DATA COLLECTION SURVEY
ON
UNIVERSAL HEALTH COVERAGE
IN
THE PHILIPPINES
DECEMBER 2016
JAPAN INTERNATIONAL COOPERATION AGENCY (JICA)
GLOBAL LINK MANAGEMENT, INC.
HM
JR
16-077
Exchange Rate
US$ 1 = ¥ 104.76
1 Philippine Peso = ¥ 2.16
(JICA Rate in November 2016)

i
LIST OF ACRONYMS/ABBREVIATIONS
Acronyms/
Abbreviations
Standard Nomenclature
ADB
Asian Development Bank
ANC
Antenatal Care
ANC01
Antenatal Care Package
AOP
Annual Operational Plan
ARMM
Autonomous Region in Muslim Mindanao
BEmONC
Basic Emergency Maternal Obstetrics and Newborn Care
BHS
Barangay Health Station
BHW
Barangay Health Worker
BMC
Bicol Medical Center
BRTTH
Bicol Regional Training and Teaching Hospital
CAR
Cordillera Administrative Region
CCT
Conditional Cash Transfer
CEmONC
Comprehensive Emergency Maternal Obstetrics and Newborn Care
CHT
Community Health Team
CHTF
Common Health Trust Fund
CS
Camarines Sur
DBM
Department of Budget and Management
DHS
Demographic and Health Survey
DMO
Development Management Officer
DOF
Department of Finance
DOH
Department of Health
DSWD
Department of Social Welfare and Development
EU
European Union
EVRMC
Eastern Visayas Regional Medical Center
FBD
Facility-based Delivery
FGD
Focus Group Discussions
FHSIS
Field Health Service Information System
FIES
Family Income and Expenditure Survey
GDP
Gross Domestic Product
GIDA
Geographically Isolated and Disadvantaged Areas
GNI
Gross National Income
GSIS
Government Service Insurance System
HMO
Health Maintenance Organization
ILHZ
Inter-Local Health Zone
IRA
Internal Revenue Allotment
IT
Information and Technology
I3QUIP
The Impact of Incentives and Information on Quality and Utilization in
Primary Care
JICA
Japan International Cooperation Agency
KII
Key Informant Interview
KOICA
Korea International Cooperation Agency
KP
Kalusugan Pangkalahatan
LGC
Local Government Code 1991
IMR
Infant Mortality Rate
LGU
Local Government Unit
LHSD
Local Health Support Division
LIPH
Local Investment Plan for Health
MCH
Maternal and Child Health

ii
Acronyms/
Abbreviations
Standard Nomenclature
MCP
Maternal Care Package
MDGs
Millennium Development Goals
MDR
Medical Data Record
MMR
Maternal Mortality Ratio
MNCHN/FP
Maternal, Neonatal, Child Health and Nutrition/ Family Planning
MNDR
Maternal and Newborn Death Review
MSW
Medical Social Worker
NBB
No Balance Billing
NCP
Newborn Care Package
NDHS
National Demographic and Health Survey
NEDA
National Economic and Development Authority
NGO
Non-Governmental Organization
NHIP
National Health Insurance Program
NHTS-PR
National Household Targeting System for Poverty Reduction
NSD
Normal Spontaneous Delivery
OBGYN
Obstetrics and Gynecology
ODA
Official Development Assistance
PCB1
Primary Care Benefit 1
PCPT
Per Capita Poverty Threshold
PhilHealth
The Philippine Health Insurance Corporation
PHRD
Policy and Human Resources Development
PI
Poverty Incidence
PMRF
PhilHealth Member Registration Form
PMT
Proxy Means Test
PNC
Postnatal Care
POC
Point of Care
PSPI
Population Services Philipinas, Inc.
PRISM2
The Private Sector Mobilization for Family Health Project – Phase 2
PSA
Philippine Statistics Authority
RHMPP
Rural Health Midwives Replacement Program
RHU
Rural Health Unit
SAEs
Small Area Estimates
SBA
Skilled Birth Attendant
SDGs
Sustainable Development Goals
SDN
Service Delivery Network
SSS
Social Security System
SSV
Supportive Supervision
TBA
Traditional Birth Attendant
TCL
Target/ Client List
TseKaP
Tamag Serbisyo para sa Kalusugan ng Pamilya
UHC
Universal Health Coverage
UNFPA
United Nations Population Fund
UNICEF
United Nations Children’s Fund
USAID
United States Agency for International Development
WHO
World Health Organization
ZFF
Zuelling Family Foundation
iii
DATA COLLECTION SURVEY
ON UNIVERSAL HEALTH COVERAGE
IN THE PHILIPPINES
TABLE OF CONTENTS
List of Acronyms/Abbreviations ................................................................................................ i
Table of Contents ...................................................................................................................... iii
Attachments ................................................................................................................................v
List of Figures, Tables and Boxes ..............................................................................................v
Executive Summary ...................................................................................................................1
Chapter 1 Overview of the Survey ..........................................................................................2
1-1 Background ...................................................................................................................2
1-2 Objectives .....................................................................................................................3
1-3 Scope of the Survey ......................................................................................................3
1-4 Survey Areas .................................................................................................................4
1-5 Methodology .................................................................................................................5
(1) Literature review ...................................................................................................5
(2) Field data collection ..............................................................................................5
1-6 Survey Team .................................................................................................................8
1-7 Survey Schedule ............................................................................................................8
Chapter 2 Socio-Economic Situation in the Philippines ...................................................... 10
2-1 Geography, Ethnicity and Religion ............................................................................. 10
2-2 Population Statistics and Future Projections ............................................................... 10
2-3 Poverty and Economic Disparity ................................................................................. 13
2-4 Industrial Structure and Labor Market ........................................................................ 15
Chapter 3 Overview of the Health Sector ............................................................................ 16
3-1 Health System with a Focus on Maternal and Child Health ........................................ 16
(1) Health Governance ............................................................................................. 16
(2) Health Policies .................................................................................................... 17
(3) Health Financing ................................................................................................. 20
(4) Health Facilities and MCH Service Delivery ...................................................... 31
(5) Health-related Information .................................................................................. 33
3-2 Maternal and Child Health Conditions ........................................................................ 35
(1) Maternal conditions ............................................................................................ 35
(2) Child mortality .................................................................................................... 36
(3) Teenage Pregnancy ............................................................................................. 36
iv
3-3 Assistance of Development Partners ........................................................................... 37
(1) Development Partners in the Philippine Health Sector ....................................... 37
(2) Trends of the Assistance by Development Partners in the Philippine Health
Sector .................................................................................................................. 38
(3) Details of Assistance by Development Partners .................................................. 39
Chapter 4 National Health Insurance Program (NHIP) – Overview and Utilization ............ 51
4-1 Current Framework of NHIP ....................................................................................... 51
4-2 PhilHealth ................................................................................................................... 51
4-3 Goals for the Philippine Health Agenda ...................................................................... 52
4-4 Membership Category ................................................................................................. 52
4-5 Enrollment Procedures ................................................................................................ 54
4-6 Premium Contributions ............................................................................................... 55
4-7 Payment Mechanisms .................................................................................................. 56
4-8 Benefit Packages ......................................................................................................... 57
(1) Inpatient Benefit Package ................................................................................... 57
(2) Outpatient Benefit Package ................................................................................. 58
(3) Z Benefit Package ............................................................................................... 59
(4) MDG related package ......................................................................................... 60
4-9 Claim Procedures ........................................................................................................ 62
4-10 Accreditation Processes............................................................................................... 63
(1) Health Facilities .................................................................................................. 63
(2) Professionals ....................................................................................................... 64
4-11 Funding for PhilHealth ................................................................................................ 64
4-12 Cross Subsidy among PhilHealth members ................................................................. 65
4-13 Enrollment and Utilization .......................................................................................... 66
(1) Population Coverage ........................................................................................... 66
(2) NHIP Utilization ................................................................................................. 67
4-14 Supporting Indigents ................................................................................................... 67
(1) Facilitating Enrollments for Indigent Members .................................................. 67
(2) No Balance Billing Policy................................................................................... 68
(3) Point-of-Care Enrollment Program ..................................................................... 69
(4) Conditional Cash Transfer .................................................................................. 70
Chapter 5 Maternal and Child Health Services in Bicol and Eastern Visayas Regions ... 73
5-1 Bicol Region (Region V) ............................................................................................. 73
(1) Regional Profile .................................................................................................. 73
(2) Overview of Study Sites ..................................................................................... 75

v
(3) Study Findings .................................................................................................... 76
5-2 Eastern Visayas (Region VIII) ..................................................................................... 87
(1) Regional Profile .................................................................................................. 87
(2) Field Study .......................................................................................................... 91
(3) Study Findings .................................................................................................... 93
Chapter 6 Good Practices and Challenges of JICA Projects ............................................ 107
6-1 Surveyed Projects ...................................................................................................... 107
6-2 Interview Sites........................................................................................................... 107
6-3 Survey Findings ........................................................................................................ 108
(1) Good Practices .................................................................................................. 108
(2) Challenges ........................................................................................................ 111
Chapter 7 Recommendations for JICA’s Future Assistance ............................................ 113
7-1 Points to be Considered ............................................................................................. 113
7-2 Recommendations for JICA’s future activities .......................................................... 113
(1) Access to Quality Essential Health-Care Services ............................................ 113
(2) Financial Risk Protection .................................................................................. 116
7-3 Project Sites .............................................................................................................. 118
7-4 Enhancement of Project Up-scaling Mechanism ....................................................... 118
ReferenceS 120
ATTACHMENTS
1. The Schedule of the First Field Survey (Manila) ....................................................... A-1
2. The Schedule of the Second Field Survey (Bicol) ...................................................... A-2
3. The Schedule of the Second Field Survey (CAR & Eastern Visayas) ........................ A-3
4. The Schedule of the Third Field Survey (Manila) ...................................................... A-5
5. The LGU Health Score Cards .................................................................................... A-6
6. Family Assessment Form ........................................................................................... A-8
LIST OF FIGURES, TABLES AND BOXES
CHAPTER 1
FIGURE 1- 1 MAP PF THE PHILIPPINES ......................................................................................... 4
FIGURE 1- 2 THE WORK FLOW OF THE DATA COLLECTION SURVEY ON UHC IN THE PHILIPPINES9
TABLE 1- 1 SCOPE OF THE SURVEY .............................................................................................. 4

vi
TABLE 1- 2 SELECTION CRITERIA OF THE FIELD DATA COLLECTION TAGET AREAS ...................... 5
TABLE 1- 3 LIST OF DATA TO BE REVIEWED DURING THE SURVEY................................................ 6
TABLE 1- 4 LIST OF KEY INFORMANTS DURING THE FIELD DATA COLLECTION ............................ 8
TABLE 1- 5 SURVEY TEAM MEMBERS ........................................................................................... 8
CHAPTER 2
FIGURE 2- 1 POPULATION PYRAMID OF THE PHILIPPINES, 2015 (IN THOUSANDS) ....................... 11
FIGURE 2- 2 NATIONAL AND REGIONAL POPULATION IN THE PHILIPPINES (2000-2015) ............ 11
FIGURE 2- 3 TRENDS OF POVERTY HEADCOUNT RATIO AT NATIONAL POVERTY LINES (% OF
POPULATION) IN ASEAN COUNTRIES IN 1997-2014 ............................................................. 14
FIGURE 2- 4 TRENDS OF POVERTY GAP AT NATIONAL POVERTY LINES (%) IN ASEAN COUNTRIES
IN 1997-2012 ...................................................................................................................... 14
FIGURE 2- 5 TRENDS OF GINI INDEX (WORLD BANK ESTIMATE) IN SOUTHEAST ASIAN
COUNTRIES IN 1981-2012 .................................................................................................... 15
CHAPTER 3
FIGURE 3- 1 HEALTH GOVERNANCE STRUCTURE IN THE PHILIPPINES ........................................ 16
FIGURE 3- 2 HEALTH EXPENDITURES, TOTAL (% OF GDP) ........................................................ 21
FIGURE 3- 3 OUT-OF-POCKET HEALTH EXPENDITURE (% OF TOTAL HEALTH EXPENDITURE ON
HEALTH) ............................................................................................................................. 21
FIGURE 3- 4 2014 HEALTH EXPENDITURES BY FACTORS OF HEALTH CARE PROVISIONS .............. 22
FIGURE 3- 5 2014 HEALTH EXPENDITURES BY HEALTH SERVICES AND HEALTH FINANCING
SCHEMES (IN MILLION PESOS) .............................................................................................. 22
FIGURE 3- 6 HEALTH EXPENDITURES BY INCOME QUINTILE GROUP: THE PHILIPPINES,
2012-2014 (IN MILLION PESOS) ........................................................................................... 23
FIGURE 3- 7 HEALTH EXPENDITURES BY INCOME QUINTILE GROUP AND HEALTH FINANCING
SCHEMES: THE PHILIPPINES, 2012-2014 (IN MILLION PESOS) ............................................... 23
FIGURE 3- 8 HEALTH EXPENDITURES BY DISEASE GROUPS AND HEALTH FINANCING SCHEMES:
THE PHILIPPINES, 2014 (IN MILLION PESOS) ......................................................................... 24
FIGURE 3- 9 HEALTH EXPENDITURES BY SPECIFIC DISEASE GROUPS AND HEALTH FINANCIAL
SCHEMES: THE PHILIPPINES, 2014 (IN MILLION PESOS) ........................................................ 25
FIGURE 3- 10 BUDGET AND BREAKDOWNS OF HEALTH BUDGET, 2011-2015 (IN PESOS) ............ 26
FIGURE 3- 11 REVENUE SOURCES AND FLOWS WITHIN THE PUBLIC HEALTH SYSTEM IN THE
PHILIPPINES ........................................................................................................................ 31
FIGURE 3- 12 TRENDS OF TOTAL FERTILITY RATE AND THE TEENAGE FERTILITY OUT OF TOTAL
FERTILITY RATE FROM 1973 TO 2013 IN THE PHILIPPINES .................................................... 37

vii
FIGURE 3- 13 DONOR CONTRIBUTIONS IN PHILIPPINE HEALTH SECTOR AS OF THE END OF
DECEMBER 2015 .................................................................................................................. 38
FIGURE 3- 14 AREAS OF ASSISTANCES BY DONORS AS OF THE END OF DECEMBER 2015 .............. 38
FIGURE 3- 15 DOH BUDGETS AND AMOUNT OF DONOR ASSISTANCES (1998-2016).................. 39
TABLE 3- 1 20 HIGH POVERTY SITES ......................................................................................... 20
TABLE 3- 2 HEALTH FINANCING IN THE PHILIPPINES ................................................................. 20
TABLE 3- 3 DISTRIBUTION OF SIN TAX INCREMENTAL REVENUE IN FY 2016 DOH BUDGET
PROPOSAL ........................................................................................................................... 27
TABLE 3- 4 IRA DISTRIBUTION VS. ESTIMATED SHARE OF DEVOLVED FUNCTIONS..................... 28
TABLE 3- 5 LOCAL TAXES .......................................................................................................... 29
TABLE 3- 6 2003-2007 CASE STUDIES OF VISAYA AND LUZON: LGU ANNUAL INCOME
BREAKDOWNS...................................................................................................................... 29
TABLE 3- 7 PUBLIC HEALTH FACILITIES ...................................................................................... 31
TABLE 3- 8 BASIS FUNCTIONS OF HEALTH FACILITIES................................................................ 32
TABLE 3- 9 MAJOR MCH SERVICES BY VARIOUS HEALTH FACILITIES ........................................... 32
TABLE 3- 10 TARGET REGIONS AND PROVINCES FOR THE USAID ASSISTED MNCHN/FP
PROGRAMS .......................................................................................................................... 42
BOX 3- 1 PHILIPPINES HEALTH AGENDA 2016-2022 ................................................................. 18
BOX 3- 2 THE 10-POINT SOCIOECONOMIC AGENDA OF PRESIDENT DUTERTE ........................... 19
CHAPTER 4
FIGURE 4- 1 ORGANIZATIONAL CHART OF PHILHEALTH ............................................................ 51
FIGURE 4- 2 REIMBURSEMENT FLOWS UNDER CASE RATE FOR PNEUMONIA II (HIGH RISK) ........ 57
FIGURE 4- 3 PREMIUM CONTRIBUTION TO PHILHEALTH BY MEMBERSHIP CATEGORIES (IN PESOS)
........................................................................................................................................... 65
TABLE 4- 1 PHILHEALTH MEMBERSHIP CATEGORY.................................................................... 53
TABLE 4- 2 ENROLLMENT PROCEDURES BY MEMBERSHIP CATEGORY ........................................ 54
TABLE 4- 3 PREMIUM PAYMENT PROCEDURES ........................................................................... 55
TABLE 4- 4 CASE RATE PAYMENT INTRODUCED IN 2011 – CASES AND RATES (IN PESOS) ............ 56
TABLE 4- 5 PRIMARY CARE SERVICE OFFERED UNDER TSEKAP PROGRAM ................................. 58
TABLE 4- 6 OUTPATIENT BENEFIT PACKAGES OFFERED BY PHILHEALTH (OTHER THAN TSEKAP)
........................................................................................................................................... 59
TABLE 4- 7 Z BENEFIT PACKAGE: YEAR OF INTRODUCTION AND CASE RATES (IN PESOS) ........... 59

viii
TABLE 4- 8 CONTRACTED HOSPITALS FOR ELECTIVE SURGERY FOR CORONARY ARTERY BYPASS
GRAPH ................................................................................................................................ 60
TABLE 4- 9 MATERNITY CARE PACKAGE (IN PESOS) ................................................................... 61
TABLE 4- 10 NCB PACKAGE (IN PESOS) ..................................................................................... 62
TABLE 4- 11 OTHER MDG RELATED PACKAGES (IN PESOS) ....................................................... 62
TABLE 4- 12 INSTITUTIONAL PROVIDERS WITH PHILHEALTH ACCREDITATIONS ........................ 64
TABLE 4- 13 NUMBER OF ACCREDITED OUTPATIENT CLINICS, NUMBER AND PERCENTAGE OF
CITIES AND MUNICIPALITIES WITH ACCREDITED OUTPATIENT CLINICS ............................... 64
TABLE 4- 14 PREMIUM CONTRIBUTIONS AND BENEFIT CLAIMS FOR 2015 BY NHIP MEMBERS ... 65
TABLE 4- 15 NUMBER OF COVERED MEMBERS AND COVERAGE RATIO FROM 2010 TO 2015 ....... 66
TABLE 4- 16 NHIP UTILIZATION FROM 2012 TO 2015NHIP ..................................................... 67
TABLE 4- 17 PATIENT CATEGORIES BASED ON THE ABILITY TO PAY AND RESPECTIVE PAYMENT
AMOUNTS ........................................................................................................................... 70
CHAPTER 5
FIGURE 5- 1 TREND OF MATERNAL DEATHS AND MMR IN BICOL ............................................... 74
FIGURE 5- 2 RURAL HEALTH UNIT IN CAMARINES SUR ............................................................. 77
FIGURE 5- 3 BRTTH ................................................................................................................. 79
FIGURE 5- 4 PHILHEALTH BICOL REGIONAL OFFICE ................................................................. 80
FIGURE 5- 5 BARANGAY HEALTH STATION IN CAMARINES SUR ................................................... 81
FIGURE 5- 6 GROUP DISCUSSION WITH PREGNANT AND LACTATING WOMEN ............................ 82
FIGURE 5- 7 MCP UTILIZATION AMOUNT IN BICOL (UP TO JUNE IN 2016).................................. 84
FIGURE 5- 8 BARANGAY HOUSES IN CAMARINES SUR ................................................................ 84
FIGURE 5- 9 MMR AND IMR OF EASTERN VISAYAS .................................................................... 88
FIGURE 5- 10 RHU STAFF OF CAN-AVID MUNICIPALITY IN EASTERN SAMAR ............................... 95
FIGURE 5- 11 INTERVIEW WITH MAYOR ..................................................................................... 96
FIGURE 5- 12 BHS DESTROYED.................................................................................................. 96
FIGURE 5- 13 MCP BENEFIT PAYMENTS IN EASTERN SAMAR AND NORTHERN SAMAR ................ 99
FIGURE 5- 14 PHILHEALTH NORTHERN SAMAR OFFICE ........................................................... 99
FIGURE 5- 15 RURAL HOUSEHOLD INTERVIEWED BY THE STUDY ............................................ 102
TABLE 5- 1 PROVINCIAL POPULATIONS IN BICOL REGION (IN THOUSAND) ................................. 73
TABLE 5- 2 NUMBER OF MATERNAL DEATHS AT TERTIARY HOSPITALS ........................................ 74
TABLE 5- 3 PROPORTION OF FBD (%) BY PROVINCE/CITY ......................................................... 74
TABLE 5- 4 IMR BY PROVINCE/CITY........................................................................................... 75
TABLE 5- 5 REGISTERED NUMBER OF PUBLIC AND PRIVATE HOSPITALS (2015-2016) .................. 75

ix
TABLE 5- 6 STUDY SITES AND COMMUNITY INTERVIEWEES ......................................................... 76
TABLE 5- 7 NHIP COVERAGE BY SECTOR AND BY PROVINCE IN BICOL AS OF JUNE 2016 .............. 84
TABLE 5- 8 PROVINCIAL POPULATIONS IN EASTERN VISAYAS REGION (IN THOUSAND) ............... 87
TABLE 5- 9 PROVINCIAL FBD RATES IN EASTERN VISAYAS ......................................................... 88
TABLE 5- 10 REGISTERED HEALTH FACILITIES IN PROVINCES OF EASTERN VISAYAS (AS OF
AUGUST 2, 2016)................................................................................................................. 89
TABLE 5- 11 DELIVERIES AND MATERNAL DEATHS AT EVRMC ................................................. 90
TABLE 5- 12 MATERNAL AND CHILD HEALTH INDICATORS IN NORTHERN SAMAR ...................... 91
TABLE 5- 13 FACILITY BASED DELIVERY IN MUNICIPALITIES OF NORTHERN SAMAR PROVINCE .. 92
TABLE 5- 14 MATERNAL AND CHILD HEALTH INDICATORS IN EASTERN SAMAR.......................... 93
TABLE 5- 15 FACILITY BASED DELIVERY RATE IN EACH MUNICIPALITY OF EASTERN SAMAR
PROVINCE (2012 – JUNE 2016) .......................................................................................... 93
TABLE 5- 16 STUDY SITES AND COMMUNITY INTERVIEWEES ...................................................... 94
TABLE 5- 17 NUMBERS OF NHIP MEMBERS IN EASTERN VISAYAS (AS OF JUNE 2016) ................. 98
BOX 5- 1 STORY OF RHU MEDICAL DOCTOR OUTSIDE CASILI ZONE ....................................... 78
BOX 5- 2 BRTTH LEADERSHIP (STORY OF DOH REGIONAL OFFICER) ..................................... 79
BOX 5- 3 STORY OF PROVINCIAL HEALTH OFFICER ................................................................... 80
BOX 5- 4 HOME DELIVERY CASES .............................................................................................. 83
BOX 5- 5 EXPERIENCE OF A 35-YEAR-OLD WOMAN ................................................................. 103
BOX 5- 6 EXPERIENCE OF A 35-YEAR-OLD WOMAN ................................................................ 105
BOX 5- 7 EXPERIENCE OF A 19-YEAR-OLD WOMAN ................................................................. 105
CHAPTER 6
FIGURE 6- 1 BHS SUPPORTED BY JICA .................................................................................... 108
FIGURE 6- 2 BHS STAFF INTERVIEWED ..................................................................................... 111
FIGURE 6- 3 MCP-ACCREDITED BHS ...................................................................................... 111
TABLE 6- 1 LIST OF INTERVIEWEES .......................................................................................... 108
TABLE 6- 2 OUTCOME OF THE JICA PROJECT IN CORDILLERA ................................................. 109
TABLE 6- 3 OUTCOME OF THE JICA PROJECT IN EASTERN VISAYAS .......................................... 110
CHAPTER 7
FIGURE 7- 1 SDN HOUSEHOLD PROFILING .............................................................................. 117
FIGURE 7- 2 RECOMMENDED JICA NEW PROJECT AND PROJECT UPSCALING MECHANISM ....... 119
1
EXECUTIVE SUMMARY
Although the national infant mortality rate and under-five mortality rate have declined steadily,
the maternal mortality ratio and neonatal death remain high and regional disparities exist in the
Philippines. In the Philippine Health Agenda 2016-2022, President Duterte announced that the
new administration would guarantee good health for all life stages by setting effective Service
Delivery Networks and providing universal health insurance.
In 1995, the National Health Insurance Program (NHIP) was established, and as of the end of
June 2016, 90 percent of Filipinos were enrolled in NHIP. However, the out-of-pocket
expenditure rate is more than 50 percent, which is higher than many other Southeast Asian
countries. Moreover, the knowledge of the LGU staff, the health care providers and the people
is still limited and utilization rate remains low at 12 percent. The government budget increased
substantially in 2014 due to increased tax revenue from the Sin Tax Reform Law of 2012 and
about 40 percent of the indigent and near-indigent population are now sponsored by the national
government. Nonetheless, the total health expenditure for the richest quintile is more than twice
as much as that of the poorest quintile. The total health expenditure as a percentage of the Gross
Domestic Product (GDP) in the Philippines is lower than most developed countries, however,
comparable to other Southeastern Asian countries.
The Philippine health system is devolved and public health service providers are primarily local
government units (LGUs). The public health services are financed by central government
subsidy and the LGU budget. The LGU budget consists of local government tax revenues, user
fees at health facilities, and payments from health insurance corporations. Health service quality
highly depends on leadership of the executives of LGUs. Functional health service networks are
indispensable particularly for emergency obstetric care. However, coordination between the
primary health facilities and the referral hospitals within the multiple LGUs has been a
challenge in the devolved Philippine health system.
While institutional delivery has been increasingly popular in the Philippines, quite a few women
still prefer home delivery. There are geographical and cultural factors that affect their
preference; however, the important factor is financial. When a woman delivers at a facility, she
has to pay for medicine not in stock, some examinations, transportation fees, food for the
attendant family members, payment of the child care-takers, and loss of income while
hospitalized. These expenditures are a huge burden on poor families.
The survey team would recommend JICA to pursue the new technical assistance project, “UHC
enhancement in the MCH services” with two approaches: improved access to quality essential
health-care services and financial risk protection. Furthermore, a mechanism to fully up-scale
the good results of the project to the entire country should be also sought in the new project.

2
Chapter 1 Overview of the Survey
1-1 Background
The Aquino administration launched the national Universal Health Care policy (Kalusugan
Pangkalahatan, known as KP) in December 2010 to provide every Filipino with affordable and
quality health services particularly the most vulnerable and remote populations through three
strategic goals: 1) financial risk protection, 2) improved access to quality hospitals and health
care facilities, and 3) the attainment of health-related Millennium Development Goals (MDGs).
The first goal, financial risk protection, is intended to insure all citizens through the
implementation of the National Health Insurance Program (NHIP) by the Philippine Health
Insurance Corporation (PhilHealth).
The new President Duterte recently introduced the Philippine Health Agenda 2016-2022 with
the theme “All for Health towards Health for All.” The Agenda aims at attaining Health-Related
Sustainable Development Goal (SDG) Targets, Financial Risk Protection, Better Health
Outcomes and Responsiveness, and guarantees (1) All Life Stages & Triple Burden of Disease,
(2) Service Delivery Network, and (3) Universal Health Insurance.
According to PhilHealth, 92,624,502 people or 90 percent of the total population
1
had become
eligible beneficiaries of the NHIP by the end of June 2016 and the enrollment rate has been
increasing somewhat.
2
Since the Sin Tax Law (RA 10351) was passed in December 2012, the
increased tax revenue has enabled many of poor families to be enrolled as indigent members.
On the other hand, household out-of-pocket spending has increased by 150 percent from 2000 to
2012.
3
Although the out-of-pocket spending rate out of the total health expenditures has been
decreasing lately, household out-of-pocket spending was still as high as 44 percent, and NHIP’s
utilization rate
4
remains low at 12 percent as of December 31, 2015.
5
In addition, it is reported
that 7.7 percent of the households experienced catastrophic health expenditure in 2012 and the
proportion had increased three-fold from 2000.
6,7
This data reveals that NHIP enrollment has
not necessarily resulted in the improvement of access to health services and financial risk
protection.
1
On the basis of the Philippine 2015 Population Census, the total population of the Philippines as of
August 1, 2015 is 100,981,437.
2
PhilHealth. (2016). Stats and Charts, December 31, 2015.
3
Bredenkamp C. & Buisman L. R. (2016).
4
Utilization rate = unique member claims reimbursed/ total eligible members
5
PhilHealth. (2016). Stats and Charts, December 31, 2015.
6
ibid
7
Bredenkamp C. & Buisman L. R. (2016).

3
The government of Japan stated promotion of universal health coverage (UHC) as a vision of
Japan’s Strategy on Global Health Diplomacy in 2013. The government also declared that Japan
would take the lead in addressing global challenges including UHC, formulating international
goals and guidelines, and making active efforts to achieve the goals in the Development
Cooperation Charter in 2015.
Japan International Cooperation Agency (JICA) has been providing assistance to the Philippines
for the improvement of maternal and child health (MCH) especially in remote and poor areas,
such as the Cordillera Administrative Region and Eastern Visayas Region. While the evidence
has shown that the JICA projects have improved the MCH service delivery in the target areas, it
is suggested that mothers are still dying in childbirth due to personal, family and community
factors as well as healthcare system factors that hinder their accessibility to health services.
8
In
order for JICA to continue the efforts of MCH development in the context of the new
Sustainable Development Goal (SDG) 3, aiming at reduction of maternal and neonatal mortality
and improved access to sexual and reproductive health-care services, and start contributing to
the new administration’s health agenda, JICA dispatched the data collection survey team to
clarify current issues affecting access to MCH services, particularly for the poor, and to explore
JICA’s future assistance in the Philippines to promote UHC in the area of MCH.
1-2 Objectives
The data collection survey had the following objectives:
1) To understand the current status of NHIP implementation in the Philippines and identify
issues preventing access to basic health services with a particular focus on MCH services
for the poor; and
2) To identify possible areas for JICA’s future assistance in strengthening MCH services and
promoting UHC in the Philippines.
1-3 Scope of the Survey
Based on the situation analysis and objectives described earlier, data collection activities of the
survey were undertaken within the scope described in Table 1- 1.
8
Saniel, O. P. & Bermudez, A. N. C. (2016, August). Why do mothers die? A Maternal Death Review
in Camarines Norte.

4
Table 1- 1 Scope of the Survey
1-4 Survey Areas
The JICA survey team reviewed the overall status of UHC
and MCH efforts of the Philippines in Manila, and drew
lessons learned from the currently conducted MCH project
in the Cordillera Administrative Region (CAR).
Moreover, the Bicol Region and Eastern Visayas Region
were selected as field data collection sites based on the
following criteria (see Table 1- 2):
Unsuccessful MCH indicators including facility- based
delivery (FBD), antenatal care (ANC) from skilled
providers and postnatal care (PNC) in the first two days
after birth according to National Demographic and
Health Survey (NDHS) 2013
20 High Poverty Sites announced by the Duterte
Administration as priority provinces
High ratio of geographically isolated and
disadvantaged area (GIDA), according to the
Department of Health (DOH)
Large population
Accessible from Manila
Acceptable security level based on JICA’s standards
(1) Heath sector analysis
Status and issues concerning the overall health sector especially MCH
Regional progress in achieving MCH indicators
Status of health system at regional level
Donor assistance
Health sector priorities under the new administration
(2) Status of basic health service provision and access for the poor through the NHIP
Basic information about the NHIP
Size of population covered by the NHIP
Health services covered by the NHIP
Proportion of costs covered by the NHIP
(3) Analysis of factors affecting access to health services particularly economic access
Systems of DOH and PhilHealth to address the issue of economic access
Situation of out-of-pocket health expenditure paid by pregnant women
Implementation status of the No Balance Billing Policy at health facilities
(4) Suggestion of JICA’s future cooperation program
Means of transportation and transportation fees for pregnant women’s access and referral
to health facilities including hospitals, RHUs and BHS
Psychological barriers for pregnant women at the time of referral to health facilities
including hospitals, RHUs and BHS
Level of awareness of patients and service providers on the MCH service package and
primary care benefits
Figure 1- 1 Map pf the Philippines

5
Table 1- 2 Selection Criteria of the Field Data Collection Target Areas
9
Region
2015
Population
1
FBD
2
ANC
2
PNC
2
GIDA(%)
3
High
Poverty
Sites
%
Rank
%
Rank
%
Rank
Rank
1.
Mimaropa - 4B
2,963,360
37
15
91
15
50
15
7
―
2.
Soccksargen - 12
4,545,276
49
13
92
14
54
14
14
〇
3.
Zamboanga Peninsula - 9
3,629,783
43
14
94
13
55
13
14
〇
4.
Northern Mindanao - 10
4,689,302
53
10
95
12
58
12
12
〇
5.
Caraga - 13
2,596,709
56
9
97
9.5
63
11
24
―
6.
Cagayan Valley - 2
3,451,410
51
12
97
7
67
10
20
―
7.
Bicol Region - 5
5,796,989
51
11
97
9.5
74
7
19
〇
8.
Eastern Visayas - 8
4,440,150
62
7
96
11
77
5
9
〇
9.
Davao Region - 11
4,893,318
63
6
98
5
73
9
14
〇
10.
Western Visayas - 6
4,477,247
61
8
98
3
73
8
21
〇
11.
Calabarzon - 4A
14,414,774
66
5
97
8
77
4
2
〇
12.
Ilocos Region - 1
5,026,128
67
4
97
6
78
3
16
〇
13.
Central Luzon - 3
11,218,177
68
3
98
4
76
6
11
―
14.
Central Visayas- 7
6,041,903
72
2
98
1
83
2
5
〇
15.
CAR
1,722,006
75
1
98
2
83
1
42
〇
Source:
1
The Philippine Population Census (2015),
2
National Demographic and Health Survey (2013),
3
Bureau of Local Health Development, DOH,
4
DOH
1-5 Methodology
The survey consisted of a literature review and field data collection to derive situation analysis
and strategic recommendations for JICA’s future assistance in the Philippines:
(1) Literature review
Existing academic research papers and reports by government, donors and
non-governmental organizations (NGOs) on the subjects mentioned in Table 1- 1 were
collected and analyzed throughout the survey period.
(2) Field data collection
The JICA survey team conducted interviews and collected materials at the Philippine
Government offices, including the Department of Health (DOH), PhilHealth, the
Department of Social Welfare and Development (DSWD), the Department of Interior and
Local Government (DILG) and the Philippine Statistics Authority (PSA), and development
partners at the national level. At the sub-national level, the survey team collected
information through key informant interviews (KIIs) and focus group discussions (FGDs)
at the DOH/PhilHealth Regional Offices, other government offices, local government units
(LGUs), health facilities, NGOs, community members and any other relevant parties.
9
National Capital Region and ARMM are not included in the table as they are not likely to be JICA
project target sites. NIR is also not included as it was newly created in 2015.

6
Table 1- 3 shows categories and sub-categories, sources and collection methods of data
collected in the survey.
Table 1- 3 List of Data to be Reviewed During the Survey
Data Category
Data Sub-Category
Data Source
Data
Collection
Method
1
Status and issues of
the health sector
especially MCH
Overview of the health sector
Achievements and challenges
pertaining to MCH
Online
Statistical data
Japanese experts
Desk
review
KII
Regional Progress in
achieving MCH
indicators
MMR
IMR
MCH service utilization rates
Online
Statistical data
Status of health
system at regional
level
System of health service provision
Human resources
Budget
Number of NHIP-accredited facilities
Online
Statistical data
Japanese experts
Donor assistance
Status of assistance in health financing
Status of assistance in MCH
Status of assistance in health system
Online
Japanese experts
New administration’s
health sector priorities
Priority issues on MCH
Other priority issues on health
Online
Japanese experts
2
Basic information
about the NHIP
Organization and structure
Financial resources and budget
Payment mechanisms
Accreditation system
Awareness-raising activities
Online
DOH and PhilHealth
Experts
Desk
review
KII
Size of population
covered by the NHIP
Enrollment and utilization rates of
each program (particularly for
indigents)
Online
DOH and PhilHealth
Beneficiaries
including indigents
Desk
review
FGD
KII
Enrollment rates in each region
DOH and PhilHealth
Desk
review
KII
Reasons for not enrolling
Community members
not enrolled in the
NHIP
FGD
KII
Characteristics of NHIP populations
PhilHealth
KII
Health services
covered by the NHIP
Details of benefits and packages
Online
PhilHealth
Desk
review
KII
Proportion of costs
covered by the NHIP
Details of out-of-pocket spending
DOH and PhilHealth
NHIP members
Details of costs covered by LGUs
DOH/LGU and
PhilHealth
Health facilities
Measures for indigents not enrolled in
the NHIP
Health facilities
PhilHealth
Indigents who are not
enrolled in the NHIP
Desk
review
FDG
KII

7
Data Category
Data Sub-Category
Data Source
Data Collection
Method
3
Means of
transportation and
transportation fees
for pregnant
women’s access and
referral to health
facilities
Distance and conditions of
infrastructure between facilities at
different levels
DOH/LGU
Healthcare
providers/BHWs
Pregnant and
lactating women
Barangay councilors/
Chairmen
Donors/NGOs
PhilHealth
Community members
Desk review
KII
FGD
Transportation options and time
required
Transportation costs and household
income sources/levels
Existing transportation support by
government/donors
Psychological
barriers for pregnant
women at the time of
referral to health
facilities
Images/perceptions of health facilities
and staff
DOH/LGU
Healthcare providers/
BHWs
Pregnant and
lactating women
TBAs
Traditional leaders
Donors/NGOs
Actual experiences at or feedback on
health facilities (including what they
heard from families and friends)
Determining factors for referral
Household decision-making on referral
Coping strategies when referral is not
utilized
DOH and
PhilHealth’s systems
to address the issue
of economic access
DOH and PhilHealth’s measures to
address the issue
Online
DOH and PhilHealth
Community members
DOH’s measures to improve economic
access to health services other than the
NHIP (such as through social security
and anti-poverty systems)
Online
DOH and PhilHealth
Desk review
KII
DOH’s systems and mechanisms on
referral and emergency transport
LGU’s systems to support
transportation fees
DOH/LGU
KII
Details of PhilHealth’s benefits and
packages (in relation to economic
access)
PhilHealth
Desk review
KII
Out-of-pocket
expenses paid by
pregnant women
Fees paid at health facilities for ANC,
delivery and PNC services
Women who gave
birth in the past year
DOH and PhilHealth
Health facilities
KII
FGD (during
PNC and at
community)
Reimbursements from the NHIP for
healthcare expenses related to ANC,
delivery and PNC services
Women who gave
birth in the past year
PhilHealth
KII
FGD (during
PNC and in
community)
Implementation
status of the No
Balance Billing
Policy at hospital
level
Healthcare providers’ level of
awareness of the No Balance Billing
Policy
Healthcare providers
KII
Implementation status of the No
Balance Billing Policy
Health facilities
DOH/LGU
Patients
KII
FGD
Awareness levels of
patients and
healthcare providers
regarding the MCH
service package and
primary care benefits
Awareness levels of pregnant women
and healthcare providers on the MCH
service package
Healthcare
providers/BHWs
Pregnant and
lactating women
Patients
Barangay councilors/
Chairmen
Donors/NGOs
Awareness levels of patients and
healthcare providers on the primary
care benefits

8
The key informants interviewed in the survey are listed in Table 1- 4.
Table 1- 4 List of Key Informants During the Field Data Collection
Informants
Government
DOH (national/regional officers)
LGU (provincial/city/municipal health officers)
Healthcare providers at DOH’s
regional/provincial/district/municipal hospitals, medical
centers, RHUs and BHS
BHWs
Barangay Chairmen and Councilors
Community Health Team (CHT)
PhilHealth (national and LGU levels)
DSWD (national/regional/provincial/municipal
officers)
Development
partners
WHO, UNICEF, UNFPA, World Bank, ADB, EU,
USAID
NGOs
Community
Pregnant and lactating women
TBA
Traditional/religious leaders
Patients at health facilities
Community-based organizations/women’s groups
Other
Private hospitals and clinics covered by PhilHealth in
survey areas
Private insurance companies
JICA Office, JICA Experts and the Embassy of Japan
Ambulatory service providers (such as Lifeline Rescue)
Universities and think tanks
1-6 Survey Team
The survey team consists of the members in Table 1- 5.
Table 1- 5 Survey Team Members
Name
Area of work
Affiliation
Ms. Haruyo Nakamura
Team Leader/UHC
Global Link Management, Inc.
Ms. Akiko Hirano
MCH /Health System Analysis
Global Link Management, Inc.
Ms. Nami Takashi
MCH /Needs Analysis
Global Link Management, Inc.
Mr. Shizuma Yokozawa
Health Financing
Deloitte Tohmatsu Financial Advisory LLC
1-7 Survey Schedule
The survey was conducted from July to December 2016. During this period field data
collections were executed in the Philippines for three times. Please see Attachments 1-4 for the
detailed schedules of the first to third field data collections. The work flow of the entire survey
is shown in Figure 1- 2.

