed at
50 mg/kg/day (systemic exposures up to 10 times the human exposure at 40 mg/day based on
AUC). In testicles of dogs treated with rosuvastatin at 30 mg/kg/day for one month, spermatidic
giant cells were seen. Spermatidic giant cells were observed in monkeys after 6-month treatment
at 30 mg/kg/day in addition to vacuolation of seminiferous tubular epithelium. Exposures in the
dog were 20 times and in the monkey 10 times the human exposure at 40 mg/day based on body
surface area. Similar findings have been seen with other drugs in this class.
14 CLINICAL STUDIES
Primary Prevention of Cardiovascular Disease
In the Justification for the Use of Statins in Primary Prevention: An Intervention Trial Evaluating
Rosuvastatin (JUPITER) study, the effect of CRESTOR on the occurrence of major
cardiovascular (CV) disease events was assessed in 17,802 men (≥50 years) and women (≥60
23
Reference ID: 5216297
This label may not be the latest approved by FDA.
For current labeling information, please visit https://www.fda.gov/drugsatfda

years) who had no clinically evident cardiovascular disease, LDL-C levels <130 mg/dL and
hsCRP levels ≥2 mg/L. The study population had an estimated baseline coronary heart disease
risk of 11.6% over 10 years based on the Framingham risk criteria and included a high
percentage of patients with additional risk factors such as hypertension (58%), low HDL-C levels
(23%), cigarette smoking (16%), or a family history of premature CHD (12%). Patients had a
median baseline LDL-C of 108 mg/dL and hsCRP of 4.3 mg/L. Patients were randomly assigned
to placebo (n=8901) or CRESTOR 20 mg once daily (n=8901) and were followed for a mean
duration of 2 years. The JUPITER study was stopped early by the Data Safety Monitoring Board
due to meeting predefined stopping rules for efficacy in CRESTOR-treated subjects.
The primary end point was a composite end point consisting of the time-to-first occurrence of
any of the following major CV events: CV death, nonfatal myocardial infarction, nonfatal stroke,
hospitalization for unstable angina or an arterial revascularization procedure.
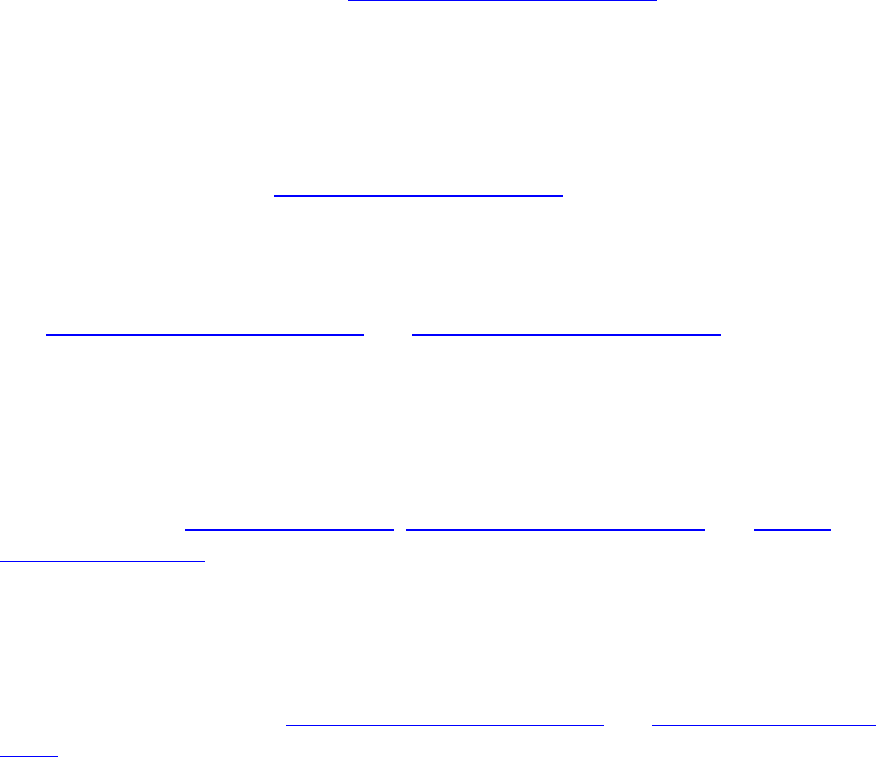
CRESTOR significantly reduced the risk of major CV events (252 events in the placebo group
vs. 142 events in the rosuvastatin group) with a statistically significant (p<0.001) relative risk
reduction of 44% and absolute risk reduction of 1.2% (see Figure 1). The risk reduction for the
primary end point was consistent across the following predefined subgroups: age, sex, race,
smoking status, family history of premature CHD, body mass index, LDL-C, HDL-C, and
hsCRP levels.
