
EDITED BY Sanjay Basu, MD, PhD, Director of Research | Jessica L. Alpert, Case Writer
Russell S. Phillips, MD, Center Director, William Applebaum Professor of Medicine;
Professor of Global Health and Social Medicine
| Harvard Medical School Center for Primary Care
Primary Care in the
COVID-19 Pandemic
Improving access to high-quality primary care,
accelerating transitions to alternative forms of
care delivery, and addressing health disparities
Sponsored by the CareQuest Institute for Oral Health and the Milbank Memorial Fund
The Harvard Medical School Center for Primary Care is strengthening health care by supporting primary
health care systems, teams, and leaders. The Center’s mission is to foster a dynamic community in and around
Harvard Medical School to promote and support primary care resilience, equity and antiracism, and healthcare
value with a goal of improving global health and well-being. The Center collaborates with partners at Harvard and
in the broader community in advocacy and leadership training, and advances the ability of primary care practices
to survive and thrive by researching and disseminating knowledge about how to build capacity for practice resil-
ience, health care equity and high-value care through best practices and innovation. Finally, the Center studies
how access to care is being preserved or improved given current and emerging challenges to health care, what
aspects of practice challenges and responses are opportunities for accelerating transitions from traditional care
to alternative care strategies such as virtual care, and how to identify the care strategies that can best address
health disparities heightened by the COVID-19 pandemic.
CareQuest Institute for Oral Health is a national nonprot championing a more equitable future where every
person can reach their full potential through excellent health. CareQuest Institute does this through their work in
grantmaking, research, health improvement programs, policy and advocacy and education as well as their leader-
ship in dental benets, care delivery and innovation advancements. CareQuest Institute collaborates with thought
leaders, health care providers, patients and local, state and federal stakeholders, to accelerate oral health care
transformation and create a system designed for everyone. To learn more, visit carequest.org.
The Milbank Memorial Fund is an endowed operating foundation that works to improve population health by
connecting leaders and decision makers with the best available evidence and experience. It does this work by:
identifying, informing, and inspiring current and future state health policy leaders to enhance their effectiveness;
working with state health policy decision makers on issues they identify as important to population health, particu-
larly in areas related to primary care, aging, and total costs of care; and publishing high-quality, evidence-based
publications and The Milbank Quarterly, a peer-reviewed journal of population health and health policy.

Primary Care in the
COVID-19 Pandemic
Improving access to high-quality primary care,
accelerating transitions to alternative forms of
care delivery, and addressing health disparities
Edited by:
Sanjay Basu, MD, PhD, Director of Research
Jessica L. Alpert, Case Writer
Russell S. Phillips, MD, Center Director
William Applebaum Professor of Medicine;
Professor of Global Health and Social Medicine
Harvard Medical School Center for Primary Care
Sponsored by the CareQuest Institute for Oral Health and the Milbank Memorial Fund
Contents
INTRODUCTION . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 1
SECTION 1: CHALLENGES OF COVID-19 TO PRIMARY CARE ACCESS AND QUALITY . . . . . 5
Chronic Care Management During the COVID-19 Pandemic . . . . . . . . . . . . . . 7
Addressing COVID-19 Proactively Through Primary Care in England’s
National Health Service . . . . . . . . . . . . . . . . . . . . . . . . . . .23
What We Can Learn from European Experiences of Primary Care Under COVID-19 . . . . .31
COVID-19 and Primary Care for Incarcerated People Released to the Community . . . . . .41
The Asia Pacic Experience of Primary Health Care in the COVID-19 Pandemic . . . . . .53
Reproductive Health: Equity and Innovation During the COVID-19 Pandemic . . . . . . 69
COVID-19 and Oral Health . . . . . . . . . . . . . . . . . . . . . . . . . 83
Addressing Food Insecurity Among At-Risk Older Adults . . . . . . . . . . . . . . 97
SECTION 2: PRACTICE TRANSITIONS: PAYMENTS AND DELIVERY . . . . . . . . . . . 107
Payer Actions and Primary Care in the Wake of COVID-19:
Will Primary Care Be There When We Need It? . . . . . . . . . . . . . . . . . 109
Financial Challenges for Primary Care Under COVID-19 . . . . . . . . . . . . . . 123
Financial Consolidation of Primary Care Practices During and After COVID-19 . . . . . . 137
Public Health Centers in Japan’s COVID-19 Response and Recovery . . . . . . . . . . 155
Community Health Workers in the COVID-19 Response and
Continuation of Primary Health Care . . . . . . . . . . . . . . . . . . . . . 163
Solutions to Oral Health Inequities . . . . . . . . . . . . . . . . . . . . . . 179
SECTION 3: STRATEGIES TO ADVANCE PRIMARY CARE EQUITY . . . . . . . . . . . . 201
Anti-Racist Primary Care Policy in the United States . . . . . . . . . . . . . . . 203
Building Community-Engaged Primary Care: Returning to Our Roots . . . . . . . . . 221
Integration of Primary Care and Oral Health . . . . . . . . . . . . . . . . . . 231
Telehealth Equity: Before and After COVID-19 . . . . . . . . . . . . . . . . . . 245
Improving Health Communication for Primary Care Practitioners
During and After COVID-19 . . . . . . . . . . . . . . . . . . . . . . . . 257
Undocumented Immigrants in the United States in the Time of COVID-19 . . . . . . . 269
Migrant Worker Health and Health Care in COVID-19 . . . . . . . . . . . . . . . 285
CONCLUSION . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 299
T
he COVID-19 pandemic has been a global disaster. A January 2021 report by the World Health
Organization Independent Panel for Pandemic Preparedness and Response summarized the
cascade of global missteps made during the course of the pandemic and the ways in which “we
have failed in our collective capacity” to respond to the challenges posed by COVID-19.
1
In the
United States, as of this writing, more than 400,000 people have died, in large part because of
a failure of leadership and the lack of a national plan to confront and control the pandemic.
2
Scientically proven methods of infection control such as masking, maintaining social distance,
testing, and contact tracing were politicized and questioned rather than uniformly followed.
3,4
However, even if eective leadership had been in place, the United States was poorly prepared to
confront such a pandemic. Public health and primary care, both essential to ghting infectious
disease, are poorly funded.
5
The payment structure for primary care was not optimized for tele-
medicine or for supporting practices when patients stay away due to fear of infection.
6,7
Personal
protective equipment was not stockpiled in adequate amounts to protect caregiving physicians,
nurses, and other sta, and primary care physicians suered the greatest mortality of any physi-
cian group.
8,9
The Centers for Disease Control and Prevention, the usual source of leadership, scien-
tic expertise, and guidance in the context of a pandemic, was sidelined and ridiculed by the lead-
ership of the country.
10
Unlike the United States, countries with better funding for and coordination
of primary care and public health closed down their economies, mounted eective messaging and
utilization of masking and social distance, and eectively implemented testing and contact-tracing
programs, demonstrating that the pandemic could be controlled.
11,12
As of January 2021, much of the national discourse is centered on vaccine dissemination, with a par-
ticular focus on prioritization strategies for underserved and vulnerable populations disproportion-
ately impacted by the pandemic. Despite the promise of vaccine availability, it is not clear whether
the United States is suciently prepared to develop and operationalize vaccination allocation plans,
leaving the potential for those at highest risk to be left behind.
13
Introduction
Jessica L. Alpert and Russell S. Phillips
The rationale for developing this report and the proceeding chapters is to put a spotlight on
(1) the ways in which countries failed or succeeded in overcoming the pandemic, (2) how
primary care innovated in response to the pandemic, (3) lessons learned that might inform
approaches to confronting future catastrophes, and (4) the ways in which innovation has
served as a tool for driving health equity. Through these chapters we aim to address some key
questions:
• How was primary care adversely impacted by the COVID-19 pandemic, and in what ways
did the eld innovate and adapt to the situation at hand?
• What is a framework for understanding the risks and opportunities posed by COVID-19 for
primary care practices?
• How have marginalized and vulnerable populations been disproportionally impacted in the
face of the COVID-19 pandemic?
• How did the social determinants of health and oppressive ideologies, including racism,
ableism, and ageism, intersect and coalesce in the health inequities observed among com-
munities and primary care patients?
• What lessons can be distilled from international experiences with COVID-19, and how can
those lessons be leveraged to catalyze systemic and structural change in the United States?
The COVID-19 pandemic highlighted long-term ineciencies and inequities in health
systems globally, and societies struggled to mitigate the contagion and loss of life. The
chapter authors celebrate the resilience, ingenuity, and devotion that primary care provid-
ers have shown during this time of uncertainty and loss. Their writings ultimately serve as
an important reminder that if systemic barriers remain unaddressed, equitable, accessible,
and sustainable primary care delivery will remain an empty promise for our patients and
communities.
2 PRIMARY CARE IN THE COVID-19 PANDEMIC
References
1. Second report on progress by the Independent
Panel for Pandemic Preparedness & Response. The
Independent Panel for Pandemic Preparedness and
Response. January 15, 2021. Accessed January 25,
2021. https://theindependentpanel.org/wp-content/
uploads/2021/01/Independent-Panel_Second-Report-
on-Progress_Final-15-Jan-2021.pdf.
2. Coronavirus in the U.S.: latest map and case count.
New York Times. Last updated January 25, 2021. Ac-
cessed January 26, 2021. https://www.nytimes.com/
interactive/2020/us/coronavirus-us-cases.html.
3. Sherling DH, Bell M. Masks, seat belts, and
the politicization of public health. J Hosp Med
2020;15(11):692-3. 10.12788/jhm.3524.
4. Gonsalves G, Yamey G. Political interference
in public health science during COVID-19. BMJ
2020;371:m3878. 10.1136/bmj.m3878.
5. Weber L, Ungar L, Smith MR, Recht H, Barry-Jester
AM. Hollowed out public health system faces more
cuts amid virus. The Associated Press. July 1, 2020.
Accessed January 26, 2021. https://apnews.com/ar-
ticle/b4c4bb2731da9611e6da5b6f9a52717a.
6. Augenstein J. Opportunities to expand telehealth
use amid the coronavirus pandemic. Health Af-
fairs Blog. March 16, 2020. Accessed January 26,
2021. https://www.healthaffairs.org/do/10.1377/
hblog20200315.319008/full/.
7. Blandford A, Wesson J, Amalberti R, AlHazme R,
Allwihan R. Opportunities and challenges for tele-
health within, and beyond, a pandemic. Lancet
Glob Health 2020;8(11):e1364-e5. 10.1016/S2214-
109X(20)30362-4.
8. Cohen J, Rodgers YVM. Contributing factors to
personal protective equipment shortages during the
COVID-19 pandemic. Prev Med 2020;141:106263.
10.1016/j.ypmed.2020.106263.
9. Gouda D, Singh PM, Gouda P, Goudra B. The
demography of deaths in health care workers: an
overview of 1,004 reported COVID-19 deaths. J Am
Board Fam Med 2021. In press.
10. Trump loyalists tried to inuence C.D.C. virus
reports. New York Times. September 12, 2020.
Accessed January 20, 2021. https://www.nytimes.
com/2020/09/12/world/covid-19-coronavirus.html.
11. Dominguez LW, Willis JS. COVID-19 and the case
for medical management and primary care. J
Prim Care Community Health October 21, 2020.
10.1177/2150132720965080.
12. Gramlich J. Americans give the U.S. low marks for
its handling of COVID-19, and so do people in other
countries. Pew Research Center. September 21,
2020. Accessed January 26, 2021. https://www.pe-
wresearch.org/fact-tank/2020/09/21/americans-give-
the-u-s-low-marks-for-its-handling-of-covid-19-and-
so-do-people-in-other-countries/.
13. Robbins R, Robles F, Arango T. Here’s why distribu-
tion of the vaccine is taking longer than expected.
New York Times. December 31, 2020. Accessed Jan-
uary 26, 2021. https://www.nytimes.com/2020/12/31/
health/vaccine-distribution-delays.html.
PRIMARY CARE IN THE COVID-19 PANDEMIC 3
SECTION 1: CHALLENGES OF
COVID-19 TO PRIMARY CARE
ACCESS AND QUALITY
Chronic Care
Management During
the COVID-19 Pandemic
Aaron Baum
U
pward of 60% of American adults have a chronic health condition, and 70% of deaths in the
United States are caused by one.
1
The most common chronic conditions, including hyperten-
sion, hyperlipidemia, and diabetes, share a set of biological risk factors, such as obesity, high blood
pressure, elevated blood glucose, and abnormal blood lipids, and behavioral risk factors, such as
tobacco use, excessive alcohol, poor nutrition, and physical inactivity. Many of these risk factors
are responsive to clinical interventions provided during routine care and can be exacerbated by
unemployment, loneliness, and stress.
The high prevalence of chronic conditions in the United States has increased the direct and indirect
burden of disease from the SARS-CoV-2 pandemic. Individuals with a chronic condition are more
likely to experience a severe outcome due to infection
2-4
and a prolonged recovery and sequelae.
5
Additionally, among the approximately 80% as-yet uninfected adults
6
and those individuals who
experience a mild course of illness after infection, the indirect burden of disease from the virus
may largely be determined by the extent to which morbidity from highly prevalent chronic condi-
tions worsens because of reduced use of routine care
7
and deteriorating psychosocial conditions.
8,9
Indeed, early evidence of excess mortality during the pandemic suggests that COVID-19 is a cause
in approximately two-thirds of estimated excess deaths. Among the remainder are deaths related
to nonrespiratory underlying causes, including diabetes, heart disease, and cerebrovascular dis-
ease.
10,11
Although many of these deaths may be directly caused by COVID-19 but misclassied (e.g.,
in part due to lack of widespread testing), others are likely related to the indirect consequences of
the pandemic on chronic conditions (e.g., delayed use of emergency services for acute exacerba-
tions of chronic conditions that benet from timely treatment).
12,13
The diagnosis and management of chronic conditions is predominantly the responsibility of pri-
mary care physicians,
14
who are in the midst of tremendous nancial strain because of declining
fee-for-service revenues.
15,16
The pandemic has necessitated that chronic care be delivered in ways
that decrease the risk of transmitting SARS-CoV-2 to patients. This challenge to care delivery
was collectively experienced by essentially every outpatient practice in the country. Because of
their central role in delivery and payment reform initiatives, many primary care practices have
experience using population health management strategies that became acutely relevant
during a pandemic that exacerbated preexisting health and socioeconomic disparities and that
challenged providers to leverage technology to deliver care in innovative ways.
In this chapter, I review the early empirical evidence on changes to chronic care delivery dur-
ing the pandemic, as well as trends in major risk factors for morbidity from common chronic
conditions. We close by describing ways that population health management approaches,
including panel management, team-based care, and social service integration, aided primary
care practices in managing chronic conditions during the pandemic.
How chronic care delivery changed during the pandemic
Visits for chronic care during the pandemic
Across all areas of the United States, evidence from multiple sources—including a conve-
nience sample of 50,000 outpatient providers,
7
a nationally representative audit of primary
care practices,
17
and the universe of outpatient Veterans Aairs clinics
18
—suggests that pri-
mary care volume declined by approximately 25%-50% during the rst four months of the
pandemic, and then rebounded by August 2020 to level o at a decline of approximately 10%
compared to prior years. The share of visits delivered by phone or video increased dramati-
cally, amounting to approximately 35% of primary care visits during the rst four months of
the pandemic relative to a pre-pandemic baseline of 10% of visits.
Given the sharp reduction in the use of primary care, a key question is whether the decline
was disproportionately driven by patients with chronic conditions. I was unable to identify
studies evaluating changes in the clinical composition of patients who used primary care
during the pandemic. To address this gap in the literature, I used national-scope electronic
health records data including diagnoses, procedures, labs, vitals, and medications sourced
from participating members of the Healthjump network, which was made available through
the COVID-19 Research Database.
19
I restricted my analysis to oce visits (Healthcare
Common Procedure Coding System codes 99201-99205, 99211-99215, 99241-99245, G0402,
G0438, and G0439) at outpatient practices that continuously belonged to the Healthjump
network since 2016.
Using the Healthjump data, we observed that the number of overall, in-person, and telehealth
visits declined similarly among patients with versus without a prepandemic history (two or
more diagnosis visits) of hypertension, hyperlipidemia, diabetes, depression, heart disease,
and congestive heart failure, respectively (Figure 1). Further, for patients with a history of hy-
pertension and diabetes prior to the pandemic, visit trends were similar among those whose
condition was well controlled versus poorly controlled during their last visit preceding the
pandemic (Figure 2). This suggests patients were neither more likely to drop out of chronic
care nor more likely to be prioritized for visits (e.g., via outreach or other panel management
eorts) during the pandemic as a function of their prepandemic health status.
8 PRIMARY CARE IN THE COVID-19 PANDEMIC
Given disparities in the prevalence of chronic condition by age, race, and ethnicity, a related
question is whether the demographic composition of patients who continued to use primary
care during the pandemic was similar to the composition of patients who used primary care
before the pandemic. Although visit rates for children remain substantially lower than for
adults, among adults overall rates did not meaningfully vary by age (though middle-aged
adults may have increased their use of telehealth more than other age groups).
7,17
Data from
the primary care practices of UCSF General Internal Medicine Practice and Zuckerberg San
Francisco General Hospital suggest that immediately after the onset of the pandemic, the
visit share of Black and Latino patients signicantly dropped, while the visit share of white
patients increased.
20
In contrast, results of a nationally representative audit of primary care
practices indicate that primary care visits declined by 17% among white patients over the rst
four months of the pandemic relative to the same four months of 2019, but by only 5% among
Black patients.
17
Changes in monitoring of major risk factors
As a consequence of the substitution of telehealth visits for in-person visits, the structure
and content of chronic care encounters changed during the pandemic. For example, audits of
a nationally representative sample of primary care practices indicate that blood pressure and
cholesterol assessments declined during the rst four months of the pandemic by 50% and
37%, respectively, driven by the decline in in-person visits.
17
Consistent with this, an IQVIA
medical claims data analysis estimates there was a reduction of 19% in oce visit lab orders
between March and September 2020, relative to the same time period in 2019. Regarding be-
havioral risk factors, data we analyzed from a national cohort of adults who used the Veterans
Health Administration during the pandemic suggest that the number of routine verbal screen-
ings for alcohol use, depression, post-traumatic stress disorder, and suicidal ideation—which
are feasible to administer during phone and video visits, but are typically conducted by nurses
in advance of a patient seeing a physician—declined by 39% in April and 37% in May 2020
compared to February, and then rebounded to a decline of only 5% by August (Figure 3).
Changes in new diagnoses
Likely as a consequence of reduced monitoring of biological and behavioral risk factors, the
nationally representative audit of primary care practices showed that rst visits for hyperten-
sion treatment declined by 39% during the pandemic; similarly, rst visits for high choles-
terol treatment declined by 27%, rst visits for depression treatment declined by 23%, and
rst visits for diabetes treatment declined by 16%.
17
Consistent with this, our analysis of electronic health records data from the Healthjump
platform suggests that the number of patients receiving their rst diagnosis of six chronic
conditions—hypertension, hyperlipidemia, diabetes, depression, heart disease, and conges-
tive heart failure—declined by between 30% and 40% in April 2020 relative to February 2020,
then rebounded back to, and in some cases, above, prepandemic levels by August (Figure 4).
This result is consistent with a diagnosis backlog model developed by IQVIA, which predicts a
PRIMARY CARE IN THE COVID-19 PANDEMIC 9

Figure 1. Trends in Overall, in-Person, and Telehealth Visits Among Patients With and Without Chronic
Conditions Prior to the Pandemic
This gure is based on electronic health records data from oce visits to outpatient practices that con-
tinuously used the Healthjump data management service between July 1, 2016, and September 1, 2020.
The patient population is the cohort of patients with a visit to any of these practices prior to March 1,
2020. Prepandemic history of chronic condition was dened as a patient receiving two or more diag-
nosis codes for the chronic condition prior to March 1, 2020. Telehealth visits were determined based on
the claim modier codes 95 or GT.
-0.6
-0.4
-0.2
0
0. 2
Hypertension
-0.6
-0.4
-0.2
0
0. 2
-500
0
50 0
10 00
1500
20 00
25 00
-0.6
-0.4
-0.2
0
0. 2
Hyperlipidemia
-0.6
-0.4
-0.2
0
0.2
-500
0
500
1000
1500
2000
2500
-0.6
-0.4
-0.2
0
0.2
Diabetes
-0.6
-0.4
-0.2
0
0.2
In-Person Visits Telehealth VisitsOverall Visits
No history of condition History of condition
1
No history of condition History of condition
-0.6
-0.4
-0.2
0
0.2
Depression
-0.6
-0.4
-0.2
0
0.2
-0.6
-0.4
-0.2
0
0.2
0.4
Heart disease
-0.6
-0.4
-0.2
0
0.2
0.4
-0.6
-0.4
-0.2
0
0.2
0.4
Congestive heart failure
-0.6
-0.4
-0.2
0
0.2
0.4
In-Person Visits Telehealth VisitsOverall Visits
-500
0
500
1000
1500
2000
2500
-500
0
500
1000
1500
2000
2500
-500
0
500
1000
1500
2000
2500
3000
-500
0
500
1000
1500
2000
2500
August-19
September-19
October-19
November-19
December-19
January-20
February-20
March-20
April-20
May-20
June-20
July-20
August-20
August-19
September-19
October-19
November-19
December-19
January-20
February-20
March-20
April-20
May-20
June-20
July-20
August-20
August-19
September-19
October-19
November-19
December-19
January-20
February-20
March-20
April-20
May-20
June-20
July-20
August-20
August-19
September-19
October-19
November-19
December-19
January-20
February-20
March-20
April-20
May-20
June-20
July-20
August-20
August-19
September-19
October-19
November-19
December-19
January-20
February-20
March-20
April-20
May-20
June-20
July-20
August-20
August-19
September-19
October-19
November-19
December-19
January-20
February-20
March-20
April-20
May-20
June-20
July-20
August-20
August-19
September-19
October-19
November-19
December-19
January-20
February-20
March-20
April-20
May-20
June-20
July-20
August-20
August-19
September-19
October-19
November-19
December-19
January-20
February-20
March-20
April-20
May-20
June-20
July-20
August-20
August-19
September-19
October-19
November-19
December-19
January-20
February-20
March-20
April-20
May-20
June-20
July-20
August-20
August-19
September-19
October-19
November-19
December-19
January-20
February-20
March-20
April-20
May-20
June-20
July-20
August-20
August-19
September-19
October-19
November-19
December-19
January-20
February-20
March-20
April-20
May-20
June-20
July-20
August-20
August-19
September-19
October-19
November-19
December-19
January-20
February-20
March-20
April-20
May-20
June-20
July-20
August-20
August-19
September-19
October-19
November-19
December-19
January-20
February-20
March-20
April-20
May-20
June-20
July-20
August-20
August-19
September-19
October-19
November-19
December-19
January-20
February-20
March-20
April-20
May-20
June-20
July-20
August-20
August-19
September-19
October-19
November-19
December-19
January-20
February-20
March-20
April-20
May-20
June-20
July-20
August-20
August-19
September-19
October-19
November-19
December-19
January-20
February-20
March-20
April-20
May-20
June-20
July-20
August-20
August-19
September-19
October-19
November-19
December-19
January-20
February-20
March-20
April-20
May-20
June-20
July-20
August-20
August-19
September-19
October-19
November-19
December-19
January-20
February-20
March-20
April-20
May-20
June-20
July-20
August-20
10 PRIMARY CARE IN THE COVID-19 PANDEMIC

Figure 1 continued.
This gure is based on electronic health records data from oce visits to outpatient practices that con-
tinuously used the Healthjump data management service between July 1, 2016, and September 1, 2020.
The patient population is the cohort of patients with a visit to any of these practices prior to March 1,
2020. Prepandemic history of chronic condition was dened as a patient receiving two or more diag-
nosis codes for the chronic condition prior to March 1, 2020. Telehealth visits were determined based on
the claim modier codes 95 or GT.
-0.6
-0.4
-0.2
0
0. 2
Hypertension
-0.6
-0.4
-0.2
0
0. 2
-500
0
50 0
10 00
1500
20 00
25 00
-0.6
-0.4
-0.2
0
0. 2
Hyperlipidemia
-0.6
-0.4
-0.2
0
0.2
-500
0
500
1000
1500
2000
2500
-0.6
-0.4
-0.2
0
0.2
Diabetes
-0.6
-0.4
-0.2
0
0.2
In-Person Visits Telehealth VisitsOverall Visits
No history of condition History of condition
1
No history of condition History of condition
-0.6
-0.4
-0.2
0
0.2
Depression
-0.6
-0.4
-0.2
0
0.2
-0.6
-0.4
-0.2
0
0.2
0.4
Heart disease
-0.6
-0.4
-0.2
0
0.2
0.4
-0.6
-0.4
-0.2
0
0.2
0.4
Congestive heart failure
-0.6
-0.4
-0.2
0
0.2
0.4
In-Person Visits Telehealth VisitsOverall Visits
-500
0
500
1000
1500
2000
2500
-500
0
500
1000
1500
2000
2500
-500
0
500
1000
1500
2000
2500
3000
-500
0
500
1000
1500
2000
2500
August-19
September-19
October-19
November-19
December-19
January-20
February-20
March-20
April-20
May-20
June-20
July-20
August-20
August-19
September-19
October-19
November-19
December-19
January-20
February-20
March-20
April-20
May-20
June-20
July-20
August-20
August-19
September-19
October-19
November-19
December-19
January-20
February-20
March-20
April-20
May-20
June-20
July-20
August-20
August-19
September-19
October-19
November-19
December-19
January-20
February-20
March-20
April-20
May-20
June-20
July-20
August-20
August-19
September-19
October-19
November-19
December-19
January-20
February-20
March-20
April-20
May-20
June-20
July-20
August-20
August-19
September-19
October-19
November-19
December-19
January-20
February-20
March-20
April-20
May-20
June-20
July-20
August-20
August-19
September-19
October-19
November-19
December-19
January-20
February-20
March-20
April-20
May-20
June-20
July-20
August-20
August-19
September-19
October-19
November-19
December-19
January-20
February-20
March-20
April-20
May-20
June-20
July-20
August-20
August-19
September-19
October-19
November-19
December-19
January-20
February-20
March-20
April-20
May-20
June-20
July-20
August-20
August-19
September-19
October-19
November-19
December-19
January-20
February-20
March-20
April-20
May-20
June-20
July-20
August-20
August-19
September-19
October-19
November-19
December-19
January-20
February-20
March-20
April-20
May-20
June-20
July-20
August-20
August-19
September-19
October-19
November-19
December-19
January-20
February-20
March-20
April-20
May-20
June-20
July-20
August-20
August-19
September-19
October-19
November-19
December-19
January-20
February-20
March-20
April-20
May-20
June-20
July-20
August-20
August-19
September-19
October-19
November-19
December-19
January-20
February-20
March-20
April-20
May-20
June-20
July-20
August-20
August-19
September-19
October-19
November-19
December-19
January-20
February-20
March-20
April-20
May-20
June-20
July-20
August-20
August-19
September-19
October-19
November-19
December-19
January-20
February-20
March-20
April-20
May-20
June-20
July-20
August-20
August-19
September-19
October-19
November-19
December-19
January-20
February-20
March-20
April-20
May-20
June-20
July-20
August-20
August-19
September-19
October-19
November-19
December-19
January-20
February-20
March-20
April-20
May-20
June-20
July-20
August-20
PRIMARY CARE IN THE COVID-19 PANDEMIC 11

Figure 2. Trends in Overall, In-Person, and Telehealth Visits Among Patients With a History of Hyper-
tension and Diabetes Prior to the Pandemic, by Whether Their Chronic Condition Was Well Controlled
Versus Poorly Controlled in Their Last Visit Before the Pandemic
This gure is based on electronic health records data from oce visits to outpatient practices that continuously used
the Healthjump data management service between January 1, 2016, and September 1, 2020. The patient popula-
tion is the cohort of patients with a visit to any of these practices prior to March 1, 2020, and a history of hypertension
and diabetes prior to the pandemic (dened as a patient receiving two or more diagnosis codes for hypertension or
diabetes prior to March 1, 2020). Well-controlled versus poorly controlled hypertension and diabetes was based on a
patient’s blood pressure > 140/90 mmHg and A1C > 8%, respectively, during their last visit before the pandemic (visits
up to six months before March 1, 2020, were included). Telehealth visits were determined based on the claim modier
codes 95 or GT.
Well Controlled Poorly Controlled
-0.8
-0.6
-0.4
-0.2
0
0.2
August-19
September-19
October-19
November-19
December-19
January-20
February-20
March-20
April-20
May-20
June-20
July-20
August-20
Blood pressure
Overall Visits
-0.8
-0.6
-0.4
-0.2
0
0.2
August-19
September-19
October-19
November-19
December-19
January-20
February-20
March-20
April-20
May-20
June-20
July-20
August-20
In-Person Visits
-500
0
500
1000
1500
August-19
September-19
October-19
November-19
December-19
January-20
February-20
March-20
April-20
May-20
June-20
July-20
August-20
Telehealth Visits
-0.8
-0.6
-0.4
-0.2
0
0.2
August-19
September-19
October-19
November-19
December-19
January-20
February-20
March-20
April-20
May-20
June-20
July-20
August-20
Glycated hemoglobin
-0.8
-0.6
-0.4
-0.2
0
0.2
August-19
September-19
October-19
November-19
December-19
January-20
February-20
March-20
April-20
May-20
June-20
July-20
August-20
-500
0
500
1000
1500
August-19
September-19
October-19
November-19
December-19
January-20
February-20
March-20
April-20
May-20
June-20
July-20
August-20
14% cumulative percent reduction by the end of 2020 in new diagnosis visits overall, with the
largest backlog expected for chronic condition diagnoses.
21
Though it remains unclear whether delayed diagnoses will impact patient outcomes, this
backlog of new chronic condition diagnoses is concerning, particularly for time-sensitive
conditions. For example, modeling studies predict poorer survival outcomes as a consequence
of the decline in cancer screenings, which are expected to cause delayed diagnoses that trans-
late to later-stage presentations and delayed surgeries.
22,23
Further, it is plausible that patients
who postponed care will present later in the course of their disease with worse symptoms at
the time of initial diagnosis. For hypertension and diabetes, our analysis of the Healthjump
data suggests that among patients with a new diagnosis, mean systolic blood pressure and
HbA1c were transiently elevated in May of 2020 (Figure 5). However, because rates of in-
person visits were also much lower in May, this pattern may simply be driven by healthier
patients delaying in-person visits more than sicker patients.
12 PRIMARY CARE IN THE COVID-19 PANDEMIC

Figure 3. Trends in Routine, Verbal Screenings for Alcohol Use, Suicidal Ideation, Depression, and
Post-Traumatic Stress Disorder (PTSD) Among a National Cohort of Veterans
This gure is based on electronic health records data from the Veterans Health Administration (VHA) Corporate
Data Warehouse, a national repository of electronic health records from visits to VHA facilities. The cohort includes
adults who rst enrolled in VHA care prior to 2019. We report monthly counts of screenings for alcohol misuse
(AUDIT-C score >4 for men and >3 for women), suicidal ideation (Item 9 from the PHQ2-i9 >1), depressive symp-
toms (PHQ-2 >2), and PTSD symptoms (PC-PTSD >3).
WWW.MILBANK.ORG
1
1 Footer Te x t
Figure 3. Trends in routine, verbal screenings for alcohol use, suicidal ideation, depression, and post-
traumatic stress disorder among a national cohort of veterans
0
100,000
200,000
300,000
400,000
500,000
600,000
700,000
Jan-19
Feb-19
Ma r-1 9
Apr-19
Ma y-19
Jun-19
Jul-19
Aug-19
Sep-19
Oct-19
Nov-19
Dec-19
Jan-20
Feb-20
Ma r-2 0
Apr-20
Ma y-20
Jun-20
Jul-20
Aug-20
Sep-20
Monthly # of mental health screenings
Figure 4. Trends in the Number of Patients Per Month Receiving a First Diagnosis of Common
Chronic Conditions
This gure is based on electronic health records data from oce visits to outpatient practices that continuously used
the Healthjump data management service between January 1, 2016, and September 1, 2020. The patient population
is the cohort of patients with a visit to any of these practices prior to March 1, 2020. A patient’s rst diagnosis of a
chronic condition was determined as the date of the rst visit during which the patient received a diagnosis code for
that condition.
WWW.MILBANK.ORG
2
2 Footer Te x t
-0.6
-0.4
-0.2
0
0.2
0.4
August-19
September-19
October-19
November-19
December-19
January-20
February-20
Ma rch-20
April-20
Ma y-20
June-20
July-20
August-20
Percent change in new diagnoses since February 2020
Hypertension Hyperlipidemia Diabetes Depression
Heart disease
Fig 4
PRIMARY CARE IN THE COVID-19 PANDEMIC 13

Changes in prescriptions
Among primary care practices overall, new medications were initiated 26% less often during
the rst four months of the pandemic compared to prior years, while continuing medica-
tions were prescribed 9% less often, per the nationally representative audit study.
17
The IQVIA
National Prescription Audit report indicates that the volume of “new-to-brand” prescriptions
(e.g., patients starting a prescription drug they have not previously used) written by primary
care physicians was down 13% between March and August 2020 compared to the same period
in 2019, though overall prescriptions were down only 4%.
21
The IQVIA report speculates that
the driver of this decline is that telehealth visits generated 33% fewer new prescriptions than
oce visits during 2020. The report also notes that changing patterns in in-person and mail-
in lls, including growth in extended lls, may aect adherence and compliance consider-
ations as patients make fewer trips back to the pharmacy.
Changes in common risk factors for poor chronic disease
control during the pandemic
It is too early to identify the population health consequences attributable to changing patterns
in patients’ use of routine care, less information being available to physicians at the point-
of-care, and the decline in new chronic condition diagnoses and new-to-brand prescriptions,
though previous studies suggest that delayed access to primary care may impact the preva-
lence and control of chronic conditions.
24,25
Although further research is required to measure
changes in morbidity and mortality related to changes in chronic care during the pandemic,
WWW.MILBANK.ORG
3
3 Footer Te x t
0
50
100
150
200
Aug-19
Sep-19
Oct-19
Nov-19
Dec-19
Jan-20
Feb-20
Ma r-20
Apr-20
Ma y-20
Jun-20
Jul-20
Aug-20
Blood pressure (mmHg)
Mean blood pressure at first diagnosis of
hypertension
Systolic BP Diastolic BP
0.00
3.00
6.00
9.00
12.00
August-19
September-19
October-19
November-19
December-19
January-20
February-20
Ma rch-20
April-20
Ma y-20
June-20
July-20
August-20
HbA1c (%)
Mean HbA1c at first diagnosis of
diabetes
HbA1c
Figure 5. Blood pressure and Glycated Hemoglobin Levels Among Patients With a New Diagnosis of Hy-
pertension and Diabetes, by Month
This gure is based on electronic health records data for oce visits to outpatient practices that continuously used
the Healthjump data management service between January 1, 2016, and September 1, 2020. The patient population
is the cohort of patients with a visit to any of these practices prior to March 1, 2020. A patient’s rst diagnosis of a
chronic condition was determined as the date of the rst visit during which the patient received a diagnosis code for
that condition.
14 PRIMARY CARE IN THE COVID-19 PANDEMIC
several studies—largely from outside of the United States, as the major representative surveys
of risk factors in the United States, such as the Behavioral Risk Factor Surveillance System,
are generally updated annually—have evaluated how shared risk factors for complications
from chronic disease, including tobacco use, alcohol use, unhealthy diet, and lack of exercise,
have changed during the pandemic.
Tobacco use
Although concerns about becoming seriously ill from COVID-19 could reduce tobacco use,
higher than usual levels of stress and isolation could increase it. A cross-sectional survey of
53,000 adults conducted in April 2020 in the United Kingdom found that, among the current
smokers surveyed, a considerably higher proportion reported a recent increase in smoking
(42%) than reported smoking less (13%).
26
A 6,800-person survey conducted in April 2020
across Italy, India, South Africa, the United Kingdom, and the United States found that a major-
ity of respondents had maintained or increased use of tobacco products, while only a quarter
of respondents reported reducing their use. In contrast, data from a series of 1,000-person
monthly surveys that is representative of adults in England found no change in smoking preva-
lence in April 2020 compared to prior years, but a small increase in quit attempts.
27
Alcohol use
Several pieces of evidence suggest increased alcohol use during the shelter-in-place period.
Though mandatory closure of bars would be expected to decrease alcohol use, March 2020
data from Nielsen showed a 54% increase in sales of alcohol in the United States compared
with one year before, likely reecting stockpiling.
28
More recent data from the nationally rep-
resentative RAND Corporation’s American Life Panel found 75% of adults consumed alcohol
one day more per month during the spring of 2020 compared to the spring of 2019.
29
Further,
heavy drinking rose 41% among women. Thus, while social alcohol use may have declined,
alcohol use at home—where higher-risk, heavy users tend to consume it—appears to have
increased, raising concerns that long-term, excessive alcohol misuse might escalate into an
alcohol use disorder during the pandemic.
30
Unhealthy diet
The United States Department of Agriculture (USDA) reported that, nationally, money spent
on food away from home dropped from $67 billion in February 2020 to $54 billion in March,
then bottomed out at $36 billion in April.
31
In contrast, sales of food at home increased over
the same period. Because food at home is less caloric and has less saturated fats and sodium,
diets may have improved during the shelter-in-place period. Consistent with this, responses
among participants in ve large cohort studies in the United Kingdom to an online question-
naire indicated moderate increases in fruit and vegetable consumption during the pandemic,
including among individuals eating more meals at home.
32
Conversely, increased unemployment during the pandemic expanded the need for nutrition
assistance. The Centers for Disease Control and Prevention (CDC) Household Pulse Survey
PRIMARY CARE IN THE COVID-19 PANDEMIC 15
data from mid-September 2020 suggest that 8% of adults in the country reported that their
household sometimes or often didn’t have enough to eat in the last seven days because they
“couldn’t aord to buy more food.”
33
National data from the USDA indicate that in May 2020
the number of Supplemental Nutrition Assistance Program (SNAP) participants was 17%
higher than in February 2020, an unprecedented growth rate.
34
However, SNAP’s capacity to
rapidly expand to meet the increased demand varied geographically, leaving many food-inse-
cure households without access to aordable nutritious food. Further, many eligible individu-
als do not receive public benets from safety-net programs that they qualify for. For example,
after Texas temporarily simplied the SNAP application process by removing paystub, work,
and interview requirements in late March 2020, the Texas Health and Human Services
Commission reported receiving four times as many applications for benets in April 2020 as
in April 2019, doubling the already historically high number of applications led in March
2020.
35
Nonetheless, a cross-sectional online survey in May 2020 found high rates of food
insecurity among young adults in Texas, with the two strongest predictors of food insecurity
changes in housing and loss of employment as a direct result of the COVID-19 pandemic.
36
Lack of exercise
According to data recorded between January and June 2020 by a convenience sample of
240,000 US-based users of a free health and wellness smartphone app, there was a 20%
decline in daily step count during March and April relative to January and February, and a
10% decline during May and June 2020.
37
Similarly, a longitudinal study of 5,000 UK-based
users of a smartphone app between January and June 2020 found a 37% reduction in weekly
minutes of physical activity during the pandemic, with greater reductions among younger and
more active people.
38
Although these declines reect a combination of changes to exercising
and to activities such as commuting and shopping, a smaller study of 1,824 young adults in
Singapore using data from wearable sensors found that changes in moderate-to-vigorous
physical activity decreased 31% during the pandemic compared with a decrease of 38% in
overall step counts.
39
Tools primary care physicians used to provide chronic care
during the pandemic
The disruption to routine care delivery in combination with the disparate exacerbation of risk
factors challenged providers to deliver chronic care in innovative ways. In response, many
primary care practices used population health strategies, tools, and data—including panel
management, team-based care, and social service integration—to continue delivering high-
quality chronic care during the pandemic.
Panel management
As the frequency of in-person interactions with patients decreased, the value of proactively
engaging with patients—reviewing patient lists, reaching out to higher-risk patients, and
16 PRIMARY CARE IN THE COVID-19 PANDEMIC
oering care on the basis of the patient’s potential risk and benet from a visit—between
visits increased. Many practices with preexisting panel management data and infrastructure
reported adapting them to the pandemic.
40
One case study was reported by primary care physicians in the Division of General Internal
Medicine at Massachusetts General Hospital.
41
Their clinics used a real-time clinical registry
that captured information on patient appointments and prescriptions to prioritize outreach
activities, for example, reaching out to a patient who had failed to rell a prescription.
Innovatively, they also allowed patients to input self-reported data on behavioral risk factors
as well as social determinants and provided patients with home monitoring devices that fed
blood pressure levels into the platform. This allowed their coordinators to prioritize outreach
to patients who experienced a change in psychosocial conditions or chronic condition control,
as well as to those who missed appointments or delayed medication rells.
Team-based care
Delivering high-quality virtual primary care was a challenge as practices massively ramped
up telehealth services in the midst of the pandemic. A side eect of the virtual care setting is
that patient ow through the oce is disrupted, as physicians, nurses, care managers, and
schedulers no longer share an oce space. As a consequence, telehealth visits often abandon
the initial portion of the visit during which nurses assess vital signs and conduct brief verbal
screenings to assess behavioral risk factors. Thus, not only were fewer changes in patients’
biological risk factors detected, likely leading to fewer new diagnoses and prescriptions, but
changes in behavioral risk factors also went undetected, likely leading to fewer interventions
related to tobacco cessation, substance abuse, and depression.
An example of an organization that invested in a virtual team-based primary care delivery
model that uses established patient-centered medical home principles is the Veterans Health
Administration (VHA). Prior to the pandemic, the VHA developed a model to provide virtual
team-based primary care services to veterans in rural and underserved areas, which it ex-
panded during the pandemic.
42-44
The model includes a central hub that houses primary care
physicians, mental health sta, and clinical pharmacy specialists. During a telehealth visit, a
primary care physician can add a team member to the patient’s video visit to provide a warm
hando—for example, adding a mental health team member to conduct a brief assessment
one-on-one with the patient. The model innovatively allows for a hybrid in-person and
telehealth visit in the event a physical exam is needed. In this case, local nursing sta can
see a patient in an exam room equipped with technology that allows for a video call between
the patient’s primary care team and the patient, during which ndings and images from the
in-person exam are shared in real time. While the share of telehealth visits recedes to pre-
pandemic levels for other health systems, the VHA has continued to expand use of and invest-
ment in video visits.
45
PRIMARY CARE IN THE COVID-19 PANDEMIC 17
Social service integration
The scale of socioeconomic disruption during the pandemic has highlighted the importance of
care models capable of engaging with patients’ social needs.
46
Millions of adults experienced
unemployment and declining household income that put their households at greater risk of
food and housing insecurity.
8
The mid-September round of the CDC’s Household Pulse Survey
found that one in three adults reported it was somewhat or very dicult for their household
to cover usual expenses in the past seven days.
33
These unmet social needs have been shown
to increase the risk of developing common chronic conditions and impair a person’s ability to
manage these conditions.
47-50
A case study on enhanced clinical–community linkages was reported by the leadership and
sta at the Contra Costa Health Service, a safety-net county health system in Northern
California.
51
Before the pandemic, it had established a large case management program oer-
ing coaching and social services to Medicaid beneciaries, powered by a data set that linked
individuals’ insurance claims, medical records, and social service utilization. During the
pandemic, program sta analyzed the data set to model and rank each Medicaid beneciary’s
risk of hospitalization from COVID-19. Case managers called the most high-risk individuals
to assess their social needs through a 21-item questionnaire. Leveraging established cross-
sectional partnerships, case managers provided information on local food pantries, assistance
with applications for public benets (e.g., SNAP), and referrals to legal aid (e.g., related to
evictions). Patients’ responses to the questionnaire were recorded in the health system’s elec-
tronic health records to provide physicians with information at the point of care on patients’
food insecurity, housing instability, unemployment, and social isolation. Particularly in disad-
vantaged communities, health systems that are able to coordinate with social services through
cross-sectional partnerships and shared data resources will be better positioned to manage
their patients’ chronic conditions and support community resilience over the long term.
Conclusions
In conclusion, during the pandemic thus far, fewer patients with preexisting chronic condi-
tions used primary care, primary care practices had less data on their patients’ biological and
behavioral risk factors, fewer new medications were prescribed, and a backlog of undiagnosed
new chronic conditions accumulated. Additionally, early evidence suggests that, on average,
alcohol use increased and physical activity decreased during the pandemic. The evidence also
suggests that overall trends in behavioral risk factors likely mask clinically relevant heteroge-
neity, as the pandemic exacerbated disparities in underlying economic conditions in opposite
ways for dierent populations (e.g., remote employees eating healthier meals at home versus
newly unemployed individuals with worsened food insecurity).
In combination with widespread escalation of socioeconomic adversity, these changes in
chronic care delivery and behavioral risk factors may have contributed to the observed in-
crease in deaths during the pandemic that were unrelated to COVID-19.
11
Finally, case stud-
ies suggest that many primary care practices successfully leveraged their population health
experience in panel management, team-based care, and social service integration in order to
adapt their model of chronic care delivery to the myriad challenges imposed by the pandemic.
18 PRIMARY CARE IN THE COVID-19 PANDEMIC
Acknowledgments
Data, technology, and services used in
the generation of these research ndings
were generously supplied pro bono by the
COVID-19 Research Database partners, who
are acknowledged at https://covid19research-
database.org/. Additionally, this article is the
result of work supported with resources and
the use of facilities at the Veterans Aairs
New York Harbor Healthcare System. The
Veterans Aairs New York Harbor Healthcare
System had no role in the design and conduct
of the study; collection, management, analy-
sis, and interpretation of the data; prepara-
tion, review, or approval of the manuscript;
or decision to submit the manuscript for
publication. The contents do not represent
the views of the US Department of Veterans
Aairs or the US government.
References
1. About chronic diseases. National Center for Chronic
Disease Prevention and Health Promotion. Last
reviewed January 12, 2021. Accessed January 29,
2021. https://www.cdc.gov/chronicdisease/about/in-
dex.htm.
2. Richardson S, Hirsch JS, Narasimhan M, et al. Pre-
senting characteristics, comorbidities, and outcomes
among 5700 patients hospitalized with COVID-19 in
the New York City area. JAMA 2020;323(20):2052-9.
10.1001/jama.2020.6775.
3. Jordan RE, Adab P, Cheng K. COVID-19: risk factors
for severe disease and death. BMJ 2020;368:m1198.
10.1136/bmj.m1198.
4. Zhou F, Yu T, Du R, et al. Clinical course and risk
factors for mortality of adult inpatients with COVID-19
in Wuhan, China: a retrospective cohort study.
Lancet 2020;395(10229):1054-62. 10.1016/S0140-
6736(20)30566-3.
5. Tenforde MW, Kim SS, Lindsell CJ, et al. Symptom
duration and risk factors for delayed return to usual
health among outpatients with COVID-19 in a multi-
state health care systems network—United States,
March–June 2020. MMWR Morb Mortal Wkly Report
2020;69(30):993-8. 10.15585/mmwr.mm6930e1.
6. Ray EL, Wattanachit N, Niemi J, et al. Ensemble fore-
casts of coronavirus disease 2019 (COVID-19) in the
US. medRxiv 2020. 10.1101/2020.08.19.20177493.
7. Mehrotra A, Chernew M, Linetsky D, et al. The impact
of the COVID-19 pandemic on outpatient visits:
changing patterns of care in the newest COVID-19
hot spots. Commonwealth Fund. August 13, 2020.
10.26099/yaqe-q550.
8. Chetty R, Friedman JN, Hendren N, et al. How did
COVID-19 and stabilization policies affect spending
and employment? A new real-time economic tracker
based on private sector data: National Bureau of Eco-
nomic Research; 2020. Report No. 27431. 10.3386/
w27431.
9. Ettman CK, Abdalla SM, Cohen GH, Sampson L,
Vivier PM, Galea S. Prevalence of depression symp-
toms in US adults before and during the COVID-19
pandemic. JAMA Netw Open 2020;3(9):e2019686.
10.1001/jamanetworkopen.2020.19686.
10. Woolf SH, Chapman DA, Sabo RT, Weinberger DM, Hill
L, Taylor DDH. Excess deaths from COVID-19 and other
causes, March-July 2020. JAMA 2020;324(15):1562-
4. 10.1001/jama.2020.19545.
11. Woolf SH, Chapman DA, Sabo RT, Weinberger DM,
Hill L. Excess deaths from COVID-19 and other
causes, March-April 2020. JAMA 2020;324(5):510-3.
10.1001/jama.2020.11787.
12. Baum A, Schwartz MD. Admissions to Veterans
Affairs hospitals for emergency conditions during
the COVID-19 pandemic. JAMA 2020;324(1):96-9.
10.1001/jama.2020.9972.
13. Lai PH, Lancet EA, Weiden MD, et al. Characteristics
associated with out-of-hospital cardiac arrests and
resuscitations during the novel coronavirus disease
2019 pandemic in New York City. JAMA Cardiol
2020;5(10):1154-63. 10.1001/jamacardio.2020.2488.
14. Bodenheimer T, Wagner EH, Grumbach K. Improving
primary care for patients with chronic illness. JAMA
2002;288(14):1775-9. 10.1001/jama.288.14.1775.
15. Basu S, Phillips RS, Phillips R, Peterson LE, Landon
BE. Primary care practice nances in the United
States amid the COVID-19 pandemic: study esti-
mates the potential impact of COVID-19 on operating
expenses and revenues of primary care practices.
Health Aff (Millwood) 2020;39(9):1605-14. 10.1377/
hlthaff.2020.00794.
16. Phillips RL, Bazemore A, Baum A. The COVID-19
tsunami: the tide goes out before it comes in. Health
Affairs Blog. April 17, 2020. Accessed January 29,
2021. https://www.healthaffairs.org/do/10.1377/
hblog20200415.293535/full/.
PRIMARY CARE IN THE COVID-19 PANDEMIC 19
17. Alexander GC, Tajanlangit M, Heyward J, Man-
sour O, Qato DM, Stafford RS. Use and content of
primary care ofce-based vs telemedicine care visits
during the COVID-19 pandemic in the US. JAMA
Netw Open 2020;3(10):e2021476. 10.1001/jamanet-
workopen.2020.21476.
18. Baum A, Kaboli PJ, Schwartz MD. Reduced in-
person and increased telehealth outpatient visits
during the COVID-19 pandemic. Ann Intern Med
2021;174(1):129-31. 10.7326/M20-3026.
19. COVID-19 Research Database. Accessed October
12, 2020. https://covid19researchdatabase.org/.
20. Nouri S, Khoong EC, Lyles CR, Karliner L. Addressing
equity in telemedicine for chronic disease manage-
ment during the COVID-19 pandemic. NEJM Catalyst
2020;1(3). 10.1056/CAT.20.0123.
21. Monitoring the impact of COVID-19 on the pharma-
ceutical market. IQVIA. January 15, 2021. Accessed
January 29, 2021. https://www.iqvia.com/-/media/
iqvia/pdfs/les/iqvia-covid-19-market-tracking-us.
pdf?&_=1612353531599.
22. Kaufman HW, Chen Z, Niles J, Fesko Y. Changes
in the number of US patients with newly identi-
ed cancer before and during the coronavirus
disease 2019 (COVID-19) pandemic. JAMA Netw
Open 2020;3(8):e2017267. 10.1001/jamanet-
workopen.2020.17267.
23. Sud A, Jones ME, Broggio J, et al. Collateral damage:
the impact on outcomes from cancer surgery of the
COVID-19 pandemic. Ann Oncol 2020;31(8):1065-74.
10.1016/j.annonc.2020.05.009.
24. Baum A, Barnett ML, Wisnivesky J, Schwartz MD.
Association between a temporary reduction in access
to health care and long-term changes in hypertension
control among veterans after a natural disaster. JAMA
Netw Open 2019;2(11):e1915111. 10.1001/jamanet-
workopen.2019.15111.
25. Wherry LR, Miller S. Early coverage, access, utiliza-
tion, and health effects associated with the Affordable
Care Act Medicaid expansions: a quasi-experimental
study. Ann Intern Med 2016;164(12):795-803.
10.7326/M15-2234.
26. Jackson SE, Brown J, Shahab L, Steptoe A, Fancourt
D. COVID-19, smoking and inequalities: a study
of 53 002 adults in the UK. Tob Control August 21,
2020. [Online ahead of print] 10.1136/tobaccocon-
trol-2020-055933.
27. Jackson SE, Garnett C, Shahab L, Oldham M, Brown
J. Association of the COVID-19 lockdown with smok-
ing, drinking, and attempts to quit in England: an
analysis of 2019-2020 data. Addiction October 21,
2020. [Online ahead of print] 10.1111/add.15295.
28. Rebalancing the “COVID-19 effect” on alcohol sales.
The Nielsen Company. May 7, 2020. Accessed
August 27, 2020. https://www.nielsen.com/us/en/
insights/article/2020/rebalancing-the-covid-19-effect-
on-alcohol-sales/.
29. Pollard MS, Tucker JS, Green HD Jr. Changes
in adult alcohol use and consequences during
the COVID-19 pandemic in the US. JAMA Netw
Open 2020;3(9):e2022942. 10.1001/jamanet-
workopen.2020.22942.
30. Clay JM, Parker MO. Alcohol use and misuse during
the COVID-19 pandemic: a potential public health
crisis? Lancet Public Health 2020;5(5):e259. 10.1016/
S2468-2667(20)30088-8.
31. Food expenditure series. United States Department of
Agriculture Economic Research Service. Last updated
June 2, 2020. Accessed October, 9 2020. https://www.
ers.usda.gov/data-products/food-expenditure-series/
food-expenditure-series/#Current%20Food%20Ex-
penditure%20Series.
32. Bann D, Villadsen A, Maddock J, et al. Changes in the
behavioural determinants of health during the corona-
virus (COVID-19) pandemic: gender, socioeconomic
and ethnic inequalities in 5 British cohort studies.
medRxiv 2020. 10.1101/2020.07.29.20164244.
33. Tracking the COVID-19 recession’s effects on food,
housing, and employment hardships. Center on Bud-
get and Policy Priorities. October 7, 2020. Accessed
October 13, 2020. https://www.cbpp.org/research/pov-
erty-and-inequality/tracking-the-covid-19-recessions-
effects-on-food-housing-and.
34. Rosenbaum D. Boost SNAP to capitalize on pro-
gram’s effectiveness and ability to respond to need.
Center on Budget and Policy Priorities. July 18, 2020.
Accessed October 9, 2020. https://www.cbpp.org/
research/food-assistance/boost-snap-to-capitalize-on-
programs-effectiveness-and-ability-to-respond.
35. Fernandez S. 230,000 Texas families led for SNAP
food assistance in March, twice as many as same
month last year. The Texas Tribune. April 13, 2020.
Accessed October 9, 2020. https://www.texastribune.
org/2020/04/13/texas-snap-applications-coronavirus/.
36. Owens MR, Brito-Silva F, Kirkland T, et al. Prevalence
and social determinants of food insecurity among
college students during the COVID-19 pandemic.
Nutrients 2020;12(9):2515. 10.3390/nu12092515.
37. Tison GH, Avram R, Kuhar P, et al. Worldwide effect
of COVID-19 on physical activity: a descriptive study.
Ann Intern Med 2020;173(9):767-70. 10.7326/M20-
2665.
20 PRIMARY CARE IN THE COVID-19 PANDEMIC
38. McCarthy H, Potts HWW, Fisher A. Physical activ-
ity behaviour before, during and after COVID-19
restrictions: a longitudinal smartphone track-
ing study of 5395 UK adults. J Med Internet Res
2021;23(2):e23701. 10.2196/23701.
39. Ong JL, Lau T, Massar SAA, et al. COVID-19 related
mobility reduction: heterogenous effects on sleep
and physical activity rhythms. Sleep 2020;zsaa179.
10.1093/sleep/zsaa179.
40. Bakshi S, Schiavoni KH, Carlson LC, et al. The es-
sential role of population health during and beyond
COVID-19. Am J Manag Care 2021;27(3). In press.
41. Mirsky JB, Horn DM. Chronic disease management in
the COVID-19 era. Am J Manag Care 2020;26(8):329-
30. 10.37765/ajmc.2020.43838.
42. Ambert-Pompey S, Konecky B, Ahlstrom D, Keefer
A. Improving access: team-based primary care via
telehealth in the VA. SGIM Forum. October 2017. Ac-
cessed January 29, 2021. https://www.sgim.org/File
Library/SGIM/Resource Library/Forum/2017/SGIM-
October-2017_02.pdf.
43. Reddy A, Gunnink E, Deeds SA, et al. A rapid
mobilization of “virtual” primary care services in
response to COVID-19 at Veterans Health Adminis-
tration. Healthc (Amst) 2020;8(4):100464. 10.1016/j.
hjdsi.2020.100464.
44. Myers US, Coulon S, Knies K, et al. Lessons learned
in implementing VA video connect for evidence-based
psychotherapies for anxiety and depression in the
Veterans Healthcare Administration. J Technol Behav
Sci 2020:1-7. [Online ahead of print] 10.1007/s41347-
020-00161-8.
45. Gfrerer JP. An innovative solution to support expand-
ed telehealth capability. Electronic Health Reporter.
September 29, 2020. Accessed January 29, 2021.
https://electronichealthreporter.com/an-innovative-
solution-to-support-expanded-telehealth-capability/.
46. Alley DE, Asomugha CN, Conway PH, Sanghavi DM.
Accountable health communities—addressing social
needs through Medicare and Medicaid. N Engl J Med
2016;374(1):8-11. 10.1056/NEJMp1512532.
47. Seligman HK, Laraia BA, Kushel MB. Food insecurity
is associated with chronic disease among low-income
NHANES participants. J Nutr 2010;140(2):304-10.
10.3945/jn.109.112573.
48. Gundersen C, Ziliak JP. Food insecurity and health
outcomes. Health Aff (Millwood) 2015;34(11):1830-9.
10.1377/hlthaff.2015.0645.
49. Charkhchi P, Fazeli Dehkordy S, Carlos RC. Housing
and food insecurity, care access, and health status
among the chronically ill: an analysis of the behavioral
risk factor surveillance system. J Gen Intern Med
2018;33(5):644-50. 10.1007/s11606-017-4255-z.
50. Sims M, Kershaw KN, Breathett K, et al. Im-
portance of housing and cardiovascular health
and well-being: a scientic statement from the
American Heart Association. Circ Cardiovasc
Qual Outcomes 2020;13(8):e000089. 10.1161/
HCQ.0000000000000089.
51. Brewster AL, Fleming M, Knox M, Roth A. Community
resilience for COVID-19 and beyond: leveraging a
system for health care and social services integra-
tion. Health Affairs Blog. August 12, 2020. Accessed
January 29, 2021. https://www.healthaffairs.org/
do/10.1377/hblog20200807.222833/full/.
PRIMARY CARE IN THE COVID-19 PANDEMIC 21
Addressing COVID-19
Proactively Through
Primary Care in
England’s National
Health Service
Azeem Majeed
H
ealth systems across the world have made radical changes to help manage the COVID-19
pandemic in their own countries.
1
As primary care is the patient’s rst point of contact with
the health system, these changes have had a dramatic eect on primary care services, including in
England’s National Health Service (NHS). Changes in how health services were provided had to be
implemented quickly once the scale of the pandemic that England was facing became apparent, and
the potential risks to both patients and primary health care sta became apparent.
Organization of primary care in England
Primary care in England is largely government-funded.
2
Every resident of England is able to reg-
ister with a general practice (irrespective of their immigration status), which then becomes their
rst point of contact for most health problems, and their gateway to investigations and referrals to
specialist services. There are no payments for consultations with professionals working in general
practice, such as general practitioners (primary care physicians), pharmacists, and nurses. Some
patients do pay a fee for their drugs (£9.15 per item, around $12). However, many groups of pa-
tients are exempt from this charge and only around 10% of prescriptions are issued to patients who
are required to pay.
Although private (paid-for directly by the patient) primary care services have increased in recent
years (mainly via online providers), the use of these services remains low. The vast majority of
England’s population remain registered with an NHS general practice, which is their sole or main
provider of primary care.
NHS general practices are largely funded through capitation payments from government, with only
a small proportion of income coming from other sources such as NHS quality incentive schemes,
pay-for-performance programs, and fee-for-service activities. During the turbulence caused by the
COVID-19 pandemic, with radical changes implemented in a very short period of time, this system
of funding has provided nancial stability for general practices. This was often not the case
for many primary care practices in the USA or elsewhere that are more reliant on fee-for-
service payments, and where there were often large reductions in income because of a decline
in the number of patient consultations.
3,4
Planning for the pandemic
The rst conrmed cases of COVID-19 in England were identied at the end of January 2020.
Cases increased during February, and by early March, it became apparent that England was
facing a large COVID-19 epidemic. This led to the Department of Health and Social Care and
NHS England (the bodies that respectively fund and manage the NHS in England) to recom-
mend radical changes to the provision of NHS primary care services to improve infection
control and increase remote consulting, and thereby reduce the risk of nosocomial infection.
For most general practices, these changes began to be implemented in the week beginning
March 16, 2020. As a rst step, general practices switched from the traditional model of face-
to-face service provision to one where all patients were initially assessed through a telephone
or video call. Patients were encouraged to register for online booking of these appointments
if they had not already done this. All patients requesting advice spoke rst to a health profes-
sional, usually general practitioners but sometimes primary care nurses or pharmacists. The
aim was to deal with as many queries as possible by telephone or a video call. Patients who
after this remote assessment then required a face-to-face appointment were booked to be
seen later that day wherever possible. This ensured that patients were largely managed on
the same day they sought medical advice. These changes resulted in around three-quarters
of patients being managed remotely during the earlier part of the pandemic; in contrast, at
the same time in 2019 only around one-quarter of patients were managed remotely. The total
volume of primary care activity (as measured by the number of consultations) also fell by
about 25%.
5
In subsequent months, there was a gradual increase in primary care activity and
also an increase in the proportion of activity that was carried out using face-to-face consul-
tations, as consulting patterns began to return to a more normal mode of delivery.
Patients with symptoms that may have been due to COVID-19 infection were usually seen in
dedicated respiratory clinics in general practices with the general practitioner wearing per-
sonal protective equipment (PPE). By early April, wearing PPE had become standard practice
for all face-to-face consultations because of concerns about exposure to patients with asymp-
tomatic infection. In an attempt to keep general practices clear of patients with COVID-19,
most parts of England also began to set up dedicated “primary care COVID-19 hubs.”
These hubs served a network of general practices in a locality and saw patients with suspected
COVID-19 infection who needed face-to-face assessment (for example, because of a prolonged
illness or a deterioration in their clinical state). In some areas of England, COVID-19 home
visiting services were also put in place by the NHS to see patients at home who would nd it
dicult to travel to a hub, or for whom hospital admission was inappropriate. Finally, some
primary care providers have also developed mobile oxygen saturation monitoring, where a
member of sta is deployed to obtain a rapid reading from a patient at home. This is used
24 PRIMARY CARE IN THE COVID-19 PANDEMIC
when oxygen saturation level may be the only discriminator of serious illness, such as in
silent hypoxia.
Information technology in primary care
For many years, the NHS has been investing to improve information technology in primary
care. Changes during the pandemic were greatly helped by this existing information technol-
ogy infrastructure. This includes full computerization with all NHS general practices using
electronic medical records; online access for patients to services such as appointment book-
ing, ordering repeat prescriptions, and viewing medical records; and the NHS Electronic
Prescription Service, whereby a prescription can be sent electronically by the physician to a
pharmacy of the patient’s choice anywhere in England. This electronic prescription service
was very helpful for general practitioners and patients, as it soon became apparent that many
people had moved away from their usual locations, particularly from large urban centers such
as London, to be closer to their families when the country went into lockdown in March 2020.
The full computerization of NHS primary care also allows primary care physicians to work
remotely from their main clinical site (usually from their home) but still have the ability
to obtain access to medical records, order investigations, and issue prescriptions. This has
allowed primary care physicians who are unable to work in clinical settings to continue to
oer telephone and video consultations from home, and to review the results of laboratory
tests and letters from specialists and other agencies. This is important for older physicians,
physicians who are pregnant, and physicians who have a medical problem that places them
at increased risk of complications and death from COVID-19. It also means that physicians
who are “self-isolating” because either they or a household member had tested positive for
COVID-19 could continue to work during their quarantine period. Without the arrangements
for remote working, facilitated by the previous investment in information technology, the
number of appointments available in general practice would have fallen substantially, as there
were periods when many doctors were unable to work from their practices. This was particu-
larly the case earlier in the pandemic when infection rates were very high and the capacity
to carry out polymerase chain reaction (PCR) antigen tests was low, resulting in many NHS
workers having to isolate because of inability to obtain an antigen test.
To help cope with the demand for advice from patients with symptoms of suspected COVID-19
infection, primary care teams were supported by the NHS 111 service.
6
This is a free to access,
nationally available service whereby patients can seek medical advice either by telephone or
online. The NHS 111 service has played a key role in advising patients and in limiting demands
on primary care and specialist services. Legal requirements around sharing data were also
changed to make it easier to share medical information between dierent NHS organizations.
COVID-19 was also made a notiable disease, placing a legal obligation on doctors to report
cases to public health agencies to support isolation of patients and contact tracing. An online
portal was also established to allow patients to book COVID-19 tests directly without going
through their physician. However, although this system allowed patients to book COVID-19
PCR tests directly and thereby reduce the need for input from a general practitioner, there
PRIMARY CARE IN THE COVID-19 PANDEMIC 25
were complaints from many general practitioners that they were unable to order tests for
their patients and instead had to direct patients to the online portal.
Reducing regulatory requirements
To further free up the time of primary care teams, some of the regulatory requirements for
general practices were relaxed. This included assessments of general practices by the Care
Quality Commission, which assesses quality of NHS services, and the suspension of annual
appraisals and revalidation for doctors. Rules around certifying death and completing death
certicates were also modied to reduce the workload of physicians. At the same time, the
income of NHS general practices has been protected to ensure they do not face nancial
pressures that threaten their viability. Later in the pandemic, the NHS began to reimplement
some of the regulatory requirements, such as inspections of general practices by the Care
Quality Commission, leading to tensions with doctors when the number of COVID-19 cases
began to increase again from September 2020 onward.
Optimizing clinical care
To support the management of patients, the National Institute for Health and Care Excellence
(NICE) published guidance on the management of patients with suspected COVID-19 infection
in the community.
7
There have also been tools developed for remote monitoring of patients.
However, concerns remain that some patients with COVID-19 infection in the community are
not being adequately monitored, leading to adverse outcomes and deaths for some patients.
8
New guidance is now also being developed on the management of patients with “long COVID”
to improve the care of people with long-term symptoms such as lethargy, breathlessness, and
mental health problems following a COVID-19 infection.
The second wave
The lockdown measures introduced across England and the other countries of the UK in late
March eventually led to a decline in cases, and by the summer, during the months of July
and August, COVID-19 cases were at a relatively low level. Unfortunately, during September
2020, case numbers began to increase, and by October, it was clear that the UK was facing a
large second wave of COVID-19 infection. Many of these cases were initially amongst students
and young people, but cases then began to spread to more vulnerable groups. This led to
another lockdown being introduced across England in early November. Genomic analysis of
the circulating strains of SARS-CoV-2 in the UK showed that around 80% were from a strain
of coronavirus that originated in Spain. This suggests that a key factor in the second wave of
COVID-19 in the UK was importation of infection by UK nationals returning from holidays in
Spain. The relaxation of overseas travel restrictions during the summer months and the lack
of a period of quarantine after return from holiday, and without antigen testing at airports,
contributed to the spread of infection across the UK. This was further compounded by a new,
more infectious strain of SARS-CoV-2 that began to circulate across England in the later part
26 PRIMARY CARE IN THE COVID-19 PANDEMIC
of 2020 and which soon became the predominant strain in circulation. By late December 2020
and in January 2021, the daily number of cases often exceeded 50,000, placing a major strain
on testing and contact tracing service and on NHS primary care and specialist providers.
Nursing homes
One group of people who were very badly aected by the COVID-19 pandemic were people
living in nursing homes (referred to as “care homes” in the UK). Currently, in the UK around
416,000 people live in nursing homes. They are generally older and frail, with high levels of
multimorbidity, and also have a high prevalence of dementia. Early in the pandemic, the NHS
aimed to increase bed capacity for acutely ill patients in hospitals. This led to the rapid trans-
fer of patients from hospitals to nursing homes, often without any test for COVID-19 before
discharge. Once in a nursing home, COVID-19 invariably spread quickly among the residents,
leading to high levels of morbidity and mortality. Policy on testing has now changed and
patients require two negative antigen tests before they can be discharged from a hospital to
a nursing home. There is also now more regular testing of the residents and sta of nursing
homes, but these changes were implemented too late in the pandemic to prevent a large death
toll among the residents of nursing homes.
National vaccine program
With the failure of the United Kingdom to suppress COVID-19 through an eective “test,
trace, and isolate” policy —in contrast to countries such as South Korea, New Zealand, and
Taiwan—it became clear that the most likely way for the UK to exit the pandemic was
through a vaccine program. This would rely on a safe and eective vaccine being devel-
oped, receiving approval from the pharmaceutical regulatory agency in the UK (Medicines
& Healthcare Products Regulatory Agency, MHRA), and then being delivered at scale to the
population of the UK. The rst vaccine to come near to approval was one produced by the US
company Pzer and the German company BioNTech, which is administered as two separate
doses. Later on, two additional vaccines, from AstraZeneca and Moderna, were also approved
for use in the UK.
In November 2020, general practices across England received guidance on how the vaccine
program would run, once regulatory approval had been obtained, with a proposed start date of
early December. General practices across England were asked to work in groups and to set up
vaccine clinics that would run for 12 hours per day, seven days per week to administer the 40
million doses of the Pzer-BioNTech vaccine that had been secured by the government. The
expectation was that there would be around 1,500 vaccination sites in England. Each vaccina-
tion will generate a fee of £12.58 ($16.60) for the practice. Target groups in the rst wave of
the vaccination program would include people living in nursing homes, followed by people
aged 80 years and over and NHS sta. The speed of implementation and scale of the vac-
cine program illustrates how England’s publicly funded NHS can respond to an urgent public
health crisis.
PRIMARY CARE IN THE COVID-19 PANDEMIC 27
Challenges
Primary care in England has faced serious challenges arising from the COVID-19 pandemic,
not all of which have yet been addressed. From the perspective of patients, the online and
telephone advice service, NHS 111, was initially overwhelmed by patient requests, resulting in
long wait times to obtain advice and with concerning reports that some ill children may have
been wrongly advised to stay at home, resulting in signicant harm.
9
Additionally, the remote
consultation model for routine primary care, whilst oering safe and timely assessment for
many patients, may also result in worsening health inequalities for patients who are not
technologically literate, patients who have hearing impairment or mental health problems, or
patients for whom English is not their rst language.
The implementation of the “COVID-19 primary care hubs” has been patchy, with services
slow to develop in many parts of England and a perception of a lack of clear central guidance.
In some areas where hubs are operational, utilization was often relatively low, indicating
that the model may not be functioning at the capacity that was planned for. This has led to
the closure of some hubs and also of home visiting services, with responsibility for managing
patients with suspected COVID-19 infection being passed back to general practices. Finally,
guidance to cease nonessential care for patients—such as physiotherapy, radiology services,
cervical screening, and spirometry—has the potential to lead to delayed diagnoses and poorer
health outcomes, and exacerbate existing health disparities.
10
Statistics published by NHS
England, for example, show that the number of people waiting for more than one year for
hospital treatment increased from 1,600 at the start of 2020 to 140,000 by September 2020,
with further increases expected during the winter of 2020-2021.
Primary care sta have also not been immune to diculties. Most notably, the quality and
availability of PPE was an issue particularly in the earlier part of the epidemic, endangering
sta health and potentially reducing the quality of care for patients.
11
Many general prac-
titioners have died from COVID-19 infection in England, and this has further exacerbated
concerns about PPE in primary care. Testing for sta who are self-isolating with symptoms
of COVID-19 has been dicult to access, meaning that sta who feel well enough to attend
work must stay at home due to mild symptoms that may not be COVID-19. This is now be-
ing addressed through an expansion in testing capacity for acute COVID-19 infection, as well
as by supplying rapid testing (lateral ow) kits to primary care sta for self-testing twice
weekly. However, testing capacity remains limited in England, as does contact tracing, both
of which are core elements of global strategies to control COVID-19.
12
Finally, the leadership
of the COVID-19 response in the UK was very fragmented with, for example, many dierent
government agencies involved and dierent public health policies in place in the four coun-
tries of the UK (England, Wales, Scotland, Northern Ireland) because of the devolved nature of
our government.
13
28 PRIMARY CARE IN THE COVID-19 PANDEMIC
Conclusions
We have seen rapid changes in primary care in England in response to the COVID-19 pan-
demic; but challenges remain, particularly if the number of people with COVID-19 infection
increases rapidly and starts to overwhelm the health system during the current second wave,
or if subsequent waves of infection occur.
14
Other challenges include providing medical care
for people who are self-isolating at home because of their age or because of underlying medi-
cal problems that increase their risk of complications and death if they contract a COVID-19
infection. There are also problems that will arise from the cutting back of many specialist
hospital services, which will have negative eects on health outcomes if restrictions in health
services remain in place for a prolonged period. This will particularly be the case for people
from poorer communities.
Overall, primary care in England has responded well to the COVID-19 pandemic, making
radical changes to how primary care services are delivered in a very short period of time.
Key to allowing this to happen is the commitment by the UK government to support general
practices nancially to prevent the loss of income that has occurred to primary care practices
in countries such as the USA. However, the future will remain challenging for primary care
teams in England until such time as a vaccine can be administered on a sucient scale to
nally bring COVID-19 under control and allow for a return to a more normal society.
15
References
1. Anderson RM, Heesterbeek H, Klinkenberg D, Hol-
lingsworth TD. How will country-based mitigation
measures inuence the course of the COVID-19
epidemic? Lancet 2020;395(10228):931-4.
2. Majeed A, Molokhia M. Primary care in the United
Kingdom. Journal of Ambulatory Care Management
2008;31(3):198-200.
3. Levey NN. Coronavirus already changing medical
care in the U.S. Los Angeles Times. April 10, 2020.
https://www.latimes.com/politics/story/2020-04-10/
coronavirus-lasting-changes-healthcare.
4. Kamerow D. COVID-19: Don’t forget the impact on
US family physicians. BMJ 2020;368:m1260.
5. Campbell D. Only one in four GP appointments now
conducted in person. The Guardian. April 19, 2020.
https://www.theguardian.com/society/2020/apr/19/tech-
revolution-only-one-in-four-seek-face-to-face-gp-visits.
6. Potential coronavirus (COVID-19) symptoms reported
through NHS Pathways and 111 online. https://digital.
nhs.uk/data-and-information/publications/statistical/
mi-potential-covid-19-symptoms-reported-through-
nhs-pathways-and-111-online/latest.
7. National Institute for Health and Care Excellence.
COVID-19 rapid guideline: managing suspected or
conrmed pneumonia in adults in the community.
National Institute for Health and Care Excellence.
COVID-19 rapid guideline: managing suspected or
conrmed pneumonia in adults in the community.
NICE Guideline [NG165]. April 23, 2020. Accessed
January 19, 2021. https://www.nice.org.uk/guidance/
ng165.
8. Giles C. UK coronavirus deaths more than double
ofcial gure, according to FT study. Financial Times,
April 22, 2020. https://www.ft.com/content/67e6a4ee-
3d05-43bc-ba03-e239799fa6ab.
9. Royal College of Paediatrics and Child Health. De-
layed access to care for children during COVID-19:
our role as paediatricians—position statement. April 3,
2020. Accessed January 19, 2021. https://www.rcpch.
ac.uk/resources/delayed-presentation-during-COVID-
19-position.
10. Coronini-Cronberg S, John Maile E, Majeed A.
Health inequalities: the hidden cost of COVID-19 in
NHS hospital trusts? J R Soc Med 2020;113(5):179-
84.10.1177/0141076820925230.
PRIMARY CARE IN THE COVID-19 PANDEMIC 29
11. Majeed A, Molokhia M, Pankhania B, Asanati K.
Protecting the health of doctors during the COVID-19
pandemic. Br J Gen Pract 2020;70(695):9.
10.3399/bjgp20X709925.
12. Pollock AM, Roderick P, Cheng KK, Pankhania B.
COVID-19: why is the UK government ignoring
WHO’s advice? BMJ 2020;368:m1284.
13. Majeed A. The impact of COVID-19 on academic
primary care and public health. J R Soc Med 2020;
113(8):319.10.1177/0141076820947053.
14. Majeed A, Maile EJ, Bindman AB. The primary
care response to COVID-19 in England’s National
Health Service. J R Soc Med 2020;113(6):208-210.
10.1177/0141076820931452.
15. Majeed A, Molokhia M. Vaccinating the UK against
COVID-19. BMJ 2020;371:m4654.
30 PRIMARY CARE IN THE COVID-19 PANDEMIC
What We Can Learn
from European
Experiences of Primary
Care Under COVID-19
Selina Rajan, Jonathan Cylus, and Martin McKee
A
lthough a global pandemic caused by a respiratory virus was highly predictable, outside the
countries of South and East Asia that had recent experience of SARS, few countries were pre-
pared for the worldwide spread, in 2020, of the SARS-CoV-2 virus. The rst identied cases of
COVID-19 in Europe occurred in northern Italy, brought by a traveler from China.
1
Within weeks,
television screens across the world were lled with pictures of hospitals in Italy struggling to cope
while the graphs of cases and, soon after, deaths rose rapidly. In health ministries across Europe
there was a growing sense of panic. But what were they to do? Although, as the editor of The Lancet
has pointed out, Chinese scientists had been publishing warnings and sharing their experiences
in the pages of this journal, few seemed to have noticed and, if they did, they were unable to act
quickly enough.
The rst problem was a lack of understanding about how the virus was transmitted. Many
European scientic advisers, trapped within a mindset shaped by the experience of pandemic
inuenza, found it dicult to adjust to a dierent threat. The initial advice focused on spread by
droplets and fomites, with the resulting advice focusing on handwashing, deep cleaning of facilities
where cases have occurred, and social distancing. It took quite some time to incorporate the evi-
dence emerging from Asia on the role of aerosol transmission, especially in the absence of symp-
toms and, in particular, the importance of face coverings to reduce transmission.
The second problem in many European countries was a failure to act early. In some cases, this
was due to a reluctance to take measures on the scale seen in China to reduce population mixing,
in part because of the unspoken assumption that such measures would not command widespread
public acceptance in what they considered was a very dierent political and social situation in
Europe. In some countries, such as the United Kingdom and Spain, it also reected weaknesses in
the political process, in the former case, because the prime minister was distracted by its attempts
to leave the European Union and his personal problems
2
and in the second because of tensions be-
tween the central government and the regions. The result was that infections spread rapidly, with
mixing in ski resorts playing a major role as returning vacationers seeded infections across much
of Western Europe. Countries in central Europe had, however, reacted quickly, perhaps because the
memory of severe outbreaks of infectious diseases such as tuberculosis (TB) persisted more
strongly in their public health systems but also likely because they experienced fewer im-
ported cases initially. As a consequence, they were relatively spared in the rst wave.
Inevitably, health services have been on the front line of the response to the pandemic in all
European countries. However, the focus has been very much on the hospital sector. Initially,
and again reecting the misunderstanding of the nature of this new disease, COVID-19 was
seen as another viral pneumonia. Those getting hospitals ready focused on the provision
of ventilators and personal protective equipment (PPE) for hospital workers. Only later did
it become clear that this was a complex multisystem disease requiring the input of many
specialties.
3
By this time, however, almost all countries had imposed severe restrictions on
movement, closing down public transport and all but essential services. This also meant stop-
pages of nonurgent health care, including primary care, and limited availability of services for
patients with milder presentations of COVID-19. Later it was recognized that this virus was
being transmitted primarily in settings where large numbers of people were mixing, in close
proximity, for prolonged periods of time. Obviously, this included hospitality venues, such as
bars and restaurants, but also care homes and, potentially, waiting rooms in primary care fa-
cilities that attracted people who were ill, at least some of whom would be likely to be spreading
the virus, even if not showing symptoms of COVID-19, in areas where the prevalence was high.
The consequences were predictable. First, people who became ill, whether with COVID-19 or
something else, found themselves unable to access care (in primary care or hospital settings)
and, even if they could, many were reluctant to expose themselves to the risk of infection.
The increasing numbers of health workers who were becoming infected, sometimes requir-
ing hospital admission and, in some cases, dying,
4
served as a daily reminder of the risks
involved. Second, those providing health care had to nd new ways of meeting the needs of
those requiring care. Primary care providers did this in two ways: by segregating the path-
ways taken by patients suspected of having COVID-19 from those with other conditions, and
by introducing remote consultations.
The rst of these approaches, having separate pathways, was already being used in many
Asian countries, with health facilities redesigned in the aftermath of SARS. However, it was
more dicult to do in Europe, given the impossibility of undertaking major construction in
the midst of a pandemic, requiring many to separate patients with symptoms of COVID-19
by either time or space. For example, in Bulgaria an ordinance from the Ministry of Health
mandated that on Tuesdays and Thursdays GPs could provide only maternal and child consul-
tations and compulsory vaccinations without admitting other patients.
The second approach, remote consultations, should have been much easier. In the preced-
ing years, there had been enormous advances in online platforms. In other sectors of society,
individuals and organizations had made the transition to online meetings, using software
such as Zoom, Skype, FaceTime, or Teams, with relative ease. Over a relatively short period of
time a new online etiquette developed and, although not without its problems, this new way
of working was soon accepted as having many advantages, not least the ability to avoid time-
consuming and often uncomfortable journeys to meetings.
32 PRIMARY CARE IN THE COVID-19 PANDEMIC
However, there was much more reluctance to embrace these new approaches in the delivery
of health care and, in many countries, the vast majority of patient contacts were conducted
face-to-face prior to the pandemic. There were a number of reasons. First, there was a sense
that they could not replace the physical interaction between health professional and patient,
even in consultations where no examination was required. Second, especially in health sys-
tems based on a fee-for-service model, there were questions about how health workers would
be remunerated.
In the remainder of this chapter, we will review what is known about changes in utilization
of primary care in Europe and how providers of primary care have adapted to the new situa-
tion, drawing extensively on the European Observatory’s COVID-19 Health System Response
Monitor.
5
We conclude by looking to the future, asking which of these adaptations are likely
to continue after the pandemic is over, and what the implications for primary care services
are of a growing number of people who have experienced persisting symptoms following
infection, suering from what is now termed long COVID.
Impact on consultations
Although there are widespread reports of declines in utilization of primary care in European
countries since the beginning of the pandemic, there is little evidence to quantify its scale.
This is in contrast with the growing number of studies that have looked at reductions in, for
example, admissions with acute coronary syndrome,
6-9
access to cancer services,
10
and emer-
gency department attendances.
11,12
Moreover, those published reports on changes in primary
care are predominantly from one country, the United Kingdom. One study, undertaken in a
single general practice in England, reported a reduction of 92.5% in face-to-face consulta-
tions in the two weeks before and two weeks after national guidance was issued to reduce these
consultations. The number of telephone consultations increased by 85.6% in the same period.
The proportion of people living in the most deprived areas who consulted before and after the
change did not dier.
13
Among 47 general practices in a deprived part of northern England, be-
tween 16% and 50% reported a reduction in primary care consultations for circulatory disease,
common mental health problems, type II diabetes, and cancer between March and May 2020
compared to what would have been expected based on data over the preceding decade.
14
Another study, in the Oxford region of England, examined consultations by patients aged 65
years and over between February and May 2020.
15
The rate of telephone and video consulta-
tions increased by just over 100%, while face-to-face consultations fell by 65% and home
visits by 63%. Among those consulting, whether face-to-face or remotely, a much higher
proportion of the total comprised those taking 10 or more medicines, or with high levels of
frailty. As in the study from northern England, the change was extremely abrupt, coinciding
with the changing national guidance. The most extensive study analyzed records of almost 10
million individuals participating in the English Clinical Practice Research Datalink database.
It found dramatic reductions in primary care contacts for all conditions after the introduc-
tion of restrictions on movement. By July 2020, none, except for unstable angina and acute
PRIMARY CARE IN THE COVID-19 PANDEMIC 33
alcohol-related events, had recovered to the previous level. The largest reductions were the
contacts for diabetic emergencies, depression, and self-harm, all of which fell by 50% or more.
16
The few studies from other parts of Europe paint a similar picture. A study of attendances at
Belgian primary care out-of-hours centers reported an initial increase in attendances fol-
lowed by a dramatic decline. However, while there were no telephone consultations in previ-
ous years, in 2020 these comprised 40% of the total.
17
In France, a similar decline was noted
during the rst wave, with 80% fewer visits to dentists, 40% fewer visits to physiotherapists
and midwives, and 30% fewer to general practitioners.
5
A look at Finnish data from the
spring of 2020 also showed that visits to child health and maternity care clinics decreased by
between 10% and 40%, while school health care visits fell by 60% to 80% compared to the
previous year. The Finnish permanent secretary of the Ministry of Social Aairs and Health
stated on April 28, 2020, that “what is more worrying than the adequacy of intensive care
capacity at the moment is the ability of our health care and social welfare system to respond
to service needs other than those associated with the Coronavirus.”
5
Impact on health
The initial fall in primary care consultations also had wider health system impacts, leaving
around 2.1 million people in the UK waiting for cancer-screening tests in June 2020, with
urgent referrals dropping to around 25% of usual levels in England at the start of the pan-
demic.
18
Similarly, in April 2020 there were 10,792 patients who had been urgently referred to
cancer services but were still awaiting treatment, compared with 13,147 in April 2019.
19
Over
three weeks in May, the World Health Organization conducted surveys in 155 countries and
reported that COVID-19 had dramatically curtailed the provision of health services for non-
communicable diseases, noting a 25% drop in new cancer diagnoses in the Netherlands since
the pandemic lockdown began.
20
Childhood vaccination uptake was also aected, with measles, mumps, and rubella vaccine
uptake falling by 20% during the rst three weeks of the lockdown in England.
21
Though
these are now believed to have returned to prepandemic levels, a similar pattern was observed
in other European countries, such as Finland, where it was attributed to the reduction in
services during lockdown and a reluctance among parents to vaccinate.
5
Meanwhile, despite fewer patients presenting to primary care for self-harm, one in ve
people reported experiencing thoughts of suicide or self-harm in the rst months of lock-
down, with one in twenty actually harming themselves, according to a representative survey
of nearly 45,000 adults in the UK.
22
Most recently, the ambulance service in London reported
an increase in the number of suicides and attempted suicides they attended at the end of
October compared to previous years.
23
While it is too early as yet to decipher the long-term impacts of the pandemic on health,
quality of life, or health care costs, Finland has led by example by commissioning an impact
assessment of the eects of the fall in primary health care access.
5
34 PRIMARY CARE IN THE COVID-19 PANDEMIC
Responding to the pandemic
In many European countries, the COVID-19 response has focused on the public health opera-
tions of testing and tracing, and on the response within hospitals. In some countries, such as
the United Kingdom, primary care was bypassed in the initial response,
24
as was the existing
public health service in local government, although in others, such as France, existing prima-
ry care providers played an important role in facilitating testing. Indeed, patients who experi-
enced COVID-19 symptoms were instructed not to attend primary care centers and to manage
their care at home unless their health deteriorated. Instead, the government contracted with
a number of large outsourcing corporations who set up their own testing operations. General
practitioners were not even able to order COVID-19 tests. As with many of these outsourcing
exercises over the past decade, these have been spectacular failures. But, once the contracts
are set, it is dicult to change them, especially as they lack any eective penalty clauses. In
some countries despite a long-standing emphasis on strengthening primary care, primary
care providers were not the rst point of contact for suspected COVID-19 cases.
Conversely, in some European countries, such as Albania, Armenia, Bulgaria, Croatia, the
Czech Republic, and Germany (to name a few), primary care was the rst point of contact,
responsible for assessing patients with symptoms and ordering and interpreting tests, with
many also involved in ongoing patient surveillance and, when necessary, facilitating ad-
mission to hospital and subsequent convalescence.
5
This is of course not without capacity
constraints, and primary care services in France conducted about 42,000 consultations for
suspected COVID-19 in week 12 of 2020 alone
5
; primary care sta were also actively involved
in contact tracing in some countries, such as Belgium, France, and Ukraine.
5
To avoid over-
burdening primary care, many countries, such as Belgium, the Czech Republic, Finland,
Denmark, and the UK, also set up telephone hotlines for the general public to access the latest
guidance and in some cases order tests. Embracing technology, Bulgaria also introduced a
chatbot, while Estonia introduced robotic contact tracers to call contacts of COVID-19 cases.
5
With growing fears of a “twin-demic,” many countries also stepped up their eorts to pro-
mote inuenza vaccinations ahead of the second wave of COVID-19, adding pressure to pri-
mary care to see more patients face-to-face. In Germany and Ireland, for example, additional
funding has been allocated to primary care for this purpose, with the United Kingdom also
expanding the eligibility criteria and funding vaccinations to all those over the age of 50.
Adaptations to COVID-19
In the early days of the pandemic, primary care providers in some countries looked for ways
to keep people with possible COVID-19 separate from others. In England, for example, some
general practices established what were termed “hot hubs,” single designated areas or sur-
gery to manage patients with suspected or conrmed COVID-19, with sta wearing full PPE.
25
Similar adaptations were made in Greece and Germany
5
as well as triage centers in Belgium,
where groups of general practitioners came together to create “corona centres.”
26
Another
innovation was the creation of ambulatory care pathways in Germany, where over 85% of
PRIMARY CARE IN THE COVID-19 PANDEMIC 35
COVID-19 cases were seen in ambulatory settings, which included fever ambulances, staed
with medical students to follow up COVID-19 patients in the community. This shift toward
community-centered care as a means to decrease nosocomial contagion has been seen previ-
ously for TB and is becoming increasingly popular in other countries, including Italy
27
and
now the UK,
28
with the imminent rollout of the NHS health at home service, including remote
pulse oximetry. Other countries, such as Croatia, shifted toward more primary care visits at
home, provided the household had not been exposed to COVID-19.
Remote consultations also became increasingly common—for example, in Greece, Hungary,
Ireland, France, and particularly Estonia, where the share of remote consultations rose 1.8
times in March compared to February.
5
This shift in the locus of care in some countries re-
quired changes in the way providers were paid. A number of countries, like Denmark and
Estonia, introduced higher fees for remote consultations and/or loosened restrictions on
reimbursing such consultations (the Czech Republic, Germany, Luxembourg, the Netherlands,
Sweden, Switzerland). The intention was to both incentivize care and shore up provider in-
comes, since some experienced signicant declines in revenues due to changes to the volume
of face-to-face care. In England, GPs were reimbursed for improving their IT capacity.
Particularly valuable insights can be obtained from a qualitative study of general practitioners
in Belgium, conducted by medical students who were unable to complete their internship as
normal.
26
They identied six themes.
The rst theme related to changes in the management of patients. General practitioners
described how primary contact with patients was now by telephone. Anyone with respiratory
symptoms was referred to the triage centers mentioned earlier. There were mixed views about
the impact on workload. The general practitioners reported seeing fewer patients but hav-
ing a greater administrative workload. They also described how their workload had become
more structured, with a greater division of tasks among the primary care teams. Nurses, in
particular, had taken on a greater role in triage. Importantly, in a health system that had been
characterized by individual practices working separately, there was much greater collabora-
tion, including pooling of resources. These changes were facilitated by the health insurance
fund agreeing to reimburse telephone consultations, something that was not possible previ-
ously. Some also changed the way that income within the practices was distributed, pooling
the fee-for-service payments among the general practitioners and redistributing them ac-
cording to the number of shifts worked. They also reported easier access to specialist advice
as hospital doctors were no longer spending time in outpatient clinics.
A second theme related to person-centered care. General practitioners highlighted the con-
straint imposed by the loss of nonverbal cues during remote consultations, as well as commu-
nication diculties in dierent languages and across cultures. However, problems also arose
as a result of the constraints imposed by wearing PPE, including the diculty of showing
empathy during such consultations. They reported their consultations were much easier with
patients with whom they were familiar.
The third theme related to their problem-solving ability, with a range of problems interven-
ing. These included the diculty of undertaking simple physical examinations, such as pulse
36 PRIMARY CARE IN THE COVID-19 PANDEMIC
rates, reduced access to specialized diagnosis, and delays in diagnosis as a result of reduced
attendance by patients.
The fourth related to the reduction in some aspects of care. These included care for people
living in nursing homes, which had been taken over by a dedicated physician rather than
the general practitioners who had previously continued to care for their patients before their
admissions, as well as cancer screening, which had been suspended.
The fth related to the traditional role of Belgian general practitioners in certifying sickness
absence. As they could no longer examine patients, they felt that they were acting as, in ef-
fect, a rubber stamp.
The nal theme related to concerns about the wider socioeconomic impact of COVID-19 in
their own ability to protect themselves in a situation where they faced shortages of PPE.
There is another important way in which primary care is likely to change. It is now appar-
ent that many people who have been infected with SARS-CoV-2 continue to have symptoms.
Although it is dicult to know how long this will persist, there is enough evidence that there
may be a substantial number of people aected. Many are likely to require primary care into
the future. The condition, referred to as long COVID, may aect up to 10% of those who have
been infected. One recent study suggested that there are two broad symptom complexes, one
characterized by fatigue, headaches, and respiratory symptoms, and another that adds multi-
system involvement, including of the cardiovascular, neurological, and renal systems.
3
Greenhalgh and colleagues have assembled the available evidence to produce guidance for the
management of this condition in primary care.
29
They note that many patients recover spon-
taneously, although slowly, with support, rest, and a gradual increase in activity. However,
they recommend specialist assessment if there is concern about lung, heart, or neurological
symptoms that are new, persistent, or progressive. Laboratory investigations are primarily to
exclude other disorders that may be giving rise to the symptoms or to assess inammatory
and prothrombotic states. Otherwise, treatment is largely directed at relief of symptoms. They
stress the importance of paying attention to the patient’s mental health, including advice on
support in the community, as well as their social and nancial situation.
Looking beyond the pandemic
As the preceding sections have shown, the day-to-day work of primary care has changed
remarkably in many countries. In some ways, this has had a clear adverse impact on the
quality of care. Thus, the decline in attendance is storing up many problems for the future,
with delayed diagnoses and failure to identify progression and complications of chronic
diseases. Remote consultations preclude many of the human interactions, including demon-
stration of empathy, that serve to build trust between patients and health professionals. On
the other hand, both rural consultations and increased use of online services, such as ordering
of electronic prescriptions, are consistent with how people increasingly live their lives, with
in-person work meetings taking place by video conference and shopping online. For many
busy people, an alternative to traveling to a surgery to spend time in a crowded waiting room
PRIMARY CARE IN THE COVID-19 PANDEMIC 37
for a ve-minute appointment will happily be consigned to history. Many have argued that
these changes should have taken place long ago, but their eorts have foundered in the face
of professional opposition. COVID-19 has changed this, although some patients have been
angered at the reduced access to face-to-face appointments.
30
It is futile to argue against the
virus. Prediction is always dicult, but it does seem very unlikely that the model of primary
care that existed until now will remain unchanged in the future.
Although the evidence is limited (itself a sad commentary on the capacity for research in
primary care), in many European countries, it is clear that primary care providers played little
direct role in the response to the pandemic. This should not distract from the major achieve-
ments in transforming their mode of practice. However, it does represent a missed opportu-
nity. If they are to play a greater role in the future, there are a number of measures that could
be taken.
First, testing should be made accessible to general practitioners for patients presenting with
symptoms of COVID-19. Ideally, these should be rapid point-of-care tests to facilitate rapid
triage in the community.
Second, to facilitate early access to care, general practitioners require timely access to and
funding for adequate and eective PPE. Determining who is responsible for the allocation of
PPE in primary care (e.g., whether it is the providers themselves or local decision makers)
can have important consequences for whether there is sucient availability where it is most
needed.
Third, although remote consultations have increased, 57% are still conducted face-to-face
in the UK,
31
where more than half of general practitioners also report that they now see more
patients for longer each day, resulting in increased exhaustion,
32
highlighting the need to
train and recruit additional sta to cope with future need. A high priority will be to ensure
that disadvantaged and vulnerable groups with less access to and familiarity with technol-
ogy will not face barriers to accessing primary care going forward as shifts to telemedicine
become the new normal.
Fourth, there is a need to ensure that exible payment structures are in place to ensure that
general practitioners can provide universal access to care to all communities, including the
most vulnerable in long-term care. While exible payment structures have been implemented
in many European countries, including Belgium, Croatia, the Czech Republic, Denmark, and
France, it was by no means universal.
Fifth, structural changes will be required to facilitate regular cleaning, to account for the
need for separate entrances for infected patients, and to incorporate telemedicine in its broader
sense—including, for example, Bluetooth-assisted stethoscopes and ECGs—into routine practice.
Finally, the events of the past year have highlighted the importance of data sharing, and it is
crucial that any future system is built on a robust system of transparent data that is shared
quickly between primary and secondary care and public health professionals.
38 PRIMARY CARE IN THE COVID-19 PANDEMIC
Conclusions
The COVID-19 pandemic has revealed opportunities to transform primary care services across
Europe, but has also created many new and unprecedented challenges, which require care-
ful planning. It is clear that focused catch-up programs will be required to resume routine
vaccinations, cancer screening, and urgent referral and treatment programs to their previous
levels. Although a number of solutions have already been identied, including the expansion
of remote consultations, it is also clear that this is not a panacea and structural changes will
be required in the future to strengthen resilience in primary health care, including workforce
expansion, reinforced infrastructure, and data connectivity.
References
1. Malara A. Diagnosing the rst COVID-19 patient in
Italy–Codogno, Italy 2020. https://www.escardio.org/
Education/COVID-19-and-Cardiology/diagnosing-the-
rst-covid-19-patient-in-italy-codogno.
2. Calvert J, Arbuthnott G, Leake J. Coronavirus: 38
days when Britain sleepwalked into disaster. The
Times. April 19, 2020. Accessed November 1, 2020.
https://www.thetimes.co.uk/article/coronavirus-
38-days-when-britain-sleepwalked-into-disaster-
hq3b9tlgh.
3. Roberts CM, Levi M, McKee M, et al. COVID-19:
a complex multisystem disorder. Br J Anaesth
2020;125(3):238-42. [Online ahead of print] 10.1016/j.
bja.2020.06.013.
4. Shah ASV, Wood R, Gribben C, et al. Risk of hos-
pital admission with coronavirus disease 2019 in
healthcare workers and their households: nationwide
linkage cohort study. BMJ 2020;371:m3582. [Online
ahead of print] 10.1136/bmj.m3582.
5. European Observatory on Health Systems and Poli-
cies. COVID-19 Health System Response Monitor
2020. https://www.covid19healthsystem.org/main-
page.aspx.
6. Mafham MM, Spata E, Goldacre R, et al. COVID-19
pandemic and admission rates for and management
of acute coronary syndromes in England. Lancet
2020;396(10248):381-89. [Online ahead of print]
10.1016/s0140-6736(20)31356-8.
7. Wu J, Mamas M, Rashid M, et al. Patient response,
treatments and mortality for acute myocardial infarc-
tion during the COVID-19 pandemic. Eur Heart J Qual
Care Clin Outcomes 2020. [Online ahead of print]
10.1093/ehjqcco/qcaa062.
8. Metzler B, Siostrzonek P, Binder RK, et al. Decline of
acute coronary syndrome admissions in Austria since
the outbreak of COVID-19: the pandemic response
causes cardiac collateral damage. Eur Heart J
2020;41(19):1852-53. [Online ahead of print] 10.1093/
eurheartj/ehaa314.
9. De Filippo O, D’Ascenzo F, Angelini F, et al. Re-
duced rate of hospital admissions for ACS during
Covid-19 outbreak in northern Italy. N Engl J Med
2020;383(1):88-89. [Online ahead of print] 10.1056/
NEJMc2009166.
10. Maringe C, Spicer J, Morris M, et al. The impact
of the COVID-19 pandemic on cancer deaths due
to delays in diagnosis in England, UK: a national,
population-based, modelling study. Lancet Oncol
2020;21(8):1023-34. [Online ahead of print] 10.1016/
s1470-2045(20)30388-0.
11. Mulholland RH, Wood R, Stagg HR, et al. Impact of
COVID-19 on accident and emergency attendances
and emergency and planned hospital admissions in
Scotland: an interrupted time-series analysis. J R Soc
Med 2020:141076820962447. [Online ahead of print]
10.1177/0141076820962447.
12. Lazzerini M, Barbi E, Apicella A, et al. Delayed
access or provision of care in Italy resulting from
fear of COVID-19. Lancet Child Adolesc Health
2020;4(5):e10-e11. [Online ahead of print] 10.1016/
S2352-4642(20)30108-5.
13. Gray DP, Sidaway-Lee K, Harding A, et al. Reduc-
tion in face-to-face GP consultations. Br J Gen Pract
2020;70(696):328. 10.3399/bjgp20X710849.
14. Williams R, Jenkins DA, Ashcroft DM, et al. Diagnosis
of physical and mental health conditions in primary
care during the COVID-19 pandemic: a retrospective
cohort study. Lancet Public Health 2020;5(10):e543-
50. 10.1016/S2468-2667(20)30201-2.
PRIMARY CARE IN THE COVID-19 PANDEMIC 39
15. Joy M, McGagh D, Jones N, et al. Reorganisation
of primary care for older adults during COVID-19: a
cross-sectional database study in the UK. Br J Gen
Pract 2020;70(697):e540. 10.3399/bjgp20X710933.
16. Manseld KE, Mathur R, Tazare J, et al. CO-
VID-19 collateral: indirect acute effects of the
pandemic on physical and mental health in
the UK. medRxiv 2020:2020.10.29.20222174.
10.1101/2020.10.29.20222174.
17. Morreel S, Philips H, Verhoeven V. Organisation and
characteristics of out-of-hours primary care during a
COVID-19 outbreak: a real-time observational study.
PLoS One 2020;15(8):e0237629-e29. 10.1371/jour-
nal.pone.0237629.
18. Cancer Research UK. Over 2 million people wait-
ing for cancer screening, tests and treatments.
June 1, 2020. Accessed November 1, 2020. https://
scienceblog.cancerresearchuk.org/2020/06/01/
impact-of-coronavirus-on-cancer-services-revealed-
over-2-million-people-waiting-for-screening-tests-and-
treatments/.
19. Mahase E. Covid-19: urgent cancer referrals fall
by 60%, showing “brutal” impact of pandemic. BMJ
2020;369:m2386. 10.1136/bmj.m2386.
20. Dyer O. Covid-19: pandemic is having “severe” impact
on non-communicable disease care, WHO survey
nds. BMJ 2020;369:m2210. 10.1136/bmj.m2210.
21. McDonald HI, Tessier E, White JM, et al. Early impact
of the coronavirus disease (COVID-19) pandemic and
physical distancing measures on routine childhood
vaccinations in England, January to April 2020. Euro
Surveill 2020;25(19):2000848. 10.2807/1560-7917.
ES.2020.25.19.2000848.
22. Iob E, Steptoe A, Fancourt D. Abuse, self-harm and
suicidal ideation in the UK during the COVID-19 pan-
demic. Br J Psychiatry 2020;217(4):543-46. 10.1192/
bjp.2020.130.
23. Lydall R. Paramedic callouts to suicides or attempted
suicides in London double in a year. Evening Stan-
dard. October 28, 2020. Accessed November 1, 2020.
https://www.standard.co.uk/news/london/paramedic-
callouts-suicides-attempted-london-double-year-
a4573283.html.
24. Harding-Edgar L, McCartney M, Pollock AM. Test and
trace strategy has overlooked importance of clini-
cal input, clinical oversight and integration. J R Soc
Med 2020:141076820967906.[Online ahead of print]
10.1177/0141076820967906.
25. Thornton J. Covid-19: how coronavirus will
change the face of general practice forever. BMJ
2020;368:m1279. 10.1136/bmj.m1279.
26. Verhoeven V, Tsakitzidis G, Philips H, et al. Impact of
the COVID-19 pandemic on the core functions of pri-
mary care: will the cure be worse than the disease? A
qualitative interview study in Flemish GPs. BMJ Open
2020;10(6):e039674. 10.1136/bmjopen-2020-039674.
27. Nacoti M, Ciocca A, Giupponi A, et al. At the epicenter
of the Covid-19 pandemic and humanitarian crises
in Italy: changing perspectives on preparation and
mitigation. NEJM Catalyst. March 21, 2020. Accessed
November 1, 2020. https://catalyst.nejm.org/doi/
full/10.1056/CAT.20.0080.
28. Haines A, de Barros EF, Berlin A, et al. National UK
programme of community health workers for CO-
VID-19 response. Lancet 2020;395(10231):1173-75.
10.1016/S0140-6736(20)30735-2.
29. Greenhalgh T, Knight M, A’Court C, et al. Manage-
ment of post-acute covid-19 in primary care. BMJ
2020;370:m3026. 10.1136/bmj.m3026.
30. Drage M. Mword Issue 70—Dr Michelle Drage’s lat-
est update for GPs and practice teams. Londonwide
LMCs. October 30, 2020. Accessed November 1,
2020. https://www.lmc.org.uk/article.php?group_
id=23931.
31. Appointments in general practice September 2020.
NHS Digital. October 29, 2020. Accessed November
1, 2020. https://digital.nhs.uk/data-and-information/
publications/statistical/appointments-in-general-prac-
tice/september-2020.
32. BMA. BMA COVID-19 tracker survey 2020 October
wave. 2020. Accessed November 1, 2020. https://
www.bma.org.uk/media/3452/bma-covid-19-survey-
results-for-primary-care-doctors-oct-2020.pdf.
40 PRIMARY CARE IN THE COVID-19 PANDEMIC
COVID-19 and Primary
Care for Incarcerated
People Released to
the Community
Lisa Puglisi, Taylor Weilnau, and Emily A. Wang
D
espite the fact that the incarceration rate is the lowest it has been in the past 20 years, the
United States is still a nation that leads in jailing its citizens.
1
Currently, 2.2 million individu-
als are incarcerated in jails (which house those awaiting adjudication of crimes or serving sentenc-
es of less than a year) or prisons (housing those serving sentences greater than a year).
2
Arrest and
incarceration as forms of punishment and social control have been used to such a large extent that
an estimated one-quarter of adults in the country have been arrested.
3
Racial and ethnic disparities
in incarceration rates are stark, reecting systemic racist policies across the criminal legal system
spectrum. Black and Hispanic men, especially the young and non-college educated, are incarcer-
ated at approximately six- and two-fold increased rates, respectively, compared to their white
counterparts.
4
Incarcerated people have high rates of chronic health conditions, with high prevalence of commu-
nicable diseases (e.g., HIV, hepatitis C, syphilis), noncommunicable diseases (e.g., hypertension,
cancers, asthma), and mental health and substance use disorders.
5
For example, at least 10% of
incarcerated people are infected with hepatitis C, a prevalence rate that is at least 10 times higher
than that of the general population.
6
Ultimately, health issues that people who are incarcerated face become issues that impact the
community health system, as 95% of incarcerated people are released back into the community
at some point.
7
Upon release, people face serious barriers in caring for themselves, including dif-
culties nding housing and employment and accessing primary care. Insurance coverage remains
a signicant issue, even in the 39 states that expanded Medicaid services by 2020 as part of the
Aordable Care Act (ACA),
8
though a growing number of states do enroll certain people in Medicaid
upon incarceration or suspend their coverage, as opposed to terminating the benet, which is the
default in most states.
9
These obstacles, along with siloed correctional and community health systems that lead to poorly
coordinated transitions of care, are thought to be some of the driving factors behind the high risk
of death, hospitalization, and worsening health outcomes (e.g., increasing HIV viral load, relapse to
substance use, overdose, and worsening of cardiovascular disease risk factors) following release.
10
And in many ways, meeting basic needs after coming home from correctional systems has
become much harder in the time of COVID-19. In this chapter, we describe the state of
COVID-19 and primary care in correctional facilities, decarceration protocols related to the
pandemic, and health care and public health systems’ adaptations related to COVID-19 for
those aected by incarceration. We end with conclusions about how the primary care system
can support the urgent need for decarceration during COVID-19.
COVID-19 in correctional facilities
Correctional facilities in the United States have been uniquely and profoundly impacted by
the COVID-19 pandemic, given long-standing vulnerabilities to infectious disease outbreaks.
11
As early as March 2020, Riker’s Island jail in New York City and Cook County jail in Chicago
reported large-scale outbreaks aecting both incarcerated people and correctional sta at
rates that outpaced local community rates.
12
During the initial period of a large outbreak in an
urban jail, the disease dynamics were such that one COVID-19 infection of a sta or incarcer-
ated person would lead to eight others being infected.
13
According to the COVID Prison Project,
by August 2020, 90 of the largest 100 cluster outbreaks in the United States had occurred in
correctional facilities.
14
Many features of the criminal legal system at large and the physical structure and function
of correctional facilities, in particular, have contributed to this elevated risk, including high
throughput and brief stays for jail populations, facility overcrowding, and the built communal
environment and old infrastructure.
15
At least a quarter of correctional facilities are estimated
to be over capacity, and this does not account for those with congregate living quarters or
eating facilities. Further, the aging prison population (over 55 years old), which has grown
by 289% in the past two decades, has a disproportionate burden of chronic medical condi-
tions, which are risk factors for COVID-19. The COVID-19 pandemic, then, becomes additive
to the normative burden of ailments in incarcerated people, and this can result in strains on
the correctional health workforce and challenges to correctional health care systems that have
been largely excluded from the public health and preparedness planning infrastructure and
oversight.
Recommendations from national and local public health agencies have not comprehensively
addressed the unique needs of the correctional systems. For example, on March 30, 2020,
the Centers for Disease Control and Prevention (CDC) provided general recommendations for
correctional and detention centers, including guidance on masking, sanitation supplies, and
implementing social distancing in facilities (such as sleeping head to toe in double-occupancy
cells).
16
While correctional facilities worked to implement this guidance, there were many
eorts led by correctional leaders, court systems, and advocacy organizations to do more,
acknowledging the uniquely high risk for large-scale outbreaks in these facilities. These mea-
sures included nding space for medical isolation units, mass testing programs, cohorting
eorts to protect the most vulnerable, and, in some places, large-scale eorts to decarcerate
correctional facilities.
15
42 PRIMARY CARE IN THE COVID-19 PANDEMIC
The state of decarceration during COVID-19
Decarceration refers to any process that reduces the number of people in correctional facili-
ties, including diverting those who might otherwise be incarcerated (such as by granting
a promise to appear for a hearing instead of bail) and by oering early release to presently
incarcerated people. During the COVID-19 pandemic, decarceration has served as a mitigation
eort for COVID-19 transmission within certain facilities. Decarceration has been shown to
be a disease mitigation strategy that, in addition to following routine CDC mitigation strategy
guidance, can reduce the epidemic potential of SARS-CoV-2 in a correctional facility and pre-
vent the impact of an outbreak.
13
Furthermore, there is consistent evidence from a number of
states showing reduction of incarcerated populations does not result in an increase of serious
crime.
15
Since the pandemic began, there have been decreases in prison and jail populations. Between
January and August 2020, jail populations decreased by 22%, but state prison populations
decreased by only 4%, and Federal Bureau of Prisons populations by 10%.
2,
Prisons have been
dicult to decarcerate given legal barriers to “compassionate release,” which is a legal provi-
sion that varies by state but typically allows people with terminal illnesses, such as metastatic
cancer and end-stage heart failure, to be released before their sentences have been served.
Consideration for compassionate release often hinges on documentation of prognosis by a
licensed physician that the person has six months or less to live. This is despite evidence
that physicians tend toward overestimating survival even in terminally ill patients
17
and
that severely impaired function in activities of daily living and frailty are better indicators of
profound disability. Rarely used before the pandemic, compassionate release has been ineec-
tive for distancing the most medically vulnerable people in prison from the risks of COVID-19
even in the Federal Bureau of Prisons, where updated guidance on compassionate release from
the United States Sentencing Commission is broadest.
18
One critical part of compassionate release planning is identifying community health services
for these frail adults, such as a dialysis center for a person with end-stage renal disease.
Consequently, while it remains important to focus on increasing decarceration processes in an
active and ongoing manner to prevent the impact of future waves of COVID-19, further ef-
forts on the community health side are needed as well to facilitate the discharge planning and
coordination of care to address the signicant health needs of people returning to the com-
munity after release from correctional systems.
Peri-release primary care for incarcerated individuals
R.D. is a 43-year-old gentleman who was incarcerated for eight years and was in good health
upon his incarceration. While incarcerated, he developed a nonischemic cardiomyopathy,
which was complicated by an episode of sudden cardiac death, after which he was started on
antiarrhythmic medications and received placement of a biventricular automated implantable
cardiac debrillator. He resided in the prison inrmary for more than a year before he was re-
leased during the COVID-19 pandemic on compassionate release. He was sponsored for release
by his elderly father, and when he returned home, he had no phone, no source of income, and
no experience navigating health care in the community.
PRIMARY CARE IN THE COVID-19 PANDEMIC 43