9
Figure 1- 2 The Work Flow of the Data Collection Survey on UHC in the Philippines
Month
Deliverable Tasks in Japan Tasks in the Philippines
JUL
AUG
SEP
OCT
NOV
DEC
・Develop and finalize the inception report
・Desk review on the health sector situation
・Prepare for the field data collection
(1) Preparation
Inception
Report
・Brief JICA Philippines, DOH etc. on the inception report
・Interview DOH, PhiliHealth, donors etc. on the system of health
care and MCH service delivery and access for the poor
(2) First Field Data Collection
・Interview LGUs, health facilities and communities in target
regions (CAR, Eastern Visayas and Bicol Region) on factors
affecting economic access to MCH services
・Analysis and documentation of the first field survey
・Prepare for the second field survey
(4) Second Field Data Collection
Summary
of Results
Final
Report
Reporting to
JICA HQ
(3) Documentation and Preparation
・Discussion with JICA Philippines and DOH on the summary
・Follow-up data collection
(5) Drafting of a Summary of Results from the Field Data Collection
・Finalize the result summary
・Devise JICA’s future assistance
(7) Documentation and Analysis
・Develop a final report
(8) Finalization
Consultation
with JICA HQ
(6) Third Field Data Collection

10
Chapter 2 Socio-Economic Situation in the Philippines
2-1 Geography, Ethnicity and Religion
The Philippines is an archipelago comprised of 7,107 islands in Southeast Asia. Its terrain is
primarily mountainous with narrow to extensive coastal lowlands. It has a tropical and maritime
climate, characterized by relatively high temperatures, high humidity and abundant rainfall.
Because of its location in the typhoon belt of the Western Pacific, the Philippines experiences
an average of twenty typhoons annually during its rainy season, from June to November. In
addition, the country is along the “Pacific Ring of Fire,” where large number of earthquakes and
volcanic eruptions occur. These factors combine to make the Philippines one of the most
disaster-prone countries on the globe.
10
According to the 2010 Census of Population and Housing, 92.6 percent of the Filipinos are
Christian, 80.6 percent of which are Roman Catholic, 5.6 percent are Muslim and 0.05 percent
are Buddhist. There are approximately 180 ethnic groups which have their own languages. The
largest linguistic group is Tagalog, which accounts for 24.4 percent of the population. Other
ethnic groups include Cebuano, Ilocano, Hillgaynon (Ilongo), Bisaya, Bicol and
Lineyte-Samarnon (Waray). The official language of the Philippines is Filipino, derived from
Tagalog and English.
2-2 Population Statistics and Future Projections
The total population of the Philippines was 76,506,928 in 2000, 92,337,852 in 2010 and
100,981,437 in 2015 (see Figure 2- 1). The average population growth rate during the period
varies from the highest in Calabarzon Region at 2.85 percent to the lowest in Negros Island
Region at 1.14 percent (see Figure 2- 2).
11
The population in 2016 is estimated to be
102,250,133 (population growth rate: 1.54 percent, population density: 343 persons per km
2
)
and projected to continuously increase to 148,260,478 by 2050.
12
10
Kwon S. & Dodd R. (Eds.). (2011). The Philippines Health System Review, WHO Health Systems in
Transition.
11
The Philippine 2015 Population Census.
https://psa.gov.ph/content/highlights-philippine-population-2015-census-population.
12
Worldometers (www.Worldometers.info) Elaboration of data by United Nations, Department of
Economic and Social Affairs, Population Division. World Population Prospects: The 2015 Revision.
(Medium-fertility variant).

11
Source: Department of Economic and
Figure 2- 1 Population pyramid of the Philippines, 2015 (in thousands)
Social Affairs, Population Division, United Nations
Figure 2- 2 National and Regional Population in the Philippines (2000-2015)
Source: The Philippine 2015 Population Census. https://psa.gov.ph/content/highlights-philippine-population-2015-census-population.
0 2,000 4,000 6,000
02,0004,0006,000
0-4
10-14.
20-24
30-34
40-44
50-54
60-64
70-74
80-84
Men Women
0 4,000,000 8,000,000 12,000,000 16,000,000
REGION XIII (Caraga)
AUTONOMOUS REGION IN MUSLIM MINDANAO (ARMM)
REGION XII (SOCCSKSARGEN)
REGION XI (DAVAO REGION)
REGION X (NORTHERN MINDANAO)
REGION IX (ZAMBOANGA PENINSULA)
REGION VIII (EASTERN VISAYAS)
NEGROS ISLAND REGION (NIR) 1
REGION VII (CENTRAL VISAYAS)
REGION VI (WESTERN VISAYAS)
REGION V (BICOL REGION)
REGION IV-B (MIMAROPA)
REGION IV-A (CALABARZON)
REGION III (CENTRAL LUZON)
REGION II (CAGAYAN VALLEY)
REGION I (ILOCOS REGION)
CORDILLERA ADMINISTRATIVE REGION (CAR)
NATIONAL CAPITAL REGION (NCR)
TOTAL POPULATION 1-Aug-15 TOTAL POPULATION 1-May-10 TOTAL POPULATION 1-May-00
0 4,000,000 8,000,000 12,000,000 16,000,000
REGION XIII (Caraga)
AUTONOMOUS REGION IN MUSLIM MINDANAO (ARMM)
REGION XII (SOCCSKSARGEN)
REGION XI (DAVAO REGION)
REGION X (NORTHERN MINDANAO)
REGION IX (ZAMBOANGA PENINSULA)
REGION VIII (EASTERN VISAYAS)
NEGROS ISLAND REGION (NIR) 1
REGION VII (CENTRAL VISAYAS)
REGION VI (WESTERN VISAYAS)
REGION V (BICOL REGION)
REGION IV-B (MIMAROPA)
REGION IV-A (CALABARZON)
REGION III (CENTRAL LUZON)
REGION II (CAGAYAN VALLEY)
REGION I (ILOCOS REGION)
CORDILLERA ADMINISTRATIVE REGION (CAR)
NATIONAL CAPITAL REGION (NCR)
TOTAL POPULATION 1-Aug-15 TOTAL POPULATION 1-May-10 TOTAL POPULATION 1-May-00

12
The proportion of age categories 0-14 years, 15-64 years and 65+ years are 31.9 percent, 63.5
percent and 4.6 percent, respectively, in 2015. The child dependency ratio
13
is 50.3, the old-age
dependency ratio
14
is 7.2, and the total dependency ratio is 57.5.
15
The total fertility rate is
3.04, the under-five mortality rate is 30 per 1,000 live births, and average life expectancy is
estimated to be 68 years.
16
The total fertility rate is similar to Japan’s in 1951-1952.
17
Life expectancy
18
and the
population proportions of 0-14 years and 15-64 years are similar to Japan in 1960; however, the
proportion of people 65+ years is lower than that of Japan in 1960 at 5.7.
19
Aging is slowly becoming an issue in the Philippines.
20
The Philippines is forecast to become
an aging society with 7 percent of aged people (65+ years) in 2030-2035 and an aged society
with 14 percent of aged people in 2070-2075. The doubling time
21
is projected to be 35 to 45
years,
22
which is much longer than that of Japan at 24 years.
23
It is predicted that the labor force ratio (15-64 years) will be 66.7 percent in 2055 at the highest
point and then will decrease, while the dependency ratio will be 33.3 percent at the lowest in the
same year and then will increase.
24
Japan experienced the same transition in the early 1990s.
25
13
The child dependency ratio is an age-population ratio of children under the age of 15 and those
typically in the labor force (the productive part). It is used to measure the pressure on the productive
population.
14
The old-age dependency ratio is an age-population ratio of those over the age of 64, not in the labor
force, and those typically in the labor force (the productive part). It is used to measure the pressure on
the productive population.
15
The Philippine 2015 Population Census.
https://psa.gov.ph/content/highlights-philippine-population-2015-census-population.
16
United Nations, Department of Economic and Social Affairs, Population Division. (2015). World
Population Prospects: The 2015 Revision. Volume II: Demographic Profiles.
17
National Institute of Population and Social Security Research. 2016. Population Statistics.
http://www.ipss.go.jp/syoushika/tohkei/Popular/P_Detail2016.asp?fname=T04-03.htm.
18
Ministry of Health, Labour and Welfare. Abridged life table.
http://kaiwa-kouza.com/contents/sub/statistics/longevity.html.
19
Statistics of Japan 2016, Statistics Bureau, Ministry of Internal Affairs and Communications.
http://www.stat.go.jp/data/nihon/02.htm
20
All the population estimates here are moderate-range estimates.
21
Number of years required for the proportion of the aged population to move from 7% to 14%. It is an
indicator that shows the speed of aging in each country.
22
United Nations, Department of Economic and Social Affairs, Population Division. Interactive data of
World Population Prospects, the 2015 Revision. https://esa.un.org/unpd/wpp/.
23
National Institute of Population and Social Security Research. 2012. Population Statistics.
http://www.ipss.go.jp/syoushika/tohkei/Popular/P_Detail2012.asp?fname=T02-18.htm
24
United Nations, Department of Economic and Social Affairs, Population Division. Interactive data of
World Population Prospects, the 2015 Revision. https://esa.un.org/unpd/wpp/.
25
Statistics of Japan 2016, Statistics Bureau, Ministry of Internal Affairs and Communications.
http://www.stat.go.jp/data/nihon/02.htm

13
In the Philippines, child dependency is currently much higher than old age dependency (child
dependency: 50.3, old-age dependency: 7.2), however, it will become equal in 2090 (both child
dependency and old-age dependency: 31.1) and then old-age dependency will become slightly
higher.
26
Japan experienced the same transition in the late 1990s.
27
2-3 Poverty and Economic Disparity
The Gross National Income (GNI) of the Philippines was US$357 billion
28
in 2015, GNI per
capita was US$3,540,
29
and the real GDP growth rate has been on average 6 percent from 2010
to 2015. The Philippines is categorized as a “lower-middle-income economy”
30
by the World
Bank.
31
In the Philippines, the poverty incidence
32
was estimated at 21.6 percent in 2015.
33
Although
the estimate was improved from 2012 at 25.6 percent, another poverty data, the poverty
headcount ratio, has not shown much change in the past decade in the country, while other
Southeast Asian countries, such as Cambodia, Thailand, Vietnam and Laos, have shown
progress (see Figure 2- 3). The Philippines’ poverty headcount ratio is in fact one of the highest
in the region today.
26
United Nations, Department of Economic and Social Affairs, Population Division. Interactive data of
World Population Prospects, the 2015 Revision. https://esa.un.org/unpd/wpp/.
27
Statistics of Japan 2016, Statistics Bureau, Ministry of Internal Affairs and Communications.
http://www.stat.go.jp/data/nihon/02.htm
28
At the time of the US$ market price.
29
Calculated using Atlas method of the World Bank (Converted to the current US$).
30
World Bank Open Data. http://data.worldbank.org/
31
The World Bank’s country classification by income level takes place in July every year and it uses
GNI per capita of the previous years as an indicator. For the current 2017 fiscal year, lower
middle-income economies are defined as those with a GNI per capita, calculated using the World
Bank Atlas method, of between $1,026 and $4,035.”
32
Poverty incidence is the proportion of people below the poverty line to the total population. The
poverty line refers to the minimum income required to meet food and non-food requirements. In 2015,
a family of five needed at least PhP 9,064, on average, every month to meet both basic food and
non-food needs. Source: Philippine Statistics Authority. https://psa.gov.ph/poverty-press-releases.
33
Philippine Statistics Authority. (2016). Philippine Poverty Statistics.
https://psa.gov.ph/poverty-press-releases

14
Figure 2- 3 Trends of poverty headcount ratio at national poverty lines (% of population)
in ASEAN countries in 1997-2014
Source: World Bank. The World Development Indicators
Figure 2- 4 Trends of poverty gap at national poverty lines (%)
in ASEAN countries in 1997-2012
Source: World Bank. The World Development Indicators
Whereas the poverty gap ratio
34
in 2012 was 5.1 percent, which had slightly improved since
2003, showing that the depth and incidence of poverty in the country has been somewhat
mitigated in the past decade. However, the country’s progress is still minimal as compared with
other Southeastern countries, such as Cambodia, Laos and Vietnam, and the Philippine poverty
gap ratio was second highest among these nations in 2012 (see Figure 2- 4).
The GINI Index, which measures the degree of inequality in the distribution of family income in
a country, shows that income is distributed quite unequally in the Philippines, at the highest
34
Poverty gap ratio is the mean shortfall of the total population from the poverty line (counting the
non-poor as having zero shortfall), expressed as a percentage of the poverty line. This measure reflects
the depth of poverty as well as its incidence.
0
10
20
30
40
50
60
1997 2000 2002 2003 2004 2006 2007 2008 2009 2010 2011 2012 2013 2014
Philippines Cambodia Lao PDR Thailand Vietnam
0
2
4
6
8
10
12
14
16
1997 2002 2003 2006 2007 2008 2009 2010 2011 2012
Philippines Cambodia Lao PDR Vietnam

15
after 1996, and it has not improved over the past three decades. In fact, the Philippines’ family
income is the most unequally distributed in all of Southeast Asia (see Figure 2- 5).
Figure 2- 5 Trends of GINI Index (World Bank estimate)
in Southeast Asian countries in 1981-2012
Source: World Bank. The World Development Indicators
2-4 Industrial Structure and Labor Market
In the Philippines, the composition ratio by industry to GDP in 2014 was as follows:
manufacturing (20.6%), trade (17.7%), agriculture (11.3%), finance (7.8%), and construction
(6.6%). The composition ratio has not changed in the past three decades.
35
The labor force
36
(ages 15-64) of the Philippines in 2014 was 41,379,000 people. Among the
labor force, 38,651,000 people were employed and 2,728,000 were unemployed. The
unemployment rate among the labor force is 6.6%.
37, 38
35
Asia Development Bank 2015. Key Indicators for Asia and the Pacific 2015.
http://www.adb.org/sites/default/files/publication/175162/phi.pdf
36
All persons who are 15 years old and over and are reported as (1) without work, (2) currently
available for work, and (3) seeking work or not seeking work due to valid reasons.
37
Proportion of people who are both jobless and looking for a job.
38
Asia Development Bank 2015. Key Indicators for Asia and the Pacific 2015.
http://www.adb.org/sites/default/files/publication/175162/phi.pdf
0
10
20
30
40
50
60
1981 1985 1988 1990 1991 1992 1994 1996 1997 1998 1999 2000 2002 2003 2004 2006 2007 2008 2009 2010 2011 2012
Philippines Cambodia Lao PDR Thailand Vietnam

16
Chapter 3 Overview of the Health Sector
3-1 Health System with a Focus on Maternal and Child Health
(1) Health Governance
The Philippine health system is comprised of five administrative bodies. The Department
of Health (DOH) in the central government is in charge of the development of policies,
regulations and guidelines, and the provision of tertiary health care. The provincial
governments are responsible for secondary health care, and the municipal/city
governments are in charge of primary health care. The general term for a provincial
government and a municipal/city government is a local government unit (LGU). Each
municipality/city is divided into barangays and the barangay health station (BHS) provides
public health services as the closest facility to the people.
In principle, LGU health personnel are employed and deployed by the LGUs. However,
LGU health facilities also have human resources assigned by DOH, such as Development
Management Officers (DMOs) who provide technical assistance to the municipalities, and
monitor and report DOH programs, Nurses and Midwives posted at Rural Health Units
(RHUs) and BHSs.
Figure 3- 1 Health Governance Structure in the Philippines
Source: Global Link Management
There are two types of health service networks in the Philippines, namely Inter Local
Health Zone (ILHZ) and Service Delivery Network (SDN). ILHZ was adopted in the
Philippines based on the District Health System
39
advocated by World Health
Organization (WHO) in 1986, aiming at promoting coordination between the primary
39
The means to achieve the end of an equitable, efficient and effective health system based on the
principles of the primary health care (PHC) approach.
DOH
DOH Regional
Offices
Provincial Health
Offices
Municipal/City Health Offices
Barangay
Policy formulation, Guidance, Tertiary
Health Care Providsion: Specialty,
Regional & Training Hospitals
Primary Health Care
Provision: BHS
Secondary & Primary &Health
Care Provision: Minicipality/City
Hospitals, RHU, Infirmary
Secondary Health Care Provision:
Provincial & Distrcit Hospitals
Development
Management Officers
Nurse/ Rural Health
MW Deployment
Program

17
health facilities and the referral hospitals within the multiple LGUs in order to ensure the
access of communities to better health services. Meanwhile, SDN was announced in
Administrative Order No. 2014-0046 in 2014 during the Aquino Administration as a health
service networking system established by the provincial or municipal government with the
participation of the private sector. DOH reportedly planned to redefine the detail roles and
functions of SDN in 2016 and scale up its implementation nationwide.
40
DOH uses the LGU Health Score Cards with 30 indicators (see Attachment 5) as a tool of
Monitoring & Evaluation on Equity & Effectiveness for each local health system. DOH
requires LGUs to develop a three-year plan called the Local Investment Plan for Health
(LIPH). The LIPH was introduced in 2014 to strengthen local health planning with
significant consideration for building the capacities of health managers in the local
government units (LGUs). The Annual Operational Plan (AOPs) is prepared every year of
the planning cycle and the Service Level Agreement is signed. The results of the LGU
Score cards are primarily used for the planning process. For LGUs whose scores of
selected LGU Score Card indicators are positive, performance based grants are provided
by the Bureau of Local Health Development, DOH. The data for LGU Score Cards are
collected by the Department of Interior and Local Government (DILG) staff that have
offices at the municipality/city level.
41,42
(2) Health Policies
Under the Aquino Administration, the Government of the Philippines placed Universal
Health Care (Kalusugan Pangkalahatan, known as KP) as a principle of national health
policy and promoted to achieve the Millennium Development Goals (MDGs).
The new Duterte Administration recently presented the Philippine Health Agenda
2016-2022, as shown in BOX 3- 1.
40
Interview with the Bureau of Local Health Systems Development, DOH (August 5, 2016).
41
Interview with the Department of Interior and Local Government (August 1, 2016).
42
Interview with the Bureau of Local Health Systems Development, DOH (August 5, 2016).

18
BOX 3- 1 Philippines Health Agenda 2016-2022
~ All for Health towards Health for All ~
Goals:
1. Ensure the best health outcomes for all, without socio-economic,
ethnic, gender and geographic disparities
2. Promote health and deliver healthcare through means that
respect, value and empower clients and patients as they interact
with the health system
3. Protect all families especially the poor and vulnerable against the
high cost of healthcare
Values: Equity, quality, efficiency, transparency, accountability,
sustainability and resilience
Guarantees:
1. Population- and individual-level interventions for all life stages
*
that promote health and wellness, prevent and treat the triple
burden of diseases,
**
delay complications, facilitate rehabilitation and provide palliation
2. Access to health interventions through functional Service Delivery Networks (SDNs)
***
3. Financial freedom when accessing these interventions through Universal Health Insurance
Strategy:
dvance Quality, Health Promotion and Primary Care
over all Filipinos against Health-Related Financial Risk
arness the Power of Strategic Human Resources for Health Development
nvest in eHealth and Data for Decision-Making
nforce Standards, Accountability, and Transparency
alue All Clients and Patients, especially the Poor and Vulnerable
licit Multi-sectoral and Multi-stakeholder support for Health
*
All Life Stages refers to services for pregnant women, children, adolescents, adults and older persons.
**
Triple Burden of Disease pertains to the (1) communicable diseases and neglected tropical diseases, (2)
non-communicable diseases, and (3) problems related to globalization, urbanization and
industrialization, including injuries and mental illness.
***
SDNs 1) consist of primary care networks (PCNs) linked to Level 3 hospitals, 2) ensure well-equipped
and fully-staffed network of health facilities, 3) render services that are compliant with clinical practice
guidelines and 4) practice gatekeeping and utilize telemedicine to expand specialty service.
Source: DOH Office of the Secretary & DOH Health Policy Development and Planning Bureau. (2016).
Philippine Health Agenda 2016-2022 Healthy Philippines 2022.
The Philippine government agencies, including DOH, determine their agenda through the
cabinet secretaries for approval of the President based on his 10-point socioeconomic
agenda (see BOX 3- 2). This 10-point agenda is the basis for the Philippine Development
Plan, the country’s multi-sectoral development plan. The Philippine Health Agenda
contributes to numbers 7 and 10 of the 10-point agenda. The Philippine Health Agenda
A
C
E
V
E
I
H
STRATEGY
GOALS + VALUES
3 GUARANTEES
Service Delivery Network
All Life Stages &
Trip le Burden of Diseases
Universal Health Insurance

19
2016-2022 will be part of the Philippine Development Plan 2017-2022, under the Chapter
on Social Development.
43
BOX 3- 2 The 10-point Socioeconomic Agenda of President Duterte
1. Continue and maintain current macroeconomic policies, including fiscal, monetary, and trade
policies.
2. Institute progressive tax reform and more effective tax collection, indexing taxes to inflation.
A tax reform package will be submitted to Congress by September 2016.
3. Increase competitiveness and the ease of doing business. This effort will draw upon successful
models used to attract business to local cities (e.g., Davao) and pursue the relaxation of the
Constitutional restrictions on foreign ownership, except as regards land ownership, in order to
attract foreign direct investment.
4. Accelerate annual infrastructure spending to account for 5% of GDP, with Public-Private
Partnerships playing a key role.
5. Promote rural and value chain development toward increasing agricultural and rural enterprise
productivity and rural tourism.
6. Ensure security of land tenure to encourage investments, and address bottlenecks in land
management and titling agencies.
7. Invest in human capital development, including health and education systems, and match skills
and training to meet the demand of businesses and the private sector.
8. Promote science, technology, and the creative arts to enhance innovation and creative capacity
towards self-sustaining, inclusive development.
9. Improve social protection programs, including the government’s Conditional Cash Transfer
program, to protect the poor against instability and economic shocks.
10. Strengthen implementation of the Responsible Parenthood and Reproductive Health Law to
enable especially poor couples to make informed choices on financial and family planning.
Moreover, the new administration prioritizes the 20 High Poverty Sites (see Table 3- 1) for
development efforts and encourages development partners to provide assistance to the
selected provinces.
43
Information shared by Chief of Health Planning Division, Health Policy Development and Planning
Bureau, DOH (October 31, 2016).
20
Table 3- 1 20 High Poverty Sites
Source: Department of Health. (2016). 20 High Poverty Sites.
(3) Health Financing
Table 3- 2 shows the current circumstances surrounding health financing in the
Philippines.
Table 3- 2 Health Financing in the Philippines
Source:
a
World Population Prospects (2015),
b
World Development Indicator (2016),
c
Department of Budget and Management website (2016) and
d
Philippine Health Accounts Based on the 20111
System of Health Accounts for CY 2012, 2013 and 2014 (2016)
CAR: Apayao
Ilocos Region: Pangasinan
Carabarzon Region: Quezon
Bicol Region: Masbate, Camarines Sur
Western Visayas Region: Negros Occidental, Ilo-ilo
Central Visayas Region: Cebu
Eastern Visayas Region: East Samar, North Samar, North Leyte
Zamboanga Peninsula Region: Zamboanga Del Sur, Zamboanga Del Norte
Northern Mindanao Region: Camiguin
Davao Region: Davao Del Sur
Soccsksargen Region: North Cotabato, Saranggani
ARMM: Sulu, Maguindanao, Lanao Del Sur
1 Macroeconomic Indicator
Population (million)
a
96.0 97.6 99.1
GDP (100 million US$)
b
2,501 2,719 2,848
GDP per capita (US$)
b
2,605 2,787 2,873
2 Government Budget
Total Government Budget (100 million US$)
c
296 323 363
Total Government Budget as % of GDP 11.8% 11.9% 12.7%
3 Government Budget for Health
Govt Budget for Health (100 million US$)
c
10.2 12.0 19.0
Govt Health Budget as % of GDP 0.4% 0.4% 0.7%
% of Total Government Budget 3.4% 3.7% 5.2%
4 Government Expenditure on Health
Total Health Expenditure (THE) (100 milllion US$)
d
108.8 123.8 127.7
THE as % of GDP 4.4% 4.6% 4.5%
5 Disbursement of THE (100 million US$)
d
Share Share Share
Government 30.8 28.3% 38.0 30.7% 39.5 30.9%
Central Government 11.1 10.2% 15.2 12.3% 12.3 9.6%
LGUs 7.2 6.6% 8.5 6.9% 8.4 6.6%
Social Security 12.5 11.5% 14.3 11.6% 18.8 14.7%
Other Government 0.03 0.03% ― ―
Private Insurance 9.4 8.6% 10.8 8.7% 11.5 9.0%
Other Private Corporation 4.6 4.2% 5.0 4.0% 4.6 3.6%
Out-of-Pocket Expenditure 64.0 58.8% 69.9 56.5% 72.0 56.4%
2012
2013
2014

21
The substantial government budget increase in 2014 derives from the increased tax income
due to the Sin Tax Reform Law of 2012. From 2012 to 2014, the Social Security budget
steadily increased, while private insurance slightly increased. In 2014, about 30 percent of
total health expenditure was from the Government, 9.6 percent of which was the Central
Government, 6.6 percent LGUs and 14.7 percent Social Security, while 9.0 percent
accounted for private insurance, 3.6 percent for private corporations, and 56.4 percent from
household out-of-pocket expenditure. The total health expenditure as percentage of GDP in
the Philippines is lower than most developed countries; but is comparable to other
Southeastern Asian countries (see Figure 3- 2). The Philippines’ out-of-pocket expenditure
out of the total health expenditure was higher than many Southeast Asian countries from
2000 to 2014 and the proportion has not decreased over the years (see Figure 3- 3).
Figure 3- 2 Health Expenditures, total (% of GDP)
Source: The World Bank. (2016). World Development Indicators.
Figure 3- 3 Out-of-Pocket Health Expenditure
(% of total health expenditure on health)
Source: The World Bank. (2016). World Development Indicators.
0.0
2.0
4.0
6.0
8.0
10.0
12.0
14.0
16.0
18.0
2000 2010 2014
0.0
10.0
20.0
30.0
40.0
50.0
60.0
70.0
80.0
90.0
2000 2010 2014
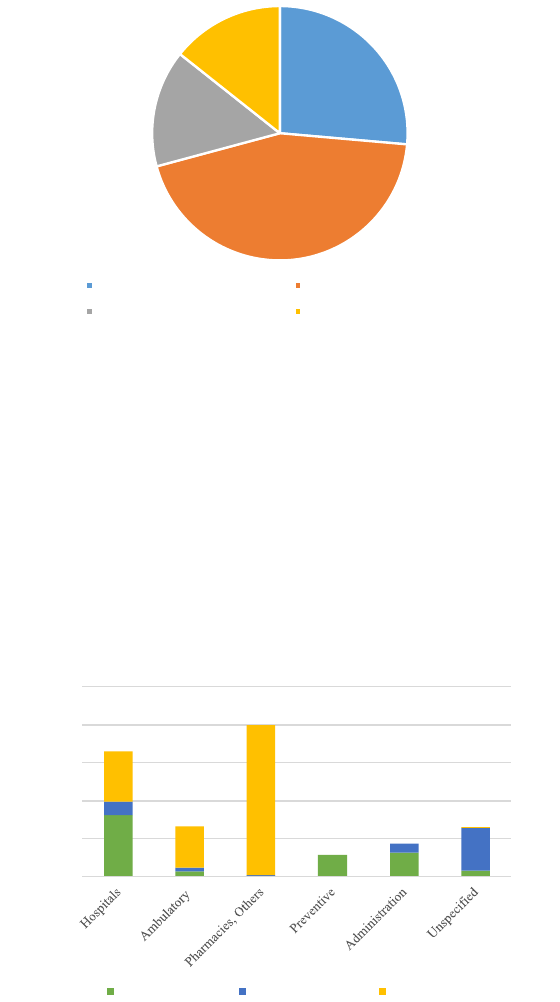
22
① Health Expenditure
Figure 3- 4 shows the breakdown of health expenditure in 2014. Pharmaceuticals account
for 44.4 percent, the largest portion, followed by compensation of employees, which
accounts for 26.4 percent, and these two categories account for over 70 percent of the total
health expenditures in the Philippines.
Figure 3- 4 2014 Health Expenditures by Factors of Health Care provisions
Source: Philippine Health Accounts Based on the 20111 System of Health Accounts
for CY2012, 2013 and 2014 (2016).
Figure 3- 5 shows Health Expenditures by Health Services and Health Financing Schemes
in 2014. Nearly 200 billion pesos was estimated to have been spent in pharmacies in 2014
and more than 99% of which was paid by household out-of-pocket. Similarly, a relatively
high portion, 82.5 percent, of ambulatory or outpatient health care services were paid by
household out-of-pocket. The high burden on the household out-of-pocket in these
expenditures can be explained by the fact that the NHIP does not cover these costs.
Figure 3- 5 2014 Health Expenditures by Health Services
and Health Financing Schemes (in million pesos)
Source: Philippine Health Accounts Based on the 20111 System of Health Accounts
for CY 2012, 2013 and 2014 (2016).
26.4%
44.4%
14.9%
14.3%
Compensation of exployees Pharmaceuticals
Other materials and services used Unspecified
0
50000
100000
150000
200000
250000
Government/NHIP Voluntary Insurance Household

23
Figure 3- 6 shows health expenditures by income quintile groups in the Philippines from
2012 to 2014. Over the three years, the health expenditures of all groups increased,
however, the health expenditure of the richest income group increased the most from 2013
to 2014. Moreover, throughout the three-year period, the lower three income quintile
groups accounted for less than their equal share, while the richest income group accounted
for more than twice its equal share.
Figure 3- 6 Health Expenditures by Income Quintile Group:
the Philippines, 2012-2014 (in million pesos)
Source: Philippine Health Accounts Based on the 20111 System of Health Accounts
for CY 2012, 2013 and 2014 (2016).
Figure 3- 7 Health Expenditures by Income Quintile Group and Health Financing
Schemes: the Philippines, 2012-2014 (in million pesos)
Source: Philippine Health Accounts Based on the 20111 System of Health Accounts
for CY 2012, 2013 and 2014 (2016).
0 50,000 100,000 150,000 200,000 250,000
Philippines
Not Specific
(
top
)
Q5
Q4
Q3
Q2
(
bottom
)
Q1
2014 2013 2012
0 50,000 100,000 150,000 200,000 250,000
2014
2013
2012
2014
2013
2012
2014
2013
2012
2014
2013
2012
2014
2013
2012
2014
2013
2012
2014
2013
2012
Philippines
Not
Specific
V
(top)
IV III II
I
(bottom)
Government/NHIP
Voluntary Insurance Household

24
Figure 3- 7 shows health expenditures by income quintile groups and health financing
schemes. The overall health expenditures in the Philippines have increased from 2012 to
2014; however, the health financing schemes for the increased amounts differ among the
income quintile groups. For the lowest quintile group, household out-of-pocket payment
has not changed and voluntary insurance has slightly increased, while the government
expenditures, including the National Health Insurance Program (NHIP), has substantially
increased. Although PhilHealth announced that it would increase the Indigent Members to
more than 40 percent of the total population in 2014,
44
the increase in the government
health expenditures for the second quintile group was not seen. On the other hand, the
government expenditure for higher quintile groups is not as much as the lowest quintile
group, and the level of increase in the government expenditure for the higher quintile
groups over the three years was also minimal. The increase in the higher quintile groups’
health expenditure derives from household out-of-pocket.
Figure 3- 8 Health Expenditures by Disease Groups and Health Financing Schemes:
the Philippines, 2014 (in million pesos)
Source: Philippine Health Accounts Based on the 20111 System of Health Accounts
for CY 2012, 2013 and 2014 (2016).
Figure 3- 8 shows health expenditures by disease groups and health financing schemes.
Expenditures for noncommunicable diseases took the largest share of health expenditures
in 2014 at about one-third, followed by infectious diseases and reproductive health. The
proportion of household out-of-pocket expenditure was generally high, but injuries were
mostly paid by households due to the fact that they are rarely covered by insurance. The
proportion of donor assistance is generally small and limited to infectious diseases and
reproductive health.
44
PhilHealth. (2014). 2014 Stats and Charts.
0 40000 80000 120000 160000 200000
Others
Non-disease Specific
Injuries
Non-communicable Diseases
Nutritional Deficiencies
Reproductive Health
Infectious Diseases
The Government/NHIP
Donor Voluntary Insurance Household

25
Figure 3- 9 Health Expenditures by Specific Disease Groups and
Health Financial Schemes: the Philippines, 2014 (in million pesos)
Source: Philippine Health Accounts Based on the 20111 System of Health Accounts
for CY 2012, 2013 and 2014 (2016).
Figure Figure 3- 9 shows health expenditures by specific disease groups and health
financing schemes in 2014. Expenditures for respiratory infections took the largest share
that accounts for 38 percent of the total health expenditures for infectious diseases. The
majority of expenditures for vaccine-preventable diseases came from the government, but
expenditures for other diseases were largely paid by household out-of-pocket. Regarding
reproductive health, the majority of health expenditures for maternal conditions are paid by
health insurance, but the household out-of-pocket payment rates are high for perinatal
conditions due to limited insurance coverage for new-born cares. Among the
non-communicable diseases, the household out-of-pocket rate is highest for endocrine and
metabolic disorders at 81.1 percent.
② Health Budget
[Central Government]
Government health expenditures are funded out of general tax revenues collected by the
Department of Finance (DOF). The DOH and the Philippine Health Insurance Corporation
(PhilHealth) are allotted annual budgets by the Department of Budget and Management
(DBM). The annual process of developing a DOH budget starts with the issuance of the
0 10000 20000 30000 40000 50000 60000 70000 80000 90000 100000
Others
Non-disease specific
Injuries
Other non-communicable diseases
Nephritis
Mental & neurological conditions
Cardiovascular diseases
Endocrine and metabolic disorders
Neoplasms
Unspecified reproductive health conditions
Perinatal Conditions
Maternal Conditions
Other infectious diseases
Vaccine preventable diseases
Neglected tropical diseases
Diarrheal diseases
Respiratory infections
HIV/AIDS, STD, TB & Malaria
Non-communicable
Diseases
Reproductive
Health Infectious Diseases
The government/NHIP
Donor Voluntary insurance Household

26
budget call and the budget ceilings by DBM around late February to the middle of March.
DOH then prepares the annual budget proposal based on these set ceilings. The DOH
proposal is consolidated into a national expenditure program, along with other line
ministries’ proposals, that is submitted to congress.
45
In 1991, the management of provincial, district, and municipal hospitals as well as primary
care facilities was transferred to LGUs. However, specialty hospitals, regional and training
hospitals, and sanitaria
46
were retained under the management of the central DOH. While
DOH-retained hospitals continue to be managed by the central DOH, they are also given
authority to set and collect user fees with a ceiling for mark ups to a maximum of 30
percent of actual cost.
47
Figure 3- 10 shows the health budget of 2011 to 2015 by the factors of health care
provision. The substantial government budget increase, particularly the budget for health
promotion and preventive medicine, since 2014 derives from the increased tax income due
to the Sin Tax Law of 2012. The reason that only the budget for health promotion and
preventive medicine increased was that health insurance subsidy is included in the budget
for health promotion and preventive medicine, rather than that for curative medicine.
Figure 3- 10 Breakdowns of Health Budget, 2011-2015 (in pesos)
Source: DOH Annual Budget 2011-2015.
45
The Philippines Health System Review 2011.
46
Health facilities for the recuperation and treatment of individuals with leprosy.
47
The Philippines Health System Review 2011.
0 20,000,000 40,000,000 60,000,000 80,000,000 100,000,000
2011
2012
2013
2014
2015
Health Promotion & Preventive Medicine Curative Medicine
Health Administration

27
Table 3- 3 Distribution of Sin Tax Incremental Revenue
in FY 2016 DOH Budget Proposal
Prescribed
Allocation
Detail of Prescribed Allocation
Allocation
(in billion pesos)
%
Universal
Health Care
(80%)
Enrollment coverage of the poor (supporting NHIP premium)
31.26
45
Health policy, regulations, general administration
7.56
11
Hospital operations
6.41
9
Health facilities enhancement including capital outlay of
DOH hospitals
5.46
8
Attainment of MDGs
4.24
6
Quick response fund
0.51
1
Health awareness program
0.04
0.06
Subtotal
55.48
80
Medical
assistance
and facility
enhancement
(20%)
Facility enhancement
7.96
11
Enhancement of doctors to remote areas
4.16
6
Medical assistance to indigent patients confined in
government hospitals
1.91
3
Subtotal
14.03
20
Total
69.51
100
Source: DOH. Sin Tax Law Incremental Revenue for Health, Annual Report CY 2015.
In December 2012, the reformed Sin Tax Law, which increased taxes on all tobacco and alcohol
products was passed. 85% of the incremental revenue from reformed Sin Tax Law was
earmarked for DOH, 80 percent of which is to be transferred to PhilHealth in order to promote
the initiative of Universal Health Care under the previous administration (promotion of NHIP,
achievement of MDG goals, increasing health awareness, etc.). The remaining 20% is to be used
to finance medical assistance and facility enhancements.
48
Table 3- 3 summarizes the allocation
of the Sin Tax increments in the 2016 DOH budget proposal. DOH’s budget increase
attributable to Six Tax increment revenue was first seen in 2014.
[Local government Units]
Provincial and district hospitals are funded out of the provincial government’s budget
while municipal/city hospitals are financed by the municipal/city budgets. Financial
management is determined primarily by the local chief executive and the local hospital
chief.
49
Local health expenditures are funded from a variety of sources, including the Internal
Revenue Allotment (IRA) from the national government, the LGU’s own budgets, user
fees, transfers from DOH, PhilHealth, congressional discretionary funds, such as Priority
Development Assistance Funds and the Philippine Charity Sweepstakes Office, and the
48
DOH. (2016). Sin Tax Law Incremental Revenue for Health, Annual Report CY 2015.
49
The Philippines Health System Review 2011.