Figure 1. Time to First Occurrence of Major Cardiovascular Events in JUPITER
The individual components of the primary end point are presented in Figure 3. CRESTOR
significantly reduced the risk of nonfatal myocardial infarction, nonfatal stroke, and arterial
revascularization procedures. There were no significant treatment differences between the
CRESTOR and placebo groups for death due to cardiovascular causes or hospitalizations for
unstable angina.
24
Reference ID: 5216297
This label may not be the latest approved by FDA.
For current labeling information, please visit https://www.fda.gov/drugsatfda

CRESTOR significantly reduced the risk of myocardial infarction (6 fatal events and 62 nonfatal
events in placebo-treated subjects vs. 9 fatal events and 22 nonfatal events in CRESTOR-treated
subjects) and the risk of stroke (6 fatal events and 58 nonfatal events in placebo-treated subjects
vs. 3 fatal events and 30 nonfatal events in CRESTOR-treated subjects).
In a post-hoc subgroup analysis of JUPITER subjects (rosuvastatin=725, placebo=680) with a
hsCRP ≥2 mg/L and no other traditional risk factors (smoking, BP ≥140/90 or taking
antihypertensives, low HDL-C) other than age, after adjustment for high HDL-C, there was no
significant treatment benefit with CRESTOR treatment.
Figure 2. Major CV Events by Treatment Group in JUPITER
At one year, CRESTOR increased HDL-C and reduced LDL-C, hsCRP, total cholesterol and
serum triglyceride levels (p<0.001 for all versus placebo).
Primary Hyperlipidemia in Adults
CRESTOR reduces Total-C, LDL-C, ApoB, non-HDL-C, and TG, and increases HDL-C, in
adult patients with hyperlipidemia and mixed dyslipidemia.
In a multicenter, double-blind, placebo-controlled study in patients with hyperlipidemia,
CRESTOR given as a single daily dose (5 to 40 mg) for 6 weeks significantly reduced Total-C,
LDL-C, non-HDL-C, and ApoB, across the dose range (Table 10).
Table 10: Lipid-modifying Effect of CRESTOR in Adult Patients with Hyperlipidemia
(Adjusted Mean % Change from Baseline at Week 6)
Dose
N
Total-C
LDL-C
Non-HDL-C
ApoB
TG
HDL-C
Placebo
13
-5
-7
-7
-3
-3
3
CRESTOR 5 mg
17
-33
-45
-44
-38
-35
13
CRESTOR 10 mg
17
-36
-52
-48
-42
-10
14
CRESTOR 20 mg
17
-40
-55
-51
-46
-23
8
CRESTOR 40 mg
18
-46
-63
-60
-54
-28
10
25
Reference ID: 5216297
This label may not be the latest approved by FDA.
For current labeling information, please visit https://www.fda.gov/drugsatfda

CRESTOR was compared with the statins (atorvastatin, simvastatin, and pravastatin) in a
multicenter, open-label, dose-ranging study of 2240 patients with hyperlipidemia or mixed
dyslipidemia. After randomization, patients were treated for 6 weeks with a single daily dose of
either CRESTOR, atorvastatin, simvastatin, or pravastatin (Figure 3 and Table 11).
Figure 3. Percent LDL-C Change by Dose of CRESTOR, Atorvastatin, Simvastatin, and
Pravastatin at Week 6 in Adult Patients with Hyperlipidemia or Mixed Dyslipidemia
Box plots are a representation of the 25th, 50th, and 75th percentile values, with whiskers
representing the 10th and 90th percentile values. Mean baseline LDL-C: 189 mg/dL
Table 11: Percent Change in LDL-C by Dose of CRESTOR, Atorvastatin,
Simvastatin, and Pravastatin From Baseline to Week 6 (LS Mean
1
) in Adult
Patients with Hyperlipidemia or Mixed Dyslipidemia (Sample Sizes Ranging
from 156–167 Patients Per Group)
Treatment Daily Dose
Treatment
10 mg
20 mg
40 mg
80 mg
CRESTOR
-46
2
-52
3
-55
4
---
Atorvastatin
-37
-43
-48
-51
Simvastatin
-28
-35
-39
-46
Pravastatin
-20
-24
-30
---
1
Corresponding standard errors are approximately 1.00.
