
Official address Domenico Scarlattilaan 6 ● 1083 HS Amsterdam ● The Netherlands
An agency of the European Union
Address for visits and deliveries Refer to www.ema.europa.eu/how-to-find-us
Send us a question Go to www.ema.europa.eu/contact
Telephone +31 (0)88 781 6000
© European Medicines Agency, 2023. Reproduction is authorised provided the source is acknowledged.
9 March 2023
EMA/INS/GCP/112288/2023
Good Clinical Practice Inspectors Working Group (GCP IWG)
Guideline on computerised systems and electronic data in
clinical trials
Adopted by GCP IWG for release for consultation 4 March 2021
Start of public consultation 18 June 2021
End of consultation (deadline for comments) 17 December 2021
Final version adopted by the GCP IWG 7 March 2023
Date of coming into effect 6 months after publication
This guideline replaces the 'Reflection paper on expectations for electronic source data and data
transcribed to electronic data collection tools in clinical trials' (EMA/INS/GCP/454280/2010).
Keywords
Computerised systems, electronic data, validation, audit trail, user
management, security, electronic clinical outcome assessment
(eCOA), interactive response technology (IRT), case report form
(CRF), electronic signatures, artificial intelligence (AI)

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 2/52
Guideline on computerised systems and electronic data in
clinical trials
Table of contents
Glossary ...................................................................................................... 5
Abbreviations .............................................................................................. 7
Executive summary ..................................................................................... 8
1. Introduction ............................................................................................ 8
2. Scope....................................................................................................... 9
3. Legal and regulatory background .......................................................... 10
4. Principles and definition of key concepts ............................................... 10
4.1. Data integrity .................................................................................................... 10
4.2. Responsibilities .................................................................................................. 11
4.3. Data and metadata ............................................................................................. 11
4.4. Source data ....................................................................................................... 11
4.5. ALCOA++ principles ........................................................................................... 12
4.6. Criticality and risks ............................................................................................. 13
4.7. Data capture ...................................................................................................... 14
4.8. Electronic signatures ........................................................................................... 15
4.9. Data protection .................................................................................................. 16
4.10. Validation of systems ........................................................................................ 16
4.11. Direct access.................................................................................................... 16
5. Computerised systems .......................................................................... 17
5.1. Description of systems ........................................................................................ 17
5.2. Documented procedures ...................................................................................... 17
5.3. Training ............................................................................................................ 17
5.4. Security and access control ................................................................................. 17
5.5. Timestamp ........................................................................................................ 18
6. Electronic data....................................................................................... 18
6.1. Data capture and location .................................................................................... 18
6.1.1. Transcription ................................................................................................... 18
6.1.2. Transfer ......................................................................................................... 18
6.1.3. Direct capture ................................................................................................. 19
6.1.4. Edit checks ..................................................................................................... 19
6.2. Audit trail and audit trail review ........................................................................... 19
6.2.1. Audit trail ....................................................................................................... 19
6.2.2. Audit trail review ............................................................................................. 20
6.3. Sign-off of data .................................................................................................. 21
6.4. Copying data ..................................................................................................... 21
6.5. Certified copies .................................................................................................. 22
6.6. Control of data ................................................................................................... 22
6.7. Cloud solutions .................................................................................................. 23

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 3/52
6.8. Backup of data ................................................................................................... 24
6.9. Contingency plans .............................................................................................. 24
6.10. Migration of data .............................................................................................. 24
6.11. Archiving ......................................................................................................... 25
6.12. Database decommissioning ................................................................................ 25
Annex 1 Agreements ................................................................................. 27
Annex 2 Computerised systems validation ................................................ 30
A2.1 General principles .............................................................................................. 30
A2.2 User requirements ............................................................................................. 31
A2.3 Trial specific configuration and customisation ........................................................ 31
A2.4 Traceability of requirements ............................................................................... 31
A2.5 Validation and test plans .................................................................................... 31
A2.6 Test execution and reporting............................................................................... 32
A2.7 Release for production ....................................................................................... 32
A2.8 User helpdesk ................................................................................................... 32
A2.9 Periodic review .................................................................................................. 33
A2.10 Change control ................................................................................................ 33
Annex 3 User management ........................................................................ 34
A3.1 User management ............................................................................................. 34
A3.2 User reviews ..................................................................................................... 34
A3.3 Segregation of duties ......................................................................................... 34
A3.4 Least-privilege rule ............................................................................................ 34
A3.5 Individual accounts ............................................................................................ 34
A3.6 Unique usernames ............................................................................................. 35
Annex 4 Security ....................................................................................... 36
A4.1 Ongoing security measures ................................................................................. 36
A4.2 Physical security ................................................................................................ 36
A4.3 Firewalls ........................................................................................................... 36
A4.4 Vulnerability management .................................................................................. 36
A4.5 Platform management ........................................................................................ 37
A4.6 Bi-directional devices ......................................................................................... 37
A4.7 Anti-virus software ............................................................................................ 37
A4.8 Penetration testing ............................................................................................ 37
A4.9 Intrusion detection and prevention ...................................................................... 37
A4.10 Internal activity monitoring ............................................................................... 37
A4.11 Security incident management .......................................................................... 38
A4.12 Authentication method ..................................................................................... 38
A4.13 Remote authentication ..................................................................................... 38
A4.14 Password managers ......................................................................................... 38
A4.15 Password policies ............................................................................................. 39
A4.16 Password confidentiality ................................................................................... 39
A4.17 Inactivity logout .............................................................................................. 39
A4.18 Remote connection .......................................................................................... 39
A4.19 Protection against unauthorised back-end changes .............................................. 39

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 4/52
Annex 5 Additional consideration to specific systems ............................... 40
A5.1 Electronic clinical outcome assessment ................................................................. 40
A5.2 Interactive response technology system ............................................................... 45
A5.3 Electronic informed consent ................................................................................ 46
Annex 6 Clinical systems ........................................................................... 50
A6.1 Purchasing, developing, or updating computerised systems by sites ........................ 50
A6.2 Site qualification by the sponsor .......................................................................... 50
A6.3 Training ........................................................................................................... 50
A6.4 Documentation of medical oversight .................................................................... 50
A6.5 Confidentiality ................................................................................................... 51
A6.6 Security ........................................................................................................... 51
A6.7 User management ............................................................................................. 51
A6.8 Direct access .................................................................................................... 51
A6.9 Trial specific data acquisition tools ....................................................................... 52
A6.10 Archiving ........................................................................................................ 52

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 5/52
Glossary
Generally used terms
Unless otherwise specified (e.g. 'source data' or 'source document') and in order to simplify the text,
'data' will be used in this guideline in a broad meaning, which may include documents, records or any
form of information.
All references to sponsors and investigators in this guideline also apply to their service providers,
irrespective of the services provided.
When a computerised system is implemented by an institution where the investigator is conducting a
clinical trial, any reference to the investigator in this guideline also includes the institution, when
applicable.
The term 'trial participant' is used in this text as a synonym for the term 'subject', which is defined in
Regulation (EU) No 536/2014 as 'an individual who participates in a clinical trial, either as a recipient of
the IMP or as a control'.
The term 'responsible party' is frequently used instead of sponsor or principal investigator. Please also
refer to section 4.2. and Annex 1.
The term 'agreement' is used as an overarching term for all types of documented agreements, including
contracts.
The term 'validation' encompasses aspects usually known as 'qualification and validation'.
Artificial intelligence
Artificial intelligence (AI) covers a very broad set of algorithms, which enable computers to mimic human
intelligence. It ranges from simple if-then rules and decision trees to machine learning and deep learning.
Audit trail
In computerised systems, an audit trail is a secure, computer generated, time-stamped electronic record
that allows reconstruction of the events relating to the creation, modification, or deletion of an electronic
record.
Clinical outcome assessment
Clinical outcome assessment (COA) employs a tool for the reporting of outcomes by clinicians, trial site
staff, observers, trial participants and their caregivers. The term COA is proposed as an umbrella term
to cover measurements of signs and symptoms, events, endpoints, health-related quality of life (HRQL),
health status, adherence to treatment, satisfaction with treatment, etc.
Computerised system life cycle
The life cycle of a computerised system includes all phases of the system; i.e. typically 1) the concept
phase where the responsible party considers to automate a process and where user requirements are
collected, 2) the project phase where a service provider can be selected, a risk-assessment is made, and
the system is implemented and validated, 3) the operational phase where a system is used in a regulated
environment and changes are implemented in a manner that maintains data confidentiality, integrity and
availability, and finally, 4) a retirement phase, which includes decisions about data retention/archiving,
migration or destruction and the management of these processes.
Configuration
Configuration sets up a system using existing (out-of-the-box) functionality. It requires no programming
knowledge.

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 6/52
Customisation
Customisation modifies and adds to existing functionality by custom coding. It requires programming
knowledge.
Data governance
The total of activities, processes, roles, policies, and standards used to manage and control the data
during the entire data life cycle, while adhering to ALCOA++ principles (see section 4.5.).
Data life cycle
All processes related to the creating, recording, processing, reviewing, changing, analysing, reporting,
transferring, storing, migrating, archiving, retrieving, and deleting of data.
Dynamic file formats
Dynamic files include automatic processing and/or enable an interactive relationship with the user. A
certified electronic copy may be retained in electronic file formats that are different from the original
record, but the equivalent dynamic nature (including metadata) of the original record should be retained.
Event log
An automated log of events in relation to the use of a system like system access, alerts or firing of edit
checks.
Patient-reported outcome
Any outcome reported directly by the trial participant and based on the trial participant's perception of
a disease and its treatment(s) is called patient-reported outcome (PRO). The term PRO is proposed as
an umbrella term to cover both single dimension and multi-dimension measurements of symptoms,
HRQL, health status, adherence to treatment, satisfaction with treatment, etc. (Source: CHMP 'Reflection
paper on the regulatory guidance for the use of HRQL measures in the evaluation of medicinal products'
- EMEA/CHMP/EWP/139391/2004)
Static file formats
Static files containing information or data that are fixed and allow no dynamic interaction.
Validation
'A process of establishing and documenting that the specified requirements of a computerized system
can be consistently fulfilled from design until decommissioning of the system or transition to a new
system. The approach to validation should be based on a risk assessment that takes into consideration
the intended use of the system and the potential of the system to affect human subject protection and
reliability of clinical trial results.' (ICH E6 R2 1.65)

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 7/52
Abbreviations
AI artificial intelligence
ALCOA++
attributable, legible, contemporaneous, original, accurate, complete,
consistent, enduring, available when needed and traceable
BYOD bring your own device
COA clinical outcome assessment
CTMS clinical trial management systems
DMP data management plan
DSMB data and safety monitoring board
eCOA electronic COA
eCRF electronic case report form
EDC electronic data collection
EMA European Medicines Agency
ePRO electronic PRO
eSource electronic source
eTMF electronic TMF
GCP IWG GCP inspectors’ working group
GCP good clinical practice
GPS global positioning system
HQRL health-related quality of life
HTML hypertext mark-up language
HTTPS hypertext transfer protocol secure
IaaS infrastructure as a service
IB investigator brochures
IMP investigational medicinal product
IRT interactive response technologies
IT information technology
JS JavaScript
KPI key performance indicator
PaaS platform as a service
PC personal computer
PDF portable document format
PRO patient-reported outcome

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 8/52
SaaS software as a service
SAE serious adverse event
SOP standard operating procedures
SUSAR suspected unexpected serious adverse reactions
TMF trial master file
UAT user acceptance test
UPS uninterruptable power supplies
URS user requirements specification
USB universal serial bus
UTC coordinated universal time
VPN virtual private network
Executive summary
Computerised systems are being increasingly used in clinical research. The complexity of such systems
has evolved rapidly in the last few years from electronic case report forms (eCRF), electronic patient
reported outcomes (ePROs) to various wearable devices used to continuously monitor trial participants
for clinically relevant parameters and ultimately to the use of artificial intelligence (AI). Hence, there is
a need to provide guidance to all stakeholders involved in clinical trials reflective of these changes in
data types and trial types on the use of computerised systems and on the collection of electronic data,
as this is important to ensure the quality and reliability of trial data, as well as the rights, dignity, safety
and wellbeing of the trial participants. This would ultimately contribute to a robust decision-making
process based on such clinical data.
This guideline will describe some generally applicable principles and definition of key concepts. It also
covers requirements and expectations for computerised systems, including validation, user
management, security, and electronic data for the data life cycle. Requirements and expectations are
also covered related to specific types of systems, processes, and data.
1. Introduction
As described above, the change in data and trial types and thereby the use of computerised systems
presents new challenges. The European Medicines Agency (EMA) 'Reflection Paper on expectations for
electronic source data and data transcribed to electronic data collection tools in clinical trials' started to
address these when it was published in 2010. However, the development of and experience with such
systems has progressed. A more up-to-date guideline is needed to replace the Reflection Paper.
There is no requirement or expectation that the sponsors and investigators use computerised systems
to collect data; however, the use of data acquisition tools if implemented and controlled to the described
standard, offers a wide variety of functions to improve data completeness, consistency and unambiguity,
e.g. automatic edit checks, automated data transfers, validation checks, assisting information and
workflow control.