28
Bottoms-up Budgeting, initiated by the Aquino administration, to provide additional
assistance to poor LGUs in class 4 to 6.
50,51
The health financing system is complex and
uncoordinated.
The LGU budget calendar is governed by a Local Budget Memorandum and typically
issued in the middle of June by DBM. Following the process prescribed by DBM, each
local health office and facility prepares a medium-term strategic plan and an annual health
plan to be submitted for review.
52
These plans are meant to be consistent with the LIPH.
53
DBM issues the budget notification stating the Internal Revenue Allotment (IRA), which is
part of the tax revenue automatically released by the national government to LGUs on a
quarterly basis. The IRA is first subdivided among the different levels of LGUs using the
following distribution: provinces 23 percent, cities 23 percent, municipalities 34 percent,
and barangays 20 percent. The shares for each level of LGU are then allocated horizontally
for provinces, cities and municipalities based on the following formula: population 50
percent, land area 25 percent and equal sharing 25 percent. For barangays, the horizontal
sharing is based on population for 60 percent and equal sharing for 40 percent. However,
past studies have suggested that the formula for distributing the IRA across the different
levels of LGUs has been inconsistent with the distribution of expenditure responsibilities
among the different levels (see Figure 3- 4).
54
Table 3- 4 IRA Distribution vs. Estimated Share of Devolved Functions
Source: World Bank. (2011). Philippines: Study on Local Service Delivery.
DOH transfers have come through direct subsidies, in-kind transfers, that is public health
commodities such as vaccines, and grants for national programs, such as maternal and
50
LGUs are divided into income classes according to their average annual income during the previous
four calendar years.
51
Interview with the Department of Interior and Local Government (August 1, 2016).
52
World Bank. (2011). Philippines: Study on Local Service Delivery.
53
Bureau of Local Health Systems Development (BLHSD) DOH & UNICEF. (2015). Local Investment
Planning for Health Handbook on Principles, Guidelines, Procedures, and Processes.
54
World Bank. (2011). Philippines: Study on Local Service Delivery.
% IRA Share % Share of Devolved Functions
Provinces 23% 46%
Cities 23% 7%
Municipalities 34% 46%
Barangays 20% Undefined
29
child health. For PhilHealth, transfer comes to health facilities to reimburse the medical
costs of the members
55,56
Table 3- 5 Local Taxes
Source: World Bank. (2011). Philippines: Study on Local Service Delivery.
X Types of local tax assigned to LGUs
* Local tax allocated from a higher LGU to a lower LGU
Table 3- 5 summarizes the various taxes that are assigned to LGUs by Local Government
Code 1991 (LGC). Cities are assigned with the widest range of taxes available, while
provinces and municipalities have either no access to certain tax measures or are required
to share the proceeds with sub-levels of LGUs. Cities are generally allowed higher tax rate
ceilings compared to provinces and municipalities, and their urbanized economies serve as
larger and more dynamic tax bases. As a result, on average, cities rely much less on the
IRA and other transfers compared to municipalities and provinces (see Table 3- 6).
57
Table 3- 6 2003-2007 Case Studies of Visaya and Luzon:
LGU Annual Income Breakdowns
Source: World Bank. (2011). Philippines: Study on Local Service Delivery.
55
PhilHealth reimburses health facilities in two checks: 1) addressed to the facility as payment for
procedures and supplies (drugs, medical supplies, laboratory, room and board), and 2) addressed to the
facility chief as payment for professional fees.
56
World Bank. (2011). Philippines: Study on Local Service Delivery.
57
ibid
Local Tax Cities Provinces Municipalities Barangays
On Real Property Transfers X X
On Business of Printing and Publication X X
On Franchises X X
On Sand, Gravel, and other Quarry Resources X X
* *
On Amusement Places X X
*
On Professionals X X
On Delivery Vans Trucks X X
On Real Property X X
* *
On Idle Lands X X
On Businesses X X X
On Community Tax X X *
Provinces Cities Municipalities
IRA & Other Transfers 83.0 43.8 78.7
Own-source Revenues 15.1 53.7 19.6
-Tax revenues 8.8 43.0 12.1
-Non-tax revenues 6.3 10.7 7.6
Loans 1.9 2.5 1.6

30
While the national average of health expenditures out of total budget of LGU is 18.6
percent, the World Bank’s case study of LGU health care expenditures
58
has shown that
there is a considerable divergence in spending levels among the different levels of LGUs
from 6.3 percent in a city to 39.4 percent in a province in Luzon; as well as different
provinces: from 20.1 percent in a Visaya province to 39.4 percent in a Luzon province.
The difference derives from the presence/absence of a tertiary provincial hospital with its
higher cost implications. It was reported by DOH that health expenditures per capita were
8.5 percent greater for provinces that operated a tertiary hospital compared to those where
DOH continued to operate the tertiary hospitals.
Despite the fact that LGUs allocate the majority of the health sector budget to payment for
personnel salaries, wages and benefits, LGUs often have difficulty maintaining the level of
staff minimally accepted by DOH. In order to mitigate the problem of under-funding and
under-staffing, the LGU health facilities could charge user fees. However, in practice, the
local chief executives and Local Council are reluctant to raise rates.
59
Devolution has created a fragmented health system. The typical planning and budgeting
process has become compliance-oriented rather than needs-oriented. Budgetary decisions
are in the hands of the local chief executives and the LGU accounting officers, and
participation of the local health officials is minimal. Consequently, it is questionable
whether the resource allocations for health are reflective of actual health needs of the
LGUs.
③ Health Financing Flow
Figure 3-11 shows revenue sources and flows within the public health system in the
Philippines. DBM transfers the general tax revenues collected by the DOF to DOH,
PhilHealth, as well as LGU. DOH further distributes the budget to the DOH-retained
hospitals and LGUs that operate hospitals and other health facilities. PhilHealth, Health
Maintenance Organizations (HMOs) and other private insurance companies reimburse the
accredited health facilities for healthcare costs of the members, and households are
responsible to pay for health expenses not covered by health insurance.
58
World Bank. (2011). Philippines: Study on Local Service Delivery & Bureau of Local Government
Finance. (2007).
59
World Bank. (2011). Philippines: Study on Local Service Delivery.

31
Figure 3- 11 Revenue sources and flows within the public health system
in the Philippines
Source: The Philippines Health System Review (2011) & Philippines: Study on Local Service Delivery (2011)
(4) Health Facilities and MCH Service Delivery
Table 3- 7 shows the public health facilities under DOH, province and municipality/city.
The private sector plays an important role for the provision of health services in the
Philippines. While it is reported that the number of beds is almost equal for private and
public facilities, 763 out of 1,971 hospitals (38.7 percent) are public and 1,208 hospitals
(61.3 percent) are owned by the private sector.
60
Table 3- 7 Public health facilities
Responsible entity
Health facility
DOH
National, specialized and regional hospitals
Provincial government
Provincial and district hospitals, and other health facilities, e. g. infirmary
61
Municipal/City government
Municipal/City hospitals, RHU, BHS and other health facilities, e. g. infirmary
Source: JICA Survey Team
The Philippine health facilities are classified as hospitals and non-hospitals on a basis of the
functions. Moreover, hospitals are classified into Level 1 to Level 3 hopitals. Non-hospitals
include infirmaries and birthing homes. The basic functions of each health facility determined
by DOH is shown in Table 3-8.
60
The Philippines Health System Review 2011.
61
Infirmary is the facility not certified as DOH level 1-3 hospitals but with beds.
DOH
DBM
DOF
PhilHealth
Firm
Household
LGU
Healthcare
Providers
Donors
HMOs &
Privare
Insurance
Legend
Budget
Tax
Premiums
Reimbursement
User fees

32
Table 3- 8 Basis Functions of Health Facilities
Health facility
Functions
Non-hospitals
Ambulatory care and basic health care including normal spontaneous delivery
is provided. The average period of hospitalization is 1 to 3 days.
Level 1 Hospitals
Health care in the areas of internal medicine, pediatrics, obstetrics and
gynecology, (including cesarean section), ssurgery, dentistry and emergency
medical care are provided. Pharmacy, secondary clinical laboratory (DOH
standard), primary image analysis laboratory and/or blood station
62
are often
attached.
Level 2 Hospitals
In addition to the health care provided by the Level 1 Hospitals, specialists
are assigned to each diagnosis and treatment department. ICU, pediatric ICU,
respiratory therapy, tertiary clinical laboratory, and secondary image analysis
laboratory are attached.
Level 3 Hospitals
In addition to the health care provided by the Level 2 Hospitals, dialysis
clinic, rehabilitation center, blood bank, tertiary clinical laboratory and
tertiary image analysis laboratory are attached. It is also functioned as a
training institution.
Source: JICA Survey Team
Table 3- 9 Major MCH services by various health facilities
Facility
MCH services
Human resource
BHS
ANC, immunization, health education,
consultation, referral
Nurse, midwife (RHU personnel make
regular visit where there are no personnel
stationed at BHS), Barangay Health
Worker (BHW), Barangay Nutrition
Scholar
RHU
In addition to BHS services, laboratory
test (no ultrasound), normal delivery
(at selected RHUs), PNC
Doctor (mainly internal medicine), nurse,
midwife, lab technician, etc.
Municipal/
District/Provin
cial Hospital,
Infirmary
ANC, normal delivery, PNC,
laboratory test and others as delivered
at BHS/RHU.
Accredited with BEmONC and
HIP-MCP. Caesarean Section can be
conducted where/when the obstetrician
and anesthetist are available.
Doctor, nurse, midwife, lab technician etc.
Regional
Hospital
All services are provided at two
regional hospitals as CEmONC.
Obstetrician, anesthetist, pediatrician,
nurse, midwife, paramedical etc.
Source: JICA Survey Team
Table 3-9 shows MCH services provided at each level of facility and the personnel serving
the services. In the Philippines, one can seek health care at any level of facility without a
medical referral letter. Generally, an expectant mother is to receive ANC at the nearest
62
At a bank station, whole blood and concentrated red blood cells are stored and provided, and red blood
cells fit inspection is performed. Whereas at a blood bank, all blood components are stored and provided,
and red blood cells fit inspection, red blood cells antibody screening, transfusion reaction test and
transfusion safety monitoring test are performed. (Administrative Order No. 2001-0008, Rules and
Regulations Governing the Regulation of Blood Service Facilities)

33
BHS, RHU or private clinic, and deliver a child at a RHU with a lying-in facility, a
municipal hospital or a district hospital for normal spontaneous delivery. A high-risk
expectant mother delivers at a Comprehensive Emergency Obstetric and Newborn Care
(CEmONC) facility, such as a provincial hospital or a regional hospital. However, it is not
uncommon, especially in urban areas, that an expectant mother receives ANC and performs
normal spontaneous delivery at a tertiary health facility.
Barangay Health Workers (BHWs) are trained health volunteers to provide basic health
care in a community. They receive fixed amount of rewards from barangay. They visit
households on a regular basis and record the information of the household members, check
with expectant mothers, mothers and infants, follow them up after they receive health care,
provide them with health information and advice, and refer them to health facilities when
necessary. Meanwhile, some women still deliver a child at home attended by a traditional
birth attendant (TBA).
(5) Health-related Information
There exist a variety of information systems dedicated to the Philippine health sector. The
basic health data on health service delivery and selected program accomplishment at the
barangay, municipality/city, provincial and regional levels are collected through the Field
Health Service Information System (FHSIS) developed by DOH. The fundamental building
block of the FHSIS is the Recording Forms and Reporting Forms for the DOH and LGU
staff with managerial or supervisory functions in facilities and program areas. The second
building block of the FHSIS is the Target Client Lists (TCL) for nurses/midwives with
planning and operation of patient care, monitoring and supervision of service delivery
activities, reporting of delivered services, and clinic-level data provided for further studies.
There are various kinds of TCLs including those in areas of Prenatal Care, Post-Partum Care,
Under 1-Year-Old Children, Family Planning, Sick Children, National TB Program Register,
and the National Leprosy Control Program. Midwives in BHS collect this data on a monthly
basis and consolidate it in the Summary Table composed of (1) Health Program
Accomplishment and (2) Morbidity Disease.
63
Institutional delivery is usually recorded on a basis of where a woman delivers a child in
FHSIS. However, the JICA project in CAR encouraged the health workers to record
institutional delivery on a basis of where a woman lives. Likewise, the project team also
63
Scribd. The field health service information system (FHSIS)
https://ja.scribd.com/doc/27872414/The-field-health-service-information-system-FHSIS

34
instructed them not to use an estimated number of expectant and nursing mothers, but use a
real number as a denominator of a consultation rate of ANC and PNC. These efforts
enabled them to understand the real situation of maternal and child health. Today, DOH is
introducing the above efforts to other areas of the country.
A census is conducted every ten years by Philippine Statistics Authority (PSA).
64
Although the first Census was conducted in 1878 by the colonial Spanish government, the
regular practice was adopted in 1960, and an inter-censal survey was added in 1995. The
last Census was conducted in 2010 and the inter-censal survey measured the size of the
population in 2015. The public-school teachers are assigned to collect data in the Census
and the PSA staff train and supervise them at the Regional, Provincial, and Municipal/City
levels. The households are enumerated based on the information obtained through Local
Chief Executives and Barangay Captains. PSA establishes the Census Board some time
before the data collecting period and tasks the Barangay Captains to confirm households in
their barangays. For migrants and people living on the streets, data collectors visit them on
an ad hoc basis. For overseas migrant workers, the data collectors ask each household
whether there is any household member working overseas and count the person if he/she
stays overseas shorter than five years.
65
The Vital Statistics Division of PSA provides DOH with the data of births and deaths. A
Birth Certificate has to be submitted to the Local Civil Registry Office in the
municipal/city office within 30 days and registered within six weeks after the birth.
Likewise, a Death Certificate has to be submitted to the Local Civil Registry Office in the
municipal/city office within 48 hours and registered within 30 days after the death. PSA
only provides supervision to the Local Civil Registry Office, and the registration is
managed by LGUs. For indigenous people, the Local Civil Registry Office goes to their
residential area and resisters them. For people living on the streets, the Department of
Social Welfare and Development (DSWD) does the registration. According to the Census
2010, 93.5 percent of births and 66.0 percent of deaths had been registered. Vital statistics
were initiated in 1939 and became computerized in 2000 in the Philippines.
66
The National Demographic and Health Survey (NDHS), globally known as the
Demographic and Health Survey (DHS), also provides DOH with health information with
64
On the basis of the Philippine Statistical Act of 2013 (Republic Act No. 10625), National Statistics
Office, National Statistical Coordination Board, Bureau of Agricultural Statistics and Bureau of Labor
and Employment Statistics were merged to be National Statistics Authority.
65
Interview with the Population and Housing Census Division, PSA (October 7, 2016).
66
Interview with the Vital Statistics Division, PSA. (August 1, 2016).

35
a specific focus on reproductive health. The enumeration is conducted based on the Census
data. The latest NDHS 2013 used the Census 2000. The data collectors are called for each
survey and trained by ICF International, supervised by the PSA staff. The contents of the
questionnaires are modified on the basis of requests by the United States Agency for
International Development (USAID), the sponsor of NDHS, and the Philippine
government. The survey is usually conducted every five years, but the next NDHS survey
will be conducted in 2017, one year earlier than originally scheduled, as the government
wishes to collect the SDG baseline data through the NDHS results.
67
Other health-related information sources include the Family Income and Expenditure
Survey (FIES) and Small Area Estimates (SAEs) conducted by PSA. There is also the
community-based household information system called the Household Profile, primarily
developed for the community-based monitoring system in which community health teams
(CHTs) are engaged. The Household Profile will be collected by Barangay Health Workers
(BHWs) in the future.
68
3-2 Maternal and Child Health Conditions
(1) Maternal conditions
Although a decline of the Maternal Mortality Ratio (MMR) has been observed in the
Philippines since 1990, it has slowed done in recent years. The MMR was estimated at 112
per 100,000 live births in 2015,
69
which was higher than the MDG target of 52 per
100,000 live births.
70
There are regional disparities exist according to the available
information from the DOH at the regional level.
71
With regard to antenatal care (ANC), nationally 95 percent of pregnant women received at
least one ANC from skilled providers in 2013, which is an increase from 2008 at 91
percent. Facility-based delivery (FBD) at the national level also improved from 44 percent
in 2008 to 61 percent in 2013 and 72 percent of mothers received post-natal care (PNC)
during the first two days after birth.
67
Interview with the Demographic and Health Statistics Division, PSA. (October 5, 2016).
68
Interviews with LGUs in Eastern Visayas and Corderilla Administration Regions.
69
WHO, UNICEF, UNFPA, World Bank Group and United Nations Population Division Maternal
Mortality Estimation Inter-Agency Group. (2015). Maternal Mortality in 1995-2015 – Philippines.
70
The Philippines Fifth Progress Report MDGs, NEDA, 2014.
71
Based on some of the available websites by regional health offices, CAR and Central Visayas
recorded MMR lower than the MDG target while higher in Caraga (at 120-150 per 100,000 live
births) between 2013-2015.

36
Regionally, Autonomous Region in Muslim Mindanao (ARMM) had a much lower ANC
rate at 53 percent compared to other regions. About 12 percent of women deliver a child
with assistance by a TBA and the most common skilled birth attendant is a midwife in
ARMM. Regarding FBD rates, it is the highest in the National Capital Region, lower in
Mindanao (except for Davao), Cagayan Valley, Mimaropa and Bicol and the lowest at 12
percent in ARMM. The factors associated with the low FBD include low educational
attainment of mother, low income, having more than six children, resided in remote area,
and not receiving ANC. It was reported that the major reason for not having FBD is the
financial burden, followed by not found necessary, distance to a health facility, and
non-availability of transportation.
72
(2) Child mortality
The National Infant Mortality Rate (IMR) and the under-five mortality rate have both
declined steadily (IMR: 23/1000, U5MR: 31/1000) and are predicted to achieve the
respective MDG targets (IMR: 19/1000, U5MR: 27/1000). However, regional
discrepancies also exist with Mindanao and Mimaropa having higher rates than the
national average, although discrepancy is not as large as that seen for maternal mortality in
ARMM. National average of early neonatal death and still birth rates remains high at
22/1000. In general, mortality rates are higher in remote areas than urban areas. Like FBD,
mothers’ lower educational attainment and income level are associated with higher child
mortality rates. As compared with the first child, the seventh and later children is five
times more likely to die before his/her first birthday.
73
(3) Teenage Pregnancy
Teenage pregnancy and motherhood is becoming a social and health concern in the
Philippines. It was found that teenage women are at higher risk of having anemia,
premature birth, and low-birth-weight baby. It is also reported that the risk of still birth or
child death within a week after birth is 50 percent higher for a child born to a teenage
mother than a child born to a mother in twentieth. While the total fertility rare decreased
from 6.0 in 1973 to 3.0 in 2013, the age-specific fertility rate of women ages 15-19 has
remained somewhat constant during the same period (see Figure 3- 12).
74
72
Philippine National Demographic and Health Survey 2013.
73
ibid
74
ibid

37
Socioeconomic concern includes the fact that many of teenage mothers drop out of school
and therefore it is not easy for them to make living by themselves. Another issue of teenage
pregnancy is that many of their children are born outside of marriage. Childbirth outside of
marriage results in social and economic disadvantages for both teenage mothers and their
children, such as ineligibility for public health insurance and social stigma.
Figure 3- 12 Trends of Total Fertility Rate and the Teenage Fertility
out of Total Fertility Rate from 1973 to 2013 in the Philippines
Source: National Demographic Survey for 1973, 1983, 1993, Republic of the Philippines Fertility Survey for 1978,
Contraceptive Prevalence Survey for 1986 and National Demographic and Health Survey for 1998 to 2013
3-3 Assistance of Development Partners
(1) Development Partners in the Philippine Health Sector
Figure 3- 13 shows the breakdown of official development assistance (ODA) by
development partners for ongoing projects as of the end of 2015.
In terms of the amount, USAID, the Global Fund and the European Union (EU) are the
three top development partners, accounting for 37%, 27% and 17%, respectively. JICA
accounts for 5% of the total ODA of development partners to the health sector.
0
10
20
30
40
50
60
0
1
2
3
4
5
6
7
1973 1978 1983 1986 1993 1998 2003 2008 2013
Total Fertility Rate Age Specific Fertility Rate (15-19)

38
Figure 3- 13 Donor Contributions in Philippine Health Sector
as of the End of December 2015
Source: Bureau of International Health Cooperation of DOH (2016). The Official Development Assistance on Health.
In terms of the areas of assistance, MDG 4 (child mortality) and MDG 5 (maternal
mortality) are by far the major areas, accounting for 43% of the total, in which
development partners are providing their assistance (See Figure 3- 14).
Figure 3- 14 Areas of Assistances by Donors as of the End of December 2015
Source: Bureau of International Health Cooperation of DOH (2016).
The Official Development Assistance on Health.
(2) Trends of the Assistance by Development Partners in the Philippine Health Sector
Figure 3- 15 compares DOH budgets and the amount of ODA by development partners in
the past 18 years, subtotaling every 6 years. While the DOH budget has increased
significantly especially since 2011, the increase in the amount of assistance by
development partners has not kept up.
USAID
37%
Global Fund
27%
EU
17%
JICA
5%
Germany
4%
KOICA
2%
UNFPA
2%
UNICEF
2%
WHO
2%
ADB
1%
World Bank
1%
MDG4 (Child Mortality)・MDG5
(Maternal Mortality), 43%
MDG 6 (HIV/AIDS, Malaria, TB
and Other Infectious Diseases),
27%
Health Systems and
Crosscutting Issues,
12%
Disaster Management
and Strengthening
Disease Survellance, …
Noncommunicable
Diseases, Environmental
Health and Mental …
Health Facility
Enhancement, 3%
Knowledge Management and Information
System, 1%

39
Figure 3- 15 DOH Budgets and Amount of Donor Assistances (1998-2016)
Source: Bureau of International Health Cooperation of DOH (2016).
The Official Development Assistance on Health.
(3) Details of Assistance by Development Partners
Major development partners assisting the Philippine health sectors, other than JICA,
include the World Bank, USAID, EU, WHO, Asian Development Bank (ADB), United
Nations Children’s Fund (UNICEF) and United Nations Population Fund (UNFPA).
Below describes the content of the assistance from each development partner.
① World Bank
75
The World Bank provides assistance in maternal and child health (MCH), health finance
and health policy and systems.
[Maternal and Child Health]
BlueStar Output Based Project
From April 2012 to December 2015, the World Bank piloted the output-based project
(Global Partnership on Output-based Aid) to improve the poor population’s health,
particularly in the area of maternal and reproductive health, in the provinces of Leyte,
Southern Leyte, Samar, Northern Samar and Eastern Samar in the Eastern Visayas
Region.
76
75
Interview with World Bank
76
World Bank. Global Partnership on Output-based Aid, Grant Reporting and Monitoring Report: Ref.
TF0101757.
28.0
24.0
12.0
417.7
97.8
75.3
0.0 100.0 200.0 300.0 400.0 500.0
2011-2016
2005-2010
1998-2004
DOH Budget (billion
pesos)
ODA (Loans and Grants,
billion pesos)

40
The project was implemented by BlueStar, a franchise developed and owned by Marie
Stopes International, the United Kingdom-based non-profit organization. The project
intends to promote enhancement and accreditation of maternal health facilities by
PhilHealth, especially in hard-to-reach areas. Population Services Philipinas, Inc. (PSPI) is
the national franchisor of BlueStar. The World Bank gave grants to PSPI when third-party
organizations
77
had verified the following three outputs:
1. Private birthing facility becomes accredited by PhilHealth.
2. Private birthing facility completes refurbishment of facility as agreed.
3. Private birthing facility completes staff training as agreed.
By the end of the project, refurbishments of 27 birthing facilities as well as construction of
seven Barangay Health Stations (BHSs) were completed, and US$ 3 million was paid out in
total.
According to the World Bank, this mechanism could be employed in other areas of the
country if a private institution is willing to take on the financial risk until the required
output targets are achieved.
Voucher Project
In conjunction with the BlueStar Output-Based Project described above, the World Bank
carried out the subsidized voucher project.
Under this project, a voucher is sold for 50 pesos at a franchised birthing facility in
Northern Samar and Eastern Samar, relatively poor provinces. The voucher allows a
woman to receive maternal health services, such as ante-natal and post-natal care, free of
charge, and she redeems the voucher for a total of 1,500 pesos at the bank designated by
the project when she completes necessary care at the birthing facility. A redemption
method can be either a single redemption or a redemption on the milestone basis at a time
of receiving a maternal health service.
The project sold a total of 10,000 vouchers in one year, 60 percent of which were
redeemed. Concurrently, World Bank placed two series of 30-second advertisements with
AM and FM radio to educate the target group of people with PhilHealth benefits.
However, the World Bank learned that radio was not effective media as residents do not
listen to the radio today: they watch television instead.
77
PRIMEX, local consulting firm, served as the third-party inspector

41
[Health Finance]
Healthcare Finance Strategy
In 2010, DOH published the Health Care Financing Strategy of the Philippines 2010-2020
– Toward Financial Risk Protection that provides a roadmap towards attaining the strategic
goals of increasing the overall level of health spending, promoting universal coverage,
improving allocative efficiency, and promoting technical efficiency. The World Bank,
DOH and PhilHealth are currently reviewing the Strategy.
Japan Policy and Human Resources Development: PHRD UHC Window
World Bank and the Japanese government have formulated a proposal of a technical
assistance project on Health Financing Review and Systems Strengthening by utilizing the
Japan Policy and Human Resources Development Fund (PHRD) established under the
partnership between World Bank and the Japanese government to achieve the goals of the
Aquino Administration's Kalusugan Pangkalahatan - Universal Health Care (KP) program
in the Philippines. The project is to start in 2016.
[Health Policy and System]
Primary Care Package
To study the best implementation mechanism for the primary care benefit package of
NHIP (Primary Care Benefit 1, or PCB1), the World Bank, in conjunction with PhilHealth
and the Korea Development Institute – School of Public Policy and Management, is
carrying out the study, the Impact of Incentives and Information on Quality and Utilization
in Primary Care (I3QUIP).
78
The I3QUIP studies the impact of different implementation mechanisms to boost
effectiveness of the PhilHealth’s performance-based payment for PCB1. The World Bank
is currently working on the baseline report that describes the current status of primary care
package implementation and compliance by LGUs and primary health providers.
② USAID
79
USAID is assisting the Philippine health sector with the following three pillars:
80
1. Improving the supply of integrated family health services
78
World Bank. (February 2016). Philippines Impact of Incentives and Information on Quality and
Utilization in Primary Care: Baseline Survey Report.
79
Interview with USAID
80
USAID website

42
2. Developing healthy behaviors and practices
3. Improving health policies and systems
Within the assistance framework of the three pillars, USAID is currently providing the
Philippine government with assistance in the following areas:
81
Maternal and Child Health (MCH)
Service Delivery Network (SDN)
Health finance
Health policy and system
[Maternal and Child Health (MCH)]
To improve the quality of Maternal, Neonatal, Child Health and Nutrition/Family Planning
(MNCHN/FP) services, USAID is carrying out the following three regional projects:
1. VisayasHealth Project
2. MindanaoHealth Project
3. LuzonHealth Project
The project period for all three is from 2013 to 2018. Table 3- 10 summarizes the target
regions and provinces for each project.
Table 3- 10 Target Regions and Provinces for the USAID Assisted MNCHN/FP Programs
Project
Regions
Province
VisayasHealth
Western Visayas
Iloilo, Negros Occidental
Central Visayas
Bohol, Cebu
Eastern Visayas
Leyte, Southern Leyte, Samar, Northern Samar
MindanaoHealth
Zamboanga Peninsula
Zamboanga del Sur, Zamboanga del Norte, Zamboanga
Sibugay
Northern Mindanao
Misamis Oriental, Bukidnon, Lanao del Norte
Davao
Davao del Sur, Compostela Valley, Davao Oriental
Soccsksargen
Cotabato Province, South Cotabato, Sultan Kudarat
Caraga
Agusan del Sur, Agusan del Norte
Autonomous Region
in Muslim Mindanao
Lanao del Sur, Basilan, Maguindanao, Sulu, Tawi-Tawi
LuzonHealth
CAR
Benguet
Ilocos
Pangasinan
Cagayan Valley
Cagayan, Isabela
Central Luzon
Neva Ecija, Balacan, Tarlac
Calabarzon
Quezon, Batangas, Laguna, Cavite, Rizal
Mimaropa
Oriental Mindoro
National Capital
Region
(City of) Caloocan, Malabon, Marikina, Pasig, Quezon,
Taguig, Valenzuela
Bocol
Albay
Source: USAID website
81
USAID website and Interview with USAID

43
USAID is planning on post-2018 MNCHN/FP projects. Regions for assistance are
expected to be selected from a list of the 20 poorest provinces, for which DOH is calling
for donor assistance. Given the direction of the current administration, USAID will place
emphasis in assisting the poorest families with difficulties in accessing health facilities.
[Service Delivery Network (SDN)]
The Private Sector Mobilization for Family Health Project – Phase 2 (PRISM2) was
implemented from 2009 to 2014 with the goal to strengthen SDN and to assist the DOH
and the LGUs in engaging and mobilizing private sector resources in delivering family
planning and MCH services and products. Involvement of the private sector in the network
has been successful in some areas. It was reported that there was one province in which the
number of SDNs increased from just a few to more than 100.
82
USAID has tested and fine-tuned various models in the PRISM2 project. Illoillo and
Cavite provinces were cited as examples in which more advanced and mature SDN
networks exist.
[Health Financing]
Since 2014, USAID has assisted Tacloban City in their efforts to re-establish the functional
health system and maximize the income of health facilities facing devastations from
Typhoon Yolanda.
83
USAID studied the status of service delivery in the area and recommended the following to
maximize the income of health facilities.
∙ USAID advised Tacloban City to open a bank account, called the Trust Fund, to
exclusively receive PhilHealth reimbursements.
84
By securing the health budget through
this arrangement, it was expected to motivate the City to provide better health services.
∙ USAID advised Tacloban City to use some of the PhilHealth reimbursements to
incentivize the volunteers and barangay health workers (BHWs) who had taken
82
Interview with USAID
83
UPecon-Health Policy Development Program. (2015). Concept Note on the Establishment of a
Service Delivery Network for Tacloban City
84
PhilHealth reimbursements are to be redistributed to health facilities and professional, and LGUs are to
open a Trust Fund bank account for PhilHealth related transactions. However, it is reported that some
LGUs have not opened the bank account and the said LGUs may not be making appropriate
redistributions, as PhilHealth reimbursements are accounted for as part of the general budget. According
to PhilHealth, health LGU-owned institutions are not able to open a bank account as they are not legal
entities.

44
expectant mothers to health facilities. Through this arrangement, it was expected that
the number of facility-based deliveries (FBD) would increase and subsequently
reimbursement for the Maternity and Child Package (MCP) would also increase in
Tacloban City.
Both of these measures became city ordinances in 2015, and Tacloban City saw significant
increase in PhilHealth reimbursement. For instance, the Tacloban City Hospital received
4.2 million pesos for PhilHealth reimbursement in 2014, but the amount increased up to
22.8 million pesos by October 2015. Moreover, in the first quarter of 2016, 9.4 million
pesos, equivalent to 6.3 times as much as that in 2014 and 2.8 times as much as that in
2015, was paid to Tacloban City by PhilHealth.
[Health Policy and System]
Health Policy
Health Policy Development Program – Phase 2 is a five-year (2012-2017) health policy
project in partnership with the UPecon Foundation, Inc. It supports the DOH-led policy
formulation process by scaling up the Government of the Philippines’ Universal Health
Care initiative.
85
So far, USAID has supported DOH with the following initiatives:
∙ Development of guidelines for implementing the Responsible Parenthood and
Reproductive Health Law
∙ Design of the 2015 National TB Prevalence Survey
∙ Implementation of monitoring operations for Universal Health Care
∙ Assessment of family planning logistics and promotion of new logistics for provider
participation
∙ Training on planning and contracts management for the staff of DOH Regional Offices
Health Governance Related
In October 2013, USAID and DOH entered into a three-year Global Development Alliance
with the Zuellig Family Foundation (ZFF).
86
ZFF has implemented leadership and
governance capacity building programs for health in various rural municipalities in the
Philippines since 2008.
85
USAID website
86
ibid

45
The goal of the capability-building programs is to improve health outcomes in the areas of
maternal and child health, family planning and tuberculosis by enhancing the leadership
and governance capabilities of local chief executives and local health officers of the 121
LGUs.
Health Information Improvement
As statistical data collected in the Philippines is not highly reliable, USAID verifies the
accuracy of data, such as the Family Income and Expenditure Survey (FIES), before it
utilizes it. On the basis of this experience, USAID has recently developed a data
standardization tool, which is now recommended by DOH and adopted by some
development partners, including UNICEF.
③ EU
87
The EU provides budget support to DOH. The current budget support is for the period of
2015-2017 and this is the third offer by the EU, followed by 2007-2010 and 2011-2013
support. Funds are paid out to DOH through the Department of Finance (DOF) upon
meeting targets, many of which are based on the FIES.
88
Current assistance by the EU for the Philippine health sector is provided in the following
areas.
Service Delivery Network (SDN)
Health financing
Health policy and system
[Service Delivery Network (SDN)]
The EU launched the SDN project in August 2016. As there are similar SDN projects
carried out by other development partners, the EU hopes to differentiate this project by
uncovering valuable information, such as why public hospitals with no PhilHealth
accreditation still exist today.
[Health Finance]
In December 2015, the EU proposed a technical assistance program to update PhilHealth
case rates. The EU believes that the new administration is positively considering the
proposal.
87
Interview with EU
88
Most targets are based on the indicators in FIES

46
[Health Policy and System]
The EU has provided following the Information and Technology (IT) -related assistance
projects:
∙ Project to link provincial-level electronic medical records to PhilHealth
The EU normally provides technical assistance and DOH prepares the necessary
hardware; however, there are some cases in which development partners provide the
hardware, such as in Calabarzon Region by the Korea International Cooperation
Agency (KOICA).
∙ Project to ensure privacy and security of data
DOH has been working on this subject since 2014 to manage electronic data records
at the LGU level.
∙ Project to improve the monitoring capacity of health enterprise architecture
The project aims at data transfer and connection through digitization of the health data.
∙ Project to build up the health information system in which DOH, PhilHealth and
hospitals play clearly defined roles
Health information systems have been adopted by merely 10 to 15 percent of
hospitals, and even when adopted, quality of data is low, both in medicine and
finance.
As IT is a broad arena in which assistance by only the EU and KOICA is not
sufficient, the EU has recommended to JICA to join them and start providing similar
assistance.
④ WHO
89
Current assistance by WHO for the Philippine health sector is in the following areas:
Service Delivery Network (SDN)
Health policy and system
89
Interview with WHO

47
[Service Delivery Network (SDN)]
WHO considers SDN as important as healthcare finance for better health in the
Philippines, and it is currently carrying out the SDN project in Davao City, Mindanao.
WHO is carrying out this initiative with KOICA, and would welcome JICA to join the
initiative in this or another region.
On the basis of the belief that motivation and morals of local government officials, especially
barangay chiefs, are keys to success in building an effective SDN, WHO recently expressed
interest in assisting LGUs to strengthen their governance structure.
In addition to the Davao project, WHO, together with UNFPA, UNICEF and DOH, is
currently carrying out a project to formulate the guidelines for MCH-related SDNs in
Cotabato City, Soccskasargen Region of Mindanao.
[Health Policy and System]
WHO is currently assisting the Asian Pacific Observatory to update the Philippine Health
System Review – Health in Transition.
⑤ ADB
90
Asian Development Bank (ADB) currently provides assistance to the Philippine health
sector in the areas of health policy and systems.
In early 2016, the National Economic and Development Authority (NEDA) drafted a
25-year strategic master plan, Philippines Strategy 2040. ADB provided comments and
suggestions with respect to the said draft from the viewpoint of universal health coverage.
This draft is the product of the former administration, and if the current administration
were to pursue the same strategic master plan, ADB would assist NEDA and DOH. Aside
from the above, ADB provides US$ 300 million budget support for the Conditional Cash
Transfer (CCT) program.
91
⑥ UNICEF
92
UNICEF currently assists the Philippine health sector in the following areas:
Maternal and Child Health (MCH)
90
Interview with ADB
91
Refer to 2-12 (4) “Supporting Indigents of Section 2 for details of CCT,
92
Interview with UNICEF

48
Service Delivery Network (SDN)
Health financing
[Maternal and Child Health (MCH)]
The Maternity Care Package (MCP) of NHIP has not substantially changed in the last ten
years and there is no benefit package for premature care. UNICEF is working towards
improvement of the situation.
∙ MCP: MCP data of ten million cases are now available. On the basis of this large
data analysis, UNICEF plans to make recommendations for improvement of the
MCP.
∙ Package for Premature Baby: UNICEF is working with PhilHealth on the creation
of a pre-mature benefit package, as the premature death rate remains high, while the
neonatal death rate has been stabilized in the Philippines.
[Service Delivery Network (SDN)]
As previously mentioned, UNICEF, together with WHO, UNFPA, UNICEF and DOH, is
working to formulate guidelines for MCH-related SDN in Cotabato City, Soccsksargen
Region of Mindanao.
[Health Finance]
Primary Care Package
As the primary care package, named Tamag Serbisyo para sa Kalusugan ng Pamilya
(TSeKaP Program), does not cover sufficient drugs for asthma and tuberculosis, UNICEF,
together with WHO and UNFPA, has been working towards improvement of the program
since 2014.
The original proposal was submitted to DOH at the time of Secretary Ona, but no progress
was seen after his resignation. The new DOH Secretary Ubial is keen on taking this
initiative further.
Rational Prioritization of Benefit Packages
Prioritization of benefit packages of NHIP tends to reflect the preference of those with
power. However, UNICEF is advising PhilHealth to rationally prioritize benefit packages.

49
⑦ UNFPA
93
Assistance by UNFPA for the Philippine health sector is provided in the following areas:
Maternal and Child Health (MCH)
Service Delivery Network (SDN)
[Maternal and Child Health (MCH)]
UNFPA is assisting the Philippine MCH service delivery in the following three areas:
1. Facility Based Deliveries (FBD): UNFPA sees the following issues in deliveries in
the Philippines.
There are facilities that are not meeting minimum requirements for Basic
Emergency Maternal Obstetrics and Newborn Care (BEmONC).
Many facilities have a shortage of drugs.
There are areas where accessible birthing facilities do not exist for expectant
mothers.
2. Skilled Birth Attendant (SBA): A higher proportion of births attended by a SBA
was one of the targets of MDG5. Although the Philippines was closer to the target,
94
it has room for improvement.
3. Family Planning: The Philippines is not likely to achieve the MDG 5 targets in
respect to contraceptive prevalence and unmet needs for family planning.
95
While
neo-natal deaths are a large proportion of all child mortality cases in the Philippines,
the study conducted by UNFPA in 2013 revealed that 50 percent of the deaths could
have been prevented if proper family planning was practiced.
[Service Deliver Network (SDN)]
UNFPA is currently involved with the following two SDN related projects.
93
Interview with UNFPA
94
Indicators of MDG 5 Target 5.A: reduce the maternal mortality ratio by three quarters between 1990
and 2015 include 5.1 - maternal mortality ratio and 5.2 - proportion of deliveries attended by skilled
health personnel.
95
Indicators of MDG 5 TARGET 5.B: achieve, by 2015, universal access to reproductive health include
5.3 contraceptive prevalence rate, 5.4 adolescent birth rate, 5.5 antenatal care coverage, and 5.6 unmet
need for family planning.
50
∙ A project targeting indigenous people in Soccskasargen, Mindanao
As their residential areas extend to more than two administrative divisions, special
consideration needs to be given in building SDNs in those areas.
∙ A project to formulate guidelines, together with other development partners, for
MCH-related SDNs in Cotabato City, Soccskasargen of Mindanao.
As previously mentioned, UNFPA is carrying out this project with WHO, UNICEF
and DOH.