2
CRESTOR 10 mg reduced LDL-C significantly more than atorvastatin 10 mg; pravastatin 10 mg,
20 mg, and 40 mg; simvastatin 10 mg, 20 mg, and 40 mg. (p<0.002)
3
CRESTOR 20 mg reduced LDL-C significantly more than atorvastatin 20 mg and 40 mg;
pravastatin 20 mg and 40 mg; simvastatin 20 mg, 40 mg, and 80 mg. (p<0.002)
4
CRESTOR 40 mg reduced LDL-C significantly more than atorvastatin 40 mg; pravastatin 40 mg;
simvastatin 40 mg, and 80 mg. (p<0.002)
Slowing of the Progression of Atherosclerosis
In the Measuring Effects on Intima Media Thickness: an Evaluation Of Rosuvastatin 40 mg
(METEOR) study, the effect of therapy with CRESTOR on carotid atherosclerosis was assessed
by B-mode ultrasonography in patients with elevated LDL-C, at low risk (Framingham risk
26
Reference ID: 5216297
This label may not be the latest approved by FDA.
For current labeling information, please visit https://www.fda.gov/drugsatfda

<10% over ten years) for symptomatic coronary artery disease and with subclinical
atherosclerosis as evidenced by carotid intimal-medial thickness (cIMT). In this double-blind,
placebo-controlled clinical study 984 adult patients were randomized (of whom 876 were
analyzed) in a 5:2 ratio to CRESTOR 40 mg or placebo once daily. Ultrasonograms of the
carotid walls were used to determine the annualized rate of change per patient from baseline to
two years in mean maximum cIMT of 12 measured segments. The estimated difference in the
rate of change in the maximum cIMT analyzed over all 12 carotid artery sites between patients
treated with CRESTOR and placebo-treated patients was -0.0145 mm/year (95% CI –0.0196, –
0.0093; p<0.0001).
The annualized rate of change from baseline for the placebo group was +0.0131 mm/year
(p<0.0001). The annualized rate of change from baseline for the group treated with CRESTOR
was -0.0014 mm/year (p=0.32).
At an individual patient level in the group treated with CRESTOR, 52.1% of patients
demonstrated an absence of disease progression (defined as a negative annualized rate of
change), compared to 37.7% of patients in the placebo group.
HeFH in Adults
In a study of adult patients with HeFH (baseline mean LDL of 291 mg/dL), patients were
randomized to CRESTOR 20 mg or atorvastatin 20 mg. The dose was increased at 6-week
intervals. Significant LDL-C reductions from baseline were seen at each dose in both treatment
groups (Table 12).
Table 12: LDL-C Percent Change from Baseline
CRESTOR (n=435)
LS Mean
1
(95% CI)
Atorvastatin (n=187)
LS Mean
1
(95% CI)
Week 6
20 mg
-47% (-49%, -46%)
-38% (-40%, -36%)
Week 12
40 mg
-55% (-57%, -54%)
-47% (-49%, -45%)
Week 18
80 mg
NA
-52% (-54%, -50%)
1
LS Means are least square means adjusted for baseline LDL-C
HeFH in Pediatric Patients
In a double-blind, randomized, multicenter, placebo-controlled, 12-week study, 176 (97 male and
79 female) children and adolescents with heterozygous familial hypercholesterolemia were
randomized to rosuvastatin 5 mg, 10 mg or 20 mg or placebo daily. Patients ranged in age from
10 to 17 years (median age of 14 years) with approximately 30% of the patients 10 to 13 years
and approximately 17%, 18%, 40%, and 25% at Tanner stages II, III, IV, and V, respectively.
Females were at least 1 year postmenarche. Mean LDL-C at baseline was 233 mg/dL (range of
129 to 399). The 12-week double-blind phase was followed by a 40 week open label dose-
titration phase, where all patients (n=173) received 5 mg, 10 mg or 20 mg rosuvastatin daily.
Rosuvastatin significantly reduced LDL-C (primary end point), total cholesterol and ApoB levels
at each dose compared to placebo. Results are shown in Table 13 below.
27
Reference ID: 5216297
This label may not be the latest approved by FDA.
For current labeling information, please visit https://www.fda.gov/drugsatfda

Table 13: Lipid-Modifying Effects of CRESTOR in Pediatric Patients 10 to
17 years of Age with Heterozygous Familial Hypercholesterolemia (Least-Squares
Mean Percent Change from Baseline To Week 12)
Dose (mg) N LDL-C HDL-C Total-C TG
1
ApoB
Placebo 46 -1% +7% 0% -7% -2%
5 42 -38% +4%
2
-30% -13%
2
-32%
10 44 -45% +11%
2
-34% -15%
2
-38%
20 44 -50% +9%
2
-39% 16%
2
-41%
1
Median percent change
2
Difference from placebo not statistically significant
Rosuvastatin was also studied in a two-year open-label, uncontrolled, titration-to-goal trial that
included 175 children and adolescents with heterozygous familial hypercholesterolemia who
were 8 to 17 years old (79 boys and 96 girls). All patients had a documented genetic defect in the
LDL receptor or in ApoB. Approximately 89% were White, 7% were Asian, 1% were Black, and
fewer than 1% were Hispanic. Mean LDL-C at baseline was 236 mg/dL. Fifty-eight (33%)
patients were prepubertal at baseline. The starting rosuvastatin dosage for all children and
adolescents was 5 mg once daily. Children 8 to less than 10 years of age (n=41 at baseline) could
titrate to a maximum dosage of 10 mg once daily, and children and adolescents 10 to 17 years of
age could titrate to a maximum dosage of 20 mg once daily.