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 9/52
2. Scope
The scope of this guideline is computerised systems, (including instruments, software and 'as a service')
used in the creation/capture of electronic clinical data and to the control of other processes with the
potential to affect participant protection and reliability of trial data, in the conduct of a clinical trial of
investigational medicinal products (IMPs). These include, but may not be limited to the following:
• Electronic medical records, used by the investigator to capture of all health information as per
normal clinical practice.
• Tools supplied to investigators/trial participants for recording clinical data via data entry (e.g.
electronic clinical outcome assessments [eCOAs]).
o Electronic trial participant data capture devices used to collect ePRO data, e.g. mobile
devices supplied to trial participants or applications for use by the trial participant on
their own device i.e. bring your own device (BYOD).
o Electronic devices used by clinicians to collect data e.g. mobile devices supplied to
clinicians.
• Tools supplied for the automatic capture of data for trial participants such as biometrics, e.g.
wearables or sensors.
• eCRFs (e.g. desktop or mobile device-based programs or access to web-based applications),
which may contain source data directly entered, transcribed data, or data transferred from other
sources, or any combination of these.
• Tools that automatically capture data related to the transit and storage temperatures for
investigational medicinal product (IMP) or clinical samples.
• Tools to capture, generate, handle, or store data in a clinical environment where analysis, tests,
scans, imaging, evaluations, etc. involving trial participants or samples from trial participants
are performed in support of clinical trials (e.g. LC-MS/MS systems, medical imaging and related
software).
• eTMFs, which are used to maintain and archive the clinical trial essential documentation.
• Electronic informed consent, for the provision of information and/or capture of the informed
consent when this is allowed according to national legislation, e.g. desktop or mobile device-
based programs supplied to potential trial participants or applications for use by the potential
trial participants on their BYOD or access to web-based applications.
• Interactive Response Technologies (IRT), for the management of randomisation, supply and
receipt of IMP, e.g. via a web-based application.
• Portals or other systems for supplying information from the sponsor to the sites (e.g. investigator
brochures (IBs), suspected unexpected serious adverse reactions (SUSARs) or training material),
from the sites to the sponsor (e.g. the documentation of the investigator's review of important
safety information), or from the sponsor or the site to adjudication committees and others.
• Systems/tools used to conduct remote activities such as monitoring or auditing.
• Other computerised systems implemented by the sponsor holding/managing and/or analysing
or reporting data relevant to the clinical trial e.g. clinical trial management systems (CTMS),
pharmacovigilance databases, statistical software, document management systems, test
management systems and central monitoring software.

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 10/52
• AI used in clinical trials e.g. for trial participant recruitment, determination of eligibility, coding
of events and concomitant medication, data clarification, query processes and event
adjudication. Requirements to AI beyond the generally applicable expectations to all systems will
not be covered in this guideline initially. This may be covered in a future Annex.
The approach towards computerised systems used in clinical practice (e.g. regarding validation) should
be risk proportionate (please also refer to section 4.6.).
3. Legal and regulatory background
• Regulation (EU) No 536/2014, or Directive 2001/20/EC and Directive 2005/28/EC
• ICH Guideline for good clinical practice E6 R2 (EMA/CHMP/ICH/135/1995 Revision 2)
This guideline is intended to assist the sponsors, investigators, and other parties involved in clinical trials
to comply with the requirements of the current legislation (Regulation (EU) No 536/2014,
Directive 2001/20/EC and Directive 2005/28/EC), as well as ICH E6 Good Clinical Practice (GCP),
regarding the use of computerised systems and the collection of electronic data in clinical trials.
The risk-based approach to quality management also has an impact on the use of computerised systems
and the collection of electronic data.
Consideration should also be given to meeting the requirements of any additional current legal and
regulatory framework that may in addition apply to the medicinal product regulatory framework,
depending on the digital technology. These may include e.g. medical devices, data protection legislation,
and legislation on electronic identification and electronic signatures.
Further elaboration of the expectations of the EU GCP Inspectors’ Working group (GCP IWG) on various
topics, including those on computerised systems, can be found as GCP IWG Q&As published on the EMA
website.
4. Principles and definition of key concepts
The following sections outline the basic principles that apply to all computerised systems used in
clinical trials.
4.1. Data integrity
Data integrity is achieved when data (irrespective of media) are collected, accessed, and maintained in
a secure manner, to fulfil the ALCOA++ principles of being attributable, legible, contemporaneous,
original, accurate, complete, consistent, enduring, available when needed and traceable as described in
section 4.5. in order for the data to adequately support robust results and good decision making
throughout the data life cycle. Assuring data integrity requires appropriate quality and risk management
systems as described in section 4.6., including adherence to sound scientific principles and good
documentation practices.
• Data governance should address data ownership and responsibility throughout the data life cycle,
and consider the design, operation, and monitoring of processes/systems to comply with the
principles of data integrity including control over intentional and unintentional changes to data.
• Data governance systems should include staff training on the importance of data integrity
principles and the creation of a working environment that enables visibility, and actively
encourages reporting of omissions and erroneous results.

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 11/52
Lack of integrity before the expiration of the mandated retention period may render the data unusable
and is equivalent to data loss/destruction.
4.2. Responsibilities
Roles and responsibilities in clinical trials should be clearly defined. The responsibility for the conduct of
clinical trials is assigned via legislation to two parties, which may each have implemented computerised
systems for holding/managing data:
• Investigators and their institutions, laboratories and other technical departments or clinics,
generate and store the data, construct the record, and may use their own software and hardware
(purchased, part of national or institutional health information systems, or locally developed).
• Sponsors that supply, store and/or, manage and operate computerised systems (including
software and hardware) and the records generated by them. Sponsors may do this directly, or
via service providers, including organisations providing e.g. eCOA, eCRF, or IRT that collect and
store data on behalf of sponsors.
Please refer to Annex 1 regarding the transfer/delegation to service providers of tasks related to the use
of computerised systems and services.
4.3. Data and metadata
Electronic data consist of individual data points. Data become information when viewed in context.
Metadata provide context for the data point. Different types of metadata exist such as: variable name,
unit, field value before and after change, reason for change, trial master file (TMF) location document
identifier, timestamp, user. Typically, these are data that describe the characteristics, structure, data
elements and inter-relationships of data e.g. audit trails. Metadata also permit data to be attributable to
an individual entering or taking an action on the data such as modifying, deleting, reviewing, etc. (or if
automatically generated, to the original data source). Metadata form an integral part of the original
record. Without the context provided by metadata, the data have no meaning. Loss of metadata may
result in a lack of data integrity and may render the data unusable.
4.4. Source data
The term source data refers to the original reported observation in a source document. Source documents
could be e.g. hospital records, clinical and office charts, laboratory notes. Other examples are emails,
spreadsheets, audio and/or video files, images, and tables in databases.
The location of source documents and the associated source data they contain, should be clearly
identified at all points within the data capture process.
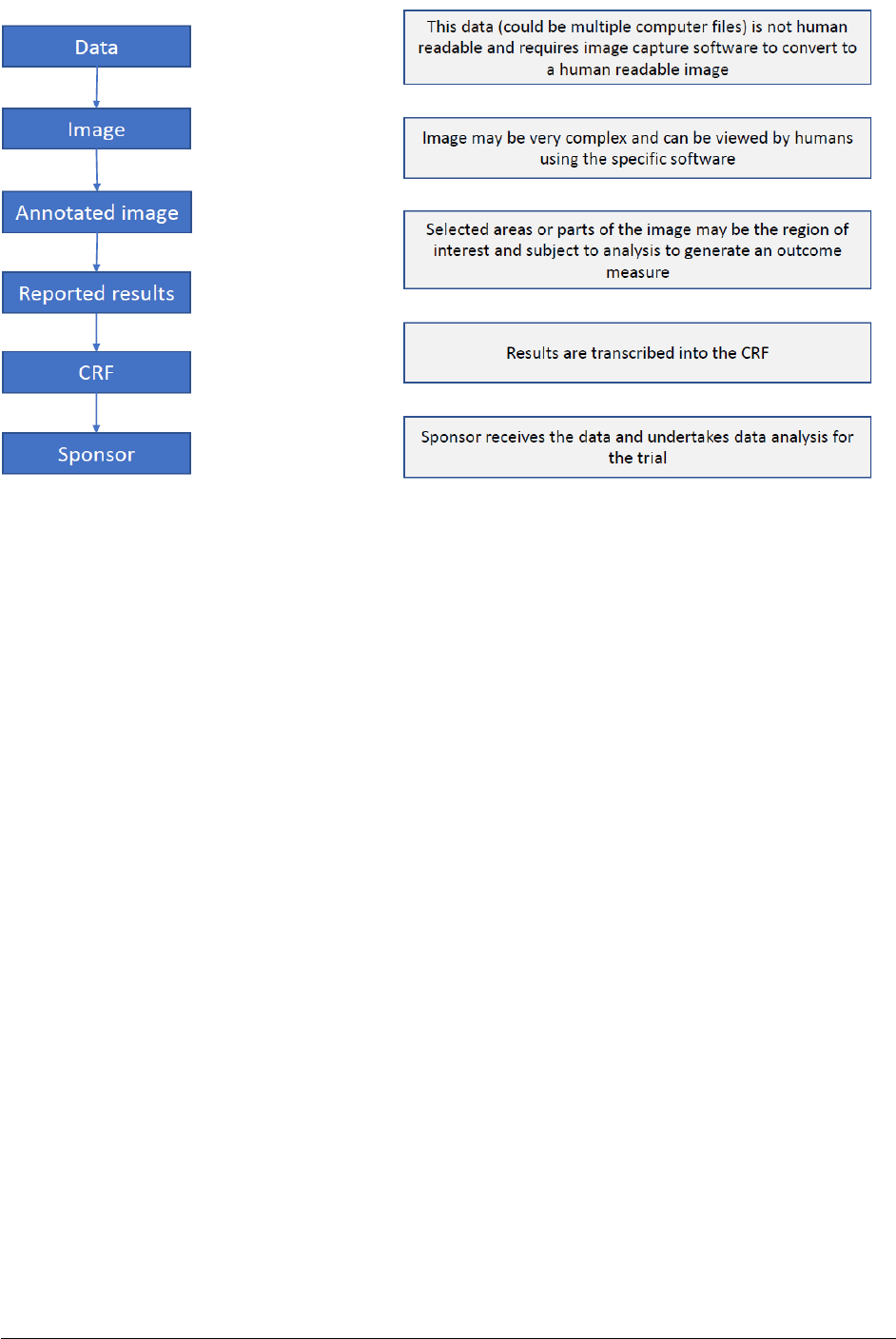
Below is an outline (figure 1) of the data processing stages, starting with the data capture. The correct
identification of source data is important for adequate source data verification and archiving. Data at
different processing stages can be considered source depending on the preceding processing steps.
Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 12/52
Figure 1
Data capture sometimes requires some degree of processing prior to data recording. In this process, the
data generated during an observation, measurement or data collection is checked, processed, and
transferred into a new format and then recorded.
The retention of unprocessed data records is not always feasible. If the processing is an integral part of
the solution used and is recognisable as such in the solution characteristics, there is no need to extract
and retain the unprocessed data. It should be possible to validate the correct operation of the processing.
As a general principle, the source data should be processed as little as possible and as much as
necessary.
From a practical point of view, the first obtainable permanent data from an electronic data
generation/capture should be considered and defined as the electronic source data. This process should
be validated to ensure that the source data generated/captured is representative of the original
observation and should contain metadata, including audit trail, to ensure adherence to the ALCOA++
principles (see section 4.5.). The location where the source data is first obtained should be part of the
metadata.
4.5. ALCOA++ principles
A number of attributes are considered of universal importance to data. These include that the data are:
Attributable
Data should be attributable to the person and/or system generating the data. Based on the criticality of
the data, it should also be traceable to the system/device, in which the data were generated/captured.
The information about originator (e.g. system operator, data originator) and system (e.g. device,
process) should be kept as part of the metadata.
Legible
Data should be maintained in a readable form to allow review in its original context. Therefore, changes
to data, such as compression, encryption and coding should be completely reversible.

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 13/52
Contemporaneous
Data should be generated by a system or captured by a person at the time of the observation. The time
point of the observation and the time point of the storage should be kept as part of the metadata,
including the audit trail. Accurate date and time information should be automatically captured and should
be linked and set by an external standard.
Original
Data should be the original first generation/capture of the observation. Certified copies can replace
original data (see section 6.5. on certified copies). Information that is originally captured in a dynamic
state should remain available in that state.
Accurate
The use of computerised systems should ensure that the data are at least as accurate as those recorded
on paper. The coding process, which consists in matching text or data collected on the data acquisition
tools to terms in a standard dictionary, thesaurus, or tables (e.g. units, scales), should be controlled.
The process of data transfer between systems should be validated to ensure the data remain accurate.
Data should be an accurate representation of the observations made. Metadata should contain
information to describe the observations and, where appropriate, it could also contain information to
confirm its accuracy.
Complete
To reconstruct and fully understand an event, data should be a complete representation of the
observation made. This includes the associated metadata and audit trail and may require preserving the
original context.
Consistent
Processes should be in place to ensure consistency of the definition, generation/capturing and
management (including migration) of data throughout the data life cycle. Processes should be
implemented to detect and/or avoid contradictions, e.g. by the use of standardisation, data validation
and appropriate training.
Enduring
Data should be maintained appropriately such that they remain intact and durable through the entire
data life cycle, as appropriate, according to regulatory retention requirements (see sections 6.8. and
6.10. on back-up and archiving).
Available when needed
Data should be stored throughout the data life cycle and should be readily available for review when
needed.
Traceable
Data should be traceable throughout the data life cycle. Any changes to the data, to the
context/metadata should be traceable, should not obscure the original information and should be
explained, if necessary. Changes should be documented as part of the metadata (e.g. audit trail).
4.6. Criticality and risks
ICH E6 describes the need for a quality management system with a risk-based approach. Risks should
be considered at both the system level e.g. standard operating procedures (SOPs), computerised
systems and staff, and for the specific clinical trial e.g. trial specific data and data acquisition tools or
trial specific configurations or customisations of systems.