51
Chapter 4 National Health Insurance Program (NHIP) – Overview
and Utilization
4-1 Current Framework of NHIP
The National Health Insurance Act of 1995 (RA No. 7875) institutionalized social health
insurance in the country through the National Health Insurance Program (NHIP), in order to
provide health insurance coverage and ensure affordable, acceptable and necessary health care
services for all citizens of the Philippines. Also in the same year, the Philippine Health
Insurance Corporation (PhilHealth) was established as the implementing agency of NHIP by
integrating the health insurance sections of the Government Service Insurance System (GSIS),
the insurance system for government employees, and the Social Security System (SSS) for
private sector employees. Although the operation became unified, there exist several
membership categories as described in 4-3, and premium collections are carried out based on
the methodology designed for each membership category. The goal of the Philippine
government is to cover all citizens under the NHIP.
96
4-2 PhilHealth
PhilHealth is the part of the Department of Health (DOH), and is governed by a board of
directors composed of seventeen members, chaired by the secretary of DOH. Figure 4- 1 is the
simplified organizational chart of PhilHealth.
Figure 4- 1 Organizational Chart of PhilHealth
Source: PhilHealth website.
96
PhilHealth website
Board of
Directors
Internal Audit
Group
President and
CEO
Actuarial Sys
and Risk
Management
Information
Management
Executive Vice
President and
COO
Management
Services
Fund
Management
Regional Office
North & Central
Luzon
NCR & South
Luzon
Visayas Mindanao
4 other offices
(8 in total)
Health Finance
Policy
Legal
Member
Management
Organization
and Systems
Development
Corporate
Planning
Corporate
Affairs
Corporate
Secretary
52
Approximately 6,400 employees work for PhilHealth and 800 of them work at the headquarters
in Quezon City.
At the local level, more than 100 branch offices (PhilHealth Local Health Insurance Office and
PhilHealth Business Center) are administered by the eight Regional Offices. Moreover,
approximately 70 express offices (PhilHealth Express) are situated at convenient locations, such as
shopping malls.
The following authorities and responsibilities are allocated to PhilHeath.
∙ To administer the NHIP
∙ To formulate and promulgate policies for the NHIP administration
∙ To formulate and implement guidelines on the above, namely premium collection, claim
procedure, cost containment, quality assurance of health care, and health care provider
accreditation, payment, and referral systems
4-3 Goals for the Philippine Health Agenda
As mentioned earlier, under the new Duterte administration, DOH has launched the Philippine
Health Agenda 2016-2022 and one of the three Guarantees is Universal Health Insurance. With
respect to Universal Health Insurance, PhilHealth has set the following goals:
∙ National Health Insurance Program (NHIP) enrolls 100% of Filipinos where formal sector
premiums are paid through payroll and non-formal sector premiums are paid by tax subsidies.
∙ NHIP’s support value is 100% (or zero-copayment) for the poor and those admitted in
basic accommodation, and predictable (fixed co-payment) for those admitted in non-basic,
private accommodation.
∙ NHIP covers a comprehensive range of services and becomes the main revenue source of
public health care providers.
4-4 Membership Category
Today, the PhilHealth memberships are classified into six categories as shown below. Table 4-
1 summarizes qualifications for each category.
1. Formal Economy
2. Informal Economy
3. Lifetime Members
4. Senior Citizens
5. Indigent Members
6. Sponsored Members
53
Table 4- 1 PhilHealth Membership Category
Membership Category
Qualification
1
Formal Economy
Workers in the government and private sectors who have established
employee-employer relations (includes housewife and driver
employed by an individual)
Business entrepreneur
2
Informal Economy
97
Migrant Workers: Filipinos who are engaged in a remunerated
activity in another country of which they are not citizens
Informal Sector: includes among others, street hawkers, market
vendors, taxi drivers, small construction workers, and home-based
industries and services
Self-Earning Individuals: individuals who render services or sell
goods as a means of livelihood outside of an employer-employee
relationship or as a career. These include professional practitioners
including but not limited to doctors, lawyers, engineers, artists,
architects and the like, businessmen, entrepreneurs, actors, actresses
and other performers, news correspondents, professional athletes,
coaches, trainers, and such other individuals
3
Lifetime Members
Individuals aged 60 years and above and have paid at least 120
monthly contributions to PhilHealth and the former Medicare
Programs – i.e., Social Security System (SSS) and Government
Service Insurance System (GSIS)
Uniformed personnel aged 56 years and above and have paid at least
120 monthly contributions to PhilHealth and the former Medicare
Programs of SSS and GSIS
SSS underground miner-retirees aged 55 years above and have paid
at least 120 monthly contributions to PhilHealth and the former
Medicare Programs of SSS and GSIS
SSS and GSIS pensioners prior to March 4, 1995
4
Senior Citizens
Filipino citizens who are residents of the Philippines, aged sixty (60)
years or above and are not currently covered by any membership
category of PhilHealth
5
Indigent Members
Persons who have no visible means of income, or whose income is
insufficient for family subsistence, as identified by the Department
of Social Welfare and Development based on specific criteria.
Indigent Members are identified under the National Household
Targeting System for Poverty Reduction (the “NHTS-PR”), will
automatically be enrolled and covered as PhilHealth Members.
6
Sponsored Members
Individual whose premium is paid for by a sponsor such as an
institution or another individual
Orphans, abandoned and abused minors, out-of-school youths, street
children, persons with disability (PWD), senior citizens
98
and
battered women under the care of the Department of Social Welfare
and Development, or any of its accredited institutions run by NGOs
or any non-profit private organizations
Barangay health workers, nutrition scholars, barangay police officer,
and other barangay workers and volunteers
Those enrolled through the Point of Care program of PhilHealth
Source: PhilHealth website and Title III Section 5 of the Implementing Rules and Regulations (IRR) of RA 7875
as amended otherwise known as the National Health Insurance Act of 2013
97
Formerly there was a category for “Overseas Filipinos”, which is now merged into Informal Economy.
Interview with PhilHealth (October 26)
98
A citizen is classified under the Senior Citizen category if a citizen is 60 years old or above and is not
under the care of the DSDW or NGO

54
Qualified dependents of the members are entitled to PhilHealth benefits without additional
premiums. Following are qualified dependents:
99
∙ Legitimate spouse who is not a member
∙ Unmarried and unemployed legitimate, legitimated, acknowledged, illegitimate children,
legally adopted or step children below 21 years of age
∙ Children who are twenty-one (21) years old or above but suffering from a disability that
renders them totally dependent on the member for support, as determined by PhilHealth
∙ Foster child as defined in Republic Act 10165 otherwise known as the Foster Care Act of 2012
A qualified dependent is claimed by a member and enlisted in the member’s Member Data
Record (MDR). MDR proves that the individuals enlisted are the PhilHealth Members.
4-5 Enrollment Procedures
Enrollment procedures to PhilHealth slightly differ depending on the membership category.
Table 4- 2 summarizes enrollment procedures to PhilHealth.
100
.
Table 4- 2 Enrollment Procedures by Membership Category
Membership Category
Enrollment Procedure
1
Formal Economy
Submission of PhilHealth Member Registration Form (PMRF”) or
other personal identification number in the PhilHealth ID card to
employer (employer will proceed to enroll the employee to
PhilHealth)
2
Informal Economy
Submission of PMRF to PhilHealth Local Health Insurance Offices
or PhilHealth Express outlets nationwide
For Migrant Worker, if in the Philippines, submission of PMRF to
either PhilHealth Regional Office, PhilHealth Local Health
Insurance Office, PhilHealth Business Center or PhilHealth Express
outlet. If overseas, electronically submitting PMRF from any branch
of accredited collecting partners of PhilHealth – i.e., iRimit, Inc. and
Ventaja Corporation
3
Lifetime Members
Submission of PMRF and other necessary documents to PhilHealth
Local Health Insurance Office
4
Senior Citizens
Submission of PMRF and other necessary documents to either
Office for the Senior Citizen Affairs or PhilHealth Local Health
Insurance Office
5
Indigent Members
Indigents are automatically enrolled to PhilHealth
6
Sponsored Members
Submission of PMRF and other necessary documents to sponsors or
at PhilHealth offices
Source: PhilHealth Website
99
PhilHealth website
100
ibid
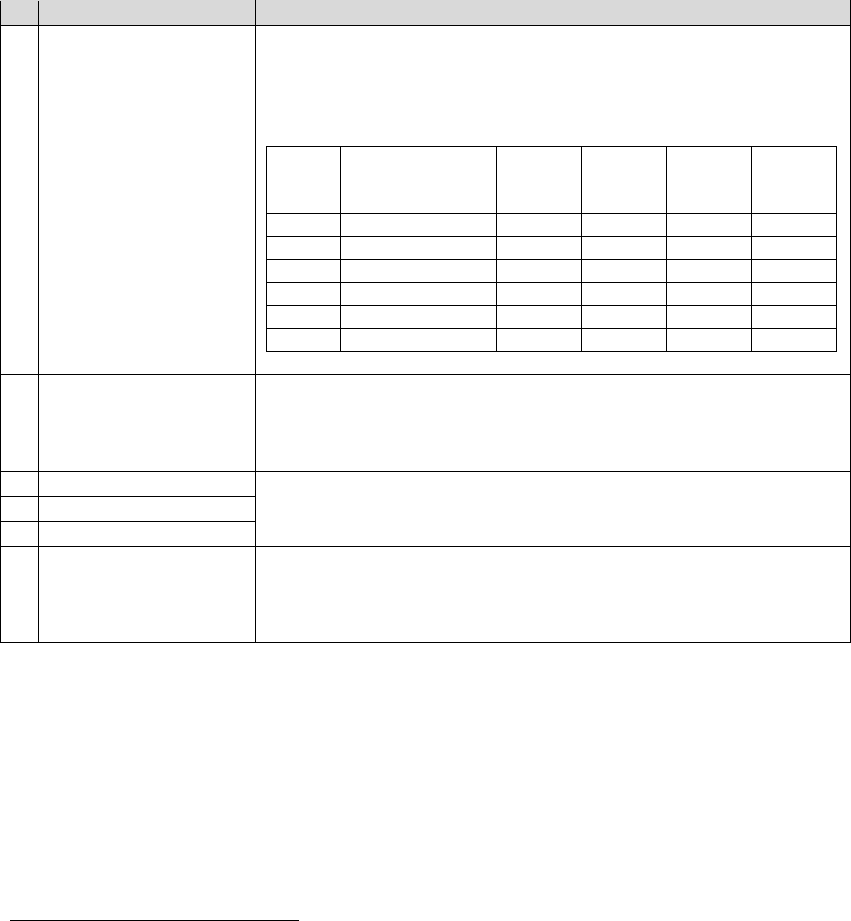
55
4-6 Premium Contributions
Premium payment procedure varies depending on the Membership category, as summarized in
Table 4- 3.
101
Table 4- 3 Premium Payment Procedures
Membership Category
Premium Payment Procedure
1
Formal Economy
Members in the formal economy shall pay the monthly contributions
to be shared equally by the employer and employee at a prescribed
rate set by PhilHealth not exceeding 5 percent of their respective
basic monthly salaries. Below is the excerpt from the Formal
Economy contribution table for 2016 (in pesos).
Salary
Bracket
Salary Range
Base
Salary
Total
Monthly
Premium
Employee
Share
Employer
Share
1
~8,999.99
8,000
200.00
100.00
100.00
2
9,000~9,999.99
9,000
225.00
112.50
112.50
3
10,000~10,999.99
10,000
250.00
125.00
125.00
…
…
…
…
…
…
27
34,000 ~ 34,999.99
34,000
850.00
425.00
425.00
28
35,000~
35,000
875.00
437.50
437.50
***
2
Informal Economy
Annual premium of 2,400 pesos are paid monthly or yearly for those
earning P25,000 or less per month.
Annual premium of 3,600 pesos are paid monthly or yearly for those
earning more than 25,000 pesos per month.
3
Lifetime Members
Annual premium of 2,400 pesos for each member is shouldered by
the National Government based on the General Appropriations Act.
4
Senior Citizens
5
Indigent Members
6
Sponsored Members
・Annual premium of 2,400 pesos for each member is shouldered by
LGU, Department of Social Welfare and Development (DSWD),
healthcare institutions, national government, private individuals,
private corporations, etc.
102
Source: PhilHealth website & Interviews with PhilHealth
101
PhilHealth website and Title III Section 5 of the Implementing Rules and Regulations (IRR) of RA
7875 as amended otherwise known as the National Health Insurance Act of 2013, annual audit report
for the year ended December 31, 2015
102
Healthcare institutions tend to pay the premium and become sponsors of the uncovered indigents upon
admission of the indigents under Point-of-Care enrollment program that enrolls them into PhilHealth
on site, offered by public healthcare institutions. As public healthcare institutions (DOH retained
hospitals and LGU owned hospitals) are subsidized by the national government and/or LGUs, they are
effectively supporting the Sponsored Members. Based on an interview with PhilHealth (October 26)

56
4-7 Payment Mechanisms
Previously, PhilHealth had employed the payment mechanism called Fee-for-Service, which
determines the fee based on the health services provided, the type of health facility and the
severity of illness. In 2011, aiming to reduce payment cost and claim document processing,
PhilHealth introduced the Case Rate Payment method for the following 11 medical cases and 12
surgical cases shown in the Table 4- 4. Case Rate Payment is a payment method that reimburses
health facilities a predetermined fixed rate for each treated case. PhilHealth had selectively used
the Case Rate Payment method for such conditions as outpatient malaria treatment, HIV/AIDS,
tuberculosis treatment and cataract surgery. However, with this introduction, approximately 50
percent of all claims filed to PhilHealth came to be reimbursed through the Case Rate Payment
method.
Table 4- 4 Case Rate Payment Introduced in 2011 – Cases and Rates (in pesos)
Medical Case
Surgical Case
Case
Rate
Case
Rate
1
Dengue I (Dengue Fever and DHF Grades I & II)
8,000
Radiotherapy
3,000
2
Dengue II (DHF Grades III & IV)
16,000
Hemodialysis
4,000
3
Pneumonia I (Moderate Risk)
15,000
Maternity Care Package
8,000
4
Pneumonia II (High Risk)
32,000
Cesarean Section
8,000
5
Essential Hypertension
9,000
Appendectomy
6,500
6
Cerebral Infarction (CVA I)
28,000
Cholecystectomy
19,000
7
Cerebro-Vasluar Accident (hemorrhage) (CVA II)
38,000
Dilatation & Curettage
24,000
8
Acute Gastroenteritis (AGE)
6,000
Thyroidectomy
31,000
9
Asthma
9,000
Herniorrhaphy
21,000
10
Typhoid Fever
14,000
Mastectomy
22,000
11
Newborn Care Package in Hospitals and Lying-in
Clinics
1,750
Hysterectomy
30,000
12
Cataract Surgery
16,000
Source: Dr. Francisco Z. Soria, Jr. (2016). PhilHealth Benefits.
In 2014, PhilHealth introduced the All Case Rate payment mechanism when reimbursing health
care providers and professionals. Through this introduction, members came to know how much
PhilHealth is paying for their illness or injury at the PhilHealth website by searching for
illness/injury, operation, ICD 10
103
or RVS codes.
104,105,106
103
International Statistical Classification of Diseases and Related Health Problems Tenth Revision (ICD
10)
104
PhilHealth. (2014). Annual Report 2014
105
PhilHealth. (January 30, 2015). Get to know your PhilHealth benefit in just one click.
106
International Statistical Classification of Diseases and Related Health Problems Tenth Revision (ICD
10) and Relative Value Scale (RVS) are codes used by PhilHealth in identifying specific rates for
every reimbursable medical condition and procedure.

57
Moreover, introduction of the Case Rate Payment curtails prolonged hospital stay,
over-utilization of diagnostic tools, and provision of un-necessary healthcare services. In some
areas of the country, turnaround time taken from claim receipt to payment was shortened from
70 days under the Fee-for-Service method to 17 days with the introduction of Case Rate
Payment method.
107
Generally speaking, for medical cases, healthcare professionals are allocated 30 percent of
PhilHealth reimbursements, with 40 percent allocation for surgical cases.
108
Figure 4- 2 is the
sample of Case Rate Payment for Pneumonia II (High Risk). A Case Rate of 32,000 pesos is
first reimbursed to a healthcare facility or the LGU that operates the healthcare facility. Then 30
percent of the reimbursement is redistributed to healthcare professionals and the remaining 70
percent goes to the healthcare facility.
Figure 4- 2 Reimbursement Flows under Case Rate for Pneumonia II (High Risk)
Source: Dr. Francisco Z. Soria, Jr. PhilHealth benefits
4-8 Benefit Packages
Broadly speaking, the following four types of benefit packages are offered by PhilHealth.
109
Benefit
packages include room and board, and doctors’, lab, procedure, and medicine fees.
1. Inpatient Benefit Packages
2. Outpatient Benefit Packages
3. Z Benefit Packages
4. MDG-related Benefit Packages
The following sub-sections describe each of the benefits.
(1) Inpatient Benefit Package
Inpatient benefits are available to all PhilHealth members.
107
Leopoldo J. Vega, Southern Philippines Medical Center. Shifting to Case Rates: Efficiency Gains.
108
There are exceptions – e.g., P500 fixed payment to healthcare professional for dialysis treatment. (Dr.
Francisco Z. Soria, Jr., PhilHealth. PhilHealth Benefits.)
109
PhilHealth website
Case Rate
Reimbursement Cap
P32,000
Healthcare Provider
Component (70%)
P22,400
Professional Fee
Component (30%)
P,9,600

58
(2) Outpatient Benefit Package
PhilHealth offers outpatient benefit packages targeting primarily indigents.
110
In 2012,
PhilHealth amended its primary benefit package and introduced the Primary Care Benefit 1
(PCB1) package in order to promote the utilization of the service. In 2014, PhilHealth
re-branded PCB1 Package into TSeKaP (see Table 4- 5). TSeKaP consists of essential
services aimed at prevention and early detection of diseases, as well as interventions for
healthy living.
111
Sponsored Members, Indigent Members and Senior Citizens can access the TSeKaP
benefit free of charge.
112
The maximum benefit is 1,800 pesos per year per family, 800
pesos of which is reimbursed to health facilities for their services, and 1,000 pesos are paid
to accredited drug stores.
113
Benefits are basically available through public health service
providers though limited privately owned facilities.
Table 4- 5 Primary Care Service Offered under TSeKaP Program
i. Preventive Services
ii. Diagnostic
Examinations
iii. Drugs and Medicines
1
Consultation
Complete
blood count
Asthma including nebulization services
2
Visual inspection with acetic acid
Urinalysis
Acute Gastroenteritis (AGE) with no or
mild dehydration
3
Regular BP measurements
Fecalysis
Upper Respiratory Tract Infection
(URTI)/Pneumonia (minimal and low risk)
4
Breastfeeding program education
Sputum
microscopy
Urinary Tract Infection (UTI)
5
Periodic clinical breast
examinations
Fasting blood
sugar
6
Counseling for lifestyle
modification
Lipid Profile
7
Counseling for smoking cessation
Chest x-ray
8
Body measurements
9
Digital rectal examination
Source: PhilHealth website
Aside from TSeKaP, outpatient benefits in Table 4- 6 are currently available for
non-Indigent Members free of charge.
110
PhilHealth. (2014). Annual Report 2014.
111
PhilHealth website
112
This program also covers Household Help, such as drivers and housekeepers, as defined in the
Republic Act 10361 or “Kasambahay Law.”
113
Dr. Francisco Z. Soria, Jr, PhilHealth. PhilHealth Benefit Packages: Understanding the Role of
Quality Medicines and Quality Pharmaceutical Care.

59
Table 4- 6 Outpatient Benefit Packages Offered by PhilHealth (other than TSeKaP)
Service
Case Rates (in pesos)
1
Day Surgeries (ambulatory or outpatient surgeries)
All Case Rate applies
2
Radiotherapy
Using Cobalt
Using linear accelerator
2,000/session
3,000/session
3
Hemodialysis
2,600/session
4
Outpatient Blood Transfusion
3,640 (including drugs & medicines,
X-ray, lab, operating room)
Source: PhilHealth website
(3) Z Benefit Package
114
In 2012, PhilHealth launched the new Z Benefit Package (Z Benefit) that gives substantial
financial risk protection for the treatment of catastrophic illnesses. Since its introduction,
the coverages have expanded annually.
Table 4- 7 Z Benefit Package: Year of Introduction and Case Rates (in pesos)
2012 (Initial implementation)
Acute Lymphoblastic Leukemia in Children (standard risk)
210,000
Breast Cancer (early stage)
100,000
Prostate Cancer (low to intermediate risk)
100,000
Low Risk Kidney Transplantation
100,000
2013 (Z benefit expansion)
Elective Surgery for Coronary Artery Bypass Graph
550,000
Tetralogy of Fallout or “Blue Baby Syndrome”
320,000
Ventricular Septal Defect (VSD)
250,000
Cervical Cancer (stage IIIB)
Low dose
High dose
120,000
175,000
Prosthetic limb
15,000
2014 (Z benefit expansion)
Selected Orthopedic Implants
9 types of implant including Total Hip Prosthesis
48,740~103,400
Peritoneal Dialysis
270,000/year
10,384.60/tranche
2015 (Z benefit expansion)
Colon Cancer
Stage I-II (Low Risk)
Stage II (High Risk) - III
150,000
300,000
Rectum Cancer
Stage I (Clinical and Pathologic)
Stage II-III (Clinical and Pathologic)
Use of linear accelerator as mode of radiotherapy
Use of cobalt as mode of radiotherapy
150,000
400,000
320,000
Source: PhilHealth. Annual Report 2014 and PhilHealth website
114
“Z” of Z Benefit package stands for “zero,” meaning that the program requires no co-payment.

60
Table 4- 7 summarizes current offerings of the Z Benefit Package.
115
Currently, 20 percent
of the Z Benefit reimbursement is allocated to healthcare professionals, with some
exceptions, such as Cervical Cancer whose professional fee is 15 percent of the case
rate.
116
Z-benefits are only offered at hospitals contracted with PhilHealth for a specific illness or
treatment in the Z Benefit Package. Table 4- 8 is the list of hospitals contracted for the
Elective Surgery for Coronary Artery Bypass Graph.
117
Table 4- 8 Contracted Hospitals for Elective Surgery for Coronary Artery Bypass Graph
Province
Contracted Hospitals for Elective Surgery
for Coronary Artery Bypass Graph
National Capital Region
Philippine Heart Center
University of Philippines - Philippine General Hospital
Central Luzon
Angeles University Foundation Medical Center
Central Visayas
Vicente Sotto Memorial Medical Center
Northern Mindanao
Northern Mindanao Medical Center
Davao
Southern Philippines Medical Center
Source: PhilHealth website
(4) MDG related package
A MDG-related package is aimed at promotion of MDG target achievements in the
Philippines, which include a maternity package such as MCP, Normal Spontaneous
Delivery Package (NSD) and Antenatal Care Package (ANC01), New Born Care Package
(NCP), and benefit packages summarized in Table 4- 9. PhilHealth Circular No. 026
requires that no fees be charged in excess of the relevant benefit package provided that the
patient pays for the full amount of the required annual premium.
[Maternity Care Package
118
]
The MCP provides for comprehensive coverage from pre-natal to post-natal care, and NSD
encourages normal low risk deliveries in birthing homes and maternity clinics in a safe
environment, as opposed to deliveries at homes.
119
As Table 4- 9 shows, MCP related
benefits differ depending on the type of health care facilities. Case rates for hospitals are
different from that for other facilities, such as, infirmaries, birthing homes and maternity
clinics.
115
PhilHealth website and “Annual Report 2014”, PhilHealth
116
Dr. Francisco Z. Soria Jr., PhilHealth. (2016). PhilHealth Benefits.
117
PhilHealth website.
118
PhilHealth. Circular No. 26, 2015.
119
PhilHealth. Annual Report 2014.

61
Table 4- 9 Maternity Care Package (in pesos)
Source: PhilHealth. Circular No. 26, 2015.
[New Born Care Package (NCP)
120
]
The NCP covers health services that newborns must receive within the first hours of life
regardless of the method of their delivery and presence of co-morbidities. Table 4- 10
summarizes the benefits and case rates.
120
PhilHealth. Circular No. 26, 2015.
Hospital
Non-
hospital
facility
Services, Conditions, etc. Allocation
MCP 6,500 8,000
Covers the essential health services during
antenatal period, normal delivery and immediate
post-partum period including follow-up visits
within the first 72 hours and 1 week after
delivery. Minimum stay of mother in the facility
shall be 24 hours. Avaliment of this package shall
be charged to the annual 45-day benefit limit.
NSD 5,000 6,500
Covers the essential health services during
normal delivery and immediate post-partum
period including follow-up visits within the first
72 hours and 1 week after delivery. Minimum
stay of mother in the facility shall be 24 hours.
Avaliment of this package shall be charged to the
annual 45-day benefit limit.
ANC01 1,500 1,500
At least 4 doctor check-ups are required with that
last check-up being in the last part of pregnancy -
i.e., last 3 months before delivery
Non-hospital facility→
eventual referral to hospital
650
Cesarean Section 19,000
Complicated Vaginal
Delivery
9,700
Breech Extraction 12,120
Vaginal Delivery after
Cesarean Section
12,120
40% to
professional
60% to
facility

62
Table 4- 10 Newborn Care Package (in pesos)
Source: PhilHealth. Circular No. 26, 2015.
[Others]
Other MDG-related benefit packages are summarized in Table 4- 11.
Table 4- 11 Other MDG Related Packages (in pesos)
Benefit Packages
Case Rates
1
Outpatient Malaria (MDG6)
Diagnostic malaria smears and other laboratory procedures; drugs and
medicines & consultation service
600
2
Outpatient HIV-AIDS (MDG6)
Drugs, medicines and laboratory examinations
30,000/Year
(7.500/Quarter)
3
Outpatient Anti-Tuberculosis Treatment (MDG6)
Diagnostic exams, consultation services, drugs, health education and
counseling during treatment
4,000
4
Voluntary Surgical Contraception (MDG5)
Health facility charges such as room and board, drugs and medicines
Physician fee
Post-operative consultation within 90 days from day of surgery
4,000
5
Animal Bite Package (MDG4)
Rabies vaccine
Rabies immune globulin
Local wound care
Tetanus toxoid and anti-tetanus serum
Antibiotics
Supplies such as syringes
3,000
Source: PhilHealth website
4-9 Claim Procedures
In order for members to claim PhilHealth benefits, members are to submit the following
documents to health service providers.
PhilHealth ID and/or MDR
PhilHealth provides ID cards to members. Membership is good for one year, after which
renewal is necessary. MDR proves that individuals are enlisted as PhilHealth Members and
dependents must be enlisted in the MDR.
Services Offered under NCB Package
Reimbursement Allocation
Essential Newborn Care (including vitamin K
administration, first dose of hepatitis B and
BCG vaccine)
1,000
40% to
professional
60% to facility
Newborn Screening Test 550
Newborn Hearing Test 200
Total 1,750
100% to facility

63
Document evidencing premium payments
Members must have made a payment of at least the 3-month premium for the last 6
months. In some cases, including MCP and NCP Packages, one-year premium payment is
required at the time of facility visit.
Claim Form 1, 2 and 3
If necessary documents are properly submitted, the value of PhilHealth case rate is
deducted from the total medical bill upon discharge. PhilHealth will later send a benefit
payment notice to the PhilHealth members.
4-10 Accreditation Processes
121
Accreditation is a process whereby the qualifications and capabilities of health care providers
are verified in accordance with the guidelines, standards and procedures set by PhilHealth.
Health facilities and health care professionals need PhilHealth accreditation in order to receive
reimbursements to PhilHealth.
(1) Health Facilities
The conditions that a health facility must satisfy before applying for PhilHealth
accreditations are (1) no record of a medical accident for at least 3 years (with some
exceptions) following the approval of its practice by DOH, (2) provision of an official
quality standard program, and (3) accountability for its own medical practice. The
following facilities may apply for accreditation.
∙ Hospitals
∙ Dialysis clinics
∙ Outpatient clinics (Rural Health Unites/ Health Centers, Dispensaries, Birthing Homes, etc.)
∙ Ambulatory surgical clinics
∙ Birthing Homes (Normal Spontaneous Delivery)
∙ TB Clinics
Table 4- 12 is the number of the accredited facilities as of the end of December 2015.
121
PhilHealth website
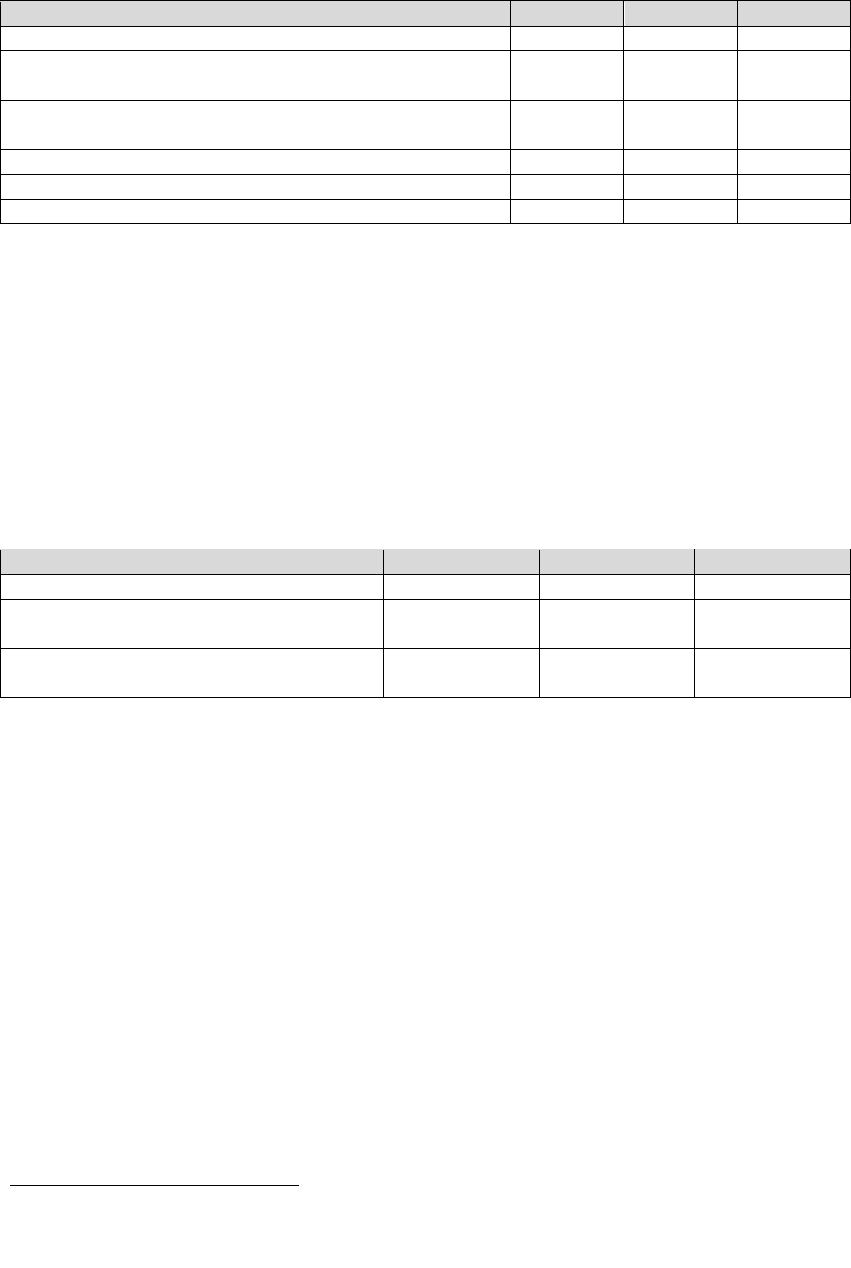
64
Table 4- 12 Institutional Providers with PhilHealth Accreditations
Category of the Institutional Providers
Private
Public
Total
Level 1: Offers primary care services
444
310
754
Level 2: Institution situating between Level1 and Level3,
equipped with general ICU and ICU for newborns
254
49
303
Level 3: Highest level institution offering education,
emergency care, and etc.
67
48
115
Other than above
370
345
715
Total
1,135
752
1,887
% Total
60%
40%
100%
Source: PhilHealth (2016). 2015 Stats & Charts.
Table 4- 13 summarizes the number of accredited outpatient clinics, the number of cities
and municipalities with accredited outpatient clinics and the proportion of cities and
municipalities with accredited clinics for Primary Care Package (PCB1), Maternity Care
Package (MCP) and TB/DOTS Package (DOTS Package.). PCB1 is available in nearly all
cities and municipalities with more than 80 percent available for MCP and DOTS Package.
Table 4- 13 Number of Accredited Outpatient Clinics, Number and Percentage
of Cities and Municipalities with Accredited Outpatient Clinics
PCB1
MCP
DOTS Package
Number of accredited outpatient clinics
2,553
2,981
1,739
Number of cities and municipalities with
accredited outpatient clinics
1,567
1,268
1,286
Percentage of cities and municipalities with
accredited outpatient clinics
99%
80%
81%
Source: PhilHealth (2016). 2015 Stats & Charts.
(2) Professionals
Physicians, dentists and midwives need to be accredited in order to receive PhilHealth
reimbursements. To ensure continuous accreditation from NHIP, renewal must be
completed annually by no later than 45 days prior to their birthday.
4-11 Funding for PhilHealth
Figure 4- 3 shows the premium contributions to PhilHealth for the years between 2008 and
2015. Significant increase in the government subsidy for the year 2014 is attributed to Republic
Act (RA) 10351, or the Sin Tax Reform Act of 2012.
122
122
15 percent of the incremental revenue collected from the excise tax on tobacco and alcohol products
shall be allocated for programs to promote economically viable alternatives for tobacco farmers and
workers. Out of the remaining 85 percent of the incremental tax revenue, 80 percent is allocated for
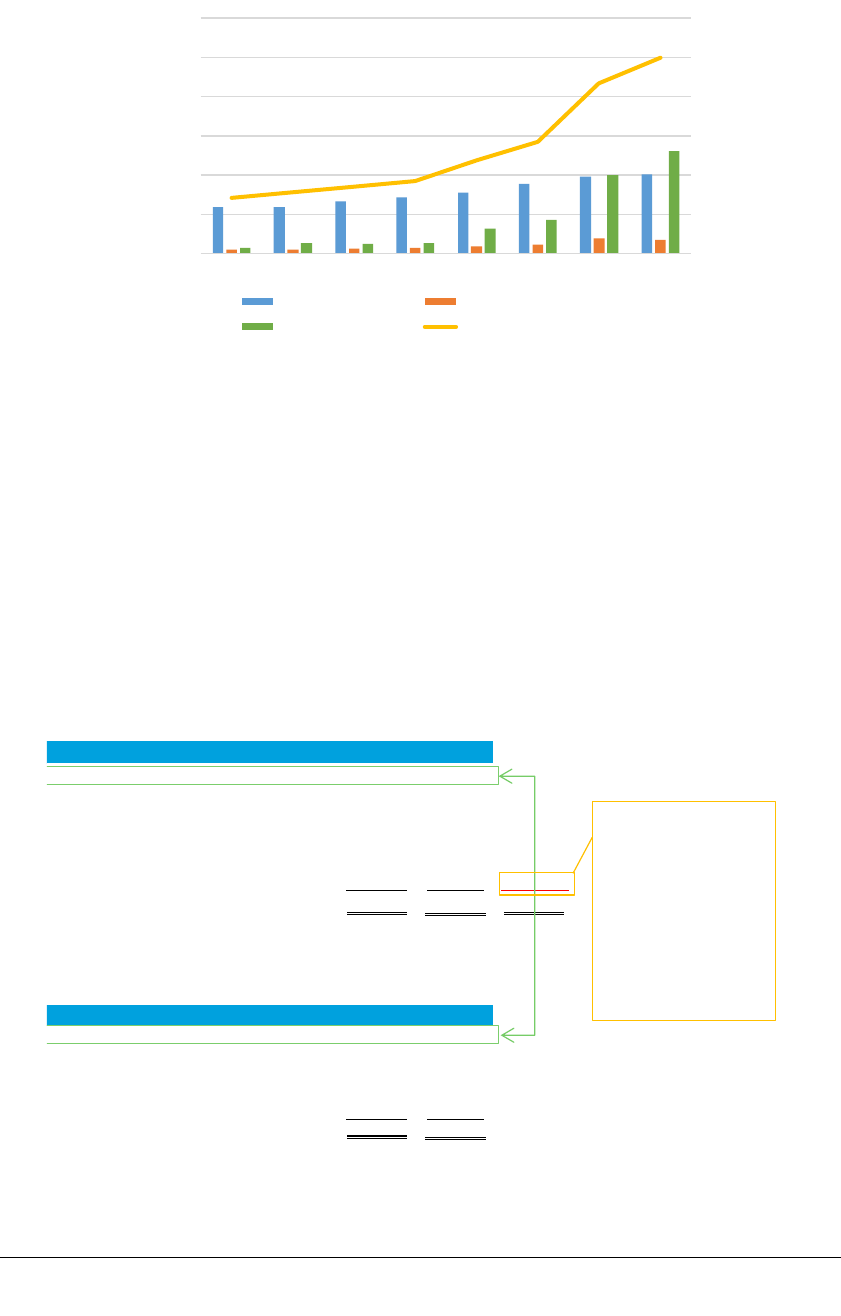
65
*
Government/Sponsored includes Indigent Members, Sponsored Members,
Senior Citizens and contributions from Special Government Programs
Figure 4- 3 Premium Contribution to PhilHealth by Membership Categories (in pesos)
Source: PhilHealth. (2010-2015). Annual Report 2009-2014 and PhilHealth. (2015). Annual Audit Report on
PhilHealth for the Year Ended December 31,2015.
4-12 Cross Subsidy among PhilHealth members
NHIP consists of Members with different professions and income levels. Consequently, some
Members pay higher contributions and claim less benefits than others.
Table 4- 14 Premium Contributions and Benefit Claims for 2015 by NHIP Members
Source: Annual audit report for the year ended December 31, 2015
universal health care under the NHIP for the attainment of MDGs and health awareness programs, and
20% for medical assistance and health enhancement facility programs.
0
20,000
40,000
60,000
80,000
100,000
120,000
2008 2009 2010 2011 2012 2013 2014 2015
Formal Economy Informal Economy
Government/Sponsored* Total
Premium Contributions for 2015
(million P)
Membership Type Amount %
Formal Economy 40,544 40.7%
Informal Economy
6,803 6.8%
Indigent-NHTS 36,258 36.4%
Senior Citizens 13,045 13.1%
Sponsored 2,893 2.9% 40,544
Special Gov't Program
82 0.1% (15,594)
99,625 100.0% 24,950
Benefit Claims Expense for 2015
(million PhP)
Membership Type Amount %
Formal Economy 24,950 25.7%
Informal Economy
20,173 20.8%
Indigent-NHTS 25,056 25.8%
Senior Citizens 19,328 19.9%
Sponsored 7,528 7.8%
97,035 100.0%
Formal Economy
claims PhP 15,549
million less in benefits
than they contributed.
This means that Formal
Economy effectively
subsidizes the other
members of PhilHealth