The reductions in LDL-C from baseline were generally consistent across age groups within the
trial as well as with previous experience in both adult and pediatric controlled trials.
HoFH in Adult and Pediatric Patients
In an open-label, forced-titration study, HoFH patients (n=40, 8-63 years) were evaluated for
their response to CRESTOR 20 to 40 mg titrated at a 6-week interval. In the overall population,
the mean LDL-C reduction from baseline was 22%. About one-third of the patients benefited
from increasing their dose from 20 mg to 40 mg with further LDL-C lowering of greater than
6%. In the 27 patients with at least a 15% reduction in LDL-C, the mean LDL-C reduction was
30% (median 28% reduction). Among 13 patients with an LDL-C reduction of <15%, 3 had no
change or an increase in LDL-C. Reductions in LDL-C of 15% or greater were observed in
3 of 5 patients with known receptor negative status.
HoFH in Pediatric Patients
CRESTOR was studied in a randomized, double-blind, placebo-controlled, multicenter, cross-
over study in 14 pediatric patients with HoFH. The study included a 4-week dietary lead-in phase
28
Reference ID: 5216297
This label may not be the latest approved by FDA.
For current labeling information, please visit https://www.fda.gov/drugsatfda

during which patients received CRESTOR 10 mg daily, a cross-over phase that included two
6-week treatment periods with either CRESTOR 20 mg or placebo in random order, followed by
a 12-week open-label phase during which all patients received CRESTOR 20 mg. Patients
ranged in age from 7 to 15 years of age (median 11 years), 50% were male, 71% were White,
21% were Asian, 7% were Black, and no patients were of Hispanic ethnicity. Fifty percent were
on apheresis therapy and 57% were taking ezetimibe. Patients who entered the study on
apheresis therapy or ezetimibe continued the treatment throughout the entire study. Mean LDL-C
at baseline was 416 mg/dL (range 152 to 716 mg/dL). A total of 13 patients completed both
treatment periods of the randomized cross-over phase; one patient withdrew consent due to
inability to have blood drawn during the cross-over phase.
CRESTOR 20 mg significantly reduced LDL-C, total cholesterol, ApoB, and non-HDL-C
compared to placebo (Table 14).
Table 14: Lipid-modifying Effects of CRESTOR in Pediatric Patients 7 to 15 years of
Age with Homozygous Familial Hypercholesterolemia After 6 Weeks
Placebo
(N=13)
CRESTOR 20 mg
(N=13)
Percent difference (95% CI)
LDL-C (mg/dL)
481
396
-22.3% (-33.5, -9.1)
1
Total-C (mg/dL)
539
448
-20.1% (-29.7, -9.1)
2
Non-HDL-C (mg/dL)
505
412
-22.9% (-33.7, -10.3)
2
ApoB (mg/dL)
268
235
-17.1% (-29.2, -2.9)
3
% Difference estimates are based on transformations of the estimated mean difference in log LDL
measurements between CRESTOR and placebo using a mixed model adjusted for study period
1
p=0.005,
2
p=0.003,
3
p=0.024
Primary Dysbetalipoproteinemia in Adults
In a randomized, multicenter, double-blind crossover study, 32 adult patients (27 with є2/є2
and 4 with apo E mutation [Arg145Cys] with primary dysbetalipoproteinemia entered a
6-week dietary lead-in period on the NCEP Therapeutic Lifestyle Change (TLC) diet.
Following dietary lead-in, patients were randomized to a sequence of treatments for 6 weeks
each: rosuvastatin 10 mg followed by rosuvastatin 20 mg or rosuvastatin 20 mg followed by
rosuvastatin 10 mg. CRESTOR reduced non-HDL-C (primary end point) and circulating
remnant lipoprotein levels. Results are shown in the table below.
29
Reference ID: 5216297
This label may not be the latest approved by FDA.