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 14/52
Risks in relation to the use of computerised systems and especially critical risks affecting the rights,
safety and well-being of the trial participants or the reliability of the trial results would be those related
to the assurance of data integrity. Those risks should be identified, analysed, and mitigated or accepted,
where justified, throughout the life cycle of the system. Where applicable, mitigating actions include
revised system design, configuration or customisation, increased system validation or revised SOPs
(including appropriate training) for the use of systems and data governance culture.
In general, risks should be determined based on the system used, its complexity, operator, use of system
and data involved. Critical component parts of any system should always be addressed. For example, a
component part of an IRT system that calculates IMP dose based on data input by the investigator would
be high risk compared to other functionalities such as the generation of an IMP shipment report. The
interface and interdependency between systems or system components should be taken into
consideration.
All data collected or generated in the context of a clinical trial should fulfil ALCOA++ principles.
Consequently, the arrangements for data governance to ensure that data, irrespective of the format in
which they are generated, recorded, processed (including analysis, alteration/imputation,
transformation, or migration), used, retained (archived), retrieved and destroyed should be considered
for data integrity risks and appropriate control processes implemented.
The approach used to reduce risks to an acceptable level should be proportionate to the significance of
the risk. Risk reduction activities may be incorporated in protocol design and implementation, system
design, coding and validation, monitoring plans, agreements between parties that define roles and
responsibilities, systematic safeguards to ensure adherence to SOPs, training in processes and
procedures, etc.
There are special risks to take into consideration when activities are transferred/delegated. These are
further elaborated on in Annex 1 on agreements.
The risk-assessment should take the relevance of the system use for the safety, rights, dignity and well-
being of the participant and the importance and integrity of derived clinical trial data into account i.e.
whether the system is used for standard care and safety measurements for participants or if systems
are used to generate primary efficacy data that are relied on in e.g. a marketing authorisation application.
Systems used for other purposes than what they were developed for, or which are used outside the
supplier’s specification/validation are inherently higher risk. In case of well-established computerised
systems, which are used as intended in a routine setting for less critical trial data, the certification by a
notified body may suffice as documentation whereas other more critical systems may require a more in-
depth validation effort. This decision should be justified prior to use in the trial.
For systems deployed by the investigator/institution specifically for the purposes of clinical trials, the
investigator should ensure that the requirements for computerised systems as described in this guideline
are addressed and proportionately implemented. For systems deployed by the investigator/institution,
the sponsor should determine during site selection whether such systems (e.g. electronic medical records
and other record keeping systems for source data collection and the investigator site file) are fit for
purpose.
For computerised systems deployed by the sponsor, the sponsor should ensure that the requirements of
this guideline are addressed and proportionately implemented.
4.7. Data capture
The clinical trial protocol should specify data to be collected and the processes to capture them, including
by whom, when and by which tools.

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 15/52
Data acquisition tools should be designed and/or configured or customised to capture all information
required by the protocol and not more. Data fields should not be prepopulated or automatically filled in,
unless these fields are not editable and are derived from already entered data (e.g. body surface area).
The protocol should identify any data to be recorded directly in the data acquisition tools and identify
them as source data.
A detailed diagram and description of the transmission of electronic data (data flow) should be available
in the protocol or a protocol-related document. The sponsor should describe which data will be
transferred and in what format, the origin and destination of the data, the parties with access to the
transferred data, the timing of the transfer and any actions that may be applied to the data, for example,
data validation, reconciliation, verification, and review. The use of a data management plan (DMP) is
encouraged.
The sponsor should ensure the traceability of data transformations and derivations during data
processing and analysis.
4.8. Electronic signatures
Whenever ICH E6 requires a document to be signed and an electronic signature is used for that purpose,
the electronic signature functionality should meet the expectations stated below regarding
authentication, non-repudiation, unbreakable link, and timestamp of the signature.
The system should thus include functionality to:
• authenticate the signatory, i.e. establish a high degree of certainty that a record was signed by
the claimed signatory;
• ensure non-repudiation, i.e. that the signatory cannot later deny having signed the record;
• ensure an unbreakable link between the electronic record and its signature, i.e. that the contents
of a signed (approved) version of a record cannot later be changed by anyone without the
signature being rendered visibly invalid;
• provide a timestamp, i.e. that the date, time, and time zone when the signature was applied is
recorded.
Electronic signatures can further be divided into two groups depending on whether the identity of the
signatory is known in advance, i.e. signatures executed in 'closed' and in 'open' systems.
For 'closed' systems, which constitute the majority of systems used in clinical trials and which are
typically provided by the responsible party or by their respective service provider, the system owner
knows the identity of all users and signatories and grants and controls their access rights to the system.
Regulation (EU) No 910/2014 ('eIDAS') on electronic identification and trust services for electronic
transactions is not applicable for 'closed' systems ('eIDAS' article 2.2). The electronic signature
functionality in these systems should be proven during system validation to meet the expectations
mentioned above.
For 'open' systems, the signatories (and users) are not known in advance. For sites located in the EU,
electronic signatures should meet the requirements defined in the 'eIDAS' regulation. Sites located in
third countries should use electronic or digital signature solutions compliant with local regulations and
proven to meet the expectations mentioned above.
Irrespective of the media used, in case a signature is applied on a different document or only on part of
a document (e.g. signature page), there should still be an unbreakable link between the electronic
document to be signed and the document containing the signature.

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 16/52
4.9. Data protection
The confidentiality of data that could identify trial participants should be protected, respecting privacy
and confidentiality rules in accordance with the applicable regulatory requirement(s).
The requirements of General Data Protection Regulation (EU) No 2016/679 (GDPR) on the protection of
individuals with regard to the processing of personal data and on the free movement of such data should
be followed except when specific requirements are implemented for clinical trials e.g. that a trial
participant does not have the right to be forgotten (and for the data to be consequently deleted) as this
would cause bias to e.g. safety data (Regulation (EU) No 536/2014 recital 76 and Article 28(3)). Trial
participants should be informed accordingly.
In accordance with EU data protection legislation, if personal data of trial participants from an EU Member
State are processed (at rest or in transit) or transferred to a third country or international organisation,
such data transfer must comply with applicable Union data protection. In summary, this means that the
transfer must be either carried out on the basis of an adequacy decision (Article 45 of GDPR, Article 47
of Regulation (EU) No 2018/1727 - EUDPR), otherwise the transfer must be subject to appropriate
safeguards (as listed in Article 46 of GDPR or Article 48 of EUDPR) or the transfer may take place only if
a derogation for specific situations apply (under Article 49 of GDPR or Article 50 of EUDPR).
4.10. Validation of systems
Computerised systems used within a clinical trial should be subject to processes that confirm that the
specified requirements of a computerised system are consistently fulfilled, and that the system is fit for
purpose. Validation should ensure accuracy, reliability, and consistent intended performance, from the
design until the decommissioning of the system or transition to a new system.
The processes used for the validation should be decided upon by the system owner (e.g. sponsors,
investigators, technical facilities) and described, as applicable. System owners should ensure adequate
oversight of validation activities (and associated records) performed by service providers to ensure
suitable procedures are in place and that they are being adhered to.
Documentation (including information within computerised systems used as process tools for validation
activities) should be maintained to demonstrate that the system is maintained in the validated state.
Such documentation should be available for both the validation of the computerised system and for the
validation of the trial specific configuration or customisation.
Validation of the trial specific configuration or customisation should ensure that the system is consistent
with the requirements of the approved clinical trial protocol and that robust testing of functionality
implementing such requirements is undertaken, for example, eligibility criteria questions in an eCRF,
randomisation strata and dose calculations in an IRT system.
See Annex 2 for further detail on validation.
4.11. Direct access
All relevant computerised systems should be readily available with full, direct and read-only access (this
requires a unique identification method e.g. username and password) upon request by inspectors from
regulatory authorities. If a computerised system is decommissioned, direct access (with a unique
identification method) to the data in a timely manner should still be ensured (see section 6.12.).

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 17/52
5. Computerised systems
Requirements for validation are described in section 4.10. and Annex 2, the requirements for user
management are described in Annex 3, while the requirements for information technology (IT) security
are detailed in Annex 4 of this guideline.
5.1. Description of systems
The responsible party should maintain a list of physical and logical locations of the data e.g. servers,
functionality and operational responsibility for computerised systems and databases used in a clinical
trial together with an assessment of their fitness for purpose.
Where multiple computerised systems/databases are used, a clear overview should be available so the
extent of computerisation can be understood. System interfaces should be described, defining how the
systems interact, including validation status, methods used, and security measures implemented.
5.2. Documented procedures
Documented procedures should be in place to ensure that computerised systems are used correctly.
These procedures should be controlled and maintained by the responsible party.
5.3. Training
Each individual involved in conducting a clinical trial should be qualified by education, training, and
experience to perform their respective task(s). This also applies to training on computerised systems.
Systems and training should be designed to meet the specific needs of the system users (e.g. sponsor,
investigator or service provider). Special consideration should be given to the training of trial participants
when they are users.
There should be training on the relevant aspects of the legislation and guidelines for those involved in
developing, coding, building, and managing trial specific computerised systems, for example, those
employed at a service provider supplying eCRF, IRT, ePRO, trial specific configuration, customisation,
and management of the system during the conduct of the clinical trial.
All training should be documented, and the records retained and available for monitoring, auditing, and
inspections.
5.4. Security and access control
To maintain data integrity and the protection of the rights of trial participants, computerised systems
used in clinical trials should have security processes and features to prevent unauthorised access and
unwarranted data changes and should maintain blinding of the treatment allocation where applicable.
Checks should be used to ensure that only authorised individuals have access to the system and that
they are granted appropriate permissions (e.g. ability to enter or make changes to data). Records of
authorisation of access to the systems, with the respective levels of access clearly documented, should
be maintained. The system should record changes to user roles and thereby access rights and
permissions.
There should be documented training on the importance of security e.g. the need to protect passwords
and to keep them confidential, enforcement of security systems and processes, identification and
handling of security incidents, social engineering and the prevention of phishing.

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 18/52
See Annexes 3 and 4 for further guidance on user management and IT security.
5.5. Timestamp
Accurate and unambiguous date and time information given in coordinated universal time (UTC) or time
and time zone (set by an external standard) should be automatically captured.
Users should not be able to modify the date, time and time zone on the device used for data entry, when
this information is captured by the computerised system and used as a timestamp.
6. Electronic data
For each trial, it should be identified what electronic data and records will be collected, modified, imported
and exported, archived and how they will be retrieved and transmitted. Electronic source data, including
the audit trail should be directly accessible by investigators, monitors, auditors, and inspectors without
compromising the confidentiality of participants’ identities.
6.1. Data capture and location
The primary goal of data capture is to collect all data required by the protocol. All pertinent observations
should be documented in a timely manner. The location of all source data should be specified prior to
the start of the trial and updated during the conduct of the trial where applicable.
6.1.1. Transcription
Source data collected on paper (e.g. worksheets, paper CRFs or paper diaries or questionnaires) need
to be transcribed either manually or by a validated entry tool into the electronic data collection (EDC)
system or database(s). In case of manual transcription, risk-based methods should be implemented to
ensure the quality of the transcribed data (e.g. double data entry and/or data monitoring).
6.1.2. Transfer
Trial data are transferred in and between systems on a regular basis. The process for file and data
transfer needs to be validated and should ensure that data and file integrity are assured for all transfers.
Data that is collected from external sources and transferred in open networks should be protected from
unwarranted changes and secured/encrypted in a way that precludes disclosure of confidential
information.
All transfers that are needed during the conduct of a clinical trial need to be pre-specified.
Validation of transfer should include appropriate challenging test sets and ensure that the process is
available and functioning at clinical trial start (e.g. to enable ongoing sponsor review of diary data, lab
data or adverse events by safety committees). Data transcribed or extracted and transferred from
electronic sources and their associated audit trails should be continuously accessible (according to
delegated roles and corresponding access rights).
Transfer of source data and records when the original data or file are not maintained is a critical process
and appropriate considerations are expected in order to prevent loss of data and metadata.

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 19/52
6.1.3. Direct capture
Direct data capture can be done by using electronic data input devices and applications such as electronic
diaries, electronic questionnaires and eCRFs for direct data entry. Where treatment-related pertinent
information is captured first in a direct data capture tool such as a trial participant diary, a PRO form or
a special questionnaire, a documented procedure should exist to transfer or transcribe information into
the medical record, when relevant.
Direct data capture can also be done by automated devices such as wearables or laboratory or other
technical equipment (e.g. medical imaging, electrocardiography equipment) that are directly linked to a
data acquisition tool. Such data should be accompanied by metadata concerning the device used (e.g.
device version, device identifiers, firmware version, last calibration, data originator, timestamp of
events).
6.1.4. Edit checks
Computerised systems should validate manual and automatic data inputs to ensure a predefined set of
validation criteria is adhered to. Edit checks should be relevant to the protocol and developed and revised
as needed. Edit checks should be validated and implementation of the individual edit checks should be
controlled and documented. If edit checks are paused at any time during the trial, this should be
documented and justified. Edit checks could either be run immediately at data entry or automatically
during defined intervals (e.g. daily) or manually.
Such approaches should be guided by necessity, should not cause bias and should be traceable e.g.
when data are changed as a result of an edit check notification.
The sponsor should not make automatic or manual changes to data entered by the investigator or trial
participants unless authorised by the investigator.
6.2. Audit trail and audit trail review
6.2.1. Audit trail
An audit trail should be enabled for the original creation and subsequent modification of all electronic
data. In computerised systems, the audit trail should be secure, computer generated and timestamped.
An audit trail is essential to ensure that changes to the data are traceable. Audit trails should be robust,
and it should not be possible for 'normal' users to deactivate them. If possible, for an audit trail to be
deactivated by 'admin users', this should automatically create an entry into a log file (e.g. audit trail).
Entries in the audit trail should be protected against change, deletion, and access modification (e.g. edit
rights, visibility rights). The audit trail should be stored within the system itself. The responsible
investigator, sponsor, and inspector should be able to review and comprehend the audit trail and
therefore audit trails should be in a human-readable format.
Audit trails should be visible at data-point level in the live system, and it should be possible to export
the entire audit trail as a dynamic data file to allow for the identification of systematic patterns or
concerns in data across trial participants, sites, etc. The audit trail should show the initial entry and the
changes (value - previous and current) specifying what was changed (field, data identifiers) by whom
(username, role, organisation), when (date/timestamp) and, where applicable, why (reason for change).
A procedure should be in place to address the situation when a data originator (e.g. investigator or trial
participant) realises that she/he has submitted incorrect data by mistake and wants to correct the
recorded data.