66
Table 4- 14 are the breakdowns of premium contributions and benefit claims for the year ended
2015. Members of the Informal Economy, the Senior Citizens and the Sponsored tend to claim
for benefits more than they contribute premiums, while Members of the Formal Economy and
the Indigent-NHTS-PR contribute more premiums than they claim for benefits. This means that
the formal economy and the public fund are subsidizing other members’ healthcare costs
through NHIP.
4-13 Enrollment and Utilization
(1) Population Coverage
Table 4- 15 summarizes the number of eligible beneficiaries
123
and population coverage of
PhilHealth as the fraction of the total population from 2010 to June 2016. Population
coverage as of the end of June 2016 stands at 90 percent.
124
It should be noted that there is
no consistency of data within the same membership categories. For example, while the
NHTS-PR was under Sponsored Members for the years 2010 to 2013, they are changed to
Indigent Members
125
for the years 2014 and 2016.
Table 4- 15 Number of Covered Members and Coverage Ratio from 2010 to 2015
Source: PhilHealth. (2010-9/2016). 2010-1st September 2016 Stats &Charts
123
Enrolled Members include those that are recorded as Members and their dependents having gone
through the enrollment procedure in the past, and includes those currently not paying contributions
(Interview with PhilHealth).
124
PhilHealth. 2015 Stats & Charts.
125
Indigents are defined by the National Household Targeting System for Poverty Reduction
Membership
Category
2010 2011 2012 2013 2014 2015 6/2016
Formal Economy
29.21 24.00 25.94 26.34 27.05 28.32 28.89
Informal Economy
9.91 9.91 11.82 11.99 7.38 8.46 8.31
Overseas Filipinos
5.09 5.09 5.23 5.86 - - -
Lifetime Members
0.95 0.95 1.25 1.32 1.61 1.73 2.05
Senior Citizens
- - - - 4.34 7.12 7.42
Indigent Members
- - - - 43.73 45.41 44.35
Sponsored Members
22.10 38.44 36.68 31.39 2.12 2.41 1.59
NHTS-PR
- 18.90 20.43 21.01 - - -
LGU/Regular
- 19.55 16.25 10.37 - - -
Covered Members
67.26 78.39 80.92 76.90 86.22 93.44 92.61
Projeted Population
90.89 95.60 95.88 97.70 99.56 101.45 102.90
Coverage Ratio(%)
74 82 84 79 87 92 90

67
(2) NHIP Utilization
Table 4- 16 summarizes the NHIP utilization rate, unique member claims reimbursed out
of the total eligible beneficiaries, from 2012 to June 2016. The rate has gradually
increased.
Table 4- 16 NHIP Utilization from 2012 to 2015NHIP
Year
Ratio of the Unique Member Claims
Reimbursed to the Total NHIP Members
2012
6%
2013
8%
2014
11%
2015
12%
6/2016
8% (January-June)
Source: “2012-2015 Stats & Charts”, PhilHealth
4-14 Supporting Indigents
(1) Facilitating Enrollments for Indigent Members
In 2011, PhilHealth adopted the National Household Targeting System for Poverty
Reduction (NHTS-PR) of the Department of Social Welfare and Development (DSWD) as
a means to identify indigent families. This has proved to be successful in increasing the
number of the Indigent Members in NHIP.
126
Families identified as indigent under the
NHTS-PR automatically become PhilHealth Members without any premium payment.
NHTS-PR is the system to determine whether a household is indigent through a proxy
means test
127
(PMT) that estimates the level of economic welfare of a household based on
its socioeconomic and demographic characteristics. DSWD, in collaboration with the
National Statistics Office (currently Philippines Statistics Authority), conducted a pilot
survey in 2007, thereafter conducting the first nationwide assessment in 2011.
NHTS-PR identifies indigents from the selected groups of population in order to make the
process efficient. On the basis of the Family Income and Expenditure Survey (FIES) and
Small Area Estimates (SMEs) results, all municipalities nationwide are classified as a
“very poor municipality,” which has more than 50 percent of Poverty Incidence (PI), and
the “moderate poor municipality,” which has less than 50 percent of PI. In the very poor
126
PhilHealth.
.
2011 Annual Report.
127
Income estimate survey based on the analyses of FIES and LFS, covering such items as household
members, their educations and professions, conditions of their house, access to basic services.
Face-to-face interviews are conducted based on the Household Assessment Form that consists of 34
questions on one double-sided sheet (Second survey is based on the Household Assessment consisting
of 52 questions.) There are two PMT Models – one for urban areas and one for rural areas

68
municipalities, all households are assessed. For the moderate poor municipalities, full
assessment is conducted only in pockets of poverty and for the rest of the moderate poor
municipalities, on-demand application was applied in which households are actively
encouraged to submit applications for assessment. In the first NHTS-PR assessment,
10,909,456 households in 489 very poor municipalities and 1,045 moderately poor
municipalities/cities were covered.
128
Interviews were conducted based on the Household
Assessment Form that consists of 34 questions. For the second NHTS-PR assessment, it
was converted into a Family Assessment Form as family is a more common unit to receive
social services (see Attachment 6). Reportedly about 55 million individuals, equivalent to
57 percent of the nationwide population, were covered in the first NHTS-PR assessment.
Thereafter, based on the latest Per Capita Poverty Threshold (PCPT) of each province, as
determined by the Philippine Statistics Authority (PSA), indigent households are identified
and listed in the Listahanan.
129
After posting the Listahanan in each community for some
period of time for the community members to request reinvestigation,
130
the Listahanan is
finalized and used for various social services.
Listahanan is mandated for renewal every four years, and the second assessment was
conducted from April to September in 2015. The data are currently analyzed. While the
first assessment was conducted on a household basis, the second assessment was
performed on the basis of the “family” unit, as are many social services, including NHIP,
are provided for a “family” (parents and children under 21),
131
instead of a household.
(2) No Balance Billing Policy
132
In addition to the NHTS-PR, PhilHealth adopted the No Balance Billing (NBB) policy for
the most common medical and surgical conditions in the country in 2011, to provide
optimal financial risk protection for the most vulnerable group, through PhilHealth Board
Resolution No. 1441, 2010. The NBB policy provides that no other fees or expenses shall
be charged or be paid for by the indigent patients above and beyond the packaged rates.
133
128
The National Household Targeting Office of the Department of Social Welfare and Development.
(2015). Listahanan.
129
Means list of household in Tagalog
130
On-site visits confirmed the postings of Listahanan at a community level. However, few residents
were aware of their rights for petitions.
131
Interview with DSWD (October 6
th
, 2016)
132
PhilHealth Circular No. 011-2011, New PhilHealth Case Rates for Selected Medical Cases and
Surgical Procedures and the No Balance Billing Policy
133
PhilHealth Circular No. 0003, s. 2014

69
The characteristics of NBB policy are as follows:
134
∙ The NBB policy is always applied when members are admitted to government health
facilities, while some private hospitals have adopted the NBB policy.
∙ The NBB policy is also applicable to non-indigent members for specific benefit
packages, such as the Maternity Care Package (MCP) and New-born Care Package
(NCP) in all accredited facilities.
In 2014, the NBB policy was expanded to cover Household Help, such as a household
driver and a housekeeper, as defined in the Republic Act 10361 or “Kasambahay Law.”
135
.
(3) Point-of-Care Enrollment Program
136
As mentioned earlier, the NHTS-PR is not able to reach all indigents in the Philippines.
Therefore, PhilHealth introduced another measure called the Point-of-Care (POC)
enrollment program in 2013 in order to cover non-NHTS-PR indigents. At health facilities
with POC accreditation, a Medical Social Worker (MSW) checks to see if the patient is
included in the list of PhilHealth Members, and if not, he/she conducts an interview. If the
patient is deemed indigent, the healthcare facility pays the annual premium of 2,400 pesos
and enrolls him/her into NHIP. POC is valid for a year and the patient is obligated to pay a
premium the following year to renew the membership. POC does not necessarily mean a
net cash outflow for a health facility because PhilHealth’s reimbursement usually makes
up for the premium payment of 2,400 pesos upon POC enrollment.
137
Adoption of POC is
mandated at all DOH-retained hospitals. LGUs and other health facilities need to obtain
approval by PhilHealth.
In enrolling patients through POC, an MSW estimates the patient’s monthly income based
on the interview compared with the PSPT
138
of the Region where the health facility exists,
and classifies the patient from A to D as stipulated in the DOH Administrative Order No.
51-A s. 2001, Implementing Guidelines on Classification of Patients and on Availment of
Medical Social Services in Government Hospitals (see Table 4- 17). The patient becomes
eligible for POC if she/he is categorized as C-3 or D. It should be noted that POC is the
PhilHealth program; however, the poverty threshold is set by PSA, while the patient
categorization into A to D is set by DOH.
134
PhilHealth Circular No. 011-2011
135
PhilHealth Circular No. 0003, s. 2014
136
PhilHealth Circular No. 0032. s.2013, October 14, 2013.
137
Interview with Jose Fabella Hospital
138
Refers to the PCPT for the region where a healthcare facility is located.

70
Table 4- 17 Patient Categories Based on the Ability to Pay
and Respective Payment Amounts
Patient
Category
Conditions for Qualification
Payment by Patient
Class A
Patient whose monthly per capita income is over 220% of
the latest PCPT for the region in which the hospital is
located, using a private room
Patient pays 100% of the
medical fee not covered by
PhilHealth
Class B
Patient whose monthly per capita income is over 220% of
the latest PCPT for the region in which the hospital is
located, using a shared room for 3 or more patients
Patient pays 100% of the
medical fee not covered by
PhilHealth
Class C-1
Patient whose monthly per capita income is between 180%
and 220% of the latest PCPT for the region where the
hospital is located
Patient pays 75% of the
medical fee not covered by
PhilHealth
Class C-2
Patient whose monthly per capita income is between 140%
and 180% of the latest PCPT for the region where the
hospital is located
Patient pays 50% of the
medical fee not covered by
PhilHealth
Class C-3
Patient whose monthly per capita income is equal to but
not more than the 140% of the latest PCPT for the region
where the hospital is located
The patient shall share any
affordable amount for
medicines provided and
ancillary services
rendered.
Class D
Patient whose monthly per capita income is less than
140% of the latest PCPT for the region where the hospital
is located
The patient shall not pay
for incurred hospital
charges.
Source: Administrative Order No. 51-A s. 2001, “Implementing Guidelines on Classification of Patients and on
Availment of Medical Social Services in Government Hospitals”
Despite the stipulation that POC can be utilized only once per Member, in reality, annual
membership renewal is not observed in many cases and some members wait until they are
hospitalized again and repeat POC.
139
Also there are some cases that A to C2 patients
insist that they cannot pay premiums and the health facilities have the MSW look for a
sponsor or become a sponsor himself/herself. When the MSW is unable to find a sponsor,
the MSW intentionally categorizes such patients as C3 or D. The patients classified as C1
and C2 are required to pay 25 percent and 50 percent of the medical bills respectively, and
encouraged to pay for the annual premium.
140
(4) Conditional Cash Transfer
The Conditional Cash Transfer (CCT) program in the Philippines, known as Pantawid
Pamilyang Pilipino Program (4Ps), is the social welfare program offered by DSWD. It was
introduced in 2008 with the objectives of providing monetary as well as social assistances
139
Interview with Dr. Jose Fabella Memorial Hospital
140
Interview with DOH Health Facility Development Bureau (October 4, 2016)

71
for poor families with children 0-18 years old.
141
Although CCT is outside the framework
of NHIP, this subject is briefly touched herein as both CCT and NHIP support indigents.
[Eligibility]
Poor households are identified by the NHTS-PR that employs a statistical model to
estimate income, as explained earlier. The following criteria must be satisfied to become
eligible for the CCT program.
142
∙ Residents of the poorest municipalities, based on the 2003 Small Area Estimates of
the National Statistical Coordination Board (incorporated into the Philippine Statistics
Authority today)
∙ Households are deemed to be “indigent” whose economic conditions are equal to or
below the provincial poverty threshold
143
∙ Households that have children 0-18 years old and/or have a pregnant woman at the
time of assessment
∙ Households that agree to meet conditions specified in the CCT program
As of August 26, 2015, there were 4,353,597 active household beneficiaries, 570,056 of
whom are indigenous households. The program also covers 10,235,657 schoolchildren
aged 0 to 18.
144
Eligible members are provided with ID cards and assigned to a health facility.
[Cash Grants and Conditions for Payment]
Two types of cash grants are provided to the household-beneficiaries:
∙ Health Grant: 500 pesos/ household every month totaling 6,000 pesos per year
∙ Education Grant: 300 pesos/ child every month for 10 months, totaling 3,000 pesos
per year
Cash grants are distributed to the household through the Land Bank of the Philippines or
any other alternate payment scheme, such as rural bank transactions.
141
Official gazette of the government of the Philippines. Pantawid Pamilyang Pilipino Program.
142
ibid
143
Poor Household, is identified through a “Household Assessment” survey conducted by DSWD,
recorded onto NHTS-PR by the same. First Household Assessment was conducted in 2009 and 2010
covering 17 million households, with the latest conducted in 2015 covering 20 million households.
Results of the 2015 survey are being complied as of the date of this writing.
144
Official gazette of the government of the Philippines. Pantawid Pamilyang Pilipino Program.

72
To receive the cash grants, all of the following conditions must be met by the household
beneficiaries.
145
1. Pregnant women use pre- and post-natal care, and be attended during childbirth by a
trained professional
2. Parents or guardians attend family development session with topics, such as
responsible parenting, and health and nutrition
3. Children aged 0-5 receive regular preventive health check-ups and vaccines
4. Children aged 6-14 receive deworming pills twice a year
5. Children-beneficiaries aged 3-18 enroll in school, and maintain an attendance of at
least 85 percent of class days every month
Compliance rates are generally high. In March and April 2015, for instance, the lowest
compliance rate was 94.84 percent for the condition 2 above.
146
[Promotions of NHIP Benefits to CCT Beneficiaries]
Although the CCT beneficiaries are automatically enrolled with NHIP, 5-6 percent of the
CCT beneficiaries are not aware of this fact.
147
Also, their NHIP utilization rate is low. In
order to promote NHIP utilization by CCT beneficiaries, DSWD is engaged in the
following promotional activities:
∙ PhilHealth representatives conduct seminars to explain PhilHealth benefits to CCT
beneficiaries.
∙ DSWD recommends health facilities place signboards indicating that the CCT
beneficiaries will not need to shoulder medical bills as they are automatically covered
under the NBB policy of NHIP, as there are many cases wherein patients are hesitant
to go to health facilities for fear of having to pay medical bills.
145
Official gazette of the government of the Philippines. Pantawid Pamilyang Pilipino Program.
146
ibid
147
Interview with DSWD
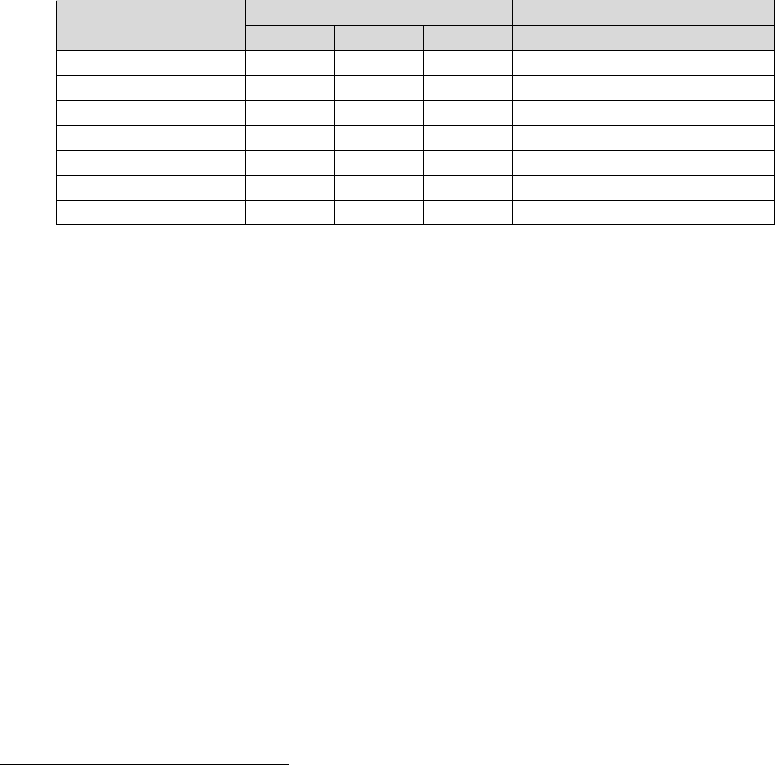
73
Chapter 5 Maternal and Child Health Services in Bicol and
Eastern Visayas Regions
5-1 Bicol Region (Region V)
(1) Regional Profile
① Socioeconomic Profile
Bicol region is comprised of the southern part of Luzon with six provinces. Legaspi city
and Naga city are the center of commerce, finance and transportation, while the main
industries of the region are agriculture and fishing. The economic growth rate in 2015 was
the highest in the country at 8.4 percent, however, the GDP per capita was the second
lowest with 25,648 pesos after ARMM.
148
Provincial populations in Bicol region is
shown in Table 5- 1.
Table 5- 1 Provincial populations in Bicol Region (in thousand)
Population
Population Growth Rates
2000
2010
2015
2010-2015
Albay
1,091
1,233
1,315
1.22
Camarines Norte
471
543
583
1.38
Camarines Sur
1,552
1,822
1,953
1.32
Catanduanes
215
246
261
1.11
Masbate
708
835
892
1.28
Sorsogon
651
741
793
1.30
Region
4,688
5,420
5,797
1.29
Source: Philippine Statistics Authority
② Maternal and Child Health (MCH) Status
Figure 5- 1 shows the trend of maternal mortality rate (MMR) in Bicol based on FHSIS
data, which are different from that of the Albay Provincial Health Office whose number of
matarnal death was 44 in 2014, 29 in 2015 and 6 up to July 2016. Although it is generally
believed that quality of FHSIS data is not high, the number of maternal death differs
depending on whether it is counted based on the patient residential area or the area of
occurrence. On the other hand, the DOH Regional Office reported that, since 2015, the
number of deaths has been registered based on the patient residential area and the data of
the private health institutions have been included in the Field Health Service Information
System (FHSIS) to enhance credibility. However, as a result, it has become difficult to
compare the data before and after 2015. In Bicol region, maternal and newborn death
review was introduced in 2015 as requested by the central government.
148
Philippines Statistics Authority 2016

74
Figure 5- 1 Trend of maternal deaths and MMR in Bicol
Source: FHSIS from DOH Bicol Regional Office
Most of maternal deaths have occurred at Level 3 hospitals or on the way to hospitals in
the Philippines. Table 5- 2 shows the number of deaths at two regional hospitals in Bicol. It
has slightly improved in 2016.
Table 5- 2 Number of maternal deaths at tertiary hospitals
2013
2014
2015
2016
Bicol Regional Training and Teaching Hospital (BRTTH)
34
47
35
16 (Aug)
Bicol Medical Center (BMC)
38
36
38
5 (June)
Source: BRTTH and BMC
Facility-based delivery (FBD) has been increasing in all areas as shown in Table 5- 3. On
the other hand, the rate of antenatal care (ANC) visits has been around 50 percent in the
region and no major change has been seen over the last few years.
Table 5- 3 Proportion of FBD (%) by province/city
Province/City
2011
2012
2013
2014
2015
Albay
67.7
76.5
90.1
87.7
93
Cumarines Norte
41
38.2
68.5
81.7
86
Cumarines Sur
19.9
38.7
37.2
58.6
63.7
Catanduanes
79.1
85.7
88.6
90.3
90.4
Masbate
30.5
39
42.6
75.4
83
Sorsogon
85.9
91.9
93.8
94.8
96.1
Iriga city
13
34.5
7.8
13.5
89.6
Legaspi city
44.9
100
33.1
95.4
98.2
Naga city
42.1
44.8
71.2
83
88.2
Region
46.5
57.2
61.9
78.9
86.2
Source: FHSIS from DOH Bicol Regional Office
The infant mortality rate (IMR) in Bicol is shown in Table 5- 4. While it has been static
over the last five years, it is lower than the national average.
0
20
40
60
80
100
120
0
20
40
60
80
100
120
140
2011 2012 2013 2014 2015
No of Death
No of Death MMR

75
Table 5- 4 IMR by province/city
Province/City
2011
2012
2013
2014
2015
Albay
8.1
8.4
5.6
4.5
4.2
Cumarines Norte
15.3
14
13.2
9.6
9.9
Cumarines Sur
11.8
8
4.9
5.3
4.4
Catanduanes
8.6
7.4
8.9
18.7
7.9
Masbate
7.3
0
18.1
20.5
11
Sorsogon
6.2
9.1
7.3
6.9
5.1
Iriga city
12.8
5.2
9
19.3
14.4
Legaspi city
10.6
8
2.4
14.2
5.6
Naga city
12.8
15.9
10.9
35
20.8
Region
9.7
8.8
8.5
10.5
7.1
Source: FHSIS from DOH Bicol Regional Office
③ Health Governance
The DOH Bicol Regional Office is composed of the Local Health Support Division
(LHSD), Licensing, Regulation and Procurement Division and Management Support
Division. LHSD is in charge of technical projects and the Family Health Cluster under
LHSD is responsible for MCH. The LHSD total budget in 2016 is 194 million pesos and
the budget of the Family Health Cluster in 2016 is 26 million pesos. Provinces develop a
three-year Local Investment Plan for Health (LIPH) and receive their budget from the
DOH regional office based on the approved plan.
The number of hospitals registered in the region is shown in Table 5- 5. Several hospitals
have been downgraded to infirmaries in 2015 through the new DOH hospital criteria.
While private hospitals are mainly located in the urban areas, private lying-in clinics exist
in most of the municipalities.
Table 5- 5 Registered number of public and private hospitals (2015-2016)
Type
Public
Private
Level 3 hospital
2 (DOH)
1
Level 2 hospital
4 (LGU)
12
Level 1 hospital
16 (LGU)
15
Source: DOH Bicol Regional Office
(2) Overview of Study Sites
The study was conducted in two provinces – Albay and Camarines Sur (CS) out of the six
provinces in Bicol.

76
[Albay]
Albay province is the center of Bicol region and the Provincial Health Office and the
PhilHealth Regional Office exist. The provincial health budget was 220 million pesos in
2016. In principle, 20 percent of the provincial budget should be allocated to the health
sector, however, the proportion is lower than that now. There is also the fund based on the
three-year LIPH.
Regarding public health facilities, the Bicol Regional Training and Teaching Hospital
(BRTTH), Level 3 hospital, is in Legaspi City, and there are four Level 1 hospitals as of
2015. FBD rate and the proportion of women receiving more than 4-time ANC are higher
than the national average.
[Cumarines Sur]
Cumarines Sur (CS) is located in the center of Bicol region and it has the largest land area
and population in the region. The provincial health budget was 20 million pesos in 2016.
There is also transferred budget from DOH, but it is usually insufficient. It was also
reported that size of the staff is also insuffient in order to execute all the health programs.
Another Level 3 hospital in the region, the Bicol Medical Center (BMC), is located in
Naga City and there are three Level 1 hospitals, including the Naga City Hospital, in CS.
Currently, a provincial hospital is being constructed. In Naga City, outside the provincial
governance, there is the Naga City Hospital and an infirmary. In CS, FBD rate is lower
than other provinces.
(3) Study Findings
[Study sites]
The study sites in Albay and CS provinces are shown in Table 5- 6. The visits/interviews
were conducted with LGU health offices, RHU, BHS, public and private health facilities,
PhilHealth offices and community members.
Table 5- 6 Study Sites and Community Interviewees
Province
City/Municipality
Barangay
Interviewees
No
Albay
Malinao
Balading, Burabad
Pregnant and lactating women
39
Camarines
Sur (CS)
Naga City
(Independence city)
Panicuason, San Isidro
Husbands
3
Pamplona
Batang, Poblacion
Women with grand children
3
Sipocot
Binahian
TBA
1
Source: JICA Survey Team

77
[Supply Side]
1) Service Delivery
While all the RHUs were supposed to be equipped with a delivery facility, the study
team observed that some of them did not have a delivery facility due to the lack of
human resources or insufficient infrastructure. It is desirable for RHUs to have a
delivery facility particularly in remote areas where no public hospitals or private
lying-ins are available. The cost of MCH services at visited RHUs is free based on
municipal policy, which could be user-friendly for community members, but it could
also burden health facilities unless enough resources are provided by the municipal
government.
Some of the district or municipal hospitals, which were downgraded to infirmaries in
2015, explained that the high-risk cases are now immediately referred to the regional
hospital as they can no longer take care of high-risk cases under the current mandate.
There are two Regional hospitals in Bicol that are located in Albay and CS provinces.
Most caesarean sections and/or high risk cases in the Region are referred to the two
hospitals. In addition, many women prefer the well-equipped Regional hospital even for
normal delivery; caesarean section accounts for approximately 30 percent of total
deliveries at the regional hospitals. Consequently, those two Regional hospitals are
always highly overcrowded and it could at times effect the implementation of
emergency operations, their original mandate. It was observed that two to three women
and their babies were sleeping in one bed. The regional hospital is considering
establishing a BEmONC for normal delivery within the compound of the hospital, so
that the Regional hospital as CEmONC could focus on high-risk cases as mandated.
2) Referral and SDN
The DOH regional office has been
strengthening/reactivating the delivery
networking system in the Region with
the assistance of LuzonHealth. In Albay,
the province was divided into three zones
and Inter-local Health Zone (ILHZ) and
Service Delivery Network (SDN) have
been established in each zone. ILHZ is
led by municipalities and its purpose is to
coordinate public health issues among
Figure 5- 2 Rural Health Unit
in Camarines Sur

78
concerned municipalities. In terms of SDN, the province issued the ordinance of the
MCH SDN and it included the public as well as private health facilities. Collaboration
with private facilities was obtained by providing them with free training and
information. Regular meetings are held separately for ILHZ and SDN.
In CS, there was one functioning ILHZ, called CASILI, with the three municipalities of
Cabusao, Sipocot and Libmanan. It started activities in 2005 when three municipalities
issued a joint ordinance on the MCH ILHZ. This joint ordinance enabled ILHZ to
continue functioning for the last 10 years even with a change of mayors as the joint
ordinance could not be invalidated unless all mayors agree. They hold a joint trust fund
with approximately 500,000 pesos of annual budget and developed a three-year plan for
the fund. Activities include joint procurement of drugs from the Regional stock yard,
bulk printing of reporting formats/booklets, death review, and discussions on common
issues. Private facilities were also involved in ILHZ and vaccines were provided free of
charge by the municipality health offices. ILHZ reactivation in the other areas was
planned; however, the issuance of joint ordinance with multiple municipalities appeared
to be challenging.
BOX 5- 1 Story of RHU Medical Doctor outside CASILI Zone
There is also a plan led by the DOH regional office to establish an inter-facility referral
system in CS. Based on the successful experience in Albay, a meeting is going to be
held with various stakeholders including public and private health facilities – both
hospitals and non-hospitals – to discuss the issues, such as the development of referral
policies/guidelines and the standardization of the referral format.
When an ambulance referring a pregnant woman to BMC passed by our RHU, I received
a call from them. I immediately went to the ambulance and gave the woman oxygen, but
I could not save her. There was only her husband and no medical staff attended her in the
ambulance. I wished I had received a call earlier, so that I could have collaborated with
other medical staff and provided her with better service. However, unfortunately, one can
only receive medical services from the RHU in the residential area.
79
3) Maternal Death Review
The majority of maternal deaths reportedly occur
at referral hospitals or on the way to the
hospitals. A death confirmed within 72 hours
from arrival is registered as non-institutional and
such cases account for around half of the deaths
at the Regional hospitals in Bicol. The two
Regional hospitals attempt to strengthen death
review activities that lead to concrete actions to
reduce the number of maternal deaths.
Bicol Regional Training and Teaching Hospital (BRTTH) receives referral cases within
and outside the province including Catanduanes and Sorsogon. It accounts for the
highest number of deaths in the region. The hospital strengthened its efforts on maternal
death review in 2015.
BOX 5- 2 BRTTH leadership (Story of DOH Regional Officer)
The maternal death review has been given strong leadership from the hospital chief. The
comprehensive and in-depth review of all deaths, namely route cause analysis,
identification of three delays, referral condition, direct death cause audit and so on was
conducted at an internal conference in 2015. Concrete recommendations and action plans
have been developed as a result. BRTTH also sought to improve collaboration with other
health facilities through participation in SDN/ILHZ meetings, provincial death review or
other opportunities and advocacy for promotion of effective referral policies/guidelines.
4) NHIP Implementation and Utilization
The number of NHIP accredited health facilities has been increasing annually in Bicol.
As of August 2016, there were 292 NHIP-accredited health facilities, 187 of which were
primary health facilities and 105 were hospitals, and 186 NHIP-MCP accredited health
facilities, 99 of which are public facilities and 87 are private facilities. The PhilHealth
office conducts regular monitoring including surprise visits to the health facilities to
ensure adherence to various policies including the No Balance Billing (NBB) Policy.
The office also visits municipalities once a year and conducts awareness-raising
campaigns for communities.
Figure 5- 3 BRTTH
80
Two regional hospitals follow the NBB
Policy and Point of Care (POC) program.
However, as described below, there were
some cases in which indigent people
could not utilize POC at the public
hospitals. PhilHealth-accredited private
facilities are also supposed to follow the
NBB and the POC Policies. The
adherence rate has been increasing due to
PhilHealth regular monitoring. Full
implementation by private facilities is PhilHealth’s current challenge.
The online system has been gradually operationalized in Bicol. The
improvement/correction of the database is required for smooth and full scale operation.
Also, it is ideal to make online payment claims possible as it is currently only accepted
in the PhilHealth provincial office. The disbursement of NHIP benefits for LGU-owned
hospitals is made to LGU bank accounts and some LGUs do not allocate facility fees
properly to the appropriate health facilities.
According to the PhilHealth Bicol Regional office, currently there are more benefit
claims than collected premiums in Bicol. Loss has been offset by other regions;
however, there was a concern that the premium amount would have to be reviewed soon
if utilization keeps increasing. The current challenges include full implementation of
NBB Policy for both public and private facilities, behavioral changes of the community
in remote areas and an increase in the number of PhilHealth officers in provincial and
regional offices.
Overall, NHIP introduction is seen to have contributed to the improvement of public
health services in the Region (see BOX 5- 3).
BOX 5- 3 Story of Provincial Health Officer
Public hospitals used to lack medical specialists, such as obstetricians or anesthetists, due
to a deficiency in the market. Now that the NHIP professional fees are available, specialists
go under contract with multiple public hospitals and receive payment per service. The
experienced doctors have improved the quantity and quality of services at the public
hospitals in Bicol. The regional hospitals are also making efforts to provide incentives for
the retention of experienced doctors, by providing them with private rooms where patients
receive exclusive care with extra professional fees.
Figure 5- 4 PhilHealth Bicol
regional office

81
5) NHIP Awareness
Awareness of NBB Policy and the POC program varies from facility to facility. In
general, the knowledge level of NHIP is found to be sufficient among LGU and regional
hospital personnel and adherence to NHIP policies was established in the regional
hospitals.
On the other hand, the knowledge level among barangay personnel, including BHWs,
seems to be limited. The NHIP Indigent Member list was produced by the DSWD and
PhilHealth distributed Member Data Record (MDR) based on the list to the members via
RHUs. The personnel at visited barangays mentioned that while they were aware of the
NHTS-PR assessment mission to have visited their community for the purpose of
producing the NHIP Indigent Member list, they did not receive feedback from the
assessment team and did not know how the list was produced.
Figure 5- 5 Barangay Health Station in Camarines Sur
For the community members, information on NHIP was usually provided through the
PhilHealth advocacy campaign held annually at all municipalities, monthly education
sessions for 4P beneficiaries and household visits and health education by BHWs. Some
of the BHWs, who were members of Community Health Team (CHT) or focal persons
for NHIP, have opportunities to receive information from LGUs or PhilHealth.
However, in general, there is limited opportunity for the BHWs. Therefore, community
members, except for 4P beneficiaries, tend to have limited knowledge about NHIP.
6) LGU Financial Assistance
Most of LGUs, barangays, and RHUs own ambulances or public transportation, such as
police or security vehicles, that can be used free of charge or with a nominal fuel fee for
emergency cases, including delivery. Some barangays established emergency

82
transportation funds to hire registered private vehicles to be used for delivery for free.
At the same time, interviews with pregnant and lactating women reveal that many are in
fact paying for transportation to go to a health facility. Details will be described below.
Provision of NHIP sponsorship by LGUs varies depending on the LGU’s priority issues
and budgetary situation.
LGUs informed TBAs of the prohibition on home delivery, and some of them are
proactively involved in safe-motherhood efforts by providing incentives for bringing
pregnant women to health facilities.
7) Effects of Devolution
The level of health service delivery depends on the capacity and leadership of the LGU.
The LGU leader is elected every three years and this can make it challenging to
maintain a high level of commitment and resources. The collaboration among health
facilities managed by different LGUs is also not easy. Under these circumstances, the
DOH Bicol Regional Office showed strong leadership to strengthen the Service
Delivery Networking and coordination mechanism among concerned facilities and
LGUs, and expanded good practices in different provinces. The DOH Reginal Office
would play an important role under the devolution in improving the collaboration among
various stakeholders and assisting resource-limited LGUs.
[Demand Side]
1) Health Service Utilization
There are still 15 percent home deliveries occurring in Bicol and it appears to be more
prevalent in the remote areas. However, it has been decreasing rapidly mainly due to the
issuance of the LGU ordinance on home delivery prohibition. Midwives/health care
providers at BHSs/RHUs constantly advise pregnant women to deliver at a health
facility. Family members also tend to
suggest the same for the sake of safe
delivery.
The majority of women responded that
they respected health care providers at
BHS/RHU or hospitals and followed
their advice for safe motherhood. Most
of those who were diagnosed high risk
Figure 5- 6 Group discussion
with pregnant and lactating women
83
had additional laboratory tests at a private facility or were referred to the regional
hospital.
On the other hand, several negative opinions were stated that the public health facilities
were overcrowded, required long wait times, provided insufficient treatment/services, and
the health care providers had disrespectful attitudes. Particularly the over-crowdedness of
the regional hospitals was emphasized by women and BHS/RHU health workers.
However, many of them took it for granted and they said that they do not have high
expectations for the public health facilities. There were a few cases of home delivery that
could have been avoided if addressed in better ways at the facility or health care providers,
as described in BOX 5- 4.
BOX 5- 4 Home delivery cases
One case involved a woman who went to the hospital with her husband for delivery, but the
midwife told them it was not time and sent them back home. As soon as they reached
home, the woman’s water broke and she went into labor. They immediately called a TBA
and the woman delivered at home.
Another case was a teenage mother who went to a private lying-in facility but was advised
to go to the hospital as a maternal age below 19 years old could not be accepted at a
non-hospital to receive the NHIP benefits. She did not consult with anyone and did not go
to the hospital, then ended up with a stillbirth delivery at home.
Better off families tend to pay extra fees, around 20,000 pesos, and use a paid room in
the public hospital where they can have an exclusive doctor and nurse with better
facility conditions. Private facilities are also cleaner and the health care providers have a
better attitude compared to the public facilities. Therefore, many women prefer the
private facilities despite additional fees for drugs or bed linens.
2) NHIP Enrollment and Utilization
NHIP Enrollment rate in the Bicol region is 89 percent as of June 2016. The detail is
summarized in Table 5- 7. Utilization rate of MCP has been rapidly increasing in recent
years (see Figure 5- 7).

84
Table 5- 7 NHIP coverage by sector and by province in Bicol as of June 2016
Source: PhilHealth regional office V
Figure 5- 7 MCP utilization amount in Bicol (up to June in 2016)
Source: PhilHealth regional office V
Among the interviewed women, all of them were NHIP members and had utilized MCP
benefits. They unanimously stated that this was extremely helpful. It was reported that
around 75 to 90 percent of households were indigents in the visited barangays. In the
ANC session, they were advised to save money as part of a birthing plan, but most of
them did not have enough income for saving. Many of them previously used to borrow
money from relatives or friends for delivery costs. However, thanks to NHIP benefits,
they said that they do not have to borrow
money or reduce expenses on food or
other essential items anymore.
However, not all indigents are covered by
the NHIP and availability of LGU
sponsorship varies as stated earlier. The
coverage of indigents by NHIP was
reportedly around 30-50 percent in the
visited barangays.
Formal
economy
Informal
sector
Indigent Sponsored
Migrant
w orker
Lifetime
Senior
citizen
Coverage
rate
Albay 273,987 42,941 671,515 28,795 13,438 26,110 96,068 87%
Camarines
Norte
88,589 38,390 329,253 9,573 7,037 10,844 43,136 89%
Camarines
Sur
329,270 73,356 1,087,065 15,161 21,081 28,805 83,202 83%
Catanduanes 44,502 6,939 176,247 1,620 2,070 6,524 13,831 95%
Masbate 91,445 10,327 707,892 15,552 1,920 7,660 23,333 95%
Sorsogon 125,518 24,711 619,876 2,439 5,822 11,065 34,748 113%
Region 953,311 196,664 3,591,848 73,140 51,368 91,008 294,318 89%
0
100
200
300
400
500
600
2011 2012 2013 2014 2015 2016
Million pesos
Figure 5- 8 Barangay houses
in Camarines Sur

85
In terms of the knowledge among communities, the majority of women knew about free
MCH services by NHIP benefits at PhilHealth accredited facilities. However, the
information, requirements and conditions for the NBB and POC Policies were unknown
to most of them. Regional hospitals reported that many referred women who were
indigents could not receive POC as they could not submit the required documents of
birth and marriage certificate on time. Community members, except for 4P beneficiaries,
did not seem to have enough opportunities to receive NHIP-related information.
3) Barriers to health services
Meanwhile, there were many women among the interviewees who would still prefer
home delivery if there were no ordinance. Barriers or challenges inhibiting their access
to health facility services mentioned during the interviews are described below.
<Economic Factors>
Medical Fee: In principle, the MCH-related medical fees are covered by NHIP for
its members at the PhilHealth accredited facilities. However, there were many
cases that out-of-pocket payment was required for some purposes, such as (1)
drugs as the facilities often run out of stock and patients need to purchase outside
the facility, (2) gloves or baby’s diapers, and (3) new-born screening. The amount
of payment ranges from 200 to 3,000 pesos at public and private facilities. The
laboratory test, such as ultrasound for high-risk cases, is usually not available at
BHSs/RHUs and it costs a woman 750-1,000 pesos at a private health center.
For those without NHIP, the public hospitals usually charge 2,000 to 5,000 pesos
for a normal delivery. Even without NHIP, indigents are supposed to be covered by
POC. However, in fact, some of the indigents report that they had made payments
at a public hospital. There are also cases, as described earlier, that POC cannot be
utilized due to the failure of document submission within the defined period.
Transportation: As previously mentioned, most hospitals or LGU health offices
provided public transportation for free or with nominal fees for delivery. The
transportation fees were claimed to be big burden. However, interviews revealed
that more than half of the women had paid for transportation. Those who lived in
the center of a city or municipality 10-20 minutes from a health facility paid 200 –
300 pesos round trip, and those who lived in remote areas 1 – 1.5 hours from a
health facility required 1,000 pesos to reach a district hospital by boat and vehicle,
and 1,500 pesos to reach a regional hospital. It would take much more time and

86
cost for people living in very remote areas or outside two provinces, to reach a
referral hospital.
Others: In addition to the cost for accompanying family members for
accommodation, food and transportation, some indigent women buy new clothes as
they feel embarrassed to wear old clothes in front of other people. Additionally,
payment is required for caretakers for their children or other family members while
they are away from home.
<Sociocultural Factors>
The majority of women answered that they could make the decision on where to deliver
on their own. Many pregnant women, who had previously delivered at home, stated that
they were planning to give birth at a facility this time as home delivery had been
prohibited. Their mothers, who predominantly delivered at home, also suggested to have
a facility-based delivery for their safety.
On the other hand, a few women answered that they had followed the advice of their
mother, husband or TBA for the first delivery. There was a case of a husband who
decided on home delivery due to financial constraints and his wife had no say. The TBA
charges 1,500 – 2,500 pesos, but payment on credit or installments is usually accepted.
However, health facilities do not discharge the patient unless payment is complete.
Women who have experienced home delivery frequently mention that they never
experienced complications or problems at home and never heard of maternal death in
their communities.
149
Therefore, it seemed that they do not feel they face risk in
delivery. They said that the home delivery was more convenient as they could do
housework until the last minute and almost right after the delivery. Facility-based
delivery requires time, money and preparation work. It was also mentioned that finding
a caretaker for children is not easy. Several of them had home deliveries due to
unavailability of caretakers.
BHSs/RHUs and hospitals regularly conduct pregnancy educational sessions and
encourage women to come with their partners. However, it was reported that not many
men actually participated in the session. In terms of family planning, the majority of
interviewed women were using or had used some kind of contraceptive devices, despite
149
Doctors, midwifes or nurses at BHSs/RGUs reported a few cases of maternal and neonatal deaths and
still births in the community and inappropriate practices of TBA or birth attendants in the home
deliveries.