For current labeling information, please visit https://www.fda.gov/drugsatfda

Table 15: Lipid-modifying Effects of CRESTOR 10 mg and 20 mg in Adult Patients
with Primary Dysbetalipoproteinemia (Type III hyperlipoproteinemia) After Six
Weeks by Median Percent Change (95% CI) from Baseline (N=32)
Median at
Baseline
(mg/dL)
Median percent change
from baseline (95% CI)
CRESTOR 10 mg
Median percent change
from baseline (95% CI)
CRESTOR 20 mg
Total-C
342.5
-43.3
(-46.9, - 37.5)
-47.6
(-51.6,-42.8)
Triglycerides
503.5
-40.1
(-44.9, -33.6)
-43.0
(-52.5, -33.1)
Non-HDL-C
294.5
-48.2
(-56.7, -45.6)
-56.4
(-61.4, -48.5)
VLDL-C + IDL-C
209.5
-46.8
(-53.7, -39.4)
-56.2
(-67.7, -43.7)
LDL-C
112.5
-54.4
(-59.1, -47.3)
-57.3
(-59.4, -52.1)
HDL-C
35.5
10.2
(1.9, 12.3)
11.2
(8.3, 20.5)
RLP-C
82.0
-56.4
(-67.1, -49.0)
-64.9
(-74.0, -56.6)
Apo-E
16.0
-42.9
(-46.3, -33.3)
-42.5
(-47.1, -35.6)
Hypertriglyceridemia in Adults
In a double-blind, placebo-controlled study in adult patients with baseline TG levels from
273 to 817 mg/dL, CRESTOR given as a single daily dose (5 to 40 mg) over 6 weeks
significantly reduced serum TG levels (Table 16).
Table 16: Lipid-Modifying Effect of CRESTOR in Adult Patients with Primary
Hypertriglyceridemia After Six Weeks by Median (Min, Max) Percent Change
from Baseline to Week 6
Dose
Placebo
(n=26)
CRESTOR
5 mg
(n=25)
CRESTOR
10 mg
(n=23)
CRESTOR
20 mg
(n=27)
CRESTOR
40 mg
(n=25)
Triglycerides
1 (-40, 72)
-21 (-58,
38)
-37 (-65, 5)
-37 (-72, 11)
-43 (-80, -7)
Non-HDL-C
2 (-13, 19)
-29 (-43, -8)
-49 (-59, -20)
-43 (-74, 12)
-51 (-62, -6)
Total-C
1 (-13, 17)
-24 (-40, -4)
-40 (-51, -14)
-34 (-61, -11)
-40 (-51, -4)
LDL-C
5 (-30, 52)
-28 (-71, 2)
-45 (-59, 7)
-31 (-66, 34)
-43 (-61, -3)
HDL-C
-3 (-25,
18)
3 (-38, 33)
8 (-8, 24)
22 (-5, 50)
17 (-14, 63)
30
Reference ID: 5216297
This label may not be the latest approved by FDA.
For current labeling information, please visit https://www.fda.gov/drugsatfda
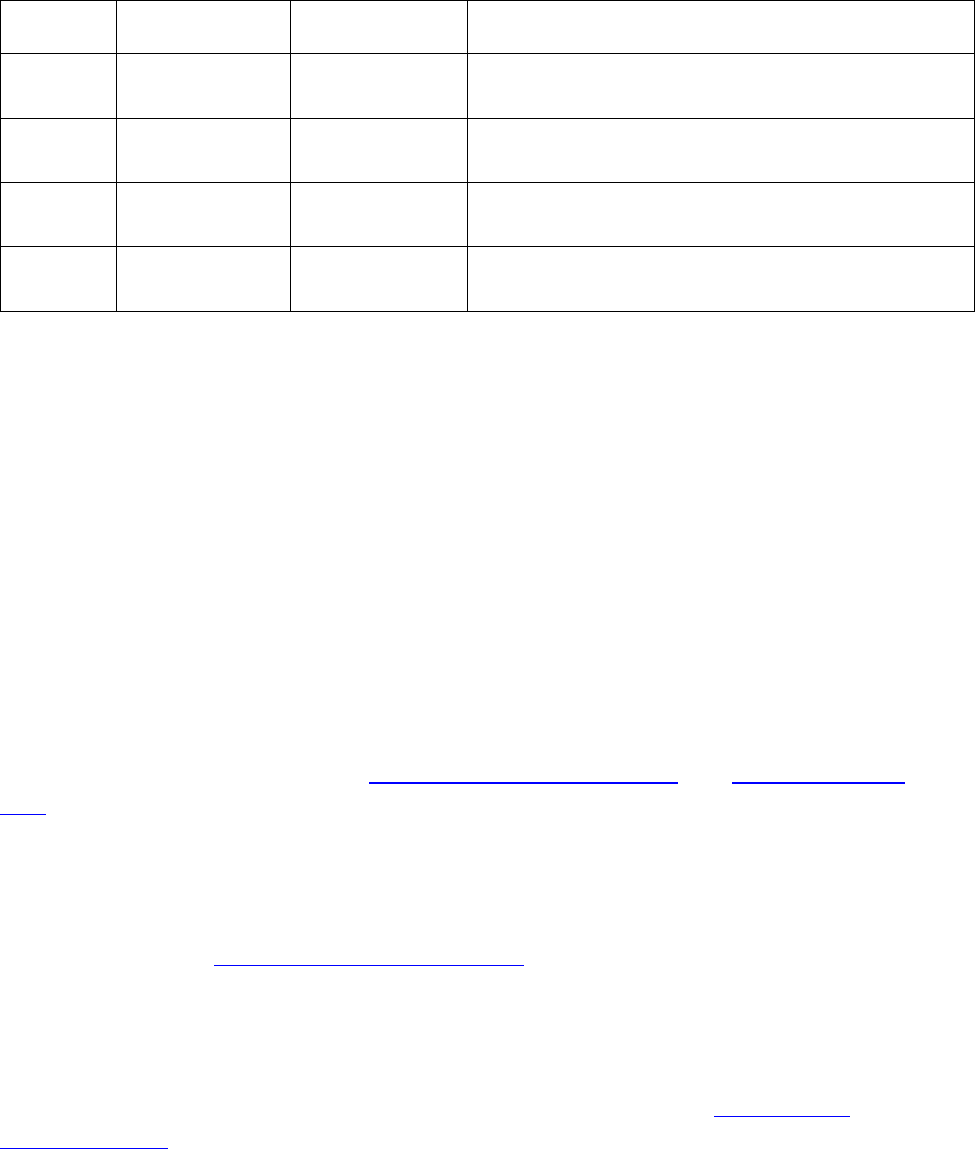
16 HOW SUPPLIED/STORAGE AND HANDLING
CRESTOR tablets are supplied as:
Strength
How Supplied
NDC
Tablet Description
5 mg
bottles of 90
tablets
0310-7560-90
Yellow, round, biconvex, coated tablets.
Debossed “ZD4522” and “5” on one side
10 mg
bottles of 90
tablets
0310-7570-90
Pink, round, biconvex, coated tablets. Debossed
“ZD4522” and “10” on one side
20 mg
bottles of 90
tablets
0310-7580-90
Pink, round, biconvex, coated tablets. Debossed
“ZD4522” and “20” on one side
40 mg
bottles of 30