People who are released from correctional facilities have intertwined health and social
needs, which present signicant barriers to engaging in primary care, especially given the
impact of factors unique to the COVID-19 pandemic. In the Behavioral Model for Vulnerable
Populations,
20
which we have adapted to reect the impact of COVID-19 on health behaviors
of people who are released from incarceration (Figure 1),
18-20
the predisposing, enabling, and
need factors predict engagement in primary care, which, in turn, predicts health outcomes.
Individuals released from correctional facilities have many predisposing factors, including
minority race (which reects their exposure to interpersonal, institutional, and structural
racism), high rates of discrimination, and criminal justice system contact. They have limited
access to stable housing and food. A majority of incarcerated people have at least one chronic
health condition, and it is estimated that approximately 40% of individuals are newly diag-
nosed with a chronic health condition while incarcerated.
20
These individuals learn to man-
age their new diagnoses within the context of correctional health care, where they rely on
correctional ocers and health professionals to administer care and medications, as well as
monitor daily adherence.
21
This is in a population with generally low levels of health literacy
22
and where self-ecacy, dened as the willingness and the ability of people to engage in vari-
ous preventive and disease management behaviors, is discouraged because it runs counter to
notions of safety and security. For instance, incarcerated people typically do not have access
to glucometers and cannot draw up their own insulin, given concerns about safety of having
needles behind bars. Additionally, many current and formerly incarcerated individuals have
never received or navigated treatment from community-based health systems and have little
to no experience utilizing pharmacy or health insurance services.
Figure 1. The Behavioral Model for Vulnerable Populations Adapted to Reect the Impact of COVID-19
on Health Behaviors of People with COVID-19-related Substance Use Disorder From Incarceration
Data derived from Gelberg, Andersen, and Leake.
20
Predisposing Enabling Need Health Behavior Health Outcome
- Age
- Gender
- Marital status
- Employment
- Education
- Minority
race/ethnicity
- Residential
history/
homelessness
- Incarceration
- Experience of
discrimination
- Income
- Food access
- Housing
- Social support
networks
- Discharge
planning
- SARS-CoV-2
testing prior to
release
- Insurance
- Location for 14
day quarantine
post-release
- Access to
telemedicine
- Perceived health
needs
- Chronic Health
Conditions
- History of SUD
- Community Level
COVID rates
- Ability to
Quarantine and
physically
distance
- Engagement in
Primary Care
- Addiction and
Mental Health
Treatment
- COVID related
morbidity
- Non-COVID
related morbidity
- Mortality
Population Characteristics
44 PRIMARY CARE IN THE COVID-19 PANDEMIC
An additional challenge to transitioning back to the community for people with a chronic
health condition is that discharge planning in correctional facilities is detached from com-
munity health systems. Most prisons have a standard basic approach to discharge planning
for these individuals. This may include a limited supply of medications (up to 30 days’ worth)
and questions about where the individual will live upon release. Meanwhile, jails less com-
monly have a formalized discharge plan focused on housing or health concerns due to the
shorter lengths of custody and unknown release date. In both prisons and jails, individuals
are scarcely provided their medical records, and if so, incarcerated people usually are required
to pay for their records. The exception to this is unique coordination-of-care programs for
people with certain health conditions such as HIV
22-25
or hepatitis C.
26
Because correctional facilities rarely refer people to community health care systems upon
release, incarcerated people face substantial barriers to engaging in primary care and chronic
condition management after release. As we noted earlier, health care is not a primary prior-
ity when individuals are released. Most people’s rst priorities are access to food, nding
somewhere to live, obtaining employment, reconnecting with family, and meeting the myriad
stipulations of probation or parole. As a result, health issues often receive less priority, and
people can be forced to make “trade-o decisions” that put their health at risk. Ninety per-
cent of individuals with a chronic health condition released from correctional facilities are
housing insecure or homeless. Many are without any access to food or employment prospects,
and they do not have identication to get state and federal benets.
27
With these barriers in
mind, in addition to the lack of transition planning and community care coordination, people
released from incarceration face disproportionately limited access to primary care.
28
One additional reason for low primary care engagement is discrimination within the primary
care system. For example, one audit study in Ontario, Canada, found that individuals who
disclosed a history of incarceration while seeking to establish primary care were half as likely
to be oered a new visit appointment.
29
This disparity of obtaining appointments for primary
care may contribute to poor health outcomes, such as higher rates of hospitalizations, inade-
quate mental health and substance use disorder treatment,
30
and high rates of opioid-involved
overdose, and warrants further study.
Strategies to address COVID-19 in primary care for
incarceration-affected populations
R.D. was referred to a primary care clinic but was not provided an appointment date because
of his rapid release. He was provided with vouchers for his necessary medications but had
never before used a pharmacy to ll a prescription and was uncertain as to how to obtain
rells when his 30-day supply ran out.
Discharge planning and improving access to primary care
Eective discharge planning during COVID-19 has required additional considerations beyond
medications and referral appointments. First, given the high risk of viral transmission in
PRIMARY CARE IN THE COVID-19 PANDEMIC 45
correctional facilities, people like R.D. being released may pose a risk to their immediate
family and to the community in which they are released. From a public health standpoint,
COVID-19 testing must therefore be considered in all reentry planning. This risk is even
more elevated for people who lack community supports upon their release and have limited
access to noncongregate housing, food, and essential needs, particularly when community
rates of COVID-19 are high. Further, people released from jail or prison should be discharged
with comprehensive education about the virus and a connection to community-based health
services for testing and expectant management should they become infected, particularly if
they have a chronic health condition or have lingering COVID-19 symptoms. Given high rates
of asymptomatic COVID-19 infection in general and high numbers of correctional outbreaks,
testing prior to discharge with quick return of results would reduce the risk of viral spread.
Moreover, given false negatives and real-world implementation complications encountered
with COVID-19 testing, a possible synergistic strategy, in collaboration with community-
based organizations and departments of public health, could be providing individuals return-
ing to congregate or crowded settings a safer and more isolated place in the community to
complete a 14-day quarantine. One example of this is arranging a subsidized hotel room for
the released individual.
Second, discharge planning from corrections should include increased medication supply (at
least a 90-day supply), acknowledging the active strain on pharmacies operating safely dur-
ing the pandemic and on people leaving their homes during community shutdowns to obtain
medications. This approach has been increasing in community medicine over the past decade,
has been associated with increased medication adherence,
31
and expands on prior recommen-
dations from the Urban Institute, which recommended 45 days’ worth of medications, ac-
knowledging that turning on medical benets took an average of 45 days.
32
Adequate medica-
tion supply and a direct connection to community primary care are essential prior to release,
as engagement in primary care has been shown to reduce reliance on emergency departments
for ambulatory care needs
19
and lower rates of other acute care utilization after release.
21
Prior
to the pandemic, some prisons and jails were piloting programs aimed to educate people on
management of their chronic diseases in the community. This education includes obtaining
medication rells and using insulin for the rst time.
33
Continuing such programs may reduce
unnecessary burden on the community system during the pandemic.
Last, as the majority of health systems work to expand telemedicine during the pandemic,
correctional health partners and discharge planners should consider increasing the use of
telemedicine for discharge planning. This may include establishing video visits with commu-
nity-based social service providers to address social determinants of health, such as housing
and food access, and community medical providers, including community health workers, to
help establish more of a connection to the community health system before release. Making
community health connections before release has been found in past interventions to be
helpful,
34
and during the time of COVID-19 where visits are restricted in many correctional
facilities, telemedicine expansion provides an avenue to more consistently oer connection to
community providers.
46 PRIMARY CARE IN THE COVID-19 PANDEMIC
Community health system adaptations to improve health behaviors
R.D. was brought into community care after his cousin referred him. He was seen in person
because he did not have a phone he could use. He did not have identication, but the health
care system created a new policy enabling those without ID to still be seen. He did not have
insurance, but enrollment was initiated by a social worker at his rst visit. A community
health worker connected him to resources to get a phone, as well as resources for food and
housing. His elderly father has stayed safe at home.
COVID-19 has created signicant tension on outpatient and inpatient services within commu-
nity settings. Many primary care and behavioral health care providers have put a momentary
pause on new appointments during the pandemic, and many have shifted to providing most
care via telemedicine. Access to primary care, substance use treatment, and mental health
care during the pandemic may be aided by community health systems partnering with pro-
grams that can provide patients with access to phones with video capabilities, especially in
situations where correctional systems have not provided them with these tools. Video com-
munication is linked with increased patient understanding and satisfaction when compared
with telephone consultation.
35
This is essential when considering primary care and substance
use and mental health care, since longitudinal relationships and clear communication are
indispensable to successful care management. It is important to note, with regard to sub-
stance use treatment, that the U.S. Drug Enforcement Agency issued new guidance due to the
pandemic that advised programs could prescribe buprenorphine via telehealth and loosened
the allotment of days for take-home medications for methadone,
36
in turn reducing in-person
visits. Enabling recently released patients with this technology could eliminate barriers to
this essential care, which is all the more critical given high rates of drug overdose after re-
lease from correctional facilities and the increased community rates of overdose during the
pandemic.
As many community health centers turn to telemedicine to protect patients and sta, they
must acknowledge that this will not be the appropriate approach for all patients. Blanket
shutdowns of in-person visits simply will harm some patients, and the community health
system must be tasked with nding ways to identify people who need face-to-face visits.
Using the patient example provided in the previous section, for a person who has never used
the community health system, has never lled a prescription or used a smartphone, and has
a physical health condition such as congestive heart failure that often requires physical exam
assessment, telemedicine appointments are simply insucient to provide proper care to the
patient. Triaging the clinical needs of patients, while also factoring in health literacy and
social needs of patients, is also part of primary care medicine and would be included in initial
in-person visits for people recently released from prison and jail.
Another evidence-based intervention to engage recently released individuals in primary care
is specially tailoring primary care for people just returning home from corrections, as is
done in the Transitions Clinic Network (TCN). TCN is a national consortium of more than 40
primary care–based programs that serves the needs of individuals returning from incarcera-
tion through interdisciplinary teams with community health workers with personal histories
of incarceration.
21
In a randomized controlled trial, participants in the TCN program in San
PRIMARY CARE IN THE COVID-19 PANDEMIC 47
Francisco had 51% fewer visits to the emergency department in a year compared with those
who were assigned to receive expedited primary care in safety-net systems.
37
TCN participa-
tion also impacts future criminal justice contact and is associated with lower rates of return-
ing to prison for a parole or probation technical violation and fewer incarceration days com-
pared with the control group.
38
In March 2020, in response to the rising pandemic concerns, some community health systems
collaborated with state prison systems to implement broad-scale innovation in coordina-
tion of care. Three such examples include systems that were designed in California, North
Carolina, and Connecticut as part of statewide TCN programs. Based on input and perceived
need from the departments of corrections, these statewide networks rapidly established easy
ways for correctional systems to refer anyone being released who had a chronic health condi-
tion. The networks took on the responsibility of linking those individuals with primary care
appointments in the communities to which they would return (even if there was not a TCN
program in that community), and connecting these individuals with a community health
worker who had a shared history of incarceration to help address some of the other stressors
and social needs associated with being rapidly released from incarceration. They facilitated
collaborations with state prison systems and local jails and community health care systems so
that people released from incarceration could receive an array of services to include expedited
primary care appointments, as well as in some locations phones upon release, and connec-
tions to rapid rehousing. Each TCN statewide program took a dierent approach, but they
all involved creation of new communication systems, such as a hotline or HIPAA-compliant
online referral platform, as well as systems to share medical information with consent that
allowed for more individualized planning before release.
Health insurance adaptations for improved health outcomes
Critical to accessing COVID-19 testing and treatment, primary care, and addiction treatment
upon release is health insurance. The Medicaid Inmate Exclusion Policy, which under the
Social Security Act prohibits use of federal funds for medical care provided to “inmates of a
public institution,” has not only led to underresourced care during incarceration, but also
created a class of uninsured individuals after release. Interruptions in insurance fuel some
of the poor care transitions
39
and disruptions in treatment for chronic health conditions
noted earlier. There are a number of opportunities within public health insurance programs
that are of importance during COVID-19, including Medicaid, Medicare, and the Veterans
Health Administration, for easing the transition from correctional to community health care.
Individuals impacted by incarceration mostly are insured by Medicaid, a state-federal health
care insurance that covers low-income adults. Importantly, Medicaid covers mental health
and substance use treatment and services, as well as intensive case management, rehabilita-
tion, and support services, heavily used by people impacted by incarceration. Enrollment in
Medicaid prior to release is associated with increased engagement in treatment among people
with serious mental illness.
40
Community health systems and public health experts can also work with their states to in-
stitute a number of policy changes that promote transition of health care during COVID-19.
48 PRIMARY CARE IN THE COVID-19 PANDEMIC
Under Medicaid administrative rules, states can suspend (as opposed to fully terminate)
Medicaid benets when a person is incarcerated. States that suspend Medicaid should facili-
tate timely reactivation of Medicaid following release.
41
Additionally, public health systems
can support prison and jail systems in allowing incarcerated people to apply for Medicaid (and
Medicare, as appropriate) prior to release. According to an inventory conducted by the Center
for Mental Health and Addiction Policy Research at Johns Hopkins University, as of January
2015, 64 programs across 21 states had sought to enroll individuals living in correctional
settings in Medicaid.
42
Although the inmate exclusion provision would continue to apply, this
pathway would be helpful once incarcerated individuals had been released, accelerating and
easing their access to Medicaid coverage.
Conclusions
The community health system, built o the backbone of primary care, has heretofore largely
ignored the health needs of the vast number of community members who have been incarcer-
ated. The pandemic has created the necessity for community health systems to rethink their
readiness to address the health needs of this large population and build the systems necessary
to care for them during the present and future pandemics. The COVID-19 pandemic provides
an opportunity to improve coordination between correctional and community health systems
and to dismantle the siloed care that has been the standard and has proven inadequate—
placing further at risk those incarcerated, those who work in correctional facilities, and the
general population. Without addressing the intersection of incarceration and the primary care
delivery system, the disparate racial impact of COVID-19-associated morbidity and mortality
cannot be fully mitigated.
References
1. World prison brief data. Institute for Crime & Justice
Policy Research. November 2019. Accessed January
14, 2021. http://www.prisonstudies.org/world-prison-
brief.
2. Franco-Paredes C, Ghandnoosh N, Latif H, et al.
Decarceration and community re-entry in the
COVID-19 era. Lancet Infect Dis 2021;21(1):e11-6.
10.1016/S1473-3099(20)30730-1.
3. Goggins BR, DeBacco DA. Survey of state criminal
history information systems, 2016: a criminal justice
information policy report. Document No. 251516.
Washington, DC: U.S. Department of Justice Bureau
of Justice Statistics, 2018. https://www.ojp.gov/pdf-
les1/bjs/grants/251516.pdf.
4. Carson EA. Prisoners in 2018. US Department of
Justice Bureau of Justice Statistics. April 2020. Ac-
cessed January 20, 2021. https://www.bjs.gov/con-
tent/pub/pdf/p18.pdf.
5. Wilper AP, Woolhandler S, Boyd JW, et al. The health
and health care of US prisoners: results of a nation-
wide survey. Am J Public Health 2009;99(4):666-72.
10.2105/AJPH.2008.144279.
6. Beckman AL, Bilinski A, Boyko R, et al. New hepatitis
C drugs are very costly and unavailable to many state
prisoners. Health Aff (Millwood) 2016;35(10):1893-
901. 10.1377/hlthaff.2016.0296.
7. Petersilia J. When prisoners come home: parole and
prisoner reentry. New York: Oxford University Press,
2003.
PRIMARY CARE IN THE COVID-19 PANDEMIC 49
8. Medicaid expansion enrollment. Kaiser Family
Foundation. June 2019. Accessed January 14, 2021.
https://www.kff.org/health-reform/state-indicator/
medicaid-expansion-enrollment/.
9. States reporting corrections-related Medicaid enroll-
ment policies in place for prisons or jails. Kaiser Fam-
ily Foundation. Accessed January 14, 2021. https://
www.kff.org/medicaid/state-indicator/states-reporting-
corrections-related-medicaid-enrollment-policies-in-
place-for-prisons-or-jails/.
10. Meyer JP, Cepeda J, Wu J, Trestman RL, Altice
FL, Springer SA. Optimization of human immu-
nodeciency virus treatment during incarcera-
tion: viral suppression at the prison gate. JAMA
Intern Med 2014;174(5):721-9. 10.1001/jamain-
ternmed.2014.601.
11. Bick JA. Infection control in jails and prisons. Clin
Infect Dis 2007;45(8):1047-55. 10.1086/521910.
12. Williams T, Ivory D. Chicago’s jail is top U.S. hot spot
as virus spreads behind bars. The New York Times.
April 8, 2020. Accessed January 14, 2021. https://
www.nytimes.com/2020/04/08/us/coronavirus-cook-
county-jail-chicago.html.
13. Puglisi LB, Malloy GSP, Harvey TD, Brandeau ML,
Wang EA. Estimation of COVID-19 basic reproduc-
tion ratio in a large urban jail in the United States.
Ann Epidemiol 2021;53:103-5. 10.1016/j.annepi-
dem.2020.09.002.
14. National COVID-19 statistics. The COVID Prison
Project. Last updated February 4, 2021. Accessed
October 20, 2020. https://covidprisonproject.com/
data/national-overview/.
15. National Academies of Science, Engineering, and
Medicine. Decarcerating correctional facilities during
COVID-19: advancing health, equity, and safety.
Washington, DC: The National Academies Press,
2020. 10.17226/25945.
16. Interim guidance on management of coronavirus dis-
ease 2019 (COVID-19) in correctional and detention
facilities. Centers for Disease Control and Prevention.
Last updated December 31, 2020. Accessed January
14, 2021. https://www.cdc.gov/coronavirus/2019-
ncov/community/correction-detention/guidance-cor-
rectional-detention.html.
17. Glare P, Virik K, Jones M, et al. A systematic review
of physicians’ survival predictions in terminally ill can-
cer patients. BMJ 2003;327(7408):195-8. 10.1136/
bmj.327.7408.195.
18. Frank JW, Andrews CM, Green TC, Samuels AM,
Trinh TT, Friedmann PD. Emergency department
utilization among recently released prisoners:
a retrospective cohort study. BMC Emerg Med
2013;13(1):16. 10.1186/1471-227X-13-16.
19. Gelberg L, Andersen RM, Leake BD. The behavioral
model for vulnerable populations: application to
medical care use and outcomes for homeless people.
Health Serv Res 2000;34(6):1273-302.
20. Mallik-Kane K, Visher CA. Health and prisoner
reentry: how physical, mental, and substance abuse
conditions shape the process of reintegration. Urban
Institute Justice Policy Center. February 2008. Ac-
cessed January 14, 2021. https://www.urban.org/
sites/default/les/publication/31491/411617-Health-
and-Prisoner-Reentry.PDF.
21. Shavit S, Aminawung JA, Birnbaum N, et al. Tran-
sitions Clinic Network: challenges and lessons
in primary care for people released from prison.
Health Aff (Millwood) 2017;36(6):1006-15. 10.1377/
hlthaff.2017.0089.
22. Hadden KB, Puglisi L, Prince L, et al. Health literacy
among a formerly incarcerated population using data
from the Transitions Clinic Network. J Urban Health
2018;95(4):547-55. 10.1007/s11524-018-0276-0.
23. Jordan AO, Cohen LR, Harriman G, Teixeira PA,
Cruzado-Quinones J, Venters H. Transitional care
coordination in New York City jails: facilitating link-
ages to care for people with HIV returning home from
Rikers Island. AIDS Behav 2013;17 Suppl 2:S212-9.
10.1007/s10461-012-0352-5.
24. Gardner LI, Metsch LR, Anderson-Mahoney P, et
al. Efcacy of a brief case management interven-
tion to link recently diagnosed HIV-infected persons
to care. AIDS 2005;19(4):423-31. 10.1097/01.
aids.0000161772.51900.eb.
25. Loeliger KB, Meyer JP, Desai MM, Ciarleglio MM,
Gallagher C, Altice FL. Retention in HIV care during
the 3 years following release from incarceration: a
cohort study. PLoS Med 2018;15(10):e1002667.
10.1371/journal.pmed.1002667.
26. Akiyama MJ, Columbus D, MacDonald R, et al. Link-
age to hepatitis C care after incarceration in jail: a
prospective, single arm clinical trial. BMC Infect Dis
2019;19(1):703. 10.1186/s12879-019-4344-1.
27. Western B. Homeward: life in the year after prison.
New York: Russell Sage Foundation, 2018.
28. Hammett TM, Roberts C, Kennedy S. Health-
related issues in prisoner reentry. Crime
and Delinquency 2001;47(3):390-409.
10.1177/0011128701047003006.
50 PRIMARY CARE IN THE COVID-19 PANDEMIC
29. Fahmy N, Kouyoumdjian FG, Berkowitz J, et al. Ac-
cess to primary care for persons recently released
from prison. Ann Fam Med 2018;16(6):549-51.
10.1370/afm.2314.
30. Wang EA, Wang Y, Krumholz HM. A high risk of
hospitalization following release from correctional
facilities in Medicare beneciaries: a retrospec-
tive matched cohort study, 2002 to 2010. JAMA
Intern Med 2013;173(17):1621-8. 10.1001/jamain-
ternmed.2013.9008.
31. Tajeu GS, Kent ST, Kronish IM, et al. Trends in
antihypertensive medication discontinuation and
low adherence among Medicare beneciaries
initiating treatment from 2007 to 2012. Hyperten-
sion 2016;68(3):565-75. 10.1161/HYPERTENSIO-
NAHA.116.07720.
32. Wachino V. Re: To facilitate successful re-entry for
individuals transitioning from incarceration to their
communities. Centers for Medicare and Medicaid
Services. April 28, 2016. Accessed January 14, 2021.
https://www.medicaid.gov/sites/default/les/Federal-
Policy-Guidance/Downloads/sho16007.pdf.
33. Reagan LA, Walsh SJ, Shelton D. Relationships
of illness representation, diabetes knowledge, and
self-care behaviour to glycemic control in incarcer-
ated persons with diabetes. Int J Prison Health
2016;12(3):157-72. 10.1108/IJPH-04-2015-0010.
34. Cunningham WE, Weiss RE, Nakazono T, et al.
Effectiveness of a peer navigation intervention
to sustain viral suppression among HIV-positive
men and transgender women released from jail:
the LINK LA randomized clinical trial. JAMA In-
tern Med 2018;178(4):542-53. 10.1001/jamain-
ternmed.2018.0150.
35. Nouri S, Khoong EC, Lyles CR, Karliner L. Ad-
dressing equity in telemedicine for chronic disease
management during the COVID-19 pandemic. NEJM
Catalyst. May 4, 2020. Accessed February 10, 2021.
10.1056/CAT.20.0123.
36. Knopf A. DEA, SAMHSA relax OTP/OBOT regula-
tions due to COVID‐19. Alcoholism & Drug Abuse
Weekly. March 20, 2020. Accessed January 14,
2021. 10.1002/adaw.32664.
37. Wang EA, Hong CS, Shavit S, Sanders R, Kessell E,
Kushel MB. Engaging individuals recently released
from prison into primary care: a randomized trial.
Am J Public Health 2012;102(9):e22-9. 10.2105/
AJPH.2012.300894.
38. Wang EA, Lin HJ, Aminawung JA, et al. Propensity-
matched study of enhanced primary care on contact
with the criminal justice system among individu-
als recently released from prison to New Haven.
BMJ Open 2019;9(5):e028097. 10.1136/bmjo-
pen-2018-028097.
39. Bryant B. NACo-NSA joint task force report: address-
ing the federal Medicaid inmate exclusion policy.
National Association of Counties. February 27, 2020.
Accessed January 14, 2020. https://www.naco.org/
resources/featured/naco-nsa-joint-task-force-report-
addressing-federal-medicaid-inmate-exclusion-policy.
40. Morrissey JP, Domino ME, Cuddeback GS. Expedited
Medicaid enrollment, mental health service use, and
criminal recidivism among released prisoners with
severe mental illness. Psychiatr Serv 2016;67(8):842-
9. 10.1176/appi.ps.201500305.
41. Rosen DL, Dumont DM, Cislo AM, Brockmann BW,
Traver A, Rich JD. Medicaid policies and practices
in US state prison systems. Am J Public Health
2014;104(3):418-20. 10.2105/AJPH.2013.301563.
42. Bandara SN, Huskamp HA, Riedel LE, et al. Leverag-
ing the Affordable Care Act to enroll justice-involved
populations in Medicaid: state and local efforts.
Health Aff (Millwood) 2015;34(12):2044-51. 10.1377/
hlthaff.2015.0668.
PRIMARY CARE IN THE COVID-19 PANDEMIC 51
The Asia Pacic
Experience of Primary
Health Care in the
COVID-19 Pandemic
Riya Master,* Neha Rana,* Lydia Chang,
Johanan Ponniah, and David B. Duong
*indicates co-lead author
T
he Asia Pacic region is a geographically, economically, socially, and politically diverse re-
gion of the world. In this review of the primary health care (PHC) response to the COVID-19
pandemic in the Asia Pacic region, we examine 19 countries and subregions within Asia Pacic,
in which 2.34 billion people live—approximately 30% of people in the world.
1
The rich diversity
of the region was reected in a diversity of responses and strategies to the COVID-19 pandemic.
We examined four domains within the Asia Pacic COVID-19 response related to PHC: (1) robust-
ness of PHC services delivery prior to the COVID-19 pandemic, as measured by the World Health
Organization’s (WHO) universal health coverage service coverage index (UHC-SCI); (2) implemen-
tation of mobile health strategies (i.e., telehealth, online information and support, etc.), (3) focus
on vulnerable populations, and (4) establishment and utilization of physical community-based
facilities in the COVID-19 response. The economic diversity among the 19 countries examined
necessitated a stratication by income level, as categorized by the World Bank. For the purposes of
this review, we summarized these four thematic areas among high-income countries and middle-
income countries. The only low-income country in our review, the Democratic People’s Republic of
North Korea, was not included because of a lack of data. Please refer to Table 1 for an overview of
all countries examined.
Robustness of PHC systems prior to COVID-19
PHC systems greatly vary in the Asia Pacic region, both among and within countries. Although
not a direct measure of the PHC system, the WHO’s UHC-SCI may be used as a proxy for primary
care eectiveness, as it assesses countries based on four domains typically provided at the PHC
service level: reproductive, maternal, newborn, and child health; infectious diseases; noncommu-
nicable diseases; and service capacity and access to essential services.
2
In this section, we discuss
UHC-SCI scores in relation to COVID-19 response, drawing out key themes both among and within
countries. Table 2 summarizes UHC-SCI scores for countries in the region.

Table 1. The Health Care, Demographic, and Geographic Diversity of the Asia Pacic Region
Country
Universal Health
Coverage (Y/N)
UHC-SCI Score
Population (in
millions)
Geographic
Orientation
High-Income Countries
Australia Y 87 25.5 Continent
Brunei Y 81 0.437 Island
Hong Kong Y unranked 7.497 Coastal
Japan Y 83 126.476 Archipelago
New Zealand Y 87 4.822 Archipelago
Singapore Y 86 5.85 Island
South Korea Y 86 51.269 Peninsula
Taiwan Y unranked 23.817 Island
Middle-Income Countries
Cambodia N 60 16.719 Peninsula
China N 79 1,429.324 Coastal
Indonesia Y 57 273.524 Archipelago
Laos Y 51 7.276 Mainland,
Peninsula
Malaysia Y 73 32.266 Peninsula,
Island
Mongolia Y 62 3.278 Mainland
Myanmar N 61 54.41 Peninsula
Philippines Y 61 109.581 Archipelago
Thailand Y 80 69.8 Peninsula
Timor-Leste N 52 1.318 Island
Vietnam N 75 97.339 Peninsula
The World Health Organization denes universal health coverage as “ensuring that all people have
access to needed health services of sucient quality to be eective while also ensuring that the use of
these services does not expose the user to nancial hardship.
54 PRIMARY CARE IN THE COVID-19 PANDEMIC

High-income countries
High-income countries examined in the Asia Pacic region all ranked high on the UHC-SCI.
For the majority of high-income Asia Pacic countries, a high UHC-SCI score correlated with
a COVID-19 strategy centered around PHC, including mobilization of PHC facilities and in-
creased investments in PHC by national governments. Specic examples are discussed later in
the chapter.
Japan’s robust PHC system played a tremendous role during the ght against COVID-19.
Between 2013 and 2017, the UHC-SCI has given a “high” score to Japan (2017 score of 83 on a
scale from 0 to 100). The high score of Japan’s universal health system was related to strate-
gies that were implemented during COVID-19, ultimately leading to Japan’s case count being
eectively lowered.
3
A vast network of community-based public health centers staed by
nurses, physicians, and volunteers spanning Japan helped maintain overall population health
in the country, with the assistance of thousands of primary care providers. The community-
based centers were central to mobilizing personal protective equipment (PPE), medical
personnel, contact tracing, COVID-19 testing, and cost coverage. Additional community treat-
ment centers were constructed at the onset of the virus to provide care and treatment services
to communities.
3
Community clinics were also essential in Singapore’s and Taiwan’s COVID-19 responses.
Using a similar approach as Japan, Singapore’s (UHC-SCI score of 86) COVID-19 strategy was
heavily reliant on primary care institutions and measures. One of the most eective strategies
was reactivating Public Health Preparedness Clinics. These are preexisting community-based
facilities that increased access to primary care during the pandemic.
4
Through these facilities,
PPE was distributed, patients were cared for, and local transmission was reduced signicant-
ly. Non-COVID-19-related primary care services were continued throughout the pandemic
through these clinics, ensuring continuity of care.
5
Taiwan (UHC-SCI unranked by WHO)
quickly mobilized 156 community clinics to screen patients exhibiting COVID-19 symptoms
to prevent overburdening hospitals and possible hospital outbreaks.
6
After screening, patients
with severe conditions were sent to designated hospitals that were well equipped.
Similarly, Australia has a strong primary care system (UHC-SCI 87) of doctors, nurses,
and integrated health care workers, such as allied health professionals, midwives, com-
munity pharmacists, and Aboriginal (indigenous Australian) health workers.
7
When the
Table 2. The WHO’s Universal Health Coverage Service Coverage Index (UHC-SCI) Among High-
and Middle-Income Countries in the Asia Pacic Region
Income Level of
Country
UHC-SCI Score
Average
UHC-SCI Score
Standard
Deviation
UHC-SCI Full
Range
UHC-SCI
Interquartile
Range
High income (n = 6) 85.00 2.45 [81, 87] 3
Middle income (n = 11) 61.91 11.81 [43, 80] 14
PRIMARY CARE IN THE COVID-19 PANDEMIC 55
rst COVID-19 cases were identied, Australia’s chief medical ocer held a Primary Care
COVID-19 Preparedness Forum with representatives from medical practices, Aboriginal and
Torres Strait Islander health workers, the disability sector, PHC delivery networks, and vari-
ous levels of government. Australia’s initial primary care response package in March 2020
was $2.4 billion, with $1.1 billion allocated specically for COVID-19, focused upon six sec-
tors: (1) funding of telehealth delivery services; (2) establishment of call centers to triage
patients with COVID-19 symptoms or exposure; (3) establishment of a network of community
respiratory clinics; (4) development and delivery of online infection training; (5) measures to
safeguard the health of Aboriginal and Torres Strait Islander communities; and (6) messaging
to primary care providers in a consistent manner.
7
New Zealand (UHC-SCI 87) also has a health care system centered around PHC. The value
placed on primary care, along with a strong existing network of primary care facilities, al-
lowed for New Zealand to quickly mobilize the COVID-19 response at the primary care level.
8
New Zealand created a national primary care COVID-19 reference guide for all providers to
follow four steps: (1) infection prevention and control for patients and sta; (2) clinical care;
(3) cleaning; and (4) management of patients. Primary care providers were given a set of
standardized instructions and triage policy for suspected COVID-19 infections.
8
Patients were
directed away from the hospitals to avoid exceeding capacity when home care was suitable.
Meanwhile, classied red-ag symptoms mandated urgent clinical review. Those at greater
risk for spreading COVID-19 were categorized as a higher index of suspicion (HIS) and
provided dierent protocols. A community-based public health unit informed patients who
tested positive and conducted daily monitoring until the patient was cleared for release. All
patients, regardless of test outcome, received ongoing primary care support depending on
their level of illness.
8
Hong Kong’s public-private health system operates in a dual system, with 90% of inpatient
care provided by public hospitals and the remaining covered by the private sector.
9
Unlike
other high-income countries and regions, Hong Kong focused on leveraging public hospitals’
services for the rst two waves of the pandemic. During the third wave, the government,
recognizing the importance of primary care and community-based care, established two
community treatment facilities to curb rising cases. The facilities admitted patients in stable
conditions to ease bed space in the public sector. In February 2020, the government provided
$129 million to secure the PPE supply in the public sector and all community treatment
facilities.
10
Middle-income countries
There is a greater range of UHC-SCI scores among the middle-income countries in Asia
Pacic. The diversity in UHC-SCI scores is reected in the country’s COVID-19 response
strategy, and whether it incorporates PHC. Overall, middle-income countries had less of a
primary care focus in their COVID-19 response, a notable dierence from the high-income
countries.
56 PRIMARY CARE IN THE COVID-19 PANDEMIC
The People’s Republic of China (UHC-SCI 79) has grown its primary care system signicantly
over the past decade. For example, China increased nancial investments into primary health
care by more than 10-fold ($29.34 billion in 2018) over the past 10 years.
11
The country has
also dedicated almost 4 million primary care practitioners to the pandemic relief eort.
10
Primary care practitioners are in charge of screening suspected cases, visiting residents in
quarantine, contact tracing, monitoring, and surveillance checkpoints. Despite this broad re-
sponsibility, primary care practitioners indicated an initial lack of PPE.
11
A shortage of profes-
sional human resources in China also made outbreak control dicult.
An independent review of Thailand’s (UHC-SCI 80) COVID-19 response identied several fac-
tors that contributed to eective pandemic management. These factors include past invest-
ments into enhancing health care capabilities (such as the Village Health Volunteer system),
public-private sector collaboration, establishment of multilingual COVID-19 hotlines for mi-
grants, extending free COVID-19 treatment to non-Thai residents, rapid expansion of health
care facilities, hospitalization of all COVID-19 cases (even asymptomatic ones), maintenance
of essential health care services, employment of telemedicine, and delivery of medicines via
the mail.
12
As the implementation of pandemic management responses directly used primary
care tactics, it eectively fed into Thailand’s high UHC-SCI score.
Laos, Cambodia, Philippines, and Vietnam all ranked lower on the UHC-SCI scale in com-
parison to other middle-income Asia Pacic countries. Diering from nations like China and
Thailand, the aforementioned countries centered their pandemic responses in hospital sys-
tems. COVID-19 patients and treatment regimens remained in the walls of hospitals, which
nevertheless remained above capacity because of hospital bed and PPE shortages. Thus, their
lower UHC-SCI score was reected in the lack of integration of primary care response tactics,
such as primary care facilities and community-based units.
Summary
Asia Pacic countries with robust PHC systems, including universal health coverage, had
ecient responses to COVID-19 and relied upon those systems for their pandemic response.
The high UHC-SCI scores of high-income countries among the Asia Pacic region correlate
to their robust PHC systems’ response to COVID-19. Factors such as emphasis on community
care, vast networks of primary care providers, and national PHC initiatives are contributors
to the robustness of PHC systems. Nations that ranked lower in the UHC-SCI index and did not
have robust PHC systems prior to the pandemic predominantly relied on hospital-based COVID-19
control and treatment strategies, utilizing primary care for screening and testing eorts.
PRIMARY CARE IN THE COVID-19 PANDEMIC 57
Implementation of mobile health strategies
The mobile health strategies in the Asia Pacic region expanded upon the onset of COVID-19.
Most countries within the region implemented strategies to increase mobile health and tele-
health to some extent, including measures such as online consultation services, webinars to
disseminate information to the health care professionals and the general public, and various
methods to reduce transmission. In this section, we outline the dierent approaches taken
by the high- and middle-income countries in the Asia Pacic region to implement mobile
health strategies.
High-income countries
Many high-income countries expanded telemedicine services and mobile health strategies to
reduce transmission of the virus. In March 2020, Japan’s Ministry of Economy, Trade, and
Industry launched an initiative to provide citizens with a free remote health consultation
service, addressing concerns regarding COVID-19. Many hospitals and community-based
treatment facilities also installed mobile applications in patients’ rooms to report body tem-
perature two times a day, minimizing contact between patient and care provider.
3,13
South
Korea took part in a similar initiative with the government’s creation of the Korean Medicine
telemedicine center, providing patients with consultation for dierent medical services. Prior
to admission into hospitals or other treatment centers, patient symptoms were assessed
through telephone interviews to reduce risk of transmission.
14
Singapore’s Ministry of Health announced a new telemedicine sector in January 2020. The
Infocomm Media Development Authority and Enterprise Singapore not only expanded tele-
consultation digital solutions but also announced grants and subsidies for smaller health care
providers, specically primary care providers, to incentivize adoption of the teleconsultation
solutions.
4,5
Increased communication and information access was achieved through email
and secure group chat on mobile devices. This mode of communication was observed to be
eective and time saving. Brunei similarly strengthened its existing mobile health platforms,
which limit patient-doctor physical contact, but allowed for continued assessment of symp-
toms via phone, email, and video.
15
Australia quickly shifted to the use of telehealth through its extensive primary care network.
Funding from the Medicare Benets Schedule allowed the government to double bulk-billing
incentives (doctors sending bills directly to Medicare) and deliver 11 million telehealth services
within the rst few months. Australia used a four-stage approach to roll out its telehealth
program: (1) consultations for most vulnerable populations; (2) consultations for obstetrics
and midwifery, nurse practitioner care, and mental health; (3) expansion of telehealth for
health care providers caring for vulnerable populations; and (4) expansion of telehealth
consultations to all patients.
7
The nation simultaneously developed a series of online education
modules for infection prevention and control, including eight modules for care workers for the
residential aged (elderly who can no longer live at home) and a 30-minute online course for all
58 PRIMARY CARE IN THE COVID-19 PANDEMIC
care workers. Regular primary care webinars were streamed and accessed by more than 100,000
health care workers.
7
Australia also established a national call center called Healthdirect to
provide free health information and advice. The program includes an online COVID-19 symptom
checker that reached a cumulative total use of 370 million people in May 2020.
7
Middle-income countries
Middle-income countries adopted new telemedicine services and mobile health strategies to
reduce transmission of the virus. Peking Union Medical College Hospital in China expanded
free online consultation and medical resources for patients during the pandemic. For example,
a scientic pandemic prevention ebook called Questions and Answers for Public Protection Against
COVID-19 Infection was released to the public to spread awareness of public health guidance.
16
Pinetree Care Group launched a virtual rehabilitation program and nursing classes to encour-
age patients and families to practice self-care at home and in their communities.
16
The Malaysian Ministry of Health ran daily webinars and Facebook Live sessions to provide
regular updates on the pandemic to local communities and primary care providers.
16
The
director-general of Health Malaysia hosted the daily live telecasts on the current status,
actions, and advice for dealing with the coronavirus.
17
All webinars included question-and-
answer sessions between the public and health care professionals. Family medicine specialists
also conducted live 30-minute sessions to engage with the public.
17
Similar to Malaysia’s online webinars, Indonesia hosted an online seminar with the World
Health Organization to enhance the role of primary health care in prevention and control of
the coronavirus.
18
Thousands of primary care providers, specically those at puskesma (remote
community health centers), participated in the seminar. Attendees were required to complete
a certication test at the end of the seminar, to ensure their competency in the COVID-19
response for their respective communities.
18
Many countries adopted new systems to help triage patients and risk-stratify them for
treatment escalation. Thailand piloted a new health model to stratify patients based on the
urgency of medical treatment and the risk of COVID-19 infection. Less urgent cases were sup-
ported through telemedicine from primary care providers and medications delivered directly
to patients’ homes.
19
The government of Philippines recently enabled telehealth providers to issue case reports
and prescriptions at community clinics.
20
Telemedicine was employed to care for vulnerable
populations, such as HIV patients, during lockdown measures. Various telemedicine methods
were employed to monitor close contacts of COVID-19 cases and individuals under quaran-
tine.
21
Vietnam implemented strategies that piloted telemedicine to link referral hospitals
to PHC facilities.
22
Tertiary care providers could advise local PHC providers through remote
communication, preventing the need for patients to travel to referral hospitals during the
pandemic, and allowing receipt of care through primary care providers in the community.
Many of the telemedicine services in Vietnam were provided for free during the outbreak of
the pandemic.
23
PRIMARY CARE IN THE COVID-19 PANDEMIC 59
Summary
Many countries in the Asia Pacic region adopted telehealth infrastructure and resources to
increase communication and limit physical contact. Telehealth spread educational content
during the pandemic response through webinars, e-pamphlets, ebooks, and more. Primary
care providers conducted online consultations for COVID-19, and participated in electronic
consultations between tertiary and primary care providers. As a result, physical doctor-to-
patient contact was limited to emergency situations to prevent spread of the disease. Primary
care experienced rapid uptake and scale of mobile health strategies in response to COVID-19,
introducing new forms of health care delivery and engagement. These innovations are ex-
pected to stay beyond COVID-19 and continue to redene the PHC ecosystem.
Focus on vulnerable populations
Vulnerable populations were given high priority for COVID-19 surveillance and treatment in
the Asia Pacic region. This category encompassed populations most likely to be infected and
populations most likely to face negative health outcomes from COVID-19, such as the elderly,
migrant workers, the immunocompromised, and remote communities.
High-income countries
Vulnerable populations were disproportionately aected by COVID-19 within Asia Pacic
countries. The large elderly population was one such group. Singapore’s response to the
risk among the elderly population was emblematic of the challenges in the region.
24
At the
onset of the pandemic, geriatric care in Singapore signicantly decreased in availability due
to shelter-in-place policies. The government took responsibility for all costs of testing and
treatment for COVID-19, and rapidly scaled up testing at nursing homes.
16
Additional vulnerable groups became infected in Singapore and similarly experienced a
government response focused on testing and contact tracing. In April 2020, Singapore expe-
rienced a rapid rise in COVID-19 infections due to widespread transmission among migrant
workers living in crowded dormitories. The high prevalence (over 15% as of October 2020)
of COVID-19 among this vulnerable population was likely due to inadequate safe distancing
and mingling of workers at common facilities such as eating areas and toilets, often due to
overcrowded living situations.
25, 26
Migrant workers had limited access to health care due to
language barriers, hesitancy to seek medical care due to a fear of forfeiting jobs or salaries,
and concern about out-of-pocket expenditures for outpatient care not covered by insur-
ance.
27
Widespread testing was conducted among dormitory residents. Workers who had mild
symptoms were sent to community care facilities for further medical care. On-site health
care centers were also quickly established in the dormitories. Health care volunteers and local
primary care networks were activated to help mitigate the outbreak through contact tracing.
Accommodations at other sites such as public housing ats and military installations were
arranged to facilitate safe distancing between workers.
26
60 PRIMARY CARE IN THE COVID-19 PANDEMIC
As in Singapore, access to geriatric care was reduced in Hong Kong due to shelter-in-place
policies. The elderly populations experienced a rise in infections. Outbreaks identied in
homes for the elderly in mid-July triggered a third wave of COVID-19 after generalized rst
and second waves had dissipated.
10
Elderly persons living in cramped rooms with poor ven-
tilation triggered the transmission within elderly care facilities.
28
Regular free testing for the
elderly and their caregivers was made available to prevent future outbreaks through isolation
and contact tracing.
Remote communities were at high risk for lack of resources and infection due to their separa-
tion from the mainland in the Asia Pacic region. Australia sought to address this through
the establishment of the National Aboriginal and Torres Strait Islander Advisory Group on
COVID-19 with the Department of Health and National Aboriginal Community Controlled
Health Organization.
7
Grants were provided for the Aboriginal and Torres Strait Islander
people to develop their own, culturally appropriate, preparedness plans. National protocols
were also adapted for local use.
7
Middle-income countries
Vulnerable populations in middle-income countries were heavily aected by COVID-19.
Malaysia focused testing on high-risk groups and locations due to limited resources. These
included migrant workers employed in the construction, manufacturing, and retail sectors,
who were particularly at risk for COVID-19 due to their crowded living accommodations. The
Ministry of Health required employers to screen employees before entering the workplace,
provide hand sanitizer, enforce physical distancing, and regularly disinfect shared spaces to
protect migrant workers.
18
More than 22,000 migrant workers were screened as of May 2020,
resulting in a 4% positive test rate.
18
The Ministry of Health tested residents and sta at
nursing homes in the country to protect the elderly, and it closely coordinated with the United
Nations High Commission for Refugees to provide refugees and asylum seekers health care
during the pandemic.
18
Among middle-income countries, an additional vulnerable population was immunocompro-
mised patients, who were overrepresented due to the endemicity of HIV and a recent increase
in diabetes and cancer. To ensure HIV patients continued to have access to antiretroviral
therapy, the Philippines increased the number of antiretroviral therapy community collec-
tion points.
29
However, continuity of medical access was not experienced in all countries; in
Laos, utilization of essential health services decreased.
30
Furthermore, the government ordered
private hospitals and clinics to close as part of COVID-19 containment eorts.
31
Summary
Like many countries globally, health inequities between vulnerable and less vulnerable
populations in the Asia Pacic region were exacerbated by the COVID-19 pandemic. Although
many countries in Asia Pacic have universal health coverage, certain groups of people still
experienced higher rates of COVID-19 than others. The elderly population composes a higher
proportion in many Asia Pacic countries, and the elderly’s fragility and multiple medical
PRIMARY CARE IN THE COVID-19 PANDEMIC 61
comorbidities place them at higher risk. The high percentage of migrant labor within the Asia
Pacic region also highlights the need for further attention to labor and living conditions of
migrant workers, for whom insurance coverage and access to primary care may be limited or
eectively inhibited by immigration status, language barriers, and fear of job loss. Finally,
those already living on the fringes of society, including people living with HIV, refugees and
asylum seekers, and indigenous communities were also disproportionately aected.
Establishment and extent of utilization of physical
community-based facilities
Asia Pacic countries utilized their community-based facilities to provide treatment and
testing for COVID-19. Middle-income countries, which were overwhelmed at a national level,
relied heavily on community-based facilities. These facilities were the rst point of contact
for many patients in the Asia Pacic region, as they are highly ingrained in the PHC system.
High-income countries
Several countries within the high-income category responded to the pandemic with either
the reactivation of physical community-based facilities that had been used during other
public health crises, or the creation and establishment of new facilities in light of COVID-19.
The government of Singapore reactivated nearly 1,000 Public Health Preparedness Clinics.
This eectively reduced “doctor hopping” amongst patients through government-subsidized
programs, while simultaneously increasing access to primary care. The primary care response
expanded in Singapore, allowing for 71% of COVID-19 positive patients to “visit primary care
doctors within two days of symptom onset.”
4,5
More notably, however, was Singapore’s triage
system implemented in the respective community-based facilities. Patient ow was heavily
amended to diminish risk for cross contamination not only from patient to patient, but also
patient to doctor. These containment measures were supplemented by new clinical protocols
that surrounded PPE strategies, a new system for electronic medical records, and vast num-
bers of aforementioned telehealth practices.
4
Similarly, South Korea instated community treatment centers throughout various regions.
Between March 3 and March 26, 2020, 3,033 patients were admitted to 15 community cen-
ters.
13,14
Japan was another actor in the coalition that utilized community-based facilities with
the formation of multiple community treatment centers in cities across the country. The cen-
ters were fully equipped with a robust sta, including multiple physicians, nurses, radiologic
technicians, public health doctors from the Ministry of Health and Welfare, and volunteers.
3
Hong Kong, unlike South Korea, Japan, and Singapore, admitted all conrmed and prelimi-
nary conrmed cases to the hospital. Recovering patients with stable conditions, who were
fever-free for 48 hours, less than 50 years old, and mobile were redirected to community
62 PRIMARY CARE IN THE COVID-19 PANDEMIC
treatment facilities.
32
Hong Kong established two community treatment facilities provid-
ing more than 2,000 beds to reduce the pressure on public hospitals. The Hospital Authority
also deployed doctors and nurses to respective community treatment facilities. In Taiwan,
156 community-based care facilities were set up to treat patients with mild symptoms.
Community-based care facilities screened individuals with COVID-19 symptoms and sent
patients to designated hospitals for treatment based on their condition.
6
Middle-income countries
COVID-19 testing and treatment was extended to community centers and public health clin-
ics due to limited capacity at public hospitals in many middle-income countries. Community
health centers were given the responsibility of conducting public health surveillance, provid-
ing treatment, and performing contact tracing. During the initial outbreak in Wuhan, China,
more than 70 primary care clinics supported screening, testing, and contact-tracing eorts.
33
More than 200 township and village doctors were drafted for 392 inspection spots along
the roads to check passengers and drivers for symptoms in Zhejiang province.
33
Similarly,
Indonesia is home to around 10,000 puskesmas in remote villages and inland regions that were
instrumental in providing COVID-19 relief.
34
Many public health programs and posyandu run
by puskesmas shut down due to the transition to pandemic-focused services.
34
Health workers
in Malaysia were mobilized from the Klinik Desa (rural health clinics) and small community
clinics to more frequented clinics to maximize resources.
18
Treatment strategies varied from country to country, predominately utilizing community-
based treatment facilities or hospital-driven responses. The Philippines developed community
treatment facilities,
35
despite only 20% of total hospital beds being set aside for COVID-19 pa-
tients.
36
Mild COVID-19 cases were not hospitalized but are isolated at home or in designated
community facilities.
37
Alternatively, Vietnam’s COVID-19 response has been hospital-driven,
though rapid-testing centers were also established in the community.
38
In Laos, COVID-19
testing and treatment were available only at hospitals, with minimal focus on PHC and/or
community-based interventions.
39
Asia Pacic countries that directed patients to public hospitals still utilized community-
based facilities to supplement national-based care. Testing was extensively conducted on a
community level in Thailand, despite all COVID-19 cases being sent to hospitals or isolation
facilities regardless of symptoms.
40
Village health volunteers assisted in case nding, contact
tracing, and health communication. Mongolia adopted a similar approach to Thailand, with
all COVID-19 cases being hospitalized and community testing being utilized. For example, a
300-bed hospital was established preemptively and walk-in testing sites were developed in
Ulaanbaatar, the capital of Mongolia.
41
PRIMARY CARE IN THE COVID-19 PANDEMIC 63
Summary
Countries with an extensive network of existing community-based facilities rapidly mobilized
these facilities for the pandemic response. In addition, countries such as Japan, South Korea,
Indonesia, Philippines, and China built new community treatment centers for individuals to
receive testing and treatment without having to go to hospitals, while Singapore reactivated
previously dormant Public Health Preparedness Clinics that had been built for previous disease
outbreaks. Thailand, Mongolia, and Vietnam had responses that were hospital-reliant, with
community-based clinics supporting contact tracing, testing, and health communication eorts.
Conclusions
The Asia Pacic region is incredibly diverse geopolitically, economically, and socially. Key
themes among the robustness of PHC systems, establishment of mobile health strategies,
focus on vulnerable populations, and utilization of community-based facilities emerged across
the region’s primary care response to COVID-19.
Among the high-income countries in the region, high scores on the UHC-SCI were associated
with a COVID-19 strategy and response relying on PHC and community-based approaches in
the prevention, testing, care, and treatment of COVID-19, in addition to contact tracing and
quarantine support functions. Countries relying on a PHC response backbone were able to
quickly scale up mobile health strategies and interventions. These actions not only helped to
stem COVID-19 cases and deaths, but also allowed for increased continuity of care for chronic
conditions that themselves serve as risk factors for COVID-19 infection. The strong commit-
ment to universal health coverage reduced health inequities in COVID-19 care and treatment as
compared to other regions that do not have universal health coverage policies in place.
Among middle-income countries in the region, the COVID-19 response at the PHC level was
more diverse. Most of the middle-income countries in the region utilized frontline health
workers and community health centers in prevention, health promotion, and testing. Care
and treatment services were more limited at community-based facilities, as compared to
high-income countries, due to varying capacities and inadequate resources. Mobile health
strategies were utilized by many middle-income countries to deploy accurate information and
train frontline health workers.
In both the high-income and middle-income countries, vulnerable populations—particu-
larly older adults and migrant workers––were at disproportionate risk and had the most
limited access to telehealth or in-person primary care facilities. Further understanding how
to expand care for these populations during the COVID-19 pandemic, and in preparation for
future outbreaks, will serve as a vital strategy to ensure PHC systems can support vulner-
able populations.
64 PRIMARY CARE IN THE COVID-19 PANDEMIC
References
1. United Nations, Department of Economic and Social
Affairs, Population Division. World population pros-
pects, 2019. New York: United Nations, 2019. Ac-
cessed January 25, 2021. https://population.un.org/
wpp/Download/Standard/Population/.
2. World Health Organization. Primary Health Care on
the Road to Universal Health Coverage 2019 Moni-
toring Report. Conference Edition. Geneva, Switzer-
land: World Health Organization, 2019. https://www.
who.int/healthinfo/universal_health_coverage/report/
uhc_report_2019.pdf?ua=1.
3. Takita M, Matsumura T, Yamamoto K, Yamashita
E, Hosoda K, Hamaki T, Kusumi E. Geographi-
cal proles of COVID-19 outbreak in Tokyo:
an analysis of the primary care clinic–based
point-of-care antibody testing. J Prim Care Com-
munity Health 2020;11:2150132720942695.
10.1177/2150132720942695.
4. Lim WH, Wong WM. COVID-19: notes from the
front line, Singapore’s primary health care perspec-
tive. Ann Fam Med 2020;18(3):259-261. 10.1370/
afm.2539.
5. Sim S, Teo S, Kong J, Lim Z, Ng M, Tang W.
COVID-19 in Singapore—a case series from primary
care. Singapore Med J May 27, 2020 [Online ahead
of print] 10.11622/smedj.2020082.
6. Han E, Chiou S-T, McKee M, Legido-Quigley H.
The resilience of Taiwan’s health system to ad-
dress the COVID-19 pandemic. EClinicalMedicine
2020;24:100437. 10.1016/j.eclinm.2020.100437.
7. Desborough J, Hall Dykgraaf S, Toca L, et al. Austra-
lia’s national COVID‐19 primary care response. Med
J Aust 2020;213(3):104. 10.5694/mja2.50698.
8. COVID-19: Primary Care. Ministry of Health New
Zealand. 2020. Accessed January 26, 2021. https://
www.health.govt.nz/our-work/diseases-and-condi-
tions/covid-19-novel-coronavirus/covid-19-informa-
tion-health-professionals/covid-19-primary-car9.
9. Act Together to Fight COVID-19. Hong Kong’s
Information Services Department. July 25, 2020. Ac-
cessed October 27, 2020. http://www.news.gov.hk/en
g/2020/07/20200725/20200725_141131_457.htm10.
10. Wing-man K. On the Record: HK Healthcare Is a
Dual-Track System. News.gov.hk. April 9, 2013. Ac-
cessed October 27, 2020. https://www.news.gov.hk/
en/record/html/2013/04/20130409_190409.shtm11.
Lessons from the Asia Pacic region emphasize the need for an extensive primary care response
to the COVID-19 pandemic. The values of primary care––technology-enabled, accessibility, and
community—were pivotal in the development of public health measures across high-income
and middle-income countries. The Asia Pacic region is home to a variety of PHC systems that,
in response to COVID-19, diered in implementation but coincided in purpose.
PRIMARY CARE IN THE COVID-19 PANDEMIC 65
11. Xu Z, Ye Y, Wang Y, et al. Primary care practitioners’
barriers to and experience of COVID-19 epidemic
control in China: a qualitative study. J Gen Intern
Med 2020;35(11):3278-3284. 10.1007/s11606-020-
0610712.
12. Ministry of Public Health and World Health Organiza-
tion. Joint Intra-Action Review of the Public Health
Response to COVID-19 in Thailand. Geneva, Swit-
zerland: World Health Organization, 2020. https://
www.who.int/docs/default-source/searo/thailand/iar-
covid19-en.pd13.
13. Park P, Kim CH, Heo Y, Kim TS, Park CW, Kim CH.
Out-of-hospital cohort treatment of coronavirus dis-
ease 2019 patients with mild symptoms in Korea: an
experience from a single community treatment cen-
ter. J Korean Med Sci 2020;35(13):e140. 10.3346/
jkms.2020.35.e1414.
14. Kim J-H, An JA-R, Min P, Bitton A, Gawande AA. How
South Korea responded to the COVID-19 outbreak
in Daegu. NEJM Catalyst 2020;1(4). https://doi.
org/10.1056/CAT.20.0159.
15. Wong J, Koh W, Alikhan M, Abdul Aziz A, Naing
L. Responding to COVID-19 in Brunei Darus-
salam: lessons for small countries. J Glob Health
2020;10(1):010363. 10.7189/jogh.10.010366.
16. Lim W, Liang C, Assantachai P, et. al. COVID‐19
and older people in Asia: Asian Working Group
for Sarcopenia calls to action. Geriatr Gerontol Int
2020;20(6):547-558. 10.1111/ggi.13939.
17. Koshy R, Hairizan bt. Nasir N. COVID-19: primary
health care initiatives in Malaysia. Primary Health
Care Performance Initiative. Ministry of Health Ma-
laysia, 2020. Accessed November 3, 2020. https://
improvingphc.org/sites/default/les/FULL%20Re-
port_COVID-19%20Primary%20Health%20Care%20
Initiatives%20in%20Malaysia%20for%20PHCPI%20
June%202020.pdf.
18. World Health Organization.
Online seminar to
strengthen the roles of primary health care in preven-
tion and control of COVID-19 in Indonesia. Geneva,
Switzerland: World Health Organization, May 17,
2020. https://www.who.int/indonesia/news/detail/17-
05-2020-online-seminar-to-strengthen-the-roles-
of-primary-health-care-in-prevention-and-control-of-
covid-19-in-indonesia.
19. World Health Organization. Thailand launches “new
normal” health care system to build back better after
COVID-19. World Health Organization. August 11,
2020. https://www.who.int/thailand/news/feature-sto-
ries/detail/thailand-launches-new-normal-healthcare-
system-to-build-back-better-after-covid-19.
20. Republic of the Philippines Department of Health.
DOH boosts telemedicine services for NCR; service
to expand to other regions soon. April 9, 2020. Ac-
cessed January 26, 2021. https://pia.gov.ph/news/
articles/1038518.
21. Republic of the Philippines Department of Health.
DOH’S telemedicine initiative strengthens provision
of primary health care services. August 31, 2020.
https://doh.gov.ph/press-release/DOH%27S-TELE-
MEDICINE-INITIATIVE-STRENGTHENS-PROVI-
SION-OF-PRIMARY-HEALTH-CARE-SERVICES.
22. Van Nguyen H, Van Hoang M, Dao ATM, et al. An
adaptive model of health system organization and
responses helped Vietnam to successfully halt the
COVID-19 pandemic: what lessons can be learned
from a resource-constrained country. Int J Health
Plann Manage 2020;35:988-992. 10.1002/hpm.3004.
23. Nguyen N. Vietnam applies telemedicine platform to
avoid COVID-19 community infection. Hanoi Times.
May 3, 2020. Accessed January 26, 2021. http://ha-
noitimes.vn/vietnam-applies-telemedicine-platform-to-
avoid-community-infection-311954.html.
24. Lam L, Chua Y, Tan D. Roles and challenges of
primary care physicians facing a dual outbreak of
COVID-19 and dengue in Singapore. Fam Pract
2020;37(4):578-579. 10.1093/fampra/cmaa047.
25. Ministry of Health Singapore. COVID-19 Situation Re-
port. Ministry of Health Singapore. Accessed Novem-
ber 2, 2020. https://covidsitrep.moh.gov.sg/.
26. Koh D. Migrant workers and COVID-19. Oc-
cup Environ Med 2020;77:634-636. 10.1136/
oemed-2020-106626.
27. Goh OQ, Islam AM, Lim JCW, Chow W-C. Towards
health market systems changes for migrant workers
based on the COVID-19 experience in Singapore.
BMJ Glob Health 2020;5:e003054. 10.1136/bm-
jgh-2020-003054.
28. The time bombs ‘set to blow’ in Hong Kong’s
COVID-19 fourth wave. South China Morning Post.
Accessed October 27, 2020. https://www.scmp.com/
news/hong-kong/health-environment/article/3104250/
coronavirus-who-will-be-hong-kongs-worst-hit.
29. Quilantang MIN, Bermudez ANC, Operario D. Re
imagining the future of HIV service implementation
in the Philippines based on lessons from COVID-19.
AIDS Behav 2020;24:3003-3005. 10.1007/s10461-
020-02934-x.
66 PRIMARY CARE IN THE COVID-19 PANDEMIC
30. World Health Organization. Minister of Health updates
Western Pacic countries on Lao PDR’s COVID-19
successes & challenges during online meeting.
World Health Organization. October 6, 2020. https://
www.who.int/laos/news/detail/06-10-2020-minister-
of-health-updates-western-pacic-countries-on-lao-
pdr-s-covid-19-successes-challenges-during-online-
meeting.
31. U.S. Department of State Overseas Security Advisory
Council. Health Alert: Laos, Private hospitals and
clinics closed. Washington, DC: U.S. Department
of State Overseas Security Advisory Council, 2020.
https://www.osac.gov/Content/Report/e69341d1-
e0e2-4621-8b46-1858e666c5f9.
32. COVID-19: Hong Kong’s Multi-Pronged Approach.
Accessed October 27, 2020. https://www.brandhk.
gov.hk/uploads/brandhk/les/factsheets/Hong_Kong_
Themes/Factsheet_COVID-19_E.pdf.
33. Li X, Krumholz H, Yip W, et al. Quality of primary
health care in China: challenges and recommenda-
tions. Lancet 2020;395(10239):1802-1812. 10.1016/
S0140-6736(20)30122-7.
34. Post T. ‘Puskesmas’ move up to COVID-19 front
lines amid overburdened health system. The Jakarta
Post. April 13, 2020. Accessed November 3, 2020.
https://www.thejakartapost.com/news/2020/04/13/
puskesmas-move-up-to-covid-19-front-lines-amid-
overburdened-health-system.html.
35. Parrocha A. Duterte submits rst Bayanihan 2 report
to Congress. The Philippine News Agency. October 5,
2020. Accessed January 26, 2021. https://www.pna.
gov.ph/articles/1117593.
36. Dancel R. Philippines rolls out ‘reboot’ of coronavi-
rus response as Manila exits lockdown. The Straits
Times. August 18, 2020. Accessed January 26, 2021.
https://www.straitstimes.com/asia/se-asia/philippines-
rolls-out-reboot-of-coronavirus-response-as-manila-
exits-lockdown.
37. Interim Management Guidance for COVID-19 Ver-
sion 3.1. Republic of the Philippines Department of
Health. July 29, 2020. Accessed October 31, 2020.
https://www.psmid.org/interim-management-guide-
lines-for-covid-19-version-3-1/.
38. Vu K, Nguyen P. Vietnam capital short of test kits as
national coronavirus cases climb. The Jakarta Post.
August 4, 2020. Accessed January 26, 2021. https://
www.thejakartapost.com/seasia/2020/08/04/vietnam-
capital-short-of-test-kits-as-national-coronavirus-
cases-climb.html.
39. Testing for COVID-19 in Laos. Laotian Times. March
17, 2020. Accessed January 26, 2021. https://laotian-
times.com/2020/03/17/testing-for-covid-19-in-laos/.
40. Ratanarat R, Sivakorn C, Viarasilpa T, Schultz MJ.
Critical care management of patients with COVID-19:
early experience in Thailand. Am J Trop Med Hyg
2020;103:48-54. 10.4269/ajtmh.20-0442.
41. Erkhembayar R, Dickinson E, Badarch D, et al.
Early policy actions and emergency response to the
COVID-19 pandemic in Mongolia: experiences and
challenges. Lancet Glob Health 2020;8:e1234-e1241.
10.1016/S2214-109X(20)30295-3.
PRIMARY CARE IN THE COVID-19 PANDEMIC 67
Reproductive Health:
Equity and Innovation
During the COVID-19
Pandemic
Mari Bentley, Cara Delaney, Kelly Treder,
Elisabeth Woodhams, Taylor Weilnau,
and Katherine Gergen Barnett
T
he COVID-19 pandemic has expanded existing disparities and created new barriers in reproduc-
tive health care, especially for women from marginalized and vulnerable communities. Primary
care providers play a central role in alleviating the barriers posed by the pandemic for women
seeking reproductive health care. In this chapter, we provide evidence-based recommendations for
primary care providers to protect their patients’ access to essential contraception and abortion ser-
vices. Our key recommendations include recognizing contraception and abortion as essential care,
leveraging telemedicine services for reproductive health care, adopting clinical innovations that are
both patient-centered and evidence-based, and supporting policy-level measures to protect future
access to care.
The role of primary care in supporting reproductive justice
The COVID-19 pandemic has amplied existing health care disparities and created new obstacles
for women seeking reproductive health care. Women from marginalized or vulnerable communities
have suered disproportionate socioeconomic impact throughout the pandemic—acting simulta-
neously as parents, teachers, and employees (when work from home was feasible).
1
With the as-
sociated economic downturn, nearly one in ten women in the United States is at risk of losing her
employer-sponsored health care coverage.
2
Loss of insurance coverage means loss of reproductive
health care coverage for most of these women.
By impeding access to reproductive health services, the COVID-19 pandemic heavily aects both
people who are low income and people of color. Low-income populations and people of color
already experience greater reproductive health disadvantages compared to higher-income or
white counterparts. For example, 75% of people who have an abortion are poor or low income,
a proportion that increased between 2008 and 2014.
3
Black women experience signicantly
higher rates of nearly every adverse outcome across reproductive health than white women,
and are three to four times more likely to die in pregnancy than white women.
4
The pandemic’s disproportionate impact on women’s reproductive health care is an issue of
Reproductive Justice. The Reproductive Justice movement centers on four human rights: (1)
the right to maintain personal bodily autonomy, (2) the right to have children, (3) the right to
not have children, and (4) the right to parent children in safe and sustainable communities.
5
Primary care providers should be guided by the tenets of Reproductive Justice in their work to
improve reproductive health outcomes. During the crisis, primary care providers have played
a central role in mitigating barriers for patients, showing great ingenuity and adopting nu-
merous innovations that will become the standard of care even after the pandemic recedes.
Recognizing contraception and abortion as essential care
Primary care providers must demand that contraception and abortion be recognized as essen-
tial care. At the outset of the pandemic, dening essential medical services was self-evident
for some types of problems—for example, bleeding in pregnancy—while for others it was
more challenging. What about patients desiring contraception? What about patients desiring
to stop their contraception? What about patients needing to terminate a pregnancy?
At a time when patients are facing heightened personal and nancial uncertainty, preserving
access to reproductive health services is critical. Due to the impact of the pandemic on their
lives, one-third of women overall—and approximately 45% of Black and Hispanic women—
changed their pregnancy-related plans (i.e., they want to either delay pregnancy or have
fewer children).
6
With the reduction in face-to-face medical encounters caused by the COVID-19 stay-at-home
orders, many patients have encountered new barriers when seeking contraceptive care. A sur-
vey of clinics delivering family planning services showed that more than 30% of clinics had
asked patients to postpone the insertion and/or removal of long-acting reversible contracep-
tives (LARC) such as the implant or intrauterine device (IUD).
7
Postponing the desired removal
of a LARC is problematic because it obligates patients to continue to use provider-controlled
contraception against their wishes. The Guttmacher Institute reports that one in three women
reported delays or cancellations in their contraception clinic appointments, a nding that was
more common among Black and Hispanic patients and among patients with an income less
than 200% of the federal poverty threshold.
8
Recognizing abortion as essential care has been even more complex than protecting access to
contraception. In Massachusetts, as well as a handful of other states, abortion was deemed
an essential service and clinics were not compelled to close. Governments in other states,
however, exploited the pandemic for political advantage, further obstructing abortion access
beyond what had been deemed feasible through the courts.
9
Access to abortion is always time-sensitive and has a profound long-term impact for pa-
tients and their families. Protecting abortion access became especially important during the
70 PRIMARY CARE IN THE COVID-19 PANDEMIC
COVID-19 pandemic because pandemic-related challenges changed women’s needs, and such
access preserves Reproductive Justice.
Leveraging telemedicine: Benets and limitations
The second step in preserving access to contraception and abortion is leveraging telemedicine
in primary care practices. The loosening of government rules and regulations by the Centers
for Medicare and Medicaid Services (CMS) during the COVID-19 pandemic allowed for pay
parity across telephone visits, video visits, and in-person visits, as well as the waiving of re-
quirements for an in-person visit before a telemedicine visit.
10
By making telemedicine widely
accessible, these regulatory changes created opportunities for innovation in delivery of health
care services during the pandemic.
The benets of telemedicine have been demonstrated over the past decade by agencies such as
Veterans Aairs, the Indian Health Service, and the Department of Defense, who have shown
that telemedicine reduced patient travel time, increased access to care for rural and disabled
veterans, and expedited care for patients in isolated communities.
11
If we extrapolate these
ndings for people seeking reproductive health care, we can posit that telemedicine improves
health care access by removing barriers caused by hospital and clinic closures, lack of child
care or transportation, work schedules, and nancial constraints.
The rapid deployment of telemedicine predictably uncovered disparities in access to the digital
world. Those who were already disadvantaged—lower income, elderly, rural, dierently abled,
and non-English-speaking populations—were not able to pivot as easily with the rest of the
health care system toward telemedicine.
12
Digital literacy limited patients’ ability to access
remote clinical care,
13
and issues of privacy were also relevant for people sharing physical
space or devices with others. Language barriers only further magnied disparities in access
to telehealth; at one clinic in San Francisco, for example, 14% of patient visits were for non-
English speakers prior to the pandemic, but only 7% after telehealth was instituted.
14
Even as telemedicine creates new access to care, its reliance on technology risks widening the
health equity gap between populations. In the future, telemedicine services must be struc-
tured with an eye to reducing disparities. Specically, to preserve equity for those vulnerable
patients who can participate in telephone but not video visits, it will be important to oer
continued pay parity for providers regardless of visit type.
Despite its limitations, telemedicine is helping to ll in some service gaps for the delivery
of reproductive health services,
8
and it can shorten or entirely replace in-person visits. In a
subsequent section of this chapter, we oer several specic recommendations for primary
care providers on optimizing the use of telemedicine for contraception and abortion care.
PRIMARY CARE IN THE COVID-19 PANDEMIC 71
Streamlining care through the use of evidence-based
practices
The third important action for primary care providers to take during the pandemic is to reas-
sess their clinical practices to ensure they are consistent with current guidelines. This section
addresses evidence-based approaches to reproductive health care that both reduce face-to-
face patient encounters and improve access to care.
Streamlining contraception care
In the United States, the Centers for Disease Control and Prevention sets evidence-based
standards of care around contraception provision.
15
These patient-centered practices are
echoed by other standard-setting organizations
16
and include “quick-start” implementation,
including same-day placement of LARC or administration of injectable depot medroxyproges-
terone acetate (DMPA).
Uptake of the recommended standards, however, has been impeded by the persistence of
non-evidence-based clinical practices,
17
including requiring a pelvic exam and/or cervical
cytology; requiring separate visits for LARC counseling and placement; and delaying the start
of a method until the patient’s next menses.
15,17,18
By eliminating outdated practices, providers
are able to forgo in-person requirements for services such as contraceptive rells, emergency
contraception, and abortion counseling and follow-up.
The pandemic has forced practices to reexamine their workows and move toward adopting
more evidence-based practices. To guide this process, several organizations released urgent
guidance on how to provide eective contraception and abortion care while minimizing
in-person visits.
7,16,19
The innovative practices presented in these evidence-based guidelines
decrease dependence on provider visits, thereby elevating the quality of care while promot-
ing patient-centeredness, autonomy, and safety. Specic innovations will be reviewed here
regarding (1) self-administration of depot medroxyprogesterone acetate (DMPA), (2) insertion
and removal of LARCs, and (3) blood pressure screening prior to prescribing combined hor-
monal contraceptives.
Self-administration of depot medroxyprogesterone acetate
Depot medroxyprogesterone acetate (DMPA) is a highly eective injectable contraceptive,
available in both subcutaneous (SC) and intramuscular (IM) formulations. DMPA is most
commonly administered in the IM formulation, requiring an in-person visit with a clinician
every 13 weeks. The subcutaneous formulation (DMPA SC) is much less commonly available,
but lends itself well to patient self-administration, something in which patients have a dem-
onstrated interest.
20,21
In a randomized controlled trial, a brief educational session successfully
taught patients how to administer their DMPA at home, and these patients reported outcomes
comparable to those of patients receiving the traditional DMPA IM.
22
72 PRIMARY CARE IN THE COVID-19 PANDEMIC
Importantly, DMPA SC and DMPA IM maintain the same contraceptive ecacy.
15
At the start
of the COVID-19 pandemic, the Society of Family Planning recommended that providers con-
sider oering DMPA SC for patient self-administration with a dosing interval up to 15 weeks
as a way to decrease in-person visits.
7
The National Family Planning and Reproductive Health
Association also disseminated a practical guide for physicians, laying out clinical consider-
ations, visual patient instructions, and administrative tips for coding and billing.
23
The provision of DMPA SC allows patients to continue their preferred method of contraception
when that method might otherwise be withheld due to limited clinic access. In a demonstra-
tion project at an urban hospital where a majority of patients had publicly funded insur-
ance, patients successfully navigated the use of DMPA SC. The project models the delivery
of patient-centered care and oers tools and workows to assist other practices, including
guidance on patient recruitment, tips for clinician education, and links to multilingual patient
education materials.
24
Notably, the project also demonstrates how to successfully improve
access when serving a patient population historically isolated by socioeconomic and language
barriers.
Enabling women to self-administer DMPA SC is an eective way to reduce in-person contact
during the pandemic and has the major benet of oering the patient increased privacy and
convenience—rendering it a practice worth sustaining in the long term. For it to be widely
adopted, however, limitations in insurance coverage and cost must be addressed.
20,24
For those patients preferring to continue with the intramuscular formulation of DMPA,
in-person contact can be minimized through telemedicine contraception counseling before
the visit,
7
and by oering “curbside service” for repeat injections.
23
Our own institution
dispatched vans and ambulances into the community to deliver prenatal care, postpartum
follow-up, and DMPA injections (among other services), thereby decreasing patient exposure
to the hospital and removing transportation barriers.
Insertion and removal of long-acting reversible contraceptives
LARCs are highly eective contraceptive methods placed by a provider during a clinic visit.
25
The US Food and Drug Administration (FDA) has approved two types of LARCs—the subder-
mal contraceptive implant, which is placed subcutaneously in the arm, and the IUD. During
the pandemic, clinical guidance issued by the Society of Family Planning provided advice
regarding both LARC insertions and removals.
7
LARC insertion
Contraception decision making is a values-based process in which the patient weighs a vari-
ety of personal priorities. To support this process, it is imperative for providers to engage in a
shared decision-making counseling model to help the patient integrate their personal priori-
ties with medical knowledge before reaching their decision. Providers who focus solely on the
clinical ecacy (especially of LARCs) risk promoting certain methods above others and giving
biased, non-patient-centered counseling. Awareness of such biases is especially important
PRIMARY CARE IN THE COVID-19 PANDEMIC 73