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 20/52
It is important that original electronic entries are visible or accessible (e.g. in the audit trail) to ensure
the changes are traceable. The audit trail should record all changes made as a result of data queries or
a clarification process. The clarification process for data entered should be described and documented.
Changes to data should only be performed when justified. Justification should be documented. In case
the data originator is the trial participant, special considerations to data clarifications might be warranted.
See Annex 5 section A5.1.1.4 for further details.
For certain types of systems (e.g. ePRO) the data entered may not be uploaded immediately but may
be temporarily stored in local memory. Such data should not be edited or changed without the knowledge
of the data originator prior to saving. Any changes or edits should be acknowledged by the data
originator, should be documented in an audit trail and should be part of validation procedures. The
timestamp of data entry in the capture tool (e.g. eCRF) and timestamp of data saved to a hard drive
should be recorded as part of the metadata. The duration between initial capture in local memory and
upload to a central server should be short and traceable (i.e. transaction time), especially in case of
direct data entry.
Data extracts or database extracts for internal reporting and statistical analysis do not necessarily need
to contain the audit trail information. However, the database audit trail should capture the generation of
data extracts and exports.
Audit trails should capture any changes in data entry per field and not per page (e.g. eCRF page).
In addition to the audit trail, metadata could also include (among others) review of access logs, event
logs, queries etc.
Access logs, including username and user role, are in some cases considered to be important metadata
and should consequently be available. This is considered necessary e.g. for systems that contain critical
unblinded data.
Care should be taken to ensure that information jeopardising the blinding does not appear in the audit
trail accessible to blinded users.
6.2.2. Audit trail review
Procedures for risk-based trial specific audit trail reviews should be in place and performance of data
review should be generally documented. Data review should focus on critical data. Data review should
be proactive and ongoing review is expected unless justified. Manual review as well as review by the use
of technologies to facilitate the review of larger datasets should be considered. Data review can be used
to (among others) identify missing data, detect signs of data manipulation, identify abnormal
data/outliers and data entered at unexpected or inconsistent hours and dates (individual data points,
trial participants, sites), identify incorrect processing of data (e.g. non-automatic calculations), detect
unauthorised accesses, detect device or system malfunction and to detect if additional training is needed
for trial participants /site staff etc. Audit trail review can also be used to detect situations where direct
data capture has been defined in the protocol but where this is not taking place as described.
In addition to audit trail review, metadata review could also include (among others) review of access
logs, event logs, queries, etc.
The investigator should receive an introduction on how to navigate the audit trail of their own data in
order to be able to review changes.

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 21/52
6.3. Sign-off of data
The investigators are responsible for data entered into eCRFs and other data acquisition tools under their
supervision (electronic records).
The sponsor should seek investigator endorsement of their data at predetermined milestones. The
signature of the investigator or authorised member of the investigator’s staff is considered as the
documented confirmation that the data entered by the investigator and submitted to the sponsor are
attributable, legible, original, accurate, and complete and contemporaneous. Any member of the staff
authorised for sign-off should be qualified to do so in order to fulfil the purpose of the review as described
below. National law could require specific responsibilities, which should then be followed.
The acceptable timing and frequency for the sign-off needs to be defined and justified for each trial by
the sponsor and should be determined by the sponsor in a risk-based manner. The sponsor should
consider trial specific risks and provide a rationale for the risk-based approach. Points of consideration
are types of data entered, non-routine data, importance of data, data for analysis, length of the trial and
the decision made by the sponsor based on the entered data, including the timing of such decisions. It
is essential that data are confirmed prior to interim analysis and the final analysis, and that important
data related to e.g. reporting of serious adverse events (SAEs), adjudication of important events and
endpoint data, data and safety monitoring board (DSMB) review, are signed off in a timely manner. In
addition, a timely review and sign-off of data that are entered directly into the eCRF as source is
particularly important.
Therefore, it will rarely be sufficient to just provide one signature immediately prior to database lock.
Signing of batches of workbooks is also not suited to ensure high data quality and undermines the
purpose of timely and thorough data review.
For planned interim analysis, e.g. when filing for a marketing authorisation application, all submitted
data need to be signed off by the investigator or their designated and qualified representative before
extracting data for analysis. The systems should be designed to support this functionality.
To facilitate timely data review and signing by the investigator or their designated representative, the
design of the data acquisition tool should be laid out to support the signing of the data at the defined
time points.
Furthermore, it is important that the investigator review the data on an ongoing basis in order to detect
shortcomings and deficiencies in the trial conduct at an early stage, which is the precondition to
undertake appropriate corrective and preventive actions.
Adequate oversight by the investigator is a general requirement to ensure participant safety as well as
data quality and integrity. Oversight can be demonstrated by various means, one of them being the
review of reported data. Lack of investigator oversight may prevent incorrect data from being corrected
in a timely manner and necessary corrective and preventive actions being implemented at the
investigator site.
6.4. Copying data
Data can be copied or transcribed for different purposes, either to replace source documents or essential
documents or to be distributed amongst different stakeholders as working copies. If essential documents
or source documents are irreversibly replaced by a copy, the copy should be certified (see section 6.5.).
Copies should contain a faithful representation of the data and the contextual information. Source
documents and data should allow accurate copies to be made. The method of copying should be practical
and should ensure that the resulting copy is complete and accurate. It should include the relevant

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 22/52
metadata and such metadata should be complete and accurate. See also section 5 of the 'Guideline on
the content, management and archiving of the clinical trial master file (paper and/or electronic)'
(EMA/INS/GCP/856758/2018), for further details on definition.
6.5. Certified copies
When creating a certified copy, the nature of the original document needs to be considered. For example,
the content of the file is either static (e.g. a PDF document) or dynamic (e.g. a worksheet with automatic
calculations) or the copy tries to capture the result of an interpreter (e.g. a web page, where a web-
browser interprets written hypertext mark-up language (HTML), JavaScript (JS) among other
programming languages). Either way, the result of the copy process should be verified either
automatically by a validated process or manually to ensure that the same information is present —
including data that describe the context, content, and structure — as in the original.
In case of dynamic files e.g. when a database is decommissioned and copies of data and metadata are
provided to sponsors, the resulting file should also capture the dynamic aspects of the original file. In
case of files, which are the result of an interpreter, special care needs to be taken to not only consider
the informative content of such a file, but also to capture and preserve aspects that are the result of the
interactions of the used interpreter(s) and system settings during the display. For example, window size,
browser type, operating system employed and the availability of software dependencies (e.g. enabled
active web content) can influence the structure and content displayed. Special considerations should be
taken whenever copies are to replace original source documents.
6.6. Control of data
Data generated at the clinical trial site relating to the trial participants should be available to the
investigator at all times during and after the trial to enable investigators to make decisions related to
eligibility, treatment, care for the participants, etc. and to ensure that the investigator can fulfil their
legal responsibility to retain an independent copy of the data for the required retention period. This
includes data from external sources, such as central laboratory data, centrally read imaging data and
ePRO data.
Exceptions should be justified in the protocol e.g. if sharing this information with the investigator would
jeopardise the blinding of the trial.
The sponsor should not have exclusive control of the data entered in a computerised system at any point
in time. All data held by the sponsor that has been generated in a clinical trial should be verifiable to a
copy of these data that is not held (or that has not been held) by the sponsor.
The requirements above are not met if data are captured in a computerised system and the data are
stored on a central server under the sole control of the sponsor or under the control of a service provider
that is not considered to be independent from the sponsor or if the sponsor (instead of the service
provider) is distributing the data to the investigator. This is because the investigator does not hold an
independent copy of the data and therefore the sponsor has exclusive control of the data. In order to
meet the requirements, the investigator should be able to download a contemporaneous certified copy
of the data. This is in addition to the record maintained at a service provider.
Instead of a system maintained by an independent service provider, the sponsor may take other
adequate technical measures that preclude sole control. E.g. the verifiability of data (transactions) by
an independent (distributed) tamper-proof ledger may provide comparable security to a system
maintained by an independent service provider. This should be justified and documented.

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 23/52
Data entered to data acquisition tools by the investigator should be available to the investigator
throughout the whole legally mandated duration and for the full duration of local legal requirements.
This can be ensured either by contemporaneous local copies at the trial site or e.g. by the use of a service
provider. Access to the data may be amended to read-only as part of the database lock process. Prior to
read-only access to the investigator being revoked, a copy including the audit trail should be made
available to the investigator in a complete and comprehensive way. In the situation where a service
provider is hosting the data, the copy should not be provided via the sponsor, as this would temporarily
provide the sponsor with exclusive control over the data and thereby jeopardise the investigator’s
control. Copies should not be provided in a way that requires advanced technical skills from the
investigators. The period between the provision of the copy to the investigator and the closure of the
investigators’ read-only access to the database(s) should allow sufficient time for the investigator to
review the copy and access should not be revoked until such a review has been performed.
Any contractual agreements regarding hosting should ensure investigator control. If the sponsor is
arranging hosting on behalf of the investigators through a service provider, agreements should ensure
the level of investigator control mentioned above.
Investigators delegating hosting of such data to service providers themselves should ensure that the
intended use is covered by local legal requirements and the in-house rules of the institution.
For investigator-initiated trials, where the data are hosted somewhere in the sponsor/institution
organisation, the degree of independence should be justified and pre-specified in agreements e.g. that
it is a central IT department, not otherwise involved in the operational aspects of the trial, hosting the
data and providing copies to the participating investigators.
6.7. Cloud solutions
Irrespective whether a computerised system is installed at the premises of the sponsor, investigator,
another party involved in the trial or whether it is made available by a service provider as a cloud
solution, the requirements in this guideline are applicable. There are, however, specific points to be
considered as described below.
Cloud solutions cover a wide variety of services related to the computerised systems used in clinical
trials. These can range from Infrastructure as a Service (IaaS) over Platform as a Service (PaaS) to
Software as a Service (SaaS). It is common for these services that they provide the responsible party
on-demand availability of computerised system resources over the internet, without having the need or
even the possibility to directly manage these services.
If a cloud solution is used, the responsible party should ensure that the service provider providing the
cloud is qualified.
When using cloud computing, the responsible parties are at a certain risk, because many services are
managed less visibly by the cloud provider.
Contractual obligations with the cloud solution provider should be detailed and explicit and refer to all
ICH E6 relevant topics and to all relevant legal requirements (see Annex 1).
Data jurisdiction may be complex given the nature of cloud solutions and services being shared over
several sites, countries, and continents; however, any uncertainties should be addressed and solved by
contractual obligations prior to the use of a cloud solution.
If the responsible party choses to perform their own validation of the computerised system, the cloud
provider should make a test environment available that is identical to the production environment.

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 24/52
6.8. Backup of data
Data stored in a computerised system are susceptible to system malfunction, intended or unintended
attempts to alter or destroy data and physical destruction of media and infrastructure and are therefore
at risk of loss. Data and configurations should be regularly backed up. Please also refer to Annex 4 for
further details on IT security.
The use of replicated servers is strongly recommended. Backups should be stored in separate physical
locations and logical networks and not behind the same firewall as the original data to avoid simultaneous
destruction or alteration.
Frequency of backups (e.g. hourly, daily, weekly) and their retention (e.g. a day, a week, a month)
should be determined through a risk-based approach.
Checks of accessibility to data, irrespective of format, including relevant metadata, should be undertaken
to confirm that the data are enduring, continue to be available, readable and understandable by a human
being. There should be procedures in place for risk-based (e.g. in connection with major updates) restore
tests from the backup of the complete database(s) and configurations and the performed restore tests
should be documented.
Disaster mitigation and recovery plans should be in place to deal with events that endanger data security.
Such plans should be regularly reviewed. Disaster mitigation and recovery plans should be part of the
contractual agreement, if applicable.
6.9. Contingency plans
Agreements and procedures should be in place to allow trial continuation and prevent loss of data critical
to participant safety and trial results.
6.10. Migration of data
Migration as opposed to the transfer of data (as described in section 6.1.2.) is the process of permanently
moving existing data (including metadata) from one system into another system e.g. the migration of
individual safety reports from one safety database to another. It should be ensured that the migration
does not adversely affect existing data and metadata.
In the course of the design or purchase of a new system and of subsequent data migration from an old
system, validation of the data migration process should have no less focus than the validation of the
system itself.
The validation of data migration should take into consideration the complexity of the task and any
foreseen possibilities that may exist to verify the migrated data (e.g. checksum, case counts, quality
control of records).
Prior to migration, the process should be planned in detail. A risk analysis identifying the most probable
risks should take place and should yield appropriate mitigation strategies. After the planning, the
intended procedure should be validated with mock data and results should be considered for risk-
assessment and mitigation. A data verification focused on key data should be performed post migration.
Verification of migrated data can be simple or complex, depending on the different platforms and systems
involved. Regardless of the effort needed, the migration process should be documented in such detail
that throughout all data operations/transformations data changes remain traceable. Mapping from the
old system onto the new system should be retained.