87
the fact that all of them were Catholic. Some mentioned that they had received
information on family planning at the church. Thus, it was inferred that the access to
family planning was not a big challenge for most of women. However, it was still not
rare to have a big family with more than 10 children.
150
5-2 Eastern Visayas (Region VIII)
(1) Regional Profile
① Socioeconomic Profile
Eastern Visayas Region is located in the eastern part of the Visayan islands in central
Philippines, composed of Samar, Leyte and Biliran islands. It has six provinces, one
independent city (Ormoc city), 1 highly urbanized city (Tacloban city) and five component
cities with 4.4 million population in 2015.
151
Tacloban is considered as a regional center
for commerce, transport, culture and trade. Main industries of Eastern Visayas include
farming (such as rice and coconuts), fishing, mining and tourism. Nevertheless, the region
has the second highest poverty incidence among families in the country.
152
In November
2013, Typhoon Yolanda devastated the region. Table 5- 8 shows populations of provinces
and a highly-urbanized city. The population of Leyte province except that of Tacloban City
is the largest, followed by Samar province.
153
Table 5- 8 Provincial populations in Eastern Visayas Region (in thousand)
Population
Population Growth Rates
2000
2010
2015
2010-2015
Biliran
140
162
172
1.13
Eastern Samar
376
429
467
1.64
Leyte
1,414
1,568
1,725
1.83
Northern Samar
501
589
632
1.36
Samar
641
733
780
1.19
Northern Leyte
360
399
422
1.05
Tacloban City
179
221
242
1.73
Region
3,611
4,101
4,440
1.52
Source: Philippine Statistics Authority
150
The total fertility rate in Bicol Region was 4.6 on the basis of the NDHS 2013. cf. The national total
fertility rate was 3.0 and that in Eastern Visayas was 4.0.
151
Philippines Statistics Authority, 2016.
152
The poverty incidence among families in Eastern Visayas is 37.4% in 2012 according to the
Philippines Statistics Authority.
153
Samar province is also called Western Samar province.

88
② Maternal and Child Health (MCH) Status
Figure 5- 9 MMR and IMR of Eastern Visayas
Source: DOH Eastern Visayas
Although MMR and IMR of Eastern Visayas Region declined after 2013, not much
improvement has been observed in the past five years (see Figure 5- 9). With regard to
FBD rates, all provinces have experienced significant improvements (see Table 5- 9).
Table 5- 9 Provincial FBD Rates in Eastern Visayas
Source: DOH Eastern Visayas
On the other hand, the FHSIS data for maternal deaths and infant deaths collected by the
DOH are calculated based on the location of the occurrence of death instead of the
residential location of the deceased. For instance, MMR in Tacloban city (359.42 per
100,000 live births) and Ormoc city (185.19 per 100,000 live births) are higher due to the
0
1
2
3
4
5
6
7
8
9
10
0
20
40
60
80
100
120
140
2011 2012 2013 2014 2015
IMR/ 1,000 live births
MMR/100,000 live births
MMR IMR
Province 2011 2012 2013 2014 2015
Biliran 95.7 95.93 99.1 97.45 97.2
Eastern Samar 64.5 74.5 82.9 88.26 91.92
Northern Leyte 7.8 80.21 87.19 90.7 92.99
Nothern Samar 29.36 41.94 52.93 64.3 77.8
Southern Leyte 78.56 64.87 74.68 97.08 98.55
Samar 34.33 30.84 57.82 72.49 81.56
Calbayog City 26.32 34.37 38.4 47.01 66.94
Massin City 84.8 90.56 96.85 99.17 98.02
Ormoc City 75.15 86.43 91.17 90.88 96.87
Tacloban City 86.72 89.6 86.62 85.51 94.64
Region-wide 62.21 66.25 75.81 83.08 89.05
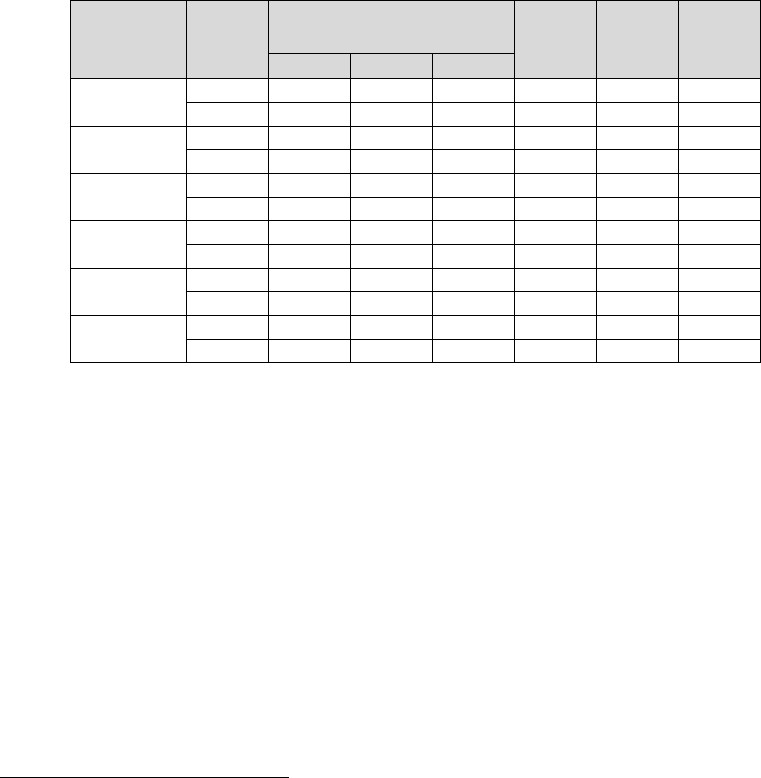
89
presence of high level hospitals
154
while in Leyte province excluding those cities has a low
MMR (41.51 per 100,000 live births). Such calculations make it difficult to have a grasp of
the situation of maternal deaths in different areas.
155
Health facilities registered at the DOH Regional Office in Eastern Visayas are listed in
Table 5- 10. It shows that 44 percent of them are located in Leyte province where Tacloban
city is. In addition, Level 3 hospitals are limited to one government hospital (EVRMC:
Eastern Visayas Regional Medical Center) and one private hospital in the entire Region.
Table 5- 10 Registered Health Facilities in Provinces of Eastern Visayas
(As of August 2, 2016)
156
Source: DOH Eastern Visayas
In addition to the fact that there is only one government Level 3 hospital, due to the
improved referral system and resultant increased facility-based deliveries in recent years,
the numbers of deliveries and maternal deaths are increasing at the EVRMC as shown in
Table 5- 11. According to the obstetrics and gynecology (OBGYN) doctors, normal
deliveries at the EVRMC have decreased because more BEmONC facilities were
established, but the number of referred cases with complications has gone up.
154
Other data are as follows: Eastern Samar 103.26, Northern Samar 99.29, Biliran 98.72, Samar 60.73,
and Southern Leyte 18.44.
155
In addition, in Leyte province, the deaths of residents were counted between 2010 and 2014 while the
location of occurrence was considered in 2015, which makes it impossible to analyze changes over
time.
156
Leyte province here includes Tacloban city and Ormoc city. The category of “other” includes clinical
labs, dental labs, drug testing labs and x-ray.
Level 1 Level 2 Level 3
Government
1 0 0 0 11 0
Private
0 0 0 0 0 6
Government
10 0 1 7 33 10
Private
3 5 1 4 16 66
Government
1 1 0 9 9 1
Private
6 0 0 0 3 12
Government
2 0 0 6 15 5
Private
1 0 0 2 1 10
Government
4 0 0 2 21 2
Private
2 1 0 1 3 12
Government
2 1 0 4 16 3
Private
4 0 0 3 0 15
Samar
Southern Leyte
Other
Biliran
Leyte
Eastern Samar
Northern Samar
Province
Government
or Private
Hospital
Infirmary
Birthing
Home

90
Table 5- 11 Deliveries and Maternal Deaths at EVRMC
Source: EVRMC
③ Health Governance
Under the leadership of the Regional Director, the DOH Regional Office of Eastern
Visayas is composed of the Local Health Support Division, the Health Standards
Regulation Division and the Management Support Division. Maternal and child health is
handled by the Family Health Unit under the Local Health Support Division.
157
The role of the Regional Office includes (1) implementation of policies developed by
central DOH, (2) technical assistance and monitoring and evaluation of programs and
facilities under LGUs (provincial and municipal/city levels), (3) provision of vaccinations,
contraceptives and medicines, and (4) compilation of FHSIS data. Moreover, each
province submits its three-year Local Investment Plan for Health through the Regional
Office and is given budget support of approximately 1.6 million pesos of Fixed Tranche
and 0.7 million pesos of Variable Tranche
158
each year.
159
Based on the devolution of power in the Philippines, health governance of provincial and
municipal/city levels is under the jurisdiction of the respective LGUs. Nevertheless, by
deploying several Development Management Officers (DMOs) who have coordination,
technical assistance and data collection responsibilities to each province, the Regional
Office has a direct management mechanism at the LGU level.
160
The office also deploys
157
The Local Health Support Division is composed of the Health Systems Development Section which
manages the Health Systems Development Unit, the Hospital Systems and Other Support System Unit
and the Health Facility Development Unit and the Local Health Technical Assistance and Program
Management Section which manages the Family Health Unit, the Communicable Disease Unit, the
Non-Communicable Disease and Health Promotion Unit and the Environmental and Occupational
Unit.
158
Variable Tranche is determined by the performance of the previous fiscal year according to the LGU
Scorecards.
159
Some of the support for the LIPH includes activities by ILHZ, trainings and procurement of
medicines.
160
In Northern Samar, there are 8 DMOs, 283 NDPs and 64 RHMPPs. In Eastern Samar, there are 6
DMOs, 219 NDPs and 55 RHMPPs.
2013 2014 2015
Total No of deliveries 4,498 5,152 5,426
(No of live births) 4,346 4,992 5,254
(No of stillbirths) 152 160 172
No of maternal deaths 18 20 23
No of OB referral cases 1,546 1,650 2,415

91
nurses and midwives to RHUs through the Nurse Deployment Program and the Rural
Health Midwives Placement Program (RHMPP) for human resource strengthening.
The DOH Regional Office of Eastern Visayas has recently set regional strategies under the
Strategic and Operational Plan (2017-2021). The Plan identifies five strategic goals: (1)
development, enhancement and maintenance of health systems and health financing, (2)
quality standardization of health facilities including PhilHealth accreditation, (3)
development and enhancement of health human resources, (4) health information
strengthening, and (5) building the Service Delivery Network.
161
(2) Field Study
Among six provinces in Eastern Visayas region, the Survey conducted field studies in
Eastern Samar and Northern Samar.
[Northern Samar]
More than half of the 24 municipalities and 569 barangays in Northern Samar province are
identified as GIDA areas. The Northern Samar Provincial Hospital in Catarman city,
registered as a Level 1 hospital, is the end referral within the province.
162
There are six
district hospitals, five private hospitals, 24 RHUs and 108 BHS. As indicated in Table 5-
12, MMR and FBD rates have improved. However, it has the second highest MMR (after
Eastern Samar)
163
and the lowest FBD in the region. Table 5- 13 shows facility based
delivery rates in each municipality. Although the issue of data quality still remains, there is
disparity between municipalities where facility-based delivery rate has been high and those
facility-based delivery rate remains low even in 2015.
Table 5- 12 Maternal and Child Health Indicators in Northern Samar
Source: Northern Samar Provincial Health Office
161
The Plan will be finalized by the end of 2016.
162
The Provincial Hospital used to be Level 2 but it was downgraded to Level 1 after the DOH’s revision
of hospital standards. It is currently under construction for expansion and plans an upgrade to Level 2
during 2016.
163
The analysis is made across provinces and excludes Calbayog City, Maasin City, Ormoc City and
Tacloban City.
2011 2012 2013 2014 2015
MMR 135 304 172 181 99
IMR 18.3 9.3 9.73 5.1 3.3
FBD (%) 31.26 41.9 52.6 65 77
ANC (%) 86 67.79 72.42 82.95 62
PNC (%) 77 58 62 71.34 65

92
Table 5- 13 Facility Based Delivery in Municipalities of Northern Samar Province
(2012 ‐ June 2016)
Municipality
2012
2013
2014
2015
June/2016
Allen
68
92
93
99
99
Biri
80
86
45
87
94
Bobon
30
38
63
64
80
Capul
3
38
100
98
95
Catarman
40
N/A
44
82
91
Catubig
53
76
76
86
89
Gamay
42
59
85
91
93
Laoang
37
52
76
91
87
Lapinig
50
70
63
97
98
Lasnavas
36
16
25
42
45
Lavezares
91
96
97
98
100
Lope de Vega
8
9
21
35
42
Mapanas
55
53
58
74
88
Mondragon
22
38
51
71
76
Palapag
65
70
84
93
93
Pambujan
24
32
36
34
46
Rosario
62
69
64
75
76
San Antonio
76
93
87
88
59
San Isidro
44
N/A
90
74
0
San Jose
35
43
95
95
87
San Roque
47
63
77
88
88
San Vicente
81
100
94
100
100
Silvino
2
N/A
57
29
39
Victoria
5
16
32
36
95
Province
42
59
65
77
80
Source: Northern Samar Health Office
[Eastern Samar]
Out of one city, 22 municipalities and 597 barangays in Eastern Samar, four municipalities
and 145 barangays are identified as GIDA areas. The Eastern Samar Provincial Hospital in
Borongan city is registered as a Level 2 hospital, which is the end referral as well as the
only CEmONC facility in the province.
164
There are nine hospitals registered as
infirmaries and 25 RHUs (out of which nine are registered as birthing homes). According
to the maternal and child health indicators in Table 5- 14, while FBD has improved in the
recent years, MMR reversed in 2015 to be the lowest in the Region.
165
164
The Felipe Abrigo Memorial Hospital in Guiuan (southern part of the province) was a CEmONC
facility until recently; however, it became a BEmONC facility after the OBGYN Specialist (who was
also the Hospital Chief) passed away in 2016.
165
The analysis is made across provinces and excludes Calbayog City, Maasin City, Ormoc City and
Tacloban City.

93
Table 5- 14 Maternal and Child Health Indicators in Eastern Samar
Source: Eastern Samar Provincial Health Office
Table 5- 15 shows facility based delivery rate in each municipality of Eastern Samar
province. Facility-based delivery rates are steadily increasing with exception of Jipapad
where nearly half of women deliver a child at home.
Table 5- 15 Facility Based Delivery Rate in each municipality of Eastern Samar Province
(2012 – June 2016)
Municipality
2012
2013
2014
2015
June 2016
Arteche
43
56
84
90
91
Balangiga
78
92
95
95
98
Balangkayaan
57
86
97
95
98
Borongan Ⅰ
90
79
97
95
98
Borongan Ⅱ
64
79
83
82
82
Can-avid
70
76
79
84
90
Dolores
62
72
77
83
89
Gen. MacArthur
84
86
90
91
89
Giporlos
82
83
85
92
97
Guiuan Ⅰ
96
98
98
97
97
Guiuan Ⅱ
37
97
94
96
99
Hernani
93
96
97
95
98
Jipapad
35
33
43
53
52
Lawaan
91
99
99
98
100
Llorente
73
71
75
80
89
Maslog
71
80
71
76
97
Maydolong
89
94
93
97
96
Mercedes
99
100
98
98
100
Oras
62
71
80
90
86
Quinapondan
76
83
75
97
99
Salcedo
84
93
99
98
92
San Julian
91
88
86
89
99
San Policarpo
88
96
99
97
94
Sulat
99
99
100
100
100
Taft
94
93
97
100
100
Province
74
85
88
91
93
Source: Eastern Samar Provincial Health Office
(3) Study Findings
[Study sites]
In the field study in Northern Samar and Eastern Samar provinces, interviews were
conducted with health officers, RHU and BHS staff, Barangay Captains, provincial and
2011 2012 2013 2014 2015
MMR 183 141 93 92 103
IMR 11.3 8.56 11.05 7.8 2.63
FBD (%) 66 74 85 88 91
ANC (%) 65 63 82 82 77
PNC (%) 69 67 75 75 69

94
municipal hospitals, a private hospital and birthing clinic, PhilHealth provincial offices and
a DSWD office as shown below.
166
In addition, individual and group interviews were
conducted with pregnant and lactating women, their family members and TBAs (see Table
5- 16).
Table 5- 16 Study Sites and Community Interviewees
Province
City and Municipality
Barangay
Interviewees
No
Northern
Samar
Catarman City
Barangay Polangi
Pregnant and
lactating women
17
San Roque Municipality
Barangay Balnasan
Eastern
Samar
Borongan City
Barangay Balacdas
Husbands
5
Llorente Municipality
Poblacion and
Barangay Naubay
Women with
grandchildren
6
Can-avid Municipality
Barangay Carolina
TBAs
3
Source: JICA Survey Team
[Supply Side]
1) Service Delivery
According to interviewed healthcare providers, a majority of deliveries are now taking
place in facilities and fewer people are practicing home delivery. Some of the
facilitating factors they pointed out include the improvement of facility services, referral
and the adoption of LGU ordinances prohibiting home deliveries, and providing
incentives to mothers who deliver at facilities and BHWs who facilitate the mothers.
On the other hand, the number of hospitals (excluding Infirmary level) in each province
remains low: two in Northern Samar and one in Eastern Samar.
167
Although there is
only one government-owned CEmONC facility in the province, the provincial hospital
is under-capacity to respond to increasing needs.
168
As the end referral hospital is either
Level 1 in Northern Samar or Level 2 in Eastern Samar that does not have a blood bank,
referred pregnant women died due to the absence of an immediate blood transfusion.
Furthermore, more deaths tend to occur in areas with limited access to the provincial
hospitals. In Eastern Samar, most of the maternal deaths occur in five LGUs (one city
and four municipalities) in the northern part, far from the CEmONC facility.
169
It is
166
In Leyte province, the Survey Team interviewed regional actors including the DOH Regional Office,
the PhilHealth Regional Office and the DSWD Regional Office.
167
Namely, they are the Provincial Hospital and Allen District Hospital in Northern Samar and the
Provincial Hospital in Eastern Samar.
168
Bed occupancy at the Northern Samar Provincial Hospital (including OB Department) is 140-160
percent on average and 103 percent at the Eastern Samar Provincial Hospital (as of 2015).
169
Namely, Canavid, Dolores, Borongan, Oras and Artetche are considered “hot spots” where more
maternal deaths occur according to the Provincial Health Office (it is high in Borongan city due to the
presence of the provincial hospital). On the other hand, in the southern part of the province, due to the

95
illustrated by the fact that many maternal and neonatal deaths occur while they are
transferred from the residential areas to the facility.
170
With regard to RHUs, most of them
function as BEmONC facilities and are
MCP-accredited by PhilHealth. Some of
the RHUs covering GIDA barangays have
maternity waiting homes. Because BHSs
are not established in each and every
barangay and the majority are not
BEmONC-capable, RHU serves as the
most accessible facility for many pregnant
women. Nevertheless, these RHUs are
faced with various human resource issues
such as the lack of doctors
171
and many midwives not equipped with BEmONC skills.
172
Furthermore, while the DOH defines the rate of ANC as more than four visits, some of the
health officers pointed to the tendency to only focus on the quantity (the number of visits)
and not the quality. In particular, without sufficient equipment (especially ultrasound) at
RHUs, appropriate laboratory tests are not conducted for pregnant women for early
detection of risks, resulting in deaths during or after delivery despite more than four ANC
visits, as revealed by Maternal and Newborn Death Review (MNDR).
Public health facilities also include district hospitals and municipal hospitals. However,
except for one hospital in Northern Samar, they are all at the Infirmary level.
173
Hence,
these hospitals provide almost the same maternal and child health services as RHUs.
Therefore, for example, they are not able to assist deliveries of women 18 years old and
presence of the government hospital in Guiuan being CEmONC until recently, there was less of an
access issue.
170
Out of the nine deaths reviewed by Maternal Death Review in 2015, four occurred at hospitals, four
while in transit and one at home.
171
Although one doctor is assigned to work in each RHU, they are often away due to conferences, etc.
172
For example, 64 percent of midwives in Northern Samar have not received BEmONC training and at
least one midwife in each RHU is trained in Eastern Samar. On the other hand, it was clarified that the
midwives who are not trained in BEmONC skills had training in Life Saving Skills, which was
implemented prior to the introduction of BEmONC. The main reason so many midwives are not
trained in BEmONC is a lack of trainers: there are only four trainers at EVRMC and they are unable
to respond to all the training needs, according to LGU health officers (they said they have sufficient
budget to organize the training).
173
The only government hospital registered as Hospital Level in the two provinces is Allen District
Hospital. Other district hospitals, municipal hospitals and community hospitals (6 hospitals in
Northern Samar and 9 hospitals in Eastern Samar) are all registered as Infirmary Level.
Figure 5- 10 RHU staff of Can-avid
municipality in Eastern Samar

96
below and older than 35 years old (for the first pregnancy). According to the healthcare
providers interviewed, some of the Infirmary level hospitals are better equipped with
personnel, medicines and equipment than RHUs, and therefore RHUs can refer their
cases. Nevertheless, some areas are in need of rationalization of the hospitals such as by
upgrading them to Level 1 hospitals given the overlap with nearby RHUs or converting
them to specialized facilities.
Although Supportive Supervision (SSV) is
considered key to improving the quality of
BEmONC services, it lacks systematic
implementation in the provinces.
Provincial officers conduct regular visits
to RHUs in Northern Samar but without
standardized tools, such as checklists. In
Eastern Samar, SSV is only conducted
when there are issues with particular
facilities. Moreover, follow-up
assessments of BEmONC trainings occur
only once after six months by EVRMC trainers’ visits. This suggests a lack of regular
mentoring and coaching, which is an important element to ensure the retention of
healthcare providers’ knowledge and skills as well as their motivation.
At the barangay level, midwives
mobilize BHWs and implement ANC,
PNC and health education regularly.
While most of the BHS do not handle
deliveries, based on the interviews with
pregnant and lactating women, many of
them access BHS for ANC and PNC. In
fact, since TBAs do not conduct ANC
and PNC in most cases, even those who
had home deliveries said they visited
BHS or RHU for check-ups.
Challenges faced by BHSs include midwives being overburdened with various tasks at
the community level and some of the BHSs not being rehabilitated after Typhoon Ruby
hit both provinces in 2014. On the other hand, it was pointed out that the southern part
Figure 5- 12 BHS destroyed
by Typhoon Ruby
Figure 5- 11 Interview with Mayor
of San Roque, Northern Samar

97
of Eastern Samar heavily hit by Typhoon Yolanda in 2013 received a large amount of
assistance from donors to rehabilitate its health facilities, which contributed to more
improvements than pre-Yolanda while unaffected areas were left under-developed.
2) Referral and SDN
In Eastern Samar and Northern Samar, many ILHZ are deemed functional by the local
health authorities,
174
and Common Health Trust Fund (CHTF) are established in some
of the zones. As part of the process to strengthen ILHZ, the awareness of health systems
increased among local chief executives, particularly Mayors,
175
and resources, such as
staff, ambulances and funds were shared in an efficient manner among LGUs. This
contributed to the strengthening of the referral system. ILHZ also implements MNDR.
176
Nevertheless, some issues were raised pertaining to management: a gap in LGU’s
contributions to CHTF depending on the commitment,
177
a change in LGU’s level of
commitment after the turnover of local chief executives, and a slow procurement
process because CHTF is managed by the provincial government.
Together with ILHZ, each province is currently in the process of establishing the
SDN.
178
While ILHZ aims to strengthen a referral system among public facilities
particularly by linking city and municipal governments, SDN is sought under the
leadership of the provincial health office with objectives to not only strengthen a referral
system, including private facilities, but also identifying and creating a manual on the
services available at each facility (including the contents of services, information about
healthcare providers and service schedules) and connecting the available services with
the health needs of poor households. The LGU health officers and healthcare providers
interviewed confirmed that some progress has been made in the mapping of health
facilities and healthcare providers and the profiling of poor households in accordance
with the DOH manual. With regard to the household profiling, CHT/BHWs collect
relevant information of pregnant women, newborns, adolescents, elderly, etc. from each
household using DSWD’s indigent household list. However, many mentioned that they
174
There are six ILHZ in Northern Samar and five in Eastern Samar.
175
In the process of strengthening ILHZ, Zuellig Family Foundation (ZFF) has assisted the Leadership
and Governance Program for policy makers and health workers at LGU level.
176
In Northern Samar, the MNDR manual developed by JICA’s maternal and child health project in
Eastern Visayas was utilized in implementing MNDR. MNDR is implemented at both ILHZ level and
provincial level.
177
There was a case where the most resource-rich LGU was not contributing to the CHTF.
178
With USAID’s assistance, the DOH Regional Office is particularly accelerating the effort to build the
SDN in Leyte province as a pilot site.

98
do not know how to conduct the following step, which is matching, based on the
information collected through the mapping and profiling.
3) NHIP Implementation and Utilization
In Eastern Visayas Region, the total number of NHIP-accredited health facilities was 70
in 2010, increased to 139 by 2011 and 308 by 2015.
179
As Eastern Visayas was heavily
effected by Typhoon Yolanda in 2013, the central government is implementing a special
measure called the “Avail All” policy for the region until the end of 2016. This policy
entitles all residents to NHIP benefits, including those who stopped paying premiums or
who were not enrolled due to their financial constraints. As Table 5- 17 shows, 80 to 90
percent of the population is enrolled in each province, and 92 percent are enrolled in the
entire region. More than 60 percent are Indigent Members in all provinces and more
than 70 percent in the three provinces of Samar island. The NHIP enrollment and
facility-based delivery have increased recently not only because of the special policy,
but because of the PhilHealth Regional Office’s advocacy efforts to LGUs to adopt an
ordinance to provide an incentive of 1,500 pesos to mothers who deliver at facilities and
that of 500 pesos to BHWs and TBAs who facilitate mothers to health facilities out of
the reimbursement from PhilHealth. Moreover, the MCP benefit payments have also
increased in recent years (see Figure 5-13).
Table 5- 17 Numbers of NHIP Members in Eastern Visayas (as of June 2016)
180
Source: PhilHealth Eastern Visayas
179
Interview with the DOH Eastern Visayas Regional Office
180
The numbers include both members and their dependents. The coverage rate is based on the estimated
population.
Province
Formal
Sector
Informal
Sector
Indigent Sponsored Lifetime
Senior
Citizens
Total
Coverage
Rate
Biliran 21,531 6,596 98,806 30 2,744 12,934 142,641 82%
Eastern Samar 69,020 14,735 336,650 62 9,401 22,547 452,415 96%
Leyte 377,878 90,310 1,229,798 199 35,849 144,052 1,878,086 94%
Northern Samar 78,714 9,619 443,879 203 7,365 29,734 569,514 89%
Samar 95,197 21,839 549,567 100 8,866 39,230 714,799 90%
Southern Leyte 70,555 10,941 232,269 37 10,944 37,115 361,861 85%
Region 712,895 154,040 2,890,969 631 75,169 285,612 4,119,316 92%

99
Figure 5- 13 MCP Benefit Payments in Eastern Samar and Northern Samar
181
Source: PhilHealth Province Offices of Eastern Samar and Northern Samar
Upon termination of the special policy at the end of 2016, LGUs are required to resume
their own sponsored programs to take over the assistance. Interviews with healthcare
providers and community members revealed the concern that some of the LGUs do not
have enough funds for the sponsored programs, which could result in increased numbers
of drop-outs and unenrolled. The Survey also confirmed the presence of an RHU that
plans to charge a delivery fee once the Avail All policy expires. Therefore, there is a risk
that many non NHTS-PR poor households will be excluded from the NHIP in Eastern
Visayas Region.
The NHIP benefit payments are deemed essential to
improve the services of health facilities. The
healthcare providers interviewed also mentioned that
the regular bonus they receive from the payments
helps motivate them. Nevertheless, an issue was
pointed out with regard to the benefit payments for
facilities. Because health facilities owned by the
provincial government receive benefit payments
from PhilHealth through the general fund, it is
unclear how the money is spent.
182
According to the
PhilHealth guidelines, LGUs are requested to
establish a trust fund to receive benefit payments
181
The data excludes the hospital level.
182
According to the city and municipal health facilities interviewed, their LGUs have trust funds for
NHIP reimbursement.
0
50
100
150
200
250
300
2010 2011 2012 2013 2014 2015
Million pesos
Eastern Samar Northern Samar
Figure 5- 14 PhilHealth
Northern Samar Office

100
specifically for the improvement of facility services.
183
However, neither province has
established a trust fund and therefore it is not known how much of the NHIP reimbursed
fund is in fact used for the relevant facilities or health purposes. At the Northern Samar
Provincial Hospital, a lack of medicine has become a major issue, leading to
out-of-pocket payments by patients. The establishment of the trust fund can help ensure
the transparency and effective use of benefit payments to respond to such needs.
In many communities, more than half of the community members are enrolled in
NHIP’s Indigent Program based on the NHTS-PR. However, the interviews at barangay
level revealed that many poor households are not included in the list and therefore they
are not NHIP members. In addition, according to the BHWs and midwives who conduct
regular household profiling based on the NHTS-PR list, the list has various issues, such
as non-poor being included as indigents, the double counting of people on the list, and
the listing of the deceased and those who have moved to other communities.
Private health facilities are also accredited by PhilHealth and many are linked with
public facilities through referral systems. The private BEmONC facility interviewed
said 99 percent of its clients are indigent and the NBB Policy is implemented. On the
other hand, the private CEmONC hospital interviewed said while it implements the
NBB Policy, it limits the coverage to 10 percent of total patients from the business
perspective. Hence, in the provinces where government-owned CEmONC facilities are
extremely few, private hospitals seem to be limited in availing services to the poor.
[Demand Side]
1) Health Service Utilization
According to the BHS and RHU staff interviewed, the facility-based delivery rates are
approximately 80 to 90 percent of the total deliveries between 2015 and 2016 in their
communities, showing much improvement in the past few years. Some of the factors
discouraging home deliveries include improved facility services, awareness raised
through community activities and the implementation of LGU ordinances prohibiting
the practice and penalizing TBAs who assisted home deliveries. Some of the TBAs are
now playing the role of a BHW to facilitate facility-based deliveries. The women who
delivered at the facilities mentioned that the choice ensured a safe delivery with the help
of professional staff.
183
In both Northern Samar and Eastern Samar, benefit payments by PhilHealth are made in the form of
check.
101
On the other hand, the Survey Team acknowledged the presence of women who had
home deliveries. Some of the GIDA barangays still have 30 to 40 percent of home
deliveries. The healthcare providers in these communities are concerned about the risk
of more dangerous home deliveries without the help of TBAs due to the strict ordinance
while the women still have limited access to health facilities.
One of the key issues regarding access to health services highlighted by many healthcare
providers is increased teenage pregnancies. Interviews also identified many teenage
couples with children. The teenage girls, being ashamed of their pregnancies, tend to
hide them as much as possible. Because BHWs have a hard time tracking them, there
are many cases of late referral. Moreover, although these couples live together and have
children, many are unmarried. As a consequence, they cannot be enrolled in the NHIP
together as a family. The Survey Team identified some teenage pregnant girls who said
their partners are enrolled in the NHIP as dependents of their parents as the parents are
the NHTS-PR members, and the girls themselves are not enrolled.
2) Enrollment and Utilization of the NHIIP
The field interviews confirmed that many pregnant women were enrolled in the NHIP as
a result of the awareness-raising efforts by BHWs and the Avail All policy and were
benefitting from the maternal and child health services. However, the Survey Team also
identified some women who did not know whether they were NHIP members or if their
memberships were updated. Their impression was that the insurance is beneficial only
when they have to be admitted to a hospital because RHUs provide free services
regardless of the enrollment status. Therefore, for the women who have only been to
RHUs, they do not feel like they have utilized the insurance program. Furthermore,
some of the women who delivered at hospitals expressed that they did not see the
benefits of the NHIP because they still had to pay for drugs out of their own pockets.
Despite the Avail All policy, there were pregnant and lactating women who were yet to
be NHIP members, including unmarried teenage girls who were due to deliver in a few
months. They are required to deliver at a hospital based on the NHIP guidelines. These
women’s vulnerability will increase particularly once the Avail All policy ends at the
end of 2016.
In addition, BHWs who play a pivotal role in awareness-raising activities seem to lack
sufficient knowledge about the NHIP. Many were specifically unaware of the NBB
Policy and POC. Because the Avail All policy which automatically provides the NHIP

102
benefit in Eastern Visayas Region, it is likely not only BHWs but also the LGU
personnel and healthcare providers who have less understanding about the NHIP
regulations.
3) Barriers to Health Services
The pregnant women interviewed by the
Study are between the ages of late teens
into their 30s, many of whom are high
school drop-outs or high school
graduates. Their husbands are farmers,
tricycle drivers or daily workers such as
construction workers. Their income is
unstable: they are paid 100 to 200 pesos a
day or 1,500 to 4,000 pesos per three
months for coconuts farming. Most of the
women identified themselves as
housewives. Some of them help their husbands’ farming, but they do not earn income.
The women who earn income are engaged in small businesses, such as selling
vegetables and rice, getting 300 to 500 pesos a week.
The interviews with women of above-mentioned socio-economic attributes revealed that
they are continuing to face various economic, geographic and socio-cultural barriers
effecting their access to health services.
<Economic Factors>
Medical Fees: In principle, PhilHealth covers most medical fees, and RHUs
essentially provide free services regardless of enrollment status in the NHIP.
Nevertheless, the field study found many cases in which the families of delivering
mothers had to go to pharmacies and pay for drugs while being admitted in health
facilities due to no stock at the facilities. These out-of-pocket payments include IV
fluids, vitamins and syringes. In particular, the payments at a CEmONC hospital
could cost them as much as 2,500 to 6,000 pesos, which is a significant amount for
poor households. Some of them said they had to get donations from relatives and
the LGU. Other out-of-pockets include newborn screening for 600 pesos and
ultrasound for 500-600 pesos that were not available at the RHUs.
Figure 5- 15 Rural household
interviewed by the Study

103
As opposed to the above-mentioned fees involved in maternal and child health
services, fees for TBAs are either free or range between 50 and 1,500 pesos.
According to the TBAs and mothers interviewed, the fee is often not fixed and the
service users can decide the amount based on their financial capabilities. Given the
financial implications, some women still choose to deliver at home. There was a
case of a mother who suffered from high blood pressure, however, decided to
deliver at home as she was afraid of medical bills at hospital, and consequently lost
her newborn (see BOX 5- 5). There was also a mother who was told that she was at
high risk at the time of ANC but did not follow the advice for financial reasons to
take an ultrasound test. These examples indicate that medical fees still burden
many poor women even if they are covered by NHIP.
BOX 5- 5 Experience of a 35-Year-old Woman
I delivered my four children at home. When I was pregnant with my fifth child in 2014, I
was advised to deliver at the hospital due to high blood pressure. But because I had no
problem with my past home deliveries and I was afraid of hospital bills, I delivered at
home and the baby died. When I was pregnant again in 2015, because home delivery was
prohibited, I was planning to deliver at a facility. When I went into labor, I went to the
RHU. However, I was referred to the Provincial Hospital due to high blood pressure. I gave
birth in transit and lost the baby. My husband is a vegetable farmer and I help him. We earn
about 200 pesos every four days and buy rice from the income. We also consume
vegetables we grow at the farm. I am now using contraceptives because we cannot afford
to have any more children.
Transportation: Hospitals and RHUs normally own one or two ambulances, but
some of them require the users to pay for the fuel. In addition, ambulances are not
available for non-urgent cases, and therefore the women and their families have to
find a means of transport such as a motorbike, tricycle or boat and bear the cost.
The actual amount depends on the access: however, even relatively accessible areas
can cost between 20 and a few hundred pesos. The fee fluctuates depending on the
time and it tends to be more expensive during evenings. Among the communities
interviewed, one barangay owns a motorbike and the mothers can use it for free
including the fuel.
Others: Other than the above-mentioned out-of-pocket payments, there are also
costs for transport, food and accommodations for family members who accompany
the women. Furthermore, the majority of women said their husbands accompany
104
them throughout the time at the hospital, which creates a concern for the loss of
family income during the period.
<Geographical Factors>
Related to transport fees, in both provinces surrounded by islands, mountains and
upstream, community members depend on the local means of transport such as
motorbikes, boats and tricycles. Nevertheless, these are not available regularly and
therefore it is difficult to transfer the pregnant women from the remote areas, especially
at night. Additionally, there are communities, even those located 30 minutes away from
the provincial capital on the main road, that do not have a network signal. Prompt
referral of pregnant women from such areas is a challenge. Furthermore, in the
typhoon-prone provinces, women are sometimes forced to deliver at home in the
aftermath of a typhoon. Many experiences in the communities revealed that these
geographical barriers delayed referral of mothers and they were forced to deliver in
transit on a tricycle or boat, causing a maternal or newborn death.
<Sociocultural Factors>
The majority of mothers interviewed said they themselves made the decision where to
deliver. In addition, their husbands accompanied them throughout the period of
admission. The husbands interviewed expressed that they prefer their wives to deliver at
facilities. As for their mothers and mothers-in-laws, they had home deliveries because
there was no accessible facility for their communities and they had no choice but to
deliver at home. However, they said they recommended to their children to deliver at
facilities for their safety.
Among the women from poor households who did not access facilities for ANC, PNC or
delivery, they mentioned gender-related reasons, such as the husband’s rejection for his
wife’s facility-based delivery, the woman’s overwhelmed reproductive and productive
responsibilities at home, and unavailability of a caretaker during the woman’s
hospitalization (see BOX 5- 6, BOX 5- 7). In addition, while contraceptive prevalence
has improved in recent years, all the interviewed women and men using contraceptives
are in fact using female contraceptives, mostly pills and injectable. There was also a
woman who said she cannot use contraceptives because her husband is against family
planning.