tablets
0310-7590-30
Pink, oval, biconvex, coated tablets. Debossed
“ZD4522” on one side and “40” on the other side
Storage
Store at controlled room temperature, 20ºC to 25ºC (68ºF to 77ºF); excursions permitted between
15°C and 30°C (59°F and 86°F) [see USP Controlled Room Temperature]. Protect from
moisture.
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information).
Myopathy and Rhabdomyolysis
Advise patients that CRESTOR may cause myopathy and rhabdomyolysis. Inform patients that
the risk is also increased when taking certain types of medication and they should discuss all
medication, both prescription and over the counter, with their healthcare provider. Instruct
patients to promptly report any unexplained muscle pain, tenderness or weakness particularly if
accompanied by malaise or fever [see Warnings and Precautions (5.1), and Drug Interactions
(7.1)].
Hepatic Dysfunction
Inform patients that CRESTOR may cause liver enzyme elevations and possibly liver failure.
Advise patients to promptly report fatigue, anorexia, right upper abdominal discomfort, dark
urine or jaundice [see Warnings and Precautions (5.3)].
Increases in HbA1c and Fasting Serum Glucose Levels
Inform patients that increases in HbA1c and fasting serum glucose levels may occur with
CRESTOR. Encourage patients to optimize lifestyle measures, including regular exercise,
maintaining a healthy body weight, and making healthy food choices [see Warnings and
Precautions (5.5)].
31
Reference ID: 5216297
This label may not be the latest approved by FDA.
For current labeling information, please visit https://www.fda.gov/drugsatfda

Pregnancy
Advise pregnant patients and patients who can become pregnant of the potential risk to a fetus.
Advise patients to inform their healthcare provider of a known or suspected pregnancy to discuss
if CRESTOR should be discontinued [see Use in Specific Populations (8.1)].
Lactation
Advise patients that breastfeeding during treatment with CRESTOR is not recommended [see
Use in Specific Populations (8.2)].
Concomitant Use of Antacids
When taking CRESTOR with an aluminum and magnesium hydroxide combination antacid, the
antacid should be taken at least 2 hours after CRESTOR administration [see Drug Interactions
(7.2)].
Missed Doses
If a dose is missed, advise patients not take an extra dose. Just resume the usual schedule [see
General Dosage and Administration Information (2.1)].
CRESTOR is a trademark of the AstraZeneca group of companies.