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 25/52
Data, contextual information, and the audit trail should not be separated. In case migration of data into
a new system results in a loss of relevant data, adequate mitigating actions should be taken to establish
a robust method to join the audit trail and the data for continuous access by all stakeholders. A detailed
explanation is expected, if no such method has been established to allow the migration of data and the
audit trail. Arrangements should ensure that the link between data and metadata can be established. If
several parties are involved, agreements should be in place to ensure this.
6.11. Archiving
The investigator and sponsor should be aware of the required retention periods for clinical trial data and
essential documents, including metadata. Retention periods should respect the data protection principle
of storage limitation. An inventory of all essential data and documents and corresponding retention
periods should be maintained. It should be clearly defined which data are related to each clinical trial
activity and where this record is located and who has access/edit rights to the document. Security
controls should be in place to ensure data confidentiality, integrity, and availability.
It should be ensured that the file and any software required (depending on the media used for storage)
remain accessible, throughout the retention period. This could imply e.g. migration of data (see
section 6.9.).
Suitable archiving systems should be in place to safeguard data integrity for the periods established by
the regulatory requirements including those in any of the regions where the data may be used for
regulatory submissions, and not just those of the country where the data are generated.
Source documents and data should always be available when needed to authorised individuals to meet
their regulatory obligations. Please refer to section 4.11 direct access.
Data should be maintained in a secure manner and should only be transferred between different
(physical) locations in a validated process. Data should be archived in a read-only state.
6.12. Database decommissioning
After the finalisation of the trial, database(s) might be decommissioned. It is recommended that the time
of decommissioning is decided taking into consideration e.g. whether the clinical trial will be used for a
marketing authorisation application in the near future in which case it is recommended to keep the
database(s) live. Please refer to figure 2 for a proposed approach. A dated and certified copy of the
database(s) and data should be archived and available on request. In case of decommissioning, the
sponsor should ensure (contractually if done by a service provider) that archived formats provide the
possibility to restore the database(s). This includes the restoration of dynamic functionality and all
relevant metadata (audit trail, event logs, implemented edit checks, queries, user logs, etc.). Where
recommissioning is no longer possible, the sponsor should ensure that all the data including metadata
files (e.g. audit trails) are available in dynamic data files. The sponsor should review the system to
determine the audit trails and logs available in the system and how these would be retained as dynamic
files. Where a service provider is involved, this should be addressed in the contractual arrangements.
Static formats of dynamic data will not be considered adequate. See definitions section on static and
dynamic formats.

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 26/52
Figure 2

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 27/52
Annex 1 Agreements
The legally responsible parties are the sponsors and investigators. They contract/delegate an increasing
number of tasks in clinical trials, contracting is frequent in the area of computerised systems where the
responsible party might lack internal knowledge or resources or they wish to purchase a product or a
service that has been developed by others. The responsible parties can delegate tasks to a service
provider, but nevertheless the full responsibility for the data integrity, security and confidentiality resides
with them.
Agreements can cover a variety of tasks such as system and trial specific configuration and
customisation, provision of a license to an application, full clinical trial service including data management
tasks e.g. site contact, training, data clarification processes, etc., but could also be restricted to hosting
services. A risk-based approach can be used in relation to agreements as well as for computerised
systems in general. It is recognised that a trial specific agreement is not required, if a product is
purchased and used as intended without the involvement of the manufacturer of the system; however,
such use will require a risk assessment by the responsible party to assess whether such a non-trial
specific system is fit for its intended use.
The responsible party should ensure that the distribution of tasks in a trial is clearly documented and
agreed on. It should be ensured that each party has the control of and access to data and information
that their legal responsibilities require and that the ethics committees and regulatory authorities
approving trials have been properly informed of distribution of activities as part of the clinical trial
application process, where applicable. This should be carefully documented in the protocol and related
documents, procedures, agreements, and other documents as relevant. It is important to consider who
is providing and controlling the computerised system being used.
Clear written agreements should be in place and appropriately signed by all involved parties prior to the
provision of services or systems. Agreements should be maintained/updated as appropriate. Sub-
contracting and conditions for sub-contracting and the responsible party’s oversight of sub-contracted
activities should be specified.
The responsible parties should ensure oversight of these trial-related duties e.g. by reviewing defined
key performance indicators (KPIs) or reconciliations.
If appropriate agreements cannot be put in place due to the inability or reluctance of a service provider
to allow access to important documentation (e.g. system requirements specifications) or the service
provider is unwilling to support pre-qualification audits or regulatory inspections, systems from such a
service provider should not be used in clinical trials.
The responsible party should ensure that service providers (including vendors of computerised systems)
have the knowledge and the processes to ensure that they can perform their tasks in accordance with
ICH E6, as appropriate to their tasks. Standards to be followed, e.g. clinical trial legislation and guidance
should be specified in the agreement, where relevant. A number of tasks involve accessing, reviewing,
collecting and/or analysing data, much of which is personal/pseudonymised data. In addition, in specific
cases involving contact with (potential) trial participants, data protection legislation needs to be followed,
in addition to the clinical trial legislation and guidance.
The approved protocol, implicitly, defines part of the specification for system configuration or
customisation (e.g. for interactive response technologies (IRT) systems and data acquisition tools) and
there should be consistency between the protocol and the wording of the agreement. In addition, it
should be clear how subsequent changes to the protocol are handled so that the vendor can implement
changes to the computerised system, where relevant.

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 28/52
It should be clear from agreements which tasks are delegated also in relation to retaining essential
documentation for performed activities. In the context of clinical trials, system-documentation (including
e.g. software/system validation documentation, vendor standard operating procedures (SOPs), training
records, issues log/resolutions) as well as trial master file (TMF) documentation (e.g. emails on important
decisions and meeting minutes) related to the individual clinical trial (including e.g. relevant helpdesk
tickets or meeting minutes) should be retained for the full retention period. It should be clear from the
agreement which party is retaining and maintaining which documentation and how and in what format
that documentation is made available when needed e.g. for an audit or an inspection. There should be
no difference in the availability of documentation irrespective of whether the documentation is held by
the sponsor/investigator or a service provider or sub-contracted party.
The responsible party is ultimately responsible for e.g. the validation and operation of the computerised
system and for providing adequate documented evidence of applicable processes.
The responsible party should be able to provide the GCP inspectors of the EU/EEA authorities with access
to the requested documentation regarding the validation and operation of computerised systems
irrespective of who performed these activities.
It should be specified in agreements that the sponsor or the institution, as applicable, should have the
right to conduct audits at the vendor site and that the vendor site could be subject to inspections (by
national and/or international authorities) and that the vendor site shall accept these. The responsible
party should also ensure that their service providers act on/respond appropriately to findings from audits
and inspections.
The sponsor has a legal responsibility under Regulation (EU) No 536/2014 to report serious breaches,
including important data and security breaches, to authorities within seven days. To avoid undue delay
in sponsor reporting from the time of discovery e.g. by a vendor, agreements and related documents
should specify which information should be escalated immediately to ensure regulatory compliance.
As set out in ICH E6, to ensure that the investigator, rather than the sponsor, maintains control over
their data, it should be specified in agreements how investigators’ access to and control over data are
ensured during and after the trial, and the revocation of investigator access to data in case of
decommissioning should be described. It should also be specified which outputs the involved parties
(e.g. sponsor and investigators) will receive during and after the clinical trial and in what formats. Types
of output could include e.g. data collected via data acquisition tools including metadata, queries, history
and status of changes to users and their access rights, and the description of format for delivery of the
complete database to sponsors.
Arrangements on the decommissioning of the database(s) should be clear, including the possibility to
restore the database(s), for instance, for inspection purposes.
The agreements should address expectations regarding potential system 'down-time' and the preparation
of contingency plans.
Tasks transferred/delegated could include hosting of data. If data are hosted by a vendor, location of
data storage and control (e.g. use of cloud services) should be described.
Agreements should ensure reliable, continued and timely access to the data in case of bankruptcy,
shutdown, disaster of the vendor, discontinuation of service by the vendor or for reasons chosen by the
sponsor/investigator (e.g. change of vendor).
Special consideration should be given on training and quality systems. Vendors accepting tasks on
computerised systems should not only be knowledgeable about computerised systems and data
protection legislation, but also on GCP requirements, quality systems, etc. as appropriate to the tasks
they perform.

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 29/52
This guideline should be read together with the notice to sponsors regarding computerised systems
(EMA/INS/GCP/467532/2019) published on the EMA website.

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 30/52
Annex 2 Computerised systems validation
A2.1 General principles
The responsible party should ensure that systems used in clinical trials have been appropriately validated
and demonstrated to meet the requirements defined in ICH E6 and in this guideline.
Systems should be validated independently of whether they are developed on request by the responsible
party, are commercially or freely available, or are provided as a service.
The responsible party may rely on validation documentation provided by the vendor of a system if they
have assessed the validation activities performed by the vendor and the associated documentation as
adequate; however, they may also have to perform additional validation activities based on a
documented assessment. In any case, the responsible party remains ultimately responsible for the
validation of the computerised systems used in clinical trials.
If the responsible party wants to use the vendor's validation documentation, the responsible party should
ensure that it covers the responsible party's intended use as well as its defined needs and requirements.
The responsible party should be thoroughly familiar with the vendor's quality system and validation
activities, which can usually be obtained through an in-depth systematic examination (e.g. an audit).
This examination should be performed by qualified staff with sufficient time spent on the activities and
with cooperation from the vendor. It should go sufficiently deep into the actual activities, and a suitable
number of relevant key requirements and corresponding test cases should be reviewed, and this review
should be documented. The examination report should document that the vendor's validation process
and documentation is satisfactory. Any shortcomings should be mitigated by the responsible party, e.g.
by requesting or performing additional validation activities.
Some service providers may release new or updated versions of a system at short notice, leaving
insufficient time for the responsible party to validate it or to review any validation documentation
supplied by the service provider. In such a situation, it is particularly important for the responsible party
to evaluate the vendor's process for validation prior to release for production, and to strengthen their
own periodic review and change control processes. New functionalities should not be used by the
responsible party until they have validated them or reviewed and assessed the vendor's documentation.
If the responsible party relies on the vendor's validation documentation, inspectors should be given
access to the full documentation and reporting of the responsible party’s examination of the vendor. If
this examination is documented in an audit report, this may require providing access to the report. The
responsible party, or where applicable, the service provider performing the examination activities on
their behalf, should have a detailed understanding of the validation documentation.
As described in Annex 1 on agreements, the validation documentation should be made available to the
inspectors in a timely manner, irrespective of whether it is provided by the responsible party or the
vendor of the system. Contractual arrangements should be made to ensure continued access to this
documentation for the legally defined retention period even if the sponsor discontinues the use of the
system or if the vendor discontinues to support the system or ceases its activities.
In case the vendor’s validation activities and documentation are insufficient, or if the responsible party
cannot rely on the vendor to provide documentation, the responsible party should validate the system.
Any difference between the test and the production configuration and environment should be
documented and its significance assessed and justified.
Interfaces between systems should be clearly defined and validated e.g. transfer of data from one system
to another.

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 31/52
A2.2 User requirements
Critical system functionality implemented and used in a clinical trial should be described in a set of user
requirements or use cases, e.g. in a user requirements specification (URS). This includes all
functionalities, which ensure trial conduct in compliance with ICH E6 and which include capturing,
analysing, reporting and archiving clinical trial data in a manner that ensures data integrity. User
requirements should include, but may not be limited to operational, functional, data integrity, technical,
interface, performance, availability, security, and regulatory requirements. The above applies
independently of the sourcing strategy of the responsible party or the process used to develop the
system.
Where relevant, user requirements should form the basis for system design, purchase, configuration,
and customisation; but in any case, they should constitute the basis for system validation.
The responsible party should adopt and take full ownership of the user requirements, whether they are
documented by the responsible party, by a vendor or by a service provider. The responsible party should
review and approve the user requirements in order to verify that they describe the functionalities needed
by users in their particular clinical trials.
User requirements should be maintained and updated as applicable throughout a system’s lifecycle when
system functionalities are changed.
A2.3 Trial specific configuration and customisation
The configuration and customisation of a system for use in a specific trial should be pre-specified,
documented in detail and verified as consistent with the protocol, with the data management plan and
other related documents. Trial specific configuration and customisation should be quality controlled and
tested as applicable before release for production. It is recommended to involve users in the testing
activities. The same process applies to modifications required by protocol amendments.
If modifications to a system are introduced due to a protocol amendment, e.g. to collect additional
information, it should be determined whether they should be applied to all trial participants or only to
those concerned by the amendment.
If new functionalities or interfaces need to be developed, or new code added, they should be validated
before use.
A2.4 Traceability of requirements
Traceability should be established and maintained between each user requirement and test cases or
other documents or activities, such as standard operating procedures, as applicable. This traceability
may have many forms and the process may be automated by software. It should be continuously updated
as requirements are changed to ensure that where applicable, for every requirement, there is a
corresponding test case or action, in line with the risk evaluation.
A2.5 Validation and test plans
Validation activities should be planned, documented, and approved. The validation plan should include
information on the validation methodology, the risk-based approach taken and if applicable, the division
of tasks between the responsible party and a service provider. Prior to testing, the risk assessment
should define which requirements and tests are related to critical system functionality.

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 32/52
Test cases should be pre-approved. They may have many formats and while historically consisting of
textual documents including tables with multiple columns corresponding to the elements below, they
may also be designed and contained in dedicated test management systems, which may even allow
automatic execution of test cases (e.g. regression testing). However, expectations to key elements are
the same.
Test cases should include:
• the version of the software being tested;
• any pre-requisites or conditions prior to conducting the test;
• a description of the steps taken to test the functionality (input);
• the expected result (acceptance criteria).
Test cases should require the tester to document the actual result as seen in the test step, the evidence
if relevant and, if applicable, the conclusion of the test step (pass/fail). Where possible, the tester should
not be the author of the test case. In case of test failure, the potential impact should be assessed and
subsequent decisions regarding the deviations should be documented.
A2.6 Test execution and reporting
Test execution should follow approved protocols and test cases (see section A2.5), the version of the
software being tested should be documented, and where applicable and required by test cases and test
procedures, evidence (e.g. screen shots) should be captured to document test steps and results. Where
relevant, the access rights (role) and the identification of the person or automatic testing tool performing
tests should be documented.
Where previously passed scripts are not retested along with the testing of fixes for previous failing tests,
this should be risk assessed and the rationale should be documented.
Deviations encountered during system validation should be recorded and brought to closure. Any failure
to meet requirements pre-defined to be critical should be solved or mitigating actions should be
implemented prior to deployment. All open deviations and any known issues with the system at the time
of release should be assessed and subsequent decisions should be documented in the validation report
and, if applicable, in the release notes. The validation report should be approved by the responsible party
before release for production.
A2.7 Release for production
The responsible party should sign off the release prior to initial use.
Training materials, user guides and any other resources required for users should be available at the
time of release.
A2.8 User helpdesk
There should be a mechanism to report, record, and solve defects and issues raised by the users e.g.
via a helpdesk. Defects and issues should be fixed in a timely manner.