when caring for populations experiencing reproductive coercion, specically low-income
patients and people of color.
26,27
When a patient chooses a LARC during the pandemic, it may be appropriate to explore the
possibility of delaying the insertion in the interest of minimizing in-person encounters and to
oer other short-term options. However, LARC insertion should be scheduled if requested by
the patient.
7
Several practices with regard to LARC insertion are important during the pandemic and
beyond. (1) The counseling portion of the visit should occur via telemedicine to shorten face-
to-face contact during the insertion.
19
(2) LARC insertion should not be delayed for results of
screening tests (e.g., for sexually transmitted infection or cervical dysplasia).
15
(3) All LARCs
can be placed immediately postpartum, after surgical abortion, and after completed medica-
tion abortion.
25
(4) The etonogestrel implant can be placed at the initiation of medication
abortion.
28
Finally, (5) LARCs should be oered as safe and eective methods for all women,
including nulliparous patients and adolescents.
25
LARC removal
The pandemic shone light on both ethical and clinical considerations for LARC removals. From
an ethical standpoint, it is important to honor a patient’s request for LARC removal because
that request constitutes a withdrawal of their consent to use the method. Informed consent at
the time of device placement includes a clear agreement that the device will be removed when
the patient chooses, and denying removal during the pandemic eectively coerces the patient
to continue its use. The imperative to respect patient autonomy looms large when caring for
populations that have been coerced in the past to use temporary or permanent contracep-
tive methods. In the interest of preserving individual reproductive autonomy, LARC removals
should be scheduled when requested by the patient.
From a clinical standpoint, the pandemic elevated the importance of using ecacy data on
the use of several LARC devices beyond the FDA-approved time frame. The contraceptive im-
plant, the 52 mg-LNG IUDs, and the copper IUD each have data supporting their extended use
beyond FDA-approved time frames.
29-32
Removal of these devices can safely be deferred, if the
patient desires, until the evidence-based duration of use as described in Table 1. The duration
Table 1. Evidence-Based Lengths of Use for LARC Devices
Device FDA-Approved Use Evidence-Based Use
Etonogestrel Implant (Nexplanon) 3 years 5 years
29,30
52 mg-LNG IUD (Mirena)
52 mg-LNG IUD (Liletta)
5 years
6 years
7 years
29–32
TCu380A (Paragard) 10 years 12 years
31,32
74 PRIMARY CARE IN THE COVID-19 PANDEMIC
of eectiveness for levonorgestrel IUDs not listed in Table 1 is still under investigation and
extended use is not recommended at this time.
25
For patients requesting LARC removal, a telemedicine visit can be used to discuss any con-
cerns or side eects the patient may be experiencing, and to explore whether the patient de-
sires another method. For patients specically desiring IUD removal, providers may oer the
option of self-removal.
7
Among patients attempting self-removal, one in ve is successful.
33
Blood pressure screening for combined hormonal contraceptives
Combined oral contraceptive (COC) pills are the most commonly prescribed reversible contra-
ceptive, with an estimated 9 million users in 2015-2017.
34
COCs, along with other combined
hormonal contraceptives (CHCs) (i.e., the intravaginal ring and transdermal patch), have the
benet of not requiring an in-person visit with a provider and can be initiated and discontin-
ued by the patient independently once a prescription has been issued.
A challenge during the COVID-19 pandemic was to measure blood pressure before CHC initia-
tion, a practice that has been the standard of care to mitigate the elevated cardiovascular risk
of CHC use among hypertensive patients.
15
The need to screen for elevated blood pressure
prior to initiating CHCs could be addressed in a number of ways. For example, it is accept-
able to rely on self-reported blood pressure measurements, with patients taking their blood
pressure at home or in a pharmacy.
15
Given that the US Preventive Services Task Force recom-
mends blood-pressure screening every three to ve years, it is also acceptable to rely on a
reading recorded in the medical record within the past ve years.
19
If neither is available due
to the pandemic, providers may prescribe CHCs after screening for a history of elevated blood
pressure and counseling patients about cardiovascular risks associated with CHC use if they
have elevated blood pressure. Providers could schedule a subsequent in-person visit for blood
pressure assessment when feasible.
35
In accordance with the standard of care in place prior to the pandemic, providers may pre-
scribe a one-year supply of CHCs. This practice is associated with increased continuation of
the method.
15
During the pandemic, oering a one-year supply of CHCs is encouraged, as is
the use of mail order for prescriptions.
7
Streamlining medication abortion care
A joint statement by the American College of Obstetricians and Gynecologists (ACOG) and
several other national organizations in March 2020 unequivocally stated that “abortion is an
essential component of comprehensive healthcare [and is] a time-sensitive service for which
a delay of several weeks, or in some cases days, may increase the risks or potentially make it
completely inaccessible.”
36
By adopting innovative but evidence-based protocols, providers
were able to continue medication abortion services throughout the pandemic. These innova-
tions were both feasible and patient-centered, and thus may endure into the future.
While medication abortion is a safe and eective way to end early pregnancy, access has been
hindered by barriers such as child care, work obligations, transportation issues, and nancial
PRIMARY CARE IN THE COVID-19 PANDEMIC 75
obstacles. These barriers were compounded during the COVID-19 pandemic by new challenges
such as stay-at-home directives and diculty accessing ultrasound and laboratory services
due to clinic closures. To address these barriers and support practices oering medication
abortion, new “no-test” protocols have been developed, supporting provision of remote
medication abortion.
33-38, 43, 44
The delivery of no-test medication abortion via telemedicine was supported by several or-
ganizations, including ACOG, the National Abortion Federation, Reproductive Health Access
Project, and the Society of Family Planning.
36-38,43
The no-test protocols were determined
to be safe and eective, with outcomes comparable to prepandemic practice.
40,42,44
Several
provider toolkits and sample protocols were also made available.
43,45
Using specic criteria,
patients were able to avoid a pretreatment ultrasound, physical exam, and laboratory testing,
and receive timely medication abortion care without an in-person visit. The approach was an
option for patients who were certain of the date of their last menstrual period (LMP), were
less than 77 days since LMP, had no contraindications, and had no risk factors for ectopic
pregnancy.
40-41
Prepandemic care models required three tests prior to initiation of medication abortion,
including an ultrasound (or bimanual exam) for pregnancy dating, Rh testing, and hemoglo-
bin screening. In contrast, no-test protocols relied on reported LMP for pregnancy dating,
the accuracy of which is well supported.
46
International evidence revealed that Rh sensitiza-
tion is highly unlikely before 56 days since LMP, and new guidelines forgo Rh testing until
then.
47
Evidence also suggests Rh testing may not be necessary until 70 days since LMP.
48
Additionally, the need for pre-abortion hemoglobin testing can be determined by screening
for a prior history of anemia or any current symptoms.
47
A number of barriers prevented providers from adopting a no-test approach to medication
abortion. Some providers expressed discomfort about potential adverse outcomes such as
missing a more advanced gestational age
46
or an ectopic pregnancy, although their concerns
were not supported by data.
40,42
Using pre-abortion screening questions, providers were able
to oer services to patients without a known adverse outcome of ectopic pregnancy.
40,42
Some
states prohibited distributing mifepristone by mail or by pharmacy; however, clinics creatively
overcame these obstacles in the short run by oering curbside pickup from a clinic sta
member or using clinic outdoor lockers with a passcode.
45
The greatest barrier to medication abortion provision was that, despite ample safety data, the
FDA designated mifepristone as a drug that requires a Risk Evaluation and Mitigation Strategy
(REMS). The REMS designation made it impossible for mifepristone to be dispensed in phar-
macies and requires prescribing providers to register with both the product distributor and
the FDA. In the summer of 2020, the American Civil Liberties Union successfully challenged
the REMS, removing the in-person provider dispensing requirement and allowing for mail
delivery from a registered provider during the COVID-19 public health emergency. Providers
still had to consider state-based regulations, however, before implementing changes to their
protocols to overcome the REMS barrier.
49
76 PRIMARY CARE IN THE COVID-19 PANDEMIC
While oering no-test medication abortion was not feasible for all clinics, it was still possible
to oer remote follow-up. Before the pandemic, medication abortion follow-up was typi-
cally performed by a provider using ultrasound examination or serial serum human chorionic
gonadotropin testing.
7
New remote follow-up options during COVID-19 included high-
sensitivity pregnancy testing about one month after the medication abortion or a telemedicine
visit based solely on patient symptoms. Both models had results comparable to an in-oce
follow-up visit.
40,50,51
Patients have also been turning to self-managed abortion due to diculties with access-
ing local medication abortion. Online services use a no-test protocol with mifepristone and
misoprostol for gestations up to 10 weeks, and consultations through the site are reviewed by
a physician. People that use this service are given precautions for bleeding, pain, infection,
and signs of ongoing pregnancy, as well as being advised to seek emergency care if needed.
52
In the rst month of the COVID-19 pandemic, one organization that provides self-managed
abortions saw a 27% increase in requests in the United States, with more signicant increases
in states with either high COVID-19 rates or more strict stay-at-home orders.
53
The COVID-19 pandemic encouraged rapid adoption of novel, evidence-based strategies for
convenient, patient-centered medication abortion services in the United States. These options
have been safe and eective, provide improved access for patients, and support the physical
distancing required by stay-at-home restrictions. The new services will likely continue to
experience demand because they are based in evidence and allow patients to have an abortion
in the privacy of their own home at a time that works best for them.
Beyond clinical care: Needed policy measures
Finally, while practices have been nimble in responding to new pressures during the
COVID-19 pandemic, changes in clinical practice alone will not suce to protect access to
needed contraception and abortion care. Primary care practices will need to advocate for pol-
icy-level changes as a vital next step, particularly with regard to regulation and funding for
reproductive health services. Additional policy-level initiatives, beyond pay parity in telemed-
icine, include permanently removing the REMS requirement for mifepristone, expanding the
prescription of oral contraceptives by pharmacists, oering CHCs over the counter, expanding
health insurance coverage of contraceptives, and passing the Women’s Health Protection Act.
Mifepristone and the REMS
Permanent removal of the REMS requirement for mifepristone is a necessary step in promot-
ing comprehensive reproductive health care. The REMS currently obstructs access not only
to exceptionally safe early abortion, but also to evidence-based medical management of early
miscarriage as well as highly eective emergency contraception.
54,55
The unnecessary REMS
status imposes cumbersome barriers for hospitals, providers, and patients; renders mifepris-
tone functionally inaccessible; and forces patients to endure less eective clinical treatments.
PRIMARY CARE IN THE COVID-19 PANDEMIC 77
Oral contraceptive prescription by pharmacists
Pharmacists are authorized to prescribe hormonal contraception in 13 states and the District
of Columbia.
56
The prescription of oral contraception by pharmacists is well received by
women
57
and appealing to pharmacists, 85% of whom reported being interested in provid-
ing hormonal contraception services.
58
Although the pharmacist prescription model has the
advantage of decentralizing care and increasing access, it has not become widespread due
to such barriers as stang, liability, and training needs.
59
Notably, the innovation retains the
barrier of requiring a prescription. The most streamlined version of the pharmacist prescribing
model is PRJKT RUBY, a nonprot organization oering online birth control and provider consul-
tation, along with follow-up care and extended rells.
56
Pharmacies interested in prescribing oral
contraceptives can nd online support from Birth Control Pharmacist—a project oering online
courses with continuing education credit to help pharmacies implement contraceptive services.
57
Over-the-counter oral contraceptives
National organizations such as the American Academy of Family Physicians, the American
Medical Association, and ACOG previously endorsed over-the-counter oral contracep-
tives.
55,59-60
Patients have found over-the-counter oral contraceptives to be convenient and
desirable; evidence suggests that over-the-counter use of oral contraceptives is safe and may
lead to improved continuation of eective contraception.
62-64
During the COVID-19 pandemic and beyond, oering over-the-counter oral contraceptives
could liberate patients from a restrictive model of care necessitating provider involvement, in
favor of a more exible and patient-centered approach.
Health insurance coverage of contraceptives
Contraceptive care has been recognized as an essential component of well-woman care, and
all methods should be covered by all private and public insurances with little or no out-of-
pocket cost.
8,62
Coverage should include all traditional and innovative routes of administration
and modes of delivery (e.g., self-administered DMPA SC, pharmacy-prescribed oral contra-
ceptives, over-the-counter contraceptives, and online pharmacy services). All states should
participate in Medicaid expansion under the Aordable Care Act, rendering basic health care
and contraceptive services accessible to vulnerable populations.
8,17
Funding for the federal
Title X Family Planning Program—which provides comprehensive family planning and related
preventive health services—should be sucient to ensure that low-income women also have
adequate access to contraception.
8,17
Title X funding should include coverage of immediate
contraception after surgical abortion.
17
Women’s Health Protection Act
Beyond specic policy changes supporting innovative contraceptive and abortion care delivery,
more comprehensive change is needed at the national level to assure all patients have access
to the reproductive health care they need, particularly those from communities that have been
historically and contemporarily oppressed.
78 PRIMARY CARE IN THE COVID-19 PANDEMIC
Congress must support legislation protecting these human rights and should pass the
Women’s Health Protection Act, which is grounded in the fundamental tenets of Reproductive
Justice. This act seeks “to protect a woman’s ability to determine whether and when to bear a
child or end a pregnancy, and to protect a health care provider’s ability to provide reproduc-
tive health care services, including abortion services.”
65
Collectively, measures such as these will both improve care during the pandemic and provide
long-term benets to all women.
66
Primary care providers are natural patient advocates;
extending that role to policy-level advocacy aimed to improve their patients’ lives and the
quality of care they receive is a natural partnership.
Conclusions
The COVID-19 pandemic has disrupted routine clinical care, compelling providers to reexam-
ine deep-rooted practice patterns in order to adapt to new pressures. This disruption resulted
in the unintended yet fortunate consequences of moving practices in the direction of greater
patient-centeredness and triggering the adoption of more evidence-based clinical practices.
Looking to the future, it will be important to sustain these new practice patterns and preserve
the innovations that serve our patients well. For example, providers should forgo unnecessary
practices that delay the initiation of contraception (such as requiring a pelvic exam, testing
for STIs, or waiting until the patient’s next menses). Innovations in the delivery of contra-
ceptive and medication abortion care are well studied and should continue to be implemented.
These include DMPA SC self-administration, remote provision of CHC, no-test medication
abortion, and telephone follow-up after medical abortion. All of these innovations and adap-
tations should remain within routine and recommended clinical standards of care.
Protecting access to reproductive health care is important in all communities, but especially
so for those most vulnerable. Some of these innovations allow us to creatively address re-
productive health inequities—for instance, by improving access through telemedicine for
people with transportation or child care barriers. Nonetheless, we must remain alert to new
disparities that arise as a result of these new models of care delivery. For example, while
telemedicine may increase access for some, it may introduce new barriers for those who have
limited access to technology or limited literacy in using it. Since much of reproductive health
care remains essential even amidst the most stringent lockdowns, it is of critical importance
for primary care providers to oer these services. It is in those moments of great crisis that
marginalized communities are at risk of even greater reproductive health inequities.
As primary care providers, we must use the momentum of ingenuity to elevate other initia-
tives stymied by legal restrictions, competing priorities, or inertia. Supporting eorts to
make oral contraceptives available over the counter and to remove the REMS restrictions from
mifepristone has never been more critical.
COVID-19 has wrought devastation locally and globally, but has also provided new op-
portunities in health care. It is our obligation to use this opportunity to decrease barriers to
reproductive health care access, increase the patient-centeredness of the care we provide, and
promote and protect all of the tenets of Reproductive Justice.
PRIMARY CARE IN THE COVID-19 PANDEMIC 79
References
1. Wenham C, Smith J, Davies SE, et al. Women are
most affected by pandemics—lessons from past
outbreaks. Nature 2020;583(7815):194-8. 10.1038/
d41586-020-02006-z.
2. Soneld A, Frost JJ, Dawson R, Lindberg LD.
COVID-19 job losses threaten insurance coverage
and access to reproductive health care for mil-
lions. Health Affairs Blog. August 3, 2020. Accessed
January 27, 2021. https://www.healthaffairs.org/
do/10.1377/hblog20200728.779022/full/.
3. Jerman J, Jones RK, Onda T. Characteristics of U.S.
Abortion Patients in 2014 and Changes Since 2008.
New York: Guttmacher Institute, 2016. https://www.
guttmacher.org/report/characteristics-us-abortion-
patients-2014#.
4. Moaddab A, Dildy GA, Brown HL, et al. Health care
disparity and pregnancy-related mortality in the United
States, 2005-2014. Obstet Gynecol 2018;131(4):707-
12. 10.1097/AOG.0000000000002534
5. Ross L, Solinger R. Reproductive justice: an introduc-
tion. Vol 1. Berkeley: University of California Press,
2017.
6. Lindberg LD, Vande Vusse A, Mueller J, Kirstein M.
Early Impacts of the COVID-19 Pandemic: Findings
From the 2020 Guttmacher Survey of Reproductive
Health Experiences. New York: Guttmacher Institute,
2020. https://www.guttmacher.org/report/early-im-
pacts-covid-19-pandemic-ndings-2020-guttmacher-
survey-reproductive-health.
7. Benson LS, Madden T, Tartelon J, Micks EA. Society
of Family Planning interim clinical recommendations:
contraceptive provision when healthcare access
is restricted due to pandemic response. Society
of Family Planning. First published April 24, 2020.
Updated May 28, 2020. Accessed October 16, 2020.
https://societyfp.org/wp-content/uploads/2020/08/
SFP-Interim-Recommendations-Contraception-and-
COVID-19_05.28.2020_doi.pdf.
8. Lindberg L, VandeVusse D, Mueller A, Kirstein J,
Mariell. Early Impacts of the COVID-19 Pandemic:
Findings From the 2020 Guttmacher Survey of Repro-
ductive Health Experiences. New York: Guttmacher
Institute, 2020. https://www.guttmacher.org/sites/
default/les/report_pdf/early-impacts-covid-19-pan-
demic-ndings-2020-guttmacher-survey-reproductive-
health.pdf.
9. Jones RK, Lindberg L, Witwer E. COVID‐19 abortion
bans and their implications for public health. Per-
spect Sex Reprod Health 2020;52(2):65-8. 10.1363/
psrh.12139.
10. Trump administration issues second round of sweep-
ing changes to support U.S. healthcare system during
COVID-19 pandemic. Centers for Medicare and Med-
icaid Services. April 30, 2020. Accessed January 27,
2021. https://www.cms.gov/newsroom/press-releases/
trump-administration-issues-second-round-sweeping-
changes-support-us-healthcare-system-during-covid.
11. Elliott V. Telehealth and telemedicine: description
and issues. R44437. Version 5. Washington, DC:
Congressional Research Service, 2016. https://www.
senate.gov/CRSpubs/757e3b90-ff10-497c-8e8c-
ac1bdbdb3aaf.pdf.
12. Aronson L. Evidence, efcacy, and economics—
a better path forward for US health. JAMA Netw
Open 2020;3(8):e2016118. 10.1001/jamanet-
workopen.2020.16118.
13. Rodriguez JA, Clark CR, Bates DW. Digital health
equity as a necessity in the 21st Century Cures
Act era. JAMA 2020;323(23):2381-2. 10.1001/
jama.2020.7858.
14. Nouri SS, Khoong EC, Lyles CR, Karliner LS. Ad-
dressing equity in telemedicine for chronic disease
management during the COVID-19 pandemic. NEJM
Catalyst May 4, 2020. 10.1056/CAT.20.0123.
15. Curtis KM, Jatlaoui TC, Tepper NK, et al. U.S. Select-
ed Practice Recommendations for Contraceptive Use,
2016. MMWR Recomm Rep 2016;65(No. RR-4):1-66.
10.15585/mmwr.rr6504a1.
16. Contraception in the time of COVID-19. Reproductive
Health Access Project. March 2020. Accessed Janu-
ary 27, 2021. https://www.reproductiveaccess.org/
resource/contraception-covid/.
17. Committee opinion no. 615: access to contraception.
Obstet Gynecol 2015;125(1):250-255. 10.1097/01.
AOG.0000459866.14114.33.
18. Lesnewski R, Prine L. Initiating hormonal contracep-
tion. Am Fam Physician 2006;74(1):105-112.
19. Ensuring access to family planning services dur-
ing COVID-19: a summary of CDC’s family planning
recommendations for healthcare providers. Centers
for Disease Control and Prevention. Last reviewed
August 17, 2020. Accessed January 27, 2021. https://
www.cdc.gov/reproductivehealth/contraception/covid-
19-family-planning-services.html.
20. Upadhyay UD, Zlidar VM, Foster DG. Interest in
self-administration of subcutaneous depot medroxy-
progesterone acetate in the United States. Contra-
ception 2016;94(4):303-13. 10.1016/j.contracep-
tion.2016.06.006.
80 PRIMARY CARE IN THE COVID-19 PANDEMIC
21. Kohn JE, Simons HR, Della Badia L, et al. Increased
1-year continuation of DMPA among women random-
ized to self-administration: results from a randomized
controlled trial at Planned Parenthood. Contracep-
tion 2018;97(3):198-204. 10.1016/j.contracep-
tion.2017.11.009.
22. Beasley A, White KOC, Cremers S, Westhoff C. Ran-
domized clinical trial of self versus clinical administra-
tion of subcutaneous depot medroxyprogesterone
acetate. Contraception 2014;89(5):352-6. 10.1016/j.
contraception.2014.01.026.
23. National Family Planning & Reproductive Health
Association. Self-Administration of Injectable
Contraception, Second Edition, Updated April 20,
2020. https://www.nationalfamilyplanning.org/le/
documents---service-delivery-tools/NFPRHA---Depo-
SQ-Resource-guide---FINAL-FOR-DISTRIBUTION.
pdf.
24. Katz M, Newmark RL, Aronstam A, et al. An imple-
mentation project to expand access to self-adminis-
tered depot medroxyprogesterone acetate (DMPA).
Contraception 2020;102(6):392-5. [Online ahead of
print] 10.1016/j.contraception.2020.09.001.
25. Committee on Practice Bulletins–Gynecology; Espey
E, Hoer L. Clinical management guidelines for
obstetrician-gynecologists: long-acting reversible con-
traception: implants and intrauterine devices. ACOG
Practice Bulletin No. 186. 2017;130(5):251-69.
26. Long-acting reversible contraception: statement of
principles. Atlanta, GA: Sister Song and National
Women’s Health Network, 2017. https://www.nwhn.
org/wp-content/uploads/2017/02/LARCStatementof-
Principles.pdf.
27. Higgins JA. Celebration meets caution: LARC’s
boons, potential busts, and the benets of a reproduc-
tive justice approach. Contraception 2014;89(4):237-
41. 10.1016/j.contraception.2014.01.027.
28. Hognert H, Kopp Kallner H, Cameron S, et al. Im-
mediate versus delayed insertion of an etonogestrel
releasing implant at medical abortion: a random-
ized controlled equivalence trial. Hum Reprod
2016;31(11):2484-90. 10.1093/humrep/dew238.
29. McNicholas C, Swor E, Wan L, Peipert JF. Prolonged
use of the etonogestrel implant and levonorgestrel
intrauterine device: 2 years beyond Food and Drug
Administration–approved duration. Am J Obstet
Gynecol 2017;216(6):586.e1-586.e6. 10.1016/j.
ajog.2017.01.036.
30. Ali M, Bahamondes L, Landoulsi SB. Extended ef-
fectiveness of the etonogestrel-releasing contracep-
tive implant and the 20 mg levonorgestrel-releasing
intrauterine system for 2 years beyond U.S. Food and
drug administration product labeling. Glob Health Sci
Pract 2017;5(4):534-539. 10.9745/GHSP-D-17-00296.
31. Wu JP, Pickle S. Extended use of the intrauterine
device: a literature review and recommendations for
clinical practice. Contraception 2014;89(6):495-503.
10.1016/j.contraception.2014.02.011.
32. Ti AJ, Roe AH, Whitehouse KC, Smith RA, Gafeld
ME, Curtis KM. Effectiveness and safety of extending
intrauterine device duration: a systematic review. Am
J Obstet Gynecol 2020;223(1):24-35.e3. 10.1016/j.
ajog.2020.01.014.
33. Foster DG, Grossman D, Turok DK, et al. Interest
in and experience with IUD self-removal. Contra-
ception 2014;90(1):54-9. 10.1016/j.contracep-
tion.2014.01.025.
34. Daniels K, Abma JC. Current contraceptive status
among women aged 15-49: United States, 2015-
2017. National Center for Health Statistics Data
Brief No. 327. December 2018. Accessed January
27, 2021. https://www.cdc.gov/nchs/data/databriefs/
db327-h.pdf.
35. Joint statement on abortion access during the
COVID-19 outbreak. American College of Obstetri-
cians and Gynecologists. March 18, 2020. Accessed
January 27, 2021. https://www.acog.org/news/news-
releases/2020/03/joint-statement-on-abortion-access-
during-the-covid-19-outbreak.
36. ACOG practice bulletin: medication abortion up to 70
days of gestation. Contraception 2020;102(4):225-236
37. NAF Sample Guideline: Medication Abor-
tion Telephone Follow-Up. Washington,
DC: National Abortion Federation, 2020.
https://5aa1b2xfmfh2e2mk03kk8rsx-wpengine.
netdna-ssl.com/wp-content/uploads/Telephone-follow-
up-for-medication-abortion.pdf.
38. No touch medication abortion protocol. Reproductive
Health Access Project. March 26, 2020. Accessed
January 27, 2021. https://www.reproductiveaccess.
org/resource/no-touch-mab-protocol/.
39. Raymond E, Grossman D, Mark A, et al. No-test
medication abortion: a sample protocol for increasing
access during a pandemic and beyond. Contraception
2020;101(6):361-366.
40. Raymond EG, Tan YL, Grant M, et al. Self-
assessment of medical abortion outcome using
symptoms and home pregnancy testing. Contra-
ception 2018;97(4):324-8. 10.1016/j.contracep-
tion.2017.12.004.
41. Aiken ARA, Digol I, Trussell J, Gomperts R. Self-
reported outcomes and adverse events after medi-
cal abortion through online telemedicine: population
based study in the Republic of Ireland and Northern
Ireland. BMJ 2017;357:1-8. 10.1136/bmj.j2011.
PRIMARY CARE IN THE COVID-19 PANDEMIC 81
42. University of Washington; Plan C. Access, delivered:
a toolkit for providers offering medication abortion.
University of Washington Medicine. 2020. https://fami-
lymedicine.uw.edu/accessdelivered/.
43. Schonberg D, Wang LF, Bennett AH, Gold M,
Jackson E. The accuracy of using last menstrual
period to determine gestational age for rst trimester
medication abortion: a systematic review. Contra-
ception 2014;90(5):480-487. 10.1016/j.contracep-
tion.2014.07.004.
44. NAF Sample Guideline: Providing Medication Abor-
tion with No Pre-Treatment Testing. Washington, DC:
National Abortion Federation, 2020. (This guideline is
only available to NAF members. To join NAF, please
contact [email protected][insert period as
regular text before the parenthesis].)
45. Horvath S, Tsao P, Huang ZY, et al. The concentra-
tion of fetal red blood cells in rst-trimester pregnant
women undergoing uterine aspiration is below the
calculated threshold for Rh sensitization. Con-
traception 2020;102(1):1-6. 10.1016/j.contracep-
tion.2020.02.011.
46. Telemedicine Policies: Board by Board Overview.
Washington, DC: Federation of State Medical Boards,
2020. https://www.hollandhart.com/pdf/telemedicine_
policies_by_state.pdf.
47. Chen MJ, Rounds KM, Creinin MD, Cansino C, Hou
MY. Comparing ofce and telephone follow-up after
medical abortion. Contraception 2016;94(2):122-126.
10.1016/j.contraception.2016.04.007.
48. Perriera LK, Reeves MF, Chen BA, Hohmann
HL, Hayes J, Creinin MD. Feasibility of telephone
follow-up after medical abortion. Contracep-
tion 2010;81(2):143-149. 10.1016/j.contracep-
tion.2009.08.008.
49. Home page. Aid Access. https://aidaccess.org/.
50. Aiken ARA, Starling JE, Gomperts R, Tec M, Scott
JG, Aiken CE. Demand for self-managed online
telemedicine abortion in the united states during the
coronavirus disease 2019 (COVID-19) pandemic.
Obstet Gynecol 2020;136(4):835-837. 10.1097/
AOG.0000000000004081.
51. Schreiber CA, Creinin MD, Atrio J, Sonalkar S,
Ratcliffe SJ, Barnhart KT. Mifepristone pretreatment
for the medical management of early pregnancy loss.
N Engl J Med 2018; 378(23):2161-70. 10.1056/nej-
moa1715726.
52. Von Hertzen H, Piaggio G, Ding J, et al. Low dose
mifepristone and two regimens of levonorgestrel
for emergency contraception: a WHO multicentre
randomised trial. Lancet 2002;360(9348):1803-10.
10.1016/S0140-6736(02)11767-3.
53. World Health Organization. Comparison of three
single doses of mifepristone as emergency contracep-
tion: a randomised trial. Lancet 1999;353:697-702.
54. Home page. Power to Decide. https://wwww.powerto-
decide.org.
55. Gardner J, James E, Downing D, Miller L, Shotor-
bani S, Le S. Acceptability of Pharmacist Prescribed
Hormonal Contraceptives for Healthy Women In the
Direct Access Study. Abstracts, Contraception 74
(2006):185.
56. American College of Obstetricians and Gynecolo-
gists. Over-the-Counter Access to Hormonal Con-
traception. Committee opinion no. 788. October
2019. https://www.acog.org/clinical/clinical-guidance/
committee-opinion/articles/2019/10/over-the-counter-
access-to-hormonal-contraception.
57. Gomez A, Availability of Pharmacist-Pre-
scribed Contraception in California, 2017.
JAMA. 2017;318(22):2253-2254. doi:10.1001/
jama.2017.15674.
58. Home page. PRJKT Ruby. https://www.prjktruby.com.
59. Training courses. Birth Control Pharmacist. https://
birthcontrolpharmacist.com/training/.
60. Coverage, patient education, and counseling for fam-
ily planning, contraceptive methods, and sterilization
procedures. American Academy of Family Physicians.
2019. Accessed January 27, 2021. https://www.aafp.
org/about/policies/all/family-planning.html.
61. Contraception: Over-the-Counter Access to Oral Con-
traceptives D-75.995. American Medical Association.
https://policysearch.ama-assn.org/policynder/detai
l/*?uri=%2FAMADoc%2Fdirectives.xml-0-2035.xml.
Accessed October 20, 2020.
62. Grossman D. Over-the-counter access to oral
contraceptives. Obstet Gynecol Clin North Am
2015;42(4):619-29. 10.1016/j.ogc.2015.07.002.
63. Grossman D. The potential impact of over-the-counter
access to oral contraceptives to reduce unintended
pregnancy. Am Fam Physician 2015;92(11):968-9.
64. Grossman D, Grindlay K, Li R, Potter JE, Trussell
J, Blanchard K. Interest in over-the-counter access
to oral contraceptives among women in the United
States. Contraception 2013;88(4):544-552. 10.1016/j.
contraception.2013.04.005.
65. S. 1645, Women’s Health Protection Act. 116th Cong.
(2019).
66. Ahmed Z, Cross L. Crisis on the Horizon: Devastating
Losses for Global Reproductive Health Are Possible
Due to COVID-19. New York: Guttmacher Institute,
2020. https://www.guttmacher.org/article/2020/04/
crisis-horizon-devastating-losses-global-reproductive-
health-are-possible-due-covid.
82 PRIMARY CARE IN THE COVID-19 PANDEMIC
COVID-19 and
Oral Health
Lisa Simon
A
lthough integral to ensuring overall health and function, oral health care remains largely
separate from the broader US health care system, and parallel to most primary care delivery.
The separation between oral health and primary care is perhaps no better exemplied than in the
response of dentistry to COVID-19. Adaptations in the dental care system throughout the pandemic
have been largely driven by economic considerations more akin to those of other small business
interests than to the broader health care system and public health response. Nevertheless, changes
in infection control, patient testing and access, and mobile health platforms enacted during the
pandemic have implications for the future of oral health and its relationship with the health care
system from which it has been historically excluded.
A prepandemic snapshot of the oral health care
delivery system
The origin of dentistry’s separation from medicine has its roots in the establishment of the na-
tion’s rst dental schools by physicians in the 1840s to 1860s. The bifurcated training path be-
tween physicians and dentists, producing separate practitioners, was followed by the independent
development of medical insurance in the 1920s and dental insurance in the 1940s.
1
Unlike medical
insurance, dental “insurance” was originally conceived as a discount plan, providing full coverage
for lower-cost preventive procedures and decreasing levels of cost sharing for more expensive in-
terventions, a model that persists today. The 1965 passage of Medicare and Medicaid, both of which
initially excluded dental coverage, facilitated a nancial system of dental delivery disconnected
from larger health systems and reimbursement structures.
2,3
The separation of dentistry from medicine had lasting implications for the practice of dentistry
in the United States. As of February 2020, the average general dentist worked in a solo private
practice or with a few other dentists and fewer than ve employees.
4
Dental specialists, such as
orthodontists, endodontists (dentists with a specialty in performing root canals), and periodontists
(dentists with a specialty in the gingiva) were even more likely to work in private practice. While
consolidation has occurred in dentistry, with a relatively high rate of increase in the number of
large-group dental practices (analogous to similar consolidation within the medical system),
such practices still make up a small minority of all dental practices and most continue to
operate in a private practice, business-ownership model.
5,6
Only about 2% of the nation’s
200,419 dentists worked in a public health setting such as a Federally Qualied Health Center,
correctional facility, or tribal clinic, and even fewer, less than 1%, practiced in integrated set-
tings with other health care providers, such as a hospital.
7
Before the pandemic, fewer Americans visited a dentist than other health providers each
year—while 84.3% of adults visited a medical clinician in 2018, only 64% had a dental visit.
8
Almost four times as many Americans lacked dental insurance as lacked medical insurance,
as 73.5 million Americans lacked dental insurance in 2018. Nearly half of the population
was enrolled in a private dental plan, while 23% received benets through public insurance,
predominantly Medicaid.
9
Though Medicaid and the Children’s Health Insurance Plan (CHIP)
are required to provide comprehensive dental benets to all low-income children through the
Early and Periodic Screening, Diagnostic and Treatment (EPSDT) mandate, dental coverage
for Medicaid-enrolled adults is elective and varies at the state level. Twelve states provide
only emergency coverage (e.g., tooth extraction for severe dental infection), while 35 oer a
broader scope of services; however, extent of coverage, mandated copays, and annual cover-
age maxima vary considerably among states.
10,11
Small increases in rates of dental coverage in
the ve years prior to the COVID-19 pandemic were largely driven by expanded adult dental
coverage through Medicaid expansion due to the Aordable Care Act.
12
Traditional Medicare
oers no dental coverage, and only 12% of Medicare beneciaries have dental coverage,
mostly through Medicare Advantage plans that include dental benets (and with the minority
purchasing a stand-alone dental benet plan).
2,13
Regardless of payer, almost the entirety of
dental care in the United States is funded through a fee-for-service model.
Dental insurance is not a guarantor of access to dental care, with more Americans reporting
nancial concerns as a barrier to dental access than for other forms of health care.
3
Because
dental insurance is typically structured as consumer discounts, rather than indemnity cover-
age for unanticipated expenses, a “paradox of dental need” has been described, in which
patients with the most intensive oral health needs are the least able to aord treatment.
14
Older adults, the population least likely to have dental insurance, spent an average of $900
out of pocket per year on dental needs.
13
Low dentist participation rates in public insurance
programs across the nation can make access challenging even when dental coverage exists.
For example, in 2018, 80% of children from families living below 200% of the federal poverty
level had an annual dental visit, compared to 91% of those making 400%.
15
The traditional structure of dental delivery and fewer pressures for innovation than the rest of
the primary care system have resulted in profound inequities in oral health outcomes. Black,
Latinx, and American Indian and Alaska Native children and adults all have higher rates of
untreated dental disease than white Americans.
16
High-risk groups including rural dwellers,
17
people with disabilities,
18
people with a history of incarceration,
19
people with chronic medical
conditions,
20,21
and institutionalized older adults
22
all face reduced dental access and poor out-
comes. With minimal dental coverage available to many low-income adults, income remains
84 PRIMARY CARE IN THE COVID-19 PANDEMIC
an unjust predictor of oral health, with individuals living below the poverty line many times
more likely to lose all their teeth.
23,24
A landmark 2000 report from the US surgeon general served as a call to action to address
oral health inequities, and prompted two decades of increased attention to oral health as an
important component of overall health.
25
Precedent-setting innovations that enhanced care
coordination and integration, such as the patient-centered medical home movement
26
and
initiatives to integrate behavioral health and primary care,
27
were adapted to pilot innova-
tive forms of dental integration into the primary care settings through colocation of dental
and medical services, task sharing between medical and dental providers, and interoperable
electronic health records.
28-31
These initiatives received additional support from an Oral Health
Strategic Framework at the US Department of Health and Human Services from 2014 to 2017,
which aected funding priorities throughout the department.
32
A follow-up to the 2000 report
was planned for late 2020, but its release has been pushed back to 2021 due to the COVID-19
pandemic.
Limited evidence from these pilot projects and observational analyses of claims data suggest
that the integration of oral health into primary care delivery and coverage may result in re-
duced health care costs and improved health outcomes;
33,34
however, overall evidence in favor
of care integration on the basis of systemic health impacts remains minimal, with several
clinical trials nding no benet to health outcomes after treatment for periodontal disease.
35,36
Preliminary ndings have been insucient to drive more denitive integration, particularly
in the face of resistance from organized dentistry. Few accountable care organizations include
dental care, and those that do generally fund dental treatment as a fee-for-service “carve-
out” service, rather than as a component of bundled care.
37,38
Lack of widespread adoption of
diagnostic codes within dentistry, as well as absent use of patient-centered outcomes, also
impairs the development of eective dental quality measures, further slowing the shift to-
ward value-based care from the fee-for-service model.
39,40
Oral health and primary care integration may be more advanced in safety-net and academic
settings. Federally Qualied Health Centers, which often have colocated medical and dental
services, have developed workows to enhance bi-directional referral and oral health screen-
ing.
41,42
Public health settings, especially those on sovereign tribal lands, were also pioneer-
ing in the adoption of advanced practice dental practitioners known as dental therapists, an
expansion of the dental team facing strenuous opposition by most private practice dentists.
43
As interprofessional education is a mandated competency for dental schools as well as mul-
tiple other health professions’ educational institutions, clinical and didactic interprofessional
training incorporating oral health occurs at academic institutions across the country.
44-46
Unfortunately, however, these innovators made up a very small proportion of the dental
delivery system. Thus, at the start of the COVID-19 pandemic, the vast majority of dental care
provision took place within a “cottage industry” of small business owners collecting fee-
for-service reimbursement directly from consumers, with limited access for many vulnerable
populations.
PRIMARY CARE IN THE COVID-19 PANDEMIC 85
Care transitions and closures in the early pandemic
Early epidemiology on the COVID-19 risk to health care workers suggested that dental prac-
titioners were at elevated risk due to high rates of aerosolization in dental treatment.
47
As
COVID-19 spread throughout the nation, practice recommendations quickly evolved during
an initial period of uncertainty. In Massachusetts, for example, a March 6 communication to
dentists from the Department of Public Health encouraged providers to continue normal care
and stated: “The risk for COVID-19 in the Commonwealth remains low; the risk for the u is
high” (personal communication, Massachusetts Department of Public Health, March 6, 2020).
By March 16, however, the American Dental Association (ADA) had released national guidance
recommending all elective dental care be deferred for three weeks—recommendations echoed
by most state departments of public health.
48
Although initially planned as a three-week pause in dental care, the closure of the dental
industry persisted for eight or more weeks across the country, depending on the length of
shutdown at a state level. Starting the week of March 23, the ADA’s Health Policy Institute
began sending waves of polling on the eect of the pandemic to more than 70,000 ADA
member dentists, garnering more than 19,000 responses each week.
49
While the respondents,
like the ADA’s membership, disproportionately represent small-business-owner dentists,
these waves of polling nevertheless provide an in-depth depiction of dental practice changes
throughout the pandemic. By April 2020, 95% of respondents had shuttered their practices;
although most were providing some emergency care, almost 20% were not providing any care
at all, despite such a decision being a violation of the ADA’s Code of Ethics.
50
By mid-April
2020, 45% of dentists had also furloughed all sta.
49
Dental practices were also aected by pandemic legislative changes that applied to the
broader health care system. The Coronavirus Aid, Relief, and Economic Security (CARES)
Act provided multiple funding opportunities for dental providers. More than 90% of dentist
respondents indicated they had applied to the Paycheck Protection Program, and almost 60%
to the Economic Injury Disaster Loan program.
51
Dentists also qualify for funding from the
Provider Relief Fund with looser restrictions than other providers; they are eligible indepen-
dent of whether they accepted any public or private insurance in the past.
52
Rates of program
application were the same among dentists who cared for Medicaid beneciaries and those
who did not.
51
The Oce of Civil Rights’ relaxation of the Health Insurance Portability and Accountability
Act (HIPAA) to allow telehealth to be practiced on a broader variety of platforms also applied
to dentists.
53
Previously, only California’s Medicaid program had reimbursed providers for
the use of two specic teledentistry codes; amidst the pandemic, public and private insurers
began reimbursing six codes from the Code on Dental Procedures and Nomenclature (CDT
Codes), including a problem-focused examination, with the goal of supporting telephone- or
video-based triage of patients experiencing dental emergencies.
54
Nonetheless, fewer than a
quarter of private practices reported billing with teledentistry codes.
55
This may have been a
result of relatively low reimbursement rates for these nonprocedural visits, which may have
prevented the provision of such care from being nancially viable. The low rates may also
86 PRIMARY CARE IN THE COVID-19 PANDEMIC
reect lack of public awareness that dentists could be accessed and could help assist patients
(such as through evaluations and recommendations that require only a video-based exam)
through this mechanism.
Public health dental settings faced a dierent set of economic pressures. Dental clinics in
Federally Qualied Health Centers and their “look-alikes” (clinics not ocially federally
qualied but having similar features) have often had slim nancial margins that challenge
sustainable dental delivery for at-risk populations. Dental department losses due to low reim-
bursement rates from public insurances and the cost of dental equipment and materials were
often supported by more favorable margins from medical services within the health center.
56
During the pandemic, however, patient visits at health centers across the nation declined
precipitously. Ten percent of health center dentists were furloughed through May.
57
To avoid
furloughing dental sta, several health centers redeployed them to COVID-19 testing or to call
center work.
58
Likely because health centers treat patients with higher rates of unmet dental
needs who require emergent management, overall patient volume dropped less precipitously
in health centers than in private practices during the rst months of the pandemic.
57
Besides private oces and public clinics, another major source of dental care was also dra-
matically aected by COVID-19. Prior to the pandemic, many patients without access to den-
tal care presented to hospital emergency departments for dental care, generating more than 4
million visits per year (more than 1.5% of all emergency department visits).
59
Patients pre-
senting to the emergency department are disproportionately young, diagnosed with multiple
comorbidities, and uninsured or publicly insured.
60
Ironically, dental treatment is generally
not available in emergency departments, with most patients receiving a prescription for an
antibiotic and opioid along with a recommendation to visit a dentist.
61
Emergency department
visits for dental problems declined during the early months of 2020 during the COVID-19
pandemic, and those patients who did present to the emergency department had more serious
infection and were more likely to be admitted to the hospital.
62,63
An analysis of utilization
and visits in the Boston area found that daily dental emergency department visits were halved
from February to April of 2020.
64
Rather than consisting of patients who no longer had access
to their routine sources of dental care during this period of dental practice closure, patients
visiting the emergency department for a dental problem during the early pandemic were still
more likely to be uninsured or a beneciary of Medicaid. Given that fewer than 50% of pa-
tients who visited the emergency department for a dental problem were able to see a dentist
within six months of their index emergency department visit, it is unknown how these trends
impacted unmet dental needs and access to oral health care in the population.
65
The rapid recovery of the dental industry
Although dental practices faced some of the most abrupt closures during the early phases of
the pandemic, resumption of dental practice also occurred with greater speed than elsewhere
in the health care system. Dentistry represented 35% of all health care jobs lost (which rep-
resented 2.4% of all jobs lost) in March and April 2020, yet 10% of all new jobs generated
by the economy in May 2020 were in the dental industry.
66
By the end of June 2020, 86% of
PRIMARY CARE IN THE COVID-19 PANDEMIC 87
dental practices had reopened for business, and more than 50% reported they were practic-
ing “business as usual” by July 13, 2020.
49
Even as COVID-19 continued to spread, and with
transmission rates higher than earlier in the pandemic, by September 21, 2020, 79% of dentists
nationwide were reporting patient volumes of 75% or greater of their prepandemic baseline.
49
While patient volumes in September 2020 were comparable to the volumes observed among
primary care practices (which stabilized in June 2020 at about 10% lower than prepandemic
levels), the dental visits were occurring entirely in person and were procedural in nature,
rather than via telehealth.
67
Dentistry’s technical demands and level of occupational exposure
and risk were more comparable to that of ophthalmology, which—by contrast with den-
tistry—experienced an 81% reduction in volume by May 2020.
68
The successful reopening of dentistry was due to a concerted eort by individual providers
and organized dentistry representatives. In August 2020, the ADA released an interim policy
on “Dentistry as Essential Health Care,” drawing direct parallels to frontline health care
workers to incent state governments to allow dental practices to reopen with fewer restric-
tions than other industries.
69
The dental industry emphasized, in consumer-facing literature,
that receiving dental care was safe despite COVID-19. Consumer polls in late August 2020
found that 80% of respondents felt safe having a dental visit.
70
Despite the move toward reopening, dental practice itself changed considerably. The increased
cost of personal protective equipment (PPE) sucient to prevent COVID-19 transmission (es-
pecially during highly aerosol-generating procedures such as those using a dental handpiece),
as well as the added turnover time required for additional antiviral agents to air-dry between
patients, reduced capacity and prot margin across dental practices. Some insurers temporar-
ily agreed to reimburse dentists for “PPE fees” to reect higher costs of operative dental care
during the pandemic, at per capita rates of $7-$10 per encounter.
71
Yet consumers balked at
the prospect of having such costs passed on to them.
72
In New York state, the Department of
Financial Services notied dental practices that directly charging consumers such fees may
violate insurance contracts.
73
Changes in practice standards for PPE utilization have precedent in the early human immu-
nodeciency virus (HIV) epidemic of the 1980s. After a period of uncertainty and fear about
appropriate infection control,
74
and a highly publicized case of HIV transmission from a den-
tist to several patients, consensus evolved to develop the set of “universal precautions,” in-
cluding gloves, masks, and disposable gowns that became standard practice.
75
The US Centers
for Disease Control and Prevention recommendations for dental providers—which included
wearing an N95 mask and goggles or a face shield during all clinical encounters—represented
an evolution of universal precautions.
76
Adoption of even more costly infrastructural changes to reduce transmission remains debated,
with limited evidence to support their use.
77
Nonetheless, some practices have advertised
adoption of technology such as high-eciency particulate air (HEPA) lters or ultraviolet
ionization to highlight safety in dental care. State-level requirements also vary; for example,
the state of Pennsylvania initially mandated dental care occur only in negative pressure
rooms, a physical alteration that was unaordable for many practices and clinics.
78
88 PRIMARY CARE IN THE COVID-19 PANDEMIC
Early evidence suggests that dental care provided with adequate PPE and risk reduction is
fairly safe; a dental clinic in Wuhan, China, during the early height of the pandemic provided
care without any evidence of intraoperative viral transmission.
79
Early results from the United
States show a rate of COVID-19 transmission among dentists that is lower than among the
general population.
80
Nevertheless, although domestic regulators and the ADA have encour-
aged patients to return to the dentist, the World Health Organization continues to recommend
against routine dental care.
81
One dental setting has been more dramatically impacted than others: school-based dental
clinics that serve as a highly cost-eective setting for the delivery of preventive oral health
services to children.
82
Many school-based dental clinics also identify and refer children with
more severe untreated dental disease for prompt treatment. With many school districts op-
erating remotely, school-based dental clinics were not available to the many thousands of
children each year who receive care through these programs.
83
Such programs disproportion-
ately benet low-income children who have higher rates of dental decay and may otherwise
have reduced access to dental care in the community.
82
Although the impact of COVID-19 on dental delivery has been well documented, its impact on
oral health is still poorly understood. Though rates of dental disease progression are based on
multiple biological and personal risk factors, some patients who could not access care dur-
ing the months-long period of closures may ultimately need more costly and invasive dental
treatment once care is accessible. This may be especially true for those patients who would
otherwise have visited an emergency department but chose to stay home despite experienc-
ing acute dental pain. Anecdotally, during COVID-19 dentists have reported a higher observed
incidence of stress-related oral conditions, such as fractured teeth and temporomandibular
joint pain related to bruxism.
49,84
Procedures required to treat more advanced disease, like
root canals and dental implants, which are less likely to be covered by dental insurance than
preventive procedures or basic treatments like llings, represent a substantial out-of-pocket
cost to patients. These procedures may be unaordable for more vulnerable patients, who are
already more likely to present to care with more severe dental problems.
3
Deferred care may
also have economic implications in the form of increased time away from work or school.
85
Looking forward: Will enduring change come to dentistry?
During the early months of the COVID-19 pandemic, when most dental care came to a halt,
many commentators saw the potential for radical change in dental practice, particularly in
aligning the eld more fully with other forms of health care delivery. Yet more than any other
health care industry, dentistry has been able to successfully resume its traditional model of
care delivery, and it appears many of the changes to dentistry foreseen at the beginning of the
pandemic have not borne out.
86
Yet even the relatively less dramatic changes seen in dental
care as a result of COVID-19 may aect practice patterns and access to health care services for
millions of Americans.
First, dental practice and reimbursement may evolve as a result of changes in infection con-
trol. Despite the ecacy of nonoperative models of dental care, dentistry remains a largely
PRIMARY CARE IN THE COVID-19 PANDEMIC 89
interventional eld. Many of dentistry’s most aerosol-generating procedures, such as drill-
ing a tooth and placing a lling, could be avoided with a medical model of oral health care.
Prevention-focused models like routine uoride varnish application and personalized risk
management, as well as less-invasive treatment such as arresting active tooth decay with
silver diamine uoride, may become more widespread if the health and economic cost of
performing aerosol-generating procedures persists.
A shift toward preventive and away from procedural services may garner support if outcomes-
driven reimbursement expands, partially or completely replacing the current predominantly
fee-for-service model that organized dentistry in the United States has defended to date. Due
to the increased cost of PPE to prevent COVID-19 transmission, and lower patient volumes
during the pandemic, dentists may nd capitated or quality-based payment models allow
them to remain protable while providing more preventive care than before the pandemic.
Next, infection risk reduction may prompt better information transfer between medical and
dental settings. Several dental facilities now require a negative COVID-19 PCR test before
treatment; however, such a requirement is only feasible in settings that allow for convenient
referral and results sharing between testing sites and dental providers, such as academic
medical centers and community health centers.
87
These settings provide a small minority of
clinical dental care. With few exceptions, electronic dental records are not interoperable with
electronic medical records, making information about patients’ COVID-19 testing history,
infection, or vaccination status inaccessible to dental providers.
88
There has previously been
limited incentive to improve interoperability, but demand may evolve with changing patient
and provider safety protocols.
As before the pandemic, the potential for enhanced integration as a direct result of COVID-19
faces resistance from dental providers themselves. Although historical precedent exists from
the 2009 H1N1 outbreak for vaccine administration by dentists,
89
less than half of dentists
reported they would consider administering a COVID-19 vaccine in their oce.
51
Broader policy changes may impact access to dental care. With 12.6 million people newly
unemployed in the United States during the COVID-19 pandemic, loss of employer-sponsored
dental insurance may lead to increased rates of unmet oral health needs.
90,91
Expanded Medicaid
enrollment of the newly unemployed will place additional budget constraints on state govern-
ments that may lead to reduction in Medicaid dental benets.
92
Similar changes occurred in
the wake of the 2007 nancial recession, resulting in higher rates of dental-related emergency
department visits and hospital admissions in the 19 states that cut or limited benets.
93-95
Ultimately, the COVID-19 pandemic reinforced the market and health system drivers of dental
delivery in the United States that make dental care in the United States unique relative to the
rest of the health care sector. Practice closures aected dental access in the short term, and
subsequent economic pressures may aect dental access and oral health in the long term
through the cost of dental delivery and availability of dental insurance coverage. However, the
COVID-19 pandemic has not served as a catalyst for the radical changes that would result in a
more integrated and equitable system of oral health care. In subsequent chapters, authors will
more fully explore the potential for these changes to take root, and address the core inequities
propagated and reinforced by the traditional model of dentistry in the United States, a model
that COVID-19 impacted but could not disrupt.
90 PRIMARY CARE IN THE COVID-19 PANDEMIC

References
1. Simon L. Overcoming historical separation between
oral and general health care: interprofessional col-
laboration for promoting health equity. AMA J Ethics
2016;18(9):941-9. 10.1001/journalofethics.2016.18.9.
pfor1-1609.
2. Willink A, Schoen C, Davis K. Dental care and
Medicare beneciaries: access gaps, cost bur-
dens, and policy options. Health Aff (Millwood)
2016;35(12):2241-8. 10.1377/hlthaff.2016.0829.
3. Vujicic M, Buchmueller T, Klein R. Dental care
presents the highest level of nancial barriers,
compared to other types of health care services.
Health Aff (Millwood) 2016;35(12):2176-82. 10.1377/
hlthaff.2016.0800.
4. Survey of dental practice. ADA Center for Profes-
sional Success. 2018. Accessed October 12, 2020.
https://success.ada.org/en/practice-management/
survey-of-dental-practice.
5. Nasseh K, Bowblis JR, Vujicic M, Huang SS. Consoli-
dation in the dental industry: a closer look at dental
payers and providers. Int J Health Econ Manag Octo-
ber 3, 2019 [Online ahead of print] 10.1007/s10754-
019-09274-x.
6. Guay A, Wall T. Considering large group practices as
a vehicle for consolidation in dentistry. ADA Health
Policy Institute. April 2016. Accessed February 18,
2021. http://www.ada.org/~/media/ADA/Science%20
and%20Research/HPI/Files/HPIBrief_0416_1.pdf.
7. Supply of dentists in the U.S. ADA Health Policy
Institute. 2018. Accessed May 19, 2020. https://www.
ada.org/en/science-research/health-policy-institute/
data-center/supply-and-prole-of-dentists.
8. Ambulatory care use and physician ofce visits.
Centers for Disease Control and Prevention. 2018.
Accessed September 25, 2020. https://www.cdc.gov/
nchs/fastats/physician-visits.htm.
9. 2019 NADP Dental Benets Report. National Asso-
ciation of Dental Plans. 2019. Accessed September
20, 2020. https://knowledge.nadp.org/products/2019-
dental-benets-report-provider-networks.
10. Medicaid benets: dental services. Kaiser Family
Foundation. 2018. Accessed April 19, 2020. https://
www.kff.org/medicaid/state-indicator/dental-services/.
11. Medicaid adult dental benets: an overview. Center for
Health Care Strategies. September 2019. Accessed
February 19, 2021. https://www.chcs.org/resource/
medicaid-adult-dental-benets-overview/.
12. Lyu W, Shane DM, Wehby GL. Effects of the recent
Medicaid expansions on dental preventive services
and treatments. Med Care 2020;58(8):749-55.
10.1097/MLR.0000000000001344.
13. Willink A, Reed NS, Swenor B, Leinbach L, DuGoff
EH, Davis K. Dental, vision, and hearing services:
access, spending, and coverage for Medicare ben-
eciaries. Health Aff (Millwood) 2020;39(2):297-304.
10.1377/hlthaff.2019.00451.
14. Gilbert GH, Shelton BJ, Chavers LS, Bradford EH.
The paradox of dental need in a population-based
study of dentate adults. Med Care 2003;41(1):119-34.
10.1097/01.MLR.0000039833.60078.DC.
15. Oral and dental health. Centers for Disease Control
and Prevention. Accessed October 15, 2020. https://
www.cdc.gov/nchs/fastats/dental.htm.
16. Treadwell HM, Northridge ME. Oral health is the
measure of a just society. J Health Care Poor Under-
served 2007;18(1):12-20. 10.1353/hpu.2007.0021.
17. Luo H, Wu Q, Bell RA, et al. Rural‐urban differ-
ences in dental service utilization and dental service
procedures received among US adults: results from
the 2016 Medical Expenditure Panel Survey. J Rural
Health July 22, 2020 [Online ahead of print] 10.1111/
jrh.12500.
18. Lewis C, Robertson AS, Phelps S. Unmet dental
care needs among children with special health care
needs: implications for the medical home. Pediatrics
2005;116(3):e426-31. 10.1542/peds.2005-0390.
19. Kulkarni SP, Baldwin S, Lightstone AS, Gelberg L,
Diamant AL. Is incarceration a contributor to health
disparities? Access to care of formerly incarcerated
adults. J Community Health 2010;35(3):268-74.
10.1007/s10900-010-9234-9.
20. Baghaie H, Kisely S, Forbes M, Sawyer E, Siskind DJ.
A systematic review and meta-analysis of the associa-
tion between poor oral health and substance abuse.
Addiction 2017;112(5):765-79. 10.1111/add.13754.
21. Saito M, Shimazaki Y, Nonoyama T, Tadokoro Y. As-
sociations of number of teeth with medical costs and
hospitalization duration in an older Japanese popula-
tion. Geriatr Gerontol Int 2019;19(4):335-41. 10.1111/
ggi.13622.
22. Glassman P, Subar P. Creating and maintaining oral
health for dependent people in institutional set-
tings. J Public Health Dent 2010;70 Suppl 1:S40-8.
10.1111/j.1752-7325.2010.00174.x.
23. Weintraub JA, Orleans B, Fontana M, Phillips C,
Jones JA. Factors associated with becoming eden-
tulous in the US health and retirement study. J Am
Geriatr Soc 2019;67(11):2318-24. 10.1111/jgs.16079.
PRIMARY CARE IN THE COVID-19 PANDEMIC 91
24. Wu B, Hybels C, Liang J, Landerman L, Plassman B.
Social stratication and tooth loss among middle-aged
and older Americans from 1988 to 2004. Community
Dent Oral Epidemiol 2014;42(6):495-502. 10.1111/
cdoe.12116.
25. Oral Health in America: A Report of the Surgeon
General. Rockville, MD: United States Department of
Health and Human Services; 2000. https://www.nidcr.
nih.gov/sites/default/les/2017-10/hck1ocv.%40www.
surgeon.fullrpt.pdf.
26. Epperly T, Bechtel C, Sweeney R, et al. The shared
principles of primary care: a multistakeholder initiative
to nd a common voice. Fam Med 2019;51(2):179-84.
10.22454/FamMed.2019.925587.
27. SAMHSA-HRSA Center for Integrated Health Solu-
tions. Accessed February 20, 2021. https://www.
samhsa.gov/integrated-health-solutions.
28. Atchison KA, Rozier RG, Weintraub JA. Integrating
oral health, primary care, and health literacy: consid-
erations for health professional practice, education
and policy. In: National Academies of Sciences, En-
gineering, and Medicine. Integrating oral and general
health through health literacy practices: proceedings
of a workshop. Washington, DC: National Academies
Press, 2019. 10.17226/25468.
29. Brownlee B. Case studies in oral health integration:
setting the stage for policy change. Qualis Health.
September 10, 2012. Accessed February 19, 2021.
http://www.qualishealth.org/sites/default/les/white-
paper-oral-health-integration-pcmh.pdf.
30. Snyder J. Kaiser Permanente: integrated value based
care model. In: Evolving the dental public health
landscape: interprofessional practice and value-based
care. San Antonio, Texas: American Institute of Dental
Public Health, 2019.
31. Acharya A, Cheng B, Koralkar R, et al. Screening for
diabetes risk using integrated dental and medical
electronic health record data. JDR Clin Trans Res
2018;3(2):188-94. 10.1177/2380084418759496.
32. Murthy VH. Oral health in America, 2000 to
present: progress made, but challenges re-
main. Public Health Rep 2016;131(2):224-5.
10.1177/003335491613100202.
33. Elani HW, Simon L, Ticku S, Bain PA, Barrow J,
Riedy CA. Does providing dental services reduce
overall health care costs? A systematic review of the
literature. J Am Dent Assoc 2018;149(8):696-703.
10.1016/j.adaj.2018.03.023.
34. Jeffcoat MK, Jeffcoat RL, Gladowski PA, Bramson JB,
Blum JJ. Impact of periodontal therapy on general
health: evidence from insurance data for ve sys-
temic conditions. Am J Prev Med 2014;47(2):166-74.
10.1016/j.amepre.2014.04.001.
35. Engebretson SP, Hyman LG, Michalowicz BS, et
al. The effect of nonsurgical periodontal therapy
on hemoglobin A1c levels in persons with type 2
diabetes and chronic periodontitis: a randomized
clinical trial. JAMA 2013;310(23):2523-32. 10.1001/
jama.2013.282431.
36. Michalowicz BS, Hodges JS, DiAngelis AJ, et al.
Treatment of periodontal disease and the risk of
preterm birth. N Engl J Med 2006;355(18):1885-94.
10.1056/NEJMoa062249.
37. Colla CH, Stachowski C, Kundu S, Harris B, Kennedy
G, Vujicic M. Dental care within accountable care
organizations: challenges and opportunities. ADA
Health Policy Institute and The Dartmouth Institute.
March 2016. Accessed February 19, 2021. https://
oralhealth.hsdm.harvard.edu/les/oralhealth/les/
ada_hpi_aco_brief.pdf?m=1498576772.
38. Dental care in accountable care organizations:
insights from 5 case studies. Leavitt Partners, ADA
Health Policy Institute, Pediatric Oral Health Research
and Policy, and America’s Pediatric Dentists. 2015.
Accessed February 19, 2021. http://www.ada.org/~/
media/ADA/Science%20and%20Research/HPI/Files/
HPIBrief_0615_1.ashx.
39. Ramoni RB, Walji MF, Kim S, et al. Attitudes toward
and beliefs about the use of a dental diagnostic
terminology: a survey of dental care providers in a
dental practice. J Am Dent Assoc 2015;146(6):390-7.
10.1016/j.adaj.2015.02.007.
40. Ni Riordain R, Glick M, Al Mashhadani SSA, et al. De-
veloping a standard set of patient-centred outcomes
for adult oral health—an international, cross-disciplin-
ary consensus. Int Dent J July 5, 2020 [Online ahead
of print] 10.1111/idj.12604.
41. Langelier M, Moore J. Case studies of 8 Federally
Qualied Health Centers: strategies to integrate
oral health with primary care. Oral Health Work-
force Research Center. 2015. Accessed Febru-
ary 19, 2021. http://www.chwsny.org/wp-content/
uploads/2016/06/042016c.pdf.
42. Langelier M, Surdu S, Goodwin N. Case studies of
6 safety net organizations that integrate oral and
mental/behavioral health with primary care services.
Center for Health Workforce Studies. February 2019.
Accessed February 19, 2021. http://www.chwsny.org/
wp-content/uploads/2019/02/OHWRC_Case_Stud-
ies_Oral_and_Behavioral_Health_Integration_With_
Primary_Care_2019.pdf.
92 PRIMARY CARE IN THE COVID-19 PANDEMIC
43. Simon L, Donoff RB, Friedland B. Dental therapy
in the United States: are developments at the state
level a reason for optimism or a cause for concern? J
Public Health Dent August 17, 2020 [Online ahead of
print] 10.1111/jphd.12388.
44. Dolce MC, Parker JL, Marshall C, et al. Expanding
collaborative boundaries in nursing education and
practice: the nurse practitioner-dentist model for pri-
mary care. J Prof Nurs 2017;33(6):405-9. 10.1016/j.
profnurs.2017.04.002.
45. Jones JA, Snyder JJ, Gesko DS, Helgeson MJ. Inte-
grated medical-dental delivery systems: models in a
changing environment and their implications for dental
education. J Dent Educ 2017;81(9):eS21-9. 10.21815/
jde.017.029.
46. Silk H. The future of oral health care provided by
physicians and allied professionals. J Dent Educ
2017;81(8s):e171-9. 10.21815/JDE.017.024.
47. Zemouri C, de Soet H, Crielaard W, Laheij A. A
scoping review on bio-aerosols in health care and
the dental environment. Zhou D, ed. PloS One
2017;12(5):e0178007. 10.1371/journal.pone.0178007.
48. Burger D. ADA recommending dentists postpone
elective procedures. ADA News. March 16, 2020.
Accessed October 2, 2020. https://www.ada.org/en/
publications/ada-news/2020-archive/march/ada-rec-
ommending-dentists-postpone-elective-procedures.
49. COVID-19: economic impact on dental practices:
week of September 21 results. ADA Health Policy
Institute. September 30, 2020. Accessed October
2, 2020. https://surveys.ada.org/reports/RC/public/
YWRhc3VydmV5cy01ZjZhMDQ1YjRjNGYyMDAw-
MGVkNjliYmQtVVJfNWlJWDFFU01IdmNDUlVO.
50. Guidance on continuing to practice ethically dur-
ing COVID-19. American Dental Association. Last
updated October 28, 2020. Accessed February 19,
2021. https://success.ada.org/~/media/CPS/Files/
COVID/ADA_COVID_How_Do_I_Ethically_See_Pa-
tients_During_Pandemic.pdf.
51. COVID-19: economic impact on dental practices:
week of September 7 results. ADA Health Policy
Institute. September 16, 2020. Accessed February
19, 2021. https://iad1.qualtrics.com/reports/RC/public/
YWRhc3VydmV5cy01ZjU3OWI5NzkzZDE2YTAwM-
TYzMjBmZWUtVVJfM3BaeGhzWm12TnNMdjB4.
52. CARES Act provider relief fund: for providers. US
Department of Health and Human Services. Last up-
dated January 19, 2021. Accessed October 4, 2020.
https://www.hhs.gov/coronavirus/cares-act-provider-
relief-fund/for-providers/index.html.
53. OCR announces notication of enforcement discre-
tion for telehealth remote communications during the
COVID-19 nationwide public health emergency. US
Department of Health and Human Services. March
17, 2020. Accessed April 8, 2020. https://www.hhs.
gov/about/news/2020/03/17/ocr-announces-notica-
tion-of-enforcement-discretion-for-telehealth-remote-
communications-during-the-covid-19.html.
54. COVID-19 coding and billing interim guidance: Virtual
visits. Version April 8, 2020. American Dental Asso-
ciation. Accessed April 8, 2020. https://success.ada.
org/~/media/CPS/Files/COVID/ADA_COVID_Cod-
ing_and_Billing_Guidance.pdf.
55. COVID-19: economic impact on public health den-
tal programs: week of June 29. ADA Health Policy
Institute. August 10, 2020. Accessed October 4, 2020.
https://surveys.ada.org/reports/RC/public/YWRhc3Vy-
dmV5cy01ZjM1OTM0NTI5ODA4ZjAwMTI2ZTA0MDc-
tVVJfM3BaeGhzWm12TnNMdjB4.
56. Financial ndings from California community health
centers. Blue Shield of California Foundation. August
2013. Accessed February 19, 2021. https://blueshield-
cafoundation.org/sites/default/les/publications/down-
loadable/BSCF_IssueBrief_Capital%20Links_Sep-
tember.pdf.
57. COVID-19: economic impact on public health dental
programs (summary report). Chicago, IL: ADA Health
Policy Institute, 2020.
58. Owen C, Speer S. Engaging dental staff in COVID-19
response efforts. National Network for Oral Health
Access, Solutions Training and Assistance for Recruit-
ment and Retention. April 15, 2020. Accessed Febru-
ary 19, 2021. http://www.nnoha.org/nnoha-content/
uploads/2020/04/NNOHA-STAR-Center-Engaging-
Dental-Providers-Webinar-4-15-20-FINAL.pdf.
59. Allareddy V, Rampa S, Lee MK, Allareddy V, Nalliah
RP. Hospital-based emergency department visits
involving dental conditions: prole and predictors of
poor outcomes and resource utilization. J Am Dent
Assoc 2014;145(4):331-7. 10.14219/jada.2014.7.
60. Kelekar U, Naavaal S. Dental visits and associated
emergency department charges in the United States:
nationwide emergency department sample, 2014. J
Am Dent Assoc 2019;150(4):305-12.e1. 10.1016/J.
ADAJ.2018.11.021.
61. Roberts RM, Bohm MK, Bartoces MG, Fleming-Dutra
KE, Hicks LA, Chalmers NI. Antibiotic and opioid
prescribing for dental-related conditions in emergency
departments: United States, 2012 through 2014. J
Am Dent Assoc 2020;151(3):174-81.e1. 10.1016/j.
adaj.2019.11.013.
PRIMARY CARE IN THE COVID-19 PANDEMIC 93
62. Long L, Corsar K. The COVID-19 effect: number of
patients presenting to the Mid Yorkshire Hospitals
OMFS team with dental infections before and during
the COVID-19 outbreak. Br J Oral Maxillofac Surg
2020;58(6):713-4. 10.1016/j.bjoms.2020.04.030.
63. Guo H, Zhou Y, Liu X, Tan J. The impact of the
COVID-19 epidemic on the utilization of emergency
dental services. J Dent Sci March 16, 2020 [Online
ahead of print] 10.1016/j.jds.2020.02.002.
64. Simon L, Marsh R, Samuels-Kalow ME. The early
impact of the COVID-19 pandemic on emergency
department visits for dental problems. American Den-
tal Association JADA+ COVID-19 Monograph 2020.
https://pages.ada.org/en/covidmonograph/impact-of-
covid-19-on-emergency-visits-for-dental-problems-dr.-
lisa-simon.
65. Singhal A, Momany ET, Jones MP, et al. Dental
care after an emergency department visit for den-
tal problems among adults enrolled in Medicaid.
J Am Dent Assoc 2016;147(2):111-9. 10.1016/j.
adaj.2015.08.012.
66. Kliff S. How’s the economy doing? Watch the dentists.
New York Times. June 10, 2020. Accessed February
19, 2021. https://www.nytimes.com/2020/06/10/up-
shot/dentists-coronavirus-economic-indicator.html.
67. Mehrotra A, Chernew M, Linetsky D, Hatch H, Cutler
D, Schneider EC. The impact of the COVID pandemic
on outpatient visits: changing patterns of care and
the newest hot spots. August 13, 2020. Accessed
February 19, 2021. https://www.commonwealthfund.
org/publications/2020/aug/impact-covid-19-pandemic-
outpatient-visits-changing-patterns-care-newest.
68. Strata Decision Technology. Analysis: ophthalmol-
ogy lost more patient volume due to COVID-19 than
any other specialty. Eyewire News. May 11, 2020.
Accessed October 15, 2020. https://eyewire.news/
articles/analysis-55-percent-fewer-americans-sought-
hospital-care-in-march-april-due-to-covid-19/.
69. An interim policy on dentistry as essential health
care. ADA Current Policies. American Dental As-
sociation. August 31, 2020. Accessed October 6,
2020. https://www.ada.org/en/advocacy/current-
policies?utm_source=adaorg&utm_medium=press-
release&utm_content=dentistry-is-essential-health-
care#publichealthemergencies.
70. How COVID-19 is impacting dental practices and
patient attitudes toward visiting the dentist: a special
webinar from the ADA. ADA Health Policy Institute.
August 5, 2020.
71. COVID-19 coding and billing interim guidance: PPE.
American Dental Association. October 27, 2020. Ac-
cessed February 19, 2021. https://success.ada.org/~/
media/CPS/Files/COVID/PPE_Coding_Billing_Guid-
ance.pdf.
72. Galewitz P. Open (your wallet) wide: dentists charge
extra for infection control. Kaiser Health News. June
3, 2020. Accessed June 8, 2020. https://khn.org/
news/open-your-wallet-wide-dentists-charge-extra-for-
infection-control.
73. Department of Financial Services. Unauthorized
charges for PPE. New York State. 2020. Accessed
October 15, 2020. https://www.dfs.ny.gov/consumers/
alerts/PPE_Charges.
74. Hastreiter RJ, Roesch MH, Danila RN, Falken MC.
Dental health care workers’ response to the HIV epi-
demic. Am J Dent 1992;5(3):160-6.
75. Daniel SJ. Compliance with infection-control pro-
cedures and attitudes of oral health care providers
toward patients with HIV/AIDS: a synthesis of the
literature. J Dent Hyg 1998;72(3):33-45.
76. Interim infection prevention and control guidance for
dental settings during the coronavirus disease 2019
(COVID-19) pandemic. Atlanta, GA: Centers for Dis-
ease Control and Prevention, 2020.
77. Kumbargere Nagraj S, Eachempati P, Paisi M, Nasser
M, Sivaramakrishnan G, Verbeek JH. Interventions
to reduce contaminated aerosols produced during
dental procedures for preventing infectious diseases.
Cochrane Database Syst Rev 2020;10:CD013686.
10.1002/14651858.CD013686.pub2.
78. Gantz S. Pennsylvania adjusts dental restrictions to
allow emergency procedures. Philadelphia Enquirer.
March 27, 2020. Accessed February 19, 2021. https://
www.inquirer.com/health/coronavirus/coronavirus-
covid19-dental-emergency-20200327.html.
79. Meng L, Hua F, Bian Z. Coronavirus disease 2019
(COVID-19): emerging and future challenges for
dental and oral medicine. J Dent Res March 12, 2020
[Online ahead of print] 10.1177/0022034520914246.
80. Estrich CG, Mikkelsen M, Morrissey R, et al. Esti-
mating COVID-19 prevalence and infection control
practices among US dentists. J Am Dent Assoc
2020;151(11):815-24. 10.1016/j.adaj.2020.09.005.
81. Considerations for the provision of essential oral
health services in the context of COVID-19. World
Health Organization. August 3, 2020. https://www.
who.int/publications/i/item/who-2019-nCoV-oral-
health-2020.1.
94 PRIMARY CARE IN THE COVID-19 PANDEMIC
82. Grifn S, Naavaal S, Scherrer C, Grifn PM, Harris
K, Chattopadhyay S. School-based dental sealant
programs prevent cavities and are cost-effective.
Health Aff (Millwood) 2016;35(12):2233-40. 10.1377/
hlthaff.2016.0839.
83. Cramer M. School closures cut a critical line to dental
care for poor students. New York Times. September
14, 2020. Accessed October 2, 2020. https://www.
nytimes.com/2020/09/14/us/school-closings-children-
dental-care.html.
84. Chen T. A dentist sees more cracked teeth. What’s
going on? New York Times. September 8, 2020.
Accessed October 2, 2020. https://www.nytimes.
com/2020/09/08/well/live/dentists-tooth-teeth-cracks-
fractures-coronavirus-stress-grinding.html.
85. Kelekar U, Naavaal S. Hours lost to planned and un-
planned dental visits among US adults. Prev Chronic
Dis 2018;15:E04. 10.5888/pcd15.170225.
86. Simon L. How will dentistry respond to the coronavirus
disease 2019 (COVID-19) pandemic? JAMA Health
Forum. May 19, 2020. 10.1001/JAMAHEALTHFO-
RUM.2020.0625.
87. Cramer M. Is it safe to go to the dentist again? New
York Times. June 25, 2020. Accessed October 15,
2020. https://www.nytimes.com/2020/06/25/health/
dentist-coronavirus-safe.html.
88. Acharya A, Schroeder D, Schwei K, Chyou P-H. Up-
date on electronic dental record and clinical comput-
ing adoption among dental practices in the United
States. Clin Med Res 2017;15(3-4):59-74. 10.3121/
cmr.2017.1380.
89. Dumcius G. Massachusetts: Dentists, pharmacists
and paramedics to administer H1N1 (swine u)
vaccine. Massachusetts Nurses Association. Au-
gust 13, 2009. Accessed April 8, 2020. https://www.
massnurses.org/health-and-safety/articles/infectious-
diseases/p/openItem/2781.
90. Choi SE, Simon L, Riedy CA, Barrow JR. Modeling
the impact of COVID-19 on dental insurance cover-
age and utilization. J Dent Res August 28, 2020 [On-
line ahead of print] 10.1177/0022034520954126.
91. Employment situation news release. Bureau of Labor
Statistics. October 2, 2020. Accessed October 15,
2020. https://www.bls.gov/news.release/archives/
empsit_10022020.htm.
92. Pucciarello M, Moran L. COVID-19 exacerbates exist-
ing oral health care access barriers for adult Medicaid
beneciaries. Center for Health Care Strategies. Sep-
tember 18, 2020. Accessed October 15, 2020. https://
www.chcs.org/news/covid-19-exacerbates-existing-
oral-health-care-access-barriers-for-adult-medicaid-
beneciaries/.
93. Salomon D, Heidel RE, Kolokythas A, Miloro M,
Schlieve T. Does restriction of public health care
dental benets affect the volume, severity, or cost of
dental-related hospital visits? J Oral Maxillofac Surg
2017;75(3):467-74. 10.1016/j.joms.2016.10.019.
94. Singhal A, Caplan DJ, Jones MP, et al. Eliminating
Medicaid adult dental coverage in California led to
increased dental emergency visits and associated
costs. Health Aff (Millwood) 2015;34(5):749-56.
10.1377/hlthaff.2014.1358.
95. Neely M, Jones JA, Rich S, Gutierrez LS, Mehra P.
Effects of cuts in Medicaid on dental-related visits
and costs at a safety-net hospital. Am J Public Health
2014;104(6):e13-6. 10.2105/AJPH.2014.301903.
PRIMARY CARE IN THE COVID-19 PANDEMIC 95
Addressing Food
Insecurity Among
At-Risk Older Adults
Lynda Flowers and Olivia Dean
F
ood insecurity—the lack of consistent access to healthy foods due to insucient resources—
has been a long-standing problem among older adults, and the COVID-19 crisis is making the
problem worse.
1,2
Among adults ages 50 and older, food insecurity has increased by an estimated
60% during the pandemic.
3
Older Black and Hispanic/Latino adults experience food insecurity at
over twice the rate of their White counterparts, an issue rooted in structural racism (Figure 1)—a
system in which laws, policies, practices, and other norms work to reinforce racial inequities.
Food insecurity is associated with chronic diseases such as diabetes mellitus, which disproportion-
ately impact Black and Hispanic/Latino populations and are risk factors for serious illness from
COVID-19.
4
Because social factors like lack of access to needed food are signicant drivers of health inequities,
it is important for primary care providers to consider them when delivering care to all older adults,
especially those who are most at risk for food insecurity. Addressing patients’ medical and social
needs is an important step toward improving health outcomes and reducing disparities. The most
impactful change, however, will come when clinicians and other parts of the health system work to
address the societal structures that create and perpetuate health inequities.
In this chapter, we describe how food insecurity impacts the health of older adults, how the
COVID-19 pandemic has impacted older adults’ food security, and some of the factors that may
help address food insecurity among older adults during and after the pandemic. We propose several
specic actions that primary care providers can take, both within their eld and with other groups,
to address food insecurity among older adults, emphasizing the importance of addressing root
causes of food insecurity in the United States.
Food insecurity negatively impacts older adults’ health
Lack of reliable, consistent access to healthy food poses signicant health risks for older adults. As
people age, their immune systems weaken, increasing their risks for illness.
5
Food insecurity de-
prives individuals of essential nutrients and further diminishes their ability to maintain a healthy
immune system. In addition, being food insecure is associated with a number of chronic
health conditions among older adults—including diabetes, asthma, and congestive heart
failure. Inconsistent calorie intake or intake of calorie-dense, cheaper, processed foods to
satisfy hunger can contribute to chronic metabolic and inammatory changes that trigger or
worsen these chronic conditions.
6
In turn, these conditions, which disproportionately impact
communities of color, are risk factors for serious complications from COVID-19.
7
Food insecurity can also diminish a person’s ability to perform activities of daily living (e.g.,
dressing and bathing) and worsen existing health conditions or make chronic conditions
more dicult to manage.
6
With limited nancial resources, food-insecure older adults make
decisions that are harmful to their health, such as not taking medications as prescribed and
postponing or forgoing needed medical care to save money for food.
How the pandemic is increasing food needs among
older adults
The COVID-19 pandemic has led to increases in food insecurity among older adults, especially
among Black and Hispanic/Latino older adults (Figure 1). Widespread job loss is likely one of
the largest reasons for this increase. Temporary loss of access to congregate meal programs,
increases in food prices, and long-standing underuse of federal nutrition benets also con-
tribute to the problem.
Increased unemployment
The COVID-19 pandemic has had a disproportionate impact on job and wage loss among Black
and Hispanic/Latino older adults. Between March and April 2020, unemployment rose sharply
among adults ages 50 and older, with Blacks and Hispanics/Latinos experiencing higher rates
of unemployment than their White counterparts (Figure 2). Among older Hispanics/Latinos, the
unemployment rate rose by 13 percentage points compared to 9 percentage points among older
Whites, exacerbating an already-existing unemployment gap. Unemployment rates fell among
older adults between April and September 2020, but the racial and ethnic unemployment rate gap
widened, and overall unemployment remained elevated compared to before the pandemic.
Temporary closure of congregate meal programs
The Older Americans Act (OAA) passed by Congress in 1965 authorized the provision of
healthy meals in congregate settings to adults ages 60 and older and their spouses of any age.
The primary goals of the OAA include improving nutritional status, alleviating food insecurity,
promoting socialization, and supporting overall health and well-being. The OAA enables con-
gregate meal programs to provide meals in a variety of community-based venues and targets
those with the greatest need: low-income people of color, those with limited English prociency,
people living in rural areas, and those at risk of needing institutional long-term care.
8
In 2018, congregate meal programs provided more than 71.5 million meals, including meals
tailored to people with diabetes, to more than 1.5 million (or 2%) of adults ages 60 and older.
9
98 PRIMARY CARE IN THE COVID-19 PANDEMIC

Figure 2. Unemployment Rate Among Adults 50 Years and Older by Race/Ethnicity in the
United States, 2020
0%
2%
4%
6%
8%
10%
12%
14%
16%
18%
20%
January
February
March
April
May
June
July
August
September
Hispanic Black White
Figure 1. Food Insecurity Prevalence Among Adults Ages 50 Years and Older in the United States,
2018 vs. 2020
7.2%
18.9%
16.4%
12.5%
26.2%
27.3%
0%
5%
10%
15%
20%
25%
30%
White Black Hispanic
2018 During COVID-19 (April 23-July 7, 2020)
Calculations by Schanzenbach and Pitts from the Current Population Survey and the
Census Pulse Survey.
Data derived from AARP Public Policy Institute analysis of 2020 Basic Monthly Current
Population Survey.
PRIMARY CARE IN THE COVID-19 PANDEMIC 99
Most participants were 75 years and older and lived alone.
10
For many, receiving a meal in a
congregate setting accounted for a signicant portion of their daily food intake, with 57% of
participants reporting that a single meal provided one-half or more of their total daily food
intake.
11
In addition to providing a signicant source of nutrition, participants in congregate
meal programs were less likely to be hospitalized or have emergency room visits than similar
older adults who did not participate in the program.
10
The onset of COVID-19 led many congregate meal sites to temporarily close their doors in
response to federal social distancing guidelines. While such guidelines were important for
slowing the spread of the virus, the meal site closures deprived many at-risk older adults of a
signicant source of healthy food. To help ll the void, many state and local Area Agencies on
Aging—which administer congregate meal programs—have partnered with local volunteers
to provide “grab-and-go” and home-delivered meals to older adults who previously received
meals in congregate settings. While these eorts are critical, more nancial resources are
needed for meal providers to fully meet the growing need.
11
Increasing food prices
Rising food prices during the pandemic also threaten the food security of low-income older
adults. Between March and June 2020, overall food prices at supermarkets and grocery stores
increased 4.3%.
12
The price increase was partly driven by beef prices, which grew 20%.
Factors contributing to price increases included demand shocks as people feared shortages
and stockpiled food, breaks in supply chains as processing plants shut down due to COVID-19
outbreaks, and higher demand for groceries as people shifted from eating at restaurants
to eating at home.
13
In a June survey, half of low-income older respondents reported being
worried about rising food prices, and 43% expressed concerns about not having the money to
pay for needed food.
14
While food prices have decreased slightly at the time of this writing in
October 2020, prices continue to remain higher than they were one year ago.
15
Low-income older adults receiving benets through the Supplemental Nutrition Assistance
Program (SNAP)—formerly known as food stamps—may be particularly vulnerable to the
impacts of higher food prices. The US Department of Agriculture calculates SNAP benet
allotments using the Thrifty Food Plan (TFP), a minimal-cost food plan based on “a national
standard for a nutritious diet at a minimal cost.”
16
Despite its denition, the TFP is insuf-
cient to meet actual food needs.
17
Thus, large increases in food prices could make it even
harder for SNAP enrollees to stretch their modest allotments to meet their food needs.
Long-standing underuse of SNAP
SNAP is the nation’s largest anti-hunger program, helping millions of Americans purchase
food, including 8.7 million low-income households with adults ages 50 and older in 2018.
18
The program is proven to reduce food insecurity, is associated with improved health, and is
designed to expand during periods of increased need, such as the current COVID-19-related
economic downturn.
100 PRIMARY CARE IN THE COVID-19 PANDEMIC
As successful as SNAP is at addressing food insecurity, enrollment in the program has been
historically low among older adults. Prior to the pandemic, about 52% (5 million) of adults
ages 60 and older who qualied for SNAP were not enrolled in the program.
19
Low-income
older adults face barriers to enrollment such as lack of awareness about SNAP, misconcep-
tions about program rules, and a burdensome application process.
20
Fortunately, the federal
government has temporarily suspended the face-to-face interview and renewal requirements
during the pandemic.
21
Another barrier to SNAP enrollment is the belief that the benet level is so low that it is not
worth the eort to apply. Although the federal minimum benet amount is quite low at $16 a
month, the average monthly benet received by households with adults ages 50 and older was
actually $144 in 2018.
18
Finally, stigma around receipt of public benets can keep some eligible older adults from
applying for SNAP. Eorts to overcome stigma can include streamlining enrollment processes,
correcting misperceptions about the program, and widely disseminating positive messages
and images that demonstrate the program’s value.
An expanded role for primary care in supporting food
security among older adults
Primary care providers and their oce sta can play an important role in helping food inse-
cure older adults access the food they need to stay healthy. They are often older adults’ main
and most-consistent point of contact with the health care system, oering an important
opportunity to address clinical and social needs. Knowing whether patients lack access to
adequate amounts of healthy food can lead to interventions that improve nutritional status
and chronic care management. As primary care providers consider a larger role in helping to
alleviate food insecurity and food insecurity disparities among older adults, here are a few
things they should consider.
Incorporate food insecurity screening and referral into the workow
Increasingly, primary care practices are addressing patients’ food needs through food in-
security screening and referral. Broadly, this means using a validated tool to systematically
screen patients and connect those who are food insecure to resources such as food banks.
Although growing in popularity, food insecurity screening and referral is still not the norm
in primary care. Barriers to screening include lack of organizational commitment, lack of
knowledge about screening tools and how to use them, perceptions that screening is too
time-consuming, not knowing how to deal with positive screens, and uncertainty about the
impact of screening on the provider-patient relationship.
22
These barriers, however, are not
insurmountable. The AARP Foundation has developed a useful resource guide for implement-
ing food security screening and referral for older patients in primary care.
23
Primary care providers face competing demands on their time and resources, and organiza-
tional leadership may not view food insecurity screening among older adults as germane to
PRIMARY CARE IN THE COVID-19 PANDEMIC 101
the provider role. A case can be made to leadership that integrating food insecurity screening
and referral into workows could reduce provider burden and may lead to improved patient
outcomes and ultimately cost savings for practices.
24
Simple but eective screening tools are available depending on the goals of the practice and
are easily incorporated into electronic health records platforms. If the goal is to screen only
for food insecurity, Hunger Vital Sign is a validated two-question instrument that can be
administered verbally or in writing.
25
Another tool, Protocol for Responding to and Assessing
Patients’ Assets, Risks, and Experiences (PRAPARE), contains 15 questions that measure a
range of social and economic risk factors, including food insecurity. Available in 26 languages,
PRAPARE takes about nine minutes to administer.
26
Practices should consider using waiting-
room time to eld screening tools.
During the pandemic, primary care providers can screen and refer through telephonic or video
visits with patients. Providers who nd this approach eective may want to continue the
practice post-pandemic. Providers may test other methods of screening and referring food-
insecure older adults, including text messages, emails, and chatbots (computer programs
that simulate conversation). Any method used should be culturally competent, ensure patient
privacy, and be evaluated for eectiveness and patient satisfaction. Chosen methods should
also be consistent with patient and family caregiver preferences.
The process should not end at referral; primary care providers should use the results to make
decisions about medical care and follow up with food-insecure patients to ensure they are
getting the help they need. Continually tracking and monitoring progress, including the
number of referrals to various resources as well as referral outcomes, is important for im-
proving patient outcomes. Training should be available for medical assistants and other oce
sta to help with these processes.
Build and nurture trust with patients and family caregivers
Patients are more likely to discuss sensitive personal issues in an atmosphere of trust. When
it comes to food insecurity, older adults may feel shame or discomfort about not being able to
aord food
or may be suspicious of provider motives for asking sensitive personal questions.
27
In addition, the COVID-19 pandemic has brought a host of new challenges that can make trust
building dicult. For example, patients and caregivers may be receiving mixed messages
about risk factors for the virus and how to protect themselves.
Mistrust of the medical system is particularly profound among Black and Hispanic Americans,
who are reeling from the disproportionate impacts of COVID-19 on the physical, mental, and
economic health of their communities. A recent national poll found that over half (55%) of
Black Americans mistrust the health care system, 70% of Black and 43% of Hispanic Americans
believe the medical system treats people unfairly based on their race or ethnicity, and more
than 20% of both Black and Hispanic Americans say they have diculty nding a clinician who
treats them with dignity and respect.
28
On a systemic level, examples of factors that continue
to contribute to mistrust include underrepresentation of Blacks and Hispanics in clinical trials,
denied access to the most benecial treatments, and health providers’ implicit or explicit bias.
102 PRIMARY CARE IN THE COVID-19 PANDEMIC
The aforementioned national poll also found that 28% of Black Americans prefer to be treated
by Black clinicians, but there are not enough to meet the need. Thus, it is especially important
to build trust where there is a lack of racial/ethnic and/or language concordance between
patients and providers.
29
Providers should be knowledgeable about the medical system’s his-
torical and ongoing harms to people of color, as well as regularly participate in trainings on
explicit and implicit bias, cultural competence and humility, and anti-racism. Organizations
should nd ways to ensure that such trainings result in tangible results.
Examples of trust-building strategies include limiting interruptions and distractions during
the visit, making eye contact with patients, taking patients at their word, respecting patients’
right to make their own choices, not making assumptions about the patient, admitting and
apologizing for mistakes, and checking in with patients to validate information about their
care.
30
Ensuring patient privacy, oering screening in a patient’s preferred language, and be-
ing mindful of literacy levels are important for trust building as well.
31
Screening every pa-
tient who comes in to the practice for food insecurity may also help normalize the process and
reduce stigma. In the long term, relationship building may increase the eciency of the visit
as patients become more comfortable and providers can easily obtain the information they
need to help patients best manage their care. Trust promotes care-seeking behaviors, patient
honesty, and adherence.
32
Build strong community partnerships
Providers should develop and nurture strong community-based partnerships that can help
them address food insecurity, as well as other social and economic issues that contribute to
health disparities among their older patients. Eective community partnerships leverage the
strengths of each partner to achieve agreed-upon goals. They also help partners understand
issues and solutions from a variety of perspectives. Though they take time to develop and
maintain, such partnerships are well worth the eort.
33
In the context of food insecurity, community partners can provide information and training
to providers that can help them connect older adults to appropriate food resources. Provider
organizations and individual providers can also work with community partners to link older
adults to needed services, like housing and energy assistance programs. Potential community
partners include Area Agencies on Aging, anti-hunger advocacy groups, relevant minority
organizations, food banks, senior centers, social service agencies, local philanthropies, and
other entities.
While primary care providers can partner directly with community organizations, it may
be useful to contract with an intermediary organization that can help build and maintain
community relationships. For example, the Center for Medicare and Medicaid Innovation’s
Accountable Health Communities is currently testing a ve-year model that funds “bridge
organizations” to partner and coordinate with clinical delivery sites and community-based
organizations to conduct social-needs screenings and referrals—including for food inse-
curity—among Medicare beneciaries who are also eligible for Medicaid.
34
Providers and
provider organizations can take advantage of value-based payment models and savings from
risk-based managed care to hire intermediary organizations to connect their practices to
community resources and help facilitate community partnerships.
PRIMARY CARE IN THE COVID-19 PANDEMIC 103
Work to dismantle structural racism
While primary care physicians play an important role in addressing patients’ clinical needs,
health is primarily determined outside of the clinical setting, with underlying social condi-
tions driving up to 80% of health outcomes.
35
In turn, these social conditions are perpetuated
by systems of structural racism that support an environment that results in signicant dis-
parities in food insecurity. For example, policies and practices that result in segregated com-
munities, income inequality, and barriers to wealth accumulation all contribute to disparities
in access to resources needed to purchase healthy foods. Health systems and clinicians who
hold biases and engage in discriminatory practices also contribute to health disparities, in-
cluding disparities in food insecurity. Health systems and individual practices should take
steps to redesign their organizational structures to optimize their ability to address social
needs, reduce health disparities, and tackle the structural barriers that promote them.
Primary care providers, their membership associations, and managed care organizations
have a responsibility to independently and collectively advocate for policies designed to chip
away at the systemic barriers that contribute to food insecurity and health inequities, includ-
ing racism. The codes of ethics for the National Black Nurses Association and the American
Nursing Association require nurses, including independent nurse practitioners, to advocate for
patients’ rights and to engage in eorts that promote social justice. Similarly, the American
Medical Association calls for physicians to advocate for social, economic, and political changes
that contribute to human well-being.
Clinicians and support sta can meet these responsibilities by advocating for policies that
increase their ability to address social needs, including payment reforms that support inte-
grated health and social care delivery systems. Provider membership associations and managed
care organizations can take the lead in making advocacy training widely available to providers.
Incorporating individual primary care professionals in their ongoing lobbying eorts can help
these professionals gain advocacy expertise. Health care professionals sharing their knowledge
and patient stories with policymakers can be incredibly valuable and may impact policy change.
Conclusions
The COVID-19 pandemic has worsened food insecurity among all older adults, with Black and
Hispanic/Latino older adults suering disproportionate harm. With increasing numbers of
older adults struggling to put food on the table, it has never been more important for provid-
ers to recognize the impact that food insecurity has on health and health disparities and to
make eorts to address patients’ nonmedical needs alongside their medical needs.
Advancing health equity requires many sectors working together, including policymakers,
public health, health care, and social care systems. While interventions in primary care set-
tings to combat food insecurity can address patients’ immediate needs and may improve
health outcomes at the individual level, they must go hand-in-hand with broader eorts that
tackle the long-standing racist policies that underlie food insecurity.
104 PRIMARY CARE IN THE COVID-19 PANDEMIC
References
1. Feeding America study projects local food insecurity
rates amid pandemic could reach up to 1 in 3 adults
and 1 in 2 children. Feeding America. May 20, 2020.
Accessed October 2, 2020. https://www.feedingamer-
ica.org/about-us/press-room/feeding-america-study-
projects-local-food-insecurity-rates-amid-pandemic-
could.
2. Ashbrook A. Nearly 60 percent increase in older adult
food security during COVID-19: federal action on
SNAP needed now. FRAC Chat. July 31, 2020. Ac-
cessed October 2, 2020. https://frac.org/blog/nearly-
60-percent-increase-in-older-adult-food-insecurity-
during-covid-19-federal-action-on-snap-needed-now.
3. Calculations for AARP Public Policy Institute by Diane
Schanzenbach and Abigail Pitts at Northwestern
University using the Current Population Survey and
the Census Pulse Survey. Compares 2018 annual
data to pooled data from April 23 through July 7,
2020. July 2020. Accessed October 8, 2020. https://
www.ipr.northwestern.edu/news/2020/schanzenbach-
household-pulse-survey-analysis.html.
4. Golden SH. Coronavirus in African Americans and
other people of color. Johns Hopkins Medicine. April
20, 2020. Accessed October 2, 2020. https://www.
hopkinsmedicine.org/health/conditions-and-diseases/
coronavirus/covid19-racial-disparities.
5. US National Library of Medicine. Aging changes in
immunity. US Department of Health and Human Ser-
vices. 2020. Accessed September 28, 2020. https://
medlineplus.gov/ency/article/004008.htm.
6. Hunger and health: the impact of poverty, food inse-
curity, and poor nutrition on health and well-being.
Food Research and Action Center. December 2017.
Accessed September 28, 2020. https://frac.org/wp-
content/uploads/hunger-health-impact-poverty-food-
insecurity-health-well-being.pdf.
7. Centers for Disease Control and Prevention. Corona-
virus disease 2019 (COVID-19): people at increased
risk. US Department of Health and Human Services.
2020. Updated January 4, 2021. Accessed Septem-
ber 28, 2020. https://www.cdc.gov/coronavirus/2019-
ncov/need-extra-precautions/index.html.
8. Administration for Community Living. Nutrition ser-
vices. US Department of Health and Human Services.
2020. Accessed September 17, 2020. https://acl.gov/
programs/health-wellness/nutrition-services#[delete;
replace with period in black text, no underscore].
9. Administration for Community Living. Data-at-a-
glance (SPR). US Department of Health and Human
Services. 2018. Accessed September 28, 2020.
https://agid.acl.gov/DataGlance/SPR/.
10. Mabli J, Ghosh A, Schmitz B, Shenk M, Panza-
rella E, Carlson B, Flick M. Final report: evaluation
of the effect of the Older Americans Act Title III-C
Nutrition Services Program on participants’ health
care utilization. Cambridge, MA: Mathematica Policy
Research, 2018. https://acl.gov/sites/default/les/pro-
grams/2018-10/NSPevaluation_healthcareutilization.pdf.
11. Tucher E, Thomas KS. The impact of COVID-19’s
closure of meal sites on older adults. Milbank Memo-
rial Fund. March 30, 2020. Accessed September 17,
2020. https://www.milbank.org/2020/03/the-impact-of-
covid-19s-closure-of-meal-sites-on-older-adults/.
12. Mead D, Ransom K, Reed SB, Sager S. The impact
of the COVID-19 pandemic on food price indexes and
data collection. Monthly Labor Review. August 2020.
Accessed September 17, 2020. https://www.bls.gov/
opub/mlr/2020/article/the-impact-of-the-covid-19-pan-
demic-on-food-price-indexes-and-data-collection.htm.
13. Waggoner J. Why the coronavirus outbreak has sent
food prices soaring. AARP. July 24, 2020. Accessed
September 17, 2020. https://www.aarp.org/money/
budgeting-saving/info-2020/food-prices-coronavirus-
outbreak.html#[delete; replace with period in black
text, no underscore].
14. Dean O, Flowers L. As pandemic wears on, food
challenges are increasing for many older Americans.
AARP. July 1, 2020. Accessed September 17, 2020.
https://blog.aarp.org/thinking-policy/as-pandemic-
wears-on-food-challenges-are-increasing-for-many-
older-americans.
15. Consumer Price Index news release. US Bureau of
Labor Statistics. August 2020. Accessed October 14,
2020. https://www.bls.gov/news.release/archives/
cpi_09112020.htm.
16. Food Research and Action Center (FRAC). Replac-
ing the Thrifty Food Plan in order to provide adequate
allotments for SNAP beneciaries. FRAC. December
2012. Accessed October 15, 2020. https://frac.org/wp-
content/uploads/thrifty_food_plan_2012.pdf.
17. Waxman E, Gundersen C, Thompson M. How far
do SNAP benets fall short of covering the cost of a
meal? Urban Institute. February 23, 2018. Accessed
October 17, 2020. https://www.urban.org/research/
publication/how-far-do-snap-benets-fall-short-cover-
ing-cost-meal.
18. Dean O, Flowers L, Figueiredo C. Millions of adults
ages 50 and older rely on the Supplemental Nutrition
Assistance Program (SNAP). AARP Public Policy In-
stitute. July 16, 2020. Accessed September 15, 2020.
https://www.aarp.org/ppi/info-2020/millions-of-adults-
ages-50-and-older-rely-on-snap.html.
PRIMARY CARE IN THE COVID-19 PANDEMIC 105
19. Food and Nutrition Service. Trends in SNAP par-
ticipation rates: scal year 2010-2017. US Depart-
ment of Agriculture. September 12, 2019. Accessed
September 15, 2020. https://www.fns.usda.gov/snap/
trends-supplemental-nutrition-assistance-program-
participation-rates-scal-year-2010.
20. Hoffman V, Pooler J, Garasky S. Missed opportunities:
lifting barriers to SNAP participation among eligible
seniors. Issue Brief. IMPAQ International. January
2016. Accessed September 17, 2020. https://impaq-
int.com/sites/default/les/les/Missed%20Opportuni-
ties_Lifting%20Barriers%20to%20SNAP%20Partici-
pation%20Among%20Eligible%20Seniors.pdf.
21. Food and Nutrition Service. SNAP—adjusting interview
requirements due to novel coronavirus (COVID-19). US
Department of Agriculture. October 7, 2020. Accessed
September 17, 2020. https://www.fns.usda.gov/snap/
adjusting-interview-requirements-covid-19.
22. Kopparapu A, Sketas G, Swindle T. Food insecurity
in primary care: patient perception and preferences.
Fam Med 2020;52(3):202-5. https://journals.stfm.org/
familymedicine/2020/march/kopparapu-2019-0162/.
23. Pooler J, Levin M, Hoffman V, Karva F, Lewin-
Zwerdling A. Implementing food security screening and
referral for older patients in primary care: a resource
guide and toolkit. AARP Foundation and IMPAQ Inter-
national. November 2016. Accessed September 17,
2020. https://www.aarp.org/content/dam/aarp/aarp_
foundation/2016-pdfs/FoodSecurityScreening.pdf.
24. De Marchis EH, Torres JM, Benesch T, Fichtenberg
C, Allen IE, Whitaker EM, Gottlieb LM. Interventions
addressing food insecurity in health care settings: a
systematic review. Ann Fam Med 2019;17(5):436-47.
10.1370/afm.2412.
25. Gundersen C, Engelhard EE, Crumbaugh AS, Selig-
man HK. Short communication: brief assessment
of food insecurity accurately identies high-risk US
adults. Public Health Nutrition. January 18, 2017.
Accessed September 27, 2020. https://children-
shealthwatch.org/wp-content/uploads/brief-assess-
ment-of-food-insecurity-accurately-identies-high-risk-
us-adults.pdf.
26. Protocol for responding to and assessing patients’
assets, risks, and experiences. National Association
of Community Health Centers. Accessed September
17, 2020. https://www.nachc.org/research-and-data/
prapare/.
27. Addressing Food Insecurity: A Toolkit for Pediatricians.
American Academy of Pediatrics and Food Research
& Action Center. February 2017. https://frac.org/aap-
toolkit.
28. Fletcher MJ. New poll shows Black Americans see
a racist health care system setting the stage for the
pandemic’s impact. The Undefeated. October 14,
2020. Accessed October 15, 2020. https://theunde-
feated.com/features/new-poll-shows-black-americans-
see-a-racist-health-care-system-setting-the-stage-for-
pandemics-impact/.
29. Shen MJ, Peterson EB, Costas-Muñiz R, Hernandez
MH, Jewell ST, Matsoukas K, Bylund CL. The effects
of race and racial concordance on patient-physician
communication: a systematic review of the literature.
J Racial Ethn Health Disparities 2018;5(1):117-40.
10.1007/s40615-017-0350-4.
30. Holman T. How to build patient trust to improve the
doctor-patient relationship. Dignity Health. June 27,
2017. Accessed September 17, 2020. https://www.
dignityhealth.org/articles/how-to-build-patient-trust-to-
improve-the-doctor-patient-relationship.
31. Food insecurity screening: health care’s role in iden-
tifying food insecurity. Delivering Community Benet:
Healthy Food Playbook. 2018. Accessed September
15, 2020. https://foodcommunitybenet.noharm.org/
resources/implementation-strategy/food-insecurity-
screening.
32. Jacobs EA, Rolle I, Ferrans CE, Whitaker EE, War-
necke RB. Understanding African Americans’ views of
the trustworthiness of physicians. J Gen Intern Med
2006;21(6):642-7. 10.1111/j.1525-1497.2006.00485.x.
33. Lavey J. The value of partnerships in community
development. Community Builders. February 9, 2017.
Accessed October 15, 2020. https://communitybuild-
ers.org/insights/the-value-of-partnerships-in-commu-
nity-development/.
34. Centers for Medicare and Medicaid Services. Ac-
countable health communities model. CMS.gov.
October 2, 2020. Accessed October 14, 2020. https://
innovation.cms.gov/innovation-models/ahcm.
35. Manatt, Phelps & Phillips, LLC. Medicaid’s role in ad-
dressing social determinants of health. Robert Wood
Johnson Foundation. February 1, 2019. Accessed
September 17, 2020. https://www.rwjf.org/en/library/
research/2019/02/medicaid-s-role-in-addressing-
social-determinants-of-health.html.
106 PRIMARY CARE IN THE COVID-19 PANDEMIC
SECTION 2: PRACTICE TRANSITIONS:
Payments and Delivery
Payer Actions and
Primary Care in the
Wake of COVID-19: Will
Primary Care Be There
When We Need It?
Christopher F. Koller
H
ealth systems experts acknowledge the benets of a strong primary care capacity as the basis
of a high-performing delivery system, but nobody in the United States wants to pay for it. It
is a classic “common good” problem. Given the United States’ fragmented, third-party-dominated
health care nancing, no single entity can derive sucient benet from their individual action
to oversee, let alone strengthen, primary care. Absent political power to inuence public policy or
economic power to drive private negotiations, primary care in the United States is overextended
and underfunded.
In this weakened state, primary care in the United States was vulnerable at the onset of COVID-19
and less able to be a strategic asset in ghting the pandemic than it could have been. Primary care
also suered as people skipped their routine and follow-up appointments. A review of public and
private payer actions to support primary care in the wake of COVID-19 shows a continuation of
previous policy: neglect with occasional bright spots of activity. These results should not be viewed
as surprising. Under stress a system will react based on previous strengths and tendencies. In the
case of the US health care system, these strengths and tendencies have not included organized and
powerful systems of primary care delivery or advocacy.
Pre-COVID-19
US primary care was weak before COVID-19. Privately insured visit rates had been declining,
1
as
was the small share of US health care expenses devoted to primary care
2
and the share of the health
care workforce in primary care.
3
These declines occurred in spite of evidence that primary care was
the major contributor—above other health care services—to increased US life expectancy
4
and
better and more equitable health outcomes.
5
Much of this lack of investment in primary care can be attributed to Medicare fee-for-service
payment policies, which systematically devalue the cognitive services and care coordina-
tion provided by primary care in favor of the more technically complex services rendered by
specialists.
3
The private negotiation process used by employer-sponsored insurers and health
providers to determine payment rates for care takes these Medicare rates as its starting point.
The process also rewards the relative economic power of the negotiating parties, further
disadvantaging primary care providers, especially those in independent practices.
In an attempt to address this, Medicare has continued to experiment with a number of pri-
mary care payment models, which have struggled to clear the high standard for widespread
scaling of beating or equaling overall Medicare fee-for-service cost and quality measures.
6
Several states, starting with Rhode Island and Oregon, had taken steps to use their authority
in comprehensive ways to invest a greater share of health care dollars into primary care.
7
COVID-19’s onset
The arrival of COVID-19 saw primary care ill-equipped for a pandemic. Absent administrative
capacity, practices struggled to acquire personal protective equipment and develop protocols
to safely test and treat potentially infectious people. Fearful of infection, patients stayed away
and oce visits fell by more than half in the initial months.
8
Paid on a per visit basis, prac-
tices saw revenue plummet and providers teetered on the edge of viability. Weekly surveys of
primary care practices by the Larry Greene Center conveyed a picture of grave emotional and
nancial distress.
9
As the pandemic has worn on, primary care has adjusted. As of October 2020, analysis for the
Commonwealth Fund indicates that larger adult primary care practices are at prepandemic
visit levels.
10
Smaller practices are not (Figure 1). Pediatric practices are slightly below base-
line levels as well. For any practice paid on a per visit basis, this negative change from base-
line is lost revenue that cannot be recovered. That translates to salary cuts, sta layos, line
of credit costs, and practice closures.
It also means less primary care capacity at a time when it is sorely needed. A further weaken-
ing of primary care does not bode well for a country in a pandemic (Table 1). Families and
individuals would lose their chief partner and navigator in maintaining their health. Public
health practitioners would lose a valued partner in testing and tracing eorts, as well as
ongoing prevention initiatives. Overburdened hospitals would lose an important triage and
treatment function for less severe COVID-19 cases. Public and private payers would lose the
capacity of their enrollees with chronic conditions to be managed more eectively in less ex-
pensive settings. Advocates for improved health equity would lose the only part of the health
care system proven to reduce disparities in health outcomes.
110 PRIMARY CARE IN THE COVID-19 PANDEMIC

Table 1. Overview of Primary Care’s Epidemic-Mitigation Capacities and Eects.
Capacity Benets
Leverage established, trusted patient
relationships
Amplies public health education eorts to
prevent infection, limit spread, and reassure
people
Test for and report positive cases
systematically
Improves surveillance and early case
identication and isolation
Participate in contact-tracing eorts
Lowers infection rates
Treat positive cases guided by the best
evidence and in a safe setting
Improves patient outcomes and minimizes
the spread of infection
Practice care coordination for cases Minimizes demands on limited acute-care
resources
Data derived from Shih and Koller.
25
Figure 1. Adult Primary Care Visits by Week in 2020 vs. Prepandemic Baseline
10
Data derived from Mehrotra et al.
10
WWW.MILBANK.ORG
1
1 Footer Te x t
-60
-50
-40
-30
-20
-10
0
10
20
16-Feb
23-Feb
1-Ma r
8-Ma r
15-Mar
22-Mar
29-Mar
5-Apr
12-Apr
19-Apr
26-Apr
3-Ma y
10-May
17-May
24-May
31-May
7-Jun
14-Jun
21-Jun
28-Jun
5-Jul
12-Jul
19-Jul
26-Jul
2-Aug
9-Aug
16-Aug
23-Aug
30-Aug
6-Sep
13-Sep
20-Sep
27-Sep
4-Oct
1–5 providers 6+ providers
Percent change from baseline
PRIMARY CARE IN THE COVID-19 PANDEMIC 111
Federal pandemic responses aecting primary care
The CARES Act funding passed by Congress—totaling $175 billion for health care providers—
was the most direct and sizable payer response to COVID-19 and reected no prioritization
of primary care. Without congressional guidance, the initial distributions of $50 billion in
CARES Act funding were made by the Centers for Medicare and Medicaid Services (CMS) based
on a provider’s historic Medicare billing.
11
Developed for speed, simplicity, and fairness, this
policy reinforced historical distributions, regardless of a provider type’s nancial vulnerability
or strategic importance in a pandemic. Subsequent distributions have relied on the Medicare
formula but set aside amounts for special provider groups,
12
including safety-net hospitals,
hospitals with high COVID-19 admissions, rural health care providers, and skilled nursing
facilities, but not primary care providers as a broad class.
This failure to recognize and designate primary care as a prioritized provider type can be
attributed entirely to the eld’s lack of political cohesiveness. The diversity of a modern
primary care team is simultaneously a clinical strength and political weakness. Comprising
internists, pediatricians, family practitioners, nurse practitioners, nurses, physician assis-
tants, and sometimes behavioral health clinicians and pharmacists, primary care, in contrast
to hospitals, nursing homes, community health centers, and every other group receiving
special consideration in CARES Act funding, lacks a unied voice in public policy discussions
or political negotiations. The resulting distributions reect that.
Beyond nancial relief, initial federal responses were not targeted to primary care but ben-
eted the eld nonetheless. The CARES Act, enacted on March 27, 2020, detailed a “range
of diagnostic items and services that plans and issuers must cover without any cost-sharing
requirements or prior authorization or other medical management requirements,”
13
including
the evaluation services required to assess and test for COVID-19.
The nancial eects of this order for primary care providers were relatively small. Far more
signicant was the declaration by secretary of Health and Human Services (HHS) Alex Azar on
January 30, 2020, of a public health emergency.
14
This gave the Trump administration broad
authority to change Medicare and Medicaid administrative practices. Those Medicare policy
changes with the most direct impact on primary care included the lifting of restrictions on
the use of telehealth services during the COVID-19 emergency. Key changes eective March
1 and lasting throughout the national public health emergency have specically included (1)
paying physicians for telehealth services at the same rate as in-person visits for all diagnoses,
not just services related to COVID-19; (2) allowing beneciaries to receive telehealth services
in all areas of the country and in all settings, including at their home; (3) expanding the list
of services eligible to be reported via telehealth; (4) expanding the list of qualied health care
professionals eligible to bill for telehealth; and (5) allowing physicians licensed in one state
to provide services to Medicare beneciaries in another state. In addition, the HHS Oce for
Civil Rights authorized exibility for telehealth via popular video chat applications, such as
FaceTime or Skype, during the pandemic.
15
Administratively CMS relaxed its reporting requirements for physicians under its Merit-
based Incentive Payment System for both program years 2019 and 2020.
16
These payment,
112 PRIMARY CARE IN THE COVID-19 PANDEMIC

benets, and administrative changes were implemented in Medicare Advantage, as well
as for fee-for-service enrollees. There were no changes to the Center for Medicare and
Medicaid Innovations’ (CMMI) payment models—including its largest model for primary care,
Comprehensive Primary Care Plus (CPC+)—in the wake of COVID-19. Like some commercial
insurers (discussed further later in the chapter) CMMI did advance its partial-capitation pay-
ments to its participating primary care practices, in its case for the third quarter of 2020.
The impact of Medicare’s telehealth policy was signicant, immediate, and positive. With
many commercial insurers and state Medicaid agencies following Medicare’s lead, researchers
for the Commonwealth Fund assessed that in early April 2020, at the peak of the pandemic’s
eect on the delivery system nationally, 14% of prepandemic visit levels were being provided
virtually.
17
By the summer, with more practices seeing more people in person, the proportion
had shrunk to 7% (Figure 2).
While Medicare’s telehealth policy changes resulted in increased services capacity and some
nancial relief for beleaguered primary care practices in the wake of COVID-19, it was not a
policy specically targeted toward primary care, based on prioritizing primary care providers
due to either evidence of particular vulnerability or strategic importance in pandemic re-
sponse. As we will see, other payer types followed this lead.
WWW.MILBANK.ORG
2
2 Footer Te x t
0
2
4
6
8
10
12
14
16
16-Feb
23-Feb
1-Ma r
8-Ma r
15-Mar
22-Mar
29-Mar
5-Apr
12-Apr
19-Apr
26-Apr
3-Ma y
10-May
17-May
24-May
31-May
7-Jun
14-Jun
21-Jun
28-Jun
5-Jul
12-Jul
19-Jul
26-Jul
2-Aug
9-Aug
16-Aug
23-Aug
30-Aug
6-Sep
13-Sep
20-Sep
27-Sep
4-Oct
Figure 2. Telehealth Visits in a Given Week in 2020 as a Percentage of Baseline Total Visits
10
Data derived from Mehrotra et al.
10
Percent telehealth visits, of overall visits in a week
PRIMARY CARE IN THE COVID-19 PANDEMIC 113