© AstraZeneca 2023
Licensed from SHIONOGI & CO., LTD., Osaka, Japan
Distributed by:
AstraZeneca Pharmaceuticals LP
Wilmington, DE 19850
32
Reference ID: 5216297
This label may not be the latest approved by FDA.
For current labeling information, please visit https://www.fda.gov/drugsatfda

PATIENT INFORMATION
CRESTOR
®
(Kres-tor)
rosuvastatin
Tablets
Read this Patient Information carefully before you start taking CRESTOR and each time you get a
refill. If you have any questions about CRESTOR, ask your doctor. Only your doctor can determine
if CRESTOR is right for you.
What is CRESTOR?
CRESTOR is a prescription medicine that contains a cholesterol-lowering medicine called
rosuvastatin.
• CRESTOR is used to:
o reduce the risk of stroke, heart attack, and the need for procedures to improve blood flow to
the heart called arterial revascularization in adults who do not have known heart disease
but do have certain additional risk factors.
• CRESTOR is used along with diet to:
o lower the level of low-density lipoprotein (LDL) cholesterol or “bad” cholesterol in adults with
primary hyperlipidemia.
o slow the buildup of fatty deposits (plaque) in the walls of blood vessels.
o treat adults and children 8 years of age and older with high blood cholesterol due to
heterozygous familial hypercholesterolemia (an inherited condition that causes high levels of
LDL).
o along with other cholesterol lowering treatments or alone if such treatments are unavailable in
adults and children 7 years of age and older with homozygous familial hypercholesterolemia (an
inherited condition that causes high levels of LDL).
o treat adults with a type of high cholesterol called primary dysbetalipoproteinemia (type III
hyperlipoproteinemia).
o lower the level of fat in your blood (triglycerides) in adults with hypertriglyceridemia.
The safety and effectiveness of CRESTOR has not been established in children younger than 8
years of age with heterozygous familial hypercholesterolemia or children younger than 7 years of
age with homozygous familial hypercholesterolemia or in children with other types of
hyperlipidemias (other than HeFH or HoFH).
Who should not take CRESTOR?
Do not take CRESTOR if you:
• have liver problems.
• are allergic to rosuvastatin or any of the ingredients in CRESTOR. See the end of this leaflet for
a complete list of ingredients in CRESTOR. Symptoms of allergic reactions include rash, itching,
hives, and swelling.
What should I tell my doctor before and while taking CRESTOR?
Tell your doctor if you:
• have unexplained muscle aches or weakness.
• have or have had kidney problems.
• have or have had liver problems.
• drink more than 2 glasses of alcohol daily.
• have thyroid problems.
• are 65 years of age or older.
• are of Asian descent.
• are pregnant or think you may be pregnant, or are planning to become pregnant. If you become
pregnant while taking CRESTOR, call your healthcare provider right away to discuss your
CRESTOR treatment.
33
Reference ID: 5216297
This label may not be the latest approved by FDA.
For current labeling information, please visit https://www.fda.gov/drugsatfda

• are breastfeeding. CRESTOR can pass into your breast milk. Breastfeeding is not recommended
while taking CRESTOR.
Tell your doctor about all the medicines you take, including prescription and over-the-counter
medicines, vitamins, and herbal supplements.
Taking CRESTOR with certain other medicines may affect each other causing side effects.
CRESTOR may affect the way other medicines work, and other medicines may affect how
CRESTOR works.
Especially tell your doctor if you take:
• cyclosporine (a medicine for your immune system)
• gemfibrozil (a fibric acid medicine for lowering cholesterol)
• fostamatinib (a medicine used to treat low platelet counts)
• febuxostat (a medicine used to treat and prevent high blood levels of uric acid)
• teriflunomide (a medicine used to treat relapsing remitting multiple sclerosis)
• capmatinib (a medicine for the treatment of non-small cell lung cancer)
• tafamidis (used to treat cardiomyopathy [enlarged and thickened heart muscle])
• darolutamide (a medicine for the treatment of prostate cancer)
• regorafenib (a medicine used to treat cancer of the colon and rectum)
• enasidenib (a medicine used to treat acute myeloid leukemia)
• anti-viral medicines including certain HIV or hepatitis C virus drugs such as:
o lopinavir, ritonavir, fosamprenavir, tipranavir, atazanavir, simeprevir
o combination of
sofosbuvir/velpatasvir/voxilaprevir
dasabuvir/ombitasvir/paritaprevir/ritonavir
elbasvir/grazoprevir
sofosbuvir/velpatasvir
glecaprevir/pibrentasvir and
o all other combinations with ledipasvir including ledipasvir/sofosbuvir
• certain anti-fungal medicines (such as itraconazole, ketoconazole and fluconazole)
• coumarin anticoagulants (medicines that prevent blood clots, such as warfarin)
• niacin or nicotinic acid
• fibric acid derivatives (such as fenofibrate)
• colchicine (a medicine used to treat gout)
Ask your doctor or pharmacist for a list of these medicines if you are not sure. Know the medicines
you take. Keep a list of them to show your doctor and pharmacist when you get new medicine.