105
BOX 5- 6 Experience of a 35-Year-old Woman
My husband is engaged in daily labor as a coconut farmer and earns 1,000 pesos every
three months. I earn 2,000 pesos a month from my laundry business. I gave birth to my five
children at home. I delivered my sixth child at the Provincial Hospital because it was a
breech delivery. For my five-day stay at the hospital, we paid about 6,000 pesos out of our
pocket for IV fluids, syringes and food for my husband. When I was pregnant with my
seventh baby, I was doing heavy labor, doing laundry at the river and noticed my baby was
not moving in my womb. I went to the hospital and found the baby was gone. I am
currently pregnant with my eighth child. A BHW comes to my house and recommends me
to take ANC, but I am busy with preparing meals for my family, helping my children to go
to school, and doing my laundry business, and cannot find time to go to the RHU.
BOX 5- 7 Experience of a 19-Year-old Woman
My 27-year-old husband is currently unemployed and I am a housewife. Together with our
five-month-old baby, we live with his parents. We are not married. He is a member of the
Indigent Program, so our baby is listed as his dependent but I’m not. I delivered the child at
home with the help of my grandmother who is a TBA. I visited BHS once for ANC when I
was still pregnant. I wanted to go back again but my husband didn’t agree with the idea
because he was afraid that we would have to pay. My husband has control over our
household expenses. I want to use contraceptives but my husband is against it because he
wants to have more children.
Some women also prefer not to deliver at health facilities because they consider the
services unsuitable for their traditional customs. According to their customs, a mother is
allowed to drink soup and eat vegetables, dried fish and noodles for at least one month
after delivery and is prohibited to eat meat. However, according to them, hospital meals
include meat, such as chicken. There was even a case where a mother died after delivery
due to hemorrhage and her family still believes it was due to the fact that she had
buffalo meat at the hospital.
There are also negative perceptions of health facilities. Some women described a health
facility as “scary” because they had never been to a facility, “lonely” without the
company of their families, and “no privacy.” Because of these perceptions, even women
in urban communities with good access to health facilities choose to deliver at home.
For them, home delivery is preferable particularly because it allows them to have a
comfortable environment with attendance of their family members. The BHWs in
communities expressed that it was challenging to change the perceptions and behaviors
of these women despite intensified awareness-raising efforts. At the same time, among

106
the health facilities, RHUs are more preferred than hospitals because they tend to be
closer to home, provide free service, and are staffed with midwives and nurses that they
are familiar with. In this respect, there are cases of women who were advised to deliver
at a hospital due to high risks but waited until the last minute so they could deliver at
RHU.
184
184
In such a case, the RHU would assist the delivery but cannot get a benefit payment from PhilHealth
even if the mother is a PhilHealth member.

107
Chapter 6 Good Practices and Challenges of JICA Projects
This Survey reviewed two JICA projects on maternal and child health in the Philippines and
identified good practices and challenges that are considered relevant for its future programming.
6-1 Surveyed Projects
The followings are the summary of the JICA technical cooperation projects reviewed by the
Survey.
The Project for Cordillera-wide Strengthening of the Local Health System for Effective
and Efficient Delivery of Maternal and Child Health Services was developed based on the
outcomes of JICA’s pervious health projects in Benguet and Ifugao provinces in the Cordillera
region. Its objective is to achieve UHC through health system strengthening and building
frameworks for efficient and effective maternal and child health services. The project has been
implemented in Benguet, Abra and Apayao provinces with the Regional DOH Office from
February 2012 to March 2017. Some of the activities include facilitation of BEmONC and MCP
accreditations of target health facilities, strengthening of ILHZs, promotion of enrollment in
NHIP among pregnant women, development of a referral manual, implementation of MNDR
and Supportive Supervision (SSV), enactment of ordinances and resolutions on maternal and
child health and dissemination of the project region- and nation-wide.
The Project for Strengthening Maternal and Child Health Services in Eastern Visayas was
implemented in partnership with the Regional DOH from July 2010 to July 2016, targeting
Leyte province and Ormoc city in Eastern Visayas region. The project objectives were to
increase facility-based delivery with skilled birth attendance and strengthen community-based
activities with involvement of local decision makers so as to improve the quality of BEmONC
and services and reduce maternal deaths. The project activities included equipping target health
facilities to provide BEmONC services and facilitating them to be MCP-accredited, provision of
BEmONC training, implementation of MNDR and SSV, enactment of ordinances and
resolutions on maternal and child health and organization and facilitation of management of
CHT.
6-2 Interview Sites
The Survey team conducted phone interviews with Japanese experts for the above-mentioned
projects and subsequently conducted interviews with the DOH Regional Office, the PhilHealth
Regional Office and Provincial Health Officers of Benguet and Apayao provinces in the
Cordillera region. Healthcare providers and community members were also interviewed in

108
Apayao province. Furthermore, a few project counterparts were interviewed in Eastern Visayas.
The details of the interviewees are indicated in Table 6- 1.
Table 6- 1 List of Interviewees
JICA Project
Interviewees
Project for Cordillera-wide
Strengthening of the Local
Health System for Effective
and Efficient Delivery of
Maternal and Child Health
Services
Benguet province: DOH Regional Office, PhilHealth Regional
Office, Benguet Provincial Health Officers
Apayao province: Apayao Provincial Health Officer, Conner
Municipality Health Officer, Far North Luzon General Hospital,
PhilHealth Provincial Office, RHU of Pudtol Municipality, BHS of
Barangay Cabatacan and Barangay Buluan, pregnant and lactating
women (14 people)
Project for Strengthening
Maternal and Child Health
Services in Eastern Visayas
DOH Regional Office, PhilHealth Regional Office, Leyte Provincial
Health Officers
6-3 Survey Findings
(1) Good Practices
According to the achievements of goals and
project purposes as shown in Table 6- 2 and
Table 6- 3, both projects contributed to
increasing facility-based deliveries, ANC
and PNC. This successful outcome seems to
be attributable to five facilitating factors.
First, in order to increase BEmONC
facilities, the projects invested in both
facility and human resources of target
health facilities. In particular, in the
Cordillera region where there are many
remote areas, a strategy was employed to upgrade many BHS to become
BEmONC-capable for the improvement of access to essential health services.
Additionally, by facilitating the NHIP accreditation of BEmONC facilities and promoting
the enrollment in NHIP among pregnant women, benefit payments by PhilHealth
increased, which in turn contributed to the improvement of maternal and child health
services.
185
Second, the projects mobilized CHT and BHWs effectively to conduct
grassroots-level awareness raising and tracking of pregnant women, which shifted
women’s awareness and behavior from home to facility. Third, the revitalization of ILHZ
185
As of August 2016, there were 87 BHS that are MCP-accredited in Cordillera, which is the highest in
the country.
Figure 6- 1 BHS supported by JICA

109
strengthened referral systems through increasing the commitments of local executive
chiefs and sharing necessary resources among LGUs. Fourth, as a result of advocacy to
LGUs, policies were adopted to promote service access including ordinances on
prohibition of home delivery and payment of incentives to mothers and BHWs and
Barangay Maternal, Newborn, Child Health and Nutrition (MNCHN) emergency plans for
provision of transport.
186
Fifth, the project in Cordillera addressed cultural factors
hindering access to services such as the introduction of culturally-sensitive service
protocols and working with TBAs as 70 percent of the regional population are indigenous
peoples.
187
At one BHS where the survey team visited, 64 percent of deliveries were done
at home in 2011 but it was gradually reduced and achieved zero home delivery by 2015.
Furthermore, a group interview with women who had deliveries in the past year revealed
all of them had the last delivery at facilities while previous deliveries were done at home.
Table 6- 2 Outcome of the JICA Project in Cordillera
Source: JICA
Because FHSIS data were found to have issues with counting deaths based on the location
of the occurrence (i.e. in which facility the death occurred) and applying an estimated
number of pregnant women as a denominator, the projects promoted the employment of
residence-based calculations (i.e. where the deceased resided) and an actual number of
pregnant women as a denominator. This enabled the stakeholders to understand the
situations accurately. In particular, in Cordillera, a system was established to tap into
186
By incorporating an MNCHN Emergency Plan into each Barangay Disaster Risk Reduction and
Management Plan, a system was established to provide emergency transport to pregnant women and
their newborn children.
187
For example, the protocols reflected traditional customs to have husbands attend delivery and mothers
deliver in a squatting position.
# Indicator Baseline Target Year 2015 Source
1 Regional MMR (per 100,000 live births) 62 Reduced 45
2 Regional IMR (per 1,000 live births) 11 Reduced 11
3 Regional FBD (%) 74 85 92
1 FBD in project sites (%) 79 85 93
2 ANC in project sites (%) 63 80 84
3 PNC in project sites (%) 90 90 98
4 N0 of functional ILHZ in the region 7 Increased 17
5 No of LGUs implementing MNDR in the region 0 Increased 7
Hospital 0 37 36
RHU 0 50 48
BHS 0 90 104
RHU 53 51
BHS 78 93
Goal
FHSIS
Project
Purpose
FHSIS,
residence-based,
TCL analysys,
project
monitoring
6
No of BEmONC dacilities in the region
7
No of MCP accredited facilities in the region
12

110
BHWs’ Client Target Lists (CTLs) to collect residence-based data through the project.
Cognizant of the advantage of the system, the DOH Regional Office has adopted this
methodology (in addition to FHSIS) for the entire region and has requested the central
DOH to review the FHSIS methodology.
Table 6- 3 Outcome of the JICA Project in Eastern Visayas
188
Source: JICA
In addition, many counterparts noted that stakeholders were involved in the project
activities. From the beginning of project design and planning, efforts were made to
coordinate and discuss with all project stakeholders (e.g. provincial and municipal health
officers, PhilHealth and local chief executives). Throughout the implementation period,
regular meetings were organized to set project targets, address challenges, establish
partnerships and document project outputs. These approaches are considered sustainable
and good practice unique to JICA.
188
The ANC and PNC rates under the project purpose are calculated based on the FHSIS data using an
estimated number of pregnant women (2.7 percent for the entire country) as a denominator, and
therefore they are underestimated. According to the JICA project, the ANC rates become 63 percent in
Leyte and 84 percent in Ormoc in 2015 and the PNC rates became 96 percent in Leyte and 99 percent
in Ormoc in 2015 by using the actual number of deliveries as a denominator.
# Indicator Baseline Target Year 2015 Source
Leyte province 74.5 Reduced 41.5
Ormoc city 64.2 Reduced 185.2
Leyte province No data Reduced 2.3
Ormoc city 6.2 Reduced 14.5
Leyte province 6 Reduced 5.9
Ormoc city 10.3 Reduced 18
Leyte province 23 Reduced 12
Ormoc city 3 Reduced 13
Leyte province No data Reduced 67
Ormoc city 29 Reduced 102
Leyte province 56 90 93
Ormoc city 65 90 97
Leyte province 56 80 93
Ormoc city 65 80 97
Leyte province 22 45 46
Ormoc city 29 45 63
Leyte province 53 80 71
Ormoc city 61 80 75
FHSIS
2
ANC in project sites (%)
3
PNC in project sites (%)
Project
Purpose
1
FBD in project sites
Goal
1
MMR (per 100,000 live births)
FHSIS
2
NMR (per 1,000 live births)
3
IMR (per 1,000 live births)
4
No of maternal deaths
5
No of neonatal deaths
6
FBD (%)

111
The project in the Cordillera region
increased impact by supporting the
regional DOH’s project expansion plan.
Good practices of the project such as
ILHZ, TCL, CHT and MNDR were scaled
up to non-project sites in the region with
strong ownership by the Regional Office.
In Eastern Visayas, the regional DOH is
planning to expand SSV to other provinces
in the region based on the experience with
the JICA project.
(2) Challenges
The Survey identified MCP-accredited BHS
that had not received benefit payments from
PhilHealth. Other related issues included
midwives’ lack of understanding of
distribution ratios of the payments received
by the LGUs for facility and personnel and
the lack of LGU’s resolution to enable such
payments to BHS. In the case of
LGU-owned health facilities, benefit
payments from PhilHealth are not made
directly to the respective facilities but to the
LGUs, and PhilHealth does not track if they are actually utilized for the relevant facilities.
In this respect, health facilities and LGUs should make further efforts to increase
healthcare providers’ understanding of the PhilHealth guidelines and improve the
distribution processes and management of the payments.
While more pregnant women are now enrolled in the NHIP, many of them still do not
understand the program.
189
In fact, group interviews with pregnant and lactating women
revealed that some were not yet enrolled and expressed financial concerns for facility
delivery. In this sense, there are existing issues of poor families left out from the
NHTS-PR, less frequent update of the NHTS-PR list, and LGU’s limited resources for the
Sponsored program. Furthermore, some of the LGU-owned hospitals do not have sufficient
189
Interviews with BHWs also revealed that some of them did not know the NBB Policy and POC.
Figure 6- 3 MCP-accredited BHS
Figure 6- 2 BHS staff interviewed
by the survey team

112
funds to implement the NBB Policy and POC. In this sense, more efforts are required for
the financial protection of the poor.
Despite the strengthening of the referral system through ILHS, there remain various
challenges for the poor to access health services due to financial, geographical, cultural and
social factors, and home delivery is still practiced. Especially in remote and mountainous
areas like Cordillera, pregnant women have to walk for more than half a day to reach
health facilities and pay out of pocket as much as a few thousand pesos for one-way
transport,
190
food and newborn screening. In addition, according to the group interviews
with pregnant and lactating women, one of the main reasons to deliver at the facility is that
home delivery with the help of TBA is prohibited by municipal ordinance. This may
suggest that poor women living in remote areas without appropriate transport to health
facilities have a lack of options, and in fact are forced to look for more risky alternatives.
In this regard, assistance should be accompanied with other approaches to facilitate access,
such as the provision of incentives to mothers and the establishment of maternity waiting
homes.
With the improvement of the referral system, more maternal deaths are occurring while
being transferred or at high-level facilities. Under these circumstances, comprehensive
efforts should be made to tackle the factors attributing to the “three delays”: unavailability
of transport, lack of immediate and appropriate treatments with drugs and blood shortages
at health facilities, and cultural and financial factors hindering women from seeking
services.
191
Future assistance should focus on these issues to devise solutions.
While DOH Regional Offices report project outcomes and provide feedback on policies to
the central DOH, it was indicated that these efforts had not resulted in improvement of the
policies. Some policies require fundamental improvements, such as that of the FHSIS data
and the standards of midwife placement.
192
In this respect, the future project should not
only share results with the central DOH, but also fully involve them from the stage of
project design and planning.
190
According to the BHS interviewed, when an ambulance is dispatched for referral, the patient has to
pay 1,500 pesos for fuel.
191
For example, among some of the indigenous people in Cordillera, the traditional customs require them
to conduct a ritual before going to the facility and use herbal medicines.
192
According to the DOH standards, one midwife is deployed for a population of 5,000. Some
interviewees commented that it should not only consider the size of population but also the distance as
an issue in remote communities.

113
Chapter 7 Recommendations for JICA’s Future Assistance
On the basis of the survey findings and good practices and challenges of the former JICA
projects in maternal and child health (MCH), the following recommendations are made for
JICA to take into consideration when formulating future assistance projects/programs for the
Philippines.
7-1 Points to be Considered
The following four points were especially considered when consolidating the recommendations
for JICA.
JICA’s knowledge and experience in the Philippines, particularly MCH projects.
Universal Health Coverage (UHC), “equitable health service delivery and financial risk
protection,” the Japanese government’s diplomatic strategy, is incorporated.
Philippine Health Agenda: ①All Life Stages & Triple Burden of Diseases, ②Service
Delivery Network and ③Universal Health Insurance are addressed.
Achievement of the Sustainable Development Goals (SDGs), particularly in reduction of
maternal and neonatal deaths, promotion of access to sexual and reproductive health-care
services and achievement of UHC,
193
is considered.
7-2 Recommendations for JICA’s future activities
The survey found that inequality among Filipinos has not diminished, even though the country’s
economy has been thriving over the past decade. Consequently, poor families are still suffering
financially when they receive medical services, even if they are enrolled in NHIP. The quality
of health services highly depends on capacity and leadership of the local executives. The survey
team recommends JICA to pursue the new technical assistance project, “UHC enhancement in
the MCH services,” with two approaches: improved access to quality essential health-care
services and financial risk protection. Each component of the recommended project is described
below.
(1) Access to Quality Essential Health-Care Services
① Service Delivery Network (SDN)-Building
Effective SDN is indispensable for all women to have a safe delivery. However, the policy
and guidelines of SDN are not clear in the Philippines at this moment and there is a variety
193
United Nations. (2016). Sustainable Development Goals: 17 Goals to Transform Our World.

114
in the state of progress in SDN establishment in different areas of the country. It is
recommended that JICA provide technical assistance to target provincial government
officials in re-defining the “SDN” and building the SDN in the way that necessary health
services are delivered to people in need when needed.
The Japanese secondary medical area
194
could be a model when re-defining the “SDN” in
the Philippines. The Japanese secondary medical area is the zone that is set for each
prefecture, in which hospital beds serving general inpatient care are prepared pursuant to
the provision of the Medical Care Act and connected to referral care. Ideally, the DOH
Regional Office should set the SDN zones as there is a chance that a SDN zone extend
over more than two provinces. SDN zones should be carefully set while taking
geographical relationships and traffic condition into consideration.
Additionally, actions are needed to mitigate the overconcentration of patients in tertiary
health facilities. While continuing efforts to upgrade RHUs into BEmONCs as performed
in previous JICA projects for hard-to-reach areas, the new project should consider setting a
secondary or primary health facility near a tertiary health facility. Upgrading a primary
health facility to a secondary health facility was intended to bring better health care close
to the people. However, now that many women are reaching a tertiary health facility, a
place for women having a normal delivery should be established near the tertiary health
facility, so that these women can stay close and the tertiary health facilities are available
for complicated cases. Moreover, maternal waiting homes nearby a tertiary health facility
would improve accessibility for women living in hard-to-reach areas, such as GIDAs. The
women can stay at the maternal waiting homes several days prior to delivery, so that they
can receive prompt emergency care if necessary.
② Continued Supportive Supervision for Health Care Providers
The survey found that most maternal deaths are occurring within or in transit to health
facilities in the Philippines. Inadequate referral systems, poor facilities and a lack of
medical supplies are some of reasons behind this, but inadequately trained and poorly
motivated health staff are another major factor in maternal death. Health staff need to make
194
The Japanese secondary medical area is set by the Ministry of Health, Labor and Welfare based on the
Medical Law, considering various factors, such as the geographical and traffic conditions. The medical
service system within the area is designed based on the necessary number of medical treatment beds. It
aims at providing general medical services, including surgery and emergency care within the area. The
Japanese secondary medical area consists of plural municipalities and a prefecture is divided into 3 to 20
secondary medical areas. In general, municipalities provide primary care and prefectures provide tertiary
care.
115
a correct decision in emergencies at a primary or a secondary health facility to refer a
patient to a higher-level facility, and in a higher-level facility, the staff should properly
provide emergency care. The survey found that untrained midwives, without BEmONC
training, are working in health facilities. Thus, training and supportive supervision in
ANC, referral services, delivery and PNC should be continually provided to health staff at
all levels of health facilities based on previous JICA experience, and the training and
supervisory process and tools utilized in the efforts should be properly compiled. These
efforts to strengthen the emergency obstetric care system should lead to prevention of
maternal mortality. In case the target area is facing a scarcity of the trainers, the new
project team should consider exchanging memorandums with a university or an academic
institution to have them send trainers to the project sites.
③ Technical Assistance for LGUs in Administration and Public Finance
Previous JICA projects assisted LGUs to issue ordinances banning TBA practices and
home delivery, and providing mothers and BHWs with incentives when they come to a
health facility for delivery. While it is recommended to continue these efforts, new projects
should also provide technical assistance in public financial management to LGUs.
The following are examples of the activities:
1. Support establish ordinances at barangays and municipalities to incentivize BHWs
and mothers for FBD and to give penalties for home delivery.
2. Support establish a system to regularly monitor the PhilHealth reimbursement to the
LGU or hospital trust fund and the utilization for the original purposes, such as
purchase of medicine.
3. Support conduct leadership trainings for local executives of LGUs, particularly in
local governance and public financial management. Through the trainings, the project
team should convince the local executives that they should provide enough budget to
the health sector as quality health care leads to healthy population and prosperity of
LGUs.
As these activities are similar to other development partners’, it is recommended for the
project team to plan on the activities through discussions with such stakeholders.
116
(2) Financial Risk Protection
① Financial Support System Development at the LGUs
The survey found that some LGUs are reluctant to sponsor near-poor people to be enrolled
in NHIP and many women are still financially burdened by health services even if they are
enrolled in NHIP. It is recommended that the new project assist LGUs to pilot a financial
support system to mitigate and eliminate this burden on child-bearing women.
The following are examples of the activities:
1. Support establish a common pooled fund, collected out of the PhilHealth
reimbursement and religious, community and charity events, and provide
childbearing women with lump sum fund.
2. Support establish a system to provide some monetary assistance to the poor families
identified by LGUs when they receive medical services. The LGU poor families
should be identified by barangay captains and LGU officers. The monetary
assistance is provided out of the above common pooled fund and it is used for
transportation to a health facility, medicine and laboratory tests, the health expenses
not covered by NHIP.
3. Support establish a labor exchange system without monetary exchange within a
barangay or a municipality. The system allows a childbearing woman to receive
child care and/or housekeeping while she is hospitalized and she can return the
similar support to the child care taker and a housekeeper later.
② Promotion of Awareness-Raising Activities
The survey found very few people thoroughly understood NHIP. In fact, it is not only the
beneficiaries who have insufficient knowledge, but health administrators, BHWs and
health service providers also lack knowledge of NHIP. Hence, it is recommended that the
new project select the most effective media and the most important messages for each
group of people and try to convey only the selected messages in clear and simple words.
For BHWs, who are in charge of raising the awareness of the beneficiaries, the
awareness-raising training should be standardized by the project team.

117
③ Effective utilization of the BHWs’ Household Profiling
Barangay Health Workers (BHWs) are
collecting and updating household data
monthly in an assigned area. The data are
consolidated in various forms, including
Household Profiling (see Figure 7- 1) and
the Target Client List (TCL). Previous JICA
projects mobilized the activities of the
BHWs and strengthened tracking of the
ANC, PNC and facility delivery status of
women primarily with the Target Client List
(TCL) for prenatal care. Based on the experiences, the new project team should first study
the availability and quality of the data-collecting system in the target areas, and use the
most reliable data for the extended purposes. The survey revealed that there are many
women who do not know whether they are enrolled in NHIP or if they have paid premiums
to renew their membership. It would be helpful if the BHWs can use the database not only
for checking people’s health, but the status of their NHIP enrollment and premium
payment, when they visit each household. BHWs can support the households with
procedures for NHIP enrollment or premium payment. That way, people can maintain an
active enrollment in NHIP and their health expenditures are covered by NHIP when
necessary. It would be more effective if BHWs raise the people’s awareness regarding
NHIP through the household visits.
④ Third-Country Training and Training in Japan
PhilHealth has been evolving for the past twenty years; however, it is still facing new
challenges. In fact, improvement of the NHIP system itself is necessary to eliminate
financial burdens on poor women in provinces. Through the survey, it was found that
PhilHealth is eager to learn how other countries are dealing with various challenges.
Hence, it is recommended for the new project to invite PhilHealth staff to Japan or other
countries such as Thailand where JICA is implementing the Partnership Project for Global
Health and Universal Health Coverage to promote Universal Health Coverage (UHC) in
ASEAN countries as well as other regions of the world. It would help PhilHealth to
improve NHIP policies through trainings and discussions with other participating countries
and observe universal health coverage in Japan. As the Philippine government suggests to
pay non-formal sector premiums by tax subsidies in the new Philippine Health Agenda, the
Universal Coverage Scheme in Thailand could be a model. On the other hand, Japanese
Figure 7- 1 Household Profiling
118
medical fee schedule and some management systems could assist solve the current issues
that PhilHealth is facing.
7-3 Project Sites
Eastern Samar and Northern Samar provinces in Eastern Visayas are recommended as the
next project sites. These two provinces are among the 20 High Poverty Sites. A good
relationship with the DOH Eastern Visayas Regional Office has been already established
through long-time assistance in the region. It is expected that the Leyte provincial office
where JICA assisted for the past six years could transfer the knowledge and skills gained
through the project into Eastern Samar and Northern Samar provinces.
In case Eastern Samar and Northern Samar provinces are chosen as the new project sites,
however, the project team should thoroughly uphold safety management as the Communist
Party guerrilla organization, New People’s Army, is hiding in the provinces. Also, after
Super Typhoon Yolanda hit the Eastern Visayas Region, a special measure, the Avail All,
was taken in the Region to support the enrollment of people in NHIP. As the Avail All is
going to end in 2016, new sponsors should be found for those who are currently enrolled
through the Avail All, for the next year on. It is also necessary for those people to be
re-educated about NHIP as they did not have to pay premiums for the past few years.
7-4 Enhancement of Project Up-scaling Mechanism
Although JICA has been assisting the Philippine health sector for a long time, its good
practices were not necessarily utilized to improve national policies. The primary reason
should be that the health policy makers do not fully understand importance of JICA’s
achievement. For the next project, JICA should build up a mechanism to fully up-scale the
good results of the project to the entire country (see Figure 7- 2).
The JICA health advisor or a project member assigned at the DOH headquarters should
play an important role in the mechanism. The health advisor or the project member should
involve the Family Health Office, the division in charge of MCH, the Bureau of Local
Health Systems Development, the division in charge of SDN, the DOH Regional Office in
the target region, and the PhilHealth headquarters, throughout the project planning process.
It is important that all the stakeholders recognize that JICA will pilot the project for the
entire nation from the planning phase and periodically and continually share the project
updates.
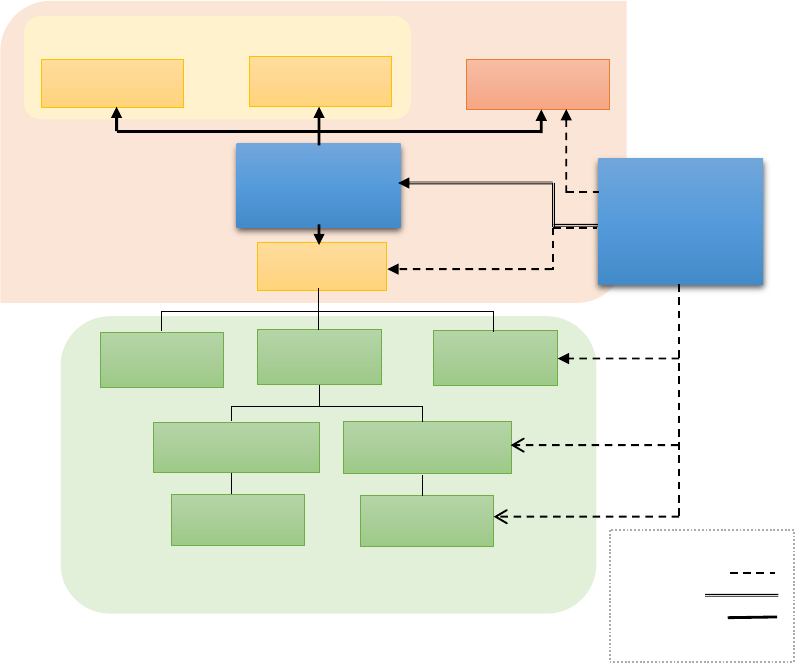
119
The counterparts of the project are primarily the DOH Regional Office and the target
LGUs. The project team works with the counterparts and periodically reports to the JICA
Health Advisor/the project member in charge, so that the Health Advisor/the project
member in charge can update the stakeholders.
Now that the Bureau of Local Health Systems Development has started reviewing the SDN
policy, it is a good time for JICA to start being involved in the area of SDN policy. When
good communication is maintained among the stakeholders in the central offices, JICA’s
good practice should be taken into account when the SDN new policy is formulated.
Likewise, other lessons learned through the new project should be utilized to improve the
policies of MCH as well as NHIP as long as the project outcomes are shared with the
stakeholders. It would take approximately five years to show exactly how LGUs can take
action towards enhancing UHC through MCH services in the project sites, and
simultaneously build the project up-scaling mechanism. Afterwards, it is expected that the
Philippine government would continue the efforts towards UHC in the entire nation based
on their own policies.
Figure 7- 2 Recommended JICA New Project and Project Upscaling Mechanism
③⑥
⑦
①②④
SDN Zone
DOH HQ
Province
JICA
Experts
JICAHealth
Advisor/ Project
expert
DOH RO
FHO
PhilHealth
LHSD
Province
Province
Barangay
City
Municipality
Barangay
③⑥
⑤
Project Upscaling
Mechanism
Legend
Assistance
Report
Plannning/
Consultation

120
REFERENCES
Asia Development Bank. (2015). Key Indicators for Asia and the Pacific 2015. Retrieved
September 12, 2016, from
http://www.adb.org/sites/default/files/publication/175162/phi.pdf
Bureau of International Health Cooperation of DOH (2016). The Official Development
Assistance on Health.
Bureau of Local Health Systems Development (BLHSD) DOH & UNICEF. (2015). Local Investment
Planning for Health Handbook on Principles, Guidelines, Procedures, and Processes.
Department of Budget and Management Official Website. http://www.dbm.gov.ph/
Department of Health. (2012). Administrative Order No. 2012-0012, Rules and Regulations Governing
the New Classification of Hospitals and Other Health Facilities in the Philippines Department of
Health. (2015). Sin Tax Law Incremental Revenue for Health, Annual Report CY 2015.
Department of Health. (2008). Administrative Order No. 2008-0008, Rules and Regulations
Governing the Regulation of Blood Service Facilities
Department of Health. (2001). Administrative Order No. 51-A s. 2001, Implementing Guidelines on
Classification of Patients and on Availment of Medical Social Services in Government Hospitals.
DOH Office of the Secretary & DOH Health Policy Development and Planning Bureau. (2016).
Philippine Health Agenda 2016-2022 Healthy Philippines 2022.
Japan International Cooperation Agency and Department of Health, Center for Health
Development – Eastern Visayas. (2016). Draft Terminal Evaluation Report on Japanese
Technical Cooperation Project for Strengthening Maternal and Child Health Services in
Eastern Visayas.
Japan International Cooperation Agency, IC Net Limited and HANDS. (2016). Strengthening
Maternal and Child Health Services in Eastern Visayas, Philippines: Project Completion
Report
Japan International Cooperation Agency. (2015). National Dissemination Forum: Reducing
Maternal and Child Health Mortality in the Cordillera.
Japan International Cooperation Agency & Department of Health. (2014). Report of Mid-term Review
on Project for Cordillera-wide Strengthening of the Local Health System for Effective and
Efficient Delivery of Maternal and Child Health Services in the Republic of the Philippines.

121
Japan International Cooperation Agency and System Science Consultants Inc. (2012-2016).
Project for Cordillera-wide Strengthening of the Local Health System for Effective and
Efficient Delivery of Maternal and Child Health Services: Progress Reports 1-8.
Japan International Cooperation Agency & Department of Health, Center for Health Development –
Eastern Visayas. (2012). Joint Mid-term Review Report on Japanese Technical Cooperation
Project for Strengthening Maternal and Child Health Services in Eastern Visayas.
Jurado F. J. (2014). An Assessment of Republic Act (RA) No. 10351 or the SinTax Reform
Law. NTRC Tax Research Journal. Vol. XXVI. 5, September to October 2014: 18-42.
Kwon S. & Dodd R. (Eds.). (2011). The Philippines Health System Review, WHO Health
Systems in Transition, Vol. 1, No.2. Geneva: WHO Press.
Ministry of Health, Labor and Welfare. (2016). Abridged Life Table. Retrieved September 14,
2016, from http://kaiwa-kouza.com/contents/sub/statistics/longevity.html.
The National Household Targeting Office, Department of Social Welfare and Development.
(2015). Listahanan.
National Institute of Population and Social Security Research. (2016). Population Statistics.
Retrieved September 12, 2016, from
http://www.ipss.go.jp/syoushika/tohkei/Popular/P_Detail2016.asp?fname=T04-03.htm.
National Institute of Population and Social Security Research. (2012). Population Statistics.
Retrieved September 14, 2016, from
http://www.ipss.go.jp/syoushika/tohkei/Popular/P_Detail2012.asp?fname=T02-18.htm
Official gazette of the government of the Philippines. Pantawid Pamilyang Pilipino Program.
(2016). Retrieved October 12, 2016, from
http://www.gov.ph/programs/conditional-cash-transfer/
Philippine Health Insurance Corporation. (2016). Stats & Charts 1
st
September 2016.
Philippine Health Insurance Corporation. (2015). Annual Audit Report on the Philippine Health
Insurance Corporation for the Year Ended December 31,2015.
Philippine Health Insurance Corporation. (2015). ANNUAL REPORT 2014.
Philippine Health Insurance Corporation. (2015). Stats & Charts 2015.
Philippine Health Insurance Corporation. (2014). ANNUAL REPORT 2013.
Philippine Health Insurance Corporation. (2014). Stats & Charts 2014.
Philippine Health Insurance Corporation. (2013). ANNUAL REPORT 2012.

122
Philippine Health Insurance Corporation. (2013). Stats & Charts 2013.
Philippine Health Insurance Corporation. (2012). ANNUAL REPORT 2011.
Philippine Health Insurance Corporation. (2012). Stats & Charts 2012.
Philippine Health Insurance Corporation. (2011). ANNUAL REPORT 2010.
Philippine Health Insurance Corporation. (2011). Stats & Charts 2011.
Philippine Health Insurance Corporation. (2010). ANNUAL REPORT 2009.
Philippine Health Insurance Corporation. (2010). Stats & Charts 2010.
PhilHealth. (2015). Circular No. 26, 2015.
PhilHealth. (2015). Get to Know Your PhilHealth Benefit in Just One Click.
PhilHealth. (2014). Annual Report 2011-2014.
PhilHealth. (2014). Circular No. 0003, s. 2014.
PhilHealth. (2013). Circular No. 0032. s.2013, 14 October 2013.
PhilHealth. (2011). Circular No. 011-2011.
Philippine Statistics Authority. (2011). The 2010 Census of Population and Housing.
Philippine Statistics Authority & ICF International. (2014). Philippines National Demographic
and Health Survey 2013. Manila, Philippines, and Rockville, Maryland, USA: PSA and
ICF International.
Philippine Statistics Authority. (2016). The Philippine 2015 Population Census. Retrieved
September 21, 2016, from
https://psa.gov.ph/content/highlights-philippine-population-2015-census-population.
Philippine Statistics Authority. (2016). Philippine Poverty Statistics. Retrieved November 3,
2016, from https://psa.gov.ph/poverty-press-releases.
Racelis R. H. et. al. (2016). Philippine Health Accounts Based on the 20111 System of Health
Accounts for CY 2012, 2013 and 2014.
Saniel, O. P. & Bermudez, A. N. C. (2016, August). Why do mothers die? A Maternal Death
Review in Camarines Norte. Unpublished Research Paper
Scribd. (2016). The field health service information system (FHSIS). Retrieved October 30, 2016, from
https://ja.scribd.com/doc/27872414/The-field-health-service-information-system-FHSIS.
Soria F. Z. (2016). PhilHealth benefits.