Medicaid responses
As a jointly funded, state-administered program, Medicaid’s policies vary considerably by
state. As with Medicare, the HHS secretary’s declaration of a public health emergency granted
new exibilities to the program, which state Medicaid agencies used in dierent ways and to
dierent extents. Few of these appear to have targeted primary care providers in particular.
A summary of COVID-19-related state Medicaid activities pertaining to provider payments
compiled by the Kaiser Family Foundation is found in Figure 3, with states most likely to
increase payment rates or provide retainer payments.
Kaiser’s analysis does not identify primary care as the target for any of these changes, al-
though some states did allocate additional funding for safety-net primary care providers such
as community health centers. A subsequent round of CARES Act funding by CMS also set aside
$15 billion in funds for Medicaid providers, including primary care providers such as commu-
nity health centers, but only if they had not participated in previous rounds.
18
This Medicaid-specic allocation is particularly important for clinical teams that care for
children, since in any given year, over 60% of US children are covered through Medicaid or
the Children’s Health Insurance Program, and children’s health care providers are excluded
WWW.MILBANK.ORG
3
3 Footer Te x t
0 10 20 30 40 50 60
Increase Provider Payment Rates
Provide Retainer Payments
Provide Interim Payments
Provide Directed Payments
Increase Nursing Facility Bed Hold or Therapeutic Leave Days
Mo dify Payment Methodology
Appendix K
State Plan Amendment or Other Administrative Authority
Section 1115
Figure 3. State Emergency Actions to Provide Support to Medicaid Providers as of June 11, 2020.
18
Number of States
Data derived from Musumeci et al.
18
114 PRIMARY CARE IN THE COVID-19 PANDEMIC
from any distributions based on Medicare billing.
19
In addition to concern about the nan-
cial viability of providers, advocates have pointed to the particular clinical needs of children
during the pandemic, including behavioral health and preventive care, and the eects of their
neglect.
20
It is not clear how these set-aside funds will be allocated and how children’s pri-
mary care providers will fare in the resulting decisions.
As with Medicare, policy decisions by Medicaid ocials in response to COVID-19 can directly
or indirectly aect primary care providers. State Medicaid activity has made telehealth ser-
vices more widely available from more providers and at enhanced rates, with 39 agencies
establishing parity with in-person visits for some portion of services.
21
Coverage has not been
as broad as Medicare, however, with only 26 states allowing telehealth services to be origi-
nated at home.
In most instances, these policies would be implemented through state contractors, or
Medicaid managed care organizations (MCOs). Beyond the state’s policy activity, many MCOs
took their own actions to respond to the pandemic. No catalog of this work exists. A review
of a voluntary compilation of activities from the largest Medicaid MCO trade group, the
Association of Community Aliated Plans (ACAP), shows some examples relating to primary
care practitioners, including advance prepayments based on historical use patterns, as well
as supplemental distributions.
22
Many of ACAP’s member MCOs are sponsored by safety-net
primary care providers or have strategic contracting relationships, which may account for
these activities.
Employer-sponsored insurance responses
Slightly less than half of employer-sponsored coverage in the United States is provided
through commercial insurance contracts overseen by state departments of insurance. The
majority is provided by self-insured employers who are exempted from state regulation
under the Employer Retirement and Income Security Act but rely on commercial insurers to
administer these benets. In the wake of COVID-19, as on other occasions, this overlapping
authority created a confusing environment for primary care providers and the delivery system
in general.
Populations covered by employer-sponsored plans were subject to the CARES mandatory
coverage requirements for testing and evaluation, but, as noted previously, these require-
ments did not have signicant eects on primary care practices. As with Medicare, of much
greater impact was the extent to which commercial insurers and self-insured employers
followed Medicare’s lead in telehealth benets and payment parity policies, waived cost-
sharing requirements for subsequent COVID-19-related treatments, or implemented primary
care–specic administrative changes.
There is no central repository for this information, but it appears that almost the entire
commercial insurance sector followed Medicare’s telehealth lead. Telehealth-related policy
changes related to employer-sponsored benets can be broken into four categories: (1) cover-
age parity with in-person visits; (2) payment parity with in-person visits; (3) cost-sharing
waivers, and (4) expansion of allowable modes and locations of origin and providers. A review
PRIMARY CARE IN THE COVID-19 PANDEMIC 115
of self-reported COVID-19-related activities by commercial insurers maintained by America’s
Health Insurance Plans (AHIP) indicates activities in all these areas and additional scattered
mentions for primary care providers but no consistent policies targeted at preserving or
strengthening primary care.
23
Some of the insurer support for telehealth may have been catalyzed by state government
activity. A review conducted for the Commonwealth Fund of state laws, regulations, and ex-
ecutive orders related to commercial insurer coverage of telehealth showed that 12 states took
action to ensure parity coverage, 12 states required parity of payment, 13 states took action
on telehealth provider networks, and 12 required parity in cost sharing. Several other states
formally encouraged their insurers to do the same thing.
A major national association of self-insured employers reported that employers followed their
administrators’ policies for telehealth coverage parity, payment parity, and networks. There
was considerably more discretion taken by these employers in implementing cost-sharing
waivers for telehealth (Pacic Business Group on Health, author inquiry).
Medicare’s sweeping changes in telehealth benets coverage created a practice that almost
all commercial insurers—with additional prodding from some state ocials—apparently felt
compelled to follow. That said, Medicare did not take actions to specically benet primary
care. Certain insurers, however, took additional steps in the wake of COVID-19 to prioritize
the importance of primary care. An Urban Institute survey of commercial insurers’ COVID-
19-related practices and concerns revealed that some were concerned about nancial rami-
cations of the pandemic on primary care practices resulting in either loss of clinicians or
consolidation into larger health systems.
24
The Milbank Memorial Fund also surveyed insurers participating in CMMI’s CPC+ program
about their activities in support of primary care during the pandemic, which gives some in-
sight into their relative prioritization of primary care practices in the pandemic (unpublished
ndings)
.
Consistent with self-reported activities by AHIP, 90% of the 44 survey respondents were cov-
ering telehealth video services at parity with in-person visits and 90% of these insurers were
paying at the same rates. Seventy-ve percent were also covering telephone services, and all
at the same rates as in-person visits. Similarly, 90% had waived cost sharing for COVID-19-
related treatments.
Of more import were the variety of practices that these insurers had either implemented or
were considering specically for primary care practices. One approach included cash ad-
vances to practices based on historical payments. To assure cash ow, insurers sometimes
adopt a practice of “interim payments” to large providers such as hospitals in the wake of a
temporary inability to pay claims. These are subsequently reconciled against actual activity.
Although the basic CPC+ payment model mixes prospective per person payments with fee for
service, there was some concern that this was not sucient to keep practices operating. While
considered by many, as of the summer of 2020, only 16% of respondents had actually imple-
mented this practice. A second approach included accelerated quality incentive payments.
Some insurers reported prepaying incentives due to the practices based on 2019 performance.
116 PRIMARY CARE IN THE COVID-19 PANDEMIC
A third approach included administrative simplication, including the relaxation of prior au-
thorization and appeals requirements, and extension of claims submission deadlines. A fourth
approach included adjusting performance standards and measurement protocols for quality
and utilization incentives for 2020.
Although objective comparisons are not possible, it is reasonable to surmise that these re-
sponses are not representative of all commercial insurer practices. Insurers that had already
committed to a primary care–oriented delivery system strategy—including participating in
multipayer activities like CPC+—would likely be more responsive to the needs of primary care
practices during the pandemic.
Similarly, because of local accountability, regional nonprot carriers could be more respon-
sive to the needs of local primary care practices than national insurers, particularly when the
equivalent needs of hospitals were being attended to by federal CARES Act eorts. Western
New York is an example of a market in which the combination of local nonprot insurers
and previous multipayer primary care transformation work allowed for a relatively quick and
comprehensive multipayer response to support primary care, including oering aligned poli-
cies to support telehealth use based on preexisting per capita payment methods, accelerating
incentive payments, and relaxing reporting requirements.
25
Looking ahead
Faced with conicting realities of the documented importance of a primary care–oriented
delivery system for population health on one hand, and the economic power of consolidated
health systems on the other, insurers have always struggled with justifying additional invest-
ments in primary care, particularly when their individual share of a given practice’s revenue
is small and the returns from such investment are likely to be diuse and long term.
Although some commercial payers—generally nonprot carriers with large market shares
such as those in the New York Capital District, Maryland, and Hawaii—had strategically dis-
tinguished themselves with delivery system strategies that prioritized primary care, COVID-19
may have made this approach more appealing.
26-28
The nancial pressure faced by primary
care increases the odds that the steadily increasing trend of employed primary care physi-
cians—most of whom work for hospitals and health systems—would accelerate.
29
For insur-
ers, this would lead to more primary care delivered in more expensive settings.
In the face of increased costs, some health insurers are reacting. For instance, Blue Cross
and/or Blue Shield insurers in Massachusetts, North Carolina, and California—each a lo-
cal nonprot with signicant market share—have all announced new contracting programs
aimed at strengthening independent primary care practices.
30-32
Although the specics vary
in each case, these insurers are hoping the nancial woes of the pandemic will make primary
care practices more willing to move from fee-for-service payment methods to a model based
on primary care capitation with additional incentives, regardless of whether these practices
become part of larger, more comprehensive risk-sharing arrangements like accountable care
organizations.
PRIMARY CARE IN THE COVID-19 PANDEMIC 117
The insurers, for their part, have presumably learned from previous experiments with pri-
mary care capitation about its important and highly sensitive components,
33
including risk
adjustment and patient attribution. It also remains to be seen if the pain of COVID-19 was a
wake-up call for independent primary care practices. Will the revenue shortfalls incurred as a
result of visit declines and a dependence on fee-for-service reimbursement motivate primary
care practices to actually shift their revenue models in fundamental ways?
The previously described activities by individual insurers are the exception, not the rule. As
the pandemic wears on, the lack of payer prioritization of primary care and the failure to align
payer practices continues to constitute a missed opportunity to reduce the pandemic’s toll and
stem the tide of primary care practice acquisition.
Voluntary, aligned prioritization of primary care by payers is unlikely. A glimpse of the
pandemic response possible when alignment is catalyzed by public policy can be seen in the
work of the Maryland Primary Care Program (MDPCP), an organized eort at primary care
transformation funded under the state’s Medicare global payment waiver. MDPCP consists
of supplemental per capita payments to participating practices from Medicare and Care First
(the state’s largest commercial insurer), as well as support for regional care transforma-
tion organizations (CTOs) that provide technical assistance, care management resources, and
data feeds to practices from CRISP, the state’s health information exchange. With the onset
of COVID-19, these resources were deployed in a systematic way as part of the pandemic
response. Capitation payments allowed practices to stay open.
34
Patients with chronic condi-
tions were identied by CRISP and prioritized for outreach and consultation by CTOs and
primary care practices. Equally important was the resulting communications network, which
has allowed public ocials to eciently reach primary care practices serving half the state’s
population with clear, consistent messaging and information.
Drawing on opportunities for more and more eective work by primary care practices to ad-
dress the pandemic and mitigate its eects, Labby et al. call for aligned payer investment in
four areas, based on lessons learned by Oregon’s care coordination organizations: (1) modern-
izing primary care access and clinical management; (2) expanding team-based care integrat-
ing behavioral health; (3) conducting screening and follow-up to address clinical, social, and
behavioral health needs; and (4) building community partnerships and trust.
35
With minimum primary care spending requirements required by law of all Oregon’s payers—
and state managed care contracts in place for public employees and Medicaid beneciaries—it
is possible to conceive of these investments being made in that state.
36
Similar minimum
spending requirements are in place in Rhode Island, and other states are making rst steps
by measuring current primary care spend rates, convening stakeholder groups, and setting
118 PRIMARY CARE IN THE COVID-19 PANDEMIC
primary care spending targets.
7
These actions create the opportunity for more future aligned
payer action in support of primary care.
Conclusions
The economic denition of a common good is a good or service that is both rivalrous (the
resource is limited, so more for one person means less for another) and nonexcludable (users
cannot be prevented from accessing the good, regardless of whether they have paid).
36
While
one might argue that morality and even US public policy—the federal Emergency Medical
Treatment and Labor Act requires that no one be turned away from an emergency room, for
instance—dictate that all health care is a common good, one could also argue that primary
care is particularly privileged as a health care common good because of both its public value
and its precarious status. Primary care provides greater increases in life expectancy and
health equity than any other health care service, and its supply continues to be diminished.
Responsible public policy requires that a common good—be it the stock of sh, grazing
grounds for farm animals or the capacity of primary care to meet the needs of a population—
merits some degree of public oversight and monitoring. In the absence of that, the good is
depleted and not available when the need for it increases.
Such has been the case with primary care in the time of COVID-19. With the possible excep-
tion of public policy in a few states that mandates payer primary care spending levels, it
was not recognized as a common good before the pandemic and its supply was weakening.
Lacking this protection, primary care has not been prioritized in public or private payer ac-
tions during the pandemic. Medicare’s (and Medicaid’s) telehealth benet changes provided
signicant relief for primary care, but the eld has received no special allocation of COVID-19
relief funds, unlike other provider groups. Commercial insurers, with some apparent excep-
tions, have largely followed Medicare’s lead and not made support of primary care—through
changes in payments or benets—a priority. Self-insured employers, with even less public
obligation or local accountability, have followed suit.
If the pandemic-era response of payers to primary care has largely been a continuation of
prepandemic policies, has the pandemic accelerated prior primary care trends, including
decreasing visit rates, clinician supply, and spending levels? It is too early to say, but visit
data and provider sentiment would indicate the pressures are increasing. The lessons of the
pandemic for those supportive of primary care, however, remain unchanged. The evidence
of primary care’s benet for the collective health of society—in general or in a time of pan-
demic—is insucient to change public policy or private payer actions. Political and economic
power is necessary.
PRIMARY CARE IN THE COVID-19 PANDEMIC 119
Acknowledgments
The research assistance of Sonika Kumar is
gratefully acknowledged.
References
1. Hargraves J, Frost A. Trends in primary care visits.
Health Care Cost Institute. November 15, 2018. Ac-
cessed November 3, 2020. https://healthcostinstitute.
org/hcci-research/trends-in-primary-care-visits.
2. Reiff J, Fuglesten Biniek J. Primary care spending in
the commercially insured population. Health Care Cost
Institute. 2019. Accessed November 3, 2020. https://
healthcostinstitute.org/images/pdfs/Academy_Health_
Poster_05102019.pdf.
3. Barbey C, Sahni N, Kocher B, Chernew ME. Physician
workforce trends and their implications for spending
growth. Health Affairs Blog. July 28, 2017. Accessed
November 3, 2020. https://www.healthaffairs.org/
do/10.1377/hblog20170728.061252/full/.
4. Basu S, Berkowitz SA, Phillips RL, Bitton A, Landon
BE, Phillips RS. Association of primary care physician
supply with population mortality in the United States,
2005-2015. JAMA Intern Med 2019;179(4):506-14.
10.1001/jamainternmed.2018.7624.
5. Stareld B, Shi L, Macinko J. Contribution of
primary care to health systems and health. Mil-
bank Q 2005;83(3):457-502. 10.1111/j.1468-
0009.2005.00409.x.
6. Peikes D, Taylor EF, O’Malley AS, Rich EC. The
changing landscape of primary care: effects of
the ACA and other efforts over the past decade.
Health Aff (Millwood) 2020;39(3):421-8. 10.1377/
hlthaff.2019.01430.
7. Jabbarpour Y, Greiner A, Jetty A, et al. Investing in
primary care: a state-level analysis. Primary Care Col-
laborative. July 2019. Accessed November 3, 2020.
https://www.pcpcc.org/sites/default/les/resources/
pcmh_evidence_es_2019.pdf.
8. Mehrotra A, Chernew M, Linetsky D, Hatch H, Cutler
D. The impact of the COVID-19 pandemic on outpa-
tient visits: a rebound emerges. Commonwealth Fund.
May 19, 2020. Accessed November 3, 2020. https://
www.commonwealthfund.org/publications/2020/apr/
impact-covid-19-outpatient-visits.
9. Quick COVID-19 survey. The Larry A. Green Center.
2020. Accessed November 3, 2020. https://www.
green-center.org/covid-survey.
10. Mehrotra A, Chernew M, Linetsky D, Hatch H, Cutler
D, Schneider EC. The impact of the COVID-19 pan-
demic on outpatient care: visits return to prepandemic
levels, but not for all providers and patients. Common-
wealth Fund. October 15, 2020. Accessed November
3, 2020. https://www.commonwealthfund.org/publica-
tions/2020/oct/impact-covid-19-pandemic-outpatient-
care-visits-return-prepandemic-levels.
11. CARES Act provider relief fund: general information.
US Department of Health and Human Services. Last
updated January 21, 2021. Accessed November 4,
2020. https://www.hhs.gov/coronavirus/cares-act-
provider-relief-fund/general-information/index.html.
12. CARES Act provider relief fund: data. US Department
of Health and Human Services. Last updated January
12, 2021. Accessed November 4, 2020. https://www.
hhs.gov/coronavirus/cares-act-provider-relief-fund/
data/index.html#fty-billion-general-distribution-alloca-
tion.
13. FAQs about Families First Coronavirus Response Act
and Coronavirus Aid, Relief, and Economic Security
Act implementation part 42. US Centers for Medicare
and Medicaid Services. April 11, 2020. Accessed No-
vember 4, 2020. https://www.cms.gov/les/document/
FFCRA-Part-42-FAQs.pdf.
14. Secretary Azar declares public health emergency for
United States for 2019 novel coronavirus. US Depart-
ment of Health and Human Services. January 31,
2020. Accessed November 4, 2020. https://www.hhs.
gov/about/news/2020/01/31/secretary-azar-declares-
public-health-emergency-us-2019-novel-coronavirus.
html.
15. Special coding advice during COVID-19 public health
emergency. American Medical Association. Last
updated May 4, 2020. Accessed November 4, 2020.
https://www.ama-assn.org/system/les/2020-05/covid-
19-coding-advice.pdf.
16. CMS announces relief for clinicians, providers, hos-
pitals and facilities participating in quality reporting
programs in response to COVID-19. US Centers for
Medicare and Medicaid Services. March 22, 2020.
Accessed November 4, 2020. https://www.cms.gov/
newsroom/press-releases/cms-announces-relief-clini-
cians-providers-hospitals-and-facilities-participating-
quality-reporting.
17. Mehrotra A, Chernew M, Linetsky D, Hatch H, Cutler
D, Schneider EC. The impact of the COVID-19 pan-
demic on outpatient visits: changing patterns of care
in the newest COVID-19 hot spots. Commonwealth
Fund. August 13, 2020. Accessed November 4, 2020.
https://www.commonwealthfund.org/publications/2020/
aug/impact-covid-19-pandemic-outpatient-visits-
changing-patterns-care-newest.
120 PRIMARY CARE IN THE COVID-19 PANDEMIC
18. Musumeci M, Rudowitz R, Hinton E, Dolan R, Pham
O. Options to Support Medicaid Providers in Re-
sponse to COVID-19. Kaiser Family Foundation. June
17, 2020. Accessed November 4, 2020. https://www.
kff.org/coronavirus-covid-19/issue-brief/options-to-
support-medicaid-providers-in-response-to-covid-19/.
19. Bump P. More than 6 in 10 American children were
enrolled in CHIP or Medicaid in 2017. Washington
Post. June 13, 2018. Accessed November 4, 2020.
https://www.washingtonpost.com/news/politics/
wp/2018/06/13/more-than-6-in-10-american-children-
were-enrolled-in-chip-or-medicaid-in-2017/.
20. Dooley DG, Bandealy A, Tschudy MM. Low-income
children and coronavirus disease 2019 (COVID-19) in
the US. JAMA Pediatr 2020;174(10):922-3. 10.1001/
jamapediatrics.2020.2065.
21. Guth M, Hinton E. State efforts to expand Medic-
aid coverage & access to telehealth in response to
COVID-19. Kaiser Family Foundation. June 22, 2020.
Accessed November 4, 2020. https://www.kff.org/coro-
navirus-covid-19/issue-brief/state-efforts-to-expand-
medicaid-coverage-access-to-telehealth-in-response-
to-covid-19/.
22. ACAP plans support providers and community organi-
zations during COVID-19. Association for Community
Afliated Plans. August 2020. Accessed November 4,
2020. https://www.communityplans.net/wp-content/
uploads/2020/08/2020_0810-COVID-Donation-Sur-
vey-Responses-1.pdf.
23. Health insurance providers respond to coronavirus
(COVID-19). America’s Health Insurance Plans. Last
updated February 3, 2021. Accessed November 4,
2020. https://www.ahip.org/health-insurance-providers-
respond-to-coronavirus-covid-19/.
24. Lucia K, Blumberg LJ, Curran E, et al. The COVID-19
pandemic—insurer insights into challenges, implica-
tions, and lessons learned. Urban Institute. June 29,
2020. Accessed November 4, 2020. https://www.
urban.org/research/publication/covid-19-pandemic-
insurer-insights-challenges-implications-and-lessons-
learned.
25. Shih A, Koller CF. Payer actions can help sustain
primary care during and after COVID-19. Milbank Me-
morial Fund Blog. April 21, 2020. Accessed November
4, 2020. https://www.milbank.org/2020/04/payer-ac-
tions-can-help-sustain-primary-care-during-and-after-
covid-19/.
26. Navathe AS, Emanuel EJ, Bond A, et al. Association
between the implementation of a population-based
primary care payment system and achievement on
quality measures in Hawaii. JAMA 2019;322(1):57-68.
10.1001/jama.2019.8113.
27. Cuellar A, Helmchen LA, Gimm G, et al. The CareFirst
patient-centered medical home program: cost and uti-
lization effects in its rst three years. J Gen Intern Med
2016;31(11):1382-8. 10.1007/s11606-016-3814-z.
28. Strengthening primary care for patients. Alliance of
Community Health Plans. 2013. Accessed November
4, 2020. https://achp.org/wp-content/uploads/CDPHP-
ACHP-Strengthening-Primary-Care-Prole.pdf.
29. Mazzolini C. Employed physicians outnumber inde-
pendent physicians for the rst time ever. Medical Eco-
nomics. May 8, 2019. Accessed November 4, 2020.
https://www.medicaleconomics.com/view/employed-
physicians-outnumber-independent-physicians-rst-
time-ever.
30. Blue Shield of California announces “primary care rei-
magined” to support network providers during COV-
ID-19 pandemic. Blue Shield of California. September
8, 2020. Accessed November 4, 2020. https://news.
blueshieldca.com/2020/09/08/blue-shield-of-california-
announces-primary-care-reimagined-to-support-net-
work-providers-during-covid-19-pandemic.
31. Blue Cross NC launches comprehensive program to
help independent primary care practices stay in busi-
ness. Blue Cross Blue Shield of North Carolina. June
24, 2020. Accessed November 4, 2020. https://me-
diacenter.bcbsnc.com/news/blue-cross-nc-launches-
comprehensive-program-to-help-independent-primary-
care-practices-stay-in-business.
32. Blue Cross Blue Shield of Massachusetts pilots new
value-based payment program for independent pri-
mary care practices. Blue Cross Blue Shield of Massa-
chusetts. July 15, 2020. Accessed November 4, 2020.
http://newsroom.bluecrossma.com/2020-07-15-Blue-
Cross-Blue-Shield-of-Massachusetts-Pilots-New-Val-
ue-Based-Payment-Program-For-Independent-Prima-
ry-Care-Practices.
33. Taylor E, Bailit M, Sayles J. Prospective payment
for primary care: lessons for future models. Milbank
Memorial Fund. September 16, 2020. Accessed No-
vember 4, 2020. https://www.milbank.org/publications/
prospective-payment-for-primary-care-lessons-for-
future-models/.
34. Klein S, Hostetter M. Maryland’s primary care pro-
gram helps practices pivot during COVID-19. Milbank
Memorial Fund. June 25, 2020. Accessed November
4, 2020. https://www.milbank.org/news/marylands-
primary-care-program-helps-practices-pivot-during-
covid-19/.
35. Labby D, DeVoe J, Morris-Singer A, Livingston C.
Supporting the critical role of primary care in the
COVID-19 response. Milbank Memorial Fund. August
19, 2020. Accessed November 4, 2020. https://www.
milbank.org/2020/08/supporting-the-critical-role-of-
primary-care-in-the-covid-19-response/.
36. Primary care spending in Oregon: a report to the
Oregon legislature. Oregon Health Authority. Febru-
ary 2020. Accessed November 4, 2020. https://www.
oregon.gov/oha/HPA/ANALYTICS/Pages/Primary-
Care-Spending.aspx.
PRIMARY CARE IN THE COVID-19 PANDEMIC 121
Financial Challenges
for Primary Care
Under COVID-19
Bruce E. Landon and Susan N. Landon
T
he COVID-19 pandemic has had a signicant and ongoing impact on the US health care system.
As of March 2020, the majority of elective procedures and in-person outpatient visits were
canceled temporarily, and only in June 2020 did in-person visits begin to rebound.
1,2
Primary care
practices, in many ways, have borne the brunt of COVID-19 on the ambulatory side of medical
practice. In addition to addressing acute conditions that might have arisen during the pandemic
and managing chronic medical conditions, they have been tasked with a myriad of new treatment
and testing issues directly related to COVID-19. In many ways, primary care practices have been
nimble in responding to the pandemic, but the pandemic also has revealed substantial challenges
and shortcomings of the nancing and payment mechanisms used for primary care in the current
US health care system.
Although in-person ambulatory care visits have rebounded to a large extent since the peak of the
shutdown in April and May 2020, primary care practices continue to feel the impact of the pan-
demic as substantial week-to-week uncertainty persists, with the virus surging in dierent parts
of the country and changes in medical practices adopted in response to COVID-19 showing no end
in sight as of the time of this writing in October 2020. In this light, we review some of the salient
issues that have impacted primary care practice nances under COVID-19 and discuss strategies
that have emerged to address these nancial challenges. We then examine some potential long-
term consequences that may emerge as a result of the pandemic, including some policy options
that may be required to help assure that a viable primary care system continues to exist after the
pandemic has receded.
The current practice environment
Primary care physicians make up just under one-third of the physician workforce in the
United States, totaling roughly 220,000 practitioners.
3
Included in this count are family
physicians, geriatricians, general practitioners, general internists, and general pediatricians.
An additional 67,600 nurse practitioners and 36,000 physician assistants contribute to the
primary care workforce.
3
Although substantial numbers of primary care physicians are em-
ployed by hospitals or health systems, more than half of US primary care physicians continue
to operate within the community as full or partial owners of independent small practices.
In contrast to hospital- or health system-owned practices, these practices lack ready access
to capital and sucient nancial reserves required to provide a base of support in the ab-
sence of ongoing revenue. Moreover, according to data from the Medical Group Management
Association (MGMA), the average primary care practice supports four support sta (including
clinical and oce sta) at a cost of well over $200,000 per year, in addition to other oper-
ating costs of similar magnitude per full-time-equivalent (FTE) physician.
4
The ability of
practices to support such operations in the current environment remains unclear.
Primary care practices are particularly vulnerable to changes in visit volume, as almost all
primary care revenue is derived from in-person evaluation and management visits. Primary
care provides more than half of the approximately 1 billion oce visits occurring annually in
the United States, and approximately 85% of visits for those with chronic medical conditions
such as hypertension and diabetes.
5
Although 89% of primary care physicians use electronic
medical record (EMR) systems, fewer practices routinely relied on telemedicine prior to the
COVID-19 pandemic.
6
This conuence of factors placed primary care practices in particularly
vulnerable nancial positions, and continues to threaten their long-term nancial viability.
Financial impact of the pandemic on primary care practices
The health system in general, and primary care practices in particular, were forced to rap-
idly pivot in response to the pandemic, though the extent to which practices have changed
in dierent parts of the country remains unclear. In the initial phases of the pandemic, in
March and April 2020, although there was no coordinated federal response, 43 states and
multiple cities and counties implemented stay-at-home orders and required the closure of
all nonessential businesses. Although health care businesses were considered essential, most
outpatient care and other elective care was deferred to minimize transmission of the virus
to other patients, clinical sta, and physicians. Moreover, many patients did not want to put
themselves at risk by leaving their homes to visit a primary care doctor for care that they felt
could be deferred. Early on in the pandemic, there also were shortages in essential protective
equipment and little guidance or knowledge as to the risk of viral transmission in dierent
settings.
According to data from Phreesia, a company that provides practice management services
to more than 50,000 providers across the country, in the immediate aftermath of the clo-
sures in March 2020, the overall number of ambulatory visits nationwide (albeit from a
124 PRIMARY CARE IN THE COVID-19 PANDEMIC
nonrepresentative sample) fell by just over 50% for primary care, with the largest changes
occurring in areas of the country most impacted by the pandemic.
1,7
As of mid-June 2020,
weekly visit counts had rebounded and plateaued at a level approximately 10% below prepan-
demic totals, and by July 2020, visit rates to primary care were just 2% below prior volumes.
2
To the surprise of many, the rebound in visit volume reected a resumption of in-person
care, though telehealth visits, which had peaked around 14% of visits nationally, continued
to be used for approximately 7% to 10% of visits. A second data source, Healthjump (an
electronic medical records database including data from 34,393 physicians), suggested that
oce visit volume fell even more dramatically, estimating that visit volume declined by as
much as 64% (compared to February 2020). Similar to what was shown in the Phreesia data,
Healthjump data showed that telehealth grew rapidly through April, but by July had pla-
teaued at 11% of visits. In contrast to the Phreesia data, the Healthjump data did not show as
dramatic a resumption of visits, with total oce visits rebounding to only 82% of baseline
(February 2020) visits by the end of July 2020 (Aaron Baum, PhD, personal communication
based on analyses of Healthjump data, October 2020).
Notably, the rebound of in-person visits showed marked variation across dierent primary
care practice settings. For example, rebound rates varied by location. Not surprisingly, as the
virus surged in dierent areas of the country, primary care practices substituted telemedicine
visits for in-person visits at higher rates, though they still continued to provide the majority
of visits in person. In addition, the rebound of in-person visits was much lower for children,
where visits across a range of ages continued to be 30% to 40% lower than normal by mid-
June.
1
Finally, community health centers had in-person visits rebound at a lower rate, and
they continued to provide telemedicine visits at a rate of twice that of other practices.
1
Through the rst six months of 2020, primary care practices pivoted to providing telehealth
(including both video and telephonic) while the government liberalized regulations allow-
ing for telehealth provision and reimbursement. Nevertheless, some practices adapted to
telehealth provision more quickly than others, as telehealth often required investments in
new technology platforms, substantial integration with existing EMRs, development of new
scheduling and workow processes and templates, and training of sta. In addition, though
all practices have the capacity to conduct visits by telephone, many may not have had suf-
cient access to high-speed Internet or other infrastructure necessary to provide video
visits. Although liberalized rules during the public health emergency allowed for provision of
telehealth services using basic equipment such as normal telephone lines or cell phones, the
process of realizing such visits proved daunting for many practices.
8
Regulations and policies governing the conduct of and reimbursement for remote visits have
rapidly evolved, producing considerable uncertainty for practices.
9
Although Medicare agreed
to pay for telephone and telemedicine visits retroactive to March 2020, and some private in-
surers also have reimbursed remote visits at standard in-person evaluation and management
visit rates, the extent to which such visits are able to replace the revenue of in-person visits
and support the existing sta of primary care practices remains unclear.
8
More important,
many patients prefer in-person visits, and not all visits and patient conditions are appropriate
for telemedicine. Thus, even in settings that have developed remote capabilities, the uptake
PRIMARY CARE IN THE COVID-19 PANDEMIC 125
of remote visits is likely to be only a percentage of practices’ prior in-person visit volume. A
serial survey of primary care physicians in 48 states, Puerto Rico, and the Virgin Islands in
late March 2020 found that 87% of respondents limited in-person visits and 60% were unable
to perform any video visits.
10
In addition to developing capabilities to deliver remote care, primary care practices also had
to respond to the pandemic in a number of other ways, all of which can impact their revenue
and cost structure. The issues presented during the pandemic impacted every facet of op-
erations of primary care practices, all with signicant nancial implications. First, though
practices limited in-person visits, anecdotal reports suggest large increases in telephone calls
to practices, often to discuss potential symptoms or exposures to COVID-19 and to request
COVID-19 testing. Due to the lack of testing resources throughout the country, testing cen-
ters required careful vetting of requests to reserve testing for those who required it most.
Screening and triage of people with potential COVID-19 infection was generally carried out by
primary care practices. Even as testing shortages eased over time, practices needed to devote
substantial personnel resources to review testing criteria with patients, provide test results,
and counsel patients with COVID-19 symptoms, exposures, or positive test results. There was
also a substantial amount of telephone triage and follow-up that occurred for patients with
acute or chronic issues unrelated to COVID-19, often outside the context of a virtual visit.
Though no systematic data are available, Figure 1 shows the volume of telephone calls to one
large academic practice in Boston. Notably, after an initial decline in calls as fewer patients
were calling to schedule appointments, calls requiring nurse triage increased more than 150%
and then maintained a volume that was just under 200% of the baseline rate. Similarly, when
compared to the same six-month period in 2019, unreimbursed patient portal messages
increased 60% from March 2020 to September 2020.
Upon the resumption of in-person visits, additional resources were required to assure the
provision of safe care in the context of the ongoing pandemic. The additional resources in-
cluded changing scheduling templates, modifying clinic workows to decrease or eliminate
use of common spaces and waiting rooms (e.g., all phlebotomy, vaccinations, and checkout
services performed in the exam room), and setting up protocols for and investing in personal
protective equipment for sta and patients visiting the practice. Because of dramatic drops
in revenue from in-person visits at the start of the pandemic, many practices, in particular
independent practices, were forced to implement some of these changes after furloughing
employees early on in the pandemic. Although minimal data are available on these issues,
the Primary Care Coalition, in collaboration with the Robert Graham Center, performed
weekly surveys of primary care practices throughout the COVID-19 pandemic. Based on ap-
proximately 150 responses from mostly family physicians, as early as late March, over 15% of
respondents employed strategies to decrease stang costs (e.g., layos, furloughs, voluntary
pay cuts, etc.).
10
The percentage increased to 37% just one month later.
11
Data on how primary care practices have fared nancially under COVID-19 are lacking. Among
the most comprehensive are projections derived from a microsimulation model of primary
care nances published by Basu et al. in Health Aairs
.
12
That study used a validated micro-
simulation model in combination with data on how COVID-19 has impacted visit volumes as
126 PRIMARY CARE IN THE COVID-19 PANDEMIC

Figure 1. Call Center Data from a Large Boston-Area Primary Care Practice (October 7, 2019 through
September 14, 2020)
Source: Personal communication from Kayla Tremblay, practice manager.
0
200
400
600
800
1000
1200
7- Oct
7-Nov
7- Dec
7-Jan
7-Feb
7- Mar
7- Apr
7- May
7-Jun
7-Jul
7- Aug
7-Sep
7- Oct
Triage Calls Answered (Weekly)
Total Calls media n
0
1000
2000
3000
4000
5000
6000
7- Oct
7-Nov
7- Dec
7-Jan
7-Feb
7- Mar
7- Apr
7- May
7-Jun
7-Jul
7- Aug
7-Sep
7- Oct
Call Center Total Calls (Weekly)
Total Calls Median
well as payment policies for telehealth instituted by the Centers for Medicare and Medicaid
Services to estimate the impact of COVID-19 on primary care practices nationally, assum-
ing no change in cost structure. In sensitivity analyses, however, the model incorporated
changes in costs that might have resulted from furloughing sta to the level of the 25th
percentile in national stang data from the Medical Group Management Association. The
analysis projects that, on average, primary care practices would experience decreased revenue
of more than $67,000 per FTE physician, amounting to approximately $15 billion in reduced
revenue for primary care practices nationally.
12
Notably, some practices would potentially
PRIMARY CARE IN THE COVID-19 PANDEMIC 127
move into negative net income for the year. The level of decreased revenue could be reduced
by about half if cost savings strategies such as sta furloughs were employed. This simula-
tion reected the liberalization in reimbursement policies for telehealth that were enacted by
the Centers for Medicare and Medicaid Services (retroactive to March 2020). Losses would be
larger if telehealth payment policies revert to baseline in the pre-COVID era and if there are
resurgences of COVID-19 causing reimplementation of shelter-in-place orders.
12
Notably, the analysis could not incorporate additional costs related to implementation of
telehealth technology, changes in practice ow and training of sta, or personal protective
equipment expenses. There also are at least three other potential costs that were not consid-
ered. First, as noted earlier, increased volume of telephone calls, whether directly related to
COVID-19 symptoms and testing or other acute or chronic medical issues, requires adequate
stang and reects activity that is not reimbursed. Similarly, increased patient portal volume
also represents additional work that currently is not reimbursed. Second, some practices col-
lect signicant ancillary revenue from performing laboratory or radiology tests in their prac-
tice. With the decrease in in-person services, these revenues also have shrunk substantially,
with tests either being deferred or done elsewhere. Finally, though no national strategy has
been released, it is likely that primary care practices will play a major role in administering
COVID-19 vaccines in the coming years, which will present additional logistical and coordina-
tion expenses for practices, particularly given the need to minimize exposures and maintain
social distance for patients coming to clinics in person to receive vaccines.
Beyond the microsimulation data, there are remarkably little representative data on the
impact of COVID-19 on primary care nances, though some small surveys suggest substantial
impacts on practice nances. For example, a survey conducted by the Physicians Foundation
in July 2020 reports responses from more than 3,500 physicians, of whom 39% reported
practicing primary care. Of note, the survey had a low response rate, so cannot be considered
representative.
11
In that survey, 43% of all respondents reported that they had reduced sta
and 8% had closed their practices.
13
Among the 8% who had closed their practices, just under
one-fourth reported practicing in primary care. Similarly, data from the monthly surveys
administered by the Graham Center and the Primary Care Coalition show that, as of the end of
June 2020, more than 70% of respondents felt under nancial strain, even if they had received
government help through Paycheck Protection Program funds (detailed in the next section).
11
Strategies to address nancial challenges to primary care
On March 27, 2020, the Coronavirus Aid, Relief, and Economic Security (CARES) Act was
signed into law, providing $2 trillion in relief for economic damage brought about by the
COVID-19 pandemic. On April 24, 2020, an additional $484 billion was allocated through the
Paycheck Protection Program (PPP) and Health Care Enhancement Act to supplement fund-
ing for CARES Act programs.
14
A number of provisions in the CARES Act directly or indirectly
targeted health care providers, practices, and hospitals, in an eort to mitigate the economic
eects on these organizations and individuals.
128 PRIMARY CARE IN THE COVID-19 PANDEMIC
One of the main mechanisms by which the CARES Act supported primary care practices was
through PPP loans. The CARES Act initially allocated $349 billion to loans for businesses with
fewer than 500 employees (including physician practices). Under this arrangement, primary
care practices meeting this criterion could receive loans up to 250% of monthly payroll ex-
penses to cover eight weeks of payroll as well as other xed costs of running the practice, up
to a maximum of $10 million.
15
If a given practice maintained employment and salary levels
above a certain threshold, the loans would be forgiven. Any portion of a PPP loan not forgiven
must be repaid within 10 years at a maximum interest rate of 4%. Additional funding for the
PPP program was provided in the Paycheck Protection Program and Health Care Enhancement
Act.
15
In addition to PPP loans, the CARES Act expanded eligibility for the Economic Injury
Disaster Loan (EIDL) and also allocated $10 billion for small businesses in low-income com-
munities to request advances of up to $10,000 that could be used for immediate working
capital needs. Though the EIDL loans must be paid back, the advances, which could be used
for employee sick leave, maintaining payroll, covering costs of materials, paying xed costs,
or repaying debt, do not need to be paid back, but the amount would be subtracted from the
amount forgiven in the PPP loan.
15
In the same way that the PPP and EIDL loans bear the
economic burden of the pandemic, they also helped physician practices to maintain nancial
stability and retain employees.
Beyond the PPP and EIDL loans, the CARES Act also included numerous relief provisions spe-
cically targeting health care organizations. For example, the CARES Act provided funding to
cover COVID-19-related expenses in health care organizations such as increased sta, train-
ing, personal protective equipment, medical supplies and devices, and COVID-19 care, as well
as general lost revenue.
15
In addition, the CARES Act set out grant programs to improve access
to care in rural areas, which may be particularly vulnerable to a wave of COVID-19. Moreover,
the CARES Act set restrictions on changes to reimbursement rates in an eort to protect pro-
viders from further nancial burden.
15
Table 1 provides a summary of strategies (both within
and beyond the CARES Act) aiming to address nancial challenges in primary care during the
COVID-19 pandemic.
As the necessity of telemedicine became inevitable, the Centers for Medicare and Medicaid
Services instituted policy changes (some of which were outlined in the CARES Act) to bet-
ter accommodate this shift and accelerate essential changes in reimbursement. First and
foremost, the Centers for Medicare and Medicaid Services expanded utilization of telephone
and telehealth services to allow all Medicare beneciaries access with no copayments. Under
these policies, both new and established patients were allowed to receive care from a broad
range of practitioners across state lines.
16
Beginning on March 1, 2020, telephone and telehealth
visits also were reimbursed at the same rates as outpatient oce visits—and requirements
such as performing a physical exam, conducting telehealth visits from a particular location, or
using a specied secure platform were waived.
17
In addition, to further support providers, the
US Department of Health and Human Services launched a program to reimburse physicians at
Medicare rates for providing diagnostic testing or treatment for uninsured COVID-19 patients.
18
Further, as part of the CARES Act, the Centers for Medicare and Medicaid Services expanded
the Accelerated and Advance Payment Program to distribute funding to hospitals and other
PRIMARY CARE IN THE COVID-19 PANDEMIC 129

Table 1. Summary of Strategies to Address Financial Challenges in Primary Care
Program Eligibility Summary of Program Elements
Paycheck Protection
Program (PPP) loans
Small businesses
with <500
employees
Provides loans up to 250% of monthly payroll costs to cover 8
weeks of payroll, rent, utilities, and other such payments
Maximum loan $10 million
Loans forgiven if threshold employment and salary levels
maintained; otherwise, must be repaid within 10 years
Economic Injury
Disaster Loans (EIDL)
Small businesses
with <500
employees
Expanded access to EIDL loans
Allows businesses in low-income areas to request advances on
Economic Injury Disaster Loans of up to $10,000
EIDL loans must be repaid but advances are forgiven (though
deducted from the amount forgiven for PPP loans)
Provider Relief grants
Any health care
entities
Provides nancing for COVID-19 expenses including sta,
training, personal protective equipment, and lost revenue
Supplemental grants for detection, treatment, prevention, and
diagnosis of COVID-19 were also distributed
Accelerated and Advance
Payments
Medicare and
other payers
Loans to providers to cover any disruptions in claims during
the pandemic
Loans start to be repaid from new claims reimbursements 1
year after loan initiation
Rural health service
grants
Rural health
centers and
providers
Renews Health Resources and Services Administration grants
to improve and expand rural community health
Expands grants specically focused on telehealth in rural
communities
Reimbursement for
uninsured
Practices testing
and treating
COVID-19
Clinicians performing diagnostic testing or treating patients
with COVID-19 can submit claims for uninsured patients to US
Department of Health and Human Services for reimbursement
Sequestration
adjustment
Medicare
providers
Exempts Medicare programs from any budget sequestrations
from May 1 through December 1, 2020
Telehealth expansion
Medicare/private
payers
Increased exibility in telehealth visits in terms of eligible
providers, patients, locations, appointment elements, and
software
Centers for Medicare and Medicaid Services now reimburses
telehealth visits as it does in-person visits
Telehealth copayments waived for patients (even if enrolled in
a high-deductible health plan)
Merit-Based Incentive
Payment System (MIPS)
changes
Medicare
providers
Practices unable to submit Merit-Based Incentive Payment
System data received neutral payments or could submit
applications to have performance scores reweighted due to
extreme, uncontrollable circumstances
Commercial health plan
value-based payment
Example: Blue
Cross of North
Carolina primary
care practices
Participating practices receive monthly payments based on
2019 revenue
Practices enroll in value-based payment program with quality
and cost benchmarks
In 2022, practices can transition from fee-for-service to
capitation-based pay
130 PRIMARY CARE IN THE COVID-19 PANDEMIC
providers experiencing disruptions in revenue.
19
These loans provided advance reimburse-
ment from Medicare fee-for-service payments. Repayment of these loans was initially slated
to begin 120 days after the rst loan payment, but on October 1, 2020, the loan repayment
timeline was extended to one year after the rst loan disbursement.
19
Repayments will be
taken directly from new claims, with 25% of new claims taken out to cover these loans for 11
months, then 50% for the following six months. Providers must fully repay the loans within
29 months of the rst disbursement or they will be charged at a monthly interest rate of 4%.
19
Numerous private insurers have also instituted advance payment programs for practices and
providers.
20
These programs, however, present challenges to primary care as they will have to
be repaid out of future operating revenue. Most primary care practices have limited ability to
increase their hours to generate additional patient volume, suggesting that loans will need to
be paid back from future physician pay.
Over the past months, the Centers for Medicare and Medicaid Services also implemented
changes to the Merit-Based Incentive Payment System (MIPS) to protect providers and prac-
tices against extreme nancial losses.
21
For example, individual clinicians who did not submit
MIPS data by April 30, 2020, will automatically receive neutral payments for 2021. Practices
that could not complete MIPS data submission due to COVID-19 also were able to submit
applications based on extreme and uncontrollable circumstances to receive reweighted MIPS
performance scores.
21
MIPS performance scores traditionally are used to determine payment
increases or reductions, so such policies protect providers and practices from seeing signi-
cant funding cuts following the unprecedented shifts seen during the COVID-19 pandemic.
In addition to these federal policies, individual health plans implemented strategies to miti-
gate economic eects on primary care providers and practices. For example, the Accelerate
to Value program of Blue Cross and Blue Shield of North Carolina (BCNC)
22
aims to promote
high-value care among independently owned primary care practices while helping them to
remain nancially viable throughout and beyond the COVID-19 pandemic. Participating prac-
tices will receive capitated monthly lump-sum payments from BCNC based on 2019 revenue,
but also have to commit to participating in a value-based care program that holds providers
accountable for reaching quality and cost benchmarks.
22
Similarly, as part of their Health
Reimagined initiative, Blue Shield of California introduced a program in September 2020 that
oers select physician practices the opportunity to shift to a capitated payment model with
additional nancial incentives for meeting quality and patient experience benchmarks.
23
These capitated payment and value-based approaches are designed to provide economic secu-
rity through the pandemic in return for a future commitment to adopting a value-based pay-
ment strategy. In July, Blue Cross Blue Shield of Massachusetts also announced an expansion
of its value-based payment approach, the Alternative Quality Contract (AQC), which extends
an AQC-type model to independent primary care practices while also shifting to a primary
care capitation model (i.e., a risk-adjusted monthly fee to provide primary care for all “en-
rolled” patients) and oering additional incentives for meeting certain quality benchmarks.
24
Although the announcement of the Massachusetts program expansion was not explicitly tied
to economic eects of the COVID-19 pandemic, today’s nancial uncertainties may accelerate
entry into alternative payment programs like this.
PRIMARY CARE IN THE COVID-19 PANDEMIC 131
Long-term consequences
Despite the mitigation strategies put into place to protect primary care practices from nan-
cial collapse, it is likely that the nancial challenges faced by primary care under COVID-19
will result in more far-reaching and long-lasting changes. In some cases, COVID-19 might
accelerate the adoption of innovative approaches to primary care; in other cases, the pandemic
could result in serious challenges for the primary care system in many parts of the country.
Continued challenges
Even with primary care visits largely rebounding since the start of the pandemic, changes
in practice organization and operations persist alongside the looming threat of another
COVID-19 surge, leaving lingering nancial concerns. Moreover, particularly for smaller,
independent practices that lack signicant sources of capital and nancial reserves, the
future remains uncertain. With this in mind, it is likely that we will see primary care practice
closures and consolidation in the wake of the pandemic. Practices with signicant nancial
resources in reserve and the capacity to adapt to new regulatory requirements within the
oce and new telehealth platforms outside of the oce are likely to withstand the test of the
pandemic, but practices without even one of these three elements are likely to struggle.
Acceleration of consolidation
Primary care practice consolidation was on the rise prior to the start of the pandemic, mir-
roring a declining trend in the percentage of providers who have ownership in their practices.
Consolidation is changing the landscape of primary care, and it is likely that the COVID-19
pandemic will hasten the demise of independent primary care practices. Such consolidation
has been associated with increased prices
25,26
and decreased physician satisfaction.
27,28
Accelerating payment reform
Despite these negative consequences of COVID-19 on primary care practices, positive eects
on payment reform, innovation, and competition are also likely to be seen in primary care.
For many years, researchers have lambasted the traditional fee-for-service payment structure
that exists in the United States. Particularly for a specialty like primary care that must provide
rst contact, continuous, coordinated, and comprehensive care, the fee-for-service payment
system that limits payment to face-to-face visits and services is poorly matched to the tasks
required to deliver such care. Moreover, a payment system that incentivizes utilization of
services is bound to generate wasteful spending and visits that are not patient-centered. At
times, this could be at a detriment to patient health and well-being.
29,30
Shifting to a payment
system based on primary care, for example, incentivizes providers to be more considerate and
discerning in their utilization of health care resources.
At the same time, capitation allows providers to expect a set payment per patient per month,
ensuring a baseline level of nancial security. When practices minimized in-person vis-
its at the peak of the pandemic, service utilization was at a nadir and thus fee-for-service
132 PRIMARY CARE IN THE COVID-19 PANDEMIC
payments were too. In a capitated payment system, providers would have seen fewer nan-
cial consequences at that time. Overall, transitioning to capitation presents an opportunity
to improve health care value in the long term while protecting providers’ nancial security.
Payment reform has been a discussion among health care researchers and policymakers for
years, but the COVID-19 pandemic may accelerate the transition to these models, as we have
already seen in some of the health plan programs mentioned earlier.
Accelerating innovation
To respond to changing circumstances, primary care practices have had to develop innova-
tive strategies in telehealth and practice organization. Although telemedicine has been on
the horizon for some time, it had yet to become a part of routine practice. For many aspects
of primary care, telehealth can provide an appealing alternative to an in-person visit, allow-
ing patients to speak to their provider easily without the hassle of coming into the oce.
For patients who may have diculty accessing a primary care clinic due to location or time
constraints, telemedicine also may eectively remove barriers to care. Thus, the pandemic has
accelerated the adoption of telemedicine and other virtual and/or asynchronous approaches to
care that will tend to enhance the ability of primary care practices to deliver patient-centered
care. Moreover, to the extent that payment reforms such as primary care capitation are
adopted, this also will ease concerns of payers that decreasing barriers to care through tele-
medicine might actually lead to increased utilization.
Finally, in spite of expected primary care practice consolidation in the wake of the pandemic,
enhanced competition may emerge from new, innovative delivery models, including conve-
nience care settings such as retail health clinics, or virtual platforms such as telemedicine-
focused companies moving into the primary care space. During the pandemic, ease of access
and eciency of care were particularly important to patients. Thus, patients may have turned
to sources such as retail clinics and virtual platforms while primary care practices were closed
or limited in their capacity. These platforms are developing new and innovative technologies
to overcome the limitation of not being able to perform physical exams, which could enhance
their ability to deliver comprehensive care. What is not known, however, is the extent to which
such innovative platforms will be reserved mostly for generally well patients or whether such
models will be able to adapt their model to care for patients with multiple chronic conditions.
Regardless of the patient population served, creating open lines of communication and coordi-
nating care across multiple providers operating through dierent health care platforms will be
crucial to the long-term viability and success of these innovations in care delivery.
Conclusions
The COVID-19 pandemic has had a profound and consequential impact on primary care prac-
tices and their nancial stability. Overall, primary care practices have responded swiftly and
creatively, adapting to telehealth platforms and restructuring care delivery, but the economic
impact of the pandemic continues to threaten their long-term viability. Strategies aim-
ing to mitigate economic eects of the pandemic on primary care practices have primarily
PRIMARY CARE IN THE COVID-19 PANDEMIC 133
References
1. Mehrotra A, Chernew M, Linetsky D, Hatch H, Cutler
D. What impact has COVID-19 had on outpatient vis-
its? Commonwealth Fund. May 19, 2020. Accessed
January 10, 2021. https://doi.org/10.26099/ds9e-
jm36.
2. Mehrotra A, Chernew M, Linetsky D, Hatch H, Cutler
D. The impact of the COVID-19 pandemic on outpa-
tient visits: practices are adapting to the new normal.
Commonwealth Fund. June 25, 2020. Accessed
January 10, 2021. https://doi.org/10.26099/2v5t-9y63.
3. Petterson S, McNellis R, Klink, K, Meyers D, Ba-
zemore A. The state of primary care in the United
States: a chartbook of facts and statistics. Robert
Graham Center. January 2018. Accessed October 14,
2020. https://www.graham-center.org/content/dam/
rgc/documents/publications-reports/reports/Primary-
CareChartbook.pdf.
4. MGMA datadrive overview. Medical Group Manage-
ment Association. August 19, 2020. Accessed Octo-
ber 14, 2020. https://www.mgma.com/data/landing-
pages/mgma-datadive-overview.
5. Ambulatory health care data. National Center for
Health Statistics. Last updated January 5, 2021.
Accessed November 15, 2020. https://www.cdc.gov/
nchs/ahcd/index.htm.
6. Myrick KL, Ogburn DF, Ward BW. Percentage of
ofce-based physicians using any electronic health
record (EHR)/electronic medical record (EMR) sys-
tem and physicians that have a certied EHR/EMR
system, by U.S. state: National Electronic Health
Records Survey, 2017. National Center for Health
Statistics. January 2019. Accessed November 15,
2020. https://www.cdc.gov/nchs/data/nehrs/2017_NE-
HRS_Web_Table_EHR_State.pdf.
7. Mehrotra A, Chernew M, Linetsky D, Hatch H, Cutler
D, Schneider EC. The impact of the COVID-19 pan-
demic on outpatient visits: changing patterns of care
in the newest COVID-19 hot spots. Commonwealth
Fund. August 13, 2020. Accessed November 15,
2020. https://doi.org/10.26099/yaqe-q550.
8. Hollander JE, Carr BG. Virtually perfect? Telemedi-
cine for COVID-19. N Engl J Med 2020;382(18):1679-
81. 10.1056/NEJMp2003539.
9. Mehrotra A, Wang B, Snyder G. Telemedicine: what
should the post-pandemic regulatory and payment
landscape look like? Commonwealth Fund. August
5, 2020. Accessed October 14, 2020. https://doi.
org/10.26099/7ccp-en63.
10. Primary care and COVID-19: week 2 survey. Pri-
mary Care Collaborative. March 26, 2020. Accessed
October 14, 2020. https://www.pcpcc.org/2020/03/26/
primary-care-covid-19-week-2-survey.
11. New data shows panic among primary care patients
as practices face mounting nancial burdens, layoffs
and closures. Primary Care Collaborative. May 27,
2020. Accessed October 14, 2020. https://www.pcpcc.
org/2020/05/27/new-data-shows-panic-among-prima-
ry-care-patients-practices-face-mounting-nancial.
focused on short-term grants and loans, as well as expansion of reimbursement for tele-
health visits to date, but they have failed to address the issue of long-term nancial stability.
Consequently, practice closures and consolidations are likely to rise in the coming months
alongside opportunities to reform primary care through payment reform, innovative care de-
livery, and increased competition. As the COVID-19 pandemic enters into its next phases, se-
curing the economic future of primary care practices will be central to overcoming COVID-19,
ensuring the health of the US population, and maintaining a functional health system.
134 PRIMARY CARE IN THE COVID-19 PANDEMIC
12. Basu S, Phillips RS, Phillips R, Peterson LE,
Landon BE. Primary care practice nances in
the United States amid the COVID-19 pandemic.
Health Aff (Millwood) 2020;39(9):1605-14. 10.1377/
hlthaff.2020.00794.
13. Pandemic dangers drive some doctors to switch jobs,
retire early. Consumer HealthDay. October 13, 2020.
Accessed October 14, 2020. https://consumer.health-
day.com/infectious-disease-information-21/coronavi-
rus-1008/pandemic-dangers-drive-some-doctors-to-
switch-jobs-retire-early-762018.html.
14. What the CARES Act means for physicians & medical
students. American Medical Association. Last updated
June 16, 2020. Accessed October 15, 2020. https://
www.ama-assn.org/delivering-care/public-health/
what-cares-act-means-physicians-medical-students.
15. H.R. 748, the “Coronavirus Aid, Relief, and Economic
Security Act” (CARES Act) health care highlights.
American Medical Association. 2020. Accessed
October 15, 2020. https://www.ama-assn.org/system/
les/2020-03/summary-H.R.%20748-cares-act.pdf.
16. Physicians and other clinicians: CMS exibilities to
ght COVID-19. Centers for Medicare and Medicaid
Services. Last updated January 28, 2021. Accessed
October 15, 2020. https://www.cms.gov/les/docu-
ment/covid-19-physicians-and-clinicians.pdf.
17. Moore K. Medicare provides more regulatory relief in
response to COVID-19. American Academy of Fam-
ily Physicians. April 6, 2020. Accessed October 15,
2020. https://www.aafp.org/journals/fpm/blogs/getting-
paid/entry/medicare_covid_changes.html.
18. Claims reimbursement to health care providers and
facilities for testing and treatment of the uninsured
during COVID-19. American Academy of Family
Physicians. Accessed October 15, 2020. https://www.
aafp.org/family-physician/patient-care/current-hot-top-
ics/recent-outbreaks/covid-19/covid-19-nancial-relief/
uninsured-patient-reimbursement-program.html.
19. Cubanski J, Schwartz K, Fuglesten Biniek J, Neuman
T. Medicare accelerated and advance payments for
COVID-19 revenue loss: more time to repay. Kaiser
Family Foundation. October 8, 2020. Accessed Octo-
ber 14, 2020. https://www.kff.org/medicare/issue-brief/
medicare-accelerated-and-advance-payments-for-
covid-19-revenue-loss-more-time-to-repay/.
20. Advanced and accelerated insurance payment pro-
grams available during COVID-19. American Col-
lege of Obstetricians and Gynecologists. Accessed
October 14, 2020. https://www.acog.org/practice-man-
agement/payment-resources/resources/advanced-
and-accelerated-insurance-payment-programs-avail-
able-during-covid-19.
21. COVID-19 response. Quality Payment Program. Last
updated December 12, 2020. Accessed October 14,
2020. https://qpp.cms.gov/about/covid19?py=2020.
22. Blue Cross NC launches comprehensive program
to help independent primary care practices stay in
business. Blue Cross Blue Shield. June 24, 2020.
Accessed October 14, 2020. https://www.bcbs.com/
press-releases/blue-cross-nc-launches-comprehen-
sive-program-help-independent-primary-care-practic-
es.
23. Blue Shield of California announces “primary care
reimagined” to support network providers during CO-
VID-19 pandemic. Blue Shield of California. Septem-
ber 8, 2020. Accessed November 17, 2020. https://
news.blueshieldca.com/2020/09/08/blue-shield-of-
california-announces-primary-care-reimagined-to-sup-
port-network-providers-during-covid-19-pandemic.
24. Blue Cross Blue Shield of Massachusetts pilots new
value-based payment program for independent
primary care practices. Blue Cross Blue Shield of
Massachusetts. July 15, 2020. Accessed October
14, 2020. http://newsroom.bluecrossma.com/2020-
07-15-Blue-Cross-Blue-Shield-of-Massachusetts-
Pilots-New-Value-Based-Payment-Program-For-Inde-
pendent-Primary-Care-Practices.
25. Baker LC, Bundorf MK, Kessler DP. Vertical inte-
gration: hospital ownership of physician practices
is associated with higher prices and spending.
Health Aff (Millwood) 2014;33(5):756-63. 10.1377/
hlthaff.2013.1279.
26. Schefer RM, Arnold DR, Whaley CM. Consolida-
tion trends in California’s health care system: im-
pacts on ACA premiums and outpatient visit prices.
Health Aff (Millwood) 2018;37(9):1409-16. 10.1377/
hlthaff.2018.0472.
27. Landon BE, Reschovsky JD, Pham HH, Blumenthal
D. Leaving medicine: the consequences of physi-
cian dissatisfaction. Med Care 2006;44(3):234-42.
10.1097/01.mlr.0000199848.17133.9b.
28. Friedberg MW, Chen PG, Van Busum KR, et al. Fac-
tors affecting physician professional satisfaction and
their implications for patient care, health systems, and
health policy. Rand Health Q 2014;3(4):1.
29. Basu S, Phillips RS, Song Z, Bitton A, Landon BE.
High levels of capitation payments needed to shift
primary care toward proactive team and nonvisit care.
Health Aff (Millwood) 2017;36(9):1599-605. 10.1377/
hlthaff.2017.0367.
30. Landon BE. Structuring payments to patient-centered
medical homes. JAMA 2014;312(16):1633-4. 10.1001/
jama.2014.9529.
PRIMARY CARE IN THE COVID-19 PANDEMIC 135
Financial Consolidation
of Primary Care
Practices During and
After COVID-19
Adam E. Block, Lauren Block, and Maya Alexandri
T
he COVID-19 pandemic changed the ways that we work, go to school, shop, and eat, and even
the way we breathe. Health care providers were dramatically aected, and often not in the
way that was expected. Somehow a public health crisis, resulting in millions of sick Americans,
counterintuitively resulted in a nancial crisis for health care providers across the country. Primary
care providers, the rst-line stop for many patients with symptoms of COVID-19, were particularly
nancially vulnerable during the spring, summer, and fall of 2020.
On March 18, 2020, in response to the COVID-19 pandemic, the Centers for Medicare and Medicaid
Services (CMS) issued recommendations to postpone all nonemergent medical care conducted in
ambulatory care sites, hospital outpatient departments, medical oces, and Federally Qualied
Health Centers (FQHCs), as well as rural health care facilities.
1,2
The purpose of these recommenda-
tions was to limit the spread of COVID-19 and to preserve personal protective equipment and other
medical resources, such as ventilators. Guidance from 36 states and the District of Columbia rein-
forced the CMS recommendations.
3
Impact of COVID-19 on primary care
Financial impact
By the end of March 2020, the number of nonemergent medical visits across all practices had dra-
matically reduced. A Commonwealth Fund study analyzing data from more than 50,000 medical
practices found a 59% decline in ambulatory care visits between March 1 and March 29 of 2020.
4
Medical Group Management Association (MGMA), surveying 724 respondents across all practice types
between April 7 and 8, 2020, conrmed a patient volume reduction of 60%.
5

In a primarily fee-for-service environment, volume downturn meant major revenue loss.
MGMA reported a 55% decrease in revenue during the rst week of April.
5
In mid-July the
Physicians Foundation, surveying medical practices in 20 states, found that 55% of respon-
dents across all practices reported income losses of between 26% and 100%.
6
The reported
income losses were consistent across geographic regions. At least 11 states released the results
of surveys conducted of their medical practices.
7-18
The majority of practices experienced both
a decline in patient volume and corresponding loss of revenue (Table 1).
Table 1. Key Findings From State-Specic Surveys of Physicians
State Period of
Survey
Key Findings
Alabama
7
Spring/
Summer 2020
59% of respondents reported revenue reduction of greater than
50% because of reduction in practice volume.
California
8
April 2020 Between March and April 2020, revenue declined by an average of
64%, with 98% of respondents reporting “substantial” declines in
patient volume.
Colorado
9,10
July 2020
August 2020
75% of respondents face challenges to the nancial survival of
their practices.
Indiana
11
April 2020 More than 80% of respondents reported more than 40% decline in
both patient volume and revenues.
Kentucky
12
April 2020 73% of respondents reported patient volume declines of greater
than 50%, and 69% reported revenue volumes declining by greater
than 50%.
Massachusetts
13
May-July
2020
A 44% reduction of in-person visits since March, with
corresponding revenue losses, was reported.
Minnesota
14
June-July
2020
Overall median patient volume decreases of 56% and overall
median revenue decrease of 46% were reported.
New York
15
April-May
2020
More than 75% of respondents reported declines in patient volume
and revenue in excess of 50%.
Pennsylvania
16
April 2020 71% of respondents reported a decline in patient volume between
51% and 100%.
Texas
17
May 2020 63% of respondents indicated that their revenue had declined by
more than 50%.
Washington
18
April 2020 The mean patient volume decrease was 62%, and 92% of practices
suered revenue losses between $150,000 and $1,000,000.
The reduction in the volume of patients seeking nonemergent care also left hospitals vulner-
able to steep revenue drops. According to the CMS tiered approach, emergent care is care that
is necessary to be provided on an in-person basis to avoid harm to the patient.
2
By contrast,
nonemergent care includes care that, if not provided, has the potential to increase patient
morbidity and mortality.
2
Management of existing medical and surgical conditions in cur-
rently stable patients are considered nonemergent, even if delay increases the risks of patient
harm in the future.
2,19,20
Nonemergent care encompasses elective surgeries, like hip and knee
replacements, which are a substantial component of hospital revenue.
19-22
Cancellation of
virtually all elective surgeries, along with large decreases in the patient volumes in specialty
138 PRIMARY CARE IN THE COVID-19 PANDEMIC
and primary care clinics, caused hospital revenues to halve in some cases and left hospitals
struggling for cash on hand.
21,23
A report by the American Hospital Association estimated that
hospital losses for cancellation of nonemergent care amounted to $161.4 billion for the four-
month period of March to June 2020 alone.
20
Additional costs of care during COVID-19
Preparing to care for COVID-19 patients and secure the safety of health care workers required
signicant increases in expenditures from primary care practices and hospitals. Primary care
practices and hospitals needed to acquire personal protective equipment and (in the latter
case) ventilators, enhance COVID-19 testing capacity, increase cleaning and disinfection, and
create or expand the availability of negative pressure rooms.
19-21
New operational processes
needed to be created to minimize the contact of patients with providers, sta, and other
patients during visits, each of which limited eciency and created additional costs. Therefore,
at the same time that practices had the lowest revenue in memory, they also had an inux in
direct costs related to treating patients during a pandemic.
Government response
Four stimulus laws impacting health care nancing were enacted during March and April
2020 in response to the COVID-19 pandemic.
1. The Coronavirus Preparedness and Response Supplemental Appropriations Act, enacted
on March 6, 2020, allocated $8.3 billion to federal agencies, including the Department
of Health and Human Services, toward vaccine development and public health.
2. The Families First Coronavirus Response Act was enacted on May 18, 2020, at a cost
of $104 billion and required Medicare and private health insurance plans to cover
COVID-19 testing.
3. The Coronavirus Aid, Relief, and Economic Security (CARES) Act was signed into law
by President Trump on March 27, 2020. The $2.2 trillion act was the most expensive
spending bill in American history. The Paycheck Protection Program (PPP) for small
businesses and the Coronavirus Economic Stabilization Act for midsize businesses
established by the CARES Act provided loans for ailing primary care practices, as did
the Economic Injury Disaster Loans (EIDL) and the Small Business Administration
Debt Relief Program.
4. The Paycheck Protection Program and Health Care Enhancement Act, which was
signed into law on April 24, 2020, replenished funding to the PPP, EIDL, and other
programs established by the CARES Act.
The CARES Act provided support for hospitals and health care providers and loans for small
businesses. By boosting Medicare payments, waiving cuts to laboratory and durable medi-
cal equipment reimbursement, and expanding eligibility for Medicare pilot programs, the
act increased Medicare payments for providers and practices. The act also paused Medicare
PRIMARY CARE IN THE COVID-19 PANDEMIC 139
“sequestration,” a 2% automatic spending cut, from May through December 2020, eectively
increasing payment for providers.
As part of the CARES Act, the Accelerated and Advance Payment Program (AAPP) authorized
CMS to provide advance payments to any Medicare provider meeting qualications includ-
ing previous Medicare billing. These payments allowed for a three-month advance equaling
the prior three-month billing estimate. Repayment was required to begin after 120 days and
nish within 210 days from payment.
24-26
Small businesses were further notied as of May
15 of potential loan forgiveness. Although almost $100 billion was distributed through AAPP,
only $16.7 million reached primary care providers (categorized as those in family practice or
general practice).
27
Smaller practices with fewer than 500 employees were potentially eligible for both the EIDL
and the PPP loan to cover dierent expenses. In the rst three months of the programs,
13% of overall PPP funds—almost $67.4 billion—owed into health care and social services.
More than 22,300 practices, almost 5% of all physician’s oces, received loans of at least
$150,000.
28
Primary care practices were also eligible for tax credits if gross earnings for March
through December 2020 were at least 50% less than those earned during the same quarter
during the prior year. Nonetheless, a survey of primary care providers conducted at the end of
May, by the Larry A. Green Center and the Primary Care Collaborative (the PCC Survey), found
that only 50% of primary care practices reported receiving a loan through the PPP or SBA pro-
grams, and almost a quarter of primary care practices received no support at all.
29
Through the public health and social services emergency fund, practices suering nancial
challenges were also eligible to receive grants totaling $30 billion based on prior Medicare
fee-for-service billing. The CARES Act Provider Relief Fund reimbursed eligible providers for
lost wages directly.
Consequences of nancial losses
Financial losses in the health care sector are better tracked among hospitals than among
primary care practices, but hospital data serve as a broad indicator for overall health care
provider nancial impact. Due to the increased costs connected with caring for COVID-19
patients, the declines in patient volume, and the loss of revenue, Moody’s Investors Service
downgraded its outlook on bonds issued by nonprot and public hospitals from stable to
negative in March 2020.
30,31
The nancial stressors on hospitals precipitated conditions of
ongoing nancial losses for many hospitals. The situation was summed up in a report com-
missioned by the AHA and released in July: before COVID-19, the typical hospital operating
margin was 3.5%; by the fourth quarter of 2020, half of American hospitals were projected to
have negative operating margins, ranging from −1% to −11%.
32
The nancial predicament in which hospitals nd themselves post-COVID-19 has led to doz-
ens of closures or bankruptcies of hospitals across the United States.
22,33,34
However, nancial
challenges facing primary care practices may be even more concerning than the challenges
facing hospitals, which are more sophisticated and have greater access to capital markets
and greater diversity in revenue streams than primary care practices. Yet due to fewer
140 PRIMARY CARE IN THE COVID-19 PANDEMIC

consolidated nancial projections or systematic tracking, the nancial losses and associated
closures and bankruptcies among primary care practices are less apparent than the nancial
conditions of hospitals in the United States, and a systematic accounting of practice closures
or bankruptcies is not yet available for primary care practices nationwide.
Provider consolidation
Provider consolidation has been occurring in US health care for decades, at the hospital level,
among health plans, and among small provider groups.
35
The economic reason for consoli-
dation is clear: market power brings negotiating leverage and negotiating leverage leads
to higher prices. Provider consolidation has occurred continuously across the spectrum of
providers over the last 20-30 years. To understand overall provider consolidation as it relates
to primary care, it is important to understand hospital consolidation as a major precedent to
other forms of provider consolidation.
Hospital consolidation
Hospital consolidation is well documented in the academic literature. According to data from
the AHA, there was an average of 78 hospital transactions per year every year between 1998
and 2015, for a total of 1,412 transactions.
36
Hospital markets are now concentrated with 90%
of metropolitan statistical areas (MSAs) considered concentrated based on the Federal Trade
Commission (FTC) standard that a highly consolidated market has a market concentration
index of 2,500 or higher.
37,38
For example, a market with only two provider groups, each with
50% market share, would be well above this threshold and be considered “highly concen-
trated” with a Herndahl-Hirschman Index (HHI)
of 5,000; meanwhile, a market with 10
providers, each with 10% market share, would have an HHI of 1,000 and have low market
concentration.
The Herndahl-Hirschman Index (HHI) is calculated by summing the squares of the individual rms’
market shares. For example, a market consisting of four rms with market shares of 30%, 30%, 20%,
and 20% has an HHI of 2,600 (30
2
+ 30
2
+ 20
2
+ 20
2
= 2,600). The HHI ranges from 10,000 (in the case
of a pure monopoly) to a number approaching zero (in the case of an atomistic market). Although it is
desirable to include all rms in the calculation, lack of information about rms with small shares is not
critical because such rms do not affect the HHI signicantly.
It is well documented that, while hospitals state that they aim to provide economies of scale
and improve quality, in reality, consolidation primarily increases negotiating leverage, which
results in increases in prices.
39
This consolidation has a real and tangible eect on hospital
pricing, and in-state hospital acquisitions yield a price increase of 7% to 9%.
40
While hos-
pitals may claim higher prices reect higher quality, there is evidence that consolidation in
the hospital sector has led to higher prices, but not to higher value.
39
Evidence of in-market
consolidation’s impact on prices is even clearer. Highly concentrated markets experiencing
mergers had price increases exceeding 20%.
41
There is little evidence of improved quality and
there is evidence that patient satisfaction declined.
42
PRIMARY CARE IN THE COVID-19 PANDEMIC 141
The general conclusions in the hospital sector are:
1. Hospitals are consolidating.
35
2. The consolidation has led to clear increases in prices with little evidence of improved
quality or patient satisfaction.
39,42,43
3. Antitrust enforcers face legal hurdles to reduce incremental acquisitions that result in
broader market consolidation.
39
Provider consolidation
Data describing trends in provider consolidation are growing in the academic literature, but
also in the trade literature, which can help provide insight when research is unavailable. The
high cost of practice management has led to hospital acquisition of practices in a movement
called vertical integration.
44
From 2010 to 2016, primary care market concentration increased
faster than market concentration in the specialties. The mean HHI increased by about 5% for
hospital providers and specialist physician organizations, while for primary care physicians,
the HHI increased by nearly 29%.
37
This means that primary care physician consolidation
occurred rapidly in the period just before the start of COVID-19, relative to consolidation
among specialists and hospitals. The share of physicians in groups less than 10 dropped 12%
between June 2013 and December 2015.
45
The number of physicians in vertically integrated
systems rose from 40% in 2016 to 51% in 2018.
46
This trend held for primary care physicians,
with 38% aliated with systems in 2016 increasing to 49% in 2018.
47
While system size grew
between 2016 and 2018, the greatest percentage change was realized by primary care physi-
cians, resulting in an 11 percentage point increase.
47
While provider consolidation increased in primary care, there may have been lower price
increases for primary care practices than for other specialties. From 2012 to 2016, primary
care reimbursement rates grew (as a percent of Medicare) 7% per year, while emergency room
provider and anesthesiology provider rates grew nearly 30% per year.
48
Private equity as a consolidation catalyst
In recent years, private-equity rms, which are nancial organizations that make invest-
ments in existing businesses in exchange for a share of ownership, have acquired primary
care practices frequently with the objective of increasing the value of the practice and selling
for a higher price. Most private-equity rms are not generally run by physicians, but many
have invested millions in medical practices. When these rms purchase medical practices,
they typically start with a multimillion-dollar acquisition of a large, popular practice, which
functions as an anchor attracting patients and doctors to the new group. Following this large
acquisition, private-equity rms often purchase smaller oces and solo practices to fold into
the larger practice brand, giving the group a regional presence.
49
As these private-equity-
owned practices grow and become major providers of outsourced services like anesthesia, they
can gain greater market power in their negotiations with hospitals and insurance companies.
Private equity has been less focused on primary care in the past, due to lower total revenue at
142 PRIMARY CARE IN THE COVID-19 PANDEMIC
primary care practices, but that could change as referrals become more important for other
private-equity-backed practices. When these private-equity-owned rms negotiate higher
insurance reimbursement rates, they can range anywhere from $25 to $125 more per visit
than among non-private-equity-owned primary care practices.
49
Primary care practice response to COVID-19
At the outset of the pandemic, primary care practices were among the most vulnerable to
nancial downturn. Approximately 56% of primary care practices are fully or partially owned
by their clinicians.
50
Primary care physician earnings are among the lowest in the profes-
sion.
50,51
Before COVID-19, primary care visits had been trending downward, resulting in lower
income over time, with a 25% drop in visits between 2008 and 2016.
52
Hence, primary care
practices had limited cash reserves before the pandemic.
51
The PCC Survey series, conducted weekly since March 2020, provided a detailed account of the
loss of patient volume and decline in patient revenue and its impact on this already vulnerable
sector. After the CMS recommendations to avoid in-person visits, 90% of primary care pro-
viders limited well and chronic care visits, and 19% stopped providing any routine care. As a
result, 50% of practices either lacked cash on hand to last four weeks or were unsure of their
cash reserves.
53
By mid-April, 85% reported such “dramatic decreases” in patient volume that
55% indicated that they either expected to close or were unsure if they could remain open.
54
Around 20% of practices closed temporarily.
55,56
For practices that remained solvent through May, 60% reported that less than half of their
work was reimbursable, with 57% reporting that payments received were insucient to cover
the cost of care delivered.
57
Practices stayed aoat by reducing payroll expenses: for weeks,
around 40% or more of practices consistently reported laying o or furloughing sta.
54,55,58
At the same time, costs were also increasing: unused vaccines owned by the practices ex-
pired and had to be destroyed, while PPE was unattainable except at exorbitant rates.
57,58
In
addition, they had to invest in creating new operating procedures to keep patients at a safe
distance from providers, sta, and each other, and consistently enforce these procedures.
In June, 25% of respondents had skipped or deferred their salaries.
39
By September, 34% of
respondents reported that clinicians in their practice had taken or were planning to take early
retirement or otherwise leave the practice.
59
Telehealth reimbursement
Telehealth provided some bulwark against this downward trajectory in patient volumes and
revenue for primary care and other providers. Beginning on March 6, CMS expanded eligibility
for telehealth services to be reimbursed at rates identical to in-person service on a temporary
and emergency basis.
60,61
The CARES Act expanded coverage and payment for telehealth, ex-
tending changes initiated in the March 6 law. Eective March 1, the act authorized Medicare
to pay providers for telehealth visits at the same rate as in-oce visits, regardless of visit
diagnosis. Providers were authorized to provide telehealth services from home and were
authorized to provide services to Medicare beneciaries in another state. Telehealth services
PRIMARY CARE IN THE COVID-19 PANDEMIC 143
could be provided to new and established patients, allowing new patients access to primary
care from their home. Remote patient monitoring and virtual check-ins were authorized for
reimbursement through Medicare. Audio-only phone visits were reimbursable, providing
access for patients who may lack smartphone technology. Telehealth access was expanded not
only for medical providers, but also for other health care professionals frequently employed
in primary care practices, including social workers, psychologists, and physical therapists.
The act expanded payment for telehealth to underserved patients by funding FQHCs and
rural health clinics to provide telehealth services. Traditionally face-to-face visits such as
for hospice recertication could be fullled through telehealth visits. The act mandated that
high-deductible health plans cover telehealth before the deductible was satised. In addi-
tion, the act allocated funding to grant programs to promote use of telehealth in training and
health care delivery. The act also provided for educational loan deferment and pension relief,
providing a potential income buer to providers and small practices.
Telehealth in primary care
Although many practices needed to enhance their technology capabilities to provide virtual
care,
62
by mid-May 85% of respondents to the PCC Survey reported providing a “signicant”
amount of telehealth care on both video- and audio-based platforms.
55
With fewer patients presenting for in-person primary care, new policies facilitating tele-
health, and larger practices incorporating platforms necessary to support technology, tele-
health visits increased dramatically by the initial peak in COVID-19 cases in April 2020. Before
the pandemic, approximately 13,000 Medicare recipients received telehealth visits weekly,
compared with 1.7 million beneciaries the last week of April, and 9 million beneciaries
throughout the spring of 2020.
63
Telemedicine facilitated distanced medical care and improved
safety for both patients and providers when an in-person visit was not necessary. Telehealth
was used for triage and management of COVID-19 cases, follow-up, and preventive health
care, as well as non-COVID-19-related chronic disease management.
64
Under an 1135 waiver, a number of additional visit types and locations were funded and reim-
bursable by Medicare, including virtual check-ins and e-visits. The US Department of Health
and Human Services also provided for reduced or waived cost sharing for telehealth visits for
patients covered by Medicare, Medicaid, and the Children’s Health Insurance Program (CHIP).
Medicare ensured parity for telehealth services, which were reimbursed at the same payment
rate as in-person services. A wider range of providers, including physical and occupational
therapists and speech and language pathologists, were allowed to provide remote services.
Patient satisfaction with telehealth is high, which will encourage practices to continue oer-
ing this service.
65
Access issues in primary care during COVID-19
The value of telehealth in primary care has been limited by patient access to the Internet,
quality of care provided via telehealth, and continued reimbursement issues.
51
In May, 68% of
respondents to the PCC Survey reported that either they had received no payment for virtual
144 PRIMARY CARE IN THE COVID-19 PANDEMIC

health care they had provided or that their bills were denied.
55
By the end of June, 34% of
providers had reduced video- or audio-based care because of reimbursement challenges,
and
by August, 62% of respondents were providing a majority of care (between 60% and 70% or
more) via in-person visits.
66
At the same time, oces were struggling to coordinate which
payers were paying for which type of telehealth services under which circumstances because
of variation in payment policies (Figure 1).
The Commonwealth Fund reported in August that telemedicine visits had plateaued at about
7% of the baseline number of weekly visits.
4
But even this modest amount is likely to decline
if CMS’s reimbursement rules revert to prepandemic norms.
6,59
The promise of telehealth is
unlikely to be realized unless more private payers begin reimbursing for telemedicine delivery
of care and CMS makes temporary and emergency expansions permanent.
67,68
The cost of
telehealth is lower than the cost of an oce visit, because it does not require a physical space.
The services rendered may be less comprehensive, and there is less additional administrative
cost such as medical assistant support.
69
Although it is reasonable for Medicare and health
plans to provide a slightly lower rate of reimbursement, it is not reasonable to return to the
pre-COVID-19 world where these visits received zero reimbursement.
WWW.MILBANK.ORG
1
Source: Telehealth Data from Fair Health New US Cases of COVID-19 Compiled by Author from
https://ourworldindata.org from Oxford University.
0.2%
0.4%
7.5%
13.0%
8.7%
6.9%
6.0%
6.1%
-
200,000
400,000
600,000
800,000
1,0 00,000
1,2 00,000
1,4 00,000
1,6 00,000
1,8 00,000
2,0 00,000
0%
2%
4%
6%
8%
10%
12%
14%
Jan Feb March Apr il May June July August
New COVID-19 Cases
Percent of Visits via Telehealth
US Telehealth Visits and New COVID-19 Cases in 2020
Telehealth Visi t Vol ume New Cases
Figure 1. US Telehealth Visits and New COVID-19 Cases in 2020
PRIMARY CARE IN THE COVID-19 PANDEMIC 145
Closures and restructuring in primary care due to COVID-19
As state stay-at-home orders issued in March 2020 expired beginning late April and May
2020, and many practices conducted outreach, patient volumes increased, although the levels
were still inadequate to ensure nancial recovery for primary care practices. According to
the Commonwealth Fund, since mid-June, weekly visits, inclusive of telehealth and across
practice areas, have been about 10% below the prepandemic baseline.
4
As the fund’s analysis
focused on average outcomes, practices with weaker baseline nancials may still be having
trouble meeting expenses like payroll and rent.
Although some primary care practices have nancially recovered from the period without
in-person visits, a breakdown of primary care practice types shows the recovery has not been
universal. For example, according to the Commonwealth Fund, FQHCs are experiencing less
of a rebound in visits than other types of practices, with patient volumes around 20% below
baseline, while pediatric practices are still operating with patient volumes 26% below prepan-
demic levels.
4
Meanwhile, half of respondents to the PCC Survey in mid-June reported that
patient volumes for in-person visits remained below 50% of baseline.
58
A microsimulation model that used data showing a low point in patient volumes in late March
and early April, and which projected a plateau in patient volume rebound in mid-June (as
happened), estimated “that primary care practices will lose more than $65,000 per FTE [full-
time equivalent] . . . from fee-for-service payments without any attempts at mitigation, even
assuming that practices quickly pivot to providing telemedicine services.”
68
According to this
model, the net loss to primary care providers in 2020 was almost $15 billion.
68
As with hospitals, primary care practices under pressure are facing closure or sale. As early as
May 2020, the PCC Survey data revealed that 0.6% of primary care practices had permanently
closed.
55
By July 2020, the Physicians Foundation reported that 8% of respondents (22% being
primary care physicians) had closed their practices due to pandemic stressors, amounting to
about 3,500 primary care practices.
6
By August, respondents to the PCC Survey were reporting
that 14% of practices were either permanently closed, considering bankruptcy, or unsure if
they would be solvent in four weeks.
66
A survey of Massachusetts practices from May through
July reported that 47% of primary care practices indicated that practice closure was a possible
response to the pandemic; the gure rose to 60% among independent primary care practic-
es.
13
The majority of respondents projected the timing of their practice closure to be December
2020 or sometime in 2021.
13
A consortium of organizations, including the American Academy
of Family Physicians (AAFP), the American Academy of Pediatrics, and the American College
of Physicians, wrote to the secretary of Health and Human Services, Alex Azar, to raise aware-
ness that “one of the most serious consequences of the COVID-19 crisis is the rapid collapse
of the community-based primary care system in many parts of the country.”
70
An AAFP and Health Landscape study analyzing conditions in March and April predicted if
conditions remained, there would be attrition of 58,000 primary care doctors—around 26%
of the country’s primary care doctors—by the end of June.
56,71,72
This theoretical loss would
translate into 1,841 counties in the United States suering a shortage of primary care physi-
cians, dened as having less than one primary care physician per 3,500 population.
71,72
146 PRIMARY CARE IN THE COVID-19 PANDEMIC
At the time of this writing, the majority of primary care practices continue to be open, al-
though in a diminished capacity. According to the PCC Survey from the end of September,
55% of respondents had furloughed practice sta, and 28% of practices were operating with
permanently reduced sta sizes.
59
At the same time, primary care practices were depleted
of cash reserves, potentially having to pay back student or business loans, exhausted after
months of pandemic-related stress and uncertainty, and facing a backlog of patients who had
forgone preventive and chronic care, as well as potentially additional waves of COVID-19 and
upcoming u season in early 2021. In the consortium’s letter to Secretary Azar, the authors
warned that “35% [of frontline primary care providers] believe most independent primary
care practices will be eliminated after the rst wave of the pandemic.”
70
Value-based payment and COVID-19
With fewer in-person visits and elective procedures, momentum for transforming fee-for-
service payments to value-based payments has accelerated.
73
Health care organizations
participating in the Medicare Shared Savings Programs and accountable care organizations
(ACOs) with capitated models rewarding health care outcomes were more likely to have had in
place care coordination and population health programs to promote needed care and preven-
tive health screening even with fewer in-person visits during the rst wave of COVID-19.
74,75
States also have been shifting Medicaid Advantage plans away from fee-for-service contracts,
and some private payers have done the same.
76
At the same time, with fewer screenings and
in-person chronic disease management visits taking place, CMS acted to protect ACOs and
assuage fears of further negative nancial implications of pandemic-related declines in health
care utilization. CMS amended quality reporting requirements and reduced downside risk in
its contracts with providing organizations.
Oering mechanisms for struggling practices to enroll in ACOs with up-front capitated and
value-based payments is one way to nancially aid practices, by paying them on the basis of
the (risk-adjusted) number of patients they take care of (a at per member, per month fee),
and for the quality of those services (including health outcomes among patients), rather than
for how many visits they achieve. With projected health care spending in 2020 down by $75
billion, to $575 billion, revenue from capitated and value-based care programs represents an
important funding stream for health care, further rewarding those practices with population
health, quality improvement, and care coordination programs in place to continue to work
toward successful chronic disease management and meet benchmarks for preventive health
care indicators even as in-person visits decline.
77-79
Population health and chronic disease
management services are increasingly oered by nurse managers over telephone/video, or via
semi- or fully automated apps, to obtain labs, arrange preventive services, adjust medica-
tions, or enable electronic communications, including email to and from patients and provid-
ers, facilitating proactive outreach, follow-up, and adjustments to medications or therapeutic
approaches that did not depend on in-person visits.
PRIMARY CARE IN THE COVID-19 PANDEMIC 147
Conclusions
Market consolidation has been a feature of US health care for several decades. Although its
impact on primary care prices has been less than consolidation’s impact on hospitals and
specialty practices, the evidence consistently shows that consolidation and subsequent high
market concentration of hospitals and provider groups leads to higher prices.
33
There is little
evidence, however, that consolidation is associated with improved patient satisfaction or
quality outcomes.
37,40
In primary care, there has been a decrease in the number of independent practices over the
past several years, with 49% of primary care providers in 2018 aliated with a hospital
system, up from 38% in 2016.
45
Current data suggest that many primary care practices are closing; it is possible that more
providers will have to close their doors if they do not consolidate. The consolidation of solo
and very small primary care practices can oer nancial stability in case of illness or ab-
sence, and it can oer economies of scale in an increasingly complex regulatory and nancial
environment. Consolidation presents an opportunity to make investments in practices, raise
capital and streamline with electronic medical records, optimize operations such as appoint-
ment scheduling, and streamline coverage. However, the shift can also lead to anticompetitive
pricing behavior and price increases that are not tied to quality improvements. Moreover,
consolidation has the potential to lead to “primary care deserts,” with swathes of the popula-
tion lacking access because of geographic distance from primary care providers.
70,71
The broad nancial instability of primary care practices due to the COVID-19 pandemic was
largely driven by the preponderance of the fee-for-service payment model. A push from
Medicare through the Merit-Based Incentive Payment System, as well as many state pro-
grams, has only partially shifted from fee-for-service to value-based payments that focus
on capitation and quality-based payments. In theory, if 100% of primary care providers
were paid by capitation, there would have been little interruption in their cash ow during
COVID-19; providers would have received a monthly payment from health plans regardless of
patient volumes.
Overall, COVID-19 has shown:
• Despite primary care providers oering frontline support to tens of millions of Americans
at risk for COVID-19, reliance on a fee-for-service model has been associated with nan-
cial instability during the pandemic. A continued shift toward capitated and value-based
payments might stabilize the nances of primary care practices not aliated with hospi-
tal systems.
• Telehealth, when reimbursed, can be an ecient option for primary care providers to oer
to patients who do not need an in-person visit and have reliable Internet access, supple-
menting revenue for primary care practices and helping continuity of care.
• Providers have consolidated across health care in the past decades. Although consolidation
is associated with higher prices, these price increases are relatively less for primary care
148 PRIMARY CARE IN THE COVID-19 PANDEMIC
providers than for other specialties.
46
At the same time, larger practice size can lead to
economies of scale and nancial stability during a pandemic.
Therefore, we argue that policies to improve primary care access, eciency, and quality in
a post-COVID-19 world given provider consolidation would continue the shift to capitated
and value-based payments to reduce the need for consolidation; make permanent telehealth
payments for providers, retaining the exibility to create a fair reimbursement rate that takes
into consideration the lower xed costs of telehealth; and monitor and b
alance the natural
progression of primary care provider consolidation into larger, more nancially stable groups,
while avoiding overconsolidation that can decrease access by expanding geographic distance
from a primary care provider and extract anticompetitive prices from the populations they treat.
References
1. CMS releases recommendations on adult elective
surgeries, non-essential medical, surgical, and dental
procedures during COVID-19 response. US Centers
for Medicare and Medicaid Services. March 18, 2020.
Accessed October 4, 2020. https://www.cms.gov/
newsroom/press-releases/cms-releases-recommen-
dations-adult-elective-surgeries-non-essential-medi-
cal-surgical-and-dental.
2. Non-emergent, elective medical services, and treat-
ment recommendations. US Centers for Medicare
and Medicaid Services. April 7, 2020. Accessed Oc-
tober 4, 2020. https://www.cms.gov/les/document/
cms-non-emergent-elective-medical-recommenda-
tions.pdf.
3. State guidance on elective surgeries. Ambulatory Sur-
gery Center Association. Last updated April 20, 2020.
Accessed October 4, 2020. https://www.ascassocia-
tion.org/asca/resourcecenter/latestnewsresourcecen-
ter/covid-19/covid-19-state.
4. Mehrotra A, Chernew M, Linetsky D, Hatch H, Cutler
D, Schneider EC. The impact of the COVID-19
pandemic on outpatient visits: changing patterns of
care in the newest COVID-19 hot spots. Common-
wealth Fund. August 13, 2020. Accessed October 4,
2020. https://www.commonwealthfund.org/publica-
tions/2020/aug/impact-covid-19-pandemic-outpatient-
visits-changing-patterns-care-newest.
5. COVID-19 nancial impact on medical practices.
Medical Group Management Association. Ac-
cessed October 6, 2020. https://www.mgma.
com/getattachment/9b8be0c2-0744-41bf-864f-
04007d6adbd2/2004-G09621D-COVID-Financial-
Impact-One-Pager-8-5x11-MW-2.pdf.aspx?lang=en-
US&ext=.pdf.
6. 2020 survey of America’s physicians: COVID-19
impact edition. Physicians Foundation. August 2020.
Accessed October 4, 2020. https://physiciansfounda-
tion.org/wp-content/uploads/2020/08/20-1278-Merritt-
Hawkins-2020-Physicians-Foundation-Survey.6.pdf.
7. COVID-19 impact on Alabama medical practices.
Medical Association of the State of Alabama. 2020.
Accessed October 5, 2020. https://alabamamedicine.
org/wp-content/uploads/2020/08/2020-MASA-COV-
ID-Financial_Impact_Survey_Report.pdf.
8. COVID-19 physician nancial health survey. Califor-
nia Medical Association. Last updated April 22, 2020.
Accessed October 4, 2020. https://www.cmadocs.org/
Portals/CMA/les/public/CMA%20COVID-19%20Fi-
nancial%20Hardship%20Survey%20Summary.pdf.
9. Colorado primary care response: COVID-19 report
#7. State Network of Colorado Ambulatory Practices
and Partners. July 2020. Accessed October 5, 2020.
https://medschool.cuanschutz.edu/docs/librariespro-
vider32/snocap-covid-19/snocap-covid-survey-7-re-
sults-and-resources.pdf?sfvrsn=66e9d3b9_2.
PRIMARY CARE IN THE COVID-19 PANDEMIC 149
10. Colorado primary care response: COVID-19 report
#8. State Network of Colorado Ambulatory Practices
and Partners. August 2020. Accessed October 5,
2020. https://medschool.cuanschutz.edu/docs/librar-
iesprovider32/snocap-covid-19/snocap-covid-survey-
8-results-and-resources.pdf?sfvrsn=8c9a5b9_2.
11. COVID-19 business impact report key ndings.
Indiana State Medical Association. May 1, 2020. Ac-
cessed October 4, 2020. https://www.ismanet.org/pdf/
COVID-businessimpactFULLreport.pdf.
12. COVID-19 member survey. Kentucky Medical As-
sociation. April 28, 2020. Accessed October 4, 2020.
https://kyma.org/shared/content/uploads/2020/04/
KMA-Physician-Survey-Results-Summarized-for-
membership.pdf.
13. Song Z, Giuriato M, Lillehaugen T, et al. Economic
and clinical impact of COVID-19 on provider practices
in Massachusetts. NEJM Catalyst. September 11,
2020. Accessed October 4, 2020. https://catalyst.
nejm.org/doi/full/10.1056/CAT.20.0441.
14. Minnesota physicians respond to COVID-19. Minne-
sota Medical Association. August 22, 2020. Accessed
October 5, 2020. https://www.mnmed.org/getat-
tachment/advocacy/Practice-Good-Health/COVID-
19-Impact-Study/MMA_COVID-19_Survey_Find-
ings_8-22-20.pdf.aspx?lang=en-US.
15. MSSNY president submits testimony on the impact
of the COVID-19 crisis on NY physician practices.
Medical Society of the State of New York. May 13,
2020. Accessed October 4, 2020. http://www.mssny-
enews.org/press-releases/mssny-president-submits-
testimony-on-the-impact-of-the-covid19-crisis-on-ny-
physician-practices/.
16. Assessing the impact of COVID-19 on outpatient
care in Pennsylvania. Pennsylvania Medical So-
ciety. May 14, 2020. Accessed October 5, 2020.
https://www.pamedsoc.org/docs/librariesprovider2/
uploadedles/physician-survey_nal_5-14-20.
pdf?sfvrsn=db4e5b93_4.
17. Survey: Texas doctor practices struggling to survive
pandemic. Texas Medical Association. May 20, 2020.
Accessed October 4, 2020. https://www.texmed.org/
TexasMedicineDetail.aspx?id=53634.
18. Washington’s physician practices in nancial crisis:
a new WSMA survey. Washington State Medical As-
sociation. May 5, 2020. Accessed October 5, 2020.
https://wsma.org/Shared_Content/News/Press_Re-
lease/2020/washingtons_physician_practices_in_-
nancial_crisis_new_wsma_survey.
19. Carroll NW, Smith DG. Financial implications of the
COVID-19 epidemic for hospitals: a case study. J
Health Care Finance 2020;46(4):11-22.
20. Hospitals and health systems face unprecedented
nancial pressures due to COVID-19. American
Hospital Association. May 2020. Accessed October
5, 2020. https://www.aha.org/system/les/media/
le/2020/05/aha-covid19-nancial-impact-0520-FI-
NAL.pdf.
21. Grimm C. Hospital experiences responding to the
COVID-19 pandemic: results of a national pulse sur-
vey March 23-27, 2020. Washington, DC: U.S. De-
partment of Health and Human Services Ofce of the
Inspector General, 2020. Accessed October 5, 2020.
https://oig.hhs.gov/oei/reports/oei-06-20-00300.pdf.
22. Block A, Van Dyke K, Dillard L. Prots of publicly
traded health plans surge amid requests for higher
rates. Managed Healthcare Executive. August 6,
2020. Accessed October 5, 2020. https://www.
managedhealthcareexecutive.com/view/prots-of-
publicly-traded-health-plans-surge-amid-requests-for-
higher-rate.
23. Block A, Van Dyke K, Dillard L. The COVID-19
pandemic: for-prot health plans win, hospitals lose.
Healthcare Business Today. May 27, 2020. Accessed
October 5, 2020. https://www.healthcarebusiness-
today.com/the-covid-19-pandemic-for-prot-health-
plans-win-hospitals-lose/.
24. CARES Act: AMA COVID-19 pandemic telehealth fact
sheet. American Medical Association. Last updated
April 27, 2020. Accessed October 12, 2020. https://
www.ama-assn.org/delivering-care/public-health/
cares-act-ama-covid-19-pandemic-telehealth-fact-
sheet.
25. CARES Act: Medicare advance payments for CO-
VID-19 emergency. American Medical Association.
Last updated April 6, 2020. Accessed October 12,
2020. https://www.ama-assn.org/delivering-care/
public-health/cares-act-medicare-advance-payments-
covid-19-emergency.
26. CARES Act/COVID 3.5: Loans & other nancial as-
sistance for physician practices. American Medical
Association. Last updated June 16, 2020. Accessed
October 12, 2020. https://www.ama-assn.org/deliver-
ing-care/public-health/cares-actcovid-35-loans-other-
nancial-assistance-physician.
27. Medicare accelerated and advance payments:
state-by-state and by provider type. US Centers for
Medicare and Medicaid Services. May 8, 2020. Ac-
cessed October 13, 2020. https://www.cms.gov/les/
document/covid-accelerated-and-advance-payments-
state.pdf.
150 PRIMARY CARE IN THE COVID-19 PANDEMIC
28. Pifer R. Here are doctors’ ofces, hospitals that got
COVID-19 paycheck protection loans over $150K.
Healthcare Dive. Last updated July 8, 2020. Ac-
cessed October 12, 2020. https://www.healthcare-
dive.com/news/here-are-doctors-ofces-hospitals-
that-got-covid-19-paycheck-protection/581094/.
29. Primary care & COVID-19: week 11 survey. Primary
Care Collaborative. May 27, 2020. Accessed October
13, 2020. https://www.pcpcc.org/2020/05/26/primary-
care-covid-19-week-11-survey.
30. Colenda CC, Applegate WB, Reier BV, Blazer DG
2nd. COVID-19: nancial stress test for academic
medical centers. Acad Med 2020;95(8):1143-5.
10.1097/ACM.0000000000003418.
31. Reed T. Moody’s, Fitch shift nancial outlook to
negative for nonprot hospitals. Fierce Healthcare.
March 20, 2020. Accessed October 5, 2020. https://
www.ercehealthcare.com/hospitals-health-systems/
healthcare-nancial-outlook-from-covid-19.
32. The effect of COVID-19 on hospital nancial health.
Kaufman, Hall & Associates, LLC. July 2020. Ac-
cessed October 5, 2020. https://www.aha.org/system/
les/media/le/2020/07/KH-COVID-Hospital-Finan-
cial-Health_FINAL.pdf.
33. Ellison A. 42 hospitals closed, led for bankruptcy
this year. Becker’s Hospital Review. June 22, 2020.
Accessed October 5, 2020. https://www.beckershos-
pitalreview.com/nance/42-hospitals-closed-led-for-
bankruptcy-this-year.html.
34. Ellison A. 15 hospitals have closed this year—here’s
why. Becker’s Hospital Review. May 15, 2020. Ac-
cessed October 5, 2020. https://www.beckershospit-
alreview.com/nance/15-hospitals-have-closed-this-
year-here-s-why-51521.html.
35. Gaynor M, Ho K, Town RJ. The industrial organization
of health-care markets. J Econ Lit 2015;53(2):235-84.
10.1257/jel.53.2.235.
36. Trendwatch chartbook 2016: trends affecting hospi-
tals and health systems. American Hospital Associa-
tion. 2016. Accessed October 7, 2020. https://www.
aha.org/system/les/2018-01/2016-chartbook.pdf.
37. Fulton BD. Health care market concentration trends
in the United States: evidence and policy responses.
Health Aff (Millwood) 2017;36(9):1530-8. 10.1377/
hlthaff.2017.0556.
38. Horizontal merger guidelines, 8/19/2010. Washington,
DC: US Department of Justice., 2010. Accessed Oc-
tober 12, 2020. https://www.justice.gov/atr/horizontal-
merger-guidelines-08192010#5c.
39. Testimony of Leemore S. Dafny, PhD before the
House Committee on Energy and Commerce
Subcommittee on Oversight and Investigations on
“Health Care Industry Consolidation: What is Hap-
pening, Why It Matters, and What Public Agencies
Might Want to Do About It.” February 14, 2018.
Accessed October 12, 2020. https://docs.house.gov/
meetings/IF/IF02/20180214/106855/HHRG-115-IF02-
Wstate-DafnyL-20180214.pdf.
40. Dafny LS, Ho K, Lee RS. The price effects of cross‐
market mergers: theory and evidence from the
hospital industry. RAND J Econ 2019;50(2):286-325.
10.1111/1756-2171.12270.
41. Gaynor M, Town R. The impact of hospital consoli-
dation. Robert Wood Johnson Foundation. June 1,
2012. Accessed October 12, 2020. https://www.rwjf.
org/en/library/research/2012/06/the-impact-of-hospi-
tal-consolidation.html.
42. Hanson C, Herring B, Trish E. Do health insurance
and hospital market concentration inuence hospi-
tal patients’ experience of care? Health Serv Res
2019;54(4):805-15. 10.1111/1475-6773.13168.
43. Beaulieu ND, Dafny LS, Landon BE, et al. Changes
in quality of care after hospital mergers and acqui-
sitions. N Engl J Med 2020;382(1):51-9. 10.1056/
NEJMsa1901383.
44. Singer LE. Considering the ACA’s impact on hospi-
tal and physician consolidation. J Law Med Ethics
2019;46(4), 913-7. 10.1177/1073110518821989.
45. Muhlestein DB, Smith NJ. Physician consolidation:
rapid movement from small to large group practices,
2013-2015. Health Aff (Millwood) 2016;35(9):1638-
42. 10.1377/hlthaff.2016.0130.
46. Schwartz K, Lopez E, Rae M, Neuman T. What we
know about provider consolidation. Kaiser Family
Foundation. September 2, 2020. Accessed October
12, 2020. https://www.kff.org/health-costs/issue-brief/
what-we-know-about-provider-consolidation/.
47. Furukawa MF, Kimmey L, Jones DJ, Machta RM,
Guo J, Rich EC. Consolidation of providers into
health systems increased substantially, 2016-18.
Health Aff (Millwood) 2020;39(8):1321-5. 10.1377/
hlthaff.2020.00017.
48. Xu T. Markups on emergency medicine and anesthe-
siology services in the United States from 2012 to
2016. JAMA Intern Med 2020;180(2):327-9. 10.1001/
jamainternmed.2019.5141.
49. Perlberg H. How private equity is ruining American
health care. Bloomberg Quint. Last updated May
26, 2020. Accessed October 12, 2020. https://www.
bloombergquint.com/businessweek/private-equity-is-
ruining-health-care-covid-is-making-it-worse.
PRIMARY CARE IN THE COVID-19 PANDEMIC 151
50. Petterson S, McNellis R, Klink K, Meyers D, Ba-
zemore A. The state of primary care in the United
States: a chartbook of facts and statistics. Robert
Graham Center. January 2018. Accessed October 7,
2020. https://www.graham-center.org/content/dam/
rgc/documents/publications-reports/reports/Primary-
CareChartbook.pdf.
51. Roehr B. COVID-19 is threatening the survival of US
primary care. BMJ 2020;369:m2333. 10.1136/bmj.
m2333.
52. Ganguli I, Shi Z, Orav EJ, Rao A, Ray KN, Mehrotra
A. Declining use of primary care among commercially
insured adults in the United States, 2008-2016. Ann
Intern Med 2020;172(4):240-7. 10.7326/M19-1834.
53. Primary care & COVID-19: week 3 survey. Primary
Care Collaborative. April 1, 2020. Accessed October
6, 2020. https://www.pcpcc.org/2020/04/01/primary-
care-covid-19-week-3-survey.
54. Primary care & COVID-19: week 5 survey. Primary
Care Collaborative. April 17, 2020. Accessed October
6, 2020. https://www.pcpcc.org/2020/04/16/primary-
care-covid-19-week-5-survey.
55. Primary care & COVID-19: week 9 survey. Primary
Care Collaborative. May 13, 2020. Accessed October
6, 2020. https://www.pcpcc.org/2020/05/13/primary-
care-covid-19-week-9-survey.
56. Primary care & COVID-19: week 14 survey. Pri-
mary Care Collaborative. June 18, 2020. Accessed
October 6, 2020. https://www.pcpcc.org/2020/06/18/
primary-care-covid-19-week-14-survey.
57. Pifer R. After 6 months of darkness, primary care
practices see little light ahead. Healthcare Dive. July
27, 2020. Accessed October 6, 2020. https://www.
healthcaredive.com/news/6-months-primary-care-
practices-covid/581170/.
58. Findlay S. Primary care doctors seek overhaul in how
they’re paid amid pandemic cuts and losses. Fortune.
August 12, 2020. Accessed October 7, 2020. https://
www.fortune.com/2020/08/12/doctors-fee-for-service-
payments-medicare-covid/.
59. Primary care & COVID-19: week 21 survey. Primary
Care Collaborative. October 1, 2020. Accessed
October 6, 2020. https://www.pcpcc.org/2020/10/01/
primary-care-covid-19-week-21-survey.
60. Medicare telemedicine health care provider fact
sheet. US Centers for Medicare and Medicaid Ser-
vices. March 17, 2020. Accessed October 6, 2020.
https://www.cms.gov/newsroom/fact-sheets/medi-
care-telemedicine-health-care-provider-fact-sheet.
61. Billing for professional telehealth distant site services
during the public health emergency—revised. US
Centers for Medicare and Medicaid Services. April 3,
2020. Accessed October 6, 2020. https://www.cms.
gov/outreach-and-educationoutreachffsprovpartprog-
provider-partnership-email-archive/2020-04-03-mlnc-
se.
62. Weiner, R. Small medical practices struggle to sur-
vive amid coronavirus pandemic. Washington Post.
May 14, 2020. Accessed October 6, 2020. https://
www.washingtonpost.com/health/small-doctor-
practices-struggle-to-survive-amid-coronavirus-
pandemic/2020/05/14/328984e6-9390-11ea-91d7-
cf4423d47683_story.html.
63. Verma S. Early impact of CMS expansion of Medicare
telehealth during COVID-19. Health Affairs Blog. July
15, 2020. Accessed October 6, 2020. https://www.
healthaffairs.org/do/10.1377/hblog20200715.454789/
abs/.
64. Monaghesh E, Hajizadeh A. The role of telehealth
during COVID-19 outbreak: a systematic review
based on current evidence. BMC Public Health
2020;20(1):1193. 10.1186/s12889-020-09301-4.
65. Telehealth: delivering care safely during COVID-19.
US Department of Health and Human Services. Last
updated July 15, 2020. Accessed October 6, 2020.
www.hhs.gov/coronavirus/telehealth.
66. Primary care & COVID-19: week 15 survey. Primary
Care Collaborative. July 1, 2020. Accessed October
6, 2020. https://www.pcpcc.org/2020/07/01/primary-
care-covid-19-week-15-survey.
67. LaPointe J. How COVID-19 imperiled physician prac-
tices, and how to save them. Recycle Intelligence.
May 6, 2020. Accessed October 6, 2020. https://rev-
cycleintelligence.com/features/how-covid-19-imper-
iled-physician-practices-and-how-to-save-them.
68. Basu S, Phillips RS, Phillips R, Peterson LE,
Landon BE. Primary care practice nances in
the United States amid the COVID-19 pandemic.
Health Aff (Millwood) 2020;39(9):1605-14. 10.1377/
hlthaff.2020.00794.
69. Alexander GC, Tajanlangit M, Heyward J, et al. Use
and content of primary care ofce-based vs. tele-
medicine care visits during the COVID-19 pandemic
in the US. JAMA Netw Open 2020;3(10):e2021476.
10.1001/jamanetworkopen.2020.21476.
152 PRIMARY CARE IN THE COVID-19 PANDEMIC
70. Joint letter to HHS on Medicaid relief during CO-
VID-19 pandemic. Alliance to Fight for Health Care,
American Academy of Family Physicians, American
Academy of Pediatrics, American Benets Council,
American College of Physicians, America’s Health
Insurance Plans, Blue Cross Blue Shield Association.
May 19, 2020. Accessed October 7, 2020. https://
www.aafp.org/dam/AAFP/documents/advocacy/pay-
ment/medicaid/LT-HHS-PrimaryCareFundingPriori-
ty-051920.pdf.
71. Norvell K, O’Donnell J. Caregivers on the sidelines.
USA Today. April 2, 2020. Accessed October 7, 2020.
https://www.pressreader.com/usa/usa-today-us-edi-
tion/20200402/281479278521251.
72. Carrozza M. Potential impact of family medicine
practice closures during COVID-19 pandemic. Health
Landscape. April 9, 2020. Accessed October 13,
2020. https://healthlandscape.org/potential-impact-
of-family-medicine-practice-closures-during-covid-
19-pandemic/.
73. Firth S. CMMI expanding direct contracting, advanc-
ing other new models. MedPage Today. September
23, 2020. Accessed October 13, 2020. https://www.
medpagetoday.com/practicemanagement/reimburse-
ment/88783.
74. Joint letter requesting COVID stimulus and support
for value-based care. American Academy of Family
Physicians, America’s Physician Groups, Health Care
Transformation Task Force, National Association of
ACOs, Premier, Inc. August 13, 2020. Accessed Oc-
tober 13, 2020. https://www.naacos.com/joint-letter-
requesting-covid-stimulus-support-value.
75. Premier, Inc. survey: clinically integrated networks
in alternative payment models expanded value-
based care capabilities to manage COVID-19 surge.
Premier. May 13, 2020. Accessed October 13, 2020.
https://www.premierinc.com/newsroom/press-releas-
es/premier-inc-survey-clinically-integrated-networks-
in-alternative-payment-models-expanded-value-
based-care-capabilities-to-manage-covid-19-surge.
76. Blue Cross NC launches comprehensive program to
help independent primary care practices stay in busi-
ness. Blue Cross Blue Shield of North Carolina. June
24, 2020. Accessed November 4, 2020. https://www.
bcbs.com/press-releases/blue-cross-nc-launches-
comprehensive-program-help-independent-primary-
care-practices.
77. Bendix J. What will COVID-19 mean for value-based
models? Medical Economics. August 7, 2020. Ac-
cessed October 12, 2020. https://www.medicaleco-
nomics.com/view/what-will-covid-19-mean-for-value-
based-models.
78. Gavidia M. How can the COVID-19 pandemic
enhance value-based health care delivery? Am J
Managed Care. August 12, 2020. Accessed October
12, 2020. https://www.ajmc.com/view/how-can-the-
covid-19-pandemic-enhance-value-based-health-
care-delivery.
79. Shah S, Kocher B. How to ensure COVID-19 doesn’t
delay value-based care. Health Affairs Blog. August
11, 2020. Accessed October 12, 2020. https://www.
healthaffairs.org/do/10.1377/hblog20200807.395079/
full/.
PRIMARY CARE IN THE COVID-19 PANDEMIC 153
Public Health Centers
in Japan’s COVID-19
Response and Recovery
June-Ho Kim, Kaeng Takahashi, Masafumi
Funato, Kay Negishi, Dan Schwarz, Masaya
Higuchi, Kei Ouichi, and Asaf Bitton
J
apan’s public health centers have played a critical, if understated, role in the country’s response
to and recovery from the COVID-19 pandemic. Japan experienced several swells of COVID-19
throughout 2020 and after the country’s early exposure to the disease through the notorious
Diamond Princess cruise ship outbreak.
1
Yet Japan notably maintained a low mortality rate, despite
its population being older than all other Organisation for Economic Co-operation and Development
(OECD) countries, and age being a major known risk factor for COVID-19 morbidity and mortal-
ity.
2,3
While the United States directed its response through the national Centers for Disease Control
and Prevention (CDC), Japan focused its response through regionalized public health centers that
acted as “miniature CDCs” within their respective communities. Japan’s experience demonstrated
the potential advantages and disadvantages of carrying out critical functions of infectious disease
response, and simultaneously promoting population health more broadly, through regional public
health centers. As such, Japan’s experience highlights key features and improvements that should
be carried forward in countries seeking to promote localized population health management during
a pandemic.
Public health centers, primary health care, and population
health in Japan
Japan’s health system is well known for achieving positive health outcomes, including the highest
life expectancy and lowest rate of obesity amongst OECD countries.
4
Japan nevertheless experienced
a rising burden of chronic disease, which prompted its adoption of a primary prevention strategy
called Healthy Japan 21 (HJ21)—a national health campaign to promote healthy lifestyles through
diet and exercise, reduced smoking and alcohol consumption, and improved mental health and
reduced stress.
5
In addition, Japan continued its extensive secondary prevention program
incorporating health checkups and screenings, supported by a universal health insurance
system with a uniform fee schedule but also no requirement of a primary care gatekeeping
function in order to access specialists.
Japan, unlike many OECD countries, does not have a robust cadre of primary care
physicians,as the vast majority of physicians are specialists and primary care can be deliv-
ered by specialists with limited training in primary care. In Japan, primary care is delivered
most commonly at community clinics, but these are often bypassed because Japanese citizens
and resident noncitizens who are enrolled in Japan’s statutory health insurance system can
freely access various areas of the health care system.
6
Amidst this fragmented structure, the
Japanese public health centers play a critical role in population health.
Japan’s public health centers, or hokenjo, have been part of Japan’s health care system since
the 1937 Public Health Center Act.
7,8
The centers were tasked with administrative roles in
food sanitation, environmental health, and medical and pharmaceutical aairs—including
infection control, nutrition, maternal and child health, health crisis management, support
to investigate and treat rare diseases, early detection of domestic violence, and oversee-
ing hospitals and pharmacies (Figure 1). The public health centers are directed by a certied
physician who oversees the three major divisions: the General Aairs Division, which col-
lects vital statistical data and audits medical facilities; the Life Environment Division, which
monitors food safety and sanitation of public spaces and audits pharmaceutical facilities; and
the Health and Prevention Division, which focuses on infectious disease control, nutritional
improvement, elder care, and primary care.
The public health centers are governed by the national Ministry of Health, Labor, and Welfare
(MHLW), operated as local governmental entities across Japan’s prefectures, directed by a
physician, and staed by a team of interdisciplinary professionals that includes public health
nurses, midwives, veterinarians, pharmacists, and clinical laboratory technicians. The centers
numbered 826 as of 1966 (with 1,173 physicians), but due to the 1994 Community Health Act
that unied and consolidated them, they numbered 469 as of 2020 (with 840 physicians as
of 2008).
9,10
Each center serves anywhere from 300,000 to over a million regional residents to
provide a wide range of public health services.
Prior to the COVID-19 pandemic, Japan’s public health centers played a major role in the
management of tuberculosis. Tuberculosis was the leading cause of death in Japan in 1950,
and the incidence of tuberculosis remained high over the past half century compared to other
developed countries. Tuberculosis was classied as a type 2 disease under the Infectious
Disease Act, which identied ve types of infectious diseases based on their severity, infectiv-
ity, and transmission route.
11
Type 1 infectious diseases were considered the most serious and
include Ebola hemorrhagic fever. Patients infected with either type 1 or type 2 diseases were
required to be admitted to an isolation ward, regardless of the severity of their illness. Though
several diseases were classied as type 1 or 2 during the 21st century—such as Severe Acute
Respiratory Syndrome (SARS), Middle East Respiratory Syndrome (MERS), H5N1, and H7N9
viruses—tuberculosis was the only one that was endemic to Japan.
156 PRIMARY CARE IN THE COVID-19 PANDEMIC