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 33/52
A2.9 Periodic review
Validation of a system should be maintained throughout the full system life cycle. Periodic system reviews
should be conducted to assess and document whether the system can still be considered to be in a
validated state, or whether individual parts or the whole system needs re-validation.
Depending on the system type and application, the following elements (non-exhaustive list) should be
evaluated and concluded, both individually and in combination:
• changes to hardware/infrastructure;
• changes to operating system/platform;
• changes to the application;
• changes to security procedures;
• changes to backup and restore tools and procedures;
• configurations or customisations;
• deviations (or recurrence thereof);
• performance incidents;
• security incidents;
• open and newly identified risks;
• new regulation;
• review of system accesses;
• updates of agreements with the service provider.
These elements should be reviewed whether the system is hosted by the responsible party or by a
service provider.
A2.10 Change control
There should be a formal change control process. Requests for change should be documented and
authorised and should include details of the change, risk-assessment (e.g. for data integrity, current
functionalities and regulatory compliance), impact on the validated state and testing requirements. For
trial specific configurations and customisations, the change request should include the details of the
protocol amendment if applicable.
As part of the change control process, all documentation should be updated as appropriate (e.g.
requirements, test scripts, training materials, user guide) and a report of the validation activities
prepared and approved prior to release for production. The system should be version controlled.
The responsible party should ensure that any changes to the system do not result in data integrity or
safety issues or interfere with the conduct of an ongoing trial. The investigator should be clearly informed
of any change to a form (e.g. electronic case report form [eCRF] or electronic clinical outcome
assessment [eCOA] page) and it should be clear when such changes were implemented.
The documentation relating to the validation of previous or discontinued system versions used in a clinical
trial should be retained (see 'Guideline on the content, management and archiving of the clinical trial
master file (paper and/or electronic)' [EMA/INS/GCP/856758/2018], section 6.3).

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 34/52
Annex 3 User management
A3.1 User management
Organisations should have a documented process in place to grant, change and revoke system accesses
in a timely manner as people start, change, and end their involvement/responsibility in the management
and/or conduct of the clinical trial projects.
Access to the system should only be granted to trained site users when all the necessary approvals for
the clinical trial have been received and all documentation is in place (e.g. signed protocol and signed
agreement with the investigator). This also applies to any updates to the system, e.g. changes resulting
from a protocol amendment should only be made available to users once it is confirmed that the
necessary approvals have been obtained, except where necessary to eliminate an immediate hazard to
trial participants.
A3.2 User reviews
At any given time, an overview of current and previous access, roles and permissions should be available
from the system. This information concerning actual users and their privileges to systems should be
verified at suitable intervals to ensure that only necessary and approved users have access and that
their roles and permissions are appropriate. There should be timely removal of access no longer required,
or no longer permitted.
A3.3 Segregation of duties
System access should be granted based on a segregation of duties and also the responsibilities of the
investigator and the sponsor, as outlined in ICH E6.
Users with privileged or 'admin access' have extensive rights in the system (operating system or
application), including but not limited to changing any system setting (e.g. system time), defining or
deactivating users (incl. 'admin users'), activate or deactivate audit trail functionality (and sometimes
even edit audit trail information) and making changes to data that are not captured in the audit trail
[e.g. backend table changes in the database(s)]). There is a risk that these privileges can be misused.
Consequently, users with privileged access should be sufficiently independent from and not be involved
in the management and conduct of the clinical trial and in the generation, modification, and review of
data.
Users of computer clients [e.g. personal computer (PC)] which record or contain critical clinical trial data,
should generally not have 'admin access' to the relevant equipment and when this is not the case, it
needs to be justified.
Unblinded information should only be accessible to pre-identified user roles.
A3.4 Least-privilege rule
System access should be assigned according to the least-privilege rule, i.e. users should have the fewest
privileges and access rights for them to undertake their required duties for as short a time as necessary.
A3.5 Individual accounts
All system users should have individual accounts. Sharing of accounts (group accounts) is considered
unacceptable and a violation of data integrity and ICH E6 principles as data should be attributable.

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 35/52
A3.6 Unique usernames
User access should be unique within the system and across the full life cycle of the system. User account
names should be traceable to a named owner and accounts intended for interactive use and those
assigned to human users should be readily distinguishable from machine accounts.

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 36/52
Annex 4 Security
A4.1 Ongoing security measures
The responsible party should maintain a security system that prevents unauthorised access to the data.
Threats and attacks on systems containing clinical trial data and corresponding measures to ensure
security of such systems are constantly evolving, especially for systems and services being provided
over or interfacing the internet.
A4.2 Physical security
Computerised systems, servers, communication infrastructure and media containing clinical trial data
should be protected against physical damage, unauthorised physical access, and unavailability.
The extent of security measures depends on the criticality of the data.
The responsible party should ensure an adequate level of security for data centres as well as for local
hardware such as universal serial bus (USB) drives, hard disks, tablets, or laptops.
At a data centre hosting clinical trial data, physical access should be limited to the necessary minimum
and should generally be controlled by means of two-factor authentication. The data centre should be
constructed to minimise the risk of flooding, there should be pest control and effective measures against
fire, i.e. cooling, and fire detection and suppression. There should be emergency generators and
uninterruptable power supplies (UPS) together with redundant Internet protocol providers. In case of
co-location (see section 6.7 Cloud solutions), the servers should be locked up and physically protected
(e.g. in cages) to prevent access from other clients. Media (e.g. hard disks) should be securely erased
or destroyed before disposal.
Data should be replicated at an appropriate frequency from the primary data centre to a secondary
failover site at an adequate physical distance to minimise the risk that the same fire or disaster destroys
both data centres. A disaster recovery plan should be in place and tested.
A4.3 Firewalls
In order to provide a barrier between a trusted internal network and an untrusted external network and
to control incoming and outgoing network traffic (from certain IP addresses, destinations, protocols,
applications, or ports etc.), firewall rules should be defined. These should be defined as strict as
practically feasible, only allowing necessary and permissible traffic.
As firewall settings tend to change over time (e.g. as software vendors and technicians need certain
ports to be opened due to installation or maintenance of applications), firewall rules and settings should
be periodically reviewed. This should ensure that firewall settings match approved firewall rules and the
continued effectiveness of a firewall.
A4.4 Vulnerability management
Vulnerabilities in computer systems can be exploited to perform unauthorised actions, such as modifying
data or making data inaccessible to legitimate users. Such exploitations could occur in operating systems
for servers, computer clients, tablets and mobile phones, routers and platforms (e.g. databases).
Consequently, relevant security patches for platforms and operating systems should be applied in a
timely manner, according to vendor recommendations.

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 37/52
Systems, which are not security patched in a timely manner according to vendor recommendations,
should be effectively isolated from computer networks and the internet, where relevant.
A4.5 Platform management
Platforms and operating systems for critical applications and components should be updated in a timely
manner according to vendor recommendations, in order to prevent their use in an unsupported state.
Unsupported platforms and operating systems, for which no security patches are available, are exposed
to a higher risk of vulnerability. Validation of applications on the new platforms and operating systems
and of the migration of data should be planned ahead and completed in due time prior to the expiry of
the supported state.
Unsupported platforms and operating systems should be effectively isolated from computer networks
and the internet.
It should be ensured that software used in clinical trials remains compatible with any changes to
platforms/operating systems in order to avoid unintended impact on the conduct/management of the
clinical trial due to interruption of functionality or requirements for alternative software and data
migration.
A4.6 Bi-directional devices
The use of bi-directional devices (e.g. USB devices), which come from or have been used outside the
organisation, should be strictly controlled as they may intentionally or unintentionally introduce malware
and impact data integrity, data availability, and rights of trial participants.
A4.7 Anti-virus software
Anti-virus software should be installed and activated on systems used in clinical trials. The anti-virus
software should be continuously updated with the most recent virus definitions in order to identify,
quarantine, and remove known computer viruses. This should be monitored.
A4.8 Penetration testing
For systems facing the internet, penetration testing should be conducted at regular intervals in order to
evaluate the adequacy of security measures and identify vulnerabilities in system security (e.g. code
injection), including the potential for unauthorised parties to gain access to and control of the system
and its data. Vulnerabilities identified, especially those related to a potential loss of data integrity, should
be addressed and mitigated in a timely manner.
A4.9 Intrusion detection and prevention
An effective intrusion detection and prevention system should be implemented on systems facing the
internet in order to monitor the network for successful or unsuccessful intrusion attempts from external
parties and for the design and maintenance of adequate information technology (IT) security procedures.
A4.10 Internal activity monitoring
An effective system for detecting unusual or risky user activities (e.g. shift in activity pattern) should be
in place.

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 38/52
A4.11 Security incident management
Organisations managing clinical trial data should have and work according to a procedure that defines
and documents security incidents, rates the criticality of incidents, and where applicable, implements
effective corrective and preventive actions to prevent recurrence. In cases where data have been, or
may have been, compromised, the procedures should include ways to report incidents to relevant parties
where applicable. When using a service provider, the agreement should ensure that incidents are
escalated to the sponsor in a timely manner for the sponsor to be able to report serious breaches as
applicable, in accordance with Regulation (EU) No 536/2014.
A4.12 Authentication method
The method of authentication in a system should positively identify users with a high degree of certainty.
Methods should be determined based on the type of information in the system. A minimum acceptable
method would be user identification and a password. The need for more stringent authentication methods
should be determined based on a risk assessment of the criticality of the data and applicable legislation
(including data protection legislation), and generally should include two-factor authentication.
User accounts should be automatically locked after a pre-defined number of successive failed
authentication attempts, either for a defined period of time, or until they are re-activated by a system
administrator after appropriate security checks.
Biometric approaches are currently not specifically addressed by ICH E6. If using biometrics to
authenticate the creation of a signature, the investigator and sponsor should ensure that these fulfil the
above-mentioned requirements and local legal requirements.
A4.13 Remote authentication
Remote access to clinical trial data, e.g. to cloud-based systems, raises specific challenges. The level of
security should be proportionate to the sensitivity and confidentiality of the data (e.g. nominative data
in electronic medical records are highly sensitive) and to the access rights to be granted (read-only,
write or even 'admin' rights). A risk-based approach should be used to define the type of access control
required. Depending on the level of risk, two-factor authentication may be appropriate or necessary.
Two-factor authentication implies that two of the following three factors be used:
• something you know, e.g. a user identification and password
• something you have, e.g. a security token, a certificate or a mobile phone and an SMS pass code
• something you are, e.g. a fingerprint or an iris scan (biometrics)
A4.14 Password managers
A secure and validated password manager, with a unique, robust user authentication each time it is used
to log into a web site or system, can help to create and use different, complex passwords for each site
or system. However, attention should be paid to insufficiently secured password managers.
Password managers built into web browsers may save and automatically fill in user identification and
passwords, regardless of whether an independent secure password manager is used or not. This poses
a risk if uncontrolled equipment is used (e.g. personal equipment, shared equipment or user accounts),
as user access control cannot be enforced; a risk that needs to be effectively mitigated. A policy or
contractual arrangement would not be considered adequate to provide a sufficient level of security in
such situations.

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 39/52
The risk linked to the potential hacking of user equipment or to key loggers should also be considered.
A4.15 Password policies
Formal procedures for password policies should be implemented. The policies should include but not
necessarily be limited to length, complexity, expiry, login attempts, and logout reset. The policies should
be enforced by systems and verified during system validation.
A4.16 Password confidentiality
Passwords should be kept confidential, sharing of passwords is unacceptable and a violation of data
integrity. Passwords initially received from the system or from a manager or system administrator should
be changed by the user on their first connection to the system. This should be mandated by the system.
A4.17 Inactivity logout
Systems should include an automatic inactivity logout, which logs out a user after a defined period of
inactivity. The user should not be able to set the inactivity logout time (outside defined and acceptable
limits) or deactivate the functionality. Upon inactivity logout, a re-authentication should be required (e.g.
password entry).
A4.18 Remote connection
When remotely connecting to systems over the internet, a secure and encrypted protocol (virtual private
network (VPN) and/or hypertext transfer protocol secure (HTTPS)) should be used.
A4.19 Protection against unauthorised back-end changes
The integrity of data should be protected against unauthorised back-end changes made directly on a
database by a database administrator. A method to prevent such changes could be by setting the
application up to encrypt its data on the database or by storing data un-encrypted with an encrypted
copy. In either case, the database administrator should not be identical to the administrator of the
application.