How should I take CRESTOR?
• Take CRESTOR exactly as your doctor tells you to take it.
• Take CRESTOR, by mouth, 1 time each day. Swallow the tablet whole.
• CRESTOR can be taken at any time of day, with or without food.
• Do not change your dose or stop CRESTOR without talking to your doctor, even if you are
feeling well.
• Your doctor may do blood tests to check your cholesterol levels before and during your treatment
with CRESTOR. Your doctor may change your dose of CRESTOR if needed.
• Your doctor may start you on a cholesterol lowering diet before giving you CRESTOR. Stay on
this diet when you take CRESTOR.
•
Wait at least 2 hours after taking CRESTOR to take an antacid that contains a combination of
aluminum and magnesium hydroxide.
34
Reference ID: 5216297
This label may not be the latest approved by FDA.
For current labeling information, please visit https://www.fda.gov/drugsatfda
• If you miss a dose of CRESTOR, take your next dose at your normal scheduled time. Do not
take an extra dose of CRESTOR.
• If you take too much CRESTOR or overdose, call your doctor or go to the nearest hospital
emergency room right away.
What are the possible side effects of CRESTOR?
CRESTOR may cause serious side effects, including:
• Muscle pain, tenderness and weakness (myopathy). Muscle problems, including muscle
breakdown, can be serious in some people and rarely cause kidney damage that can lead to
death. Tell your doctor right away if:
o you have unexplained muscle pain, tenderness, or weakness, especially if
you have a fever or feel more tired than usual, while you take CRESTOR.
o you have muscle problems that do not go away even after your doctor has
told you to stop taking CRESTOR. Your doctor may do further tests to
diagnose the cause of your muscle problems.
Your chances of getting muscle problems are higher if you:
o are taking certain other medicines while you take CRESTOR
o are 65 years of age or older
o have thyroid problems (hypothyroidism) that are not controlled
o have kidney problems
o are taking higher doses of CRESTOR
• Liver problems. Your doctor may do blood tests to check your liver before you start taking
CRESTOR and if you have symptoms of liver problems while you take CRESTOR. Call your
doctor right away if you have any of the following symptoms of liver problems:
o feel unusually tired or weak
o loss of appetite
o upper belly pain
o dark urine
o yellowing of your skin or the whites of your eyes
• Protein and blood in the urine. CRESTOR may cause you to have protein and blood in your
urine. If you develop protein or blood in your urine, your doctor may decrease your dose of
CRESTOR.
• Increase in blood sugar (glucose) levels
. CRESTOR may cause an increase in your blood
sugar levels.
The most common side effects may include headache, muscle aches and pains, abdominal pain,
weakness, and nausea.
Tell your doctor if you have any side effect that bothers you or that does not go away.
For more information, ask your doctor or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-
FDA-1088.
How should I store CRESTOR?
• Store CRESTOR at room temperature, between 68°F to 77°F (20°C to 25°C) and in a dry place.
• Safely throw away medicine that is out of date or no longer needed.
Keep CRESTOR and all medicines out of the reach of children.
General Information about the safe and effective use of CRESTOR
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information
leaflet. Do not use CRESTOR for a condition for which it was not prescribed. Do not give
CRESTOR to other people, even if they have the same medical condition you have. It may harm
them.
You can ask your pharmacist or doctor for information about CRESTOR that is written for health
professionals.
35
Reference ID: 5216297
This label may not be the latest approved by FDA.
For current labeling information, please visit https://www.fda.gov/drugsatfda

What are the Ingredients in CRESTOR?
Active Ingredient: rosuvastatin as rosuvastatin calcium
Inactive Ingredients: crospovidone NF, hypromellose NF, lactose monohydrate NF, magnesium
stearate NF, microcrystalline cellulose NF, red ferric oxide NF, titanium dioxide USP, triacetin NF,
tribasic calcium phosphate NF and yellow ferric oxide.
CRESTOR is a trademark of the AstraZeneca group of companies.
© AstraZeneca XXXX
Licensed from SHIONOGI & CO., LTD., Osaka, Japan
Distributed by:
AstraZeneca Pharmaceuticals LP
Wilmington, DE 19850
For more information, go to the CRESTOR website at www.crestor.com or call 1-800-CRESTOR
This Patient Information has been approved by the U.S. Food and Drug Administration Revised 07/2023
36
Reference ID: 5216297
This label may not be the latest approved by FDA.
For current labeling information, please visit https://www.fda.gov/drugsatfda