PHC
Public health center
Triage and
monitoring
Cluster
surveillance
PCR testing
+
+
Community health statistics
collection and dissemination
Auditing and licensing of
medical, pharmaceutical,
and public facilities
Assurance of food safety
and environmental
sanitation of public spaces
Management of preventive
care for maternal, child, elderly,
dental, and psychiatric health
Dedicated COVID-19 clinics
(undisclosed to public)
Hospitals
Patients Health care workers
Infectious disease
management
Expanded roles in the context of COVID-19
+
M
tf ti
t
t
f
t
f
He
He
al
al
th
th
c
c
ar
ar
e
e
w
wo
rk
e
Figure 1. Organization and Functions of Public Health Centers in Japan
For tuberculosis patients, Japan’s Infectious Disease Act mandates that infected patients be
isolated and receive inpatient treatments, covered by public subsidies, until cleared as no
longer infectious. Additionally, close contacts of patients with tuberculosis are given health
checkups to prevent spread of the disease. In Japan, when there are concerns about a tubercu-
losis outbreak, clinicians notify the local public health center where public health nurses visit
patients to assess them and trace their contacts. In addition, the public health nurses provide
guidance on medical treatment as well as nancial coverage from the government. Public health
centers are also involved in the process of tuberculosis testing and hospital isolation. These
tuberculosis-oriented activities became immediately relevant to Japan’s response to COVID-19.
The core roles of public health centers in Japan range from environmental and food safety to preventive
care. During the COVID-19 pandemic, the public health centers’ role in infectious disease management
expanded into triage, testing, and tracing clusters of infection.
Illustration by Ryoko Hamaguchi (Harvard Medical School).
PRIMARY CARE IN THE COVID-19 PANDEMIC 157
Japan’s response to the COVID-19 pandemic through public
health centers
Since the initial identication of COVID-19 in Wuhan, China, and Japan’s involvement in con-
taining the outbreak of the disease aboard the Diamond Princess cruise ship, Japan’s public
health centers served a central role in the country’s overall pandemic response. The public
health centers specically managed three critical responsibilities: patient triage, COVID-19
testing, and regional cluster surveillance (Figure 1).
Japan’s public health centers established telephone-based triage. If a patient felt unwell or
suspected exposure to COVID-19, their initial point of contact was not a walk-in visit to a
primary care oce or emergency department, but rather a call to a local call center, which
was either housed within or in close communication with a public health center.
12
Under
the direction of the MHLW in early February 2020, public health centers in each prefecture
established regional call centers (formally named Returnee and Contact Call Centers), which
were publicly available phone lines that connected callers to a triage desk primarily operated
by public health center sta. Citizens were initially advised to contact these call centers if
they met certain criteria, such as prolonged fever (37.5 degrees Celsius or more for four days
or longer), fatigue, and respiratory symptoms, or if they had risk factors such as advanced
age and comorbidities (e.g., diabetes, heart failure, respiratory illness, immunocompromised
status), averting overload at emergency departments and clinics.
Following this contact-free initial triage, the public health center directed a subset of pa-
tients to undisclosed COVID-19-dedicated outpatient clinics established within select regional
hospitals, for further in-person assessment by a medical provider. From February 1 to March
31, 2020, the triage system recorded a total of 313,475 phone-based consultations and 16,730
visits to COVID-19 clinics across the nation.
13
Once patients were assessed and conrmed
to be COVID-19 positive, the public health center facilitated transfer to specied hospitals
equipped with the resources, personnel, and experience to manage inpatient-level infectious
disease and respiratory distress. In response to the shortage of resources in some regions,
some public health centers took additional roles beyond their ocial core functions, including
but not limited to providing physical patient transportation to clinic sites and doubling as an
occupational health equivalent for hospitals managing infections among health care workers.
Finally, the public health center was also tasked with the larger epidemiological role of imple-
menting Japan’s “cluster-based approach,” which placed focus on proactive contact tracing
and isolation of possible contacts from small regional clusters that were hypothesized to be
driving community-based transmission in Japan. The experience centers had with contact
tracing of tuberculosis cases was thereby applied to the COVID-19 outbreak, with the public
health center a common node of external triage for all regional civilians; a liaison and consul-
tant for regional hospitals; and the workhorse in cluster surveillance and contact tracing for
entire geographical regions.
Japan’s public health center approach to contact tracing diered from some of its peers
through its lower reliance on technology and its emphasis on maintaining privacy of the
patients as well as businesses or regions aected by clusters of COVID-19 infection. Hence,
158 PRIMARY CARE IN THE COVID-19 PANDEMIC
while emphasizing the critical role of contact tracing spearheaded by several other countries,
Japan’s response was fundamentally dierent from eorts in peer countries such as Germany
and South Korea. Japan’s focus on privacy was thought to build trust with the public and
ensure people would be forthcoming about their symptoms and contacts.
During the rst small wave of infections in Japan, public health centers focused on testing
most persons without involvement of the traditional health care system. At the end of March
2020, a new wave of cases created bottlenecks for testing, leaving possible asymptomatic
COVID-19 cases untested and in their communities.
14
Hospitals designated for COVID-19
reached capacity, as COVID-19-positive patients with mild disease lled beds for multiple
weeks during mandatory hospitalizations, while more severe cases of the illness crowded am-
bulance bays. As COVID-19 hospitals began to turn away non-COVID-19 patients to preserve
beds, and conversely, non-COVID-19 hospitals shut doors on any patient at risk of having
COVID-19, a severely unbalanced and wasteful ecosystem emerged; in a single catchment
area, one hospital could face critical bed shortages while a neighboring hospital had empty
wards. Once COVID-19 patients began overowing into nondesignated hospitals, the latter
hospitals were unprepared to meet the infection control needs of this pandemic, lacking the
resources, space, and systems that had been previously allocated to designated hospitals to
protect both patients and health care workers from the spread of COVID-19.
A national state of emergency was declared in Japan in mid-April 2020, which resulted in
restructuring and fortication of the strained hospital system. Through the strong joint
advocacy of the public health centers and local governmental bodies, the initially narrow
triage pathway—built between the public health centers and an exclusive group of special-
ized hospitals—was restructured into a more expansive network of downstream care sites.
Public health centers began to systematically allocate patients to a wider network of hospitals,
including privately owned facilities, matching patients to appropriate designated or non-
designated hospitals by symptom severity and resource availability, while urging mild and
asymptomatic cases to stay home or in converted hotels without a mandatory hospitaliza-
tion.
15,16
The role of the public health centers was also modied by sharing its gatekeeping role
of COVID-19 testing with commercial testing facilities after the latter were included in the
national health insurance coverage. Diagnostics were expedited by relaxing testing criteria
to include those with mild symptoms, so that they could be triaged faster if they clinically
worsened.
Japan subsequently experienced a gradual plateau in cases and an unexpectedly low death
rate. Over the summer of 2020, cases, testing rates, and test positivity initially spiked, then
decreased into the autumn before a winter surge. Japan’s daily number of COVID-19 deaths
never exceeded 50 deaths per day in 2020, in a country with a third of the population of the
United States where daily deaths exceeded 3,000. While Japan’s ability to control the outbreak
was likely multifactorial, it appeared that Japan’s system of regionalized public health—pre-
pared from years of tuberculosis management and contact tracing, and bolstered by the rapid
adjustments made during a surge of COVID-19 cases—played a role in minimizing the dam-
age from the pandemic. Thus, Japan’s model, evolving rapidly in parallel with the virus’s
trajectory, oered key lessons about the strengths and potential pitfalls of deploying similar
systems amidst a public health crisis.
PRIMARY CARE IN THE COVID-19 PANDEMIC 159
Evolving the role of public health centers in the wake of
COVID-19
In Japan, the public health center was the critical resource for achieving a local triage system
that organized the ow of patients from the community to the most well-equipped hospi-
tals, many of them with a wealth of experience with infectious disease and respiratory care
through their management of patients with active tuberculosis and other communicable
illnesses. The public health centers, with a much smaller radius of surveillance than national
public health agencies such as the US CDC, were the key to Japan’s approach in quelling the
early phase of the virus by nipping local clusters of infections in the bud. Once the increasing
caseload exposed the ineciencies of this system, the regionalized public health centers—in
coalition with their local hospitals—were the rst to identify these pain points and rapidly
restructure a deeply ingrained playbook, including allocating patients across a wider network
of hospitals to boost health care capacity, as well as creatively repurposing nonhospital facili-
ties to free up beds for more severe cases. With their deep understanding of its local commu-
nity as well as its aliated hospitals and their respective capacities and needs, public health
centers were able to mobilize change in a much more nimble and customized fashion than a
large, centralized public health entity could. Japan’s regionalized model may be a powerful
advantage in future infectious disease outbreaks, in which epidemiological trajectories de-
mand rapid, coordinated, and locally responsive pivots in approach.
Despite its positive contributions in Japan’s COVID-19 response, the nation’s regionalized
public health framework still had many cracks in its system—ineciencies that, if not ad-
dressed, may hamstring its response in future public health crises.
First, early in the pandemic, when short-staed public health centers were tasked to serve as
the initial gatekeepers to COVID-19 care by fullling multiple roles on top of their standard
duties, they became a rate-limiting step to scaling up the response as the situation wors-
ened. In Japan’s case, with the onset of COVID-19, public health centers were quickly charged
with numerous roles that both leveraged existing capabilities (such as cluster surveillance)
and created new capacities (such as patient triage). As COVID-19 case numbers climbed,
Japan’s public health centers were spread too thin to maintain an adequate level of response.
Executing a sustainable regional public health network amidst a pandemic required early re-
distribution of workload to a wider network of facilities, such as delegating testing to private
testing centers and hospitals.
Second, despite the public health centers’ leadership in coordinating the local health care
response, communication and general sharing of data within and between these systems were
slow. In Japan, handwritten faxes and paper charts remained the norm, severely delaying
and complicating sharing of medical and epidemiological data among stakeholders within
and between dierent prefectures.
17,18
Initiatives for data digitization, data transparency, and
streamlined electronic communication were needed to bolster the public health centers’ abil-
ity to coordinate various hospitals and clinics into united action.
Third, the ability of regional public health centers to act was dependent on the network of
hospitals, which began the pandemic with an inadequate distribution of resources. The lack
160 PRIMARY CARE IN THE COVID-19 PANDEMIC
of infectious control expertise and material resources such as negative pressure rooms within
many nondesignated hospitals caused them to hesitate to accept COVID-19 patients when
public health centers attempted to recruit them into COVID-19 care. COVID-19-designated
hospitals, on the other hand, faced frustrating situations where they possessed the beds and
machines for intensive care, but did not have access to intensivists who worked at nondes-
ignated sites. Such lopsided resource allocations were not only ineective but also wasteful,
within a regionalized system that relied on a limited number of hospitals to absorb a large
number of infections. This gap may be bridged with expedited sharing of protocols for infec-
tion control and health care worker protection, as well as creative sharing of human resources
through modalities such as tele-consultations.
Finally, building a regionalized public health system takes a village, and Japan lacked adequate
national support to keep its system sustainable and eective with insucient government
investment into the public health centers and the public health sector in general. With Master
in Public Health programs in existence only for the past two decades, and only ve institutions
accredited as professional graduate schools, public health remained relatively undervalued in
Japan as an academic discipline—a stark contrast to the critical importance of public health as
an integral pillar of the nation’s health care system.
19
When the pandemic hit Japan, the public
health centers were called on to dramatically expand their already wide-ranging purview in the
background of dwindling numbers of public health centers in the country, without concomitant
increases in sta to serve larger areas. Public health center employees were severely overbur-
dened by the vast responsibilities in a time of great uncertainty, stretching the public health
centers dangerously thin. Any future implementation of a similar regionalized public health
model demands proportional support by the government through investment in public health
education and expansion of human resources to match the regional need.
Conclusions
Public health centers embody many of the core principles of high-quality primary health
care that have been critical during the health crisis. Japan’s public health centers provide
community-based care that promotes the values of rst-contact accessibility and person-
centeredness. Given its many functions, the public health center promotes comprehensiveness
and coordination. Finally, the Japanese public health center provides continuity for its local
population, particularly during the pandemic through its team-based care model.
Japan’s unique regionalized public health model has been the key to the country’s COVID-19
response, while also maintaining their many functions to keep communities healthy and
protect the well-being of their local communities. Relatively compact and deeply integrated
into the local community and hospital network, this system appeared to have been one of the
drivers of Japan’s success in weathering the COVID-19 crisis. As such, Japan provides an ex-
ample for countries looking to employ locally responsive public health centers to lead regional
coordination, surveillance, and triage during a pandemic. As Japan enters a “new normal”
amidst the ongoing pandemic, it will inevitably need to grapple with the aforementioned
challenges to maintain the ecacy of its public health infrastructure.
PRIMARY CARE IN THE COVID-19 PANDEMIC 161
Acknowledgments
Thank you to Ryoko Hamaguchi for contribut-
ing to the research, illustration, interviews, and
literature review in preparing this chapter.
References
1. Rocklöv J, Sjödin H, Wilder-Smith A. COVID-19 out-
break on the Diamond Princess cruise ship: estimat-
ing the epidemic potential and effectiveness of public
health countermeasures. J Travel Med 2020;27(3).
10.1093/jtm/taaa030.
2. Kang SJ, Jung SI. Age-related morbidity and mortal-
ity among patients with COVID-19. Infect Chemother
2020;52(2):154-64. 10.3947/ic.2020.52.2.154.
3. Working better with age: Japan. Organisation for
Economic Cooperation and Development. Last up-
dated December 11, 2018. Accessed May 20, 2020.
10.1787/9789264201996-en.
4. OECD reviews of public health: Japan. Organiza-
tion for Economic Cooperation and Development.
February 6, 2019. Accessed January 15, 2021.
10.1787/9789264311602-en.
5. Sakurai H. Healthy Japan 21. Journal of the Japan
Medical Association 2003;46(2):47-9. https://www.
med.or.jp/english/pdf/2003_02/047_049.pdf.
6. Tikkanen R, Osborn R, Mossialos E, Djordjevic A,
Wharton GA. Japan. Commonwealth Fund. June 5,
2020. Accessed January 15, 2021. https://www.com-
monwealthfund.org/international-health-policy-center/
countries/japan.
7. Hamaguchi R, Negishi K, Higuchi M, Funato M, Kim
JH, Bitton A. A regionalized public health model
to combat COVID-19: lessons from Japan. Health
Affairs Blog. July 22, 2020. Accessed October 13,
2020. https://www.healthaffairs.org/do/10.1377/
hblog20200721.404992/full/.
8. Katsuda N, Hinohara Y, Tomita K, Hamajima N. Struc-
ture and roles of public health centers (hokenjo) in
Japan. Nagoya J Med Sci 2011;73(1-2):59-68.
9. Trend in the number of public health centers, 1996-
2020. Japanese Association of Public Health Center
Directors. Accessed May 20, 2020. http://www.phcd.
jp/03/HCsuii/pdf/suii_temp02.pdf.
10. Imamura T, Saito T, Oshitani H. Roles of public health
centers and cluster-based approach for COVID-19
response in Japan. Health Secur 2020 [Online ahead
of print] 10.1089/hs.2020.0159.
11. Act on the prevention of infectious diseases
and medical care for patients with infectious
diseases. Japanese Law Translation. Trans-
lated July 13, 2016. Accessed May 18, 2020.
http://www.japaneselawtranslation.go.jp/law/
detail/?vm=04&re=01&id=2830.
12. About the health care system for a novel coronavi-
rus infection. Japan Ministry of Health, Labour and
Welfare. Accessed May 20, 2020. https://www.mhlw.
go.jp/content/10900000/000591991.pdf.
13. Total consultations of returnee and contact call center.
Japan Ministry of Health, Labour and Welfare. Ac-
cessed May 20, 2020. http://www.mhlw.go.jp/con-
tent/10906000/000619807.pdf.
14. Park J, Nakagawa I, Yamamitsu E. Running out
of beds and gear, Tokyo medical staff say Japan’s
“state of emergency” already here. Reuters. April 6,
2020. Accessed May 19, 2020. https://www.reuters.
com/article/us-health-coronavirus-japan-hospitals-in/
running-out-of-beds-and-gear-tokyo-medical-staff-
say-japans-state-of-emergency-already-here-idUSK-
BN21O0K4.
15. About medical follow-up and infection control for
patients with a novel coronavirus treating at home.
Japan Ministry of Health, Labour and Welfare. Ac-
cessed May 20, 2020. http://www.mhlw.go.jp/con-
tent/000618528.pdf.
16. About securing beds for a novel coronavirus patients.
Japan Ministry of Health, Labour and Welfare. Ac-
cessed May 28, 2020. http://www.mhlw.go.jp/con-
tent/000609963.pdf.
17. Dooley B, Inoue M. Japan needs to telework. Its
paper-pushing ofces make that hard. New York
Times. Last updated April 16, 2020. Accessed May
19, 2020. https://www.nytimes.com/2020/04/14/busi-
ness/japan-coronavirus-telework.html.
18. Doi S. Data entry for new infections a pain for medical
institutions. Asahi Shimbun. September 29, 2020. Ac-
cessed October 13, 2020. http://www.asahi.com/ajw/
articles/13770892.
19. List of graduate professional schools. Japan Ministry
of Education, Culture, Sports, Science and Technol-
ogy. Accessed May 20, 2020. https://www.mext.
go.jp/a_menu/koutou/senmonshoku/__icsFiles/aeld-
le/2019/08/06/1418138_2.pdf.
162 PRIMARY CARE IN THE COVID-19 PANDEMIC
Community Health
Workers in the
COVID-19 Response
and Continuation of
Primary Health Care
Ami Waters,
*
Jordan Downey,
*
Marion Subah,
E. John Ly, Lisa R. Hirschhorn, and Raj Panjabi
*
co-lead authors
C
ommunity health workers (CHWs) are increasingly recognized as a critical component of
a strong primary health care system. Forming part of the health team with nurses, physi-
cians, and public health ocers, CHWs are hired from their own communities and have been
a “human connection” for some of the most vulnerable.
1,2
CHWs extend the reach of primary
health care systems to communities otherwise underserved or unserved by formal health
systems. CHWs accomplish this by delivering primary care services in homes, community in-
stitutions, or peripheral health posts.
3
They provide a range of services that vary from health
education and promotion to curative patient care depending on the country’s epidemiological
priorities, health system structure, and political context.
4
The role of CHWs in primary care practice
CHW scope of practice in primary care varies by country. CHWs across geographies receive
training, varying in duration from weeks to months, in carrying out basic health care and
social tasks. In high-income countries, CHWs often provide support and education to patients
living with chronic illnesses, help screen for noncommunicable diseases (NCDs), and con-
nect patients to social and nancial support services.
5,6
In low- and middle-income countries
(LMICs), in addition to health education and health promotion, CHWs often provide diagnostic
and curative services for common infectious diseases (e.g., treating uncomplicated malaria);
reproductive health (e.g., delivering contraceptives), and linkage to maternal, neonatal, and
child health (MNCH) care (e.g., tracking the health of expectant mothers); mental health
and psychosocial support (e.g., screening for major depressive disorder); support for chronic
illnesses, including HIV, tuberculosis, and NCDs (e.g., supporting treatment adherence and
reducing loss-to-follow-up); and referrals to encourage appropriate utilization of health
services (e.g., immunizations).
7,8
They also address the social determinants of health, such as
ensuring patients have access to social services (e.g., employment, transportation, insurance).
Community-based primary health care provision, including through CHWs, has been shown
to have substantial impact on treatment seeking as well as maternal, neonatal, and child
health around the world.
4
A review of community-based interventions in Asia and Africa, in-
cluding those delivered by CHWs, showed that these interventions led to a signicant increase
in care-seeking behaviors for childhood pneumonia and diarrhea, as well as 32% reduction in
pneumonia mortality.
9
In Liberia, the National Community Health Assistant program was able
to signicantly increase access to treatment for children with malaria and other infectious
diseases in remote rural counties.
10
A comprehensive review by Henry Perry and colleagues
showed that provision of care in the community, especially care focused on antenatal, mater-
nity, and preventive care, decreases maternal morbidity and mortality.
11
Additionally, provi-
sion of neonatal care including breastfeeding and nutrition interventions, immunizations,
and infectious disease prevention and treatment can improve nutritional status and reduce
neonatal morbidity and mortality.
12
Community-based workers like CHWs can reduce not only
morbidity but also mortality from major causes of childhood illness in low-resource settings,
including malaria, diarrhea, pneumonia, vaccine-preventable illnesses, and malnutrition.
13
A
review of the impact of CHWs delivering curative interventions for malaria, pneumonia, and
diarrhea on child morbidity and mortality in sub-Saharan Africa found that national CHW
programs can reduce mortality by up to 63% when both curative and preventive services were
provided.
14
Brazil integrated community health workers into family health teams with nurses,
with a focus on lowering the number of patients with hypertension and diabetes who dropped
out of care. This has been associated with a 15%-20% reduction in mortality from heart
disease and strokes.
15
In 2005, Ethiopia launched its Health Extension Program, rapidly hir-
ing, training, and equipping more than 35,000 community health extension workers to sta
17,000 rural health posts. This increased geographic access to health services from 64% to
92%, and signicantly improved the coverage of prenatal care, contraceptives, and antibiotics
for acute respiratory infections; during this same time there was an acceleration in under-ve
mortality reduction.
16
However, all CHW programs are not equal. A 2020 study of exemplar CHW programs in
Bangladesh, Brazil, Ethiopia, and Liberia revealed investments in ve key systems are criti-
cal to developing eective CHW programs. Each of the exemplar CHW programs investigated
followed a set of best practices identied in the recently released WHO guidelines to optimize
CHW programs.
17
These guidelines, along with insights from exemplar CHW programs, high-
light investing in ve foundational system components (also sometimes referred to as the 5
Ss), regardless of contextual factors (Box 1).
18
164 PRIMARY CARE IN THE COVID-19 PANDEMIC

The role of CHWs during the COVID-19 pandemic
CHWs are crucial to both key public health objectives of health systems during the COVID-19
pandemic: rst, to contain the direct eects of COVID-19 by stopping transmission, and
second, to address the indirect eects of a pandemic on routine primary health care by
preventing interruptions to essential services like vaccinations, antenatal and postnatal
care, infectious disease prevention and treatment, and noncommunicable disease screening
and treatment.
3,19
Health systems with exemplar CHW programs, such as those in Ethiopia,
Liberia, Brazil, and Bangladesh, demonstrate that the best emergency response systems are
actually resilient primary health care systems that can respond rapidly and eectively to
pandemics like COVID-19 through deploying networks of trusted CHWs to prevent new infec-
tions, detect cases, and educate their communities.
3,19
CHWs can also play an important role
in disease surveillance, outbreak detection, active case nding and screening, and epidemic
response (Box 2).
20-23
Many CHWs visit each household in their community on a regular basis,
providing an opportunity to do active case nding and screening for COVID-19 symptoms at
the community level. For example, in the rst weeks after its rst case, South Africa trained
and equipped 27,000 community health workers previously serving HIV and TB patients to
go door-to-door to screen more than 11 million residents (20% of the country’s population)
for COVID-19 symptoms, referring those with positive screens for testing at primary care
clinics.
24
When CHWs are eectively integrated into national health systems and equipped
with data collection tools and training, they can submit epidemiological surveillance data to
national monitoring systems, alerting subnational and national health systems of outbreaks
while they are still small and saving valuable time in mobilizing an eective response,
25
and
thus expediting appropriate infection prevention and treatment as necessary.
Box 1. The 5 Ss: Eective CHW Programs Invest in Systems, Not Just the Services
They Deliver
Selection: Strong engagement from the community contributes to more effective CHW programs. CHW
selection systems are rooted in the communities they serve, and favor women. Strong CHW density (ratio of
CHWs per population) can be sufcient to equitably provide coverage for the entire population.
Skills: The training system, which includes preservice training and continuing education, is standardized at
the national level. Minimum standards are set for skills to be acquired upon completion of the training. All
CHWs satisfactorily complete competency certication processes prior to beginning their work as CHWs.
Supervision: A robust supervision system, in which supervisors—often frontline clinicians like nurses—are
trained to provide CHWs supportive supervision on a regular basis, strengthens performance and improves
outcomes.
Salary: Strong payment systems can ensure CHWs are paid adequately and in a timely manner, reducing
turnover and improving CHW performance. CHWs are contracted to receive nancial remuneration consis-
tent with the job demands, complexity, number of hours, training, and roles. Opportunities for salary increas-
es are available commensurate with experience, advancement in skills, and completion of additional training
(including opportunities to progress to higher-level positions in the health system).
Supply: CHWs require a strong supply system that ensures they are properly and regularly supplied with
high-quality commodities and consumables needed to deliver health care services.
Source: Recommendations. Exemplars in Global Health. Accessed February 16, 2021. https://www.exemplars.health/topics/
community-health-workers/cross-country-synthesis/recommendations.
PRIMARY CARE IN THE COVID-19 PANDEMIC 165

CHWs are in a unique position, based in the community, viewed as trusted deliverers of
education and care, and serving as a link to facility-based care. Some of these roles reect
lessons from earlier epidemics, such as Ebola, as well as emerging lessons from the COVID-19
pandemic. In the case study on Liberia presented next, we describe these dual roles, their
overlapping nature, and the strategies needed to achieve success in CHWs contributing to direct
COVID-19 response and supporting work to prevent and respond to drops in primary health
care demand and delivery. We begin with a review of how Liberia’s primary health system
learned lessons about preparedness and response from the country’s 2013-2016 Ebola epidemic.
Box 2. Roles for CHWs in Responding to COVID-19 and Preventing Disruption to Primary Care Services
23
Prevent Educate communities regarding signs, symptoms, and transmission routes, as well
as promoting personal preventive measures such as social distancing, hand hygiene,
coughing/sneezing into elbows, and water, sanitation, and hygiene interventions.
Organize hand hygiene stations in communities and health facilities.
Support, lead, or reinforce community and facility-based infection prevention and
control (IPC) measures, such as construction of triage areas and use of personal
protective equipment (e.g., face masks, gloves, gowns).
Support preparation of health systems and communities for the eventual
introduction of COVID-19 vaccines in development, including outreach to high-risk
groups.
Detect With supervision from nurses, identify signs and symptoms in community members,
support safe collection in communities and health facilities of samples, and support
rapid transport to laboratories for analysis, thus reducing risks of nosocomial
transmission.
Respond Communicate rapidly and eectively to residents.
Support self-isolation and monitor patients in the community while ensuring
delivery of food, social, and medical support.
Monitor patients for clinical deterioration and support rapid referral of individuals
who require hospitalization, reinforcing links between the health system and
communities.
Support contact tracing, symptom reporting, and monitoring of contacts of COVID-19
patients to ensure access to testing and treatment for those who develop signs and
symptoms.
Implement or support disinfection of high-risk surfaces in communities using
appropriate IPC supplies and procedures.
Sustain routine primary health care services (e.g., vaccinations and integrated
community case management of young children with malaria, pneumonia, or
diarrhea).
166 PRIMARY CARE IN THE COVID-19 PANDEMIC
Liberia: Keeping primary health systems resilient, from
Ebola to COVID-19
During the 2013-2016 Ebola outbreak in West Africa, underresourced health systems, weak-
ened from years of conict, were confronted with a pathogen that was previously unrecog-
nized in the region. Health care workers, at the front lines, were among the rst stricken and
were often unprotected, thus limiting the human resources needed to combat the outbreak
and maintain services. In Liberia, a country of 4.5 million people, the virus infected more
than 10,000 people and claimed the lives of 8% of its health workers.
26
Public distrust of
government and lack of condence in the safety of health facilities kept many people from
seeking routine health services, including prenatal care and treatment for infectious dis-
eases.
27
There was a 140% increase in patients not receiving treatment for malaria, increasing
the indirect mortality associated with the outbreak.
27,28
In September of 2014, models indicated that without interventions, up to 1.4 million people
could be infected by January 2015.
29
Ultimately, control of the outbreak relied on strengthen-
ing testing, contact tracing, and infection prevention and control (IPC) in primary health care
facilities and communities.
30
CHWs were central in this eort. More than 10,000 community
health workers were mobilized, and they worked to educate communities on preventing the
spread of the virus, to identify cases and refer them for testing, to trace contacts, and to
facilitate early treatment.
31
Investments in CHW training resulted not only in early detection
of cases and prevention of transmission, but also in continuity of essential health services.
Prior to and during the Ebola epidemic, in Konobo, a district in Grand Gedeh County in south-
eastern Liberia, the government of Liberia, with support from Last Mile Health, had been
implementing a program in which primary health care services were extended from a primary
health care clinic into villages by nurse-supervised, salaried CHWs. The clinic and community
health teams implemented training on IPC measures. This included training and equipping
midwives, nurses, and community health workers with appropriate personal protective equip-
ment (PPE) to promote care seeking among mothers, deliver clinic and home-based prenatal
care, and provide safe labor and delivery services at the facility level. Last Mile Health and
the government had invested in these strong everyday systems in Konobo including supply
chains, supportive supervision, and salaries for health workers for years. Due to this invest-
ment, facility-based delivery during the epidemic dropped by only 3% in Konobo compared
to 300% nationwide.
32
While treatment for malaria was disrupted across other parts of the
country, malaria treatment remained steady in Konobo district because supplied, supervised,
and protected community health workers delivered it to homes in their communities.
32
In 2016, Liberia’s Ministry of Health, armed with the lesson of the need to have a primary
health care system that reaches the most vulnerable before threats emerge, and just under
a year after the last case of Ebola in the country, revised its prior community health policy
and launched the National Community Health Assistant Program. This policy was supported
by seven implementing partners with a commitment to a standardized model of community
recruitment, monthly payment, training curriculum and service delivery, supervision by
professional health workers (i.e., nurses or physician assistants), and the consistent stock of
PRIMARY CARE IN THE COVID-19 PANDEMIC 167

life-saving medications and supplies necessary for diagnosis and treatment. Integral in the
service delivery package were the components of community-based surveillance for infectious
diseases, including hemorrhagic fever, but also routine services such as provision of family
planning, health promotion for care of pregnant women, and the community case manage-
ment of childhood illnesses, namely diarrhea, malaria, pneumonia, and malnutrition. Between
2016 and just prior to the COVID-19 pandemic in 2020, Liberia’s National Community Health
Assistant program hired, trained, and equipped more than 3,500 CHWs across Liberia, linking
them to 316 primary care clinics serving close to 700,000 rural people—approximately 70%
of the rural remote population.
33
Between 2016 and 2020, these CHWs conducted 3.6 mil-
lion home visits; provided more than 1.2 million treatments and screenings for children with
malaria, pneumonia, diarrhea, and malnutrition; and increased access to reproductive and
maternal health services. CHWs test and treat 48% of Liberia’s rural children with conrmed
malaria in their communities.
10
Importantly, the community health assistant program had
established a community event-based surveillance system through which CHWs had helped
identify more than 5,000 potential public health outbreaks (e.g., Lassa fever) of signicance.
Given the prominent role CHWs play in ensuring access to routine primary health care, as
well as their crucial role in the Ebola response, when the rst case of COVID-19 in Liberia
was conrmed by polymerase chain reaction (PCR) on March 16, 2020, the country was pre-
pared to leverage its national CHW system to play a vital role in both the direct COVID-19
response and ensuring continuity of primary care. In anticipation of a pandemic in January
2020, Liberia was proactive in reinstating an Incident Management System and began health
Figure 1. CHW Community Education Job Aid
35
168 PRIMARY CARE IN THE COVID-19 PANDEMIC
promotion awareness on coronavirus with printed posters at centralized areas. In March,
Liberia established both community engagement and risk communication pillars, bringing to-
gether partners and government stakeholders, including the Community Health Division. The
role of community health workers in the COVID-19 response was designed to be one inclusive
of prevention, detection, and response and emphasizing continuity of primary care (Table 1).
23
The rst priority was to ensure the safety of primary care workers, including CHWs.
Safety of health workers
Central to the design of the role of health workers in the response was the prioritization of
their safety. During the Ebola pandemic, it had been seen that provision of risk-appropriate
PPE and training on how to use it was key in keeping health workers safe. Whereas many
countries struggled to procure PPE and equip their community health workers,
34
Liberia’s
Ministry of Health made the commitment at the onset of the COVID-19 outbreak to include
CHWs and their supervisors in the projection, procurement, and distribution of PPE, along-
side all of its frontline health workers. PPE became integrated into the already scheduled
bimonthly restocking of CHW supplies through supervision visits. Additionally, these workers,
along with those working at health facilities, were trained on how to don and do the PPE
appropriately, and which PPE is required for which services. This vigilance decreased the like-
lihood of health workers falling ill and transmitting infection to others, thus serving to main-
tain community trust in health workers and preventing stigma due to perceived increased risk
of workers as vectors of transmission.
Prevention
Community health workers have been equipped with job aids and training on facts about
coronavirus transmission, symptoms, and treatment to combat misinformation that may im-
pact health-seeking behaviors and prevent uptake of public health measures (Figure 1).
35,36
As
trusted members of the community, CHWs reach out to community members during routine
household visits and through meetings with community leaders in formalized community
health committees that assist in implementing community-wide activities to support the
health of their communities. They activated handwashing stations with counseling on appro-
priate handwashing technique and frequency, educate community members about respiratory
hygiene, and emphasize masking and social distancing.
Detection
Using a community case denition with a series of questions, CHWs, from six feet away and
while wearing a mask, screen patients and household members for possible COVID-19 infec-
tion as the rst step during all routine household and sick visits. If the screening is positive
and thus indicates a possible COVID-19 case, then the CHW acts as a link to the surveillance
team for activation of testing. The CHWs create a list of contacts of the patient, counsel on
isolation, and work with nurse supervisors to develop a monitoring plan for the development
of symptoms among these contacts that would necessitate further testing.
23
PRIMARY CARE IN THE COVID-19 PANDEMIC 169
Response
Even before a suspected patient is identied, CHWs work with community leaders and mem-
bers to develop a response plan for the 24 hours after one is identied. Each home is also
supported to work through an isolation plan for household members in the event someone
were to fall ill or to identify barriers to safe isolation that would necessitate isolation outside
of the home supported by the community. Once a trigger is identied, the CHWs work with
family and community to implement these plans. While awaiting testing or referral to a facil-
ity, the patient and identied caretaker would be provided masks, and gloves for the care-
taker, with instructions to always mask when in same room, to minimize time spent within
six feet of one another, and for the caretaker to use gloves for any necessary direct contact
with the patient or the patient’s belongings.
Continuity of primary health care services
During the Ebola outbreak, much care was taken to design and implement modied clini-
cal care protocols that would allow CHWs to continue providing primary health care in the
community in situations where PPE was not available or where there were concerns about
appropriate PPE use. Coupled with further training on the nature of Ebola transmission and
protective measures, CHWs were able to continue working during the outbreak. In an era
when caregivers were fearful of bringing their sick children to facilities, they continued to
get care from CHWs.
37
Similarly, protocols for service delivery were altered during COVID-19 to
prioritize the safety of health workers and community members, while balancing the need for
continued proximal, life-saving treatment. If a patient or household member is identied as
a suspected COVID-19 patient during screening, making the patient a contact, then a six-foot
distance is maintained at all times between provider and patient and caregiver. If screening is
negative, then the CHW proceeds with the visit following no-touch protocol for services that do
not necessitate touch, such as providing medications, which can be done through careful place-
ment of medications for the caregiver to pick up once the CHW has backed away to more than
six feet from the medication. However, in the event that the CHW must get closer to perform a
service, such as a malaria rapid diagnostic test, the CHW puts on eye protection (goggles or face
shield) in addition to the mask and the usual gloves worn as standard precautions. Some proto-
cols have been altered to involve the caretaker in providing the diagnostic services that require
touch, such as checking for pitting edema as a danger sign of malnutrition.
Similar to the altering of protocols just mentioned, there were a few instances where substi-
tutions of treatment were oered. Before COVID-19, administration of the contraceptive sub-
cutaneous depot medroxyprogesterone acetate by CHWs was being pilot tested with plans for
future scale. Altered COVID-19 protocols prevented the CHWs from entering homes, mean-
ing that injections would have had to take place outside patient homes, limiting ability to
maintain patient condentiality and thus increasing potential for stigma. Due to this, and to
minimize potential of further exposure to asymptomatic cases, CHW provision of this service
was discontinued and patients were given the option of going to a facility for injectable family
planning or to transition to oral contraceptives or condoms, both of which remained available
at community level. While options were made available for those who wished to continue family
170 PRIMARY CARE IN THE COVID-19 PANDEMIC
planning, this cessation removed the preferred method of contraception for some and required
transfer of some patients to unpreferred methods or travel to the facility for ongoing injectables.
Responding to or mitigating drops in primary health care
Nationally, there was a decrease in health-seeking behavior with an 18% drop in antena-
tal care and facility-based deliveries.
38
However, only 1% of community members served
by CHWs reported not going to the facility because of a fear of COVID-19, with 97% of 603
patients who reported needing to go to a facility successfully seeing a health provider at
the health clinic.
38
Additionally, in communities serviced by CHWs, routine household visits
continued under modied protocols. Data on routine household visits showed a small dip in
March but with recovery to pre-COVID-19 numbers by May. These routine household visits
served as an important monthly touchpoint for provision of counseling and health promotion
and an opportunity for actively identifying cases through screening for potential COVID-19.
Finally, according to unpublished ndings by Rozelle and colleagues, approximately half of
rural children in Liberia received diagnostic and treatment services for malaria from commu-
nity health workers—and this has been sustained during the COVID-19 pandemic.
Disruption of primary health care
There were a number of primary health care services that were determined to be risky to de-
liver and for which specic strategies for mitigation of risk were not possible through altering
the protocol. For example, during the initial risk assessment and resulting policy change, it
was deemed too risky to continue malnutrition screening for children six months to ve years
of age using mid-upper arm circumference (MUAC) straps, as they could not be easily cleaned
in between users and there were not enough individual straps to prevent possible cross-
contamination. While the screening for the danger sign of pitting edema continued through
the alteration of a protocol as noted, the limitation of use of the more sensitive MUAC straps
increased the likelihood of missing moderate and acute malnutrition cases.
Additionally, concerns about vaccine hesitancy and safety of vaccinators acted as impetus for
the cessation of facility outreach to remote communities and a transition to facility deliv-
ery while community education could be provided to counter community concerns.
39
There
had been rumors of a new COVID-19 vaccine and anecdotal reports of children being hidden
from vaccinators due to fear that the government or donors may attempt to test the vaccine
on those receiving routine vaccinations. This moratorium on community-level vaccination
lasted from March to May 2020 while a media campaign was deployed and health promotion
strengthened to counter misinformation. Modeled estimates showed a 30% drop in adminis-
tration of the third dose of pentavalent vaccine for coverage of diptheria, tetanus, pertussis,
hepatitis B, and Haemophilus inuenza type B as well as a 35% reduction in childhood vaccina-
tion overall and outpatient visits.
39
Although the policy was reversed after only two months, it
would be another two months for the outreach numbers to climb to pre-COVID-19 numbers,
indicating a lag in changing practice (Figure 2). This demonstrates the challenge of continual
policy change in an epidemic with evolving evidence; in these situations, delays in implemen-
tation as policy shifts are inevitable, and subsequent reversal or adjustment can be confusing
and dicult for implementers.
PRIMARY CARE IN THE COVID-19 PANDEMIC 171

Global evidence: Roles, challenges, and opportunities for
CHWs in COVID-19 response
The challenges and opportunities Liberia found in engaging CHWs in the direct COVID-19
response and in maintaining primary health care services during the COVID-19 pandemic can
be compared to experiences in other countries. A rapid review found that in countries with
well-established CHW programs, CHW roles change signicantly during pandemics, includ-
ing COVID-19. Additional activities, on top of their usual responsibilities, included commu-
nity awareness, engagement, and sensitization; and contact tracing. Health system support
is required to facilitate the addition of these activities, including role clarity, supplemental
training, and supportive supervision to ensure preparedness and safe, quality care delivery.
Challenges faced by CHW programs during pandemics include supply chain and logistics is-
sues, as well as insucient supervision and increased risk of contracting disease.
40
In Liberia, Bangladesh, Ethiopia, and Brazil, CHWs educate communities on COVID-19 and
support their communities to develop realistic, evidence-based response plans. To support
COVID-19 prevention, CHWs in all four countries help organize handwashing stations, dis-
tribute IPC supplies, and in some cases support prevention of transmission at health facilities.
In Brazil, CHWs are further involved in COVID-19 education and health promotion through
Figure 2. Rivercess—Pentavalent Vaccine Third Doses
Source: University of Oslo. District Health Information System (DHIS2). Published online 2019.
https://dhis2.org/.
172 PRIMARY CARE IN THE COVID-19 PANDEMIC
identifying people in their communities who are at high risk of severe COVID-19 illness to
help them implement better prevention strategies.
18
CHWs play critical roles in screening, identifying suspected cases at the community level,
connecting them to response teams, and supporting tracing and isolation of their contacts. In
Ethiopia, CHWs conducted house-to-house screenings of more than 11 million households. In
Brazil, in addition to these roles, CHWs also monitor the symptoms of suspected cases by phone.
18
CHWs in all four countries are crucial in ensuring continued access to primary health care. In
some countries they also deliver care through telemedicine, supporting patients to use smart-
phones to get care. In Brazil and in some CHW programs in the United States, they deliver
prescriptions to patients in isolation.
18,41,42
In the United States, CHWs have reported providing
support, including psychosocial support, to their patients throughout the pandemic, espe-
cially while patients are isolated or having symptoms.
41,43,44
In the Navajo Nation in the United
States, CHWs help COVID-19 patients better understand their diagnoses through providing
information in patients’ native language and explaining important public health protocols.
42
Recommendations
Based on the available body of evidence in Liberia and globally, we recommend the follow-
ing to health care leaders seeking to engage CHWs in the control of COVID-19 and eorts to
reduce its impact on primary health care services during this pandemic and the next one
23
:
1. Build government-led coalitions and design integrated programs. Ensure both regular
primary health care provision and pandemic response are cross-cutting, with roles and
responsibilities dened across dierent health worker cadres and community health
workers integrated into national health systems and national pandemic response.
2. Establish strong data systems that include community-based surveillance and moni-
toring of quality of service delivery. Strong data systems that start at the community
level can identify emerging infectious diseases early and stop outbreaks before they
become pandemics. They can also reveal reductions in primary health service use and
facilitate procedures like contact tracing.
3. Prioritize strong community engagement before pandemics hit (as well as during and
afterward). As trusted members of their communities, CHWs are crucial to engaging
community structures to promote healthy behaviors that prevent disease transmission,
spread correct information about diseases and counteract myths, and link those who
may be infected or at high risk to appropriate care.
4. Provide frontline health workers, including CHWs, with updated training. CHWs need
fast and accurate training on emerging infectious diseases like COVID-19 that may pose
a threat to their communities. Training needs to be updated as new evidence emerges;
digital training tools can help to rapidly update protocols and guidelines and to maintain
IPC measures such as social distancing.
PRIMARY CARE IN THE COVID-19 PANDEMIC 173
5. Protect CHWs as vital frontline health workers. CHWs need protection to continue
providing care; therefore, risk-appropriate PPE for CHWs, with equal quality standards
to that of other health workers, should be included in national forecasts and budgets,
and strong supply chains should be established before pandemics hit to ensure continued
provision of crucial medicines and diagnostics, as well as the ability to accommodate
protective equipment. Additionally, restrictions such as PPE export bans and policies
that prevent international development aid to be spent on PPE must be limited to en-
sure continuation of the supply chain that is developed.
34
Tools that can estimate PPE
consumption based on service delivery package and population served are needed. They
should be developed, studied, validated, and shared for context-specic adjustments.
6. Ensure continuity of CHW salaries and supportive supervision. During a pandemic,
frontline workers like CHWs take on extraordinary risk as they work to continue caring
for their communities. They must be supported accordingly through continued salaries
and supervision, with supplemental hazard pay and extra supervision visits if possible.
7. Seize the window of opportunity. Design responses to outbreaks with an eye to long-
term health system strengthening. Frame health system challenges as problems that
could be solved by well-designed, well-resourced CHW programs to galvanize the politi-
cal will and mobilize the necessary resources to remake and strengthen the health sys-
tem. Use data to more rapidly learn, adapt, choose, and implement strategies.
8. Establish an immunization framework that prioritizes equity of access and uptake. As
the COVID-19 vaccines become available, CHWs are an important resource in counter-
ing misinformation and facilitating community acceptance of the vaccine. Additionally,
similar to their role in vaccination for children under ve years of age, they may play
a key role in organizing community-level vaccination, tracking those who have been
vaccinated to ensure adequate coverage, and in some countries, even administering
vaccinations.
45
By including CHWs in the immunization plans for COVID-19, and other
vaccine-preventable diseases, an opportunity arises to increase demand and, in doing so,
increase equity, which is required for the actual elimination of disease.
Conclusions
The experience of Liberia and other countries facing COVID-19 has revealed that investing in
people closest to the problem is the core of resilience in primary health systems. Community
health workers are the closest to the patient and the challenges they face. Investing in them
is vital for responding to endemic diseases as it is in times of epidemics.
Outbreaks and pandemics have an unforgiving ability to highlight health system vulnerabili-
ties and inequities. In doing so, they point to the immediate need for emergency response but
also the opportunity for building more resilient and equitable health systems. Among the key
174 PRIMARY CARE IN THE COVID-19 PANDEMIC
References
1. Qureshi C, Panjabi R. Expanding our health force can
save lives and create jobs simultaneously. The Hill.
August 7, 2020. Accessed November 8, 2020. https://
thehill.com/opinion/healthcare/511052-expanding-
our-health-force-can-save-lives-and-create-jobs-
simultaneously.
2. Waters R. Community workers lend human connec-
tion to COVID-19 response. Health Aff (Millwood)
2020;39(7):1112-7. 10.1377/hlthaff.2020.00836.
3. Phillips DE, Bhutta ZA, Binagwaho A, et al. Learning
from exemplars in global health: a road map for miti-
gating indirect effects of COVID-19 on maternal and
child health. BMJ Glob Health 2020;5(7):e003430.
10.1136/bmjgh-2020-003430.
4. Cometto G, Ford N, Pfaffman-Zambruni J, et al.
Health policy and system support to optimise com-
munity health worker programmes: an abridged WHO
guideline. Lancet Glob Health 2018;6(12):e1397-404.
10.1016/S2214-109X(18)30482-0.
5. Perry HB, Zulliger R, Rogers MM. Community
health workers in low-, middle-, and high-income
countries: an overview of their history, recent evolu-
tion, and current effectiveness. Annu Rev Public
Health 2014;35:399-421. 10.1146/annurev-publ-
health-032013-182354.
6. Kangovi S, Mitra N, Norton L, et al. Effect of com-
munity health worker support on clinical outcomes
of low-income patients across primary care fa-
cilities: a randomized clinical trial. JAMA Intern
Med 2018;178(12):1635-43. 10.1001/jamain-
ternmed.2018.4630.
7. Scott K, Beckham SW, Gross M, et al. What do we
know about community-based health worker pro-
grams? A systematic review of existing reviews on
community health workers. Hum Resour Health
2018;16(1):39. 10.1186/s12960-018-0304-x.
lessons that were learned during the past Ebola outbreak, and that are being further empha-
sized during the COVID-19 pandemic, are (1) investing in robust health systems during normal
times leads to more resilient health systems during emergencies; (2) CHWs are integral mem-
bers of a resilient health system; and (3) countries should be supported in further profession-
alization of community health workers and developing stronger community health systems.
Analyses of health service utilization during prior outbreaks have emphasized both the
underlying supply and demand factors.
46
Supply factors include the number of available
health care workers, available PPE, and open health facilities. Demand factors include pa-
tient health care–seeking behavior and trust in the health system. In incorporating CHWs in
outbreak response and continuation of essential health services, it is critical to provide them
the training and resources needed to recognize the danger at hand and to safely continue
working. This contributes to the supply side of health utilization. However, CHWs’ biggest
impact may be in their ability to aect the demand for health services before, during, and
after an outbreak. They are uniquely positioned to provide education about the emerging
disease and dispel myths and rumors, and they are familiar providers of health care in their
communities.
It is important to note that public trust in the health system is cultivated during normal
times, not just during outbreaks. CHWs that had been well supported and professional-
ized (equipped, trained, supervised, and paid) were more likely to be providing reliable,
routine services before the outbreak and therefore more utilized during the outbreak. As the
Ebola outbreak served as a catalyst for Liberia to further expand and formalize its National
Community Health Assistant Program, the COVID-19 pandemic should further the push for
CHW programs and community-based health systems that will get everyone closer to uni-
versal health coverage and more resilient global health systems.
PRIMARY CARE IN THE COVID-19 PANDEMIC 175

8. World Health Organization; Global Health Workforce
Alliance. Global experience of community health
workers for delivery of health related Millennium De-
velopment Goals: a systematic review, country case
studies, and recommendations for integration into
national health systems. Geneva, Switzerland: World
Health Organization, 2010. Accessed October 25,
2020. https://www.who.int/workforcealliance/knowl-
edge/publications/CHW_FullReport_2010.pdf?ua=1.
9. Das JK, Lassi ZS, Salam RA, Bhutta, ZA. Effect of
community based interventions on childhood diar-
rhea and pneumonia: uptake of treatment modali-
ties and impact on mortality. BMC Public Health.
2013;13(Suppl 3):S29. 10.1186/1471-2458-13-S3-
S29.
10. White EE, Downey J, Sathananthan V, et al. A
community health worker intervention to increase
childhood disease treatment coverage in rural
Liberia: a controlled before-and-after evaluation.
Am J Public Health 2018;108(9):1252-9. 10.2105/
AJPH.2018.304555.
11. Jennings MC, Pradhan S, Schleiff M, et al. Com-
prehensive review of the evidence regarding the
effectiveness of community-based primary health
care in improving maternal, neonatal and child health:
2. maternal health ndings. J Glob Health 2017;7(1).
10.7189/jogh.07.010902.
12. Sacks E, Freeman PA, Sakyi K, et al. Comprehensive
review of the evidence regarding the effectiveness
of community-based primary health care in improv-
ing maternal, neonatal and child health: 3. neonatal
health ndings. J Glob Health 2017;7(1). 10.7189/
jogh.07.010903.
13. Freeman PA, Schleiff M, Sacks E, et al. Comprehen-
sive review of the evidence regarding the effective-
ness of community-based primary health care in im-
proving maternal, neonatal and child health: 4. child
health ndings. J Glob Health 2017;7(1). 10.7189/
jogh.07.010904.
14. Christopher JB, Le May A, Lewin S, Ross DA. Thirty
years after Alma-Ata: a systematic review of the im-
pact of community health workers delivering curative
intervention against malaria, pneumonia and diar-
rhoea on child mortality and morbidity in sub-Saharan
Africa. Hum Resour Health 2011;9:27. 10.1186/1478-
4491-9-27.
15. Brazil Overview. Exemplars in Global Health. Ac-
cessed February 27, 2021. https://www.exemplars.
health/topics/community-health-workers/brazil.
16. Ethiopia Overview. Exemplars in Global Health. Ac-
cessed February 27, 2021. https://www.exemplars.
health/topics/community-health-workers/ethiopia.
17. World Health Organization. WHO guideline on health
policy and system support to optimize community
health worker programmes. Geneva, Switzerland:
World Health Organization, 2018. Accessed Febru-
ary 16, 2021. https://apps.who.int/iris/bitstream/
handle/10665/275474/9789241550369-eng.
pdf?ua=1&ua=1.
18. Panjabi R, Boyda D, Giugliani C, et al. Community
health programs and COVID-19: understanding how
countries are leveraging strong community health
systems to prevent, detect and respond to the virus.
Exemplars in Global Health. Accessed November 9,
2020. https://www.exemplars.health/emerging-topics/
epidemic-preparedness-and-response/covid-19/ap-
pendix/perspectives/thread?forumId=9&threadId=18.
19. Cross Country Synthesis. Exemplars in Global
Health. Accessed February 27, 2021. https://www.
exemplars.health/topics/community-health-workers/
cross-country-synthesis.
20. Clara A, Ndiaye SM, Joseph B, et al. Community-
based surveillance in Côte d’Ivoire. Health Secur
2020;18(S1):S23-33. 10.1089/hs.2019.0062.
21. Ballard M, Bancroft E, Nesbit J, et al. Prioritising the
role of community health workers in the COVID-19
response. BMJ Glob Health 2020;5(6). 10.1136/bm-
jgh-2020-002550.
22. Panjabi R. The role of community based PHC in
COVID-19. Global Financing Facility. May 19, 2020.
Accessed November 8, 2020. https://www.globalnanc-
ingfacility.org/sites/gff_new/les/documents/Role-of-
Community-Based-PHC-in-COVID-19_ENG.pdf.
23. Olasford Wiah S, Subah M, Varpilah B, et al. Prevent,
detect, respond: how community health workers
can help in the ght against COVID-19. BMJ Opin-
ion. March 27, 2020. Accessed November 8, 2020.
https://blogs.bmj.com/bmj/2020/03/27/prevent-detect-
respond-how-community-health-workers-can-help-
ght-covid-19/.
24. Abdool Karim SS. The South African response to the
pandemic. N Engl J Med 2020;382(24):e95. 10.1056/
NEJMc2014960.
25. Miller NP, Milsom P, Johnson G, et al. Commu-
nity health workers during the Ebola outbreak in
Guinea, Liberia, and Sierra Leone. J Glob Health
2018;8(2):020601. 10.7189/jogh-08-020601.
26. Evans DK, Goldstein M, Popova A. Health-care
worker mortality and the legacy of the Ebola epidem-
ic. Lancet Glob Health. 2015;3(8):e439-40. 10.1016/
S2214-109X(15)00065-0.
176 PRIMARY CARE IN THE COVID-19 PANDEMIC
27. Ly J, Sathananthan V, Grifths T, et al. Facility-
based delivery during the Ebola virus disease
epidemic in rural Liberia: analysis from a cross-
sectional, population-based household survey.
PLoS Med 2016;13(8):e1002096. 10.1371/journal.
pmed.1002096.
28. Brolin Ribacke KJ, Saulnier DD, Eriksson A, von
Schreeb J. Effects of the West Africa Ebola virus
disease on health-care utilization—a systematic
review. Front Public Health 2016;4:222. 10.3389/
fpubh.2016.00222.
29. Meltzer MI, Atkins CY, Santibanez S, et al. Estimating
the future number of cases in the Ebola epidemic—
Liberia and Sierra Leone, 2014-2015. MMWR Suppl
2014;63(3):1-14.
30. Bell BP, Damon IK, Jernigan DB, et al. Overview,
control strategies, and lessons learned in the CDC
response to the 2014–2016 Ebola epidemic. MMWR
Suppl 2016;65(3):4-11. 10.15585/mmwr.su6503a2.
31. Perry HB, Dhillon RS, Liu A, et al. Community health
worker programmes after the 2013–2016 Ebola
outbreak. Bull World Health Organ 2016;94(7):551-3.
10.2471/BLT.15.164020.
32. Tackling the next plague: recommendations from the
Ebola crisis to prevent and deal with future epidem-
ics. Princeton-Fung Global Forum, 2015. March 23,
2016. Accessed November 9, 2020. https://issuu.
com/woodrowwilsonschool/docs/monograph_nal_is-
suu-version1.
33. Liberia Overview. Exemplars in Global Health. Ac-
cessed February 27, 2021. https://www.exemplars.
health/topics/community-health-workers/liberia.
34. Ballard M, Westgate C. COVID-19: it ain’t over until
there’s PPE all over. Think Global Health. May 4,
2020. Accessed November 9, 2020. https://www.
thinkglobalhealth.org/article/covid-19-it-aint-over-
until-theres-ppe-all-over.
35. Liberia Ministry of Health. CHA COVID-19 Job Aid.
Published online 2020. https://drive.google.com/le/
d/1J8Ea_VxL5MHWO5icnZJN64VzXO5ut1Aq/view.
36. Community Event Based Surveillance for Coronavirus
(COVID-19). Liberia Ministry of Health. 2020. https://
drive.google.com/le/d/1L_2f035H7s5aPL_utPtZ5ZC-
wfEXFG3ab/view.
37. Siekmans K, Sohani S, Boima T, et al. Community-
based health care is an essential component of a
resilient health system: evidence from Ebola out-
break in Liberia. BMC Public Health 2017;17(1):84.
10.1186/s12889-016-4012-y.
38. Implementation Fidelity Initiative Data, August 2020.
Liberia Ministry of Health. 2020. https://docs.google.
com/presentation/d/1LIGlFpUs_kYz_gJ-5xYVrbb6z-
e55sgEYQy09nEZyCPM/edit?usp=sharing.
39. New ndings conrm global disruptions in essential
health services for women and children from
COVID-19. Global Financing Facility. September 18,
2020. Accessed November 9, 2020. https://www.
globalnancingfacility.org/new-ndings-conrm-glob-
al-disruptions-essential-health-services-women-and-
children-covid-19.
40. Bhaumik S, Moola S, Tyagi J, Nambiar D, Kakoti M.
Community health workers for pandemic response:
a rapid evidence synthesis. BMJ Glob Health
2020;5(6):e002769. 10.1136/bmjgh-2020-002769.
41. Kerkhoff AD, Sachdev D, Mizany S, et al. Evalu-
ation of a novel community-based COVID-19
“Test-to-Care” model for low-income populations.
PloS One 2020;15(10):e0239400. 10.1371/journal.
pone.0239400.
42. Rosenthal EL, Menking P, Begay MG. Fighting the
COVID-19 merciless monster: lives on the line—com-
munity health representatives’ roles in the pandemic
battle on Navajo Nation. J Ambul Care Manage
2020;43(4):301-5. 10.1097/JAC.0000000000000354.
43. Mayeld-Johnson S, Smith DO, Crosby SA, et al.
Insights on COVID-19 from community health worker
state leaders. J Ambul Care Manage 2020;43(4):268-
77. 10.1097/JAC.0000000000000351.
44. Goldeld NI, Crittenden R, Fox D, et al. CO-
VID-19 crisis creates opportunities for com-
munity-centered population health. J Ambul
Care Manage 2020;43(3):184-90. 10.1097/
JAC.0000000000000337.
45. Perry HB. National Community Health Worker
Programs from Afghanistan to Zimbabwe. Accessed
November 9, 2020. https://chwcentral.org/national-
community-health-worker-programs-descriptions-
from-afghanistan-to-zimbabwe/.
46. Loha Shumbullo E, Maestad O. Ebola outbreak 2014-
2016: effects on other health services. CMI Brief No.
3. Chr. Michelsen Institute. April 2020. Accessed
November 9, 2020. https://issuu.com/cmi-norway/
docs/7212-ebola-outbreak-2014-2016-effects-on-
other-hea
PRIMARY CARE IN THE COVID-19 PANDEMIC 177
W
hen the coronavirus reached the United States in early 2020, as a nation we did not
anticipate the full impact that the pandemic would have on nearly every facet of our
lives. Dentistry was no exception. In March and April many of the country’s dental providers
were under state mandates to limit provision of care.
1
As a result, access to care was severely
curtailed, and dental practices and clinics were forced to close or restricted to provide only
emergent or urgent dental care. Providers struggled to identify and implement best practices
for providing care with increased precautions to prevent disease transmission, acquiring the
required personal protective equipment (PPE) available in limited supplies, leveraging new
technologies aorded by teledentistry to provide services remotely, and preparing for the
nancial challenges ahead.
As the months passed, health inequities were magnied as the elderly, people in congregate
living facilities, people with underlying health conditions, and minority groups had not only
higher rates of COVID-19, but also worse health outcomes and higher mortality rates. Health
inequities among population groups have been a long-standing issue, but for many who were
unaware of this simmering challenge, COVID-19 brought the matter to the forefront in a way
that could not be overlooked. Such inequities are all-encompassing. Beyond health and oral
health, they touch on many other factors, such as education, nutrition, and employment.
Although currently there is no evidence of the development of new and specic oral health
inequities causally resultant from the COVID-19 pandemic, the pandemic has exacerbated
previously existing inequities, bringing them into sharper focus.
This chapter addresses solutions to oral health inequities and complements the foundational
information provided throughout this broader volume, particularly the two other oral health
Solutions to Oral
Health Inequities
Caswell A. Evans, Patrick D. Smith, Alex Narváez,
Chelsea Fosse, and Julie Frantsve-Hawley
chapters (COVID-19 and Oral Health; Integration of Primary Care and Oral Health), by ad-
dressing three factors: (1) oral health inequities; (2) current challenges in addressing inequi-
ties; and (3) the impact of the COVID-19 pandemic on dental care delivery.
Oral health and oral health inequities
Oral health is inseparable from general health and welfare. Eating, drinking, speaking, laugh-
ing, smiling, socialization, personal appearance, self-perception, perception of others, em-
ployability, promotability, and overall quality of life are inuenced by oral health. Oral health
is also associated with systemic conditions such as diabetes, cardiovascular disease, obesity,
dementia, respiratory health, and adverse birth outcomes.
2-8
Dental caries is a bacteria-mediated disease that results in subsequent cavities in teeth.
Bacteria causing the disease are transmissible. Dental caries is the most prevalent child-
hood disease. This disease process leads to tooth decay, or cavities in teeth, and can result
in pain and suering, tooth loss, abscess development, migration of the abscess, and related
consequences aecting concentration, ability to sleep, ability to study, productivity in work,
disrupted leisure time, and emotional distress. Although a rare occurrence, migration of a
dental abscess has led to brain infections and death of children and adults. Left untreated,
dental caries in children continues into their adolescent and adult years. Gum disease (peri-
odontal disease) aects large numbers of adults and can also lead to pain, diculty chewing,
alteration in diet and nutrition, and eventual tooth loss. Several studies have shown associa-
tions between periodontal disease and diabetes, certain forms of heart disease, and premature
births and low birthweight.
2-8
The challenge of oral health inequities can be summarized by the following conundrum: the
population cohort relatively least in need of dental care receives the most care; the population
cohort relatively most in need of dental care receives the least. This is evidenced by the fact
that 93% of individuals living in poverty have unmet dental needs, compared to 58% in high-
income families; meanwhile, only 28% of individuals living in poverty utilized dental services
compared to 55% of high-income families.
9
It is the imbalance in access to care that has been
exacerbated by the eects of the pandemic.
While the prevalence of tooth decay in children has declined over the past 20 years, inequi-
ties by income and racial categorization persist. Nineteen percent of children ages 2-19 living
below the federal poverty level (FPL) have untreated dental caries compared to only 7% living
at 300% or more of the FPL.
10,11
People in poverty spend 10 times more as a proportion of their
annual family income on dental services compared to high-income families (Figure 1).
9
The
prevalence of dental caries also varies signicantly among population groups. As an example,
57% of Hispanic and 48% of Black children and youth have experienced tooth decay (treated
and untreated) as a result of dental caries disease, compared to 40% of white and 45% of
Asian children and youth.
10
The dierences in dental caries experience among these racial and
income categories demonstrate oral health inequities.
180 PRIMARY CARE IN THE COVID-19 PANDEMIC

Some children with high levels of tooth decay, as well as children with special health care
needs that make them poor candidates for dental care in a typical care setting, receive their
care in a hospital operating room (OR) or ambulatory surgical center under general anes-
thesia. These settings and modalities of care are also necessary for the dental treatment for
some adults with intellectual and developmental disabilities or medical complexities. The
availability of OR time and space for dental procedures has been a long-standing challenge
for hospital-based and hospital-privileged dentists, often needing to compete with medical
procedures that are reimbursed at higher rates. Reimbursement rates are signicantly lower
for dental care provided in an OR setting despite similar overhead costs of supplies, person-
nel, and related factors. As a result, the provision of dental care in hospital ORs appears to be
given lower priority by hospital administrations. This can delay or prevent severely aected
and vulnerable children and adults from receiving the dental care they need. This represents
another facet of oral health inequity exacerbated by the pandemic.
Evidence of oral health inequities among population groups continues through adulthood.
Adult population cohorts, most notably those who are low income and people of color, have
been severely aected by COVID-19. Black adults aged 20-64 exhibit twice the level of un-
treated tooth decay as their white counterparts.
12
These trends accentuate into later years
of life.
13
Edentulism, or complete tooth loss, has been declining among older adults, but to
a lesser degree among racial/ethnic minorities and lower-income populations.
14
The gap in
dental care utilization among low- and high-income older adults has widened in recent years.
High-income older adults utilize dental care services substantially more than their low-income
Figure 1. Average Annual Proportion of Family Income Spent on Dental Services, 2011-2016
9
Used with permission from the CareQuest Institute for Oral Health.
WWW.MILBANK.ORG
1
1 Footer Te x t
3.0%
1.7%
1.4%
0.8%
0.3%
0.0%
0.5%
1.0%
1.5%
2.0%
2.5%
3.0%
3.5%
Poor (<100% FPL) Near Poor (100-124%) Low Income (125-
199% FPL)
Middle Income (200-
399% FPL)
High Income (400%+
FPL)
% of Family Income
PRIMARY CARE IN THE COVID-19 PANDEMIC 181
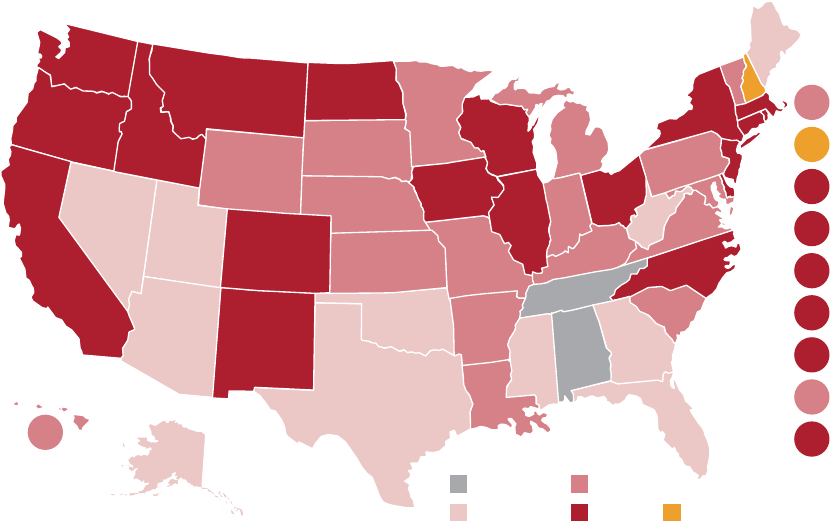
counterparts.
15
The self-reported overall condition of the mouth and teeth is lower among low-
income adults and older adults, compared to those with middle or high income.
15,16
Oral health inequities, untreated dental cavities, and periodontal disease are particularly
prominent among older adults and other populations living in long-term care settings such
as nursing homes and assisted living facilities. Oral health examination and care are under-
prioritized, infrequent, and often absent in custodial settings for seniors and people with
disabilities. Typically nursing, caregiver, and direct support sta in these facilities are not
trained in assisting residents and patients with regular oral hygiene.
17
Access to dental care is important to prevent disease and improve function and appearance.
Dental insurance is one of the most important factors enabling access to dental care. More
than 70 million people are insured by state Medicaid programs, but there are signicant
state-to-state variations in dental coverage oered by these programs for adult beneciaries.
Many states do not include dental care provisions for adults in their Medicaid program (Figure
2). Roughly 40 million children covered by Medicaid and the Children’s Health Insurance
Program (CHIP) have dental coverage due to the Early and Periodic Screening, Diagnosis and
Treatment (EPSDT) program benet required in state Medicaid programs. Almost 90% of all
children have dental benets coverage through private or public insurance, compared to 66%
of working-age adults and 34% of older adults.
18
However, only 50% of children utilize dental
care, or have at least one dental visit, in a given year, compared to 36% of working-age adults
and 44% of older adults.
19
Across all age groups, the cost of care presents the greatest barrier
to utilization of dental care services.
20
Figure 2. State Medicaid Coverage of Adult Dental Benets, January 2020
21
Used with permission from the CareQuest Institute for Oral Health.
WY
WI
WV
WA
VA
VT
UT
TX
TN
SD
SC
RI
PA
OR
OK
OH
ND
NC
NY
NM
NJ
NV
NE
MT
MO
MS
MN
MI
MA
NH
ME
LA
KY
KS
IA
IN
IL
ID
HI
GA
FL
DC
DE
CT
CO
CA
AR
AZ
AK
AL
Under development
MD
No coverage
Emergency
Limited
Extensive
182 PRIMARY CARE IN THE COVID-19 PANDEMIC
Medicare provides access to health care for 60 million older adults. The fastest-growing age
cohort in the United States is the population 65 and older. However, there is no dental care
benet in traditional Medicare (Parts A and B). Some older adults may have dental cover-
age through their state Medicaid program, depending on their eligibility and whether their
state Medicaid program contains a benet for adult dental service, but many state Medicaid
programs do not include dental service for adults.
22
Other seniors may have dental coverage
through a retirement plan; however, the proportion of seniors with that type of coverage is
diminishing. As of 2020, more than half of the Medicare Advantage (Part C) supplemental
plans oer dental services. Still, many older adults living on limited xed incomes cannot
utilize the supplemental plans as they require greater out-of-pocket costs. Out of every dollar
spent on dental services among Medicare beneciaries, 75 cents is paid out of pocket.
23-25
Nationally, less than half of dentists are enrolled in their state’s programs for children cov-
ered by Medicaid or CHIP, yet not all of these dentists actively provide care to these popula-
tions.
26
Less than a third of general and pediatric dentists bill at least $10,000 to Medicaid
annually, a threshold often used to measure meaningful participation in Medicaid programs.
27
There are fewer dentists willing to treat the adult population that is covered by Medicaid.
28,29
This makes access to care a challenge for children and adults who have a dental benet
through Medicaid.
The Patient Protection and Aordable Care Act requires the availability of dental and vision
care in marketplace health insurance plans as essential health benets specically for the
pediatric population, but it does not include a provision for dental services for adults.
30
The 38
states that expanded their Medicaid programs following the passage of the Aordable Care Act
also expanded access to dental care for lower-income children by its inclusion in the EPSDT
program. However, some states with an adult dental benet in Medicaid did not expand those
benets, as a cost-saving measure.
31
Lack of a comprehensive adult dental benet in Medicaid programs in states has resulted
in shifting costs to hospital settings. Tooth decay, its potential subsequent infections, and
abscess development are not self-healing. People in pain will, and must, seek care wherever
some relief can be found. Consequently, many people turn to hospital emergency departments
to address unmet dental needs. Visits to emergency rooms for dental pain can cost anywhere
from $400 to $1,500, compared to a $90 to $200 dental oce visit.
32
Oral health–related
conditions result in more than two million visits to hospital emergency departments annually,
accounting for a $2.7 billion expense.
33
This approach to addressing dental pain and infection
is costly for hospitals in time and resources, and it does not address and resolve the present-
ing dental problem. At best, most emergency departments provide prescriptions to address
infection and pain only.
People may or may not be able to, or have the resources to, have the
prescriptions lled. Nevertheless, their underlying oral health problem has not been ad-
dressed and would certainly reemerge.
The distribution of dentists also contributes to the challenge of accessing care. Populations in
rural areas and people living in low-income and inner-city locations are particularly troubled
in this regard. There are 6,500 dental health professional shortage areas across the nation
designated by the US Health Resources and Services Administration (HRSA). An estimated
PRIMARY CARE IN THE COVID-19 PANDEMIC 183
11,000 additional dental practitioners would be required to meet the needs of the 60 million
people living in these areas without adequate access to dental care.
34,35
What is commonly referred to as “the dental care safety net” comprises Federally Qualied
Health Centers (FQHCs), other volunteer and nonprot clinics, academic dental institutions,
school-based oral health programs, and dentists who are active providers in their state’s
Medicaid and CHIP programs. This “safety net” has some capacity to provide dental care to
those who are uninsured, poor, or low income and who experience barriers accessing tra-
ditional private dental care practice settings. There are nearly 13,000 FQHC sites across the
country. Thirty million people in the United States receive their health care services at these
sites, including a third of all those living in poverty and one in ve who are uninsured.
36
Nationwide, approximately three-quarters of FQHCs oer dental care services, rendering
dental care to just under ve million people annually.
37
Provider and patient concordance has been shown to be an issue for many in accessing medi-
cal care.
38,39
The number of Black and Latino dentists lags far behind the percentage of these
respective population groups in the United States. While Black people represented 12% and
Latinos 18% of the US population in 2016, only 4% of dentists were Black and 5% Latino.
40,41
Dental school enrollment and graduation of Black and Latino students have shown little
increase over the recent years.
42
Current challenges in addressing inequities
Several factors contribute to the persistence of preventable dental disease in the US popula-
tion. The reasons are complex, and multifactorial.
First, we have a limited focus on preventive dentistry. Existing payment systems reward
dental providers for the treatment of dental disease rather than encouraging its prevention.
Reimbursement structures incentivize provision of costly services rather than focusing on
disease prevention, oral health promotion, minimally invasive procedures, and options for
more cost-eective dental care. As such, dentists spend more time and resources providing
surgical interventions rather than oering care that prevents the onset of disease, such as
prophylactic cleanings delivered on evidence- and risk-based intervals, uoride varnish ap-
plication, and addressing oral health and nutritional behaviors. More recently, many Medicaid
programs, some private insurers, and the American Dental Association (ADA) have begun to
recognize the value of less invasive services like the use of silver diamine uoride and glass
ionomers, which have therapeutic benets for existing tooth decay. Yet there remain incon-
sistencies in levels of coverage and payment for these types of services among state Medicaid
programs, private insurance plans, and institutional policies.
43
Second, we face challenges to population oral health. Population health refers to the approach
taken by public health leaders and other community partners oering services and support
to achieve positive health and well-being outcomes in the population. The public health
approach views the population as the “patient” and focuses on what is the best interven-
tion to prevent disease and protect and promote health for that population. The population
184 PRIMARY CARE IN THE COVID-19 PANDEMIC
can be dened as demographic segments of the population or an entire local community, as
well as cities, states, and the nation. Community water uoridation and community-based
sealant programs are examples of public health interventions. The dental care safety net is
also a component of population health. Without the dental care safety net, millions of people
would not be able to access dental care. The concept of population oral health, and its practi-
cal applications, is often a weak element in dental school curricula. In part, this may result in
dentists who do not view population health as a practical approach or nancially viable model
for their practice. The patient population traditionally seen in private practice settings is not
the same population seen in the safety-net settings. Population health services reach people
not being served in private practice settings.
Third, we need education on the social determinants of health. Dental schools dedicate con-
siderable time to teaching biomedical sciences and ne motor skills, but often dedicate less
attention to educating students on social determinants of health (SDOH).
44
The economic,
educational, and environmental factors of individuals’ lives have a greater impact on indi-
viduals’ health status than does the receipt of health care services.
45
There does not yet ex-
ist an educational standard that calls upon dental programs to incorporate SDOH into their
curricula.
46
The importance of SDOH for health and oral health outcomes, and the practical
applications of addressing SDOH in dental care, seems to be underutilized and warrants both
study and application in practice settings.
Fourth, we need to address the positioning of dental providers in the broader health care
landscape. Some health care providers, as well as the public, may perceive dentists as hav-
ing a focus limited to addressing problems of the teeth, rather than being engaged members
of interdisciplinary health care teams focused on optimizing oral health as a component of
overall health. Few dentists treat caries and periodontal (gum) disease as chronic diseases,
rearming this perception. Typically dentists treat caries with dental restorations that
replace damaged tooth structure. However, dental restorations alone do not eliminate the
bacterial etiology and causes of the caries disease process. A more comprehensive approach to
dental disease management that includes continuous monitoring of disease status, its impact
on systemic health, and treatment modalities that are pharmacologic or nonsurgical could
reposition dentists in the minds of health care colleagues and the public.
Finally, we must address nancial demands. Dental students commonly graduate with sig-
nicant student debt. In 2019, the average dental school graduate had $292,000 in student
loan debt.
47
Early career dentists face signicant accumulated loan obligations, and those that
pursue purchasing or establishing a new dental practice face even greater nancial debt. The
requirements needed to maintain a practice are also expensive, given the high costs of dental
equipment and supplies. These nancial demands, combined with a fee-for-service reim-
bursement structure, leave early career dentists with very few options or latitude to practice
in a manner beyond that prescribed by the traditional payment models.
The impact of the COVID-19 pandemic on dental care delivery
People most in need have experienced a shortfall in the availability of dental care, and the
challenges they routinely face accessing care have been exacerbated during the COVID-19
PRIMARY CARE IN THE COVID-19 PANDEMIC 185
pandemic. The inability to access care has, in turn, exacerbated inequities in oral health con-
ditions aecting numerous population groups. Most notable among these population cohorts
and communities are children, low-income people, rural and marginalized urban communi-
ties, elderly adults, Alaska Natives, American Indians, immigrants, and those in long-term-
care residential settings. Cross-hatched among these cohorts are populations identied by
racial category and ethnicity. About one-third of the US population is represented among
these groups.
The initial eects of COVID-19 disproportionately aected large urban settings in the spring
of 2020, then spiked in rural areas in late summer and early fall 2020. The end of 2020
brought a surge that spared essentially no location nationwide. In rural settings, medi-
cal infrastructure was overwhelmed by the eects of COVID-19 in terms of people aected,
available health workforce, health service capacity, and related supplies.
48
It is expected that
health inequities, including those related to oral health, will become more extreme as a re-
sult of COVID-19.
49,50
During the early stages of the COVID-19 pandemic, in April and May
2020, dental care safety-net settings were forced to close or were restricted to providing only
emergent or urgent dental care.
1
After state and local restrictions were lifted, the demand for
dental care resumed in those facilities. However, new challenges emerged and will continue
to evolve as providers and systems determine how best to provide dental care safely in a “new
normal” context. This section explores those challenges.
• Redeployment of the workforce. Many dental professionals working in safety-net settings
were redeployed during the public health emergency, temporarily unable to address
the dental needs of the communities they serve. Resources were understandably pri-
oritized for COVID-19-related activities such as testing, contact tracing, and planning
and implementing revised safety and operational protocols.
• Stang. In late May 2020, 31% of dental care providers in FQHCs reported that they
had laid o or furloughed most or all of their sta. By late August 2020 only 9%
reported that most or all of their sta continued to be laid o or furloughed, although
44% had at least some sta still furloughed or laid o.
51
• Personal protective equipment. During earlier phases of the pandemic, in the spring of
2020, dental practices and safety-net dental clinics experienced shortages not just of
PPE
52
but also other dental supplies, such as syringes needed to provide local anes-
thetics. Many providers lacked condence that they could get the PPE needed to keep
sta and patients safe.
53
As PPE supplies became more available for purchase by dental
settings in summer 2020, a new challenge emerged due to the drastically increased
prices of many types of PPE (e.g., gloves, gowns, N95 respirators, and surgical masks).
By December 2020, nearly a third of dentists nationally indicated that the cost of PPE
had at least tripled compared to before the pandemic.
54
In some cases, dental provid-
ers responded by increasing fees for services or introducing a PPE surcharge. Shifting
these costs to patients may have exacerbated the cost barrier to dental care, especially
for lower-income and underserved populations.
186 PRIMARY CARE IN THE COVID-19 PANDEMIC
• Service disruption. A September 2020 survey of dental providers from a 20-state dental
insurance network found that 94% of dental oces in that network were open for
most services, including routine care; 4% were open only for urgent or emergency oral
health needs; and 2% were closed and not seeing any patients through in-person or
telehealth modes.
53
More than half of dental providers reported an increase in patients
who no longer had commercial dental insurance due to loss of their employment as a
result of the COVID-19 pandemic.
53
• School-based oral health. Many children in underserved populations have access to den-
tal care services through school-based oral health (SBOH) programs. SBOH programs
have been a major access point for dental services for children, especially those in low-
income families or who are traditionally underserved. However, SBOH programs have
been severely curtailed due to the pandemic.
55
Among children continuously enrolled in
Medicaid who received school-based dental services in 2017, 66% had never received
dental care, 36% of whom went on to receive care in an oce setting.
55
This access
was halted in the spring of 2020 when a large segment of the nation’s schools quickly
pivoted to remote learning environments due to the pandemic.
55
As a specic example,
in the northwest region of Washington State, the school-based sealant programs were
suspended, impacting 45,500 children.
56
• Medicaid provider disenrollment. There has been a reduction in the number of Medicaid
dental providers in private practice. The pandemic led to 8% of Medicaid providers
in private practices disenrolling from their state’s program from March to December
2020.
54
An additional 15% of Medicaid dental providers reported considering disenroll-
ing, and 20% reduced the number of patients covered by Medicaid in their practice.
54
• Disproportionate impact on providers of color. The COVID-19 pandemic-related changes
have disproportionately aected dental providers of color in terms of patient and pay-
ment volumes and capacity.
57
Survey data from a national network of dentists found
that 71% of dentists of color reported signicant reductions in patient volumes since
the COVID-19 pandemic began, compared to 57% of white providers. Dentists of color
were more likely than white providers to report a reduction in the maximum number
of patients seen per day due to the pandemic-related changes in patient treatment
protocols, at 85% compared to 70%, respectively. Fifty-three percent of oral health
providers of color reported seeing fewer new patients than before COVID-19, compared
to 40% of white providers. Dentists of color treat more patients of color than white
dentists. People of color experience more oral health inequities than the general popu-
lation. The lower volume of people of color seeking dental care suggests that preexist-
ing oral health inequities among that population would become exacerbated.
• Patient return to care. Nationally, patients’ return to dental care safety-net settings has
lagged compared to patients’ return to private practices. Patient volume in private
practices initially rebounded in September 2020 to an estimated 80% of pre-COVID-19
levels, but it was less than 60% in public health settings.
52,58
In the late 2020 COVID-19
PRIMARY CARE IN THE COVID-19 PANDEMIC 187
surge, less than a third of private practices reported being “open and business as
usual,” and only one in ve dentists practicing in public health settings reported the
same.
58
• Funding. In addition to multiple impacts on patient care, COVID-19 has aected care
delivery and funding for FQHCs.
59
Widespread sta furloughs occurred due to a collec-
tive $34 billion reduction in revenue—a consequence of limited patient visits during
the pandemic.
59
Yet FQHCs were able to leverage opportunities to establish systems
that can translate into a value-based system of care, create exibility in workforce
modeling, and leverage telehealth to sustain capacity for underserved populations.
59
• Providers’ longer-term expectations. Between 60% and 70% of providers in public health
settings, compared to less than half of providers in other practice settings, anticipate
long-term changes in the work process of front desk and clinical sta, including
changes in infection control, the number of patients seen in a typical day, ongoing
attention to occupational hazards, and increased use of minimally invasive and limited
aerosol-generating procedures.
51
Dental practice changes as a result of the COVID-19 pandemic have generated concerns among
dental providers about how dental care delivery will be impacted long term. The 20-state sur-
vey of dentists also found that 47% anticipated decreased patient volumes.
53
Nearly one-third
anticipated increased use of less-invasive dental procedures. Additionally, approximately
half of dental providers reported that they expected increased infection control procedures to
remain in eect to reduce contact, droplet, and airborne transmission of viral particles, while
44% anticipated increased concerns among their dental teams about occupational hazards,
such as virus exposure.
53
The sustained cumulative eect of lower patient volumes, less
invasive (and less-revenue-generating) dentistry, increasing demands of time and resources
for proper infection control, and stang concerns could signicantly reduce dental practice
revenues. Lower revenues for dental practices could result in higher treatment costs for
consumers, further limiting treatment opportunities for individuals for whom the cost of care
is already a barrier.
Solutions through delivery system innovation
In this section, we oer solutions that will address inequities in dental care during the pan-
demic period and beyond. These solutions include sustained enhanced use of teledentistry,
minimally invasive dentistry, interprofessional collaborative practice, workforce expansion,
value-based care, and enhanced public insurance programs.
Teledentistry
Due to state mandates suspending or limiting dental practices at the onset of the COVID-19
pandemic, there was a sudden high demand for teledentistry visits. Teledentistry is the
use of technology that allows dental providers to educate, assess, and make treatment
188 PRIMARY CARE IN THE COVID-19 PANDEMIC
recommendations via Internet-based software programs.
60
Some dental practices were able to
make the transition to teledentistry platforms more easily than others. This was in large part
due to the amended telehealth regulations issued by the Oce of Civil Rights, Department
of Health and Human Services, which softened restrictions on Internet-based platforms that
dentists were allowed to use for communication and transfer of protected health informa-
tion.
61
Additionally, in May of 2020, as an immediate response to dental oce closures, the
ADA released COVID-19 Coding and Billing Interim Guidance: Virtual Visits, which outlines insur-
ance reimbursement and recommended communication strategies for teledentistry visits.
62
Resources also became available to help states create regulatory environments more conducive
to teledentistry.
63,64
Telehealth platforms were being used to expand access to dental care prior to the COVID-19
pandemic. However, there was no widespread usage among dentists. In 2015, the ADA issued
a policy statement as guidance for state policy development, which was updated in 2020.
65
The document covered issues for dentists to consider regarding patients’ rights and protec-
tions, supervision of allied personnel, licensure requirements, and expectation for insurance
reimbursement. Still, dentistry has been slow to adopt the usage of teledentistry platforms
to address oral health. Several states have yet to adopt teledentistry policies or promote its
usage.
66,67
The slow adoption of teledentistry is the result of concerns about state licensure policies,
scope of dental practice, insurance reimbursement, patient protection, training of allied
dental personnel, technology gaps among underserved populations, and patient acceptance.
63
Solutions to address health inequities through teledentistry will require attention to each of
those concerns. Even so, in July of 2020, the percentage of private practice dentists using
teledentistry was 12.2%. In public health settings, the percentage of dentists using tele-
dentistry during that same time period was 57%, which appears to be a consistent trend.
68
A recent study found that 86% of patients were satised with their overall teledentistry
experience, and nearly one-third (31%) reported they did not need in-oce care following
their teledentistry visit.
69
However, most patients receiving teledentistry visits were receiving
triage for emergencies and/or advanced-stage dental diseases that would eventually require
in-oce care at some point. A survey of providers that work in public health settings indicat-
ed that adopters of teledentistry are twice as likely as other providers to anticipate increased
use of noncontact dental services as a long-term change.
70
Dental providers should develop teledentistry systems that improve access to care while
maximizing in-oce treatment eciency. Dentistry should advocate for permanent legisla-
tion that would expand the use of teledentistry. Additionally, states that currently do not
allow teledentistry should adopt clear guidance for teledentistry usage within dental practice
acts. Furthermore, not all private insurers and state Medicaid programs currently reimburse
for teledentistry visits. Providing insurance coverage for teledentistry visits would incentivize
its usage among dentists.
66,67,71,72
Professional organizations, dental education programs, and continuing education programs
need to oer training courses to develop ecient teledentistry systems. This should in-
clude education on state policies, the scope of practice of teledentistry visits, and licensure
PRIMARY CARE IN THE COVID-19 PANDEMIC 189
jurisdictions. For example, a state may not permit dentists to legally provide teledentistry
visits to individuals who reside in another state. Additionally, states should provide guidelines
regarding the supervision of dental team members when conducting teledentistry consulta-
tions. Dental practice systems for teledentistry should also ensure adequate protection of pa-
tients’ health information, as well as record keeping of teledentistry visits, patient referrals,
and follow-up visits. Furthermore, all dental personnel should have a clear understanding of
the various uses of teledentistry for patient consultations and problem-focused evaluations.
Many dental services may be provided via teledentistry, including case management for pa-
tients requiring specialty and/or emergency care, oral hygiene instructions, patient education,
outreach programs to underserved or remote areas, and motivational interviewing.
Finally, patients should be aware of teledentistry and its functionality. Dental providers need
to be aware of any concerns and limitations that patients may have for using teledentistry
and develop strategies to address them. Patients and providers who have adequate capacity
and knowledge of how to use teledentistry to address oral health concerns will be in a better
position to reduce inequities in oral disease experience and access to care. Thus, it should be
a priority to ensure that underserved and low-income populations are equipped to receive the
benets of teledentistry visits.
Minimally invasive dentistry
Minimally invasive dentistry (MID) is an evidence-based approach to dental care that em-
braces pharmacologic treatment of the dental caries disease process as a means to limit
or stop the progression of tooth decay. The premise behind MID is that tooth decay can be
treated with minimal to no surgical intervention, contrary to traditional treatment approaches
requiring “drilling and lling.” This can reduce the progression of tooth decay, along with
treatment times, treatment costs, and patient anxiety, which have been reported as signi-
cant barriers to dental care.
73
A transition toward MID requires that dentists learn how to use the MID model of dental care
and embrace it as an evidence-based, ecient, and cost-saving treatment in their practices.
This can be accomplished through predoctoral and postdoctoral dental education and training
programs and through continuing education for dentists in practice.
Dental insurers should also reimburse dentists for MID procedures at rates that are compara-
ble to traditional restorative procedures given that they have similar, if not better, outcomes.
Minimally invasive dental procedures are typically reimbursed at lower rates than surgical
interventions, if coverage even exists. For example, silverdiamine uoride (SDF) is a topical
medication that can treat some tooth decay conditions due to dental caries disease, reducing
the need for “drill and ll” treatment of tooth decay. This is an ecient, therapeutic, and
low-cost service.
74,75
If MID is to become a preferred choice of treatment that providers oer,
reimbursement incentives could help propel that change.
190 PRIMARY CARE IN THE COVID-19 PANDEMIC
Interprofessional collaborative practice
Dental care systems are often not included in interprofessional collaborative care teams. Most
dental practice occurs in private oces solely focused on dental care. There are opportunities
for dentists to practice collaboratively in safety-net primary care clinics, many of which are
FQHCs, among other opportunities.
Dental providers can assist in primary care eorts in a number of ways, particularly dur-
ing periods of restriction on dental practice, such as those experienced with the COVID-19
pandemic. In some settings, dentists have performed COVID-19 testing and assisted in
contact-tracing eorts.
76
With more eective medical-dental integration and integrated
health records, there is potential for dental professionals to assist medical colleagues in the
identication of patients with chronic conditions such as diabetes and high blood pressure,
those who smoke, and other high-risk individuals. By identifying these individuals, dental
providers can not only assess patients’ oral health needs, provide minimally invasive dental
care, and develop treatment protocols so that existing oral health problems do not worsen,
but can also refer these patients for follow-up care with medical colleagues.
Similarly, other health care professionals can help identify oral diseases and work collabora-
tively with dental providers to develop interventions aimed to reduce oral health complica-
tions. Individuals requiring extended isolation periods or experiencing prolonged eects of
COVID-19 complications may require additional support managing their oral health due to
their inability to visit a dental oce.
2-8,77
Dental providers can also help manage chronic diseases of COVID-19 patients who are at
higher risk of morbidity and mortality. Individuals with preexisting health conditions such as
diabetes, heart disease, elevated blood pressure, or cancer; older adults; and individuals from
racial minority groups have a higher risk of death from COVID-19. Those individuals may also
be at higher risk for oral diseases due to biologic or social determinants of health. Thus, den-
tal providers’ attempts to address chronic disease eects, through interventions such as oral
health education, nutritional education, or smoking cessation, could have signicant benets
in helping patients reduce their risk and the severity of COVID-19 complications.
Workforce expansion and distribution
The dental care workforce is commonly made up of dentists, dental hygienists, dental as-
sistants, dental therapists, community dental health coordinators (CDHCs), community health
workers, and others. Each member of the dental team has a dened role and contribution to
patient care and oral disease prevention. Currently the dental profession—including private
and safety-net settings—services only 55% of the population, including those with com-
mercial insurance, Medicaid, or self-pay. There are several strategies that federal and state
governments can adopt to address workforce shortages and ensure that the remaining 45% of
the population can access dental care. For example, more student loan repayment programs
and increased Medicaid reimbursement may incentivize dental providers to accept Medicaid
enrollees or seek practice opportunities in underserved areas. States can also expand direct
access for dental hygienists to deliver dental care in remote and underserved areas without
PRIMARY CARE IN THE COVID-19 PANDEMIC 191
requiring the supervision of a licensed dentist. Currently, eight states do not allow direct
access for dental hygienists.
78,79
In addition, states that allow direct access can reduce restric-
tions on dental hygienists’ ability to take advantage of those policies, such as extensive con-
tinuing education and/or work requirements.
80,81
Another workforce strategy aimed at improving access to care is the use of dental therapists,
who can assist in the anticipated shortfall of licensed dentists to treat new and existing
Medicaid enrollees, as well as individuals living in tribal communities or other underserved
areas.
82
Dental therapists are educated and trained to provide a limited range of clinical ser-
vices that are also provided by a dentist. As of January 2021, legislation in 12 states permits
dental therapists to practice in collaboration with a supervising dentist. More states have
active legislative proposals to initiate dental therapy practice. Additionally, CDHCs can educate
patients, improve oral health literacy, and ensure their awareness and capacity to seek appro-
priate dental care.
83
CDHCs are somewhat similar in function to community health workers.
To include and increase the number of dental therapists and CDHCs in dental care settings,
more awareness among dental providers, educational opportunities, and funding opportuni-
ties to support their employment in dental settings are needed.
84-86
Value-based care
Value-based care is a payment system in which providers’ reimbursement levels are driven by
health outcomes, and service delivery is focused on prevention and health promotion.
59
These
systems dier from traditional fee-for-service models that reimburse providers based on
volume of procedures, most of which are surgical interventions. Value-based reimbursement
systems typically include bundled incentive payments to encourage provision of preventive
services and improving oral health outcomes for individuals and the patient population within
a practice.
Some health care systems structured on value-based payments during the early days of
COVID-19 restrictions had fewer nancial setbacks compared to health care organizations
with fee-for-service payment systems, allowing the value-based health care systems to
remain open and avoid provider furloughs. Those organizations also had more exible nan-
cial capacity that enabled them to focus more eectively on COVID-19 testing, contact tracing,
telehealth, home-based care, and patients’ social needs.
87
Bringing more dental providers into value-based payment systems may oer an opportunity
to minimize the impact of dental care disruptions that ultimately put dental providers in situ-
ations where they lose productivity and revenue necessary to maintain their dental practices.
59
Public insurance programs
Restructuring public insurance programs could have a profound impact on reducing oral
health inequities that have been exacerbated due to COVID-19. There is no Medicare coverage
for routine dental care for seniors.
88
Only 19 state Medicaid programs oer extensive adult
dental benets.
22
As of July 2020, 35 states opted to expand Medicaid under the Aordable
Care Act. At that time, it was estimated that Medicaid expansion in the 15 remaining states
192 PRIMARY CARE IN THE COVID-19 PANDEMIC
would increase the number of insured adults by four million. By November 2020, three ad-
ditional states had expanded their Medicaid programs, further increasing the number of
insured individuals.
31
Many of those newly insured would be from underserved populations
that experience high rates of oral diseases due to their challenges accessing dental care.
89,90
The number of Medicaid-eligible and -insured individuals could substantially increase as a
result of the economic impacts of COVID-19. The Centers for Medicare and Medicaid Services
(CMS) indicates that Medicaid and CHIP enrollment increased nationally by nearly 8% from
September 2019 through August 2020.
91
Adults with poor oral health may also have additional diculty nding employment, as most
people—including employers—make instant judgments based on appearance, including
someone’s smile and teeth.
92
Increasing adult dental benet coverage in Medicaid may reduce
unemployment among those adults, promote productivity, and boost the economy. It has
been estimated that employment gains from expanding adult Medicaid benets could reduce
the number of individuals receiving unemployment benets for an aggregate savings of $7.9
million. Additionally, tax revenue generated from newly employed individuals was estimated
at $14.2 million.
92,93
In addition to already limited state Medicaid funding for adult dental care, there is a pos-
sibility that some states could eliminate all funding for these services. During previous times
of economic downturn, states have reduced Medicaid funding for adult dental care. This
was evident during the recession in the United States nearly 10 years ago. This prospect has
already been noted in response to COVID-19. Washington State is currently exploring elimi-
nating adult dental benets. Other states have reported budget constraints, leading to stalled
eorts to expand adult dental coverage. Tennessee has reversed previous plans to extend
Medicaid dental coverage for pregnant and postpartum women.
94
On a more positive note, some states have taken action to oset the possibility of worsened
oral health inequities among adult Medicaid enrollees. Eorts have been successful to pre-
serve these benets in California and Nevada,
94
and Kansas and Louisiana have committed to
moving forward with previous decisions to provide more funding for adult dental care in their
Medicaid programs.
95,96
The preservation of Medicaid dental benets for adults among those
states may have been boosted by federal relief programs that were implemented in response
to COVID-19. For example, the Families First Coronavirus Response Act (FFCRA; “Families
First”) increased the federal Medicaid assistance percentage by 6.2% for qualifying states,
increasing the amount of money that the federal government provided for states’ Medicaid
expenditures. The FFCRA also included a “maintenance of eort” requirement that prevented
state Medicaid agencies from enacting more restrictive eligibility criteria during the COVID-19
public health emergency.
97,98
However, in November 2020, CMS issued an Interim Final Rule
that reversed prior interpretation of the Families First Act and associated guidance for states,
allowing states to change eligibility of its beneciaries and to cut optional benets such as
adult dental benets.
99
The preservation and expansion of dental benets in the midst of
COVID-19 has merit, but eorts to sustain benets must continue. Due to the negative nan-
cial impact on state budgets from the pandemic, it is possible that legislatures will attempt to
reintroduce dental Medicaid budget cuts in future legislative sessions.
PRIMARY CARE IN THE COVID-19 PANDEMIC 193
The COVID-19-related legislation that became law over the course of 2020 included the
FFCRA, signed on March 18, 2020; the Coronavirus Aid, Relief, and Economic Security
(CARES) Act, signed on March 27, 2020; and the Economic Aid to Hard-Hit Small Businesses,
Nonprots, and Venues Act (as a part of the Consolidated Appropriations Act), signed on
December 27, 2020. These packages authorized various economic relief options for health
centers, hospitals, and communities. There were also relief programs that enabled dentists
to apply for nancial support to sustain operations and continue serving their communities.
These relief programs included the Department of Health and Human Services Provider Relief
Fund and the Small Business Administration Paycheck Protection Program and Economic
Injury Disaster Loan program. At the time of this writing, It is anticipated that there will be
more COVID-19 relief packages passed in the new administration.
The impact of these relief
programs to sustain the dental care delivery system during a time of extreme vulnerability
and to prevent further exacerbation of the lack of access to dental care experienced by much
of the population is yet to be assessed.
Conclusion
The COVID-19 pandemic has yet to be contained and its impacts continue to evolve. As new
information emerges, the dental care delivery system will need to adapt. The COVID-19 pan-
demic has brought to light long-standing inequities that put populations at risk for adverse
health outcomes, including those aecting oral health. It is expected that conditions resulting
from the COVID-19 pandemic will present further barriers in access to care due to nancial
and health care systems’ limitations. Many of these barriers can be anticipated and addressed
through the strategies proposed in this chapter. These system changes would help ameliorate
oral health inequities that have become more apparent as a consequence of the pandemic.
These changes would also position dental professionals to eectively address oral health
inequities pertaining to the COVID-19 pandemic and beyond, and improve the health of all.
Collectively we now have an opportunity to redesign the dental care delivery system to correct
its frailties and the resultant oral health inequities.
Acknowledgments
We would like to thank Drs. Myechia Minter-Jordan and Sean Boynes for their guidance and
critical review of this manuscript.
194 PRIMARY CARE IN THE COVID-19 PANDEMIC
References
1. COVID-19 state mandates and recommendations.
American Dental Association Center for Professional
Success. Accessed November 19, 2020. https://suc-
cess.ada.org/en/practice-management/patients/covid-
19-state-mandates-and-recommendations.
2. Oreskovic NM, Gallucci GO, Chase II, Milliren CE,
Richmond TK. Oral health status and longitudinal car-
diometabolic risk in a national sample of young adults.
J Am Dent Assoc 2017;148(12):930-5. 10.1016/j.
adaj.2017.09.029.
3. Pietropaoli D, Del Pinto R, Claudio F, et al. Poor oral
health and blood pressure control among US hyper-
tensive adults. Hypertension 2018;72(6):1365-73.
10.1161/HYPERTENSIONAHA.118.11528.
4. Müller F. Oral hygiene reduces the mortality from aspi-
ration pneumonia in frail elders. J Dent Res 2015;94(3
Suppl):14S-16S. 10.1177/0022034514552494.
5. Preshaw PM, Bissett SM. Periodontitis and diabetes.
Br Dent J 2019;227(7):577-84. 10.1038/s41415-019-
0794-5.
6. Teeuw WJ, Gerdes VE, Loos BG. Effect of periodontal
treatment on glycemic control of diabetic patients: a
systematic review and meta-analysis. Diabetes Care
2010;33(2):421-7. 10.2337/dc09-1378.
7. Baranowski MJ, Wojtowicz A, Wysokinska-Miszczuk
J, Klempka J, Kubiszyn M. Diabetes in dental
practice: review of literature. J Educ Health Sport
2019;9(2):264-74. 10.5281/zenodo.2564551.
8. Daalderop LA, Wieland BV, Tomsin K, et al. Periodon-
tal disease and pregnancy outcomes: overview of
systematic reviews. JDR Clin Trans Res 2018;3(1):10-
27. 10.1177/2380084417731097.
9. Halasa-Rappel YA, Brow A, Frantsve-Hawley J,
Tranby EP. Poor families spent 10 times more of
their income on dental care than wealthier families.
DentaQuest Partnership for Oral Health Advance-
ment. 2019. Accessed February 26, 2021. 10.35565/
DQP.2019.2007.
10. Fleming E, Afful J. Prevalence of total and untreated
dental caries among youth: United States, 2015-2016.
No. 307. Hyattsville, MD: National Center for Health
Statistics, 2018. https://www.cdc.gov/nchs/data/data-
briefs/db307.pdf.
11. Dye BA, Mitnik GL, Iafolla TJ, Vargas CM. Trends in
dental caries in children and adolescents according to
poverty status in the United States from 1999 through
2004 and from 2011 through 2014. J Am Dent Assoc
2017;148(8):550-65.e7. 10.1016/j.adaj.2017.04.013.
12. Dental caries (tooth decay). National Institute of
Dental and Craniofacial Research. Last updated July
2018. Accessed November 19, 2020. https://www.
nidcr.nih.gov/research/data-statistics/dental-caries.
13. Fleming E, Afful J, Grifn SO. Prevalence of tooth
loss among older adults: United States, 2015-2018.
No. 368. Hyattsville, MD: National Center for Health
Statistics, 2020. https://www.cdc.gov/nchs/data/data-
briefs/db368-h.pdf.
14. Dye BA, Weatherspoon DJ, Lopez Mitnik G. Tooth
loss among older adults according to poverty status in
the United States from 1999 through 2004 and 2009
through 2014. J Am Dent Assoc 2019;150(1):9-23.e3.
10.1016/j.adaj.2018.09.010.
15. Oral health and well-being among seniors in the
United States. ADA Health Policy Institute. Accessed
November 19, 2020. https://www.ada.org/~/media/
ADA/Science%20and%20Research/HPI/Files/HPI-
graphic_0916_2.pdf?la=en.
16. Oral health and well-being in the United States. ADA
Health Policy Institute. Accessed November 19,
2020. https://www.ada.org/~/media/ADA/Science%20
and%20Research/HPI/OralHealthWell-Being-State-
Facts/US-Oral-Health-Well-Being.pdf?la=en.
17. Weintraub JA, Zimmerman S, Ward K, et al. Improv-
ing nursing home residents’ oral hygiene: results of
a cluster randomized intervention trial. J Am Med
Dir Assoc 2018;19(12):1086-91. 10.1016/j.jam-
da.2018.09.036.
18. Dental benets coverage in the U.S. ADA Health
Policy Institute. Accessed November 19, 2020. https://
www.ada.org/~/media/ADA/Science%20and%20Re-
search/HPI/Files/HPIgraphic_1117_3.pdf?la=en.
19. Dental care utilization in the U.S. ADA Health Policy
Institute. Accessed November 19, 2020. https://www.
ada.org/~/media/ADA/Science%20and%20Research/
HPI/Files/HPIgraphic_1117_2.pdf?la=en.
20. Cost barriers to dental care in the U.S. ADA Health
Policy Institute. Accessed November 19, 2020. https://
www.ada.org/~/media/ADA/Science%20and%20Re-
search/HPI/Files/HPIgraphic_1117_4.pdf?la=en.
21. Healthy mouths: why they matter for adults and state
budgets. DentaQuest Partnership for Oral Health
Advancement. February 2020. Accessed February 26,
2021. 10.35565/DQP.2020.1001.
22. Medicaid adult dental benets: an overview. Center
for Health Care Strategies. 2019. Accessed Novem-
ber 19, 2020. https://www.chcs.org/resource/medic-
aid-adult-dental-benets-overview/.
PRIMARY CARE IN THE COVID-19 PANDEMIC 195
23. Wix D, Fontana JE. Understanding dental costs and
utilization in the Medicare Advantage population.
Milliman. November 17, 2020. Accessed November
19, 2020. https://us.milliman.com/en/insight/under-
standing-dental-costs-and-utilization-in-the-medicare-
advantage-population.
24. Dental services among Medicare beneciaries: source
of payment and out-of-pocket spending. Centers for
Medicare and Medicaid Services, Ofce of Enterprise
Data & Analytics. March 2016. Accessed November 9,
2020. https://www.cms.gov/Research-Statistics-Data-
and-Systems/Research/MCBS/Downloads/DentalDa-
taHighlightMarch2016.pdf.
25. Tranby EP, Halasa-Rappel YA, Brow AR, Jacob M,
Frantsve-Hawley J. The burden of out-of-pocket
expenditures for dental care on Medicare-enrolled
elderly and disabled: Part 3 of 3. DentaQuest Partner-
ship for Oral Health Advancement. 2020. Accessed
February 26, 2021. 10.35565/DQP.2020.2002.
26. Dentist participation in Medicaid or CHIP. ADA Health
Policy Institute. Accessed November 19, 2020. https://
www.ada.org/~/media/ADA/Science%20and%20Re-
search/HPI/Files/HPIGraphic_0217_1.pdf?la=en.
27. Warder CJ, Edelstein BL. Evaluating levels of dentist
participation in Medicaid: a complicated endeavor.
J Am Dent Assoc 2017;148(1):26-32.e2. 10.1016/j.
adaj.2016.09.010.
28. Medicaid Coverage of Dental Benets for Adults.
Washington, DC: Medicaid and CHIP Payment and
Access Commission, June 2015. https://www.macpac.
gov/wp-content/uploads/2015/06/June-2015-Report-
to-Congress-on-Medicaid-and-CHIP.pdf.
29. Hinton E, Paradise J. Access to dental care in Med-
icaid: spotlight on nonelderly adults. Kaiser Family
Foundation. March 17, 2016. Accessed November 19,
2020. https://www.kff.org/medicaid/issue-brief/access-
to-dental-care-in-medicaid-spotlight-on-nonelderly-
adults/.
30. Essential health benets: HHS informational bulletin.
Centers for Medicare and Medicaid Services. Last
updated February 24, 2012. Accessed November
19, 2020. https://www.cms.gov/CCIIO/Resources/
Fact-Sheets-and-FAQs/essential-health-benet-
s12162011a.
31. Status of state action on the Medicaid expansion deci-
sion. Kaiser Family Foundation. Accessed November
19, 2020. https://www.kff.org/health-reform/state-
indicator/state-activity-around-expanding-medicaid-
under-the-affordable-care-act/.
32. Wall T, Nasseh K, Vujicic M. Majority of dental-related
emergency department visits lack urgency and can be
diverted to dental ofces. ADA Health Policy Institute.
August 2014. Accessed November 19, 2020. https://
www.ada.org/~/media/ADA/Science%20and%20Re-
search/HPI/Files/HPIBrief_0814_1.ashx.
33. Emergency department visits for dental conditions:
a snapshot. ADA Health Policy Institute. Accessed
November 19, 2020. https://www.ada.org/~/media/
ADA/Science%20and%20Research/HPI/Files/HPI-
graphic_0819_1.pdf?la=en.
34. Dental care health professional shortage areas
(HPSAs). Kaiser Family Foundation. Last updated
September 30, 2020. Accessed November 19, 2020.
https://www.kff.org/other/state-indicator/dental-care-
health-professional-shortage-areas-hpsas/.
35. Shortage areas. Health Resources and Services
Administration. Accessed November 19, 2020. https://
data.hrsa.gov/topics/health-workforce/shortage-areas.
36. Health center program: impact and growth. Health
Resources and Services Administration. Last updated
December 2020. Accessed January 10, 2021. https://
bphc.hrsa.gov/about/healthcenterprogram/index.html.
37. Surdu S, Langelier M. Trends in the provision of
oral health services by Federally Qualied Health
Centers. Oral Health Workforce Research Center.
January 2018. https://www.chwsny.org/wp-content/
uploads/2018/01/OHWRC_Trends_in_Provision_of_
Oral_Health_Services_by_FQHCs_2018.pdf.
38. LaVeist TA, Nuru-Jeter A, Jones KE. The associa-
tion of doctor-patient race concordance with health
services utilization. J Public Health Policy 2003;24(3-
4):312-23. 10.2307/3343378.
39. Williams KA, Demko CA, Lalumandier JA, Wot-
man S. Caring for African-American patients in
private practice: disparities and similarities in den-
tal procedures and communication. J Am Dent
Assoc 2008;139(9):1218-26. 10.14219/jada.ar-
chive.2008.0337.
40. Racial and ethnic diversity among dentists in the U.S.
ADA Health Policy Institute. Accessed November 19,
2020. https://www.ada.org/~/media/ADA/Science%20
and%20Research/HPI/Files/HPIgraphic_1117_6.
pdf?la=en.
41. The dentist workforce: key facts. ADA Health Policy
Institute. 2021. Accessed November 19, 2020. https://
www.ada.org/~/media/ADA/Science%20and%20Re-
search/HPI/Files/HPIgraphic_0221_1.pdf?la=en.
42. Dental education. ADA Health Policy Institute. Ac-
cessed November 19, 2020. https://www.ada.org/en/
science-research/health-policy-institute/data-center/
dental-education.
196 PRIMARY CARE IN THE COVID-19 PANDEMIC
43. Slayton RL, Urquhart O, Araujo MWB, et al.
Evidence-based clinical practice guideline on non-
restorative treatments for carious lesions: a re-
port from the American Dental Association. J Am
Dent Assoc 2018;149(10):837-49.e19. 10.1016/j.
adaj.2018.07.002.
44. Tiwari T, Palatta A, Stewart J. What is the value of
social determinants of health in dental education?
National Academy of Medicine. April 6, 2020. Ac-
cessed November 19, 2020. https://nam.edu/what-is-
the-value-of-social-determinants-of-health-in-dental-
education/.
45. Social determinants of health. HealthyPeople.gov.
Accessed November 19, 2020. https://www.healthy-
people.gov/2020/topics-objectives/topic/social-deter-
minants-of-health.
46. Accreditation standards for dental education pro-
grams. American Dental Association. Accessed No-
vember 19, 2020. http://www.ada.org/~/media/CODA/
Files/predoc.ashx.
47. Educational debt. American Dental Education Asso-
ciation. 2020. Accessed November 19, 2020. https://
www.adea.org/godental/money_matters/educational_
debt.aspx.
48. Vestal C. COVID-19 patients swamp rural hospitals.
PEW. October 20, 2020. Accessed November 19,
2020. https://www.pewtrusts.org/en/research-and-
analysis/blogs/stateline/2020/10/20/covid-19-patients-
swamp-rural-hospitals.
49. Berkowitz SA, Cene CW, Chatterjee A. COVID-19
and health equity—time to think big. N Engl J Med
2020;383(12):e76. 10.1056/NEJMp2021209.
50. Pollack HA, Kelly C. COVID-19 and health dispari-
ties: insights from key informant interviews. Health
Affairs Blog. October 27, 2020. Accessed November
19, 2020. https://www.healthaffairs.org/do/10.1377/
hblog20201023.55778/full/.
51. Kelly A, Thakkar M, Tranby EP, Frantsve-Hawley
J. Public health dental providers embrace COVID-
19-related changes: these providers are faster to
anticipate and adjust to changes amid the pandemic.
DentaQuest Partnership for Oral Health Advance-
ment. November 2020. Accessed February 26, 2021.
10.35565/DQP.2020.2023.
52. The impact of COVID-19 on the dental care sector:
insights from data for week of September 7th. ADA
Health Policy Institute. September 9, 2020. Accessed
November 19, 2020. https://www.ada.org/~/media/
ADA/Science%20and%20Research/HPI/Files/HPI_
COVID_Webinar_Sept_2020_2.pdf?la=en.
53. Tranby EP, Jacob M, Diep VK, Thakkar M. A difcult
path to COVID-19 recovery: challenges remain for
dental providers. DentaQuest Partnership for Oral
Health Advancement. October 2020. Accessed Febru-
ary 26, 2021. 10.35565/DQP.2020.2016.
54. The impact of COVID-19 on the dental care sector:
insights from data for the week of November 30th.
ADA Health Policy Institute. December 1, 2020. Ac-
cessed December 15, 2020. https://www.ada.org/~/
media/ADA/Science%20and%20Research/HPI/Files/
HPI_COVID_Webinar_Dec_2020_1.pdf?la=en.
55. Access to oral health in schools: key to improved oral
health among young children. DentaQuest Partner-
ship for Oral Health Advancement and Association
of State and Territorial Dental Directors. Decem-
ber 2020. Accessed February 26, 2021. 10.35565/
DQP.2020.4008.
56. Sea Mar Community Health Center Sealant Quarterly
Report. Washington: North Sound ACH, 2020.
57. Tranby EP, Jacobs M, Thakkar Samtani M, Perry K,
Frantsve-Hawley J. Oral health providers of color
face greater hardships from the impact of COVID-19.
DentaQuest Partnership for Oral Health Advance-
ment. December 2020. Accessed February 26, 2021.
https://www.dentaquestpartnership.org/system/les/
Oral_Health-Providers-of-Color.pdf.
58. The impact of COVID-19 on the dental care sector:
insights from data for the week of December 14th.
ADA Health Policy Institute. Accessed December 20,
2020. https://www.ada.org/~/media/ADA/Science%20
and%20Research/HPI/Files/HPI_COVID_Webinar_
Dec_2020_2.pdf?la=en.
59. Oral health value-based care: the Federally Qualied
Health Center (FQHC) story. DentaQuest Partnership
for Oral Health Advancement. August 2020. Ac-
cessed February 26, 2021. 10.35565/DQP.2020.2013.
60. Glassman P. Expanding oral health: teledentistry; im-
proving oral health using telehealth connected teams
and the virtual dental home system of care: program
and policy considerations. DentaQuest Partnership for
Oral Health Advancement. 2019. Accessed February
26, 2021. 10.35565/INN.2019.2001.
61. Notication of enforcement discretion for telehealth
remote communications during the COVID-19 na-
tionwide public health emergency. US Department of
Health and Human Services. Accessed November 19,
2020. https://www.hhs.gov/hipaa/for-professionals/
special-topics/emergency-preparedness/notication-
enforcement-discretion-telehealth/index.html.
PRIMARY CARE IN THE COVID-19 PANDEMIC 197
62. COVID-19 coding and billing interim guidance: virtual
visits. American Dental Association. May 11, 2020.
Accessed November 19, 2020. https://success.ada.
org/~/media/CPS/Files/COVID/ADA_COVID_Cod-
ing_and_Billing_Guidance.pdf.
63. Fast-track to teledentistry: removing barriers to care
while maximizing overall health. DentaQuest Partner-
ship for Oral Health Advancement. March 2020. Ac-
cessed February 26, 2021. 10.35565/DQP.2020.2010.
64. Teledentistry: providing access to care during the
COVID-19 crisis. DentaQuest Partnership for Oral
Health Advancement. March 2020. Accessed Febru-
ary 26, 2021. 35565/DQP.2020.2009.
65. ADA policy on teledentistry. American Dental Asso-
ciation. Accessed November 19, 2020. https://www.
ada.org/en/about-the-ada/ada-positions-policies-and-
statements/statement-on-teledentistry.
66. Current state laws & reimbursement policies. Center
for Connected Health Policy. Accessed November
19, 2020. https://www.cchpca.org/telehealth-policy/
current-state-laws-and-reimbursement-policies#.
67. Teledentistry by state: quick facts interactive map.
MouthWatch. Accessed November 19, 2020. https://
www.mouthwatch.com/teledentistry-regulations-start-
ing-points-for-exploration-of-how-to-use-teledentistry-
in-your-state/.
68. How COVID-19 is impacting dental care delivery in
public health settings. ADA Health Policy Institute.
July 28, 2020. Accessed November 19, 2020. https://
www.ada.org/~/media/ADA/Science%20and%20
Research/HPI/Files/HPI_COVID_Webinar_Public_
Health_2.pdf?la=en.
69. Tranby E, Fiehn R, Jacob M, Frantsve-Hawley J.
Patients give high marks to their teledentistry experi-
ence. DentaQuest Partnership for Oral Health Ad-
vancement. June 2020. Accessed February 26, 2021.
10.35565/DQP.2020.2012.
70. Kelly G. How do intellectual disabilities affect oral
health? Evid Based Dent 2020;21(1):26-7. 10.1038/
s41432-020-0083-9.
71. Blair C. COVID-19 & dentistry: coding for teleden-
tistry, billing for PPE, and in-ofce testing. McGill &
Hill Group. Accessed November 19, 2020. https://
www.mcgillhillgroup.com/Webinar/53/COVID-19-and-
Dentistry-Teledentistry-Billing-for-PPE-and-In-Ofce-
Testing.
72. D9995 and D9996 – ADA guide to understanding and
documenting teledentistry events. American Dental
Association. March 27, 2020. Accessed November 19,
2020. https://www.ada.org/~/media/ADA/Publications/
Files/CDT_D9995D9996-GuideTo_v1_2017Jul17.pdf.
73. Ericson D. What is minimally invasive dentistry? Oral
Health Prev Dent 2004;2 Suppl:287-92.
74. State Medicaid fee schedules—D1354. American
Dental Association. June 22, 2018. Accessed No-
vember 19, 2020. https://www.ada.org/~/media/ADA/
Public%20Programs/Files/StateLeg_Silver_Diamine_
Fluoride_Coverage_of_D1354_SDF_fees_paid_
state_list.pdf?la=en.
75. Are your kids covered? Medicaid coverage for the
essential oral health benets. Pediatric Oral Health
Research and Policy Center, American Academy
of Pediatric Dentistry. September 2017. Accessed
November 19, 2020. https://www.aapd.org/assets/1/7/
AreYourKidsCoverednal.pdf.
76. Kulsrud Z. How a 230-location DSO is planning to test
all patients for COVID-19 and assist with follow-up
care. Dentistry iQ. June 30, 2020. Accessed Novem-
ber 19, 2020. https://www.dentistryiq.com/covid-19/
article/14178705/how-230-dental-practices-are-plan-
ning-to-test-all-their-patients-for-covid19.
77. Suh M. Dental and medical collaboration during
COVID‐19. J Dent Educ June 15, 2020 [Online ahead
of print] 10.1002/jdd.12251.
78. Direct access states. American Dental Hygien-
ists’ Association. Revised January 2020. Accessed
November 19, 2020. https://www.adha.org/resources-
docs/7513_Direct_Access_to_Care_from_DH.pdf.
79. Variation in dental hygiene scope of practice by state.
Oral Health Workforce Research Center. Last updated
January 2019. Accessed November 19, 2020. http://
www.oralhealthworkforce.org/resources/variation-in-
dental-hygiene-scope-of-practice-by-state/.
80. Naughton DK. Expanding oral care opportunities:
direct access care provided by dental hygienists in
the United States. J Evid Based Dent Pract 2014;14
Suppl:171-82.e1. 10.1016/j.jebdp.2014.04.003.
81. Development of a new dental hygiene professional
practice index by state, 2016. Oral Health Workforce
Research Center. November 2016. Accessed Febru-
ary 26, 2021. https://www.chwsny.org/wp-content/
uploads/2016/12/OHWRC_Dental_Hygiene_Scope_
of_Practice_2016-2.pdf.
82. Yee A, McGlaston K, Restuccia R. How dental
therapists can address the social and racial dis-
parities in access to care. Am J Public Health
2017;107(S1):S28-9. 10.2105/AJPH.2016.303641.
83. Grover J. Community dental health coordinators:
cultural “connectors” for oral health. N C Med J
2017;78(6):383-5. 10.18043/ncm.78.6.383.
198 PRIMARY CARE IN THE COVID-19 PANDEMIC
84. Brickle CM, Self KD. Dental therapists as new oral
health practitioners: increasing access for under-
served populations. J Dent Educ 2017;81(9):eS65-72.
10.21815/JDE.017.036.
85. Friedman JW, Mathu-Muju KR. Dental therapists:
improving access to oral health care for underserved
children. Am J Public Health 2014;104(6):1005-9.
10.2105/AJPH.2014.301895.
86. Koppelman J, Vitzhum K, Simon L. Expanding
where dental therapists can practice could in-
crease Americans’ access to cost-efcient care.
Health Aff (Millwood) 2016;35(12):2200-6. 10.1377/
hlthaff.2016.0844.
87. Roiland R, Japinga M, Singletary E, et al. Value-
based care in the COVID-19 era: enabling health care
response and resilience. Duke University Margolis
Center for Health Policy. June 2020. Accessed No-
vember 19, 2020. https://healthpolicy.duke.edu/sites/
default/les/2020-07/best_practices_brief_nal.pdf.
88. Medicare dental coverage. Centers for Medicare and
Medicaid Services. Last updated November 19, 2013.
Accessed November 19, 2020. https://www.cms.gov/
Medicare/Coverage/MedicareDentalCoverage.
89. Cross-Call J, Broaddus M. States that have expanded
Medicaid are better positioned to address COVID-19
and recession. Center on Budget and Policy Priorities.
July 14, 2020. Accessed November 19, 2020. https://
www.cbpp.org/research/health/states-that-have-
expanded-medicaid-are-better-positioned-to-address-
covid-19-and.
90. Medicaid expansion enrollment. Kaiser Family Foun-
dation. June 2019. Accessed November 19, 2020.
https://www.kff.org/health-reform/state-indicator/
medicaid-expansion-enrollment.
91. Medicaid and CHIP enrollment trends snapshot
through August 2020. Centers for Medicare and Med-
icaid Services. Accessed January 10, 2021. https://
www.medicaid.gov/medicaid/national-medicaid-chip-
program-information/downloads/august-medicaid-
chip-enrollment-trend-snapshot.pdf.
92. Halasa‐Rappel YA, Tschampl CA, Foley M, Della-
penna M, Shepard DS. Broken smiles: the impact of
untreated dental caries and missing anterior teeth on
employment. J Public Health Dent 2019;79(3):231-7.
10.1111/jphd.12317.
93. Aleccia J. Bad teeth, broken dreams: lack of dental
care keeps many out of jobs. CNBC. Last updated
September 13, 2013. Accessed November 19, 2020.
https://www.cnbc.com/2013/06/12/bad-teeth-broken-
dreams-lack-of-dental-care-keeps-many-out-of-jobs.
html.
94. Protecting and expanding access to oral health in
2020: learning from state trends in Medicaid adult
dental coverage. Families USA. September 2020.
Accessed November 19, 2020. https://familiesusa.
org/wp-content/uploads/2020/09/OH-180_FINAL-
Protecting-and-Expanding-Access-to-Oral-Health-
in-2020-Analysis-002.pdf.
95. Ollove M. Virus imperils health care safety net. PEW.
September 1, 2020. Accessed November 19, 2020.
https://www.pewtrusts.org/en/research-and-analysis/
blogs/stateline/2020/09/01/virus-imperils-health-care-
safety-net.
96. Atkeson A. State levers to support dental care in
COVID-19’s public health and economic emergency.
National Academy for State Health Policy. August 31,
2020. Accessed November 19, 2020. https://www.
nashp.org/state-levers-to-support-dental-care-in-cov-
id-19s-public-health-and-economic-emergency/.
97. Levin H. Increased Medicaid funding authorized by
the Families First Coronavirus Response Act. KPMG.
Accessed November 19, 2020. https://institutes.kpmg.
us/government/articles/2020/covid-19-medicaid-fmap.
html.
98. Solomon J, Wagner J, Aron-Dine A. Medicaid protec-
tions in Families First Act critical to protecting health
coverage. Center on Budget and Policy Priorities.
April 17, 2020. Accessed November 19, 2020. https://
www.cbpp.org/research/health/medicaid-protections-
in-families-rst-act-critical-to-protecting-health-cover-
age.
99. Park E. New CMS rule would weaken Families First
continuous coverage protection in Medicaid. George-
town University Health Policy Institute. November
2, 2020. Accessed November 19, 2020. https://ccf.
georgetown.edu/2020/11/02/new-cms-rule-would-
weaken-families-rst-continuous-coverage-protection-
in-medicaid/.
PRIMARY CARE IN THE COVID-19 PANDEMIC 199
SECTION 3: STRATEGIES TO
ADVANCE PRIMARY CARE EQUITY
Anti-Racist Primary
Care Policy in the
United States
Michelle Morse, Sanjay Basu, and Bram Wispelwey
S
imultaneous with the COVID-19 pandemic in the United States was a national uprising against
police violence, sparked by the killings of Black Americans in several cities. As protests grew
in scope and attention in parallel to the pandemic, and as COVID-19 disproportionately impacted
Black, indigenous, and people of color (BIPOC) communities, the medical establishment in the
United States debated how to address racism within health care institutions. In this chapter, we
describe the origins of racial health inequities in the United States, their relationship to health care
and public health access and infrastructure, and the important role of primary care in advancing
anti-racist policies for the future.
The origins of racial health inequities: Settler colonialism,
racial capitalism, and their living legacy in primary care
It is impossible to understand the inequitable distribution of primary care resources in the United
States without an honest accounting of the country’s historical origins as a nation-state. The
United States is a settler colonial nation, meaning that its historical genesis is characterized less
by exogenous domination and exploitation of native peoples (colonialism) than by their elimina-
tion and supersession by European aliens (settler colonialism).
1,2
Along with the displacement of
indigenous communities, settler colonists by denition establish a paradigm of unequal relations in
which they claim superiority, which distinguishes the settler colonialism process from migration,
as migrants move to a new territory without superiority claims or attempts at social dominance.
The social establishment of unequal relations is where settler colonialism intersects with, and
claims justication by, European or white supremacy. The United States is thus an archetypal, liv-
ing example of settler colonialism, which is an enduring “structure not an event.”
3
The United States is the wealthiest country in the history of the world in terms of gross
domestic product, but its present aggregate economic condition hinges on the fact that it
expropriated land from American Indians—whom the settler colonists killed o via murder,
war, starvation, slavery, and disease, from a population of 50 million to 100 million in 1492 to
3.5 million by the mid-1600s
4
—and it exploited the labor of people who were kidnapped from
West Africa, enslaved, and brutalized. From 1619 to 1865, the value of stolen labor amounts to
$97 trillion at minimum wage rates with modest interest, or more money than the 2020 GDP
of all countries in the world, combined.
4
The racial capitalism that informed the economic and
social development of the United States continues to shape the distribution of wealth, racial
categorization and hierarchy, political power, and health access and outcomes today.
5
That
this settler colonial framing of US history is little discussed,
6
both in general and in health
policy circles specically, speaks directly to the need for epistemic reconstitution
7
that centers
knowledge, narratives, and reparative claims from BIPOC communities and remarginalizes
continental whiteness.
Because ability to pay determines one’s access to health care in the United States, these his-
torical factors remain highly relevant to ongoing health care access inequities. Racial inequi-
ties in rates of insurance and insurance type are driven in large part by employment status,
8
where institutional racism has long disadvantaged BIPOC.
9
By creating and perpetuating an
insurance system that presents nancial barriers to preventive and primary care, the United
States de facto rations care for the very people who have been historically wronged by legacies
of racial capitalism and settler colonialism.
Additionally, these very same legacies have led to an inequitable distribution of health risks,
as is increasingly legible in the discourse on essential workers during the COVID-19 pan-
demic.
10,11
Not only do BIPOC suer higher prevalence of noncommunicable diseases due to
structural racism and settler colonialism,
12
but they are also at higher risk for contracting
infectious pathogens, like the coronavirus that causes COVID-19, because of their overrep-
resentation in “the top nine essential occupations,”
13
including transportation and material
moving, health care support, food preparation and serving, building and grounds cleaning and
maintenance, and personal care and service. The historical and ongoing realities of structural
racism and settler colonialism generate a need for preferential access to primary care and
health care overall for BIPOC. Instead, health care access is signicantly and often dramati-
cally worse for BIPOC than for white Americans.
Segregation, geography, and lack of access to care
Segregation and resultant inequities in primary care access are a product of structural racism
that goes beyond the 250 years of slavery and 100 years of Jim Crow policies in the United
States. US policies implemented at the federal, state, and local levels throughout the 20th
century, and in violation of Amendments 5, 13, and 14 of the US Constitution, have been
among the key drivers of housing inequities and racial segregation in the country. Redlining
(the systematic denial of federal housing loans to those living in predominantly Black neigh-
borhoods), blockbusting (the persuading of white homeowners to sell cheaply by playing on
fears of racial neighborhood change), and contract buying (predatory deedless “ownership”
204 PRIMARY CARE IN THE COVID-19 PANDEMIC
contracts with high eviction risk) were all utilized or tolerated by the government to inhibit
home buying and equity for Black Americans, further entrenching wealth inequality—an
inequality of such extreme degree in the early 21st century that ocial economic segregation
policies are no longer required to maintain de facto segregation.
14
The urban, predominantly coastal metropoles of American settler colonial society retain a
high density of health services and professionals, while more sparsely populated rural areas
suer shortages.
15
Racial segregation in rural areas, which is rampant, is associated with
worse health care access.
16
Similarly, within urban areas, there are stark dierences in access
by race. For example, the odds of being in a low-access primary care zone in Philadelphia
are 28 times higher for those in heavily Black areas of the city than for those not living in
these areas.
17
Despite the evidence that increasing access to primary care improves high-value
care and outcomes,
18
including reduced mortality, the United States has a disproportionately
high number of specialists relative to primary care providers, and the density of primary care
physicians is continuing to decrease.
19
This inequitable burden is disproportionately borne by
BIPOC, who already have higher nancial, insurance, and geospatial barriers to primary care,
as described earlier.
While the Patient Protection and Aordable Care Act (ACA) of 2010 expanded access to insur-
ance and primary care for tens of millions of Americans, it has failed to address the shortage
of primary care providers. Signicant barriers to obtaining adequate primary care access
remain for patients with Medicaid coverage and those accessing care in safety-net institu-
tions, in particular.
20
Commodication of the sick care system
Moving further upstream to public health, the trajectory is similarly grim. While public health
spending has always represented an inappropriately small share of health expenditure in the
United States,
21
per capita ination-adjusted public health spending has decreased by 9.3%
since 2008, and continues to make up a shrinking percentage of national health expenditure
from a peak of 3.18% in 2002 to a projected 2.40% in 2023.
22
The de-prioritization of public health expenditure and primary care investment derives from
the misalignment of incentives in the health system. Population-level interventions are
responsible for much of the 20th-century gains in life expectancy in wealthy countries, and
primary care expansions led to improved outcomes. Yet there are a number of stakeholders
who benet nancially from a sicker population, including hospitals and the pharmaceutical
industry, who are paid more when they care for sicker patients and receive payments that
correspond to higher utilization of higher complexity (more serious illness) through dominant
fee-for-service payment mechanisms. Furthermore, the insurance industry is incentivized
to increase the cost of health care over time, as insurance companies receive payments as a
portion of total costs.
23
The modern medical industrial complex has been “characterized by
interlocking relationships between business and government” and the “blurring of the line
between for-prot and not-for-prot status,”
24
a scenario that ironically allows “nonprot”
hospitals and academic medical centers to be prot signicantly
25
and at the expense of their
PRIMARY CARE IN THE COVID-19 PANDEMIC 205
BIPOC patients.
26
Given the historically racialized capture of nancial means that has led to
a massive racial wealth gap, this multimodal capitalist health care system inevitably exac-
erbates racial inequities in care and access as those individuals with more favored insurance
status (such as commercial employer-sponsored insurance) receive the greatest health care
access and services, while those at greater risk for unemployment and poverty (receiving
Medicaid or no insurance) have disproportionately fewer providers, longer wait times for
service, and poorer quality care.
27
History of community health centers and community health workers
Despite the tremendous historical and ongoing barriers to adequate primary care for BIPOC in
the United States, there remains a rich history of reforms, resistance, and alternative meth-
ods of community care. One example, spearheaded by H. Jack Geiger and John Hatch, is the
creation of the community health center. The goal of Geiger and Hatch’s Tufts-Delta Health
Center in Mississippi was to secure “active involvement with its target populations in ways
that will change their knowledge, attitudes, and motivation—address the social, economic,
environmental, and political circumstances that determine their ill health.”
28
The success of
the community health center model in serving impoverished communities can be summed
up in its replication, with more than 1,300 community health centers created, to date, in both
urban and rural areas.
In response to racial inequities in care and access, the Black Panther Party extended its ad-
vocacy and pragmatic work to health care in the late 1960s and early 1970s. Eorts “included
providing basic medical care to the poor, working with lay community members and trusted
professional health workers in alternative facilities established by the activists.”
29
The party
simultaneously confronted health system neglect and the damage accumulated by overt
racism in the research and clinical elds, which left a lasting rational suspicion by BIPOC of
biomedical abuse and predation that lingers in primary care today. The positive and trans-
formative impact on health workers who volunteered in the Black Panther clinics has been
profound and lasting.
30
Federal policy ensures that sick-care spending prevails over primary care
and prevention
The United States has long invested preferentially in health care treatment over primary care,
prevention, and social service spending,
31
and the federal government response to COVID-19
has followed the same unfortunate pattern.
32
Had employers and commercial health plans
paid hospitals using Medicare’s payment formulas, total payments over the 2016–2018 period
would have been reduced by $19.7 billion, a potential savings of 58% that could be used to
fund anti-racist primary care and prevention.
33
But because the medical industrial complex
under the US system of racial capitalism stands to prot handsomely from sick care, incen-
tives to shift investments toward social support, primary care, and prevention are lacking.
34
Global spending comparisons show that relative to other Organisation for Economic Co-
operation and Development (OECD) countries, the United States consistently spends more on
206 PRIMARY CARE IN THE COVID-19 PANDEMIC
health services and less on social services than all other OECD countries despite evidence that
social supports improve population health.
35
The distribution of funds in the Coronavirus Aid, Relief, and Economic Security (CARES) Act
again demonstrated that even within hospital-based care, private hospitals were prioritized
over safety-net hospitals, defying public health and equity principles. Additionally, private
hospitals refused or delayed service to people needing transfer to intensive care facilities
from rural hospitals and lower-capacity hospitals serving primarily BIPOC communities.
36
Researchers who studied allocation of CARES Act and Paycheck Protection Program funds to
examine the impact on BIPOC communities noted that disproportionately Black communi-
ties received the same level of relief funding as counties with less health and nancial need,
which resulted in inequity and ineciency.
37
Another analysis of the rst $50 billion in relief
grants showed that hospitals normally deriving most of their revenue from patients with
private insurance received more than twice as much federal coronavirus relief funding per bed
than the hospitals with the smallest share of private insurance money; institutions represent-
ing the top 10% of hospitals based on share of private insurance revenue received $44,321 in
COVID-19 relief per hospital bed, which was more than double the $20,710 per hospital bed
among hospitals in the bottom 10% of private insurance revenue.
38
Finally, the federal budgeting process requires Congressional Budget Oce scoring frame-
works and PAYGO (the pay-as-you-go requirement in federal budgeting, which prohibits
creation of new scal decits), with the costs and savings of federal spending calculated over
ve- and ten-year time horizons. This PAYGO approach creates structural barriers to ap-
propriately valuing the long-term savings and secondary noneconomic benets created by
improved population health from public health and prevention programs.
39
Because budget-
ary forecasting necessarily manages doubt and unpredictability, and projections that extend
beyond ve or ten years are even more uncertain, actuaries and forecasters are hesitant to
change this limiting time horizon. An example of the paradox produced by the PAYGO re-
quirement is coverage of “expensive” treatment for HIV in the early 2000s, which was clearly
life-extending, but did not generate sucient return on investment to meet PAYGO require-
ments until an extended time horizon of analysis, making it more dicult for federal govern-
ment ocials to agree to pay for treatment.
39
Such structural barriers hinder anti-racist pri-
mary care, which should prioritize primary care access, prevention, and public health despite
the longer time horizon for impact on health outcomes and savings in health spending.
Expansive workforce inequities undermine health equity
The December 2017 report of the United Nations Special Rapporteur on Extreme Poverty and
Human Rights highlighted that the United States was far behind other developed nations in
poverty alleviation and equitable health care access, which is dependent upon the availability
of health providers.
40
Life expectancy in the United States consistently declined from 2015
through 2017, making it the only developed nation in the world to experience this trend.
41
In the United States, the average life expectancy was 75.6 years for Blacks and 79 years for
whites as of 2017.
42
Among BIPOC and white communities living in the same city or county,
life expectancy inequities were stark. For example, as of 2012, within Boston, Massachusetts,
PRIMARY CARE IN THE COVID-19 PANDEMIC 207
the predominantly Black community of Roxbury had a life expectancy of 58.9 years compared
with the predominantly white community of Back Bay, which had a life expectancy of 91.9
years (i.e., a gap of 33 years).
43
Even when elite academic medical systems are located in historically Black communities, they
may prioritize attracting wealthy patients from across the country or even internationally
instead of serving surrounding communities. In Boston, for example, The Boston Globe revealed
that only 5% of patients receiving care at the Dana Farber Cancer Institute, a global leading
institution in cancer care, were Black in 2017, despite the broad catchment area spanning
regionally to internationally.
44
Health care providers are the cornerstone of health care systems globally and represent
among the largest portions of nationwide spending for health budgets. Health providers serve
as critical human capital. They care for the sick, design and implement preventive health
strategies, conduct crucial research, and are rst responders in public health emergencies,
such as the COVID-19 pandemic. But primary care physicians have been undervalued and
underpaid for decades.
45
Other providers, including nurse practitioners, physician assistants,
and community health workers, among others, have been marginalized in the health care
system and often overlooked or undervalued by physicians despite growing evidence of their
eectiveness in delivering quality care.
46,47
In the United States, health professional shortage areas (HPSAs) are designated by the Health
Resources and Services Administration as geographic regions, population groups, and facili-
ties that have a lack of primary, dental, or behavioral health care providers.
48
The agency also
denes medically underserved areas (MUAs) as those that lack access to primary care services
dened through the ratio of primary medical care physicians to population, infant mortality
rate, percentage of the population with incomes below poverty level, and percentage of the
population age 65 years or over.
49
BIPOC are more likely to live in both HPSAs and MUAs.
50
BIPOC also face signicant barriers to entering the health professions—a direct symptom
of our system of racial capitalism. In the United States, only 4% of physicians are Black.
51
Armative action programs in the 1960s and 1970s resulted in a doubling of underrepre-
sented minority matriculants in medical schools.
52
Unfortunately, the leveling o in such
matriculants correlated temporally with the Supreme Court ruling against admission quotas in
the case of Regents of the University of California v. Bakke, which outlawed the consideration of
race in university admissions. Programs like the Association of American Medical Colleges’ ini-
tiative “3000 by 2000,” which were successful in increasing representation of BIPOC in medical
school, have unfortunately not been funded to continue. As a result of these and other trends,
there were fewer Black men in medical school in 2014 than there were in 1978.
51
To provide care to underserved communities, the US health care delivery system depends on
the systematic appropriation of international physicians. About 40% of primary care physi-
cians practicing in the United States are international medical graduates, who tend to practice
in the most economically and educationally deprived communities.
53
Many international
medical graduates are talented BIPOC physicians from the Caribbean and sub-Saharan Africa
who have migrated to the United States for better job opportunities, improved salaries, the
208 PRIMARY CARE IN THE COVID-19 PANDEMIC
option to work in better-equipped hospitals and clinics, and career development opportuni-
ties. The United States systematically avoids its duty to train BIPOC to be physicians, while it
benets from the educational investment made by immigrant physicians’ countries of origin,
without having to compensate those countries for their human capacity investments. For
several decades, these trends have left global South countries with even worse health care
access and quality.
Increasing the primary care workforce has been associated with reduced mortality and in-
creases in life expectancy. For every 10 additional primary care physicians per 100,000 popu-
lation, life expectancy increases by 51.5 days, while the same increase in specialist physicians
is only associated with a 19.2-day increase in life expectancy.
19
Primary care physicians are
critical for preventive care, community outreach, chronic disease management, and other
essential population health functions. Unfortunately, the mean density of primary care physi-
cians relative to population size has decreased, from 46.6 per 100,000 population in 2005 to
41.4 per 100,000 population in 2015, with greater losses in rural areas in the United States.
19
As the primary care provider shortage worsens, the adverse eects will disproportionately
harm BIPOC communities who already have worse health provider shortages and suer from a
higher burden of chronic disease and poor health due to an unfair exposure to increased risk.
Anti-racist primary care workforce analysis
We sought to answer the question, how much would redistribution of the primary care
workforce in a fundamentally anti-racist manner—that is, by redistributing preferentially to
BIPOC communities—be expected to improve inequities in mortality and life expectancy? We
performed statistical regressions with the primary outcome of age-standardized life expec-
tancy at birth in a county, from the National Center for Health Statistics for the years 2010,
2015, and 2017 (having imputed estimates from 2015 to 2017).
54
The key independent vari-
able of interest was primary care physician density, dened as the number of non–federally
employed physicians younger than 75 years old who were not hospital residents and whose
major professional activity was outpatient care in general practice, family medicine, general
internal medicine, or general pediatrics, per 100,000 population in each US county and the
District of Columbia (N = 3,103 counties), from the American Medical Association Physician
Masterle for 2010, 2015, and 2017.
55
We separately interacted the primary care physician
density variable with each of three race/ethnic variables (the percent Black, percent Latino,
or percent indigenous population in a county), to estimate how much more benet may be
achieved in high-minority counties than low-minority counties from an increase in primary
care physician density.
56
We controlled for the density of specialist physicians reporting a
principal activity of patient care per 100,000 population,
58
the urban or rural status of the
county,
57
percentage of the population under the federal poverty threshold,
58
percent female,
59
unemployment rate,
59
density of hospital beds per 100,000 population,
60
percent enrolled in
Medicare,
60
and medical care cost index
61
(the relative cost of medical care in the county, in
ination-adjusted 2017 US dollars).
62
PRIMARY CARE IN THE COVID-19 PANDEMIC 209
We performed quantile regressions to estimate how much life expectancy increases associ-
ated with an increase in primary care density diered for counties with lower minority versus
higher minority populations. The quantile regressions were performed at the 25th, 50th
(median), and 75th percentiles of minority population percentage across all counties (for each
of Black, Latino, and indigenous minority populations), to understand how lower minority
versus higher minority counties had dierent slopes in their regression line between primary
care physician density and life expectancy. Regressions were performed after controlling for
secular trends (including xed eects for year) and calculating bootstrapped standard errors
with clustering at the county level. Estimates were performed in R (version 4.0.2).
As shown in Table 1, among counties that are only at the 25th percentile of Black population
proportion (0.8% Black), each additional 10 primary care physicians per 100,000 population
had a nonsignicant impact on life-expectancy at the p < 0.05 level (from a baseline life
expectancy of 78.6 years or 28,701 days). By contrast, counties at the 50th percentile (2.5%
Black) averaged a 104.9-day increase in life expectancy for each additional 10 physicians per
100,000 (95% condence interval [CI]: 14.6, 195.2; p = 0.022, from a baseline of 78.1 years or
28,518 days), and those at the 75th percentile (11.0% Black) had the greatest benets, aver-
aging a 175.1-day increase (95% CI: 100.4, 249.7; p < 0.001, from a baseline of 76.3 years or
27,853 days).
When conducting the regressions by percentiles of Latino population percentage, we estimat-
ed an even larger gain in life expectancy per each additional 10 primary care physicians per
100,000 population. Although the life expectancy gain was at least 130 days across all quan-
tiles, it also increased as the Latino population percentage increased, to a gain of 252.3 days
(95% CI: 156.8, 347.8; p < 0.001, from a baseline of 78.3 years or 28,605 days) among counties
at the 75th percentile (9.5% Latino).
When conducting the regressions by percentiles of the indigenous population percentage, the
life expectancy gain was similarly patterned, with a gain of 118 days among the 25th percen-
tile counties (0.4% indigenous) up to a gain of 157 days among the 75th percentile counties
(1.3% indigenous).
Toward an anti-racist primary care agenda
A model of equitably distributed primary care physicians and services should not be created
from scratch, as a number of real-world examples exist that oer elements or whole pro-
grams that can be emulated in the United States. We would argue that it is essential, however,
that any model considered introduce a foundation of community control and accountability.
Community-based approaches to program planning allow for novel ideas and frameworks
that can help avoid planning pitfalls generated by ignorance of the communities served.
Ensuring that community members shape primary care development means that local issues
are taken into account, health services are relevant to specic community needs, greater pub-
lic acceptability and accountability is attained, future directions are equitable, and community
members are able to participate—through paid work—in primary care delivery.
210 PRIMARY CARE IN THE COVID-19 PANDEMIC