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 40/52
Annex 5 Additional consideration to specific systems
All computerised systems used in clinical trials should fulfil the requirements and general principles
described in the previous sections. The following sub-sections define more specific wording for selected
types of systems where the GCP inspectors’ working group (GCP IWG) has found that supplemental
guidance is needed. For electronic trial master files (eTMFs), please refer to the respective guideline
1
.
A5.1 Electronic clinical outcome assessment
Electronic clinical outcome assessment (eCOA) employs technology in addition to other data acquisition
tools for the reporting of outcomes by investigators, trial participants, care givers and observers. This
guideline does not address the clinical validation or appropriateness of particular eCOA systems. The
guideline aims at addressing the topics specifically related to these eCOA systems and also to those
related to the situation where bring-your-own-device (BYOD) solutions are used.
Data can be collected by any of several technologies and will be transferred to a server. Data should be
made available to involved/responsible parties such as the investigator e.g. via portals, display of source
data on the server, generation of alerts and reports. These processes should be controlled and clearly
described in the protocol (high-level) and protocol-related documents, and all parts of the processes
should be validated.
Collecting data electronically may offer more convenience to some trial participants and may increase
participant compliance, data quality, reduce variability, reduce the amount of missing data (allowing
automatic reminders) and potentially reduce data entry errors. Of importance, whilst use of such
measures might be of benefit to some trial participants and patient groups, it may be inconvenient for
or even result in the exclusion of others. This should be considered when using any data acquisition tool
and the choice should be justified.
A5.1.1 Electronic patient reported outcome
A5.1.1.1
System design
Electronic patient reported outcome (ePRO) should be designed to meet the specific needs of the end
users. It is recommended to involve representatives of intended site staff and of the intended trial
participant population, where relevant, in the development and testing.
One of the advantages of using an ePRO system is that the timestamps of data entry are recorded. The
timestamp should record the time of the data entry and not only the time of the data
submission/transmission.
Trial participants should be able to view their own previously entered data, unless justified and unless it
is against the purpose of the clinical trial design or the protocol. Therefore, the period that data are
viewable by the participant should be considered when designing/configuring the ePRO. Decisions about
the 'view-period' should be based on considerations regarding risk for bias on data to be entered. If
viewing of recently entered data is not possible by the participant, then there is a risk that the participant
could forget if relevant data have been collected. This is especially the case if the planned entry is event-
driven. In addition, this prevents an unnecessary burden to site staff, as they will be contacted by trial
participants in case of doubt less often.
Logical checks should be in place to prevent unreasonable data changes such as 'time travel' e.g. going
back (months, years in time) or forward into the future based on the protocol design.
1
Guideline on the content, management and archiving of the clinical trial master file (paper and/or electronic)
(EMA/INS/GCP/856758/2018
).

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 41/52
It should be considered to include a scheduling/calendar component with alerts or reminders to assist
compliance.
A5.1.1.2 Data collection and data transfer
The same ICH E6 standards apply to data collected via ePRO as to any other method of data collection,
i.e. that there are processes in place to ensure the quality of the data, and that all clinical information is
recorded, handled and stored in such a way as to be accurately reported, interpreted and verified.
An ePRO system typically requires an entry device. Data saved on the device is the original record created
by the trial participant. Since the data stored in a temporary memory are at higher risk of physical loss,
it is necessary to transfer the data to a durable server at an early stage, by a validated procedure and
with appropriate security methods during data transmission. Data should be transferred to the server
according to a pre-defined procedure and at pre-defined times. The data saved on the device are
considered source data. After the data are transferred to the server via a validated procedure, the original
data can be removed from the device as the data on the server are considered certified copies. The
sponsor should identify the source data in the protocol and protocol-related documents and should
document the time and locations of source data storage.
In addition to the general requirements on audit trails (please refer to section 6.2.), if an ePRO system
is designed to allow data correction, the data corrections should be documented, and an audit trail should
record if the data saved on the device are changed before the data are submitted.
Data loss on devices should be avoided. Procedures should be in place to prevent data loss if web access
to the trial participant reported data is interrupted, (e.g. server outage, device battery drained, loss of
or unstable internet connection). There should be a procedure in place to handle failed or interrupted
data transmission.
It should be ensured/monitored that the transmission of data from ePRO devices is successfully
completed.
Important actions should be time-stamped in an unambiguous way, e.g. data entries, transfer times and
volume (bytes).
A5.1.1.3 Investigator access
Unlike data collected in the electronic case report form (eCRF), ePRO data are not managed (although
available for review) by the investigator and are often hosted by a service provider. The investigator is
overall responsible for the trial participants’ data (including metadata). Those should consequently be
made available to the investigator in a timely manner. This will allow the investigator to fulfil their
responsibilities for oversight of safety and compliance and thereby minimise the risk of missed adverse
events or missing data.
A5.1.1.4 Data changes
As stated in section 6.2.1. on audit trails, a procedure should be in place to address and document if a
data originator (e.g. investigator or trial participant) realises that they have submitted incorrect data by
mistake and want to correct the recorded data.
Data changes for ePRO typically differ from that of other data acquisition tools because trial participants
typically do not have the possibility to correct the data in the application. Hence, procedures need to be
in place in order to implement changes when needed. This depends on the design of tools and processes
and could be in the form of data clarification processes initiated by trial participants on their own reported
data or initiated by investigators.

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 42/52
Data reported should always be reliable. Data clarification procedures introduced by the sponsor or
service provider, whether or not described in the protocol should not prohibit changes in trial participant
data when justified e.g. if the trial participant realises that the data have not been entered correctly.
It is expected that the possibility for changes is implemented based on a justified and trial specific risk-
assessment and that any changes are initiated in a timely manner by the participant or site staff and in
case of the latter is based on a solid source at investigator sites e.g. phone notes or emails from trial
participants documenting the communication between sites and trial participants immediately after the
error was made/discovered.
One of the advantages of direct data entry by the trial participant is that recall bias is minimised as the
data are entered contemporaneously. Consequently, corrections should not be done at a much later
stage without good reason and justification. Whether collected on paper or by electronic means, the
regulatory requirements are that all clinical data should be accurately reported and should be verifiable
in relation to clinical trials.
It is expected that the number of changes to ePRO data are limited; however, this requires both designs
of ePROs that are appropriate to ensure proper understanding by trial participants and appropriate
training of trial participants, thereby avoiding entry errors.
A5.1.1.5 Accountability of devices
There should be an accountability log of devices handed out to trial participants and this should include
the device identification number in order to be reconciled to a particular trial participant.
A5.1.1.6 Contingency processes
Contingency processes should be in place to prevent loss of data critical for participant safety or trial
results. In case of device malfunction or loss of devices, there should be a procedure in place to replace
the device and to merge data from several devices of a trial participant without losing traceability.
A5.1.1.7 Username and password
The trial participant’s passwords should only be known to the trial participant.
The username and password should not be used in a manner that would breach a trial participant’s
confidentiality.
In relation to BYOD, sponsors should ensure that basic user access controls are implemented. When
mobile applications are used for data entry, access controls need to be in place to ensure attributability.
See section A5.1.3 for further guidance on BYOD.
A5.1.1.8 Training
Training should be customised to meet the specific needs of the end users.
A5.1.1.9 User support
Support to the trial participant and the trial site staff should be readily available (e.g. support via phone
or email) in order to ensure reliable data and minimise the risk of data loss. Trial participant
confidentiality should be ensured at all times, including in the communication process.
Procedures for service desk, user authentication and access restoration should be implemented.

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 43/52
A5.1.2 Clinician reported outcome
Tools to directly collect clinician reported outcomes should generally follow the same requirements as
those described for systems in general and for ePROs. The main difference is the user (investigators,
other clinicians, or independent assessors instead of trial participants), not the system requirements.
Special attention should be given to access control in order to avoid jeopardising any blinding, when
relevant.
A5.1.3 Bring your own device
Both ePRO data and clinician reported outcome data may be captured by privately owned devices such
as mobile phones, tablets, computers and wearables, i.e. BYOD. This can either be achieved via a web-
application with pre-installed browser applications or by installing an application on the device. Solutions
can be either a combination of web and application (hybrid) or coded to the device operating system
(native).
It is necessary to provide alternative ways of data collection e.g. devices provided by the sponsor, as
the trial participants should not be excluded from a trial if not capable of or willing to use BYOD.
A5.1.3.1 Technical and operational considerations
When using BYOD, a variety of devices, operating systems and where applicable web browsers commonly
used, should be considered for the application. It should be ensured that it is not exclusive to one model
or operating system.
The sponsor should describe the minimum technical specifications for participants’ devices (e.g.
operating system, web browser and storage capacity). These should take into account which operating
systems are still supported by the manufacturer and if bug fixes and security patches have been released,
when relevant.
The sponsor should ensure the quality and integrity of the data across all accepted models and versions.
The sponsor has no control over the implementation of updates to the operating system or over the
applications on the trial participant’s device. These aspects should be taken into consideration in their
risk evaluation and subsequent validation activities.
The application should use an external source for date and time and should not rely on information from
the user's device.
Procedures and processes should be in place for when the trial participant discontinues the clinical trial
or the clinical trial ends and access to applications and data collection should be terminated.
A5.1.3.2 Considerations on security and trial participant confidentiality
The confidentiality of data that could identify trial participants should be protected, respecting the privacy
and confidentiality rules in accordance with the applicable regulatory requirements.
A number of challenges for BYOD are related to security, and security should be ensured at all levels
(mobile device security, data breach security, mobile application security, etc.). As mobile devices may
be lost or stolen and it cannot be ensured that the trial participants use any authentication methods to
secure their device, access control should be at the application level. Section A.4.14 on the use of
password managers also applies.
Risks linked to known application and operating system vulnerabilities should be minimised.

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 44/52
The hardware, operating system and applications are all factors that affect the total security status of
the device, and there should be procedures in place regarding e.g., when trial participants/clinicians use
less secure devices.
Data capture by BYOD may require the device to be identified to ensure data attributability. Only
information that is needed for proper identification of and service to the user should be obtained. Trial
participant confidentiality should be ensured if device identification information is stored. Access to the
application and trial participant data may be protected with multiple barriers (e.g. unlock mobile phone,
open application, access data).
If the device’s built-in capabilities for auto fill formula data and/or using photo, video, and global
positioning system (GPS) data, etc. are used, this should be described and justified in the protocol.
Procedures and processes should ensure that only protocol mandated data are collected, and that the
confidentiality of data is maintained. In accordance with the principle of 'data minimisation' mobile
applications should only collect data that are necessary for the purposes of the data processing and not
access any other information on the person’s device. For example, location data should only be collected
if it is necessary for the clinical trial activities and the trial participant must be informed about it in the
patient information and agree to it in the consent form.
Providers may have end-user licensing agreements or terms of service that allow the sharing of data.
This may be in conflict with ICH E6 and (local) legal requirements or require information to be provided
to the participant and may require specific informed consent. In some cases, the application may not be
suitable for use. If an application is to be installed on a BYOD, the privacy labels/practices (e.g. regarding
tracking data, linked and not linked data) should be clearly communicated to the trial participant upfront.
The sponsor should be aware that explicit consent may be required related to the above. The informed
consent should describe the type of information that will be collected via ePRO and how that information
will be used.
A5.1.3.3 Installation and support
When using an application, it is recommended that appropriately trained staff assist in the installation
even if the application is available through an app-store or service provider platform.
Independently of whether the BYOD solution is based on an application installed on the device or a
website/web application, the software and the use should be explained thoroughly via targeted training,
which may include user manuals, one-to-one training, and multimedia tools. Users of the system should
have access to user support e.g. from a help desk. There should be a procedure in place in case an
application cannot be installed, or the web service is unavailable on a device, if the device has
malfunctioned or the participant has purchased a new device. Helpdesk contacts by users should be
logged (participant or site staff study ID, purpose of contact, etc.) with due consideration of protecting
participant information.
The software and software installation should not limit or interfere with the normal operations of the
device. Any unavoidable limitation to the device after installation should be part of the informed consent
material.
A5.1.3.4 Uninstallation
It should be possible to uninstall software or applications without leaving residues on BYOD devices, e.g.
entries in the registry, incorrect mappings or file fragments. The user should be able to uninstall at any
time without expertise or assistance. The uninstallation process should not compromise the device.

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 45/52
A5.2 Interactive response technology system
A5.2.1 Testing of functionalities
In addition to the content of the sections A2.6, A2.10, of this guideline, sponsors should also consider
the issues mentioned below when writing test scripts for user acceptance tests (UAT).
A5.2.1.1 Dosage calculations
Where dosage calculations/assignments are made by the IRT system based on user entered data (e.g.,
trial participant body surface area or weight), and look-up tables (dosage assignment based on trial
participant parameters), the tables should be verified against the approved protocol and input data used
to test allocations, including test data that would be on a borderline between differing doses. Assigning
the incorrect dosage to a trial participant is a significant risk to safety and well-being and such inaccurate
assignments should be thoroughly mitigated.
A5.2.1.2 Stratified randomisation
Where the randomisation is stratified by factors inputted by the user, all the combinations of the strata
should be tested to confirm that the allocation is occurring from the correct randomisation table.
A5.2.1.3 Blinding and unblinding
Unblinded information should only be provided and accessible to pre-identified user roles.
A5.2.2 Emergency unblinding
The process for emergency unblinding should be tested. A backup process should also be in place in case
the online-technology emergency unblinding is unavailable.
It should be verified that a site’s ability for emergency unblinding is effectively available before
administering IMP to a trial participant.
A5.2.3 IRT used for collection of clinical data from the trial site
Where the IRT system is collecting clinical data, important data should be subject to source data
verification and/or reconciliation with the same data collected in the data acquisition tool. For example,
the data used for stratification may also be contained in the data acquisition tool. Where clinical data is
entered into the IRT system and integrated in the electronic data collection (EDC) system (electronic
data transfer to EDC) the additional functionality and ICH E6 requirement concerning data acquisition
tools (eCRFs) should be addressed in the IRT system requirements and UAT e.g. investigator control of
site entered data, authorisation of data changes by the investigator, authorisation of persons
entering/editing data in the system by the investigator.
A5.2.4 Web-based randomisation
Where justified, sponsor or investigator/sponsor may also use a web-based application to create
randomisation lists for clinical trials. When using a web-service, the process to evaluate the suitability of
the system and GCP compliance as well as the fitness for purpose of the created randomization list should
be documented. The version of the service used, and where applicable, the seed should be maintained.
Ad hoc randomization via a web-service is not recommended as randomization distribution is unknown,
the sponsor is not in control of the process e.g. the seed may vary.