123
Soria. F. Z. PhilHealth Benefit Packages: Understanding the Role of Quality Medicines and
Quality Pharmaceutical Care.
Statistics Bureau, Ministry of Internal Affairs and Communications. (2016). Statistics of Japan
2016. Retrieved September 14, 2016, from http://www.stat.go.jp/data/nihon/02.htm
Title III Section 5 of the Implementing Rules and Regulations (IRR) of RA 7875 as amended
otherwise known as the National Health Insurance Act of 2013
United Nations, Department of Economic and Social Affairs, Population Division (2015).
World Population Prospects: the 2015 Revision. Volume II: Demographic Profiles
(ST/ESA/SER.A/380). Retrieved September 23, 2016, from https://esa.un.org/unpd/wpp/.
United Nations, Department of Public Information. (2016). Sustainable Development Goals: 17
Goals to Transform Our World. Retrieved November 1, 2016, from
http://www.un.org/sustainabledevelopment/sustainable-development-goals/
Vega. L. J. Shifting to Case Rates: Efficiency Gains. Southern Philippines Medical Center.
WHO, UNICEF, UNFPA, World Bank Group and United Nations Population Division Maternal
Mortality Estimation Inter-Agency Group (2015), Maternal Mortality in 1995-2015 –
Philippines
World Bank (2016). Philippines Impact of Incentives and Information on Quality and Utilization in
Primary Care: Baseline Survey Report.
World Bank. (2016). World Development Indicators. Retrieved September 14, 2016, from
http://data.worldbank.org/data-catalog/world-development-indicators
World Bank. (2016). World Development Indicators. Retrieved October 29, 2016, from
http://databank.worldbank.org/data/reports.aspx?source=2&series=SH.XPD.TOTL.ZS&co
untry=#
World Bank. (2015). Concept Note on the Establishment of a Service Delivery Network for
Tacloban City, UPecon-Health Policy Development Program.
World Bank. (2015). Global Partnership on Output-based Aid, Grant Reporting and
Monitoring Report: Ref. TF0101757.
World Bank. (2011). Philippines: Study on Local Service Delivery.
World Bank. (2016). World Bank Open Data. Retrieved September 14, 2016, from
http://data.worldbank.org/
ATTACHMENTS

Time
Venue
Agency
Contact
2016/7/24 Sun 17:30
0830-0900
JICA PP Office JICA PP office
SR Mr. Morita, Ms. Itsuki
0900-0945
JICA PP office JICA PP office
Ms. Marry Ann, Ms Mendoza Teresa
1000-1200
UNFPA, 31/F Yuchengco Tower,
RCBC Plaza, 6819, Ayala Ave
UNFPA Dr Angelito Umali
1400-1600
UNICEF UNICEF
Dr Raoul Bermejo, Health & Nutrition
United Nations Children's Fund
2016/7/26
Tue 0900-1100
JICA PP Office
@Meeting Room 2
EU Consultant Team
DR. UTE SCHUMANN
Team Leader/Health Policy Planning & Financing Expert
EU PHILIPPINES HEALTH SECTOR REFORM CONTRACT
Mrs Melahi Pons.
Interim Financing Expert
0900-1100
ADB ADB
Dr. Eduardo Banzon
Regional Adviser for Health, Economics and Financing
Asssitant: Raygie dela Cruz (Ms)
1400-1500
Richmonde Hotel Ortigas NKTI
Dr Enrique Ona
Former Secretary of Health (2010-2014)
Medical Doctor, National Kidney and Transplant Institute (NKTI)
0730-0900
DSWD
Central Office, Batasan Complex,
Quezon City, Philippines
DSWD
Mr. Leonardo C. Reynoso, CESO III, National Program Manager (Conditional
Cash Transfer Program)
Mr. Gil R. Tuparan, Senior Technical Officer
Ms. Johhanna Acebes. Technical Assistance Unit
1000-1130
Jose Fabella Hospital
Lope de Vega St., Sta Cruz
Manila, Philippines
Jose Fabella Hospital
Dr. Esmeraldo T. Ilem
Medical Center Chief II
Dr. Jose Fabella Memorial Hospital
1300-1400
WHO country office WHO
Dr. Benjamin D Lane, PhD
Coordinator Health Systems, WHO Philippines
0900-1100
World Bank
26th Floor, One Global Place 5th Ave.
corner 25th St. Bonifacio Global City
World Bank
Ms. Tomo Morimoto, Senior Operations Officer
Health, Nutrition & Population Global Practice
Dr. Roberto Antonio F. Rosadia, Health Specialist
1300-1400
DOH
San Lazaro Compound, Tayuman, Sta.
Cruz, Manila
DOH
Ms. Georgina Ramiro,
Dr. Grace Fe R. Buquiran, Medical Officer N BIHC
Project Monitoring Division, Bureau of International Health Cooperation
1400-1600
DOH
San Lazaro Compound, Tayuman, Sta.
Cruz, Manila
DOH
Ms. Zeny Dy Recidoro
Chief Health Program.Officer, Program Manager of National Safe Motherhood
Program, Family Helath Office, Disease Prevention and Control Bureau,
Department of Health
2016/7/30
Sat
2016/7/31
Sun
10:00-11:00
Department of Interior and Local
Government located at EDSA corner at
Quezon Avenue in Quezon City
DILG
Ms. Girlie Zkra, Division Chief/Local Governance Performance Management
Supervision/Bureau of Local Government Supervision
13:30-14:30
Bureau of Local Health Development DOH
Mr. Raul R. Alamis, Bureau of Local Health Systems Development, Health System
Development Division of DOH
16:15-16:45
National Statistics Authority NSA Ms. AURORA T. REOLALAS, OIC-Division Chief, Vital Statistics Division
1000-1200
DOH
San Lazaro Compound, Tayuman, Sta.
Cruz, Manila
DOH
Ms. Frances Mamaril, Division Chief Planning, Health Policy Development and
Planning Bureau
1400-1500
Makati Medical Center
Credit and Collections Department
Makati Medical Center
Dr. Flor Cruz, Patient Billing Unit、2.
Ms. Janet Medina, Billing and Collections Unit, 3.
Ms. Grace Salvador, Billing and Collection Unit, Makati Medical Center , Credit
and Collections Department
1000-1100
USAID USAID
Dr. Yolanda E. Oliveros, MD MPH, Development Assistance Specialist,
Ms. Reynalda L. Perez, Project, Management Specialist, Office of Health, USAID
1330-1500
PhiHealth PhilHealth
Ms. Evelyn C. Bangalan, Senior Manager,
Ms. Christine Frances D. Limson, Project Planning and Development Officer in
International and Local Engagement Department
Dr. Mary Antonetter Rimon
16:00-17:20
Mandaluyong City Hall Mandaluyong City Office
Dr. Recos Reyes Ibanes Camarinesm MD, MHA, Obstetrician-Gynecologist,
Mandalyuong City Health Officer
Dr. Cesar Tutaan, Mandaluyong City Health Officer
2016/8/4
Thu 14:00-15:00
Executive Office
Manila Doctors Hospital
#667 United Nations Avenue,
Ermita, Manila
Manila Doctors Hospital
Ms. Dr.Bernadette Hogar-Manlapat, Quality Management Representative
Ms. Julie S. alvamz@maniladoctors_com.joh Head, SCRO, Social Sector,
Ms. Ma Thresa A. Acosta, PhilHealth Specialist
Ms. Estrella M. Garcia, Finance Director
Mr. Noel Jonathan T. See, Officer In Charge, Business Development Division,
Manila Doctors Hospital
10:00-11:00
Bureau of Local Health Development DOH
Ms. Rosario S. Torralba, Supervising Health Program Officer, Bureau of Local
Health Systems Development, Department of Health
12:30-13:30
Health Human Resource
Development Bureau DOH
DOH
DOH OIC-Asec Kenneth G Ronquillo, Director IV Health Human Resource
Development Bureau
15:30-16:30
DOH JICA PP office
Ms. Itsuki, Mr. Kanamori
2016/8/6
Sat 14:40
Leave (PR432)
2016/8/2
Tue
2016/8/3
Wed
2016/8/5
Fri
2016/7/28
Thu
2016/7/29
Fri
2016/8/1
Mon
Arrive (PR427)
2016/7/25
Mon
2016/7/27
Wed
Attachment 1
A-1

A
tta
chment 2
Bicol schedule (28th August - 10th September)
Time Activity Venue Accomodation
2016/8/28 Sun Arrived in Manila (PR 427: 17:30)
10:00-12:00 Mtg with JICA
14:00-16:00 Internal meeting
7:25-8:25 Move from Manila to Legaspi, Albay (5J 319)
11:00-13:00 Mtg with DOH regional office
DOH regional office V,
Legaspi
14:00-15:00
Mtg with MHO Malinao@RHU
RHU in Malinao
Municipality
16:00-17:00 Mtg with local consultant (Meg) Villa Amanda hotel
9:00-:10:30
Mtg with Albay Provincial health officer
(MNCHN coordinator)
Albay provincial office
11:00-12:00 Mtg with PhilHealth regional director
PhilHealth Albay
regional office
13:00-15:30
Visit to Bicol regional training and teaching
hospital
BRTTH, Legaspi
18:00-19:00 Luzon Health (NGO) café
(parallel conduct by consultant: FGD at Burabad)
Burabad
Barangay/Malinao
9:00 - 12:00 FGD/interiew at Balading Barangay
13:00-13:40
DSWD officer in Municipalty, Municipal
social worker
14:00-15:00 Interview with BHWs at Burabad Barangay
6:00:-9:00 Moving to Naga city, Camarines Sur (by car)
9:00-11:00 Mtg with PHO Camarines Sur Eurotel hotel
15:00-16:00
Visit to Bombon lying in clinic (privte)
Bombon
Municipality/Naga city
17:00-18:00 Mtg with Naga City health officer Naga city office
9:00-12:00
FGD/visit to BHS at Panicuason Barangay
in Naga city
Panicuason Barangay
in Naga city
Naga
13:00-15:00 Internal meeting Hotel Naga
2016/9/4 Sun Report writing Naga
2016/9/5
Mon 9:00-12:00
FGD/visit to BHS at San Isidro Barangay in
Naga city
San Isidro iBrangay in
Naga city
Naga
9:00-10:30
Municipal health office/RHU in Pamprona
Municipality
11:00-12:30
FGD/visit to BHS at Batang Barangay in
Pamprona Municipality
15:00-16:00
FGD/visit to BHS at Poblacion Barangay in
Pamprona Municipality
18:00-19:00
Interview with MHO of Sipocot
Municipality
Hotel
Naga
10:00-15:00
FGD/visit to BHS at Binahian Barangay in
Sipocot Municipality
Binahian Barangay in
Sipocot Municipality
17:00-18:00 Visit to Sipocot District hospital
Sipocot District
hospital
9:30-12:00 Visit to Bicol Medical Center BMC
14:00-16:00
PhilHealth Cum Sur provincial office in
Naga
PhilHealth Cum Sur
provincial office
10:00-10:30 Internal meeting Hotel
12:30-13:20
2016/9/10 Sat
Leave for Japan (PR 432: 14:40)
2016/9/9 Fri
Legasipi
Legaspi
Remington Hotel, Manila
Move from Naga to Manila (PR 2262)
2016/9/8
Tur
Naga
Naga
Naga
Naga2016/9/7 Wed
2016/9/2
Fri
2016/9/3
Sat
Pamprona Municipality
Date
2016/8/30 Tue
2016/8/31
Wed
2016/9/6 Tue
Legasipi
Manila
2016/8/29 Mon
Tur2016/9/1
Balading & Burabad
Barangay/Malinao
A-2

CAR and Eastern Visayas schedule (28th August - 21st September)
Time Activity
Venue
Accomodation
2016/8/28 Sun
17:30
2016/8/29 Mon
10:00
M
eeting with JICA
Starbucks at Greenbelt 1
AM
Travel from Manila to Baguio (road)
13:30 Benguet PHO
D
OH-Benguet Office
15:00 CAR Regional DOH
DOH-CAR RO
16:00
PhilHealth Regional Office
P
hilHealth Regional Office
2016/8/31 Wed
All day
Luna
8:00 Farnorth Hospital
Farnorth Hospital
10:00
PhilHealth Provincial Office
Farnorth Hospital
11:00
Main Health Center (RHU) in Pudtol
RHU Pudtol
13:00
BHS (midwife) and BHWs in Barangay Cabatacan BHS Barangay Cabatacan
20:00
Apayao PHO
Las Palmas Hotel
8:00
BHS (midwife) and BHWs in Barangay Buluan BHS Barangay Buluan
10:00
2 FGDs with women beneficiaries (pregnant and
lactating women)
BHS Barangay Buluan
13:00 Conner MHO
BHS Barangay Buluan
2016/9/3 Sat
12:55
Manila
2016/9/4 Sun
13:00
9:00
DOH Region VIII DOH Regional Office
13:00
PHO Leyte PHO Leyte
15:00
EngenderHealth (VisayasHealth)
DOH RO
17:00
PhilHealth Regional Office PH R08 (Burgos St.)
8:30 EVRMC EVRMC
PM
9:00 PHO Northern Samar Provicial Health Office
11:00 PhilHealth Northern Samar PhilHealth Office
13:00
Nothern Samar Provincial Hospital Provincial Hospital
15:00 Catarman RHU RHU
8:00
Catarman Doctors Hospital Incorporated
CDHI
10:00
Barangay Balnasan: Barangay Captain Balnasan Barangay Hall, San Roque
12:00
Barangay Balnasan: Midwife and Nurse Balnasan Barangay Hall, San Roque
13:30
Barangay Balnasan: Pregnant women who received
ANC and will deliver at RHU
Balnasan Barangay Hall, San Roque
14:30 Barangay Balnasan: Women who delivered at home Balnasan Barangay Hall, San Roque
16:00
Barangay Balnasan: Wome who delivered at
hospital
Balnasan Barangay Hall, San Roque
9:00
Barangay Balnasan: Grandmothers I Balnasan Barangay Hall, San Roque
10:30
Barangay Balnasan: Grandmothers II Balnasan Barangay Hall, San Roque
11:15
Barangay Balnasan: Husbands of pregnant and
lactating women
Balnasan Barangay Hall, San Roque
13:00
San Roque MHO and PHN San Roque RHU
14:30
Mayor of San Roque Municipality Municipal Office
16:00
Barangay Balnasan: BHWs Balnasan Barangay Hall, San Roque
17:00
Barangay Balnasan: TBA/BHW Balnasan Barangay Hall, San Roque
18:00
Barangay Balnasan: Woman who had neonatal
deaths
Balnasan Barangay Hall, San Roque
10:00
Barangay Polangi: BHWs Polangi Barangay Hall, Catarman
12:00
Barangay Polangi: Woman who had neonatal death Private home, Barangay Polangi
19:00
DOH Northern Samar (DMO)
Local restaurant
2016/9/11 Sun
PM Travel from Northern Samar to Borongan
2016/9/12 Mon
All day
2016/9/13 Tue 8:00
Eastern Samar Provicial Hospital Provincial Hospital
9:30 PHO Eastern Samar PHO
11:30
Borongan RHU1 RHU Borongan
15:00 Eastern Samar PhilHealth PhilHealth
16:30 PHO Eastern Samar PHO
2016/9/14 Wed 8:00
Borongan CSWD City Hall
10:00 Llorente RHU RHU
11:30
Barangay Naubay: Pregnant women BHS Barangay Naubay
13:00
Barangay Naubay: Women who had home
deliveries
BHS Barangay Naubay
14:00
Barangay Naubay: BHWs BHS Barangay Naubay
16:00
Llorente Municipal Hospital Municipal Hospital
2016/9/15 Thu 8:00
DOH Eastern Samar (DMO) CHD Borongan
10:30
Dr. Leon Domingo Memorial Maternity Clinic
Dr. Leon Clinic
13:00
Barangay Balacdas: Pregnant and lactating women
who accessed facilities
Private home, Barangay Balacdas
14:30
Barangay Balacdas: Woman who had a home
delivery
Private home, Barangay Balacdas
15:00
Barangay Balacdas: TBA/BHW Private home, Barangay Balacdas
15:45
Barangay Balacdas: Midwife BHS Barangay Balacdas
Fri
Borongan
Report Writing (*national holiday)
2016/9/10
Sat
Travel from Tuguegarao to Manila (5J505)
Travel from Manila to Tacloban (PR2985)
Tacloban
2016/9/5 Mon
2016/9/6 Tue
Catarman
Travel from Tacloban to Northern Samar (road)
2016/9/7 Wed
2016/9/8
Thu
2016/9/9
Travel from Baguio to Luna (road)
2016/9/1
Thu
Tuguegarao
2016/9/2 Fri
Date
Arrive in Manila (PR 427)
Manila
2016/8/30 Tue Chalet Baguio
Attachment 3
A-3
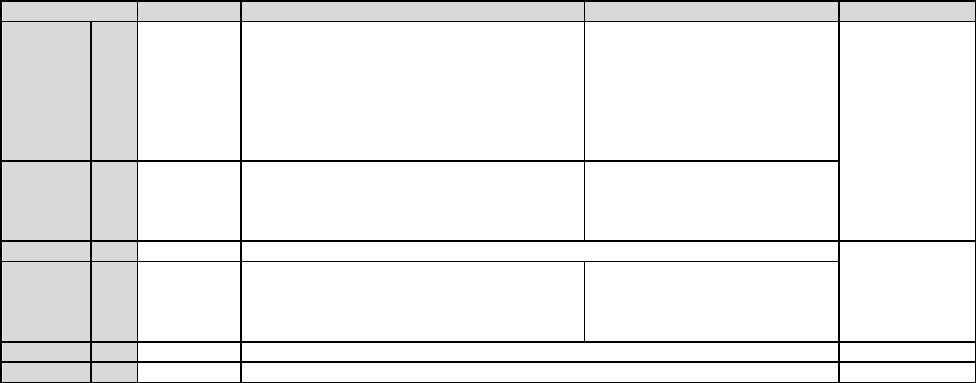
CAR and Eastern Visayas schedule (28th August - 21st September)
Time
Activity
Venue Accomodation
2016/9/16
Fri
10:00
Llorente Poblacion 1: Women who had home
deliveries
Barangay Hall
10:50 Llorente Poblacion 1: Husbands of pregnant women Barangay Hall
11:30 Llorente Poblacion 1: TBA
Barangay Hall
12:10 Llorente Poblacion 1: Grandmothers
Barangay Hall
17:00
MHO Llorente Municipality
Dona Vicenta Hotel
10:30
MHO Can-avid Municipality
Can-avid RHU
13:00
Barangay Carolina: Woman who had home
deliveries
Private home, Barangay Carolina
14:00
Barangay Carolina: Woman who delivered at RHU Private home, Barangay Carolina
2016/9/18 Sun
PM
10:00 JOCV (RHU San Isidro)
13:30 EVRMC (data collection)
EVRMC
14:00 Regional DSWD
Patawid Panilya Regional Program
Management Office
2016/9/20 Tue
14:55
Manila
2016/9/21 Wed
6:45 Depart Manila (PR428)
Travel from Tacloban to Manila (PR2986)
Borongan
Date
2016/9/17 Sat
Travel from Borongan to Tacloban (road)
Tacloban
2016/9/19 Mon
Attachment 3
A-4

Manila schedule (2nd - 8th October)
Time
Venue
Agency
Contact
2016/10/2 Sun 17:30
10:00-12:00
Room 1701 on the 17th Floor of
PhilHealth, Citystate Center, 709
Shaw Boulevard, Pasig City
PhilHealth
Dr. Israel Francis A. Pargas, M.D., OIC, Vice President Corporate
Affairs Group
Ms. Evelyn C. Bangalan, Senior Manager, International and Local
Engagement Department
Dr. Joy Maala, Primary Care Benefit Team Head
Ms. Abcean Estrada, MDG Team
Ms. Zarah Jane E. Ignacio
Ms. Christine Frances D. Limson, Project Planning and Development
Officer, International & Local Cooperation Department
14:00-15:00
DOH
San Lazaro Compound, Tayuman,
Sta. Cruz, Manila
DOH
Ms. Madelaine Gabriel Doromal
DOH, Health Facility Development Bureau
2016/10/5 Wed 15:00-16:30
PSA
Eton Centris 3,
Queson City
PSA, DHS Division
Ms. Plenee Castillo, Division Chief
Ms. Wima Suit
Mr. Jeremias Luis
Mr. Val Salting
Demographic and Health Statistics Division (DHSD)
9:00-10:30 JICA PP Office JICA PP office
SR Mr. Morita, Ms. Kawaguchi of JICA Philippine Office
Mr. Kanamori, JICA Health Advisor
Mr. Yoshida, Ms. Ito of JICA HQ
14:00-16:00
DOH
San Lazaro Compound, Tayuman,
Sta. Cruz, Manila
Jose Fabella Hospital
Dr. Minerva Vinluan,
Program Manager, Family Helath Office, Disease Prevention and
Control Bureau, Department of Health
2016/10/7 Fri 10:00-12:00
Meeting Room 3, 17th floor,
Cyberpod III, Eton Centris, EDSA
Quezon City
PSA, Population and
Housing Division
Ms. Minerva Eloisa P. Esquivias, Assistant National Statistician for
National Censuses Service,
Ms. Maribelle Baluyot, OIC, Population and Housing Census
Division,
Mr. Raul Ludovice, Supervising Statistical Specialist, PHCD
Ms. Jana Flor Vizmanos, Statistical Specialist I, Office of ANS,
Population and Housing Census Division
2016/10/8
Sat 8:45
Arrive(PR427)
Date
2016/10/3 Mon 9:00-16:30 Mandalyon City
Mandalyon City Hall,
City Hospital, Balangay
Health Center & private
clinic
Ms. Milagros Lagaran, Focal Person of Pantawid Pamilya Pipilino
Program, Mandaluyon City
Ms. Arlene Gampal, CSWD Social Worker, Mandaluyon City
Leave(PR422)
Tue2016/10/4
2016/10/6 Thu
Attachment 4
A-5

DCF Year: 2014
External
Benchmark
Internal
Benchmark
Health Data 2014
Health Data
2013
Nat'l Ave. 2012 Nat'l Target 2016
1.1 Increase LGU Investment for Health
201401
Percentage of Provincial/City (HUCs or ICCs)
Budget Allocated to Health
15.00 16.50 21.71 22
201403 Percentage of MOOE Allocated to Health
42.00 14.40 33.94 45
201404
Percentage of Provincial/City/Municipal Health
Expenditures
61.40 83.40 85.12 100
2.1 Local Health Facility Services
201405
Bed Occupancy Rate in all LGU-administered
Hospitals
50.44 137.80
96.10
80-85
201406 Gross Death Rate in all LGU-administered Hospitals
0.00 0.78
2.73
<1
3.1 Adequate Human Resource for Health
201407 RHU/Health Center Physician to Population Ratio
48287 26157 35497 20000
201408 RHU/Health Center Midwife to Population Ratio
16096 12390 6591 5000
201409 RHU/Health Center Midwife to Population Ratio
16096 12390 22947 20000
3.2 Essential Drugs/Medicines
201410 ComPack Anti-Hypertensive Drugs
N.D.
88.53
100
201411 ComPack Anti-Diabetic Drugs
N.D.
87.72
100
3.3 Health Emergency Management
201412 Percentage of LGUs with Operational HEPRRP
100.00
22.88
100
3.4 Support to Health Human Resource
201413
Percentage of LGUs Providing Full Magna Carta
Benefits
0.00
20.66
100
3.5 Client Satisfaction Survey
201414 Client Satisfaction Survey
N.D.
71.66
100
3.6 Blood Voluntary Program
201415 Blood Donation Rate
0.01
0.93
1
4.1 Disease Free Zone Initiatives
201416
Percentage Coverage of Target Population in
Endemic Area(s) with Mass Treatment for Filariasis
N.A. ND 71.72 85
201417 Annual Parasite Incidence for Malaria
N.A. NA 0.69 0.8
4.2 Intensified Disease Prevention and Control
201418 TB Case Detection Rate (All Forms of TB)
95.00 105.00 82.78 90
201419 TB Treatment Success Rate
66.00 88.00 82.53 90
4.3 Child Health
201420 Percentage of Fully Immunized Child
62.00 78.00 76.91 95
201421
Percentage of Infants (0-6 months old) Exclusively
Breastfed
68.00 68.00 61.81 70
201422
Prevalence of Underweight and Severely
Underweight 0-59 Months Old Children
N.D. 5.87 7.15 5
ID Performance Indicator
Performance Level Reference Table
Attachment 5
A-6
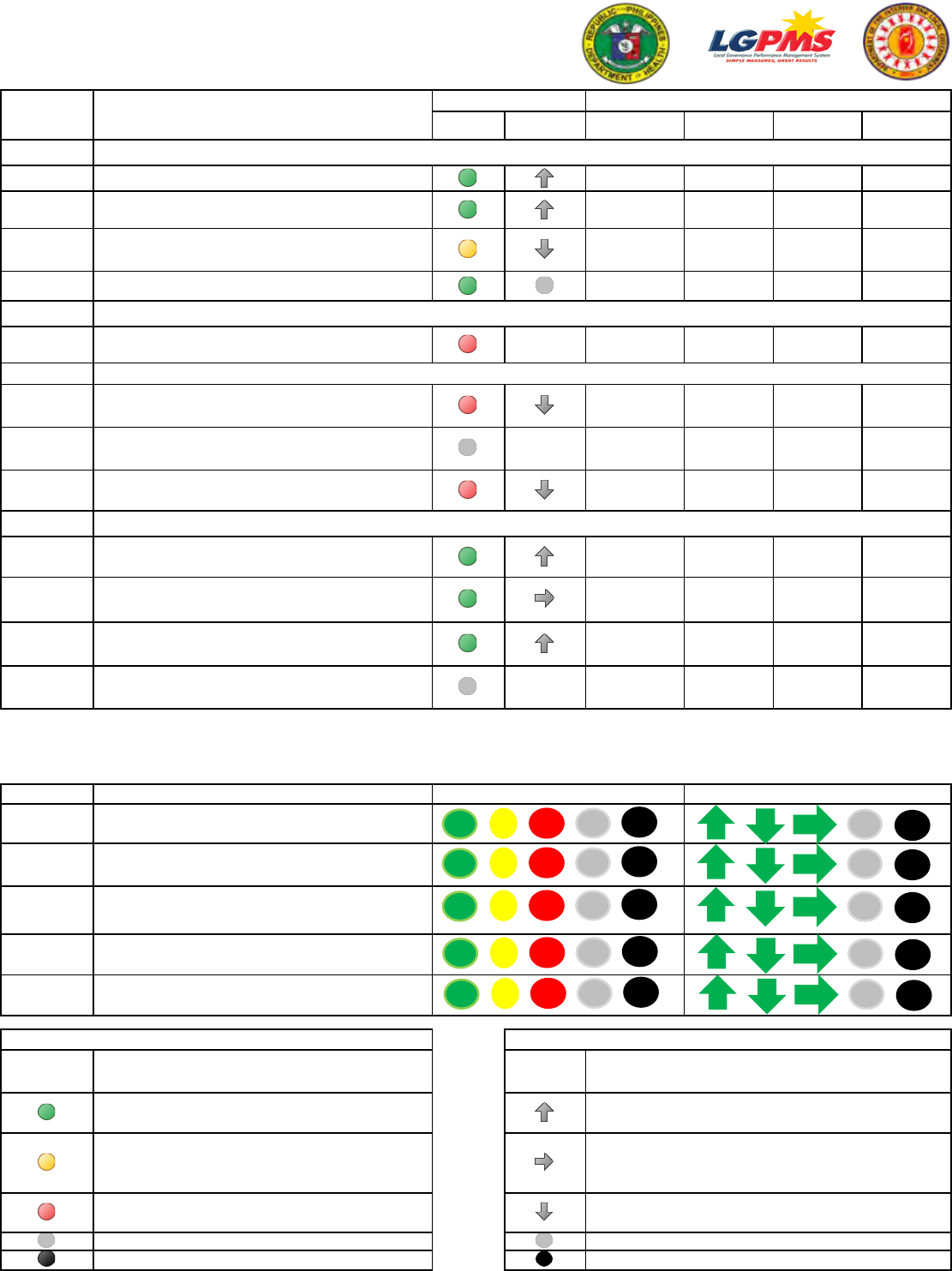
DCF Year: 2014
External
Benchmark
Internal
Benchmark
Health Data 2014
Health Data
2013
Nat'l Ave. 2012 Nat'l Target 2016
ID Performance Indicator
Performance Level Reference Table
4.4 Maternal Health
201423 Percentage of Facility-Based Deliveries
92.00 85.60 73.87 90
201424
Percentage of Deliveries Attended by Skilled Health
Professionals
93.00 85.60 83.15 90
201425
Contraceptive Prevalence Rate for Modern Family
Planning Methods
57.00 58.30 39.31 65
201426
Percentage of Functional Community Health
Teams
100.00 ND 78.01 100
4.5 HIV and AIDS
201427
Percentage of HIV and AIDS local response core
criteria adopted at the LGU
25.00 16.81 100
4.6 Environmental Health
201428
Percentage of Households with Access to Safe
Water
70.00 81.74 84.06 88
201429
Percentage of Drinking Water Sources Complying
with Microbiological Standards
N.D.
68.10
100
201430
Percentage of Households with Sanitary Toilet
Facilities
63.00 69.50 80.90 90
5.1 Accreditation of Health Facilities
201431
Percentage of RHUs/Health Centers Engaged with
PHIC on Primary Care Benefits (PCB)
100.00 72.72 37.54 100
201432
Percentage of RHUs/Health Centers Engaged with
PHIC on Maternity Care Package (MCP)
100.00 100.00 34.93 100
201433
Percentage of RHUs/Health Centers Engaged with
PHIC on TB-DOTS
100.00 18.18 31.20 100
201434
Utilization Rate of Enrolled NHTS Families of the PCB
Package
N.D. 0.00
35.07
100
Note: Highlighted in Blue are 2014 National Averages used as baseline for new indicators.
Summary of Results
No. Strategic Thrusts
I
Efficient Health Sector Spending
(PPAs 1.1)
II
Health Facilities Enhancement Program
(PPAs 2.1)
III
Governance for Health – Internal Management Support
(PPAs 3.1 - 3.6)
IV
Scaling-Up Public Health Intervention for MDGs
(PPAs 4.1 - 4.6)
V
Financial Risk Protection
(PPAs 5.1)
External
Benchmark
Performance Descriptions
External
Benchmark
Performance in current year is equal to or better
than 2016 National Target
Performance in current year is lower than 2016
National Target but equal to or better than 2012
National Average
Performance in current year is lower than 2012
National Average
No Data
Not Applicable / Non-endemic LGU
External Benchmark Internal Benchmark
Not Applicable / Non-endemic LGU
Legend: Legend:
Performance Descriptions
Performance in current year is better than previous
year
No change in performance
Performance in current year is not as good as previous
year
No Data
0
1
2 0
0
1
0
2
0
4
2
5 2
2
2
1
6
2
3
0
0 1
0
2
1
0
0
0
2
0
1
0
5 3
0
0
0
3
0
0
1
0
1 0
0
1
0
1
0
0
Attachment
5
A-7

I. IDENTIFICATION
SYSTEM GENERATED:
Household ID (to be filled up by the encoder)
Barangay Region Province
City / Municipality
Purok / Zone / Sitio
Street Address
2. Address
4. Contact Number
yrs
5. Length of Stay of Household in Barangay
6. Number of Sleeping Rooms
II. SOCIOECONOMIC INFORMATION
:
AM
PM
Time Started:
12. What kind of toilet facilities does the household have
in the house?
1. Water-sealed
2. Closed pit
3. Open pit
4. Others (pail system, etc.)
5. None
13. Is there electricity in the building / house?
1. Yes
2. No
14. What is the household’s main source of water supply?
1. Own use, faucet, community water system
2. Shared, faucet, community water system
3. Own use, tubed / piped well
4. Shared, tubed / piped well
5. Dug Well
6. Spring, river, stream, etc.
7. Rain
8. Peddler
15. How many of each of the following items does the
household own? (Input numbers from 0 to 9)
a. Radio
b. Television Set
c. VTR / VHS / VCD / DVD
d. Stereo / CD
e. Refrigerator / Freezer
f. Washing Machine
7. In what type of building/house does the household reside?
1. Single House
2. Duplex
3. Apartment / accessoria / condominium / townhouse
4. Commercial / industrial / agricultural building / house
5. Other housing unit (e.g. cave, boat)
8. What type of construction materials are the roofs made of?
1. Strong materials (galvanized iron, aluminum, tile,
concrete, brick, stone, asbestos)
2. Light materials (cogon, nipa, anahaw)
3. Salvaged / makeshift materials
4. Mixed but predominantly strong materials
5. Mixed but predominantly light materials
6. Mixed but predominantly salvaged materials
9. What type of construction materials are the outer walls made of?
1. Strong materials (galvanized iron, aluminum, tile,
concrete, brick, stone, wood, plywood, asbestos)
2. Light materials (bamboo, sawali, cogon, nipa, anahaw)
3. Salvaged / makeshift materials
4. Mixed but predominantly strong materials
5. Mixed but predominantly light materials
6. Mixed but predominantly salvaged materials
10. What is the tenure status of the housing unit and lot occupied
by the household?
1. Own or owner-like possession of house and lot
2. Rent house / room including lot
3. Own house, rent lot
4. Own house, rent-free lot with consent of owner
5. Own house, rent-free lot without consent of owner
6. Rent-free house and lot with consent of owner
7. Rent-free house and lot without consent of owner
11. Does the household own another house and lot?
1. Yes, please specify where the property is located
________________________________________
________________________________________
2. No
Encoded Verified
1. Household
Number
3. Number of Households in the housing unit
Continuation of 15
g. Air Conditioner
h. Sala Set
i. Dining Set
j. Car / Jeep
k. Telephone / Cellphone
l. Personal Computer
m. Microwave Oven / Gas Range
n. Motorcycle / Tricycle
16a. Has any household member experienced displacement
in the last 12 months?
1. Yes
2. No (proceed to item 17a)
16b. If yes, what are the causes? (check all applicable)
1. Natural / Manmade Disaster
2. Armed Conflict
3. Infrastructure Development Project
4. Other
17a. Has any household member received programs /
services from government agencies, LGUs or NGOs?
1. Yes
2. No (proceed to item 18)
Republic of the Philippines
Department of Social Welfare and Development
National Household Targeting Office
Family Assessment Form
Page 1 of 4 NHTO Rev v2.2.15 - Apr.8.2014
17b. If yes, what are the programs / services received? (check all applicable)
1. Scholarship
2. Day Care Service / ECCD
3. Supplemental Feeding
4. Subsidized Rice
5. Philhealth
6. Skills / Livelihood Training
7. Housing
8. Microcredit
9. Self-Employment Assistance
10. Pantawid Pamilya, please specify ID number/s
a.
b.
c.
11. Other Cash Transfer Program
12. Other
18. Do you consider your household as part of an Indigenous People’s
Group?
1. Yes, please specify _____________________________
2. No
Attachment 6
A-8

III. HOUSEHOLD ROSTER (PART 1)
20 Name
Last First
Middle
Ext
21 Date of Birth
Month Day Year
22 Age
23 Sex
25 MS
26 SP
27 RH
28 FN
Line No
Line No
Republic of the Philippines
Department of Social Welfare and Development
National Household Targeting Office
Family Assessment Form
Page 2 of 4 NHTO Rev v2.2.15 - Apr.8.2014
29 RF
24 Preg
19 TOH Type of Household 1. Single Family
2. Extended Family
3. Two or more non-related families / persons
1
1
2
2
3
3
4
4
5
5
6
6
7
7
8
8
9
9
27 RH Relationship to Household Head
01 - Household Head
02 - Wife/Spouse
03 - Son/Daughter
04 - Brother/Sister
05 - Son-in-Law/Daughter-in-Law
06 - Grandson/Granddaughter
07 - Father/Mother
08 - Other Relative
09 - Boarder
10 - Domestic Helper
11 - Non-Relative
25 MS Marital Status
1 - Single
2 - Married
3 - Widowed
4 - Divorced/Separated
5 - Annulled
6 - Unknown
26 SP Solo Parent
1 - Yes 2 - No
23 Sex Sex
1 - Male 2 - Female
If Code 1, proceed to
25 Marital Status
24 Preg Currently Pregnant
1 - Yes 2 - No
CODES
38 Name of Health Facility
Write the name of the health facility the
HH member goes.
39 AS Attending School / Day Care / Preschool
1 - Yes 2 - No
If Code 2, proceed to 41 Highest Education
Attained
20 Name
Write the complete name of the
household member
21 Date of Birth
Write the date of birth of the HH
member.
If complete (MDY), proceed to
23 Sex
22 Age
Write the age of the HH member.
28 FN Family Number
Write the corresponding number.
40 School / DCC / Preschool
Write the name of school the HH member attends.
29 RF Relationship to Nuclear Family Head
01 - Family Head
02 - Wife/Spouse
03 - Son/Daughter
04 - Brother/Sister
05 - Son-in-Law/Daughter-in-Law
06 - Grandson/Granddaughter
07 - Father/Mother
08 - Other Relative
30 Dis Disability
1 - Yes 2 - No
37 AHF Attending Health Facility
1 - Yes 2 - No
If Code 2, proceed to 39Attending School
41 Educ Highest Education Attained
00 - No Grade Completed 11 - Grade 10 (HS Graduate)
01 - Kinder or Day Care 12 - Grade 11
02 - Grade 1 13 - Grade 12
03 - Grade 2 14 - 1st Year College
04 - Grade 3 15 - 2nd Year College
05 - Grade 4 16 - 3rd Year College
06 - Grade 5 17 - 4th Year College or Higher
07 - Grade 6 or Elementary (Undergraduate)
08 - Grade 7 (1st Year HS) 18 - College Graduate
09 - Grade 8 (2nd Year HS) 19 - Above (M.A./M.S./Ph.D.)
10 - Grade 9 (3rd Year HS)
31 See Seeing
Does ___ have any difficulty/problem in
seeing, even when wearing eyeglasses?
1 - Yes 2 - No
32 Hear Hearing
Does ___ have any difficulty/problem in
hearing, even when using a hearing aid?
1 - Yes 2 - No
33 Walk Walking or Climbing Steps
Does ___ have any difficulty/problem in
walking or climbing steps?
1 - Yes 2 - No
34 Rem Remembering or Concentrating
Does ___ have any difficulty/problem in
remembering or concentrating?
1 - Yes 2 - No
35 Care Self-Caring
Does ___ have any difficulty/problem in
self-caring (bathing or dressing)?
1 - Yes 2 - No
36 Com Communicating
Does ___ have any difficulty/problem in
communicating using his/her usual lan-
guage?
1 - Yes 2 - No
10
11
12
13
14
15
16
10
11
12
13
14
15
16
Attachment 6
A-9

III. HOUSEHOLD ROSTER (PART 2)
41 Educ
46 CW
42 Emp
38 Name of Health Facility 40 School / DCC / Preschool 44 Primary Occupation / Business
39 AS
52 HO
51 SM
50 OFI
49 Ove
48 NE
47 BP
45 PSOC
37 AHF
Line No
Line No
43 JB
ROSTER LIST
of
count max
30 Dis
Republic of the Philippines
Department of Social Welfare and Development
National Household Targeting Office
Family Assessment Form
Page 3 of 4 NHTO Rev v2.2.15 - Apr.8.2014
31 See
32 Hear
33 Walk
34 Rem
35 Care
36 Com
1
1
2
2
3
3
4
4
5
5
6
6
7
7
8
8
9
9
CODES
50 OFI Overseas Filipino Indicator
Is _____ Overseas Contract Worker?
1 - OCW
2 - Workers other than OCW
3 - Employees in Phil Embassy, Consulates &
other missions
4 - Students abroad/tourists
5 - Others
If Code 4 or 5, proceed to the next HH member
51 SM Sending money to the household
Does _____ send money to the household?
1 - Yes 2 - No
If Code 2, proceed to the next HH member
52 HO How often member sends money in a year
How often does _____send money?
1 - Once or twice
2 - 3 to11 times
3 - 12 & above
46 CW Class of Worker
Where does _____ work? (mention the choices listed)
0 - Worked for private household
1 - Worked for private establishment
2 - Worked for gov’t/gov’t corporation
3 - Self-employed without any paid employee
4 - Employer in own family-operated farm or business
5 - Worked with pay in own family-operated farm or
business
6 - Worked without pay in own family-operated farm or
business
If Code 3, 4, 6, proceed to 48 Nature of Employment
42 Emp Employment
Did _____ do any work/business for at least an
hour during the past week?
1 - Yes 2 - No
If Code 1, proceed to 44 Primary Occupation /
Business
49 Ove Overseas
Is ______ overseas?
1 - Yes 2 - No
If Code 2, proceed to the next HH member
43 JB Job or Business
Although_____ did not work, does ____ have a
job or business?
1 - Yes 2 - No
If Code 2, proceed to 49 Overseas
44 Primary Occupation / Business
Write the primary occupation / business of the HH
45 PSOC Philippine Standard Occupation Code
Leave this column blank. Your AS will fill this out.
47 BP Basis of Payment
What is the basis of the payment
that _____ receives? Is it (mention
the choices listed below)?
0 - In kind, imputed
(received as wage/salary)
1 - Per piece
2 - Per hour
3 - Per day
4 - Monthly
5 - Pakyaw
6 - Other salaries / wages
7 - Not salaries / wages
48 NE Nature of Employment
Is _____’s work permanent, short-term, or on a
day-to-day/week-to-week basis?
1 - Permanent job / business / unpaid family work
2 - Short-term or seasonal or casual job /
business / unpaid family work
3 - Worked for different employers or
customer on day-to-day or week-to-week basis
10
11
12
13
14
15
16
10
11
12
13
14
15
16
Attachment 6
A-10

I
IV. DECLARATION
I declare that the data set forth herein is true and I authorize its
use for social protection programs.
_______________________________
Name of Respondent
Signature of Respondent
Thumbmark of Respondent
:
AM
PM
Time Ended:
I declare that the data set forth herein was obtained / reviewed by me personally.
V. CERTIFICATION
Signature over Printed
Name of Enumerator
Signature over Printed
Name of Area Supervisor
- -
MM DD YYYY
Date Accomplished
1
2 0
- -
MM DD YYYY
Date Reviewed
1
2 0
REMARKS
S/N - 1234567890
Republic of the Philippines
Department of Social Welfare and Development
National Household Targeting Office
Family Assessment Form
Page 4 of 4 NHTO Rev v2.2.15 - Apr.8.2014
Attachment 6
A-11