Global models of success: Community health workers and beyond
One mechanism for participation of community members in primary care delivery is by inte-
grating community health worker (CHW) programs into primary care delivery models. CHWs
are frontline public health workers who come from the communities they serve and continue
to be embedded within these communities, providing knowledge and a basis for trust in pa-
tient care. CHWs liaise directly with other health care workers, including doctors and nurses.
Table 1. Regressions of Primary Care Physician Density Against Age-Standardized Life Expectancy
Percent of county
populations that are of each
minority group (%)
Baseline life expectancy in
years (interquartile range)
and days
Estimated change in life
expectancy in days from
each additional 10 primary
care physicians per 100,000
population in county (95%
condence interval; p-value)
Minority
population
25th
percentile
among
counties
50th
percentile
among
counties
75th
percentile
among
counties
25th
percentile
among
counties
50th
percentile
among
counties
75th
percentile
among
counties
Counties
at the
25th
percentile
of
minority
population
Counties
at the
50th
percentile
of
minority
population
Counties
at the
75th
percentile
of
minority
population
Black 0.8 2.5 11.0
78.6 yrs
(77.5,
80.1), or
28,701
days
78.1 yrs
(76.7,
79.6), or
28,518
days
76.3 yrs
(74.7,
77.7), or
27,853
days
+47.9
(-25.9,
+121.7; p =
0.204)
+104.9
(+14.6,
+195.2; p
= 0.022)
+175.1
(+100.4,
+249.7; p
< 0.001)
Latino 2.2 4.1 9.5
77.2 yrs
(75.3,
79.2), or
28,202
days
77.7 yrs
(76.0,
79.5), or
28,389
days
78.3 yrs
(76.9,
79.7), or
28,605
days
+131.2
(+49.6,
+212.9; p
= 0.002)
+197.3
(+101.0,
+293.6; p
< 0.001)
+252.3
(+156.8,
+347.8; p
< 0.001)
Indigenous
0.4 0.6 1.3
77.4 yrs
(75.6,
79.3), or
28,267
days
77.9 yrs
(76.2,
79.6), or
28,451
days
77.9 yrs
(76.6,
79.4), or
28,457
days
+118.0
(+18.0,
+217.9; p
= 0.021)
+133.1
(+38.5,
+227.6; p
= 0.006)
+156.7
(+58.7,
+254.7; p
= 0.002)
We performed quantile regressions to estimate how much life expectancy increases associated with
an increase in primary care density diered for counties with lower minority versus higher minority
populations. The quantile regressions were performed at the 25th, 50th (median), and 75th percentiles
of minority population percentage across all counties (for each of Black, Latino, and indigenous minority
populations), to understand how lower minority versus higher minority counties had dierent slopes in
their regression line between primary care physician density and life expectancy. Regressions were per-
formed after controlling for secular trends (including xed eects for year) and calculating bootstrapped
standard errors with clustering at the county level. Estimates were performed in R (version 4.0.2).
PRIMARY CARE IN THE COVID-19 PANDEMIC 211
It is now clear that well-designed CHW programs in the United States not only positively
impact health outcomes, but may also supply a return on investment (as much as $2.47 to an
average Medicaid payer for every dollar invested).
63
Although a number of political barriers
remain to scaling CHW programs nationally, their broader inclusion within the primary care
landscape can be a boon for underserved patients and BIPOC who are underrepresented in
other health professional roles.
One primary care model that is a reference for equitable population-based health care cover-
age is Cuba’s primary health care delivery system. The Cuban primary care system includes
a primary care nurse and doctor-staed clinic (consultorio) for every 600-700 people,
64
both
in rural and urban settings, to achieve universal access. The physician and nurse live on the
city block or in the rural community in which they serve, and these teams are also stationed
in factories and schools. The primary care system is a bedrock of the equitable and ecient
Cuban health system, ensuring that primary doctors are nearby and integrated into the com-
munity. Applying a similar geospatial and physician-integrated approach into US primary
care design would potentially have an important impact on primary care access, although
race-specic measures—beyond such universal initiatives—are needed given the persistent
impact of racism in the United States at every socioeconomic level.
65
Another relevant model is that of the US’s northern neighbor, Canada. Canada’s health care
system provides universal access to primary care through a decentralized, publicly funded (on
a per capita basis) set of clinics in each province or territory. The primary care system was
leveraged during the COVID-19 pandemic as part of the COVID-19 Primary Care Pathway, in
which the province of Alberta standardized virtual care rapidly.
66
Essential to this approach
was a focus on social wraparound services for the most vulnerable patients that included
connections to community agencies that provided income support, food and meal delivery,
isolation hotels, and linguistically and culturally appropriate support. The ability to recognize
“safety-net ags,” including social isolation, food insecurity, low health literacy, and lack of
caregiver support, was a built-in functionality essential for providing equitable, as opposed to
simply equal or universal, primary care. The pathway may have utility beyond the pandemic,
as a tool for linking primary care with community initiatives.
Other international models provide further learnings for the US system. The Basque Country,
an autonomous region in northern Spain with the highest life expectancy in the European
Union, has a universal health care coverage system for all 2.2 million of its residents, through
a single-payer, tax-funded model. In 2010, recognizing the impending crisis of an aging
population combined with economic strain and an increased burden of chronic disease, the
Basque government launched a program that inculcated “a culture of shared leadership” to
achieve a “balance between top-down and bottom-up change.”
67
The ve core elements of
the program, carried out through integrated health organizations—hospital and primary care
structures within a single organization and with a shared strategic plan—were “a population
health approach; prevention of chronic illnesses; patient responsibility and autonomy; inte-
grated care; and ecient interventions adapted to the needs of the chronically ill patient.”
68
The Basque integrated health organizations focused on building “relationships with the
community-based social support agencies,”
68
which resulted in coordination between health
212 PRIMARY CARE IN THE COVID-19 PANDEMIC
facilities and community-based resources in housing, employment, integration, or food sup-
port. The model has led to reduced health care costs, reduced hospitalizations, and improved
patient reports of care coordination, with two-thirds of patients stating the coordination
between health and social services was good or very good.
69
Within the US health care system,
accountable care organizations could benet from a similar approach as the Basque integrated
health organizations, one that would signicantly address issues of equity, community self-
determination, and accountability. Such innovations have recently begun, most notably with
the Accountable Health Communities approach that comprehensively screens for social needs
among Medicare and Medicaid beneciaries and provides assistance while analyzing the
health and care utilization impacts of the model.
70
Reparations are foundational in anti-racist primary care
Health workers have a moral obligation to understand and address health inequities.
Applicative justice, which describes injustice as a curable ill, attempts to revolutionize how
health care system resources are distributed in order to advance anti-racist primary care.
71
To ght historical and ongoing structural inequities, guiding principles from applicative
justice are useful: (1) when giving priority to the worst o, address historical and ongoing
discrimination; (2) prioritize equitable treatment rather than equal treatment (meaning that
historically marginalized populations will need more than their equal share of resources to
reduce inequity); and (3) maximize health care outcomes within and among communities.
Applicative justice also demands that reparations be implemented to address the historical
atrocities and the health inequities experienced by today’s marginalized BIPOC communities.
71
Unfortunately, few places have implemented this approach to date.
Based on modeling of COVID-19 outbreaks in South Korea and Louisiana, evidence shows that
COVID-19 transmission and mortality would have been signicantly decreased if monetary
reparations had been paid to Black American descendants of enslaved people prior to the start
of the COVID-19 pandemic.
72
By increasing wealth amongst Black American descendants of
enslaved people, reparations would have decreased Black Americans’ overrepresentation as
frontline workers, decreased rates of living in overcrowded housing, and increased access to
things like personal protective equipment and hand sanitizer, all of which would have reduced
COVID-19 transmission amongst Blacks and the community at large. As a result, prominent
academics have called for reparations for US enslavement of Africans as a key solution to ra-
cial health inequities related to COVID-19, other infectious conditions, and chronic diseases.
73
Reparations, usually described using legal frameworks, have not been prominently discussed
in a health or health equity context until the COVID-19 pandemic.
73
Economists have advanced
the moral and academic evidence base for reparations for Black American descendants of
persons enslaved in the United States—using a framework of acknowledgment, redress, and
closure—and described why it is the responsibility of the federal government rather than lo-
cales to implement reparations.
74
Because the federal government failed to deliver its promise
of land grants to newly emancipated Americans at the end of the civil war, the racial wealth
gap between Blacks and whites persists in modern America and inuences several other
outcomes, including racial health inequities.
75
Thus, policy solutions that advance applicative
PRIMARY CARE IN THE COVID-19 PANDEMIC 213
justice and anti-racist primary care frameworks must uplift reparations as a critical path
forward in addressing racial health inequities as well as reestablishing the trustworthiness of
institutions like the federal government.
Anti-racist primary care health policy opportunities
and limits
Health policy solutions for racial health inequities are numerous but are often considered not
politically feasible because of ongoing white supremacist ideologies and values, acknowledged
or not. Our review provides only a limited sampling of the plentiful opportunities for policy
action that would advance anti-racist primary care, but political will to act on these policy
proposals at the time of this writing appears limited.
Potential sources of funding for the programs and policies discussed in this chapter abound.
For example, nonprot hospitals, many of which are academic medical centers, benet
from signicant tax breaks, especially on real estate, but wealthy organizations like Harvard
University do not currently fully contribute to voluntary programs like Payment in Lieu of
Taxes (PILOT).
76
Full contributions to PILOT programs could increase local government fund-
ing of essential and underfunded sectors like public health departments. Similarly, declaring
racism a public health crisis at both local and federal levels has the potential to mobilize
funds and realign priorities to meet the material needs of BIPOC communities while advanc-
ing healing and racial justice.
77
A public policy prescription to advance anti-racist primary care should at a minimum include:
Fully funding the Indian Health Service (IHS). For years, the National Congress of American
Indians has called for full funding of the Indian Health Service, which is currently funded at
less than half the national per capita federal funding rate, to ensure equity and address the
unjust racial health inequities in outcomes for indigenous communities.
78
Medicare for All. Health workers, activists, and communities across the country have been call-
ing for Medicare for All as a solution for massive health inequities, barriers to accessing care,
and rising costs in the health care industry.
79
Despite extensive support for the policy across
the nation, including support by 69% of voters, it did not become a part of the Democratic
party platform or presidential candidate Joe Biden’s plans in 2020.
80
Federal workforce equity programs and federal funding for community health workers. Primary
care is not considered an attractive career path, and the lives of Americans are unnecessar-
ily shortened because of gaps in primary care access. Federal policies to incentivize work in
HPSAs and MUAs are urgently needed as are policies to increase racial diversity in medicine.
Despite growing evidence of the benet of CHWs in cost-eectively improving health out-
comes, increasing trust, and addressing social determinants of health, CHWs are still not
funded at the federal level.
63
Housing rst. Housing is one of the most important rights and should be easy to ensure in
a wealthy democracy like the United States, but only one in ve renters has access to the
214 PRIMARY CARE IN THE COVID-19 PANDEMIC
assistance they need, and the number of unhoused individuals has not improved due to inad-
equate funding for the Department of Housing and Urban Development.
81
Increased federal funding for public health. As the COVID-19 pandemic has demonstrated, fund-
ing must be allocated to modernize public health departments and public health preparedness.
Federally qualied health centers (FQHCs) should be fully funded as entitlements instead of
through annual appropriations. The Anti-Racism in Public Health Act would create a Center
on Anti-Racism in Health at the Centers for Disease Control and Prevention, while improving
the federal government’s ability to develop anti-racist health policy and creating a law en-
forcement violence prevention program at the CDC.
82
Criminal legal reform. The BREATHE Act, developed by the Movement for Black Lives in part-
nership with hundreds of community-based partner organizations, shifts funding from
defense and carceral programs to community-led justice, housing, health programs, and
commissions to advance justice, carceral reform, and health equity.
83
Reparations for Black American descendants of persons enslaved in the United States. Reparations
would have a meaningful impact on decreasing the racial wealth gap and thus meaningful
impact on the social determinants of health and health outcomes. If the promise of racial
justice and health equity is to be fullled, reparations must be paid by the federal government
to Black American descendants of persons enslaved in the United States.
Conclusions
In this chapter, we argued that the origins of racial health inequities in the United States are
rooted in the country’s settler colonialism and racial capitalism, but that forms of resistance
through US history—including community health centers, community health care workers,
and progressive activism—are important sources of potential hope in repairing the historical
legacy in the United States. Further investments in public health, primary care, and prevention—
pivoting away from a sick-care model—are vital for the reduction of inequities along race lines.
Nevertheless, we argue that a combination of health, economic, and social policies—including
reparations—are vital to fully adopt an anti-racist agenda in the primary care space.
PRIMARY CARE IN THE COVID-19 PANDEMIC 215
References
1. Veracini L. Introducing: settler colonial studies. Settl
Colon Stud 2011;1(1):1-12.
2. Wolfe P. Settler colonialism and the elimination of the
native. J Genocide Res 2006;8(4):387-409.
3. Wolfe P. Settler colonialism and the transformation of
anthropology: the politics and poetics of an ethno-
graphic event. New York: Cassell, 1999.
4. HickelJ.Enoughofaid—let’stalkreparations.The
Guardian. 2015. Accessed December 6, 2020. https://
www.theguardian.com/global-development-profes-
sionals-network/2015/nov/27/enough-of-aid-lets-talk-
reparations.
5. Robinson CJ. Black Marxism: the making of the Black
radical tradition. Chapel Hill: University of North Caro-
lina Press, 2000.
6. Mamdani M. Settler colonialism: then and now. Crit
Inq 2015;41(3):596-614.
7. Mignolo W. Decoloniality and phenomenology: the
geopolitics of knowing and epistemic/ontological colo-
nial differences. J Specul Philos 2018;32(3):360-87.
8. Sohn H. Racial and ethnic disparities in health
insurance coverage: dynamics of gaining and losing
coverage over the life-course. Popul Res Policy Rev
2016;36(2):181-201.
9. Yearby R. The impact of structural racism in employ-
mentandwagesonminoritywomen’shealth.Hum
Rights 2018;43(3):21.
10. Silver SR, Li J, Boal WL, Shockey TL, Groenewold
MR. Prevalence of underlying medical conditions
among selected essential critical infrastructure
workers—Behavioral Risk Factor Surveillance Sys-
tem, 31 states, 2017-2018. Morb Mortal Wkly Rep
2020;69(36):1244-9.
11. Krisberg K. Essential workers facing higher risks dur-
ing COVID-19 outbreak. Nations Health 2020;50(6):1-
16.
12. Mitchell FM, Sangalang C, Lechuga-Peña S, Lopez
K, Beccera D. Health inequities in historical context: a
critical race theory analysis of diabetes among African
Americans and American Indians. Race Soc Probl
2020;12(4):289.
13.RogersTN,RogersCR,VanSant‐WebbE,GuLY,Yan
B,QeadanF.RacialdisparitiesinCOVID‐19mortality
among essential workers in the United States. World
Med Health Policy 2020;12(3):311-27.
14. Rothstein R. The color of law: a forgotten history of
how our government segregated America. New York:
Liveright, 2017.
15. Naylor KB, Tootoo J, Yakusheva O, Shipman SA,
Bynum JPW, Davis MA. Geographic variation in spa-
tial accessibility of U.S. health care providers. PLoS
One 2019;14(4):e0215016.
16. Caldwell JT, Ford CL, Wallace SP, Wang MC, Taka-
hashi LM. Racial and ethnic residential segregation
and access to health care in rural areas. Health Place
2017;43:104-12.
17. Brown EJ, Polsky D, Barbu CM, Seymour JW,
Grande D. Racial disparities in geographic access
to primary care in Philadelphia. Health Aff (Millwood)
2016;35(8):1374-81.
18. Levine DM, Landon BE, Linder JA. Quality and
experience of outpatient care in the United States for
adults with or without primary care. JAMA Intern Med
2019;179(3):363-72.
19. Basu S, Berkowitz SA, Phillips RL, Bitton A, Landon
BE, Phillips RS. Association of primary care physician
supply with population mortality in the United States,
2005-2015. JAMA Intern Med 2019;179(4):506-14.
20. Saluja S, McCormick D, Cousineau MR, et al. Bar-
riers to primary care after the Affordable Care Act: a
qualitativestudyofLosAngelessafety-netpatients’
experiences. Health Equity 2019;3(1):423-30.
21. Institute of Medicine; Committee on Public Health
StrategiestoImproveHealth.Forthepublic’shealth:
investing in a healthier future. Washington, DC:
National Academies Press, 2012.
22.HimmelsteinDU,WoolhandlerS.Publichealth’sfall-
ing share of US health spending. Am J Public Health
2016;106(1):56-7.
23. Primas S. The quirky incentives that have made
US healthcare sick. Medium. November 18, 2017.
Accessed December 13, 2020. https://medium.com/@
sidneyprimas/the-quirky-incentives-that-have-made-
us-healthcare-sick-e2c611a9afca.
24. Burlage R, Anderson M. The transformation of the
medical-industrialcomplex:nancialization,thecorpo-
rate sector, and monopoly capital. In: Waitzkin H, ed.
Health care under the knife: moving beyond capital-
ism for our health. New York: Monthly Review Press;
2018.
25. Appelbaum E, Batt R. How academic medical centers
made out on coronavirus bailouts. The American
Prospect. September 28, 2020. Accessed December
19, 2020. https://prospect.org/economy/how-aca-
demic-medical-centers-made-out-on-coronavirus-
bailouts/.
26. Johnson SF, Ojo A, Warraich HJ. Academic health
centers’antiracismstrategiesmustextendtotheir
business practices. Ann Intern Med December 8,
2020. https://doi.org/10.7326/M20-6203.
216 PRIMARY CARE IN THE COVID-19 PANDEMIC
27.OfceofInspectorGeneral,DepartmentofHealthand
Human Services. Access to Care: Provider Availability
in Medicaid Managed Care. Washington, DC: Depart-
ment of Health and Human Services, 2014. https://
oig.hhs.gov/oei/reports/oei-02-13-00670.asp.
28.GeigerHJ.TherstcommunityhealthcenterinMis-
sissippi: communities empowering themselves. Am J
Public Health 2016;106(10):1738-40.
29. Nelson A. Body and soul: the Black Panther Party and
theghtagainstmedicaldiscrimination.Minneapolis:
University of Minnesota Press, 2011.
30. Bassett MT. No justice, no health: the Black Panther
Party’sghtforhealthinBostonandbeyond.JAfrAm
Stud (New Brunsw) 2019;23(4):352-63.
31. Bradley EH, Canavan M, Rogan E, et al. Variation in
health outcomes: the role of spending on social ser-
vices, public health, and health care, 2000–09. Health
Aff (Millwood) 2016;35(5):760-8.
32. Halpern SD, Truog RD, Miller FG. Cognitive bias and
public health policy during the COVID-19 pandemic.
JAMA 2020;324(4):337-8.
33.WhaleyCM,BriscombeB,KerberR,O’NeillB,Kof-
ner A. Nationwide Evaluation of Health Care Prices
Paid by Private Health Plans: Findings from Round
3 of an Employer-Led Transparency Initiative. Santa
Monica, CA: RAND Corporation, 2020.
34.UnitedHealthraises2020protforecastaspharmacy
benetsbusinessdrivesgrowth.CNBC.October14,
2020. Accessed December 19, 2020. https://www.
cnbc.com/2020/10/14/unh-earnings-q3-2020.html.
35. Bradley EH, Elkins BR, Herrin J, Elbel B. Health and
social services expenditures: associations with health
outcomes. BMJ Qual Saf 2011;20(10):826-31.
36. Evans M, Berzon A, Hernandez D. Some California
hospitalsrefusedCOVID-19transfersfornancial
reasons, state emails show. Wall Street Journal. Octo-
ber 19, 2020. Accessed December 19, 2020. https://
www.wsj.com/articles/some-california-hospitals-
refused-covid-19-transfers-for-nancial-reasons-state-
emails-show-11603108814.
37. Kakani P, Chandra A, Mullainathan S, Obermeyer Z.
Allocation of COVID-19 relief funding to disproportion-
ately Black counties. JAMA 2020;324(10):1000-3.
38. Schwartz K, Damico A. Distribution of CARES Act
funding among hospitals. Kaiser Family Foundation.
May 2020. Accessed December 19, 2020. https://
www.kff.org/coronavirus-covid-19/issue-brief/distribu-
tion-of-cares-act-funding-among-hospitals/.
39. Westmoreland T. Standard errors: how budget rules
distort lawmaking. Georgetown Law J 2007;95(5):1555.
40. Alston P. Statement on visit to the USA. United
NationsHumanRightsOfceoftheHighCommis-
sioner. December 15, 2017. Accessed December 19,
2020. https://www.ohchr.org/EN/NewsEvents/Pages/
DisplayNews.aspx?NewsID=22533.
41. Centers for Disease Control and Prevention National
Center for Health Statistics. FastStats—Life Expec-
tancy. Mortality in the United States, 2018. 2018.
Accessed December 19, 2020. https://www.cdc.gov/
nchs/fastats/life-expectancy.htm.
42. Bailey ZD, Krieger N, Agénor M, Graves J, Linos
N, Bassett MT. Structural racism and health inequi-
ties in the USA: evidence and interventions. Lancet
2017;389(10077):1453-63.
43. Zimmerman E, Evans BF, Woolf SH, Haley AD. Social
capital and health outcomes in Boston. Center on
Human Needs, Virginia Commonwealth University.
September 2012. Accessed December 19, 2020.
https://societyhealth.vcu.edu/media/society-health/
pdf/PMReport_Boston.pdf?TB_iframe=true&width=92
1.6&height=921.6.
44. Kowalczyk L. Color line persists, in sickness as in
health. Boston Globe. December 12, 2017. Accessed
December 19, 2020. https://apps.bostonglobe.com/
spotlight/boston-racism-image-reality/series/hospi-
tals/.
45. Schwartz MD. Health care reform and the pri-
mary care workforce bottleneck. J Gen Intern Med
2012;27(4):469-72.
46. Lassi ZS, Cometto G, Huicho L, Bhutta ZA. Quality of
care provided by mid-level health workers: systematic
review and meta-analysis. Bull World Health Organ
2013;91(11):824-33I.
47. Rifkin SB. Community health workers. In: Quah SR,
ed. International encyclopedia of public health. 2nd
ed. Oxford, England: Academic Press, 2017:93-102.
http://www.sciencedirect.com/science/article/pii/
B9780128036785000837.
48. Shortage areas. Health Resources & Services
Administration. Updated February 1, 2021. Accessed
December 19, 2020. https://data.hrsa.gov/topics/
health-workforce/shortage-areas.
49. Negrusa S, Ghosh P, Warner JT. Provider Retention
in High Need Areas. ASPE. US Department of Health
and Human Services. December 22, 2014. Accessed
February 2, 2021. https://aspe.hhs.gov/report/pro-
vider-retention-high-need-areas.
PRIMARY CARE IN THE COVID-19 PANDEMIC 217
50. Allen NB, Diez-Roux A, Liu K, Bertoni AG, Szklo M,
Daviglus M. Association of health professional short-
age areas and cardiovascular risk factor prevalence,
awareness, and control in the multi-ethnic study of
atherosclerosis (MESA). Circ Cardiovasc Qual Out-
comes 2011;4(5):565-72.
51. Association of American Medical Colleges. Altering
the Course: Black Males in Medicine. 2016. Accessed
February 2, 2021. https://store.aamc.org/download-
able/download/sample/sample_id/84/.
52. Komaromy M, Grumbach K, Drake M, et al. The role
of black and Hispanic physicians in providing health
care for underserved populations. N Engl J Med
1996;334(20):1305-10.
53.PinskyW.Trump’stravelrestrictionswillmake
Americans sicker, not safer. Stat. August 7, 2018.
Accessed December 19, 2020. https://www.statnews.
com/2018/08/07/trump-travel-restrictions-interna-
tional-physicians/.
54. National Center for Health Statistics. US Small-
Area Life Expectancy Estimates Project. Centers for
Disease Control and Prevention. 2018. Accessed
December 19, 2020. https://www.cdc.gov/nchs/nvss/
usaleep/usaleep.html.
55. American Medical Association. AMA Physician Mas-
terle.AccessedDecember19,2020.https://www.
ama-assn.org/practice-management/masterle/ama-
physician-masterle.
56. United States Census Bureau. Explore Census Data.
Accessed December 19, 2020. https://data.census.
gov/cedsci/.
57. National Center for Health Statistics. NCHS Urban-
RuralClassicationSchemeforCounties.June1,
2017. Accessed December 19, 2020. https://www.cdc.
gov/nchs/data_access/urban_rural.htm.
58. United States Census Bureau. Small Area Income
and Poverty Estimates (SAIPE) Program. 2019.
https://www.census.gov/programs-surveys/saipe.html.
59. U.S. Bureau of Labor Statistics. Databases, tables,
and calculators by subject. Updated February 2,
2021. Accessed December 19, 2020. https://data.bls.
gov/timeseries/LNS14000000.
60. American Hospital Association. AHA Annual Survey
Database. Accessed December 19, 2020. https://
www.ahadata.com/aha-annual-survey-database.
61. Centers for Medicare and Medicaid Services. Pub-
lic Use File. Updated February 28, 2020. Accessed
December 19, 2020. https://www.cms.gov/Research-
Statistics-Data-and-Systems/Statistics-Trends-and-
Reports/Medicare-Geographic-Variation/GV_PUF.
62. United States Census Bureau. American Community
Survey. Accessed December 19, 2020. https://www.
census.gov/programs-surveys/acs.
63. Kangovi S, Mitra N, Grande D, Long JA, Asch DA.
Evidence-based community health worker pro-
gram addresses unmet social needs and generates
positive return on investment. Health Aff (Millwood)
2020;39(2):207-13.
64. Brotherton PS. Revolutionary medicine: health and
the body in post-Soviet Cuba. Durham: Duke Univer-
sity Press, 2012.
65. Williams DR, Sternthal M. Understanding racial-ethnic
disparities in health: sociological contributions. J
Health Soc Behav 2010;51(1 Suppl):S15-S27.
66. Chakraborty S, Vyse A, Coakley A. Engaging primary
care in the community management of COVID-19:
global lessons from a small town in Alberta, Canada.
Health Affairs Blog. August 28, 2020. Accessed
December 19, 2020. https://www.healthaffairs.org/
do/10.1377/hblog20200826.583052/full/.
67.Nuño-SolinísR,ShortellSM,ScheferRM,Kellogg
MA. Implementing population health in the US: les-
sons from Spain. Health Affairs Blog. July 9, 2019.
Accessed December 19, 2020. https://www.healthaf-
fairs.org/do/10.1377/hblog20190702.380604/full/.
68. Hagland M. Health policy experts: Basque healthcare
innovations offer population health lessons to U.S.
healthcare leaders. Healthcare Innovations. July 14,
2019. Accessed December 19, 2020. https://www.
hcinnovationgroup.com/population-health-manage-
ment/care-management/blog/21088376/health-policy-
experts-basque-healthcare-innovations-offer-popula-
tion-health-lessons-to-us-healthcare-leaders.
69. Polanco NT, Zabalegui IB, Irazusta IP, Solinís RN, Del
Río Cámara M. Building integrated care systems: a
case study of Bidasoa Integrated Health Organisation.
Int J Integr Care 2015;15(2):e026.
70. Alley DE, Asomugha CN, Conway PH, Sanghavi DM.
Accountable health communities—addressing social
needs through Medicare and Medicaid. N Engl J Med
2016;374(1):8-11.
71. Zack N. Applicative justice: a pragmatic empirical
approach to racial injustice. Lanham, MD: Rowman &
Littleeld,2016.
72. Richardson ET, Malik MM, Darity WA, et al. Repara-
tions for Black American descendants of persons
enslaved in the U.S. and their estimated impact on
SARS-CoV-2 transmission. medRxiv. June 5, 2020.
https://www.medrxiv.org/content/10.1101/2020.06.04.
20112011v1.
73. Bassett MT, Galea S. Reparations as a public health
priority—a strategy for ending black–white health
disparities. N Engl J Med 2020;383(22):2101-3.
218 PRIMARY CARE IN THE COVID-19 PANDEMIC
74. Darity W, Mullen AK. True reparations are a national
debt: localities and individuals should not foot the bill
and cannot build systemic remedies alone. Roosevelt
Institute. February 25, 2020. Accessed December
19, 2020. https://rooseveltinstitute.org/2020/02/25/
true-reparations-are-a-national-debt-localities-and-
individuals-should-not-foot-the-bill-and-cannot-build-
systemic-remedies-alone/.
75. Darity WJ, Mullen AK. Resurrecting the promise of
40 acres: the imperative of reparations for Black
Americans. Roosevelt Institute. June 2020. Accessed
December 19, 2020. https://rooseveltinstitute.org/
wp-content/uploads/2020/07/RI_Report_Resurrecting-
thePromiseof40Acres_202005.pdf.
76. Levien SJ, Li AW. For eighth year in a row, Harvard
fails to meet Boston PILOT Program request. The
Harvard Crimson. February 18, 2020. Accessed
December 19, 2020. https://www.thecrimson.com/
article/2020/2/18/harvard-pilot-program/.
77. American Public Health Association. Declarations of
Racism as a Public Health Issue. Accessed Decem-
ber 19, 2020. https://www.apha.org/topics-and-issues/
health-equity/racism-and-health/racism-declarations.
78. National Congress of American Indians. Health Care:
Reducing Disparities in the Federal Health Care
Budget. 2016. Accessed December 19, 2020. https://
www.ncai.org/policy-issues/tribal-governance/budget-
and-approprations/07_FY2016_Health_NCAI_Budget.
pdf.
79. Medicare-for-All Improves Health Disparities. Public
Citizen. Accessed February 2, 2021. https://www.
citizen.org/article/medicare-for-all-improves-health-
disparities/.
80. Schulte G. Two-thirds of voters support providing
Medicare to every American. Physicians for a National
Health Program. April 24, 2020. Accessed December
19, 2020. https://pnhp.org/news/two-thirds-of-voters-
support-providing-medicare-to-every-american/.
81. Kingsley GT; Urban Institute. Trends in housing prob-
lems and federal housing assistance. J Afford Hous
Community Dev Law 2018;27(1):20.
82. Warren, Pressley, Lee Introduce Legislation to Con-
front the Public Health Impacts of Structural Racism.
Elizabeth Warren. September 3, 2020. Accessed
December 19, 2020. https://www.warren.senate.gov/
newsroom/press-releases/warren-pressley-lee-intro-
duce-legislation-to-confront-the-public-health-impacts-
of-structural-racism.
83. Movement for Black Lives. The BREATHE Act. 2020.
Accessed December 19, 2020. https://breatheact.org/.
PRIMARY CARE IN THE COVID-19 PANDEMIC 219
Building Community-
Engaged Primary Care:
Returning to Our Roots
Ann Hwang
P
rimary care has long been oriented toward serving the needs of our communities, and it is
steeped in a tradition that emphasizes community participation and leadership. In the United
States, the community health center movement was birthed in the civil rights movement, at a
similarly tumultuous time in our nation’s history. Its beginnings were embedded in a broader
agenda of community action, which attacked poverty and powerlessness at the neighborhood level
and emphasized maximum participation of community members themselves.
The COVID-19 pandemic has exposed the weaknesses of the US primary care and community
health infrastructure along with our increasingly tattered social safety net. Even as we combat the
devastation wrought by COVID-19 and magnied by a shocking degree of political and operational
dysfunction, we have an obligation to plan for a better, more resilient, and more equitable future.
In this work of rebuilding, we would do well to go back to our roots of a community-oriented,
mission-driven model of care.
In this chapter, I provide a brief introduction to the recent history of primary care and patient
and community engagement in the United States, survey denitions of engagement, and suggest
opportunities for improving engagement during and after the long winter of COVID-19. I focus
in particular on the role of primary care in serving low-income populations. In this role, I argue
for expanding engagement from its current inward focus to a muscular, activist engagement that
breaches the four walls of the clinic to address the fundamental social and economic conditions that
are driving health inequities in the communities we serve.
Primary care’s strong history of community engagement
Primary care has a long and proud tradition of community orientation and of emphasizing
community participation and leadership. From its beginnings, the health center movement
incorporated a strong emphasis on community empowerment. The progenitor health center
site, the Delta Health Center, was established in Bolivar County, Mississippi, in the 1960s,
and its rst employee was Dr. John Hatch, the director of Community Health Action. Before
establishing Bolivar County as the location of the center, Dr. Hatch spent several months liv-
ing with poor families in the area and working as a farm laborer. As he put it, “Experiencing
diarrhea in a crowded rural home without toilet facilities is considerably more impressionable
than reviewing data on the high rate of intestinal disorders.”
1
The Delta Health Center’s focus went far beyond provision of clinical services. In a fore-
shadowing of many of the issues that we continue to encounter today, the center challenged
exclusionary lending practices, established a bus transportation system, addressed educational
and employment opportunities, and established a farming program to tackle one of the great-
est challenges faced by the community: widespread hunger.
2
Community empowerment and leadership was as much as—if not more than—a part of the
vision and impact of the Delta Health Center as clinical services. Structures for governance
included 10 local community health associations and the North Bolivar County Health Council,
which represented all of the local communities, developed programs, operated signicant
components of the health center program, and served as the owner, the governing body for
the health center program.
3
The health center program was established under the Oce of Economic Opportunity and
was part of the War on Poverty. As such, it had a particular focus on building power among
poor populations, urban and rural. When legislation authorizing community health centers
as a permanent program was passed in 1975, it mandated that all centers have a consumer-
majority governing board.
4
Over time, and through a number of dierent administrations,
the emphasis on community organizing, job creation, and nonhealth services has generally
waned, though some centers have been successful in maintaining a strong culture of patient
and community engagement.
5
The community-organizing aspect of the health center movement has not extensively perme-
ated primary care as a whole, with models for community leadership and ownership being the
exceptions that prove the rule. However, over the past few decades, there has been a renewed
focus on mechanisms for patient and family engagement in health care and an understand-
ing that—perhaps not surprisingly—being able to engage patients and families matters for
achieving high-quality care.
In its landmark 2001 report Crossing the Quality Chasm, the Institute of Medicine named
patient-centeredness as one of six aims for the health care system, and subsequent work
identied strategies for incorporating patient engagement in patient-centered medical home
models.
6
This priority was reected in the 2015 National Quality Strategy, which included an
emphasis on “ensuring that each person and family is engaged as partners in their care.”
7
222 PRIMARY CARE IN THE COVID-19 PANDEMIC
In recent years, a number of primary care transformation eorts, such as the Comprehensive
Primary Care Initiative and the Comprehensive Primary Care Plus program, both developed by
the Center for Medicare and Medicaid Innovation, have incorporated a focus on patient and
family engagement. The American College of Physicians issued a position paper with prin-
ciples for authentic patient and family engagement in health care.
8
And numerous organiza-
tions, including my own, have developed toolkits and best practice guides.
Despite these eorts, engagement is generally not the norm in primary care in the United
States, as suggested by data on one specic structure for engagement—the patient-family
advisory council. A review of community health centers in Arizona, California, Nevada,
and Hawaii found that 69% had advisory councils.
9
A survey of 112 patient-centered medi-
cal homes found that only 21% had a patient-family advisory council.
10
A survey of family
medicine physicians found that 24% of respondents reported that their practice had a patient
advisory council and that 19% had patient members on their board of directors.
11
Among geri-
atricians, the percentage of respondents reporting that their work site has a patient advisory
council was 28%.
12
As we shape the next chapter for primary care, we have an opportunity to go back to our roots
and to reenvision primary care, in the words of community health center founder Dr. Jack
Geiger, who recently passed away, “as an instrument of social change.”
3
This will require re-
building our focus on patient, family, and community engagement and reclaiming the potent
legacy of primary care as a contributor to a broader movement for addressing poverty, racism,
and inequity.
Dening engagement
The term engagement in health care is often used to encompass a broad set of concepts
and practices that seek to better orient care with patient, family, and community goals.
The National Academy of Medicine has dened patient- and family-engaged care as “care
planned, delivered, managed and continuously improved in active partnership with patients
and their families (or care partners as dened by the patient) to ensure integration of their
health and health care goals, preferences and values. It includes explicit and partnered de-
termination of goals and care options, and it requires ongoing assessment of the care match
with patient goals.”
13
This paradigm holds the potential to improve health and health care
outcomes by actively engaging patients and families as true partners in their care and in the
redesign of health care policies, programs, and practices.
Relatedly, in the eld of public health, community engagement has been dened as “the
process of working collaboratively with and through groups of people aliated by geographic
proximity, special interest, or similar situations to address issues aecting the wellbeing of
those people.”
14
In this chapter, I intentionally draw on engagement’s health as well as public
health lineages, as both intersect with primary care’s role in health, health promotion, and
social change.
PRIMARY CARE IN THE COVID-19 PANDEMIC 223
Strategies for fostering engagement can be grouped into those occurring at the clinical, or-
ganizational, and policymaking levels.
15
Examples of interventions to improve engagement
at the clinical level can include shared decision-making and patient goals-directed care.
Organizational-level interventions could include establishing structures for patient and com-
munity input into health system initiatives, quality improvement, and other clinic or health
system activities. In policymaking, engagement strategies include building consumer repre-
sentation in governance and oversight bodies, establishing advisory structures for consumer
input, and strengthening the voice of politically vulnerable constituencies.
At each of these levels, there can be varying degrees of engagement. Several frameworks have
worked to delineate a spectrum of engagement, including an eort by the Centers for Disease
Control and Prevention that conceptualizes community engagement as ranging from outreach
to consultation, involvement, collaboration, and shared leadership.
16
Particularly when think-
ing about engagement in programs and policy, the political science domain also provides
helpful heuristics for understanding the manifold opportunities and pitfalls for citizen par-
ticipation. Arnstein’s classic “ladder of citizen participation” groups eight degrees of par-
ticipation into categories of nonparticipation (manipulation, therapy), tokenism (informing,
consultation, placation), and citizen power (partnership, delegated power, citizen control).
17
A more recent model, the “democracy cube,” analyzes opportunities for participation along
three dimensions: who is participating, what power do participants have, and what is the
mode for decision-making.
18
These dierent frameworks are helpful to keep in mind when thinking about the dierent
dimensions of engagement. Broadly speaking, there are opportunities to increase engagement
at each of the three levels, which I address next; within those levels, there are opportunities
to deepen the degree of engagement.
Improving engagement in the clinical setting
Even as clinical care in the United States has undergone seismic changes due to COVID-19, the
need for us to engage patients and families in care has only increased. I focus on two specic
aspects of patient and family engagement in care: (1) better aligning care to patients’ goals,
values, and preferences and (2) reimagining primary care as a service, freed from the site
constraints of traditional fee-for-service billing.
Clinicians have an important role to play in ensuring that patients’ goals, values, and prefer-
ences guide the plan of care. Shifting from a disease-centered approach to a patient-goal-di-
rected approach begins with clinicians eliciting patients’ health outcome goals and care pref-
erences.
19
The importance of goal-concordant care has only been heightened by the pandemic,
with dicult decisions to make around level and setting of care, particularly given that these
decisions could mean not being able to see one’s loved ones. Resources such as the GOOD
(Goals, Options, Opinions, Documentation) framework, templates collected by the Coalition to
Advance Palliative Care COVID-19 Response Resources Hub, and the “4M” framework (what
matters, medication, mentation, and mobility) of the Age-Friendly Health Systems movement
are just a few examples of the tools that could be useful for understanding patients’ goals and
224 PRIMARY CARE IN THE COVID-19 PANDEMIC
priorities.
20,21
Throughout our clinical work, our ability to connect with and build trust with
patients and families will be critical, as information about COVID-19 prevention, testing, and
treatment continues to emerge in a highly scrutinized and politicized context.
A second opportunity for engagement comes from how COVID-19 has started to redene
what primary care actually is. While prior to COVID-19, reimbursement (and thus practice)
was driven largely by in-person visits, during the pandemic peak in the spring of 2020, the
fundamental service of primary care shifted to one of multimodal engagement (by gateway,
email, phone, and video), care coordination, and case management, with a smaller role for
traditional, in-person oce visits. Although the demise of fee-for-service medicine has been
long anticipated yet still unrealized, the glimpse of the future that COVID-19 oers sug-
gests a future state more aligned to global payment models where a primary care clinician
would have accountability for the care of a panel of patients, regardless of the site of care
and whether that care is broken out into discrete, CPT-sized chunks. In the optimistic, ideal
vision of that future, clinicians would modulate their care delivery—both the “what” and the
“how”—to what patients and families want and need, and be closely attuned to identify and
address access gaps and inequities, whether these are due to socioeconomic status, access to
necessary equipment and connectivity, disability, literacy, or medical and behavioral health
conditions. Achieving this vision, while avoiding the pitfalls of payment reform initiatives of
the past, will require the time and attention of US primary care leaders, in partnership with
patients, families, and community leaders.
Improving engagement at the organizational level
The community health center model included a formal requirement for community gover-
nance and leadership. This standard is not widely replicated in the United States outside of
community health centers, though many health care organizations do have other mechanisms
for patient, family, and community input. These structures include patient and family ad-
visory councils, participation on quality improvement teams,
22
engagement in sta training
and orientation, participation in research, and involvement in administration of community
benet programs. Across the board, structures promoting transparency, visibility, and inclu-
sion are an important component for building a culture of patient and family engagement.
When carried out deliberately and intentionally, with attention to the dynamics of power,
racism and discrimination, they can generate communication and feedback loops between
leadership, frontline clinicians, and patients, families, and community members that can
foster co-creation of a patient-centered health care system.
23,24
As primary care organizations contemplate their future, engagement becomes more important
than ever to ensure that our future system is built around the needs of the patients, families,
and communities we serve. Focus groups exploring what low-income patients want from pri-
mary care surface several consistent themes around trust, relationships, ease of access, avail-
ability of services (including nonmedical services), and responsiveness to community needs.
25,26
This ideal system is far from what exists in most places. To achieve it will require a stronger
voice for consumers and communities in creating this blueprint, and will require advocacy
PRIMARY CARE IN THE COVID-19 PANDEMIC 225
on the part of consumers, providers, payers, and policymakers alike to be successful. Within
organizations, there are opportunities to deepen engagement and move up the ladder of
engagement to truly share power and leadership. One place to start is by examining existing
engagement structures, working to reinvigorate those structures, and identifying opportuni-
ties to build new mechanisms for engagement.
Much like how the civil rights movement gave shape to the community health center move-
ment in the 1960s, the convulsions of our time call out for creative and bold approaches for
community leadership. Community-ownership models are rare but promising,
27
and em-
bolden us to reconsider whether our current business orientation in health care is the best
model for primary care moving forward. Even within more traditionally structured organiza-
tions there are powerful opportunities to grow organizations’ roles as anchors and economic
engines for their communities.
Improving engagement in policies and programs
Over the past several years, there has been an eort to build and reinvigorate community en-
gagement in the design, implementation, and oversight of health care programs and policies.
Since the 1970s, states have been required to operate advisory committees for their Medicaid
programs, though reviews of these structures suggest that a lack of resources and other
constraints limit their eectiveness.
28,29
More recently, the Financial Alignment Initiative,
which launched integrated health plans serving Medicare-Medicaid beneciaries, included
requirements for states and health plans to establish advisory structures for beneciary
input.
30,31
Medicaid accountable care organizations have also created structures for consumer
engagement,
32,33
and nonprot hospitals are required by Internal Revenue Service regulations
to obtain community input into how they deploy their community benet dollars.
34
Program enrollees have direct insight into whether a service is operating as intended and are
therefore a critical voice for troubleshooting and rapid cycle improvement. With COVID-19,
citizen participation has become more important than ever and we should seize the moment
to rebuild the conditions necessary for civic participation. This includes establishing struc-
tures for consumer input, but also supporting the infrastructure of community organizations
that focus on empowerment and civic engagement among low-income populations. Building
consumer and community input to shape Medicaid policy should be a particularly important
area of focus, given Medicaid’s critical role in serving low-income, politically vulnerable
populations and because its structure, policy, and operation can further diminish participants’
sense of political engagement and activation.
35
226 PRIMARY CARE IN THE COVID-19 PANDEMIC
Conclusions
As we continue to adapt to life with COVID-19, and simultaneously imagine what comes next,
this is the time for primary care to expand engagement from an inward focus—on improving
clinical care—to an outward one. The lives of our patients and their families take place out-
side of our walls. Even well-intentioned eorts to address social needs can fall into a “fantasy
paradigm” that presumes that short-term, targeted interventions can somehow address the
fundamental inequities that drive poor health.
36
Primary care clinicians can make common cause with consumers and community organiza-
tions working to shore up our badly eroded health and social safety net. We have both the
power of the privilege of our professional identities and the responsibility that comes with our
role in bearing witness. Although the role of advocate may feel unfamiliar to some clinicians,
professional physician organizations have endorsed physicians’ responsibility in addressing
societal needs. The American Medical Association’s Declaration of Professional Responsibilities,
passed in 2001 and rearmed in 2017, states that physicians must “advocate for the social,
economic, educational, and political changes that ameliorate suering and contribute to hu-
man well-being.” Similarly, in 2002, the American Board of Internal Medicine Foundation, in
conjunction with the American College of Physicians Foundation and the European Federation
of Internal Medicine, authored Medical Professionalism in the New Millennium: A Physician Charter.
This charter articulated a fundamental principle of social justice and armed that the “medi-
cal profession must promote justice in the health care system.”
In these times, the paradigm for engagement needs to broaden and deepen. It needs to ex-
pand its scope beyond a narrow focus on clinical care to confront the social, economic, and
environmental circumstances that indelibly shape health. Simultaneously, it needs to deepen,
to examine the uncomfortable dynamics of power and privilege, to create room for the trans-
formational work of engagement that can strengthen the very fabric of society.
COVID-19 has doubly worsened inequity in the United States, through its impacts on health
and the economy. This is a time to reexamine how primary care can draw from its history of
building empowerment and economic opportunity and reclaim our heritage as advocates. The
times that we are in call for us to partner with patients, families, and communities in a way that
is both old and new, that draws from our heritage yet pushes the frontier of what is possible.
PRIMARY CARE IN THE COVID-19 PANDEMIC 227
References
1. Hatch J. John Hatch on community organiz-
ing in the Mississippi Delta, 1965. Am J Pub-
lic Health 2014;104(11):2066-7. 10.2105/
AJPH.2014.104112066.
2. Geiger HJ. Community-oriented primary care: a
path to community development. Am J Public Health
2002;92(11):1713-6. 10.2105/ajph.92.11.1713.
3. GeigerHJ.TherstcommunityhealthcenterinMis-
sissippi: communities empowering themselves. Am
J Public Health 2016;106(10):1738-40. 10.2105/
AJPH.2016.303421.
4. Lefkowitz B. The health center story: forty
years of commitment. J Ambulatory Care Man-
age 2005;28(4):295-303.
5. HodinRM,McGafganE,DestrampeM,GreenK,
Traylor J, Pierce-Wrobel C, Zook M. Organizational-
Level Consumer Engagement: What It Takes; Case
Study: Hudson River Health Care. Center for Con-
sumer Engagement in Health Innovation and Health
Care Transformation Task Force. Accessed October
31, 2020. https://www.healthinnovation.org/consulting/
Consumer-Engagement-Case-Study_Hudson-River-
Health-Care.pdf.
6. Scholle SH, Torda P, Peikes D, Han E, Genevro J.
Engaging Patients and Families in the Medical Home.
(Prepared by Mathematica Policy Research under
Contract No. HHSA290200900019I TO2.) AHRQ Pub-
lication No. 10-0083-EF. Rockville, MD: Agency for
Healthcare Research and Quality, June 2010. https://
pcmh.ahrq.gov/sites/default/les/attachments/Engag-
ing%20Patients%20and%20Families%20in%20
the%20Medical%20Home.pdf.
7. Priorities of the National Quality Strategy. Agency
for Healthcare Research and Quality. Content last
reviewed September 2018. https://www.ahrq.gov/
research/ndings/nhqrdr/nhqdr15/priorities.html.
8. Nickel WK, Weinberger SE, Guze PA, for the Patient
Partnership in Healthcare Committee of the American
College of Physicians. Principles for patient and fam-
ily partnership in care: an American College of Physi-
cians position paper. Ann Intern Med 2018;169:796-
9. 10.7326/M18-0018.
9. Willard-Grace R, Sharma AE, Parker C, Potter MB.
Engaging patients as partners in practice improve-
ment: a survey of community health centers. J Clin
Outcomes Manag 2016;23. https://www.mdedge.com/
jcomjournal/article/146364/practice-management/
engaging-patients-partners-practice-improvement.
10. Han E, Scholle SH, Morton S, Bechtel C, Kessler
R. Survey shows that fewer than a third of patient-
centered medical home practices engage patients
in quality improvement. Health Aff (Millwood)
2013;32:368-75. 10.1377/hlthaff.2012.1183.
11. Sharma AE, Knox M, Peterson LE, Willard-Grace
R, Grumbach K, Potter MB. How is family medicine
engaging patients at the practice-level? A national
sample of family physicians. J Am Board Fam Med
2018;31:733-42. 10.3122/jabfm.2018.05.170418.
12. Hwang A, Warshaw G. Joint AGS-CCEHI survey
offers insights into patient engagement in geriatric
clinical settings. J Am Geriatr Soc. 2019;67(9):1791-4.
10.1111/jgs.16016.
13. Frampton SB, Guastello S, Hoy L, Naylor M, Sheridan
S, Johnston-Fleece M. Harnessing Evidence and
Experience to Change Culture: A Guiding Framework
for Patient and Family Engaged Care. NAM Perspec-
tives. Discussion Paper. National Academy of Medi-
cine. January 31, 2017. 10.31478/201701f.
14. Centers for Disease Control and Prevention. Prin-
ciples of community engagement. 1st ed. Atlanta, GA:
CDC/ATSDR Committee on Community Engagement,
1997.
15. Carman KL, Dardess P, Maurer M, Sofaer S, Adams
K, Bechtel C, Sweeney J. Patient and family engage-
ment: a framework for understanding the ele-
ments and developing interventions and policies.
Health Aff (Millwood) 2013;32(2):223-31. 10.1377/
hlthaff.2012.1133.
16. Centers for Disease Control and Prevention. Princi-
ples of Community Engagement. 2nd ed. June 2011.
Accessed February 3, 2021. http://www.atsdr.cdc.gov/
communityengagement/pdf/PCE_Report_508_FINAL.
pdf.
17. Arnstein S. A ladder of community participation. J Am
Institute Plann 1969;35:216-24.
18. Fung A. Varieties of participation in complex gov-
ernance. Public Adm Rev 2006;66(s1):66-75.
10.1111/j.1540-6210.2006.00667.x.
19. Tinetti ME, Naik AD, Dodson JA. Moving from
disease-centered to patient goals-directed care for
patients with multiple chronic conditions: patient
value-based care. JAMA Cardiol 2016;1(1):9-10.
10.1001/jamacardio.2015.0248.
20. Petriceks AH, Schwartz AWN. Goals of care and
COVID-19: a GOOD framework for dealing with
uncertainty. Palliat Support Care 2020;1-3. [Online
ahead of print] 10.1017/S1478951520000474.
21. COVID-19 Response Resources Hub. Center to
Advance Palliative Care. 2020. Accessed November
5, 2020. https://www.capc.org/covid-19/.
228 PRIMARY CARE IN THE COVID-19 PANDEMIC
22. Greene J, Farley D, Amy C, Hutcheson K. How patient
partnersinuencequalityimprovementefforts.Jt
Comm J Qual Patient Saf 2018;44(4):186-95.
10.1016/j.jcjq.2017.09.006.
23. Bombard Y, Baker GR, Orlando E, et al. Engag-
ing patients to improve quality of care: a systematic
review. Implement Sci 2018;13(1):98. 10.1186/
s13012-018-0784-z.
24. Person-Centered Engagement Change Package.
Center for Consumer Engagement in Health Innova-
tion and Health Care Transformation Task Force.
2020. Accessed October 31, 2020. https://www.
healthinnovation.org/change-package/introduction/
about.
25. Lewis C, Zephyrin L, Abrams MK, Seervai S. Listening
to low-income patients and their physicians (series).
Commonwealth Fund. May 15, 2019. Accessed
October 31, 2020. https://www.commonwealthfund.
org/blog/2019/listening-low-income-patients-and-their-
physicians--improving-access-and-quality.
26. Center for Consumer Engagement in Health Innova-
tion.InTheirOwnWords:Consumers’Visionfora
Person-Centered Primary Care System. Boston,
MA: Center for Consumer Engagement in Health
Innovation, 2019. https://www.healthinnovation.org/
resources/publications/in-their-words-consumers-
vision-for-a-person-centered-primary-care-system.
27. Eby DK. Customer ownership in equity-oriented health
care. Milbank Q 2018;96(4):672-4. 10.1111/1468-
0009.12350.
28. Davidson SM, Herold TE, Simon MB. The Medical
Care Advisory Committee for state Medicaid pro-
grams: current status and trends. Health Care Financ
Rev 1984;5(3):89-98.
29. Ciesla JR, Samuels ME, Stoskopf CH. The role of
the Medical Care Advisory Committee in the admin-
istration of state Medicaid programs. A twenty-year
perspective. Eval Health Prof 1992;15(3):282-98.
10.1177/016327879201500302.
30. Center for Consumer Engagement in Health Innova-
tion; LeadingAge LTSS Center @ UMass Boston.
The One Care Implementation Council: Stakeholder
Engagement Within a Duals Demonstration Initiative.
Community Catalyst. June 2018. Accessed February
3, 2021. https://www.healthinnovation.org/resources/
publications/body/One-Care-Implementation-Council-
Review-June-2018-1.pdf.
31. Isaacson R, Sharma L, Cohen M, Hodin RM. “The
Biggest Value Is Getting the Voice of the Member”:
An Exploration of Consumer Advisory Councils Within
Medicare-Medicaid Plans Participating in the Financial
Alignment Initiative. Center for Consumer Engage-
ment in Health Innovation. January 2019. Accessed
February 3, 2021. https://www.healthinnovation.org/
resources/publications/an-exploration-of-consumer-
advisory-councils-within-medicare-medicaid-plans.
32. Hodin RM, Tallant M. Supporting Meaningful Engage-
ment Through Community Advisory Councils: Lessons
From the Oregon Health Authority. Milbank Memo-
rial Fund and Community Catalyst. August 12, 2020.
Accessed February 3, 2021. https://www.milbank.
org/publications/supporting-meaningful-engagement-
through-community-advisory-councils/.
33. Wiitala K, Metzger MA, Hwang A. Consumer Engage-
ment in Medicaid Accountable Care Organizations:
A Review of Practices in Six States. Community
Catalyst. September 2016. Accessed February 3,
2021. https://www.communitycatalyst.org/resources/
publications/document/ConsumerEngagementMedic-
aidACOs.pdf?1474915709.
34. Internal Revenue Service. Community Health Needs
Assessment (CHNA)—Section 501(r)(3). Accessed
February 3, 2021. https://www.irs.gov/charities-non-
prots/community-health-needs-assessment-for-chari-
table-hospital-organizations-section-501r3.
35. Michener J. Fragmented democracy: Medicaid, feder-
alism, and unequal politics. Cambridge, UK: Cam-
bridge University Press; 2018.
36. Scott-Samuel A, Smith K. Fantasy paradigms of
health inequalities: utopian thinking? Soc Theory
Health 2015;13:418-36. 10.1057/sth.2015.12.
PRIMARY CARE IN THE COVID-19 PANDEMIC 229
Integration of Primary
Care and Oral Health
Hugh Silk
P
rimary care, like the rest of medicine, has been signicantly challenged during the COVID-19
pandemic. Especially in the beginning, the public was reluctant to visit emergency rooms and
hospitals, while other medical care sites such as urgent care and specialty oces were often closed
or limited in hours. Emergency departments saw 40% fewer patients during the early months of
COVID-19.
1
Although primary care dipped in in-person visits, telemedicine visits rebounded very
quickly.
2
Even as oces remained at lower overall volume, the calls for reassurance and health
inquiries continued to pour in.
3
Patients knew they could get answers from their primary care
providers (PCPs). Patients called about every topic, and if they could not contact a specialist, they
called their PCP. In some cases, primary care oces were initiating the calls to check on patients.
The Primary Care Collaborative surveyed PCPs and patients throughout the spring and conrmed
this special long-term relationship played an important role during the pandemic.
4
One of the
important conclusions of the surveys showed that more than 70% of respondents reported having
a usual source of care and a “doctor they can trust,” and two-thirds felt their “doctor helps them
make sense of what’s going on with them.”
During COVID-19, many calls and visits to PCPs included oral health issues. PCPs are not well
trained in dealing with oral health issues, and yet Ian McWhinney, the grandfather of family medi-
cine in Canada, said that a good generalist is a “manager of resources.”
5
This is especially true
during crises and accurately denes the role of primary care during the pandemic with all the many
uncertainties it has brought.
Dr. Lisa Simon outlined in an earlier chapter the historical context for medical-dental disintegra-
tion, including a reliance of patients on the emergency room for urgent dental care needs. She
also explained that much more of the population visits a PCP than a dental provider. Finally, she
outlined how the dental industry is returning to its former routine of seeing patients, and
yet many aspects of the dental public health force (e.g., school-based health) continue to be
devastated by the pandemic. All of this puts the country at risk for maintaining the same level
of disparities currently present in the US oral health system. Dr. Caswell Evans et al., in an
earlier chapter, delved further into the details of these inequities, clarifying that the majority
of preventive care is provided to those who need it the least, resulting in a great deal of acute
care being needed by those from lower socioeconomic backgrounds. The authors outlined
the complexity of the problem, from inadequate public dental coverage and access issues, to
providers who are not well educated in social determinants of health and the need for dras-
tic change in delivery of care, including diverse locations, expansion of providers, and more
noninvasive care. These collective conclusions highlight a new focus on the role of PCPs in
the ght for better oral health across the United States during and post-pandemic, especially
in populations that are experiencing health inequities. In this chapter, I look closer at this
emerging and evolving role for primary care and the essential need for an improved relation-
ship between dental and medical systems and providers to nally address these care gaps.
Bridging the historical medical-dental disconnect
Prior to the pandemic, medical and dental care professionals operated mainly in their silos.
This issue of separation between medical and dental services contributes to health dispari-
ties; those who are isolated within the health care system are also usually isolated in the
oral health system and often have to navigate it for themselves. This is due to both societal
bias and racial injustice, as well as institutional bias and unfairness in the health care infra-
structure and systems. However, there are impressive examples of early adopters
who have
developed eective models of medical-dental integration that oer hope for addressing these
inequities.
6
Their work has overcome a system of two dierent health insurance systems,
dierent oces, and—unlike collaboration between the specialties of medicine—limited
communication and coordination.
7
For those health systems that are working in this sphere,
the Substance Abuse and Mental Health Services Administration and Health Resources and
Services Administration’s six-level framework of “coordinated, co-located, integrated” is a
model that many are embracing.
8
In Massachusetts, the MassHealth accountable care organi-
zation (ACO) model has ve levels along the spectrum of integration, evolving from a formal
referral process to full integration.
9
Examples of success include a range of possibilities, from
integrating a dental hygienist into primary care to sharing electronic health records.
10,11
Eorts to date fall into categories that mimic the levels of coordination just mentioned. On
the most basic level, having PCPs actually take notice of the importance of oral health and
begin to address it in their oce with oral exams, dental hygiene advice, and uoride varnish
application is an essential rst step. Medical providers’ lack of interest in oral health is often
a result of their education, with many not being trained in oral health concepts at the under-
graduate and graduate levels.
12-17
The most famous and comprehensive example of PCPs changing their style of practice is in
North Carolina with the Into the Mouths of Babes initiative. Thousands of PCPs have been
232 PRIMARY CARE IN THE COVID-19 PANDEMIC
trained in dental care, resulting in hundreds of thousands of oral health interventions in
medical oces and ultimately leading to a statistically signicant reduction in caries for the
children of North Carolina.
18,19
This approach includes training PCPs to assess risk, provide
caregiver education, and apply uoride varnish to young children. This requires altering oce
ow and ensuring reimbursement. The results include a 20% reduction in caries, including
a reduction in the gap in disease prevalence between those from higher and lower incomes.
Many other states, like Ohio and Iowa, have similar initiatives that focus on the role of the
PCP in addressing oral health in their oces.
20,21
These are important rst steps to addressing
equity, as prevention is extended to more children from dierent backgrounds who otherwise
would go without dental preventive services. Yet, these eorts alone do not address access to
the dental oce. Although these eorts encourage dental referrals, other projects have of-
fered more focus on the dental referral from the primary care setting.
With more children visiting a PCP than a dental provider, the coordinated dental referral from
the primary care oce has the potential to be a game changer for initiating access. A North
Carolina study demonstrated that children who are referred to dentists by primary care pro-
viders are three times more likely to actually see a dentist.
22
Of course, there are many other
aspects that need to be addressed, as outlined by Evans et al., including insurance coverage,
societal change, and dental provider attitudes.
Although work continues on these enormous issues, we also need to improve the process for
the pipeline of referrals to dental care providers. The Health Policy Institute at the American
Dental Association has shown that physicians are frustrated with the current system for
dental referrals. It lacks the ease with which physicians are used to making referrals to other
specialists.
23
Concerted eorts backed by grant funding have helped some health centers to
overcome this. According to a systematic review of referral rates from primary care to sec-
ondary specialists, conducted by the Cochrane Database, this is what is needed: active local
educational interventions that involve the secondary care specialists, coupled with structured
referral templates.
24
DentaQuest’s Medical-Oral Expanded Care (MORE) initiative has focused
on this referral process.
25
They have worked with rural agencies in South Carolina, Colorado,
and Pennsylvania to improve referrals. One technique they have used is to employ community
dental health coordinators, who can help with unique, local logistics.
26
Bringing these two types of initiatives together, PCP oral health awareness and better dental
referral systems, is a comprehensive strategy for addressing oral health in the PCP oce and
getting patients to the dental setting in a timely and systematic manner. Qualis Health, in its
document Organized, Evidence-Based Care: Oral Health Integration, outlined a clear process for
improving workow in the oce and systemizing referrals as part of the after-visit process.
27
The authors described the barriers, drivers, and roles for each member of the team with the
mantra “Ask, Look, Decide, Act, Document.” Qualis has worked with sites from Washington
to Kansas and from Massachusetts to Kentucky. It has documented the success and barri-
ers.
28
In another example, Harborview Medical Center in Seattle implemented change and
then over two years was able to measure an improvement from zero obstetrical patients being
referred to the dentist to an increase of 50% of patients being referred. Another example is
the Bluegrass Community Health Center (BCHC) in Lexington, Kentucky, which has a protocol
PRIMARY CARE IN THE COVID-19 PANDEMIC 233
for assessment and referrals. BCHC uses its electronic health records (EHR) to close the loop,
checking whether patients followed through on a referral when they attend their next PCP
visit. What BCHC lacks is the next level of integration of a shared EHR to avoid the work-
arounds that so many are forced to use to see if the patient attended the dental visit and what
the outcomes were.
The organization on the forefront of medical-dental integration is Marsheld Clinic in
Wisconsin. All providers have access to the same information in a shared EHR, thereby reduc-
ing the need to contact PCPs to check on medication lists or test results on the dental side;
and medical clinicians know when their patients have been seen in a dental oce and what
was done.
29
Furthermore, the system can run data on groups of patients, such as those with
diabetes, and nd out who has been seen in the past 12 months. They can then reach out to
patients who need a dental visit.
30
This shared use of the EHR moves PCPs from addressing
oral health and making referrals from their silo into a sphere of working together virtually.
This is yet another step in the direction of improving inequities through improved communi-
cation and reduction in ineciencies of care. This is particularly important for those popula-
tions that heretofore have been lost to follow-up, misplaced in the system, or never engaged in
the rst place. This powerful tool of a shared EHR has the potential to oer all patients the same
reminders, follow-up, and notices of missed care that systems with no communication lack.
The highest levels of coordinated care include colocation and full integration. Many Federally
Qualied Health Centers (FQHCs) have medical and dental practices colocated. This can be
ideal for integration; however, it is not very useful if the two departments are not commu-
nicating, planning, and referring to one another in a coordinated manner. In other words,
colocation alone does not result in integrated care.
31
Two examples of fully coordinated care
come from opposite sides of the country. The Dimock Center in Boston, Massachusetts, has
a system for screening children, referring them, and checking on referrals through a shared
EHR via eClinicalWorks.
32
This coordinated eort has seen an increase from zero screenings
and uoride varnish applications to 80% of patients receiving these services, and 35% of
patients getting to the dentist. Meanwhile, Terry Reilly Health Services in Boise, Idaho, has
added all of this as well as checklists for integration and case conferences.
33
The clinic does
this with behavioral health as part of the team. Coming together to discuss specic patients
as a team is a high-level process of organized care that has the potential to oer very person-
alized care to patients in need. To succeed, the process took a lot of organization, champions,
and analysis of the process followed by incremental changes. This level of coordinated care
requires leadership, buy-in at all levels, and systems in place to make it easy for the busy cli-
nicians and their auxiliary sta to complete the process. Yet, this is what is needed if we are
going to oer eective care to vulnerable populations; this is what health equity looks like. It
is challenging; it requires up-front planning and nancing; and in the end, it saves lives and
money when wellness is improved through fair and ecient systems.
Clearly these health centers, systems, and case examples give hope for the future. These early
adopters have worked through the barriers and studied what works. Their results are well
documented, as are the steps they took. We need to consider how the pandemic aects these
234 PRIMARY CARE IN THE COVID-19 PANDEMIC
levels of integrated care oerings and how a crisis like the pandemic might ultimately push
coordinated care to a new level.
Oral health during the pandemic and the role of primary care
Simon and Evans et al., and others in this eld, have presented the fact that there are egre-
gious rates of disparities in oral health care in the United States, with Latino and Black
populations, as well as poor or less educated patients, experiencing more dental caries and
less access to formal dental care.
34,35
With even less access during the pandemic, the dispari-
ties naturally widened.
36,37
Society will need momentous changes to rectify this situation;
disparities have many roots and are centuries in the making. Dental education and practice,
including reimbursement structures and professional development, will also need signi-
cant improvements that specically teach about racial injustice and health eects. The fear
is that oral health inequity will continue post-COVID-19 due to dentists working down a
backlog of preventive care for those who already have teeth without issues—mainly those
who have dental insurance, are nancially stable, and, in many cases, are white. Couple this
with the fact that due to protocols during the pandemic to keep dental sta and patients
safe, more than half of all dental practices are still operating at a lower volume than usual.
38
Furthermore, many of the people who need dental care the most were more likely to lose their
jobs during the pandemic and therefore may be without the dental coverage they once had.
This means less preventive care and management of early disease. The oral health care sys-
tem will require creative changes to overcome this combination of hurdles. However, Simon
reported that dental care is trending back to the same old system of overcaring for those
who need care the least and using the same oce-based approach that is focused on highly
technical invasive care. The creativity may need to come from primary care providers, who
will need to evolve to be more active team players in addressing oral health and the disparities
that exist in rates of disease and access to prevention and management.
Despite the examples showcased in this chapter, the vast majority of medical oces were
not ready for the dental issues that have come during the pandemic. Studies have shown that
practicing physicians do not have the knowledge and skill to address emergent oral health
issues and have not fully embraced setting up their practices to screen and educate on this
topic.
39-41
Where does this deciency stem from? One factor is lack of oral health training in
medical schools and residency programs, which we have noted. Even when there is inter-
professional education, a meta-analysis shows that dentistry is often not included.
42
Another
factor is the way our system incentivizes care with fee-for-service. In addition, the pandemic
showed how little dental and medical practices were prepared to coordinate care even on the
most basic level. Dentists in parts of the country oered their medical colleagues PPE;
43,44
however, there was no plan to resupply dental oces later in the pandemic when dentists
returned to work.
45
This is an example of the lack of coordination needed among all health
providers during the pandemic. Furthermore, medical professionals did not coordinate to
assist their dental counterparts with COVID-19 testing for high-risk patients and high-risk
procedures. If anything, dental facilities stepped up to run some of the COVID-19 testing in
parts of the country,
46
but again as testers and leaders of the care, not as coordinators to bring
PRIMARY CARE IN THE COVID-19 PANDEMIC 235
the two systems together. Clearly, there is room to work together to avoid redundancies,
improve safety, and ensure high-quality care during and after the pandemic.
The future promise and pathway
Primary care can help revolutionize how we decrease oral health disparities in the United
States; however, we will need more oral health education in health schools, continuing edu-
cation, and incentives for medical providers to address dental issues in the oce and work
closer with their dental colleagues. We don’t have to reinvent the wheel, as there are already
many evidence-based curricula and practice-based models available.
27,47-49
Smiles for Life
and the American Academy of Pediatrics PACT program are two curricula that have proven
success. We know that eorts to integrate oral health into health care education programs
in the United States continue through organizations such as Oral Health Nursing Education
and Practice and the National Interprofessional Initiative on Oral Health.
50,51
The Center for
Integration of Primary Care and Oral Health has recently initiated an ambitious goal of cre-
ating 50 state oral health education champions and engaging every health program in the
country to teach oral health through their One Hundred Million Mouths campaign.
52
There is a strong need for spreading and scaling up in the clinical setting the implementation
of the workow models mentioned earlier. What has been achieved to date is mostly from
grant-funded projects, proving that the integration of oral health into primary care with den-
tal collaboration is helpful. The next step is to move beyond grant-funded projects and evolve
the medical-dental integration into a normal partnership of how we oer comprehensive
health care. This will require proper reimbursement, EHR coordination, and likely training
that assumes that medical and dental providers are meant to be teammates, much in the same
way that other specialists and providers, from podiatrists to pharmacists, have been part of
the teaching of interprofessional education and practice modeling.
The best pathway forward for medical-dental integration in terms of reimbursement in-
cludes ACOs and value-based care (VBC). As outlined in other chapters, ACO models and other
insurer-based studies in the United States have already shown that medical-dental integra-
tion saves money and improves outcomes.
53-55
Disparities have the greatest opportunity in
health care to be rooted out when people have access. In VBC and ACOs, the goal is overall
wellness, which means preventing disease and promoting wellness so that a patient does not
overutilize the health system. This involves providing care where people already tend to visit.
Currently, one-third of people in the United States, or approximately 110 million people, do
not visit the dentist annually.
56
This number increases to 45% for the Black and Latino popu-
lation. Meanwhile, 75% of people identify as having a primary care provider, resulting in 300
million visits a year to primary care oces.
57,58
If we capitalize on this in an ACO model, we
could oer preventive oral care in the medical oce. Of course, there are patients who visit
the dentist more than they visit their physician, and for that reason we should also explore
administering vaccines and blood pressure checks in the dental setting.
Dentistry is likely concerned about PCPs oering oral health care in their oces. Primary care
providers will never provide full dental treatments in their oce, however, just as they do not
236 PRIMARY CARE IN THE COVID-19 PANDEMIC
oer full surgical services in their oce. Nevertheless, PCPs do oer ways to prevent surgery
(e.g., weight loss counseling, joint injections) and oer less-invasive oce-based surgery
(e.g., mole excision, lipoma removal) when appropriate. The comparison to dental services
would be to oer prevention in the form of oral hygiene counseling, oral exams, uoride
varnish, and dental referrals, much like the early adopters are doing. The pandemic has
shown that noninvasive oral health services are on the rise and oer legitimate quality dental
care. Some are advocating for this as a permanent change.
59
The future will see an increase
in caries treatment with silver diamine uoride (SDF), a liquid painted onto asymptomatic
caries in their early stages to arrest the further development of the caries process.
60
Training
to implement SDF is not challenging, and it has already had limited success in the primary
care setting and is being further studied.
61,62
Other noninvasive dental care techiques such
as atraumatic restorative treatments are being encouraged during the pandemic and have
been used for years in the United States and globally. This technique avoids the need for local
anesthetic and the use of a drill. Again, with proper training, this treatment has been used
in primary care settings in other countries and could provide options for certain geographic
locations in the United States where access to dentistry is a challenge.
63,64
In some settings, models could include even more creative care. A practice change model that
has developed over the past few years includes deploying a dental hygienist into the medi-
cal setting or a nurse practitioner into the dental setting. This allows for cross-pollination of
ideas and care. This is not needed, nor could it practically be implemented, in every medical
setting. Some medical and dental practices are already colocated in the same building or quite
close to one another. Others are already working together through shared EHRs or coordi-
nated care. Many oces would be too small to generate enough work for this level of care. So,
having a dental or medical representative in the oce is not practical for all situations. For
others, this model can lead to improved care and warm handos to the main dental or medi-
cal oce of the transplanted provider.
In Colorado, dental hygienists are being placed in rural medical settings across the state. This
has resulted in a decrease in caries prevalence in the cohort studied.
65
The Harvard School of
Dental Medicine has had success with incorporating a nurse practitioner into the dental set-
ting.
66
The team has noted addressing more general health issues that were previously being
missed. What is needed in many settings are virtual versions of these models, with teleden-
tistry and telemedicine for medical and dental providers, respectively. A synchronous and
asynchronous opportunity for consults similar to what the Extension for Community Health
Outcomes (ECHO) system does for hepatitis C and other health issues
67
is a model that might
work for smaller oces or rural settings that cannot attract or utilize a full-time advanced
practitioner from another discipline.
The important outcome in all of these models is accessibility for all. Since African American
and Latino patients, as well as other people who have been marginalized in the dental care
system, such as veterans, those with disabilities, and LGBTQ patients, are in their PCP’s oce
more than the dental setting, each person could be getting the preventive management in the
setting they are in. There is no reason dental advice and basic care should be contained to the
dental setting; this approach is contributing to health inequities. For that matter, we need
PRIMARY CARE IN THE COVID-19 PANDEMIC 237
to get outside of formal primary care settings as well, following the lead of current models
of school health, Head Start, and the Special Supplemental Nutrition Program for Women,
Infants, and Children (WIC), as well as care mobiles, all of which are also oering oral health
promotion and disease prevention. Delivering health care in diverse settings levels the playing
eld; people work, they go to school, they go to church—they are busy. Care can be oered in
these alternate settings. The key is coordinating what is done so that we avoid overtreatment,
overtesting, and complaints from patients and providers about the discoordination of eorts. Of
course, setting standards of care is also a prime consideration to ensure safety and high quality.
The National Academy of Medicine, in its document Integration of Oral Health and Primary Care:
Communication, Coordination, and Referral, stresses the importance of communication through
technology.
68
Sharing an electronic health record is the gold standard and is the pathway
to coordinated care that avoids duplication. Companies such as Epic have created the Epic
Wisdom module to help medical and dental practitioners work together.
69
Marsheld Clinic in
Wisconsin and eClinicalWorks are expanding their role in this space. They have proven that
a shared EHR makes it easier to create referrals and search for patients with certain condi-
tions that make them higher risk for poor dental health, which aects medical outcomes.
Physicians can then contact those patients if their dental follow-up has lapsed.
70
This type
of application has the opportunity to improve equity through better reminders and eventu-
ally access to dental care. We need to go further to include cloud-based sharing of oral care
management to communicate across EHR platforms, health care settings, and nontraditional
health settings. Other countries and many states are storing health data within a microchip
on a plastic pocket-sized card, on a smart device, or in personalized cloud platforms. Medical
record portals are helping with this evolution, but we need to have a portal for all health care,
not just hospital-system-based care.
Barriers to transformation
The fear is that we are trending back to old models as the pandemic wears on and we will let
this opportunity to improve care, outcomes, and disparities slip away. Telemedicine, for ex-
ample, has improved access for patients whose lives are more challenging or who lack trans-
portation. I can attest that I have had an easier time having virtual visits with patients who
were previously experiencing challenges getting to the oce. This included those with dental
issues who suered during the pandemic and could not see a dentist due to limited access. If
telemedicine is not continued as a billable service, this will aect equity eorts for all aspects
of health access in the primary care setting, including access to acute oral health care. We
need to not only preserve telemedicine and teledentistry, but also take it in new directions.
Time and a lack of reimbursement are perennial barriers for many changes in health care.
However, immunizations are a great model for quality improvement. They work because they
have been folded into oce workow and they are reimbursed. Some practices have used
this model to implement uoride varnish applications for pediatric patients in primary care.
States that reimburse PCPs for oral health services such as varnish and risk assessments
have been shown to now have children with signicantly greater odds of having very good or
238 PRIMARY CARE IN THE COVID-19 PANDEMIC
excellent teeth compared to states that do not reimburse.
71
Protocols have been designed for
improving oce workow for oral health services; we simply need to scale and implement
them. Current incentives have engaged the early adopters but are not enough for the bulk of
practices. ACOs and VBC models are one answer; quality markers and other reimbursement
changes might be another. This type of work also depends on champions. Champions are not
born, they are made. This will require investment in leadership from government and non-
governmental sources of funding. It will also take creative social marketing; interventions like
uoride varnish will have to be promoted as the “vaccine of the mouth,” for example.
Not all patients facing disparities are seen in their PCP’s oce, hence the need for care in
the community as well. Just as dental oces need to have more dental care extenders in the
community, PCPs also need to work with health care extenders. It is a barrier to expect every-
one to come to our oces. Community health workers (CHWs) can do assessments and give
advice, school nurses can apply uoride varnish, and visiting nurses can assure that patients
who are homebound are practicing good oral hygiene. We need to change our mindset or risk
contributing to the present disparities. The status quo is not a plan nor a solution, as stagna-
tion will also leave many practitioners without patients in their oces as society and health
delivery evolves. We have already seen this with urgent care settings drawing patients away.
Visits to primary care oces were down 18% before the pandemic.
72
So extending care beyond
our oces is the new reality. Dentists are facing the same challenge, and dental therapists are
part of a newer discipline that will allow dentists to achieve this goal if the collaboration is
embraced. For primary care, our extension may come through CHWs (who now have a train-
ing designated for them on Smiles for Life)
47
and the use of nurse practitioners and physician
assistants, who have seen a 129% increase in visits during the same time that primary care
was losing visits.
72
Finally, we often lack creativity in the health system. We are hemmed in by embracing the
status quo and rules meant to protect the public from unsafe care. We cling to a system that
often focuses on prot over care for the vulnerable and an emphasis on avoiding malprac-
tice. All of these factors have merit and lead to stagnation. At the very least we need to make
changes to be better prepared to face another pandemic or equivalent. This includes evolving
our system so that medical and dental professionals can work together to use the same cen-
tralized screening systems for viral testing so that both medical and dental oces can be safe
and accessible to patients. We need to have dental oces work with medical oces so they
can help patients get emergency access. We need to allow dentists access to medical settings
that have negative pressure rooms so that emergent care can be conducted. This takes or-
ganization at the state level of professional organizations and an acceptance that the greater
good for the public is working together and letting former rules and guidelines be rewritten or
relaxed in crisis situations. We saw this creative approach during the pandemic at times (e.g.,
reimbursing for telemedicine conducted by phone calls) and we will need more of this. After
the pandemic will be the time to prepare for the next disaster, not waiting and relearning our
lessons again when a new national or global crisis occurs.
However, our evolution of medical-dental integration is not just about preparing for a fu-
ture crisis like a pandemic. It needs to be about facing the current and long-standing crisis
PRIMARY CARE IN THE COVID-19 PANDEMIC 239
of health and social inequity. This is our chance to work together to overcome the biggest
problem in our country. We have to avoid the urge to compete with one another for providing
oral health services and aim to oer appropriate, timely service in the best setting for each
patient to maximize outcomes and wellness. There are approximately 150,000 general and
pediatric dentists in the United States, while there are approximately 335,000 PCPs (includ-
ing MDs, DOs, NPs, and PAs, not to mention thousands more CHWs and personnel in schools,
Head Start programs, WIC, community centers, and more. Clearly, access to basic oral health
services is more practically achieved through care in other settings. The biggest barrier is
the limitation of our imagination, morality, and desire for a better system and outcomes that
serve all in an equitable manner.
References
1. Hartnett KP, Kite-Powell A, DeVies J, et al. Impact of
the COVID-19 pandemic on emergency department
visits—United States, January 1, 2019–May 30, 2020.
MMWR Morb Mortal Wkly Rep 2020;69(23):699-704.
10.15585/mmwr.mm6923e1.
2. Mehrotra A, Chernew M, Linetsky D, Hatch H, Cutler
D. The impact of the COVID-19 pandemic on outpa-
tient visits: a rebound emerges. Commonwealth Fund.
May 19, 2020. Accessed January 15, 2021. https://
www.commonwealthfund.org/publications/2020/apr/
impact-covid-19-outpatient-visits.
3. DeVoe JE, Cheng A, Krist A. Regional strategies
for academic health centers to support primary care
during the COVID-19 pandemic: a plea from the front
lines. JAMA Health Forum. April 8, 2020. Accessed
January 15, 2021. https://jamanetwork.com/channels/
health-forum/fullarticle/2764405.
4. Primary care & COVID-19: week 11 surveys. Primary
Care Collaborative. May 27, 2020. Accessed January
15, 2021. https://www.pcpcc.org/2020/05/26/primary-
care-covid-19-week-11-surveys.
5. McWhinney IR. Teaching the principles of family medi-
cine. Can Fam Physician 1981;27:801-4.
6. Powers B, Donoff B, Jain SH. Bridging the dental
divide: overcoming barriers to integrating oral health
and primary care. Health Affairs Blog. January 19,
2017. Accessed January 15, 2021. https://www.
healthaffairs.org/do/10.1377/hblog20170119.058211/
full/.
7. Simon L. Overcoming historical separation between
oral and general health care: interprofessional col-
laboration for promoting health equity. AMA J Ethics
2016;18(9):941-9. 10.1001/journalofethics.2016.18.9.
pfor1-1609.
8. Standard framework for levels of integrated care.
Center of Excellence for Integrated Health Solu-
tions. January 1, 2020. Accessed January 15, 2021.
https://www.thenationalcouncil.org/wp-content/
uploads/2020/01/CIHS_Framework_Final_charts.
pdf?daf=375ateTbd56.
9. Oral health integration for MassHealth ACOs. MA
DSRIP TA Marketplace. Accessed January 15,
2021. https://www.ma-dsrip-ta.com/wp-content/
uploads/2020/09/Oral-Health-FAQ-Factsheet.pdf.
10. Braun PA, Cusick A. Collaboration between medical
providers and dental hygienists in pediatric health
care. J Evid Based Dent Pract 2016;16 Suppl:59-67.
10.1016/j.jebdp.2016.01.017.
240 PRIMARY CARE IN THE COVID-19 PANDEMIC
11. MacNeil RLM, Hilario H, Ryan MM, Glurich I, Nycz
GR, Acharya A. The case for integrated oral and
primarymedicalhealthcaredelivery:MarsheldClinic
Health System. J Dent Educ 2020;84(8):924-31.
10.1002/jdd.12289.
12. Dalal M, Savageau JA, Silk H, Isong I. Oral health
training in pediatric residency programs: pediat-
ric program director perspectives. J Dent Educ
2019;83(6):630-7. 10.21815/JDE.019.058.
13. Thompson L, Jiang T, Savageau JA, Silk H, Riedy CA.
An assessment of oral health training among geriatric
fellowship programs: a national survey. J Am Geriatr
Soc 2019;67(5):1079-84. 10.1111/jgs.15755.
14. Simon L, Silk H, Savageau JA, Sullivan K, Riedy CA.
Oral health training in osteopathic medical schools:
results of a national survey. J Am Osteopath Assoc
2018;118(7):463-71. 10.7556/jaoa.2018.100.
15. Silk H, Savageau JA, Sullivan K, Sawosik G, Wang M.
An update of oral health curricula in US family medi-
cine residency programs. Fam Med 2018;50(6):437-
43. 10.22454/FamMed.2018.372427.
16. Ticku S, Savageau JA, Harvan RA, et al. Primary
care and oral health integration: comparing training
across disciplines. J Health Care Poor Underserved
2020;31(4):344-59. 10.1353/hpu.2020.0158.
17. Ferullo A, Silk H, Savageau JA. Teach-
ing oral health education in U.S. medical and
osteopathic schools: results of a national sur-
vey. Acad Med 2011;86(2):226-30. 10.1097/
ACM.0b013e3182045a51.
18.AchembongLN,KranzAM,RozierRG.Ofce-based
preventive dental program and statewide trends
in dental caries. Pediatrics 2014;133(4):e827-34.
10.1542/peds.2013-2561.
19. Kranz AM, Preisser JS, Rozier RG. Effects of physi-
cian-based preventive oral health services on dental
caries. Pediatrics 2015;136(1):107-14. 10.1542/
peds.2014-2775.
20. What is I-Smile? Iowa Department of Public Health.
Accessed January 15, 2021. https://ismile.idph.iowa.
gov/About-ISmile.
21.MOCuoridevarnishproject.OhioAssociationof
Community Health Centers. Accessed January 15,
2021. https://www.ohiochc.org/page/MOC.
22.PahelBT.Referralsfordentalcareinmedicalofce-
based preventive dental program. University of North
Carolina School of Public Health. 2008. Accessed
January 15, 2021. https://core.ac.uk/download/
pdf/210605076.pdf.
23.MiloroMB,VujicicM.Physiciansdissatisedwith
current referral process to dentists. ADA Health Policy
Institute. March 2016. Accessed January 15, 2021.
http://www.ada.org/~/media/ADA/Science%20and%20
Research/HPI/Files/HPIBrief_0316_5.pdf.
24. Akbari A, Mayhew A, Al-Alawi MA, et al. Interven-
tions to improve outpatient referrals from primary
care to secondary care. Cochrane Database Syst
Rev 2008;2008(4):CD005471. 10.1002/14651858.
CD005471.pub2.
25. MORE Care: the interprofessional oral health referral.
DentaQuest Partnership for Oral Health Advance-
ment. October 2019. Accessed January 15, 2021.
https://www.dentaquestpartnership.org/sites/default/
les/InterprofessionalNetworkReferralProcess_FINAL.
pdf.
26. Boynes SG, Davis L, Adams G, Mills M, Deutchman
M. MORE Care: narrowing the rural interprofessional
oral health care gap. DentaQuest Partnership for
Oral Health Advancement. January 2019. 10.35565/
dqp00002.
27. Organized, evidence-based care: oral health integra-
tion. Safety Net Medical Home Initiative. October
2016. Accessed January 15, 2021. http://www.safe-
tynetmedicalhome.org/sites/default/les/Guide-Oral-
Health-Integration.pdf.
28. Oral health: an essential component of primary care.
Safety Net Medical Home Initiative. Accessed January
15, 2021. http://www.safetynetmedicalhome.org/sites/
default/les/Case-Example-Oral-Health-Integration-
Referral.pdf.
29.AcharyaA.Marsheldclinichealthsystem:integrated
care case study. J Calif Dent Assoc 2016;44(3):177-
81.
30. Acharya A, Cheng B, Koralkar R, et al. Screening
for diabetes risk using integrated dental and medical
electronic health record data. JDR Clin Trans Res
2018;3(2):188-94. 10.1177/2380084418759496.
31. Pourat N, Martinez AE, Haley LA, Crall JJ. Colo-
cation does not equal integration: identifying and
measuring best practices in primary care integration
ofchildren’soralhealthservicesinhealthcenters.J
Evid Based Dent Prac 2020;20(4):101469. 10.1016/j.
jebdp.2020.101469.
32. Sengupta N, Nanavati S, Cericola M, Simon L. Oral
health integration into a pediatric practice and coor-
dination of referrals to a colocated dental home at a
federallyqualiedhealthcenter.AmJPublicHealth
2017;107(10):1627-9. 10.2105/AJPH.2017.303984.
PRIMARY CARE IN THE COVID-19 PANDEMIC 241
33. Pace KB. Integration of medical and dental ser-
vices: case study of the Terry Reilly Health Services
Latah Clinic experience. Boise State University.
June 13, 2017. Accessed January 15, 2021. https://
scholarworks.boisestate.edu/cgi/viewcontent.
cgi?article=2394&context=td.
34. Disparities in oral health. Centers for Disease Control
and Prevention. Accessed January 15, 2021. https://
www.cdc.gov/oralhealth/oral_health_disparities/index.
htm.
35. Koppelman J, Cohen RS. Dental health is worse in
communities of color. PEW. May 12, 2016. Accessed
January 15, 2021. https://www.pewtrusts.org/en/
research-and-analysis/articles/2016/05/12/dental-
health-is-worse-in-communities-of-color.
36. Kalash DA. How COVID-19 deepens child oral health
inequities. J Am Dent Assoc 2020;151(9):643-5.
10.1016/j.adaj.2020.05.015.
37. Brian Z, Weintraub JA. Oral health and COVID-19:
increasing the need for prevention and access. Prev
Chronic Dis 2020;17:E82. 10.5888/pcd17.200266.
38. COVID-19: economic impact on dental practices:
week of October 19 results. ADA Health Policy
Institute Accessed January 15, 2021. https://sur-
veys.ada.org/reports/RC/public/ YWRhc3VydmV-
5cy01ZjhmNTg0MTYyNzFiYzAwMGUwZDI4NDQtV-
VJfM3BaeGhzWm12TnNMdjB4.
39. Needleman HL, Stucenski K, Forbes PW, Chen Q,
StackAM.Massachusettsemergencydepartments’
resourcesandphysicians’knowledgeofmanage-
ment of traumatic dental injuries. Dent Traumatol
2013;29(4):272-9. 10.1111/j.1600-9657.2012.01170.x.
40. Lewis CW, Boulters, Keels MA, et al. Oral health and
pediatricians: results of a national survey. Acad Pedi-
atr 2009;9(6):457-61. 10.1016/j.acap.2009.09.016.
41. May L, Suminski RR, Yeung AY, et al. Pregnant
patient knowledge of and obstetric provider advice
on oral health. J Dent Oral Disord Ther Novem-
ber 24, 2014 [Online ahead of print] 10.1016/j.
wombi.2014.11.004.
42. Olson R, Bialocerkowski A. Interprofessional educa-
tion in allied health: a systematic review. Med Educ
2014;48(3):236-46. 10.1111/medu.12290.
43. Versaci MB. Wisconsin dentists donate personal
protective equipment amid COVID-19 pandemic. ADA
News. April 17, 2020. Accessed January 15, 2021.
https://www.ada.org/en/publications/ada-news/2020-
archive/april/wisconsin-dentists-donate-personal-
protective-equipment-amid-covid-19-pandemic.
44. Massachusetts dentists donate 175,000 PPE to
help with COVID-19 crisis. ADA News. April 1, 2020.
Accessed January 15, 2021. https://www.ada.org/
en/publications/new-dentist-news/2020-archive/april/
massachusetts-dentists-donate-175000-ppe-to-help-
with-covid19-crisis.
45. Miller D. Dental clinics facing PPE shortages after
donating to frontline medical workers. WUSF Public
Media. May 26, 2020. Accessed January 15, 2021.
https://wusfnews.wusf.usf.edu/health-news-or-
ida/2020-05-26/dental-clinics-facing-ppe-shortages-
after-donating-to-frontline-medical-workers.
46. Simon L. How will dentistry respond to the corona-
virus disease 2019 (COVID-19) pandemic? JAMA
Health Forum. May 19, 2020. Accessed January
15, 2021. https://jamanetwork.com/channels/health-
forum/fullarticle/2766388.
47. Clark MB, Douglass AB, Maier R, et al. Smiles
for life: a national oral health curriculum. Soci-
ety of Teachers of Family Medicine. September
17, 2015. Accessed January 15, 2021. https://
resourcelibrary.stfm.org/resourcelibrary/ourlibrary/
viewdocument?DocumentKey=45fd7cd7-ccda-42f0-
9999-c8bfc0d0df05.
48.ProtectingAllChildren’sTeeth(PACT):apediatricoral
health training program. American Academy of Pedi-
atrics. Accessed January 15, 2021. https://www.aap.
org/en-us/advocacy-and-policy/aap-health-initiatives/
Oral-Health/Pages/Protecting-All-Childrens-Teeth.
aspx.
49. Integration of oral health and primary care practice.
Rockville, MD: U.S. Department of Health and Human
Services Health Resources and Services Administra-
tion, 2014. https://www.hrsa.gov/sites/default/les/
hrsa/oralhealth/integrationoforalhealth.pdf.
50. About OHNEP. Oral Health Nursing Education and
Practice. Accessed January 15, 2021. http://ohnep.
org/.
51. National Interprofessional Initiative on Oral Health.
Primary Care Collaborative. Accessed January 15,
2021.https://www.pcpcc.org/executive/national-inter-
professional-initiative-oral-health
52. One Hundred Million Mouths Project. Center for Inte-
gration of Primary Care and Oral Health. Accessed
January 15, 2021. https://cipcoh.hsdm.harvard.edu/
one-hundred-million-mouths-project.
53. Jeffcoat MK, Jeffcoat RL, Gladowski PA, Bramson
JB, Blum JJ. Impact of periodontal therapy on general
health:evidencefrominsurancedataforvesys-
temic conditions. Am J Prev Med 2014;47(2):166-74.
10.1016/j.amepre.2014.04.001.
242 PRIMARY CARE IN THE COVID-19 PANDEMIC
54. Nasseh K, Vujicic M, Glick M. The relationship
between periodontal interventions and healthcare
costs and utilization: evidence from an integrated
dental, medical, and pharmacy commercial claims
database. Health Econ 2017;26(4):519-27. 10.1002/
hec.3316.
55. Dental care in accountable care organizations:
insights from 5 case studies. ADA Health Policy
Institute and Leavitt Partners. Accessed January 15,
2021. http://www.ada.org/~/media/ADA/Science%20
and%20Research/HPI/Files/HPIBrief_0615_1.ashx.
56.WittersD.One-thirdofAmericanshaven’tvisitedden-
tist in past year. Gallup. April 28, 2014. Accessed Jan-
uary 15, 2021. https://news.gallup.com/poll/168716/
one-third-americans-haven-visited-dentist-past-year.
aspx.
57. Carroll L. Declining numbers of Americans have a
primary care provider. Reuters. December 16, 2019.
Accessed January 15, 2021. https://www.reuters.
com/article/us-health-pcp-trends/declining-numbers-
of-americans-have-a-primary-care-provider-idUSK-
BN1YK1Z4.
58. Rao A, Shi Z, Ray KN, Mehrotra A, Ganguli I. National
trends in primary care visit use and practice capabili-
ties, 2008-2015. Ann Fam Med 2019;17(6):538-44.
10.1370/afm.2474.
59. Monopoli M. DentaQuest on dental care safety in the
COVID-19era.America’sHealthInsurancePlans.
September 22, 2020. Accessed January 15, 2021.
https://www.ahip.org/dentaquest-on-dental-care-
safety-in-the-covid-19-era/.
60. Benzian H, Niederman R. A dental response to the
COVID-19 pandemic—safer aerosol-free emergent
(SAFER) dentistry. Front Med (Lausanne) 2020;7:520.
10.3389/fmed.2020.00520.
61. Bernstein RS, Johnston B, Mackay K, Sanders J.
Implementation of a primary care physician–led Cav-
ityClinicusingsilverdiamineuoride.JPublicHealth
Dent 2019;79(3):193-7. 10.1111/jphd.12331.
62.RuffRR,NiedermanR.Silverdiamineuorideversus
therapeutic sealants for the arrest and prevention of
dental caries in low-income minority children: study
protocol for a cluster randomized controlled trial. Tri-
als 2018;19(1):523. 10.1186/s13063-018-2891-1.
63. Ibiyemi O, Bankole OO, Oke GA. Assessment
of atraumatic restorative treatment (ART) on the
permanent dentition in a primary care setting in
Nigeria. Int Dent J 2011;61(1):2-6. 10.1111/j.1875-
595X.2011.00001.x.
64. Shenoy R, Jain A, Kundabala M. Atraumatic restor-
ative treatment for dental caries among preg-
nant women attending primary health centres: a
small scale demonstration. J Interdiscip Dentistry
2014;4(2):71-5. 10.4103/2229-5194.142937.
65. Braun PA, Widmer-Racich K, Sevick C, Star-
zyk EJ, Mauritson K, Hambidge SJ. Effective-
ness on early childhood caries of an oral health
promotion program for medical providers. Am J
Public Health 2017;107(S1):S97-S103. 10.2105/
AJPH.2017.303817.
66. Dolce MC, Parker JL, Da Silva JD. Nurse practitioner
& dentist model for primary care: a guide for imple-
menting collaborative care in U.S. dental schools.
Harvard School of Dental Medicine and Northeastern
University. 2018. Accessed March 7, 2021. https://
hsdm.harvard.edu/les/dental/les/npd_model_imple-
mentation_guide3.pdf.
67. ECHO impact and initiatives: touching one billion lives
by 2025. Extension for Community Health Outcomes
(ECHO). Accessed January 15, 2021. https://hsc.
unm.edu/echo/echos-impact/.
68. Atchison KA, Rozier RG, and Weintraub JA. Integra-
tion of oral health and primary care: communica-
tion, coordination, and referral. National Academy of
Medicine Perspectives. October 8, 2018. Accessed
January 15, 2021. https://nam.edu/integration-of-oral-
health-and-primary-care-communication-coordination-
and-referral/.
69. Patient experience. EPIC Software and Service.
Accessed January 15, 2021. https://www.epic.com/
software#PatientEngagement.
70. Glurich I, Acharya A, Shukla SK, Nycz GR, Bril-
liant MH. The oral-systemic personalized medicine
modelatMarsheldClinic.OralDis2013;19(1):1-17.
10.1111/j.1601-0825.2012.01921.x.
71. Kranz AM, Duffy E, Dick AW, Sorbero M, Rozier RG,
Stein BD. Impact of Medicaid policy on the oral health
of publicly insured children. Matern Child Health J
2019;23(1):100-8. 10.1007/s10995-018-2599-6.
72. Hargraves J, Frost A. Trends in primary care visits.
Health Care Cost Institute. November 15, 2018.
Accessed January 15, 2021. https://healthcostinsti-
tute.org/hcci-research/trends-in-primary-care-visits.
PRIMARY CARE IN THE COVID-19 PANDEMIC 243
Telehealth Equity:
Before and After
COVID-19
Elaine Khoong and Courtney Lyles
T
elehealth during the COVID-19 pandemic has represented an abrupt and rapid transformation
of primary care with near- and long-term implications for health equity. When considering
telehealth rollout within safety-net health care settings serving diverse patients, there are multiple
factors at play: existing challenges at both the clinician/system and patient levels, as well as new
opportunities for engagement and proactive planning for sustaining implementation as a core
component of care post-pandemic.
Telehealth can refer to a variety of remotely delivered health care, including real-time synchronous
health care (e.g., video visits), asynchronous care (e.g., store and forward services like teleder-
matology), and adjunctive digital tools, such as wearables or remote patient monitoring. Of these
domains, prior to COVID-19 there was higher adoption of asynchronous telemedicine—such as
teledermatology, telemedicine retinopathy screening, and electronic specialty consultations—in
underserved settings to address gaps and delays in access to specialty care. COVID-19, however,
ignited unprecedented growth primarily in synchronous, patient-facing telehealth, including both
telephone and video visits.
1
We will focus the remainder of this chapter on this synchronous remote
clinical care, which we will call telemedicine.
Telemedicine care has been primarily limited to video visits, as audio-only telemedicine had lim-
ited or no reimbursement from most payers. Therefore, much of the literature and prior imple-
mentation has focused exclusively on video visits. By contrast, many safety-net systems delivering
telemedicine care in the initial stages of COVID-19 (and continuing to deliver care) use audio-only
telephone visits.
2,3
While no data exist comparing telephone to video visits directly, prior literature
suggests that video interpretation is better than phone interpretation for communication outcomes
(satisfaction, comprehension).
4,5
Therefore, telemedicine equity must also consider variations in
access and quality of care for telephone versus video visits. We will address overall equity
considerations for telemedicine in this chapter, including broad telephone or video visit
implementation processes as well as more specic digital considerations for use of video calls
on smartphones or other devices.
Finally, it is important to note that there has been high satisfaction with telemedicine in sys-
tems routinely oering video/phone visits prior to the pandemic, such as Kaiser Permanente
Northern California or the Veterans Aairs system.
6,7
We will expand upon that knowledge
but additionally focus on the state of telemedicine for safety-net health care settings such as
Federally Qualied Health Centers (FQHCs) and public hospitals that disproportionately serve
patients who are low-income or on Medicaid, who are from race/ethnic minority backgrounds,
and who have limited English prociency or communication barriers such as limited literacy.
The impact of telehealth during COVID-19 on
primary care access
The building blocks of high-quality primary care include engaged leadership, data-driven
improvement, empanelment, prompt access to care, and team-based care.
8
Prior to COVID-19,
there were large inequities in implementation of these building blocks between safety-net
settings and health care settings that served higher-income populations. Low-income, im-
migrant, or chronically ill populations have been more likely to experience barriers to prompt
access to primary care.
9
Eorts to address gaps in access were disrupted by the growth of
telemedicine implementation. When the COVID-19 pandemic began, despite the dramatic in-
crease in use of telemedicine for ambulatory care, there was a decrease in overall primary care
utilization.
1
This reduction was particularly dramatic in community health centers that cared
for many underserved populations.
10
Moreover, at the onset of the COVID-19 pandemic, in
practices that switched to telemedicine, patients with known barriers to digital access (older,
low-income, limited English procient, and minority individuals) were particularly less likely
to utilize primary care.
11
Yet regardless of health care setting, clinical practices are beginning to return to in-person
visits, while maintaining a larger presence of telemedicine than they did previously.
12
Therefore, it is crucial that health systems develop standard work for remote ambulatory
care that explicitly ensures equitable access to telemedicine. To ensure telemedicine equity,
policy makers, health system leaders, and clinicians need an understanding of the state of the
digital divide among health systems and patients. It will also be helpful to incorporate lessons
learned from eorts to increase electronic health record adoption, the most widespread previ-
ous digital disruption in health care.
Barriers to telemedicine for safety-net health care settings
Though most conversations on telehealth equity focus on patient-level barriers, there are dis-
parities in preparedness for and capability of transitioning to telemedicine at multiple levels
of the health care system between underresourced health systems, which disproportionately
246 PRIMARY CARE IN THE COVID-19 PANDEMIC