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 46/52
The sponsor should ensure that the process of randomisation can be reconstructed via retained
documentation and data and that a final randomisation schedule is retained.
A5.3 Electronic informed consent
Ethics committees will review all material related to the informed consent process. Before the
implementation of an electronic consent procedure is considered, the sponsor should ensure that the
electronic consent procedure is GCP compliant and legally acceptable in accordance with the
requirements of the independent ethics committees concerned and of the national regulatory authorities.
The principles of consent as set out in legislation and guidance should be the same regardless of whether
the process involves a computerised system. A hybrid approach could be considered, where national
requirements preclude cern parts of an electronic informed consent procedure. At present, in some
countries failure to provide 'written on paper' proof of a trial participant’s informed consent is considered
a legal offense.
An electronic informed consent refers to the use of any digital media (e.g. text, graphics, audio, video,
podcasts or websites) firstly to convey information related to the clinical trial to the trial participant and
secondly to document informed consent via an electronic device (e.g. mobile phones, tablets or
computers). The electronic informed consent process involves electronic provision of information, the
procedure for providing the opportunity to inquire about details of the clinical trial including the answering
of questions and/or electronic signing of informed consent. For example, it would be possible for the trial
participant to sign informed consent on a paper form following provision of the information electronically
or the information and informed consent could be entirely electronic. If using a ‘wet ink’ signature
together with an electronic informed consent document (a hybrid approach), the patient information, the
informed consent document and the signature should be indisputably linked.
The method of obtaining an informed consent should ensure the broadest possible access to clinical
trials. Alternative methods for provision of information and documentation of informed consent should
be available for those unable or unwilling to use electronic methods. Any sole use of electronic informed
consent should be justified and described in the protocol.
A5.3.1 Provision of information about the clinical trial
The trial participants should have been informed of the nature, objectives, significance, implications, the
expected benefit, risks, and inconveniences of the clinical trial in an interview with the investigator, or
another member of the investigating team delegated by the principal investigator. The interview should
take into account the individual disposition (e.g. comorbidities, patient references, etc.) of the potential
participant (or legal representative). This interview should allow interaction, the asking of questions and
allow confirmation of the trial participant’s identity and not just simply the provision of information. The
interview should be conducted in person or, it could be done remotely where this can be justified and is
allowed nationally and if approved by an ethics committee using electronic methods that allow for two-
way communication in real time. Whichever method is used it is important that confidentiality is
maintained, and therefore communication methods should be private/secure. Consideration should be
given as to how the system would be presented to the ethics committee for approval so that it captures
the functionality of the system and the experience of the potential trial participant using it. Direct system
access should be provided to the ethics committee upon request in a timely manner.
Provision of the information electronically may improve the trial participants’ understanding of what
taking part in the clinical trial will involve. Computerised systems could facilitate features to assess the

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 47/52
participant’s understanding e.g. via questions at key points, which self-evaluate trial participants'
understanding as they work their way through the information. This, in turn, can be used to highlight
areas of uncertainty to the person seeking consent so that they can cover this area in more detail with
the trial participant.
A5.3.2 Written informed consent
The informed consent of the trial participant should be in writing and electronic methods for documenting
the trial participant’s informed consent should ensure that the informed consent form is signed and
personally dated by at least two (natural) persons; the trial participant or the trial participant’s legal
representative, and the person who conducted the informed consent discussion. The identity of the
persons signing should be ensured.
The method used to document consent should follow national legislation with regard to e.g. acceptability
of electronic signatures (see section 4.8.), and in some countries 'wet ink' signature will be required.
There should be no ambiguity about the time of signature. The system should use timestamps for the
audit trail for the action of signing and dating by the trial participant and investigator or qualified person
who conducted the informed consent interview, which cannot be manipulated by system settings. Any
alterations of the document should invalidate the electronic signature.
If an electronic signature is used, it should be possible for monitors, auditors, and inspectors to access
the signed informed consent forms and all information regarding the signatures, including the audit trail.
Secure archiving should ensure availability and legibility for the required retention period.
A5.3.3 Trial participant identity
It should always be possible to verify the identity of a trial participant with documentation available to
the investigator. Documentation which makes it possible to demonstrate that the person entering the
electronic 'signature' was indeed the signatory, is required. The electronic signing should be captured by
the audit trail.
Where consent is given remotely, and the trial participant is required at some point to visit a clinical trial
site for the purposes of the trial, verification should be done in person e.g. by using information from an
official photo identification if such an ID document is required in the trial site country.
A5.3.4 Sponsor notification on the consent process
Notification to the sponsor should only contain essential, non-personal identifiable information to allow
the sponsor to have an overview of how many trial participants have been enrolled in a clinical trial so
far and which versions of the electronic informed consent form have been used. Remote access to
personal identifiable information in the electronic system should only be permitted for the corresponding
participant, legal representative, investigator, monitor, auditor, or inspector. Any unjustified accesses,
which lead to the disclosure of non-pseudonymised information, are likely to be viewed as an
infringement of data privacy laws.
A5.3.5 Trial participant confidentiality
As for all other computerised systems in clinical trials, the confidentiality of data that could identify trial
participants should be protected, respecting the privacy and confidentiality rules in accordance with
applicable national and EU regulatory requirements.

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 48/52
A5.3.6 Trial participant access
Potential trial participants (or, where applicable, their legal representative) should be provided with
access to written information about the clinical trial prior to seeking their informed consent. The trial
participant should be provided with their own copy of the informed consent documentation (including all
accompanying information and all linked information) once their consent has been obtained. This includes
any changes to the data (documents) made during the process.
The information about the clinical trial should be a physical hard copy or electronic copy in a format that
can be downloaded. The copy should be available immediately to the trial participant.
A5.3.7 Investigator responsibilities
The investigator should take appropriate measures to verify the identity of the potential trial participant
(see section A5.3.3) and ensure that the participant has understood the information given. The informed
consent documents are essential documents that should be available at the trial site in the investigator
TMF for the required retention period (see section A5.3.9). The investigator should retain control of the
informed consent process and documentation (e.g. signed informed consent forms) and ensure that
personal identifiable data are not inappropriately disclosed beyond the site. The system used should not
limit the investigator’s ability to ensure that trial participants’ confidentiality is protected with appropriate
access and retention controls in the system. The investigator should ensure an appropriate process for
the copy of the informed consent documentation (information sheet and signed consent form) to be
provided to the trial participant. All versions of signed and dated electronic consents should be available
to the trial participant for the duration of and after the trial. The system used should ensure that the
investigator can grant and revoke access to the electronic informed consent system to monitors, auditors
and regulatory authority inspectors.
A5.3.8 Version control and availability to sites
The electronic informed consent information (electronic trial participant information and informed
consent form) may be subject to updates and changes during the course of the trial. Regardless of the
nature of the change or update, the new version containing relevant information has to receive the
favourable opinion/approval of the ethics committee(s) prior to its use. Additional information should be
made available to the ethics committee(s) concerning technical aspects of the electronic informed
consent procedure to ensure continued understanding of the informed consent processes. Only versions
approved by the ethics committee(s) should be enabled and used for the informed consent process and
documentation. Release of electronic trial participant information and informed consent forms to the
sites prior to IRB/IEC approval should be prevented. The system should prevent the use of obsolete
versions of the information and informed consent document.
A5.3.9 Availability in the investigator’s part of the trial master file
All documents of the informed consent procedure (including all accompanying information and all linked
information) are considered to be essential documents and should be archived as such. Replacement of
the documents with copies is only acceptable if the copies are certified copies (see section 6.5.).
A5.3.10 Withdrawal from the trial
There should be procedures and processes in place for a trial participant to be able to withdraw their
consent. If there is a possibility for the trial participant to withdraw from the trial through the
computerised system, it should be ensured that such a withdrawal of consent generates an alert to the
investigator in order to initiate the relevant steps as per protocol and according to the extent of

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 49/52
withdrawal. Any withdrawal of informed consent should not affect the results of activities already carried
out, such as the storage and use of data obtained on the basis of informed consent before withdrawal.

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 50/52
Annex 6 Clinical systems
As stated in sections 2. and 4.6., computerised systems implemented at the trial site are also within the
scope of this guideline, and the general approach towards computerised systems used in clinical practice
is that the decision to use a system in a clinical trial should be risk proportionate and justified pre-trial.
This section is dedicated to specific and additional considerations regarding electronic medical records
and other systems implemented at sites, which are primarily used in clinical practice but are also
generating clinical trial data.
For computerised systems built specifically for data collection in clinical trials please refer to the relevant
sections of this guideline.
A6.1 Purchasing, developing, or updating computerised systems by sites
The investigator/institution should have adequate facilities for a clinical trial. This also applies to the
computerised systems of the institution if considered to be used for clinical trial purposes. It is
recommended that institutions planning to perform clinical trials consider whether system functionality
is fit for the clinical trial purpose. This should also be considered prior to the introduction of a new
electronic medical record or equipment planned to be used in clinical trials (e.g. scanners, X-ray,
electrocardiograms), or prior to changes to existing systems.
To ensure that system requirements related to GCP compliance (e.g. audit trail for an electronic medical
record) are addressed, experienced clinical trial practitioners should be involved by the institution in the
relevant steps of the procurement and validation processes.
As many systems are designed with different configuration options, it should be ensured that the systems
are configured in a GCP compliant manner.
A6.2 Site qualification by the sponsor
As part of the site qualification, the sponsor should assess the systems in use by the
investigator/institution to determine whether the systems are fit for their intended use in the clinical trial
(e.g. include an audit trail). The assessment should cover all computerised systems used in the clinical
trial and should include consideration of the rights, safety, dignity and wellbeing of trial participants and
the quality and integrity of the trial data.
If the systems do not fulfil the requirements, the sponsor should consider whether to select the
investigator/institution. The use of systems not fulfilling requirements should be justified, either based
on planned implementation of effective mitigating actions or a documented impact assessment of
residual risks.
A6.3 Training
If the use of the systems in the context of a specific trial is different from the use in clinical practice e.g.
different scanning procedures, different location of files, different requirements regarding documentation
etc., trial specific training is required.
A6.4 Documentation of medical oversight
The investigator should be able to demonstrate their medical oversight of the clinical trial when electronic
medical records are used. Where all or part of the entries into the medical records are made by a research
nurse/dedicated data entry staff it can be difficult to reconstruct the investigator's input. The system

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 51/52
should allow the investigator to document the assessment and acknowledgement of information entered
into the system by others.
A6.5 Confidentiality
Pseudonymised copies of electronic medical records may be provided to sponsors, or service providers
working on their behalf, outside the clinical environment e.g. if needed for endpoint adjudication or safety
assessments according to the protocol. National regulations need to be followed by the sites. In such
cases there should be:
• procedures in place at the site to redact copies of medical records, in order to protect the trial
participants' identity, before transfer;
• security measures in place, which are relevant to the process, including pseudonymisation and
redaction;
• a copy of the pseudonymised records and a proof of the transfer made at the site;
• organisational and technical procedures in place on the receiving side to ensure that the
requirements of the data protection regulation are met.
Due to the sensitive nature of information documented in medical records, the extent to which sponsors
request these data should be ethically and scientifically justified and limited to specific critical
information. Any planned collection of redacted copies of medical records by the sponsor should be
described in the protocol, or related documents, and should be explicit in the patient information.
A6.6 Security
Security measures that prevent unauthorised access to data and documents should be maintained.
Please refer to section 5.4. regarding more details on the general requirements for security systems,
which are equally applicable to research institutions.
A6.7 User management
Robust procedures on user management should be implemented (see Annex 3).
For systems deployed by the investigator/institution, the investigator should ensure that individuals have
secure and attributable access appropriate to the tasks they are delegated to in the trial.
Robust processes for access rights are particularly important in trials where parts of the information
could unblind the treatment. Such information should only be accessible to unblinded staff.
A6.8 Direct access
Sponsor representatives (monitors and auditors) and inspectors should have direct, read-only access to
all relevant data for all trial participants as determined by the monitors, auditors or inspectors while
taking the collected data and the clinical trial protocol into account. This may require access to several
different sections or modules of the respective (medical) record e.g. imaging. This requires the use of a
unique identification method e.g. username and password.
The access of monitors, auditors and inspectors should be restricted to the trial participants (including
potential participants screened but not enrolled in the trial) and should include access to audit trails.

Guideline on computerised systems and electronic data in clinical trials
EMA/INS/GCP/112288/2023
Page 52/52
If the site has accepted to provide remote access, appropriate security measures and procedures should
be in place to support such access without jeopardising patient rights and data integrity and national
legislation.
A6.9 Trial specific data acquisition tools
The electronic medical record contains information, which is crucial for the management of patients and
are designed to fulfil legal requirements.
Any trial specific data acquisition tools implemented cannot replace the medical record and their use
should not result in a depletion of relevant information in the medical record.
Monitoring activities should not be limited to information in the data acquisition tools and should also
consider relevant information in the medical record.
Please also refer to the published qualification opinion on eSource Direct Data Capture (DDC)
EMA/CHMP/SAWP/483349/2019.
A6.10 Archiving
Appropriate archiving should be in place to ensure long term readability, reliability, retrievability of
electronic data (and metadata), in line with regulatory retention requirements. Please also refer to
section 6.11. Requirements for the retention of clinical trial data and documents are frequently different
from requirements for other data and documents held by the investigators. It should be ensured that
there is no premature destruction of clinical trial data in case of e.g. institution relocation or closure. It
is the responsibility of the sponsor to inform the hospital, institution or practice as to when these
documents will no longer need to be retained.
There are specific requirements for backup, etc. of electronic data, which can be seen in section 6.8 and
which are equally applicable to research institutions. Please also refer to the guideline on the content,
management and archiving of the clinical trial master file (paper and/or electronic)
EMA/INS/GCP/856758/2018.