care for minority and low-income patients, and higher-resourced systems (Table 1).
Underresourced health systems have less device, software, and broadband access as well as
lower payment rates per care episode, which often results in lower telemedicine payments for
practices that disproportionately care for patients with low digital access.
In 2016, only 15% of clinicians worked in practices with telehealth programs, and these
were most frequently hospital-based health systems or large practices with at least 50 clini-
cians.
13,14
By 2018, fewer than half of community health centers used any form of telehealth,
and less than one-third of those using telehealth in those systems were primary care provid-
ers.
10
Therefore, safety-net settings (particularly FQHCs) were not prepared to transition to
telemedicine. Since many of these centers had not adopted telehealth prior to the pandemic,
most did not have hardware (i.e., video-enabled devices) and/or software (video capabili-
ties embedded into the electronic health records and compliant with the Health Insurance
Portability and Accountability Act [HIPAA]) to rapidly increase telemedicine services. Since the
COVID-19 pandemic began, investment in this infrastructure has been nearly impossible as the
reduction of in-person care also meant health centers were suering daily nancial losses.
Reimbursement policies only exacerbate disparities between health systems. Although the
Centers for Medicare and Medicaid Services (CMS) quickly made changes to its telemedicine
reimbursement policies for Medicare patients, Medicare covers only 18% of the US popula-
tion.
15
Adoption of telemedicine policies varied across commercial payers, Medicaid, the
Veterans Health Administration, and the Indian Health Service (among others).
16,17
Moreover,
initially CMS policy changes did not fully include health care systems that care for larger
proportions of indigent patients, such as FQHCs and rural health centers, though a policy
change later ameliorated this problem.
18
In addition, although most health centers were able
to immediately oer telephone visits (and audio-only visits may have been more accessible
for patients with digital access challenges),
19
audio-only telemedicine visits have tradition-
ally been paid for at a much lower rate than video visits.
20
Changes to reimbursement for
Table 1. Barriers to Telemedicine Equity in Primary Care
Level Barriers to Equity
Health care system Reimbursement policy
Health practice/clinician Hardware access
HIPAA-compliant software
High-quality Internet connection
Mission and workow alignment
Capacity to provide technical support
Sta turnover
Patient Digital device access
High-quality Internet connection
Digital literacy
PRIMARY CARE IN THE COVID-19 PANDEMIC 247
audio-only services only occurred after advocacy by many primary care organizations, and it
is unclear how long these policies will remain.
Barriers to telemedicine for diverse patient populations
Multiple trends in digital access inuence the ability of patients to use telemedicine services.
There are growing rates of smartphone ownership in the United States, with more than 80%
of Americans having access to a device and more than 90% of Americans self-reporting
using the Internet.
21,22
Yet, when these data are examined further, there are clear subgroups
who still fall behind in device access and home Internet use. Specically, 71% of low-income
Americans (i.e., those making less than $30,000 per year) own a smartphone and 56% have
Internet access at home, compared to 97% and 94%, respectively, of those making $100,000
or more annually.
23
Similar disparities are present by age groups (i.e., lower use among those
65 years or older versus younger groups) and community (lower use comparing rural versus
urban populations).
22
Relatedly, there is a new emerging trend that shows a sharp increase in
smartphone-only Internet use, particularly among the lowest-income groups in the United
States; 26% of Americans making $30,000 or less per year rely on their smartphones only to
access online resources and apps or tools.
22
This presents unique challenges with respect to
lower quality of data service (e.g., cellular coverage with potential data use restrictions ver-
sus higher speed and higher bandwidth coverage at home)—especially for services like video
visits that can use more data than other tasks.
Beyond device ownership rates and access to high-quality Internet service, there is a third
component of the digital divide that requires attention: digital literacy, or the skills to be able
to use digital platforms to complete tasks. For example, only 26% of those aged 65 years or
older in the United States report being very condent in using digital devices.
24
But these
dierences in digital literacy persist among other groups as well. A recent survey by the San
Francisco Digital Equity Initiative found that 92% of San Francisco residents both report
home Internet use and basic digital literacy skills to go online, dened as completing basic
online searches, sending an email, nding a website, and completing an online form.
25
Yet
when stratied, only 53% of the lowest-income San Franciscans report both home Internet
use and basic digital literacy skills, with similar trends among those with limited English
prociency. Other peer-reviewed research also supports low digital literacy as a fundamental
barrier to uptake of digital health services.
26,27
Finally, there is a clear literature on the need to preserve patient-clinician relationships re-
gardless of the digital care modality introduced. For example, some patients report preference
for in-person visits instead of remote/virtual care, as well as the need to understand how
clinicians recommend remote care modalities.
28
The trust in telehealth as well as other digi-
tal health care services will be linked to supporting ongoing care team relationships. When
considering trust at an institutional or structural level, concerns about security and privacy
(as well as mistrust in the medical system itself) are prevalent and must be communicated
and addressed up front with patients.
29
248 PRIMARY CARE IN THE COVID-19 PANDEMIC
Lessons from previous digital health implementations
Experiences at underresourced health care settings
As we begin to envision how to equitably incorporate telemedicine into primary care, we can
look to the experience of electronic health record (EHR) adoption. The Health Information
Technology for Economic and Clinical Health Act (HITECH) of 2009 signicantly increased
adoption of EHRs.
30,31
Despite eorts to specically support centers in serving rural or disad-
vantaged populations, however, practices and systems that served larger Medicaid and low-
income populations were less likely to achieve success in EHR implementation or in using
advanced EHR tools.
30,32,33
HITECH had an incentive structure that was not designed with equity in mind. HITECH
incentives to adopt EHRs included performance targets related to patient access to medical
records. To reach these targets, safety-net practices often needed substantial resources and
personnel to digitally prepare their patients to achieve these targets for patient use of por-
tals tied to EHRs.
34
For health systems that served patients with digital barriers, reaping the
nancial incentives (or benets) of reaching these performance targets may not have been the
best use of their limited resources to meet their patients’ needs.
34
Subsequent research has
found that pay-for-performance programs disproportionately penalize safety-net practices
when the performance highly depends on the social and economic circumstances of the pa-
tient population.
35,36
Disparities in EHR adoption were also inuenced by the need for continued support beyond
initial investment.
30,37
Innovations have not generally been designed with safety-net set-
tings in mind, and they require adaptations to meet the needs of such systems. For example,
purchasing decisions must consider workow and workforce concerns in safety-net systems,
yet the investment options for digital products and solutions might not be suited to the needs
of their patients or clinical team.
30,38
For example, some systems lack language-concordant
patient platforms. While English-only patient-facing tools clearly harm patients, they also
impact clinical teams because they require health care teams (which are often understaed in
safety-net systems) to nd time to support diverse patients in accessing these digital tools.
Since patients with limited English prociency often receive care in safety-net systems,
health care teams in these settings are most impacted by the limited number of digital prod-
ucts designed for diverse populations. Time is also needed to develop the capacity for the spe-
cic technical assistance or skills that are needed to fully leverage a new technology.
39-41
This
capacity building requires resources that may be less readily available in safety-net systems.
Implementation challenges more common to safety-net settings include sta turnover and
the need for mission alignment for the organization.
39,41
Turnover can be particularly chal-
lenging when leadership or an innovation champion leaves—stalling progress through loss
of knowledge, impact on sta morale, and added burden to remaining sta who may need to
recruit, hire, and onboard a new team member. Furthermore, safety-net systems are more
likely to implement innovations that have been proven in other similar settings or are a good
cultural t for their populations.
37
Thus, specic types of digital innovations that directly
PRIMARY CARE IN THE COVID-19 PANDEMIC 249
address high-priority challenges in safety-net systems (such as electronic consult services
to help improve specialty care access) have been more easily adopted than general solutions
common to higher-resourced facilities.
42,43
Previous digital health implementation successes among diverse
populations
Despite sobering statistics about the fundamental barriers of device ownership, high-quality
Internet access, and digital skills, especially for older adults, low-income Americans, and
other communities such as those with limited English prociency, the statistics do not
imply that these groups are not interested or able to use digital tools and services like tele-
health if adequate and proactive measures are put into place. National surveys suggest that
public interest in electronic communication with providers and the ability to access medical
records or services online is extremely high.
44
Further, research in Medicaid populations
shows the same rates of high interest in digital health tools, underscoring the demand.
45
Early research among safety-net populations during the pandemic also shows high levels of
interest in telemedicine.
46
Eorts to introduce patient portals and mobile health applications among diverse populations
provide lessons for how to overcome other barriers to patient adoption of digital health in di-
verse populations. First, the fundamental connectivity and device barriers patients face often
require creative solutions outside the health care system. Partnering with community-based
organizations already working on digital inclusion strategies (such as by providing access
through public libraries) can be a successful approach to overcome gaps in both device access
and digital literacy.
47
Patient portal implementation eorts to enable electronic health record access have shown
that robust technical support,
34
such as creation of enrollment helplines, weekly training
sessions, distribution of educational brochures, or one-on-one support from clinical teams
or volunteers, to assist patients is also a crucial element to successful patient adoption.
Importantly, this technical support needs to be maintained and cannot be viewed as a one-
time investment.
28,34
Among patients with digital literacy challenges, training may be needed
to increase use of digital health tools,
48,49
and one-time trainings may not be sucient for all
patients. Previous limited success with individual or patient-level interventions to increase
patient portal use among diverse populations suggests that a multilevel approach, including
incorporating health system changes, collaborating with community-based organizations, or
redesigning a digital tool, is needed to increase use of similar digital tools. Strategies such as
codeveloping more usable tools with diverse end users, and forming sustainable partnerships
between health care and existing community organizations providing linkages to low-cost
programs for devices or Internet access, are fruitful opportunities.
49
250 PRIMARY CARE IN THE COVID-19 PANDEMIC

Moving forward: Strategies to address equity in
telemedicine
Despite the barriers outlined here, clinical and health care sector leaders have never been
more engaged to improve telemedicine and rapidly iterate and try telemedicine workows.
The rapid pace of change has impacted all health care systems, and the unique moment of the
pandemic has required safety-net systems to embrace telemedicine (at a minimum, phone
visits) to deliver primary care safely. The changes induced by COVID-19 present an opportu-
nity to develop and implement an equitable approach to telemedicine that will be sustainable
and continued in a future practice state.
We map next steps for various stakeholders to achieve telemedicine equity in Table 2.
Table 2. Strategies to Promote Telemedicine Equity in Primary Care
Group Recommendations
Policymakers Incentives for health care systems to purchase
infrastructure and develop technical capacity to provide
ongoing support.
Expansion of free or low-cost digital devices and
broadband access.
Health care payers Flexibility in payment models to provide the type of care
(telemedicine video vs. telemedicine phone vs. in-person
visit) most appropriate for each patient.
Payment for activities (e.g., technology support) and
devices (e.g., home monitoring equipment) that support
telemedicine care.
Payment structure that explicitly considers underserved
populations and does not penalize safety-net systems.
Requirement of private solutions to meet patients’
accessibility needs, particularly with literacy and language.
Health care system operators
and clinicians
Collaborate with digital inclusion organizations.
Seek guidance and resources on selecting most usable
technology platforms.
Develop digital training for patients.
Screen for digital access barriers.
Train team members on providing technology support.
Train clinicians and provide resources on how to address
communication challenges (e.g., language barriers).
Health services researchers Evaluate how and when telemedicine advances equity and
improves clinical or patient-reported outcomes.
PRIMARY CARE IN THE COVID-19 PANDEMIC 251
First, there is a clear role for policymakers and health care payers to ensure telemedicine
equity.
50
As the experience of the HITECH Act shows, safety-net systems need additional
nancial support to acquire digital infrastructure and technical expertise to support ongoing
maintenance of digital infrastructure. Furthermore, telemedicine cannot be equitably imple-
mented if payment policies do not support telemedicine access for all patients by paying for
multiple visit types at a reasonable level or paying for patient-monitoring tools that allow for
safe telemedicine care. These incentives need to be developed so as not to penalize high-need
patients or the systems that serve them. Similarly, as many have noted, high-speed Internet
and digital access are no longer luxuries. They are crucial elements of life, much like electric-
ity and running water; policies are needed to lower barriers to the Internet and digital devices.
Second, health care systems and clinicians have important roles in addressing many patient-
facing barriers to accessing telemedicine. Systems must recognize that many of their patients
may have barriers accessing telemedicine and design technical support that meets patient
needs. To proactively address these issues, systems can also partner with organizations
already conducting digital inclusion work as well as explicitly evaluating core usability prin-
ciples when selecting and purchasing patient-facing digital tools.
51
Clinical systems should
develop workows to help health care teams screen for and identify barriers, such as device
access, home Internet service, and digital literacy. These barriers are likely common and
health care teams should have received training and support to provide technical support to
patients to engage in telemedicine care. As the patient portal experience shows, health sys-
tems should anticipate this technical support will be an ongoing need and should have clear
workows for linking patients to these services. Similarly, health care settings can simplify
the patient-facing aspects of the workow, such as by simplifying log-ins to video visit
platforms whenever possible and generating patient-focused, simple instructions to use for
the services oered at each clinical site.
52
Another clear need to engage patients more meaningfully is a better match of existing tech-
nologies to diverse patients’ needs. As with all patient-facing resources, platforms need to be
designed with accessibility in mind by ensuring usability for limited health literate popula-
tions and translation into multiple languages for patients with limited English prociency—
which is not currently the standard in digital health. We can collectively demand this devel-
opment from the private sector and actively partner with them to ensure diverse perspectives
are considered up front.
Our nal recommendations are for health service researchers. Since many safety-net systems
prioritize mission alignment and are often not early adopters of innovations, health services
researchers play a crucial role by evaluating how, when, and if telemedicine can improve
equitable care for underserved populations or address other needs in safety-net systems.
Without evidence supporting outcomes important in underresourced settings, such as clinical,
patient-reported, cost, or clinician outcomes, telemedicine likely will not be made accessible
to patients disproportionately served in safety-net settings.
252 PRIMARY CARE IN THE COVID-19 PANDEMIC
References
1. Mehrotra A, Chernew M, Linetsky D, Hatch H, Cutler
D. The Impact of the COVID-19 Pandemic on Outpa-
tient Visits: Practices Are Adapting to the New Nor-
mal. Commonwealth Fund. June 25, 2020. Accessed
October 14, 2020. https://www.commonwealthfund.
org/publications/2020/jun/impact-covid-19-pandemic-
outpatient-visits-practices-adapting-new-normal.
2. Varma S. Early Impact of CMS expansion of Medicare
telehealth during COVID-19. Health Affairs Blog. July
15, 2020. Accessed October 14, 2020. https://www.
healthaffairs.org/do/10.1377/hblog20200715.454789/
full/.
3. Uscher-Pines L, Sousa J, Jones M et al. Telehealth
use among safety-net organization in California dur-
ing the COVID-19 Pandemic. JAMA. 2021. 10.1001/
jama.2021.0282.
4. Lion KC, Brown JC, Ebel BE, et al. Effect of telephone
vs video interpretation on parent comprehension,
communication, and utilization in the pediatric emer-
gency department: a randomized clinical trial. JAMA
Pediatr 2015;169(12):1117-25. 10.1001/jamapediat-
rics.2015.2630.
5. Locatis C, Williamson D, Gould-Kabler C, et al.
Comparing in-person, video, and telephonic medical
interpretation. J Gen Intern Med 2010;25(4):345-50.
10.1007/s11606-009-1236-x.
6. Reed ME, Huang J, Graetz I, et al. Patient character-
istics associated with choosing a telemedicine visit
vsofcevisitwiththesameprimarycareclinicians.
JAMA Netw Open 2020;3(6):e205873. 10.1001/jama-
networkopen.2020.5873.
7. Zulman DM, Wong EP, Slightam C, et al. Making con-
nections: nationwide implementation of video tele-
health tablets to address access barriers in veterans.
JAMIA Open 2019;2(3):323-9. 10.1093/jamiaopen/
ooz024.
8. Bodenheimer T, Ghorob A, Willard-Grace R, Grum-
bach K. The 10 building blocks of high-performing pri-
mary care. Ann Fam Med 2014;12(2):166-71. https://
doi.org/10.1370/afm.1616[insert period at end; period
should be black, regular text, not part of hyperlink].
9. Corscadden L, Levesque JF, Lewis V, Strumpf E,
Breton M, Russell G. Factors associated with multiple
barriers to access to primary care: an international
analysis. Int J Equity Health 20;17(1):28. 10.1186/
s12939-018-0740-1.
10. Kim J-H, Desai E, Cole MB. How the rapid shift to
telehealth leaves many community health centers
behind during the COVID-19 pandemic. Health
Affairs Blog. June 2, 2020. Accessed June 9,
2020. https://www.healthaffairs.org/do/10.1377/
hblog20200529.449762/full/.
11. Nouri S, Khoong EC, Lyles CR, Karliner L. Addressing
equity in telemedicine for chronic disease manage-
ment during the COVID-19 pandemic. NEJM Catalyst.
May 4, 2020. Accessed February 4, 2021. https://
catalyst.nejm.org/doi/abs/10.1056/CAT.20.0123.
12. Mehrotra A, Wang B, Snyder G. Telemedicine: What
Should the Post-Pandemic Regulatory and Payment
Landscape Look Like? Commonwealth Fund. August
5, 2020. Accessed October 14, 2020. https://www.com-
monwealthfund.org/publications/issue-briefs/2020/aug/
telemedicine-post-pandemic-regulation.
Conclusions
Despite ongoing concerns about equitable access to telemedicine,
11,53,54
we believe it is im-
portant to highlight that telemedicine can be implemented to assist patients with challenges
attending in-person care (e.g., mobility issues, distance from a health center, child care/
work constraints). Though telemedicine has been implemented in the past year in response
to an unanticipated global health pandemic, there has always been a role for telemedicine to
help facilitate equitable, patient-centered, high-quality care. By capitalizing on this time of
rapid change to design telemedicine for equity using some of the approaches suggested in this
chapter, we are hopeful that telemedicine can be leveraged to reduce instead of exacerbate
existing health disparities.
PRIMARY CARE IN THE COVID-19 PANDEMIC 253
13. Kane CK, Gillis K. The use of telemedicine by physi-
cians: still the exception rather than the rule. Health
Affairs (Millwood) 2018;37(12):1923-30. 10.1377/
hlthaff.2018.05077.
14. Barnett ML, Ray KN, Souza J, Mehrotra A. Trends
in telemedicine use in a large commercially insured
population, 2005-2017. JAMA 2018;320(20):2147.
10.1001/jama.2018.12354.
15. Berchick ER, Barnett JC, Upton RD. Health Insurance
Coverage in the United States: 2018. Washington,
DC: US Census Bureau, 2019. https://www.census.
gov/content/dam/Census/library/publications/2019/
demo/p60-267.pdf.
16. Augenstein J. Opportunities to expand telehealth
use amid the coronavirus pandemic. Health Affairs
Blog. March 16, 2020. Accessed October 14,
2020. https://www.healthaffairs.org/do/10.1377/
hblog20200315.319008/full/.
17. Center for Connected Health Policy. COVID-19
related state actions. 2020. Accessed October 14,
2020. https://www.cchpca.org/covid-19-related-state-
actions.
18. Wicklund E. CARES Act Expands Telehealth Cover-
age for Medicare, FQHCs and the VA mHealthIntel-
ligence. March 30, 2020. Accessed October 14, 2020.
https://mhealthintelligence.com/news/cares-act-
expands-telehealth-coverage-for-medicare-fqhcs-and-
the-va.
19. Lam K, Lu AD, Shi Y, Covinsky KE. Assessing
telemedicine unreadiness among older adults in
the United States during the COVID-19 pandemic.
JAMA Intern Med 180(10):1389-1391. 10.1001/
jamainternmed.2020.2671. Accessed August 5, 2020.
https://jamanetwork.com/journals/jamainternalmedi-
cine/fullarticle/2768772.
20.D’AmbrosioA.Audio-onlytelemedicine:docssay
payment falls short. MedPage Today. July 13, 2020.
Accessed October 14, 2020. https://www.medpageto-
day.com/practicemanagement/telehealth/87531.
21. Pew Research Center. Internet/broadband fact sheet.
June 12, 2019. Accessed October 14, 2020. https://
www.pewresearch.org/internet/fact-sheet/internet-
broadband/.
22. Pew Research Center. Mobile fact sheet. June 12,
2019. Accessed October 14, 2020. https://www.
pewresearch.org/internet/fact-sheet/mobile/.
23. Anderson M, Kumar M. Digital divide persists even as
lower-income Americans make gains in tech adop-
tion. Pew Research Center. May 7, 2019. Accessed
October 14, 2020. https://www.pewresearch.org/fact-
tank/2019/05/07/digital-divide-persists-even-as-lower-
income-americans-make-gains-in-tech-adoption/.
24. Anderson M, Perrin A. Barriers to adoption and
attitudes towards tech among older Americans. Pew
Research Center. May 17, 2017. Accessed Octo-
ber 14, 2020. https://www.pewresearch.org/inter-
net/2017/05/17/barriers-to-adoption-and-attitudes-
towards-technology/.
25.SanFranciscoOfceofDigitalEquity.Digitalinclusion
in San Francisco. 2018. Accessed February 5, 2021.
https://www.cpuc.ca.gov/uploadedFiles/CPUC_Pub-
lic_Website/Content/Utilities_and_Industries/Com-
munications_-_Telecommunications_and_Broadband/
Consumer_Programs/California_LifeLine_Program/
SF%20Ofce%20of%20Digital%20Equity.pdf.
26. Berg K, Davis W, Sheon A, et al. Strategies for
addressing digital literacy and Internet access
as social determinants of health. Innov Aging
2018;2(Suppl 1):679. 10.1093/geroni/igy023.2526.
27. Tieu L, Schillinger D, Sarkar U, et al. Online patient
websites for electronic health record access among
vulnerable populations: portals to nowhere? J Am
Med Inform Assoc 2017;24(e1):e47-54. 10.1093/
jamia/ocw098.
28. Lyles CR, Allen JY, Poole D, Tieu L, Kanter MH,
Garrido T. “I want to keep the personal relationship
with my doctor”: understanding barriers to portal use
among African Americans and Latinos. J Med Internet
Res 2016;18(10):e263. 10.2196/jmir.5910.
29. Lyles CR, Nelson EC, Frampton S, Dykes PC, Cem-
balli AG, Sarkar U. Using electronic health record por-
tals to improve patient engagement: research priori-
ties and best practices. Ann Intern Med 2020;172(11
Suppl):S123-9. 10.7326/M19-0876.
30. Gold M, McLaughlin C. Assessing HITECH imple-
mentation and lessons: 5 years later. Milbank Q
2016;94(3):654-87. 10.1111/1468-0009.12214.
31. Adler-Milstein J, Jha AK. HITECH Act drove large
gains in hospital electronic health record adoption.
Health Affairs (Millwood) 2017;36(8):1416-22. https://
doi.org/10.1377/hlthaff.2016.1651.
32. Adler-Milstein J, Holmgren AJ, Kralovec P, Worzala C,
Searcy T, Patel V. Electronic health record adoption
in US hospitals: the emergence of a digital “advanced
use” divide. J Am Med Inform Assoc 2017;24(6):1142-
8. 10.1093/jamia/ocx080.
33. Ancker JS, Singh MP, Thomas R, et al. Predictors
of success for electronic health record implementa-
tion in small physician practices. Appl Clin Inform
2013;4(1):12-24. 10.4338/ACI-2012-09-RA-0033.
254 PRIMARY CARE IN THE COVID-19 PANDEMIC
34. Ackerman SL, Sarkar U, Tieu L, et al. Meaningful use
in the safety net: a rapid ethnography of patient portal
implementationatvecommunityhealthcentersin
California. J Am Med Inform Assoc 2017;24(5):903-
12. 10.1093/jamia/ocx015.
35. Liao JM, Navathe AS. Does the merit-based incentive
payment system disproportionately affect safety-net
practices? JAMA Health Forum 2020;1(5):e200452.
https://jamanetwork.com/channels/health-forum/fullar-
ticle/2766082.
36. Gilman M, Adams EK, Hockenberry JM, Milstein AS,
Wilson IB, Becker ER. Safety-net hospitals more likely
thanotherhospitalstofarepoorlyunderMedicare’s
value-based purchasing. Health Affairs (Millwood)
2015;34(3):398-405. 10.1377/hlthaff.2014.1059.
37. Lyles CR, Aulakh V, Jameson W, Schillinger D,
Yee H, Sarkar U. Innovation and transformation in
California’ssafetynethealthcaresettings:aninside
perspective. Am J Med Qual 2014;29(6):538-45.
10.1177/1062860613507474.
38. Craven CK, Sievert MC, Hicks LL, Alexander GL,
Hearne LB, Holmes JH. CAH to CAH: EHR imple-
mentation advice to critical access hospitals from peer
experts and other key informants. Appl Clin Inform
2014;5(1):92-117. 10.4338/ACI-2013-08-RA-0066.
39. Lyles CR, Handley MA, Ackerman SL, et al.
Innovative implementation studies conducted
in US safety net health care settings: a system-
atic review. Am J Med Qual 2019;34(3):293-306.
10.1177/1062860618798469.
40. Garg SK, Lyles CR, Ackerman S, et al. Qualitative
analysis of programmatic initiatives to text patients
with mobile devices in resource-limited health
systems. BMC Med Inform Decis Mak 2016;16:16.
10.1186/s12911-016-0258-7.
41. Sugarman JR, Phillips KE, Wagner EH, Coleman
K, Abrams MK. The safety net medical home initia-
tive: transforming care for vulnerable populations.
Med Care 2014;52(11 Suppl 4):S1-10. 10.1097/
MLR.0000000000000207.
42. Chen AH, Murphy EJ, Yee HF Jr. eReferral—a
new model for integrated care. New Engl J Med
2013;368(26):2450-3. 10.1056/NEJMp1215594.
43. Daskivich LP, Vasquez C, Martinez C, Tseng C-H,
Mangione CM. Implementation and evaluation of a
large-scale teleretinal diabetic retinopathy screening
program in the Los Angeles County Department of
Health Services. JAMA Intern Med 2017;177(5):642-
9. 10.1001/jamainternmed.2017.0204.
44. Abrams K, Korba C. Consumers are on board with
virtual health options. Deloitte. August 29, 2018.
Accessed October 14, 2020. https://www2.deloitte.
com/us/en/insights/industry/health-care/virtual-health-
care-consumer-experience-survey.html.
45. Schickedanz A, Huang D, Lopez A, et al. Access,
interest, and attitudes toward electronic communica-
tion for health care among patients in the medical
safety net. J Gen Intern Med 2013;28(7):914-20.
10.1007/s11606-012-2329-5.
46. Khoong EC, Butler BA, Mesina O, et al. Patient
interest in and barriers to telemedicine video visits
in a multilingual urban safety-net system. J Am Med
Inform Assoc 2021;28(2):349-53. 10.1093/jamia/
ocaa234.
47. Fields J, Cemballi AG, Michalec C, et al. In-home
technology training among socially isolated older
adults:ndingsfromthetechalliesprogram.JAppl
Gerontol 2020;733464820910028. [Online ahead of
print] 10.1177/0733464820910028.
48. Lyles CR, Tieu L, Sarkar U, et al. A randomized trial to
train vulnerable primary care patients to use a patient
portal. J Am Board Fam Med 2019;32(2):248-58.
10.3122/jabfm.2019.02.180263.
49. Grossman LV, Masterson Creber RM, Benda NC,
Wright D, Vawdrey DK, Ancker JS. Interventions to
increase patient portal use in vulnerable popula-
tions: a systematic review. J Am Med Inform Assoc
2019;26(8-9):855-70. 10.1093/jamia/ocz023.
50. Gupti A, Nguyen AM, Chang JE, Lai AY, Berry C,
Shelley DR. Five ways—beyond current policy—to
truly integrate telehealth into primary care practices.
Health Affairs Blog. September 9, 2020. Accessed
October 14, 2020. https://www.healthaffairs.org/
do/10.1377/hblog20200903.597561/full/.
51. Eichner J, Dullabh P. Accessible Health Information
Technology (Health IT) for Populations With Limited
Literacy: A Guide for Developers and Purchasers
of Health IT. Rockville, MD: Agency for Healthcare
Research and Quality, 2007. Accessed October 14,
2020. https://digital.ahrq.gov/health-it-tools-and-
resources/consumer-engagement-and-human-factors/
health-it-literacy-guide.
52. UCSF Center for Vulnerable Populations. Resources
for telehealth at safety net settings. April 24, 2020.
Accessed October 14, 2020. https://cvp.ucsf.edu/tele-
health.
53. Velasquez D, Mehrotra A. Ensuring the growth of
telehealth during Covid-19 does not exacerbate
disparities in care. Health Affairs Blog. May 8, 2020.
Accessed October 14, 2020. https://www.healthaffairs.
org/do/10.1377/hblog20200505.591306/full/.
54. Rodriguez JA, Clark CR, Bates DW. Digital health
equity as a necessity in the 21st Century Cures
Act era. JAMA 2020;323(23):2381-2382. 10.1001/
jama.2020.7858.
PRIMARY CARE IN THE COVID-19 PANDEMIC 255
Improving Health
Communication
for Primary Care
Practitioners During
and After COVID-19
Ramya Pinnamaneni and K. Viswanath
T
he role of communication in primary care draws on a “patient-centered communication”
framework
1
and is generally discussed in the context of building a relationship that inuences
the “expression and interpretation” of messages in interpersonal interactions between patients and
the health care personnel.
2
This should, ideally, lead to the building of trust and openness in con-
versations and disclosures of symptoms and concerns, resulting in easing of anxiety, management
of uncertainty, satisfaction with decisions, adherence to recommended actions such as behaviors
or medical regimens, and improvement in health outcomes. In short, communication in a primary
care setting is not just about an exchange of technical or medical information, but also includes
nontechnical dimensions that aect patients’ experiences and the course of the illness.
With COVID-19, some additional concerns crop up. One, standardized and recommended treat-
ments are emerging much later in the course of the pandemic, which means a greater reliance on
nonpharmaceutical interventions and management of uncertainty because of the “newness” of the
disease. Second, the recent emergence of COVID-19, the evolving science of the disease, and the
resulting lack of information are likely to inuence public trust and openness in the future. Third,
physical distancing and other legally mandated restrictions of movement have impeded the fre-
quency of patient-provider contacts and in-person interpersonal interactions that usually facilitate
communications.
Last, it has become clear that underserved groups, such as those from lower socioeconomic posi-
tion (SEP), people of color, immigrants, those who cannot work remotely, and people in certain
neighborhoods that are segregated, suered disproportionately because of COVID-19.
3-5
As has
been repeatedly documented, it is these same groups that have historically suered disproportion-
ately from disease burden on a range of health conditions.
6
Interestingly enough, it is also well
documented that these same groups are aected by communication inequalities—dierences
in access to, processing of, and capacity to act on information—that have been implicated
in health inequalities.
7
That is, the role of class, place, race, and ethnicity has compounded
already existing inequalities in COVID-19-related health care including health care communi-
cation, though communication may also provide an opening for addressing them more readily
than other factors.
This chapter provides an overview of how communication within and outside the primary
health care system may inuence health care under COVID-19, and what we need to mitigate
the current crisis and improve health care in the future. Where appropriate, we draw from
a national, probability-based sample survey of 1012 Americans aged 18 years and older, on
COVID-19 communication. The survey was administered in July/August 2020 through a panel
to 1822 members, with a response completion rate of 55.5%.
8
Patient-provider interaction and communication during
COVID-19
In the constantly evolving information environment about COVID-19, it is vital for health care
professionals (HCPs) to keep up-to-date with both the science around SARS-CoV-2 and the
public health guidelines. However, no matter how knowledgeable an HCP is, be it a primary
care physician, a nurse, or a specialist, their communication with the patient is of utmost
importance to determine a patient’s adoption of and adherence to preventive health behaviors
or medical recommendations, management of emotions, self-management of chronic condi-
tions, and ultimately health outcomes.
9
Clarity in communication from a physician and expressions of support help in building pa-
tients’ trust and understanding. Primary care practices have an established rapport with their
patients and community. This can result in a benecial exchange of information to address
the concerns and questions of patients, reconcile conicting messages, and facilitate adher-
ence to public health recommendations during the COVID-19 pandemic. The provider-patient
trust also helps improve the disclosure of symptoms, thus improving contact tracing and lim-
iting the spread of COVID-19. In the absence of validated and standardized treatments, this
is extremely important. During these times of fear and anxiety, primary care physicians may
also focus on keeping the essential services and their practice open (virtually or in-person)
while adhering to all safety standards and ensuring that the patients feel safe and heard.
Keeping up-to-date
The newness of the SARS-CoV-2 virus and its infection has led to an immense amount of re-
search to gain more clarity about its spread, treatment, and prevention. Within eight months
of discovery, even a rudimentary search with the term “COVID-19” on PubMed yielded close
to 70,000 papers. A number of papers and preprints have been published and some have been
retracted. Many of the research papers have been contradictory. Systematic reviews have been
slow to come out and authors are recognizing the shortcomings of the reviews, especially
258 PRIMARY CARE IN THE COVID-19 PANDEMIC
concerning rigor and timeliness. In such a situation, how can individual primary care physi-
cians keep themselves updated?
The same question may be raised about the patients. The sheer ood of information across
communication platforms, including health care settings as well as news media and social
media, has resulted in a confused and bewildered audience that has expressed a sense of
information fatigue and avoidance. In a recent nationally representative survey we conducted,
about 25% of the sample of 1012 respondents reported avoiding COVID-19 information. Of
these 25% of respondents, 40% reported being “overwhelmed by all the COVID-19 informa-
tion” and around 40% felt that the “information kept changing anyways.”
Addressing misinformation
COVID-19 is the rst pandemic in the social media era. Almost half of the world population,
about 3.5 billion people, in theory, are online with about one-third of them on social media.
10
Growth in this arena has been rapid. For example, in 2005, just 5% of American adults used
at least one social media platform. By 2011, that share had risen to half of all Americans, and
today 72% of the American public uses some type of social media.
11
While social media is
being used to keep people safe, informed, productive, and connected, at the same time, the
technology is enabling and amplifying an “infodemic” that continues to undermine the global
response and jeopardizes measures to control the pandemic. According to the World Health
Organization (WHO), an infodemic is an overabundance of information, both online and
oine. It includes deliberate attempts to disseminate wrong information to undermine the
public health response and advance the alternative agendas of groups or individuals.
12
Misinformation is a phenomenon of both social media and traditional media. The coverage of
COVID-19 in traditional media outlets has largely amplied the unscientic voices of leaders
across political spectra who have advocated for unproven cures, proposed conspiracy theories
to explain the origins of the coronavirus, and have undermined the impacts of the nonphar-
maceutical public health interventions.
Misinformation about treatments for COVID-19 can prompt people to try cures that can harm
them, while fears and distrust about a possible vaccine could undermine vaccine uptake. False
information can also lead to a decreased observance of preventive strategies such as hand-
washing, distancing, mask wearing, and lockdowns, causing substantive threats to public
health globally. It is important to address misinformation at all levels: individual, community,
national, and global.
In a recent nationally representative survey we conducted, close to 80% of 1012 respondents
were misinformed on some aspect of COVID-19, with most of the confusion being around how
COVID-19 is transmitted. The science of transmission has been evolving over time and it is
understandable that there is confusion, but more importantly, the survey underscored that
people are likely to look to their HCPs for guidance and information on such topics. Patients
and families may expect that primary care settings should be a reliable source of information.
HCPs have long served a learned intermediary function for patients. But the speed at which
misinformation can spread through today’s digital media ecosystem can overwhelm any
PRIMARY CARE IN THE COVID-19 PANDEMIC 259
information gatekeeping, especially during public health emergencies such as a pandemic.
Physicians working individually cannot tackle the totality of misinformation about SARS-
CoV-2, either in the exam room or online. Their time with patients is limited, and few phy-
sicians have social media followings that rival those of celebrities, politicians, and citizen
journalists. It is dicult for physicians and primary care practitioners to chase every bit of
misinformation out there and then try to refute it.
However, the good news is that public condence and trust in physicians remain fairly high.
13
Primary care practitioners are the rst contact point for the general public for health infor-
mation. Given their credibility, it is critical that they do not sit on the sidelines and that they
actively and aggressively intervene whenever it is warranted. Physician organizations can
provide critical support as gatekeepers and as arbiters of fact and evidence-based informa-
tion. This practice has a long history. In 1849, for example, in an eort to curb quack rem-
edies, the American Medical Association (AMA) established a board to enlighten the public in
regard to the nature and danger of such remedies.
14
Individual physicians can help counteract misinformation about SARS-CoV-2 by refuting
misinformation without drawing more attention to it. The empirical evidence on how to
eectively counteract misleading facts is mixed. In general, it is recognized that rebuttals of
misleading information are more eective when they do not repeat the false information.
15
Physicians may also embrace their role with journalists. Physicians as a group have high
credibility and are often a primary source of health news for health journalists.
16
Journalists
are critical gatekeepers and can inuence the availability of information in the media through
this gatekeeping function.
Even if individual physicians do not have a huge media following, they have the ability to
leverage the power of institutions because of their credibility over nonscientic people in the
media.
Risk communication and management of uncertainty
When communicating health and science information to patients and their communities, it
is important that health care providers inform them about risk and how various actions or
inactions either mitigate or increase their risk. Covello denes risk communication as the
“process of exchanging information among interested parties about the nature, magnitude,
signicance, or control of a risk.”
17
By denition, risk is the probability of occurrence of an
event or threat and involves uncertainty, and communication about risk is intended to help
manage uncertainty through actions. Health care providers routinely deal with communica-
tion of risks drawing from genetic, family, lifestyle, and societal backgrounds of patients
and draw on guidelines to recommend actions. Patient reception to risk messages is driven
by a number of factors such as how they perceive risk, including perceived susceptibility and
perceived severity.
18
Perceived susceptibility is the feeling of personal vulnerability to the
threat, while severity deals with the extent to which the patient feels that the consequences of
the threat are severe.
260 PRIMARY CARE IN THE COVID-19 PANDEMIC
One can easily glean the challenge in applying this to the context of COVID-19-related com-
munication in primary health care. Although our understanding of the pathogen and the
health consequences are better understood now, emerging infectious disease by denition
carries a lot of uncertainty, and the COVID-19 pandemic in the early months was no excep-
tion. All aspects of the disease—including how one contracts the pathogen, symptoms, treat-
ments, and potential health consequences—were unclear to start with, which created fraught
conditions within the primary health care context. Standard diagnostic tools such as testing
were dicult to access, which compounded the problem. The dependence on nonpharma-
ceutical interventions such as face coverings, hygiene, and physical distancing became para-
mount, making communication and persuasion more critical. Few tools to aid in communica-
tion and decision-making were available to primary health care providers, which magnied
the problem of uncertainty.
As the scientic community gained further understanding of the pathogen and the ways in
which the disease spread and as the standards for treatment grew, one might speculate that
communication within the primary care setting might have also improved. What is yet to be
tested is the extent to which the larger mis/disinformation environment outside the clinical
settings has aected the interactions between providers and patients and the implications for
health outcomes.
Patient-centered communication in the context of COVID-19
Many physicians face challenges in communicating with patients about serious illnesses.
Although many residents and medical students receive training in evidence-based methods of
communicating with patients with serious illness to support shared decision-making, a crisis
such as the COVID-19 pandemic entails a shift in focus from individual values to population-
based resource allocation in order to maximize the care delivered to the population as a whole.
19
Although the core communication skills of rapport building, assessing the patient’s and fam-
ily’s perspectives, responding empathically, giving information, facilitating understanding,
and participating in shared decision-making by including the patient and family continue to
be fundamental to eective communication through the course of this pandemic,
20
health care
workers have had to adapt. The modied “goals of care” and “breaking bad news” discus-
sions with patients and their families need to factor in the changed COVID-19 circumstances,
such as virtual encounters, explaining triaging of scarce resources, virtually connecting family
and dying patients, and dealing with grief and isolation. Although these communication chal-
lenges seem trivial from a distance, they are taking a toll on the well-being of the health care
workers. The stress and emotional toll associated with such interactions are only now being
explored, and few health care providers were prepared for such discussions with patients and
their families.
21
PRIMARY CARE IN THE COVID-19 PANDEMIC 261

Impact on trust, engagement, and mutual respect
One of the most important roles of the primary care physician network is to serve as trusted
sources of health information for the community. According to a survey of 21,196 individuals
conducted in August 2020 to study the levels of trust in people and organizations “to do the
right thing to handle the COVID-19 outbreak,” doctors, hospitals, scientists, researchers, and
the Centers for Disease Control and Prevention (CDC) ranked high compared to other groups
(Figure 1).
12
Despite the waning amount of trust in each institution, doctors and hospitals still
remain the most trusted sources. Other surveys similarly demonstrated that the public has the
highest trust in physicians or doctors.
22
Now that the COVID-19 vaccines are available, trust in health care providers becomes even
more critical given the general mistrust of vaccines among the American public. For example,
according to a survey by the Pew Research Center, the proportion of Americans who re-
sponded that they will “denitely” get the vaccine decreased from 72% in May 2020 to 51% in
September 2020, thereby raising serious questions about any chances of herd immunity.
23
On
the other hand, childhood immunization remains high, and trust in pediatricians is often the
principal driver of immunization.
At least two factors may inuence the issue of trust in HCPs in the near future. The high
degree of politicization of all things COVID-19 may aect any preventive actions people may
accept and abide with. For example, the same Pew study also shows that respondents who
identify with the Republican Party are much less likely to get the vaccines than those who
identify with the Democratic Party. A second factor is that since in-person interactions are
impeded by physical distancing and other legally mandated restrictions of movement, main-
taining trust and continued engagement could remain a challenge.
Figure 1. Trust in Institutions and Leaders to Manage the COVID-19 Crisis, April to August 2020.
12
WWW.MILBANK.ORG
1
Ap ri l Early May Late May Jun e July August
City Government
State Government
Whit e House
Congress
Donald Tr ump
Joe Biden
CDC
Anthony Fauci
Doctors and hospitals
Scientists and Researchers
Phar maceutical comp ani es
Police
Banks
News media
Social media companies
100%
90%
80%
70%
60%
50%
40%
30%
Trust (some or a lot)
262 PRIMARY CARE IN THE COVID-19 PANDEMIC
Issues of equity
The recognition that COVID-19 led to dierential impact in morbidity and mortality among
dierent people was slow to dawn on our collective psyche. Early on, documentation of
disease spread was limited and data on how it impacted dierent groups were sparse or
nonexistent. This is the classic problem of data absenteeism, in which data on some groups,
especially the underserved and racial and ethnic minorities, are not available or are sparse,
leading to poorer understanding and poorer delineation of how some groups are adversely
aected as well as the conditions and consequences of the adversity.
24
It took several months
after the start of the pandemic to realize that communities with higher proportions of racial
or ethnic minorities, immigrants, higher levels of poverty, and people with daily wage occu-
pations were suering disproportionately more than others, leading to literally deadly conse-
quences among those groups.
3,5
This phenomenon of dierential impact, disparities in health
and well-being, is a continuation of a long history of suering of underserved groups. The
reasons, well documented through copious investigations in health, social epidemiology, and
social and behavioral sciences, include risk factors, disease conditions, and health outcomes
that are aected by factors such as economic disruptions,
25
neighborhoods with limited ser-
vices and poor conditions, access to health care services, education and literacy, low income,
and racism, among many others.
6
All of these factors contributed to the disparities observed
during the COVID-19 pandemic.
Another phenomenon that received only passing and selective attention is that of communica-
tion inequalities. A signicant component of communication inequalities is access to health
care information in parallel to health care services. In the context of COVID-19 these inequities
might manifest in two ways: knowledge about the disease and access to telehealth services.
Research has identied that in times of signicant ows of information, especially in science
and health, people from higher SEPs benet more compared to those from lower SEP groups,
leading to knowledge gaps between the two.
26,27
Given the complexity and the continuing
change in our understanding of the science of COVID-19, one can hypothesize increasing
knowledge gaps among dierent social groups. This might manifest in the form of both “cor-
rect” knowledge as well as misinformation about disease etiology and preventive measures to
avoid contracting the disease. For example, in our recent survey on the role of communica-
tion during COVID-19, we found that misinformation on transmission was more likely to be
believed than conspiracy theories. However, the fact that at least 20% of the 1012 respondents
questioned the value of face masks in preventing COVID-19 suggests that misinformation
persists among some groups.
Some have suggested that health literacy, especially among patients, is important for better
health outcomes. The WHO denes health literacy as the ability of individuals to “gain access
to, understand and use information in ways which promote and maintain good health” for
themselves, their families, and their communities.
28
Poor health literacy is associated with
poor education and low SEP,
29
and given the novelty of COVID-19, this may adversely aect
health outcomes in vulnerable groups until they have learned about the disease, how it aects
them, and how it can be prevented.
PRIMARY CARE IN THE COVID-19 PANDEMIC 263
In this phase of complex and inconsistent information overload, conicting messages and
scientic research are being disseminated directly to the public with limited gatekeeping,
causing the public to get overwhelmed by technical details. This in turn can lead to anxiety
and fear of the unknown. Health care providers can mitigate this by addressing patient and
community concerns and questions and mitigating suspicion and mistrust.
In parallel with the issue of access to health care information lies the issue of access to ser-
vices. In the current COVID-19 crisis, access to primary care was aected by job losses or
temporary furloughs, disruption in transit services on which the poor usually rely, and loss of
insurance coverage, among others. Given the restrictions on physical movement, telehealth
has been proposed and used as a promising solution to promote access. Telehealth increases
convenience for both the physician and the patient while decreasing the risk of exposure to
COVID-19.
But telehealth also has limitations, including the potential to exacerbate health disparities.
30
Patients face three overlapping barriers to accessing telehealth: the absence of technology,
digital literacy, and reliable Internet coverage. Together, these barriers make up the digital
divide, which disproportionately aects older people of color and those with low socioeco-
nomic status.
31
Older and Black patients are much less likely to use their patient portal sites,
where patients and physicians can communicate, than younger and white patients.
32
This is
especially more problematic in areas and communities where physicians are shutting down
outpatient clinics and delivering care exclusively through phones and computers.
Post-COVID-19 future
Where do we go from here? There is no question that the novel SARS-CoV-2 and consequently
COVID-19 have disrupted our lives in ways that one could not have imagined previously.
Along with almost every social institution, primary care has been severely disrupted even
while the burden to address the disease and expectations have increased multifold. Globally,
primary care is the rst point of contact between the community and the health system, and
as such, it has been at the forefront of COVID-19 care and prevention. As COVID-19 becomes
part of the “new normal,” primary care health care providers will be expected to address a
range of health care problems caused not just by COVID-19 but also other routine missed
services. Amidst several factors that take disease control out of the primary care setting, com-
munication with patients and families will be central to managing health care.
As of now, there are few empirical studies that actually document how patient-centered com-
munications in primary care health settings have been aected by COVID-19, and it will have
to become a high priority for future work. A few areas where communications will be critical
are described here.
First, communication and negotiations on such critical and delicate issues as triaging of
patients and resource reallocation—including chronic disease management, screenings, and
immunizations—as well as treatment decisions and delivery of bad news, which have always
been dicult, will be much more so post-COVID-19.
264 PRIMARY CARE IN THE COVID-19 PANDEMIC
While keeping track of the research, treatment, and vaccines, it is also crucial for physi-
cians to be aware of the epidemiological trends in the spread of the novel SARS-CoV-2 virus
and the hotspots in their coverage area. By staying informed, physicians can prepare for an
outbreak, take up surveillance, and disseminate mitigation measures. The physicians should
adequately communicate the resources and preparedness plans with the sta and the com-
munity. Following the COVID-19 resource centers and guidelines or bulletins issued by the
WHO, the CDC, physician organizations such as the AMA and the American Academy of Family
Physicians, the primary care practice, and the local city and state public health departments
could be helpful.
The unusual politicization of COVID-19 means that there will be continued resistance among
certain pockets of citizenry to medically and scientically informed recommendations. One
of the most potentially politically fraught subjects will be that of COVID-19 vaccine uptake.
Preparing the public for COVID-19 vaccinations, building up vaccine condence, and improv-
ing vaccine uptake will remain a time-consuming challenge for health care providers.
Telehealth is likely to become more appealing and may very well grow as a critical platform
for health care delivery. Leaving aside infrastructural and economic problems that need to be
addressed, how telehealth will aect patient-provider interactions and implications for health
outcomes will have to be a focus of empirical work.
Considerations of future physician trainings in some selected areas will have to take into
account severe illness communication and end-of-life communication in resident trainings,
with assessments. While COVID-19 is raging, online communication skills instruction and
workplace learning for residents and trainee physicians become vitally important.
An issue that deals less with patients but is critical within the primary care setting is the
well-being of health care workers who have had to face the brunt of managing the pandemic
on the front lines with inadequate safeguards, protections, and information. How these con-
versations are opened, managed, and resolved will become a critical area to investigate.
Last, equity or the lack of it will remain a if not the central issue. COVID-19 has taught us
once more that existing disparities, if not addressed with urgency, will compound, leading
to needless deaths and suering. That this has even become an issue speaks to the collective
failure of the system, requiring urgent answers.
PRIMARY CARE IN THE COVID-19 PANDEMIC 265
References
1. Epstein RM, Street RL Jr. Patient-centered communi-
cation in cancer care: promoting healing and reduc-
ing suffering. No. 07-6225. Bethesda, MD: National
Cancer Institute, 2007. https://cancercontrol.cancer.
gov/sites/default/les/2020-06/pcc_monograph.pdf.
2. Duggan A, Street RL Jr. Interpersonal communication
in health and illness. In: Glanz K, Rimer BK, Viswa-
nath K, eds. Health behavior: theory, research, and
practice. 5th ed. San Francisco, CA: Jossey-Bass,
2015:243-67.
3. Clark E, Fredricks K, Woc-Colburn L, Bottazzi
ME, Weatherhead J. Disproportionate impact of
the COVID-19 pandemic on immigrant commu-
nities in the United States. PLoS Negl Trop Dis
2020;14(7):e0008484. 10.1371/journal.pntd.0008484.
4. Bassett MT, Chen JT, Krieger N. Variation in racial/
ethnic disparities in COVID-19 mortality by age in
the United States: a cross-sectional study. PLoS
Med 2020;17(10):e1003402. 10.1371/journal.
pmed.1003402.
5. Krieger N, Waterman PD, Chen JT. COVID-19 and
overall mortality inequities in the surge in death
rates by zip code characteristics: Massachusetts,
January 1 to May 19, 2020. Am J Public Health
2020;110(12):1850-2. 10.2105/AJPH.2020.305913.
6. Braveman P, Egerter S, Williams DR. The social
determinants of health: coming of age. Annu Rev
Public Health 2011;32:381-98. 10.1146/annurev-
publhealth-031210-101218.
7. Viswanath K, Ramanadhan S, Kontos EZ. Mass
media. In: Galea S, ed. Macrosocial determinants of
population health. New York, NY: Springer, 2007:275-
94.
8. Bekalu MA, Dhawan D, McCloud R, Pinnamaneni
R, Viswanath K. Adherence to COVID-19 mitiga-
tion measures among American adults: the need for
consistent and unied messaging. Health Educ Res
2021; published online Jan 26. 10.1093/her/cyab002.
9. Street RL, Makoul G, Arora NK, Epstein RM. How
does communication heal? Pathways linking clini-
cian–patient communication to health outcomes.
Patient Educ Couns 2009;74(3):295-301. 10.1016/j.
pec.2008.11.015.
10. Ortiz-Ospina E. The rise of social media. Our World
in Data. September 18, 2019. Accessed October 26,
2020. https://ourworldindata.org/rise-of-social-media.
11. Social media fact sheet. Pew Research Center. June
12, 2019. Accessed October 26, 2020. https://www.
pewresearch.org/internet/fact-sheet/social-media/.
12. Managing the COVID-19 infodemic: promoting
healthy behaviours and mitigating the harm from
misinformation and disinformation. World Health
Organization. September 23, 2020. Accessed
October 26, 2020. https://www.who.int/news/item/23-
09-2020-managing-the-covid-19-infodemic-promot-
ing-healthy-behaviours-and-mitigating-the-harm-from-
misinformation-and-disinformation.
13. Baum MA, Lin J, Ognyanova K, et al.; the COVID
States Project. The state of the nation: a 50-state
COVID-19 survey, report #13: public trust in institu-
tions and vaccine acceptance. OSF Preprints. Sep-
tember 15, 2020. Accessed October 28, 2020. https://
osf.io/qzsxn/.
14. AMA History. American Medical Association. Ac-
cessed October 24, 2020. https://www.ama-assn.org/
about/ama-history/ama-history.
15. Ecker UKH. Why rebuttals may not work: the psychol-
ogy of misinformation. Media Asia 2017;44(2):79-87.
10.1080/01296612.2017.1384145.
16. Viswanath K, Blake KD, Meissner HI, et al. Occu-
pational practices and the making of health news:
a national survey of US health and medical science
journalists. J Health Commun 2008;13(8):759-77.
10.1080/10810730802487430.
17. Covello VT. Risk communication: an emerg-
ing area of health communication research.
Ann Int Commun Assoc 1992;15:359-73.
10.1080/23808985.1992.11678816.
18. Skinner CS, Tiro J, Champion VL. The health belief
model. In: Glanz K, Rimer BK, Viswanath K, editors.
Health behavior: theory, research, and practice. 5th
ed. San Francisco, CA: Jossey-Bass, 2015:75-94.
19. Crisis standards of care: a systems framework for
catastrophic disaster response. Washington, DC: The
National Academies Press, 2012. 10.17226/13351.
20. Rubinelli S, Myers K, Rosenbaum M, Davis D.
Implications of the current COVID-19 pandemic for
communication in healthcare. Patient Educ Couns
2020;103(6):1067-9. 10.1016/j.pec.2020.04.021.
21. Benedek DM, Fullerton C, Ursano RJ. First respond-
ers: mental health consequences of natural and
human-made disasters for public health and public
safety workers. Annu Rev Public Health 2007;28:55-
68. 10.1146/annurev.publhealth.28.021406.144037.
22. Earnshaw VA, Eaton LA, Kalichman SC, Brousseau
NM, Hill EC, Fox AB. COVID-19 conspiracy beliefs,
health behaviors, and policy support.Transl Behav
Med 2020;10(4):850-6. 10.1093/tbm/ibaa090.
266 PRIMARY CARE IN THE COVID-19 PANDEMIC
23. Tyson A, Johnson C, Funk C. U.S. public now di-
vided over whether to get COVID-19 vaccine. Pew
Research Center. September 17, 2020. Accessed
October 31, 2020. https://www.pewresearch.org/
science/2020/09/17/u-s-public-now-divided-over-
whether-to-get-covid-19-vaccine/.
24. Lee EWJ,Viswanath K. Big data in context: ad-
dressing the twin perils of data absenteeism and
chauvinism in the context of health disparities
research. J Med Internet Res 2020;22(1):e16377.
10.2196/16377.
25. Stuckler D, Basu S. The body economic: why auster-
ity kills. New York: Basic Books, 2013.
26. Tichenor PJ, Donohue GA, Olien CN. Mass me-
dia ow and differential growth in knowledge.
Public Opinion Quarterly 1970;34(2):159-70.
10.1086/267786.
27. Viswanath K, Finnegan JR. The knowl-
edge gap hypothesis: twenty-ve years later.
Ann Int Commun Assoc 1996;19:187-228.
10.1080/23808985.1996.11678931.
28. Nutbeam D. Health promotion glossary. Health
Promotion International 1998;13(4):349-64. 10.1093/
heapro/13.4.349.
29. Sørensen K, Van den Broucke S, Fullam J, et al.
Health literacy and public health: a systematic review
and integration of denitions and models. BMC Public
Health 2012;12:80. 10.1186/1471-2458-12-80.
30. Viswanath K, Nagler RH, Bigman-Galimore CA,
McCauley MP, Jung M, Ramanadhan S. The com-
munications revolution and health inequalities in the
21st century: implications for cancer control. Cancer
Epidemiol Biomarkers Prev 2012;21(10):1701-8.
10.1158/1055-9965.EPI-12-0852.
31. Velasquez D, Mehrotra A. Ensuring the growth of
telehealth during COVID-19 does not exacerbate
disparities in care. Health Affairs Blog. May 8, 2020.
Accessed October 26, 2020. https://www.healthaf-
fairs.org/do/10.1377/hblog20200505.591306/full/.
32. Walker DM, Hefner JL, Fareed N, Huerta TR, McAle-
arney AS. Exploring the digital divide: age and race
disparities in use of an inpatient portal. Telemed J E
Health 2020;26(5):603-13. 10.1089/tmj.2019.0065.
PRIMARY CARE IN THE COVID-19 PANDEMIC 267
Undocumented
Immigrants in the
United States in the
Time of COVID-19
Kathleen R. Page
T
he COVID-19 epidemic in the United States has disrupted both preventive and therapeutic care
for many people in the country. While health plans and practitioners increasingly focused on
maintaining the health of existing primary care patients at a time when in-person visits were
mostly canceled, the health care needs of undocumented immigrants—many of whom lacked
insurance or a relationship to a medical home, and had chronic conditions such as diabetes mel-
litus—were largely overlooked. As the COVID-19 epidemic expanded throughout the country,
undocumented immigrants became increasingly at risk for delays in routine health care, infection
with COVID-19, and poor access to COVID-19 testing and treatment.
As the epidemic unfolded, it became increasingly evident that undocumented immigrants were at
heightened and disproportionate risk for morbidity and mortality from COVID-19. The dispropor-
tionate impact of the disease on this community was caused by multiple factors, among them oc-
cupational exposures, marginalization, poverty, and systematic exclusion from safety-net benets,
including health care. The epidemic highlighted key challenges to care for undocumented immi-
grants—the digital divide, language barriers, immigration fears, and lack of familiarity navigating
the health care system—that exacerbated preexisting health disparities between undocumented
immigrants and more privileged populations in the United States.
The epidemic also highlighted the profound individual, societal, and public health cost of sys-
tematically excluding populations from the safety net, while presenting unique opportunities to
expand access to primary care for all, including for undocumented immigrants. Addressing the
challenges to care for undocumented immigrants through innovations in how primary care is
delivered, including through modication and tailoring of academic-community partnerships and
telemedicine solutions, can enhance primary care access in underserved areas and for people with
limited English prociency, ensuring exibility of service at lower cost while addressing the
digital divide. In this chapter, we review health care access barriers facing undocumented
immigrants, particularly highlighting issues of insurance coverage and primary care delivery
strategies, key initiatives to improve access and delivery, and how COVID-19 has shined light
on areas to focus our attention to improve primary care outcomes among undocumented im-
migrants in the United States.
Undocumented immigrants and access to care
There are an estimated 10.2 million undocumented immigrants in the United States, a decline
from a peak of 12.2 million in 2007.
1
The majority, 8.1 million, are from Latin America (65%
from Mexico and Central America), and 1.45 million (13.8%) are from Asia.
2
Over the past
two decades, the undocumented immigrant population has matured; 66% have lived in the
United States for more than a decade, and it is estimated that 5.1 million children, the major-
ity US-born (79%), live with an undocumented immigrant parent in the United States.
3
Nearly
half of undocumented immigrants live in New York, California, and Texas, but there has been
increasing dispersion, with “emergent” communities appearing throughout the country.
4
Capacity to provide culturally and linguistically appropriate services is often limited in emer-
gent Latino communities, and has been particularly strained during the COVID-19 pandemic.
Both the changes in the numbers of undocumented immigrants and their areas of residence
within the United States aect access to and delivery of health care. The decline in tempo-
rary and rise in permanent migration, in part driven by enhanced border enforcement that
makes it dicult for migrants to travel back and forth from their country of origin, means
that many undocumented migrants are laying down roots, establishing families, and aging in
the United States. Almost three-quarters of undocumented immigrants are younger than 45
years of age, but the proportion of older adults is growing and it is estimated that 1.3 million
undocumented immigrants are over 55 years of age.
5
In addition, despite high participation in
the labor force, undocumented immigrants suer signicant structural and social disadvan-
tages that can aect health care access and delivery. Almost half do not speak English, half
do not have a high school degree, and more than half live below the 200% poverty level.
5
The
rapid growth of the undocumented immigrant population in areas of the country with limited
infrastructure and capacity to provide linguistically and culturally appropriate services can
also limit access to care.
Health policy exclusions
We argue that a barrier to health care for undocumented immigrants is their systematic
exclusion from safety-net programs. The Personal Responsibility and Work Opportunity
Reconciliation Act (PRWORA) passed in 1996 dramatically altered social benet programs
and excluded undocumented immigrants from receiving benets other than public health or
emergency health services required by the 1986 Emergency Medical Treatment and Labor Act
(EMTALA).
6,7
As a result, many immigrants avoid medical care unless absolutely essential to
avoid high out-of-pocket costs.
270 PRIMARY CARE IN THE COVID-19 PANDEMIC
The Aordable Care Act
Until the full implementation of the Aordable Care Act (ACA) in 2014, lack of health insur-
ance was common among both US citizens and noncitizens. The ACA almost halved the
number of uninsured adults, from more than 46 million in 2010 to less than 27 million in
2016, though these gains have started to reverse in recent years, and coverage varies by
state depending on the degree to which the state decided to expand Medicaid to low-income
households.
8
The ACA also enhanced coverage for some immigrants.
9
Refugees, asylees, and
legal permanent residents, for example, were permitted to enroll in the ACA, and those who
met income eligibility criteria could be covered through Medicaid or the Children’s Health
Insurance Program (CHIP).
8
Legal permanent residents, however, had a ve-year waiting pe-
riod prior to eligibility, although some states waived the waiting period for pregnant women
and children.
8,10
Immigrants with Temporary Protected Status (TPS)—granted to approxi-
mately 317,000 individuals from designated countries where armed conict, environmental
disasters, and other situations prevent safe return—could purchase insurance through the
ACA marketplaces but were not eligible for Medicaid/CHIP coverage.
8,11
By contrast, undocumented immigrants have not been eligible for coverage under Medicaid/
CHIP or able to purchase health insurance through the ACA marketplaces. Recipients of
Deferred Action for Childhood Arrivals (DACA), which provides temporary work permits and
protection from deportation to immigrants who arrived in the United States before their 16th
birthday, have likewise been excluded from the ACA marketplaces, Medicaid, and CHIP.
10,12
As of March 2020, there were 643,540 DACA recipients, all of them under 40 years of age (as
only people under the age of 31 years by June 15, 2012, could apply).
13
ACA exclusions have inevitably widened disparities in health care coverage. Undocumented
immigrant adults are nine times more likely to be uninsured than US citizens and almost
twice as likely to lack health care coverage as legal permanent residents.
8
The disparity be-
tween undocumented immigrants and others living in the United States is also evident among
undocumented children, who are eight times more likely to be uninsured than children who
are US citizens.
8
Low-income adults and children are most likely to be left out of health care
coverage. It is estimated that 45% of undocumented immigrants lack health care insurance.
8
Although some immigrants have limited access to employer-sponsored coverage or may be
able to purchase private insurance, these options are typically limited to higher-income earn-
ers or those working in companies that oer employer-sponsored insurance.
Employer-based coverage
Even prior to the ACA, gaps in health care coverage between undocumented immigrants and
US citizens could be largely explained by variability in employer-based coverage and the type
of occupations performed by low-income undocumented immigrants.
14
Approximately 7.8
million undocumented immigrants participate in the US labor force, and the vast majority of
undocumented immigrants (over 80%) live in families with at least one full-time worker.
15
Despite high employment rates, 60% of undocumented immigrants have incomes below the
200% federal poverty level.
5
This is largely explained by their disproportionate representation
PRIMARY CARE IN THE COVID-19 PANDEMIC 271
in low-wage occupations in the service industry, agricultural workforce, and construction
sectors.
5
Many undocumented immigrants work in the informal and unregulated sector as
“jornaleros,” day laborers or migrant farmworkers, performing dangerous jobs with few
protections, low wages, employer abuse, wage theft, and limited options for recourse.
16
Even
those working in regular occupations face discrimination and unsafe working conditions, but
rarely report violations of employment law due to concerns about immigration repercussions,
language barriers, and limited knowledge of worker protection laws. These conditions con-
tribute to exploitation and make access to employer-based health care coverage an exception
rather than the rule.
Health coverage at the local level
Some states and local jurisdictions have established special programs to provide health care
coverage for undocumented immigrants. For example, California, Illinois, Massachusetts, New
York, Oregon, Washington, and the District of Columbia use state or district funds to provide
health care coverage for all income-eligible children, regardless of immigration status.
10
In
2019, Mayor Bill de Blasio of New York City announced a program expected to spend $100
million annually to oer health care coverage to all low-income New York City residents,
including undocumented immigrants. California’s state government announced a plan to
oer health care coverage to an estimated 90,000 low-income undocumented adults up to the
age of 25.
17,18
New York, California, Massachusetts, and Washington, DC, have also extended
Medicaid/CHIP coverage to DACA recipients.
10,12
Health system barriers
Despite recent initiatives, almost half of undocumented immigrants remain uninsured.
Uninsured undocumented immigrants primarily rely on Federally Qualied Health Centers
(FQHC) or community clinics for primary care, public health clinics for specic services, or
emergency departments for urgent care needs. In the United States, there are 1,362 registered
FQHCs operating almost 12,000 service delivery sites.
19
These sites provide sliding-scale
payment options for low-income individuals and provide services regardless of immigration
status. Unfortunately, the demand for primary care sites exceeds the supply, with regional
variations in the degree of demand-supply mismatch. Urban areas have a higher concentra-
tion of FQHCs, and there is signicant state-to-state variability in FQHC access, quality,
and outcomes, with general improvements in access, quality, and outcome indicators among
states that expanded Medicaid following the ACA.
19-22
Beyond health care insurance, key features of health care systems can present barriers to ac-
cessible primary care for undocumented immigrants. Access to language services or bilingual
providers for patients with limited English prociency (LEP) can be a signicant challenge
for undocumented immigrants at these and other health care sites, especially in “emerging”
destinations where such immigrants have not traditionally resided. In a recent survey, fewer
than 50% of LEP Spanish-speaking callers in emerging destinations were able to make an
appointment at an FQHC, compared to more than 80% among English speakers.
23
In addi-
tion to language barriers, lack of familiarity with the system can make it dicult to navigate.
272 PRIMARY CARE IN THE COVID-19 PANDEMIC
Perceptions of health and disease may prioritize seeking care for acute conditions rather than
seeking preventive care. Practical considerations such as lack of transportation, conict with
work hours, and diculty nding child care can also limit access to care. Institutional racism,
discrimination, and cultural insensitivity can dissuade immigrants from seeking care.
24
Anti-immigrant policy and access to health care
Explicit anti-immigrant policies and rhetoric in the political sphere can have a further “chill-
ing eect” on health care utilization.
25
Perceived or real fear of deportation when interacting
with governmental agencies and health care institutions has led to reduced uptake of safety-
net services, even among people who are eligible for such services. After implementation of
the ACA, for example, eligible individuals living in mixed-status families (where some rela-
tives are undocumented) in nonexpansion Medicaid states had the lowest health insurance
uptake.
26
Similarly low insurance uptake was observed among US-born children with immi-
grant parents. Heightened immigration enforcement has been associated with lower Medicaid
participation among citizen children with noncitizen parents, who are twice as likely to be
uninsured compared to children with citizen parents.
8,27
Conversely, protection from deporta-
tion can have a “warming eect,” as is evident in the higher participation in the Women,
Infants, and Children (WIC) program among citizen children of DACA-eligible mothers.
28
Disincentives to receive care have been particularly acute during COVID-19 due to the
Inadmissibility on Public Charge Grounds,
29
which went into eect on February 24, 2020, as
the COVID-19 epidemic began. Since the 1800s, US immigration law has restricted admis-
sion of individuals unable to care for themselves without becoming public charges, and the
1996 Personal Responsibility and Work Opportunity Reconciliation Act states that immigrants
must be self-sucient. The 2020 public charge rule, however, provides specic guidance on
implementation, indicating that participation in a broad array of social service programs can
be used as evidence against applications to become a permanent resident of the United States.
In particular, the rule change in 2020 added the use of Medicaid coverage for non-pregnant
adults and certain nutrition and housing programs to the list of programs that could be used
to deny a permanent residency application. Although the rule applies primarily to permanent
resident applicants, a path not readily available to most undocumented immigrants, it caused
ripple eects throughout immigrant communities. Findings from a national survey of com-
munity health centers revealed that as the public charge rule circulated through the court
system,
30
many immigrants (including a broader group than those targeted by the rule) did
not enroll in Medicaid even if eligible. Clinics also reported that patients were hesitant about
disclosing personal information, delayed their engagement with prenatal care, and feared that
services beyond those included in the rule would be aected, such as WIC and school lunch
programs. In the 2018 nationally representative Well-Being and Basic Needs Survey, 20.7%
of adults in low-income immigrant families reported reduced participation in noncash public
benet programs for fear of disqualication from eventually obtaining permanent residency
status.
31
There are an estimated 8.3 million children with at least one non-citizen parent en-
rolled in Medicaid/CHIP or receiving SNAP benets who could be at risk of losing benets.
30,32
PRIMARY CARE IN THE COVID-19 PANDEMIC 273
The perfect storm: Limited access to care, undocumented
status, and COVID-19
Although having health insurance does not guarantee that people will have a medical home,
there is strong evidence that having insurance greatly facilitates access to primary care.
Uninsured children, for example, are much less likely to have a usual source of care or to have
seen a provider in the last year and are more likely to forgo needed medical or dental care.
33
Models estimate that lack of insurance explains 25%-40% of disparities in preventive care
between non-elderly adults with incomes below the 400% federal poverty level and those
with higher incomes.
34
Following ACA implementation, an analysis of a nationally representa-
tive sample of non-elderly adult patients receiving care at community health centers found
that those without insurance were more likely to live under 200% of the federal poverty level,
be foreign-born, have limited English prociency, be Latino, and be less likely to receive
necessary medical care, including preventive care and follow-up for abnormal cancer screen-
ing tests.
35
Early detection of cancer, heart disease, diabetes, and other chronic conditions can
promote healthier lifestyles and better disease management. Although proving that health
insurance saves lives has been dicult, in part because death is a rare outcome in non-elderly
adults, evidence from quasi-experimental studies conrms lower use of preventive services
among the uninsured and trends toward lower survival for select conditions.
36
National data on COVID-19 mortality and insurance status or access to primary care has not
been published (and may not be readily available), but the experience of clinicians caring for
COVID-19 patients strongly suggests that health insurance and primary care were important
contributors to racial/ethnic disparities in COVID-19 outcomes, including mortality. As has
been widely reported, African Americans and Latinos have borne a disproportionate burden
of COVID-19 incidence and mortality. Among Latinos, the rate of COVID-19 is more than
three times higher than in non-Hispanic whites, and the age-adjusted hospitalization rate
more than four times higher (160.7 vs. 40.1 per 100,000).
37
The disparities have been particu-
larly stark among younger individuals. For example, 34.9% of Latino individuals who died
of COVID-19 were less than 65 years of age, compared to 13.2% of non-Hispanic whites.
38
Almost half (44.6%) of COVID-19 patients less than 21 years of age have been Latino.
39
Access to health care and health insurance impacted when and how undocumented immi-
grants presented to care during the COVID-19 epidemic. Patients without health insurance
or primary care providers delayed access to care until they became severely ill.
40
Fear of high
medical bills, lack of familiarity with the health system, institutional mistrust, and concern
about the public charge rule dissuaded many from seeking care unless severely ill. In a mul-
tistate survey of 350 individuals diagnosed with SARS-CoV-2, Latinos were more than twice
as likely as whites to have been admitted to the hospital with severe COVID-19.
41
Among 326
patients admitted with COVID-19 to Massachusetts General Hospital between March 14 and
April 20, 2020, Spanish-speaking Latino patients were more likely to have more severe dis-
ease on chest imaging associated with delayed presentation to care.
42
Lack of health insurance may also have exacerbated the risk of severe COVID-19 from
untreated underlying conditions commonly addressed in the primary care setting. The
274 PRIMARY CARE IN THE COVID-19 PANDEMIC
prevalence of diabetes mellitus, for example, is higher among Latinos than among most other
race/ethnic groups in the United States.
43
Undiagnosed diabetes is also more prevalent among
Latinos than non-Latinos, especially among individuals from Mexico and Central America.
42
Undocumented immigrants with diabetes are less likely to have seen a health care provider in
the last six months or ever compared to documented immigrants.
44
Clinical experience sug-
gests that COVID-19 unmasked previously undiagnosed diabetes among many undocumented
patients without a medical home. The Johns Hopkins Health System, for example, partnered
with community clinics to ensure continued diabetes care among Spanish-speaking patients
newly diagnosed with diabetes during their admission for COVID-19.
Though Latino populations have been disproportionately represented in terms of COVID-19
infections, the overall statistic of Latino prevalence does not provide sucient granularity to
fully understand the drivers of these disparities. The Latino population in the United States,
for example, is highly heterogenous: 67% are US born and 79% are US citizens, but foreign-
born Latinos have lower socioeconomic/educational attainment and access to health care.
8,40
These factors heavily impacted the risk of COVID-19 infection among some Latinos. Although
systematic data collection is missing, clinical experience as well as review of the lay press
demonstrate the particularly high toll of COVID-19 among undocumented immigrants.
40
At
the Johns Hopkins Health System, for example, almost 70% of Latino patients admitted to
the hospital had limited English prociency, and between March 11 and May 25, 2020, the
SARS-CoV-2 positivity rate among Latinos was 42.6% compared to 17.6% and 8.8% among
non-Hispanic Black and white patients, respectively.
46
Community testing at a high-density
foreign-born Latino neighborhood from June to October 2020 showed persistent dispari-
ties (SARS-CoV-2 positivity rate of 33% among Latinos compared to 3% for whites), and
higher likelihood of having limited English prociency among Latinos with a positive test.
In this setting, 75% of Latino patients diagnosed with COVID-19 had no primary care pro-
vider. Serologic studies in other areas of the country are also nding evidence of high rates
of infection in areas with large foreign-born Latino populations.
47-49
Data on non-Latino
undocumented immigrants is lacking altogether. This data gap is worrisome and the risk of
COVID-19 among non-Latino undocumented immigrants may not be easily discernible in ag-
gregate statistics by race/ethnicity due to relatively low representation at a population level.
The high infection rates observed among undocumented immigrants is fundamentally rooted
in the systematic exclusion from benets, political disempowerment, and systemic racism
that perpetuate poverty among undocumented immigrants despite their high employment
rates. As the COVID-19 epidemic accelerated in the United States and unemployment levels
rose precipitously, the Coronavirus Aid, Relief, and Economic Security (CARES) Act extended
unemployment relief to contractors and other workers not ordinarily eligible, and a $1,200
stimulus check was sent to individuals with a social security number who met income eli-
gibility.
50,51
Undocumented immigrants, however, were ineligible for either of these benets
and the stimulus check was withheld from any individual living with undocumented family
members. Low-income Latinos were heavily impacted by the economic downturn related to
COVID-19; approximately 60% lived in households that experienced job losses or pay cuts,
and 70% had no emergency funds to cover three months of living expenses.
52
Undocumented
immigrants often support more than one family and have remittance obligations, and those
PRIMARY CARE IN THE COVID-19 PANDEMIC 275
living in states without access to driver’s licenses face additional obstacles to opening bank-
ing and savings accounts.
53
The pressure to generate income was so acute that undocumented immigrants continued to
work even in the peak of the pandemic, often without adequate occupational protections,
and with limited options to demand their rights. The fear of losing a job dissuaded those
with symptoms from seeking care unless extremely ill, placing coworkers at risk, especially
in spaces where distancing was not possible or where transportation to and from work was
shared, as happened in the meat and poultry industry.
54,55
In addition, crowded living condi-
tions, common among immigrants who have to share rent for aordable housing, fueled
ongoing transmission in households were isolation was simply not feasible.
41
For further
discussion on the health challenges faced by migrant workers, see the chapter titled Migrant
Worker Health and Health Care in COVID-19.
Opportunities and challenges
The devastating impact of COVID-19 among undocumented immigrants should galvanize
society and the health system to capitalize on new opportunities to promote health equity and
expand access to primary care. The impact on undocumented immigrants was tragic at an
individual and community level, but it has broader implications and ripple eects for public
health and the economy at large. Ignoring the deep problems revealed by the disproportionate
impact of COVID-19 on undocumented immigrants will continue to impact society as a whole.
Linkage to primary care
An obvious rst step is to facilitate access to COVID-19 testing, follow-up, and linkage to
primary care to address underlying chronic conditions and potential long-term COVID-19
complications. At the Johns Hopkins Health System, for example, several partnerships were
formed to facilitate access to care and promote continuity of care for undocumented immi-
grants. Early in the epidemic, Johns Hopkins partnered with a trusted community organiza-
tion with extensive experience serving undocumented immigrants to establish a COVID-19
hotline. Patients meeting COVID-19 testing criteria were referred to Johns Hopkins for test-
ing, with telemedicine follow-up for those patients testing positive but not having a primary
care provider. Johns Hopkins partnered with community-based clinics to facilitate warm
transfer of patients from the COVID-19 provider to a primary care provider, and reserved pri-
mary care at hospital-based primary care clinics for the subset of patients who had complex
medical conditions requiring care coordination among multiple specialties. The Johns Hopkins
After Care Clinic provided an additional resource to ensure timely follow-up for patients
discharged with COVID-19 from the emergency department, until the transition to primary
care was established.
56
The transition to primary care practices relied heavily on a charity program, The Access
Partnership (TAP), a charity program established by Johns Hopkins in 2009 to provide access
to eective, compassionate, evidence-based primary and specialty care for uninsured and
underinsured residents in the hospitals’ catchment area.
57-59
TAP’s long-standing agreement
276 PRIMARY CARE IN THE COVID-19 PANDEMIC
with community-based clinics facilitated access to specialty care for uninsured patients, free
of charge, at Johns Hopkins. Bilingual and bicultural TAP patient navigators collaborated
closely with medical teams and social workers to coordinate care. The TAP workow relied
heavily on existing and mutually benecial partnerships between Johns Hopkins and commu-
nity clinics, including FQHCs. In the TAP model, limited capacity in hospital-based primary
care clinics was reserved for complex cases, but specialty care was facilitated for patients from
partnering community clinics. For basic primary care needs, patients were linked to com-
munity clinics that can best serve their needs. TAP’s patient-centered approach prioritized
patient convenience (e.g., clinic location and proximity) and other social determinants. For
example, patients with housing instability, substance use disorder, limited English procien-
cy, and/or immigration-related concerns were preferentially linked to clinics with expertise
and resources to address these issues.
Having existing programs and community relationships with clinics that serve undocumented
immigrants was critical to the success of the TAP initiative during a time of crisis, and
these relationships should be strengthened for the long run. The electronic medical record,
for example, could be used to alert care teams that a patient does not have a primary care
home, triggering multidisciplinary collaboration, including social work, to facilitate access.
Implementation and systems innovations from other chronic conditions can be adapted to
monitor outcomes. The HIV continuum of care cascade, for example, which tracks patient en-
gagement steps from HIV diagnosis to virologic suppression, could be applied to track prog-
ress in primary care engagement, especially for patients with underlying chronic conditions.
60
Given the risk of severe COVID-19 in patients with diabetes, COVID-19 testing could be paired
with point-of-care hemoglobin A1C measurements (for the diagnosis and evaluation of dia-
betes glycemic control) to prioritize rapid linkage to care for patients diagnosed with diabetes
and out of care. An approach emphasizing follow-through would monitor patient attendance
to the primary care home and, ultimately, disease outcome metrics such as glycemic control.
Telemedicine to improve access
The rapid increase in utilization of telemedicine services during COVID-19 presents another
opportunity to enhance access to primary care for undocumented immigrants. While over-
reliance on telemedicine could exacerbate health disparities among patients with limited
technology literacy or access to Internet, computers, and phones, when used appropriately,
telemedicine can be an important adjunct and facilitate patient engagement and care. For
example, telemedicine can provide added exibility for patients without transportation or
for patients living far from primary care sites or in remote areas. For patients with inex-
ible work schedules or child care responsibilities, the option to call into a visit may be more
convenient and reduce time and opportunity costs of an in-person visit. Seasonal workers and
migrant laborers could also benet if able to maintain continuity of care with one provider
using telemedicine as they move for work.
Telemedicine could also increase access to provider-patient language-congruent care. While
language access services are essential to the care of patients with limited English pro-
ciency, it is well documented that having a language-congruent provider improves patient
PRIMARY CARE IN THE COVID-19 PANDEMIC 277
communication, satisfaction, patient-centeredness, and trust in the provider.
61-63
Emergent
cities with rapidly growing immigrant populations often struggle to scale up bilingual and
bicultural capacity in the service sector to meet increasing demands. Telemedicine makes
it possible to leverage existing capacity in other regions with more established immigrant
populations, and could be useful for scarce services that are dicult to provide through third-
party translation. Mental and behavioral health, for example, are best provided by linguisti-
cally and culturally congruent providers who understand the cultural nuances and perspec-
tives of mental health across diverse populations. Undocumented immigrants are at high risk
of exposure to traumatic events, whether in their country of origin, during the migration
journey, or on arrival to the United States. Discrimination, stress, economic insecurity, and
the impact of COVID-19, among other factors, can exacerbate depressive and stress-related
conditions.
64
Access to mental health services is notoriously limited for uninsured patients with
limited English prociency. Telemedicine could help address some of these challenges. A small
pilot program oering telemedicine cognitive behavioral therapy to Latina adolescents suer-
ing from post-traumatic stress disorder revealed high engagement, and parents of the patients
reported fewer logistic barriers to care, including fewer transportation, child care, and work
schedule conicts.
65
There are barriers to telehealth that predominantly impact the lowest-income and most
vulnerable patients, which must be overcome for a telemedicine approach to primary care ac-
cess to be successful for undocumented immigrants. Many in this cohort have low educational
attainment, so telemedicine resources need to be adapted to the appropriate literacy and
technology level, and they must accommodate limited data plans and service interruptions.
Nonetheless, cell phone ownership is high even among low-income immigrants, including
those without documentation.
66,67
Small studies of culturally and linguistically adapted apps
have demonstrated feasibility and acceptability of telemedicine to immigrant populations.
68
For example, a randomized controlled study of a culturally adapted web-based Spanish-
language app for patients with substance use disorder had very high completion rates (98% in
the intervention group) and achieved reduced substance use prevalence among those exposed
to the app.
69
The transition to telemedicine during COVID-19 could enhance uptake of such
interventions, when appropriately tailored to the target patient populations.
At the Johns Hopkins Health System, uptake of the electronic medical record MyChart exten-
sion (providing access to health records and an electronic communication portal for provider
messaging) was low among patients with limited English prociency prior to COVID-19, but
uptake increased signicantly, even among LEP patients, during the pandemic, as patients
valued quick access to their COVID-19 test results. Community health workers were instru-
mental in developing videos to demonstrate the steps of MyChart enrollment (including how
to set up an email account), and system-level changes were made through Epic health care
software to facilitate uptake by removing, for example, the need to be preregistered in the
health system by scheduling sta.
278 PRIMARY CARE IN THE COVID-19 PANDEMIC
The power of community health workers
The community health worker (CHW, or promotor/a in Spanish) model is an evidence-based
solution that has been successfully implemented to improve the management of chronic
diseases and should be expanded to facilitate access and retention in primary care.
70,71
CHWs
are trusted members of the community who build individual and community health capacity
through outreach, education, advocacy, linkage to care, psychosocial support, and counseling.
They are particularly eective because they have rsthand understanding of the communities
they serve and can act as cultural ambassadors, mediating between the health system and
patients. They typically have extensive community networks that can be leveraged for dis-
seminating health information, dispelling myths and misinformation, or addressing stigma.
They are also well positioned to elicit community feedback, identify priority problems, and
explore solutions proposed by impacted communities, which can help develop more practical
and culturally sensitive interventions.
CHWs have been instrumental in the COVID-19 response, acting as contact tracers and
helping patients navigate the complex and fragmented US health care system. At the New
York-Presbyterian Hospital, for example, CHWs performed more than 9,600 wellness checks
and helped bridge the digital divide by enrolling more than 3,400 patients in online patient
portals.
72
Bilingual and bicultural CHWs provided critical support to undocumented patients,
referring them to resources available outside the federally funded safety-net programs. At
Johns Hopkins, a small team of CHWs supported the emergency department and commu-
nity testing sites by calling all Spanish-speaking LEP patients with their COVID-19 results,
providing educational information, and linking patients with positive tests to resources to
facilitate isolation (such as food distribution, isolation hotels, and cash assistance). During u
season, they are collaborating with the health department to promote u vaccine uptake and
access.
The CHW approach can also be leveraged to engage undocumented immigrants in primary
care. CHWs can emphasize the importance of primary and preventive care. This is important
as in many cultures and countries, health care is primarily available or perceived as episodic
and associated with acute health conditions. CHWs can begin to educate the community about
the benets of preventive care and highlight the general benets of health care engagement
by referring patients to services that address other priorities, such as nancial assistance pro-
grams for health care, housing, employment, food assistance, and other social determinants
of health. As trusted advisors, they can also dispel fears related to immigration and potential
interactions with the health system, and help provide warm handos to primary care clinics.
Leveraging multistakeholder partnerships
COVID-19 accelerated nontraditional public-private-academic partnerships, including among
institutions that were previously competing for nancial and personnel resources. At a na-
tional and local level, as various stakeholders collaborated to expand testing capacity, develop
COVID-19 therapeutics and vaccines, and operationalize high-volume delivery of care, pro-
ductive partnerships emerged across health care systems, health technology companies, and
PRIMARY CARE IN THE COVID-19 PANDEMIC 279
community service providers. In Baltimore, for example, a public-private partnership was
established under the leadership of the chief executive ocers (CEOs) of CareFirst BlueCross
BlueShield, Johns Hopkins Health System, and the University of Maryland Medical System,
the mayor of Baltimore, and Maryland state representatives to address the disproportion-
ate impact of COVID-19 on high-poverty areas. Productive partnerships should be sustained
beyond the pandemic to improve equity in our health system and expand access to primary
care for undocumented immigrants and other vulnerable groups. The same urgency to ad-
dress COVID-19 that catalyzed these collaborations, broke silos, and brought complementary
strengths to the table should be applied to addressing other chronic medical conditions that
disproportionately impact underserved communities, such as substance use disorder, diabetes,
cardiovascular disease, and obesity.
The electronic medical record—in particular, regional health information exchange (HIE)
programs such as the Chesapeake Regional Information System (CRISP) in Maryland
73
—could
facilitate care coordination and help identify vulnerable patients without a medical home.
For example, analysis of data in the CRISP HIE has been applied to ascertain fragmentations
in care among patients with substance use disorder and to develop predictive models of fatal
overdoses.
74,75
A similar approach could be used to develop predictive models to (1) prioritize
patients in need for primary care based on hospital utilization and/or underlying conditions,
(2) identify populations or neighborhoods for targeted interventions, and (3) monitor outcome
measures. Public health institutions and policy leaders can play a role in this space by es-
tablishing health equity metrics and providing nancial incentives for population health and
community health outcomes.
Conclusions
The COVID-19 pandemic has led to changes at an unprecedented pace in health care delivery.
It has also highlighted major deciencies in our health care system that need urgent atten-
tion. For undocumented immigrants, exclusion from health insurance programs resulted
in limited access to primary care and created signicant barriers to testing and care as the
epidemic unfolded. Language barriers, competing priorities, institutional mistrust, the
digital divide, and lack of familiarity with the health care system further complicated the
timely implementation of strategies to reduce the burden of COVID-19 in this population.
But the COVID-19 crisis should not go to waste. There are practical approaches that could
help mitigate the impact of the disease and, importantly, expand access to primary care for
undocumented immigrants. Lessons learned from COVID-19 present a unique opportunity for
transformational change. First, the community health care workforce should be expanded.
CHW-based outreach is evidence based and cost eective, particularly in resource-limited
settings. Second, the digital divide can be mitigated by expanding access to the Internet, capi-
talizing on existing platforms popular among immigrants, disseminating culturally and lin-
guistically appropriate health information, and using hybrid models with CHW support. Third,
public-private-academic partnerships should be leveraged to expand access to care at the most
appropriate setting and establish systems to identify and facilitate linkages to care. Investments
now will pay o in lives saved, long-term cost savings, and gains in public health.
280 PRIMARY CARE IN THE COVID-19 PANDEMIC
References
1. Budiman A. Key ndings about U.S. immigrants. Pew
Research Center. August 20, 2020. Accessed No-
vember 15, 2020. https://www.pewresearch.org/fact-
tank/2020/08/20/key-ndings-about-u-s-immigrants/.
2. Passel JS, Cohn D. Mexicans decline to less than
half the U.S. unauthorized immigrant population for
the rst time. Pew Research Center. June 12, 2019.
Accessed November 15, 2020. https://www.pewre-
search.org/fact-tank/2019/06/12/us-unauthorized-
immigrant-population-2017/.
3. Capps R, Fix M, Zong J. Fact sheet: prole of U.S.
children with unauthorized immigrant parents. Migra-
tion Policy Institute. January 2016. Accessed Novem-
ber 15, 2020. https://www.migrationpolicy.org/sites/
default/les/publications/ChildrenofUnauthorized-
FactSheet-FINAL.pdf.
4. Unauthorized immigrant populations by country and
region, top states and counties of residence, 2018.
Migration Policy Institute. Accessed November 15,
2020. https://www.migrationpolicy.org/programs/
data-hub/charts/unauthorized-immigrant-populations-
country-and-region-top-state-and-county.
5. Prole of the unauthorized population: United States.
Migration Policy Institute. Accessed November 15,
2020. https://www.migrationpolicy.org/data/unauthor-
ized-immigrant-population/state/US.
6. Summary of immigrant eligibility restrictions under
current law. U.S. Department of Health and Human
Services. February 25, 2009. Accessed November
15, 2020. https://aspe.hhs.gov/basic-report/summary-
immigrant-eligibility-restrictions-under-current-law.
7. Emergency Medical Treatment & Labor Act (EM-
TALA). Centers for Medicare and Medicaid Services.
Last updated March 26, 2012. Accessed November
15, 2020. https://www.cms.gov/Regulations-and-
Guidance/Legislation/EMTALA.
8. Health coverage of immigrants, footnote 2. Kaiser
Family Foundation. March 18, 2020. Accessed
November 15, 2020. https://www.kff.org/racial-equity-
and-health-policy/fact-sheet/health-coverage-of-
immigrants/#footnote-454226-2.
9. Compilation of Patient Protection and Affordable Care
Act. Washington, DC: U.S. Ofce of the Legislative
Counsel, 2010. https://www.hhs.gov/sites/default/
les/ppacacon.pdf.
10. Brooks T, Roygardner L, Artiga S. Medicaid and CHIP
eligibility, enrollment, and cost sharing policies as of
January 2019: ndings from a 50-state survey. Kaiser
Family Foundation. March 27, 2019. Accessed No-
vember 15, 2020. https://www.kff.org/medicaid/report/
medicaid-and-chip-eligibility-enrollment-and-cost-
sharing-policies-as-of-january-2019-ndings-from-a-
50-state-survey/.
11. Cohn D, Passel J, Bialik K. Many immigrants with
Temporary Protected Status face uncertain future
in U.S. Pew Research Center. November 27, 2019.
Accessed November 16, 2020. https://www.pewre-
search.org/fact-tank/2019/11/27/immigrants-tempo-
rary-protected-status-in-us/.
12. Mann C. Individuals with Deferred Action for Child-
hood Arrivals. Center for Medicaid and CHIP Servic-
es. August 28, 2012. Accessed November 15, 2020.
https://www.medicaid.gov/Federal-Policy-Guidance/
downloads/SHO-12-002.pdf.
13. López G, Manuel Krogstad J. Key facts about
unauthorized immigrants enrolled in DACA. Pew
Research Center. September 25, 2017. Accessed
November 15, 2020. https://www.pewresearch.org/
fact-tank/2017/09/25/key-facts-about-unauthorized-
immigrants-enrolled-in-daca/.
14. Buchmueller TC, Lo Sasso AT, Lurie I, Doln S.
Immigrants and employer-sponsored health insur-
ance. Health Serv Res 2007;42(1 Pt 1):286-310.
10.1111/j.1475-6773.2006.00600.x.
15. Passel JS, Cohn D. Unauthorized immigrant work-
force is smaller, but with more women. Pew Re-
search Institute. November 27, 2018. Accessed
November 15, 2020. https://www.pewresearch.org/
hispanic/2018/11/27/unauthorized-immigrant-work-
force-is-smaller-but-with-more-women/.
16. Haro AY, Kuhn R, Rodriguez MA, Theodore N,
Melendez E, Valenzuela A Jr. Beyond occupational
hazards: abuse of day laborers and health. J Immigr
Minor Health 2020;22(6):1172-83. 10.1007/s10903-
020-01094-3.
17. Goodman JD. De Blasio unveils health care plan for
undocumented and low-income New Yorkers. New
York Times. January 8, 2019. Accessed November
15, 2020. https://www.nytimes.com/2019/01/08/nyre-
gion/de-blasio-health-care-plan.html.
18. Allyn B. California is 1st state to offer health benets
to adult undocumented immigrants. NPR. July 10,
2019. Accessed November 15, 2020. https://www.
npr.org/2019/07/10/740147546/california-rst-state-
to-offer-health-benets-to-adult-undocumented-
immigrants.
PRIMARY CARE IN THE COVID-19 PANDEMIC 281
19. Community health center delivery sites and patient
visits. Kaiser Family Foundation. 2018. Accessed
November 15, 2020. https://www.kff.org/other/state-
indicator/community-health-center-sites-and-visits/.
20. Ku L, Jones K, Shin P, Bruen B, Hayes K. The
states’ next challenge—securing primary care for
expanded Medicaid populations. N Engl J Med
2011;364(6):493-5. 10.1056/NEJMp1011623.
21. Cole MB, Wright B, Wilson IB, Galárraga O, Trivedi
AN. Medicaid expansion and community health
centers: care quality and service use increased for
rural patients. Health Aff (Millwood) 2018;37(6):900-7.
10.1377/hlthaff.2017.1542.
22. Cole MB, Wilson IB, Trivedi AN. State variation in
quality outcomes and disparities in outcomes in com-
munity health centers. Med Care 2017;55(12):1001-
7. 10.1097/MLR.0000000000000818.
23. Nathenson RA, Saloner B, Richards MR, Rhodes
KV. Spanish-speaking immigrants’ access to safety
net providers and translation services across tra-
ditional and emerging US destinations. Milbank Q
2016;94(4):768-99. 10.1111/1468-0009.12231.
24. Morey BN. Mechanisms by which anti-immigrant
stigma exacerbates racial/ethnic health disparities.
Am J Public Health 2018;108(4):460-3. 10.2105/
AJPH.2017.304266.
25. Page KR, Polk S. Chilling effect? Post-election
health care use by undocumented and mixed-status
families. N Engl J Med 2017;376(12):e20. 10.1056/
NEJMp1700829.
26. Cohen MS, Schpero WL. Household immigration
status had differential impact on Medicaid enroll-
ment in expansion and nonexpansion states.
Health Aff (Millwood) 2018;37(3):394-402. 10.1377/
hlthaff.2017.0978.
27. Watson T. Inside the refrigerator: immigration enforce-
ment and chilling effects in Medicaid participation.
Am Econ J Econ Policy 2014;6(3):313-38. 10.1257/
pol.6.3.313.
28. Venkataramani M, Pollack CE, DeCamp LR, Leifheit
KM, Berger ZD, Venkataramani AS. Association of
maternal eligibility for the Deferred Action for Child-
hood Arrivals program with citizen children’s partici-
pation in the Women, Infants, and Children program.
JAMA Pediatr 2018;172(7):699-701. 10.1001/jamape-
diatrics.2018.0775.
29. Public charge. U.S. Citizenship and Immigration
Services. Last updated September 22, 2020. Ac-
cessed November 15, 2020. https://www.uscis.gov/
green-card/green-card-processes-and-procedures/
public-charge.
30. Tolbert J, Artiga S, Pham O. Impact of shifting immi-
gration policy on Medicaid enrollment and utilization
of care among health center patients. Kaiser Family
Foundation. October 15, 2019. Accessed November
15, 2020. https://www.kff.org/report-section/impact-of-
shifting-immigration-policy-on-medicaid-enrollment-
and-utilization-of-care-among-health-center-patients-
issue-brief/.
31. Bernstein H, Gonzalez D, Karpman M, Zuckerman
S. One in seven adults in immigrant families report
avoiding public benet programs in 2018. Urban Insti-
tute. May 2019. Accessed February 23, 2021. https://
www.urban.org/sites/default/les/publication/100270/
one_in_seven_adults_in_immigrant_families_report-
ed_avoiding_publi_7.pdf.
32. Zallman L, Finnegan KE, Himmelstein DU, Touw
S, Woolhandler S. Implications of changing public
charge immigration rules for children who need
medical care. JAMA Pediatr 2019;173(9):e191744.
10.1001/jamapediatrics.2019.1744.
33. Newacheck PW, Stoddard JJ, Hughes DC, Pearl
M. Health insurance and access to primary care for
children. N Engl J Med 1998;338(8):513-9. 10.1056/
NEJM199802193380806.
34. McMorrow S, Kenney GM, Goin D. Determinants of
receipt of recommended preventive services: implica-
tions for the Affordable Care Act. Am J Public Health
2014;104(12):2392-9. 10.2105/AJPH.2013.301569.
35. Cole MB, Trivedi AN, Wright B, Carey K. Health insur-
ance coverage and access to care for community
health center patients: evidence following the Afford-
able Care Act. J Gen Intern Med 2018;33(9):1444-6.
10.1007/s11606-018-4499-2.
36. Woolhandler S, Himmelstein DU. The relationship
of health insurance and mortality: is lack of insur-
ance deadly? Ann Intern Med 2017;167(6):424-31.
10.7326/M17-1403.
37. Tai DBG, Shah A, Doubeni CA, Sia IG, Wieland ML.
The disproportionate impact of COVID-19 on racial
and ethnic minorities in the United States. Clin Infect
Dis 2020:ciaa815. 10.1093/cid/ciaa815.
38. Wortham JM, Lee JT, Althomsons S, et al. Character-
istics of persons who died with COVID-19—United
States, February 12–May 18, 2020. MMWR Morb
Mortal Wkly Rep 2020;69(28):923-9. 10.15585/
mmwr.mm6928e1.
39. Bixler D, Miller AD, Mattison CP, et al. SARS-
CoV-2–associated deaths among persons aged 21
years—United States, February 12–July 31, 2020.
MMWR Morb Mortal Wkly Rep 2020;69(37):1324-9.
10.15585/mmwr.mm6937e4.
282 PRIMARY CARE IN THE COVID-19 PANDEMIC
40. Page KR, Flores-Miller A. Lessons we’ve learned—
COVID-19 and the undocumented Latinx com-
munity. N Engl J Med 2021;384(1):5-7. 10.1056/
NEJMp2024897.
41. Bucay-Harari L, Page KR, Krawczyk N, Robles
YP, Castillo-Salgado C. Mental health needs of an
emerging Latino community. J Behav Health Serv
Res 2020;47(3):388-98. 10.1007/s11414-020-09688-3.
42. Stewart RW, Orengo-Aguayo RE, Gilmore AK, de
Arellano M. Addressing barriers to care among
Hispanic youth: telehealth delivery of trauma-focused
cognitive behavioral therapy. Behav Ther (N Y N Y)
2017;40(3):112-8.
43. Mobile fact sheet. Pew Research Center. June 12,
2019. Accessed November 15, 2020. https://www.
pewresearch.org/internet/fact-sheet/mobile/.
44. Leite L, Buresh M, Rios N, Conley A, Flys T, Page
KR. Cell phone utilization among foreign-born
Latinos: a promising tool for dissemination of
health and HIV information. J Immigr Minor Health
2014;16(4):661-9. 10.1007/s10903-013-9792-x.
45. Noe-Bustamante L, Flores A. Facts on Latinos in the
U.S. Pew Research Center. September 16, 2019.
Accessed November 15, 2020. https://www.pewre-
search.org/hispanic/fact-sheet/latinos-in-the-u-s-fact-
sheet/.
46. Martinez DA, Hinson JS, Klein EY, et al. SARS-CoV-2
positivity rate for Latinos in the Baltimore-Washing-
ton, DC region. JAMA 2020;324(4):392-5. 10.1001/
jama.2020.11374.
47. Naranbhai V, Chang CC, Beltran WFG, et al. High se-
roprevalence of anti-SARS-CoV-2 antibodies in Chel-
sea, Massachusetts. J Infect Dis 2020;222(12):1955-
9. 10.1093/infdis/jiaa579.
48. Rosenberg ES, Tesoriero JM, Rosenthal EM, et al.
Cumulative incidence and diagnosis of SARS-CoV-2
infection in New York. Ann Epidemiol 2020;48:23-9.
e4. 10.1016/j.annepidem.2020.06.004.
49. Menachemi N, Yiannoutsos CT, Dixon BE, et al.
Population point prevalence of SARS-CoV-2 infec-
tion based on a statewide random sample—Indiana,
April 25-29, 2020. MMWR Morb Mortal Wkly Rep
2020;69(29):960-4. 10.15585/mmwr.mm6929e1.
50. Unemployment insurance relief during COVID-19
outbreak. U.S. Department of Labor. Accessed
November 15, 2020. https://www.dol.gov/coronavirus/
unemployment-insurance.
51. Recovery rebate credits and economic impact pay-
ments. Internal Revenue Service. Accessed No-
vember 15, 2020. https://www.irs.gov/coronavirus/
economic-impact-payments.
52. Manuel Krogstad J, Hugo Lopez M. Coronavirus
economic downturn has hit Latinos especially hard.
Pew Research Center. August 4, 2020. Accessed
November 15, 2020. https://www.pewresearch.org/
hispanic/2020/08/04/coronavirus-economic-down-
turn-has-hit-latinos-especially-hard/.
53. States offering driver’s licenses to immigrants. Na-
tional Conference of State Legislatures. February 8,
2021. Accessed February 9, 2021. https://www.ncsl.
org/research/immigration/states-offering-driver-s-
licenses-to-immigrants.aspx.
54. Dyal JW, Grant MP, Broadwater K, et al. COVID-19
among workers in meat and poultry processing facili-
ties—19 states, April 2020. MMWR Morb Mortal Wkly
Rep 2020;69(18). 10.15585/mmwr.mm6918e3.
55. Waltenburg MA, Victoro T, Rose CE, et al.
Update: COVID-19 among workers in meat and
poultry processing facilities—United States,
April-May 2020. MMWR Morb Mortal Wkly
Rep 2020;69(27):887-92. 10.15585/mmwr.
mm6927e2.
56. Tenforde MW, Billig Rose E, Lindsell CJ, et
al. Characteristics of adult outpatients and
inpatients with COVID-19—11 academic
medical centers, United States, March-
May 2020. MMWR Morb Mortal Wkly
Rep 2020;69(26):841-6. 10.15585/mmwr.
mm6926e3.
57. Joseph NP, Reid NJ, Som A, et al. Racial and
ethnic disparities in disease severity on
admission chest radiographs among pa-
tients admitted with conrmed coronavirus
disease 2019: a retrospective cohort study.
Radiology 2020;297(3):e303-e12. 10.1148/ra-
diol.2020202602.
58. Cheng YJ, Kanaya AM, Araneta MRG, et al. Preva-
lence of diabetes by race and ethnicity in the United
States, 2011-2016. JAMA 2019;322(24):2389-98.
10.1001/jama.2019.19365.
59. Do EK, Matsuyama RK. Healthcare utilization
among Hispanic immigrants with diabetes:
investigating the eect of US documentation
status. J Immigr Minor Health 2014;16(2):189-
94. 10.1007/s10903-012-9729-9.
60. The After Care Clinic. Johns Hopkins Medicine.
Accessed November 15, 2020. https://www.hopkins-
medicine.org/gim/clinical/ACC/.
61. The Access Partnership. Johns Hopkins Medicine.
Accessed November 15, 2020. https://www.hopkins-
medicine.org/health_care_transformation_strategic_
planning/access_partnership/.
PRIMARY CARE IN THE COVID-19 PANDEMIC 283
62. Block L, Cook BG, Hanyok LA, et al. Coverage isn’t
enough: building primary care capacity in the setting
of health reform. J Health Care Poor Underserved
2014;25(1):25-8. 10.1353/hpu.2014.0046.
63. Polk S, DeCamp LR, Guerrero Vázquez M, et al.
Centro SOL: a community-academic partnership to
care for undocumented immigrants in an emerging
Latino area. Acad Med 2019;94(4):538-43. 10.1097/
ACM.0000000000002508.
64. Gardner EM, McLees MP, Steiner JF, Del Rio C,
Burman WJ. The spectrum of engagement in HIV
care and its relevance to test-and-treat strate-
gies for prevention of HIV infection. Clin Infect Dis
2011;52(6):793-800. 10.1093/cid/ciq243.
65. Fernandez A, Schillinger D, Grumbach K, et al.
Physician language ability and cultural competence:
an exploratory study of communication with Spanish-
speaking patients. J Gen Intern Med 2004;19(2):167-
74. 10.1111/j.1525-1497.2004.30266.x.
66. González HM, Vega WA, Tarraf W. Health care
quality perceptions among foreign-born Latinos and
the importance of speaking the same language. J
Am Board Fam Med 2010;23(6):745-52. 10.3122/
jabfm.2010.06.090264.
67. Wilson E, Chen AH, Grumbach K, Wang F, Fernan-
dez A. Effects of limited English prociency and
physician language on health care comprehension.
J Gen Intern Med 2005;20(9):800-6. 10.1111/j.1525-
1497.2005.0174.x.
68. Dahne J, Collado A, Lejuez CW, et al. Pilot random-
ized controlled trial of a Spanish-language behavioral
activation mobile app (¡Aptívate!) for the treatment of
depressive symptoms among United States Latinx
adults with limited English prociency. J Affect Disord
2019;250(1):210-7. 10.1016/j.jad.2019.03.009
69. Paris M, Silva M, Añez-Nava L, et al. Culturally
adapted, web-based cognitive behavioral therapy for
Spanish-speaking individuals with substance use dis-
orders: a randomized clinical trial. Am J Public Health
2018;108(11):1535-42. 10.2105/AJPH.2018.304571..
70. Promotores de salud/community health workers.
Centers for Disease Control and Prevention. Last
updated September 17, 2019. Accessed November
15, 2020. https://www.cdc.gov/minorityhealth/promo-
tores/index.html.
71. Peretz PJ, Matiz LA, Findley S, Lizardo M, Evans D,
McCord M. Community health workers as drivers of
a successful community-based disease management
initiative. Am J Public Health 2012;102(8):1443-6.
10.2105/AJPH.2011.300585.
72. Peretz PJ, Islam N, Matiz LA. Community health
workers and COVID-19: addressing social determi-
nants of health in times of crisis and beyond. N Engl
J Med 2020;383(19):e108. 10.1056/NEJMp2022641.
73. Welcome to CRISP. Chesapeake Regional Informa-
tion System for Our Patients (CRISP). Accessed No-
vember 15, 2020. https://crisphealth.org/about-crisp/.
74. Gryczynski J, Nordeck CD, Martin RD, et al. Leverag-
ing health information exchange for clinical research:
extreme underreporting of hospital service utiliza-
tion among patients with substance use disorders.
Drug Alcohol Depend 2020;212:107992. 10.1016/j.
drugalcdep.2020.107992.
75. Saloner B, Chang HY, Krawczyk N, et al. Predictive
modeling of opioid overdose using linked statewide
medical and criminal justice data. JAMA Psychiatry
2020;77(11):1-9. 10.1001/jamapsychiatry.2020.1689.
284 PRIMARY CARE IN THE COVID-19 PANDEMIC
M
igrant workers are one of the most vulnerable and marginalized populations in the United
States because of considerable threats to their well-being and systemic and structural bar-
riers to health. A migrant worker is considered an individual whose “principal employment is
seasonal agriculture and who travels and lives in temporary housing.”
1
For centuries, systems
of oppression and slavery in the United States have perpetuated exploitative working conditions
and cheap labor that have contributed to the disenfranchisement of migrant worker populations.
Additionally, constantly evolving and destabilized economic systems and governments in regions
such as Latin and Central America, as well as the Caribbean, have forced millions of individuals to
seek refuge in the United States.
2
These unstable conditions have contributed to a steep rise in US
migrant worker populations and immigration over decades.
3,4
For many migrant workers, the deci-
sion to plunge into an uncertain foreign workforce is often done in the face of staggering poverty,
work scarcity, and violence in their native country. It is worth noting that although a majority of
the modern migrant workforce in the United States comes from immigrant backgrounds, these
deeply entrenched systems of injustice aect all migrant workers regardless of immigration status.
To date, the US agriculture industry relies heavily on the labor of more than 2.5 million migrant
workers, both documented and undocumented.
5
The current COVID-19 crisis has uprooted and disrupted the American economy, forcing millions
of workers to shelter at home in order to curtail rates of transmission. Despite the threat of a novel
pathogenic agent, the agriculture industry has maintained workers on the front lines of America’s
farms and meat-processing plants to sustain the nation’s food supply.
6
Farmworkers, as well as
meatpacking workers, have been ubiquitously labeled “essential” as a consequence of their direct
role in the food production chain. However, in this situation, the workers’ essential status has
failed to protect them from the spread of COVID-19 infection. The nature of migrant labor and the
Migrant Worker
Health and Health
Care in COVID-19
Patricia Fuentes, Gerardo Reyes Chavez, Caroline
Murtagh, Cody Nolan, and Daniel Palazuelos
working conditions on the elds and in plants make it virtually impossible for workers to
adhere to national COVID-19 preventive guidelines to keep themselves and their families safe.
As vaccines for COVID-19 roll out, some states, such as Florida, have not seen their essential
worker status as a reason to provide early access to vaccinations.
7
Often migrant workers are exposed to hazardous and exploitative working conditions. To
reach the work site, farmworkers must travel shoulder to shoulder in enclosed and crowded
buses. Once on the job site, laborers work under strenuous physical and psychological condi-
tions.
8
Migrant workers often live in crowded or congregate spaces found in substandard
and decrepit conditions.
9
Additionally, migrant workers face language barriers, long working
hours, and an extensive history of government mistrust, all of which directly hinders many
from equitably accessing health care services and social support resources.
10
Such socioeconomic conditions have led to a higher prevalence of noncommunicable and
chronic diseases such as hypertension, diabetes, and heart disease among migrant worker
populations. These poor baseline health outcomes compounded with emerging COVID-19
challenges have amplied the existence of systemic and social barriers to health in this popu-
lation, rendering the migrant farmworker especially vulnerable to COVID-19 infection.
This chapter critically discusses the pervasive health disparities that exist in migrant farm-
worker populations with an emphasis on how COVID-19 has exacerbated existing vulnerabili-
ties and aected access to health care services in this population. To fully explore the plight
of migrant farmworkers, a key part in this analysis rst looks at the centuries of systemic and
structural abuse faced by agricultural laborers in America. Doing so will delineate the long
history of pervasive neglect of immigrant and migrant worker populations that has resulted
in generations of grinding poverty and declining health outcomes.
With an understanding of the historical and structural context of agricultural and migrant
workers, this chapter will then delve into the complexities of migrant farmworker health and
health outcomes. Due to strenuous physical farm labor and substandard living conditions, mi-
grant farmworkers bear a greater burden of illness, including chronic conditions, occupational
injuries and sickness, and risk of infection. Most recently, COVID-19 infection has poignantly
amplied existing vulnerabilities to illness, structural barriers to health, and social inequities.
In spite of this, migrant farmworkers were pushed to the front lines of the pandemic without
the adequate knowledge, resources, and support to ensure their health. The declining health
of essential migrant farmworkers has broad-reaching economic, social, and community
health consequences. Thus, it is paramount that we meet existing structural and systemic
disparities; seek best health care practices to relieve the disproportionate burden of disease;
and mitigate generations of entrenched legal and economic marginalization and abuse that
plague migrant farmworker populations in the United States.
286 PRIMARY CARE IN THE COVID-19 PANDEMIC
History of migrant workers and agricultural labor in the
United States
To understand the structural vulnerability of migrant farmworkers to illness, it is essential
to understand the systems and legislation that have contributed to their disenfranchise-
ment. A historical exploration of agricultural labor in the United States reveals that social
determinants such as poverty and lack of political voice, which hinder the health and health
care outcomes of migrant farmworkers, are not randomly distributed but structured into the
political, economic, and social fabrics of the nation.
The exploitation that is ubiquitous in the agricultural industry of the American South dates
back to the system of chattel slavery. After the end of the Civil War in 1865, slavery in the
elds was not eliminated but took on new forms through debt bondage and convict labor.
Soon after the passage of the Thirteenth Amendment, former slaves were coerced by poverty
and lack of political power to enter into systems of sharecropping, where landowners al-
lowed agricultural workers to plant on their properties in exchange for a share of the prot.
11
However, high interest rates, unpredictable harvest seasons, and dishonest landowners led
debts to increase each year. This prevented workers from gaining independence or accumu-
lating wealth.
12-14
Additionally, landowners worked with prison ocials to implement debt
bondage, where individuals who were convicted of crimes, felonies, and misdemeanors and
were unable to pay nes could “bind out” to work for farmers. As employers added costs for
food, shelter, and other living expenses, the laborer’s debt increased, cementing the reality of
generational exploitation and poverty.
15
Meanwhile, as the South perpetuated systems of slavery to obtain its workforce, landowners
in the West relied on immigrant labor to implement large-scale farming. After the Mexican-
American War in 1848, California saw an inux of Mexican immigrants, who provided cheap
and seasonal labor. This population was followed by Chinese immigrants after the opening of
the transcontinental railroad in 1869, until the passage of legislation limiting Chinese im-
migration at the end of the century. Mexican immigration increased again with the Bracero
Program in 1942, which brought millions of temporary Mexican workers to the United
States in response to labor shortages caused by World War II.
12,16
Although the demographic
landscape of the agricultural workforce uctuated, the workers’ shared willingness, bred by
poverty and inequity, to labor in uncertain conditions for low wages made them attractive
employees to farm owners.
Similarly, in the South, the ethnic and racial identity of farmworkers shifted as African
Americans left agriculture for other industries but were replaced by groups of laborers
that would also confront brutal conditions and low wages. Throughout the 1970s to 1990s,
Haitians arrived rst in the South to escape oppressive conditions during the dictatorships of
the Duvaliers.
17
They were followed by Guatemalans, many of whom were seeking refuge from
the Guatemalan Civil War, and Mexicans, whose ability to make competitive wages through
farming had been hampered by the North American Free Trade Agreement (NAFTA).
18,19
Thus,
although many of these individuals arrived in the United States with hopes of a better life,
they were instead met with dicult working conditions that perpetuated historical systems of
PRIMARY CARE IN THE COVID-19 PANDEMIC 287
slavery and exploitation. It is important to note that the disruptions experienced in the home
countries were often a result of US foreign policies and practices that manipulated foreign
governments, often to benet US business interests.
20
In the 20th century, the marginalization of farmworkers was further codied through the
establishment of exclusionary legislation. In the wake of the Great Depression, Congress
passed two major pieces of legislation that sought to protect the rights of workers. First,
the National Labor Relations Act (NLRA) of 1935 guaranteed employees the right to organize
into trade unions, take collective action such as strike, and engage in collective bargaining.
21
Second, the Fair Labor Standards Act (FLSA) of 1938 introduced the federal regulation of
wages and hours by establishing a minimum wage and overtime compensation.
22
However,
lawmakers excluded agricultural laborers and domestic workers from the protections aorded
by the NLRA through the act’s denition of employee, which stated it “shall not include any
individual employed as an agricultural laborer.” The FLSA furthered its discriminatory treat-
ment by excluding agricultural laborers from its coverage and by expanding the denition of
agriculture to include more jobs (horticulture, for example). Although legislators later added
a minimum wage for agricultural work to the FLSA in 1966, the FLSA continues to exclude
agricultural laborers from its overtime protections, and it retains its broader denition of ag-
riculture, which now also applies to the NLRA. Additionally, enforcement of the minimal FLSA
protection that does exist for farmworkers remains a challenge due to many factors, including
that farmworkers are increasingly employed by subcontracted “farm labor contractors” whose
legal distance from the farm itself fosters increased levels of violating employees’ rights, and
that most employers choose not to use formal timekeeping systems in an industry that is
heavily dependent on an itinerant workforce and changes in weather and season.
12
Today, it is estimated that 50% to 70% of migrant farmworkers are undocumented im-
migrants, which puts workers at risk of wage theft, physical and sexual abuse, and unsafe
working conditions and prevents many individuals from issuing complaints for fear of retali-
ation.
23
Furthermore, many undocumented workers are excluded from social services such as
food stamps and government-subsidized housing. Thus, active eorts to dismantle legaliza-
tion processes for immigrants serve to further oppress this group of essential workers.
The H-2A visa program, which is reminiscent of the earlier Bracero Program, constitutes one
eort to facilitate the legal movement of migrant farmworkers. H-2A farmworkers, who are
issued a visa to work temporarily in the United States, make up 10% of crop farmworkers in
the country.
24
Over the past decade, the number of H-2A workers has been growing steadily.
25
However, investigators have found that the program is still rife with human rights abuses that
routinely expose workers to human tracking, debt servitude, and forced labor, to name a few.
26
The American agricultural industry is built on systems of slavery, racism, and exploitation;
thus, active eorts on the part of workers, agribusinesses, consumers, and corporations are
necessary to alleviate centuries of injustice. Although this structural context contributes to the
socioeconomic challenges facing agricultural workers, they are often excluded from common
benets such as health insurance, disability insurance, paid leave, and retirement benets,
and many lack access to social services. Thus, when farmworkers become sick, the conse-
quences can be devastating.
288 PRIMARY CARE IN THE COVID-19 PANDEMIC
Baseline health challenges in migrant worker populations
Today, migrant worker populations face staggering socioeconomic challenges, which have
important implications for their health and produce disproportionate structural vulnerability
to illness. They represent a highly impoverished and underserved community, resulting from
low wages without overtime pay, lack of benets, employment instability, and stagnation of
earnings, which have failed to grow in tandem with the agricultural sector. Indeed, according
to the most recent National Agricultural Workers Survey (NAWS), 33% of migrant farmwork-
ers live below the federal poverty line, almost double the national average.
27
As a result, these
populations demonstrate especially high prevalence of food insecurity and hunger—as much as
50% more than the general US population living below the poverty line.
28
Food insecurity and
under/malnutrition have long been associated with poor health outcomes and increased risk for
development of noncommunicable diseases like diabetes, hypertension, and heart disease.
At home, migrant workers often face substandard living conditions with crowded housing,
lack of utilities or few utilities split among many tenants, and, in rural areas, poor access
to public transportation, grocery stores, clinics or hospitals, and other services important to
wellness.
29
One study of North Carolina migrant labor camps found that “crowding, lack of
access to sucient bathing facilities, pest infestation, and structural damage are common to
dwellings in farmworker labor camps.”
30
Although all migrant workers face barriers, escape
from, or improvement of, such living conditions can be especially challenging for undocu-
mented migrant workers, whose inability to apply for subsidized public housing and reliance
on migrant worker housing allows owners to charge exorbitant rent. These living conditions,
in turn, render migrant workers especially vulnerable to infectious diseases like tuberculosis,
hepatitis, and most recently COVID-19.
31
The physical and psychological occupational hazards faced by migrant workers while on
the job are numerous. They typically work long hours performing dangerous and physically
laborious work, all while beset by perilous environmental conditions including harsh sun,
heat, and dust. They are at risk of myriad occupational injuries ranging from crush injuries to
falls.
29
In spite of this, less than half have workers’ compensation. Additionally, as a result of
inhalation of organic and inorganic particles, as well as the various chemicals used on crops,
they are at higher risk of pulmonary diseases like asthma, chronic obstructive pulmonary
disease, and hypersensitivity pneumonitis.
32
Beyond the immediate danger of acute organo-
phosphate poisoning, long-term exposure to pesticides has been associated with neurotoxic-
ity, multiple cancers, and higher incidence of birth defects.
33
Experiences of workplace abuse,
including verbal and physical violence, are disturbingly common. In the most extreme cases,
migrant workers are victim to human tracking and forced labor.
34
In spite of structural vulnerability to poor health and working conditions that routinely lend
themselves to both illness and injury, migrant worker populations have limited access to
health care. Per the most recent NAWS, 53% of farmworkers have no health insurance.
27
Very
few employers provide health insurance benets to migrant workers, and undocumented
workers do not qualify for government programs like Medicaid or CHIP. The majority of
health care for migrant workers is delivered through Federally Qualied Health Centers
PRIMARY CARE IN THE COVID-19 PANDEMIC 289
(FQHCs), where there is a shortage of primary care providers and access to specialists is
limited. Diculty of access is further compounded by language barriers, lack of transporta-
tion, long working hours, no sick leave, and unavailability or expense of child care to attend
appointments. As a result of these multiple barriers, migrant farmworkers have very low rates
of health care utilization.
35
Without regular quality health care maintenance, “silent” but signicant health conditions
like hypertension, hyperlipidemia, and diabetes go undiagnosed and untreated. Although
there is a lack of data, studies suggest rates of chronic illness are persistently high for mi-
grant workers. For example, the California Agricultural Workers Health Survey found that half
of all surveyed workers carried at least one diagnosis of either hypertension, hyperlipidemia,
or obesity.
36
These illnesses place migrant workers, who are already more likely to contract
infections, at higher risk of severe COVID-19 disease and mortality.
37
Emerging health challenges during COVID-19
The long-standing marginalization and systemic oppression of migrant workers has created
health inequities that have been further amplied during the COVID-19 pandemic. Although
agricultural laborers are the source of the nation’s food, placing them arguably among the
country’s most essential workers, the conditions in which they live and work put them par-
ticularly at risk during the pandemic.
Substandard living conditions and occupational hazards lead to increased susceptibility to
chronic and noncommunicable diseases. This puts migrant workers at greater risk of poor
COVID-19 outcomes. Despite this increased danger, the nature of agricultural work often
places migrant workers in situations that hinder preventive measures. The overcrowded trail-
ers in which farmers live, as well as the enclosed buses that take them to work, make social
distancing, a measure known to decrease transmission, virtually impossible.
Another key component of the COVID-19 response is testing, but migrant workers are often
excluded from testing services for structural and social reasons. A lack of transportation to
and from testing centers and a shortage of culturally and linguistically appropriate materi-
als about testing opportunities prevent many migrant workers from accessing testing at
all. Those who do have access are often discouraged from seeking out the service because
of stigma at work, fear of losing employment, and other severe nancial repercussions if
they test positive. For instance, some employers require two negative tests before allowing a
worker with a former positive test to return to employment. However, due to laboratory de-
lays in returning results and the risk of false positive results that are detecting inactive parts
of the virus, this requirement can take weeks to achieve, which puts workers at risk of losing
signicant portions of their incomes if they test positive once (regardless of symptoms).
38
When farmworkers test positive or are exposed to a person infected with COVID-19, be-
coming cases and contacts, they are advised to isolate and quarantine, respectively. Public
health experts advise that these individuals follow several guidelines to protect their health
and prevent transmission to others, including instructions to stay home; avoid contact with
290 PRIMARY CARE IN THE COVID-19 PANDEMIC
others; sleep in a separate room and use a dierent bathroom from other household members;
regularly disinfect household surfaces; avoid sharing household items; and seek medical care
when needed.
37
For migrant workers, however, these recommendations are often impossible
to follow. The need to put food on the table and pay exorbitant rent makes missing two weeks
of work nancially devastating. Those who can aord to stay home often share close, con-
ned spaces with up to a dozen strangers and may lack access to disinfectants, creating ideal
conditions for household transmission. As described previously, many migrant farmworkers
are uninsured or underinsured, which leads to challenges in accessing and receiving quality
health care.
Finally, contact tracing is an essential tool to slow the spread of COVID-19. This strategy
requires positive cases to answer phone calls, often from local health departments, share
information about their close contacts, quarantine, and closely monitor symptoms. However,
a history of exploitation and fear of the US health system has made some workers hesitant
to answer calls from state ocials. Thus, culturally humble navigators with rich community
expertise and local rapport, such as community health workers, are necessary to gather this
sensitive information and connect individuals to local social and clinical resources. In turn,
it can make isolation and quarantine a feasible option for migrant workers and help prevent
further transmission.
Under the recent public charge rule, immigrants are disincentivized from accessing health
care services out of fear of deportation or future repercussions, a fear that has manifested in
low-utilization rates of medical services in this population, especially during COVID-19.
39,40
This is a visceral reality for many migrant workers since a large percentage are from immi-
grant backgrounds. When the long-standing marginalization of migrant workers is taken into
account, it becomes clear that health inequities have been structured into the working and
living conditions of this population for centuries. The COVID-19 pandemic has only served to
further amplify these disparities, as migrant workers are more likely to become infected and
to suer poor health outcomes from COVID-19. Thus, it is essential to understand how strat-
egies can be tailored to protect and promote the health of this underserved and vulnerable
population in order to advance health care as a human right.
Establishing and enforcing migrant workers’ right to health
As the preceding section demonstrates, farmworkers are not aorded the same safety nets as
other employees in the United States. Farmworkers are an essential part of the food produc-
tion system, harvesting the fruits and vegetables millions of American citizens rely on to
stay healthy. In spite of their essential role in America’s farms, farmworkers do not receive
adequate support to safely do their job, especially in the face of a novel public health threat.
Simple public health messages are not enough to mitigate the eects of COVID-19 on migrant
worker populations. Systematic and comprehensive reform is necessary to address the health
disparities that plague migrant worker populations, and to reduce the high risk of COVID-19
infection. Farmworkers are vital frontline workers, and vital to their job are the protective
resources, paid leave, and targeted outreach that enable them to work safely.
PRIMARY CARE IN THE COVID-19 PANDEMIC 291
To address this situation, we have identied four main types of solutions: (1) expand health
care options in general and during COVID-19 specically; (2) expand social supports in gen-
eral and particularly during COVID-19; (3) mandate best practices in workplace safety; and (4)
legislate the broader changes that are both necessary and possible.
Expand public health and health care options in general and during
COVID-19 specically
Expanding general health care services to migrant worker populations needs to be a prior-
ity in order to foster greater community resilience in times of crisis and address underlying
health issues endemic to farmworker communities. As illustrated in the overview of migrant
workers’ living and working conditions as well as the history of exclusionary legislation,
migrant workers’ lack of access to health care is woven into American legislation and public
policy, and it has produced generations of health disparities. To cultivate an equitable food
production system in the United States, these frontline workers require comprehensive and
accessible community health care services and protective legislation.
In California, for example, the Clinica de la Raza is dedicated to serving the underserved,
including low-income residents, immigrants both documented and undocumented, and
historically marginalized groups. The clinic oers multilingual, accessible health care services
and a range of available specialties, as well as community health education and social support
resources.
41
Community health clinics such as this can mobilize local resources in farmworker
communities to oer the necessary health care and specialized services that are often too far
to reach, expensive, or simply closed by the end of the working day. Access to free, rapid, and
reliable COVID-19 testing, along with easy access to retesting if a negative test is needed to
return to work, is a tangible goal that could be prioritized during the pandemic. New models
for primary care delivery, such as mobile services and after-hours telemedicine with tech-
nologically accessible options, will help to meet the needs of previously unreached migrant
populations. Eective contact tracing programs that reach all cases and their contacts are
another critical tool for combating the COVID-19 pandemic, but too few contact tracers in the
United States reach migrant populations eectively; this can be improved if funding is allo-
cated specically for reaching this group and more contact tracers are hired from the aected
communities. Finally, vaccines for COVID-19 should be available to migrant workers early in
light of the disproportionate burden of disease in this population, and additional eorts will
need to be made to connect with those eligible to assist them in learning about, scheduling,
and receiving the vaccine. Online scheduling portals in English have too often systematically
excluded migrant workers from getting in line, but these additional outreach eorts can be
eective if implemented correctly.
Expand social supports in general and particularly during COVID-19
Social safety nets and support systems must ensure that social determinants of health in
migrant worker populations are actively targeted and improved. Often, migrant workers
face language barriers that prevent them from accessing health care and receiving accurate
292 PRIMARY CARE IN THE COVID-19 PANDEMIC
medical information. The inclusion of culturally appropriate education and linguistically
accessible information will have far-reaching benets for migrant worker health and health
care access. To best deliver this life-saving information, health systems can employ and
deploy community health workers with rich community ties and extensive local knowledge
on common practices and behaviors.
42
Such workers can be a powerful cadre of health profes-
sionals that can help expand access to health care and health information during COVID-19.
Access to information, however, does not guarantee that migrant workers will be able to
follow good public health advice, because their choices are often constrained by their vulner-
able societal position. The ability to self-isolate and quarantine is a key example, since many
migrant workers live in crowded conditions and/or multigenerational homes. Programs that
assure people who test positive have access to safe, clean, and comfortable spaces to live
separate from their contacts when advised are indispensable.
As long as a positive COVID-19 test equals lost wages, migrant workers who live paycheck to
paycheck will naturally be disincentivized to seek care for COVID-19-related symptoms. Lost
wage funds that soften some of that economic penalty, coupled with medical-legal partner-
ships that ensure employers guarantee that workers have a job once they are able to return
to work, will be a good investment in the long run for controlling the spread of the pandemic
among migrant worker communities.
Mandate workplace safety best practices
The health and safety of migrant farmworkers begins in the elds, where they are routinely
exposed to harsh working conditions with limited access to legal representation. For migrant
workers without documentation, these issues are compounded by the fear of deportation or
repercussions from farm owners if workers report violations of their rights. For all migrant
farmworkers, it is imperative that worker-led, enforceable protections are established and
expanded throughout the United States.
Worker-driven Social Responsibility (WSR) programs are one such powerful mechanism with
a proven record of addressing the structural and systemic barriers to health. The Fair Food
Program (FFP), created in Immokalee, Florida, by the Coalition of Immokalee Workers (CIW)
and operating in seven states along the eastern seaboard, established the WSR model. It has
improved wages and virtually eliminated forced labor, sexual violence, wage theft, and dan-
gerous working conditions on participating farms. It oers education and a 24-hour com-
plaint resolution process to workers as well as an in-depth monitoring and auditing regime,
conducted by a third-party monitor, the Fair Food Standards Council (FFSC), which returns
to farms and speaks with workers year after year, bringing technical expertise and unique
familiarity with the work environment and worker population. The program is enforced
through legally binding agreements between the CIW and major food retailers that commit to
buy from farms in good standing with the CIW’s Fair Food Code of Conduct and to cut pur-
chases from agricultural employers that fail or refuse to ensure the human rights protections
laid out in the code. Because the code requires, at a minimum, compliance with existing law,
the CIW’s Fair Food Agreements also enforce true legal compliance with applicable worker
PRIMARY CARE IN THE COVID-19 PANDEMIC 293
protections—including those related to health and safety—in an industry in which govern-
ment enforcement and private litigation have otherwise failed to fundamentally change the
historical reality of widespread noncompliance with the legal rights of farmworkers.
Critically, new COVID-19 protections have been integrated into the Code of Conduct and are
subject to the same enforcement and monitoring protocols as other provisions of the code.
This means that the FFP brings to farmworkers real, enforceable protection against the
violation of COVID-19 safety laws where they exist—which is only in a handful of states, as
neither the Occupational Safety and Health Administration (OSHA) nor the Centers for Disease
Control and Prevention have currently issued binding rules to protect farmworkers—as well
as enforceable protections under the code even in the absence of any COVID-19 safety laws on
the books (as is the case in Florida, for example).
It should thus come as no surprise that the WSR model is now being replicated in new indus-
tries and geographies across the United States as well as internationally and is considered the
emerging gold standard of social responsibility.
12,43
During the COVID-19 pandemic, workers will need access to information on how to protect
themselves, in the language they are most comfortable with, and a dependable supply of ma-
terials such as personal protective equipment that they can use reliably. The FFP requires all
of this. A longer list of best practices has been compiled by Data for Progress, but these mea-
sures will only be as strong as the legal and economic frameworks articulating and enforcing
them, which is why WSR programs like the FFP are absolutely necessary.
44
Legislate the broader changes that are both necessary and possible
Despite the reality that COVID-19 has ravaged migrant farmworker communities across the
country, the Coronavirus Aid, Relief, and Economic Security (CARES) Act does not provide the
necessary safety net for undocumented immigrants, who constitute a signicant portion of
migrant farmworkers.
39,45
Arguably, this has left millions of workers even more vulnerable
to COVID-19 infection and mortality. Specic actions must be taken to address the historical
structural and systemic barriers that have long stood between migrant workers and health.
Strengthening the H-2A guest-worker program and OSHA regulations to implement some of
the suggestions outlined in this chapter, such as paid sick leave, is a practical and immedi-
ately available example that would provide many workers new capacity to better participate in
the measures aiming to control the spread of the virus. All such measures must be accompa-
nied by adequate funding for eective enforcement mechanisms.
294 PRIMARY CARE IN THE COVID-19 PANDEMIC
Conclusion
Although COVID-19 has struck the United States and countries across the globe with the worst
public health crisis in a generation, there is far more at stake with this pandemic than defeat-
ing a novel virus. From the profound health disparities in how the virus aects communities
of color, to the swift and deadly spread through migrant worker camps, COVID-19 has laid
bare long-standing inequities and vulnerabilities in US society, challenges that are deeply
rooted in the country’s history and that can no longer be ignored. In migrant worker com-
munities, COVID-19 has painfully demonstrated the country’s failure to fully end an economy
built on the backs of enslaved people. Systems of forced and coerced labor persist to this day,
accompanied by the degraded living and working conditions inextricably tied to that economic
system. In addition, US foreign policy over the past century has contributed to economic and
political conditions abroad that force laborers to emigrate from their homes to seek work and
safety in the United States. In light of the chapters of history that have led up to this mo-
ment—and contributed to today’s public health crisis—the question of how the United States
addresses health risks to migrant laborers is not only a technical question that aects the US
food supply chain, but also a moral question that forces a deeper reckoning with injustices
that have challenged the soul of the nation since its founding.
References
1. United States farmworker fact sheet. Coalition of
Immokalee Workers. Accessed November 16, 2020.
http://www.ciw-online.org/fwfactsheet.pdf.
2. Philip M, Edward Taylor J. Ripe with change: evolving
farm labor markets in the United States, Mexico, and
Central America. Washington, DC: Migration Policy
Institute, 2013. https://www.migrationpolicy.org/sites/
default/les/publications/RMSG-Agriculture.pdf.
3. Koreishi S, Donohoe M. Historical and contemporary
factors contributing to the plight of migrant farmwork-
ers in the United States. Soc Med 2010;5(10):64-73.
4. Arcury TA, Quandt SA. Delivery of health services to
migrant and seasonal farmworkers. Annu Rev Public
Health 2007;28:345-63. 10.1146/annurev.publ-
health.27.021405.102106.
5. Asbed G. What happens if America’s 2.5 million
farmworkers get sick? New York Times. April 3, 2020.
Accessed November 16, 2020. https://www.nytimes.
com/2020/04/03/opinion/coronavirus-farm-workers.
html.
6. Axon R, Bagentose K, Chadde S. Coronavirus
outbreaks climb at U.S. meatpacking plants despite
protections, Trump order. USA Today. June 6, 2020.
Accessed November 16, 2020. https://www.usatoday.
com/story/news/investigations/2020/06/06/meatpack-
ing-plants-cant-shake-covid-19-cases-despite-trump-
order/3137400001/.
7. Asbed G, Palazuelos D. Honor essential workers with
vaccines / Commentary. Orlando Sentinel. January
19, 2021. https://www.orlandosentinel.com/opinion/
guest-commentary/os-op-coronavirus-honor-essen-
tial-workers-vaccines-20210119-dqy6dpcdgzhvrfu-
muuhu2zz75q-story.html.
8. Mohan P. Farmworkers like me are always the last to
be protected in a crisis. Fast Company. April 13, 2020.
Accessed November 16, 2020. https://www.fastcom-
pany.com/90489038/farmworkers-like-me-are-always-
the-last-to-be-protected-in-a-crisis.
9. Quandt SA, Brooke C, Fagan K, et al. Farm-
worker housing in the United States and its im-
pact on health. New Solut 2015;25(3):263-86.
10.1177/1048291115601053.
10. Hargreaves S, Rustage K, Nellums LB, et al. Occupa-
tional health outcomes among international migrant
workers: a systematic review and meta-analysis. Lan-
cet Glob Health 2019;7(7):e872-82. 10.1016/S2214-
109X(19)30204-9.
PRIMARY CARE IN THE COVID-19 PANDEMIC 295
11. Graff G. Post Civil War African American history: brief
periods of triumph, and then despair. J Psychohist
2016;43(4):247-61.
12. Marquis SL. I am not a tractor: how Florida farmwork-
ers took on the fast food giants and won. Ithaca, NY:
Cornell University Press, 2017.
13. Slavery by another name: sharecropping. PBS. Ac-
cessed November 16, 2020. https://www.pbs.org/tpt/
slavery-by-another-name/themes/sharecropping/.
14. Florida modern-day slavery museum: an examina-
tion of the history and evolution of slavery in Florida’s
elds. Coalition of Immokalee Workers. Accessed
November 16, 2020. https://www.ciw-online.org/mu-
seum/booklet0811.pdf.
15. Bonded labor. End Slavery Now. Access November
16, 2020. http://endslaverynow.org/learn/slavery-
today/bonded-labor/.
16. About. Bracero History Archive. Accessed November
16, 2020. http://braceroarchive.org/about.
17. Nicholls D. From Dessalines to Duvalier: race, colour,
and national independence in Haiti. New Brunswick:
Rutgers University Press, 1996.
18. Tienda M, Sanchez S. Latin American immigration
to the United States. Daedalus 2013;142(3):48-64.
10.1162/DAED_a_00218.
19. Weisbrot M, Merling L, Mello V, Lefebvre S, Sammut
J. Did NAFTA help Mexico? An update after 23 years.
Mexican Law Rev 2018;11(1):159-83. 10.22201/
iij.24485306e.2018.1.12515.
20. Schlesinger SC, Kinser S. Bitter fruit: the untold story
of the American coup in Guatemala. 2nd ed. Garden
City: Anchor Press, 1983.
21. National Labor Relations Act. National Labor Rela-
tions Board. Accessed November 16, 2020. https://
www.nlrb.gov/guidance/key-reference-materials/
national-labor-relations-act.
22. Editors. Fair Labor Standards Act: United States
[1938]. Encyclopedia Britannica. Accessed November
16, 2020. https://www.britannica.com/event/Fair-
Labor-Standards-Act.
23. Selected statistics on farmworkers (2015-16 data).
Farmworker Justice. 2019. Accessed November
16, 2020. http://www.farmworkerjustice.org/wp-
content/uploads/2019/05/NAWS-Data-FactSheet-
05-13-2019-nal.pdf.
24. Costa D, Martin P. Coronavirus and farmworkers: farm
employment, safety issues, and the H-2A guestworker
program. Economic Policy Institute. March 24, 2020.
Accessed November 16, 2020. https://www.epi.org/
publication/coronavirus-and-farmworkers-h-2a/.
25. Guild A, Richards C, Ruiz V. Out of sight, out of mind:
the implementation and impact of the Affordable Care
Act in U.S. farmworker communities. J Health Care
Poor Underserved 2016;27(4A):73-82. 10.1353/
hpu.2016.0183.
26. Close to slavery: guestworker programs in the United
States. Southern Poverty Law Center. February 19,
2013. Accessed November 16, 2020. https://www.
splcenter.org/20130218/close-slavery-guestworker-
programs-united-states.
27. Gabbard S, Hernandez T. Findings from the National
Agricultural Workers Survey (NAWS) 2015-2016: a
demographic and employment prole of United States
farmworkers. Research Report no. 13. Bethesda,
MD: JBS International, 2018. https://wdr.doleta.gov/
research/FullText_Documents/ETAOP_2019-01_
NAWS_Research_Report_13.pdf.
28. Hill BG, Moloney AG, Mize T, Himelick T, Guest
JL. Prevalence and predictors of food insecurity in
migrant farmworkers in Georgia. Am J Public Health
2011;101(5):831-3. 10.2105/AJPH.2010.199703.
29. Arcury TA, Quandt SA. Living and working safely:
challenges for migrant and seasonal farmworkers. N
C Med J 2011;72(6):466-70.
30. Summers P, Quandt SA, Talton JW, Galván L,
Arcury TA. Hidden farmworker labor camps in North
Carolina: an indicator of structural vulnerability.
Am J Public Health 2015;105(12):2570-5. 10.2105/
AJPH.2015.302797.
31. Hansen E, Donohoe M. Health issues of migrant and
seasonal farmworkers. J Health Care Poor Under-
served 2003;14(2):153-64. 10.1353/hpu.2010.0790.
32. Respiratory health hazards in agriculture. Am J Respir
Crit Care Med 1998;158(5 Pt 2):S1-S76. 10.1164/
ajrccm.158.supplement_1.rccm1585s1.
33. Gilden RC, Hufing K, Sattler B. Pesticides
and health risks. J Obstet Gynecol Neona-
tal Nurs 2010;39(1):103-10. 10.1111/j.1552-
6909.2009.01092.x.
34. Moyce SC, Schenker M. Migrant workers and their
occupational health and safety. Annu Rev Public
Health 2018;39:351-65. 10.1146/annurev-publ-
health-040617-013714.
35. Frank AL, Liebman AK, Ryder B, Weir M, Arcury TA.
Health care access and health care workforce for
immigrant workers in the agriculture, forestry, and
sheries sector in the southeastern US. Am J Ind Med
2013;56(8):960-74. 10.1002/ajim.22183.
36. Villarejo D. The health of U.S. hired farm workers.
Annu Rev Public Health 2003;24:175-93. 10.1146/an-
nurev.publhealth.24.100901.140901.
296 PRIMARY CARE IN THE COVID-19 PANDEMIC
37. COVID-19: People with certain medical conditions.
Centers for Disease Control and Prevention. Last up-
dated February 3, 2021. Accessed February 5, 2021.
https://www.cdc.gov/coronavirus/2019-ncov/need-ex-
tra-precautions/people-with-medical-conditions.html.
38. Jia X, Xiao L, Liu Y. False negative RT-PCR and false
positive antibody tests—concern and solutions in
the diagnosis of COVID-19. J Infect October 8, 2020
[Online ahead of print] 10.1016/j.jinf.2020.10.007.
39. Wilson FA, Stimpson JP. US policies increase vulner-
ability of immigrant communities to the COVID-19
pandemic. Ann Glob Health 2020;86(1):57. 10.5334/
aogh.2897.
40. Wilson FA, Stimpson JP. Federal and state policies af-
fecting immigrant access to health care. JAMA Health
Forum. April 6, 2020. Accessed November 16, 2020.
https://jamanetwork.com/channels/health-forum/fullar-
ticle/2764349.
41. La Clinica celebrates over 45 years of service. La Cli-
nica. Accessed November 16, 2020. https://laclinica.
org/about/history/.
42. Ballard M, Bancroft E, Nesbit J, et al. Prioritising the
role of community health workers in the COVID-19
response. BMJ Glob Health 2020;5(6):e002550.
10.1136/bmjgh-2020-002550.
43. About the Fair Food Program. Fair Food. Accessed
November 16, 2020. https://www.fairfoodprogram.org/
about-the-fair-food-program/.
44. Feldman M, Mulholland M. Guidebook: best practices
to support farmworkers during coronavirus. Data for
Progress. September 9, 2020. Accessed November
16, 2020. https://www.dataforprogress.org/memos/
best-practices-to-support-farmworkers-during-corona-
virus.
45. Quandt SA, LaMonto NJ, Mora DC, Talton JW,
Laurienti PJ, Arcury TA. COVID-19 pandemic among
Latinx farmworker and nonfarmworker families in
North Carolina: knowledge, risk perceptions, and
preventive behaviors. Int J Environ Res Public Health
2020;17(16):5786. 10.3390/ijerph17165786.
PRIMARY CARE IN THE COVID-19 PANDEMIC 297
C
OVID-19 has killed more than 2.4 million people worldwide, including nearly 500,000 people in
the United States, at the time of this writing.
1
COVID-19 infections and deaths continue to rise
during this winter period, and several more months will pass before the vaccines recently approved
for distribution are widely available.
2
COVID-19 has—like so many diseases—exposed the fault
lines of our societies, revealing the most vulnerable populations and the most striking inequalities
within them. COVID-19 in the United States, for example, has disproportionately impacted Latino
and non-English-speaking workers in meat-packing plants;
3
Native Americans isolated from
health care sources and frequently occupying multigenerational households;
4
Black Americans,
especially those held in US jails and prisons;
5
people living in understaed and underequipped
nursing homes;
6
and lower-income populations who could not aord to stop working or work from
home because they were employed through in-person jobs, as varied as sanitation and nursing.
7
Some countries, such as South Korea, responded to COVID-19 with comprehensive government-led
testing, rapid contact tracing, supportive isolation in subsidized housing, and proactive dissemina-
tion of health care equipment and treatments.
8
In the United States, by contrast, testing systems
were left federalized and overwhelmed,
9,10
infection control guidelines and epidemiological reports
were undermined or suppressed by political appointees,
11
and some groups refused to disband large
gatherings under the premise that the coronavirus was a hoax or an eort to undermine personal
freedoms.
12
Years from now, our children and grandchildren will ask: What did we do during this epidemic?
Did we stand idly by, or did we act? The experience of primary care providers during COVID-19
has been varied, but almost everywhere we see primary care providers following the call of duty
to provide care for those infected with COVID-19, as well as those impacted by the loss of avail-
ability of care for chronic conditions, the mental health impacts of isolation and profound loss,
and economic impacts of recession and unemployment. If prior disasters—the two world wars,
the HIV epidemic, and the Great Recession—are to guide our response to COVID-19, they suggest
that primary care providers must brace for prolonged, multitiered impacts of COVID-19, beginning
with the acute infections themselves, continuing through the consequences of missed chronic care
Conclusion
Sanjay Basu
as varied as delayed cancer screenings
13
and exacerbated chronic illness, and continuing with
mental health and substance use challenges accelerated by economic upheaval.
14,15
As primary care providers continue caring for patients during COVID-19, the authors of the
preceding chapters have highlighted practical and philosophical barriers to and opportunities
for delivering excellent primary care.
First, international responses to COVID-19 were diverse, and many systems relied on dis-
tributed but coordinated primary care centers to triage patients, oer testing, support social
barriers to safe isolation, address exacerbated social determinants of health such as worsened
food insecurity, and maintain support for chronic disease management. Hence, COVID-19
responses did not have to be based on tertiary care and intensive care units, but could more
proactively rely on strong community-based primary care and population health centers
where such investment—particularly in universal health coverage—had taken place.
16-18
Many providers were able to reach vulnerable and often isolated populations, engaging people
through community health workers, on-site services nearing sites of employment or housing,
or expanded technology access to telemedicine services.
4,19
In the experience of this author in
San Francisco, health care services for homeless or marginally housed adults were provided
through motels designated for isolation or quarantine, and “room service medicine” through
mobile teams going door-to-door in such facilities was a strategy to maintain medical care for
those with chronic conditions or those with COVID-19 who were not sick enough for hospitals
or needed to be treated in improved settings once hospitals were full. It remains to be seen
to what degree pent-up demand for medical care will lead to increased utilization in 2021,
particularly for exacerbations of routine chronic conditions such as heart failure, diabetes, and
hypertension, as well as due to missed preventive activities such as cancer screening.
Second, COVID-19 brought into sharp relief the contrast between universal capitation-based
health care nancing and the traditional US fee-for-service approach. Primary care practices
reliant on fee-for-service medicine were adversely nancially impacted despite rapid ef-
forts by payers to pay for telemedicine services. Many practices lacked technical capabilities
to reliably deliver telemedicine, and destitute patients were unable to reliably gain access in
some locales.
20
By contrast, capitation-based nancing clearly enabled capitated practices to
pivot toward new forms of comprehensive care, and will need to be furthered to ensure care
delivery through diverse workforce members including community health workers. Expanding
the disciplines of the primary care team requires further understanding of the value and
strategies for delivering integrated behavioral health and integrated oral health, as well as
breaching divides between primary and specialty care, virtual and in-person care, and com-
munity- or home-based and clinic- or hospital-based care.
Third, COVID-19 has shined a light on the need for primary care practitioners to engage in
the political processes that dene risk and mortality across our societies. During the height
of the rst wave of COVID-19 infections in the United States, the Black Lives Matter move-
ment staged protests around the country to highlight and protest the disproportionate deaths
of Black people and members of other minority groups at the hands of police ocers. The
irony was not lost on the primary care provider community that Black Americans were at
300 PRIMARY CARE IN THE COVID-19 PANDEMIC
disproportionate risk from both police violence and the structural racism that led to dispro-
portionate Black infection rates and mortality from COVID-19
21
—from housing and lending
discrimination leading to crowded living conditions in multigenerational households; to
education, employment, and health care discrimination leading to people having less con-
dence in public health advice and less ability to access employment that facilitated sheltering
in place and working from home during peak incidence periods.
22
The history of community health centers explored in this volume reveals how consistently the
primary care provider community has been inspired by community movements and has be-
come necessary for the success of movements for civil rights and the mitigation of injustice.
As COVID-19 continues to have a disproportionate impact on disadvantaged communities, and
as we seek to address the underlying structural determinants of disease, we as primary care
providers have a responsibility to address structural barriers to good health in anticipation of
the next pandemic. This means overcoming concerns that ignoring political processes is the
same as being politically fair (a false equivalence between scientically minded and scien-
tically unsound policy proposals); scientic societies, including those publishing The New
England Journal of Medicine and Scientic American, endorsed political candidates and policies
for the rst time during COVID-19, given the dangers to public health posed by anti-science
politicians during the pandemic.
23,24
As we proceed with improving primary care practice into the future, the authors of this report
have put forward specic strategies to improve access to high-quality primary care, including
adoption of a diverse mobile workforce and telehealth technologies with greater accessibil-
ity features. The authors have emphasized that practice challenges can be addressed through
alternative nancing arrangements for practices. The authors have also revealed that care
strategies focused on vulnerable populations can be adapted to logistical challenges if provid-
ers focus on an integrated experience delivered across multiple diverse disciplines through the
same clinic infrastructure.
The perspectives in this report are, therefore, ultimately optimistic—demonstrating that the
resilience of populations to this pandemic and future ones can be bolstered by exible, coor-
dinated, and dedicated primary care providers. We proceed into 2021 with great uncertainty
about how vaccines will be allocated, who will benet or be left behind by the hoarding of
health care resources, and how the health of populations may recover from this pandemic.
We nevertheless hear the voices of these authors as exalting the perseverance of primary care
during this period of disparity and the desire to ensure that primary care’s service to popula-
tion health continues to deliver chronic disease prevention, infectious disease control, and a
broad suite of services ultimately driven by community needs.
PRIMARY CARE IN THE COVID-19 PANDEMIC 301
References
1. Coronavirus in the U.S.: latest map and case count.
New York Times. Last updated February 18, 2021.
Accessed February 18, 2021. https://www.nytimes.
com/interactive/2020/us/coronavirus-us-cases.html.
2. Mullard A. How COVID vaccines are being divvied
up around the world. Nature. November 30, 2020.
Accessed December 16, 2020. https://www.nature.
com/articles/d41586-020-03370-6.
3. Middleton J, Reintjes R, Lopes H. Meat plants—
a new front line in the COVID-19 pandemic. BMJ
2020;370:m2716. 10.1136/bmj.m2716.
4. Close RM, Stone MJ. Contact tracing for Native Amer-
icans in rural Arizona. N Engl J Med 2020;383(3):e15.
10.1056/NEJMc2023540.
5. Wang EA, Western B, Berwick DM. COVID-19,
decarceration, and the role of clinicians, health
systems, and payers: a report from the National Acad-
emy of Sciences, Engineering, and Medicine. JAMA
2020;324(22):2257-8. 10.1001/jama.2020.22109.
6. McGarry BE, Grabowski DC, Barnett ML. Severe
stafng and personal protective equipment short-
ages faced by nursing homes during the COVID-19
pandemic. Health Aff (Millwood) 2020;39(10):1812-21.
10.1377/hlthaff.2020.01269.
7. Humber L. Class, inequality and the COVID-19 pan-
demic. In: Lavalette M, Ioakimidis V, Ferguson I, eds.
Social work and the COVID-19 pandemic: interna-
tional insights. Bristol, UK: Bristol University Press,
2020:103-10. 10.2307/j.ctv1850gc4.19.
8. Kim H. The sociopolitical context of the COVID-19
response in South Korea. BMJ Glob Health
2020;5(5):e002714. 10.1136/bmjgh-2020-002714.
9. Bourdeaux M, Cameron B, Zittrain J. Testing is on the
brink of paralysis. That’s very bad news. New York
Times. July 16, 2020. Accessed December 16, 2020.
https://www.nytimes.com/2020/07/16/opinion/corona-
virus-testing-us.html.
10. Mervosh S, Fernandez M. Months into virus crisis,
U.S. cities still lack testing capacity. New York Times.
Last updated July 15, 2020. Accessed December
16, 2020. https://www.nytimes.com/2020/07/06/us/
coronavirus-test-shortage.html.
11. Weiland N. “Like a hand grasping”: Trump appointees
describe the crushing of the C.D.C. New York Times.
December 16, 2020. Accessed December 16, 2020.
https://www.nytimes.com/2020/12/16/us/politics/cdc-
trump.html.
12. Romer D, Jamieson KH. Conspiracy theories as
barriers to controlling the spread of COVID-19 in the
US. Soc Sci Med 2020;263:113356. 10.1016/j.socs-
cimed.2020.113356.
13. Bakouny Z, Paciotti M, Schmidt AL. Cancer screen-
ing tests and cancer diagnoses during the COVID-19
pandemic. JAMA Oncology 2021. 10.1001/jamaon-
col.2020.7600.
14. Kumar A, Nayar KR. COVID 19 and its mental
health consequences. J Ment Health 2020:1-2.
10.1080/09638237.2020.1757052.
15. Czeisler MÉ, Lane RI, Petrosky E, et al. Mental
health, substance use, and suicidal ideation dur-
ing the COVID-19 pandemic—United States,
June 24-30, 2020. MMWR Morb Mortal Wkly Rep
2020;69(32):1049-57. 10.15585/mmwr.mm6932a1.
16. Dominguez LW, Willis JS. COVID-19 and the case
for medical management and primary care. J Prim
Care Community Health 2020;11:2150132720965080.
10.1177/2150132720965080.
17. Kraef C, Juma P, Kallestrup P, Mucumbitsi J,
Ramaiya K, Yonga G. The COVID-19 pandemic
and non-communicable diseases—a wake-up
call for primary health care system strengthen-
ing in sub-Saharan Africa. J Prim Care Com-
munity Health 2020;11:2150132720946948.
10.1177/2150132720946948.
18. Lal A, Erondu NA, Heymann DL, Gitahi G, Yates
R. Fragmented health systems in COVID-19:
rectifying the misalignment between global
health security and universal health coverage.
Lancet 2021;397(10268):61-7. 10.1016/S0140-
6736(20)32228-5.
19. Nouri S, Khoong EC, Lyles CR, Karliner L. Addressing
equity in telemedicine for chronic disease manage-
ment during the COVID-19 pandemic. NEJM Catalyst.
May 4, 2020. Accessed December 16, 2020. https://
catalyst.nejm.org/doi/full/10.1056/CAT.20.0123.
20. Basu S, Phillips RS, Phillips R, Peterson LE,
Landon BE. Primary care practice nances in
the United States amid the COVID-19 pandemic.
Health Aff (Millwood) 2020;39(9):1605-14. 10.1377/
hlthaff.2020.00794.
21. Bassett MT. #BlackLivesMatter—a challenge to the
medical and public health communities. N Engl J Med
2015;372(12):1085-7. 10.1056/NEJMp1500529.
22. Richardson J, Mitchell BC, Meier HCS, Lynch E,
Edlebi J. Redlining and neighborhood health. National
Community Reinvestment Coalition. Accessed
December 16, 2020. https://ncrc.org/holc-health/.
23. Editors. Dying in a leadership vacuum. N Engl J Med
2020;383(15):1479-80. 10.1056/NEJMe2029812.
24. Editors. Scientic American endorses Joe Biden.
Scientic American. October 1, 2020. Accessed
December 16, 2020. https://www.scienticamerican.
com/article/scientic-american-endorses-joe-biden1/.
302 PRIMARY CARE IN THE COVID-19 PANDEMIC
About the Authors
Maya Alexandri is a fourth-year medical student at the Donald and Barbara Zucker
School of Medicine at Hofstra/Northwell. Her research has focused on occupational
medicine and the patient-centered medical home.
Jessica Alpert is a case writer for the Center for Primary Care at Harvard Medical
School. She has assisted in the editing, compilation, and organization of chapters for this
report. Jessica has also conducted research on primary care and oral health integration,
as well as high-value practices for successful primary care outcomes.
Katherine Gergen Barnett, MD, is an associate clinical professor of family medicine
at Boston University School of Medicine, vice chair of primary care innovation and
transformation, and program director in the Department of Family Medicine at Boston
Medical Center. Her research focuses on innovative models of care to address chronic
medical conditions, physician burnout, and engaging community partners in addressing
health disparities, trauma, and medical distrust in urban communities.
Sanjay Basu, MD, PhD, is the director of research at the Harvard Medical School Center
for Primary Care and vice president of population health and research at Collective
Health, an organization that helps people with complex health care needs to navigate
the health system. His research focuses on chronic disease management, primary care
payment reform, and social determinants of health.
Aaron Baum, PhD, is an assistant professor of health system design and global health
at Mount Sinai and an economist at the Arnhold Institute for Global Health. He studies
primary care quality, social determinants of health, and health care payment reform.
Mari Bentley, MD, MPH, is an assistant professor of family medicine at Boston University
School of Medicine/Boston Medical Center. She has a special interest in women’s
reproductive health, the care of immigrant populations, and palliative care.
Asaf Bitton, MD, MPH, is the executive director of Ariadne Labs and has led efforts
globally and nationally to transform and improve primary health care delivery systems. He
is a senior advisor to the Center for Medicare and Medicaid Innovation on primary care
policy, an assistant professor of medicine at the Division of General Medicine at Brigham
and Women’s Hospital, and an assistant professor of health care policy in the Department
of Health Care Policy at Harvard Medical School.
Adam E. Block, PhD, is an assistant professor of public health in the Division of Health
Policy and Management at the School of Health Sciences and Practice at New York
304 PRIMARY CARE IN THE COVID-19 PANDEMIC304 PRIMARY CARE IN THE COVID-19 PANDEMIC
Medical College. He is a health economist and his research activities focus on patient
selection of hospitals, design providers, hospitals, and insurance plans as well as
evaluations of medical technology.
Lauren Block, MD, MPH, is a primary care physician and associate professor of
medicine and science education at the Donald and Barbara Zucker School of Medicine
at Hofstra/Northwell. Her research interests include trainee wellness, interprofessional
education, and curriculum development.
Sean G. Boynes, DMD, MS, is the vice president of health improvement at the
DentaQuest Partnership for Oral Health Advancement. He is a dentist anesthesiologist
focusing on systems change and disruption.
Lydia Chang, MPH, is a researcher at the School of Public Health at the University of
Hong Kong. Her work has included research on health care system strategies to control
COVID-19 in East Asia.
Gerardo Reyes Chavez is a leader of the Coalition of Immokalee Workers. He is a
farmworker himself and has worked in the elds since age 11. He has worked closely with
consumer allies to organize national actions for the Fair Food Program.
Jonathan Cylus, PhD, is the head of the London Hubs of the European Observatory
on Health Systems and Policies, a senior research fellow at the London School of
Economics, and an honorary research fellow at the London School of Hygiene and
Tropical Medicine. His main research is on health systems, focusing primarily on health
nancing policy, health economics, and health system performance.
Olivia Dean, MPH, is a policy research senior analyst at the AARP Public Policy Institute
(PPI). Her work at PPI focuses on public health, health disparities, nutrition, private
coverage, and emerging health trends.
Cara Delaney, MD, MPH, is a fellow in complex family planning and an instructor in the
Department of Obstetrics and Gynecology at Boston Medical Center. Her work focuses on
challenges in women’s reproductive health access and delivery.
Jordan Downey, MPH, is a senior technical coordinator at Last Mile Health. Her work
has focused on research, monitoring, and evaluation of community health worker
interventions in rural communities, as well as health systems strengthening, community
health policy, and quality of community-based care.
PRIMARY CARE IN THE COVID-19 PANDEMIC 305 PRIMARY CARE IN THE COVID-19 PANDEMIC 305
David Duong, MD, MPH, is the director of the Harvard Medical School Program in Global
Primary Care and Social Change. His work has included health systems strengthening,
medical education, and primary care systems innovation.
Caswell A. Evans Jr., DDS, MPH, is the associate dean for prevention and public health
sciences at the University of Illinois at Chicago (UIC) College of Dentistry, and professor
in the UIC School of Public Health. He has been appointed to the Illinois State Board of
Health. Dr. Evans was the executive editor and project director for Oral Health in America:
A Report of the Surgeon General, released in May 2000, and subsequently directed the
development of the National Call to Action to Promote Oral Health, released in April 2003.
Prior to that, Dr. Evans was the director of public health programs and services for the
Los Angeles County Department of Health Services and served as director of the County
Division of the Seattle-King County Department of Public Health in Washington State.
Lynda Flowers, JD, MSN, RN, is a senior policy advisor at the AARP Public Policy
Institute (PPI). Her work at PPI focuses on Medicaid, dual eligibility, dual-eligible
demonstration projects, public health, prevention, health disparities, and health care
quality.
Chelsea Fosse, DMD, MPH, is the senior health policy analyst at the Health Policy
Institute of the American Dental Association. She is responsible for researching policy
changes that impact dentistry and oral health in the broader health care landscape,
particularly those related to Medicaid, Medicare, the Affordable Care Act, and other public
health issues.
Julie Frantsve-Hawley, PhD, is the director of analytics and evaluation at the
DentaQuest Partnership for Oral Health Advancement. In this role, she is responsible
for working with the team to create and implement a strategy to transform data into
knowledge that can be used to elevate oral health’s visibility and inform policy, care,
community, and nancing system decisions.
Patricia Fuentes is a student at Harvard University in the Department of History of
Science and the Global Health and Health Policy program. Her work has focused on
the intersection of medicine and public health, particularly in comprehensive health
campaigns among underserved communities.
Masafumi Funato, MD, is a board-certied Japanese family physician and MPH
candidate at Harvard T.H. Chan School of Public Health in Boston, Massachusetts. His
research interests lie in the areas of health systems and global health.
306 PRIMARY CARE IN THE COVID-19 PANDEMIC306 PRIMARY CARE IN THE COVID-19 PANDEMIC
Christine Haran, MA, is the communications director for the Milbank Memorial Fund and
has led the organization and layout of this volume. She has worked as a health journalist
and been published in The Hartford Courant, abcnews.com, and other outlets.
Masaya Higuchi, MD, MPH, is a geriatrician and palliative care physician at
Massachusetts General Hospital in Boston, Massachusetts. His clinical and research
interests include population health, quality improvement in health care for older adults,
and the role of palliative care in public health.
Lisa R. Hirschhorn, MD, MPH, is a professor of medical social sciences at Northwestern
University in the Feinberg School of Medicine and senior director of implementation and
improvement science at Last Mile Health. She has worked for three decades to study and
improve the effectiveness and quality of care in the United States and low- and middle-
income countries in HIV, primary care, maternal and child health, and noncommunicable
diseases.
Ann Hwang, MD, is a primary care physician and was the founding director of the Center
for Consumer Engagement in Health Innovation at Community Catalyst. She focuses on
improving care for people with complex health and social needs, through health system
partnership, state and federal policy, and community-led transformation.
Elaine Khoong, MD, MS, is a general internist and assistant professor of medicine at the
University of California, San Francisco, based at San Francisco General Hospital. Her
work has included leveraging informatics and implementation science to reduce health
inequities in safety-net populations.
June-Ho Kim, MD, MPH, is technical lead for the research and development work
under the Primary Health Care Performance Initiative at Ariadne Labs. He leads the
development of novel indicators and data collection tools to measure the delivery of
primary health care in low- and middle-income countries and disseminate insights to key
stakeholders and policymakers.
Christopher Koller is president of the Milbank Memorial Fund, a 114-year operating
foundation that improves population health by connecting leaders with the best
information and experience. Before joining the Fund, he served the state of Rhode
Island as the country’s rst health insurance commissioner, which introduced insurance
regulations to promote payment reform, primary care revitalization, and delivery system
transformation.
Bruce E. Landon, MD, MBA, MSc, is a professor of health care policy at Harvard
Medical School and a professor of medicine at the Beth Israel Deaconess Medical Center.
Dr. Landon studies tools that help translate macrolevel policies and incentives into
PRIMARY CARE IN THE COVID-19 PANDEMIC 307 PRIMARY CARE IN THE COVID-19 PANDEMIC 307
treatment strategies that lead to better care at lower cost, namely, strategies to promote
integrated care, payment incentives at both the organization and physician level, and
approaches to quality management and improvement.
Susan N. Landon, MSc, is a medical student at the New York University School of
Medicine. Her work includes research on health system performance assessment and
health system factors related to improved patient satisfaction, health care value, and
cancer survival.
E. John Ly, MD, is an internal medicine hospitalist at the University of California Los
Angeles Medical Center. He works with Last Mile Health, a nonprot nongovernmental
organization in Liberia that is delivering health care to remote villages through a network
of community health workers.
Courtney Lyles, PhD, is an associate professor in the University of California San
Francisco (UCSF) Division of General Internal Medicine at San Francisco General
Hospital and core faculty in the UCSF Center for Vulnerable Populations. Her research
focuses on harnessing digital health tools to reduce disparities in health and health care
outcomes for diverse populations.
Azeem Majeed, MD, FRCGP, is a professor of primary care and public health and head
of the Department of Primary Care and Public Health at Imperial College London. He
is a general practitioner in south London, and his research focuses on chronic disease
management, health policy, and the organization and delivery of primary care.
Riya Master is a research fellow at the Program in Global Primary Care and Social
Change at Harvard Medical School and a student at the University of California, Berkeley.
Her work focuses on migrant health, primary care systems, and health in conict zones.
Martin McKee, MD, DSc, is professor of European public health and medical director
at the London School of Hygiene and Tropical Medicine, and research director of the
European Observatory on Health Systems and Policies. His research focuses on the
health impacts of major social, political, and economic change in countries at all levels of
development.
Myechia Minter-Jordan, MD, MBA, is the president and CEO for the DentaQuest
Partnership for Oral Health Advancement and Catalyst Institute. She leads research and
grantmaking activities focused on improving oral health, integrating oral health and overall
health through medical/dental collaborations, moving toward a value-based payment
model, and guiding a growing research and data portfolio.
308 PRIMARY CARE IN THE COVID-19 PANDEMIC308 PRIMARY CARE IN THE COVID-19 PANDEMIC
Michelle Morse, MD, MPH, is cofounder of EqualHealth, an organization that builds
critical consciousness and collective action globally toward achieving health equity, and
assistant professor at Harvard Medical School. She was previously deputy chief medical
ofcer for Partners in Health (PIH), now serves on the PIH board of directors, and in
September 2019 began an RWJF health policy fellowship with the Ways and Means
Committee, Majority Staff, working on health equity priorities.
Caroline Murtagh works with Partners in Health. She has been supporting the COVID-19
response through the US Public Health Accompaniment Unit as a project manager
in Immokalee, Florida, a community that is home to many migrant farmworkers and
essential workers, in partnership with the local department of health, Federally Qualied
Health Centers, and community organizations such as the Coalition of Immokalee
Workers and Mision Peniel.
Alejandro Narváez, DDS, is director of dental services at Sea Mar Community Health
Center in Washington State. He oversees clinical practice and operations for all Sea Mar
dental clinics. Dr. Narváez earned a Doctor of Dental Surgery degree from the University
of Washington in 1982 and completed a course for general practitioners in orthodontics in
1998. He presently practices dentistry in the White Center and South Park clinics, with a
focus on children and limited orthodontics.
Kay Negishi, MD, is a hospitalist at Massachusetts General Hospital in Boston,
Massachusetts. She is passionate about teaching and using point-of-care ultrasound in
internal medicine, both domestically and abroad.
Cody Nolan, MD, is a resident physician in internal medicine and global health equity
at Brigham and Women’s Hospital. During the COVID-19 pandemic, he has served as a
clinician on the front lines and worked with the Holyoke Board of Health to implement a
community serosurvey in western Massachusetts. His prior work has focused on refugee
health and cardiovascular disease among people living with HIV in East Africa.
Kei Ouichi, MD, MPH, is an assistant professor of emergency medicine at Brigham
and Women’s Hospital. His research focuses on the quality of care for older adults with
serious, life-limiting illness.
Kathleen Page, MD, is an associate professor in the Division of Infectious Diseases at
Johns Hopkins University School of Medicine. She is the founding codirector of Centro
SOL and the medical director of The Access Partnership at Johns Hopkins, which
provides care to uninsured patients with nancial need. Her research focuses on migrant
health, health disparities, and implementation science.
PRIMARY CARE IN THE COVID-19 PANDEMIC 309 PRIMARY CARE IN THE COVID-19 PANDEMIC 309
Daniel Palazuelos, MD, MPH, is a clinician-educator hospitalist at Brigham and Women’s
Hospital, assistant professor at Harvard Medical School, and director of community health
systems at Partners in Health (PIH). His work has included the study and implementation
of health system improvements in rural and low-income communities globally, rst as the
cofounder of PIH-Mexico (locally known as Compañeros En Salud) and most recently as
the lead technical advisor in the PIH Public Health Accompaniment Unit responding to the
COVID-19 pandemic affecting migrant workers based in Immokalee, Florida.
Raj Panjabi, MD, is CEO of Last Mile Health and assistant professor of medicine
at Harvard Medical School and the Division of Global Health Equity at Brigham and
Women’s Hospital. In 2007, he cofounded Last Mile Health, a nongovernmental
organization that delivers health care in remote communities, and serves as technical
advisor to former Liberian president Ellen Johnson Sirleaf in her role as cochair of the
Independent Panel for Pandemic Preparedness and Response at the World Health
Organization.
Russell S. Phillips, MD, is director of the Center for Primary Care and the William
Applebaum Professor of Medicine and professor of global health and social medicine
at Harvard Medical School. He is a general internist at Beth Israel Deaconess Medical
Center and has been a leader in innovation in practice and payment in primary care,
implementing new care models for patients with chronic illness and testing the impact of
global payment on value.
Ramya Pinnamaneni, MBBS, MPH, is a research fellow at the Harvard T.H. Chan
School of Public Health. Her research focuses on building public agenda and improving
public health practice in the elds of primary health care, maternal-child health, and
nutrition in India.
Johanan Ponniah is team lead for the COVID-19 international research project in
Singapore. His work has collected and systematized national data on the economic
impact of COVID-19, incorporating data from over 100 countries.
Lisa Puglisi, MD, is an assistant professor of medicine at Yale University, where she
practices primary care and addiction medicine. She is the director of Transitions Clinic–
New Haven, a multidisciplinary clinic that is part of a national network of programs that
focus on care of individuals who are returning to the community from incarceration.
Selina Rajan, MFPH, is a public health specialist registrar and honorary research fellow
in the Department of Health Services Research and Policy at the London School of
Hygiene and Tropical Medicine. She has a particular focus on the interaction between
noncommunicable diseases and mental disorders and health systems.
Neha Rana is a research fellow at the Program in Global Primary Care and Social
Change at Harvard Medical School and a student at the University of Virginia. Her work
focuses on disparities in health care access, primary care systems, and refugee health.
310 PRIMARY CARE IN THE COVID-19 PANDEMIC310 PRIMARY CARE IN THE COVID-19 PANDEMIC
Dan Schwarz, MD, MPH, is the director of primary health care at Ariadne Labs, an expert
lead for the Program in Global Primary Care, and previously chief medical ofcer for
Possible Health, which built health facilities to serve over 500,000 people in Nepal. His
work has focused on global primary care delivery.
Hugh Silk, MD, MPH, is a professor in the Department of Family Medicine and
Community Health at the University of Massachusetts Medical School. He has an interest
in medical-dental integration and is co-PI for the Center for Integration of Primary Care
and Oral Health (CIPCOH).
Lisa Simon, MD, DMD, is a fellow in oral health and medicine integration at the Harvard
School of Dental Medicine and a resident in the Internal Medicine Residency program at
Brigham and Women’s Hospital. Her work focuses on the integration of oral health and
medicine and its impact on health equity.
Patrick D. Smith, DMD, MPH, is an assistant professor in the Division of Prevention
and Public Health Sciences at the University of Illinois at Chicago. His interest is to
develop dental school curricula and research that broadens dentists’ perspectives on
issues affecting population oral health, while developing solutions to address oral health
inequities.
Marion Subah, CNM, CRN, a reproductive, maternal newborn, and public health
systems strengthening specialist, is Last Mile Health’s country director in Liberia, where
she manages the organization’s partnership with the Ministry of Health to scale and
sustain the National Community Health Assistant Program. In this role, she leads the
organization’s technical assistance to the government, manages the implementation of
the program across three counties, and oversees a staff of 180 people.
Kaeng Takahashi an implementation project assistant at Ariadne Labs, where she is
responsible for the technical management of Ariadne Labs’ Community of Practice, an
online community where specialists and clinicians learn and share resources and lessons
learned from integrating Ariadne Labs innovations in their home institutions. During
the COVID-19 pandemic, she was a member of the research team studying Japan’s
response.
Kelly Treder, MD, MPH, is an instructor of obstetrics and gynecology at the Boston
University School of Medicine. She is also a junior fellow at the Society of Family
Planning and a member of the American College of Obstetricians and Gynecologists.
K. “Vish” Viswanath, PhD, is Lee Kum Kee Professor of Health Communication in
the Department of Social and Behavioral Sciences at the Harvard T.H. Chan School of
Public Health and in the McGraw/Patterson Center for Population Sciences at the Dana-
PRIMARY CARE IN THE COVID-19 PANDEMIC 311 PRIMARY CARE IN THE COVID-19 PANDEMIC 311
Farber Cancer Institute. His work, drawing from literature in communication science,
social epidemiology, and social and health behavior sciences, focuses on translational
communication science to inuence public health policy and practice with a particular
focus on health equity.
Emily Wang, MD, is an associate professor in the Yale School of Medicine, directs
the SEICHE Center for Health and Justice, and leads the Health Justice Lab research
program, which studies how incarceration inuences chronic health conditions. She is
cofounder of the Transitions Clinic Network, a consortium of 40 community health centers
nationwide dedicated to caring for individuals recently released from correctional facilities
by employing community health workers with histories of incarceration.
Ami Waters, MD, is an internal medicine-pediatrics physician and hospitalist at the
University of Texas Southwestern Medical Center. She is co-medical director of Last Mile
Health, a nongovernmental organization dedicated to ensuring health access to those in
remote and rural communities.
Taylor Weilnau is a member of the research team at the Center for Primary Care at
Harvard Medical School. Her work has included research on improving capacity for
primary care teams in community health centers, oral health integration into primary care,
and high-risk complications of pregnancy such as preeclampsia and preterm birth.
Bram Wispelwey, MD, MPH, MS, is a hospitalist at Brigham and Women’s Hospital and
cofounder and chief strategist of Health for Palestine, a community-organizing initiative in
Palestinian refugee camps that seeks to maximize wellness and address health barriers
via social accompaniment and creative integration with existing facilities. He is a senior
fellow at the Atlantic Fellows for Health Equity and senior project lead for Partners in
Health’s US Public Health Accompaniment Unit. His work focuses on anti-racist strategies
to address hospital admission inequities, community health worker impact, and settler
colonial determinants of health.
Elisabeth Woodhams, MD, MSc, is an assistant professor of obstetrics and gynecology
at Boston University School of Medicine and division director of family planning and
contraception, associate director of the Obstetrics and Gynecology Residency Program,
and assistant director of the Fellowship in Family Planning, all at Boston Medical Center.
Her work has centered on the intersection of substance use disorder and reproductive
health, contraceptive decision-making, improving postpartum contraception care, and
abortion service delivery improvement.
312 PRIMARY CARE IN THE COVID-19 PANDEMIC312 PRIMARY CARE IN THE COVID-19 PANDEMIC

Sponsored by the CareQuest Institute for Oral Health and the Milbank Memorial Fund
